Coughing that makes me gag
Coughing So Hard That You Vomit: Causes, Treatments, and Diagnosis
Sometimes, a cough is so severe that it may cause you to vomit. This may be an indication of an underlying illness or allergy, and it can be treated in a number of ways.
Why do we cough?
Coughing is the body’s way of trying to rid the lungs of mucus, foreign matter, and microbes that can cause infection and illness. You might develop a cough from irritants in the environment that you’re sensitive to. This could be because of an allergic reaction, a virus, or bacterial infection.
Some illnesses and conditions can cause both adults and children to cough so intensely that they vomit.
Several conditions can cause severe bouts of coughing in adults. These may be the result of an acute, short-term illness or allergy. They may also be chronic and last for many weeks, months, or even years.
Causes of coughing severe enough to induce vomiting include:
- Cigarette smoking.
Cigarette smoking causes smoker’s cough. It can be wet or dry, and may induce vomiting, and other severe health issues such as emphysema.
- Postnasal drip. Postnasal drip is when mucus that’s produced drips down the throat, triggering coughing bouts that can cause vomiting.
- Asthma. Symptoms of asthma include coughing, wheezing, breathlessness, and excessive production of mucus. These symptoms can also cause vomiting.
- Cough variant asthma. Coughing is the only symptom of cough variant asthma. It produces a dry, persistent cough that can be severe enough to induce vomiting.
- Acid reflux and gastroesophageal reflux disease (GERD). Acid reflux and GERD can both cause irritation in the lower esophagus. This can trigger coughing and a sore throat, among other symptoms.
- Acute bronchitis. Acute bronchitis causes a cough that may produce large amounts of mucus, which can create gagging and vomiting.
 A dry, wheezing cough that’s intense enough to trigger vomiting may continue to linger for weeks after the infection has dissipated.
A dry, wheezing cough that’s intense enough to trigger vomiting may continue to linger for weeks after the infection has dissipated. - Pneumonia. Pneumonia can produce extreme bouts of coughing and vomiting as a result of mucus being expelled from the lungs or from a severe, postnasal drip.
- Some blood pressure medications. Angiotensin-converting enzyme (ACE) inhibitors is a blood pressure medication that sometimes causes severe, chronic coughing. ACE inhibitors are used to treat high blood pressure and heart failure.
Some conditions that cause coughing-related vomiting in adults can have the same effect in children. These include pneumonia, bronchitis, asthma, cough variant asthma, postnasal drip, and acid reflux.
Other conditions include:
- Pertussis (whooping cough). This is a respiratory tract infection. It causes intense and rapid coughs that typically drain the lungs of air, causing the person to gasp in oxygen.
 This causes a whooping sound. Vomiting is a common reaction to these symptoms.
This causes a whooping sound. Vomiting is a common reaction to these symptoms. - Respiratory syncytial virus (RSV). RSV causes inflammation of the lungs and breathing passages. It’s a leading cause of bronchitis and pneumonia in babies.
Vomiting induced by coughing is not by itself a medical emergency. If it’s accompanied by these other symptoms, seek medical treatment immediately:
- coughing up blood
- trouble breathing or rapid breathing
- lips, face, or tongue turns blue or dusky-colored
- dehydration symptoms
A doctor will want to rule out seasonal allergies and other potential allergens as a cause. They will ask about other symptoms you may have, such as heartburn, fever, and muscle aches to determine if you might have acid reflux, GERD, a common cold, or the flu.
Several tests may be used to diagnose this condition in adults and children. They include:
- chest X-ray: to look for signs of pneumonia
- sinus X-ray: to look for sinus infection
- CT scan: to look for areas of infection in the lungs or sinus cavities
- lung function test: to give the doctor information about your ability to intake air to diagnose asthma
- spirometry test: to gather information about air intake ability and asthma
- scope tests: require a bronchoscope, which has a small camera and a light to look at your lungs and air passages, or a similar type of tube called a rhinoscope can be used to look at the nasal passages
The underlying conditions for your symptoms need to be treated in order for your coughing and vomiting to resolve (dissipate). Some medications used to treat coughs include:
Some medications used to treat coughs include:
- decongestants: for allergies and postnasal drip
- glucocorticoids: for asthma, allergies, or postnasal drip
- bronchodilator or inhaler: for asthma
- antihistamines: for allergies and postnasal drip
- cough suppressants: for coughs with a cause that cannot be specified
- antibiotics: for bacterial infection, including pertussis
- acid blockers: for acid reflux and GERD
Most conditions benefit from bed rest and drinking lots of fluids. If symptoms get worse or do not improve within a few days, ask your doctor about the next steps.
