Cure to depersonalization
Depersonalization-Derealization Disorder | Co-Occuring Disorder Treatment
There is no cure for depersonalization derealization disorder, but treatment can reduce distressing symptoms and even lead to full remission of the disorder.
Depersonalization-derealization disorder is a dissociative disorder that was once only vaguely understood. Advances in understanding and treating trauma-related disorders have led to improved insight into depersonalization and other dissociative disorders, which are now known to be trauma-related disorders. Depersonalization disorder treatment typically involves using one or more therapeutic interventions to address different aspects of the disorder. Individual therapy is the primary depersonalization treatment, though medications are sometimes used in conjunction with therapy to treat the disorder. While derealization is considered to be a distinct aspect of this condition, derealization treatment is incorporated fully into interventions for depersonalization.
Article at a Glance:
- Depersonalization-derealization disorder is typically treated with individual therapy and sometimes medication too.
- SSRIs and antipsychotic medications do not cure this condition but can reduce distressing symptoms.
- Therapy options include teletherapy, psychotherapy, cognitive behavioral therapy, dialectical behavioral therapy, and eye movement desensitization and reprocessing.
- Depression and anxiety are the most common co-occurring disorders alongside this condition.
- Alcohol and drug use is common among people with depersonalization-derealization disorder.
Medications for Depersonalization-Derealization Disorder
There is no depersonalization cure, but treatment can reduce distressing symptoms and even lead to full remission of the disorder. It’s important for people experiencing depersonalization or derealization to talk to a professional about their symptoms so they can begin treatment and start feeling like themselves again. Antidepressant and antipsychotic medications may be prescribed to help with symptoms of depersonalization.
Antidepressant and antipsychotic medications may be prescribed to help with symptoms of depersonalization.
Selective Serotonin Reuptake Inhibitors (SSRIs)
Most people with dissociative disorders have co-occurring conditions, and depression is one of the most common. Antidepressants, especially selective serotonin reuptake inhibitors (SSRIs), are frequently prescribed to treat comorbid depression. Popular SSRIs for dissociative disorders include:
- Sertraline (Zoloft)
- Fluoxetine (Prozac)
- Citalopram (Celexa)
These SSRIs can treat several symptoms specific to depersonalization-derealization disorder. The sense of detachment that accompanies depersonalization is often closely linked with flat affect and blunted emotion, all of which can be improved with SSRIs. Antidepressants can also stabilize mood and reduce the intrusive symptoms that trigger dissociative symptoms. Research shows that a combination of an SSRI and lamotrigine, a mood stabilizer, is an effective treatment for dissociative disorders, especially depersonalization-derealization disorder. SSRIs can also be used to treat anxiety, which is another commonly co-occurring condition with depersonalization-derealization disorder. They are often the best medical option for treating dissociative disorders with comorbid anxiety.
SSRIs can also be used to treat anxiety, which is another commonly co-occurring condition with depersonalization-derealization disorder. They are often the best medical option for treating dissociative disorders with comorbid anxiety.
Antipsychotic Medications
One of the defining features of dissociative disorders like depersonalization is that they are not psychotic disorders. People who experience them maintain an intact sense of reality. However, antipsychotic drugs can be an effective option for treating these disorders.
Antipsychotics can provide a number of desirable effects for people with depersonalization-derealization disorder, including mood stabilization, anxiety reduction, and improved range of affect. They may even target and reduce depersonalization and derealization symptoms.
Therapy for Depersonalization-Derealization Disorder
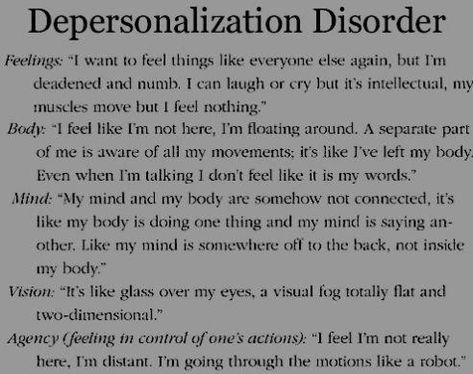
Depersonalization and derealization symptoms can make someone feel unreal. At various times, the self, body, emotions and the external world may all feel like they don’t exist or as if they are distorted or distant.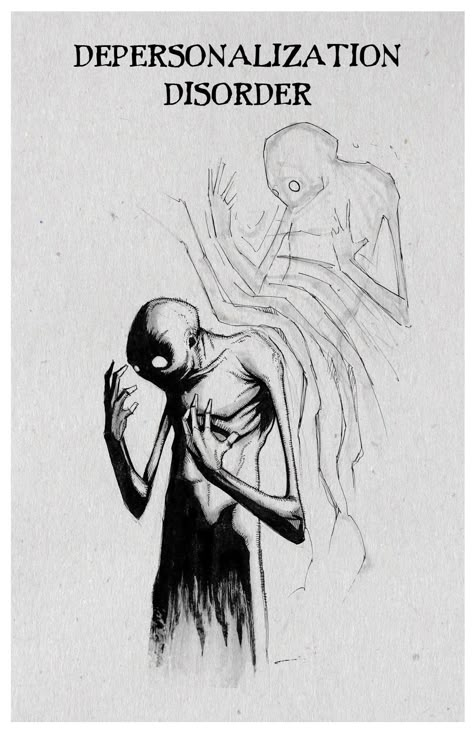 The extent to which any of these symptoms are present can point to a diagnosis of depersonalization-derealization disorder.
