Dating someone with complex ptsd
When You Love Someone With Complex PTSD – Couples Institute Counseling Services
Skip to content When You Love Someone With Complex PTSDThis article gives a brief overview of some basics about Complex Post Traumatic Stress Disorder (CPTSD) and what you can do to support yourself as well as nurture your relationship when you love someone with Complex PTSD. You may be wondering if reading this article will be helpful to you.
- If your partner experienced significant trauma during childhood and you find yourself in awe of all that they are in spite of what they have been through, yet uncertain at times about how to provide the right kind of support, then this article is for you.
- If you recognize the wisdom within your partner that is derived from their experiences, but struggle to access your own wisdom when you see your partner suffering then this article is for you.
- Lastly, if you sometimes see your partner as someone who would benefit from healing work but, are not sure of the right place to start then this article is for you.
This article is about how to bring your best self to your relationship by forging one that is defined by security, consistency, and honesty as well as understanding the importance of your own self-care in cultivating these bonds.
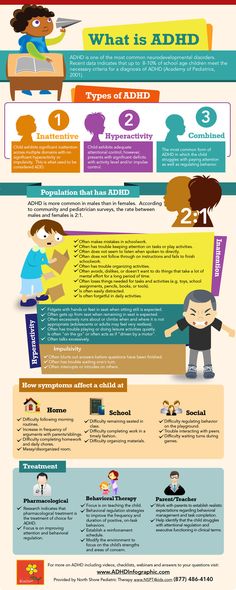
Complex Post Traumatic Stress Disorder (CPTSD) can occur when a person experiences multiple or prolonged traumatic experiences (Complex Trauma) over the course of a lifetime. Oftentimes, the traumas are relational in nature which means that the events occur within relationships during developmental periods such as childhood. For example, periods of childabuse or neglect and/or multiple ruptures or transitions with primary caregivers; such as multiple foster placements in which attachment bonds are ruptured or substance abuse or dependence by a primary caregiver.
There are two areas of human development that are impacted by Complex Trauma. When these areas are impacted it can result in CPTSD. They are:
- Attachment: the ways in which a person learns to have relationships with others
- Self-Regulation: the way in which a person handles self soothing in the face of stress.
Let’s look at both more closely.
In terms of Attachment, a child who experienced multiple adverse experiences such as abuse, domestic violence, neglect or community violence is likely to, as an adult, experience frequent mistrust, fear of abandonment, and difficulty feeling secure in their intimate relationships. The reason for this is that the template that was formed early on about how to have relationships was developed under the pretense that “those who love me either hurt me, or leave.” These recurring experiences often cause the belief that people are not safe to trust; leading to the lived experience of, “I’m hurt when you stay and I’m hurt when you leave:a double edged sword.”
Self-Regulation is a set of skills that are learned by internalizing the soothing actions of our caregivers when we are hurt, scared, hungry, sad etc. The capacity by which we are able to do this for ourselves as adults is largely made possible by the quality and quantity of that which was given to us.![]() The opportunities to learn from and observe adults practicing self regulation in ways that are healthy and nourishing for children with Complex Trauma often are minimal. Instead, the stress response system, the internal regulation system that is in charge of keeping us safe in the face of stressors, becomes overloaded due to a lack of opportunities to return to a calm state. In CPTSD this results in an elevated baseline and a stress response system that is overly sensitive to stressors. Thus the system responds by vacillating between extreme states of hyperarousal to hypoarousal (dissociation) rather than remaining within an ideal, more balanced “window of tolerance.” People who have not experienced trauma typically remain in this window within their normal day to day lives. This might account for why your partner may appear to have seemingly disproportionate reactions to stimuli that doesn’t impact you as severely: their system’s degree of sensitivity and reactivity is such that a smaller event can cause them great distress and dysregulation.
The opportunities to learn from and observe adults practicing self regulation in ways that are healthy and nourishing for children with Complex Trauma often are minimal. Instead, the stress response system, the internal regulation system that is in charge of keeping us safe in the face of stressors, becomes overloaded due to a lack of opportunities to return to a calm state. In CPTSD this results in an elevated baseline and a stress response system that is overly sensitive to stressors. Thus the system responds by vacillating between extreme states of hyperarousal to hypoarousal (dissociation) rather than remaining within an ideal, more balanced “window of tolerance.” People who have not experienced trauma typically remain in this window within their normal day to day lives. This might account for why your partner may appear to have seemingly disproportionate reactions to stimuli that doesn’t impact you as severely: their system’s degree of sensitivity and reactivity is such that a smaller event can cause them great distress and dysregulation.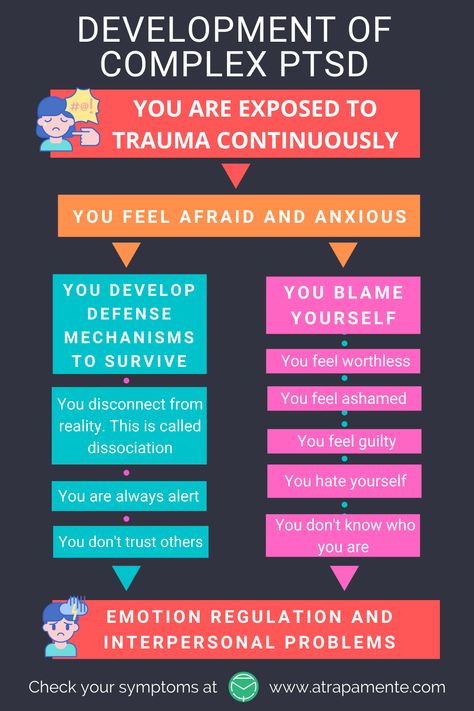
The hopeful news is that the medicine for CPTSD can be found within the healing power of relationships and within our brains’ incredible ability to create new templates for relationships by a process called neuroplasticity, our brain’s ability to make new neural connections throughout our lifetime. The incredible healing power of relationships as they relate to Complex Trauma has been well documented by neuroscientists such as Dr. Bruce Perry1, who specializes in the impacts of childhood trauma and neglect and its impact on neurodevelopment, and Dr. Daniel Siegel2 who has also well documented the process of neurodevelopment. What this means is that you and your partner have the ability to form a secure attachment in adulthood EVEN IF your partner has not yet experienced that in their life3 -VERY EXCITING!!! But where do you begin? It is important to know the following:
- You can not erase existing templates but you can create new ones.
- Your efforts should be patterned and repetitive, as these templates live in lower, less “plastic” ie. not as easily changed, parts of the brain that are only accessed and changed through doing things over and over again.
- You don’t need to figure this out on your own. Finding a couples therapist educated about Complex Trauma is recommended and can help facilitate the healing process.
Here are some other ideas you’ll want to consider:
-
- Be Consistent, be predictable: Repetition is the key to building a secure attachment. It also facilitates the ability to trust. For example, calling your partner every night before bed to say goodnight, this may seem simple, but it can have a profound effect on shaping a new, loving, and secure template of what a relationship can be in your partner’s brain.
- Know your boundaries: This is a big one and related back again to being consistent and predictable. What is and what is not in your control? If your partner is struggling with mood symptoms including anxiety or depression and struggling with self regulation, it is not your job to fix that, but you can encourage your partner to establish a relationship with a therapist or make an appointment with an existing one.
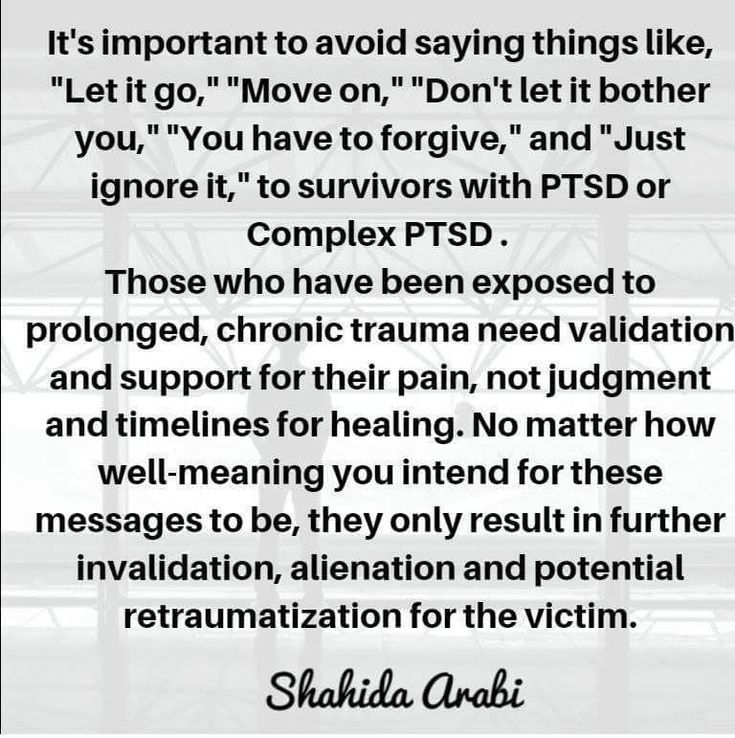
 It can be powerful to validate your partner’s suffering while simultaneously acknowledging that you do not have the power to make it all better. In all relationships it is important for each partner to own their own struggles and work on them independently from the relationship.
