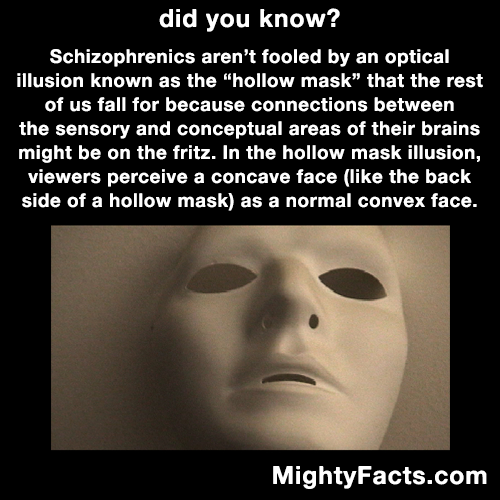
Can you make yourself schizophrenic
Causes - Schizophrenia - NHS
The exact causes of schizophrenia are unknown. Research suggests a combination of physical, genetic, psychological and environmental factors can make a person more likely to develop the condition.
Some people may be prone to schizophrenia, and a stressful or emotional life event might trigger a psychotic episode. However, it's not known why some people develop symptoms while others do not.
Increased risk
Genetics
Schizophrenia tends to run in families, but no single gene is thought to be responsible.
It's more likely that different combinations of genes make people more vulnerable to the condition. However, having these genes does not necessarily mean you'll develop schizophrenia.
Evidence that the disorder is partly inherited comes from studies of twins. Identical twins share the same genes.
In identical twins, if a twin develops schizophrenia, the other twin has a 1 in 2 chance of developing it, too. This is true even if they're raised separately.
In non-identical twins, who have different genetic make-ups, when a twin develops schizophrenia, the other only has a 1 in 8 chance of developing the condition.
While this is higher than in the general population, where the chance is about 1 in 100, it suggests genes are not the only factor influencing the development of schizophrenia.
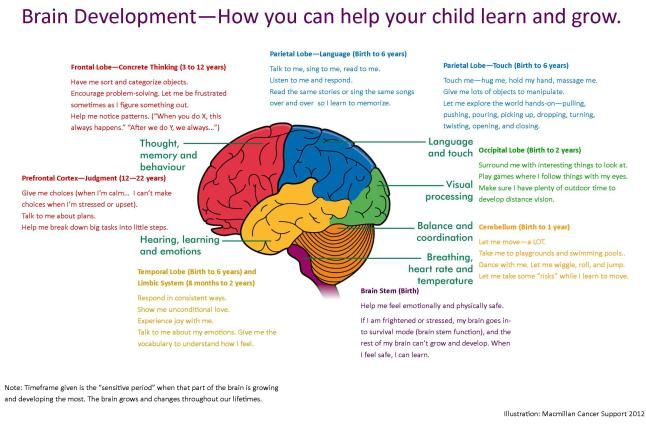
Brain development
Studies of people with schizophrenia have shown there are subtle differences in the structure of their brains.
These changes are not seen in everyone with schizophrenia and can occur in people who do not have a mental illness. But they suggest schizophrenia may partly be a disorder of the brain.
Neurotransmitters
Neurotransmitters are chemicals that carry messages between brain cells.
There's a connection between neurotransmitters and schizophrenia because drugs that alter the levels of neurotransmitters in the brain are known to relieve some of the symptoms of schizophrenia.
Research suggests schizophrenia may be caused by a change in the level of 2 neurotransmitters: dopamine and serotonin.
Some studies indicate an imbalance between the 2 may be the basis of the problem. Others have found a change in the body's sensitivity to the neurotransmitters is part of the cause of schizophrenia.
Pregnancy and birth complications
Research has shown people who develop schizophrenia are more likely to have experienced complications before and during their birth, such as:
- a low birthweight
- premature labour
- a lack of oxygen (asphyxia) during birth
It may be that these things have a subtle effect on brain development.
Triggers
Triggers are things that can cause schizophrenia to develop in people who are at risk.
These include:
Stress
The main psychological triggers of schizophrenia are stressful life events, such as:
- bereavement
- losing your job or home
- divorce
- the end of a relationship
- physical, sexual or emotional abuse
These kinds of experiences, although stressful, do not cause schizophrenia. However, they can trigger its development in someone already vulnerable to it.
Drug abuse
Drugs do not directly cause schizophrenia, but studies have shown drug misuse increases the risk of developing schizophrenia or a similar illness.
Certain drugs, particularly cannabis, cocaine, LSD or amphetamines, may trigger symptoms of schizophrenia in people who are susceptible.
Using amphetamines or cocaine can lead to psychosis, and can cause a relapse in people recovering from an earlier episode.
Research has shown that teenagers and young adults who use cannabis regularly are more likely to develop schizophrenia in later adulthood.
Want to know more?
- Mind: How can recreational drugs affect mental health?
- Mind: What causes schizophrenia?
Page last reviewed: 11 November 2019
Next review due: 11 November 2022
What Causes Schizophrenia? Plus, How to Treat and Seek Help
Schizophrenia is a chronic, psychiatric disorder that affects a person’s:
- behaviors
- thoughts
- feelings
A person living with this disorder may experience periods in which they seem to have lost touch with reality. They may experience the world differently than the people around them.
