Bipolar and exercise addiction
Can Exercise Cause Mania?
Very few people with bipolar disorder get much physical activity. 78% are reported to lead sedentary lives.
For those who do exercise, little is known about the effect of exercise on this mood disorder. And yet, some people maintain that vigorous exercise can bring on manic episodes.
Could this be true?Well, yes and no.
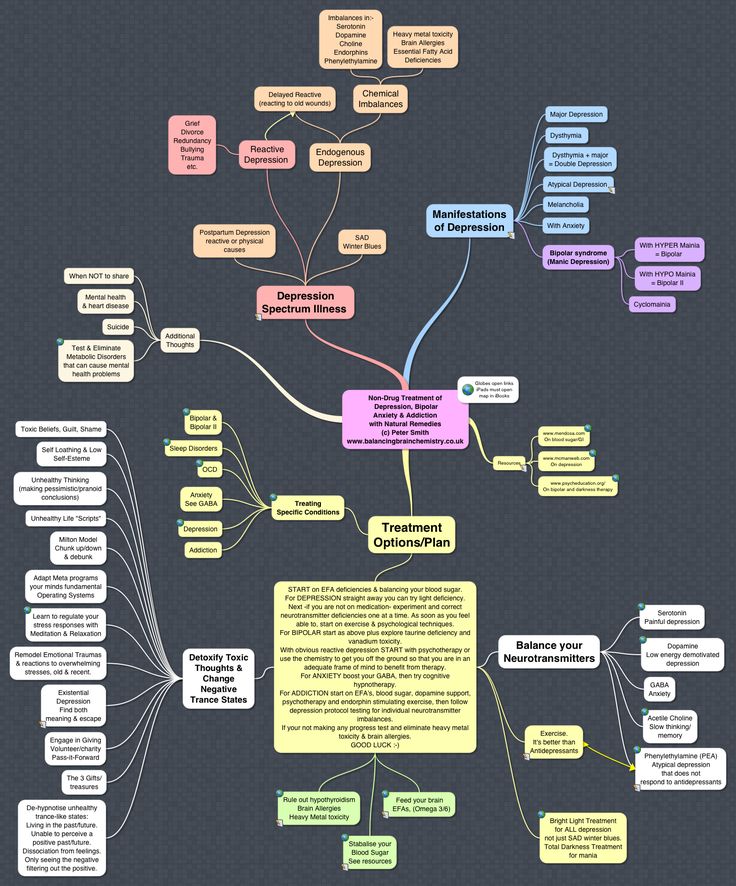
The ways exercise can help those with depression are well-researched and overwhelmingly positive.Regular physical activity can lift a persons mood from despair to upbeat, and many of the physical symptoms of depression can be improved by exercise.
Results of research into the effects of activity on depression lead many to believe that exercise should be considered a primary therapy when treating depression.
For people with bipolar disorder that tend toward mania, the results are a little murkier.
No one is advocating for a sedentary lifestyle. No one thinks inactivity is good for those with bipolar disorder. The level of activity is whats in question.
Moderate physical activity can help regulate moods and improve sleep, thus avoiding the onset of manic episodes. Exercise can also positively impact all of the physical conditions that are co-morbid with bipolar disorder.
Regular, moderate exercise can help anyone live better and live longer. This is crucial in bipolar disorder, where lifespan is shortened so severely by the effects of co-morbidity. Exercise can help ameliorate the effects of co-morbid, physical diseases.
But can exercise cause mania?
A study made the rounds a while ago and caused many headlines. It inferred that vigorous exercise can bring on a manic episode, or at least hypomania, in many with bipolar disorder.
No one will deny that vigorous activity is stimulating. Runners speak of the runners high, and exercise addiction, for a small group of people, seems to be a real thing.