It can be powerful to validate your partner’s suffering while simultaneously acknowledging that you do not have the power to make it all better. In all relationships it is important for each partner to own their own struggles and work on them independently from the relationship. - Establish and keep up with your own self care plan: When we fall in love it is so easy to give and give and then one day we wake up and we realize, “Oops! I have given to everyone except me!” You have got to fill your own bucket. Keeping up with a routine that nourishes you and keeps you connected to yourself and those in your support system is crucial. You are modeling for your partner that it is okay to practice self care and encouraging the process called differentiation (an ongoing process of self-defining within the context of the relationship that is a key developmental milestone within relationship and is that which sets the stage for further development and deeper intimacy as your relationship progresses).
- Don’t try to explain, instead “connect and redirect”: Emotions are not logical, yet it is our tendency to try to explain our way through them. When your partner is in an emotional state of activation, remember, first connect by reflecting back what you hear them say, including their feelings. Listen and mirror without the intention of problem solving. Once your partner has expressed to you that they are feeling heard, ask them if they want support in problem solving (re-direct). Once you check for their interest, you may find that you have already helped enough!
- Do find out what is soothing to your partner: People who have experienced complex trauma are often well aware of what they do and do not like. Ask them their preferences, you may find out that your partner can not tolerate massage but loves a warm bath. If so, draw them a bath and draw it often! Remember: repetition, consistency, predictability.
- Practice consent in intimacy and beyond: Trauma is defined as an extreme loss of control to a perceived threat or life threatening situation.
 Healing for trauma survivors always includes establishing a sense of safety. A way to safety is though experienced control– practicing consent is a powerful vessel for this. This means asking permission before and during intimate encounters as well as throughout your day-to-day interactions, for example, “Is it okay if I move your things while I clean this room?”
Healing for trauma survivors always includes establishing a sense of safety. A way to safety is though experienced control– practicing consent is a powerful vessel for this. This means asking permission before and during intimate encounters as well as throughout your day-to-day interactions, for example, “Is it okay if I move your things while I clean this room?” - Anticipate events that could cause anxiety for your partner: Work together to create a safety plan. For example, if your partner feels anxious in social settings like big events such as a wedding, decide ahead of time where to sit during the ceremony and have a signal that you can give to one another if your partner needs a break. This can be a good opportunity to step outside and get a breather, check in about how you are both doing, and make adjustments to your plan as necessary.
- Don’t take it personally: Your partner has been through a lot. It is likely that if your partner has a reaction to something that you do or say that it has less to do with you than you think and more to do with what that thing reminds them of.
 When this happens take a deep breath and do your own physiological self soothing, then when you feel regulated check back in, try to think of these moments as opportunities to learn more about what your partner’s triggers are so that you can work with them in a thoughtful and meaningful way.
When this happens take a deep breath and do your own physiological self soothing, then when you feel regulated check back in, try to think of these moments as opportunities to learn more about what your partner’s triggers are so that you can work with them in a thoughtful and meaningful way.
Remember, it all goes back to the incredible healing power of relationships and the bonds that are formed when we are present and available for one another. Even as therapists we can get stuck in the trap of thinking that we should be able to fix it all right then and there and we jump too quickly to problem solving. Yet it is always meaningful to take a step back and remember that the key to building a secure relationship is not in your ability to offer a quick fix. Rather, it lies within your ability to take your time, be consistent, and show your commitment to being there again and again. If past trauma is impacting you or your relationships and you need help, reach out to us, establishing a relationship with a therapist can be the first step in creating a path to healing that can seem overwhelming and uncertain, more clear, manageable, and supportive.