Most conditions that cause this symptom are acute and short-lived. Once the underlying cause has been addressed, your coughing and vomiting will go away.
Some conditions that cause this symptom are long-lasting and require a doctor’s care and ongoing medication.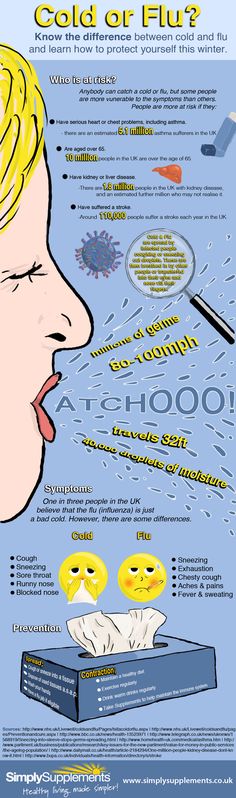
In many cases, your symptoms will get better if you stick to the treatment plan your doctor creates for you.
Not smoking cigarettes is one of the best ways to safeguard your health. If you smoke, consider talking with your doctor about a smoking-cessation regimen as a way of helping prevent chronic coughing.
Other ways you can prevent this symptom is by keeping your environment free of allergens, dust, and chemical irritants. An air purifier may help you do this.
Washing your hands often and avoiding individuals who are sick can help you avoid many germs (disease-causing agents) that cause the common cold, flu, and other illnesses that have coughing and vomiting as symptoms.
Because there are many different ailments that may lead to a cough, there are many different ways to treat it. Some people prefer home remedies instead of an over-the-counter (OTC) treatment.
Here are a few known cough remedies that you may be able to find in your own home.
1.
 Ginger
GingerFor thousands of years, people have used ginger to help manage coughs, fever, sore throats, and asthma. Research has shown that polysaccharides in ginger can help suppress coughing.
Ginger has also demonstrated antioxidant and anti-inflammatory properties, though more research involving humans is needed to further understand these benefits.
An easy way to treat your cough with ginger is by drinking a hot ginger tea, which may help reduce irritation in your throat.
2. Peppermint
Peppermint contains menthol, which has both anti-inflammatory and antiviral effects.
The Mentha species, which includes plants in the mint family, has a variety of health benefits, including antioxidant and antimicrobial potential.
You can use peppermint in the form of peppermint tea or through peppermint essential oil drops infused in a steam treatment.
While research suggests there are health benefits, the FDA doesn’t monitor or regulate the purity or quality of essential oils. It’s important to talk with a healthcare professional before you begin using essential oils, and be sure to research the quality of a brand’s products. Always do a patch test before trying a new essential oil.
It’s important to talk with a healthcare professional before you begin using essential oils, and be sure to research the quality of a brand’s products. Always do a patch test before trying a new essential oil.
3. Honey tea
Honey can help reduce coughing and related symptoms like mucus in the throat.
Research has shown giving honey to children before bed reduced cough severity and frequency.
You can mix half a teaspoon of honey with milk for children or consume it in the form of honey tea for adults. However, be sure to avoid feeding honey to children younger than 1 year.
It’s important to check with a doctor if your cough is severe or persists for several weeks.
Causes of Cough Attacks and How to Stop Them
Violent coughing fits, or paroxysmal coughing, is usually caused by bacteria, although there are other causes.
Paroxysmal coughing involves frequent and violent coughing that can make it hard for a person to breathe.
Coughing is an automatic reflex that helps your body to get rid of extra mucus, bacteria, and other foreign substances.
With an infection like pertussis, your cough may persist for long periods of time, making it hard to get enough oxygen or catch your breath. This can cause you to inhale sharply and gasp loudly for air, which is why pertussis is also known as whooping cough.
