Disruptive mood dysregulation disorder diagnosis criteria
DMDD Diagnosis: DSM 5 Criteria for Disruptive Mood Dysregulation Disorder
Jenna Jarrold
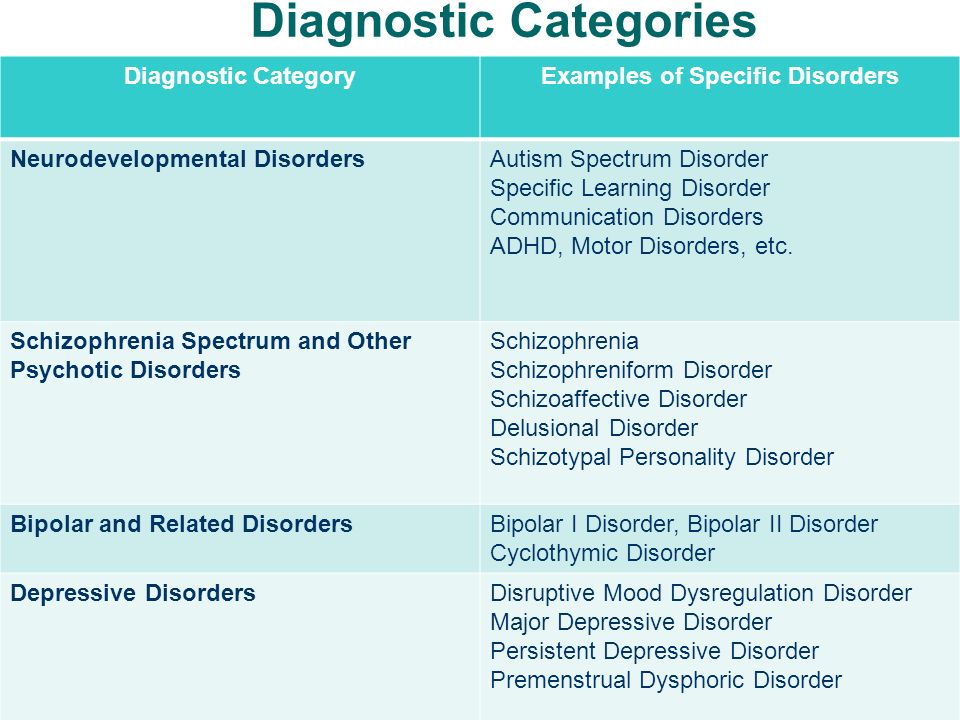
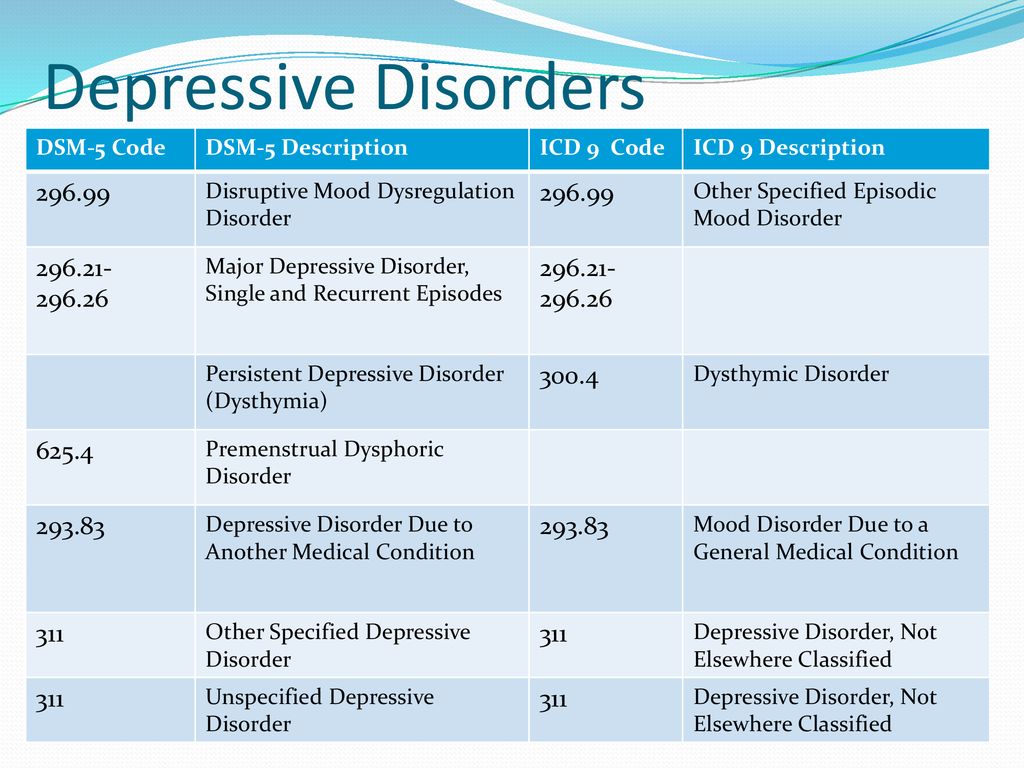
Assigning the disruptive mood dysregulation disorder (DMDD) diagnosis in a child has not always been an option. In fact, this is a relatively new diagnosis, added to the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) in 2013.
The addition of DMDD to the DSM-5 was, in part, to address the over-diagnosis and overtreatment of bipolar disorder in children. Since disruptive mood dysregulation disorder is a newly recognized mental health disorder, there are no specific assessment tools used for diagnosis. Thus, even for trained medical and mental health professionals, it can be difficult to determine whether a child should be assigned a DMDD diagnosis or that of another psychiatric disorder. Yet, the difficulty in diagnosing is not only due to the lack of assessment tools; disruptive mood dysregulation disorder symptoms can look similar to those found in other psychiatric disorders in children (i.
e. – depression, posttraumatic stress disorder, oppositional defiant disorder, bipolar disorder, etc.) Nonetheless, an accurate diagnosis is possible, as there are specific disruptive mood dysregulation disorder criteria a child must meet to receive the DMDD diagnosis.
DMDD Diagnosis: Criteria
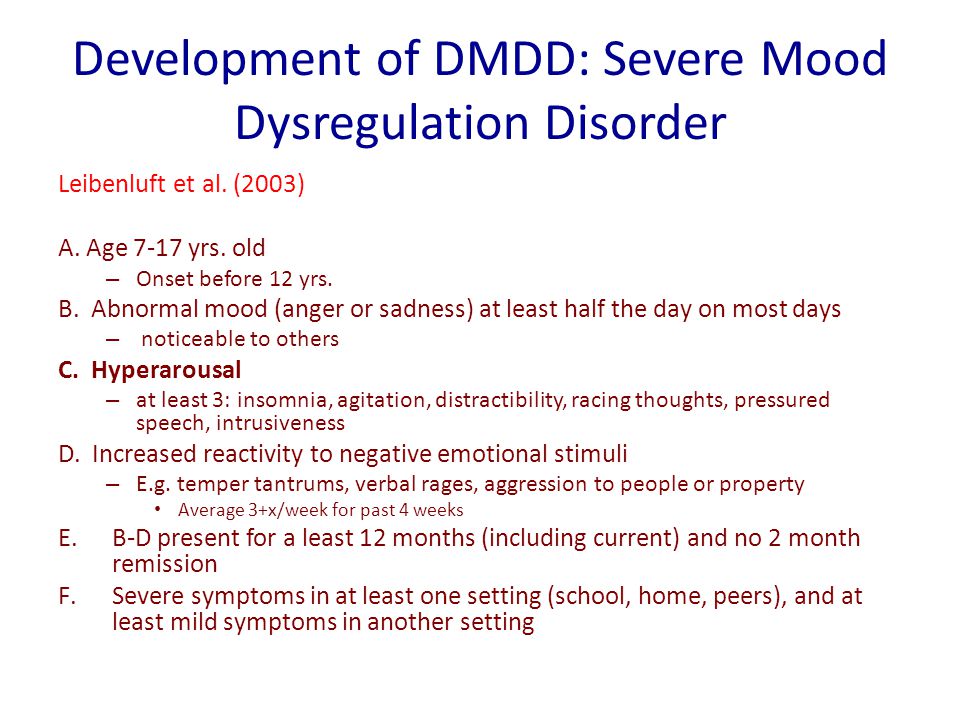
In general, a clinician considering disruptive mood dysregulation disorder will look for severe temper outbursts and consistent irritability and anger in between the outbursts. Prior to making a diagnosis of DMDD, the clinician will rule out any other possible causes or contributing factors to the presenting DMDD symptoms. The diagnostic criteria a child must meet in order to receive a DMDD diagnosis is:
- Recurrent and severe temper tantrums or outbursts
- The tantrums/outbursts may be expressed verbally and/or behaviorally (physical aggression towards other people or property).
- The tantrums/outbursts are considered out of proportion (in duration and intensity) to the situation or triggering event
- The tantrums/outbursts are inconsistent with the child’s developmental level
- The tantrums/outbursts occur three or more times per week, on average
- Persistent irritability or anger
- The irritable/angry mood occurs nearly every day, for most of the day
- The irritable/angry mood is observable by others (peers, parents, teachers, etc.
 )
)
- The recurrent temper tantrums and persistent irritability/anger have been present for 12 months or longer
- Throughout the 12 months of ongoing temper tantrums and irritability/anger, the child has not had a period lasting 3 or more consecutive months without all of the diagnostic symptoms.
- Symptoms are present in at least two of three primary settings, either home, school, or in social situations.
- Symptoms are severe in at least one of the three primary settings.
- DMDD diagnosis should not be assigned before age 6 or after age 18.
- The age of onset of disruptive mood dysregulation disorder is before 10 years old.
- The symptoms are not better explained by another mental illness, such as depression, posttraumatic stress disorder, or autism (DMDD and Autism: How Are the Two Related?).
