Behavioural treatment for adhd
Parent Training in Behavior Management for ADHD
Please bookmark this to the Finding the right therapy for your child
View full-size | View text version
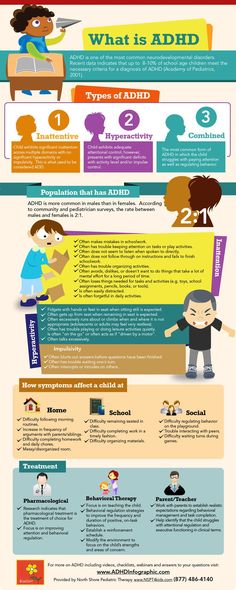
Behavior therapy is an effective treatment for attention-deficit/hyperactivity disorder (ADHD) that can improve a child’s behavior, self-control, and self-esteem. It is most effective in young children when it is delivered by parents. Experts recommend that healthcare providers refer parents of children younger than 12 years old for training in behavior therapy. For children younger than 6 years old, parent training in behavior management should be tried before prescribing ADHD medication.
When parents become trained in behavior therapy, they learn skills and strategies to help their child with ADHD succeed at school, at home, and in relationships. Learning and practicing behavior therapy requires time and effort, but it has lasting benefits for the child and the family.
Parent training in behavior management is also known as parent behavior therapy, behavioral parent training, or just parent training.
What should parents look for?
If possible, families should look for a therapist who focuses on training parents. Some therapists will have training or certification in a parent training program that has been proven to work in young children with ADHD.
Therapists may also use strategies like those in proven programs1,2. The following list of questions can be used to find a therapist who uses a proven approach:
- Does this therapist
- Teach parents skills and strategies that use positive reinforcement, structure, and consistent discipline to manage their child’s behavior?
- Teach parents positive ways to interact and communicate with their child?
- Assign activities for parents to practice with their child?
- Meet regularly with the family to monitor progress and provide coaching and support?
- Re-evaluate treatment plans and remain flexible enough to adjust strategies as needed?
Learn more about finding a therapist »
New, easy-to-use, interactive web tools for children and teens to deal with thoughts and feelings in a healthy way.
What can parents expect?
Parents typically attend eight or more sessions with a therapist. Sessions may involve working with groups of parents or with one family alone. The therapist meets regularly with the parents to review their progress, provide support, and adjust strategies, as needed, to ensure improvement. Parents typically practice with their child between sessions.
Parents have the greatest influence on their young child’s behavior. Only therapy that focuses on training parents is recommended for young children with ADHD because young children are not mature enough to change their own behavior without their parents’ help. Some therapists may use play therapy or talk therapy to treat young children with ADHD. Play therapy provides a way for children to communicate their experiences and feelings through play. Talk therapy uses verbal communication between the child and a therapist to treat mental and emotional disorders. Neither of these has been proven to improve symptoms in young children with ADHD.
Learning and practicing behavior therapy requires time and effort, but it has lasting benefits for the child. Ask your healthcare provider about the benefits of parent training in behavior therapy for young children with ADHD.
What can healthcare providers do?
Healthcare providers can:
- Follow the clinical practice guideline for diagnosis and treatment of ADHD in young children
- Discuss with parents the benefits of behavior therapy and why they should consider getting training.
- Identify parent training providers in their area and refer parents of young children with ADHD for training in behavior therapy before prescribing medicine.
For more information:
- Vital Signs: ADHD in young children
- Treatment patterns for young children with ADHD
For Parents and Providers:
- Finding a therapist: A guide for parents [PDF – 975 KB]
- Behavior therapy for young children with ADHD: Overview for parents [PDF – 330 KB]
- Behavior therapy for children with ADHD: Overview for parents [PDF – 795 KB]
- Behavior therapy for young children with ADHD: What healthcare providers can do [PDF – 749 KB]
- ADHD treatment options
- National Resource Center on ADHD
- Webinar series for educators working with young children with ADHD
- American Academy of Pediatrics clinical practice guideline for ADHD
For States:
- State profiles of treatment patterns for young children with ADHD
- Medicaid policy research
Parents typically attend 8-16 sessions with a therapist and learn strategies to help their child.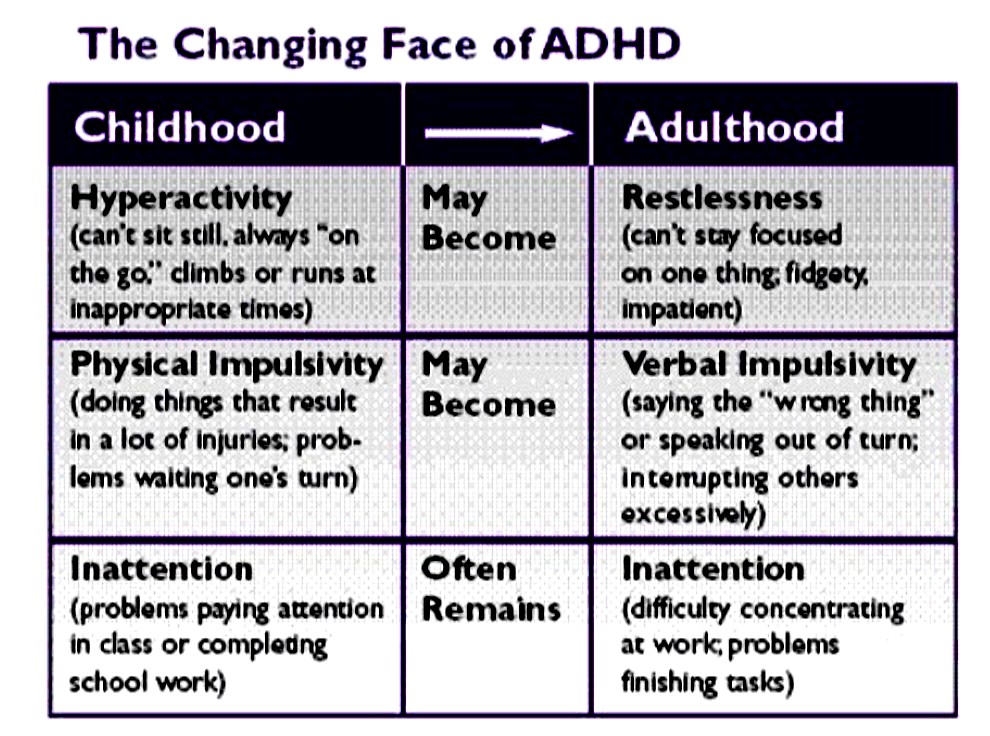 Sessions may involve groups or individual families.