In 2012, the last peak year for whooping cough, the Centers for Disease Control and Prevention (CDC) reported nearly 50,000 cases of pertussis.
More recently, in 2019, the CDC reported nearly 19,000 cases. Many of these cases, especially in young children, involve paroxysmal coughing fits.
Read on to learn what causes paroxysmal coughing, how it’s treated, how to prevent it, and when you should see a doctor.
Paroxysmal coughing is commonly caused by Bordetella pertussis bacterium. This bacterium infects your respiratory tract (your nose, throat, windpipe, and lungs) and causes whooping cough. This infection is extremely contagious.
This infection is extremely contagious.
Paroxysmal coughing is the second stage of whooping cough. According to the CDC, this stage comes about 2 weeks into the infection. A typical case of paroxysmal coughing lasts from 1 to 6 weeks before it lets up.
In severe cases, fits of paroxysmal coughing can become so intense that you vomit, and your lips or skin can turn blue from a lack of oxygen in the blood. Seek emergency medical care if you experience these symptoms.
Other possible causes of paroxysmal coughing include:
- asthma, a respiratory condition in which your airways become swollen and filled with excess mucus
- bronchiectasis, a condition in which tubes in your lungs are permanently widened with thickened walls due to inflammation, causing a buildup of bacteria or mucus
- bronchitis, an inflammation in the bronchi of the lungs
- gastroesophageal reflux disease (GERD), a condition in which acid from your stomach comes back up your esophagus and into your throat and sometimes into your airways
- lung injury from trauma, smoke inhalation, or drug use
- pneumonia, a type of lung infection
- tuberculosis (TB), a bacterial infection of the lungs that can spread to other organs if left untreated
If your cough is caused by a respiratory infection in your chest, such as pneumonia or bronchitis, you may have the following symptoms:
- a wet cough
- coughing up yellow or green mucus
- wheezing or feeling out of breath
- chest discomfort
- fever
- headache
A chest infection may last about 7 to 10 days before going away on its own. The wet coughing can last up to 3 weeks.
The wet coughing can last up to 3 weeks.
A cough due to pneumonia may be louder than other types of coughs, according to a 2021 study.
Researchers collected cough sounds from 30 adults and then used an artificial intelligence (AI)-based algorithm to diagnose those with pneumonia, with about 85% accuracy.
The pneumonia cough sounds were louder, especially at the end of the cough.
If you see a doctor about a coughing fit, they may order one or more of the following tests to diagnose the cause:
- nasal or throat swab to test for the presence of infectious bacteria
- blood test to check for a high white blood cell count, which can indicate an infection
- X-ray or CT scan of the chest or sinuses to look for symptoms of respiratory infections, damage, or abnormalities
- spirometry or other lung function tests to assess how your body takes in and expels air, to diagnose asthma
- bronchoscopy with a thin, lighted tube and camera that can show real-time images of the inside of your lungs
- rhinoscopy to see real-time images of the inside of your nose and nasal passages
- upper gastrointestinal endoscopy of your digestive tract to check for GERD
Once a doctor diagnoses a cause, they may prescribe a variety of treatments. These may include:
These may include:
- antibiotics, including azithromycin (Z-Pack), to help your immune system fight infectious bacteria
- decongestants, such as pseudoephedrine (Sudafed), or the cough expectorant guaifenesin (Mucinex), to reduce mucus buildup, coughing, and other symptoms
- antihistamines, such as cetirizine (Zyrtec), to reduce allergy symptoms that may worsen coughing, such as congestion, sneezing, and itching
- an inhaler or nebulized bronchodilator treatment to help open airways during coughing fits or asthma attacks
- antacids for symptoms of GERD
- proton pump inhibitors like omeprazole (Prilosec), which reduce stomach acid production, to help your esophagus heal from GERD
- breathing exercises for conditions like bronchitis
Try the following at home to reduce coughing fits:
- Drink at least 64 ounces of water a day to keep yourself hydrated.
- Bathe regularly to keep your body clean and limit bacterial spread.

- Wash your hands often to keep bacteria from building up and spreading.
- Use a humidifier to keep your airways moist, which can help loosen mucus and make it easier to cough up. Don’t overuse your humidifier, as this can make it easier for bacteria to reproduce.
