Depression worsens during period
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.

-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly. Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Depression during menstruation: how hormones affect our mood
Health
- Photo
- Getty Images
It is generally accepted that it is female hormones that make mood unstable. But doctors say with confidence: progesterone and estrogen protect the woman's psyche from mental disorders. This was discussed by the speakers at the III International Medical Conference “Brain Functioning: Control Leverage, Recovery Options and Ways of Improvement”.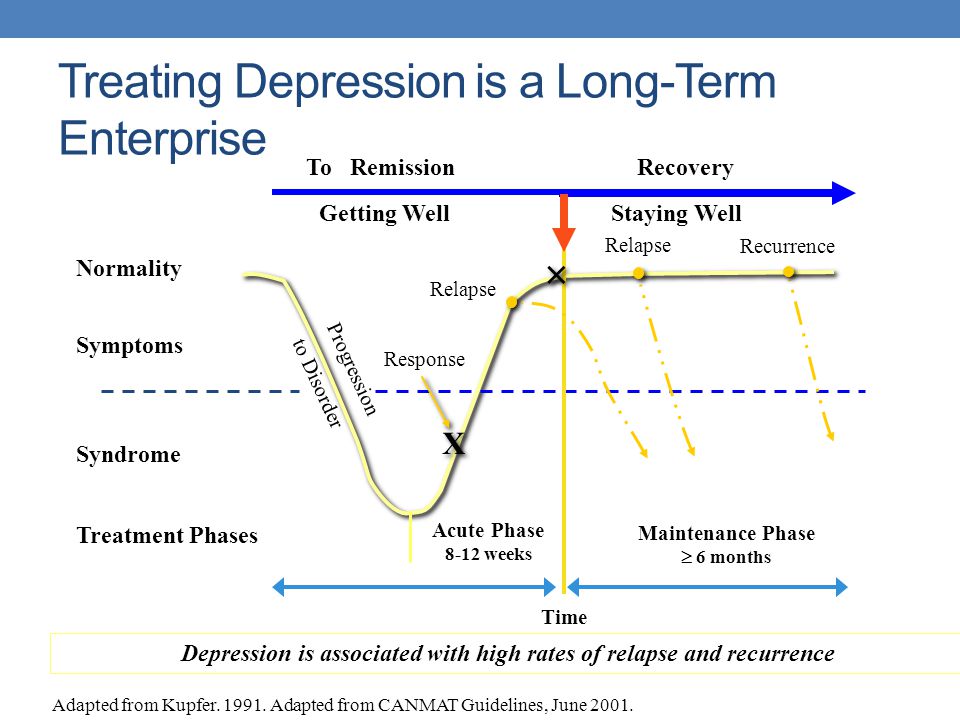
Prof. Dr. med.
General Therapist, General Therapist Mayer, Deputy Chief Physician for Development and Research at the Austrian Health Center Verba Mayr
The organs in our body do not work by themselves. All processes are controlled by the nervous system and the system of hormones associated with it. Emotions are no exception. Hormones not only control the growth and function of cells, tissues, and organs, but they also serve as neurotransmitters—mediators between the nervous system and the body.
The more cortisol in the body, the lower the level of happiness hormones. The less the latter, the more pronounced the stress state. As a rule, cortisol is produced in the morning, because in ancient times, a person needed stress in order to get out of the cave and get his own food. Therefore, in the morning, very often people wake up with a bad mood. It is very important to take a shower, do physical exercises in order to disperse cortisol and reduce stress levels a little.
It is precisely because of the constant stressful situations in our lives that a new term is gaining popularity - “syndrome of tired adrenal glands”. The latter produce a large amount of hormones: cortisol, adrenaline, norepinephrine and some others. Together with the hypothalamus and pituitary gland, they form a normal and vital response to stress. But when stressful conditions are a constant phenomenon, then cortisol is constantly produced in the body, the work of the nervous, cardiovascular, immune systems, and the gastrointestinal tract is disrupted.