Disruptive Mood Dysregulation Disorder Controversy
The addition of DMDD to the DSM-5 is helpful in many ways, but it comes with controversy as well.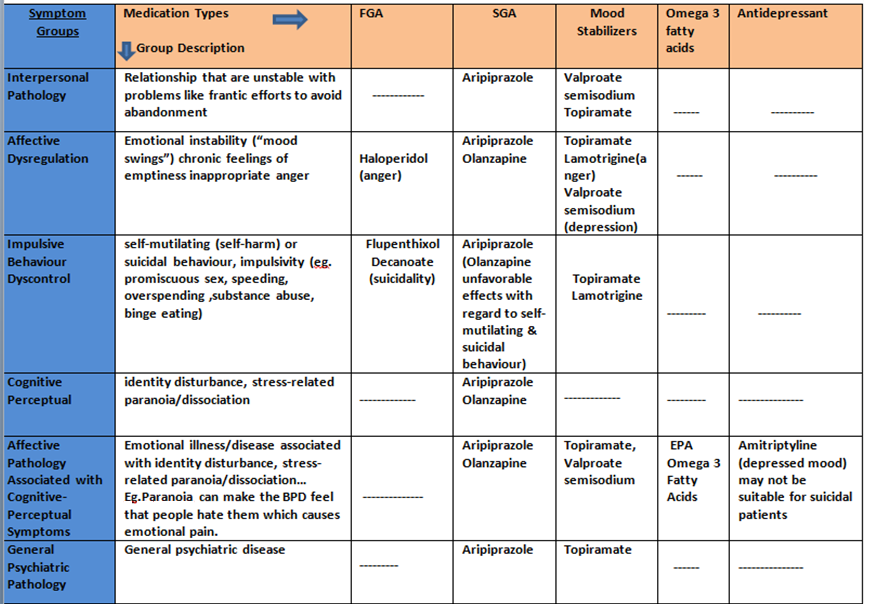 Many are concerned this new mental health disorder will lower the threshold for diagnosing children who are perhaps just going through a difficult time (What are the Causes of DMDD?). There is fear DMDD will be over-diagnosed (as was previously the case with bipolar disorder), as tantrums and bad moods are not uncommon in children. Yet being inaccurately diagnosed with DMDD prevents professionals from identifying what might truly be going on with a child.
Many are concerned this new mental health disorder will lower the threshold for diagnosing children who are perhaps just going through a difficult time (What are the Causes of DMDD?). There is fear DMDD will be over-diagnosed (as was previously the case with bipolar disorder), as tantrums and bad moods are not uncommon in children. Yet being inaccurately diagnosed with DMDD prevents professionals from identifying what might truly be going on with a child.
article references
APA Reference
Jarrold, J. (2018, July 22). DMDD Diagnosis: DSM 5 Criteria for Disruptive Mood Dysregulation Disorder, HealthyPlace. Retrieved on 2023, April 21 from https://www.healthyplace.com/parenting/dmdd/dmdd-diagnosis-dsm-5-criteria-for-disruptive-mood-dysregulation-disorder
Last Updated: May 25, 2019
Medically reviewed by Harry Croft, MD
More Info
The Impact of ADHD on Siblings
The Partnership Between the Psychiatrist, Psychologist and Caregiver
Symptoms of Disruptive Mood Dysregulation Disorder
Children and Scary News Events
Parenting Tips for When Your Tween Has a Meltdown
Tips to Improve Communication with Your Teenager
Getting Help to Deal with Aftermath of Suicide Attempts
Disruptive Mood Dysregulation Disorder (DMDD)
Table of Contents
Disruptive Mood Dysregulation Disorder (DMDD)
Primer
DSM-5 Diagnostic Criteria
Signs and Symptoms
Screening and Rating Scales
Controversy and Criticism
Pathophysiology
Differential Diagnosis
Investigations
Treatment
Resources
For Patients
For Providers
Primer
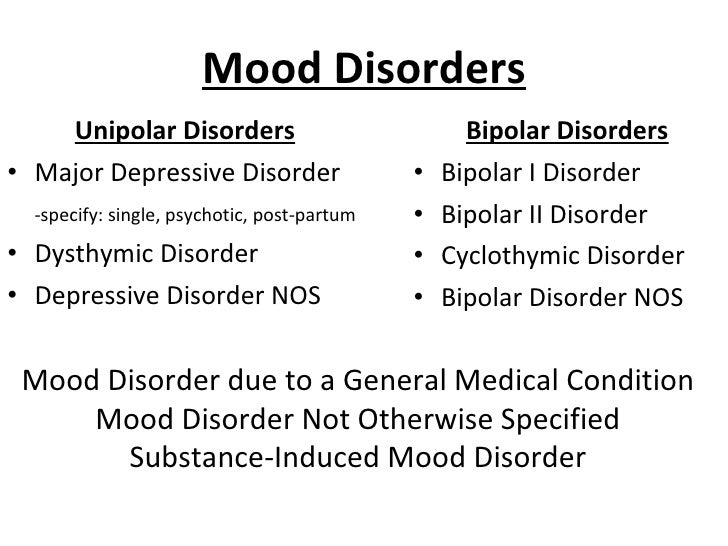
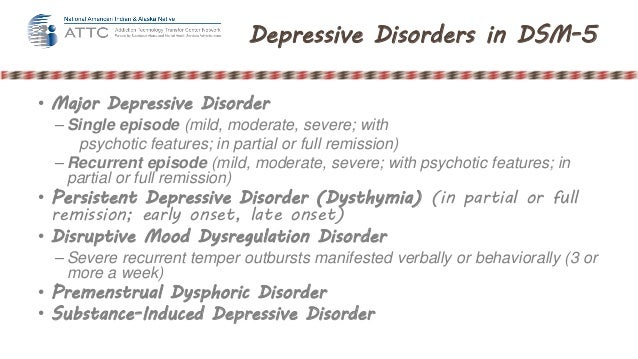
Disruptive Mood Dysregulation Disorder (DMDD) is a new controversial DSM-5 diagnosis for children with chronic and severe persistent irritability and severe anger outbursts.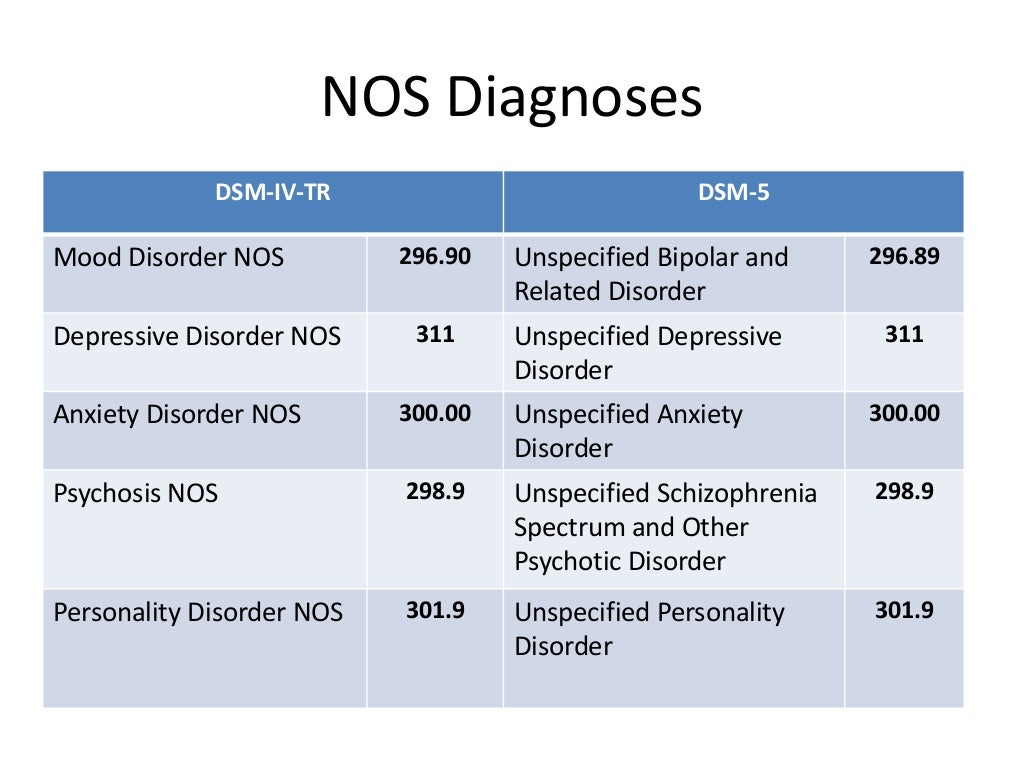 DMDD was created for patients previously diagnosed with the also controversial diagnosis of childhood (pediatric) bipolar disorder and concerns about over-diagnosis and over-treatment with antipsychotics. Although DMDD is officially classified as a mood disorder under the DSM-5, it often co-presents during childhood with other non-mood diagnoses such as conduct disorder and oppositional defiant disorder.
DMDD was created for patients previously diagnosed with the also controversial diagnosis of childhood (pediatric) bipolar disorder and concerns about over-diagnosis and over-treatment with antipsychotics. Although DMDD is officially classified as a mood disorder under the DSM-5, it often co-presents during childhood with other non-mood diagnoses such as conduct disorder and oppositional defiant disorder.
Epidemiology
The epidemiology of DMDD is not well understood as it is a new diagnosis; it is estimated to have a prevalence between 2 to 5%.
Individuals presenting to clinical attention are most commonly male.
Prognosis
Approximately 50% of children with severe, chronic irritability will have a presentation that continues to meet criteria for DMDD 1 year later.
DMDD is not a “pre-bipolar” diagnosis, and the rates of conversion from severe, nonepisodic irritability to true bipolar disorder are very low.

In both DMDD and pediatric bipolar disorder, severe aggression, reckless behavior, suicidal ideation or suicide attempts, and psychiatric hospitalization can be common.
Comorbidity
DMDD has extremely high comorbidity with other psychiatric disorders and it would be rare for an individual to only have a diagnosis of DMDD.
The strongest overlap is with oppositional defiant disorder (ODD)
Individuals can present with a wide variety of concerns including disruptive behavior, mood, anxiety, and sometimes autism spectrum symptoms.
Risk Factors
DSM-5 Diagnostic Criteria
Criterion A
Severe recurrent temper outbursts manifested verbally (e.g. - verbal rages) and/or behaviourally (e.g. - physical aggression toward people or property) that are grossly out of proportion in intensity or duration to the situation or provocation.
