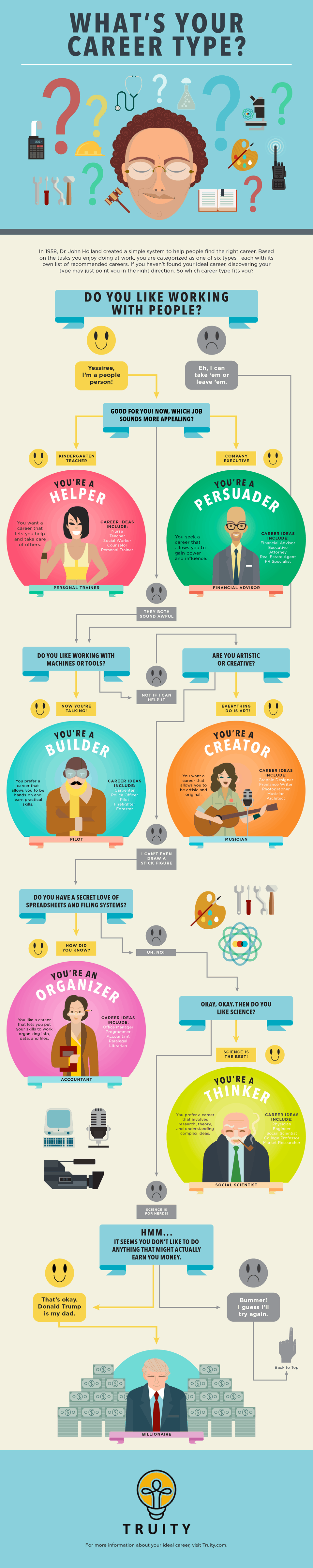
Child rolling eyes tic
Tics Are Uncontrollable—and Completely Normal
Believe it or not, eye rolling isn’t always a sign of disrespect. It’s one of the most common tics that children can develop. Other common tics are blinking, coughing and throat clearing.
“A tic is an uncontrollable movement or noise,” says Steven Trau, MD, a UNC Health child neurologist and director of the UNC Clinic for Tourette Syndrome and Tic Disorders. “It’s very common—about 25 percent of children have tics.”
Tics are almost never harmful. However, they can make a child a target of bullying or teasing. Tics may hurt a child’s self-esteem and can sometimes cause depression. In addition, some motor tics can be physically painful.
“If a tic is actively bothersome to a child, then it’s time to talk to a doctor,” Dr. Trau says. “Otherwise, the best thing to do is ignore it.”
What Causes Tics?
The exact cause is not known, although tics seem to run in families.
“No one has found a gene connected to tics,” Dr. Trau says, “but if a parent has tics, there’s a 50 percent chance the child will, too.”
Some experts think environmental factors or inflammation can contribute to the onset of tics, which typically occurs between ages 4 and 6 but can happen earlier or later, Dr. Trau says.
“I explain to patients that there’s a structure in the brain that’s designed to keep some types of movements from happening,” he says. “When it’s not working quite as well, tics can come out.”
About 50 to 70 percent of the time, children with tic disorders also have attention deficit hyperactivity disorder (ADHD), obsessive-compulsive disorder (OCD) or anxiety.
“The circuits that control movement interact with the circuits in the brain that control and regulate emotions,” Dr. Trau says. “When they overlap a bit too much or too strongly, tics and psychological issues can come together.”
Tic Disorders and Tourette Syndrome
Tourette syndrome is the term used when someone has both motor and vocal tics that have lasted for more than a year. It is not an indication of severity.
It is not an indication of severity.
Unfortunately, the syndrome has become the butt of jokes.
“Tourette syndrome has gotten a really bad reputation from TV and movies,” Dr. Trau says, “but rarely does someone with Tourette syndrome have coprolalia, or uncontrolled swearing. That occurs in fewer than 10 percent of children with Tourette syndrome.”
Boys are three times more likely than girls to have tic disorders and Tourette syndrome.
