Bipolar 1 with mixed episodes
Mixed Bipolar Disorder Symptoms, Causes, and Treatments
Written by Matthew Hoffman, MD
In this Article
- What Are Mixed Episodes in Bipolar Disorder?
- Who Gets Mixed Bipolar Episodes?
- What Are the Symptoms of a Mixed Features Episode?
- What Are the Risks of Mixed Features During Mood Episodes of Bipolar Disorder?
- What Are the Treatments for Mood Episodes With Mixed Features in Bipolar Disorder?
What Are Mixed Episodes in Bipolar Disorder?
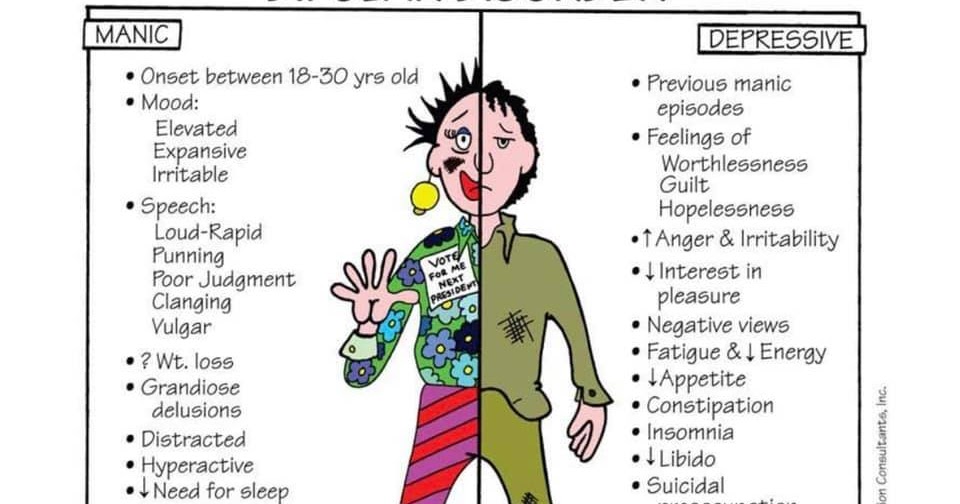
Mixed features refers to the presence of high and low symptoms occurring at the same time, or as part of a single episode, in people experiencing an episode of mania or depression. In most forms of bipolar disorder, moods alternate between elevated and depressed over time. A person with mixed features experiences symptoms of both mood "poles" -- mania and depression -- simultaneously or in rapid sequence.
Who Gets Mixed Bipolar Episodes?
Virtually anyone can develop bipolar disorder. About 2.5% of the U.S. population -- nearly 6 million people -- has some form of bipolar disorder.
Mixed episodes are common in people with bipolar disorder -- half or more of people with bipolar disorder have at least some mania symptoms during a full episode of depression. Those who develop bipolar disorder at a younger age, particularly in adolescence, may be more likely to have mixed episodes. People who develop episodes with mixed features may also develop "pure" depressed or "pure" manic or hypomanic phases of bipolar illness. People who have episodes of major depression but not full episodes of mania or hypomania also can sometimes have low-grade mania symptoms. These are symptoms that are not severe or extensive enough to be classified as bipolar disorder. This is referred to as an episode of "mixed depression" or a unipolar (major) depressive episode with mixed features.
Most people are in their teens or early 20s when symptoms from bipolar disorder first start.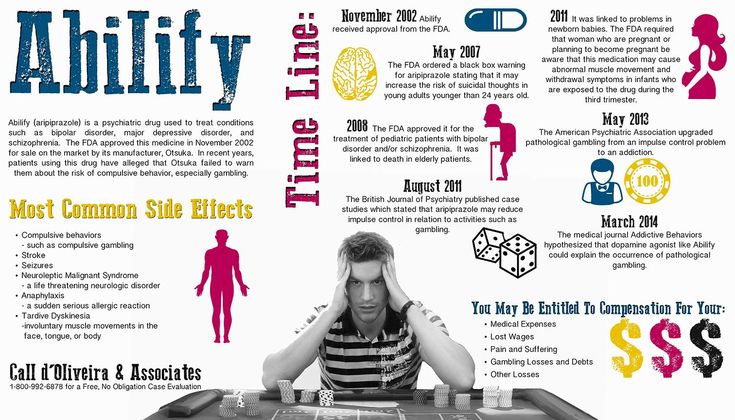 It is rare for bipolar disorder to develop for the first time after age 50. People who have an immediate family member with bipolar are at higher risk.
It is rare for bipolar disorder to develop for the first time after age 50. People who have an immediate family member with bipolar are at higher risk.
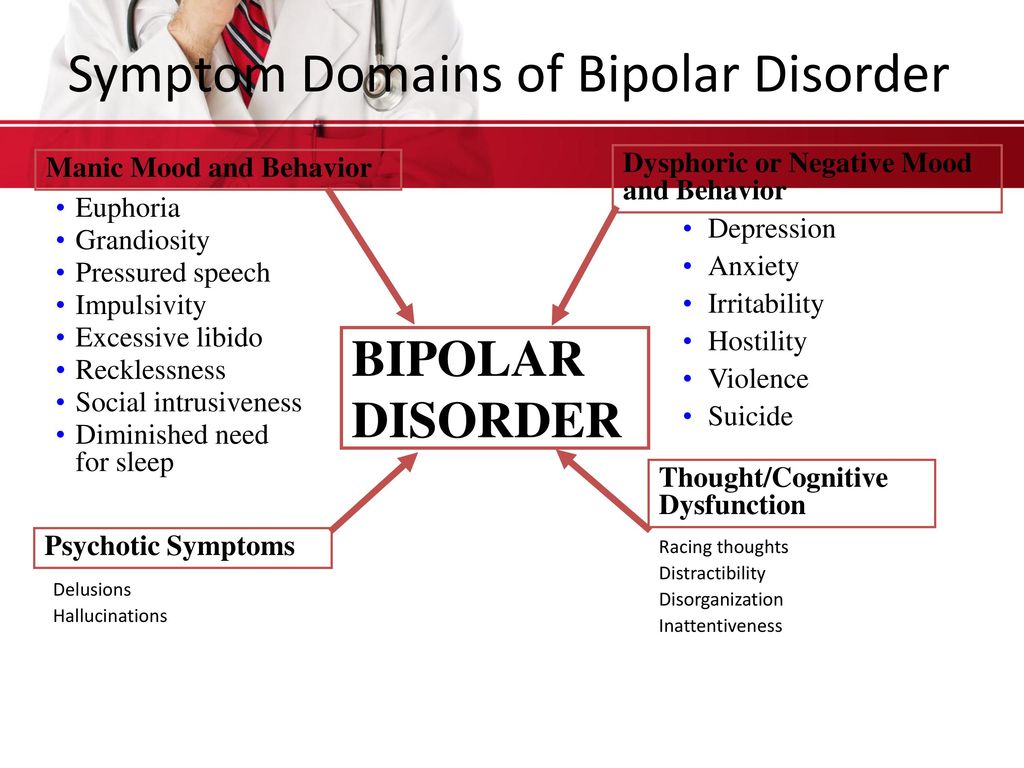
What Are the Symptoms of a Mixed Features Episode?
Mixed episodes are defined by symptoms of mania and depression that occur at the same time or in rapid sequence without recovery in between..
- Mania with mixed features usually involves irritability, high energy, racing thoughts and speech, and overactivity or agitation.
- Depression during episodes with mixed features involves the same symptoms as in "regular" depression, with feelings of sadness, loss of interest in activities, low energy, feelings of guilt and worthlessness, and thoughts of suicide.
This may seem impossible. How can someone be manic and depressed at the same time? The high energy of mania with the despair of depression are not mutually exclusive symptoms, and their co-occurrence may be much more common than people realize.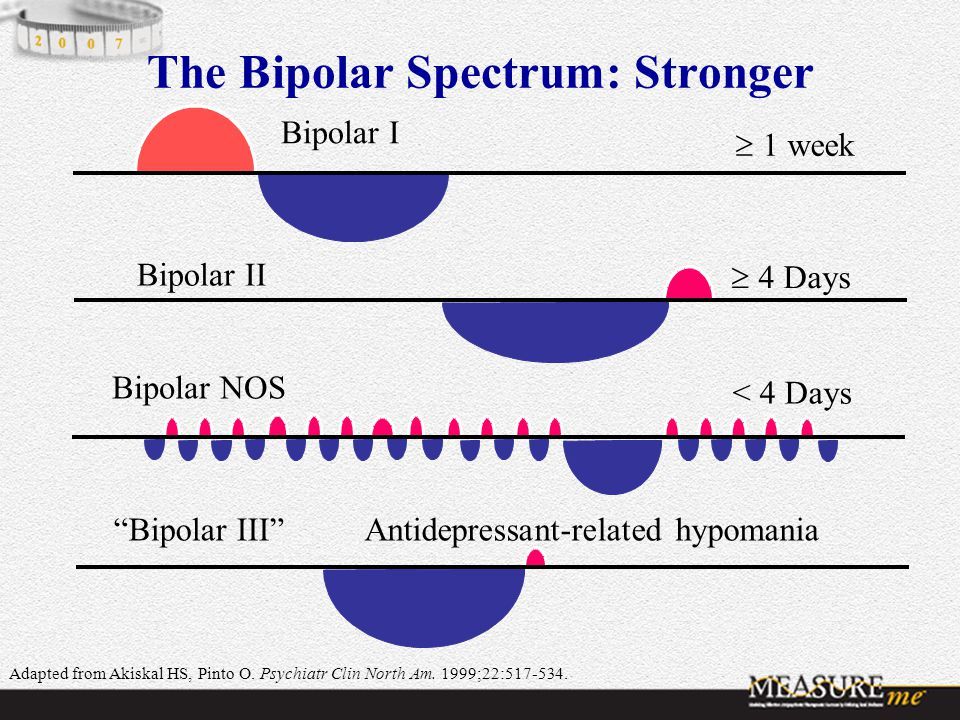
For example, a person in an episode with mixed features could be crying uncontrollably while announcing they have never felt better in their life. Or they could be exuberantly happy, only to suddenly collapse in misery. A short while later they might suddenly return to an ecstatic state.
Mood episodes with mixed features can last from days to weeks or sometimes months if untreated. They may recur ,and recovery can be slower than during episodes of "pure" bipolar depression or "pure" mania or hypomania.
What Are the Risks of Mixed Features During Mood Episodes of Bipolar Disorder?
The most serious risk of mixed features during a manic or depressive episode is suicide. People with bipolar disorder are 10 to 20 times more likely to commit suicide than people without bipolar disorder. Tragically, as many as 10% to 15% of people with bipolar disorder eventually lose their lives to suicide.