- Perry, Bruce Duncan, and Maia Szalavitz. The Boy Who Was Raised as a Dog: and Other Stories from a Child Psychiatrists Notebook: What Traumatized Children Can Teach Us about Loss, Love, and Healing. Basic Books, 2017.
- Siegel, Daniel J., and Tina Payne. Bryson. The Whole-Brain Child. Constable & Robinson, 2012.
- (David Wallin breaks this down beautifully in his book, Attachment in Psychotherapy)Wallin, David J. Attachment in Psychotherapy. Guildford Press, 2015.
To receive more articles and free tools as they come out sign up for our newsletter here
- Name
Name
- Email*
Dana Hartman
Dana has been practicing Marriage and Family Therapy since 2013 and has over 15 years of experience providing education and healing services for individuals and their families who have experienced being marginalized in various ways. Because of this Dana has a special interest in working with adults who experienced childhood trauma as well as healing after incarceration.
Because of this Dana has a special interest in working with adults who experienced childhood trauma as well as healing after incarceration.
Go to Top
Healing and Growing With Your Partner – Bridges to Recovery
April 26, 2018, Tyler DabelBridges to Recovery
Dating someone with complex PTSD is no easy task. But by understanding why the difference between traditional and complex PTSD matters and addressing PTSD-specific problems with treatment, you and your loved one will learn what it takes to move forward together and turn your relationship roadblocks into positive, lifelong learning experiences.
Being in a relationship means being open with your partner and sharing life experiences, both the good and the bad. When you’re dating someone with complex post-traumatic stress disorder, however, it might sometimes feel like there is more bad than good.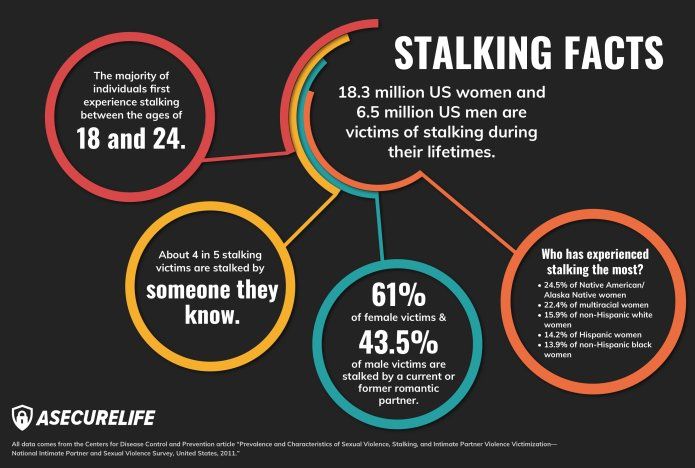 Your partner’s anxiety, paranoia, and on-edge nature can make them extremely volatile, leaving you wondering how you can possibly help. And when it comes to complex PTSD, it is likely influencing the way that your partner perceives the world—and your relationship—in a negative way.
Your partner’s anxiety, paranoia, and on-edge nature can make them extremely volatile, leaving you wondering how you can possibly help. And when it comes to complex PTSD, it is likely influencing the way that your partner perceives the world—and your relationship—in a negative way.
You might have accepted that you will never have a “normal” relationship, believing that the turbulence of your relationship is something that simply needs to be accepted. But in truth, guiding your loved one in the direction of residential treatment can pave the way to so much more. Through professional guidance and support, both you and your partner can learn how to deal with the unique challenges of PTSD in the context of a relationship and use them to drive personal growth.
Why the Difference Between Traditional and Complex PTSD Matters
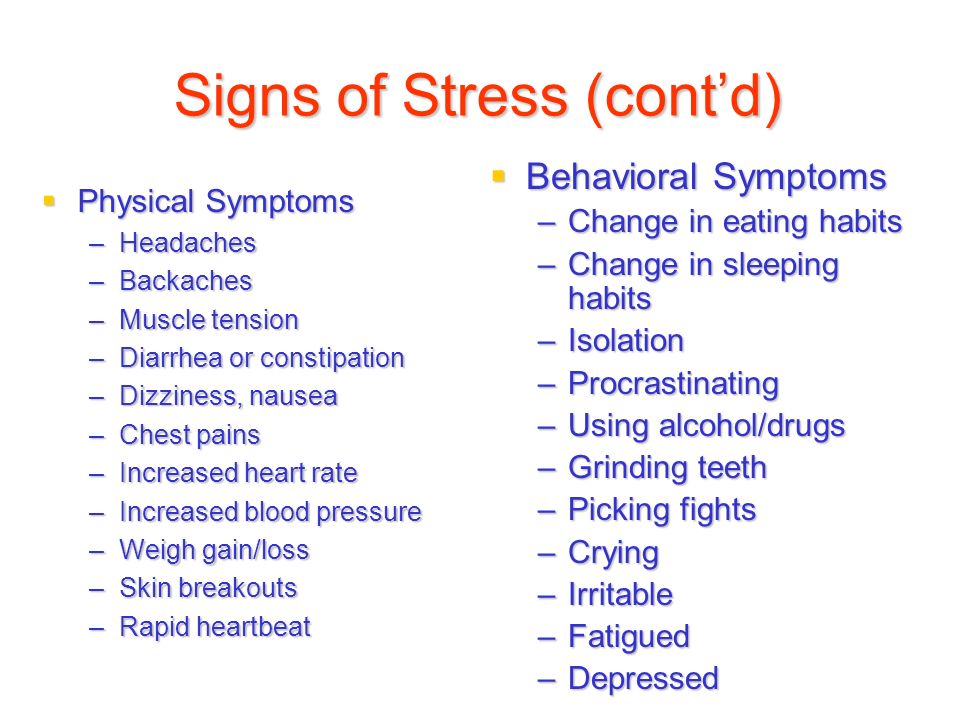
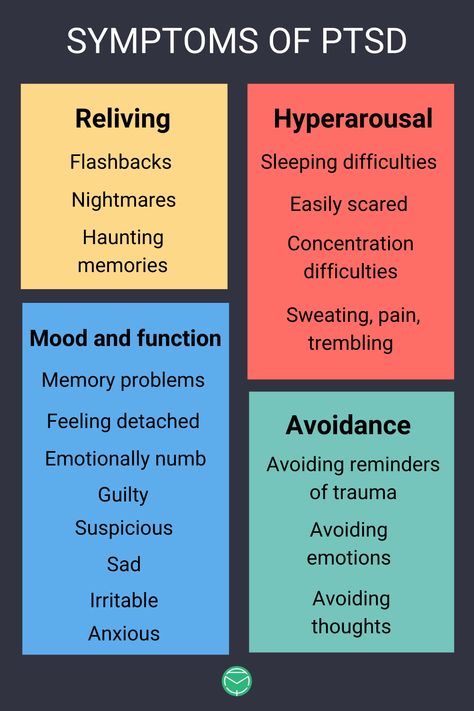
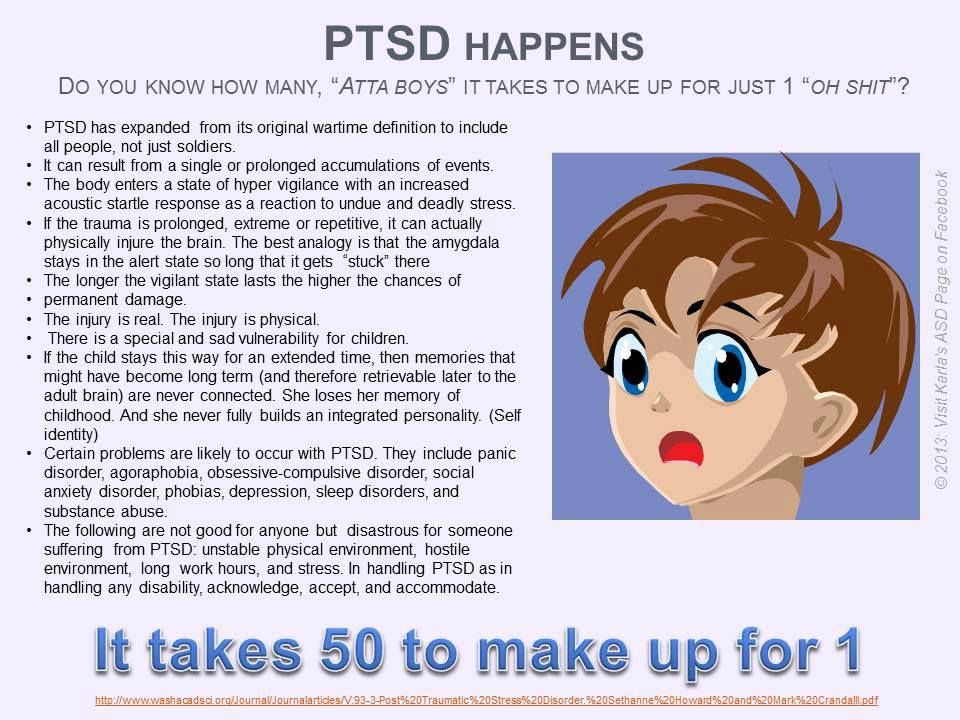
Traumatic events are never easy, and the coping period after a traumatic experience is painful and difficult. Both our bodies and minds try to regain their balance as we attempt to move forward and continue our lives.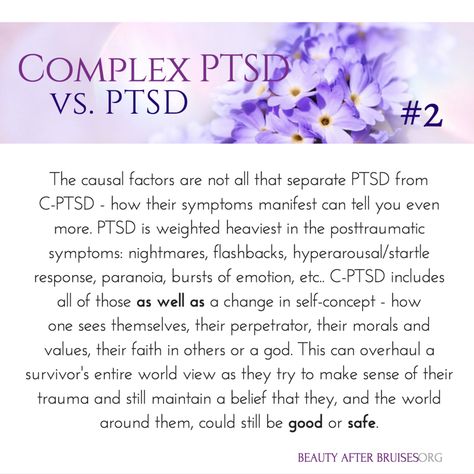 But for those with PTSD, this period never quite ends. The lingering effects of trauma lead to hyperarousal, the re-living or traumatic memories, and negative changes in feelings and beliefs.
But for those with PTSD, this period never quite ends. The lingering effects of trauma lead to hyperarousal, the re-living or traumatic memories, and negative changes in feelings and beliefs.
And when this trauma repeats itself, such as in the case of repeated personal victimization, the traditional PTSD symptoms began to develop into something even more deep-rooted. These situations are classified as complex PTSD.
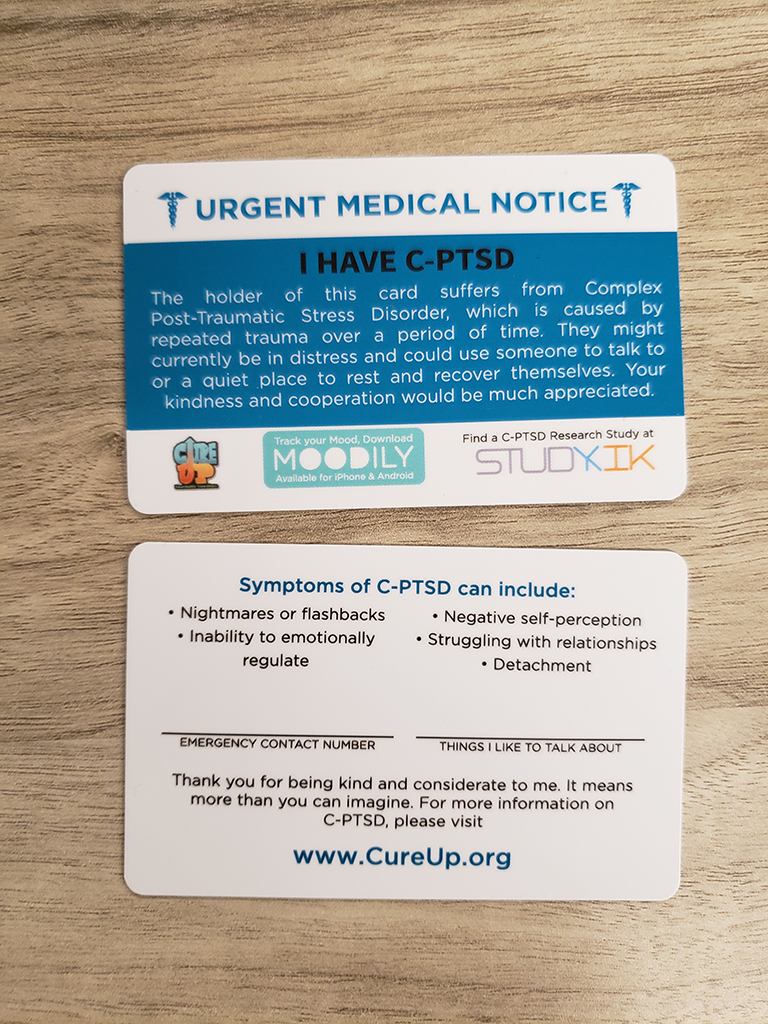
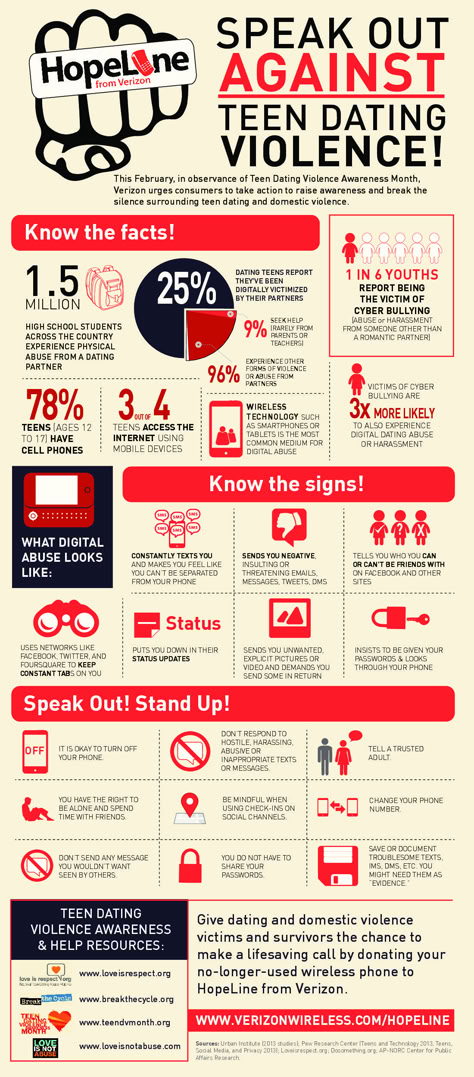
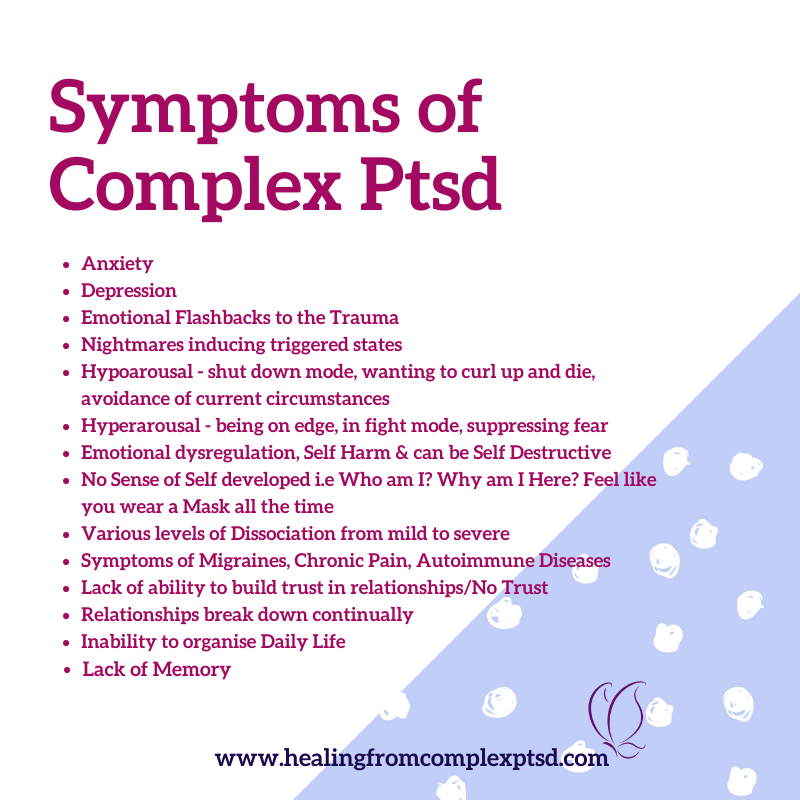
Common symptoms of complex PTSD are:
- Difficulty with emotional regulation
- Dissociation
- Negative self-perception
- Trouble relating to others
- Distorted views of the perpetrator of the trauma
- Loss of faith or hope
These are problematic symptoms in any situation, but in the context of a relationship, they can be even more destructive. You might feel like your partner is drifting away, isolating themselves from their support systems and sinking further down into their negative emotions and memories. Even when you reach out, they might react in an extremely emotional manner, and may become overly critical of themselves or your relationship.
