Can iuds cause mood swings
Do IUDs Cause Depression? Here's What You Should Know
An intrauterine device (IUD) is a small device that your doctor can put into your uterus to stop you from getting pregnant. It’s a long-acting and completely reversible form of birth control.
IUDs are very effective at preventing pregnancy. Like many types of birth control, they can also cause some side effects.
There are two main types of IUD: copper and hormonal. Some studies suggest that using a hormonal IUD might increase your risk of depression. However, research findings on this topic have been mixed. Most people who use a hormonal IUD don’t develop depression as a side effect.
Your doctor can help you understand the potential benefits and risks of using a hormonal or copper IUD, including any effects it might have on your mood.
A copper IUD (known by the brand name Paragard) is wrapped in copper, a metal that kills sperm. In most cases, a copper IUD can last up to 12 years before it needs to be removed and replaced.
Unlike hormonal IUDs, copper IUDs don’t contain any progestin or other hormones. They haven’t been linked to a higher risk of depression.
A hormonal IUD (known by the brand names Kyleena, Liletta, Mirena, and Skyla) releases small amounts of progestin, a synthetic form of the hormone progesterone. This causes the lining of your cervix to thicken, making it harder for sperm to enter your uterus.
This type of IUD can last around 3 to 7 years before needing to be replaced, depending on the brand.
IUDs are more than 99 percent effective at preventing pregnancy, according to Planned Parenthood. They’re one of the most effective methods of birth control.
They also require little upkeep. Once an IUD has been inserted, it provides 24-hour protection from pregnancy for multiple years.
For people who have heavy or painful periods, hormonal IUDs offer additional benefits. They can reduce period cramps and make your periods lighter.
If you decide you want to get pregnant, a healthcare professional can remove your IUD for you at any time. The birth control effects of copper IUDs are instantly reversible, and the effects of hormonal IUDs wear off in less than a month.
The birth control effects of copper IUDs are instantly reversible, and the effects of hormonal IUDs wear off in less than a month.
For people who want to avoid hormonal birth control, the copper IUD offers an effective option. However, the copper IUD tends to cause heavier periods.
IUDs don’t stop the spread of sexually transmitted infections (STIs). To protect yourself and your partner(s) from STIs, you can use a barrier method, like condoms, along with an IUD.
Some studies suggest hormonal IUDs and other hormonal methods of birth control — for example, birth control pills — may raise the risk of depression. Other studies have found no link at all.
One of the largest studies on birth control and depression was completed in Denmark in 2016. The researchers studied 14 years’ worth of data from more than 1 million women, aged 15 to 34 years old. They excluded women with a history of depression or antidepressant use.
From this data, the researchers estimated that 2. 2 percent of women who begin using hormonal birth control methods are prescribed antidepressants within a year, compared with 1.7 percent of women who don’t use hormonal birth control.
2 percent of women who begin using hormonal birth control methods are prescribed antidepressants within a year, compared with 1.7 percent of women who don’t use hormonal birth control.
Women who used a hormonal IUD are an estimated 1.4 times more likely to be prescribed antidepressants than women who don’t use any form of hormonal birth control. The risk was greater for younger women between the ages of 15 and 19 years old.
Other studies, however, have found no link between hormonal birth control and depression. In a review published in 2018, researchers looked at 26 studies evaluating progestin-only contraceptives, including five that looked at hormonal IUDs. Only one study linked hormonal IUDs to a higher risk of depression. The other four studies found no link between hormonal IUDs and depression.
The review authors also estimated that many of the reviewed studies had a high risk of bias or varied in quality, highlighting the lack of research on birth control and depression.
If you suspect your birth control is causing depression or other side effects, speak with your doctor. In some cases, they might encourage you to change your method of birth control.
They might also prescribe antidepressant medications, refer you to a mental health specialist for counseling, or recommend other treatments.