The extent to which any of these symptoms are present can point to a diagnosis of depersonalization-derealization disorder.
There is a depersonalization-derealization disorder test a therapist may use to diagnose the disorder. While a specific test like the structured clinical interview for dissociative disorders may be used, the main depersonalization disorder test is the Steinberg Depersonalization Questionnaire. There is a similar derealization test, the Steinberg Derealization Questionnaire.
While philosophical inquiries can lead to questions about what is real, the feeling that the self and the external world aren’t real is usually a dissociative response, often one that was learned to detach from terrifying or painful traumatic experiences. The goal of any therapeutic treatment of depersonalization-derealization disorder is to help individuals regain access to their full emotional range, which often requires establishing both safety and insight.
Teletherapy
Using teletherapy, patients are matched with a licensed therapist. The therapist will work with the patient on a personalized treatment plan, guiding him or her on the path to lifelong recovery. Read more about getting started with teletherapy.
The therapist will work with the patient on a personalized treatment plan, guiding him or her on the path to lifelong recovery. Read more about getting started with teletherapy.
Psychotherapy
Psychotherapy is the general term used to describe any form of talk therapy in which a client explores their thoughts and feelings by speaking to a therapist about them.
While significant advances have been made in the pharmacotherapeutic treatment of mental health conditions, psychotherapy remains the primary and essential psychiatric intervention. This is especially true in the treatment of depersonalization-derealization disorder, which may not be fully treatable with any medication. Psychodynamic psychotherapy is one of the oldest styles of therapy. This form of therapy is now much less popular than it once was, but it still can be effective in particular therapeutic contexts.
Psychodynamic psychotherapy focuses on exploring the past to gain insight into what caused a person to think and feel in certain ways. By making the unconscious sources of emotional reactions conscious, someone with depersonalization-derealization disorder can start to understand the reasons they feel disconnected from reality and take steps to remedy this.
By making the unconscious sources of emotional reactions conscious, someone with depersonalization-derealization disorder can start to understand the reasons they feel disconnected from reality and take steps to remedy this.
Insight may be the most effective tool to treat depersonalization-derealization disorder, opening the door to once-blocked emotions. By unlearning previously unconscious ways of responding to the world, people can start to experience emotions and thoughts that they once found intolerable and that previously triggered their dissociative symptoms.
Cognitive Behavioral Therapy
Cognitive behavioral therapy (CBT) is one of the most well-researched therapeutic modalities and is considered an evidence-based practice for the treatment of many psychiatric disorders. It works by helping people identify cognitive distortions and irrational beliefs. By challenging and reframing these thoughts, people can reduce or eliminate the negative emotions and behaviors caused by them.
Individuals with depersonalization-derealization disorder usually respond well to CBT. Many symptoms of the disorder have a cognitive basis. Obsessive thinking about the self and the world intensifies feelings of unreality. People with depersonalization-derealization disorder can use CBT to examine and question thoughts that exacerbate derealization and learn grounding and breathing techniques that counteract disembodiment and other dissociative symptoms.
Dialectical Behavioral Therapy
Dialectical behavioral therapy (DBT) was developed for the treatment of borderline personality disorder, which is a trauma-related condition. DBT combines cognitive-behavioral tools and techniques with mindfulness practices and a philosophy of acceptance.
By shifting from the CBT approach of labeling certain thoughts or feelings as negative, DBT helps people with histories of abuse and trauma to explore painful emotions without guilt or shame and to feel more comfortable in sharing what they think and feel. Interventions in DBT help people develop distress tolerance and improve emotional regulation.
Interventions in DBT help people develop distress tolerance and improve emotional regulation.
This kind of behavioral therapy yields key insights and benefits for the treatment of depersonalization disorder. People with this dissociative disorder often learned to mistrust their thoughts or feelings and to label them as bad. This mistrust is what makes them feel as if these inner states or even their very selves aren’t real.
By teaching people to accept their inner states, DBT can help people reconnect to them. The mindfulness, breathing, and self-soothing techniques taught in DBT can also help people with depersonalization-derealization disorder to reconnect with their bodies and the sensations of being in the moment.
Eye Movement Desensitization and Reprocessing
Eye movement desensitization and reprocessing (EMDR) is another intervention developed specifically for people with trauma-related disorders. Its goal is to help people who have been repressing or avoiding traumatic memories, thoughts and feelings to gradually and safely process them.
In EMDR, clients talk or think about traumatic memories while tracking a back-and-forth visual or auditory cue designed to help their brains reprocess these events. While people debate the reasons this technique works, research shows that EMDR is an effective approach for people with histories of trauma, including people with depersonalization-derealization disorder.
Like CBT, EMDR can help people change their thought processes, and, like DBT, it can help them do so in a way that is nurturing and grounded in physical experience. Since this form of treatment specifically focuses on exploring trauma, it can help people who have repressed or avoided traumatic memories begin to address them in a safe environment.