Given the deep-rooted nature of trauma, especially in the case of complex PTSD, it can be nearly impossible to overcome these relationship struggles without professional help. Your attempts to break through to them might be rooted in good intentions, but you might be doing more harm than good by fueling their insecurities and desire for isolation. For this reason, a professional treatment program is necessary, both for your partner’s mental well-being and for the health of your relationship.
Begin Your Recovery Journey.
877-727-4343Addressing PTSD-Specific Problems with Treatment
Isolation, heightened emotional responses, and negative self-perception—these are all common ways that PTSD can manifest in a person, and all of these symptoms can cause damage to a relationship. However, with the right treatment, both you and your loved one will be able to address these issues in a healthy way.
- Eye Movement Desensitization and Reprocessing (EMDR) therapy is one way that people struggling with PTSD can relieve themselves of the distress attached to their trauma.
 Through carefully guided therapy, they learn to focus on both their internal memories and external stimuli, creating new positive associations that draw the attention away from negative emotions and loosen the grip that they have on their psyche. These benefits will help them focus on engaging positive emotions and relationships.
Through carefully guided therapy, they learn to focus on both their internal memories and external stimuli, creating new positive associations that draw the attention away from negative emotions and loosen the grip that they have on their psyche. These benefits will help them focus on engaging positive emotions and relationships. - Support groups and networks can help your loved one break out of the pattern of isolation that their PTSD constantly pushes them into. During treatment, they will learn how to identify, use, and sustain support networks. These are invaluable skills that will help them better integrate into the world and engage in personal relationships in a way that is healthy for them and everyone involved.
- Holistic therapies like yoga can help promote the grounded sense of control and body awareness that is so beneficial for PTSD recovery. Many people think of it as a way to de-stress, but for a loved one with complex PTSD, it’s so much more—it will help them develop a sense of strength and establish a positive relationship with their body.
 And in order to establish a healthy, positive relationship with another person, you need to be able to create one with yourself.
And in order to establish a healthy, positive relationship with another person, you need to be able to create one with yourself.
By addressing the driving forces of complex PTSD, treatment can help your partner learn to cope with their struggle in a positive way that promotes personal growth. And with so many options for support through family and couples therapy, you will be able to contribute to this growth both in your partner and yourself.
Seeking Treatment and Moving Forward Together
In order to move forward together, both you and your partner need to learn the most effective and adaptive ways of addressing the problems that complex PTSD creates in your relationship. Through a comprehensive residential treatment program, you will be connected to the professional tools and supports necessary to address this mental health challenge. After these unique learning therapeutic learning experiences, you will have the positive energy and outlook to move past the negativity that has held you both back, allowing you to focus on developing a lifelong bond with each other.
Bridges to Recovery offers comprehensive treatment for people struggling with mental health disorders as well as co-occurring substance use disorders, eating disorders, and process addictions. Contact us to learn more about our renowned Los Angeles programs and how we can help you or your loved one start the journey toward healing.
PTSD
") end if %>
Variant of Acrobat Samana Gaze | Acrobat Reader Samana Download
PTSD is a normal response
for severe traumatic events.
This booklet deals with signs,
symptoms and treatments for PTSD.
New York State
Department of Mental Health
Have you experienced a terrible and dangerous event? Note please, those cases in which you recognize yourself.
- Sometimes, out of the blue, everything that happened to me is happening again.
I never know when to expect it again.
- I have nightmares and memories of the terrible incident which I have experienced.
- I avoid places that remind me of that incident.
- I jump on the spot and feel uneasy at any sudden movement or surprise. I feel alert all the time.
- It's hard for me to trust someone and get close to someone.
- Sometimes I just feel emotionally drained and deaf.
- I get angry very easily.
- I am tormented by guilt that others died, but I survived.
- I sleep poorly and experience muscle tension.
PTSD is a very serious condition that needs to be treated.
Many people who have experienced terrible events suffer from this disease.
It is not your fault that you fell ill, and you should not suffer from it.
Read this booklet to find out how you can be helped.
You can get well and enjoy life again!
What is post-traumatic stress disorder (PTSD/PTSD)?
PTSD is a very serious condition. PTSD symptoms may occur in a person who has experienced a terrible traumatic event. This disease is susceptible medical and therapeutic treatment.
PTSD can occur after you:
- Have been a victim of sexual abuse
- Have been a victim of physical or emotional domestic violence
- Victim of a violent crime
- Been in a car accident or plane crash
- Survived a hurricane, tornado, or fire
- Were at war
- Survived a life-threatening event
- Witnessed any of the above events
If you have post-traumatic stress disorder, you often have nightmares or memories associated with the event. you try to hold on away from anything that might remind you of the experience.
You are bitter and unable to trust or care for others. You are always on your guard and see a hidden threat in everything. You become not by itself, when something happens suddenly and without warning.
When does PTSD start and how long does it last?
In most cases, post-traumatic stress manifests itself approximately three months after the traumatic event. In some cases, signs Post-traumatic stress symptoms only show up years later. Post-traumatic Stress affects people of all ages. Even children are not immune from it.
Some get better after six months, others may suffer from it illness for much longer.
Am I the only one with this disease?
No, you are not alone. Every year, 5.2 million Americans suffer from PTSD.
Women suffer from this disease two and a half times more often than men. The most common traumatic events that cause PTSD in men are: rape, participation in hostilities, abandonment and abuse in childhood. The most traumatic events in women are rape, sexual molestation, physical assault, threat weapons and childhood abuse.
What other conditions can accompany PTSD?
Common depression, alcoholism and drug addiction, or other anxiety disorders. The likelihood of successful treatment increases if these comorbidities to identify and treat in time.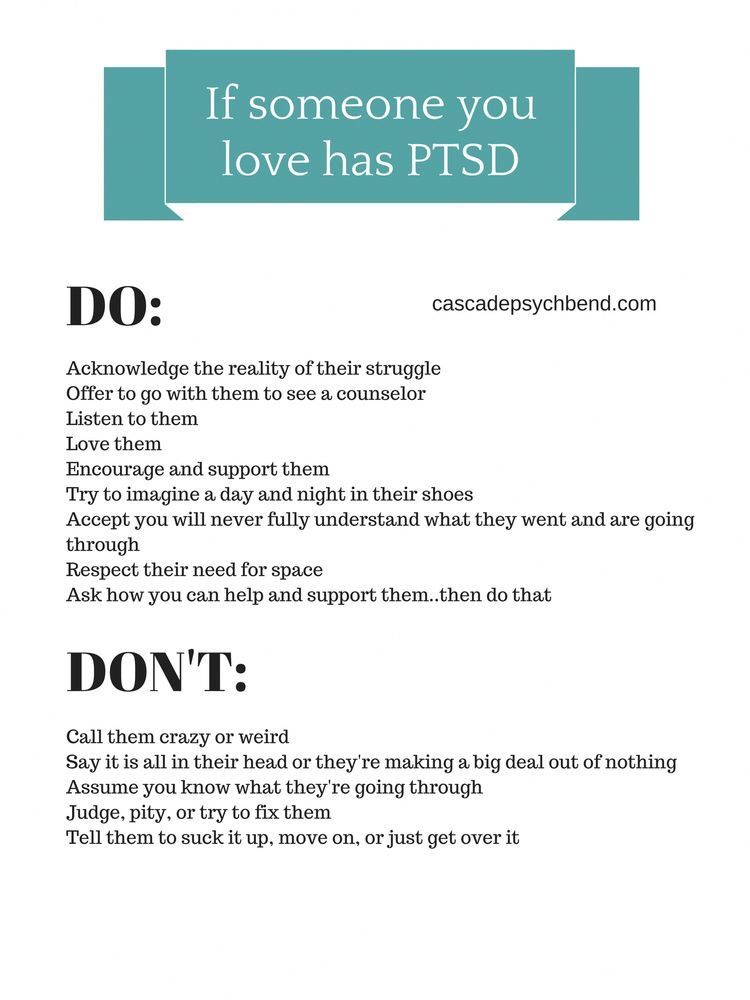
Frequent headaches, gastroenterological problems, problems with the immune system, dizziness, chest pain or discomfort in other parts of the body. It often happens that a doctor treats physical symptoms, unaware that their cause lies in PTSD.