Criterion B
The temper outbursts are inconsistent with developmental level.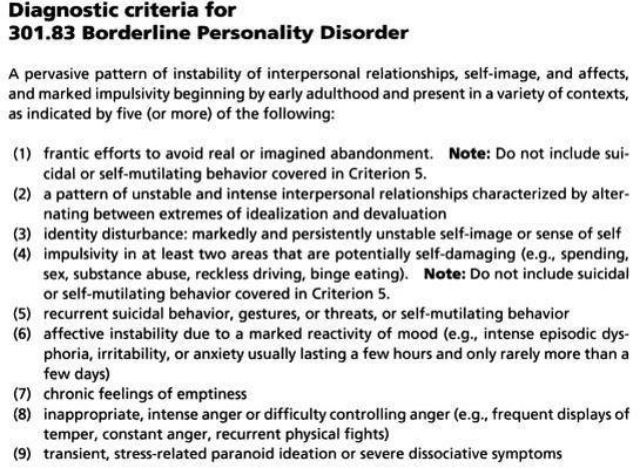
Criterion C
The temper outbursts occur, on average, 3 or more times per week.
Criterion D
The mood between temper outbursts in persistently irritable or angry most of the day, nearly every day, and is observable by others (e.g. - parents, teachers, peers).
Criterion E
Criteria A, B, C, and D have been present for 12 or more months. Throughout that time, the individual has not had a period lasting 3 or more consecutive months without all of the symptoms in Criteria A to D.
Criterion F
Criteria A and D are present in at least 2 of the 3 settings (i.e. - at home, at school, with peers) and are severe in at least 1 of these.
Criterion G
The diagnosis should not be made for the first time before age 6 years or after age 18 years
Criterion H
By history or observation, the age of onset of Criteria A to E is before 10 years.
Criterion I
There has never been a distinct period lasting more than 1 day during which the full symptom criteria, except duration, for a manic or hypomanic episode have been met.
Note: Developmentally appropriate mood elevation, such as occurs in the context of a highly positive event or its anticipation, should not be considered as a symptom of mania or hypomania.
Criterion J
The behaviors do not occur exclusively during an episode of major depressive disorder and are not better explained by another mental disorder (e.g., autism spectrum disorder, posttraumatic stress disorder, separation anxiety disorder, persistent depressive disorder.
Note:
The diagnosis of DMDD cannot coexist with oppositional defiant disorder, intermittent explosive disorder, or bipolar disorder, though it can coexist with others, including major depressive disorder, attention-deficit/hyperactivity disorder, conduct disorder, and substance use disorders.
Individuals whose symptoms meet criteria for both disruptive mood dysregulation disorder and oppositional defiant disorder should only be given the diagnosis of disruptive mood dysregulation disorder.
If an individual has ever experienced a manic or hypomanic episode, the diagnosis of disruptive mood dysregulation disorder should not be assigned (as this indicates a diagnosis of bipolar disorder).
Criterion K
The symptoms are not attributable to the physiological effects of a substance or to another medical or neurological condition.
Signs and Symptoms
It is important to note that according to the DMDD diagnostic criteria, the age of onset of the primary symptoms must have occurred before age 10.
In addition, the diagnostic label can only be applied to individuals between age
6to18.
Screening and Rating Scales
There are no validated scales for DMDD.
National Institute for Mental Health (NIMH) research groups have used versions of the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Aged Children to diagnose DMDD.
Controversy and Criticism
See main article: Cognitive Biases, Misdiagnosis, Iatrogenesis, and Overdiagnosis
The inclusion of DMDD has been questioned because the diagnostic criteria failed the DSM-5 field trials. The agreement between clinicians using the DMDD was poor, with questionable agreement (kappa = 0.25).
There remains additional concern that the DMDD diagnosis too broadly includes symptoms from other diagnoses, including oppositional defiant disorder, ADHD, anxiety, and depression.
“DMDD will capture a wildly heterogeneous and diagnostically meaningless grab bag of difficult to handle kids. Some will be temperamental and irritable, but essentially normal and just going through a developmental stage they will eventually outgrow without a stigmatizing diagnosis and a harmful treatment.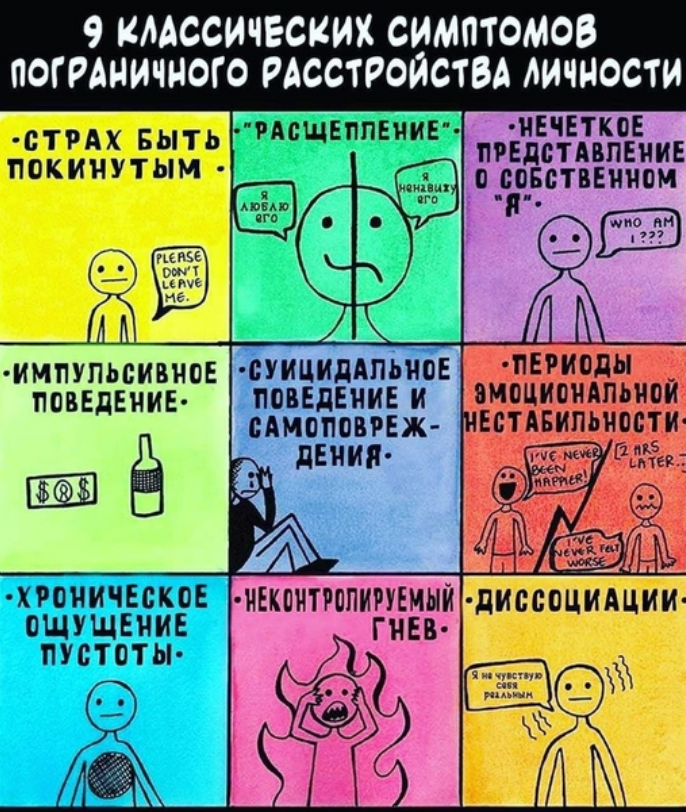 Others will have conduct or oppositional problems that gain nothing by being mislabeled as mood disorder. Yet others will have serious, but not yet clearly defined psychiatric disorders that require careful and patient monitoring before an accurate diagnosis can be made.”
Others will have conduct or oppositional problems that gain nothing by being mislabeled as mood disorder. Yet others will have serious, but not yet clearly defined psychiatric disorders that require careful and patient monitoring before an accurate diagnosis can be made.”
– Allen Frances, MD, Chair of the DSM-IV Task Force
Pathophysiology
See also: Baweja, R. et al. (2016). Disruptive mood dysregulation disorder: current insights. Neuropsychiatric disease and treatment.
Differential Diagnosis
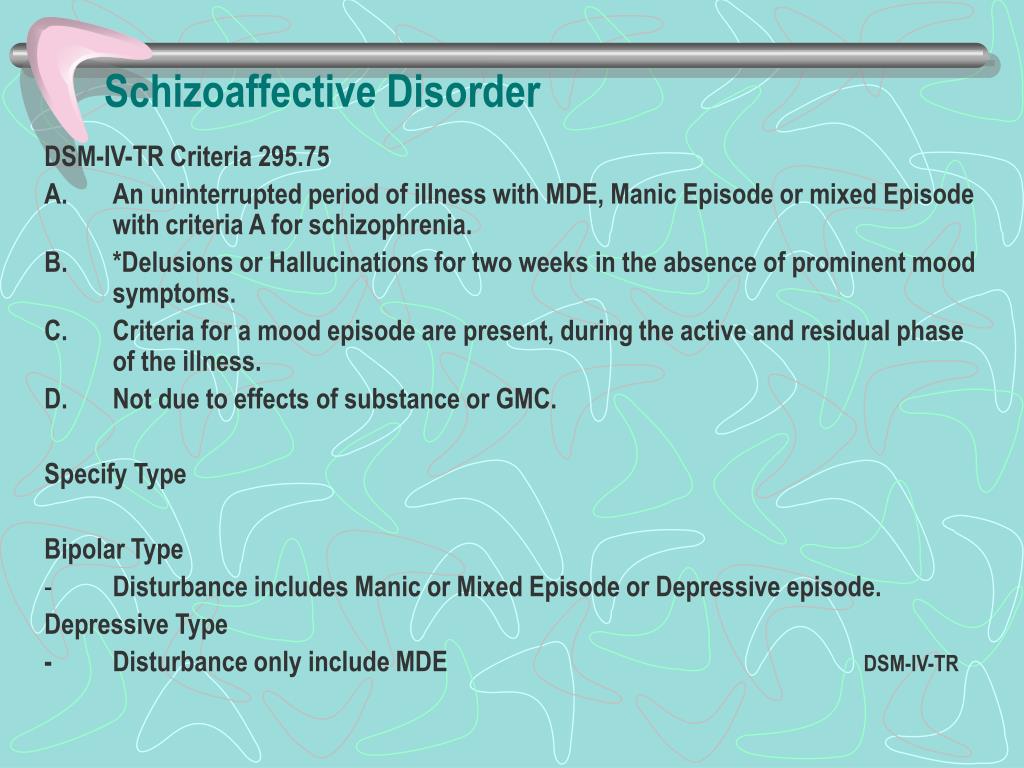
Bipolar I and Bipolar II disorder
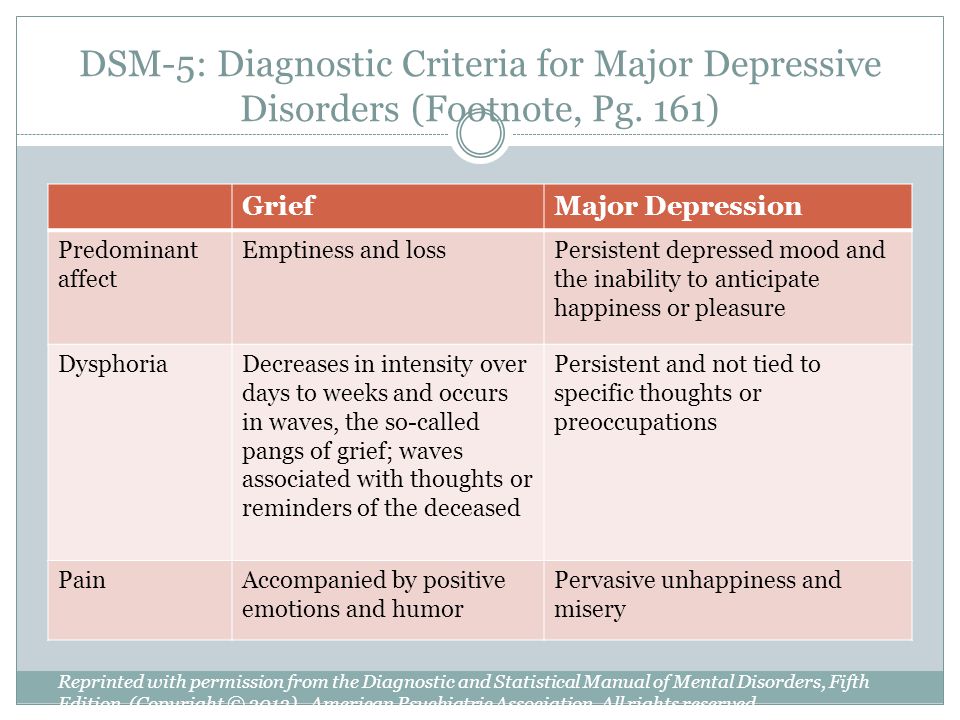
The central feature differentiating disruptive mood dysregulation disorder and bipolar disorders in children involves the longitudinal course of the core symptoms. In children, as in adults, bipolar disorders are an episodic illness with discrete episodes of mood changes that can be differentiated from the child's typical presentation. For example, the mood change that occurs during a manic episode is distinctly different from the child's usual baseline mood.