Treatment for Tic Disorders
Most of the time, no treatment is needed. In about a third of children, the tics go away. In another third, the tics become less frequent, or they come and go. For the remaining third, the condition may stay the same or become more pronounced.
Behavior modification tactics can help children recognize the uncomfortable feeling or urge to tic and channel that urge into a non-tic activity.
An ideal way to learn these tactics is through comprehensive behavioral intervention for tics, or CBIT. Unfortunately, COVID-19 precautions have delayed training for professionals, so CBIT availability is limited right now. However, there are online resources that can help families, Dr. Trau says, including materials from the Tourette Association of America.
Unfortunately, COVID-19 precautions have delayed training for professionals, so CBIT availability is limited right now. However, there are online resources that can help families, Dr. Trau says, including materials from the Tourette Association of America.
Several medications can help lessen the number or severity of tics, although none of them cure the disorder.
“In many patients, the tics themselves aren’t actually severe enough to cause issues,” Dr. Trau says. “However, a patient’s ADHD, OCD or anxiety can be quite severe. It’s very important in taking care of these patients to evaluate and help address both the tics and non-tic symptoms.”
Communicating About Tics to Others
Some tics cause physical pain. They can also cause emotional or psychological distress if the child is embarrassed or treated poorly by others.
Often, the best thing teachers, friends and parents can do is ignore the tics. That may be easier, though, if the adults and other kids understand the condition.
“Most teachers are wonderful,” Dr. Trau says, “but I know of at least one case where a teacher sent a child to the principal’s office for rolling his eyes. She thought he was being disrespectful, but he couldn’t control it.”
Dr. Trau recommends that parents send a letter to the child’s teachers and other school officials explaining the child’s diagnosis. Parents also can help their child find words to explain the condition to their friends, such as, “I have a medical condition, and I cannot control my tics. We can ignore them and keep playing.”
“You can even make a wallet-sized card that the kid can carry around if the child gets tired of explaining,” Dr. Trau says.
Ready-made cards can be downloaded from the Tourette Association’s website, explaining, “Why do I act this way? Because I can’t control it. … I am grateful for your understanding and empathy.”
The Bottom Line: Only Act if the Child Is Struggling
“It’s all about the kids and how they are doing,” Dr. Trau says. “If the child is not affected, then ignore it. If things get worse or the tics start bothering the child, then contact your pediatrician.”
Trau says. “If the child is not affected, then ignore it. If things get worse or the tics start bothering the child, then contact your pediatrician.”
Pediatricians may refer patients to the UNC Clinic for Tourette Syndrome and Tic Disorders for evaluation and, if appropriate, an individualized plan that might include CBIT, medications and addressing co-existing conditions.
Does your child have tics that interfere with his or her quality of life? Talk to your pediatrician. If you don’t have a pediatrician, find one near you.
Tics and Tourette’s Syndrome - Minneapolis Clinic of Neurology
Though involuntary movements in children are not uncommon, they can arouse a great deal of anxiety in parents, teachers and the child. Tics are a type of involuntary motor movements, which typically involve the head and neck; however, tics can also include a variety of noises and verbal expressions. Both motor and verbal tics can be variable in type and frequency, and they can change from one type to another, sometimes on a daily basis. Tics may run in families.
Tics may run in families.
Tics are abnormal involuntary movements or sounds. We all have habits that could be called tics, but they occur only rarely and briefly. When these motor or verbal habits become excessive, a tic disorder may be present. Tics come and go, sometimes on a daily basis.
Tics – Different Types
- Motor Tics
- Eye blinking (this is probably one of the most common tics seen)
- Eye rolling (eyes may “dart” in various directions)
- Facial grimacing (nose wiggles, mouth movements)
- Hands (may “comb” hair repeatedly; bring hands to nose to “sniff”)
- Vocal Tics
- Throat clearing (very common)
- Intermittent “cough”, in absence of any illness
- “Sniffing” without signs of a cold
- Guttural sounds
- Humming
- Rarely, saying actual words or swearing
Tics usually begin over a period of time and may be ignored at first when they are very infrequent and mild. Rarely, they may start abruptly. In these circumstances, some acute change in the child’s health, such as a strep infection, might be noted. This may be of importance in rare cases due to an autoimmune reaction to common strep throat. Research studies are still active in this area.