Potential signs and symptoms of depression include:
- frequent or lasting feelings of sadness, hopelessness, or emptiness
- frequent or lasting feelings of worry, anxiety, irritability, or frustration
- frequent or lasting feelings of guilt, worthlessness, or self-blame
- loss of interest in activities that used to intrigue or please you
- changes to your appetite or weight
- changes to your sleep habits
- lack of energy
- slowed movements, speech, or thought
- difficulty concentrating, making decisions, or remembering things
If you develop signs or symptoms of depression, let your doctor know.
If suicidal thoughts are surfacing
- Call a crisis hotline, such as the National Suicide Prevention Lifeline at 800-273-8255.
- Text HOME to the Crisis Textline at 741741.
- If you feel you’re at immediate risk, reach out to a trusted friend, family member, or healthcare professional. Consider calling 911 or your local emergency number if you can’t get in touch with them.
If you’re concerned about the potential risk of depression or other side effects from birth control, speak with your doctor.
They can help you understand the potential benefits and risks of using an IUD or other methods of birth control. Based on your medical history and lifestyle, they can help you choose a method that fits your needs.
Do IUDs Cause Depression? Here's What You Should Know
An intrauterine device (IUD) is a small device that your doctor can put into your uterus to stop you from getting pregnant. It’s a long-acting and completely reversible form of birth control.
IUDs are very effective at preventing pregnancy. Like many types of birth control, they can also cause some side effects.
There are two main types of IUD: copper and hormonal. Some studies suggest that using a hormonal IUD might increase your risk of depression. However, research findings on this topic have been mixed. Most people who use a hormonal IUD don’t develop depression as a side effect.
Your doctor can help you understand the potential benefits and risks of using a hormonal or copper IUD, including any effects it might have on your mood.
A copper IUD (known by the brand name Paragard) is wrapped in copper, a metal that kills sperm. In most cases, a copper IUD can last up to 12 years before it needs to be removed and replaced.
Unlike hormonal IUDs, copper IUDs don’t contain any progestin or other hormones. They haven’t been linked to a higher risk of depression.
A hormonal IUD (known by the brand names Kyleena, Liletta, Mirena, and Skyla) releases small amounts of progestin, a synthetic form of the hormone progesterone. This causes the lining of your cervix to thicken, making it harder for sperm to enter your uterus.
This causes the lining of your cervix to thicken, making it harder for sperm to enter your uterus.
This type of IUD can last around 3 to 7 years before needing to be replaced, depending on the brand.
IUDs are more than 99 percent effective at preventing pregnancy, according to Planned Parenthood. They’re one of the most effective methods of birth control.
They also require little upkeep. Once an IUD has been inserted, it provides 24-hour protection from pregnancy for multiple years.
For people who have heavy or painful periods, hormonal IUDs offer additional benefits. They can reduce period cramps and make your periods lighter.
If you decide you want to get pregnant, a healthcare professional can remove your IUD for you at any time. The birth control effects of copper IUDs are instantly reversible, and the effects of hormonal IUDs wear off in less than a month.
For people who want to avoid hormonal birth control, the copper IUD offers an effective option. However, the copper IUD tends to cause heavier periods.
However, the copper IUD tends to cause heavier periods.
IUDs don’t stop the spread of sexually transmitted infections (STIs). To protect yourself and your partner(s) from STIs, you can use a barrier method, like condoms, along with an IUD.
Some studies suggest hormonal IUDs and other hormonal methods of birth control — for example, birth control pills — may raise the risk of depression. Other studies have found no link at all.
One of the largest studies on birth control and depression was completed in Denmark in 2016. The researchers studied 14 years’ worth of data from more than 1 million women, aged 15 to 34 years old. They excluded women with a history of depression or antidepressant use.
From this data, the researchers estimated that 2.2 percent of women who begin using hormonal birth control methods are prescribed antidepressants within a year, compared with 1.7 percent of women who don’t use hormonal birth control.
Women who used a hormonal IUD are an estimated 1. 4 times more likely to be prescribed antidepressants than women who don’t use any form of hormonal birth control. The risk was greater for younger women between the ages of 15 and 19 years old.