They may experience the world differently than the people around them.
Researchers don’t know what exactly causes schizophrenia. A combination of factors are thought to play a role.
Understanding the possible causes and risk factors for schizophrenia can help clarify who might be at risk.
Genetics
One of the most significant risk factors for schizophrenia may be genes. This disorder tends to run in families. If you have a parent, sibling, or another close relative with the condition, you may have a higher likelihood of developing it, too.
However, researchers don’t believe a single gene is responsible for this disorder. Instead, they suspect a combination of genes can make someone more susceptible.
Studies on twins have shown that genes play an integral role, but they aren’t the only determining cause.
Researchers found that if one identical twin sibling has schizophrenia, the other has a 1 in 2 chance of developing it. This remains true even if the twins are raised separately.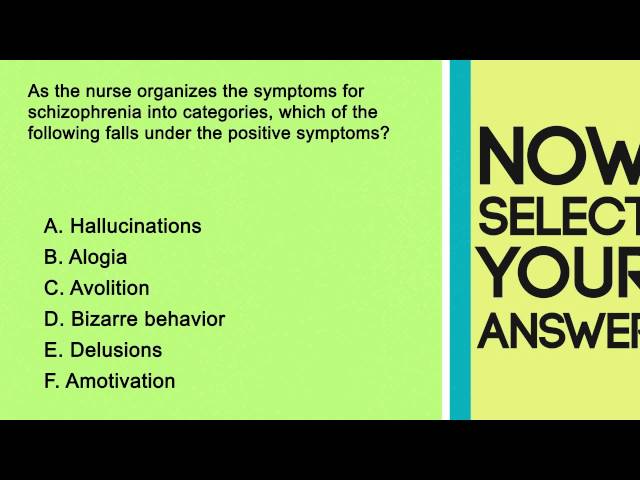
If a twin is nonidentical (fraternal) and has been diagnosed with schizophrenia, the other twin has a 1 in 8 chance of developing it. In contrast, the risk for disease in the general population is 1 in 100.
Structural changes in the brain
If you’ve been diagnosed with schizophrenia, you may have subtle physical differences in your brain. But these changes aren’t seen in everyone with this disorder.
They may also occur in people who don’t have a diagnosed mental health disorder.
Still, the findings suggest that even minor differences in brain structure may play a role in this psychiatric disorder
Chemical changes in the brain
A series of complex interrelated chemicals in the brain, called neurotransmitters, are responsible for sending signals between brain cells.
Imbalances of these chemicals are believed to play a role in the development of schizophrenia and other mental health conditions.
Dopamine, in particular, seems to play a role in the development of schizophrenia. Researchers have found evidence that dopamine causes an overstimulation of the brain in people with schizophrenia. It may account for some of the symptoms of the condition.
Researchers have found evidence that dopamine causes an overstimulation of the brain in people with schizophrenia. It may account for some of the symptoms of the condition.
Glutamate is another chemical that’s been linked to schizophrenia. Evidence has pointed toward its involvement. However, there are several limitations to this research.
Pregnancy or birth-related factors
Complications before and during birth may increase the likelihood that a person will develop mental health disorders, including schizophrenia.
These complications include:
- infection during pregnancy
- preterm labor
- delivery complications, including lack of oxygen during delivery (asphyxia)
- low birth weight
- maternal obesity in pregnancy
- certain maternal health conditions, like diabetes
- certain pregnancy-related health issues, like preeclampsia
- season of birth
Because of the ethics involved in studying pregnant people, many of the studies that have looked at the connection between prenatal complications and schizophrenia have been on animals.
People living with schizophrenia are also at an increased risk for complications during pregnancy.
It’s unclear if their children are at an increased likelihood of developing the condition because of genetics, pregnancy complications, or a combination of the two.
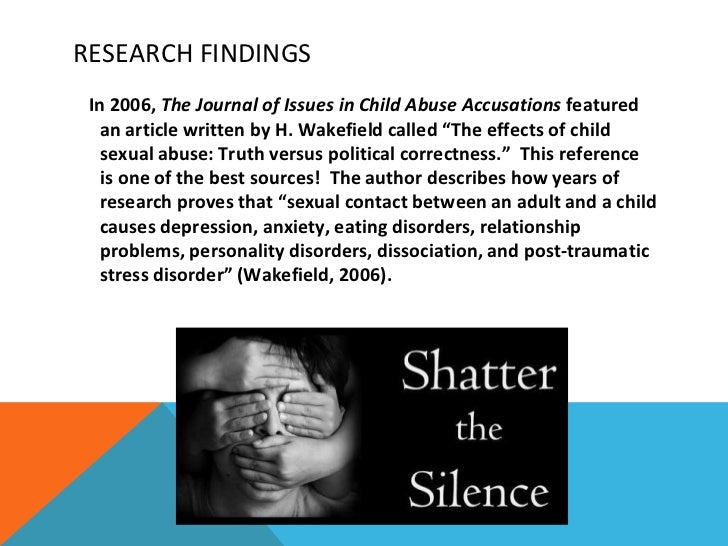
Childhood trauma
Childhood trauma is also thought to be a contributing factor in developing schizophrenia. Some people with schizophrenia experience hallucinations related to abuse or neglect they experienced as children.