I remember a manic episode I had a few years ago. I began running.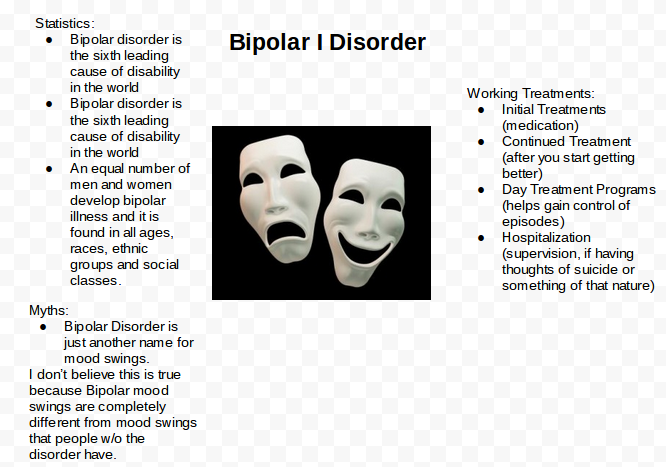 I ran far and fast, every day. As with many things I have undertaken during episodes, I overdid it. I ended up with a stress fracture in my femur, the strongest bone in the body, and I could barely walk. But its unclear if the manic episode fueled my running, or if the running fired the manic episode.
I ran far and fast, every day. As with many things I have undertaken during episodes, I overdid it. I ended up with a stress fracture in my femur, the strongest bone in the body, and I could barely walk. But its unclear if the manic episode fueled my running, or if the running fired the manic episode.
Studies on exercise and bipolar disorder have reached the same chicken and egg dilemma.Researchers cant be sure which came first, the intense activity or the mania, or if theyre just bidirectional.
The studies that imply that exercise causes mania are also limited because theyre qualitative (not statistically measured or controlled) and result from small sample sizes.
What these and other studies on bipolar disorder and exercise do conclude is that the type of exercise undertaken by the subject is key. Regular, moderate exercise seems to have no detrimental effect on mood, and can even improve it.
While vigorous exercise may lift mood into a phase a bit too exuberant for safe mental health in those with bipolar disorder, the type and frequency of exercise can change outcomes.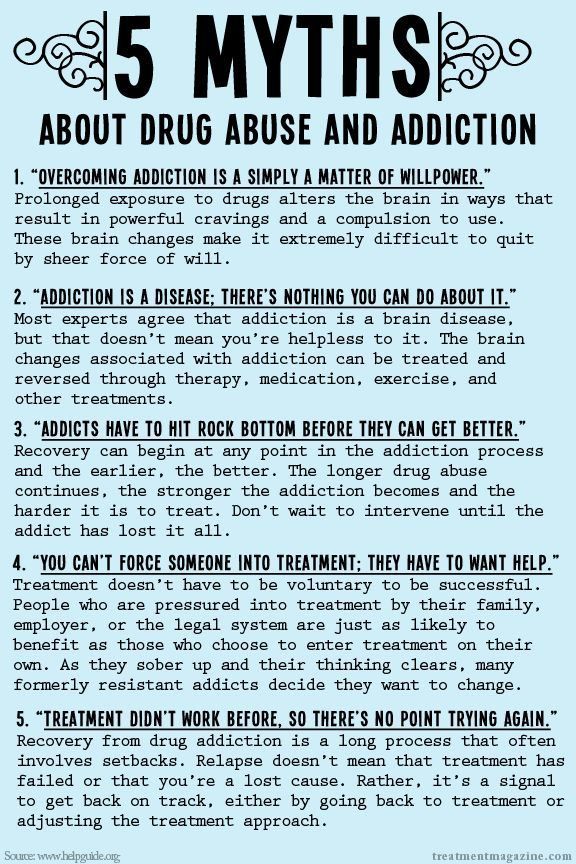
It seems rhythmic exercises like walking, running, or swimming can have a calming effect, while more multi-directional intense activity may lift the mood too high and lead the exerciser into hypomania, or mania, over time.
The point is to experiment.Many different types of exercise are available, and the person with bipolar disorder needs to get up, raise their pulse rate, and find a type of exercise that works for them.
It amazes me how headlines stir behavior. The implication of a link between exercise and mania can lead many with bipolar disorder and sedentary lives to say, why bother? No, you dont have to run to a cross fit gym, and maybe you shouldnt.But you do have to move around.
The physical and mental health benefits of exercise far outweigh any risk. Just dont overdo it.
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4349127/
Psych Central has closed its blog network to new content. Find more atPracticing Mental Illness.
Can Exercise Cause Mania?
Very few people with bipolar disorder get much physical activity. 78% are reported to lead sedentary lives.
78% are reported to lead sedentary lives.
For those who do exercise, little is known about the effect of exercise on this mood disorder. And yet, some people maintain that vigorous exercise can bring on manic episodes.
Could this be true?Well, yes and no.
