Cymbalta in pregnancy
Is it safe to take Cymbalta while pregnant?
Pregnancy can be overwhelming. There are the changes in your body, often lots of nausea, and the stress of simply preparing for parenthood. And for women who take medication, either for their mental health or pain relief, another question enters the equation, “Is my prescription safe for my baby?”
Taking an Rx during pregnancy isn’t uncommon—according to the FDA, 50% of pregnant women take at least one medication. But, not all drugs are safe for pregnant and lactating women.
Cymbalta is a serotonin-norepinephrine reuptake inhibitor (SNRI) drug used to treat anxiety and depression, and chronic pain. During pregnancy, depression and anxiety can increase, making it even more critical for women to know their options.
Is it safe to take Cymbalta during pregnancy?
The short answer is: It depends. Like all medications, it’s essential to immediately consult with your doctor if you are or plan to become pregnant. The use of Cymbalta during pregnancy is often decided on a case-by-case basis. “It is generally not used in pregnancy unless the benefits greatly outweigh the risk to the fetus,” according to Kecia Gaither, MD, MPH, an OB-GYN and the director of Perinatal Services at NYC Health + Hospitals/Lincoln.
There is less research on Cymbalta and pregnancy than other antidepressants, such as Zoloft. There is the potential for adverse effects, and it is contraindicated in the third trimester. “If a patient has been taking Cymbalta for anxiety or depression before pregnancy, and it’s working well for them, I’d recommend that they continue taking it,” says Carly Synder, MD, a reproductive and perinatal psychiatrist in private practice in NYC. If there are no other treatment options, including other medications, your healthcare may suggest you keep taking Cymbalta, despite the potential adverse effects. Compromised mental health during pregnancy poses a significant risk to the mother and her unborn child.
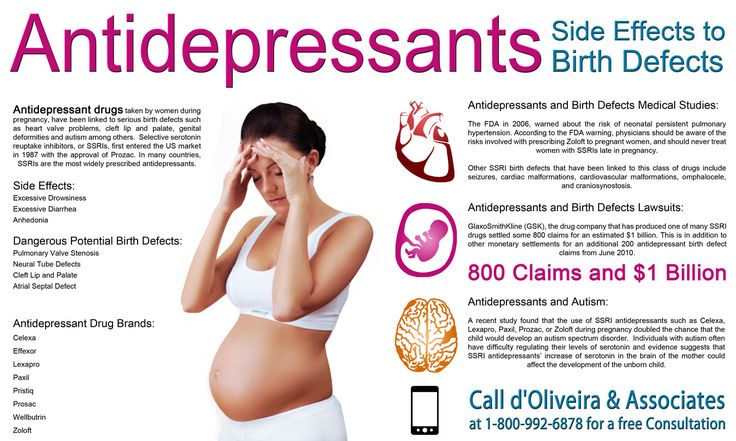
With that said, Cymbalta is likely not the first medication your doctor will recommend if you begin experiencing symptoms of depression during pregnancy.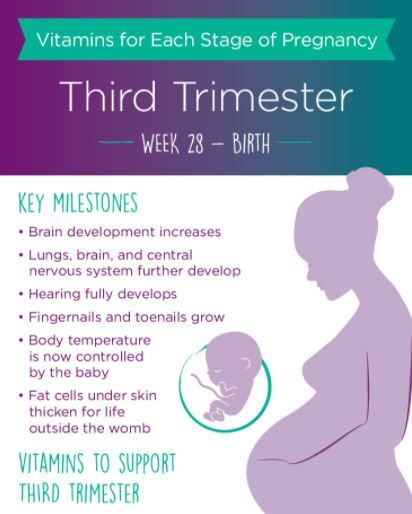 Meaning, you should not start using Cymbalta for the first time during pregnancy. Selective serotonin reuptake inhibitors (SSRIs) like Zoloft or Celexa are more commonly prescribed because more research exists demonstrating their safety.
Meaning, you should not start using Cymbalta for the first time during pregnancy. Selective serotonin reuptake inhibitors (SSRIs) like Zoloft or Celexa are more commonly prescribed because more research exists demonstrating their safety.
