Best antidepressants for men
What's the best antidepressant for me?
There are dozens of options. This guide can help you determine which might be the best for your needs.
Types of antidepressants | Compare common antidepressants | Most effective antidepressant | Discontinuation syndrome | Side effects | Newest antidepressant | How to find the best antidepressant | Safety tips
The National Institute of Mental Health estimates that in 2019, about 19 million people—or 7.8% of the U.S. population—experienced at least one major depressive episode. There are several types of depression, but major depressive disorder is one of the most common.
A major depressive episode is defined as having persistent feelings of sadness, loss of interest in usual activities, changes to appetite and sleep patterns, loss of energy, difficulty concentrating, and suicidal ideation for at least two weeks, per the American Psychiatric Association.
Despite the fact that so many adults, across all age groups, live with depression each year, there are still many hurdles to receiving proper treatment. One is finding the right antidepressant medication to treat your individualized symptoms: with seven classes of antidepressants and roughly two dozen common medications available, identifying the right drug for you can seem as hard as finding a needle in a haystack.
Thankfully, there are ways to narrow down your options with your healthcare provider to make the search less intimidating. Here are some strategies for honing in on the best antidepressant to meet your needs.
RELATED: Depression statistics
Types of antidepressants
When you hear the word antidepressant, your mind might immediately jump to drugs like Prozac and Zoloft. That makes sense; those drugs are selective serotonin reuptake inhibitors (SSRIs) and are some of the most commonly prescribed antidepressants in the U.S.
But SSRIs aren’t the only type of antidepressant out there—and not everyone with depression needs to increase their levels of serotonin, a neurotransmitter (a.k. a chemical messenger) responsible for feelings of well-being.
a chemical messenger) responsible for feelings of well-being.
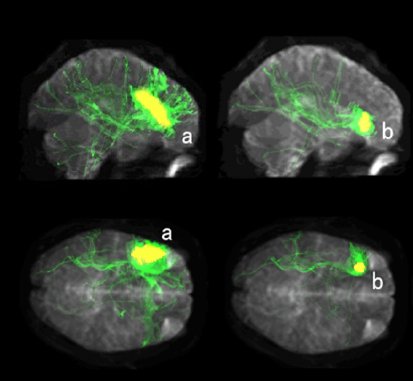
“Antidepressants target the neurotransmitters in your brain, increasing or decreasing activity in the brain circuits related to mood regulation,” says adult and geriatric psychiatrist David A. Merrill, MD, Ph.D., director of the Pacific Neuroscience Institute’s Pacific Brain Health Center at Providence Saint John’s Health Center in California.
The neurotransmitters most commonly affected by antidepressants include serotonin, norepinephrine, and dopamine; different classes of antidepressants work on these different neurotransmitter systems.
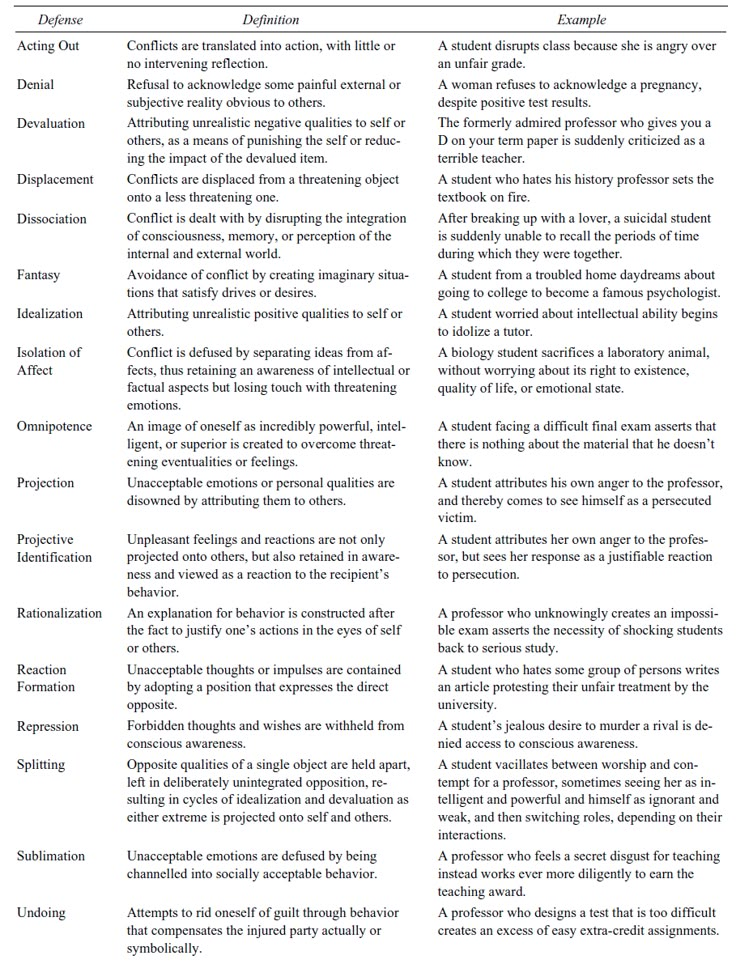
There are seven types of antidepressants:
- Selective serotonin reuptake inhibitors (SSRIs), including Prozac (fluoxetine), Paxil (paroxetine), Lexapro (escitalopram), Celexa (citalopram), and Zoloft (sertraline)
- Serotonin-norepinephrine reuptake inhibitors (SNRIs), including Cymbalta (duloxetine), Pristiq (desvenlafaxine), and Effexor XR (venlafaxine)
- Atypical antidepressants, including Wellbutrin (bupropion), Desyrel (trazodone), and Remeron (mirtazapine)
- Tricyclic antidepressants (TCAs), including amitriptyline, Tofranil (imipramine), and Pamelor (nortriptyline)
- Monoamine oxidase inhibitors (MAOIs), including Marplan (isocarboxazid) and Nardil (phenelzine)
- Norepinephrine and dopamine reuptake inhibitors (NDRIs), including dexmethylphenidate, and Wellbutrin (bupropion)
- Serotonin antagonist and reuptake inhibitors (SARIs), including Oleptro (trazodone), and Brintellix (vortioxetine)
Although all of these antidepressants are prescribed by healthcare providers to treat different types of patients and different types of depression, SSRIs are used the most often as a first-line treatment, says Dr. Merrill, with some SSRIs prescribed far more frequently than others.