Many people with symptoms of depersonalization and derealization have had experiences that caused them to invalidate their emotions and to repress thoughts and memories — traumatic or otherwise. EMDR can help them break through those defenses and feel their emotions more directly again.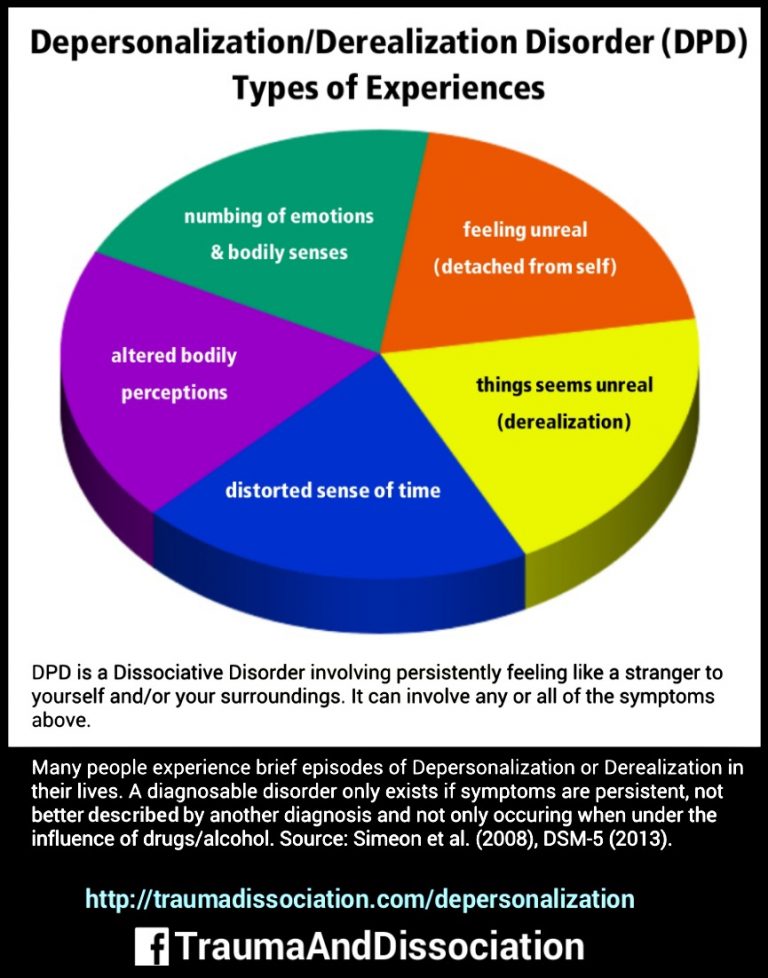
Treating Depersonalization-Derealization Disorder and Co-Occurring Conditions
Most people with dissociative disorders have co-occurring conditions, with depression and anxiety being the most common. The symptoms of these disorders are deeply interconnected and are best treated simultaneously.
For example, depressive symptoms, like blunted emotions, naturally arise from the experience of depersonalization and derealization. When symptoms of derealization and depersonalization are caused by emotional abuse and trauma, they function as defenses. Anxiety can arise when repressed material starts becoming conscious.
When people have depersonalization-derealization disorder and co-occurring anxiety or depression, medication can be an especially effective tool in the therapeutic process. Taking medications is not always necessary or the best option, however, depending on the person being treated and the existence of any other comorbid medical or mental health conditions.
You can also check out the Nobu app to learn more about depersonalization-derealization disorder and other mental health topics. It is free and for anyone that is looking to reduce anxiety, work through depression, build self-esteem, get aftercare following treatment, attend teletherapy sessions and so much more. Download the Nobu app today!
Depersonalization-Derealization Disorder and Substance Abuse
Drug and alcohol use is common among people with dissociative disorders. Depersonalization-derealization disorder can drive substance abuse in one of two ways. People may take substances to intensify depersonalization and derealization symptoms as well as to further entrench their protective function. In some cases, they might use alcohol or drugs to break down dissociative defenses and feel emotions they normally can’t feel. These dynamics can quickly lead to the development of substance dependence.
The best and most effective way to treat co-occurring depersonalization-derealization and substance use disorders is to use an integrated approach. This means several interventions should be provided in a coordinated way, ideally by the same organization or treatment team.
This means several interventions should be provided in a coordinated way, ideally by the same organization or treatment team.
Many treatment centers throughout the United States, like The Recovery Village, use an integrated approach to treating drug and alcohol addiction and co-occurring disorders, including those involving depersonalization derealization disorder. To learn more about the benefits of treating co-occurring disorders, contact The Recovery Village today.
Editor – Camille Renzoni
Cami Renzoni is a creative writer and editor for The Recovery Village. As an advocate for behavioral health, Cami is certified in mental health first aid and encourages people who face substance use disorders to ask for the help they deserve. Read more
Medically Reviewed By – Stephanie Hairston, MSW
Stephanie Hairston received her Bachelor of Arts degree in Psychology and English from Pomona College and her Master of Social Work degree from New York University. Read more
Medical Disclaimer
The Recovery Village aims to improve the quality of life for people struggling with substance use or mental health disorder with fact-based content about the nature of behavioral health conditions, treatment options and their related outcomes. We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.
We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.
How to Stop Depersonalization: 10 Methods
Do you frequently feel detached from reality, like you’re watching yourself in a movie? If so, you may want to know how to feel some relief from depersonalization.
Depersonalization can be a frightening or confusing experience. The good news is, learning what causes depersonalization, as well as using a few self-care tools, can help make it more manageable.