Additionally, during a manic episode onset (just like adults), there are additional associated cognitive, behavioural, and physical symptoms (e.g. - grandiosity, distractibility, increased goal-directed activity)
Thus, in the case of a manic episode, parents and/or children should be able to identify a distinct time period during which the mood and behavior were markedly different from usual.
Compare this with DMDD, where irritability is persistent and is present over many months to years. This is why the diagnosis of DMDD cannot be assigned to a child who has ever experienced a full-duration hypomanic or manic episode (irritable or euphoric) or who has ever had a manic or hypomanic episode lasting more than 1 day.
Oppositional defiant disorder (ODD)
While symptoms of ODD also occur in children with DMDD, the mood symptoms seen in DMDD are relatively rarer in ODD.
 The diagnosis of DMDD requires severe impairment in at least
The diagnosis of DMDD requires severe impairment in at least 1setting (i.e. - home, school, or among peers) and mild to moderate impairment in a2ndsetting. Thus, a child that meets diagnosis for DMDD will very likely meet criteria for ODD, but not vice versa (only 15% of individuals with ODD would meet criteria for DMDD).
Attention-deficit/hyperactivity disorder, major depressive disorder, anxiety disorders, and autism spectrum disorder.
Unlike children with bipolar disorder or ODD, a child whose symptoms meet criteria for DMDD also can receive a comorbid diagnosis of ADHD, major depressive disorder, and/or anxiety disorder. However, children whose irritability is present only in the context of a major depressive episode or persistent depressive disorder (dysthymia) should receive one of those diagnoses and not a diagnosis of DMDD.
Children with autism spectrum disorder can also have temper outbursts and the child should not receive a DMDD diagnosis.

Intermittent explosive disorder (IED)
Children with IED present with episodes of severe temper outbursts, much like children with DMDD. However, unlike DMDD, IED does not require persistent irritability and/or disruption in mood between outbursts.
In addition, IED requires only
3months of active symptoms, compared to the12-month requirement for DMDD. Thus, these two diagnoses should never be made in the same child. For children with severe outbursts plus persistent irritability, the diagnosis of DMDD should be made over IED.
Investigations
Treatment
Management of DMDD should focus on helping children and adolescents improving emotional dysregulation through parental, school, and professional support. Social skills training may also be helpful.
There are no FDA-approved medications for use in DMDD.
Resources
For Patients
NIMH - Disruptive Mood Dysregulation Disorder: The Basics
For Providers
Articles
NYT Magazine: The Bipolar Puzzle
NPR: Children Labeled 'Bipolar' May Get A New Diagnosis
Research
Parker, Gordon, and Gabriela Tavella. "Disruptive Mood Dysregulation Disorder: A Critical Perspective." The Canadian Journal of Psychiatry 63, no. 12 (2018): 813-815.
References
1) American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA.
2) American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA.
3) American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA.
4) American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA.
(2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA.
5) American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA.
6) American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA.
7) American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA.
8)Baweja, R., Mayes, S. D., Hameed, U., & Waxmonsky, J. G. (2016). Disruptive mood dysregulation disorder: current insights. Neuropsychiatric disease and treatment.
9) American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA.
Psychology of stress: theory and practice
%PDF-1.5 % 10 obj > /Metadata 4 0 R >> endobj 5 0 obj /Author /Title >> endobj 20 obj > endobj 3 0 obj > endobj 40 obj > stream
 L.1.5Microsoft® Word 20102018-11-16T12:28:31+05:002018-11-16T12:28:31+05:00 endstream endobj 6 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] /XObject> >> /MediaBox[0 0 595.
L.1.5Microsoft® Word 20102018-11-16T12:28:31+05:002018-11-16T12:28:31+05:00 endstream endobj 6 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] /XObject> >> /MediaBox[0 0 595. 32 841.92] /Contents[129 0 R 130 0 R 131 0 R] /group> /Tabs /S /StructParents 0 /Annots [132 0R] >> endobj 70 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 134 0 R /group> /Tabs /S /StructParents 1 >> endobj 80 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 135 0 R /group> /Tabs /S /StructParents 2 >> endobj 9 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 136 0R /group> /Tabs /S /StructParents 3 >> endobj 10 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 137 0R /group> /Tabs /S /StructParents 4 >> endobj 11 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 138 0 R /group> /Tabs /S /StructParents 5 >> endobj 12 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 140 0R /group> /Tabs /S /StructParents 6 >> endobj 13 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.
32 841.92] /Contents[129 0 R 130 0 R 131 0 R] /group> /Tabs /S /StructParents 0 /Annots [132 0R] >> endobj 70 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 134 0 R /group> /Tabs /S /StructParents 1 >> endobj 80 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 135 0 R /group> /Tabs /S /StructParents 2 >> endobj 9 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 136 0R /group> /Tabs /S /StructParents 3 >> endobj 10 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 137 0R /group> /Tabs /S /StructParents 4 >> endobj 11 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 138 0 R /group> /Tabs /S /StructParents 5 >> endobj 12 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 140 0R /group> /Tabs /S /StructParents 6 >> endobj 13 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595. 32 841.92] /Contents 141 0 R /group> /Tabs /S /StructParents 7 >> endobj 14 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 142 0 R /group> /Tabs /S /StructParents 8 >> endobj 15 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 143 0 R /group> /Tabs /S /StructParents 9 >> endobj 16 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 145 0 R /group> /Tabs /S /StructParents 10 >> endobj 17 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 148 0 R /group> /Tabs /S /StructParents 11 >> endobj 18 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 149 0 R /group> /Tabs /S /StructParents 12 >> endobj 19 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 150 0 R /group> /Tabs /S /StructParents 13 >> endobj 20 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.
32 841.92] /Contents 141 0 R /group> /Tabs /S /StructParents 7 >> endobj 14 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 142 0 R /group> /Tabs /S /StructParents 8 >> endobj 15 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 143 0 R /group> /Tabs /S /StructParents 9 >> endobj 16 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 145 0 R /group> /Tabs /S /StructParents 10 >> endobj 17 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 148 0 R /group> /Tabs /S /StructParents 11 >> endobj 18 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 149 0 R /group> /Tabs /S /StructParents 12 >> endobj 19 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 150 0 R /group> /Tabs /S /StructParents 13 >> endobj 20 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.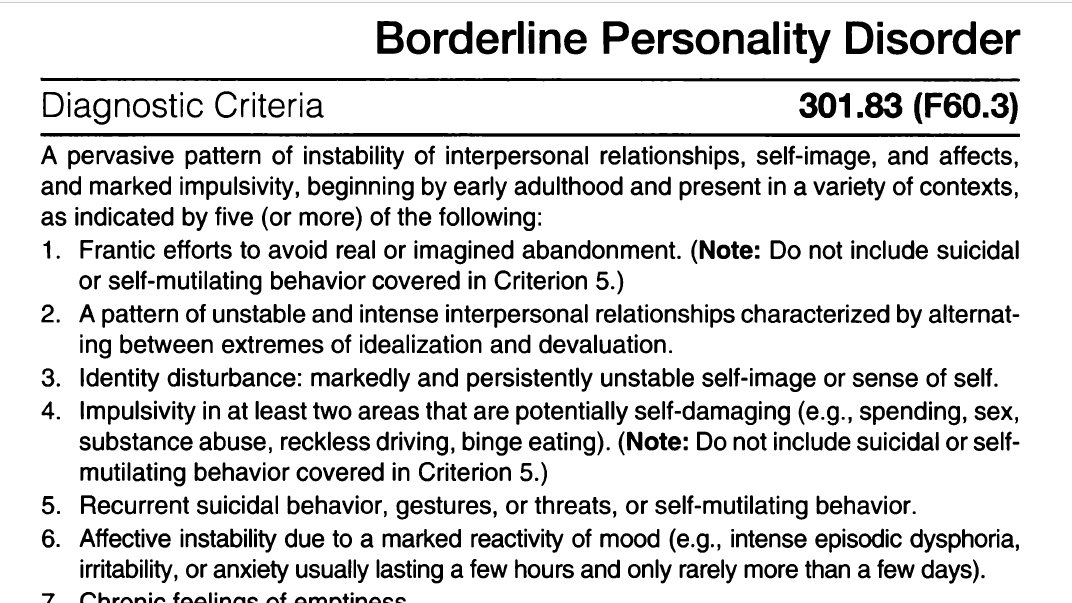 32 841.92] /Contents 151 0 R /group> /Tabs /S /StructParents 14 >> endobj 21 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 152 0R /group> /Tabs /S /StructParents 15 >> endobj 22 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 153 0R /group> /Tabs /S /StructParents 16 >> endobj 23 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 154 0R /group> /Tabs /S /StructParents 17 >> endobj 24 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 155 0 R /group> /Tabs /S /StructParents 18 >> endobj 25 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 156 0 R /group> /Tabs /S /StructParents 19 >> endobj 26 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 157 0 R /group> /Tabs /S /StructParents 20 >> endobj 27 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.