- If you are vomiting, eat small portions at meals to reduce the volume of vomit.
- Reduce or eliminate your exposure to smoke from tobacco products or fumes from cooking and fireplaces.
- Stay isolated from others as much as possible to keep the bacterial infection from spreading. This includes 5 days of isolation while you’re taking antibiotics. Wear a mask if you plan to be around others.
- Don’t use heavily scented products like air freshener sprays, candles, cologne, or perfume that can irritate your airways.
Paroxysmal coughing from whooping cough is common in young children. Get your child vaccinated with the diphtheria-tetanus-pertussis (DTaP) or tetanus-diphtheria-pertussis (Tdap) vaccine to prevent them from being susceptible to infection by pertussis bacteria.
If someone close to you has whooping cough, avoid touching or being near them until they’ve taken antibiotics for at least 5 days.
Here are other ways to help prevent paroxysmal coughing:
- Avoid smoking tobacco products or other inhaled drugs.
- Sleep with your head elevated to keep mucus or stomach acid from moving up your airways or throat.
- Exercise often to make it easier to breathe and to prevent weight gain that can contribute to acid reflux and GERD.
- Eat at a slow pace and chew at least 20 times per bite for easier digestion.
- Use an essential oil diffuser to help open your airways. Certain oils can be more potent than others, so be careful if you try this for relief. If this worsens your coughing, avoid using them.
- Try relaxation techniques, such as yoga or meditation, to gain control of your breathing, strengthen your immune system, and prevent acid reflux.
See a doctor as soon as possible if paroxysmal coughing fits last longer than a week and becomes increasingly frequent or violent.
Some accompanying symptoms may mean you have a serious infection or underlying condition causing your coughing fits. Seek emergency medical help if you experience any of the following:
- coughing up blood
- vomiting
- not being able to breathe or breathing quickly
- lips, tongue, face, or other skin turning blue
- losing consciousness
- fever
- chills
Paroxysmal coughing can have a variety of causes, but it’s commonly a result of a pertussis infection.
In some cases and depending on the cause, it will go away on its own, but some causes, such as asthma, pertussis, and TB, require immediate treatment or long-term management.
See a doctor if you have a persistent cough that’s disrupting your life or regularly making it difficult for you to breathe. Many causes can be treated without the risk of complications if they’re diagnosed early.
Cough in adults - causes, examination and treatment in Astrakhan | Symptoms
Exacerbation of chronic obstructive pulmonary disease (COPD)
Signs: Wheezing, shortness of breath and breathing through pursed lips. Cough is often accompanied by phlegm. In people who already have COPD.
Cough is often accompanied by phlegm. In people who already have COPD.
Foreign body
Signs: A cough that comes on suddenly in people with an underlying medical condition that makes it difficult to communicate, swallow, or both. No symptoms of an upper respiratory tract infection. In people who feel good in every other way.
Heart failure
Signs: Shortness of breath that worsens when lying down and occurs 1-2 hours after falling asleep. Usually, lung sounds heard through a stethoscope indicate the possible presence of fluid in the lungs. Usually swelling of the legs.
Pneumonia
Signs: Fever, malaise, coughing up sputum (productive cough), and shortness of breath. Sudden attacks of pain in the chest, aggravated by taking a deep breath. Some unusual breathing sounds heard through a stethoscope.
Post nasal syndrome (associated with allergy, virus or bacteria)
Signs: Headache, sore throat and nasal congestion with pale, edematous mucosa. Nausea. Sometimes postnasal drip is seen on the back of the throat.
Nausea. Sometimes postnasal drip is seen on the back of the throat.
Pulmonary embolism (sudden blockage of the pulmonary artery, most often by a blood clot)
Signs: Sudden onset of chest pain that usually worsens with inspiration, shortness of breath, rapid heart rate, and rapid breathing. Risk factors: cancer, weakness, pregnancy, use of birth control pills, recent surgery or hospitalization, and a family history of a similar disease.
Upper respiratory infections (acute bronchitis)
Signs: Runny nose, nasal congestion with reddening of the mucous membrane. Sore throat and feeling unwell.