Sessions may involve groups or individual families.
- The therapist meets regularly with the family to monitor progress and provide support
- Between sessions, parents practice using the skills they’ve learned from the therapist
After therapy ends families continue to experience improved behavior and reduced stress.
- Positive Communication
- Positive Reinforcement
- Structure and Discipline
- Behavior therapy, given by parents teaches children to better control their own behavior, leading to improved functioning at school home and in relationships. Learning and practicing behavior therapy requires time and effort, but has lasting benefits for the child.
ADHD Behavioral Treatment | Therapy for ADHD
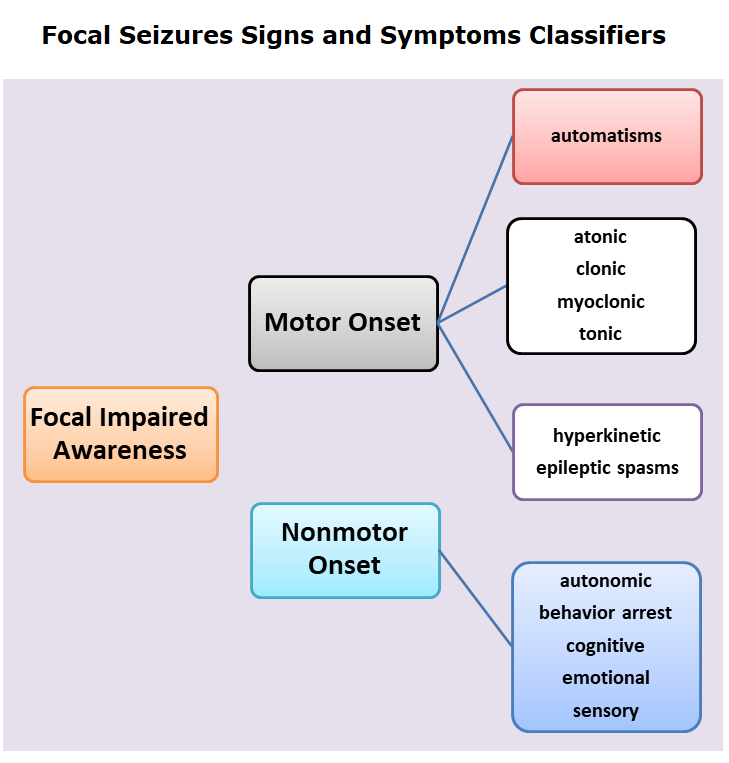
There are two kinds of behavioral interventions that can help children with ADHD manage their symptoms of hyperactivity, impulsiveness, and inattention. These ADHD therapies don’t affect the core symptoms, but they teach children skills they can use to control them. Some focus on strategies for staying organized and focused. Others aim at cutting down on the disruptive behaviors that can get these children into trouble at school, make it difficult for them to make friends, and turn family life into a combat zone.
Some focus on strategies for staying organized and focused. Others aim at cutting down on the disruptive behaviors that can get these children into trouble at school, make it difficult for them to make friends, and turn family life into a combat zone.
Some children, especially those with severe ADHD symptoms, benefit from behavioral therapy along with medication; for others, the training may make enough difference to enable them to succeed in school and function well at home without medication.
One important reason for kids to participate in behavioral therapy (whether or not they also take medication) is that ADHD medications stop working when you stop taking them, while behavioral therapy can teach children skills that will continue to benefit them as they grow up.
For behavior problems
For kids whose impulsive behavior is creating conflict at home and getting them into trouble at school, therapy can help them rein in the behavior that’s problematic and establish more positive relationships with the adults in their lives. It’s called, generally, parent training, because it involves working with parents and children together. It trains parents to interact differently with children, in order to elicit desirable behavior on the part of the child and discourage behavior that’s causing them trouble.