In these circumstances, some acute change in the child’s health, such as a strep infection, might be noted. This may be of importance in rare cases due to an autoimmune reaction to common strep throat. Research studies are still active in this area.
In most children, no precipitating factors can be well defined. On occasion, a medication (such as stimulant medication for ADHD, or excessive use of caffeine products) may be implicated, which leads to an exacerbation of, but does not cause, the underlying tic disorder.
The diagnosis of Tourette’s Syndrome can be made when a child has changing motor and verbal tics that have been present for over a year (DSM-IV criteria). The diagnosis of this syndrome is still based upon the presence of clinical symptoms, but, in the future, there may be more specific genetic testing available. In many families, there is a positive history of tics in other relatives, or the presence of obsessive-compulsive disorder. The relationship of ADHD to Tourette’s syndrome is still debated, although many children have both problems. For many children with isolated tics, the diagnosis of Chronic Tic Disorder may be more appropriate than Tourette’s syndrome, especially when the family history is negative and the child has no other behavioral problems.
For many children with isolated tics, the diagnosis of Chronic Tic Disorder may be more appropriate than Tourette’s syndrome, especially when the family history is negative and the child has no other behavioral problems.
Many children with tics also have other behavior disorders, with ADHD and obsessive-compulsive disorder being most common. Some will develop anxiety symptoms or depression. These other problems must be considered in the child with social and academic difficulties.
Many children with tics can be managed without medication. Parents, teachers and peers need to be understanding and supportive. Avoiding negative feedback is very important.
Some children seem to have more tics when under stress. There are ways to deal with the stress level without beginning medication. Diet may not matter except in some who need to avoid caffeine products. Regular sleep habits may be important in some cases.
If tics become excessive and cause increasing problems at home and/or school, a medication trial may be considered. Frequent, loud verbal tics are difficult to ignore and may need treatment, while a constant head jerking can lead, on occasion, to neck discomfort and headache. If medication is used, it should be used in the lowest effective dose. After a period of decreased tics, one needs to consider if the drug can be slowly decreased or discontinued. Many drugs are available and they all have potential side effects. Generally, it is best to try those with the least severe side effects first.
Frequent, loud verbal tics are difficult to ignore and may need treatment, while a constant head jerking can lead, on occasion, to neck discomfort and headache. If medication is used, it should be used in the lowest effective dose. After a period of decreased tics, one needs to consider if the drug can be slowly decreased or discontinued. Many drugs are available and they all have potential side effects. Generally, it is best to try those with the least severe side effects first.
Many children will respond favorably to Clonidine, a blood pressure drug that must be increased very slowly to avoid sedation. Higher doses of Clonidine may also lower blood pressure and some rare cardiac effects have been reported. It can, however, be used effectively in small doses in many children, although usually it lasts only part of the day. Another variant, Tenex, may be helpful when Clonidine is not tolerated. Orap, another drug that is useful at times, is longer acting than Clonidine; however, it has potential side effects.
Haldol, the classical medication for Tourette’s syndrome, has the most side effects, especially with adverse behavioral changes or sedation; however, in small doses and increased slowly, it can be quite effective and well tolerated by most children. The medication should be discontinued periodically. Some physicians will try to use Risperidal, which in one of the “next-generations” of Haldol.
There is an ongoing search for more specific drugs with fewer side effects to treat tic disorders.
For further information about Tics and Tourette’s Syndrome, click on the following link:
- National Tourette’s Syndrome Association
Tics in children / Children's neurology / Articles about health / Articles and encyclopedia / madez.ru
Tics, or hyperkinesis, are repeated unexpected short stereotyped movements or statements that are outwardly similar to voluntary actions. A characteristic feature of tics is their involuntary nature.