Evidence shows that during episodes with mixed features, people may be at even higher risk for suicide than people in episodes of bipolar depression.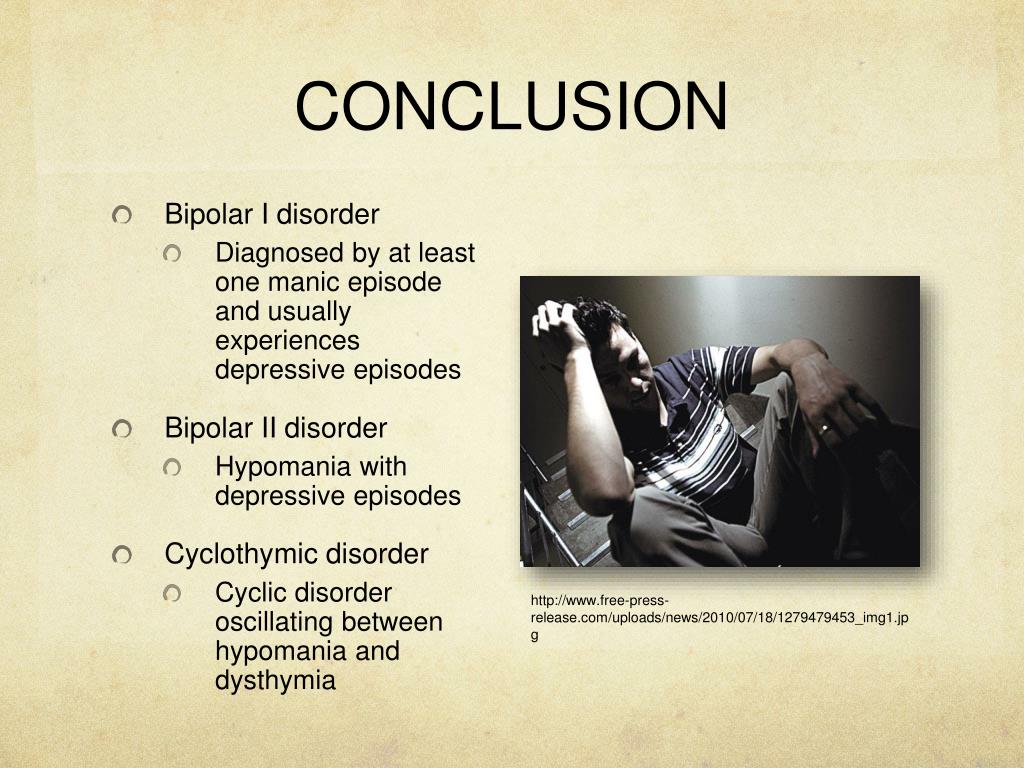
Treatment reduces the likelihood of serious depression and suicide. Lithium (Eskalith, Lithobid) in particular, taken long term, may help to reduce the risk of suicide.
People with bipolar disorder are also at higher risk for substance abuse. Nearly 60% of people with bipolar disorder abuse drugs or alcohol. Substance abuse is associated with more severe or poorly controlled bipolar disorder.
What Are the Treatments for Mood Episodes With Mixed Features in Bipolar Disorder?
Manic or depressive episodes with mixed features generally require treatment with medication. Unfortunately, such episodes are more difficult to control than an episode of pure mania or depression. The main drugs used to treat episodes with mixed features are mood stabilizers and antipsychotics.
Mood Stabilizers
While lithium is often considered a gold standard treatment for mania, it may be less effective when mania and depression occur simultaneously, as in a manic episode with mixed features. Lithium has been used for more than 60 years to treat bipolar disorder. It can take weeks to work fully, making it better for maintenance treatment than for acute manic episodes. Blood levels of lithium and other lab test results must be monitored to avoid side effects.
Lithium has been used for more than 60 years to treat bipolar disorder. It can take weeks to work fully, making it better for maintenance treatment than for acute manic episodes. Blood levels of lithium and other lab test results must be monitored to avoid side effects.
Valproic acid (Depakote) is an antiseizure medication that also levels out moods in bipolar disorder. It has a more rapid onset of action, and in some studies has been shown to be more effective than lithium for the treatment of manic episodes with mixed features.
Some other antiseizure drugs, such as and carbamazepine (Tegretol) and lamotrigine (Lamictal), are also effective mood stabilizers.
Antipsychotics
Many atypical antipsychotic drugs are effective FDA-approved treatments for manic episodes with mixed features. These includearipiprazole (Abilify), asenapine (Saphris), cariprazine (Vraylar), olanzapine (Zyprexa), quetiapine (Seroquel), risperidone (Risperdal), and ziprasidone (Geodon). Antipsychotic drugs are also sometimes used alone or in combination with mood stabilizers for preventive treatment.
Antipsychotic drugs are also sometimes used alone or in combination with mood stabilizers for preventive treatment.
Electroconvulsive Therapy (ECT)
Despite its frightening reputation, electroconvulsive therapy (ECT) is an effective treatment for any phase of bipolar disorder, including manic episodes with mixed features. ECT can be helpful if medication fails or can't be used.
Treatment for Depression in Mixed Bipolar Disorder
Common antidepressants such as fluoxetine (Prozac, Sarafem), paroxetine (Paxil), and sertraline (Zoloft) have been shown to worsen mania symptoms without necessarily improving depressive symptoms when depressive and manic symptoms occur together. Most experts therefore advise against using antidepressants during episodes with mixed features. Mood stabilizers (particularly Depakote), as well as atypical antipsychotic drugs, are considered the first-line treatments for mood episodes with mixed features.
Bipolar disorder usually involves recurrences of mixed, manic, or depressed phases of illness. Therefore, it is usually recommended that medications be continued in an ongoing fashion after an acute episode resolves in order to prevent relapses. This is sometimes called maintenance treatment.
Therefore, it is usually recommended that medications be continued in an ongoing fashion after an acute episode resolves in order to prevent relapses. This is sometimes called maintenance treatment.
Bipolar Disorder Guide
- Overview
- Symptoms & Types
- Treatment & Prevention
- Living & Support
What is Bipolar Disorder with Mixed Episodes?
When people are diagnosed with bipolar disorder, it’s because they are showing signs of experiencing manic episodes and depressive ones, swinging from one extreme to the other. No wonder the condition used to be called “manic depression.”
However, in some cases, people do experience symptoms of both mania and depression at the same time.
When that happens, it is commonly referred to as bipolar disorder with mixed features. The more you know about the causes, symptoms, and treatment options, the easier it will be to understand and follow your health care providers’ treatment plan for you.
What are Mixed Episodes in Bipolar Disorder?
“Mixed episodes in bipolar disorder occur when a patient exhibits symptoms of both depression and mania, or depression and hypomania (a milder form of mania) at the same time,” says Robert Bornstein of the Derner School of Psychology, a Division of Adelphi University in New York. “Although it may seem counterintuitive, some individuals actually experience symptoms of mania (for example, impulsivity, irritability, racing thoughts) at the same time as they experience an episode of depression. It is possible to feel sad and hopeless at the same time as one feels anxious, pressured, and full of energy.”
“Most people are in their teens or early 20s when they experience their first episode of bipolar disorder with mixed episodes,” Bornstein says. “Women and men are at equal risk. Having a relative who has experienced bipolar disorder is a risk factor as well, suggesting that one may be more likely to develop the disorder."
Bornstein says that overall, between 40% and 50% of people who are diagnosed with bipolar disorder experience mixed episodes at some point in their illness.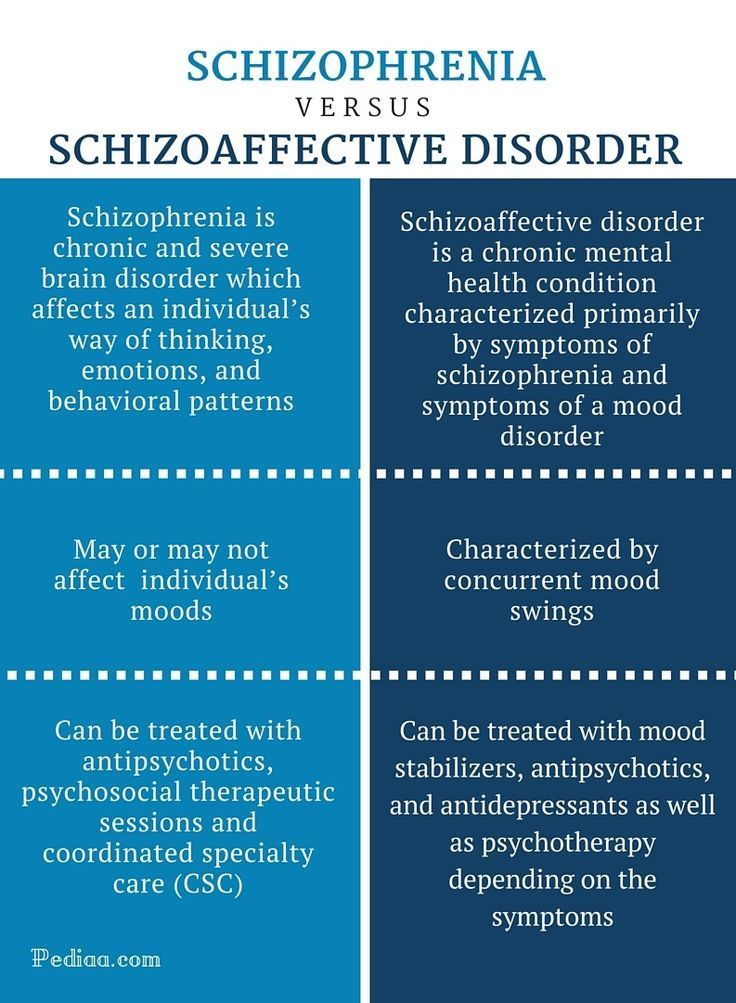
Symptoms of a Mixed Features Episode
Don’t confuse “depression” with being sad over having a bad day, or “mania” as being extremely happy because something great happened in your life. Every person will experience natural ups and downs on a daily basis, depending upon what is happening to them. That’s completely normal, and not a cause for alarm.
But people with bipolar disorder tend to feel as if they have endless and excessive energy when they are experiencing a manic state. During these times, people with bipolar disorder are in danger of making unwise decisions, acting impulsively, and in ways that are out of character.
Some specific signs and symptoms for a manic state include:
Feeling abnormally upbeat—described as “beyond a normal good or happy mood”
Racing thoughts–the overwhelming (and exhausting) feeling of thoughts that are bouncing around your head at rapid speed
Excessive talking–way beyond just being “chatty”
On edge–having so much energy you overreact to everything around you
Feeling as if you don’t need to sleep–the false belief that little or no sleep is needed right now
There are basically two types of mixed episodes in bipolar disorder. In one form, the patient is primarily depressed, but also has some symptoms of mania or hypomania. In the other form, the patient is primarily manic, but also experiences symptoms of depression.
In one form, the patient is primarily depressed, but also has some symptoms of mania or hypomania. In the other form, the patient is primarily manic, but also experiences symptoms of depression.
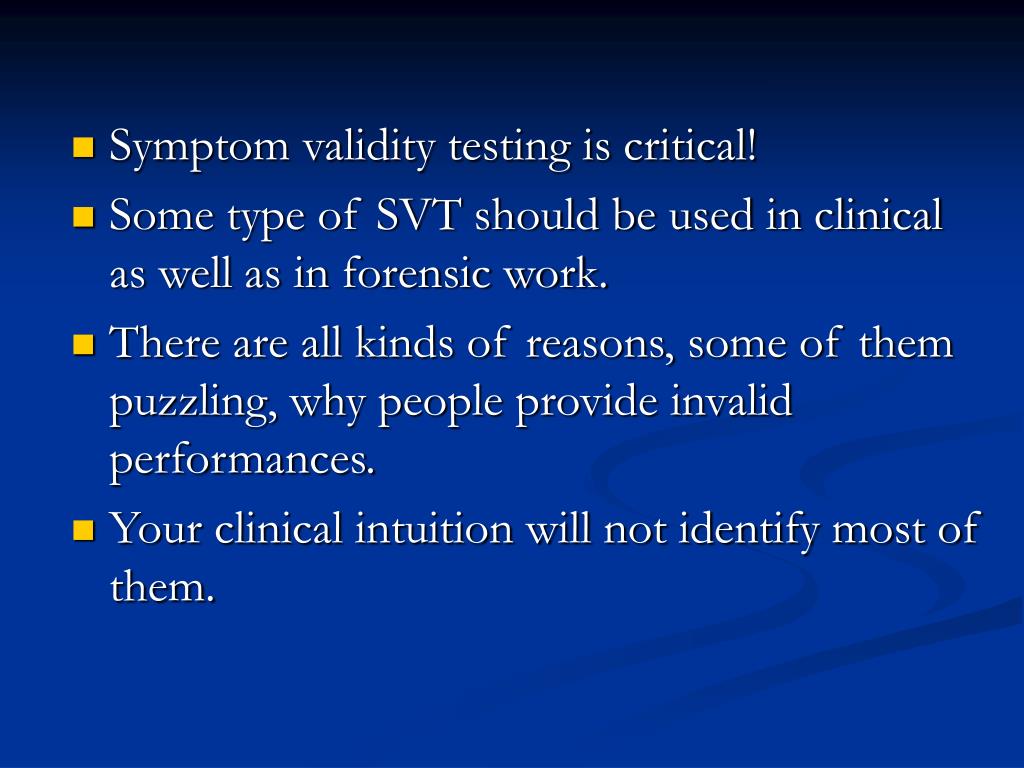
Diagnosis with Depression and Mania
“One of the issues that complicates diagnosis of bipolar disorder is that it frequently co-occurs with other psychological disorders,” Bornstein says. “When this happens the patient manifests symptoms of two or more disorders simultaneously, making it difficult for the diagnostician to separate the symptoms of the two co-occurring disorders.”