People are also more likely to develop schizophrenia if as children they experienced the death or permanent separation of one or both parents.
This kind of trauma is tied to a variety of other adverse early experiences, so it’s still unclear if this trauma is a cause of schizophrenia or just associated with the condition.
Triggers are other factors that may also play a role in the development of schizophrenia in those who are at risk. A couple of triggers are thought to play a role.
Stress
While stress doesn’t cause schizophrenia, it can trigger an episode of psychosis.
In particular, stressful life events may bring on an episode, such as:
- abuse (emotional, physical, or sexual)
- a breakup or divorce
- death of a loved one
- job loss
While stress doesn’t directly cause schizophrenia, research shows that it may play a role in the development of schizophrenia in those who are already at risk.
Previous drug use
Using cannabis, cocaine, LSD, amphetamines, or similar drugs doesn’t cause schizophrenia. However, research shows that the use of these drugs may trigger symptoms of schizophrenia in people who are more at risk.
Because researchers don’t completely understand what causes schizophrenia, there’s no sure way to prevent it.
However, if you’ve been diagnosed with this disorder, following your treatment plan can reduce the likelihood of relapse or worsening symptoms.
Likewise, if you know that you’re at an increased risk for the disorder — such as by a genetic link — you can take steps to avoid known triggers like stress and drug use.
Symptoms of schizophrenia usually first appear between the ages of 16 and 30. Rarely, children can also show symptoms of the disorder.
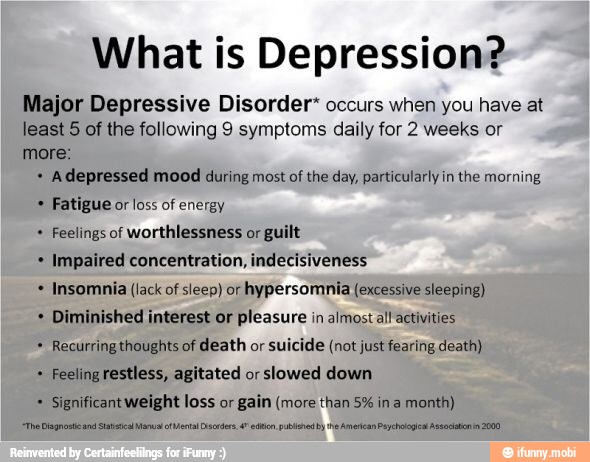
Symptoms fall into four categories:
- positive
- negative
- cognitive
- disorganization, or catatonic behaviors
Some of these symptoms are always present and occur even during periods of low disorder activity. Other symptoms only show up when there’s a relapse or increased activity.
Positive
Positive symptoms may be a sign that you’re losing touch with reality:
- hallucinations or hearing voices
- delusions
- thought disorders or dysfunctional ways of thinking
Negative
These negative symptoms interrupt normal behaviors. Examples include:
- lack of motivation
- reduced expressions of emotions (“flat affect”)
- loss of pleasure in everyday activities
- difficulty concentrating
Cognitive
Cognitive symptoms affect memory, decision-making, and critical-thinking skills. They include:
They include:
- trouble focusing
- poor “executive” decision-making
- problems with using or recalling information immediately after learning it
Disorganization
Disorganization symptoms are both mental and physical. They show a lack of coordination.
Examples include:
- motor behaviors, such as uncontrolled body movements
- speech difficulties
- memory recollection problems
- loss of muscle coordination, or being clumsy and uncoordinated
If you believe you or a loved one is showing signs of schizophrenia, it’s important to seek immediate treatment.
Keep these steps in mind as you seek help or encourage someone else to find help.
- Remember that schizophrenia is a biological illness: Treating it is as important as treating any other illness.
- Find a support system: Find a network you can rely on or help your loved one find one they can tap into for guidance.
 This includes friends, family, colleagues, and healthcare providers.
This includes friends, family, colleagues, and healthcare providers. - Check for support groups in your community: Your local hospital may host one, or they can help connect you to one.
- Encourage continuing treatment: Therapy and medications help people lead productive and rewarding lives. You should encourage a loved one to continue treatment plans.
There’s no cure for schizophrenia. It requires lifelong treatment. However, treatments focus on easing and eliminating symptoms, which can help you manage the condition.
Management decreases the probability of relapse or hospitalization. It can also make symptoms easier to handle and improve daily life.
Typical treatments for schizophrenia include:
- Antipsychotic medications: These medications affect brain chemistry. They help decrease symptoms by affecting the level of chemicals believed to be involved with the disorder.
- Psychosocial therapy: You can learn coping skills to help you manage some of the challenges this disorder causes.
 These skills can help to complete school, hold a job, and maintain quality of life.
These skills can help to complete school, hold a job, and maintain quality of life. - Coordinated specialty care: This approach to treatment combines medication and psychosocial therapy. It also adds family integration, education, and employment counseling. This type of care aims to reduce symptoms, manage periods of high activity, and improve quality of life.
Finding a healthcare professional you trust is an important first step toward managing this condition. You’ll likely need a combination of treatments to manage this complex condition.