What are the risks of Cymbalta and pregnancy?
Because the data on this drug is limited, the risks are somewhat unknown. The existing research suggests that infants exposed to SNRIs in the third trimester could experience side effects such as: cyanosis, apnea, respiratory distress, seizures, temperature instability, feeding difficulty, hypoglycemia, jitteriness, irritability, constant crying, or tremor. “There have been a few reports of preterm labor, miscarriage, small for gestational age babies, and pregnancy complications such as hypertension—however, whether that’s due to the drug or not is left up to speculation,” Dr. Gaither says.
Antidepressants taken in the third trimester can also present a risk of the baby experiencing temporary withdrawal symptoms for up to a month after delivery. These temporary withdrawal symptoms, known as poor neonatal adaptation syndrome, can include jitteriness, restlessness, irritability, increased muscle tone, and rapid breathing and occur for 25% to 30% of babies born to women on SNRIs and SSRIs. While it sounds scary, Dr. Snyder reassures patients that “it’s completely transient.” However, in some cases it may cause an ICU admission, disrupt parental bonding, or disrupt breastfeeding.
These temporary withdrawal symptoms, known as poor neonatal adaptation syndrome, can include jitteriness, restlessness, irritability, increased muscle tone, and rapid breathing and occur for 25% to 30% of babies born to women on SNRIs and SSRIs. While it sounds scary, Dr. Snyder reassures patients that “it’s completely transient.” However, in some cases it may cause an ICU admission, disrupt parental bonding, or disrupt breastfeeding.
Research doesn’t indicate that discontinuing antidepressant use during the final trimester decreases the likelihood of these symptoms. And tapering off or completely stopping medication puts the mother at risk of sinking back into depression or experiencing heightened anxiety levels during the final months of pregnancy into the postpartum period. If you’re taking Cymbalta and become pregnant, schedule a consultation with a psychiatrist for medication recommendations.
Should dosage change during pregnancy?
Among the many changes a woman’s body goes through during pregnancy is increased blood volume. With those changes, a common assumption might be to increase the dosage of Cymbalta, but Dr. Synder explains that, “in most cases, patients don’t need to adapt their dosage, but sometimes they do. That’s why it’s so important to work with your doctor to find out what works for you.”
With those changes, a common assumption might be to increase the dosage of Cymbalta, but Dr. Synder explains that, “in most cases, patients don’t need to adapt their dosage, but sometimes they do. That’s why it’s so important to work with your doctor to find out what works for you.”
Is it safe to breastfeed on Cymbalta?
Like pregnancy, there is limited data on the use of Cymbalta during breastfeeding. You should weigh the potential risks to your infant with your healthcare provider. Given the limited data, many women and their providers may prefer an alternative. However, the available research does indicate that the dose in breast milk is extremely low.
Generally, it is not recommended to start taking Cymbalta for the first time while breastfeeding. Dr. Snyder recommends maintaining consistency between the pregnancy and postpartum period. “If a mother is taking something during pregnancy,” she says, “it’s typically fine during breastfeeding, particularly if the mother is doing well with it. ” It’s important to monitor the infant for drowsiness and adequate feeding, weight gain, and developmental milestones, especially if they breastfeed exclusively. And, consult with your doctor if there are ever any concerns.
” It’s important to monitor the infant for drowsiness and adequate feeding, weight gain, and developmental milestones, especially if they breastfeed exclusively. And, consult with your doctor if there are ever any concerns.
Remember to prioritize postpartum self-care
Life as a new parent can get overwhelming. But taking care of yourself is the first step in being able to care for your child. And that includes maintaining a consistent schedule with your medication, especially medications taken for mental health. Try a pillbox, use alerts on your phone, or work with your partner to create an accountability system that works for your new schedule as a mom.
If you’re experiencing depression or anxiety during pregnancy, it’s important to remember that you aren’t alone. Talk to your provider and find a solution that will be best for you and your baby.