- Types of ticks
- Motor tics - blinking, rolling eyes, rolling eyes, fixing gaze, raising eyebrows, furrowing eyebrows, twitching cheeks, licking, shrugging shoulders, twitching hands, snapping fingers.
Allocate simple and complex motor tics.
Simple tics capture one muscle group, mainly mimic muscles, rapid blinking, squinting, sniffing, lip stretching, frowning predominate.
Complex motor tics resemble coordinated actions, the implementation of which includes several muscle groups. Complex motor tics include grimacing, jumping up and down, touching body parts, people or objects, sniffing objects, throwing the head back. Other manifestations of complex motor tics are echopraxia (imitation of other people's gestures and movements) and copropraxia (offensive gestures).
- Vocal tics are also divided into simple and complex.

Simple vocal tics include the reproduction of individual, mostly low sounds: coughing, "clearing the throat", grunting, noisy breathing, sniffing. Less common are such high-pitched sounds as “i”, “a”, “u-u”, “uf”, “af”, “ay”, squeal and whistle.
Complex vocal tics are manifested in the pronunciation of words, phrases and sentences that have a certain meaning and include echolalia (repetition of sounds, words spoken by others), palilalia (repetition of one's own words or part of words), coprolalia (pronunciation of aggressive, offensive or socially unacceptable words and phrases).
- Generalized tic (Tourette syndrome). It is manifested by a combination of common motor and vocal simple and complex tics.
Causes of tics
The mechanism of tics is complex, and many of the causes are not fully understood. But it is known that an important role is played by genetic, immune mechanisms, perinatal pathology (entanglement of the umbilical cord around the neck, severe neonatal jaundice, caesarean section, delivery with forceps), as well as psychosocial factors (sudden fright, school adaptation stress, "tics of the first of September" , separation from one of the parents, after a long mental overload).
Tics often occur in children with pre-existing central nervous system (CNS) disorders such as attention deficit hyperactivity disorder (ADHD), cerebrovascular disorder, and anxiety disorders including generalized anxiety disorder, specific phobias, and obsessive-compulsive disorder .
Diagnostics
Children with tics should be consulted by specialists:
- neurologist
- psychotherapist
Treatment
Treatment of tics in children is complex and is best done on an outpatient basis, as hospitalization may exacerbate tics.
1. For the correction of tics, it is recommended to eliminate provoking factors first. Of course, it is necessary to observe the sleep and nutrition regimen, the adequacy of physical activity.
2. Family psychotherapy, exclusion of traumatic situations.
3. Psychological correction (individual and group lessons).
4. Drug treatment. Medications are prescribed by a neurologist depending on the clinical picture and additional examination data.
Medications are prescribed by a neurologist depending on the clinical picture and additional examination data.
- Tips for parents
- Do not focus on tics, pull the child, or force him to restrain hyperkinesis.
- Do not show parents your emotional reaction to the appearance of tics in a child.
- Create a positive emotional environment.
- Restrict TV viewing, computer games for 1 month.
Prognosis and prevention
The prognosis for children who have tics at the age of 6-8 years is favorable (i.e. tics disappear without a trace). The early onset of tics (3-6 years) is typical for their long course, up to adolescence.
If tics appear before age 3, they are usually a symptom of some serious illness (eg schizophrenia, autism, brain tumor, etc.). In these cases, a thorough examination of the child is required.
Belonogova Elena Georgievna
causes and treatment of nervous tics of the eye, lips and face
Nervous tics are, in fact, an involuntary contraction of muscles on the face of a stereotyped type, less often a muscle of the neck. This deviation is expressed in twitching in small attacks. Everyone has experienced uncontrollable muscle twitching at least once in their life. Such a stereotypical reduction of the eyelid occurs in case of severe mental or emotional overload.