4 times more likely to be prescribed antidepressants than women who don’t use any form of hormonal birth control. The risk was greater for younger women between the ages of 15 and 19 years old.
Other studies, however, have found no link between hormonal birth control and depression. In a review published in 2018, researchers looked at 26 studies evaluating progestin-only contraceptives, including five that looked at hormonal IUDs. Only one study linked hormonal IUDs to a higher risk of depression. The other four studies found no link between hormonal IUDs and depression.
The review authors also estimated that many of the reviewed studies had a high risk of bias or varied in quality, highlighting the lack of research on birth control and depression.
If you suspect your birth control is causing depression or other side effects, speak with your doctor. In some cases, they might encourage you to change your method of birth control.
They might also prescribe antidepressant medications, refer you to a mental health specialist for counseling, or recommend other treatments.
Potential signs and symptoms of depression include:
- frequent or lasting feelings of sadness, hopelessness, or emptiness
- frequent or lasting feelings of worry, anxiety, irritability, or frustration
- frequent or lasting feelings of guilt, worthlessness, or self-blame
- loss of interest in activities that used to intrigue or please you
- changes to your appetite or weight
- changes to your sleep habits
- lack of energy
- slowed movements, speech, or thought
- difficulty concentrating, making decisions, or remembering things
If you develop signs or symptoms of depression, let your doctor know.
If suicidal thoughts are surfacing
- Call a crisis hotline, such as the National Suicide Prevention Lifeline at 800-273-8255.
- Text HOME to the Crisis Textline at 741741.
- If you feel you’re at immediate risk, reach out to a trusted friend, family member, or healthcare professional. Consider calling 911 or your local emergency number if you can’t get in touch with them.

If you’re concerned about the potential risk of depression or other side effects from birth control, speak with your doctor.
They can help you understand the potential benefits and risks of using an IUD or other methods of birth control. Based on your medical history and lifestyle, they can help you choose a method that fits your needs.
Understanding the types of contraception, their pros and cons with an obstetrician gynecologist
Every woman is concerned about how to prevent unwanted pregnancy and protect herself from sexually transmitted infections.
The questions of how to prevent unwanted pregnancy and protect against sexually transmitted infections are of concern to every woman. Choosing reliable contraception is not an easy task, and this issue should be discussed with your doctor. Obstetrician-gynecologist of the clinic "Euromed" Marina Pavlovna GLUSHENKOVA talks about the existing methods of contraception, their pros and cons.
Contraception is barrier, hormonal and intrauterine. Methods such as coitus interruptus and calendar methods cannot be considered reliable and effective. Fortunately, in the XXI century there are many ways and means of protection from unwanted pregnancy and unpleasant diseases.
Methods such as coitus interruptus and calendar methods cannot be considered reliable and effective. Fortunately, in the XXI century there are many ways and means of protection from unwanted pregnancy and unpleasant diseases.
Barrier methods
Condoms
Pluses
-
reliable protection against sexually transmitted diseases (STDs) and unwanted pregnancies (when used correctly)
-
affordable price
-
no systemic effect on the body
-
ideal for those who have an irregular sex life
-
do not require preliminary examinations for selection
Cons
Spermicides
Spermicides are substances that immobilize spermatozoa, due to which they do not penetrate into the uterine cavity.
Pluses
-
partial protection against sexually transmitted infections (some viruses do not work)
-
suitable for those who cannot use hormonal and intrauterine contraception
Cons
-
low efficiency (60–70%), this method cannot be used as a standalone method
-
requires very strict enforcement of the rules of use
-
Possible irritation, allergic reactions of the skin of the genital organs
Intrauterine methods
Copper intrauterine system (coil)
The coil thickens cervical mucus and forms a barrier to spermatozoa. Copper acts toxically on spermatozoa, immobilizing them, and also suppresses ovulation.
Copper acts toxically on spermatozoa, immobilizing them, and also suppresses ovulation.