Your healthcare professional may also need to alter your treatment plan during different times in your life.
Schizophrenia is a lifelong psychiatric condition. Researchers don’t know exactly what causes it. A combination of factors likely play a role.
Understanding the possible causes and risk factors for schizophrenia can help clarify who might be at risk and how to help them.
Schizophrenia
Schizophrenia- Healthcare issues »
- A
- B
- B
- G
- D
- E
- and
- 9000 About
- P
- P
- With
- T
- in
- F
- x
- 9 h
- K.

- S
- B
- E
- S
- I
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- Newsletter
- The facts are clear
- Publications
- Find country »
- A
- B
- C
- g
- D
- E
- and
- th
- K
- L
- 9000 N
- 9000
- in
- Ф
- x
- C hours
- Sh
- Sh.
- K
- E 9000 WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A nine0005
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Highlights " nine0005
- About WHO »
- General director
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/ nine0004 Schizophrenia
Key Facts
- Schizophrenia is a severe mental disorder that affects approximately 24 million people, or 1 in 300 people worldwide.
- Schizophrenia causes psychosis, is associated with severe disability, and can negatively affect all areas of life, including personal, family, social, academic and work life.
- People with schizophrenia are often subject to stigma, discrimination and human rights violations. nine0286
- Worldwide, more than two thirds of people with psychosis do not receive specialized mental health care.
- There are a number of effective care options for patients with schizophrenia that can lead to a complete recovery of at least one in three patients.
Symptoms
Schizophrenia is characterized by significant disturbances in perception of reality and behavioral changes such as:
- persistent delusions: the patient has a persistent belief in the truth of certain things, despite evidence to the contrary;
- persistent hallucinations: the patient hears, sees, touches non-existent things and smells non-existent smells;
- feeling of external influence, control or passivity: the presence in the patient of the feeling that his feelings, impulses, actions or thoughts are dictated from outside, put in or disappear from consciousness at the will of others, or that his thoughts are broadcast to others; nine0005
- disorganized thinking, often expressed in incoherent or pointless speech;
- Significant disorganization of behavior, which is manifested, for example, by the patient performing actions that may seem strange or meaningless, or in an unpredictable or inappropriate emotional reaction that does not give the patient the opportunity to organization of their behavior;
- "negative symptoms" such as extreme poverty of speech, smoothness of emotional reactions, inability to feel interest or pleasure, social autism; and/or
- Extreme agitation or, on the contrary, slowness of movements, freezing in unusual postures.
People with schizophrenia often also experience persistent cognitive or thinking problems that affect memory, attention, or problem-solving skills.
At least one third of patients with schizophrenia experience complete remission of symptoms (1). In some, periods of remission and exacerbation of symptoms follow each other throughout life, in others there is a gradual increase in symptoms. nine0322
Scope and impact
Schizophrenia affects approximately 24 million people, or 1 in 300 people (0.32%) worldwide. Among adults, the rate is 1 in 222 (0.45%) (2). Schizophrenia is less common than many other mental disorders. Onset is most common in late adolescence and between the ages of 20 and 30; while women tend to have a later onset of the disease. nine0322
Schizophrenia is often accompanied by significant stress and difficulties in personal relationships, family life, social contacts, studies, work or other important areas of life.
Individuals with schizophrenia are 2-3 times more likely to die early than the population average (2).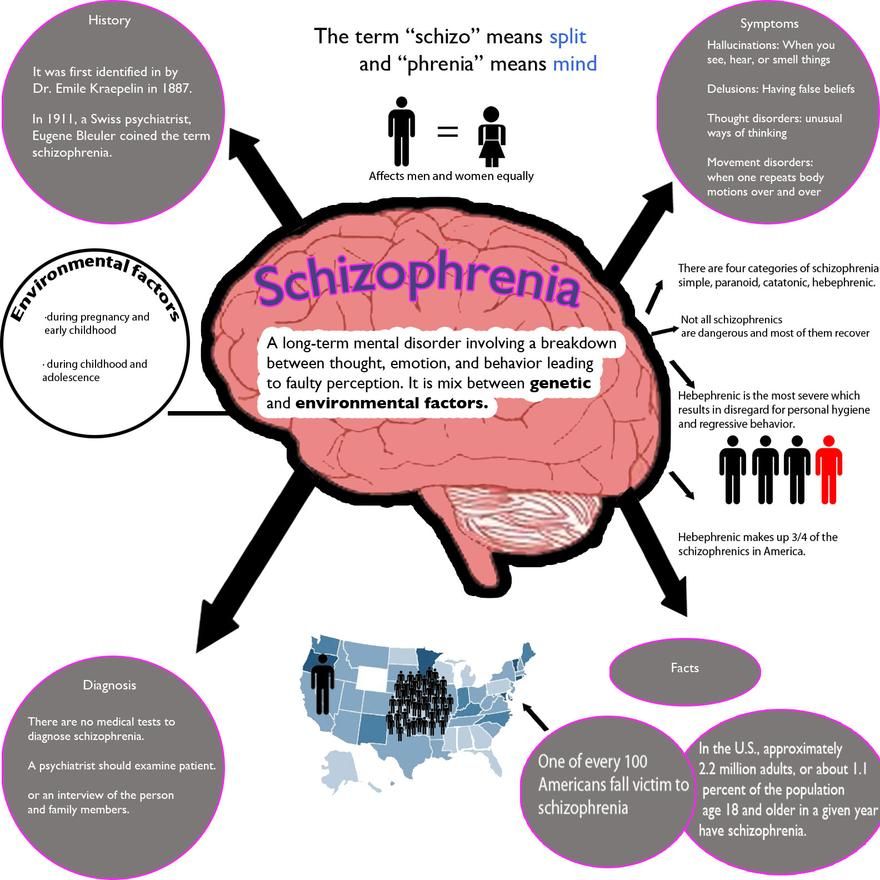 It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
Patients with schizophrenia often become the object of human rights violations both within the walls of psychiatric institutions and in everyday life. Significant stigmatization of people with this disease is a widespread phenomenon that leads to their social isolation and has a negative impact on their relationships with others, including family and friends. This creates grounds for discrimination, which in turn limits access to health services in general, education, housing and employment. nine0322
Humanitarian emergencies and health crises can cause intense stress and fear, disrupt social support mechanisms, lead to isolation and disruption of health services and supply of medicines. All these shocks can have a negative impact on the lives of people with schizophrenia, in particular by exacerbating existing symptoms of the disease. People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion. nine0322
nine0322
Causes of schizophrenia
