Emotional abuse depression
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.

-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly.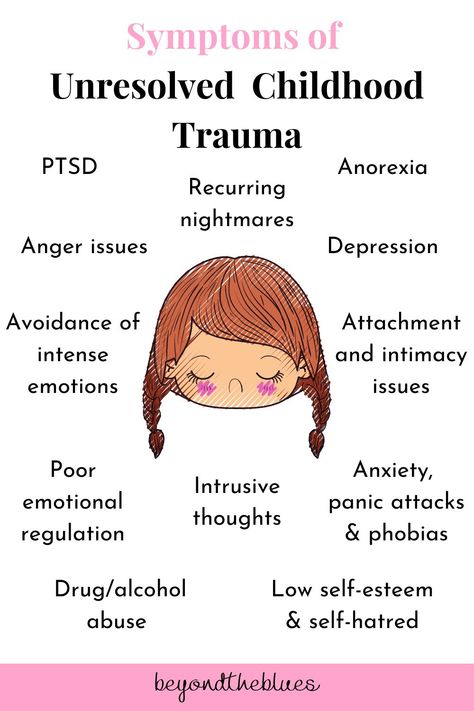 Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Depression in female victims of domestic violence (forensic psychiatric observations)
It is known that recently there has been an increase in depressive disorders. According to WHO 1 , in 2020 depression will be the second (after coronary heart disease) cause of lost healthy years of life and premature death. Among those suffering from depression, there is a predominance of women. The occurrence of depression is seen as the result of a complex interaction of social, psychological and biological factors. Depression, in turn, often acquires a pathogenetic role in the development of eating disorders, dependence on psychoactive substances, disorders of the sexual sphere, can contribute to the deterioration of the somatic condition of patients, leading to social deprivation and maladjustment, a decrease in the quality of interpersonal, including family, relationships and quality life in general.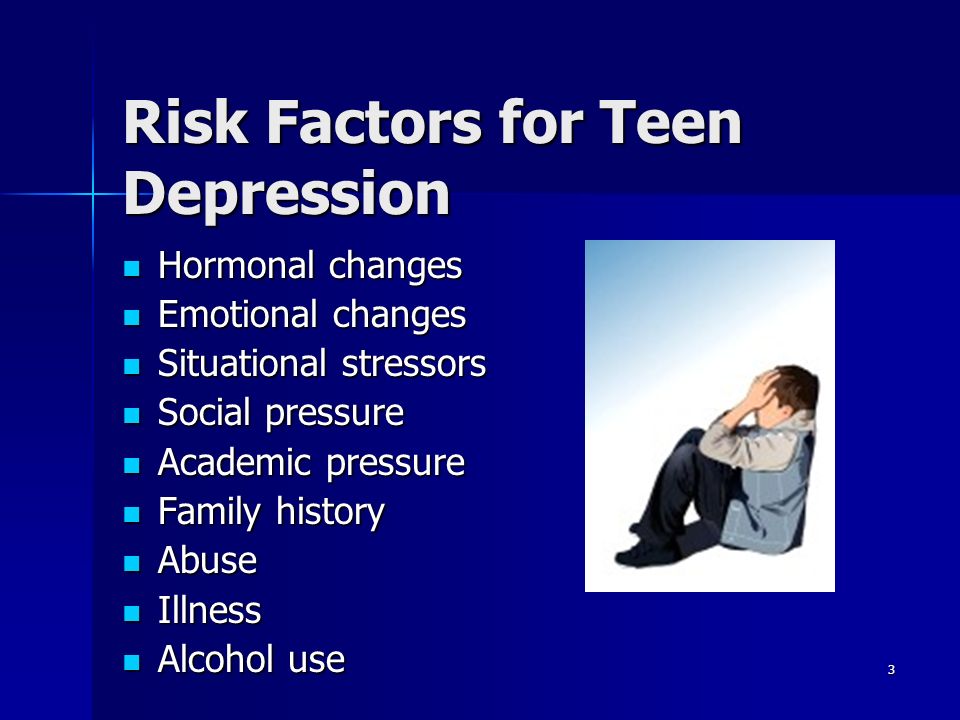
In modern literature [1-9] in the development of depression in women, a significant role is assigned to the situation of domestic violence (physical, including sexual, psychological, emotional). At the same time, we are talking not only about psychogenic depression, but also about its more severe forms. So, V. Nanni et al. [10] and L. Chen et al. [11] found a positive correlation between the development of malignant forms of depressive disorders and the presence of a situation of family violence at different periods of life. Great importance, where appropriate, is attached to the consequences of domestic violence in childhood [12-19].