Among the disorders that frequently co-occur with bipolar disorder:
Substance use disorders
Anxiety disorders
Borderline personality disorder
Prevention of Bipolar with Mixed Episodes
While there is no known way of preventing a bipolar disorder with mixed episodes, when you work together with your mental health care team you can take positive action steps that will help you in your daily life and activities.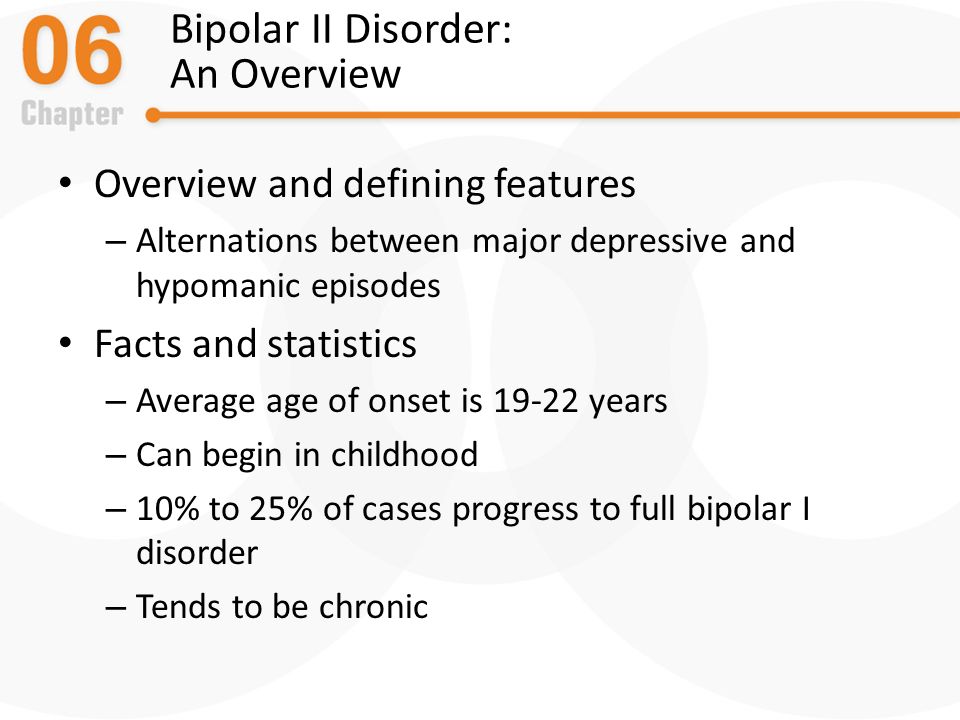
Here are some well-established ways to manage bipolar disorder symptoms overall:
Stick to a sleep schedule, getting up and going to sleep around the same times every day (and getting around 7-8 hours of good rest a night).
Limit caffeine and alcohol intake.
Minimize stress.
Follow a daily routine as best you can.
Get exercise daily or multiple times a week.
Stick to your medication plan, if you have one.
Keep track of your moods day to day and the things that cause mood changes. Do you feel better after 8 hours of sleep versus 9? Worse after eating processed or fast food? Jot it down.
And, know that even if you’re doing everything “right” to prevent episodes, they can still happen, and it isn’t your fault. Working with mental health professionals, caregivers, or a support group can help you learn coping skills or adjust medications to better deal with episodes.
Like with other disorders, psychiatrists and researchers are starting to recognize that bipolar can be thought of as a spectrum, not just a series of symptoms where you either check the box or you don’t.
Different people can experience bipolar in very different ways, whether that means the ratio of depressive cycles to manic ones, having mixed episodes, or the ways the symptoms manifest.
In adolescents, sussing out mixed states can be especially tricky. It's important to understand how mixed states may be manifesting in this population. Teenagers have described the experience as "making them feel like they are being torn apart from the inside". Emotional torture like this can put them at risk of self harm.³
Bipolar Mixed Episode Risks
A 2017 study found those with a history of bipolar disorder with mixed states were at higher risk of suicidal behavior, compared to those without a history of mixed states.¹
Treatment for Mood Episodes with Mixed Features
Medication is somewhat effective in managing bipolar disorder symptoms when they occur, and some psychological interventions (for example, stress reduction techniques) can be helpful in minimizing the frequency of bipolar disorder episodes, according to Bornstein.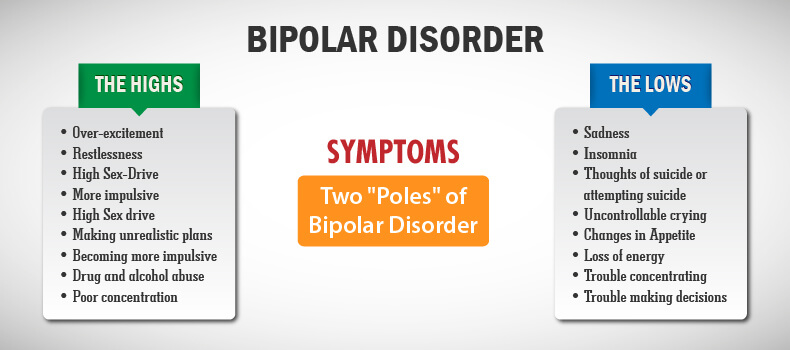
“One of the challenges confronting researchers in this area is developing better tools to predict who will develop bipolar disorder with mixed episodes,” he says. “Once our ability to predict the onset of the illness improves, our ability to develop effective prevention techniques will follow.”
Lithium as a mood stabilization drug has been successful as a medication for treating people with Bipolar 1 disorder. In recent years other medications have also been used to effectively treat bipolar disorders. Some of these include:
Other types of psychotherapy have also been helpful in treating bipolar issues. Some of these include:
Cognitive behavioral therapy (CBT): This type of treatment can be helpful in identifying and reframing unhealthy negative beliefs and behaviors.
Interpersonal and social rhythm therapy (IPSRT): This type of treatment will focus on helping a person stabilizing daily rhythms. Research has proven that a consistent daily routine in your eating, sleeping and even exercising habits goes a long way in helping to manage your moods.
 ²
²Family-focused therapy: When a person who has been diagnosed with a bipolar disorder has the support of their family and friends, it can help you stick with a treatment plan. It also helps your loved ones be aware of any warning signs of a bipolar episode.
Psychoeducation: When you take the time to learn everything there is to know about your own bipolar disorder journey, it does make a big difference. When you understand your own personal triggers and symptoms, it will help you create a plan of action to stay in control.
If you have been diagnosed with a bipolar disorder and are not sure what to do next, make sure you seek and follow the advice of a trusted mental health professional (especially ones that are familiar with all aspects of bipolar disorders). When you have a plan developed that works specifically for you, it can help you to feel more in control of your life.
What do bipolar mixed episodes feel like?
When someone experiences symptoms of mania (for example, impulsivity, irritability, racing thoughts) at the same time as they experience an episode of depression, it is possible to feel sad and hopeless at the same time as one feels anxious, pressured, and full of energy.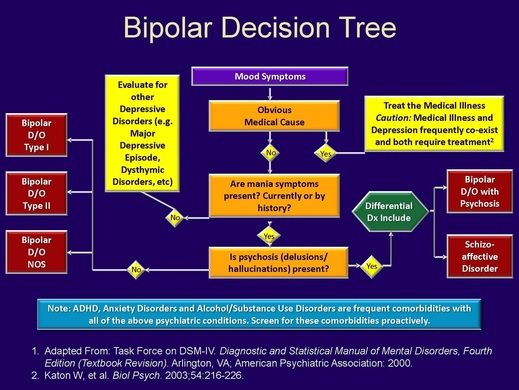 Or, it can feel like one minute you’re happy, excited, full of energy and ideas, and the next minute, wanting to cry.
Or, it can feel like one minute you’re happy, excited, full of energy and ideas, and the next minute, wanting to cry.
How long do bipolar mixed episodes last?
According to the National Institute of Mental Health, mixed bipolar episodes can last a week or two, or longer. The symptoms themselves last most of the day, every day, during these periods.
What is bipolar switching?
Bipolar switching is the term used to describe alternating between opposite states of mania and depression. It is the distinguishing characteristic of bipolar disorder, and this process in the brain is still not well understood.
What triggers bipolar cycles?
What triggers bipolar cycles will vary from person to person. It can be as simple as a stressful situation that doesn’t resolve itself in a timely fashion, to something as drastic as drug misuse, either with illegal substances, alcohol, or not taking your medications as prescribed. Other common triggers include not getting enough sleep and change of seasons.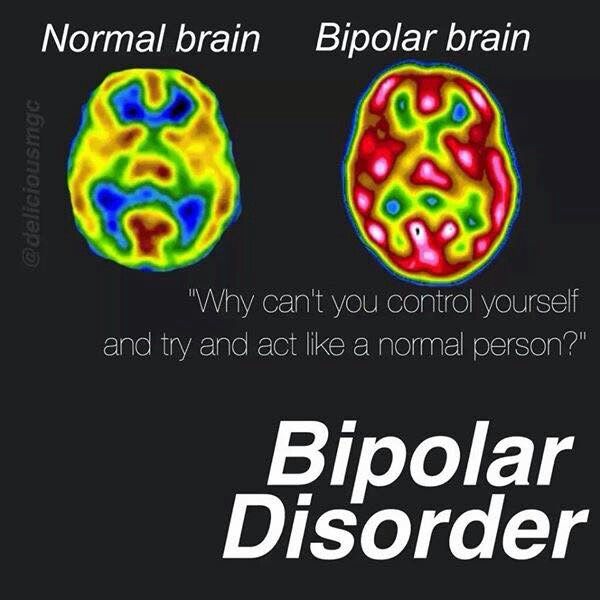
What does rapid cycling bipolar feel like?
When a person experiences a rapid cycling bipolar episode it is characterized by frequent mood swings. That type of an episode can include depression, mania, or hypomania, and usually happens within four or more incidents within a 12-month time frame. Mood changes can happen over days or hours. For most, this is temporary, but for some this pattern of cycling can continue indefinitely.