The ways exercise can help those with depression are well-researched and overwhelmingly positive.Regular physical activity can lift a persons mood from despair to upbeat, and many of the physical symptoms of depression can be improved by exercise.
Results of research into the effects of activity on depression lead many to believe that exercise should be considered a primary therapy when treating depression.
For people with bipolar disorder that tend toward mania, the results are a little murkier.
No one is advocating for a sedentary lifestyle. No one thinks inactivity is good for those with bipolar disorder. The level of activity is whats in question.
Moderate physical activity can help regulate moods and improve sleep, thus avoiding the onset of manic episodes.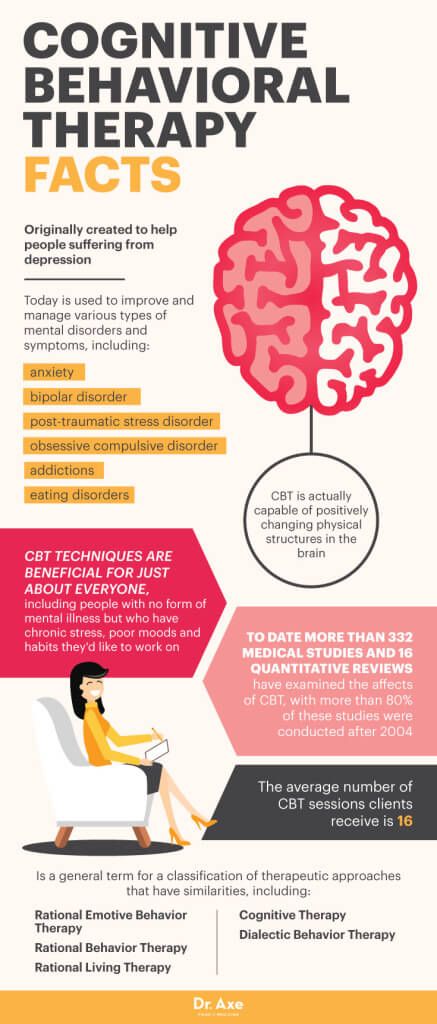 Exercise can also positively impact all of the physical conditions that are co-morbid with bipolar disorder.
Exercise can also positively impact all of the physical conditions that are co-morbid with bipolar disorder.
Regular, moderate exercise can help anyone live better and live longer. This is crucial in bipolar disorder, where lifespan is shortened so severely by the effects of co-morbidity. Exercise can help ameliorate the effects of co-morbid, physical diseases.
But can exercise cause mania?
A study made the rounds a while ago and caused many headlines. It inferred that vigorous exercise can bring on a manic episode, or at least hypomania, in many with bipolar disorder.
No one will deny that vigorous activity is stimulating. Runners speak of the runners high, and exercise addiction, for a small group of people, seems to be a real thing.
I remember a manic episode I had a few years ago. I began running. I ran far and fast, every day. As with many things I have undertaken during episodes, I overdid it. I ended up with a stress fracture in my femur, the strongest bone in the body, and I could barely walk. But its unclear if the manic episode fueled my running, or if the running fired the manic episode.
But its unclear if the manic episode fueled my running, or if the running fired the manic episode.
Studies on exercise and bipolar disorder have reached the same chicken and egg dilemma.Researchers cant be sure which came first, the intense activity or the mania, or if theyre just bidirectional.
The studies that imply that exercise causes mania are also limited because theyre qualitative (not statistically measured or controlled) and result from small sample sizes.
What these and other studies on bipolar disorder and exercise do conclude is that the type of exercise undertaken by the subject is key. Regular, moderate exercise seems to have no detrimental effect on mood, and can even improve it.
While vigorous exercise may lift mood into a phase a bit too exuberant for safe mental health in those with bipolar disorder, the type and frequency of exercise can change outcomes.