Pros
-
prolonged action, allowing you to forget about contraception for several years
-
no systemic effect on the body
-
can be used during lactation
Cons
-
it is impossible to put nulliparous, because against the background of the spiral there is a risk of the formation of intrauterine synechia, adhesions, which can lead to infertility; Also, nulliparous due to anatomical features have a narrower cervical canal, which makes it difficult to install the spiral.
-
the spiral does not protect against STDs, respectively, it is only suitable for women who have one permanent healthy sexual partner;
-
against the background of the use of a copper-containing spiral, the risk of inflammatory diseases of the uterus and appendages increases by 5-6 times compared with women who do not have spirals;
-
the spiral can provoke longer and more painful periods;
-
if a woman has a history of multiple abortions, invasive interventions, curettage, there is a risk of developing cervical insufficiency, i.
 e. failure of the cervix, which can lead to expulsion (falling out) of the spiral.
e. failure of the cervix, which can lead to expulsion (falling out) of the spiral.
Protected hormonal coils
The hormones contained in the system act in the uterine cavity, make the mucous membrane thinner, and immobilize spermatozoa. All this makes fertilization and implantation of the fetal egg impossible.
Pluses
-
Reliable contraceptive action for five years
-
No systemic action
-
has a therapeutic effect: it is indicated for patients with a history of endometrial hyperplastic processes, uterine myoma
-
can be used during lactation
Cons
Hormonal contraception
This is perhaps the most effective method of all existing today.
Hormonal preparations differ in dosage (mini-dose - estrogen content no more than 30 mcg, micro-dose - no more than 20 mcg, large doses are not currently used), components, and the method of entry into the body.
There are two types of drugs: combined and the “mini-drank” group. Combined contraceptives contain estrogens (ethinyl estradiol) and gestagens, "mini-drank" - only gestagens.
Preparations from the "mini-drank" group are indicated for lactating women who should not take estrogens, but only gestagens. Also, "mini-pills" can be taken by women who do not tolerate the estrogen component.
Types of drugs: tablets (taken orally), vaginal ring (hormones penetrate the vaginal mucosa) and patch (transdermal route - hormones enter through the skin).
Reception methods. Tablets should be taken daily, at the same time. It is especially important to take at the same time for drugs from the "mini-drank" group. Tablets are generally taken for 21 days, after which they take a break for 7 days.
The vaginal ring is inserted into the vagina for 21 days, after which there is a break for a week.
The patch is changed every 7 days.
The advantage of alternative routes of administration (ring, patch) is that you do not need to remember to take the pill every day and there is no primary passage through the liver and gastrointestinal tract, which reduces the load on them. This is especially important if a woman has problems with the gastrointestinal tract or chronic cholecystitis.
This is especially important if a woman has problems with the gastrointestinal tract or chronic cholecystitis.
Pluses
-
reliable contraceptive effect (if a woman does not miss taking pills, the guarantee is almost 100%)
-
active protection of the ovaries and endometrium (mucosa) of the uterus from cancer
-
regulation of the menstrual cycle
-
reduction of pain during menstruation
-
cosmetic effect (some OK help to cope with acne, normalize skin condition)
-
therapeutic effect (the doctor will help you choose hormonal contraceptives, which are indicated for patients with uterine fibroids, with endometriosis).
Cons
-
the need for strict discipline, control of taking drugs at the same time (especially important for "mini-pill")
-
do not protect against STDs
-
any hormonal drugs affect metabolism (metabolism), which can lead to fluctuations in body weight, although in modern drugs this effect is minimal;
-
there is an effect on the vascular link, on the blood coagulation system, therefore, when taking contraceptives, constant monitoring of hemostasis is necessary.
