Am i manic depressive or bipolar
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid.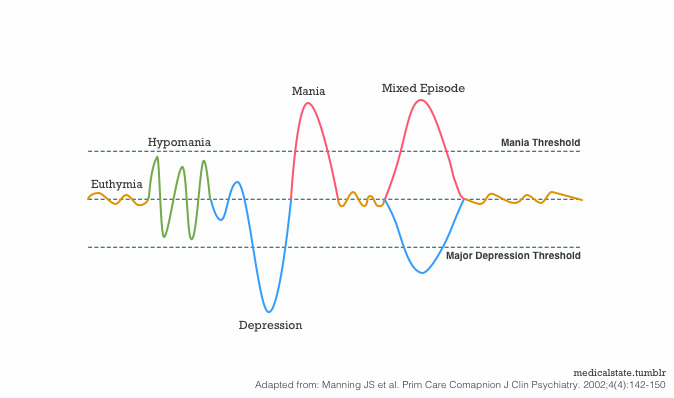 If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery.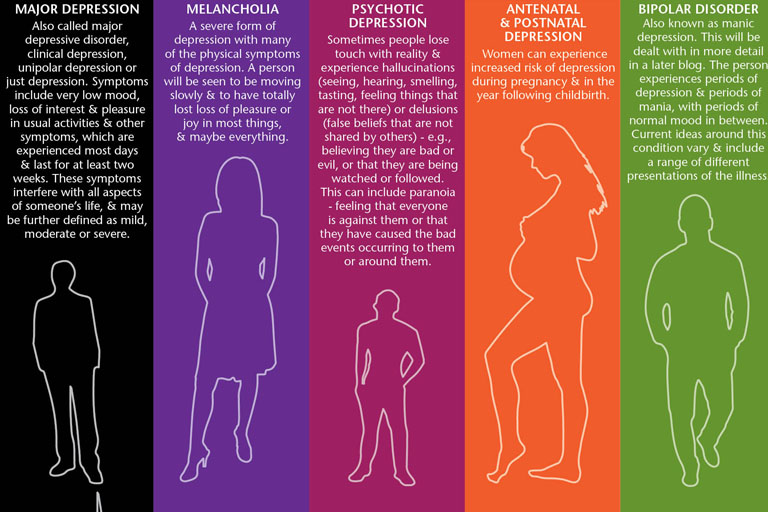 Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.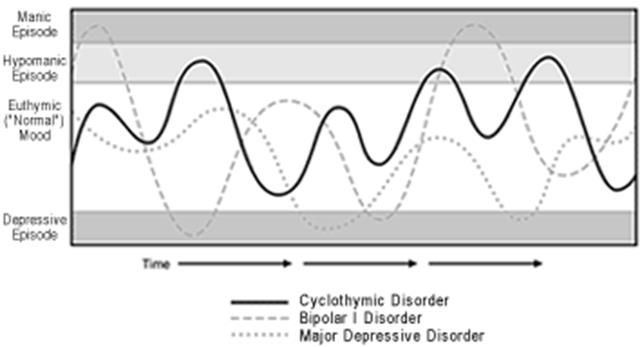
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.
-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly. Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Bipolar Disorder | Symptoms, complications, diagnosis and treatment
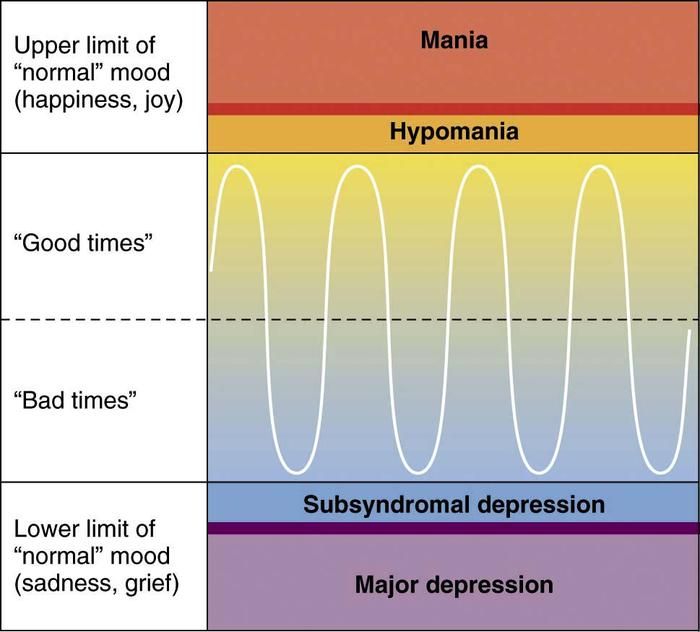
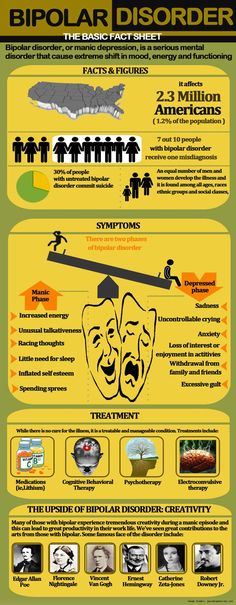
Bipolar disorder, formerly called manic depression, is a mental health condition that causes extreme mood swings that include emotional highs (mania or hypomania) and lows (depression). Episodes of mood swings may occur infrequently or several times a year.