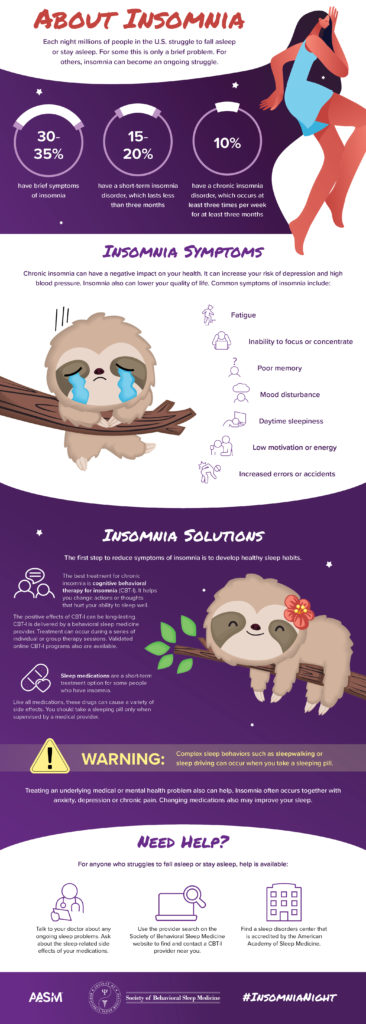
Symptoms of adrenal gland fatigue syndrome:
-
Strong fatigue in the morning,
-
Mental Disorders,
-
Insomnia,
-
Unsuitable malfunctions in the digestive tract,
- 9000 9000 9000 hair and nails.
More than just hormones
In terms of the effect of hormones on health, women are in a better position. In the United States, experiments were conducted when it was noticed that in the presence of estrogen, a coronavirus infection is much easier to tolerate. Studies show men and women are affected by COVID-19differently: the former get sick more often, their disease is much more severe.
In the United States, experiments were conducted when it was noticed that in the presence of estrogen, a coronavirus infection is much easier to tolerate. Studies show men and women are affected by COVID-19differently: the former get sick more often, their disease is much more severe.
Estrogen has a protective function against stress. Studies have shown that this female hormone is associated with the formation of post-traumatic disorders. The degree of exposure to them depends on the level of estrogen in the body. The more it is, the less psychotrauma a woman has.
- Photo
- Getty Images
Women's depression
During menstruation, the level of estrogen in a woman's body decreases, but there is more progesterone. Strong emotional swings are connected with this during this period. It is thanks to the increased emotionality that occurs due to hormone surges that the myth of female instability has appeared. But is it?
But is it?
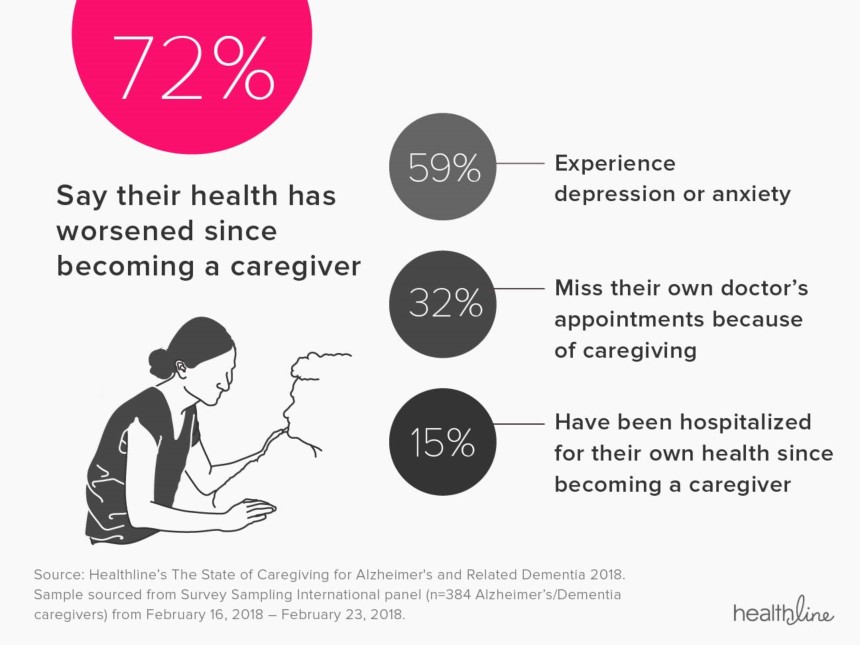
Indeed, clinical evidence suggests that fluctuating ovarian hormones are associated with an increased risk of depression. Women experience depression almost twice as often as men. And the difference is obvious only in the reproductive age.