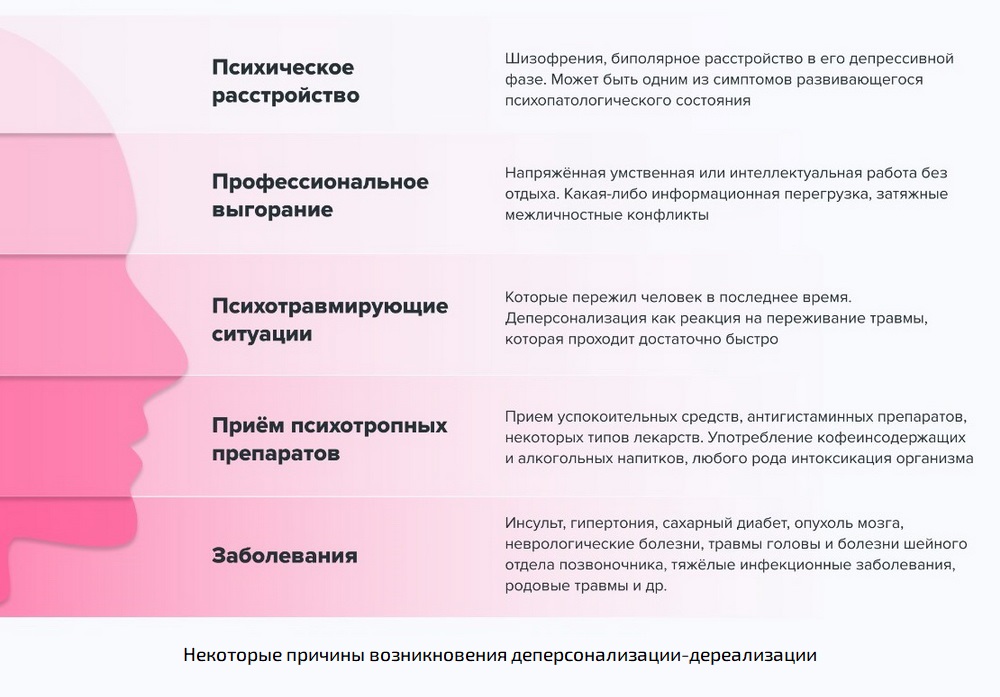
Depersonalization is a complex topic, and researchers still don’t know a lot about it. What they do know is that it’s a type of dissociation, often caused by traumatic or stressful events like a panic attack, an accident, abuse, or assault. Sometimes, depersonalization is caused by a negative experience with cannabis or other substances.
Additional symptoms of depersonalization can include memory loss and out-of-body experiences. In addition, anxiety or depression can often occur alongside depersonalization, which can make your experience more intense.
If you’ve experienced any of these symptoms, you’re not alone. Various types of support may help ease your distress around depersonalization — from self-care and online groups, to therapy and education. With that in mind, here are several resources that you may find helpful.
About 75% of people experience feelings of depersonalization at some point in their lives. For 2% of the population, the symptoms become more frequent. This can result in a diagnosis of depersonalization/derealization disorder (DPDR).
Dissociation can also occur with post-traumatic stress disorder (PTSD) and borderline personality disorder (BPD), so you may not necessarily be diagnosed with DPDR separately.
Many theorists believe that dissociation is your body’s way of protecting you from extreme trauma or stress.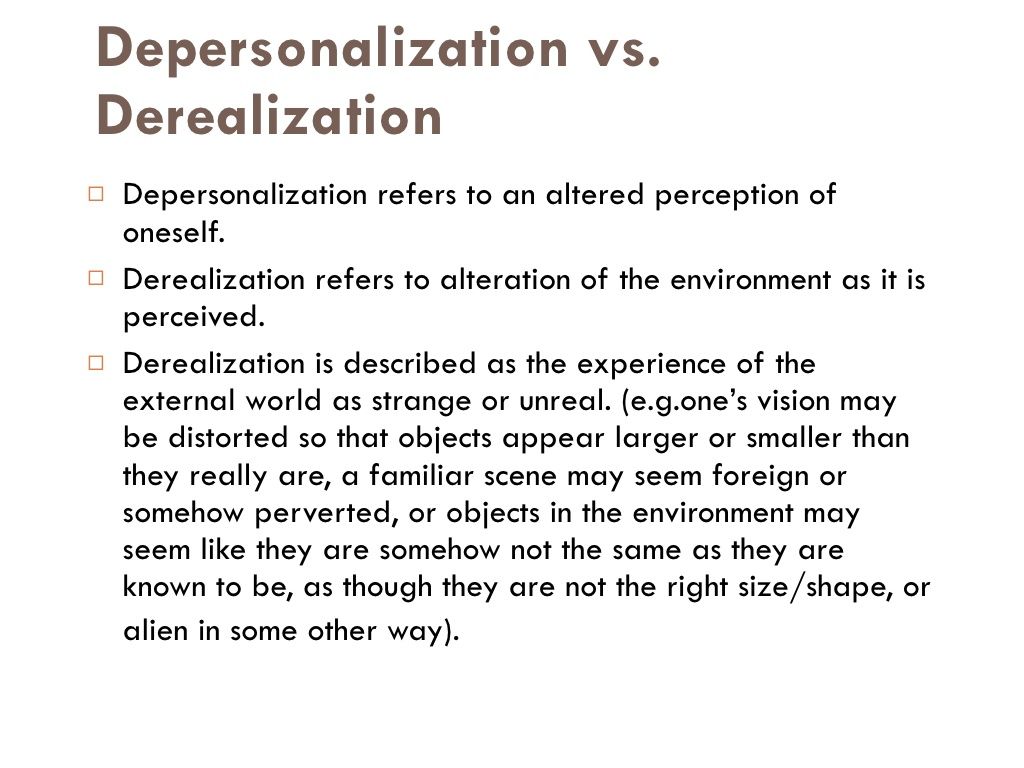 Others assert that it’s less of a protective function and more like a scar from the traumatic event (or set of events) itself.
Others assert that it’s less of a protective function and more like a scar from the traumatic event (or set of events) itself.