When you become depressed, you may feel sad or hopeless and lose interest or pleasure in most activities. When the mood shifts to mania or hypomania (less extreme than mania), you may feel euphoric, full of energy or unusually irritable.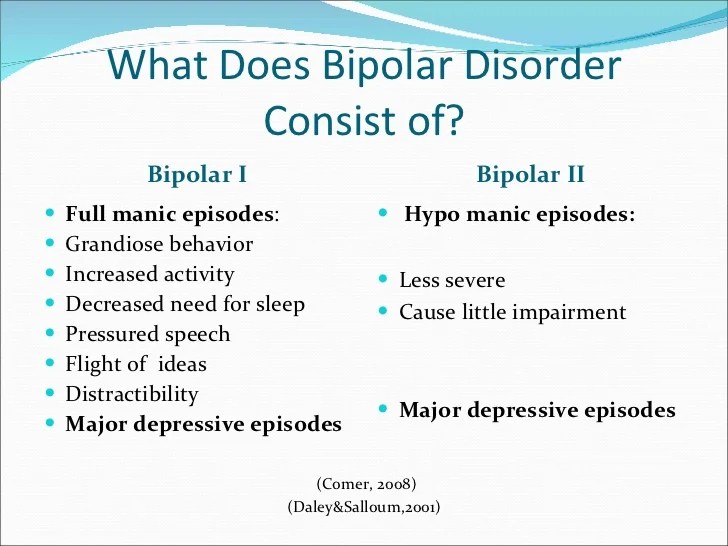 These mood swings can affect sleep, energy, alertness, judgment, behavior, and the ability to think clearly. nine0003
These mood swings can affect sleep, energy, alertness, judgment, behavior, and the ability to think clearly. nine0003
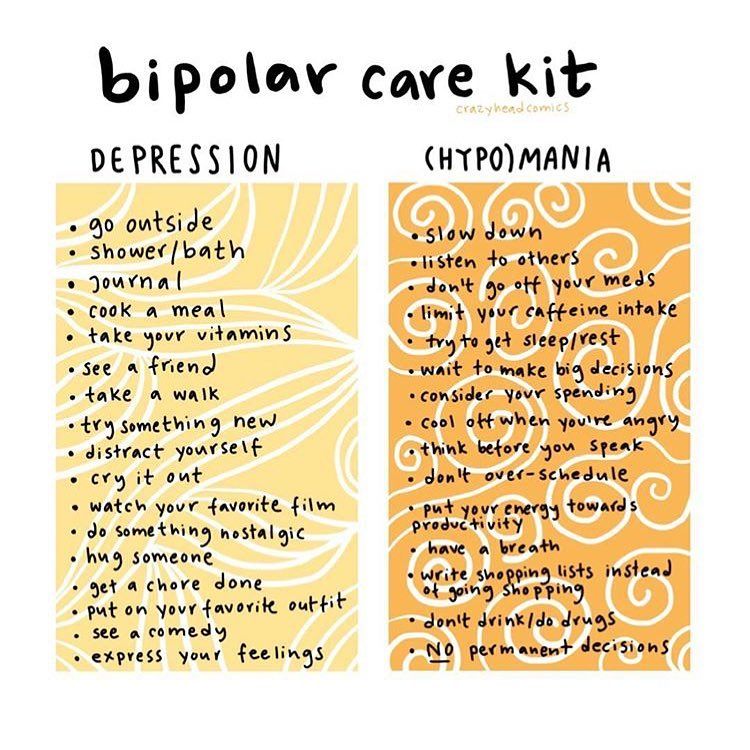
Although bipolar disorder is a lifelong condition, you can manage your mood swings and other symptoms by following a treatment plan. In most cases, bipolar disorder is treated with medication and psychological counseling (psychotherapy).