Some women experience severe affective symptoms during the late luteal phase of the menstrual cycle, when progesterone and its metabolite, allopregnanolone, rise gradually and then fall rapidly. During menstruation, estrogen is at its lowest and brain activity tends to decrease. During a decrease in ovarian hormones, namely in the postpartum period, during menopause, there is a high risk of mood changes and depression.
However, during ovulation, estrogen levels are high, so brain activity is at its peak. During this period, the female representatives are stress-resistant and tolerant to pain.
More and more often you can hear from a woman: "I have a wonderful family, no financial worries, everything is very good, but severe depression.
" And the reason is in progesterone, or rather, in its absence, - Dr. Huber gives an example from practice in his lecture “Aging from the point of view of gynecology and reproductive medicine”. - I urge not to treat such women with psychotropic drugs. It is necessary to check the hormones and, if necessary, prescribe progesterone to the patients. And you will see that the hormonal balance will provide a mood-lifting effect.”
Disappointing statistics
After the age of 45, women begin to experience depression more often. Experts in the field of psychosomatics say that this is easy to explain. So, by the age of fifty, children leave their parental nest, a woman is left alone with a man. It also affects the decrease in sexual activity.
But the main reason is that at this stage of life, progesterone starts to decline. Namely, this hormone has a psychotropic effect on the body of a woman. For these reasons, menopause is often associated with depression. We should also not forget that the ovaries are responsible not only for mood changes, but also for accelerated biological aging.
We should also not forget that the ovaries are responsible not only for mood changes, but also for accelerated biological aging.
- Photo
- Getty Images
How to avoid depression
So now we understand the importance of hormone balance for mental health. But what to do about it? To maintain natural hormone levels follow these simple guidelines:
-
follow a healthy lifestyle . Good sleep (at least eight hours), proper nutrition with a minimum sugar content and no caffeine, moderate exercise are important;
-
try to minimize your stress levels . Self-regulation skills are useful for this: meditation, relaxing and breathing practices;
-
seek natural stimulation of pleasure hormones . Hugs, sex, delicious food, communication with children will help;
-
regularly undergo a medical examination.

Anna Gerasimenko
PMS and depression - HealthInfo
It is known that there are about 150 symptoms of premenstrual syndrome (PMS). This unpleasant condition is familiar to approximately 80% of all women (and their families), but only approximately 10% suffer from it for real, often with severe symptoms of depression.
Many women habitually associate nervousness, mood swings, depression, aggression with the menstrual cycle. But this relationship does not always exist. Can't changes in a woman's mood be related, for example, to weather conditions or occupation? How do you know when it's time to ask for help?
Depends on the weather…
“When we do research related to PMS, many women report that they generally feel a little better in the spring and summer (closer to summer), and worse in the winter,” says Jean Endicott, PhD, Professor of Clinical Psychology and Psychiatry at Columbia University.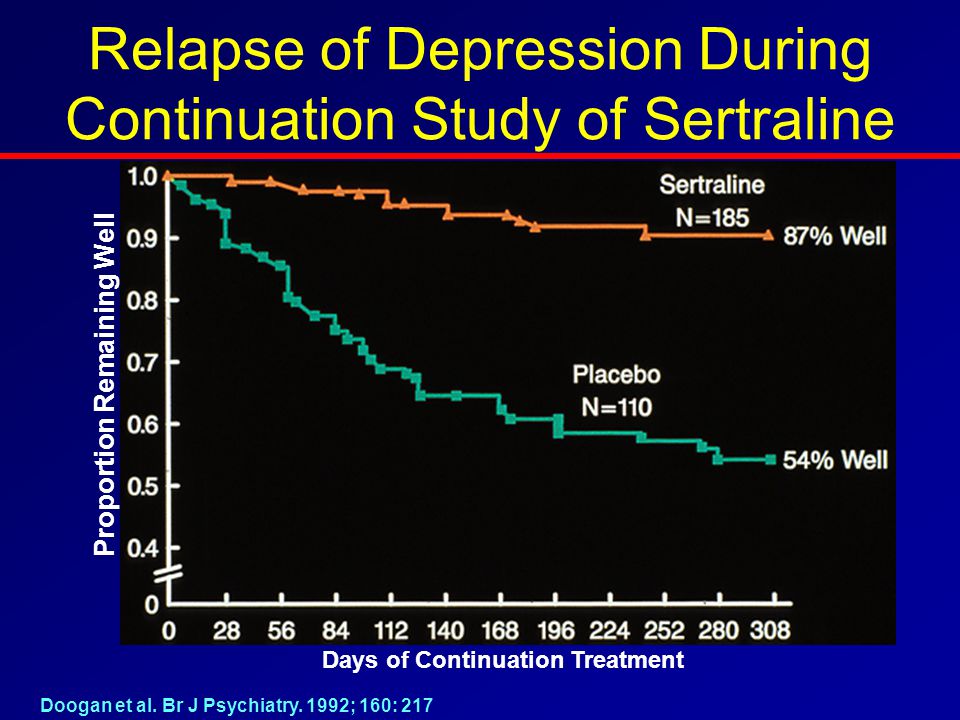 “That is, in itself, the connection between the mental state of a woman and the current season clearly exists, although there is no scientific justification for this.”