 If a woman has a predisposition to varicose veins, to hypertension, or in the family there were cases of diseases of the cardiovascular system, accompanied by thrombosis, heart attacks, strokes, then the patient needs a comprehensive examination of the hemostasis system before taking hormonal contraceptives;
If a woman has a predisposition to varicose veins, to hypertension, or in the family there were cases of diseases of the cardiovascular system, accompanied by thrombosis, heart attacks, strokes, then the patient needs a comprehensive examination of the hemostasis system before taking hormonal contraceptives; -
there is a period of adaptation to hormones. Within 2-3 months, nausea, headaches and pains in the mammary glands can sometimes be observed, there may be slight spotting in the middle of the cycle, changes in libido, mood swings. Therefore, mandatory medical supervision of the use of drugs during the first months of admission.
-
hormonal contraceptives have a number of contraindications: active smoking (more than 5 cigarettes per day), severe somatic diseases, severe decompensated diabetes mellitus, thrombosis, varicose veins, heart attacks, strokes, arterial hypertension, frequent migraines, etc.
Sterilization
Medical sterilization is a surgical technique that can be used by both men and women.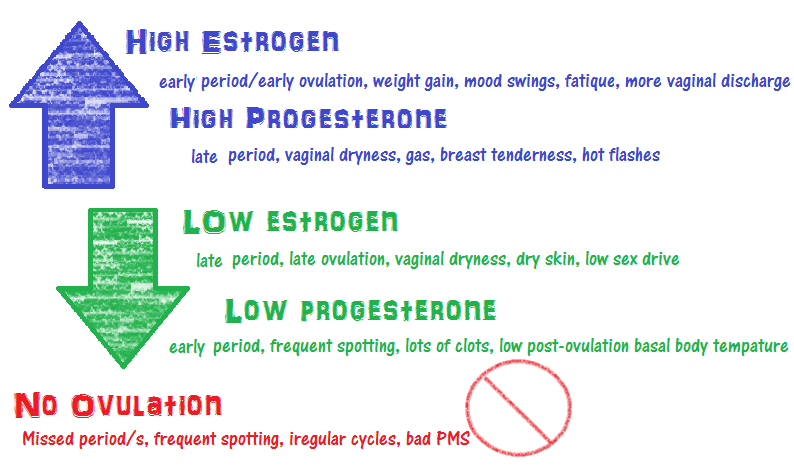 This is a reliable method of 100% protection against pregnancy, a good choice for people who are definitely not planning more children.
This is a reliable method of 100% protection against pregnancy, a good choice for people who are definitely not planning more children.
After the operation, the ability to conceive can no longer be restored for women, in men there is a small (less than 30%) chance of restoring reproductive function by re-operation within five years after the intervention.
Female sterilization is a laparoscopic operation during which the fallopian tubes are cut, which reliably prevents the possibility of pregnancy.
Male sterilization (vasectomy) is a simple operation that takes about 20 minutes. During surgery, the vas deferens are tied up and crossed. Sterilization does not affect the erection, the amount of seminal fluid and the ability to experience an orgasm.
Pluses
Cons
-
irreversibility of the operation
-
the need for surgery
-
there are legal restrictions on this operation
Medical sterilization as a special medical intervention in order to deprive a person of the ability to reproduce offspring or as a method of contraception can only be carried out upon a written application of a citizen over the age of thirty-five or a citizen with at least two children, and if there are medical indications and informed voluntary consent citizen - regardless of age and the presence of children.
Article 57
emergency contraception
In the case of unprotected intercourse, you can use the so-called emergency contraception. These drugs are aimed at protection, this is not an abortion. The tablet contains a large dose of progestin preparations that cause rejection of the endometrial mucosa.
Pluses
Cons
When choosing contraception, be sure to contact a gynecologist. Before prescribing this or that drug, the doctor will conduct an examination, which includes an examination on a chair, taking a smear for oncocytology. Also, if there are signs of endocrinopathy (increased hair growth, acne), it is necessary to investigate the hormonal background. Since hormones thicken the blood, affect hemostasis (blood coagulation system), it makes sense to conduct a comprehensive examination of the state of the hemostasis system. In addition, it is recommended to do an ultrasound examination of the pelvic organs (uterus and appendages) and mammary glands. All these procedures are minimally invasive, painless, they are not difficult to pass, and they will help to avoid possible complications against the background of long-term use of contraceptives.