It seems rhythmic exercises like walking, running, or swimming can have a calming effect, while more multi-directional intense activity may lift the mood too high and lead the exerciser into hypomania, or mania, over time.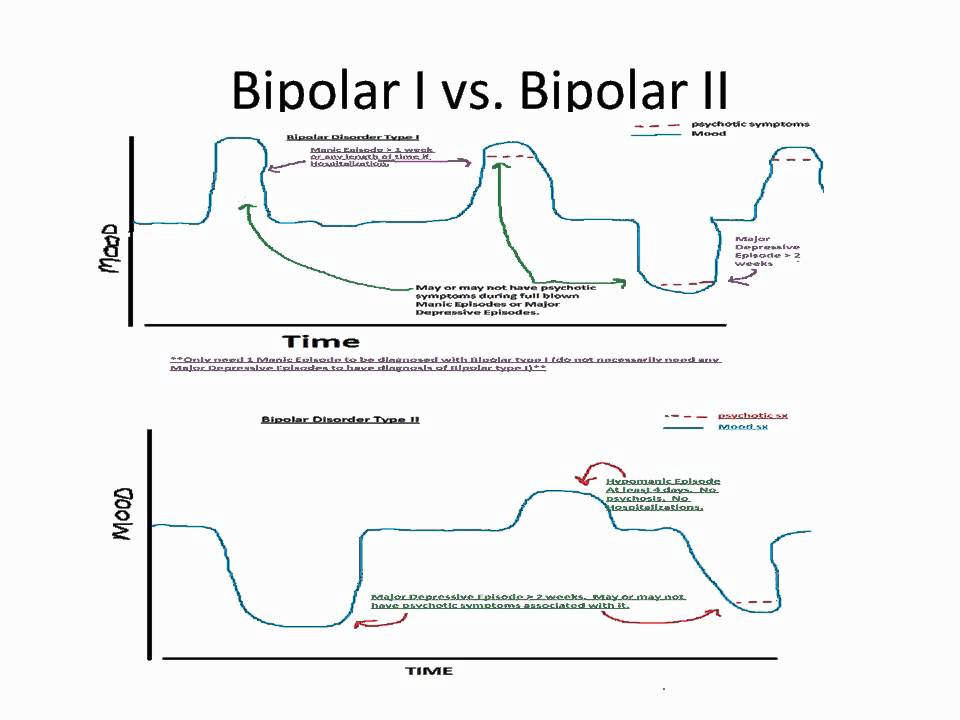
The point is to experiment.Many different types of exercise are available, and the person with bipolar disorder needs to get up, raise their pulse rate, and find a type of exercise that works for them.
It amazes me how headlines stir behavior. The implication of a link between exercise and mania can lead many with bipolar disorder and sedentary lives to say, why bother? No, you dont have to run to a cross fit gym, and maybe you shouldnt.But you do have to move around.
The physical and mental health benefits of exercise far outweigh any risk. Just dont overdo it.
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4349127/
Psych Central has closed its blog network to new content. Find more atPracticing Mental Illness.
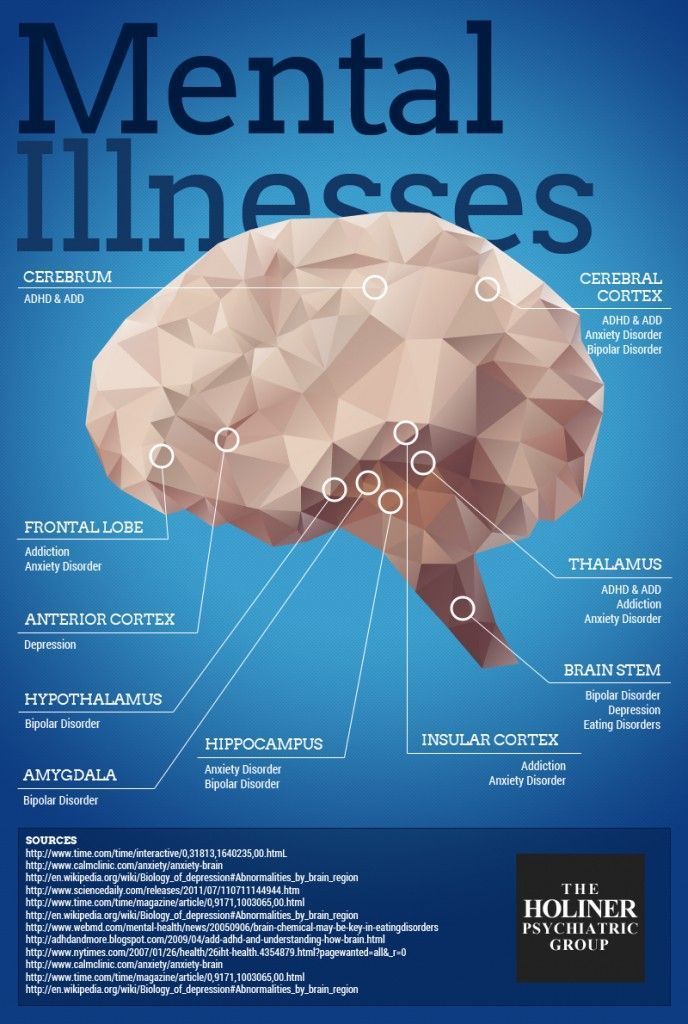
Classification and risk factors, Comorbidity
In this section
I and Bar II
Type II Bipolar Disorders differ in the nature of affective episodes 1.2 :
Bipolar disorder.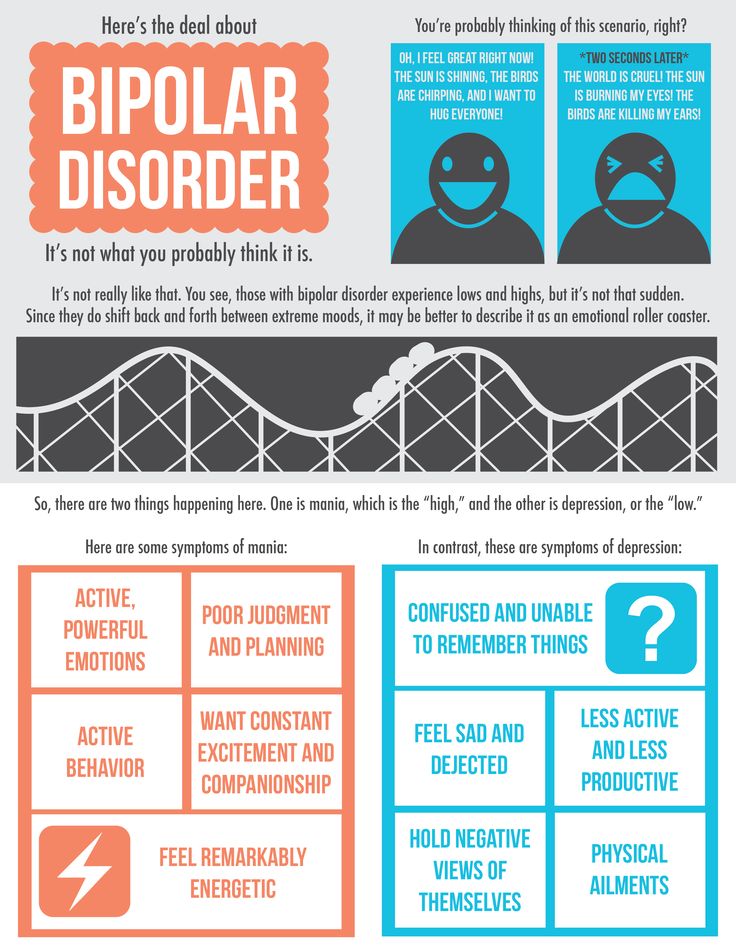 Type I : the patient has a history of or currently has a manic episode (a pathologically elevated mood over an extended period of time). Also, patients often experience depression and hypomania, but these conditions are not mandatory for the diagnosis.
Type I : the patient has a history of or currently has a manic episode (a pathologically elevated mood over an extended period of time). Also, patients often experience depression and hypomania, but these conditions are not mandatory for the diagnosis.
Bipolar II Disorder : The patient has experienced at least one episode of hypomania (a milder and shorter form of mania) and one major depressive episode.
Individuals with type I bipolar disorder also have euthymic periods when mood is "normal"; that is, at this time there is no elevated or depressed mood 1 .
Fluctuations in mood and energy levels are common, especially during times of stress. However, people with bipolar I disorder have severe mood swings ( mania, hypomania and depression ) persisting for a certain time 3 .
Bipolar I and Bipolar II: risk factors
The exact mechanism underlying the development of bipolar disorder is unknown. Risk factors include, but are not limited to:
Risk factors include, but are not limited to:
Heredity 3 . Heritability in bipolar disorder has been estimated to be as high as 85%
Childhood abuse 4 . For example, physical, sexual and emotional abuse and neglect.
Substance abuse 4 . Use of cannabinoids, opioids, cocaine, sedatives, alcohol.
Psychologically traumatic situations 4 . Family history of first-degree relative suicide, divorce, unemployment, early loss of parents.