Is Duloxetine (Cymbalta) Safe To Use During Pregnancy?
Previous Next
- View Larger Image
You can find a more recent post on this topic here:
Venlafaxine and Duloxetine: Pooled Analysis Shows No Increase in Risk of Malformations
We receive a fair number of questions on the use of duloxetine during pregnancy. Duloxetine (sold in the United Sates under the brand name of Cymbalta) is a serotonin-norepinephrine reuptake inhibitor (SNRI) effective for major depressive disorder and generalized anxiety disorder (GAD). It has also been FDA-approved for the treatment of chronic musculoskeletal pain and fibromyalgia. Although it is used fairly commonly in women of child-bearing age, information regarding its reproductive safety is limited. For those of you interested, there is a thorough review on the use of duloxetine during pregnancy in the December 2014 issue of the Journal of Clinical Psychiatry. I will summarize here the points made in this review.
Duloxetine (sold in the United Sates under the brand name of Cymbalta) is a serotonin-norepinephrine reuptake inhibitor (SNRI) effective for major depressive disorder and generalized anxiety disorder (GAD). It has also been FDA-approved for the treatment of chronic musculoskeletal pain and fibromyalgia. Although it is used fairly commonly in women of child-bearing age, information regarding its reproductive safety is limited. For those of you interested, there is a thorough review on the use of duloxetine during pregnancy in the December 2014 issue of the Journal of Clinical Psychiatry. I will summarize here the points made in this review.
In a prospective observational study, Einarson and colleagues followed 208 women who contacted Motherisk regarding the reproductive safety of duloxetine. Of these, 206 women (99.0%) took duloxetine before conception and during the first trimester. In the duloxetine group, there were 3 (1.8%) major malformations (clubfoot, hydronephrosis, kidney agenesis).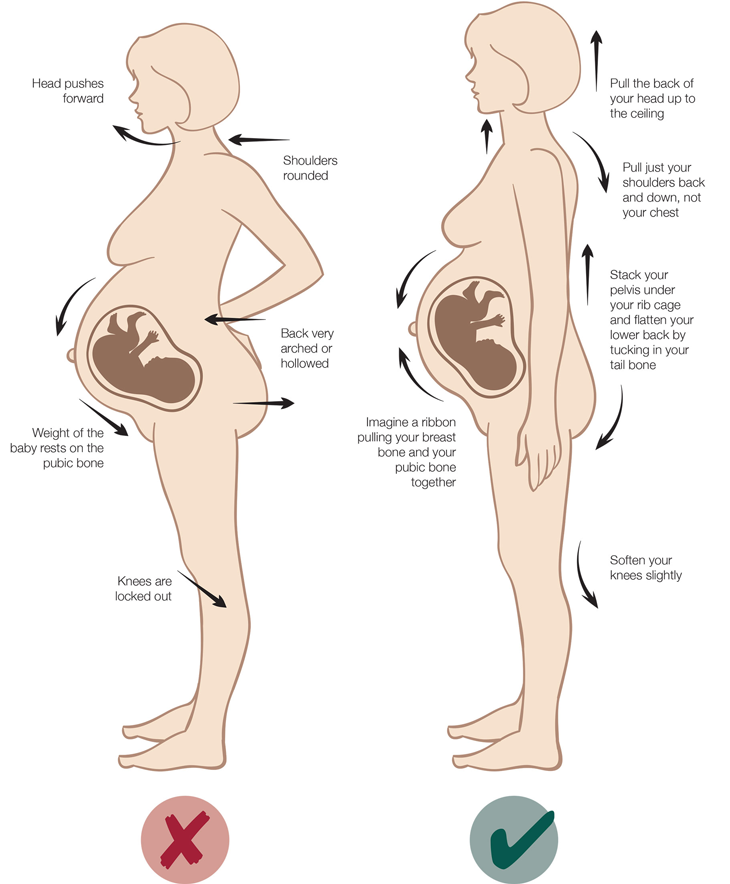 The rates of malformation in this group did not differ from two comparison groups: (1) women who were inquiring about exposure to other antidepressants (n=208) and (2) women inquiring about an exposure to medications not considered to be teratogens, such as acetaminophen (n=208).