Science has not established any one cause of the disease. It is believed that schizophrenia may be the result of the interaction of a number of genetic and environmental factors. Psychosocial factors may also influence the onset and course of schizophrenia. In particular, heavy marijuana abuse is associated with an increased risk of this mental disorder.
Assistance services
At present, the vast majority of people with schizophrenia do not receive mental health care worldwide. Approximately 50% of patients in psychiatric hospitals are diagnosed with schizophrenia (4). Only 31.3% of people with psychosis get specialized mental health care (5). Much of the resources allocated to mental health services are inefficiently spent on the care of patients admitted to psychiatric hospitals.
Available scientific evidence clearly indicates that hospitalization in psychiatric hospitals is not an effective treatment for mental disorders and is regularly associated with the violation of the basic rights of patients with schizophrenia. Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is essential the patient with schizophrenia, his family members and members of local communities. nine0322
Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is essential the patient with schizophrenia, his family members and members of local communities. nine0322
Schizophrenia management and care
There are a number of effective approaches to treating people with schizophrenia, including medication, psychoeducation, family therapy, cognitive behavioral therapy, and psychosocial rehabilitation (eg, life skills education). The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care. nine0322
The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care. nine0322
WHO action
steps are in place to ensure that appropriate services are provided to people with mental disorders, including schizophrenia. One of the key recommendations The action plan is to transfer the function of providing assistance from institutions to local communities. WHO Special Mental Health Initiative aims to further progress towards the goals of the Comprehensive Plan mental health action 2013–2030 by ensuring that 100 million more people have access to quality and affordable mental health care. nine0322
The WHO Mental Health Gap Action Program (mhGAP) is working to develop evidence-based technical guidelines, tools and training packages to scale up services in countries, especially in low-resource settings. The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States. nine0322
The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States. nine0322
The WHO QualityRights project aims to improve the quality of care and better protect human rights in mental health and social care settings and to expand opportunities of various organizations and associations to defend the rights of persons with mental disorders and psychosocial disabilities.
The WHO guidelines on community mental health services and human rights-based approaches provide information for all stakeholders who intend to develop or transform mental health systems and services. health in accordance with international human rights standards, including the UN Convention on the Rights of Persons with Disabilities. nine0322
Bibliography
(1) Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J. Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
(2) Institute of Health Metrics and Evaluation (IHME). Global Health Data Exchange (GHDx). http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/27a7644e8ad28e739382d31e77589dd7 (accessed 25 September 2021)
(3) LaursenTM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annual Review of Clinical Psychology , 2014;10, 425-438.
(4) WHO. Mental health systems in selected low- and middle-income countries: a WHO-AIMS cross-national analysis. WHO: Geneva, 2009
(5) Jaeschke K et al. Global estimates of service coverage for severe mental disorders: findings from the WHO Mental Health Atlas 2017 Glob Ment Health 2021;8:e27.
"I saw creatures from a parallel reality" How people with schizophrenia live: Lenta.ru
Schizophrenia is a severe mental disorder that affects more than 20 million people worldwide. Often people with this disease hallucinate, hear voices, see things that are not really there, and are prone to delusional ideas. Lenta.ru, with the support of the pharmaceutical company Gedeon Richter, talked to people diagnosed with schizophrenia and learned how to identify a mental disorder and what to do about it. nine0322
Often people with this disease hallucinate, hear voices, see things that are not really there, and are prone to delusional ideas. Lenta.ru, with the support of the pharmaceutical company Gedeon Richter, talked to people diagnosed with schizophrenia and learned how to identify a mental disorder and what to do about it. nine0322
Sarah, 28: “It all started innocently: I felt like I could hear people's thoughts”
I was diagnosed with paranoid schizophrenia while in a psychiatric hospital. The diagnosis was made almost immediately, after the first consultation of specialists.