Perinatal factors 3 . Influenza, mother smoking during pregnancy.
BAD I and BAD II: comorbidity
Comorbidity with mental and somatic diseases in bipolar disorder is the norm rather than the exception. The lifetime prevalence is 90%; 50% of patients with bipolar disorder are polymorbid (i.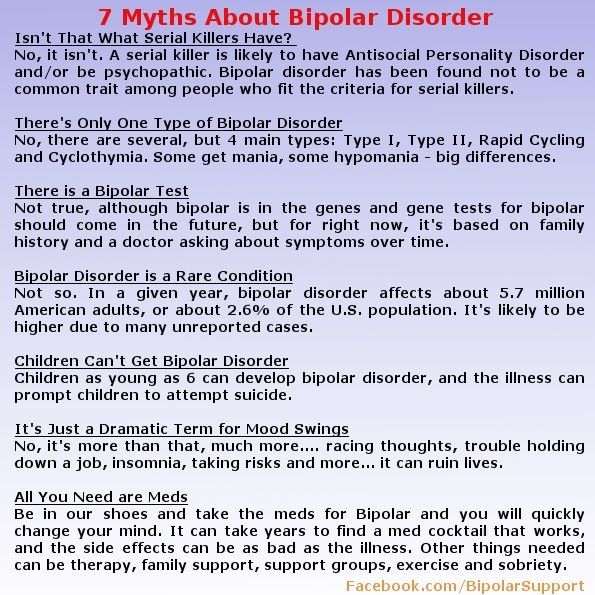 e., the presence of at least 3 comorbid diseases) 5 .
e., the presence of at least 3 comorbid diseases) 5 .
The most common comorbid psychiatric disorders are anxiety disorders and substance abuse, which occur in 60% and 40% of patients with bipolar disorder, respectively 6 .
Care must be taken when making a diagnosis of comorbid disease: the diagnosis should be made solely on the basis of symptoms present during euthymic periods or when symptoms of bipolar disorder are controlled 6 .
Non-psychiatric comorbidity includes metabolic syndrome, diabetes mellitus, osteoporosis, fibromyalgia and other endocrine and cardiovascular diseases
3 .
Comorbidity is associated with earlier age of onset, more complex manifestations of bipolar disorder, increased risk of suicide, worse treatment response and prognosis compared with bipolar disorder without comorbidities 5 .
Sources:
- McIntyre, R. S. et al.
 Bipolar disorders. Lancet 396, 1841–1856 (2020).
Bipolar disorders. Lancet 396, 1841–1856 (2020). - National Collaborating Center for Mental Health (UK). Bipolar Disorder: The NICE Guideline on the Assessment and Management of Bipolar Disorder in Adults, Children and Young People in Primary and Secondary Care . (The British Psychological Society and The Royal College of Psychiatrists, 2014).
- Vieta E, Berk M, Schulze TG, et al. bipolar disorders. Nat Rev Dis Primers . 2018;4:18008.
- Rowland, T. A. & Marwaha, S. Epidemiology and risk factors for bipolar disorder. Ther. Adv. Psychopharmacol. 9 , 251–269 (2018).
- McIntyre, R. S. et al. Bipolar disorders. Lancet 396, 1841–1856 (2020).
- National Collaborating Center for Mental Health (UK). Bipolar Disorder: The NICE Guideline on the Assessment and Management of Bipolar Disorder in Adults, Children and Young People in Primary and Secondary Care .
 (The British Psychological Society and The Royal College of Psychiatrists, 2014).
(The British Psychological Society and The Royal College of Psychiatrists, 2014).
Login to Unlock
Cariprazine uses … Cariprazine uses …
Bipolar I manic or mixed episodes. Depressive episodes in bipolar type I disorder (bipolar depression). Manic or mixed episodes of bipolar type I disorder. Depressive episodes in bipolar I disorder (bipolar depression).