Merrill, with some SSRIs prescribed far more frequently than others.
“Within the SSRIs, the most commonly used is Prozac because it has a lot of evidence [to support its use],” he explains, adding that Zoloft and Lexapro are also broadly prescribed.
RELATED: SSRIs vs. SNRIs: What’s the difference?
What’s the best antidepressant?
Let’s be clear: The best antidepressant for you is the one that you and your healthcare provider agree provides the most symptom relief with the least amount of side effects. Only you, in conjunction with your healthcare team, can decide what specific drug that is.
However, there are some antidepressants prescribed more often than others to people within certain population groups—and certain factors, like age, gender, pregnancy, and overall health, can determine which group you fall into (and which different antidepressants might be worth trying first).
Here are the most commonly prescribed antidepressants for the following groups of people:
The best antidepressants were chosen through a combination of expert interviews and popular data. SingleCare doesn’t endorse any particular drug over another.
SingleCare doesn’t endorse any particular drug over another.
What’s the most effective antidepressant?
There’s no single best antidepressant. Because everyone has a unique body chemistry, all antidepressants will work differently across the population of users. But some antidepressants have been shown to work more reliably and effectively for large groups of patients.
A 2018 study in The Lancet asserts that, based on extensive reviews of published studies, the antidepressants Lexapro, Paxil, Zoloft, and Remeron performed better than many other antidepressants, including popular drugs like Prozac, Luvox, and Desyrel.
It should be noted, though, that the study wasn’t able to look at how well these antidepressants work alongside other treatments, like therapy, or the side effects they may cause. (In other words, a drug that technically works to treat your depression may still not be feasible for you if it causes disruptive or serious side effects.)
It’s also important to note that most antidepressants take a long time to show their full effectiveness. “Despite brain changes happening quickly, the mood changes can take a couple of months with most of the broadly prescribed antidepressants,” says Dr. Merrill, adding that it can take anywhere from six to eight weeks, or even 12 weeks for older adults.
“Despite brain changes happening quickly, the mood changes can take a couple of months with most of the broadly prescribed antidepressants,” says Dr. Merrill, adding that it can take anywhere from six to eight weeks, or even 12 weeks for older adults.
While two or three months is a long time to wait to see if your antidepressant is truly helping you, it may not be necessary to wait quite so long if you aren’t feeling any improvement at all. “Many times, if patients are going to benefit [from a specific drug], they’ll start feeling improvement within two weeks; if you’re not, it might be worth considering moving on more rapidly, depending on how severe your depression is,” Dr. Merrill says.
Which is the hardest antidepressant to come off of?
Some antidepressants, particularly SSRIs and SNRIs, can cause a condition called “discontinuation syndrome” when therapeutic use is abruptly stopped; Dr. Merrill says this occurs because of the way the brain and body respond to the loss of serotonin support.
Per Harvard Health, typical symptoms of discontinuation syndrome include:
- Gastrointestinal upset
- Difficulty sleeping
- Flu-like symptoms
- Sweating and flushing
- Dizziness
- Hyperarousal
- Anxiety
- Agitation or irritability
While any SSRI or SNRI can cause discontinuation syndrome, the SNRI Effexor (venlafaxine) can be one of the trickiest to wean off, says psychiatrist and sleep medicine specialist Alex Dimitriu, MD, founder of Menlo Park Psychiatry & Sleep Medicine.
“Venlafaxine is an excellent medication, but missed doses can give people ‘brain zaps’ and quick feelings of vertigo, which I’ve called ‘vestibular jitters,’” Dr. Dimitriu explains. “These go away, fortunately, but it can make it hard to stop venlafaxine in particular.”
Dr. Merrill notes that Paxil is similarly difficult to discontinue, to the point where people will often put up with a lot of side effects simply to avoid having to stop its use. There are ways to make this process easier, though, so you don’t have to either suffer from discontinuation syndrome or stay on a drug in spite of your desire to wean off.
There are ways to make this process easier, though, so you don’t have to either suffer from discontinuation syndrome or stay on a drug in spite of your desire to wean off.
“Prozac has a longer half-life [than some of these other drugs], so it can be used as a bridging drug,” Dr. Merrill says. “We can transition off shorter-acting antidepressants into Prozac until your mood remains stable and we can get you off [the short-acting drug completely].”
Which antidepressants have the mildest side effects?
In general, SSRIs are considered the most well-tolerated antidepressants, per the Mayo Clinic; they typically have fewer side effects than other types and can be safely used at higher doses. Common side effects of SSRIs include sexual dysfunction, weight gain, trouble sleeping, drowsiness, dizziness, and nausea. SNRIs are also considered fairly safe, though Dr. Dimitriu says they can sometimes cause insomnia and elevate your blood pressure.
Atypical antidepressants all come with a common side effect profile, which includes dry mouth, headaches, dizziness, nausea, and fatigue. Tricyclic antidepressants are an older class and often carry more side effects: They have what Dr. Merrill calls a strong “cross-reactivity” with other drugs, a high instance of anticholinergic effects like blurred vision, sudden drops in blood pressure, and confusion, and can result more easily in toxicity than other antidepressants.
Tricyclic antidepressants are an older class and often carry more side effects: They have what Dr. Merrill calls a strong “cross-reactivity” with other drugs, a high instance of anticholinergic effects like blurred vision, sudden drops in blood pressure, and confusion, and can result more easily in toxicity than other antidepressants.
MAOIs can be complicated because they inhibit the metabolic response to an enzyme called tyramine, which causes them to potentially interact with a significant number of foods and drugs containing tyramine. As tyramine levels in the body rise, people can experience headaches, heart problems, nausea, and visual disturbances. It can be more challenging to take these drugs safely, but they do work well for some people.