Each person who has encountered schizophrenia has a different course of the disease. Anything can serve as a trigger for its development - any severe stress, childbirth, death of a loved one or drug use.
The first symptoms of the disease appeared a year and a half ago, I was 27. Then I was a master's student, a trainee teacher in one of the leading universities in the country. It all started quite innocently: I seemed to hear people's thoughts. To some extent, it was interesting - it seemed to me that my superpowers had awakened. I could ride in a trolleybus and hear the buzz of other people's thoughts: “I need to pick up the child from the garden”, “I'm sad”, “I want to buy a TV”. And this at a time when I have no children, and I do not need a TV. Fortunately, this did not affect the quality of life and work, I could control it. nine0322
To some extent, it was interesting - it seemed to me that my superpowers had awakened. I could ride in a trolleybus and hear the buzz of other people's thoughts: “I need to pick up the child from the garden”, “I'm sad”, “I want to buy a TV”. And this at a time when I have no children, and I do not need a TV. Fortunately, this did not affect the quality of life and work, I could control it. nine0322
After some time, the colors began to thicken - this coincided with the increased level of responsibility at work and the approaching deadline for defending a master's thesis. I could no longer move away from other people's thoughts, they literally settled in my head, there was no more room left for me. When I was in any society, I heard non-verbal threats from others. I was scared to ride the subway because I was convinced that anyone could read my mind.
Image: Sveta Kobrakova
The exam in philosophy was the culmination. Then I was convinced that someone took the brain out of my head, so I don’t remember anything. It became clear to me that something was wrong with me.
It became clear to me that something was wrong with me.
The disease worsened my condition, it became more and more difficult to live in a world that seemed to take up arms against me. But in reality, my own brain turned against me, which seems even more terrifying.
I told my parents everything, they took me to my native provincial town and sent me to the center of border states. There I was prescribed antipsychotic drugs. nine0322
Surely everyone has heard the expression "suffering from schizophrenia" - and this perfectly describes the disease. The disease torments, exhausts, makes existence unbearable. The most terrible thing is, let's say, the seal of fate imposed by her. Chronic... incurable... progressive... All these words lie like tombstones on us, people with a diagnosis.
Isolation from the world, the impossibility of realization, disability, stigmatization - this is the round dance that we face. We will never be able to communicate with this world, to speak out into it. We will never be understood, because it cannot be explained in the way that love, earache or despair, which all people have experienced in one way or another, can be explained. nine0322
We will never be understood, because it cannot be explained in the way that love, earache or despair, which all people have experienced in one way or another, can be explained. nine0322
Image: Sveta Kobrakova
There are people with schizophrenia who, under the supervision of a specialist, after many years of trying different drugs, were able to find the optimal treatment regimen. A good example is Elin Sachs, an American professor, Ph.D. Her book "The center cannot hold" at some point lit up my life with hope and showed that it's too early to give up - everything can be changed. Yes, you have to constantly fight, become a real warrior, but it's worth it.
Schizophrenia is a reason for getting a disability, but not in all cases. Although I am registered with the PND, I managed to avoid disability. And yet, I have some limitations in life in general and in work in particular. I can't teach anymore, I can't drive. I think that the work does not shine for me in responsible leadership positions.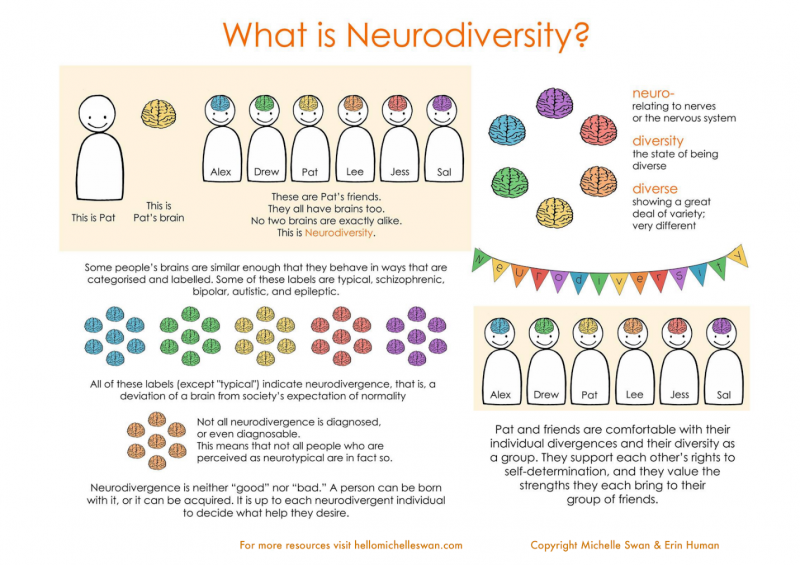 nine0322
nine0322
It is impossible to completely recover from schizophrenia, but it is possible to achieve stable remission and complete social and labor rehabilitation.
People with a disease need support, so the relatives of the “ill” person need to be ready to fight. The most qualified specialists are also needed. But in no case should you turn to psychics, shamans and magicians who exorcise demons. So you can lose very valuable time, money and also aggravate the disease.