- Persons, JE, Coryell, WH, Solomon, DA, Keller, MB, Endicott, J, Fiedorowicz, JG. Mixed state and suicide: Is the effect of mixed state on suicidal behavior more than the sum of its parts?. Bipolar Disord. 2018; 20: 35– 41. https://doi.org/10.1111/bdi.12538
- Steardo, Luca Jr., et al. Efficacy of the interpersonal and social rhythm therapy (IPSRT) in patients with bipolar disorder: results from a real-world, controlled trial. Ann Gen Psychiatry. 2020; 19: 15. Published online 2020 Mar 9. doi: 10.1186/s12991-020-00266-7
- Psychiatric Times.
 How to Diagnose Mixed Features without Overdiagnosing Bipolar. Chris Aiken, MD. Published September 6, 2018. Available at https://www.psychiatrictimes.com/view/how-diagnose-mixed-features-without-over-diagnosing-bipolar. Accessed October 7, 2022.
How to Diagnose Mixed Features without Overdiagnosing Bipolar. Chris Aiken, MD. Published September 6, 2018. Available at https://www.psychiatrictimes.com/view/how-diagnose-mixed-features-without-over-diagnosing-bipolar. Accessed October 7, 2022.
Notes: This article was originally published August 8, 2022 and most recently updated August 25, 2022.
John Riddle
John is the author of 34 books, including several health and medical titles. His byline has appeared in major publications across the US, and he has written articles for over 200 websites.
Evolution of the concept of mixed states in the clinic of bipolar affective disorder
Mixed affective states are a controversial area of psychopathology. Along with mania and depression, they act as an independent phase of manic-depressive disorder [47], forming a family of separate forms of affective syndromes. Characterized by the introduction of depressive features into mania/hypomania or, conversely, manic into depression, mixed states are often not recognized by clinicians due to the polymorphism of symptoms and the lack of adequate diagnostic criteria.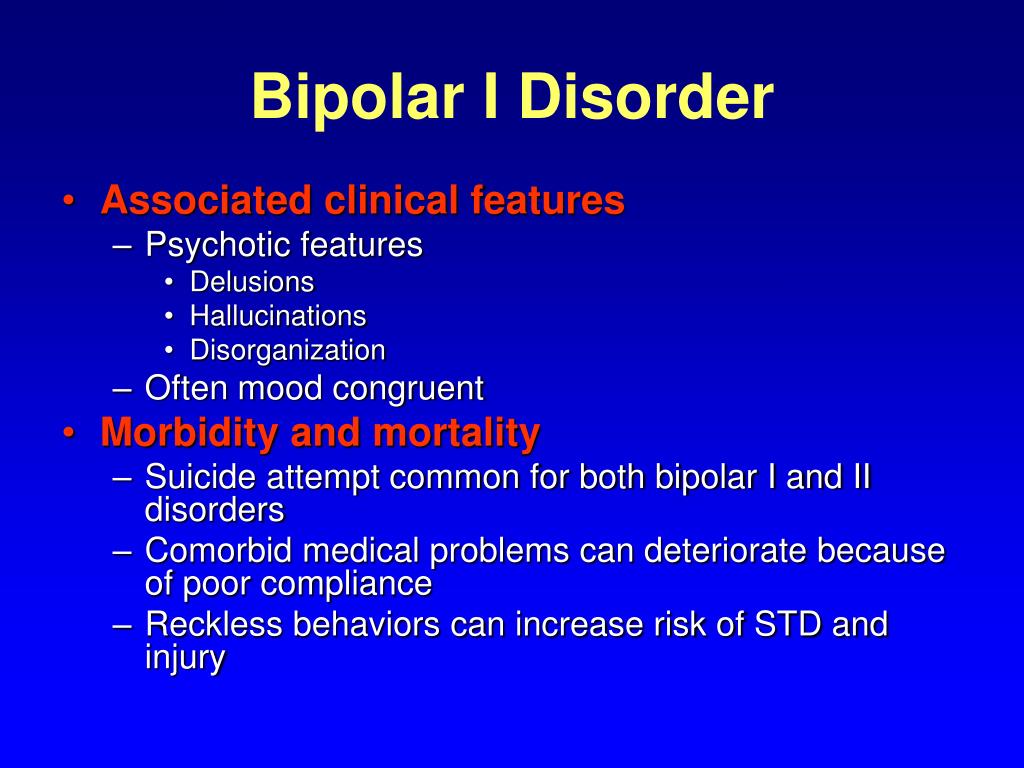
The history of the concept of mixed states had four stages: the stage of creation of the Kraepelinian concept of mixed states, which generalized all earlier indications of their existence; relative oblivion of the concept of mixed states; introduction into practice of their criteria within the framework of modern classifications of mental disorders; scientific search for new diagnostic criteria. For a deeper understanding of the essence of mixed states, each of them should be considered in more detail, prefaced by a description of the stage of prototypes of mixed states.
Mixed states prototype stage. As pointed out by A. Koukopoulos and A. Koukopoulos [54], the first mentions of conditions that could essentially be called mixed are found in Lorry, Boissier de Sauvages and Cullen in descriptions of individual variants of melancholia ( melancholia moria, melancholia enthusiastica and etc.).
In the classification of mental disorders proposed by J. Heinroth [51], states of exaltation and excitation (hyperthymia), depressed states (asthenia), mixed states of excitation and weakness (hypoasthenia) were distinguished. The last diagnostic category included "mixed emotional disorders" ( animi morbi complicati ), "mixed mental disorders" ( morbi mentis mixti ) and "mixed impulse disorders" ( morbi voluntatis mixti, athymia ). The first two groups correspond to modern definitions of mixed affective and schizoaffective disorders. The French psychiatrist J. Guislain [49] classified “grumpy depression”, “grumpy exaltation”, “depression with exaltation and recklessness”, and “depression with anxiety” as mixed states, while noting the long duration of episodes characteristic of the first type and an unfavorable prognosis. . In his opinion, "gloomy insanity precedes frenzy", and the transition from one state to another can be accomplished through numerous steps, representing a "mixture of mental disorders" in various combinations.
Heinroth [51], states of exaltation and excitation (hyperthymia), depressed states (asthenia), mixed states of excitation and weakness (hypoasthenia) were distinguished. The last diagnostic category included "mixed emotional disorders" ( animi morbi complicati ), "mixed mental disorders" ( morbi mentis mixti ) and "mixed impulse disorders" ( morbi voluntatis mixti, athymia ). The first two groups correspond to modern definitions of mixed affective and schizoaffective disorders. The French psychiatrist J. Guislain [49] classified “grumpy depression”, “grumpy exaltation”, “depression with exaltation and recklessness”, and “depression with anxiety” as mixed states, while noting the long duration of episodes characteristic of the first type and an unfavorable prognosis. . In his opinion, "gloomy insanity precedes frenzy", and the transition from one state to another can be accomplished through numerous steps, representing a "mixture of mental disorders" in various combinations. Similar descriptions can be found in J. Baillarger [25]. F. Richarz [72] used the term " melancholia agitans ". W. Griesinger [48] noted that depressive ideas and ideas of grandeur "do not necessarily exclude" each other, but can be observed simultaneously during the transition from one state to another, representing a "conglomerate of manic and depressive symptoms." The same opinion was shared by J. Falret [42], describing the period of “transition from excitation to depression” with the onset of a hard-to-characterize state formed by weakened excitation and beginning depression. Studying circular psychosis, R. Kraft-Ebing [57] singled out the phase of “indefinite symptoms, when excitement follows depression and vice versa”: in the transitional period, these states “merge” and one can observe the phenomenon when “temporary symptoms” appear in a depressive or manic picture. opposite state." In the group of "combined" psychoses, C. Wernicke [86] described "agitated melancholia" with characteristic features: intense anxiety, speech pressure and a jump in ideas.
Similar descriptions can be found in J. Baillarger [25]. F. Richarz [72] used the term " melancholia agitans ". W. Griesinger [48] noted that depressive ideas and ideas of grandeur "do not necessarily exclude" each other, but can be observed simultaneously during the transition from one state to another, representing a "conglomerate of manic and depressive symptoms." The same opinion was shared by J. Falret [42], describing the period of “transition from excitation to depression” with the onset of a hard-to-characterize state formed by weakened excitation and beginning depression. Studying circular psychosis, R. Kraft-Ebing [57] singled out the phase of “indefinite symptoms, when excitement follows depression and vice versa”: in the transitional period, these states “merge” and one can observe the phenomenon when “temporary symptoms” appear in a depressive or manic picture. opposite state." In the group of "combined" psychoses, C. Wernicke [86] described "agitated melancholia" with characteristic features: intense anxiety, speech pressure and a jump in ideas. According to him, "agitated melancholy" combined elements of depression and melancholy.
According to him, "agitated melancholy" combined elements of depression and melancholy.
Thus, already in the 19th century, most well-known psychiatrists noted the existence of mixed states, denoting in their first prototypical descriptions fundamentally different positions, considering these states as an independent form or as a stage of transition between opposite affective phases.
The period of conceptualization of mixed states. By the beginning of the 20th century, numerous indications of the existence of mixed states needed to be generalized and were conceptualized by E. Kraepelin and his student W. Weygandt [87]. The latter, working under the guidance of E. Kraepelin in the psychiatric clinic of the University of Hedelberg, drew attention to the frequency of the simultaneous appearance of symptoms of different poles of manic-depressive psychosis (in 20% of the “circular” patients he observed). In his first monograph on mixed states in psychiatric literature - "On mixed states in manic-depressive insanity" ("Uber die Mischzustande des Manisch-depressiven Irreseins") - he outlined the fundamental approaches to their diagnosis - a different combination of opposite manic and depressive symptoms from triads: elated mood, psychomotor agitation and a jump in ideas, on the one hand, and low mood, psychomotor and ideator retardation, on the other. According to the author, instability of mood, motility and thinking is a characteristic feature of manic-depressive (circular) psychosis. He also noted that in some cases, mixed symptoms determine the clinical picture of the entire episode, contributing to a more protracted course (weeks, months, and even years) than in pure manic or depressive states. W. Weygandt believed that with various combinations of symptoms of the manic and depressive triad, at least six variants of mixed states can occur for a short time. Avoiding speculativeness, he attached practical importance to only three of their types, which are more common in clinical practice and have the longest duration - "manic stupor", "agitated depression" and "unproductive mania".
According to the author, instability of mood, motility and thinking is a characteristic feature of manic-depressive (circular) psychosis. He also noted that in some cases, mixed symptoms determine the clinical picture of the entire episode, contributing to a more protracted course (weeks, months, and even years) than in pure manic or depressive states. W. Weygandt believed that with various combinations of symptoms of the manic and depressive triad, at least six variants of mixed states can occur for a short time. Avoiding speculativeness, he attached practical importance to only three of their types, which are more common in clinical practice and have the longest duration - "manic stupor", "agitated depression" and "unproductive mania".
According to P. Salvatore [75], the works of W. Weygandt were a powerful impetus to the creation of Kraepelin's concept of manic-depressive psychosis, which was finally published in the 8th edition of his manual [55]. In this work, E. Kraepelin developed the concept of mixed states (Mischzustande) with a circular form of periodic insanity, pointing to the “internal relationship of seemingly opposite states”, in which there is a multidirectionality of the three components of an affective state - thinking, motor activity and mood itself. Singling out six mixed states (see table) , he believed that depressive or anxious mania (depressive oder ängsliche Manie), excited depression (erregte Depression), mania with scarcity of thoughts (ideenarme Manie) are based on three fundamental symptoms of mania (high euphoric mood, jump ideas, hyperactivity), while manic stupor (manischer Stupor), depression with a flight of thoughts (ideenfluchtige Depression), inhibited mania (gehemmte Manie) - on the fundamental symptomatology of depression ("ideational weakness", "depressed mood", "decreased motivation "). Analyzing the stereotype of the development of mixed states, E. Kraepelin singled out the transient form as a stage of transition from depression to mania or vice versa and an independent form characterized by a tendency to a protracted course.