Finally, it’s important to know that starting any new antidepressant can lead to increased suicidal thoughts; while these are considered rare adverse events, they are still possible, especially in children and adolescents taking antidepressants.
It’s difficult for researchers to assess the risk of suicide related to antidepressants since there are so many factors to account for. However, one 2015 study in The BMJ found that MAOIs, atypical antidepressants, and SNRIs were more likely to result in suicide or self harm than SSRIs and tricyclic antidepressants, with the highest risks found with Remeron (mirtazapine), Effexor (venlafaxine), and Desyrel (trazodone).
If you start taking a new antidepressant and notice an increase in thoughts related to suicide or death, reach out to a healthcare professional or trusted friend or family member as soon as possible. You can also contact the National Suicide Prevention Lifeline at 1-800-273-8255 or text GO to 741741 for immediate help.
What’s the newest antidepressant on the market?
SSRIs and SNRIs are newer antidepressants among the five major classes, and
vortioxetine, or Trintellix, is one of the more recent SSRIs to come on the market, says Dr. Dimitriu. Approved by the FDA for treating major depressive disorder in 2013, it works a bit differently than other SSRIs by directly interacting with serotonin receptors.
Dimitriu. Approved by the FDA for treating major depressive disorder in 2013, it works a bit differently than other SSRIs by directly interacting with serotonin receptors.
“It touts lower sexual side effects and possibly improved cognition as its features,” Dr. Dimitriu explains. “These benefits have seen mixed results in clinical practice, [but] for people who have not responded to the older SSRIs, Trintellix may offer hope.”
RELATED: Trintellix side effects
How to find the best antidepressant for you
If you’re ready to start finding the right antidepressant for you, here are four basic steps you should take to ensure the process moves as seamlessly and quickly as possible.
1. Talk to a healthcare professional
It can be your PCP, your gynecologist, your therapist—it doesn’t matter who you talk to, just that you find a healthcare professional you’re comfortable with. If they can’t personally prescribe an antidepressant, most providers will happily refer you to someone who can or work with that healthcare provider to coordinate your care.
2. Identify your target symptoms
As you can see, different symptoms, types of depression, and co-existing factors like age and gender can determine which antidepressant might be the best fit. It’s important to know what areas you, personally, need the most help with or want to see the most improvement in. Dr. Merrill says these are called “target symptoms of depression,” and they include things like energy, appetite, concentration, and sleep.
If you struggle with energy and motivation, for example, Dr. Dimitriu says a combination drug that targets more than just serotonin may be particularly helpful: “Adding the norepinephrine piece to the SSRI helps with energy and motivation, [and] bupropion, which is a dopamine and norepinephrine reuptake inhibitor, is also good.”
RELATED: What to expect from a depression screening
3. Consider pharmacogenomic testing
One of the most fascinating medical advances in recent history is pharmacogenomic testing, which helps you identify how your body will metabolize a drug and how your brain will respond to it, says Dr. Merrill.
Merrill.
Using this testing (which involves a simple blood draw or saliva swab) can make it easier for your healthcare provider to tell which antidepressants you might have a hard time metabolizing. This is important information, because if your body can’t metabolize a drug the way it’s supposed to, it will likely either not work well or cause troublesome side effects. With testing, you might be able to identify more quickly the class of drugs that will benefit you rather than going through months of ineffective drug trials.
“If you’ve failed with one or more antidepressants, it could be reasonable to do a pharmacogenomic test to see which one you’re most likely to tolerate,” advises Dr. Merrill.
4. Discuss all depression treatment options
Unfortunately, the best antidepressant for you won’t completely cure or eliminate your depression—it’s a whole body condition that affects every part of your life, and it’s important to use antidepressants as only part of a comprehensive treatment plan.
“Sleep and exercise are essential to getting better; as a sleep specialist, we have had extraordinary breakthroughs by getting people to sleep better,” says Dr. Dimitriu. “[You have] to meet your medicine halfway…[as the saying goes], you cannot push the gas pedal if there is no gas in the tank.”
It’s also recommended to receive some type of therapy in addition to taking medication, such as psychotherapy. While drugs can alter your neurochemistry, says Dr. Merrill, they can’t change your life circumstances. You will see better results if you can address the origin of your depression and work to heal or resolve the things that contribute to it. A good therapist can assist with that, as can increasing your social support network.
“There are no silver bullets—antidepressants aren’t going to work in isolation even under the best of circumstances,” Dr. Merrill asserts. “They are modulators of the responses to what’s going on in our lives, and it really takes an all-around holistic approach [to feel better]. ”
”
RELATED: How to get therapy without insurance
How to take antidepressants safely
Once you find the right antidepressant for you, it’s important to always take it safely. Remember to:
- Take the medication every day—don’t skip doses.
- Avoid drug interactions (ask your doctor or pharmacist what foods, medications, or supplements you should avoid while taking your antidepressant).
- Don’t stop taking the medication suddenly; talk to your healthcare provider about safely discontinuing use.
- Make note or keep a diary of side effects so you can share them with your provider.
- Avoid excessive alcohol use while taking antidepressant drugs.
Above all else, be patient—it may take several months for the medication to be fully effective, so as long as you’re seeing some improvement after a few weeks, try to stay the course for a bit rather than switching medications too frequently. If you still feel your medication isn’t helping, however, please reach out to a healthcare professional for assistance.
If you still feel your medication isn’t helping, however, please reach out to a healthcare professional for assistance.
The most effective antidepressants for adults revealed in major review
This is a plain English summary of an original research article
Antidepressants are effective to treat moderate to severe depression in adults. Five antidepressants appear more effective and better tolerated than others.
A major review of 522 antidepressant trials found that all of the 21 drugs studied performed better than placebo, in short-term trials measuring response to treatment. However, effectiveness varied widely.
Researchers ranked drugs by effectiveness and acceptability after eight weeks of treatment. Several drugs were more effective and were stopped by fewer people than others:
- escitalopram
- paroxetine
- sertraline
- agomelatine
- mirtazapine.