32 841.92] /Contents 151 0 R /group> /Tabs /S /StructParents 14 >> endobj 21 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 152 0R /group> /Tabs /S /StructParents 15 >> endobj 22 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 153 0R /group> /Tabs /S /StructParents 16 >> endobj 23 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 154 0R /group> /Tabs /S /StructParents 17 >> endobj 24 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 155 0 R /group> /Tabs /S /StructParents 18 >> endobj 25 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 156 0 R /group> /Tabs /S /StructParents 19 >> endobj 26 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 157 0 R /group> /Tabs /S /StructParents 20 >> endobj 27 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.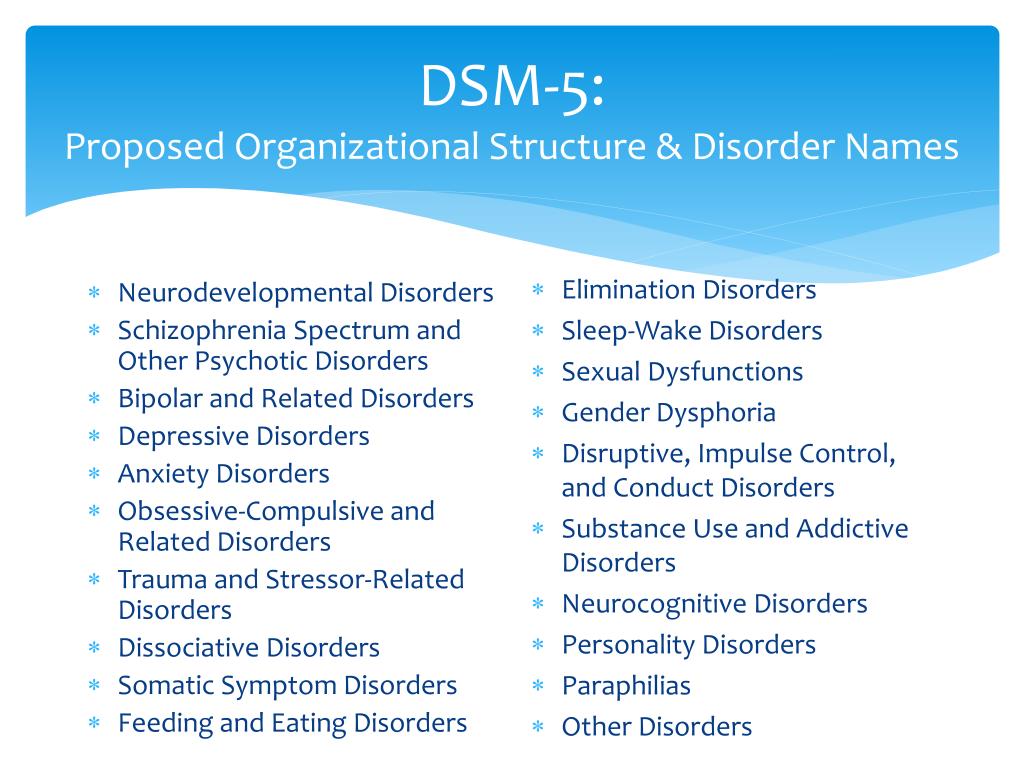 32 841.92] /Contents 160 0R /group> /Tabs /S /StructParents 21 >> endobj 28 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 161 0R /group> /Tabs /S /StructParents 22 >> endobj 29 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 162 0 R /group> /Tabs /S /StructParents 23 >> endobj 30 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 163 0R /group> /Tabs /S /StructParents 24 >> endobj 31 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 164 0 R /group> /Tabs /S /StructParents 25 >> endobj 32 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 165 0 R /group> /Tabs /S /StructParents 26 >> endobj 33 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 166 0 R /group> /Tabs /S /StructParents 27 >> endobj 34 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.
32 841.92] /Contents 160 0R /group> /Tabs /S /StructParents 21 >> endobj 28 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 161 0R /group> /Tabs /S /StructParents 22 >> endobj 29 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 162 0 R /group> /Tabs /S /StructParents 23 >> endobj 30 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 163 0R /group> /Tabs /S /StructParents 24 >> endobj 31 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 164 0 R /group> /Tabs /S /StructParents 25 >> endobj 32 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 165 0 R /group> /Tabs /S /StructParents 26 >> endobj 33 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 166 0 R /group> /Tabs /S /StructParents 27 >> endobj 34 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.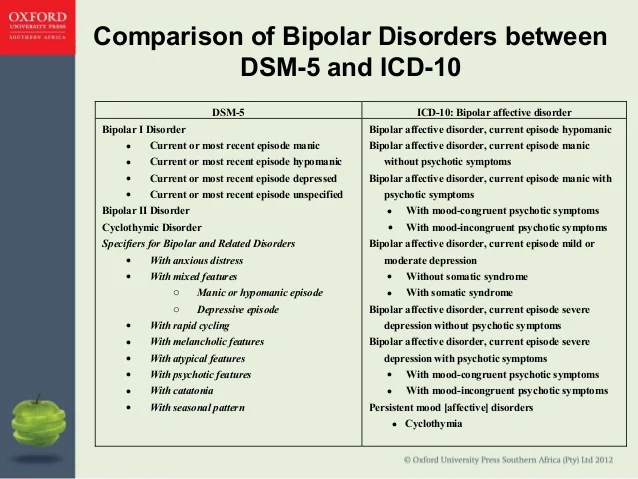 32 841.92] /Contents 167 0R /group> /Tabs /S /StructParents 28 >> endobj 35 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 168 0R /group> /Tabs /S /StructParents 29 >> endobj 36 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 169 0 R /group> /Tabs /S /StructParents 30 >> endobj 37 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 170 0 R /group> /Tabs /S /StructParents 31 >> endobj 38 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 171 0 R /group> /Tabs /S /StructParents 32 >> endobj 39 0 obj > /XObject> /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 173 0R /group> /Tabs /S /StructParents 33 >> endobj 40 0 obj > /XObject> /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 176 0R /group> /Tabs /S /StructParents 34 >> endobj 41 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.
32 841.92] /Contents 167 0R /group> /Tabs /S /StructParents 28 >> endobj 35 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 168 0R /group> /Tabs /S /StructParents 29 >> endobj 36 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 169 0 R /group> /Tabs /S /StructParents 30 >> endobj 37 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 170 0 R /group> /Tabs /S /StructParents 31 >> endobj 38 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 171 0 R /group> /Tabs /S /StructParents 32 >> endobj 39 0 obj > /XObject> /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 173 0R /group> /Tabs /S /StructParents 33 >> endobj 40 0 obj > /XObject> /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 176 0R /group> /Tabs /S /StructParents 34 >> endobj 41 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.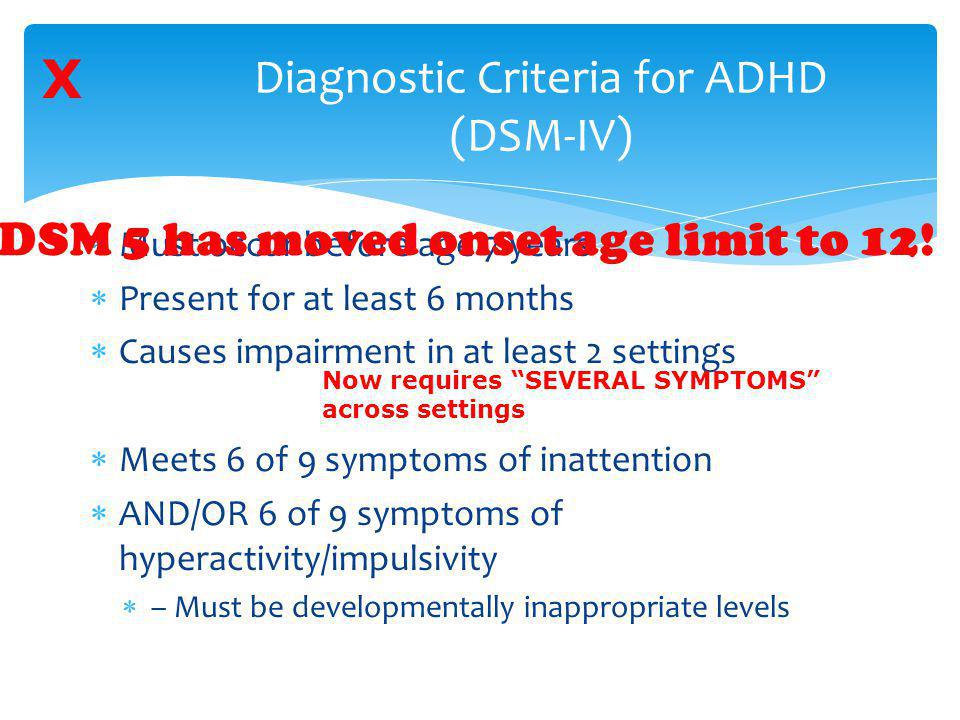 32 841.92] /Contents 177 0 R /group> /Tabs /S /StructParents 35 >> endobj 42 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 178 0R /group> /Tabs /S /StructParents 36 >> endobj 43 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 179 0R /group> /Tabs /S /StructParents 37 >> endobj 44 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 180 0 R /group> /Tabs /S /StructParents 38 >> endobj 45 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 181 0 R /group> /Tabs /S /StructParents 39 >> endobj 46 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 182 0 R /group> /Tabs /S /StructParents 40 >> endobj 47 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 183 0 R /group> /Tabs /S /StructParents 41 >> endobj 48 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.