Image: Sveta Kobrakova
If you notice that there is a big difference between reality and what is happening in your head, you should go to a specialist. You should always be very critical of yourself and include rational thinking. That is, for example, what is the probability that you are the earthly incarnation of some god?
I would like to appeal to everyone who has experienced schizophrenia: be strong, do not give up, do not spare money for specialists and drugs - all this will pay off with your condition. The path will be long and difficult, but worth it. Find those who understand you, do not stigmatize the disease, get treated - and you will achieve remission. Well, get as creative as possible. nine0322
The path will be long and difficult, but worth it. Find those who understand you, do not stigmatize the disease, get treated - and you will achieve remission. Well, get as creative as possible. nine0322
In 2019, Gedeon Richter launched a new drug on the Russian market that can alleviate the positive and negative symptoms of the disease. Immediately, pictures are drawn about the absence of a future, about life in a mental hospital. But today it is not so! Many people diagnosed with schizophrenia are quite successful, both professionally and personally. nine0322
Yes, the diagnosis is really difficult to accept. I sobbed when the specialist suggested that I had schizophrenia - it's like finding out that you are mortally ill, only not in body, but in soul and mind.
There is a problem that a person with such a diagnosis, without explaining anything, is prescribed a bunch of rather heavy drugs with a huge number of side effects. And people do not even understand why all this is necessary and whether it is necessary at all. People do not know that drugs can be changed, the dose adjusted. This often leads to an unauthorized refusal of drug treatment, which, with the right selection of drugs, makes it possible to be conscious. Some 50 years ago, patients did not have such an opportunity! nine0322
People do not know that drugs can be changed, the dose adjusted. This often leads to an unauthorized refusal of drug treatment, which, with the right selection of drugs, makes it possible to be conscious. Some 50 years ago, patients did not have such an opportunity! nine0322
When the first signs of the disease appeared, I didn't even understand that it was a disease - that's its cunning. At some point, I began to live in two realities, as it were. And every day these realities became more. It's like living in different dimensions, in which it is not space that differs, but your life, experience, destiny.
It is very difficult to describe... Imagine that there is you, and there is another you, only he is in another dimension. Perhaps in another time. There are many of you, and they are all connected. Their own future, the future of their loved ones and all the events around depend on the actions of each of these personalities. Then the ball grows to such a size that it is impossible to unravel it. And despair sets in. Like an abyss into which you are rapidly drawn in, from which you cannot get out. nine0322
And despair sets in. Like an abyss into which you are rapidly drawn in, from which you cannot get out. nine0322
At some point, I began to see different creatures, as if from a parallel reality. Some were aggressive and attacked me, others defended. But I understood that only I see it, and I did not tell anyone about it.
Image: Sveta Kobrakova
Well, then the moment came when some symptoms came to the surface. Relatives realized that it was bad, and called an ambulance. I was not dangerous either for myself or for others, so at first the doctors did not want to take me away - there was no reason for this. But then they saw my old, many years old, scars from self-harm, and it was these scars that became the reason for admission to the hospital. nine0322
I would not wish anyone, not a single person in the world, to get this disease. It is difficult to convey the full range of feelings that one has to experience in a state of psychosis (I have had three of these over the past year and a half). You find yourself in circumstances that you cannot influence in any way, and together with you, through your fault, people dear to you are here. What can a person experience who, for example, is sure that he is locked forever in his apartment with his children, and at that time a night has come that will never end? It is fear and utter despair. nine0322
You find yourself in circumstances that you cannot influence in any way, and together with you, through your fault, people dear to you are here. What can a person experience who, for example, is sure that he is locked forever in his apartment with his children, and at that time a night has come that will never end? It is fear and utter despair. nine0322
When you come out of psychosis, the recovery period begins. This is also very difficult. It can be very difficult to do at least something - even get out of bed. It happens that there is a complete emptiness inside, and you do not feel anything, nothing at all - neither joy, nor sadness, nor love, nor pain, or any other experiences. And here again there is a feeling of guilt, because you cannot even carry out everyday activities.