Residual respiratory tract irritation (after recovery from respiratory tract infection)
Signs: Dry, non-productive cough that occurs immediately following a respiratory tract infection. No nasal congestion and sore throat.
Aspiration
Signs: Wet cough after eating or drinking, noticeable difficulty swallowing, or both. People who have had a stroke or have another condition that causes communication difficulties (dementia).
People who have had a stroke or have another condition that causes communication difficulties (dementia).
Asthma (cough variant)
Signs: Cough that occurs when exposed to various irritants, such as pollen or other allergen, a cold, or exercise. Perhaps wheezing and shortness of breath.
Chronic bronchitis (in smokers)
Signs: Productive cough on most days of the month for 3 months of the year for 2 years in a row. Frequent attempts to clear the throat and shortness of breath. No nasal congestion and sore throat. In people with COPD.
Gastroesophageal reflux
Signs: Burning pain in the chest (heartburn) or abdomen, often worse after eating certain foods, exercising, or lying down. Sour taste, especially after waking up. Hoarseness of voice, wheezing. Cough that comes on at night or in the early morning. Sometimes there are no other symptoms other than a cough.
Lung tumor
Signs: Cough, sometimes with blood. Weight loss, fever and night sweats. Enlarged, hard, painless lymph nodes in the neck.
Weight loss, fever and night sweats. Enlarged, hard, painless lymph nodes in the neck.
Tuberculosis or fungal infections
Signs: Cough, sometimes with blood. Weight loss, fever and night sweats. Contact with a person with tuberculosis. Living or staying in an area where tuberculosis or fungal lung infections are common. Having HIV infection or risk factors for developing HIV infection.
How to get rid of a cough and when to go to the doctor
Coughing can be a concern at any time of the year. Together with the general practitioner, we understand the possible causes and consider treatment options.
The respiratory tract of our body is covered with a thin layer of cells with cilia. They are constantly moving and remove all the mucus and dirt from the lungs and bronchi to the outside. But if the amount of irritants or mucus is too high, as well as when a foreign body enters, the second one comes to the rescue of the first defense mechanism - cough.
Andrey Besedin, PhD, general practitioner, family doctor at GMS Clinic.
Coughing is a protective reflex of our airways. It is needed to shake off all the excess that gets there. Coughing effectively rids the body of almost any irritant that can enter the respiratory tract.
Why there is a cough
A cough can start due to any object or substance that has entered the respiratory tract: food fragments, perfume vapors or aerosol. Sometimes it's caused by allergies, and sometimes it's stress.
Most often, coughing is provoked by viruses or bacteria and their metabolic products. In this case, the cough is called infectious, and its manifestations will differ depending on the pathogen:
Manifestations of infectious cough:
- Coronavirus infection. The cough is most often dry, debilitating, in addition to this, there are other symptoms: shortness of breath, weakness, fever, headache.
- Pneumonia.
 Symptoms depend on the type of infection, but often the disease begins with a cough that grows and turns into a persistent wet cough. The amount of sputum increases, chest pain, fever, weakness may appear. There is a general deterioration in the condition.
Symptoms depend on the type of infection, but often the disease begins with a cough that grows and turns into a persistent wet cough. The amount of sputum increases, chest pain, fever, weakness may appear. There is a general deterioration in the condition. - Bronchitis. The cough is wet, after expectoration it becomes easier. With deep breathing, sounds are sometimes heard in the chest - they are caused by the fact that sputum accumulates in the bronchi.
- Whooping cough. The cough in this disease is debilitating, paroxysmal, prolonged, it interferes with sleep. It is difficult to find a position to alleviate the condition. From constant coughing, the intercostal muscles hurt, and hemorrhage in the eye may occur. Over time, the frequency of seizures decreases, but this condition sometimes lasts for several months.
Cough can be a sign not only of an infectious disease, but also of other conditions and diseases.
More common than others are:
- Allergy and asthma.
 In most cases, coughing fits occur after contact with an irritant in the air.
In most cases, coughing fits occur after contact with an irritant in the air. - Chronic obstructive pulmonary disease (COPD) is a lung disease characterized by chronic airflow limitation in the airways. The main symptoms of COPD are cough with phlegm and shortness of breath.