The rates of malformation in this group did not differ from two comparison groups: (1) women who were inquiring about exposure to other antidepressants (n=208) and (2) women inquiring about an exposure to medications not considered to be teratogens, such as acetaminophen (n=208).
In another report, Hoog and colleagues reported on 400 cases of duloxetine exposure identified through the Eli Lilly Safety System database. There were 233 prospectively recorded cases. In this group, there were six congenital malformations (3%). This report did not include a control group; however, the rate of malformations in the exposed group is similar to that expected rate in the general population. (This study did not specify what malformations were observed.)
If we combine these two studies, we have prospectively collected data on a total of 439 pregnancies, with a total of 9 malformations; a rough and dirty calculation would give you a malformation rate of 2.1% which is comparable to the rate we see in the general population.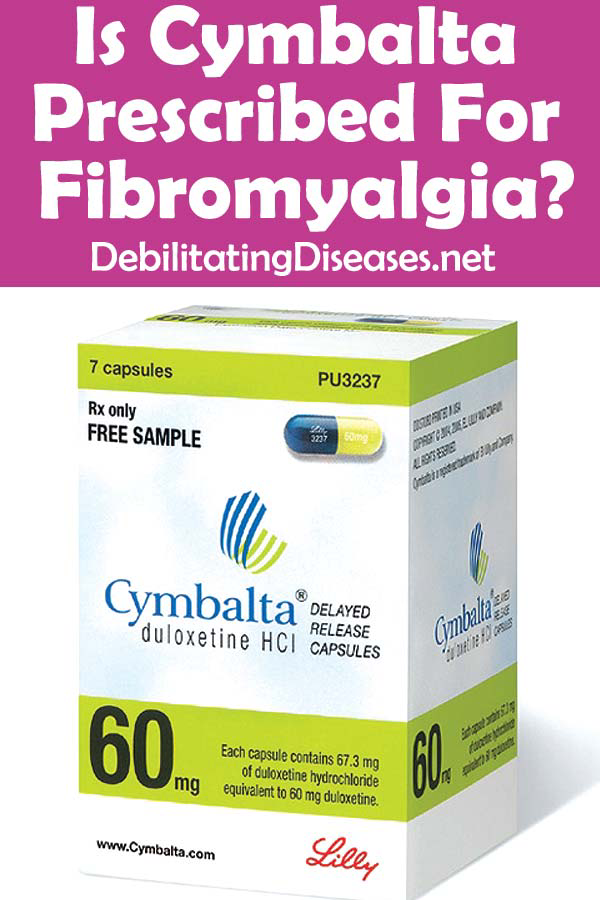 While this information is reassuring, Einarson and colleagues note that approximately 750 subjects in each group would be required to detect a 2-fold increase in major malformations, and thousands would be required to detect an increase in the risk of rarer anomalies. These results suggest that duloxetine does not appear to increase the rate of major malformations above baseline.
While this information is reassuring, Einarson and colleagues note that approximately 750 subjects in each group would be required to detect a 2-fold increase in major malformations, and thousands would be required to detect an increase in the risk of rarer anomalies. These results suggest that duloxetine does not appear to increase the rate of major malformations above baseline.
Several studies suggest that duloxetine, as seen with other antidepressants, may increase the risk of spontaneous abortion. In the report from Hoog, the risk of spontaneous abortion was about 18% among women taking duloxetine. Reassuringly, the risk of pregnancy loss in women taking Cymbalta is not increased significantly over the 12%-15% risk of miscarriage seen in the general population. This is a complicated issue: it appears that having depression itself may impact the risk of miscarriage and more recent analyses have not documented an association between antidepressant exposure and spontaneous abortion.
There is not adequate data to comment on the risk of other outcomes such as preterm delivery, low birth weight, poor neonatal adaptation, and persistent pulmonary hypertension of the newborn.
Would We Recommend Using Duloxetine?