“That is, in itself, the connection between the mental state of a woman and the current season clearly exists, although there is no scientific justification for this.”
Perhaps this is due to the fact that there are more sunny days in summer, or because this season women have more opportunities to be outdoors and are more physically active, and physical activity is known to be a good remedy for depression. In winter, there are fewer such opportunities. In addition, scientists believe that women who are dependent on seasonality may be partially dependent on circadian rhythms.
Circadian rhythms are biological cycles that repeat every 24 hours and include periods of wake and sleep, activity and rest, hunger and food intake, and fluctuations in hormone levels and body temperature. How strongly all these rhythms affect the condition of a woman, in all likelihood, depends on her individual characteristics.
PMS, depression… or is that the nature?
Nevertheless, one should not treat one's mood lightly, just as one should not raise a panic ahead of time.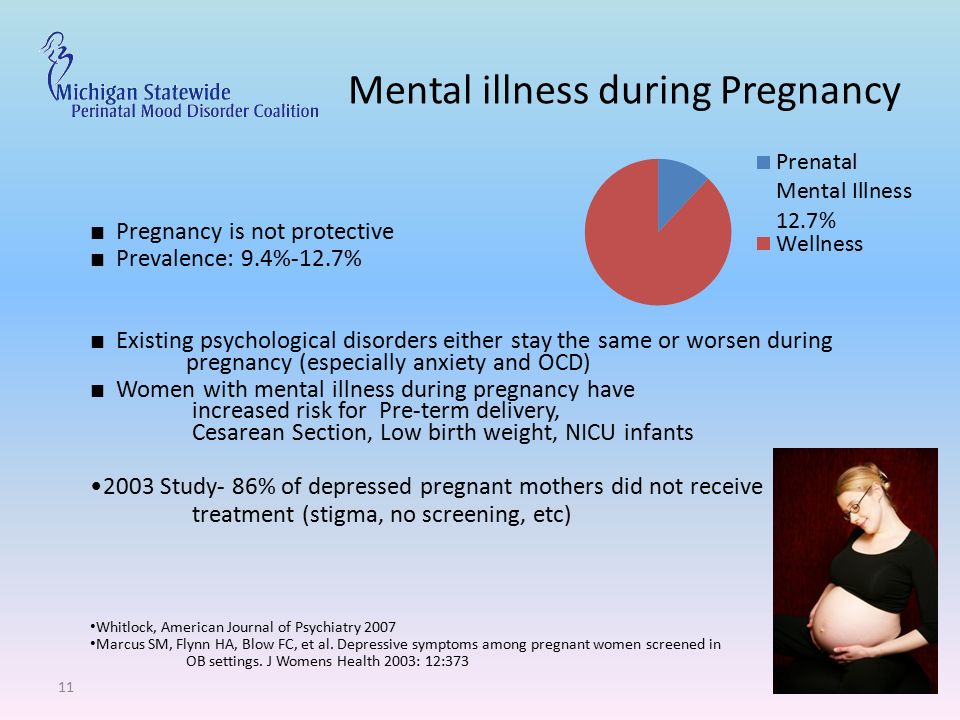 It is important to understand why irritability is replaced by tearfulness, and quiet "bright" sadness suddenly turns into "black longing".