While depersonalization symptoms can interfere with your quality of life, managing the distress caused by them is possible. It’s important to work with a mental health professional who’s able to support you with the best treatment plan for your symptoms.
Many tools can help you manage feelings of anxiety, depression, or distress about living with depersonalization. Treatments for PTSD and BPD may also have a beneficial effect on depersonalization symptoms.
First things first: When symptoms arise, try to remind yourself that you’re OK and that you’re safe. Naming your feelings, practicing deep breathing, or listening to music can also help you feel calmer. In addition, challenging your intrusive thoughts and reaching out to close friends may help you feel grounded.
1. Acknowledge your feelings
According to many psychology researchers, depersonalization may be an adaptive way to cope with stress. Some believe that it’s your brain’s way of protecting you from danger. When your body and mind distance you from intense emotional pain, overwhelming feelings may decrease, which may help you feel safe at that moment.
Some believe that it’s your brain’s way of protecting you from danger. When your body and mind distance you from intense emotional pain, overwhelming feelings may decrease, which may help you feel safe at that moment.
If your body and mind ignore your feelings for too long, symptoms of depersonalization may drag on. In these cases, your brain misreads danger, and feelings of depersonalization increase.
When this happens, you might try to name your feelings. Some research suggests that by acknowledging certain emotions (in this case, fatigue), you can lessen stress. It’s possible that this concept may work on other painful emotions as well. In turn, this may decrease symptoms of derealization, though more research is obviously needed.
Self-compassion exercises may help you accept whatever feelings arise at that moment.
2. Take deep breaths
When stress arises, your body’s nervous system fires up. For people living with depersonalization disorder, this can disrupt brain functioning and lead to feelings of depersonalization.
Breathing exercises, like taking deep belly breaths, may help against this stress.
If you want some guidance from a meditation teacher, consider downloading a mindfulness app or look for a free guided meditation on YouTube or TikTok. If deep breathing is helpful, you might consider practicing your exercises for a few minutes each day. Like exercise, deep breathing can become easier with practice.
3. Listen to music
Feelings of derealization can be more intense when your brain focuses on them. A grounding technique, like listening to music, may help you feel less anxious about the experience.
Research shows that music can help reduce cortisol levels, a stress hormone, in your system.
You might consider making a playlist of your favorite songs and keep the playlist on your phone. When symptoms arise, even if you’re at work or waiting for the bus, you can pop in your earbuds, press play, and let the music soothe you.
4. Read a book
If you enjoy reading, it may help with depression and the anxious thoughts that often occur alongside depersonalization. Try picking up an old favorite book, or a story that brings you comfort. You might find that you’re able to concentrate on the words and their meanings enough to quiet intrusive thoughts.
Try picking up an old favorite book, or a story that brings you comfort. You might find that you’re able to concentrate on the words and their meanings enough to quiet intrusive thoughts.
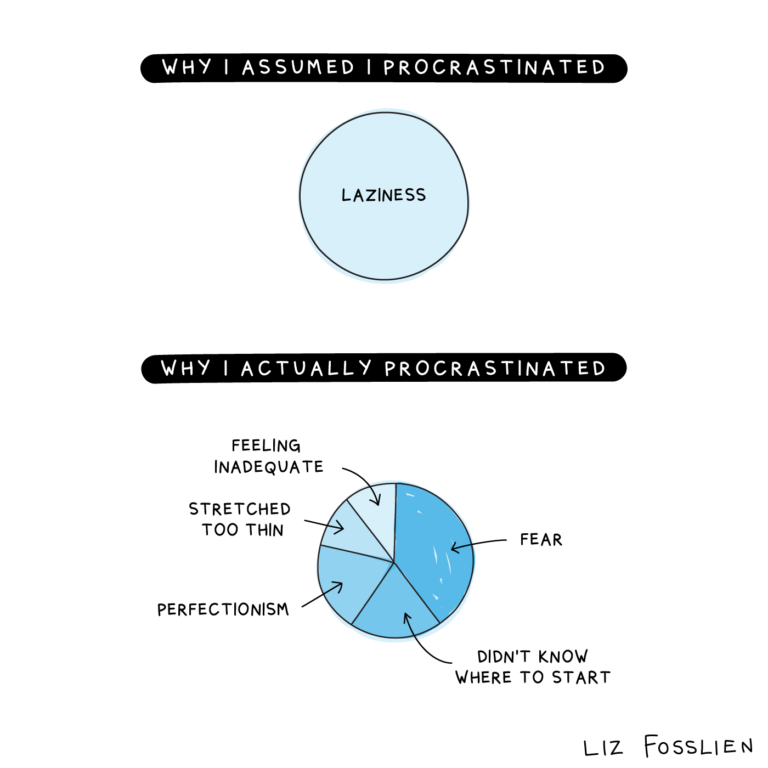
5. Challenge your intrusive thoughts
For some, depersonalization involves a lack of intrusive thoughts. For others who live with depersonalization as well as anxiety or PTSD, intrusive thoughts can pose a real challenge.
Cognitive psychologists point out that a tool called psychological distancing can help quiet intrusive thoughts. Psychological distancing means finding some space between the upsetting thoughts and painful emotions.
Taking a few deep breaths can help quiet intrusive thoughts. As odd as it might sound, talking to yourself out loud can also help. You might ask yourself, “What evidence do I have that my worry is real?”
Basically, when your mind focuses on something else, intrusive thoughts often go away.