The National Institute of Mental Health (NIMH) recommends therapists to learn from patients about experiences of violence, recent losses and traumatic events, especially when symptoms persist are returning. After diagnosing PTSD, it is recommended to refer patient to a mental health specialist who has experience in the treatment of patients with PTSD.
What should I do to help myself in this situation?
Talk to your doctor and tell him about your experience, and how you feel. If you are visited by terrible memories, overcomes depression and sadness if you have trouble sleeping and constantly embittered - you should tell your doctor about all this. Tell him Are any of these conditions preventing you from doing your daily activities? lead a normal life. You may want to show this booklet to your doctor. This may help explain to him how you feel. Ask your doctor examine you to make sure there are no physical illnesses.
You may want to show this booklet to your doctor. This may help explain to him how you feel. Ask your doctor examine you to make sure there are no physical illnesses.
Ask your doctor if he has had patients with post-traumatic stress. If your doctor does not have a special preparation, ask him for directions to doctor with relevant experience.
How can a doctor or psychotherapist help me?
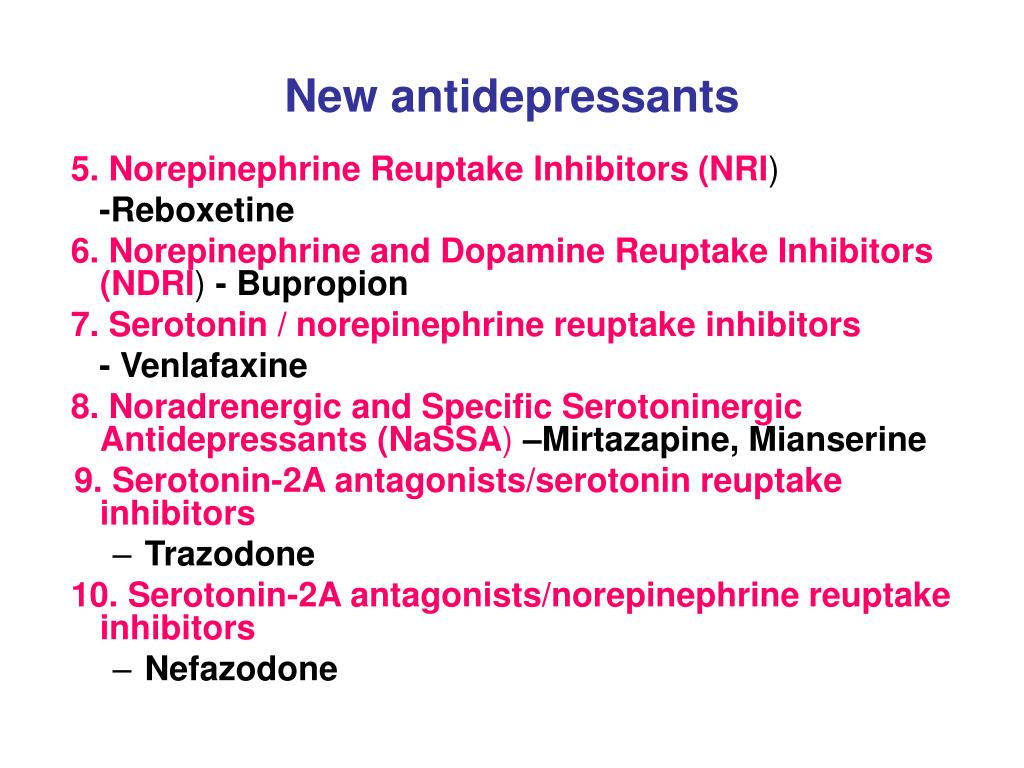
Your doctor may prescribe medicine to help reduce your fear or tension. However, it should be borne in mind that usually several weeks before the medicine starts to work.
Many PTSD sufferers benefit from talking with a professional or other people who have experienced traumatic events. This is called "therapy". Therapy will help you get over your nightmare.
One man's story:
"After I was attacked, I He constantly felt fear and depression, became irritable. I couldn't sleep well and lost my appetite. Even when I tried not think about what happened, I was still tormented nightmares and terrible memories.
Even when I tried not think about what happened, I was still tormented nightmares and terrible memories.
“I was completely at a loss and didn't know what to do. one buddy advised to see a doctor. My doctor helped me find a specialist in post-traumatic stress."
“I needed a lot of strength, but after medication and a course of therapy, I gradually come to my senses. It’s good that I called my doctor then.”
PTSD and the military
If you are in the military, you have probably been in combat. You, probably got into terrible and life-threatening situations. They shot at you you have seen your friend shot, you have seen death. experienced you events can cause PTSD.
Experts say that PTSD occurs:
- Nearly 30% of Vietnam War veterans
- Nearly 10% of Gulf War veterans (Operation Desert Storm)
- Almost 25% of veterans of the war in Afghanistan (operations "Introducing freedom") and veterans of the war in Iraq (operations "Iraqi Freedom")
Other factors of the military situation can serve as an additional stress to and so stressful situation and can contribute to the development of PTSD and other mental problems. Among these factors are the following: your military specialty, the political aspects of the war, where the battle takes place and who your enemy is.
Among these factors are the following: your military specialty, the political aspects of the war, where the battle takes place and who your enemy is.
Another reason that contributes to PTSD in military personnel can be Military Sexual Assault (MST) – any form of sexual harassment or sexual abuse while serving in the military. MST can happen with men and women, and can occur in peacetime, during war training or during the war.
Veterans Affairs (VA) health care approximately:
- 23 out of 100 women (23%) report sexual violence during military service
- 55 out of 100 women (55%) and 38 out of 100 men (38%) were exposed to sexual harassment while serving in the army
Although the trauma of sexual assault is more common in the military among women, more than half of veterans who have experienced sexual trauma violence in the army - it's men.
Remember, you can get the help you need right now:
Tell your doctor about your experience and how you feel. If your doctor does not have special training in the treatment of PTSD, ask him for a referral to a doctor who has relevant experience.
If your doctor does not have special training in the treatment of PTSD, ask him for a referral to a doctor who has relevant experience.
PTSD research
To help those suffering from PTSD, the National Institute of Conservation Mental Health (NIMH) supports research into the study of PTSD, as well as other thematically related to PTSD research on problems anxiety and fear. The challenge for research is to find new ways to help people cope with trauma, as well as find new treatment options and, The main thing is to prevent disease.
Research on possible risk factors for PTSD
Today, the attention of many scientists is focused on genes that play a role in having terrible memories. Understanding the mechanism of "creation" of scary memories can help improve or find new ways to alleviate symptoms of PTSD. For example, PTSD researchers have identified genes that are responsible for:
Statmin is a protein involved in the formation of terrible memories. During one experiment, mice were placed in environment designed to instill fear in them. In this situation mice lacking the statmin gene, in contrast to normal mice were less likely to "freeze" - i.e. exercise natural defensive response to danger. Also in the environment designed to evoke innate fear in them, they demonstrated it to a lesser extent than normal mice, more willingly mastering the open "dangerous" space. 1
During one experiment, mice were placed in environment designed to instill fear in them. In this situation mice lacking the statmin gene, in contrast to normal mice were less likely to "freeze" - i.e. exercise natural defensive response to danger. Also in the environment designed to evoke innate fear in them, they demonstrated it to a lesser extent than normal mice, more willingly mastering the open "dangerous" space. 1
GRP (gastrin-releasing peptide/GRP) - signal substance brain released during emotional events. At in mice, GWP helps control the fear response, and lack of GWP can lead to a longer memory of fear. 2
Scientists have also discovered a variant of the 5-HTTLPR gene that controls serotonin (a brain substance associated with mood), which, as it turns out, feeds the fear response. 3 It seems that, like in the case of other mental disorders, in the development of PTSD different genes are involved, each of which contributes to the formation of the disease.