The results of numerous studies [20-48] indicate a high prevalence of depression among women during pregnancy (10%) and childbirth (13%). Not only the role of the lack of necessary support from the partner and other family members is noted, but also dissatisfaction with marriage, depression of the partner, often accompanied by dependence on psychoactive substances, episodes of postpartum depression in the woman herself in the past, low socioeconomic status of the family and material shortage, the presence chronic somatoneurological and endocrine diseases, as well as the mutual potentiation of all existing factors and the "accumulation" of the past experience of violence [49-53].
The purpose of this study is to study the features of the development of depressive disorders in female victims of domestic violence in cases of aggressive acts by them.
Material and methods
We examined 12 women (mean age 35.8 ± 12.3 years) with the consequences of the development of acute depressive states as a result of domestic violence. Depending on the criminological data, the patients were divided into two groups: the 1st group included 4 women who committed the murder of their children, the 2nd group included 8 women who were accused of killing their husbands.
Results and discussion
In the premorbid period, women of the 1st group were characterized by such traits as self-doubt, timidity, indecision, a tendency to fixate on negatively colored psychogenic experiences, pessimism, and vulnerability. These features were exacerbated in difficult life situations.
The development of depressive symptoms was preceded by severe mental trauma, different in nature, strength, severity and duration of exposure. The most frequent were difficult family situation, domestic disorder, husband's alcoholism, child's illness, adultery, death of close relatives, troubles at work. There were conflicting relations with her husband, cruel, sadistic behavior, beatings. Some women were subjected to systematic humiliating torture and moral abuse.
The most frequent were difficult family situation, domestic disorder, husband's alcoholism, child's illness, adultery, death of close relatives, troubles at work. There were conflicting relations with her husband, cruel, sadistic behavior, beatings. Some women were subjected to systematic humiliating torture and moral abuse.
Psychopathological analysis of the clinical picture during the examination of patients of the 1st group made it possible to identify certain stages in the development of acute depressive reactions, during which aggressive actions are committed.
Under the influence of prolonged exposure to traumatic experiences, affective tension increased, depression, sleep disturbance, increased fatigue, and irritable weakness appeared. At this stage, depression proceeded at the neurotic level (mild depressive episode according to ICD-10, heading F32.0). At the same time, various vegetative and functional somatic disorders "masked" depressive symptoms. Women often turned to doctors of various specialties with complaints of insomnia, headaches, pain in the heart area and fluctuations in blood pressure, menstrual irregularities, and often they were diagnosed with such diagnoses as neurasthenia, vegetative dystonia, asthenic condition, etc. In those cases when there were significant difficulties in the performance of household, social and professional duties, the condition of women was defined as a moderate depressive episode (F32.1 according to ICD-10). At the same time, depressive mood was accompanied by a decrease in mental activity and an increase in volitional disorders with the absence of attempts to resolve the psychotraumatic situation. There was a narrowing of the circle of interests and a concentration of attention on a traumatic situation, thoughts about which took on a dominant character. Ideas of low value were formed, which at first reflected the real situation.
Women often turned to doctors of various specialties with complaints of insomnia, headaches, pain in the heart area and fluctuations in blood pressure, menstrual irregularities, and often they were diagnosed with such diagnoses as neurasthenia, vegetative dystonia, asthenic condition, etc. In those cases when there were significant difficulties in the performance of household, social and professional duties, the condition of women was defined as a moderate depressive episode (F32.1 according to ICD-10). At the same time, depressive mood was accompanied by a decrease in mental activity and an increase in volitional disorders with the absence of attempts to resolve the psychotraumatic situation. There was a narrowing of the circle of interests and a concentration of attention on a traumatic situation, thoughts about which took on a dominant character. Ideas of low value were formed, which at first reflected the real situation.
The development and deepening of the depressive state was facilitated by the addition of additional somatogenic factors associated with vegetative-endocrine changes in the woman's body: pregnancy, childbirth, complications of the postpartum period, the onset of menopause. Such manifestations of depression were already assessed by doctors as a severe depressive episode without psychotic symptoms (F32.2 according to ICD-10).
Such manifestations of depression were already assessed by doctors as a severe depressive episode without psychotic symptoms (F32.2 according to ICD-10).
The intensification of depression was characterized by the appearance of melancholy, which sometimes acquired a vital character. The emergence of melancholy, diurnal mood swings, vitalization of depression was accompanied by the development of depressive ideas. Women felt deep despair, acute grief. They regarded the difficult life situation as unbearable, they had a false conclusion about the absence of a way out of the situation, suicidal thoughts were revealed. Persistent overvalued ideas about the meaninglessness, worthlessness of existence, ideas of low value and self-blame were formed.