Once I almost went out the window of the sixth floor, and my children were nearby. It didn't happen because I wanted to take my own life. It was just that at that moment in my reality, I believed that my physical body was invulnerable.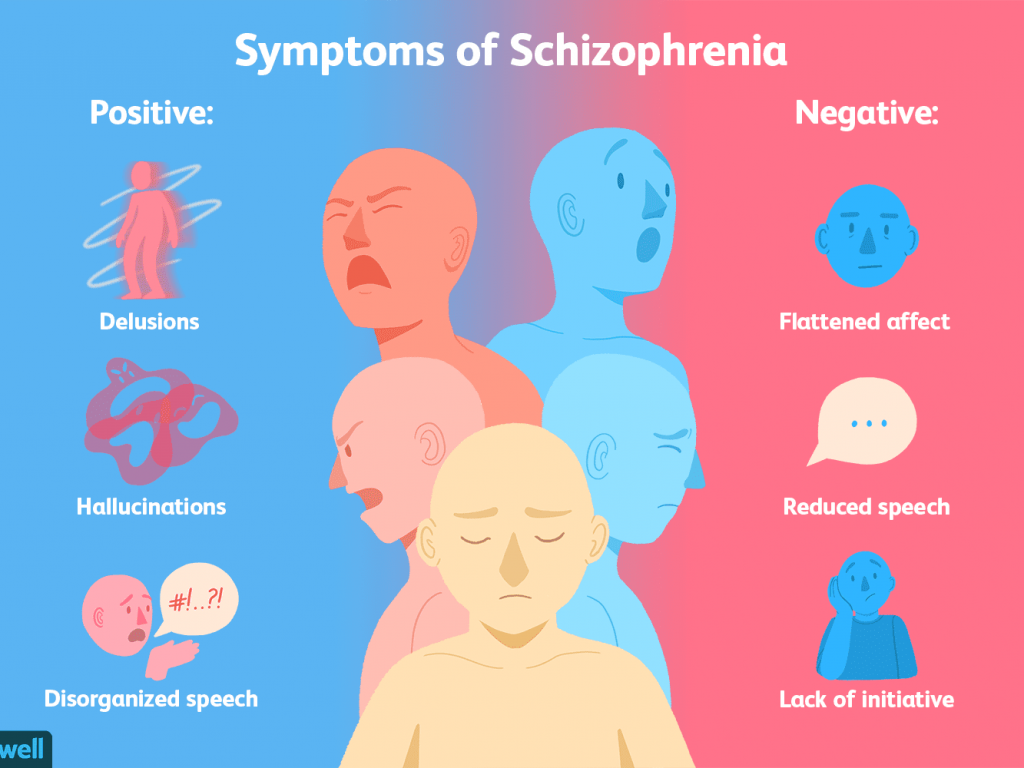 But I was lucky, I was stopped. The mother-in-law, seeing me standing at the window, said in a calm voice: “Close it, please.” And I closed. nine0322
But I was lucky, I was stopped. The mother-in-law, seeing me standing at the window, said in a calm voice: “Close it, please.” And I closed. nine0322
Image: Sveta Kobrakova
At one point, I realized that I need relatives, children, and this is more important for me than "superpowers". And I have to do everything to live in the real world. When I realized this, my healing became conscious. I began to cooperate more actively with specialists, listen to their recommendations, search for information, read literature related to psychiatry. It was a lot of work, but it was important for me to return - for the sake of those who need me. The key, in my opinion, is just this: find the strength in yourself to admit that you are sick and begin to be treated. nine0322
If you are a relative of a person who has experienced schizophrenia, you need to understand that schizophrenia is not a whim, not fooling around, not laziness, not mental retardation. This is a disease that needs to be treated, and the sooner you start, the better. It is desirable that the treatment consists not only in observation by a specialist, but also in work with a psychotherapist, a social worker, and participation in self-help groups.
It is desirable that the treatment consists not only in observation by a specialist, but also in work with a psychotherapist, a social worker, and participation in self-help groups.
If one person in the family is ill, then everyone needs support and help. The problem is not only with the patient. One way or another, this situation affects the whole family. For children, this is generally a serious trauma, so you can’t taboo this topic, somehow hush it up. Children of people with mental illness need support in this matter. nine0322
I want to draw attention to the word "support". Not guardianship. In no case should you do everything for the patient, it only hurts. And there is no need to load him with some kind of excessive activity, especially if this activity is not in the sphere of his interests. It is necessary to support and encourage him in all endeavors, talents, abilities. I know from experience that often the phrase “Cheer up, we will overcome this” is sometimes more important than long motivating conversations.
I have three children. The eldest was seven years old when I first went to the hospital. The fact that I was sick, we did not talk to him right away. The topic was almost taboo in our family, and even then I did not recognize the disease in myself. But it was clear that the older child was going through. Everything changed after the third episode - then we talked. I said that in all the variety of different diseases, there are also mental ones. My son has changed right before my eyes, now he asks various questions about the disease, goes to events with me and is quite well versed in the topic of mental health. Children are able to understand, you just need to call a spade a spade, although it is scary to admit a lot to yourself. nine0322
I took medication for about three years. Today I manage to do without them. I take them occasionally when I feel some of the familiar signals of an oncoming psychosis. But this happens extremely rarely - against the background, for example, of a strong stressful situation. Of course, I am satisfied that I live in our time, and I have a chance to help myself with medicines. They don’t torture me with a lobotomy, they don’t put a wet rag on me, they don’t hang me from the ceiling. Once upon a time, these methods were considered quite adequate, however, as we know now, all this did not work or only made things worse. nine0322
Of course, I am satisfied that I live in our time, and I have a chance to help myself with medicines. They don’t torture me with a lobotomy, they don’t put a wet rag on me, they don’t hang me from the ceiling. Once upon a time, these methods were considered quite adequate, however, as we know now, all this did not work or only made things worse. nine0322
Image: Sveta Kobrakova
I like the comparison of schizophrenia with influenza, although it is not correct enough. Is it possible to get rid of the flu forever? No. For some period of time you feel bad, you need to take antipyretic and drink a lot, observe bed rest. And then everything went away, and you don’t need to do anything special to feel good. But the symptoms can return, and you need to be prepared for this.
Treatment allows you to live a full life. But you need to understand that drugs alone are not enough. Medicines only provide an opportunity to return to reality in order to fully work on the deeper causes of the disease.