The review provides new evidence which may help people decide which antidepressant to choose first-line for moderate to severe depression. However, it did not assess antidepressants compared to other treatments such as cognitive behavioural therapy, or treatments in combination. Though there are some concerns over items not reported by individual trials, this review is likely to be reliable. It is extensive, included only placebo controlled double blind trials and searched successfully for unpublished trials.
However, it did not assess antidepressants compared to other treatments such as cognitive behavioural therapy, or treatments in combination. Though there are some concerns over items not reported by individual trials, this review is likely to be reliable. It is extensive, included only placebo controlled double blind trials and searched successfully for unpublished trials.
Why was this study needed?
Depression is a common condition, affecting an estimated 1 in 10 adults at some point in their lives. Antidepressants are widely prescribed in primary and secondary care, along with psychological interventions such as cognitive behavioural or interpersonal therapy. There is conflicting evidence to guide which antidepressants should be prescribed first-line, although NICE recommends a selective serotonin reuptake inhibitor (SSRI).
There has been uncertainty in recent years about the effectiveness of antidepressants. Their mode of action is poorly understood, and improvement in mood tends to be modest.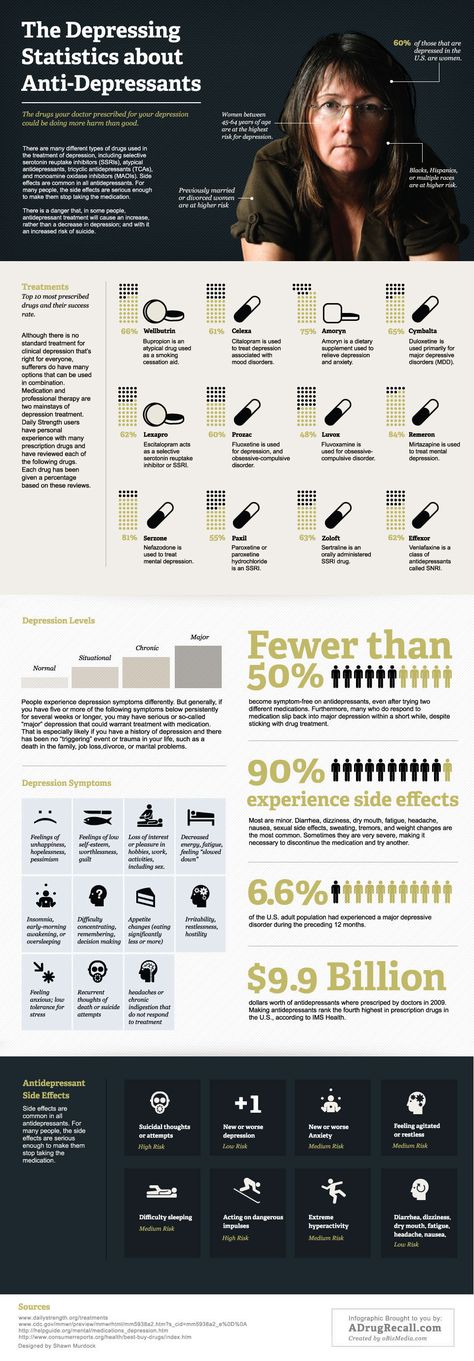 One 2008 meta-analysis suggested that antidepressants gave little benefit over placebo for mild to moderate depression.
One 2008 meta-analysis suggested that antidepressants gave little benefit over placebo for mild to moderate depression.
This new analysis went to some lengths to find unpublished studies and additional data from published studies, to give us the best overview of the current state of research.
What did this study do?
This systematic review and network meta-analysis compared 21 antidepressants with placebo or each other, directly within trials and indirectly across trials. They included 522 double-blind randomised controlled trials of 116,477 adults with moderate to severe depression.
More than 100 trials were previously unpublished. As well as publication databases, international trial registers and drug approval websites, the researchers had contacted all pharmaceutical companies marketing antidepressants to ask for unpublished studies.
The antidepressants were compared for effectiveness (at least 50% improvement in symptoms) and acceptability (assessed as drop-out rate). They found 380 trials at possible risk of bias due mainly to lack of reporting of randomisation methods, and 46 at high risk. However, the trials were all placebo controlled.
They found 380 trials at possible risk of bias due mainly to lack of reporting of randomisation methods, and 46 at high risk. However, the trials were all placebo controlled.
What did it find?
- All 21 antidepressants were more likely to produce a treatment response after eight weeks treatment than a placebo. The most effective antidepressant compared to placebo was the tricyclic antidepressant amitriptyline, which increased the chances of treatment response more than two-fold (odds ratio [OR] 2.13, 95% credible interval [CrI] 1.89 to 2.41). The least effective was the serotonin and noradrenaline reuptake inhibitor reboxetine, which increased treatment response by 37% (OR 1.37, 95% CrI 1.16 to 1.63).
- Drop-out rates by eight weeks of treatment were similar to placebo for the majority of antidepressants. People were 30% more likely to stop taking the tricyclic clomipramine than placebo (OR 1.30, 95% CrI 1.01 to 1.68) and slightly less likely to stop taking agomelatine (an “atypical” antidepressant) or the SSRI fluoxetine (OR for agomelatine 0.
 84, 95% CrI 0.72 to 0.97; OR for fluoxetine 0.88, 95% CrI 0.8 to 0.96).
84, 95% CrI 0.72 to 0.97; OR for fluoxetine 0.88, 95% CrI 0.8 to 0.96). - In head-to-head comparisons between the drugs, five were identified as having a combination of better effectiveness and lower drop-out rates, compared to others: the SSRIs escitalopram, paroxetine and sertraline, and atypicals agomelatine and mirtazapine. Reboxetine (atypical), trazodone (similar to a tricyclic) and fluvoxamine (SSRI) were identified as having lower effectiveness and higher drop-out rates.
- Though absolute effect sizes were not reported in the results, the researchers described the effect sizes as “modest”. However, they also said that “non-response to treatment will occur.”
What does current guidance say on this issue?