More…
Login to Unlock
World Bipolar Day… World Bipolar Day…
World Bipolar Day is an important event for psychiatrists. All events that take place on this day are aimed at raising awareness of World Bipolar Day, an important event for psychiatrists. All events that take place on this day are aimed at raising awareness n
More…
Please confirm your consent to the use of cookies
Yes, I agree
No, I refuse0008
Please confirm that you are a healthcare worker
Showing 0 result(s).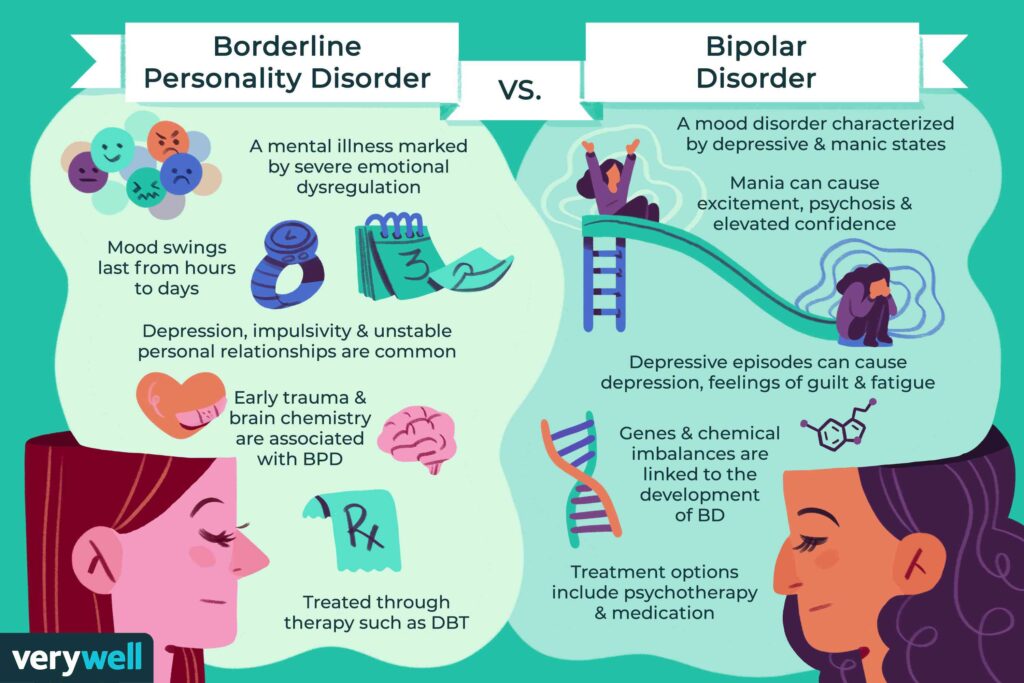
Please log in to see 0 more result(s).
Bipolar affective disorder: symptoms
In this section
Bipolar affective disorder (BAD) is designated in the International Static Classification of Diseases and Related Health Problems as 1 :
F31 - Bipolar affective disorder;
F31.0 - Bipolar affective disorder, current hypomanic episode;
F31.1 - Bipolar affective disorder, current episode of mania without psychotic symptoms current;
F31.2 - Bipolar affective disorder, current episode of mania with psychotic symptoms current;
F31.3 - Bipolar affective disorder, current episode of moderate or mild depression current;
F31.30 - Bipolar affective disorder, current episode of moderate or mild depression without physical symptoms;
F31.31 - Bipolar affective disorder, current episode of moderate or mild depression current with somatic symptoms;
F31.4 - Bipolar affective disorder, current episode of severe depression without psychotic symptoms current;
F31.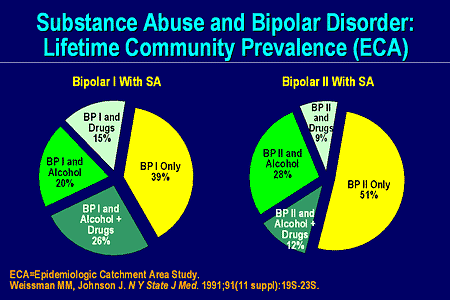 5 - Bipolar affective disorder, current episode of severe depression with psychotic symptoms current;
5 - Bipolar affective disorder, current episode of severe depression with psychotic symptoms current;
F31.6 - Bipolar affective disorder, current episode mixed;
F31.7 - Bipolar affective disorder, state of remission;
F31.8 - Other bipolar affective disorders;
F31.9 - Bipolar affective disorder, unspecified.
In accordance with ICD-10, the diagnosis is made if there is at least one manic or mixed episode during the course of the disease.
Symptoms. Depressive episode
1.2Depressive mood
Loss of interest or pleasure.
Weight loss or gain.
Insomnia or hypersomnia.