6. Call a friend
When you’re anxious and symptoms of depersonalization arise, you might be tempted to isolate. But at times like these, talking to a trusted friend or family member can really help.
But at times like these, talking to a trusted friend or family member can really help.
Opening up can make you feel vulnerable. But talking gives you a chance to receive empathy from someone who cares about you. If you’re not sure who to lean on, try to identify two or three loved ones that you can text or keep on speed dial, no matter what.
Self-care tools can help relieve symptoms of depersonalization. In addition, psychotherapy, education, nutrition, and exercise can help you maintain a sense of well-being in the long run.
7. Talk therapy
If your symptoms of depersonalization are caused by a stressful or traumatic experience, talking with a therapist may really help.
Several types of therapy can work. Cognitive-behavioral therapy (CBT) can teach you to challenge intrusive thoughts and manage symptoms of depersonalization. Trauma-focused therapy like eye-movement desensitization and reprocessing therapy (EMDR) can help you process traumatic memories.
Once your trauma heals, symptoms of depersonalization may lessen.
8. Education
Learning more about the symptoms and causes of depersonalization disorder can also help. The National Alliance on Mental Illness (NAMI) has resources and information. Finding out how depersonalization affects your brain can make symptoms less frightening. In addition, reading about other people’s experiences is one way to feel less alone.
9. Sleep
Going to bed when your body feels tired can help you manage stress and decrease anxiety. The Centers for Disease Control and Prevention (CDC) recommends going to bed and waking up at the same time each day.
If you’d like to improve your sleep, you might also consider banning your phone and other electronics from your bedroom. If possible, try to keep your sleep space as dark as you can. Darkness helps regulate the body’s circadian rhythms, which can improve the quality of your sleep.
10. Exercise
Like getting enough rest, exercise can also help you manage stress. One study found that aerobic exercise can help decrease burnout, and one symptom of burnout is depersonalization.
If you’re interested in exercise but aren’t sure what to choose, walking could be a good option. Walking can help lower your body’s cortisol, which can help decrease stress.
If you’re living with depersonalization disorder, finding the right type of support can be an essential part of self-care.
If you’d like to find a mental health professional, the American Psychiatric Association (APA) has a searchable database that can help you find a therapist. If you’re looking for a local support group, you might contact your local National Alliance on Mental Health (NAMI) chapter.
If you’d like to read about other people’s experiences with depersonalization, you can check out the NAMI blog post, “The Scariest Panic Symptoms People Don’t Talk About,” which is one person’s story about living with depersonalization disorder. You can find other blog posts here and here.
If you’re interested in checking out some mental health podcasts, The Anxiety Podcast seeks to support anyone struggling with anxiety, stress, and panic attacks. The Spin Cycle is another mental health podcast that features interviews with mental health professionals.
The Spin Cycle is another mental health podcast that features interviews with mental health professionals.
Maybe you’re ready to check out meditation, but you aren’t sure where to start. Meditation Minis is a podcast that includes several types of guided meditations. And if you’re on Clubhouse, meditation teacher Lisa Abramson leads mindfulness classes every day.
Finally, know that taking care of your mental health takes courage! Sure, it can feel frustrating at times, and that’s OK. No one expects you to be perfect. With more mental health resources and tools available, living with depersonalization disorder is much easier.
Treatment of depersonalization and derealization in St. Petersburg
- Main
- Psychiatry
- Treatment of depersonalization and derealization
We treat depersonalization and derealization in our clinic. To start the treatment of the syndrome, a face-to-face consultation with a psychiatrist and a differential examination are necessary to clarify the diagnosis and exclude / confirm diseases that cause a similar condition against the background of the course (for example, OCD, phobic and depressive disorders, delusional and dissociative disorders, early dementia). nine0011
About half of the world's population has experienced a state of depersonalization-derealization at least once in their lives. But only 2% of them fully meet the diagnostic criteria for the syndrome.
In order to shorten the period of selection of pharmacotherapy in the treatment of depersonalization and derealization, hospitalization is required (4–6 weeks). The conditions of the hospital allow you to monitor the patient's condition in dynamics and promptly adjust drug treatment. Also, in the hospital of the clinic, patients are provided with psychotherapeutic assistance, which precedes individual and / or group sessions after discharge, adapting to a full life in the family and society. nine0011
Also, in the hospital of the clinic, patients are provided with psychotherapeutic assistance, which precedes individual and / or group sessions after discharge, adapting to a full life in the family and society. nine0011
In particular, if the disease has caused intra-family conflicts, they can be resolved in family therapy sessions. In addition, participation in a group of open problems will allow you to get rid of internal experiences, restore lost communication skills. In parallel with outpatient treatment (taking prescribed drugs), one should not forget about visits to the attending physician, who should be informed of any conditions that cause anxiety or seem unusual. Such an approach to the treatment of depersonalization and derealization will make it possible to correct drug treatment in a timely manner, get rid of addictive attitudes and, as a result, prevent a relapse of the disease. nine0011
Doctor's consultation on the treatment of depersonalization:
+7 (812) 407-18-00
Thank you for your trust!