32 841.92] /Contents 177 0 R /group> /Tabs /S /StructParents 35 >> endobj 42 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 178 0R /group> /Tabs /S /StructParents 36 >> endobj 43 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 179 0R /group> /Tabs /S /StructParents 37 >> endobj 44 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 180 0 R /group> /Tabs /S /StructParents 38 >> endobj 45 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 181 0 R /group> /Tabs /S /StructParents 39 >> endobj 46 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 182 0 R /group> /Tabs /S /StructParents 40 >> endobj 47 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 183 0 R /group> /Tabs /S /StructParents 41 >> endobj 48 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.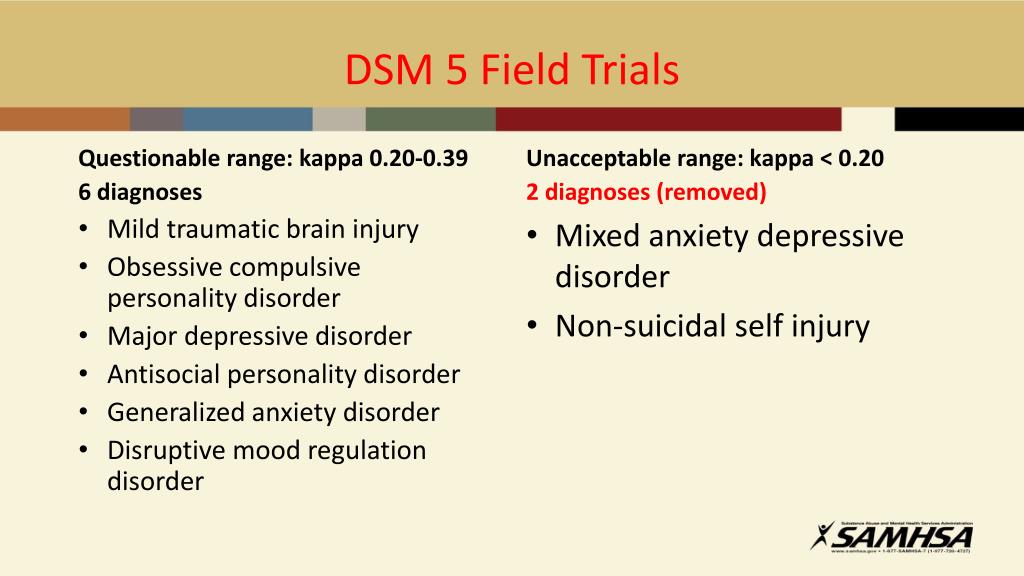 32 841.92] /Contents 184 0 R /group> /Tabs /S /StructParents 42 >> endobj 49 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 185 0 R /group> /Tabs /S /StructParents 43 >> endobj 50 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 186 0 R /group> /Tabs /S /StructParents 44 >> endobj 51 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 187 0 R /group> /Tabs /S /StructParents 45 >> endobj 52 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 188 0 R /group> /Tabs /S /StructParents 46 >> endobj 53 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 189 0 R /group> /Tabs /S /StructParents 47 >> endobj 54 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 190 0 R /group> /Tabs /S /StructParents 48 >> endobj 55 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.
32 841.92] /Contents 184 0 R /group> /Tabs /S /StructParents 42 >> endobj 49 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 185 0 R /group> /Tabs /S /StructParents 43 >> endobj 50 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 186 0 R /group> /Tabs /S /StructParents 44 >> endobj 51 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 187 0 R /group> /Tabs /S /StructParents 45 >> endobj 52 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 188 0 R /group> /Tabs /S /StructParents 46 >> endobj 53 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 189 0 R /group> /Tabs /S /StructParents 47 >> endobj 54 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 190 0 R /group> /Tabs /S /StructParents 48 >> endobj 55 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595. 32 841.92] /Contents 191 0 R /group> /Tabs /S /StructParents 49 >> endobj 56 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 192 0 R /group> /Tabs /S /StructParents 50 >> endobj 57 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 193 0 R /group> /Tabs /S /StructParents 51 >> endobj 58 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 194 0R /group> /Tabs /S /StructParents 52 >> endobj 59 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 195 0R /group> /Tabs /S /StructParents 53 >> endobj 60 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 196 0 R /group> /Tabs /S /StructParents 54 >> endobj 61 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 197 0R /group> /Tabs /S /StructParents 55 >> endobj 62 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.
32 841.92] /Contents 191 0 R /group> /Tabs /S /StructParents 49 >> endobj 56 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 192 0 R /group> /Tabs /S /StructParents 50 >> endobj 57 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 193 0 R /group> /Tabs /S /StructParents 51 >> endobj 58 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 194 0R /group> /Tabs /S /StructParents 52 >> endobj 59 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 195 0R /group> /Tabs /S /StructParents 53 >> endobj 60 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 196 0 R /group> /Tabs /S /StructParents 54 >> endobj 61 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 197 0R /group> /Tabs /S /StructParents 55 >> endobj 62 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595. 32 841.92] /Contents 198 0 R /group> /Tabs /S /StructParents 56 >> endobj 63 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 199 0 R /group> /Tabs /S /StructParents 57 >> endobj 64 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 200 0R /group> /Tabs /S /StructParents 58 >> endobj 65 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 201 0 R /group> /Tabs /S /StructParents 59 >> endobj 66 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 202 0 R /group> /Tabs /S /StructParents 60 >> endobj 67 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 203 0 R /group> /Tabs /S /StructParents 61 >> endobj 68 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 204 0 R /group> /Tabs /S /StructParents 62 >> endobj 69 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.
32 841.92] /Contents 198 0 R /group> /Tabs /S /StructParents 56 >> endobj 63 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 199 0 R /group> /Tabs /S /StructParents 57 >> endobj 64 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 200 0R /group> /Tabs /S /StructParents 58 >> endobj 65 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 201 0 R /group> /Tabs /S /StructParents 59 >> endobj 66 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 202 0 R /group> /Tabs /S /StructParents 60 >> endobj 67 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 203 0 R /group> /Tabs /S /StructParents 61 >> endobj 68 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 204 0 R /group> /Tabs /S /StructParents 62 >> endobj 69 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.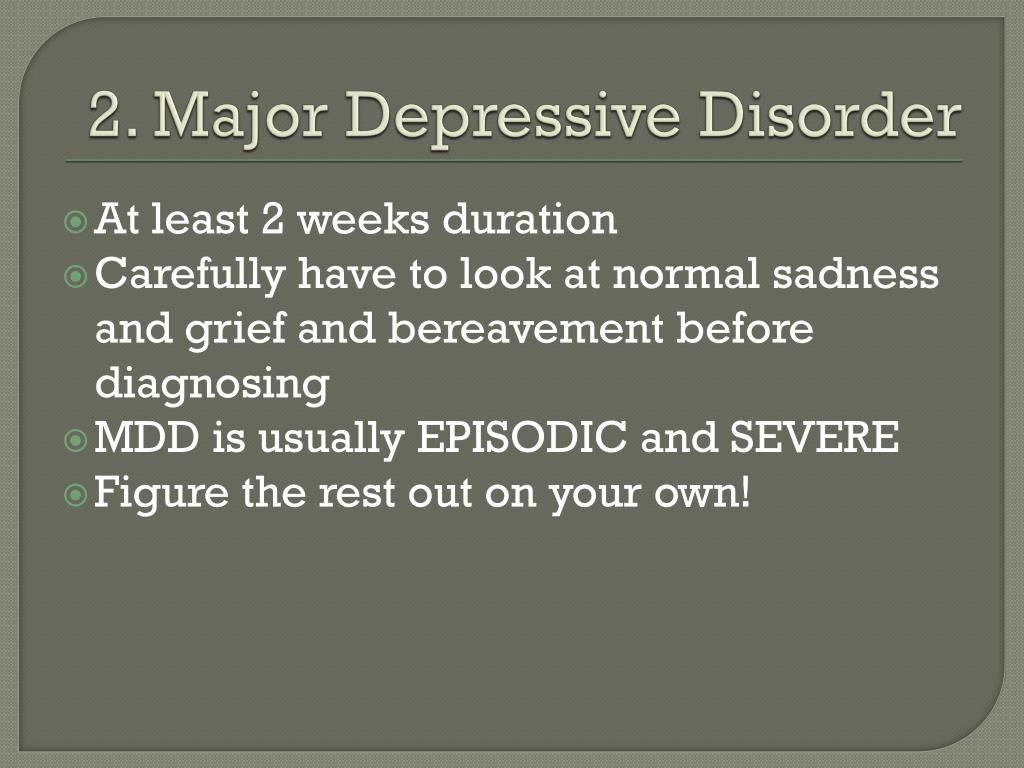 32 841.92] /Contents 205 0 R /group> /Tabs /S /StructParents 63 >> endobj 70 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 206 0 R /group> /Tabs /S /StructParents 64 >> endobj 71 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 207 0 R /group> /Tabs /S /StructParents 65 >> endobj 72 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 208 0 R /group> /Tabs /S /StructParents 66 >> endobj 73 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 209 0 R /group> /Tabs /S /StructParents 67 >> endobj 74 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 210 0 R /group> /Tabs /S /StructParents 68 >> endobj 75 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 211 0R /group> /Tabs /S /StructParents 69 >> endobj 76 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.
32 841.92] /Contents 205 0 R /group> /Tabs /S /StructParents 63 >> endobj 70 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 206 0 R /group> /Tabs /S /StructParents 64 >> endobj 71 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 207 0 R /group> /Tabs /S /StructParents 65 >> endobj 72 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 208 0 R /group> /Tabs /S /StructParents 66 >> endobj 73 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 209 0 R /group> /Tabs /S /StructParents 67 >> endobj 74 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 210 0 R /group> /Tabs /S /StructParents 68 >> endobj 75 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 211 0R /group> /Tabs /S /StructParents 69 >> endobj 76 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595. 32 841.92] /Contents 212 0 R /group> /Tabs /S /StructParents 70 >> endobj 77 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 213 0 R /group> /Tabs /S /StructParents 71 >> endobj 78 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 214 0 R /group> /Tabs /S /StructParents 72 >> endobj 79 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 215 0R /group> /Tabs /S /StructParents 73 >> endobj 80 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 216 0R /group> /Tabs /S /StructParents 74 >> endobj 81 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 217 0R /group> /Tabs /S /StructParents 75 >> endobj 82 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 218 0R /group> /Tabs /S /StructParents 76 >> endobj 83 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.
32 841.92] /Contents 212 0 R /group> /Tabs /S /StructParents 70 >> endobj 77 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 213 0 R /group> /Tabs /S /StructParents 71 >> endobj 78 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 214 0 R /group> /Tabs /S /StructParents 72 >> endobj 79 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 215 0R /group> /Tabs /S /StructParents 73 >> endobj 80 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 216 0R /group> /Tabs /S /StructParents 74 >> endobj 81 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 217 0R /group> /Tabs /S /StructParents 75 >> endobj 82 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 218 0R /group> /Tabs /S /StructParents 76 >> endobj 83 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595. 32 841.92] /Contents 219 0R /group> /Tabs /S /StructParents 77 >> endobj 84 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 220 0 R /group> /Tabs /S /StructParents 78 >> endobj 85 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 221 0R /group> /Tabs /S /StructParents 79 >> endobj 86 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 222 0 R /group> /Tabs /S /StructParents 80 >> endobj 87 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 223 0R /group> /Tabs /S /StructParents 81 >> endobj 88 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 224 0 R /group> /Tabs /S /StructParents 82 >> endobj 89 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 225 0R /group> /Tabs /S /StructParents 83 >> endobj 90 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.