The NICE 2009 guideline on depression advises that people with moderate to severe depression should be offered an antidepressant and psychological therapy such as cognitive behavioural therapy or interpersonal therapy. It says the antidepressant prescribed “should normally be an SSRI in a generic form because SSRIs are equally effective as other antidepressants and have a favourable risk-benefit ratio. ”
”
The guideline warns that venlafaxine is more associated with risk of death from overdose than other SSRIs, while “tricyclic antidepressants, except for lofepramine, are associated with the greatest risk in overdose.”
The guideline, last updated in 2016, is under review.
What are the implications?
The findings are of interest to GPs and psychiatrists, who need to decide on the best initial treatment for adults with moderate to severe depression. The comparative data may help doctors select drugs with better efficacy and side-effects.
However, treatment choice will be guided by an individual patient's circumstances and preferences. The meta-analysis was unable to look at the potentially different effects of treatment on subgroups based on age, sex, the severity of symptoms or duration of illness.
The review did not consider combined drug and psychological treatments, as recommended by NICE for moderate to severe depression, or long-term effects which limit its applicability.
Citation and Funding
Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet. 2018. [Epub ahead of print].
This project was funded by the National Institute for Health Research Oxford Health Biomedical Research Centre (BRC-1215-20005) and the Japan Society for the Promotion of Science.
Bibliography
Parikh SV, Kennedy SH. More data, more answers: picking the optimal antidepressant. Lancet 2018.
NICE. Depression in adults: recognition and management. CG90. London: National Institute for Health and Care Excellence; 2009.
Produced by the University of Southampton and Bazian on behalf of NIHR through the NIHR Dissemination Centre
Fighting depression: 10 modern drugs
{{if type === 'partner-stocks'}}
{{/if}}
{{/if}} {{each list}}${this} {{if isGorzdrav}}
Delete
{{/if}}
{{/each}} {{/if}} Search by drug, disease, substance: DERMAKOSMETIKA, SOLGAR, NaturAge, Voltaren, KagocelHome
Articles
Fighting depression: 10 modern drugs
Depression is an urgent problem, the number of visits to doctors is growing every year. It can be solved by contacting a psychotherapist and taking antidepressants . These are drugs that regulate the production of hormones and biochemical processes in the body. It is strictly forbidden to prescribe them to oneself , as these are complex drugs with certain restrictions, side effects effects . The doctor must authorize their appointment and control the intake. We will tell you which of them are the most effective and common in medicine, how many they have pluses and minuses.
It can be solved by contacting a psychotherapist and taking antidepressants . These are drugs that regulate the production of hormones and biochemical processes in the body. It is strictly forbidden to prescribe them to oneself , as these are complex drugs with certain restrictions, side effects effects . The doctor must authorize their appointment and control the intake. We will tell you which of them are the most effective and common in medicine, how many they have pluses and minuses.
What is meant by
depression Doctors have known it since ancient Greece and Egypt. Hippocrates described it as melancholy - a condition that is accompanied by anxiety, despondency, insomnia, refusal of food, irritability. Most often, the cause is childhood trauma or severe, frequent stress in adulthood. There are many provoking factors: the death of a loved one, deterioration of living conditions, alcoholism, brain diseases. Such cases are referred to as psychogenic depression.
Such cases are referred to as psychogenic depression.
The second type is endogenous. The problem appears not from large external shocks, but because of internal causes. A person is constantly dissatisfied with himself, subjecting himself to criticism. Many patients have panic attacks , haunted by a feeling of fear, anxiety.
How long the period of depression lasts
Many people mistake ordinary periods of low mood for depression. If they do not last long and are quickly replaced by periods of recovery, then we are not talking about a depressive state. The problem is obvious when the symptoms persist for months and dramatically change a person's life. Then you need to see a doctor.
What happens to the body
The most common theory is that there is a malfunction of neurotransmitters located in the brain. These substances transmit signals from neuron to neuron and are responsible for a person's mood. Dysfunction leads to a slowdown in the rate of this transmission and a decrease in the number of neurotransmitters themselves. Serotonin, which is called the "hormone of happiness", suffers the most. For clarity, this biochemical process can be compared, for example, with a drop in blood sugar levels in diabetes mellitus.
Dysfunction leads to a slowdown in the rate of this transmission and a decrease in the number of neurotransmitters themselves. Serotonin, which is called the "hormone of happiness", suffers the most. For clarity, this biochemical process can be compared, for example, with a drop in blood sugar levels in diabetes mellitus.
How is
treated depressionDepression has been treated in different ways. In the ancient world - emetics and laxatives. In the Renaissance - wine and sunbathing. In the Age of Enlightenment - external stimuli, for example, insects. The 19th century brought new recipes - in particular, a solution of camphor in tartaric acid. The treatment also included the use of drugs, which are now no longer allowed for sale, and some are recognized as narcotic.
Obviously, all these drugs had no effect on increasing the amount of serotonin. And the treatment is precisely to normalize its production. This was done after creating modern antidepressants , which have a minimum of side effects, are safe for the body and are not addictive. These are medicines, whose action is aimed specifically at balancing the disturbed balance of neurotransmitters: serotonin, norepinephrine, dopamine.
These are medicines, whose action is aimed specifically at balancing the disturbed balance of neurotransmitters: serotonin, norepinephrine, dopamine.
Prescription
If a healthy person takes antidepressants , there will be no effect . For a depressed patient, taking them will help:
- improve psychological state;
- get rid of irritability;
- panic fear;
- increase mental and physical activity;
- overcome the dreary mood.
Psychiatrists prescribe antidepressants for chronic back pain, headaches. And also with irritable bowel syndrome, incontinence and other cases when the body stops producing its own painkillers. Medication helps restore pain suppression mechanisms.