There is no single or simple answer to this question, and we must make all decisions on a case-by-case basis. Let’s consider a woman taking duloxetine for major depression who is planning pregnancy within the next year. If she has not tried other, better characterized, antidepressants, we might try switching her over to one of these older antidepressants prior to conception. On the other hand, there is a growing body of data to support the reproductive safety of duloxetine. In a woman who has not responded well to other antidepressants or who is unwilling to accept the risk of relapse of her illness in the setting of a medication switch, we might elect to maintain duloxetine throughout the pregnancy.
Ruta Nonacs, MD PhD
Andrade C. The safety of duloxetine during pregnancy and lactation. J Clin Psychiatry. 2014 Dec;75(12):e1423-7.
The safety of duloxetine during pregnancy and lactation. J Clin Psychiatry. 2014 Dec;75(12):e1423-7.
Einarson A, Smart K, Vial T, et al. Rates of Major Malformations in Infants Following Exposure to Duloxetine During Pregnancy: A Preliminary Report. J Clin Psychiatry 2012;73(11):1471.
Hoog SL, Cheng Y, Elpers J, et al. Duloxetine and pregnancy outcomes: safety surveillance findings. Int J Med Sci. 2013; 10(4):413–419.
Related Posts
Simbalta pregnancy and lactation - Medum.ru
Pregnancy and lactationPlease note: the use of any drugs, including the drug Simbalta, with planning and during periods of pregnancy, lactation (breastfeeding) is necessary agree with the attending physician. Women of reproductive potential are advised to undergo pregnancy testing. nine0003
Use during pregnancy and lactation
Due to insufficient experience with the use of duloxetine during pregnancy, the drug should be used during pregnancy only if the potential benefit to the patient far outweighs the potential risk to the fetus. Patients should be warned that if pregnancy occurs or is planned during treatment with duloxetine, they should inform their physician. nine0003
Patients should be warned that if pregnancy occurs or is planned during treatment with duloxetine, they should inform their physician. nine0003
Epidemiological evidence suggests that the use of selective serotonin reuptake inhibitors (SSRIs) during pregnancy, especially in late pregnancy, may increase the risk of persistent pulmonary hypertension in the newborn. Despite the lack of studies on the relationship of persistent pulmonary hypertension of the newborn and the use of SSRIs, a potential risk cannot be excluded, given the mechanism of action of duloxetine (serotonin reuptake inhibition). nine0003
As with other serotonergic drugs, "withdrawal" syndrome may occur in newborns if the mother takes duloxetine late in pregnancy.
"Withdrawal" syndrome includes the following symptoms: low blood pressure, tremor, hyperexcitability syndrome, feeding difficulties, respiratory distress syndrome, convulsions. Most of the symptoms were observed during childbirth or in the first few days after childbirth. nine0003
nine0003
Due to the fact that duloxetine passes into breast milk (the concentration in the fetus is approximately 0.14% of the concentration in the mother based on mg / kg body weight), breast-feeding is not recommended during duloxetine therapy.
Important additional information
Active ingredient of Simbalta
It is recommended to read the description of the active substance of the drug Cymbalta - duloxetine. nine0003
- Category of action on the fetus according to the FDA - C
Forms
Pay attention to the description of the use of the drug Simbalta during periods pregnancy and lactation may differ depending on the manufacturer and the form of release used. In the directory Medum provides the following information on the dosage forms of Simbalta:
- Simbalta - release forms (1)
Other information
- FDA Fetal Categories
See more detailed information about Cymbalta:
- Cymbalta - leaflet
- Reviews
- Questions
Didn't find what you were looking for?
If you need to know more about Cymbalta, ask your question. Professionals or Users Medum will answer it shortly.
Professionals or Users Medum will answer it shortly.