32 841.92] /Contents 219 0R /group> /Tabs /S /StructParents 77 >> endobj 84 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 220 0 R /group> /Tabs /S /StructParents 78 >> endobj 85 0 obj > /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 221 0R /group> /Tabs /S /StructParents 79 >> endobj 86 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 222 0 R /group> /Tabs /S /StructParents 80 >> endobj 87 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 223 0R /group> /Tabs /S /StructParents 81 >> endobj 88 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 224 0 R /group> /Tabs /S /StructParents 82 >> endobj 89 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 225 0R /group> /Tabs /S /StructParents 83 >> endobj 90 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.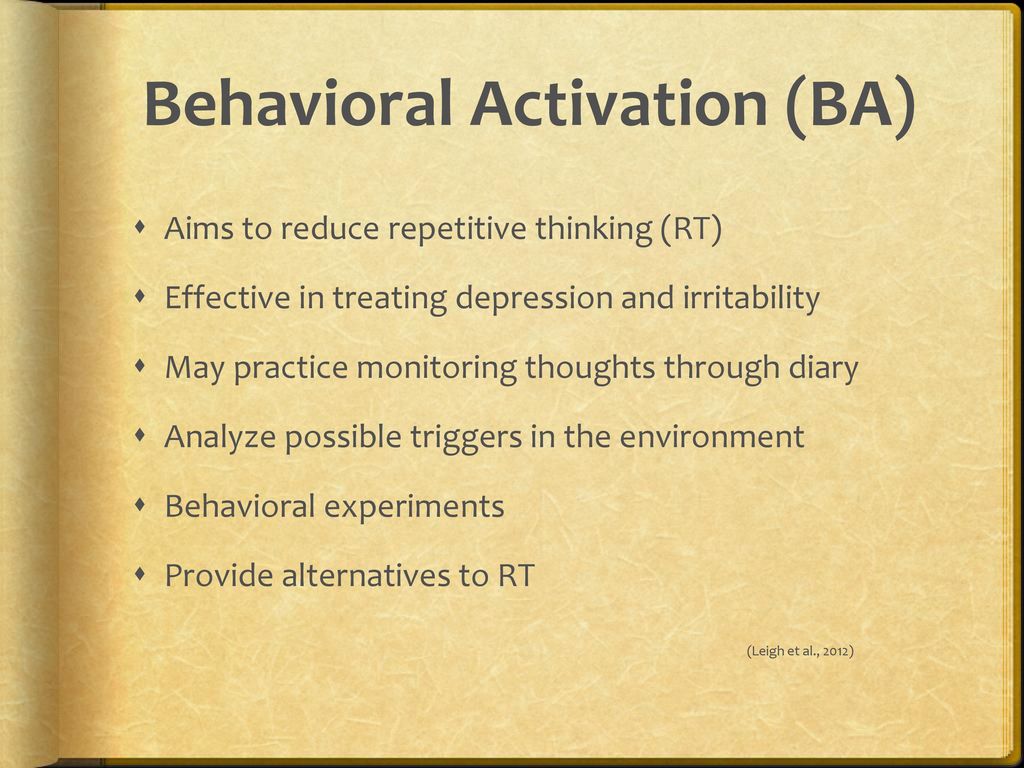 32 841.92] /Contents 226 0 R /group> /Tabs /S /StructParents 84 >> endobj 91 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 227 0 R /group> /Tabs /S /StructParents 85 >> endobj 92 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 228 0R /group> /Tabs /S /StructParents 86 >> endobj 93 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 229 0 R /group> /Tabs /S /StructParents 87 >> endobj 94 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 230 0 R /group> /Tabs /S /StructParents 88 >> endobj 95 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 231 0 R /group> /Tabs /S /StructParents 89 >> endobj 96 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 232 0 R /group> /Tabs /S /StructParents 90 >> endobj 97 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.
32 841.92] /Contents 226 0 R /group> /Tabs /S /StructParents 84 >> endobj 91 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 227 0 R /group> /Tabs /S /StructParents 85 >> endobj 92 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 228 0R /group> /Tabs /S /StructParents 86 >> endobj 93 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 229 0 R /group> /Tabs /S /StructParents 87 >> endobj 94 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 230 0 R /group> /Tabs /S /StructParents 88 >> endobj 95 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 231 0 R /group> /Tabs /S /StructParents 89 >> endobj 96 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 232 0 R /group> /Tabs /S /StructParents 90 >> endobj 97 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.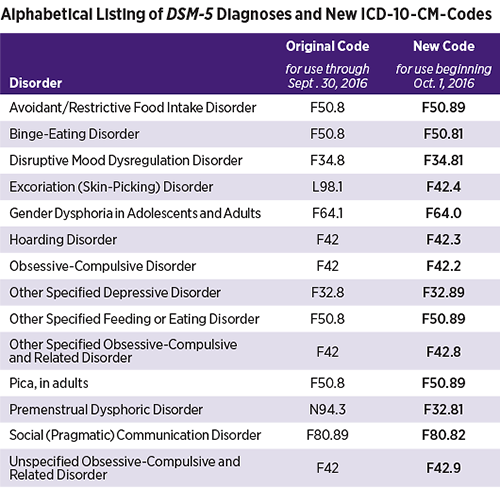 32 841.92] /Contents 234 0 R /group> /Tabs /S /StructParents 91 >> endobj 98 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 235 0R /group> /Tabs /S /StructParents 92 >> endobj 99 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 237 0R /group> /Tabs /S /StructParents 93 >> endobj 100 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 238 0 R /group> /Tabs /S /StructParents 94 >> endobj 101 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 239 0 R /group> /Tabs /S /StructParents 95 >> endobj 102 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 240 0 R /group> /Tabs /S /StructParents 96 >> endobj 103 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 241 0R /group> /Tabs /S /StructParents 97 >> endobj 104 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.
32 841.92] /Contents 234 0 R /group> /Tabs /S /StructParents 91 >> endobj 98 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 235 0R /group> /Tabs /S /StructParents 92 >> endobj 99 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 237 0R /group> /Tabs /S /StructParents 93 >> endobj 100 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 238 0 R /group> /Tabs /S /StructParents 94 >> endobj 101 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 239 0 R /group> /Tabs /S /StructParents 95 >> endobj 102 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 240 0 R /group> /Tabs /S /StructParents 96 >> endobj 103 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 241 0R /group> /Tabs /S /StructParents 97 >> endobj 104 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595. 32 841.92] /Contents 242 0 R /group> /Tabs /S /StructParents 98 >> endobj 105 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 243 0 R /group> /Tabs /S /StructParents 99 >> endobj 106 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 244 0 R /group> /Tabs /S /StructParents 100 >> endobj 107 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 245 0 R /group> /Tabs /S /StructParents 101 >> endobj 108 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 246 0R /group> /Tabs /S /StructParents 102 >> endobj 109 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 247 0R /group> /Tabs /S /StructParents 103 >> endobj 110 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.
32 841.92] /Contents 242 0 R /group> /Tabs /S /StructParents 98 >> endobj 105 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 243 0 R /group> /Tabs /S /StructParents 99 >> endobj 106 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 244 0 R /group> /Tabs /S /StructParents 100 >> endobj 107 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 245 0 R /group> /Tabs /S /StructParents 101 >> endobj 108 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 246 0R /group> /Tabs /S /StructParents 102 >> endobj 109 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 247 0R /group> /Tabs /S /StructParents 103 >> endobj 110 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841. 92] /Contents 248 0R /group> /Tabs /S /StructParents 104 >> endobj 111 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 249 0 R /group> /Tabs /S /StructParents 105 >> endobj 112 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 250 0 R /group> /Tabs /S /StructParents 106 >> endobj 113 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 251 0 R /group> /Tabs /S /StructParents 107 >> endobj 114 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 252 0 R /group> /Tabs /S /StructParents 108 >> endobj 115 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 253 0 R /group> /Tabs /S /StructParents 109 >> endobj 116 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 254 0 R /group> /Tabs /S /StructParents 110 >> endobj 117 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.