Understanding the causes of PTSD can also be helped by studying different areas brain responsible for fear and stress. One of these areas is cerebellar amygdala, responsible for emotions, learning and memory. It turned out that she plays an active role in the emergence of fear (or other words, "teaches" to be afraid of something, for example, to touch a hot stove), as well as in the early phases of fear repayment (or in other words, "teaches" Do not be scared). 4
The retention of faded memories and the weakening of the initial fear reaction are associated with the prefrontal cortex (PFC / PFC) of the brain, 4 responsible for decision making, problem solving and situation assessment. Each zone PFC has its own role. For example, when the PFC believes that a stressor is amenable to control, the medial prefrontal zone of the PFC suppresses the anxiety center deeply in the brainstem and controls the response to stress.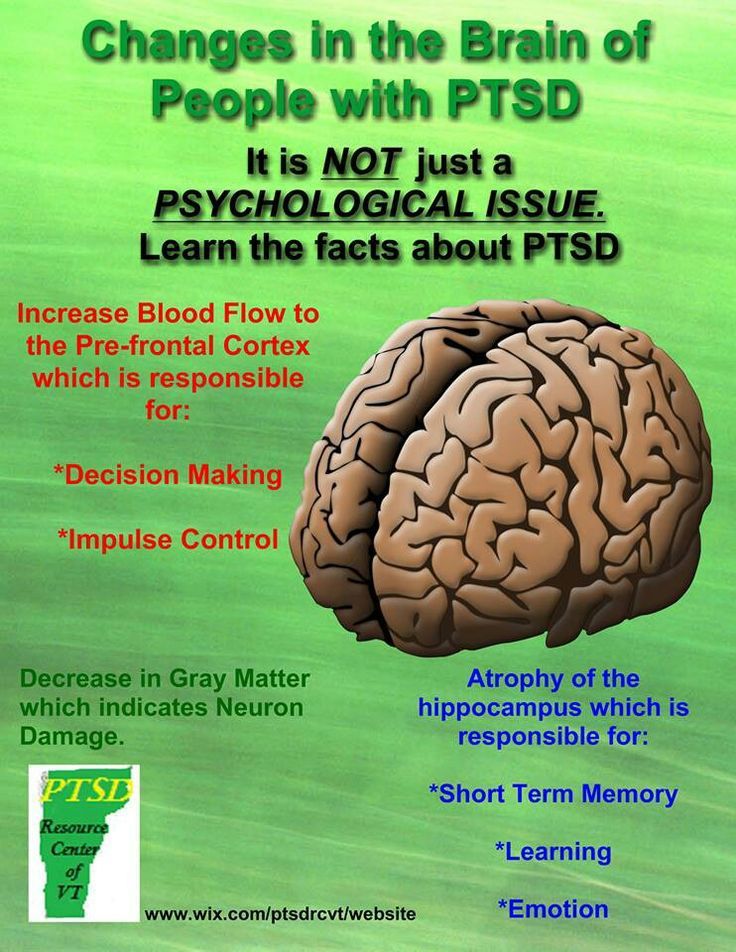 5 Ventromedial PFC helps maintain long-term fading of fearful memories, and her ability to perform this feature can be affected by its size. 6
5 Ventromedial PFC helps maintain long-term fading of fearful memories, and her ability to perform this feature can be affected by its size. 6
Individual differences in genes or characteristics of regions of the brain brain can only set the stage for PTSD, but by themselves do not cause no symptoms. environmental factors such as childhood trauma, head trauma or mental illness in family, favor the development of the disease and increase the risk of disease, affecting the brain in the early stages of its growth. 7 Except In addition, how people adapt to trauma is likely to be influenced by and characteristics of character and behavior, such as optimism and a tendency to consider problems in a positive or negative way, as well as social factors such as availability and use of social support. 8 Further research may show what combination of these factors or what other factors will allow ever predict who has a traumatic event cause PTSD, and who doesn't.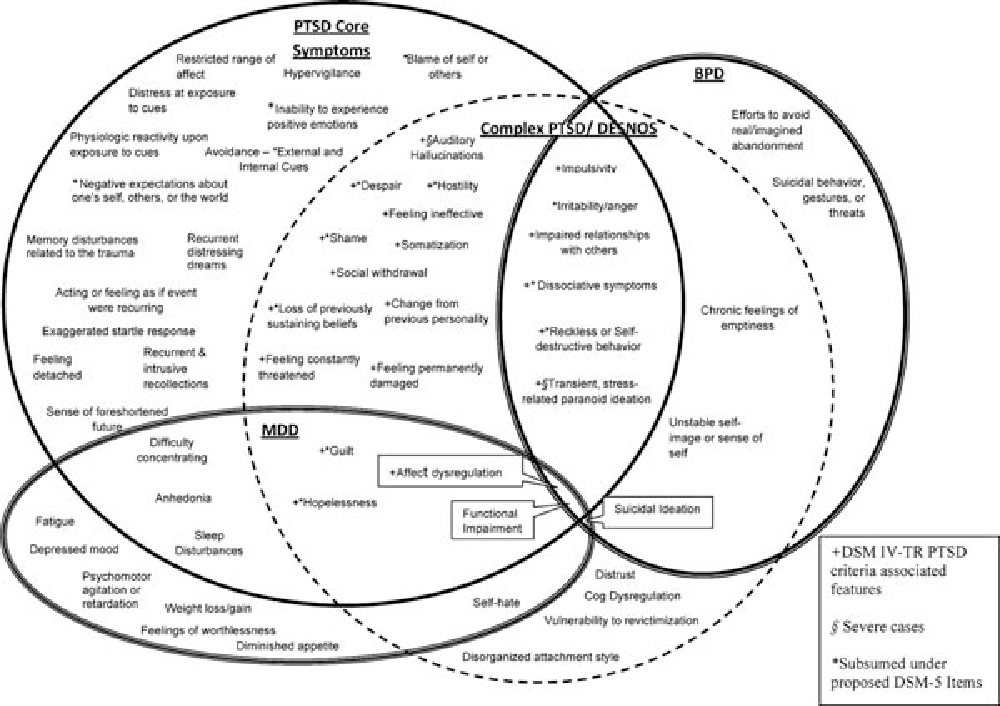
PTSD research
Currently, psychotherapy is used in the treatment of PTSD ("talk" therapy), drugs or drug-therapeutic combination.
Psychotherapy
Cognitive behavioral therapy (CBT) helps you learn differently think and react to frightening events that are the impetus for development PTSD, and can help bring the symptoms of the disease under control. There are several types cognitive behavioral therapy, including:
"Push" method - uses mental images, notes or visiting a place experienced trauma to help those affected face the overwhelming their fear and take control of it.
Behavior restructuring (cognitive restructuring) - encourages survivors of a traumatic event express depressing (often erroneous) thoughts about experienced trauma, challenge these thoughts and replace them with more balanced and appropriate.
Implementation in a stressful situation - teaches ways to reduce anxiety and the ability to cope with it, helping to reduce the symptoms of PTSD, and helps to correct the erroneous train of thought associated with the trauma experienced.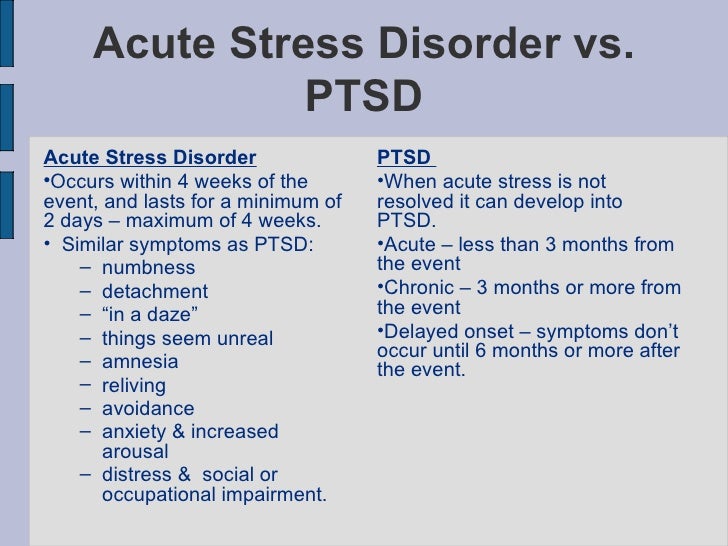 NIMH is currently conducting research to study the reaction brain response to cognitive behavioral therapy versus response sertraline (Zoloft) - one of two drugs recommended and approved US Food and Drug Administration funds (FDA) for the treatment of post-traumatic stress. This research may help find out why some people respond better to medications, and others for psychotherapy
NIMH is currently conducting research to study the reaction brain response to cognitive behavioral therapy versus response sertraline (Zoloft) - one of two drugs recommended and approved US Food and Drug Administration funds (FDA) for the treatment of post-traumatic stress. This research may help find out why some people respond better to medications, and others for psychotherapy
Drugs
Recently, in a small study, NIMH scientists found that if patients who are already taking a dose of prazosin (Minipress) at bedtime, add a daily dose, then this weakens the general symptoms of PTSD and stress reaction to reminders of the trauma experienced. 9
Another drug of interest is D-cycloserine (Seromycin), which increases the activity of a brain substance called N-methyl-D-aspartate, needed to pay off fear. During the study, which was attended by 28 people suffering from a fear of heights, scientists found that patients who received "push" therapy before a session D-cycloserine, showed lower levels of fear during the session compared to those who did not receive the drug. 10 Currently scientists study the effectiveness of the combined use of D-cycloserine and therapy for the treatment of post-traumatic stress.
10 Currently scientists study the effectiveness of the combined use of D-cycloserine and therapy for the treatment of post-traumatic stress.
Propranolol (Inderal), a beta-blocker drug, also under study whether it can be used to reduce post-traumatic stress and break the chain of scary memories. First experiments gave consoling results: it was possible to successfully weaken and, it seems, prevent PTSD in a small number of victims of traumatic events. 11
For example, in one preliminary study, scientists created a website self-help, based on the use of a psychotherapeutic method implementation in a stressful situation. First, patients with PTSD meet in person with doctor. After this meeting, participants can go to the site to find more information about PTSD and how to deal with the problem; their doctors may also visit the site to give advice or briefing. In general, scientists believe that therapy in this form - promising treatment for a large number of people suffering from PTSD. 12
12
Scientists are also working to improve methods for testing early treatment and monitoring of survivors of massive trauma, on developing ways to teach them self-assessment skills and introspection and referral mechanism to psychiatrists (if necessary).
Prospects for PTSD research
In the last decade, rapid progress in the study of mental and biological PTSD has led scientists to conclude that there is a need to focus on prevention, as the most realistic and important goal.
For example, in order to find ways to prevent PTSD, with funding NIMH conducts research to develop new and orphan drugs, aimed at combating the underlying causes of the disease. During another research scientists are looking for ways to enhance behavioral, personality and social protective factors and minimizing risk factors for prevent the development of PTSD after trauma. Another study is studying the question of what factors influence the difference in response to one or another method of treatment, which will help in the development of more individual, effective and productive methods of treatment.