- Heartburn or gastroesophageal reflux disease (GERD). The movement of the acidic contents of the stomach up the esophagus causes irritation of the mucous membrane of the throat and vocal cords, which contributes to coughing and itching.
- Nervous breakdown. In a stressful situation, especially in children, a nervous cough is possible as a variant of a nervous breakdown like a tic.
- Foreign body or tumor.
- Smoking.
- Tuberculosis.
Understanding the cause of a cough
To understand the cause of a cough, you need to answer a few questions:
- When does cough occur? At night in a dream, after physical exertion or after eating?
- Has there been contact with SARS patients in the last few days?
- Are there any gastrointestinal diseases or symptoms of stomach upset?
- Is there sputum, what does it look like?
- Did the cough occur during birch blossoms or after contact with other allergens?
- Is the cough accompanied by other symptoms? Is there a temperature, chills, weakness, is there weight loss?
- Has there been a lot of stress recently?
- Is the office or apartment well ventilated, is there a humidifier?
- How long does the cough last? Is it decreasing or increasing?
If you characterize a cough, it will be approximately clear where to look for the cause and how urgently you need to see a doctor. Any kind of cough that lasts more than a few days, interferes with sleep, is accompanied by a high fever, or produces a pronounced colored discharge is an occasion to see a doctor. You need to go to the appointment especially quickly if, due to coughing, it is difficult to inhale and exhale when there is not enough breathing.
Any kind of cough that lasts more than a few days, interferes with sleep, is accompanied by a high fever, or produces a pronounced colored discharge is an occasion to see a doctor. You need to go to the appointment especially quickly if, due to coughing, it is difficult to inhale and exhale when there is not enough breathing.
How to get rid of a cough
You need to go to the doctor and not self-medicate, but this is not always possible to do right away. If you can’t get an appointment right away, there are ways to alleviate the condition using proven methods.
Clean air
If you fantasize, the best option is to live on the shores of the warm Mediterranean Sea, not stress, eat well and tasty and not get sick. But this is not always possible, so you need to take care of respiratory hygiene. The first and most important thing is to moisturize the mucous membranes. We forget to humidify the air where we are constantly. Offices often have a central air filtration system that is not efficient enough. In this case, walks in the forest or square help.
In this case, walks in the forest or square help.
Dry dusty air irritates the mucous membranes and intensifies coughing. Therefore, you can put a humidifier at home or put a damp towel on the battery, in addition, you should do wet cleaning more often and do not forget to open windows for ventilation.
Natural remedies
Evidence-based medicine treats herbal infusions with caution. Herbs can cause allergies, and the concentration of the beneficial substance in them is unknown, it is difficult to measure it for normal dosing of the drug.
Lozenges
The easiest way to moisturize the mucous membranes is to use any lozenges for resorption. It is not necessary to buy medical ones from a pharmacy, you can take any delicious ones in the store. This stimulates saliva flow and slightly moistens the oropharynx.
Drink a lot
It moisturizes the mucous membranes and thins the sputum, and it becomes easier for the body to get rid of it. If there is not enough fluid in the body, then the sputum thickens, coughs up worse, can become a breeding ground for bacteria and cause complications.
If there is not enough fluid in the body, then the sputum thickens, coughs up worse, can become a breeding ground for bacteria and cause complications.
Salt solution
Salt solution should be instilled into the nose when coughing, which appeared due to irritation of the posterior pharyngeal wall with discharge from the nose. You can buy saline solution at a pharmacy or make it at home: dissolve a quarter teaspoon of soda and half a teaspoon of salt in a glass of water (250 ml).
Inhalation with saline
They moisturize the respiratory tract well and help to remove sputum, but in recent decades, world medicine has increasingly warned against inhalation without a preliminary examination by a doctor.