Share this page
instructions for use, home delivery
Features
| Minimum age from. | 18 years old |
| Pack quantity | 14 pcs |
| Minimum allowable storage temperature, °С | 15 °C |
| Maximum allowable storage temperature, °С | 30 °C |
| Expiration date | 36 months |
| Storage conditions | Keep out of reach of children | nine0067
| Release form | Capsules |
| Country of origin | US |
| Release procedure | Prescription |
| Active ingredient | nine0063 Duloxetine|
| Pharmacological group | N06AA Non-selective monoamine reuptake inhibitors |
| Registered as | Medicine |
Description
Opaque, blue/white, hard gelatin capsules (size 3) imprinted with green ink at dosage "30 mg" and identification code "9543".
Active substances
Dulcosetin
Form of release
Capsules
Composition
Each capsules contain:
Active substance: Dulsetine hydrochloride, equivalent to 30 mg or 60 MOST DULSTINE,
excipients:
capsule content - sucrose, hypromellose, granulated sugar (not more than 91.5% sucrose, starch), talc, hypromellose acetate succinate, triethyl citrate, white dye (titanium dioxide, hypromellose),
capsule shell - indigo carmine, titanium dioxide, sodium lauryl sulfate, gelatin, iron oxide yellow (only for 60 mg capsules).
Pharmacological effect
Antidepressant.
Duloxetine is an antidepressant, serotonin and norepinephrine reuptake inhibitor, and weakly inhibits dopamine uptake without significant affinity for histaminergic, dopaminergic, cholinergic, and adrenergic receptors. The mechanism of action of duloxetine in the treatment of depression is to suppress the reuptake of serotonin and norepinephrine, resulting in increased serotonergic and noradrenergic neurotransmission in the CNS. nine0003
nine0003
Duloxetine has a central mechanism of pain suppression, which, first of all, is manifested by an increase in the threshold of pain sensitivity in pain syndrome of neuropathic etiology.
Pharmacokinetics
Absorption. Duloxetine is well absorbed when taken orally. Absorption begins 2 hours after taking the drug. The maximum concentration of the drug is reached 6 hours after ingestion.
Eating does not affect the maximum concentration of the drug, but increases the time to reach the maximum concentration from 6 to 10 hours, which indirectly reduces the degree of absorption (approximately 11%). nine0003
Distribution.
Duloxetine binds well to plasma proteins (> 90%), mainly to albumin and α1-globulin, but liver or kidney disorders do not affect the degree of protein binding.
Metabolism.
Duloxetine is extensively metabolized and its metabolites are primarily excreted in the urine. Both CYP2D6 and CYP1A2 catalyze the formation of two major metabolites (4-hydroxyduloxetine glucuronic conjugate, 5-hydroxy,6-methoxyduloxetine sulfate conjugate). nine0003
nine0003
Circulating metabolites have no pharmacological activity.
Removal.
The half-life of duloxetine is 12 hours. The mean clearance of duloxetine is 101 l/h.
Selected patient groups.
Gender:
Although differences in pharmacokinetics between men and women have been identified (mean clearance of duloxetine is lower in women), these differences are not so great that there is a need for dose adjustment depending on sex. Age: Although pharmacokinetic differences have been identified between middle-aged and elderly patients (AUC - area under the concentration / time curve is higher and the half-life of the drug is longer in the elderly), these differences are not enough to change the dose depending only on the age of patients. nine0003
Impaired renal function:
in patients with severely impaired renal function (end-stage renal disease - chronic renal failure) on hemodialysis, the values of Cmax (maximum concentration) and AUC of duloxetine increased by 2 times. In this regard, the feasibility of reducing the dose of the drug in patients with clinically significant impaired renal function should be considered.
In this regard, the feasibility of reducing the dose of the drug in patients with clinically significant impaired renal function should be considered.
Impaired liver function:
Patients with clinical signs of hepatic impairment may experience slow metabolism and excretion of duloxetine. Following a single dose of 20 mg duloxetine in 6 patients with cirrhosis of the liver with moderate hepatic impairment (Child-Pugh Class B), the half-life of duloxetine was approximately 15% longer than in healthy subjects of the corresponding sex and age with a five-fold increase in mean exposure ( AUC). Despite the fact that Cmax in patients with cirrhosis was the same as in healthy people, the elimination half-life was approximately 3 times longer. nine0003
Indications
- Depression.