Where can I find more information?
MedlinePlus - resource from the American National Library of Medicine (U.S. National Library of Medicine and the National Institutes of Health) - offers the latest information on many health issues. Information about You can find PTSD at: www.nlm.nih.gov/medlineplus/posttraumaticstressdisorder.html.
National Institute of Mental Health
Office of Science Policy, Planning, and Communications
[National Institute of Mental Health
Science Policy Division research, planning and communications]
6001 Executive Boulevard
Room 8184, MSC 9663
Bethesda, MD 20892-9663
Phone: 301-443-4513; Fax: 301-443-4279
fax answering system Free answering machine: 1-866-615-NIMH (6464)
Text phone: 1-866-415-8051 toll-free
Email: [email protected]
National Center for Post-traumatic Stress Disorder
[National PTSD Center]
VA Medical Center (116D)
215 North Main Street
White River Junction, VT 05009
802-296-6300
www.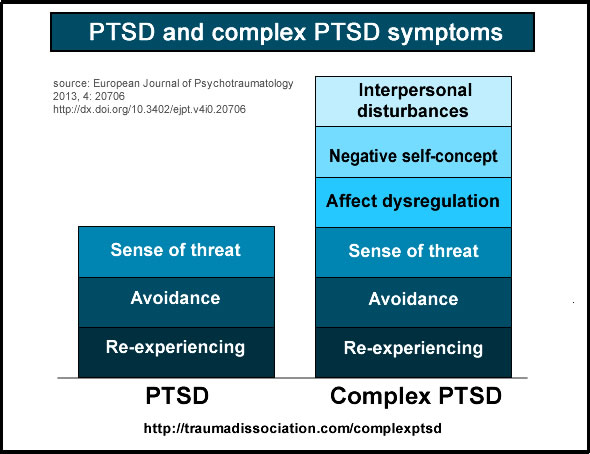 ncptsd.va.gov
ncptsd.va.gov
NOTES
- Shumyatsky GP, Malleret G, Shin RM, et al. Stathmin, a Gene Enriched in the Amygdala, Controls Both Learned and Innate Fear. cell. Nov 18 2005;123(4):697-709.
- Shumyatsky GP, Tsvetkov E, Malleret G, et al. Identification of a signal network in lateral nucleus of amygdala important for inhibiting memory specifically related to learned fear. cell. Dec 13 2002;111(6):905-918.
- Hariri AR, Mattay VS, Tessitore A, et al. Serotonin transporter genetic variation and the response of the human amygdala.Science. Jul 192002;297(5580):400-403.
- Milad MR, Quirk GJ. Neurons in medial prefrontal cortex signal memory for fear extinction. Nature. Nov 7 2002;420(6911):70-74.
- 5 Amat J, Baratta MV, Paul E, Bland ST, Watkins LR, Maier SF. Medial prefrontal cortex determines how stressor controllability affects behavior and dorsal raphe nucleus.
 Nat Neurosci. Mar 2005;8(3):365-371.
Nat Neurosci. Mar 2005;8(3):365-371. - Milad MR, Quinn BT, Pitman RK, Orr SP, Fischl B, Rauch SL. Thickness of ventromedial prefrontal cortex in humans is correlated with extinction memory. Proc Natl Acad Sci USA. Jul 26 2005;102(30):10706-10711.
- Gurvits TV, Gilbertson MW, Lasko NB, et al. Neurological soft signs in chronic posttraumatic stress disorder.Arch Gen Psychiatry. Feb 2000;57(2):181-186.
- Brewin CR. Risk factor effect sizes in PTSD: what this means for intervention. J Trauma Dissociation. 2005;6(2):123-130.
- Taylor FB, Lowe K, Thompson C, et al. Daytime Prazosin Reduces Psychological Distress toTrauma Specific Cues in Civilian Trauma Posttraumatic stress disorder. Biol Psychiatry. Feb 3 2006.
- Ressler KJ, Rothbaum BO, Tannenbaum L, et al. Cognitive enhancers as adjuncts to psychotherapy: use of D-cycloserine in phobic individuals to facilitate extinction of fear.
 Arch Gen Psychiatry. Nov 2004;61(11):1136-1144.
Arch Gen Psychiatry. Nov 2004;61(11):1136-1144. - Pitman RK, Sanders KM, Zusman RM, et al. Pilot study of secondary prevention of posttraumatic stress disorder with propranolol.Biol Psychiatry. Jan 15 2002;51(2):189-192.
- Litz BTWL, Wang J, Bryant R, Engel CC.A therapist-assisted Internet self-help program for traumatic stress. Prof Psychol Res Pr. December 2004;35(6):628-634.
New York State Department of Mental Health expresses thanks to the National Institute of Mental Health for the information, used in this booklet.
Published by the State Department of Mental Health New York, June 2008.
New York State
Andrew M. Cuomo Governor
Mental Health
Head of Department Michael F. Hogan, PhD
For more information about this edition contact:
New York State Office of Mental Health
Community Outreach and Public Education Office
[New York State Department of Mental Health
Public Relations and Community Education Department]
44 Holland Avenue
Albany, NY 12229
866-270-9857 (toll free)
www. omh.ny.gov
omh.ny.gov
For questions and complaints about mental health services Health in New York contact:
New York State Office of Mental Health
Customer Relations
[New York State Department of Mental Health
Customer Service ]
44 Holland Avenue
Albany, NY 12229
800-597-8481 (toll-free)
For information about mental health services in your neighborhood, contact
nearest New York State Department of Mental Health (NYSOMH) regional office:
Western New York Field Office
[Western New York Regional Office]
737 Delaware Avenue, Suite 200
Buffalo, NY 14209
(716) 885-4219
Central New York Field Office
[Central New York Regional Office]
545 Cedar Street, 2nd Floor
Syracuse, NY 13210-2319
(315) 426-3930
Hudson River Field Office
[Hudson River Regional Office]
4 Jefferson Plaza, 3rd Floor
Poughkeepsie, NY 12601
(845) 454-8229
Long Island Field Office
[Long Island Regional Office]
998 Crooked Hill Road, Building #45-3
West Brentwood, NY 11717-1087
(631) 761-2508
New York City Field Office
[NYC Regional Office]
330 Fifth Avenue, 9th Floor
New York, NY 10001-3101
(212) 330-1671
Mental trauma from sexual abuse persists for many years.
 Example - Christina Blasi Ford
Example - Christina Blasi Ford - Artem Voronin
- BBC Russian Service
Image copyright, Getty Images
Image caption,Ford took a polygraph test in early August
Psychologist Christina Blasey Ford testified before a Senate committee accusing Supreme Court Justice candidate Brett Kavanaugh of attempted rape.
Blasi, professor of psychology at the University of Palo Alto in California, attempted to scientifically explain to a Senate committee how the trauma of this experience persists for years to come.
We tried to understand her testimony together with scientists.
Christina Blasey Ford alleges that a Supreme Court Justice candidate attempted to rape her with a friend at a high school party 36 years ago.
- Cavanaugh and Blasy Ford under oath.
 Two versions of what happened in the bedroom 36 years ago
Two versions of what happened in the bedroom 36 years ago - Are all eyewitnesses waiting for the terrible "Afghan syndrome"?
- Locked underground: the psychology of survival in a cave
According to her, at a party at the house of a mutual friend, Kavanaugh and his friend Mark Judge unexpectedly pushed her into the bedroom. Kavanaugh pushed the teenage girl on the bed, his friend Mark Judge laughed, she met his eyes, hoping for help, but he continued to laugh while Kavanaugh tried to pull off her clothes. He, she said, burst out laughing too.
A key role in Blasi's story is post-traumatic stress disorder (PTSD), which she links to an attempted rape. PTSD is a long-term mental disorder that affects those who have experienced severe trauma or witnessed terrible events.
PTSD, also known as "trench syndrome", and in the countries of the former USSR - as "Afghan syndrome", has been well studied by psychologists and neuroscientists.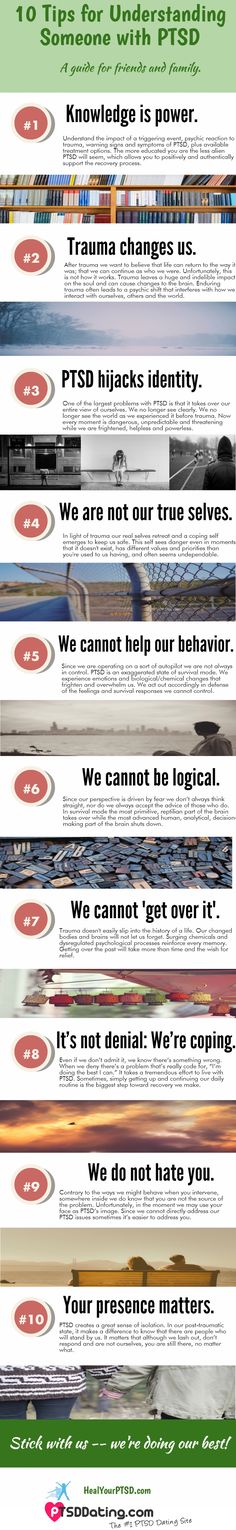 It was first diagnosed in soldiers after the First World War. Since then, scientists have learned a lot about the impact of PTSD on the structure of the brain, the behavior and habits of those who have suffered trauma.
It was first diagnosed in soldiers after the First World War. Since then, scientists have learned a lot about the impact of PTSD on the structure of the brain, the behavior and habits of those who have suffered trauma.
Experience
Skip Podcast and continue reading.