It’s called, generally, parent training, because it involves working with parents and children together. It trains parents to interact differently with children, in order to elicit desirable behavior on the part of the child and discourage behavior that’s causing them trouble.
Parent training is not just for children with ADHD, but since kids with ADHD are often prone to tantrums, defiance, and tuning out parental instructions, it can substantially improve their lives, and the wellbeing of their whole families. Though it focuses on interaction with parents, it’s also been shown to reduce outbursts and other problem behaviors at school, as the skills kids learn in responding to very predictable parental interactions are transferrable to other settings. The training is generally done by clinical psychologists.
There are several kinds of parent training that have been shown to be effective, including Parent-Child Interaction Therapy (PCIT), Parent Management Training (PMT), Positive Parenting Program (Triple P). They all teach parents how to use praise, or positive reinforcement, more effectively, as well as consistent consequences when kids don’t comply with instructions. They result in better behavior on the part of children, decreased arguing and tantrums, better parent-child interactions, and reduced parental stress.
They all teach parents how to use praise, or positive reinforcement, more effectively, as well as consistent consequences when kids don’t comply with instructions. They result in better behavior on the part of children, decreased arguing and tantrums, better parent-child interactions, and reduced parental stress.
Young children with ADHD often find themselves scolded or punished much more than they are praised, so a clear way to earn positive attention from the most important people in their lives can be a big motivator. It’s not unusual for kids who’ve been negatively affected by their behavior problems—kicked out of preschool, black-listed from play dates—to make dramatic improvements through parent training.
School interventions
Young children with ADHD can benefit from systems that encourage positive behavior, like the “Daily Report Card.” These approaches pinpoint specific goals for behavior in school, give kids feedback on how they’re doing, and reward them for meeting those goals successfully.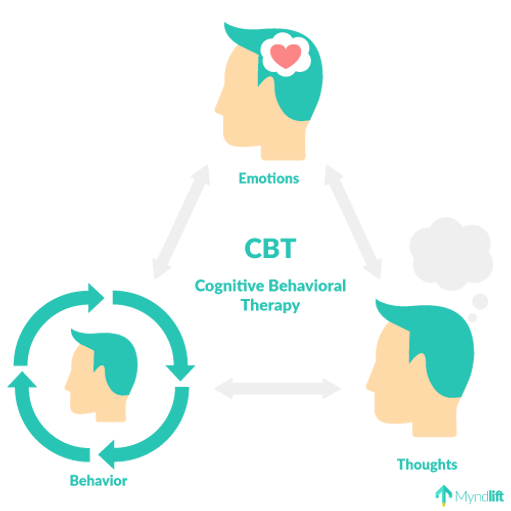
Parents and teachers work together on the Daily Report Card. Teachers choose goals for an individual child based on the behaviors that present the biggest challenges for them. Goals might involve academic work (finishing tasks), behavior towards peers (reducing teasing or fighting) and adherence to classroom rules (not interrupting, staying in their seat, following instructions). The teacher rates the child’s performance each day on each goal. They get a star or a check for each positive behavior, and if they get enough during the day, there is a prize for them when they get home—coveted screen time or some other small reward.
This kind of system can be very helpful for children from preschool to as old as 12.
For attention problems
The other broad area of behavioral help for kids with ADHD includes skills-based interventions to teach techniques they can use to stay on top of their schoolwork and manage their responsibilities at home. This kind of training, which is done by learning specialists, teaches kids skills to maximize their strengths and compensate for their weaknesses.
Children with ADHD tend to be weak in what we call “executive functioning.” Executive functions are the self-regulating skills that we all use to accomplish tasks, from getting dressed to doing homework. They include planning, organizing time and materials, making decisions, shifting from one situation to another, controlling our emotions and learning from past mistakes.
To bolster kids with weak skills in these areas, learning specialists teach a mix of specific strategies and alternative learning styles that complement or enhance a child’s particular abilities.
With elementary school children, the learning specialist usually works with parents and kids together, to establish routines and tools to use to get work done successfully and with minimal conflict. For instance:
- Checklists can be useful for anything from getting out of the house on time in the morning to doing homework after school to the bedtime routine. Since the steps necessary for completing a task often aren’t obvious to kids with ADHD, defining them clearly ahead of time, and posting them prominently, makes a task less daunting and more achievable.

- Educational therapists also recommend assigning a time limit for each step, particularly if it is a bigger, longer-term project. Deadlines can sneak up on all of us, but kids with ADHD are particularly susceptible to underestimating how long it will take to do something.
- Using a Planner is essential for Kids with ADHD who have what’s called poor working memory, which means it is hard for them to remember things like homework assignments.
- A rewards chart at home, as well as at school, can help motivate kids who are easily distracted and struggle to acquire new skills.
For middle and high school aged students, educational therapists work with kids to develop systems for tackling the work, both organizationally and academically. For kids with ADHD, managing their time and school materials can be a huge issue—not leaving enough time to study or complete projects, forgetting to use their planner, losing track of assignments. Materially, their backpacks may be a disaster, notes Michael Rosenthal, PhD, a neuropsychologist. Specific skills like studying, memorizing, note-taking, and doing assignments on time can all be addressed.