- Painful form of diabetic neuropathy.
- generalized anxiety disorder
Contraindications
- Hypersensitivity to the drug.
- Simultaneous use with monoamine oxidase inhibitors (MAOIs) (see section "Special Instructions").
- Uncompensated angle-closure glaucoma
Precautions
With an exacerbation of a manic / hypomanic state, epileptic seizures, mydriasis, impaired liver or kidney function, with the likelihood of suicidal attempts (see section "Special Instructions").
Use in pregnancy and lactation
Due to insufficient experience with the use of duloxetine during pregnancy, the drug should be administered during pregnancy only if the potential benefit to the patient significantly outweighs the potential risk to the fetus. Patients should be warned that if pregnancy occurs or is planned during treatment with duloxetine, they should inform their physician. nine0003
Due to the lack of experience with the use of duloxetine in breastfeeding women, breastfeeding during duloxetine therapy is not recommended.
Dosage and administration
Inside. Capsules should be swallowed whole, without chewing or crushing. Do not add the drug to food or mix it with liquids, as this can damage the enteric coating of the pellets.
Capsules should be swallowed whole, without chewing or crushing. Do not add the drug to food or mix it with liquids, as this can damage the enteric coating of the pellets.
The recommended starting dose of duloxetine is 60 mg once daily with or without food. In some patients, to achieve a good result, it is necessary to increase the dose from 60 mg 1 time per day to a maximum dose of 120 mg per day in two divided doses. A systematic evaluation of the drug in a dose of more than 120 mg was not carried out. nine0003
In patients with renal insufficiency: the initial dose should be 30 mg 1 time per day in patients with severe renal impairment (end-stage renal disease) (creatinine clearance In patients with impaired liver function: the initial dose of the drug should be reduced or the frequency of administration should be reduced). patients with cirrhosis
Age: Recommended in patients ≥ 18 years of age
No clinical experience with duloxetine in patients under 18 years of age
Side effects
The most common (≥ 10%) reported in clinical studies were:
dizziness (except vertigo), dry mouth, nausea, constipation, sleep disturbances (drowsiness or insomnia) and headache.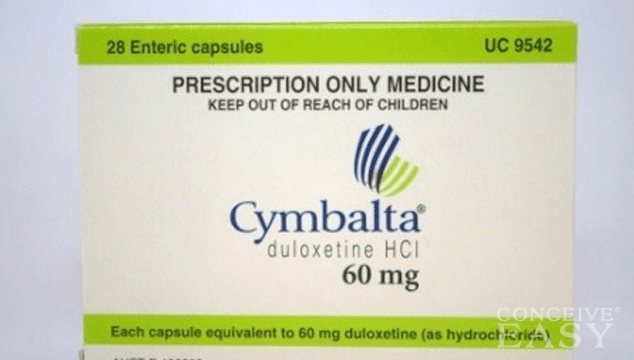 Headache was less common than with placebo.
Headache was less common than with placebo.
Less common (≥ 1 to) Dizziness, nausea, headache have been reported as common adverse effects with discontinuation of duloxetine.
Effects on glucose levels in patients with painful diabetic neuropathy: there may be a slight increase in fasting blood glucose while taking duloxetine. nine0003
Overdose
Several cases of overdose with a single oral intake of up to 1400 mg of the drug, which did not have fatal consequences, have been reported. Overdose may be accompanied by the following symptoms: tremor, clonic convulsions, ataxia, vomiting and loss of appetite.
Treatment for overdose. The specific antidote is not known. Cardiac monitoring and vital signs are recommended, along with symptomatic and supportive treatment. nine0003
Interaction with other drugs
Drugs metabolized by CYP1A2.
Co-administration of duloxetine (60 mg twice daily) did not significantly affect the pharmacokinetics of theophylline metabolized by CYP1A2. Duloxetine is unlikely to have a clinically significant effect on the metabolism of CYP1A2 substrates.