Symptoms
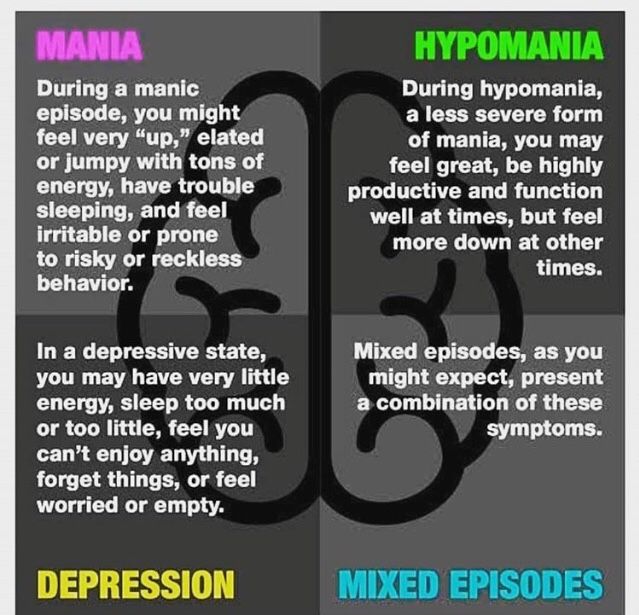
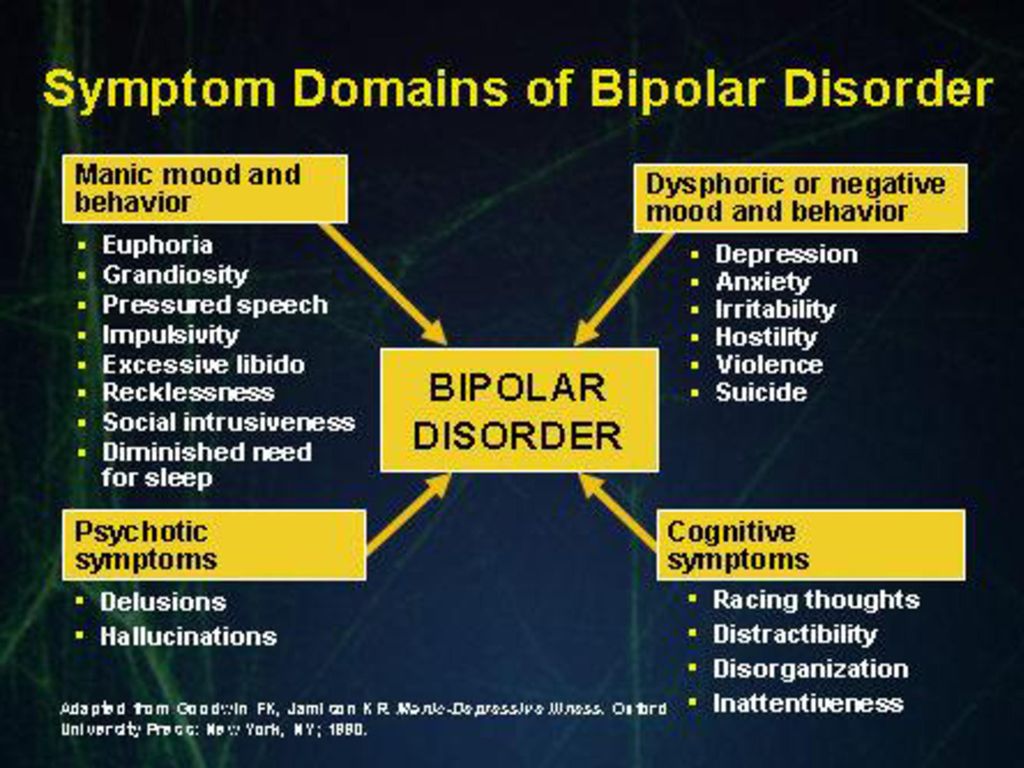
There are several types of bipolar and related disorders. These may include mania, hypomania, and depression. The symptoms can lead to unpredictable changes in mood and behavior, leading to significant stress and difficulty in life. nine0003
- Bipolar disorder I. You have had at least one manic episode, which may be preceded or accompanied by hypomanic or major depressive episodes. In some cases, mania can cause a break with reality (psychosis).