All these procedures are minimally invasive, painless, they are not difficult to pass, and they will help to avoid possible complications against the background of long-term use of contraceptives.
Hormonal contraceptives: everything you need to know
Despite the fact that only the lazy does not talk about hormonal contraception, there are fewer reliable facts about it than myths. It should be noted that in our country, women of reproductive age use it by only 9%, while in the USA, for example, by 45%. How to choose and whether to use such contraceptives at all, what to look for and how to take in order to eliminate side effects and get health benefits.
Nowhere in the literature, on the Internet or in a doctor's office, will you find comprehensive information about why you should start taking hormonal contraceptives or why not. The opinions of some experts argue that they should be taken for life from an early age, while others are inclined to believe that it is acceptable to use them in short courses for treatment purposes. But in fact, the truth is on both sides of the scale.
But in fact, the truth is on both sides of the scale.
Hormones play an important role in the human body, controlling all vital processes, including reproductive ones. When the hormonal background is in balance, a person’s life is in a state of “zen”. But the hormonal system, like any other in our body, can fail. In this case, synthetic derivatives come to the rescue.
In women, in general, hormonal fluctuations lead to a number of “uncomfortable” consequences:
- Menstrual disorders
- Mood swings and psycho-emotional disorders
- Weight jumps
- Diseases of the genital area
- Inability to conceive or bear a child
- Cosmetic defects, blackheads and pimples, rashes on the face and body, hair loss
And many other troubles when hormonal correction is required. In addition to treating the female reproductive system, drugs are also used as a targeted method of contraception. But correct in this case, it will be mandatory to undergo at least a minimal examination, because this is a serious drug, not vitamins.
But correct in this case, it will be mandatory to undergo at least a minimal examination, because this is a serious drug, not vitamins.
How do hormonal contraceptives work?
The mission of such contraceptives is to prevent pregnancy. And this happens under the influence of synthetic hormones or combined oral contraceptives (COCs), which in microdoses either “lull” eggs or increase the viscosity of mucus in the vagina and suppress the function of ovulation, which is controlled by the pituitary gland. It also maintains a normal level of progesterone, necessary for bearing a baby. That is, the pituitary gland has paused the reproduction of offspring, the eggs are not ejected from the ovary unnecessarily, so fertilization becomes impossible.
Before the doctor understands the full picture of your health based on tests, be sure to share as much information as possible about your lifestyle, hereditary and chronic diseases, if any.
For example, for girls who smoke, oral contraception is banned, because taking these drugs can affect the blood circulation process, thicken the blood, which, in combination with nicotine, can significantly increase the risk of cardiovascular diseases and vein pathologies.
A biochemical blood test is considered desirable (COCs are contraindicated in diabetes mellitus, liver and kidney diseases), urinalysis, ultrasound of the internal organs and pelvic organs, and a mandatory examination by a doctor.
It would be ideal if you take a blood test to check the level of progesterone, estrogen, prolactin, LH - luteinizing hormone and FSH - follicle stimulating hormone, estradiol, androgenic steroid hormone, which, in addition to male organs, is also present in the ovaries, and all of the above items affect the general condition of the reproductive system.
But the quality of the female body depends not only on the functioning of the female genital organs. Derivatives of the thyroid gland also help to ensure a harmonious life, which, if possible, is also desirable to pass. These are TSH, T4 free, T3 free - they affect overall well-being, nervous system, blood pressure, skin and hair condition, carbohydrate metabolism, and hence weight.
These are TSH, T4 free, T3 free - they affect overall well-being, nervous system, blood pressure, skin and hair condition, carbohydrate metabolism, and hence weight.
This is the perfect picture. But, most often, the doctor prescribes contraceptives, guided by minimal information, which is sometimes enough. Whether or not to undergo examinations is a matter of the patient's consciousness, but not a mandatory doctor's appointment.
All of them are divided into 2 types: combined tablets (COCs) and mini-pills. As you can understand, the combined ones consist of two components, the mini-tablets are based on one.