Feeling tired.
Feelings of worthlessness/guilt.
Inability to concentrate.
Thoughts of death or suicidal attempt.
Psychomotor retardation or agitation.
Symptoms.
 Mania/hypomania 1.2
Mania/hypomania 1.2 Inflated self-esteem or ideas of grandeur.
Reduced need for sleep.
Increased talkativeness.
Many ideas or a leap of thought.
Increased distractibility.
Increased activity.
Excessive participation in pleasurable activities with potentially negative consequences.
Hypomania: same symptoms, but milder and shorter.
Symptoms. Mixed state
3During a mixed episode, symptoms of mania/hypomania and depression are present simultaneously. The patient may experience:
an excess of energy at the same time as feeling sad;
need for communication, conversations against the background of pessimism;
leap of ideas and indecision.
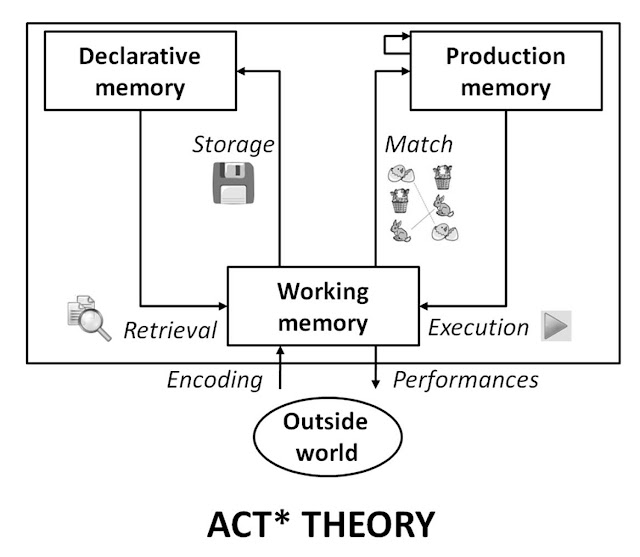
BAD is a complex disease. In different periods of time there are various psychopathological symptom complexes. Affective phases of different poles, having different degrees of severity and typology (mania, depression, mixed states, affective-delusional formations) can end spontaneously with the formation of intermissions characterized by euthymic mood and full criticality to the transferred painful episode. Along with mood and behavioral disorders, bipolar disorder often causes disorders in other areas of mental activity (for example, cognitive, perception), as well as neurovegetative symptoms (disturbances in sleep, appetite, circadian rhythm, energy balance, etc.). In different periods of the disease, the presence and severity of these symptoms can vary significantly 1 . More than half of patients with bipolar disorder have psychotic symptoms at different stages of the disease 1 .
Along with mood and behavioral disorders, bipolar disorder often causes disorders in other areas of mental activity (for example, cognitive, perception), as well as neurovegetative symptoms (disturbances in sleep, appetite, circadian rhythm, energy balance, etc.). In different periods of the disease, the presence and severity of these symptoms can vary significantly 1 . More than half of patients with bipolar disorder have psychotic symptoms at different stages of the disease 1 .
In the euthymic period, patients with bipolar disorder show normalization of mood and absence of excessive mood swings; patients have no clinical symptoms of either depression or mania/hypomania. During this period, patients receive maintenance therapy. However, euthymia does not mean a complete return to normal life: patients continue to experience problems in the areas of social and professional activities that need to be addressed by continuing maintenance therapy 4 .
Sources:
- Clinical guidelines. Bipolar affective disorder. Ministry of Health of Russia. 2021.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders 5th ed: 2013.
- Vraylar drug web page: Available at: www.vraylar.com/. Accessed March 20, 2019.
- Bhatia, P., Sidana, A., Das, S. & Bajaj, M. K. Neuropsychological Functioning in Euthymic Phase of Bipolar Affective Disorder. Indian J. Psychol. Med. 40, 213–218 (2018).
Login to Unlock
Bipolar disorder and schizophrenia… Bipolar disorder and schizophrenia…
Bipolar affective disorder (BAD) is a chronic relapsing disease from the category of affective mental disorders. Bipolar affective disorder (BAD) is a chronic, relapsing illness from the category of mental disorders of the affective sphere. BAR character
More…
Login to Unlock
Cariprazine Options… Cariprazine Options…
Bipolar I Manic or Mixed Episodes.