Singling out six mixed states (see table) , he believed that depressive or anxious mania (depressive oder ängsliche Manie), excited depression (erregte Depression), mania with scarcity of thoughts (ideenarme Manie) are based on three fundamental symptoms of mania (high euphoric mood, jump ideas, hyperactivity), while manic stupor (manischer Stupor), depression with a flight of thoughts (ideenfluchtige Depression), inhibited mania (gehemmte Manie) - on the fundamental symptomatology of depression ("ideational weakness", "depressed mood", "decreased motivation "). Analyzing the stereotype of the development of mixed states, E. Kraepelin singled out the transient form as a stage of transition from depression to mania or vice versa and an independent form characterized by a tendency to a protracted course.
E. Kraepelin's concept had many supporters.
E. Bleuler [36] emphasized the importance of "such a quality of manic-depressive psychosis as confusion", reflecting, in his opinion, the possibility of a diverse combination of symptoms.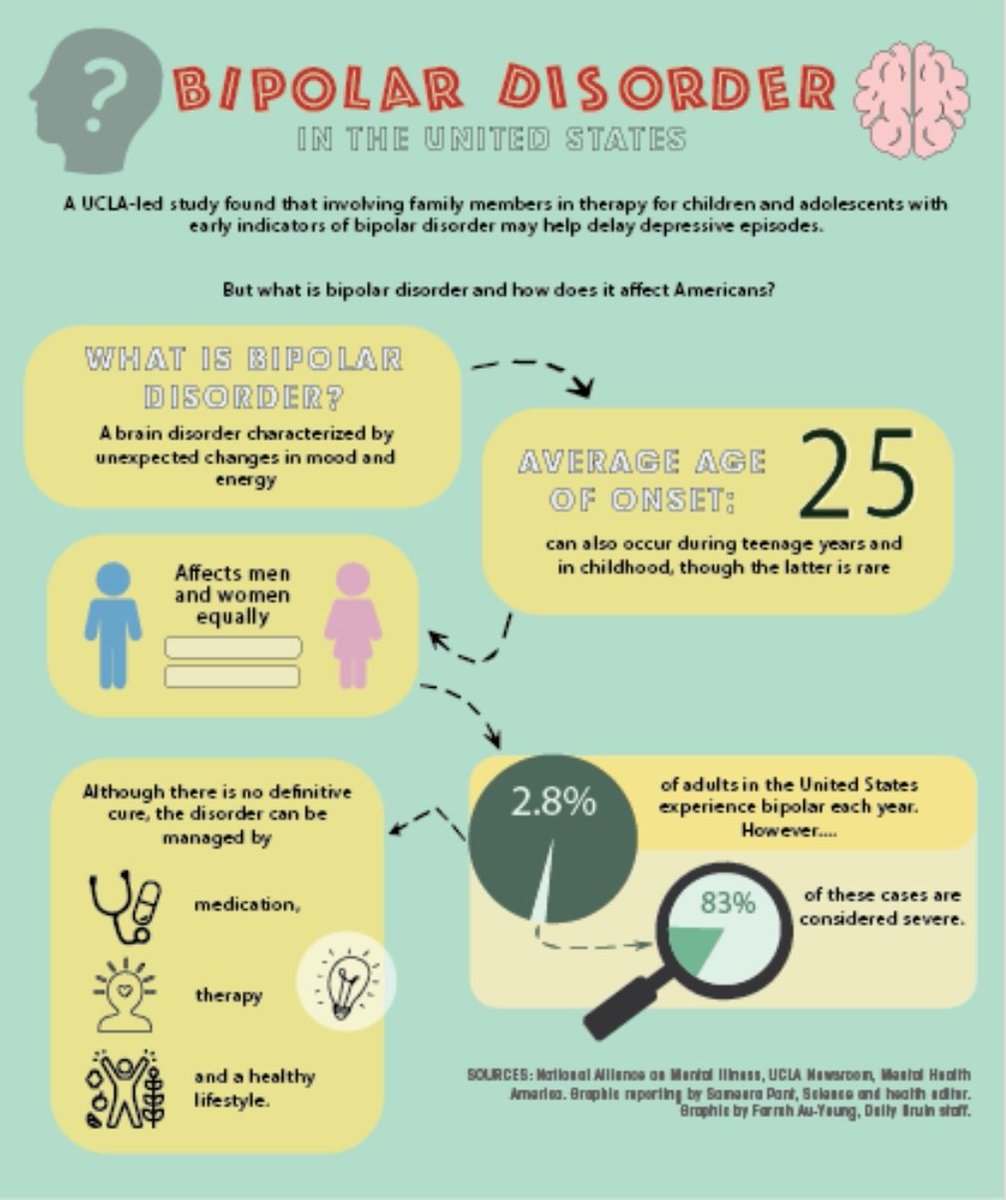 K. Leonhard [59] believed that the allocation of mixed states indicates the potential properties of manic-depressive psychosis "to involve the characteristics of the opposite affective pole." However, other opinions were also expressed.
K. Leonhard [59] believed that the allocation of mixed states indicates the potential properties of manic-depressive psychosis "to involve the characteristics of the opposite affective pole." However, other opinions were also expressed.
In particular, K. Jaspers [52] and K. Schneider [77], questioning the independent significance of mixed states, considered it unlawful to “break” manic-depressive disorders into affective, intellectual and cognitive components. In their opinion, mixed states are nothing more than a change from a manic state to a depressive state and vice versa.
In parallel with E. Kraepelin, other researchers also worked on the issue of mixed states. O. Rehm [71], using the term "mixed affect" and separating "speech" and "general motor skills" from the psychomotor component of the affective state, proposed a more complex typification of mixed states. A different classification principle was proposed by E. Stransky [81], who divided mixed states depending on the nature of the predominant affect (manic and depressive types of mixed states), as well as taking into account the mechanisms of their formation (simultaneous and successive variants).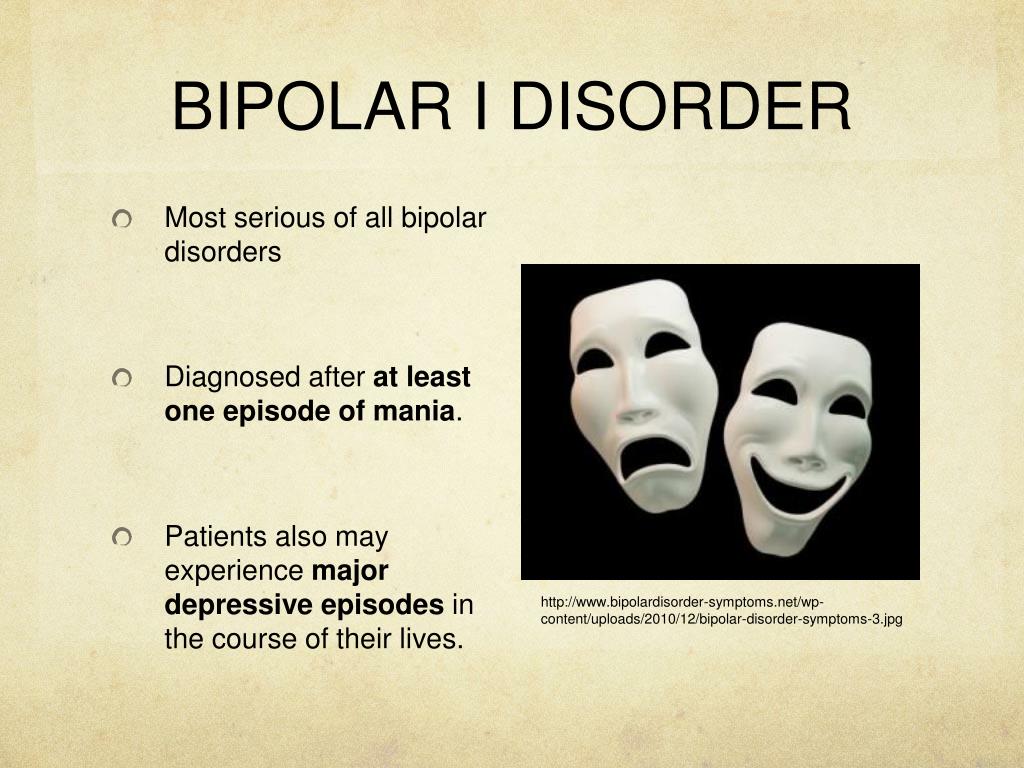 At the same time, simultaneous mixed states were characterized by the simultaneous coexistence of individual signs of an affect of different polarity, and successive ones were characterized by a successive change of individual components of different polarity in the structure of one phase.
At the same time, simultaneous mixed states were characterized by the simultaneous coexistence of individual signs of an affect of different polarity, and successive ones were characterized by a successive change of individual components of different polarity in the structure of one phase.
In domestic psychiatry of the beginning of the 20th century, works devoted to mixed states are relatively few in number. Mixed states were mentioned by P.B. Gannushkin, S.A. Sukhanov [3], V.P. Serbian [11, 12], A.N. Bernstein [1], Yu.V. Kannabih [6], E.S. Lokshin [8]. A particularly detailed study of mixed states was carried out by S.A. Sukhanov [13]. The author noted that mixed states appear at more distant stages of the disease as a "further evolution of manic-depressive psychosis" after the stage of alternation of typical manic and depressive phases.
The middle of the 20th century became a period of relative oblivion for mixed fortunes . Nevertheless, in a few publications of foreign psychiatrists (K. Kleist [56], G. Ewald [41], J. Rouart [74], M. Fischetti [44], J. Lange [58], J. Campbell [37] ) you can find indications of the importance of identifying mixed conditions, which, combining the symptoms of different affective poles, thereby reflect the commonality of a single cyclothymic process with the possibility of developing any of these forms in a particular patient.
Kleist [56], G. Ewald [41], J. Rouart [74], M. Fischetti [44], J. Lange [58], J. Campbell [37] ) you can find indications of the importance of identifying mixed conditions, which, combining the symptoms of different affective poles, thereby reflect the commonality of a single cyclothymic process with the possibility of developing any of these forms in a particular patient.
During this period, in domestic psychiatry, with some delay, active disputes continued about the validity of E. Kraepelin's ideas in relation to these conditions. One of the followers of the Kraepelinian model of mixed states in the Russian psychiatric school, V.A. Gilyarovsky [4] pointed out that "in addition to pure states of excitation or depression, mixed patterns are observed, characterized by a longer course and an unfavorable prognosis." The author believed that out of nine theoretically possible combinations of excitation and oppression in three areas of mental activity (emotional, intellectual and volitional), the real value among mixed states with an emphasis on the manic component is angry mania, with an emphasis on the depressive - agitated melancholia. Opposite views were expressed by V.M. Bekhterev [2], pointing out the inconclusive evidence for the existence of mixed or transient manic-melancholic states.
Opposite views were expressed by V.M. Bekhterev [2], pointing out the inconclusive evidence for the existence of mixed or transient manic-melancholic states.