Materially, their backpacks may be a disaster, notes Michael Rosenthal, PhD, a neuropsychologist. Specific skills like studying, memorizing, note-taking, and doing assignments on time can all be addressed.
And executive functions apply to academics, as well as managing homework, explains Dr. Rosenthal. Reading, writing and math all involve skills kids may be weak in. A middle schooler might be a perfectly fluent reader, he explains, but at the same time have difficulty capturing the point of each paragraph or summarizing what they’ve read. Writing requires organizing thoughts into a narrative, imagining what the intended audience needs to know, staying on topic, and writing to a chosen length, among other skills. Math requires multi-step operations, and word problems require extracting the information important to solve the problem. These are all skills that educational therapists can focus on with children to strengthen their learning strategies.
Spelling out the rationale
While a child is learning new skills, they need to understand how they will help them. “Kids with attention problems, in particular, are very pragmatic in a way about how much effort to put into things,” explains Matthew Cruger, PhD, director of the Child Mind Institute’s Learning and Development Center. “We think of it as ‘neuroeconomics’ — they save their energy for things they are confident will pay off.” A good educational therapist will structure skill building so that kids score successes. “When kids put hard work into something, they expect a return, and if they don’t see the return, it’s doubly frustrating,” says Dr. Cruger. “They’ll think, ‘You see, it wasn’t a good idea to try.’”
“Kids with attention problems, in particular, are very pragmatic in a way about how much effort to put into things,” explains Matthew Cruger, PhD, director of the Child Mind Institute’s Learning and Development Center. “We think of it as ‘neuroeconomics’ — they save their energy for things they are confident will pay off.” A good educational therapist will structure skill building so that kids score successes. “When kids put hard work into something, they expect a return, and if they don’t see the return, it’s doubly frustrating,” says Dr. Cruger. “They’ll think, ‘You see, it wasn’t a good idea to try.’”
The frustrating thing about behavioral interventions like parent training and Daily Report Card is that they are labor-intensive for parents and teachers, in addition to the kids themselves. “Parents may have the preconception that when they bring a child for therapy the child is going to be doing the work,” notes Jill Emanuele, PhD, Senior Director of the Mood Disorders Center at the Child Mind Institute.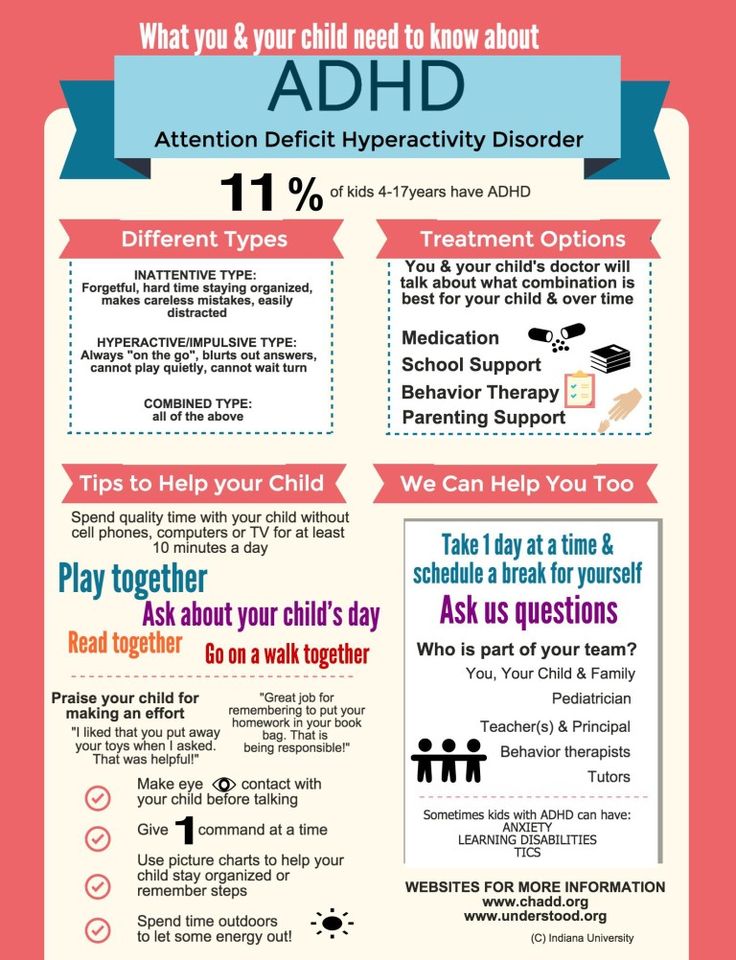 “But this takes a huge investment on the part of parents.” On the other hand, she adds, “the training can be a huge help to parents, too, who often come to us feeling burned out and ineffective in handling these kids. They develop a lot of confidence.”
“But this takes a huge investment on the part of parents.” On the other hand, she adds, “the training can be a huge help to parents, too, who often come to us feeling burned out and ineffective in handling these kids. They develop a lot of confidence.”