Against the background of a steady increase in depressive affect under the influence of additional traumatic factors, an acute depressive psychotic state developed, a severe depressive episode with psychotic symptoms (F32.3 according to ICD-10), which is characterized by the presence of deep melancholy, a sense of hopelessness, anxiety, fear, despair, depressive ideas about imminent death, thoughts about the hopelessness of the current situation, which determined the aggressive actions of women. In women of the 1st group, it was about aggressive actions directed at children, in which a pathologically transformed altruistic motivation of behavior was clearly revealed - the murders were committed out of a sense of "compassion".
In women of the 1st group, it was about aggressive actions directed at children, in which a pathologically transformed altruistic motivation of behavior was clearly revealed - the murders were committed out of a sense of "compassion".
Further dynamics of the state was determined by the reaction to the deed. It reflected, on the one hand, the depth of the psychotic state, and, on the other hand, its psychogenic nature. In all cases, the dynamics of depression was progressive. After the commission of the delict, women experienced motor and ideational retardation, confusion, insomnia, suicidal mood, melancholy, and depression. Sometimes depression was accompanied by agitation and patients made true suicidal attempts.
In the described cases in patients of the 1st group, acute psychotic depression passed into a protracted phase, often with the development of a protracted reactive psychosis.
Depression in patients of the 2nd group was characterized by short-term psychotic states with impaired consciousness, which arose by the mechanism of "short circuit". In this group, in all women, an asthenizing factor was identified, which was determined by the presence of residual effects after repeated craniocerebral injuries resulting from beatings of her husband.
In this group, in all women, an asthenizing factor was identified, which was determined by the presence of residual effects after repeated craniocerebral injuries resulting from beatings of her husband.
All cases in the 2nd group were distinguished by a special drama that preceded the delict of a psychotraumatic situation. This is a difficult family situation, associated with bullying, moral and physical torture on the part of husbands. According to the materials of criminal cases, all the husbands of women of the 2nd group abused alcohol, their actions were unlawful, illegal, immoral, sometimes sadistic and cynical, accompanied by violence, grave insults, terror against their wives and children. Many years of systematic torture and torture took place.
Strong, long-acting traumatic effects could not but affect the dignity of the personality of women. As for the nature of the aggressive actions committed by women of the 2nd group, they were directed directly at the offenders, the perpetrators of psychotraumatic experiences. In all cases, the criminal actions of women were distinguished by particular cruelty, they were alien, not characteristic of the individual.
In all cases, the criminal actions of women were distinguished by particular cruelty, they were alien, not characteristic of the individual.
In psychopathological terms, in the 2nd group, it was about acute depressive reactions that proceeded according to the "short circuit" mechanism. But the dynamics of the development of reactive depression as a whole was similar to that in the 1st group - with the change of a neurotic syndrome by an acute psychotic state with aggression and subsequent prolonged depression.
At the neurotic stage of the development of reactive depression in women of the 2nd group, against the background of persistent mood disorders of a depressive nature, such character traits inherent in them as indecision, passivity, inability to make a decision were sharpened. Depression was accompanied by emotional and volitional disorders, which determined the absence of attempts to find a rational way out of the situation.
Characteristically, women of the 2nd group never appealed to official authorities with complaints about their husband's behavior, did not call for help from relatives or friends. On the contrary, they hid the family situation from others, patiently endured all bullying.
On the contrary, they hid the family situation from others, patiently endured all bullying.
The neurotic stage was characterized by polymorphic neurotic, emotional-volitional and characterological disorders (in some cases with a change in personality structure according to the type of neurotic development).
Under the influence of severe psychogenic traumatic effects in women of the 2nd group, depression deepened, accompanied by a real fear for their lives. At the prepsychotic stage of the development of reactive depression, affective tension reached an extreme degree of severity. Under the influence of an acute mental trauma, directly related in its content to the entire previous painful situation (“the last straw”), women developed an acute psychotic depressive state with the participation of the “short circuit” mechanism. This state had all the signs inherent in deep depression, with the presence of melancholy and feelings of hopelessness, anxiety, fear, despair. However, a feature in women of the 2nd group was the mechanism of discharge of affective tension, phenomenologically expressed by the explosive nature of aggressive actions, impaired consciousness, phenomena of motor automatism with impulsive actions, a feeling of "double strength", complete or partial amnesia of the period of the offense.
However, a feature in women of the 2nd group was the mechanism of discharge of affective tension, phenomenologically expressed by the explosive nature of aggressive actions, impaired consciousness, phenomena of motor automatism with impulsive actions, a feeling of "double strength", complete or partial amnesia of the period of the offense.