92] /Contents 248 0R /group> /Tabs /S /StructParents 104 >> endobj 111 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 249 0 R /group> /Tabs /S /StructParents 105 >> endobj 112 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 250 0 R /group> /Tabs /S /StructParents 106 >> endobj 113 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 251 0 R /group> /Tabs /S /StructParents 107 >> endobj 114 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.32 841.92] /Contents 252 0 R /group> /Tabs /S /StructParents 108 >> endobj 115 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 253 0 R /group> /Tabs /S /StructParents 109 >> endobj 116 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox [0 0 595.32 841.92] /Contents 254 0 R /group> /Tabs /S /StructParents 110 >> endobj 117 0 obj > /ExtGState> /ProcSet [/PDF /Text /ImageB /ImageC /ImageI] >> /MediaBox[0 0 595.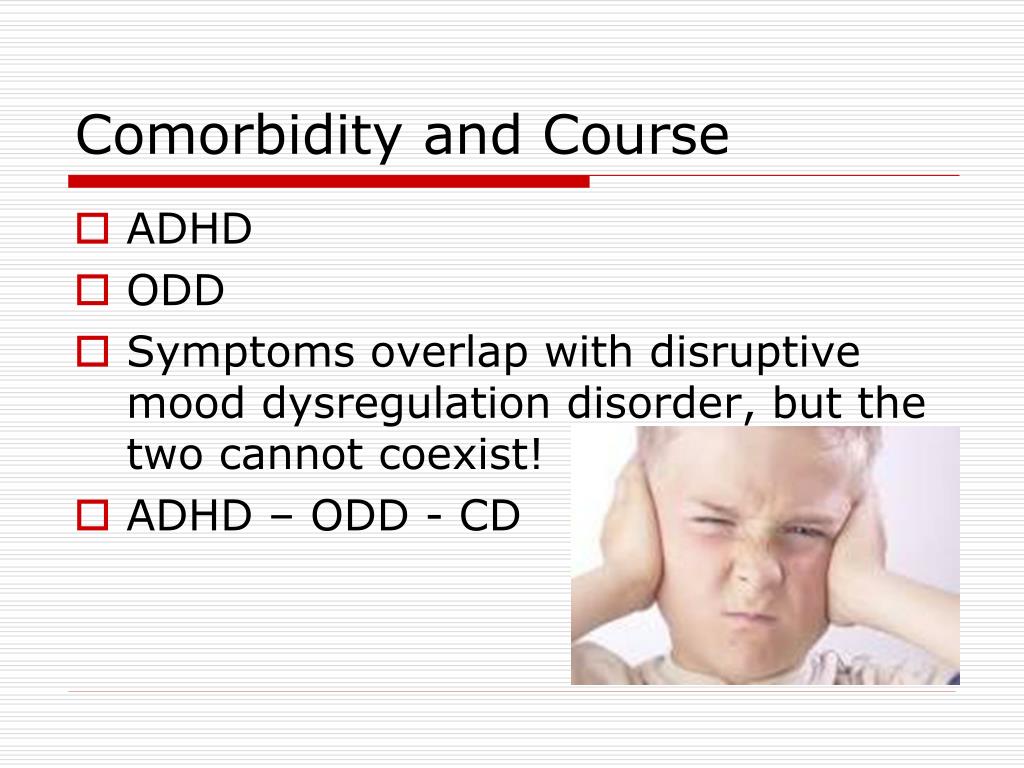 32 841.92] /Contents 255 0 R /group> /Tabs /S /StructParents 111 >> endobj 118 0 obj > endobj 119 0 obj > endobj 120 0 obj > endobj 121 0 obj > endobj 122 0 obj > endobj 123 0 obj > endobj 124 0 obj > endobj 125 0 obj > endobj 126 0 obj > endobj 127 0 obj > endobj 128 0 obj > stream x
32 841.92] /Contents 255 0 R /group> /Tabs /S /StructParents 111 >> endobj 118 0 obj > endobj 119 0 obj > endobj 120 0 obj > endobj 121 0 obj > endobj 122 0 obj > endobj 123 0 obj > endobj 124 0 obj > endobj 125 0 obj > endobj 126 0 obj > endobj 127 0 obj > endobj 128 0 obj > stream x Borderline Personality Disorder Test - Competent Parent
Uncategorized
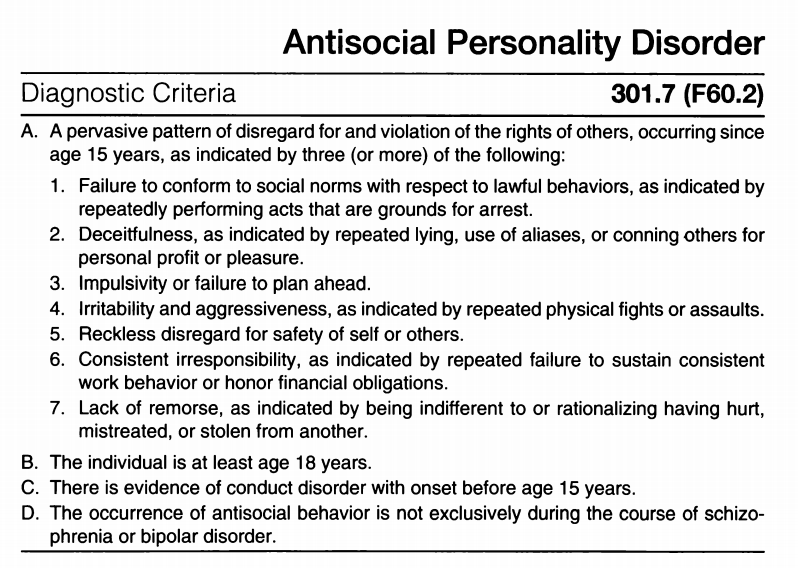
The technique is a personality questionnaire developed on the basis of diagnostic criteria for borderline personality disorder according to DSM-III-R and DSM-IV in 2012 by a team of authors (T. Yu. Lasovskaya, S. V. Yaichnikov, Yu. V. Sarycheva, Ts. P. Korolenko).
According to the DSM diagnostic criteria, the diagnosis of borderline personality disorder is carried out according to the following criteria:
- Pattern of unstable and intense interpersonal relationships , characterized by polar, negative or positive assessments.
 It is assumed that persons with borderline personality disorder are unable to see the true reasons for the behavior of others (for example, caring or helping) and the behavior is rated as absolutely positive if it is pleasurable, or as absolutely negative if it does not. This characteristic is important in diagnosing borderline personality disorder, as it reflects a psychological splitting mechanism that effectively alleviates strong feelings, such as anger.
It is assumed that persons with borderline personality disorder are unable to see the true reasons for the behavior of others (for example, caring or helping) and the behavior is rated as absolutely positive if it is pleasurable, or as absolutely negative if it does not. This characteristic is important in diagnosing borderline personality disorder, as it reflects a psychological splitting mechanism that effectively alleviates strong feelings, such as anger. - Impulsivity in at least two areas that are potentially self-injurious, eg spending money, sex, substance abuse, risky driving, overeating (does not include suicidal and self-injurious behavior). Impulsivity as a feature is characteristic of antisocial personality disorder, as well as states of mania (hypomania). However, it is only in borderline personality disorder that impulsivity has a connotation of direct or indirect self-harm (self-directedness), such as chemical addictions or bulimia. The criterion of impulsivity explains the difficulties described in early works in conducting psychotherapy for people with borderline personality disorder - frequent conflicts, interruption of therapy at the very beginning.
- Emotional instability : pronounced deviations from the isoline from the side of mood towards depression, irritability, anxiety, usually lasting from several hours to several days. The affective instability and propensity to depression in borderline disorder resemble those in individuals with emotion regulation problems such as depression and bipolar 2 disorder. Therefore, the meaning of this criterion should be clarified, namely: we are talking about increased emotional reactivity, where mood swings occur, but they occur more often, proceed softer and less long than in depression and bipolar disorder.
- Inadequate, intense anger or poor anger control (eg, frequent irascibility, persistent anger, attacking others). Kernberg considered anger to be a characteristic feature of borderline personality disorder and noted that the anger reaction is associated with a situation of excessive frustration. Anger is both a result of genetic predisposition and environmental influences and may lead to future acts of self-harm.
 Signs of self-harm as a result of the realization of anger, it would seem, are easily detected, for example, cuts, but they are not always possible to establish during a conversation with the patient. Many patients experience anger most of the time, but very rarely put it into action (the anger is hidden). Sometimes anger becomes apparent only after the patient's destructive actions. In some cases, indications of anger and its manifestations appear in the anamnesis or are revealed during active questioning on this topic. Anger is easily provoked in a purposeful confrontational interview.
Signs of self-harm as a result of the realization of anger, it would seem, are easily detected, for example, cuts, but they are not always possible to establish during a conversation with the patient. Many patients experience anger most of the time, but very rarely put it into action (the anger is hidden). Sometimes anger becomes apparent only after the patient's destructive actions. In some cases, indications of anger and its manifestations appear in the anamnesis or are revealed during active questioning on this topic. Anger is easily provoked in a purposeful confrontational interview. - Repeated suicidal behavior , destructive behavior and other self-injurious behavior. Repeated suicide attempts and self-injurious behavior are reliable markers of borderline personality disorder.
- Identity disorder manifesting itself in at least two areas - self-esteem, self-image, sexual orientation, goal setting, career choice, type of friends preferred, values.
 This criterion was described by O. Kernberg when describing the construct of a borderline personal organization. Since DSM-III, the criterion has been modified to distinguish between situations where identification instability is a manifestation of the norm, such as during adolescence. This criterion, more than any other, is self-related and therefore specific to borderline personality disorder. This may be important in pathology, when the perception of the body image is impaired - body dysmorphic disorders and anorexia nervosa.
This criterion was described by O. Kernberg when describing the construct of a borderline personal organization. Since DSM-III, the criterion has been modified to distinguish between situations where identification instability is a manifestation of the norm, such as during adolescence. This criterion, more than any other, is self-related and therefore specific to borderline personality disorder. This may be important in pathology, when the perception of the body image is impaired - body dysmorphic disorders and anorexia nervosa. - Chronic feeling of emptiness (or boredom). Early analysts (Abraham and Freud) described the oral phase of development, noting that failure to complete it leads in adulthood to symptoms of depression, dependence, and emptiness in interpersonal relationships. This concept was developed and supplemented by M. Kline's theory of object relations, which showed that due to poor early relationships, a person becomes incapable of internalizing positive emotions during interpersonal communication (that is, inability to internalize feelings in oneself / oneself) and incapable of self-comfort.
 The feeling of emptiness in borderline personality disorder has somatic manifestations, localized in the abdomen or chest. This sign should be distinguished from fear or anxiety. Emptiness or boredom, which takes the form of intense mental pain, as a subjective experience of the patient, is extremely important for making a diagnosis of borderline personality disorder.
The feeling of emptiness in borderline personality disorder has somatic manifestations, localized in the abdomen or chest. This sign should be distinguished from fear or anxiety. Emptiness or boredom, which takes the form of intense mental pain, as a subjective experience of the patient, is extremely important for making a diagnosis of borderline personality disorder. - Real or imagined fear of leaving . Masterson sees the fear of leaving as an important diagnostic feature of the borderline construct. However, this criterion needs some clarification, since it is necessary to differentiate it from the more pathological separation anxiety. Gunderson proposed to change the wording of this criterion, namely, to transform it into " lack of tolerance for loneliness ". It is believed that exposure in the early period, from 16 to 24 months of life, is important in the formation of the symptom
- Stress-related incoming paranoid ideas and dissociative symptoms .
The short version contains 20 questions and is a convenient and valid tool for screening, daily diagnosis and verification of the diagnosis in psychiatric, general clinical and non-medical practice.
1. I am often disappointed in people who seemed ideal to me
Yes
No
2. I can be called a "risk guy" - I like everything that helps to feel the brightness of the world - drive a car at high speed, spend big money, experiment with alcohol or drugs
Yes
No
3. I experience an unprecedented high of mood if I manage to win at least a small amount of money (for example, in cards or a casino)
Yes
No
4. I have episodes when I can eat a large amount of food in a short time (sweets, cake) and in general everything that is in the refrigerator
Yes
No
5. My mood is often good, even and stable
Yes
No
6. Others notice that my mood can be very changeable - sometimes several times a day
Yes
No
7. If I am really angry, I can easily insult a person or provoke a fight
If I am really angry, I can easily insult a person or provoke a fight
Yes
No
8. Sometimes I get very angry, which is difficult to contain
Yes
No
9. At moments of difficult emotional experiences, I have thoughts of suicide or self-harm
Yes
No
10.Sometimes I suddenly want to do something that may or may not end in my death, such as taking a large dose of medication
Yes
No
11. From time to time such bad thoughts come into my head that it is better not to talk about them
Yes
No
12. There were episodes in my life when I hurt myself (cut my hand with a razor, burned my skin with a cigarette, etc.
Yes
No
13. Others notice that I can sometimes do rash things
Yes
No
14.Sometimes it happened that I did not finish almost finished work, because it ceased to interest me
Yes
No
15.