There is evidence that these parent and teacher-based interventions do improve the outcome for children with ADHD, though they don’t directly affect symptoms. “Ideally, these environmental adjustments will alter the developmental trajectory of the child or adolescent with ADHD,” explains ADHD specialist Russell Barkley, PhD. “However, such interventions are not expected to produce fundamental changes in the underlying deficits of ADHD, rather they only prevent an accumulation of failures and problems secondary to ADHD.”
The strongest gains, Dr. Barkley notes, are in children who are particularly defiant or oppositional. “Thus, researchers and clinicians should anticipate,” he notes, “that long-term studies are more likely to find treatment effects on problems secondary to ADHD than on deficits specific to ADHD.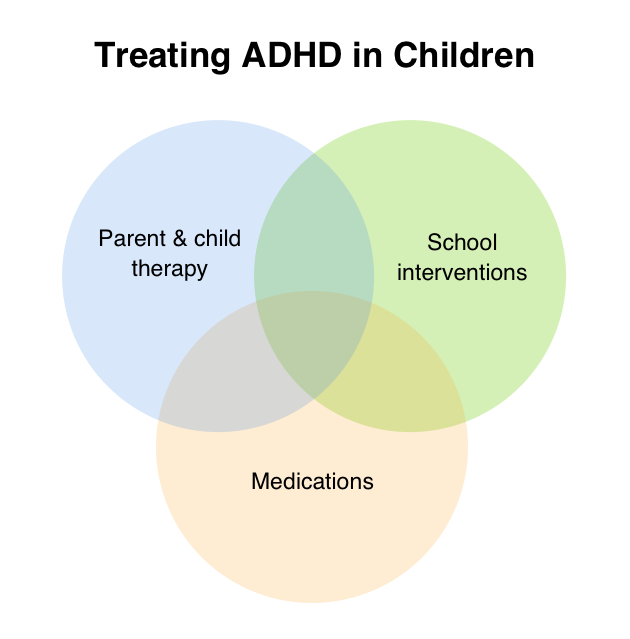 ”
”
Teenagers with ADHD
Once children with ADHD reach adolescence, there is less evidence for the effectiveness of behavioral training. Several studies have failed to show results for cognitive behavioral therapy for teens with ADHD, Dr. Barkley explains, but CBT does have a role for kids with ADHD who develop secondary problems like conduct disorder and oppositional defiant disorder.
And Dr. Emanuele notes that since ADHD puts kids at risk for developing an anxiety or mood disorder, many of them are treated with CBT for those disorders. In some cases, she notes, kids have actually outgrown their ADHD symptoms but they’re still struggling.
ADHD in adults - treatment, symptoms, diagnosis
Make an appointment
Treatment of ADHD in adults
Rehabilitation clinic "A NEW DAY" specializes in the treatment of adults with ADHD. We have developed and effectively applied a set of rehabilitation measures for ADHD.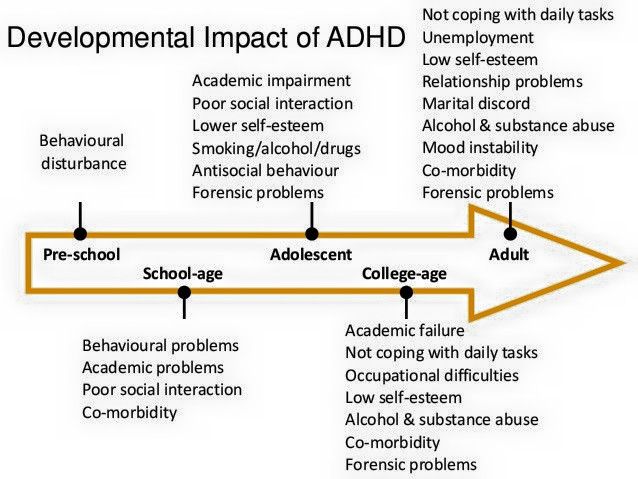
Individual approach
Each patient has his own doctor - a neurologist. He knows everything about the patient and his disease, if necessary, he can make adjustments to the course of treatment at any stage. The main thing is the result. At the end of the course of treatment, individually developed recommendations are issued. nine0006
Treatment is always a complex
Taking into account the variant of the course, the age of the patient, the severity of manifestations, the most appropriate methods and their combinations are selected: (BOS).
In everyday life, ADHD patients are not recommended to engage in those sports that involve a competitive nature and have a pronounced emotional component, for example, martial arts, team games. Useful jogging, swimming (non-competitive), cycling, skiing. nine0003
To improve the psychological and emotional state, reduce anxiety, overcome depression, sleep disorders, various methods of psychotherapy are used.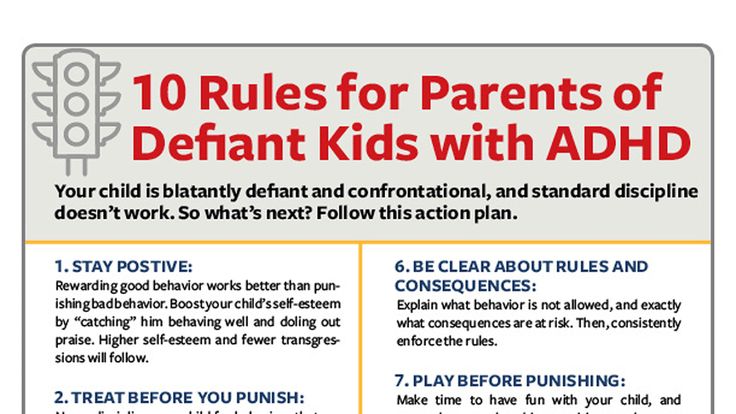 The choice of a technique suitable for a particular patient is carried out by a psychologist or psychotherapist.