It is important to note that after the offense in patients of the 2nd group, there was an exhaustion of affect, accompanied by mental and physical relaxation, a subjective experience of relief from unbearable affective tension. This state of exhaustion of affect is usually clearly reflected in the testimony of the witnesses: "numb", "stupefied", "was aloof", "looked terribly calm".
At the third, protracted stage of the depressive reaction, women noted partial or complete amnesia during the period of aggressive actions, often with a feeling of alienation of the deed, which is evidence of a deep disorder of consciousness during the period of the delict. After the commission of the crime, the main content of depression in women was determined by the reaction to the murder. During the examination, they were depressed, depressed, confused, sad, complained of insomnia, blamed themselves for what they had done, expressed suicidal thoughts.
After the commission of the crime, the main content of depression in women was determined by the reaction to the murder. During the examination, they were depressed, depressed, confused, sad, complained of insomnia, blamed themselves for what they had done, expressed suicidal thoughts.
In general, in the 2nd group of patients, the third, protracted stage was characterized by a milder course of acute depressive reactions, since they lacked the development and systematization of depressive ideas of self-blame.
Thus, the analysis of clinical observations in women of both groups revealed a number of regularities in the emergence and development of short-term psychotic disorders that develop against the background of long-term depressive states. They occur in women in conditions of a long-term objectively difficult and subjectively significant psychogenic-traumatic situation caused by intra-family violence with a combined effect of additional mental trauma and asthenic factors caused by vegetative-endocrine changes associated with the biological periods of the female body. The interaction of somatogenic and situational-psychogenic factors contributes to the development and deepening of psychogenic depressive states that have arisen, characterized by gradual progressive dynamics, which reflects the deepening of depression and the complication of psychopathological syndromes - neurotic, acute psychotic, culminating in aggressive actions.
The interaction of somatogenic and situational-psychogenic factors contributes to the development and deepening of psychogenic depressive states that have arisen, characterized by gradual progressive dynamics, which reflects the deepening of depression and the complication of psychopathological syndromes - neurotic, acute psychotic, culminating in aggressive actions.
The authors declare no conflict of interest.
Information about authors
Kharitonova N.K. - Dr. med. Sci., Prof., Head of Department, National Medical Research Center for Psychiatry and Narcology named after N.N. V.P. Serbsky" of the Ministry of Health of Russia, Moscow; e-mail: [email protected] [ Kharitonova N.K. - doctor of medical sciences, professor, head of department FGBU "National medical research center of psychiatry and narcology. V.P. Serbsky, Moscow, Russia; e-mail: [email protected]; https://orcid.org/0000-0002-0238-1690]
Kachaeva M. A. - Dr. med. Sci., Prof., Chief Researcher, National Medical Research Center for Psychiatry and Narcology named after N.N. V.P. Serbsky" of the Ministry of Health of Russia, Moscow; e-mail: [email protected]; https://orcid.org/0000-0002-7642-9829 [ Kachaeva M.A. - doctor of medical sciences, professor, chief researcher FGBU "National medical research center of psychiatry and narcology. V.P. Serbsky, Moscow, Russia; e-mail: [email protected]]
A. - Dr. med. Sci., Prof., Chief Researcher, National Medical Research Center for Psychiatry and Narcology named after N.N. V.P. Serbsky" of the Ministry of Health of Russia, Moscow; e-mail: [email protected]; https://orcid.org/0000-0002-7642-9829 [ Kachaeva M.A. - doctor of medical sciences, professor, chief researcher FGBU "National medical research center of psychiatry and narcology. V.P. Serbsky, Moscow, Russia; e-mail: [email protected]]
Kazakovtsev B.A. - Dr. med. Sci., Prof., Head of the Department of Epidemiological and Organizational Problems of Psychiatry, Federal State Budgetary Institution National Medical Research Center for Psychiatry and Narcology named after N.N. V.P. Serbsky" of the Ministry of Health of Russia, Moscow; e-mail: [email protected] [ Kazakovtsev B.A. - MD, professor, head of Department of epidemiological and organizational problems of psychiatry of V.P. Serbian National Medical Research Center for Psychiatry and Narcology of Ministry of Health of Russia, Moscow, Russia; e-mail: bakazakovtsev@serbsky. ru]
ru]
Vasyanina V.I. - Cand. honey. Sci., Senior Researcher, National Medical Research Center for Psychiatry and Narcology named after N.N. V.P. Serbian, Ministry of Health of Russia, Moscow; e-mail: [email protected] [ Vasyanina V.I. – candidate of medical sciences, senior researcher FGBU “National medical research center of psychiatry and narcology. V.P. Serbsky, Moscow, Russia; e-mail: [email protected]; https://orcid.org/0000-0002-4882-4303]
Shishkina O.A. - doctor forensic psychiatric expert of the Federal State Budgetary Institution "National Medical Research Center for Psychiatry and Narcology named after N.N. V.P. Serbsky" of the Ministry of Health of Russia, Moscow; e-mail: [email protected] [ Shishkina O.A. - doctor forensic psychiatric expert FGBU "National medical research center of psychiatry and narcology. V.P. Serbsky, Moscow, Russia; e-mail address: [email protected]]
*e-mail: spe-gray@yandex. ru
ru
https://orcid.org/0000-0002-0238-1690
Psychological violence and its 7 invisible effects
3 min.