These drugs can only be taken with a doctor's prescription, as many of them are strong stimulants.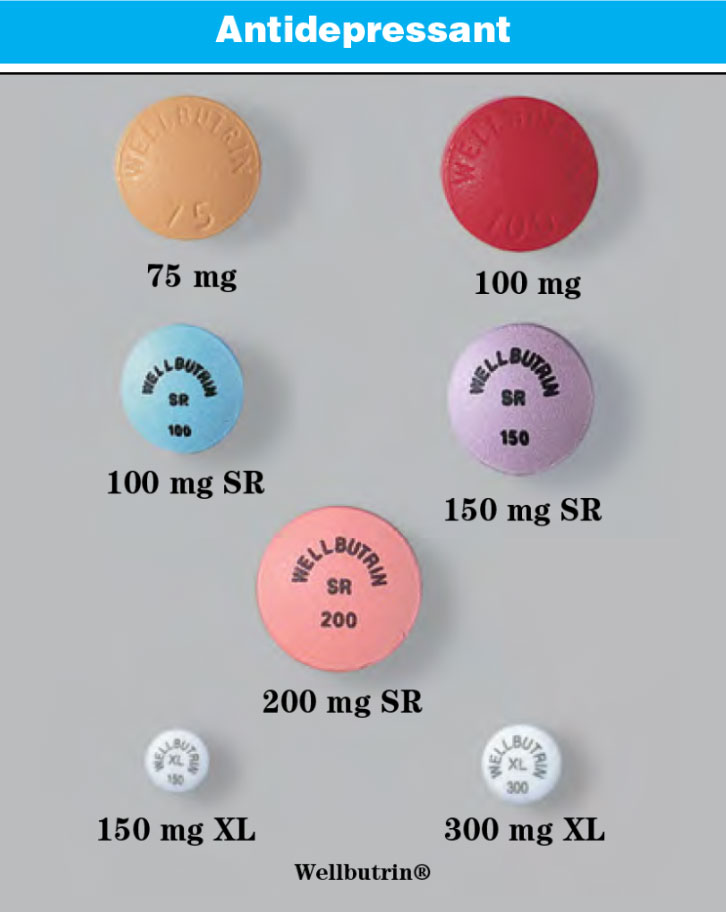 Self-administration may cost dearly - the condition may worsen. Only a doctor will correctly calculate how many medicines to take per day. In parallel with the treatment by a psychiatrist, a neurologist, a consultation of a psychotherapist is required.
Self-administration may cost dearly - the condition may worsen. Only a doctor will correctly calculate how many medicines to take per day. In parallel with the treatment by a psychiatrist, a neurologist, a consultation of a psychotherapist is required.
Precautions
- Prescribed drug start drinking from a small dose - the first couple of days they take a quarter of a tablet. Gradually increase the dose to normal. So the body adapts better. Finish the course by reducing the dose.
- The first effect of appears only 2 weeks after the start of administration. Sustained action - after six months. All this time, you need to take remedy, without making passes, breaks.
-
Products are not combined with melatonin, St. John's wort, products and dietary supplements based on sibutramine, 5-HTP. Their combination can raise serotonin to dangerous levels.
 Also, you can not combine them with monoamine oxidase inhibitors, for example, Cipralex. When writing a prescription, the doctor takes these points into account.
Also, you can not combine them with monoamine oxidase inhibitors, for example, Cipralex. When writing a prescription, the doctor takes these points into account. - Drinking antidepressants is better in parallel with visits to a psychotherapist. If the drugs normalize the biochemical processes in the body, then this doctor will help normalize the psychological state after depression.
The best antidepressants
In medicine, they have long argued that some drugs give only a placebo effect. The purpose of the study was to find out which of them are the most effective and valid . The project involved 116 thousand patients, and its results were published by the authoritative edition of the Lancet. We offer a list of the best.
1. Agomelatine
New generation drug. Agomelatine is used for severe depressive disorders, high levels of anxiety. Enhances the release of dopamine and norepinephrine, stimulates melatonin receptors. The standard therapeutic dose is 25-50 mg 1 time / day. Helps to restore the normal structure of sleep, get rid of anxiety and panic attacks attacks
The standard therapeutic dose is 25-50 mg 1 time / day. Helps to restore the normal structure of sleep, get rid of anxiety and panic attacks attacks
Pros
+ Does not adversely affect attention and memory.
+ No lethargy during the day.
+ No sexual deviations.
+ No relation to blood pressure.
+ Do not reduce dosage upon discontinuation.
Cons
— In 1-10% of cases, increased sweating, diarrhea, constipation.
- Possible increased fatigue, drowsiness.
- There are no evidence-based safety studies in people with renal or hepatic insufficiency, therefore, such patients are advised to refrain from taking drugs with active ingredient agomelatine.
2. Amitriptyline
Tricyclic antidepressant. Moreover, the World Health Organization considers Amitriptyline the most reliable in this group. The standard dose is 200-250 mg / day. The action is to block the reuptake of neurotransmitters. A good remedy for moderate to severe disorders of the endogenous type. Additionally, it has a sedative and hypnotic effect. Effective in the treatment of neuropathic pain, for the prevention of migraine.
A good remedy for moderate to severe disorders of the endogenous type. Additionally, it has a sedative and hypnotic effect. Effective in the treatment of neuropathic pain, for the prevention of migraine.
Pluses
+ Preparations with active ingredient amitriptyline are inexpensive.
+ High reliability, minimum side effects.
+ Relatively safe during breastfeeding.
Cons
- Possible side effect in the form of blurred vision, dry mouth.
- Lowering blood pressure.
- Some patients experience constipation.
- Drowsiness.
3. Escitalopram
It belongs to the group of modern serotonin reuptake inhibitors (SSRIs). Most often, it is recommended to take for anxiety, panic attacks. It is taken once, the standard dose is 10 mg per day. Escitalopram has a milder effect and is prescribed to patients for whom tricyclic drugs are contraindicated.
Pluses
+ Lasting effect comes after 3 months.
+ Indicated for patients with disorders of the cardiovascular system.
+ Soft action.
Cons
- In some patients, the functions of the gastrointestinal tract are disturbed, which is most often expressed in diarrhea.
- Anxiety may increase during the first 2 weeks, therefore it is recommended to start treatment with low doses and gradually increase them.
- Contraindicated in pregnancy and lactation.
4. Mirtazapine
A drug of the tetracyclic group. Mirtazapine - good stimulant for anxious depressions, has a moderate sedative effect. The average amount is 30 mg / day, it must be consumed once. Usually it is prescribed to patients who lose interest in life, cease to experience joy, pleasure. Effective in the correction of sleep, in particular, early awakenings.