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it is important and what will happen next.
episodes
End of story Podcast
"Sexual assault causes disorders that vary from person to person. Personally, in my case, it was symptoms such as anxiety, phobias, and PTSD symptoms. In particular, claustrophobia, panic, and the like" Ford told members of the Senate committee.
She shared how she told her husband about the attack. When they were renovating their house a few years ago, she insisted on installing a second front door. In response to a request to explain why she needed it, she spoke about the attempted rape. She said that the man she was afraid of could become a member of the Supreme Court and that it would be easier for her if there was another exit in the house just in case.
In response to a request to explain why she needed it, she spoke about the attempted rape. She said that the man she was afraid of could become a member of the Supreme Court and that it would be easier for her if there was another exit in the house just in case.
"I did my best to forget the attack because the memory of it made me relive it, causing panic," Ford said.
Panic attacks, claustrophobia or agoraphobia, and anxiety are indeed well-known symptoms of PTSD. They are caused by changes in the structure of the brain that make the victim experience violence again and again.
Many people have experienced this - a painful memory comes again and again for no reason, causing great stress. In fact, this is the action of a well-known neurobiological mechanism that is not fully understood.
- Lady Gaga admitted that she suffers from PTSD
- PTSD. Is the disease from childhood?
Pavel Balaban, a specialist in the field of cellular mechanisms of memory, director of the Institute of Higher Nervous Activity and Neurophysiology of the Russian Academy of Sciences, told the BBC.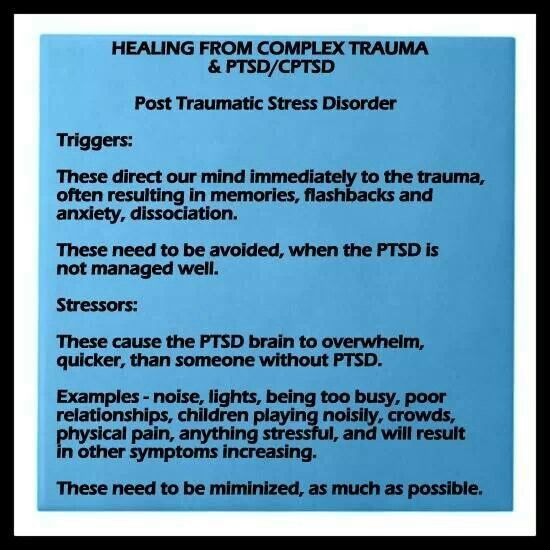
"Trauma is indeed an intrusive memory, which, unfortunately, pops up and confirms itself from time to time. Nobody really knows the mechanism of this yet, although research is very serious. This memory is self-maintaining in a very strong form. Positive memory can weaken, and negative - No," says the scientist.
"This is due to the fact that with any memory of an event, even partial, a very large amount of the mediator is released, which participated in its consolidation. Usually for negative memory it is dopamine. When remembering, it is released again, and the memory seems to be strengthened once again "It may not be as detailed anymore. The brain tries to limit it, but it is there and present. The memory is sort of overwritten," he says.
As a result, in PTSD, our ability to calm down after encountering something frightening in the external environment is disturbed - any unpleasantness reminds us of that very traumatic experience.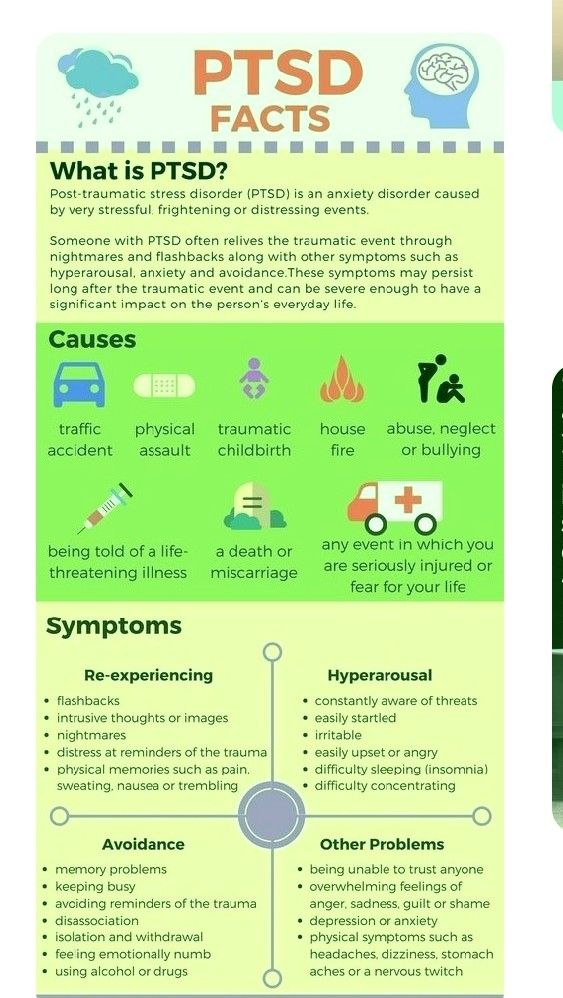
Memories stay with us for life because of a special, biologically programmed reaction of the brain to trauma.
Eternal laughter
"Just as human pain sensitivity differs from other types of sensitivity, traumatic memory stands apart from other types of memory. In fact, it is a separate type of memory that is associated with a strong emotional experience that occurs every time when a person remembers him, but, unfortunately, they remember him very often,” says Balaban.
According to him, in an effort to avoid traumatic memories, victims quite often try not to remember the experience. “They are afraid that things will get even worse. They try to suppress these memories. There is a pure fear of what you will tell someone - and you will feel worse. Fear of not even the consequences, but fear of fully reliving the memory. They refuse to worry. Sometimes they put a mental block - "no, this was not." This is pure fear of pain, fear of experiencing something of this kind again, "Balaban explains.
Image copyright, Getty Images
Image caption,PTSD is often associated with post-war injuries to veterans, but it's not just in war that you can get injured
In the case of Cristina Blasi, one of the "keys" to the traumatic memory was the laughter of the man who attacked her and his friend.
"This laughter - the loud laughter of both - cannot be erased from the hippocampus," she said at the Senate hearing. In the language of clinical science, this means that the laughter of the attackers returns to her time after time, and she cannot get rid of this memory.
"Our work shows that memory can be changed in a certain way. Experiments on animals show that this is possible. But for this, it is necessary to change the release of the reinforcing mediator. In humans, as experiments show, this is impossible, because the same mediators participate in the mass other life processes," Balaban adds.
Memory and the brain
Some memories change the structure of our brain. Such changes can be reversed, but only through clinical intervention, and so many people suffer from their symptoms, and most people do not realize that something is wrong with their brain.
Such changes can be reversed, but only through clinical intervention, and so many people suffer from their symptoms, and most people do not realize that something is wrong with their brain.
One of the functions of the brain structure called the hippocampus is storing and forgetting information. The hippocampus filters information and chooses what to keep and what to forget. As we have seen, PTSD is not a memory disorder in the truest sense of the word, but memory plays an important role in its mechanism.
You need JavaScript enabled or a different browser to view this content
Video Caption,Ford vs. Cavanaugh: What Lesson Can Russian Society Learn?
In 2003, a study was published on changes in the hippocampus in women who had gone through a traumatic experience. The test subjects were three groups of young women - sexually traumatized and suffering from PTSD, traumatized and not suffering from PTSD and not traumatized.
Scientists examined their brains using magnetic resonance imaging and positron emission tomography and found differences in brain function in different groups when performing control tasks related to remembering verbal information.
The hippocampus of women with PTSD was, on average, 16% smaller than those who experienced trauma without consequences, and 22% smaller than those who did not experience trauma. In addition, their brains showed a reduced ability to generate new neurons.
The hippocampus is one of the evolutionarily oldest parts of the human brain, which is why it is very multifunctional. In particular, he, for example, is responsible for orientation in space and remembering places. Grossly simplifying, we can say that in PTSD, memories of traumatic experiences are perceived at the same level.
Possible error?
"I'm just as sure of that as I'm talking to you now," Christina Blasey Ford said when asked by the senator whether Kavanaugh was really the man who attacked her.
She is sure that she cannot be mistaken, but this happened 36 years ago. Is there a contradiction here?
Pavel Balaban says that a traumatic memory can change in detail, but if the essence of what happened is distorted, it will simply disappear.
"We often do experiments on erasing memory on animals and see that they have already forgotten what exactly happened, but they remember that they felt very bad in this particular context, when literally two or three keys from the context remain. We have There are no faces in experiments, because animals do not remember them very well, but they perceive what happened precisely as a holistic image," he says.
"What was the color, sound, level of illumination - this can be distorted. But it is the context as a whole, the main one - it goes like a gestalt. In psychology there is the concept of gestalt - an inseparable whole. And here the contextual memory is most acutely preserved," - the scientist says.
Any detail of what happened can serve as a "key" - the laughter of the attackers, a similar voice or clothing. However, if its central detail disappears - the identity of the attacker, for example, then nothing will remain of the memory.
"If this image is thrown out, then the memory may disappear. Therefore, if this lady remembered some image in some environment, then this will not change," says Balaban.
The routine of sexual violence
The initiator of violence may perceive the same episode in a fundamentally different way. The authors of a 2015 study studied dozens of cases similar to the one that happened to Christina Blasey Ford.
As indicated in the work, sexual violence in a group of young people often acts as a component of a ritual of rapprochement and serves to self-affirmation of each of them in the group. This is typical for young men who, at school or student age, may show violent behavior, but then stop.