This deviation is expressed in twitching in small attacks. Everyone has experienced uncontrollable muscle twitching at least once in their life. Such a stereotypical reduction of the eyelid occurs in case of severe mental or emotional overload.
Nervous tics of the eye or twitching of the facial muscles are more common than others. In childhood, the risk group for the appearance of a nervous tic mainly includes boys. In this case, drug treatment is not required for either children or adults. However, in the case of the transition of a tick to the stage of a permanent phenomenon, it is necessary to begin treatment.
Causes
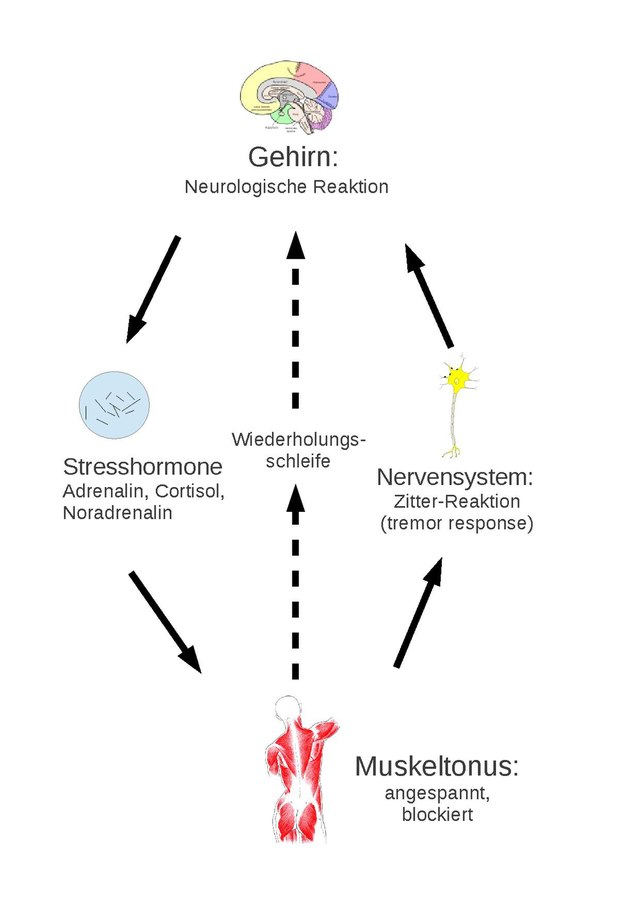
The main cause of nervous tics is a malfunction of the nervous system. Dysfunction involves sending inadequate impulses from the brain to the muscles, resulting in an uncontrolled, rapid contraction. At the same time, a person is not able to stop such a twitching by a strong-willed decision.
Nervous tics are classified according to their causes:
- primary or psychogenic, idiopathic,
- secondary or symptomatic,
- genetic or hereditary - damage to the structure of the cells of the nervous system.

Childhood causes of the development of primary nervous tic of the eye:
- trauma of the psycho-emotional type, as a rule, is of an acute single character;
- hyperactivity or lack of attention;
- fears and phobias;
- neuroses and anxiety.
Primary causes of eye twitching in adults:
- constant stress and overexertion;
- mobility of the nervous system;
- chronic fatigue syndrome.
At the same time, this type of tick, if the root cause is excluded, goes away on its own.
Causes of a nervous tic of a secondary nature:
- brain infection;
- carbon monoxide poisoning;
- taking pharmaceuticals - psychotropic or anticonvulsant;
- violation of the blood circulation of the brain - stroke or atherosclerosis;
- renal or hepatic insufficiency;
- mental disorders - autism or schizophrenia and others;
- trigeminal neuralgia;
- birth injuries;
- formation of tumors in the brain;
- the presence of VSD.

In childhood, the habit of making monotonous muscle movements is of great importance to alleviate the state of a particular disease. Subsequently, they begin to repeat themselves spontaneously.