The choice of a technique suitable for a particular patient is carried out by a psychologist or psychotherapist.
Relaxation techniques: special relaxation massages, relaxation sessions, medical treatment.
Cognitive training is used for attention deficit. Acupuncture (IRT) is traditionally used to restore the regulation of many organs, including the brain. nine0006
Innovative techniques
Translingual neurostimulation (TLNS) is an effect on the brain through the stimulation of tongue receptors. This is an advanced innovative technique, most effectively used in the treatment of diseases of the central nervous system, and as we know, ADHD belongs to such diseases. The use of TLNS allows you to restore the regulation of excitation-inhibition processes in a short time, which ultimately leads to an improvement in the course of ADHD, the best psychological and motor correction. In addition, TLNS has a positive effect on cognitive functions, such as concentration and memory, improves sleep, allowing the body to restore its neurotransmitter stores and have a good rest.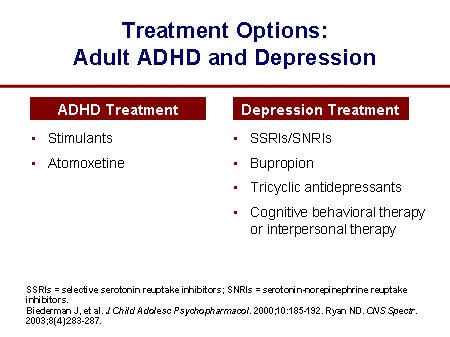 nine0006
nine0006
Continuity and recurrence
ADHD has a favorable course when properly treated. It is important to maintain the results achieved. To do this, at discharge, we give detailed individually developed recommendations. As long as there is any residual symptomatology, courses of treatment should be repeated, as a rule, 2-3 times a year.
Sign up for a consultation
Fill out the form
+7 (812) 603-70-10
Attention deficit disorder in adults
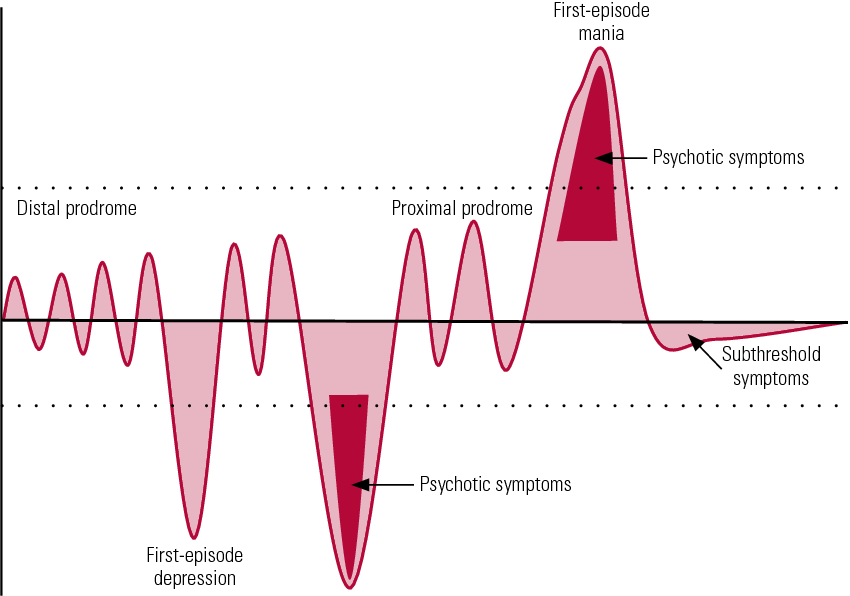
ADHD is a childhood-onset neurological behavioral disorder characterized by difficulty concentrating and maintaining attention, excessive motor activity (hyperactivity) and incontinence (impulsivity).