Stage of introduction of criteria within the framework of modern classifications of mental disorders. Subsequently, in the wake of the consequences of the psychopharmacological "revolution" in the works of a number of researchers [22, 68, 88], a revival of interest in mixed states began, which was characterized by two features: on the one hand, confirmation of the previously formulated provisions regarding this concept, on the other hand, dissatisfaction with the accumulated by that time, ideas about the structure of mixed states as a simple combination of polar symptoms. Deepening knowledge about the dependence of the psychopathological structure of mixed affective syndromes on syndromokinesis, S. Mentzos [66] proposed to distinguish between stable and unstable mixed states. The clinical picture of stable mixed states is represented by a synchronous combination of symptoms of depression and mania and is characterized by the replacement of one or more elements of mania (hypomania) by signs of depression and vice versa (for example, agitation in depression or lethargy in a manic state).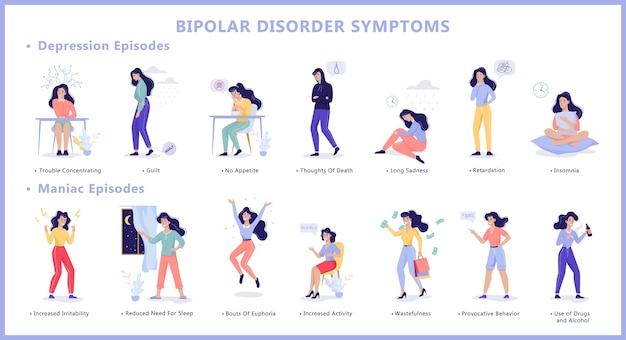 So, during the period of the greatest severity of affective disorders, anxiety can be accompanied by motor restlessness (patients are tense, cannot find a place for themselves, can neither sit nor lie down) and speech excitation with groans, lamentations, anxious verbigeration - repeated monotonous repetition of monotonous short phrases and expressions ( agitated depression). Unstable mixed states are formed during the rapid change of polar affective phases within the "short cycle". At the same time, depressive and manic manifestations overlap in various, sometimes very chaotic combinations. Their psychopathological structure, in contrast to "pure" depression and hypomania, is determined by a large polymorphism; the variety of manifestations is associated both with the formation of general symptoms (irritability, anxiety, ideomotor restlessness, internal tension, impaired concentration, insomnia), and the addition of psychopathological disorders of other registers (obsessive-compulsive, panic attacks, depersonalization).
So, during the period of the greatest severity of affective disorders, anxiety can be accompanied by motor restlessness (patients are tense, cannot find a place for themselves, can neither sit nor lie down) and speech excitation with groans, lamentations, anxious verbigeration - repeated monotonous repetition of monotonous short phrases and expressions ( agitated depression). Unstable mixed states are formed during the rapid change of polar affective phases within the "short cycle". At the same time, depressive and manic manifestations overlap in various, sometimes very chaotic combinations. Their psychopathological structure, in contrast to "pure" depression and hypomania, is determined by a large polymorphism; the variety of manifestations is associated both with the formation of general symptoms (irritability, anxiety, ideomotor restlessness, internal tension, impaired concentration, insomnia), and the addition of psychopathological disorders of other registers (obsessive-compulsive, panic attacks, depersonalization). Such unstable mixed states were described in the domestic literature [7] under the term “atypical”, often associated with the consequences of the use of antidepressants.
Such unstable mixed states were described in the domestic literature [7] under the term “atypical”, often associated with the consequences of the use of antidepressants.
T.F. put another meaning into the term "atypical mixed states". Papadopoulos [10]. Noting the relative clarity in terms of the psychopathological structure of the periods of "mixed affect" during the transition from one phase to another, he singled out true mixed states that require special analysis within the atypical phases of not only circular, but also affective psychoses in a broader sense. The author suggested considering the "atypia" of individual phases of manic-depressive psychosis, taking into account the premorbid personality and age of patients.
Yu.L. Nuller and I.N. Mikhalenko [9] to the assumption that the typology of mixed states proposed by E. Kraepelin is limited.
Uniformity in the diagnosis of mixed states began with the creation in the 80s of unified criteria for assessing mental disorders - Research Diagnostic Criteria (RDC) [78, 79] and the DSM-III-R classification [20].
In the RDC, two variants of mixed states were distinguished: when depressive and manic syndromes were presented simultaneously during one episode and when they followed one after the other without interruption. RDC criteria were partly incorporated into the DSM-III-R classification, which provided a rather vague description of the category "bipolar disorder - mixed". Its diagnosis required the presence of a complete symptomatological picture of a manic and major depressive episode, coexisting simultaneously or rapidly replacing each other every few days. At the same time, depressive symptoms had to be sufficiently pronounced and persist at least throughout the day. The advent of the DSM-III-R did not add clarity to the diagnosis of mixed conditions. As noted by G. Perugi et al. [69], such criteria ruled out the possibility of the presence of individual competing symptoms of opposite polarity, which led to an underdiagnosis of mixed conditions.
A more specific definition of a "mixed episode" was given in DSM-IV [21]. Its diagnosis required meeting the criteria for both manic and major depressive episodes almost every day for at least 1 week. Thus, the category of mixed episodes did not include unstable forms characterized by a successive change of manic and depressive symptoms, which were classified under the heading specifier “rapid cyclicity”.
Its diagnosis required meeting the criteria for both manic and major depressive episodes almost every day for at least 1 week. Thus, the category of mixed episodes did not include unstable forms characterized by a successive change of manic and depressive symptoms, which were classified under the heading specifier “rapid cyclicity”.
In this regard, the criteria of the modern American classification correspond only to stable forms of mixed conditions.
The DSM-IV criteria for mixed states have also been criticized as narrow, restrictive, and inconsistent with clinical reality [17, 26, 65, 69, 83], primarily due to the high prevalence of non-syndromic symptoms of the opposite polarity. Thus, F. Benazzi [27] cites data that the formation of complete syndromic hypomania in patients with a major depressive episode was observed in 2.8% of cases, while in the presence of individual hypomanic symptoms - in 28.5%.
In accordance with the results of the study by F.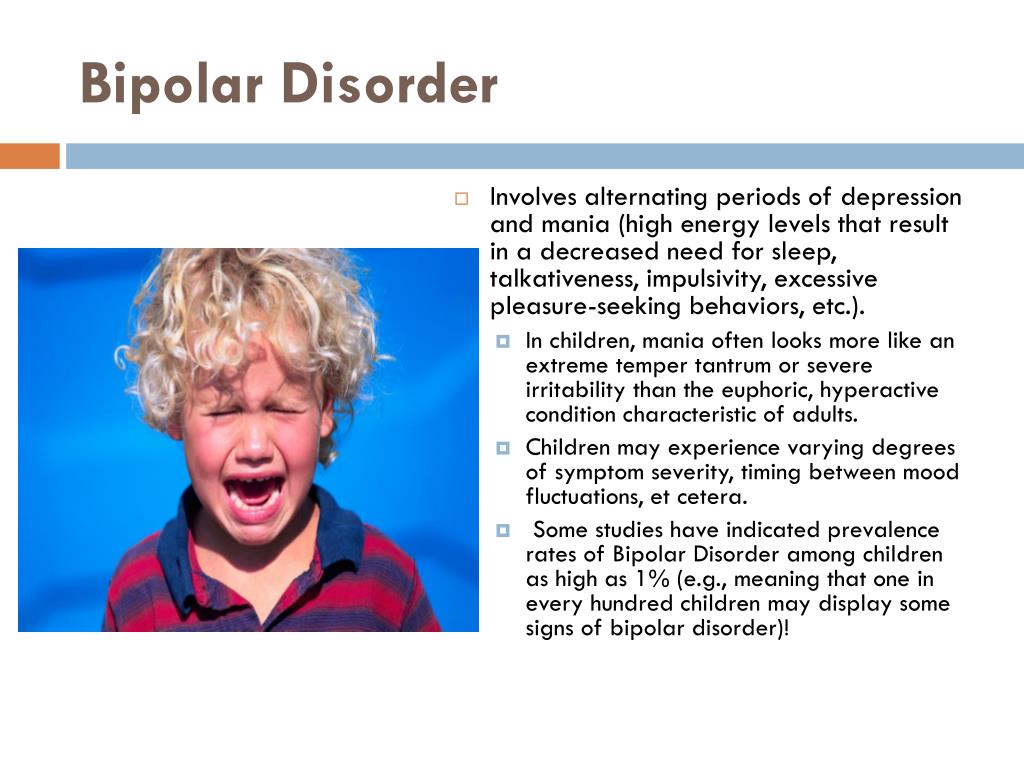 Benazzi, H. Akiskal [29], 48.7% of patients with major depression as part of bipolar affective disorder type II (BAD II) had three or more competing hypomanic symptoms coexisting.
Benazzi, H. Akiskal [29], 48.7% of patients with major depression as part of bipolar affective disorder type II (BAD II) had three or more competing hypomanic symptoms coexisting.
The ICD-10 [89] defines a mixed episode as “an affective episode lasting at least 2 weeks and characterized by either a mixture or a rapid alternation (often within hours) of hypomanic, manic and depressive symptoms.” Both sets of symptoms must be "significantly pronounced during most of the current episode of the disease." It further clarifies that "depressive mood is often accompanied for days or weeks by hyperactivity and the pressure of speech, and a manic state with grandiosity - agitation and loss of energy and libido." Thus, the ICD-10, compared to DSM-IV, offers less restrictive criteria for mixed states, requiring only "pronounced" manic or hypomanic and depressive symptoms, but not full syndromes, and explicitly embraces ultradian cyclicity. Moreover, unlike the DSM-IV, the description of the ICD-10 recognizes the existence of mixed depression and mania.
Search for new diagnostic criteria. In recent decades, the concept of mixed states has received increasing attention in light of the increasing interest in the problem of bipolar disorders (especially type II). Research is directed, on the one hand, to the search for new, more realistic diagnostic criteria, and, on the other hand, to clarify the phenomenology of mixed states.
During the search for new diagnostic criteria for a mixed state, evidence has been accumulated for the sufficiency of verification of several competing contrapolar symptoms for the diagnosis of subsyndromal depression in the structure of syndromic mania [63, 69] or subsyndromal mania in the structure of syndromic depression [15, 53, 69]. At the same time, the discussions concerned the question of the number of these contrapolar symptoms that are optimally sufficient for the diagnosis of a mixed state: S. McElroy et al. [63] proposed to consider more than three depressive symptoms in the structure of mania in this vein, H.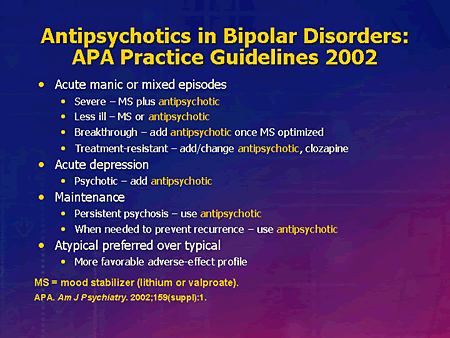 Akiskal et al. [17] - more than two, and A. Swann et al. [83] - more than one, which predetermined the expansion of the concept of mixed states.
Akiskal et al. [17] - more than two, and A. Swann et al. [83] - more than one, which predetermined the expansion of the concept of mixed states.
Alternative criteria for mixed states proposed at that time (three of the best known - Cincinnati [63], Vienna [32-34], Pisan [69]) were not sufficiently valid and did not provide the same diagnostic accuracy when compared with each other and with DSM-IV-TR and ICD-10 diagnostic criteria [50]. Thus, mixed mania, detected by clinical assessment in 23.2% of patients with BAD I, could be diagnosed using Cincinnati criteria in 16.7% of cases, and DSM-IV-TR and ICD-10 criteria - only in 12.9 and 9% of cases, respectively [85].
H. Akiskal [14-16, 18] expanded the interpretation of mixed states by including signs that appear as part of the manifestation of an affective episode based on temperament of the opposite polarity (hyperthymic, depressive, cyclothymic, irritable and anxious).