Genetic Tourette's disease causes nervous tics mainly in children, against the background of the following factors:
- autoimmune disorders;
- stress;
- bad ecology;
- infection with bacteria such as streptococci and staphylococci;
- lack of magnesium and pyridoxine.
Symptoms
The most important symptom of a nervous tic of the eye is considered to be voluntary uncontrolled contraction of the muscles. Moreover, the more efforts a person makes to stop an attack of contractions, the stronger and more often the twitching begins. It is worth noting that there are a number of strong personalities that can delay the onset of an attack of twitching and weaken the degree of muscle contraction.
Most often, symptoms appear after serious physical or mental stress against the background of overwork or deep conflict, as well as after psycho-emotional trauma.
External signs of muscle contraction are always visible to people around and are localized in the zone of formation of a nervous tic:
- facial - twitching of the eye, eyelid, twitching of the eyebrow or nose, frequent blinking, self-opening of the mouth or movement of the lips;
- head or neck - mechanical head turns or impulsive nodding;
- voice - pronunciation of an unrelated set of words, syllables, sounds or grunts, howling and barking cough;
- body - reflex movement of the abdominals, diaphragm, trembling of the muscles of the pelvis or buttocks; 90,005 limbs - uncontrollable clapping of hands or stomping and bouncing of feet;
- vocal - smacking, foul language, shouting at emotions and coughing.
In general, all nervous tics are noticed by others, while the patient himself rarely focuses on them. The development of the process of strengthening the manner of tic takes place over a rather long period of time.
The hallmark of any tic is the lack of control by the patient himself. Symptoms come out at the moment of strong excitement or extreme fatigue. Very rarely, these states occur against the background of relaxation.
Nerve contractions do not affect the performance and functioning of the nervous system and mental abilities of the patient. They are more likely to accompany mental and emotional disorders.
The initial stage of a nervous tic is an increase in tension, which a person consciously wants to release. Then comes the moment of muscle contractions, which is accompanied by relief or a feeling similar to itching.
Complicated twitches are outwardly similar to convulsions and are extremely rare.
When a doctor's appointment is needed
In the event that attacks of a nervous tic become more frequent or cause discomfort, ranging from the ridicule of others to the internal states of the body, a person needs the help of a specialist. As a rule, these areas are diagnosed by neurologists or psychologists and psychotherapists.
Diagnosis
As part of the diagnosis, a distinction is made between nervous tics and motor acts of a pathological status, such as chorea, dystonia, and others. At the same time, differential diagnosis along the way finds out the cause of the development of tic muscle contractions, which allows you to build an effective treatment regimen.
Diagnosis of tics practically does not use laboratory tests, except in a number of rare clinical diseases of a hereditary type. In this case, CT and MRI, EEG, blood tests for genetic mutations and hormone levels can be performed. Urine and blood tests can show drug intoxication, as well as kidney and liver failure.
To collect anamnesis, neurologists conduct a thorough survey, during which they identify:
- the time and circumstances of the attack;
- attack duration;
- presence of chronic diseases;
- the ability to control the onset of an attack;
- presence of tics in other family members.

Next, there is an assessment of the adequacy of the functioning of motor and sensory activity, the degree of muscle tone and the intensity of reflexes.
Imaging may include an ionogram for electrolytes in the blood, a complete blood count for inflammation and infection, and stool for helminths.
Treatment
Treatment is based on eliminating the root cause of the tic by minimizing exposure to the irritant. Sometimes you just need to give your body enough rest.
There are special exercises for stopping an attack of a nervous tic:
- relaxation with eyes closed for 15 minutes;
- cotton pads moistened with warm water should be applied to the eyelids;
- open your eyes wide, and then close them for a couple of seconds;
- slight pressure on the middle of the superciliary arch of the twitching eye;
- intensive 15-second blinking and relaxation with closed eyes for two minutes.
Medications are used from the group of relaxing drugs in the primary form, the secondary form is anti-anxiety drugs.