In recent years, the frequency of ADHD has increased, including among adults. It used to be thought that by adolescence, the symptoms of ADHD would significantly lessen or go away. However, now these ideas have changed: in 30-70% of cases, ADHD persists into adulthood.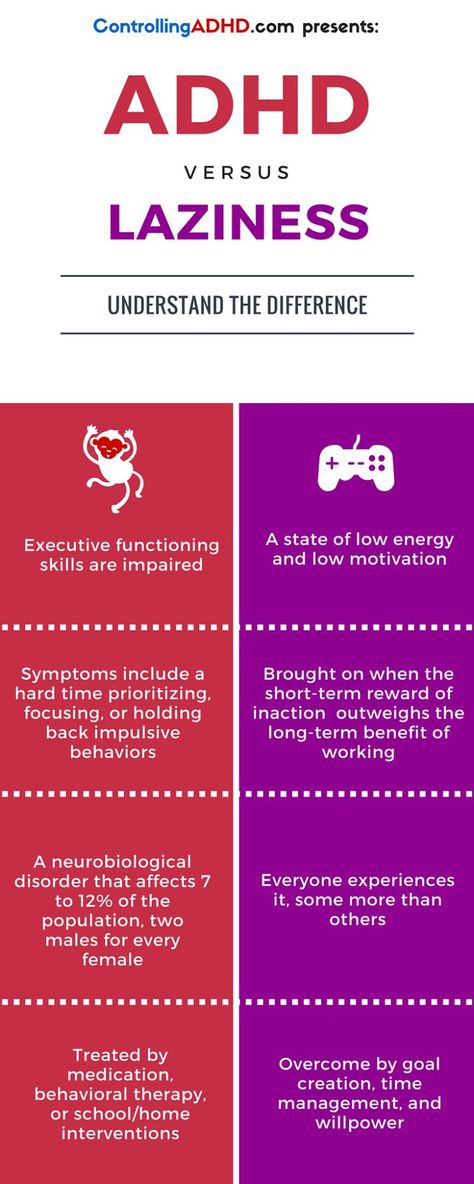 Most often this is due to insufficiently effective treatment in childhood. nine0006
Most often this is due to insufficiently effective treatment in childhood. nine0006
More about ADHD
All processes occurring in the nervous system are based on two oppositely directed mechanisms: excitation and inhibition. Normally they are balanced. However, the formation of the nervous system does not occur immediately after birth. The brain is mainly formed before the age of 8 years, but finally only by the age of 25. Therefore, in children, arousal and inhibition often get out of control, in some cases leading to ADHD. Over time, the brain matures and the symptoms of ADHD improve or go away on their own. But even in an adult, cognitive, behavioral, and motor
disorders resulting from ADHD. That is why the prevalence of ADHD in adults, although it has increased in recent years, still remains much less than in children.
In general, the manifestations in children and adults do not differ, but there are features.
First, if a child does not have ADHD, then an adult will not develop this disease. Therefore, ADHD in adults is not a separate disease, but disorders that have persisted since childhood.
Secondly, in adults, attention disorders prevail over manifestations of hyperactivity. It is difficult for such people to concentrate and maintain attention, so many activities that require concentration may not be available to them. Hyperactivity can be manifested by restlessness, so sedentary sedentary work is not suitable for them. nine0006 Impulsivity can be manifested by conflicts in the family and at work.
And thirdly, the presence of ADHD in adulthood requires careful examination to exclude other disorders, incl. mental illness.
Manifestations of ADHD depend on the course of the disease.
Types of ADHD in adults
-
With a predominance of attention deficit (deficit)
-
With a predominance of hyperactivity
-
Mixed version of ADHD
Symptoms of ADHD in adults
Symptoms of inattention (in at least 5 symptoms for at least 6 months):
- Inability to concentrate on details, errors of incorrect
- Inability to hold attention for a long time
- Often one gets the impression that he does not listen to spoken speech
- Inability to follow instructions, algorithms, for example, to fulfill conditions tasks
- Resistance to getting involved in tasks, avoiding or active resistance
- Frequent loss of things, especially those necessary to complete tasks
- Easy distractibility to extraneous stimuli or thoughts (“hovering” in thoughts)
- Routine forgetfulness (errands, chores, being late)
Symptoms of hyperactivity (in adults, at least 5 symptoms for at least 6 months):
- Constant movements in the hands, feet, fidgeting in a chair
- Getting up from a place
- Inability to sit still
- Inability to pass time calmly
- Constantly in motion, as if “wound9”, as if “attached a motor” 908088
- Answers a question without listening to the question itself
- Difficulty waiting in line
- permissions.
 nine0088
nine0088
These symptoms must reach a degree of severity that interferes with learning, communication, work. They should be observed both at home and in other places (at work, at a party, etc.). They should be noticed not only by relatives, but also by those around them.
An additional examination may be required to clarify the diagnosis and exclude other diseases that have similar symptoms:
- EEG (electroencephalography)
- Doppler ultrasonography0088
- Evoked potential (EP) method
- Psychotherapist's consultation
- Brain MRI
- Psychiatrist's consultation (if indicated)
)
– ADHD CR (expanded complex)
– Cognition CS (standard complex)
– Cognition CR (expanded complex)
– Psychotherapy ind. COP (complex standard)
– Psychotherapy ind. CR (advanced complex)
Comparative table of all programs
ADHD in adults - treatment, symptoms, diagnosis
Make an appointment
Treatment of ADHD in adults
with ADHD. We have developed and effectively applied a set of rehabilitation measures for ADHD.
Individual approach
Each patient has his own doctor - a neurologist. He knows everything about the patient and his disease, if necessary, he can make adjustments to the course of treatment at any stage. The main thing is the result. At the end of the course of treatment, individually developed recommendations are issued.
Treatment is always a complex
Taking into account the variant of the course, the age of the patient, the severity of manifestations, the most appropriate methods and their combinations are selected: (BOS). nine0003
In everyday life, ADHD patients are not recommended to engage in sports that involve a competitive nature and have a pronounced emotional component, for example, martial arts, team games. Useful jogging, swimming (non-competitive), cycling, skiing.