Pros
+ Earlier onset of action than SSRIs (1 week).
+ Works well with most general medicines.
+ Full effect in 4 weeks.
+ Does not affect sexual function.
Cons
- The active substance mirtazapine is contraindicated in diabetes mellitus, arterial hypotension, increased intraocular pressure.
— During the appointment, you must drive carefully and engage in potentially hazardous types of work.
- 18% of patients experience drowsiness, 15% dry mouth, 5% weight loss. Other side effects occur in 1-3% of cases.
5. Paroxetine
Belongs to the SSRI group, is used most often for severe anxiety, panic, social phobia, nightmares, stress after trauma. Paroxetine can resolve the problems of anxious depression, anxiety-phobic disorders. Take once a day at a dose of 20 mg.
Pros
+ The most powerful stimulant among SSRIs.
+ Anxiety and insomnia pass quickly.
+ Minimal side effects in the form of vomiting, diarrhea.
+ Suitable for patients with cardiovascular problems.
Cons
— Not suitable for patients with severe motor, mental inhibition.
- Reduces libido.
- Harmful to the fetus when taken during pregnancy.
6. Fluoxetine
One of the most commonly used antidepressants in the SSRI group. Known as Prozac. Fluoxetine is also known as a good mood stimulant. Patients have a feeling of fear, tension, anxiety, gloomy dislike for others. Depending on the indications, the average daily dose is 20-60 mg.
Pluses
+ There is practically no effect on the work of the heart.
+ Does not cause sedation.
+ Effective for patients with motor retardation and excessive daytime sleepiness.
Cons
- May cause weight loss.
— Hypoglycemia is possible in diabetes mellitus.
- Contraindicated in severe renal impairment.
7. Fluvoxamine
Another SSRI drug. Fluvoxamine is similar to Prozac Fluoxetine but is fast acting and may cost cheaper. The effect is in a more active slowing down of the reuptake of serotonin by neurons. It is indicated for depression of various origins, as well as obsessive-compulsive disorders. The average daily dose is 100 mg.
Fluvoxamine is similar to Prozac Fluoxetine but is fast acting and may cost cheaper. The effect is in a more active slowing down of the reuptake of serotonin by neurons. It is indicated for depression of various origins, as well as obsessive-compulsive disorders. The average daily dose is 100 mg.
Pros
+ Lower price than traditional Prozac.
+ Faster action than him.
+ Relatively minor side effects (diarrhea, dry mouth, drowsiness).
Cons
- Contraindicated in diabetes.
- Pregnant women - with caution, lactation - prohibited.
- Causes nausea in some patients.
8. Sertraline
One of the widely used and universal drugs of the SSRI group. They treat almost any depressive condition, panic disorder, social phobia. However, in severe clinical cases, sertraline may not be effective enough. The standard dose is 50 mg/day.
Pros
+ No cardiotoxicity.
+ The patient's psychomotor activity does not change.
+ Does not increase body weight.
+ Combines well with other groups of antidepressants.
Cons
— In the first 2 weeks there may be problems with sleep, diarrhea.
- Side effects of a sexual nature.
- Contraindicated in pregnant women.
9. Escitalopram
The drug is classified as an SSRI. Its difference is in its effectiveness in depression, which is accompanied by involuntary movements (tic, tremor, chewing, smacking). Escitalopram is prescribed to patients with panic, anxiety, phobias, obsessive thoughts or actions. The daily dose is 20 mg.
Pluses
+ Effective in tardive dyskinesia.
+ One of the most powerful SSRIs.
+ More pronounced thymoleptic effect (improvement of mood) compared to many antidepressants of the same group.
Cons
- In some patients, anxiety increases within 2 weeks after starting treatment.
— Gastrointestinal disorders, insomnia, agitation are possible.
— Use during pregnancy only in extreme cases, incompatible with feeding.
10. Venlafaxine
Belongs to the SNRI group. In addition to blocking the reuptake of serotonin, venlafaxine has a similar effect on another neurotransmitter, norepinephrine. The medicine is prescribed for depressive conditions of various origins, social phobias, anxiety, panic. Usually take 150 mg per day.
Pros
+ Better tolerated by patients than most tricyclics.
+ More pronounced effect than classic SSRIs.
+ Fewer contraindications.
Cons
- Traditional side effects of most antidepressants: nausea, drowsiness, dry mouth, diarrhea or constipation.
- May increase eye pressure.
- The most severe withdrawal syndrome among antidepressant drugs.
This list is not to be used as a recommendation. In any case, consult your doctor before purchasing. Be healthy!
list of the best drugs without prescriptions
Can I buy antidepressants without prescriptions? What mood improvers are most effective, when will lighter drugs help, and when powerful ones are needed, how do they affect the body, and can they be taken on their own? The main thing when choosing a medicine is not to harm your health.
I'm depressed!
This can often be heard from friends or read on the forum. But, as a rule, the person making such statements is mistaken. After all, what is meant by "depression" in a colloquial environment? Usually it means just a short-term deterioration in mood, irritability, fatigue under the influence of circumstances. Sometimes a person just has a "bad day" or "gets up on the wrong foot" and calls it depression.
Nowadays, people are constantly faced with stress: overload at work, a frantic pace of life, excessive demands on themselves, a huge amount of information that flows from all sources. Not surprisingly, many people cannot cope with so many stressors, and this can manifest itself in various symptoms:
- anxiety;
- irritability;
- fatigue;
- sleep disorders;
- obsessive thoughts;
- panic attacks.
If these symptoms are short-lived and go away on their own, don't get too upset. In most cases, they will be defeated by just a good rest. But sometimes vacation is not enough, and the body needs a little help. It is very important to choose the right medicines for this.
In most cases, they will be defeated by just a good rest. But sometimes vacation is not enough, and the body needs a little help. It is very important to choose the right medicines for this.