The concept of the bipolar spectrum, which has numerous supporters, also has a certain influence on the formation of new views on mixed states.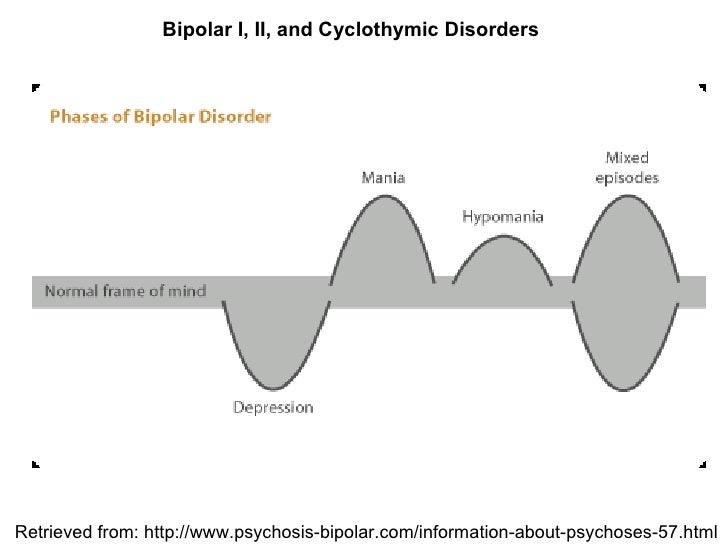 S. McElroy [65], considering mixed bipolar episodes in relation to their belonging to the bipolar spectrum, indicates the possibility of countless variants of combinations of different severity of manic and depressive symptoms. In its extreme form, the dimensional approach was presented by A. Swann et al. [82], who proposed to consider mixed states in the form of a continuum of various combinations of manic and depressive manifestations, including not only Kraepelinian subtypes, but also many of their transitional forms.
S. McElroy [65], considering mixed bipolar episodes in relation to their belonging to the bipolar spectrum, indicates the possibility of countless variants of combinations of different severity of manic and depressive symptoms. In its extreme form, the dimensional approach was presented by A. Swann et al. [82], who proposed to consider mixed states in the form of a continuum of various combinations of manic and depressive manifestations, including not only Kraepelinian subtypes, but also many of their transitional forms.
Recent research is moving away from categorical positions towards a dimensional study of the individual symptoms of mania and depression involved in the formation of mixed states in order to identify underlying symptomatic clusters that determine response to therapy and prognosis.
The need to develop a modern phenomenology of mixed states forced researchers to turn again to the Kraepelin typology when describing the most common variants of mixed states - dysphoric mania [49, 63, 70] and agitated depression [15, 30, 31, 53, 61].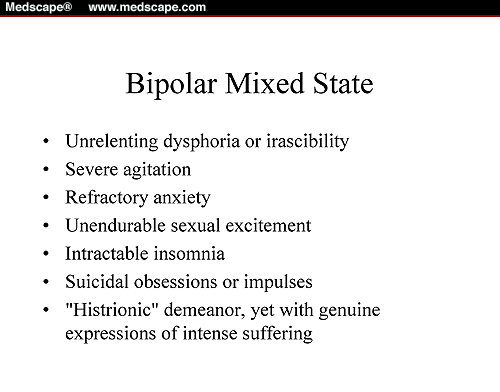 F. Cassidy [38] and T. Sato [76] confirm the validity of the subtype of mania with severe symptoms of dysphoria, corresponding to Kraepelin's "anxiety-depressive mania". N. Akiskal and F. Benazzi [19], considering mixed depression as a combination of a complete depressive syndrome and three competing hypomanic symptoms, also indicate the existence of two subtypes corresponding to Kraepelin's "depression with a leap of ideas" and "agitated depression".
F. Cassidy [38] and T. Sato [76] confirm the validity of the subtype of mania with severe symptoms of dysphoria, corresponding to Kraepelin's "anxiety-depressive mania". N. Akiskal and F. Benazzi [19], considering mixed depression as a combination of a complete depressive syndrome and three competing hypomanic symptoms, also indicate the existence of two subtypes corresponding to Kraepelin's "depression with a leap of ideas" and "agitated depression".
To the most common manic symptoms in the structure of a depressive episode in BAD I and II J. Goldberg et al. [46] refer to distractibility, ideational acceleration, agitation, and C. Pae et al. [67] - jump of ideas, increased distractibility, irritability, of which the latter, according to the authors, seems to be the main predictor of response to antipsychotic therapy. Symptoms of anxiety and dysphoria, which are related to the nuclear symptoms of mixed mania [35, 40], are attracting more and more attention from researchers.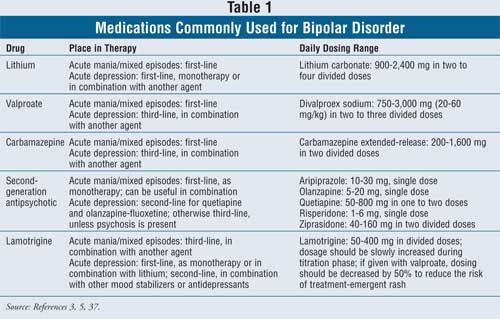 At the same time, dysphoria is considered as a special component of the affective syndrome, which correlates with irritability, increased sensitivity to external physical influences, impulsivity, and a sense of internal tension. F. Cassidy [40], based on the results of a factor analysis of a large sample of bipolar patients with mania, indicates that anxiety is an extremely common symptom of states corresponding to Kraepelin's "anxiety-depressive mania", and proposes to include it in the criteria for mixed states. A comparable level of anxiety in a comparative study of agitated depression and mixed mania by A. Swann [82] also confirms its inherent belonging to a mixed bipolar phenomenology.
At the same time, dysphoria is considered as a special component of the affective syndrome, which correlates with irritability, increased sensitivity to external physical influences, impulsivity, and a sense of internal tension. F. Cassidy [40], based on the results of a factor analysis of a large sample of bipolar patients with mania, indicates that anxiety is an extremely common symptom of states corresponding to Kraepelin's "anxiety-depressive mania", and proposes to include it in the criteria for mixed states. A comparable level of anxiety in a comparative study of agitated depression and mixed mania by A. Swann [82] also confirms its inherent belonging to a mixed bipolar phenomenology.
Factor analysis of individual symptoms of a mixed state showed that the predominance of manic or depressive symptoms in them already leads to heterogeneity in terms of subsequent dynamics, response to treatment and prognosis. Thus, according to the observations of J. Azorin [24], mixed states with a predominance of depressive symptoms are characterized by a lower probability of relapses compared with mixed states with a predominance of manic symptoms; the former often turn into depression, the latter into mania.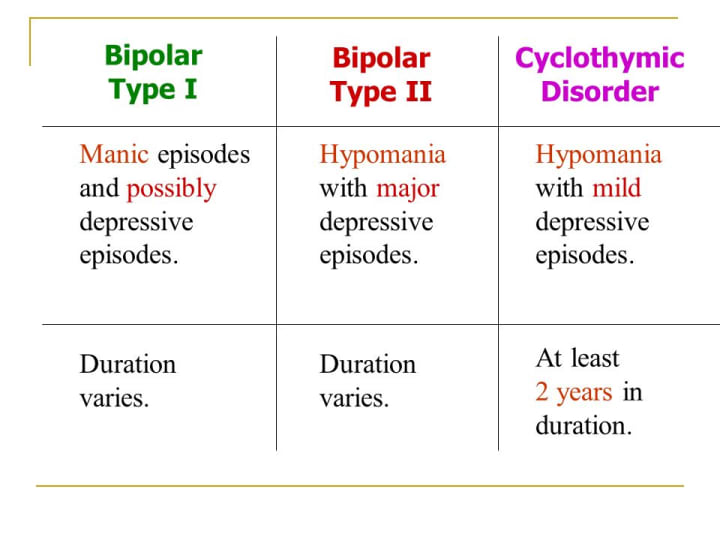
Further perspectives. The proposed DSM-V classification criteria published to date demonstrate the intention of its developers to bring the controversy of recent years to a common denominator and continue the clearly emerging trend towards expanding the criteria for mixed conditions by reducing the number of symptoms of the opposite affect, sufficient for its diagnosis. Presumably, the DSM-V will be different from the DSM-IV: the category "mixed episode" will disappear altogether and instead the specifier "with mixed features" will be introduced, applicable to the diagnosis of both depression and mania if at least three symptoms are present. opposite polarity. The latter comes from the already mentioned data confirming that distinct differences between "pure" and "mixed" mania/hypomania or major depression appear when the number of contrapolar symptoms reaches at least three (cited in [84]). The list of counterpolar symptoms will be excluded from those occurring in both mania and depression: psychomotor agitation, irritability, insomnia (to be distinguished from a decrease in the need for sleep), increased distractibility and loss of appetite.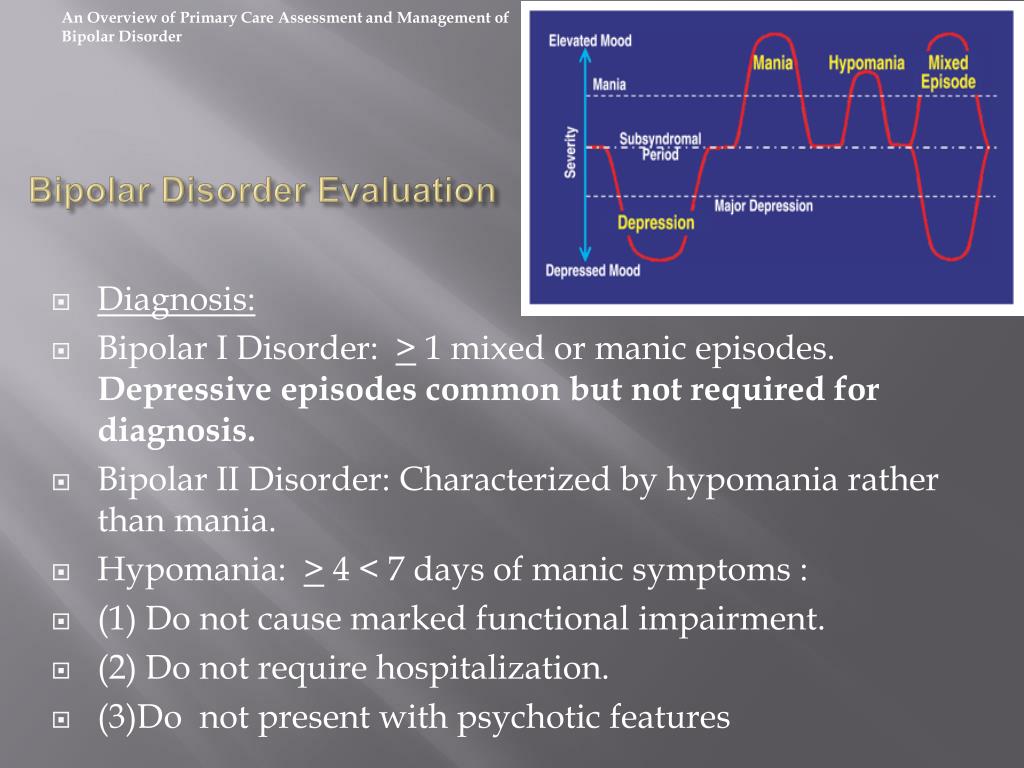
Thus, the proposed definition of mania/hypomania "with features of confusion" in the DSM-V requires that the criteria for a manic or hypomanic episode be fully met and that at least three of the following symptoms be present almost every day during the episode: severe dysphoria or depressed mood, decreased interest or pleasure in almost all activities, psychomotor retardation, fatigue or loss of energy, feelings of inadequacy and excessive or unjustified guilt, recurring thoughts of death or a suicide attempt or suicide planning. The proposed definition of a major depressive episode "with features of confusion" requires meeting the criteria for a major depressive episode and having at least three of the symptoms presented almost every day during the episode: high or expansive mood, high self-esteem, or grandiosity, unusual talkativeness, or verbal rush, racing of ideas, or subjective feeling of speeding up thoughts, increased energy, purposeful activity, involvement in activities with a high risk of unpleasant consequences, reduced need for sleep.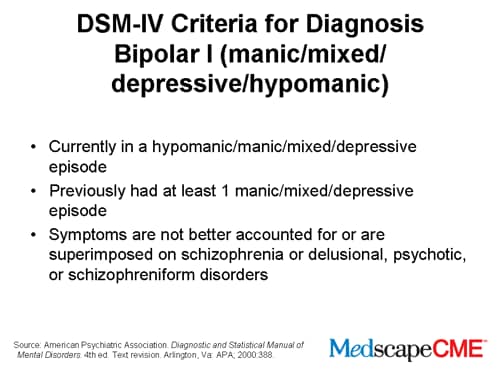
In addition, the use of the specifier “with mixed traits” for manic, hypomanic and depressive episodes would mean that mixed states are included not only in the circle of BAD I and II, but also in the depressive episode. Thus, the application of this criterion will mean that the diagnosis of major depression "with features of confusion" will not indicate the phenomena of bipolarity. Thus, a patient with three typical manic competing symptoms (eg, high spirits, high self-esteem or grandiosity, excessive involvement in activities with a high risk of adverse consequences) in the structure of a major depressive episode can be classified as unipolar.