Duloxetine is unlikely to have a clinically significant effect on the metabolism of CYP1A2 substrates.
CYP1A2 inhibitors.
Because CYP1A2 is involved in the metabolism of duloxetine, co-administration of duloxetine with potential CYP1A2 inhibitors is likely to result in increased duloxetine concentrations. The potent CYP1A2 inhibitor fluvoxamine (100 mg once daily) reduced the mean plasma clearance of duloxetine by approximately 77%. Caution should be exercised when prescribing duloxetine with CYP1A2 inhibitors (eg, some quinolone antibiotics) and lower doses of duloxetine should be used. nine0003
Drugs metabolized by CYP2D6.
Duloxetine is a moderate inhibitor of CYP2D6. When taking duloxetine at a dose of 60 mg 2 times a day, along with a single dose of desipramine, a CYP2D6 substrate, the AUC of desipramine increases 3 times. Co-administration of duloxetine (40 mg twice daily) increased the stable fraction of the AUC of tolterodine (2 mg twice daily) by 71% but had no effect on the pharmacokinetics of the 5-hydroxyl metabolite. Thus, caution should be exercised when using duloxetine with drugs that are primarily metabolized by the CYP2D6 system and have a narrow therapeutic index. nine0003
Thus, caution should be exercised when using duloxetine with drugs that are primarily metabolized by the CYP2D6 system and have a narrow therapeutic index. nine0003
CYP2D6 inhibitors.
Since CYP2D6 is involved in the metabolism of duloxetine, concomitant use of duloxetine with potential CYP2D6 inhibitors may result in increased duloxetine concentrations. Paroxetine (20 mg once daily) reduced the mean clearance of duloxetine by approximately 37%. Caution should be exercised when using duloxetine with CYP2D6 inhibitors (eg SSRIs).
Drugs affecting the central nervous system.
Caution should be exercised when co-administering duloxetine with other drugs and agents that affect the central nervous system, especially those that have a similar mechanism of action, including alcohol. nine0003
Highly protein bound preparations.
Duloxetine is highly bound to plasma proteins (> 90%). Therefore, the administration of duloxetine to a patient who is taking another drug that is highly bound to plasma proteins may lead to an increase in the concentration of the free fractions of both drugs.
Special instructions
Monoamine oxidase inhibitors (MAOIs). In patients receiving a serotonin reuptake inhibitor in combination with a MAOI, there have been cases of serious reactions, sometimes fatal, including pyrexia, rigidity, myoclonus, peripheral disturbances with possible sharp fluctuations in vital signs and changes in mental status, including marked arousal with the transition to delirium and to whom. These reactions have also been observed in patients who had their serotonin reuptake inhibitor discontinued shortly before MAOIs. In some cases, patients experienced symptoms characteristic of neuroleptic malignant syndrome. The effects of the combined use of duloxetine and MAOIs have not been evaluated in humans or animals. Therefore, given the fact that duloxetine is an inhibitor of both serotonin and norepinephrine, it is not recommended to take duloxetine in combination with an MAOI or for at least 14 days after stopping MAOI treatment. nine0003
Based on the length of the half-life of duloxetine, a break of at least 5 days after the end of duloxetine should be taken before taking MAOIs.
Manic/hypomanic exacerbation: As with similar CNS drugs, duloxetine should be used with caution in patients with a history of manic episodes. Seizures: As with similar drugs that affect the central nervous system, duloxetine should be used with caution in patients with a history of epileptic seizures. nine0003
Mydriasis: Cases of mydriasis have been observed with duloxetine, so caution should be exercised when prescribing duloxetine to patients with elevated intraocular pressure or in individuals at risk of developing acute angle-closure glaucoma.
Impaired liver or kidney function: in patients with severely impaired renal function (creatinine clearance) Suicide attempts: in depression, there is a possibility of suicide attempts, which may persist until a stable remission occurs. Careful monitoring of patients at risk is necessary.
Driving and performing tasks that require increased attention
Studies of duloxetine showed no impairment of psychomotor reactions, cognitive functions and memory.