It is important to understand why irritability is replaced by tearfulness, and quiet "bright" sadness suddenly turns into "black longing".
If you are prone to mood swings or feel down, try keeping a diary for three months in which you record absolutely every change in your mood every day.
Buy a calendar and chart daily mood swings: up and down, happy, sad, tired, euphoric, angry, irritable. But only this needs to be done every day, without waiting for the mood to deteriorate sharply or only when menstruation approaches.
Time to see a doctor?
If your diary shows that depression is indeed related to your monthly cycle, how do you know if you should seek medical help? Try to answer questions:
- Are you not just irritable at this time, but do you get into conflicts on any occasion with family members and make scandals for them?
- Are you unable to work productively and enjoy family life at this time?
- Do you have difficulty performing your daily functions, change your eating habits or lose your appetite, or do you sleep poorly?
- Do you experience severe anxiety or bouts of self-criticism?
- Do you have thoughts of death or suicide?
If you answered yes to several of these questions (especially the last one), see your doctor. If your cycle symptoms are really starting to interfere with your work or personal life, it's time to seek professional help.
If your cycle symptoms are really starting to interfere with your work or personal life, it's time to seek professional help.
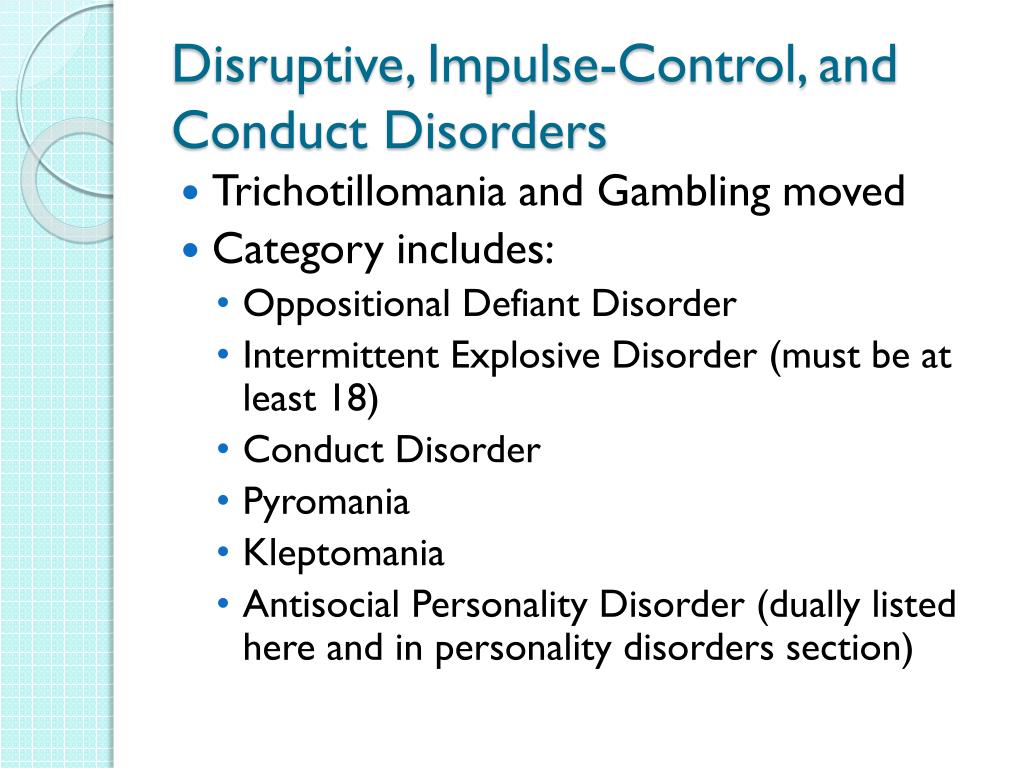
Fighting PMS is a must
There are several options for dealing with depression associated with PMS, which one to choose - the doctor will advise. This, for example, can be a course of cognitive behavioral therapy or light therapy. It is possible that a course of antidepressants or other drugs will be prescribed (on a strictly individual basis).