The definition of mania/hypomania “with features of confusion” is consistent with available research data and operational criteria reported earlier in the literature [65] and is not likely to change. On the contrary, the definition of major depression "with features of mixed depression" is likely to be debatable, since it includes typical manic symptoms, such as elation and grandiosity, which are rare in patients with mixed depressions, while among the excluded symptoms are those often observed in them.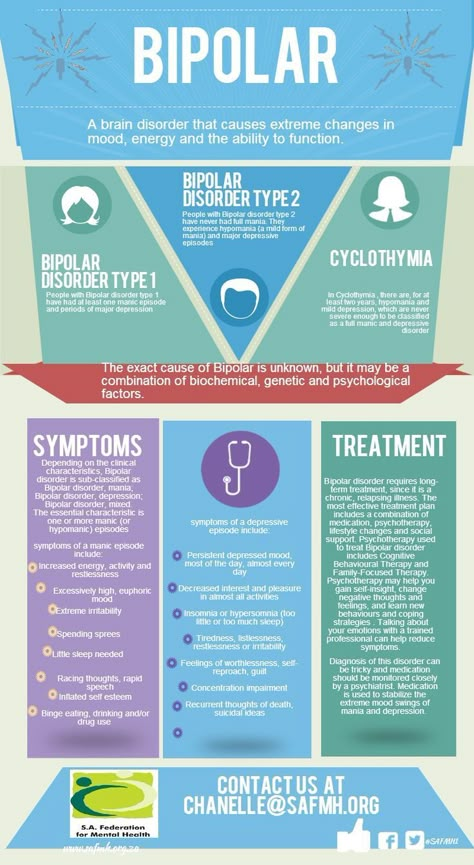 - irritability, psychomotor agitation and distractibility [46, 60]. It is important to note that the putative criteria for the "mixed-feature" specifier in DSM-V, like the criteria for "mixed episode" in DSM-IV, do not include ultradian cyclicity, which may be the subject of further research.
- irritability, psychomotor agitation and distractibility [46, 60]. It is important to note that the putative criteria for the "mixed-feature" specifier in DSM-V, like the criteria for "mixed episode" in DSM-IV, do not include ultradian cyclicity, which may be the subject of further research.
As for the forthcoming edition of ICD-11, the same difficulties may arise before its creators. If the data on insufficient effectiveness and an increased risk of affect reversal against the background of the use of antidepressants in mixed depression are not generally recognized as sufficiently convincing [43], then all researchers emphasize a higher suicidal risk among patients with mixed states [45, 73, 80]. Moreover, mixed states belong to those clarifying diagnostic categories that significantly affect the choice of therapeutic tactics, requiring the use of specific approaches.
From the point of view of the practical orientation of modern classifications, all this justifies the need to use new criteria for the diagnosis of mixed conditions.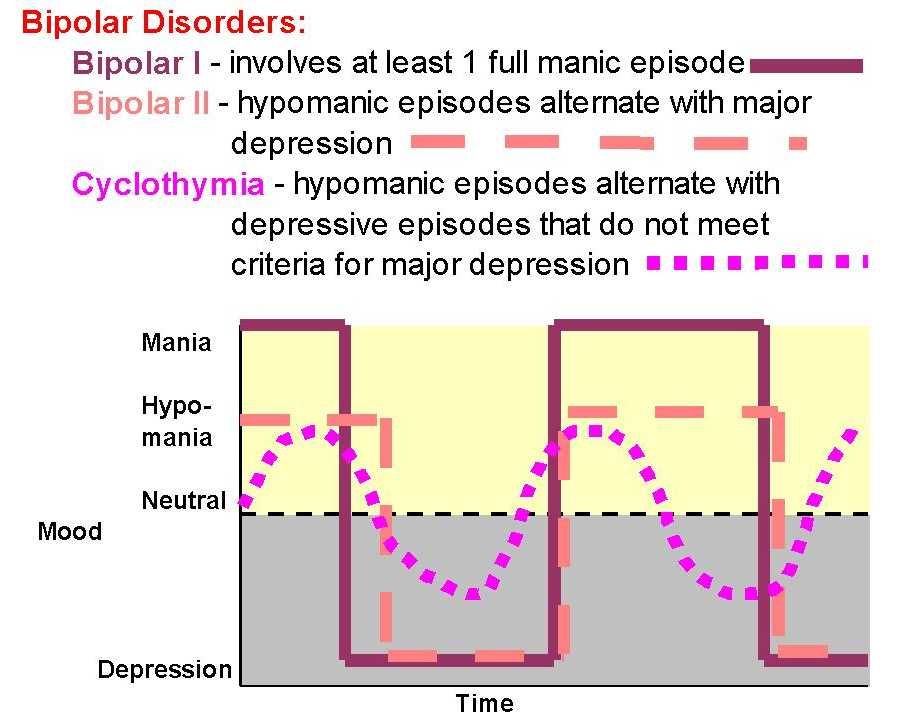
Thus, the definition of mixed states over more than 100 years of history has undergone a number of changes due to the search for optimal approaches to their diagnosis, and at the present stage is firmly included in the unified classifications of mental disorders. The ideas of E. Kraepelin, without losing their relevance, are reflected in all the concepts proposed by researchers, both categorical and dimensional in nature. The knowledge accumulated to date about mixed states indisputably proves the practical significance of this psychopathological unit not only in a prognostic sense, but also in the aspect of choosing a rational pharmacotherapy. The works of recent decades have formed a consensus on the need to expand the diagnostic criteria for mixed conditions, substantiating their inconsistency with clinical reality, which is reflected in the DSM-V project.
Bipolar Disorder | Symptoms, complications, diagnosis and treatment
Bipolar disorder, formerly called manic depression, is a mental health condition that causes extreme mood swings that include emotional highs (mania or hypomania) and lows (depression).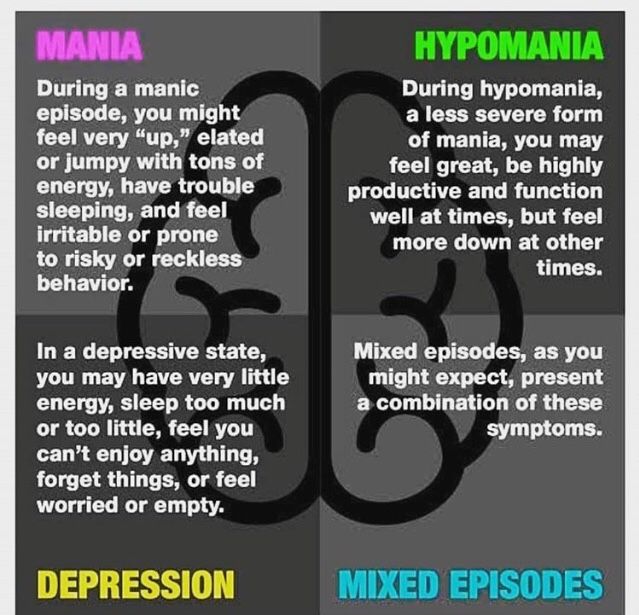 Episodes of mood swings may occur infrequently or several times a year.
Episodes of mood swings may occur infrequently or several times a year.
When you become depressed, you may feel sad or hopeless and lose interest or pleasure in most activities. When the mood shifts to mania or hypomania (less extreme than mania), you may feel euphoric, full of energy or unusually irritable. These mood swings can affect sleep, energy, alertness, judgment, behavior, and the ability to think clearly.
Although bipolar disorder is a lifelong condition, you can manage your mood swings and other symptoms by following a treatment plan. In most cases, bipolar disorder is treated with medication and psychological counseling (psychotherapy).
Symptoms
There are several types of bipolar and related disorders. They may include mania, hypomania, and depression. Symptoms can lead to unpredictable changes in mood and behavior, leading to significant stress and difficulty in life.
- Bipolar I. You have had at least one manic episode, which may be preceded or accompanied by hypomanic or major depressive episodes.
 In some cases, mania can cause a break with reality (psychosis).
In some cases, mania can cause a break with reality (psychosis). - Bipolar disorder II. You have had at least one major depressive episode and at least one hypomanic episode, but never had a manic episode.
- Cyclothymic disorder. You have had at least two years - or one year in children and adolescents - many periods of hypomanic symptoms and periods of depressive symptoms (though less severe than major depression).
- Other types. These include, for example, bipolar and related disorders caused by certain drugs or alcohol, or due to health conditions such as Cushing's disease, multiple sclerosis, or stroke.
Bipolar II is not a milder form of Bipolar I but is a separate diagnosis. Although bipolar I manic episodes can be severe and dangerous, people with bipolar II can be depressed for longer periods of time, which can cause significant impairment.
Although bipolar disorder can occur at any age, it is usually diagnosed in adolescence or early twenties. Symptoms can vary from person to person, and symptoms can change over time.
Mania and hypomania
Mania and hypomania are two different types of episodes, but they share the same symptoms. Mania is more pronounced than hypomania and causes more noticeable problems at work, school, and social activities, as well as relationship difficulties. Mania can also cause a break with reality (psychosis) and require hospitalization.
Both a manic episode and a hypomanic episode include three or more of these symptoms:
- Abnormally optimistic or nervous
- Increased activity, energy or excitement
- Exaggerated sense of well-being and self-confidence (euphoria)
- Reduced need for sleep
- Unusual talkativeness
- Distractibility
- Poor decision-making - such as in speculation, in sexual encounters, or in irrational investments
Major depressive episode
Major depressive episode includes symptoms that are severe enough to cause noticeable difficulty in daily activities such as work, school, social activities, or relationships. An episode includes five or more of these symptoms:
- Depressed mood, such as feeling sad, empty, hopeless, or tearful (in children and adolescents, depressed mood may present as irritability)
- Marked loss of interest or feeling of displeasure in all (or nearly all) activities
- Significant weight loss with no diet, weight gain, or decreased or increased appetite (in children, failure to gain weight as expected may be a sign of depression)
- Either insomnia or sleeping too much
- Either restlessness or slow behavior
- Fatigue or loss of energy
- Feelings of worthlessness or excessive or inappropriate guilt
- Decreased ability to think or concentrate, or indecisiveness
- Thinking, planning or attempting suicide
Other features of bipolar disorder
Signs and symptoms of bipolar I and bipolar II disorder may include other signs such as anxiety disorder, melancholia, psychosis, or others.