Differences between COCs and minipills
They differ not only in composition, but also in their effect on the body.
Mini-pills, usually consist of microdosed progestogens. Their clinically proven effectiveness is lower than that of the combined ones, but there is a plus - they are suitable for breastfeeding and 1. 5 months after childbirth. Due to the fact that the drug contains one low-dose component, it affects only the endometrium, without affecting the main functions of the reproductive system. So, their intake makes the attachment of a fertilized egg impossible and pregnancy does not occur.
5 months after childbirth. Due to the fact that the drug contains one low-dose component, it affects only the endometrium, without affecting the main functions of the reproductive system. So, their intake makes the attachment of a fertilized egg impossible and pregnancy does not occur.
This principle of action of the mini-pill gives an undeniable advantage over COCs - minimizing side effects. The choice in favor of the mini-pills is also made by the doctor when the patient has serious reasons for prohibiting the use of combined OCs - arterial hypertension, chronic liver disease, diabetes, migraines.
COC, , unlike the previous version, has a more massive effect, because the contraceptive effect occurs through the pituitary gland. Combined are further divided into three types:
monophasic - each pill in the package contains the same dose of hormones, does not cause an increase in pressure, does not provoke an increase in body weight, does not retain fluid, and does not have a significant effect on the liver. Diana, Silest, Marvelon, Silest, Laktinet, Logest.
Diana, Silest, Marvelon, Silest, Laktinet, Logest.
biphasic - contain different doses of hormones: the first majority contain estrogens, in the rest, gestagens are connected to estrogens. This approach imitates the natural fluctuation of hormones in a girl at different periods of the cycle. Drugs in this group are prescribed infrequently. Antiovin, Regevidon, Minisiston, Adepal
three-phase - contain different doses of hormones, but in total - the smallest or microdose - in comparison with previous drugs. They are considered the most modern and most naturally imitate cycle. Triziston, Tri-regol, Tri-merci, Trinovum.
Pros and cons of COC
If the question of choosing contraceptive pills is on your agenda, you should understand that even a full examination, a thorough consultation with a gynecologist and an examination will not be able to give completely favorable forecasts regarding the use of hormonal pills. The body of each lady is individual, as well as the selection of funds.
- Considered the most effective way to prevent unwanted pregnancy
- They have “nice bonuses” in the form of clear skin, getting rid of blackheads and acne, the absence of oily skin, weight loss, reducing pain during menstruation and eliminating PMS, increasing breast size.
- additionally have a preventive and therapeutic effect on the female reproductive system
- convenient and easy to use
- reduce the risk of developing ovarian, endometrial and cervical cancers
Cons:
- will not protect against vaginal infections and fungi, dangerous diseases
- require strict discipline to receive at the same time every day
- may cause unwanted side effects: headaches, nausea, fluid retention, increased appetite, mood swings
- complete restoration of the ability to conceive is restored in a woman from 2 to 6 months
- incompatible with certain medications (anticonvulsants and antibacterials) and lifestyle (even occasional drinking and smoking)
How to take hormones correctly
- All contraceptives are available with either 21 active tablets in a blister or 28.
- Carefully read the instructions, follow all manufacturer's instructions
- Tablets should be taken from the 1st to the 5th day of the onset of menstruation. If this is a pack of 21 tablets, then after taking the last one, a break is made for 7 days and after that it is important to proceed to the next pack, regardless of which day the menstruation began. If there are 28 birth control pills in a package, then no breaks are needed. After the last pill, immediately start the next one. In this case, menstruation occurs from the 21st to the 28th day.
- Control the time of reception every day! (strict reception at the same time applies to the mini-pill, since its effect is short-lived and being late even for 2-3 hours reduces the contraceptive effect to zero)
- In the first week of taking the drug, it is recommended to use additional methods of protection against unwanted pregnancy.
- With a sharp appearance of nausea, vomiting, diarrhea after drinking a pill, you should immediately stop taking hormones and try to find other drugs and methods.

Learn more