- Bipolar disorder II. You have had at least one major depressive episode and at least one hypomanic episode, but never had a manic episode.
 nine0015 Cyclothymic disorder. You have had at least two years - or one year in children and adolescents - many periods of hypomanic symptoms and periods of depressive symptoms (though less severe than major depression).
nine0015 Cyclothymic disorder. You have had at least two years - or one year in children and adolescents - many periods of hypomanic symptoms and periods of depressive symptoms (though less severe than major depression). - Other types. These include, for example, bipolar and related disorders caused by certain drugs or alcohol, or due to health conditions such as Cushing's disease, multiple sclerosis, or stroke. nine0018
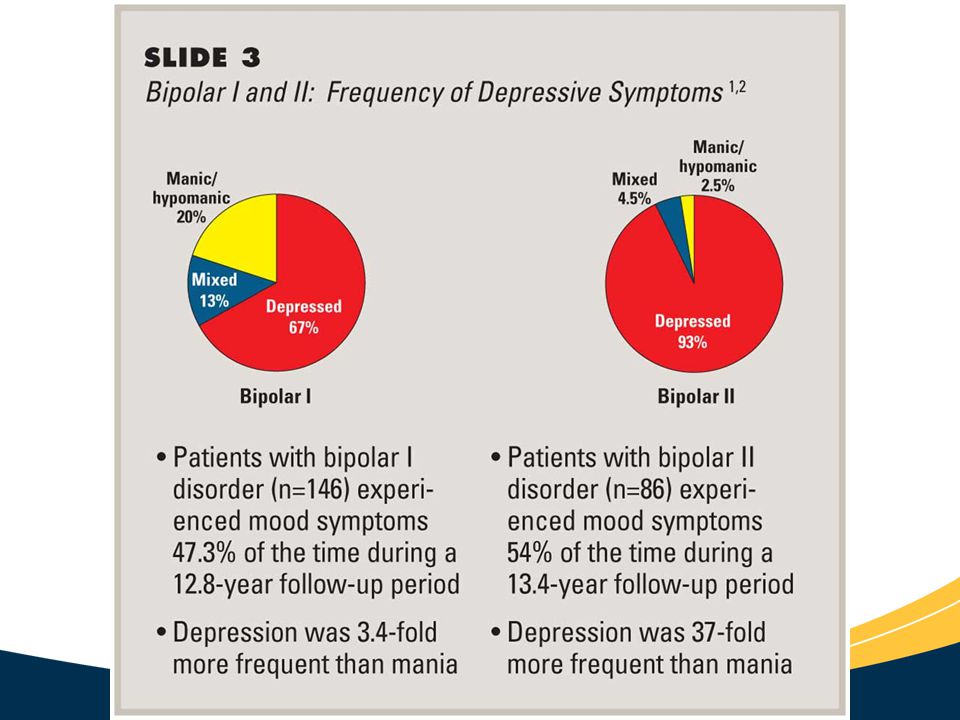
Bipolar II is not a milder form of Bipolar I but is a separate diagnosis. Although bipolar I manic episodes can be severe and dangerous, people with bipolar II can be depressed for longer periods of time, which can cause significant impairment.