Medicines
For the treatment of coughs, there are many drugs that are freely sold in pharmacies. But you can take them only after consulting a doctor. With ordinary SARS, moisturizing the mucous membranes and drinking plenty of water work no worse than drugs, and buying inappropriate drugs can worsen the condition.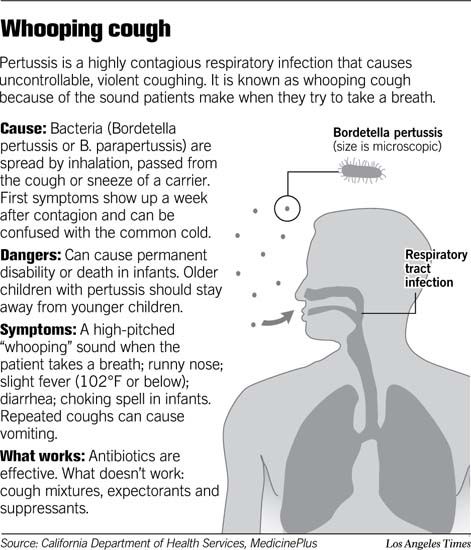
For example, if you take antitussives to get rid of a boring cough, then sputum can accumulate in the bronchi and cause bacterial complications.
The doctor may prescribe medication if he sees the need. Most often it is:
- Antitussives. They are prescribed for a dry, debilitating cough, when the cough interferes with sleep, such as whooping cough.
- Expectorants. They are prescribed for sputum that does not cough up on its own. Children under the age of four should not take these medicines without a doctor's permission.
- Nasal drops. If the cause of the cough is a runny nose and mucus flowing into the oropharynx, then they can help. But drops from the common cold should not be used for more than 3-5 days due to the danger of addiction.
- Medicinal inhalations. In this case, bronchodilators or hormonal drugs are added to saline to reduce inflammation and relieve spasm.
- Attacks of respiratory failure (bronchial obstruction) in children are relieved by inhalation drugs, but this is discussed at a face-to-face appointment with parents.
 There is no need to create a home first aid kit based on articles from the Internet. After all, there is no identical course of even a common cold, and understanding how to reduce bronchial obstruction in a particular patient is not always possible right away, even at the reception.
There is no need to create a home first aid kit based on articles from the Internet. After all, there is no identical course of even a common cold, and understanding how to reduce bronchial obstruction in a particular patient is not always possible right away, even at the reception.
How to recognize a chronic cough
If the cough lasts more than three weeks, you need to beware. Only a doctor can help determine the cause of a cough, its type and choose the right treatment.
The diagnosis of "Chronic cough" is made based on the results of a discussion with a doctor; it is impossible to determine this on your own. Sometimes it happens that a person comes to an appointment and says that he has a chronic cough. It turns out that for the first three weeks he was recovering from an acute respiratory viral infection, then for two weeks there was an exacerbation of GERD (gastroesophageal reflux disease), which provoked a cough. And another whole month fell in the early spring and the spraying of some birch or alder. In this case, we are not talking about chronic cough. And it happens that a patient has chronic obstructive pulmonary disease, and he coughs precisely because of it.
In this case, we are not talking about chronic cough. And it happens that a patient has chronic obstructive pulmonary disease, and he coughs precisely because of it.
What to do if the cough interferes
First of all, you need to sit or stand up and try to inhale through your nose. If the inhalation and exhalation with the help of the nose is successful, then everything is fine for now. If you can’t take a breath, then you need to wake up someone close, try to scream or say something. If it works out, then breathing is preserved - already not bad. If you can’t scream and breathe, then you need to urgently call an ambulance.
If at night the cough interferes so that it is impossible to sleep, you need to find out if an ambulance and hospitalization are required.
While the ambulance is on its way, you need to:
- open window for fresh cool air;
- turn on hot water in the bathroom and breathe over the steam;
- calm down.
How heart disease and cough are related
If the heart ceases to cope with its work and slowly pumps out blood, then pressure rises in the lungs, fluid accumulates, and this causes a reflex cough. This condition is characterized by bouts of dry cough. In severe cases, blood-streaked sputum may appear. That is, coughing is associated with the formation of heart failure, there is excess pressure in the pulmonary circulation. Fortunately, this doesn't happen often.
How to treat cough during pregnancy
In pregnant women, coughing may be associated with increased pressure on the lungs or heartburn in the later period, but there may be more serious reasons.
Any cough in pregnant women, even a slight one, is a reason to visit a doctor. There can be many reasons for coughing, and pregnancy is a period of increased attention to health.
Peculiarities of cough in children
You should not buy expectorant and expectorant drugs for children on your own, they can worsen the condition and cause complications.