Very often, the victim of psychological abuse experiences a strong sense of guilt, which prevents her from breaking off painful relationships and at the same time causes the development of depression.
Last updated: May 11, 2019
Psychological abuse, without a doubt, is about one of the most severe types of maltreatment of people . Such an attitude always raises certain doubts, but is it really bad for a person? But the biggest problem is that in the absence of physical aggression, the victim psychological violence is not always aware of the full drama of the situation.
And while psychological abuse is invisible, it also has negative consequences for our emotional health.
This cannot be seen with the naked eye, but the victim bears the burden of guilt and suffering for a very long time even after leaving such a relationship.
1. Constant feeling of worthlessness
Low self-esteem can be one of the triggers psychological abuse against a person . A man with self-respect would never allow such a thing. Nevertheless, the habit of underestimating oneself is a very common phenomenon.
In addition, after a person has experienced the effects of psychological abuse, the feeling of worthlessness and worthlessness may further intensify. To the point where sometimes you can't raise your head.
Asking for help and surrounding yourself with reliable people is a very important and correct decision.
Read also: The problem is not with you, but with your low self-esteem
2. Encounter with loneliness
In most cases of psychological abuse the offender tries to isolate his victim as much as possible . He can even force her to stop communicating with friends and relatives.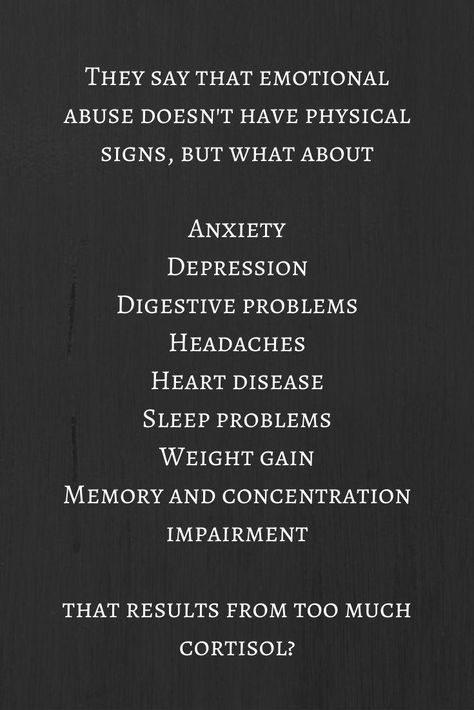
The aggressor wants to make sure that the victim does not have any support. Then she is unlikely to try to break off these destructive relationships for her.
It also happens that he intentionally creates a derogatory image of his victim so that the people around him move away from him.
3. Feeling of guilt
One of the aggressor's main trump cards is the feeling of guilt, which he cultivates in his victim. So, at any moment she will think that she herself is to blame for everything that happens to her. And the other side (the offender) simply reacts to this with some offensive words or actions.
This feeling of guilt is directly related to low self-esteem. And that's really hard to deal with.
This is interesting: Guilt: 5 things you shouldn't feel guilty about
4. Depression lurks around every corner
Depression is the great evil of our time. This is something that victims of psychological abuse deal with on a regular basis.
Depression can be so severe that a person may have suicidal thoughts.
The constant feeling of guilt, the belief that he deserved everything that happens, and loneliness make people regard suicide as the only possible way out.
5. Is it difficult to express your feelings?
One of the most noticeable consequences for people who have experienced psychological abuse is that they have difficulty expressing their emotions. This is what is called "emotional dumbness".
After all, they “swallowed insults” for so long and stifled their feelings in themselves, because they believed that they themselves were to blame for everything and deserved it.
That is, it was a kind of defensive reaction. They tried to drown out their emotions in order to survive. However, this leads, as a rule, to the previous point - to depression.
6. I can't sleep!
Insomnia is another common problem for those who have experienced psychological abuse.