What depression really is
This is a long-term (2 weeks or more) marked decrease in mood, which is accompanied by several additional symptoms: decrease in activity, slowing down of mental activity, lack of joy from life. That is, if you are no longer touched by the usual joys - hobbies, family, gatherings with friends, then this is an occasion to think, observe your condition and, possibly, consult a doctor.
If you are no longer touched by the usual joys, then this is an occasion to think and, perhaps, consult a doctor.True depression is a serious and often serious illness that requires mandatory treatment by a psychiatrist with the appointment of special medications.
What drugs are used to treat depression?
They are collectively called antidepressants. It is worth noting that in recent years, the indications for prescribing antidepressants have expanded significantly. Numerous studies have been conducted that have shown the effectiveness of antidepressants not only for depression, but also for anxiety, sleep disorders (insomnia), neurosis, and even neuropathic pain. Today, drugs from different groups of antidepressants are widely prescribed by psychiatrists, neurologists, and even therapists.
It is worth noting that in recent years, the indications for prescribing antidepressants have expanded significantly. Numerous studies have been conducted that have shown the effectiveness of antidepressants not only for depression, but also for anxiety, sleep disorders (insomnia), neurosis, and even neuropathic pain. Today, drugs from different groups of antidepressants are widely prescribed by psychiatrists, neurologists, and even therapists.
Two groups of drugs are most commonly used.
Tricyclic antidepressants
These are the oldest drugs that are considered the most powerful:
- Amitriptyline is a drug with a strong sedative and powerful antidepressant effect. Large doses are used to treat severe depression, and small doses are used for milder disorders. It relieves anxiety and has a hypnotic effect.
- Anafranil is a drug of balanced action, usually more easily tolerated than amitriptyline, and also relieves anxiety well.
 It is prescribed for the treatment of depression from mild to severe, various anxiety disorders.
It is prescribed for the treatment of depression from mild to severe, various anxiety disorders. - Melipramine - has a stimulating effect, they treat apathetic depression.
Selective serotonin reuptake inhibitors (SSRIs)
This is a more modern group of drugs. Their advantages are good tolerability and few or no side effects.
Often prescribed from this group:
- Fevarin — has anti-anxiety and good antidepressant effect. With prolonged use, it normalizes sleep, if it has been disturbed.
- Zoloft is a fairly strong daytime antidepressant. It relieves anxiety, obsessive thoughts, while not causing drowsiness.
- Paxil - relieves anxiety, often prescribed for the treatment of panic attacks.
There are many more modern antidepressants that have few side effects and are well tolerated:
- Ixel;
- Velaxin;
- Valdoxan;
- Trittiko;
- Simbalta and others.

But strong antidepressants are not sold without a prescription . They can only be prescribed by a doctor: a psychiatrist, a neurologist, sometimes a therapist.
Why can't I take antidepressants without a prescription?
- Only a doctor can assess the risk of side effects for a particular patient.
- Different antidepressants have different nuances of therapeutic action. If the medicine is chosen incorrectly, at best it will not help, at worst it will hurt.
- Dose selection is carried out individually. If you increase the dose too quickly on your own, you can experience a lot of unpleasant consequences.
- Cancellation should also be carried out gradually and under the supervision of a physician. Otherwise, you risk getting a withdrawal syndrome.
What to do?
There are a number of drugs available without a prescription. They are not effective for clinical depression, but they will help to cope with stress, short-term sleep disorders and irritability. With their help, you can try to alleviate your psycho-emotional state a little:
With their help, you can try to alleviate your psycho-emotional state a little:
- Glycine is one of the most popular products. It is prescribed, starting from childhood, with stress, overwork, emotional overstrain. Sometimes effective for minor sleep disturbances.
- Afobazole . Has an anti-anxiety effect, eliminates the feeling of fear, tearfulness, irritability. It is used in the treatment of vegetative-vascular dystonia and even in alcoholism, to alleviate the symptoms of alcohol withdrawal. Not addictive. It should be borne in mind that children under 18 years of age are contraindicated.
- Novo-passit . Quite a strong sedative for nervousness and irritability. Effective in reducing concentration, memory, fatigue. Helps to restore the nervous system during periods of increased stress.

- Stressovit . Well calms, relieves irritability, anxiety, improves sleep. It is not recommended to drive a car and other activities that require increased concentration of attention during the period of treatment.
- Persen is a herbal medicine. Contains extracts of valerian, lemon balm and peppermint. It has a calming and anti-anxiety effect. It helps well with increased excitability, emotional lability, tearfulness. It can be used in the complex therapy of mild anxiety depressive disorders, facilitates the withdrawal of potent drugs.
- Magne B6 . Increases the body's resistance to stress. Magnesium deficiency can lead to an imbalance of the nervous system, irritability, sleep disturbances, so Magne B6 has a positive effect in these cases.
- Tenoten . It has an anti-anxiety, calming, anti-asthenic effect, helps to cope with stress and psycho-emotional stress.
 Relieves irritability and tension. Can be used in neurotic conditions.
Relieves irritability and tension. Can be used in neurotic conditions.
When should I see a doctor?
- If the decrease in mood persists for more than two weeks, and attempts at self-treatment have not been effective.
- If you have thoughts about unwillingness to live or suicidal thoughts.
- If depression significantly disrupts the usual course of life: you cannot work, fully communicate with your family, enjoy what used to bring joy.
You can consult a psychiatrist in confidence. Information about the very fact of treatment, not to mention the diagnosis and treatment, is a medical secret: they are not reported to work, they are not disclosed. It is better to diagnose depression early and start treatment than to bring it to advanced stages.
Literature
- Bauer M., Pfennig A., Severus E., Vaibrau P.S., Angst J., Muller H. Clinical recommendations of the World Federation of Biological Psychiatry on Biological Therapy of Unipolar Depressive Disorders Part 1: Acute and Acute and Acute CONTINUOUS TREATMENT OF UNIPOLAR DEPRESSIVE DISORDERS AS OF 2013//CURRENT THERAPY OF MENTAL DISORDERS Number: 4 Year: 2015 Pages: 33-40
- Antidepressant therapy and other treatments for depressive disorders.

Learn more