Although bipolar disorder can occur at any age, it is usually diagnosed in adolescence or early twenties. Symptoms can vary from person to person, and symptoms can change over time. nine0003
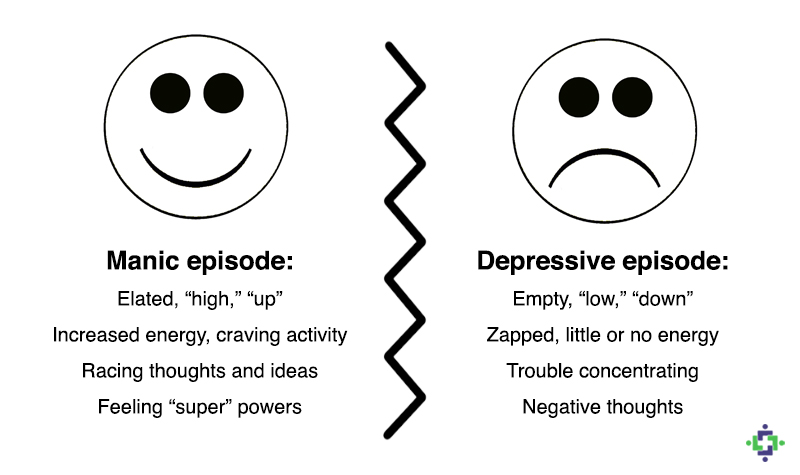
Mania and hypomania
Mania and hypomania are two different types of episodes, but they share the same symptoms.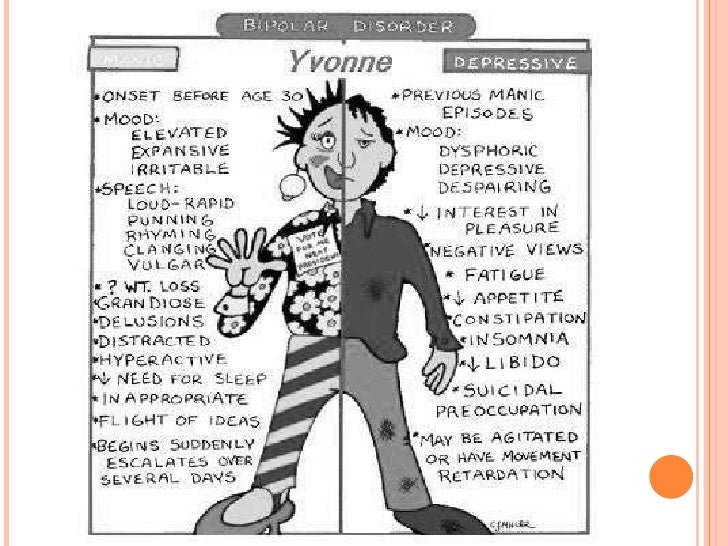 Mania is more pronounced than hypomania and causes more noticeable problems at work, school, and social activities, as well as relationship difficulties. Mania can also cause a break with reality (psychosis) and require hospitalization.
Mania is more pronounced than hypomania and causes more noticeable problems at work, school, and social activities, as well as relationship difficulties. Mania can also cause a break with reality (psychosis) and require hospitalization.
Both a manic episode and a hypomanic episode include three or more of these symptoms:
- Abnormally optimistic or nervous
- Increased activity, energy or excitement
- Exaggerated sense of well-being and self-confidence (euphoria)
- Reduced need for sleep
- Unusual talkativeness
- Distractibility
- Poor decision-making - for example, in speculation, in sexual encounters or in irrational investments
Major depressive episode
Major depressive episode includes symptoms that are severe enough to cause noticeable difficulty in daily activities such as work, school, social activities, or relationships. Episode includes five or more of these symptoms:
- Depressed mood, such as feeling sad, empty, hopeless, or tearful (in children and adolescents, depressed mood may manifest as irritability)
- Marked loss of interest or feeling of displeasure in all (or nearly all) activities
- Significant weight loss with no diet, weight gain, or decreased or increased appetite (in children, failure to gain weight as expected may be a sign of depression)
- Either insomnia or sleeping too much
- Either anxiety or slow behavior
- Fatigue or loss of energy nine0015 Feelings of worthlessness or excessive or inappropriate guilt
- Decreased ability to think or concentrate, or indecisiveness
- Thinking, planning or attempting suicide
Other features of bipolar disorder