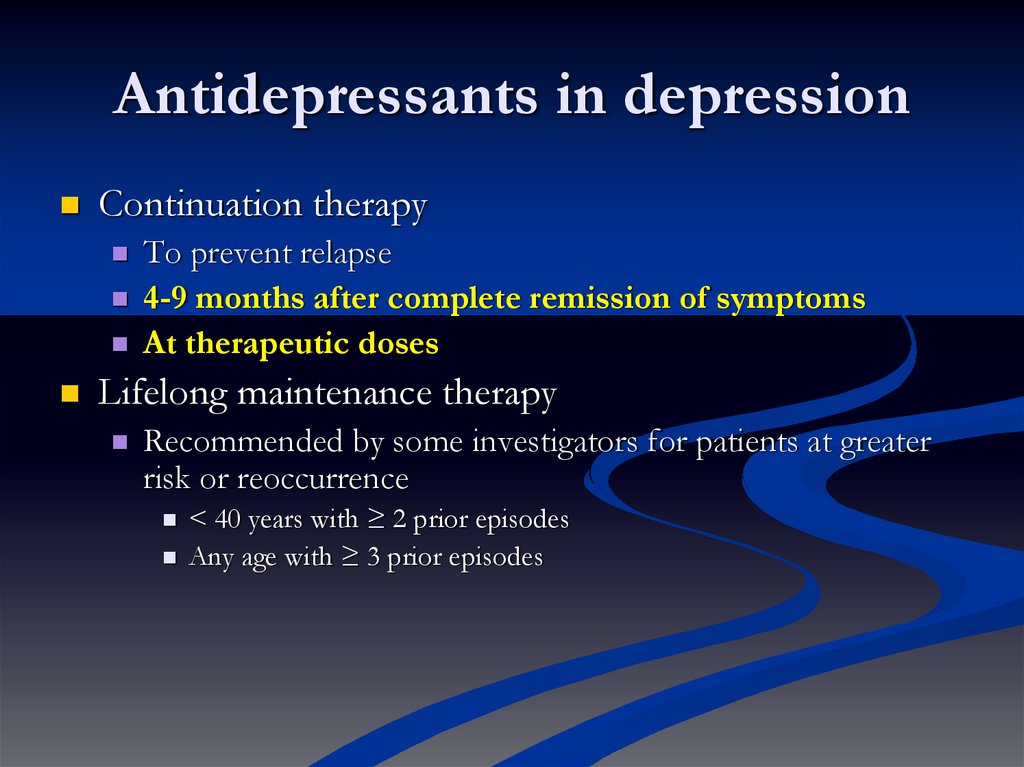
Antidepressants
Antidepressants of the SSRI group (selective serotonin reuptake inhibitors) are sometimes prescribed in such cases. They elevate mood by increasing the brain's use of chemicals called serotonin, which are responsible for transmitting impulses between cells (neurotransmitters). SSRIs have become the most popular treatment for depression because they are proven to be highly effective and have fewer side effects. The intake of such drugs begins on the 14th day of the cycle and stops with the onset of menstrual bleeding. As a rule, several weeks pass before the onset of a lasting effect, but in women suffering from depressive conditions due to PMS, it occurs faster. Remember that only a doctor can give you medicine!
As a rule, several weeks pass before the onset of a lasting effect, but in women suffering from depressive conditions due to PMS, it occurs faster. Remember that only a doctor can give you medicine!
Cognitive behavioral therapy
Cognitive behavioral therapy can help develop skills to manage depression and change moods associated with the menstrual cycle. This method is based on ideas, according to which the feelings and behavior of a person are determined not by the situation in which the person finds himself, but by his perception of this situation. This technique can prompt a woman to sometimes very simple methods of correcting her lifestyle and behavior, for example, not to plan difficult work these days, or attend relaxing massage courses and not skip yoga classes.
It is useful to make a list of things to do and things in advance that are pleasant for you and will really help you control yourself and cheer you up. Only the list needs to be drawn up in advance, because when the “moment” comes, you will have neither the desire nor the energy for this.