To improve the psychological and emotional state, reduce anxiety, overcome depression, sleep disorders, various methods of psychotherapy are used. The choice of a technique suitable for a particular patient is carried out by a psychologist or psychotherapist. nine0003
The choice of a technique suitable for a particular patient is carried out by a psychologist or psychotherapist. nine0003
Relaxation techniques: special relaxation massages, relaxation sessions, medical treatment.
Cognitive training is used for attention deficit. Acupuncture (IRT) is traditionally used to restore the regulation of many organs, including the brain.
Innovative techniques
Translingual neurostimulation (TLNS) is an effect on the brain through the stimulation of tongue receptors. This is an advanced innovative technique, most effectively used in the treatment of diseases of the central nervous system, and as we know, ADHD belongs to such diseases. The use of TLNS allows you to restore the regulation of excitation-inhibition processes in a short time, which ultimately leads to an improvement in the course of ADHD, the best psychological and motor correction. In addition, TLNS has a positive effect on cognitive functions, such as concentration and memory, improves sleep, allowing the body to restore its neurotransmitter stores and have a good rest. nine0006
nine0006
Continuity and recurrence
ADHD has a favorable course when properly treated. It is important to maintain the results achieved. To do this, at discharge, we give detailed individually developed recommendations. As long as there is any residual symptomatology, courses of treatment should be repeated, as a rule, 2-3 times a year.
Sign up for a consultation
Fill out the form
+7 (812) 603-70-10
Attention deficit disorder in adults
ADHD is a childhood-onset neurological behavioral disorder characterized by difficulty concentrating and maintaining attention, excessive motor activity (hyperactivity) and incontinence (impulsivity).
In recent years, the frequency of ADHD has increased, including among adults. It used to be thought that by adolescence, the symptoms of ADHD would significantly lessen or go away. However, now these ideas have changed: in 30-70% of cases, ADHD persists into adulthood.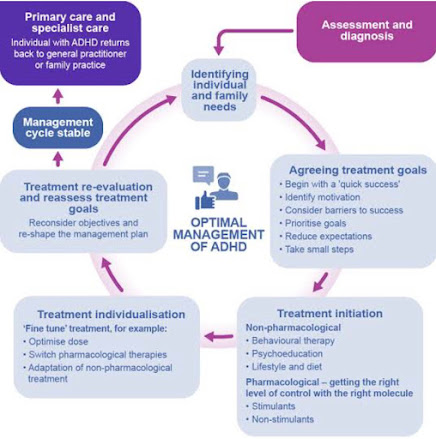 Most often this is due to insufficiently effective treatment in childhood. nine0006
Most often this is due to insufficiently effective treatment in childhood. nine0006
More about ADHD
All processes occurring in the nervous system are based on two oppositely directed mechanisms: excitation and inhibition. Normally they are balanced. However, the formation of the nervous system does not occur immediately after birth. The brain is mainly formed before the age of 8 years, but finally only by the age of 25. Therefore, in children, arousal and inhibition often get out of control, in some cases leading to ADHD. Over time, the brain matures and the symptoms of ADHD improve or go away on their own. But even in an adult, cognitive, behavioral, and motor
disorders resulting from ADHD. That is why the prevalence of ADHD in adults, although it has increased in recent years, still remains much less than in children.
In general, the manifestations in children and adults do not differ, but there are features.
First, if a child does not have ADHD, then an adult will not develop this disease. Therefore, ADHD in adults is not a separate disease, but disorders that have persisted since childhood.
Secondly, in adults, attention disorders prevail over manifestations of hyperactivity. It is difficult for such people to concentrate and maintain attention, so many activities that require concentration may not be available to them. Hyperactivity can be manifested by restlessness, so sedentary sedentary work is not suitable for them. nine0006 Impulsivity can be manifested by conflicts in the family and at work.
And thirdly, the presence of ADHD in adulthood requires careful examination to exclude other disorders, incl. mental illness.
Manifestations of ADHD depend on the course of the disease.
Types of ADHD in adults
-
With a predominance of attention deficit (deficit)
-
With a predominance of hyperactivity
-
Mixed version of ADHD
Symptoms of ADHD in adults
Symptoms of inattention (in at least 5 symptoms for at least 6 months):
- Inability to concentrate on details, errors of incorrect
- Inability to hold attention for a long time
- Often one gets the impression that he does not listen to spoken speech
- Inability to follow instructions, algorithms, for example, to fulfill conditions tasks
- Resistance to getting involved in tasks, avoiding or active resistance
- Frequent loss of things, especially those necessary to complete tasks
- Easy distractibility to extraneous stimuli or thoughts (“hovering” in thoughts)
- Routine forgetfulness (errands, chores, being late)
Symptoms of hyperactivity (in adults, at least 5 symptoms for at least 6 months):
- Constant movements in the hands, feet, fidgeting in a chair
- Getting up from a place
- Inability to sit still
- Inability to pass time calmly
- Constantly in motion, as if “wound9”, as if “attached a motor” 908088
- Answers a question without listening to the question itself
- Difficulty waiting in line
- permissions.
Learn more