- Assistance in resocialization
- Safe drug therapy
- Psychologists with clinical experience
| Service | Price | |
|---|---|---|
| Psychotherapist appointment | 5 000 ₽ | nine0043|
| Family Therapy | 10 000 ₽ | |
| Hypnotherapy | 8 000 ₽ | |
| Psychiatric consultation | 5 000 ₽ Depersonalization under academic stress — https://pubmed. Update date: 12/28/2020
Make an appointment Date and time: (not set) Make an appointment with a psychiatrist nine0010 Make an appointment with a psychiatristSelect the date and time of your appointment Today Dec 30 Sunday January 01 Monday January 02 Tuesday January 03 Wednesday 04 January Thursday 05 January Friday January 06 Saturday 07 January Sunday January 08 Monday January 09 Tuesday January 10 Wednesday January 11 Thursday January 12 Friday January 13 Saturday January 14 Sunday January 15 Monday January 16 Tuesday January 17 Wednesday January 18 Thursday January 19 Friday January 20 Saturday January 21 Sunday January 22 Monday January 23 Tuesday January 24 Wednesday January 25 Thursday January 26 Friday January 27 Saturday January 28 Sunday January 29 Monday January 30 Tuesday January 31 Treatment of depersonalization and derealization is carried out Bocharov Alexey Psychiatrist, psychotherapist Psychiatrist, psychotherapist, sexologist, child psychiatrist Experience 41 years Sinenchenko Andrey Psychiatrist, psychotherapist Psychiatrist, psychotherapist, narcologist Work experience 22 years Zun Sergey Psychiatrist, narcologist Psychiatrist, narcologist, psychotherapist Work experience 33 years Lisitsyna Elena Psychiatrist Psychiatrist Work experience 33 years nine0010 Buchelnikova VictoriaViktorovna Psychiatrist Psychiatrist Work experience 15 years Voronina Elvira Psychiatrist Psychiatrist Work experience 27 years Efimova Evgenia Second category Work experience 19 years Psychiatrist Work experience 19 years Gorobets Elena Psychiatrist Psychiatrist Work experience 16 years Travnikova Oksana Psychiatrist Psychiatrist Work experience 21 years Kurochkina Nadezhda Psychiatrist Psychiatrist Work experience 19years Suslennikova Elena Psychiatrist, psychotherapist Psychiatrist, psychotherapist Work experience 25 years Chuban Olga Psychiatrist, psychotherapist Psychiatrist, psychotherapist, psychologist Work experience 13 years nine0010 Popov AndreyPetrovich Psychiatrist Psychiatrist Experience 35 years Stetsiv Ludmila Psychiatrist, psychotherapist Psychiatrist, psychotherapist Work experience 31 years Prokhorchev Konstantin Psychiatrist, psychotherapist Psychiatrist, psychotherapist Work experience 12 years Gulevsky Roman Head of hospital Experience 25 years Psychiatrist, narcologist Experience 25 years Konoplin Dmitry Narcologist, psychiatrist Narcologist, psychiatrist Work experience 24 years Stavitskaya Svetlana Psychiatrist Psychiatrist Work experience 24 years Pylskaya Anna Psychiatrist Psychiatrist Work experience 7 years Trofimova Alexandra Psychiatrist, child psychiatrist Psychiatrist, child psychiatrist Experience 28 years Zhelobetskaya Maria Psychiatrist, psychotherapist Psychiatrist, psychotherapist Work experience 22 years nine0010 Endrzheevskaya DianaVadimovna Psychiatrist, psychotherapist Psychiatrist, child psychiatrist, psychotherapist Work experience 14 years nine0010 Ivanov AlexanderNikolaevich Psychiatrist, narcologist Psychiatrist, narcologist Experience 20 years Semenov Andrey Psychiatrist, narcologist Psychiatrist, narcologist, transfusiologist Work experience 24 years Leave a request for a call: +7 (812) 407-18-00 nine0000 Depersonalization and derealization in Moscow Depersonalization and derealization are manifested in the form of sensations, when it seems to a person that he is living in a dream or is watching himself from the outside. Depersonalization and derealization are experienced by ordinary people, but usually these feelings are fleeting. However, if they occur constantly or do not go to the end and affect the quality of life (they interfere with living a normal life), then it can be assumed that this is a disorder. More common in people who have had a traumatic experience, or as a symptom of anxiety or depression. nine0011 Depersonalization-derealization disorder can be severe and interfere with relationships, work, and other daily activities. The main treatment for depersonalization-derealization disorder is talking therapy (psychotherapy), although drugs are sometimes used. Symptoms of depersonalizationDuring derealization, a person feels like an outside observer of life:
Symptoms of derealizationMost often, the symptoms manifest themselves in the form of "strange" sensations:
Such distortions can usually last for several minutes, hours, days, weeks or even months. nine0011 When to See a DoctorMomentary feelings of depersonalization or derealization are common and not necessarily a cause for concern. However, persistent or strong feelings of detachment and distortion of the world around you, which impair the quality of life, may be a sign of an emotional disorder. See a doctor if feelings of depersonalization or derealization:
CausesThe exact cause of depersonalization-derealization disorder has not been fully elucidated. Some people may be more prone to depersonalization and derealization than others, possibly due to genetic and environmental factors. An increased state of stress and fear, prolonged anxiety or depression can provoke seizures. nine0011 Symptoms of depersonalization-derealization disorder may be related to childhood trauma or other experiences or events that caused severe emotional stress or trauma. Causing factorsFactors that may increase the risk of developing depersonalization/derealization disorder include:
What are the risks?Difficulty concentrating on tasks or remembering things Interference in work and other daily activities Relationship problems with family and friends Feeling of hopelessness DiagnosisYour doctor may diagnose or rule out depersonalization/derealization disorder based on:
DSM-5. Your mental health professional may use the criteria for depersonalization-derealization disorder listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) published by the American Psychiatric Association. Treatment Treatment of depersonalization-derealization disorder is primarily psychotherapy. PsychotherapyPsychotherapy is the main treatment for these symptoms. The goal of therapy is to control symptoms so that they decrease or disappear. Several types of evidence-based therapy are suitable for this - CBT (cognitive behavioral therapy) and ACT (acceptance and responsibility therapy). How psychotherapy can help:
learn techniques to help you take your mind off your symptoms and feel more connected to your world and feelings PharmacotherapyThere are no drugs specifically approved for the treatment of depersonalization/derealization disorder. However, medications may be used to reduce specific symptoms or to treat depression and anxiety, which often cause symptoms of derealization or depersonalization.
Preparing for your doctor's appointmentMake a list before you see your doctor:
Questions to ask your doctorTop questions to ask your doctor include:
What to expect from your consultation Your doctor will likely ask you a number of questions. |
 ncbi.nlm.nih.gov
ncbi.nlm.nih.gov  branch
branch 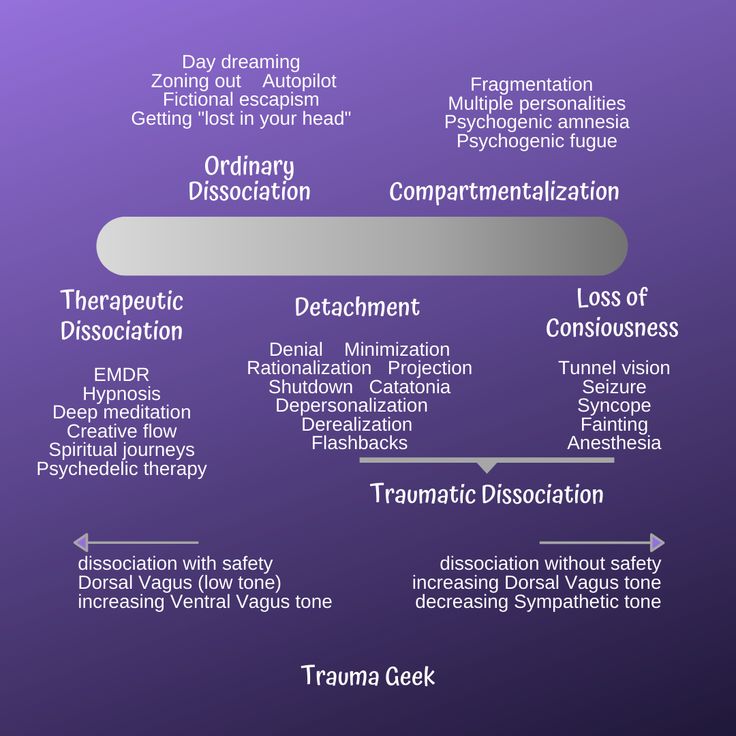

 nine0011
nine0011 
 In some cases, symptoms of depersonalization or derealization may be related to an underlying physical health problem, medications, recreational drugs, or alcohol. nine0011
In some cases, symptoms of depersonalization or derealization may be related to an underlying physical health problem, medications, recreational drugs, or alcohol. nine0011  However, sometimes drugs may be added to the treatment plan. nine0011
However, sometimes drugs may be added to the treatment plan. nine0011 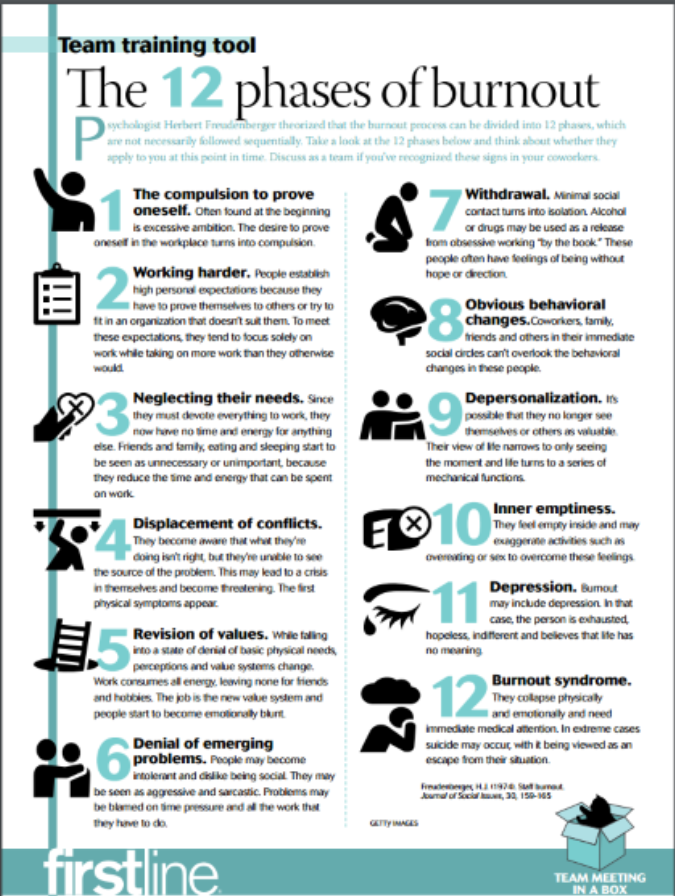 nine0011
nine0011  In books and online resources you can find information about why depersonalization and derealization occur and how to deal with them. Ask your mental health professional for recommendations on educational materials and resources. nine0011
In books and online resources you can find information about why depersonalization and derealization occur and how to deal with them. Ask your mental health professional for recommendations on educational materials and resources. nine0011