Signs and symptoms of bipolar I and bipolar II disorder may include other signs such as anxiety disorder, melancholia, psychosis, or others.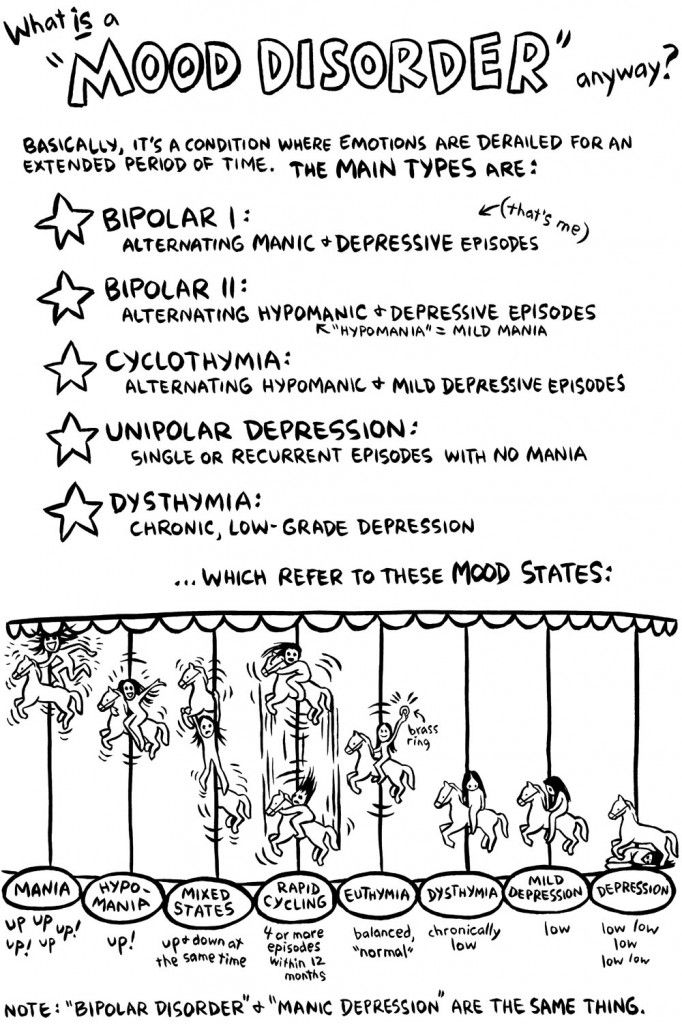 The timing of symptoms may include diagnostic markers such as mixed or fast cycling. In addition, bipolar symptoms may occur during pregnancy or with the change of seasons. nine0003
The timing of symptoms may include diagnostic markers such as mixed or fast cycling. In addition, bipolar symptoms may occur during pregnancy or with the change of seasons. nine0003
When to see a doctor
Despite extreme moods, people with bipolar disorder often do not realize how much their emotional instability disrupts their lives and the lives of their loved ones and do not receive the necessary treatment.
And if you are like people with bipolar disorder, you can enjoy feelings of euphoria and be more productive. However, this euphoria is always accompanied by an emotional disaster that can leave you depressed and possibly in financial, legal, or other bad relationships. nine0003
If you have symptoms of depression or mania, see your doctor or mental health professional. Bipolar disorder does not improve on its own. Getting mental health treatment with a history of bipolar disorder can help control your symptoms.
Bipolar disorder or manic-depressive psychosis: description, diagnosis, treatment, prevention in Israel
During the off-season, people with a tendency to various mental disorders have an increased risk of an initial episode of the disease or a relapse of the disease.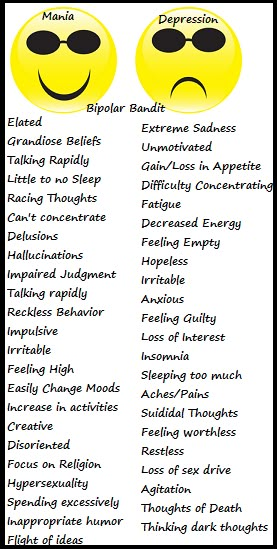 Patients with bipolar disorder, or manic-depressive psychosis, should be especially attentive to their condition. The disease is manifested by the alternation of opposite phases - mania and depression. If mania is hyperactivity, talkativeness, energy and little sleep, then depression is the opposite condition, characterized by complete apathy and reduced functioning. nine0003
Patients with bipolar disorder, or manic-depressive psychosis, should be especially attentive to their condition. The disease is manifested by the alternation of opposite phases - mania and depression. If mania is hyperactivity, talkativeness, energy and little sleep, then depression is the opposite condition, characterized by complete apathy and reduced functioning. nine0003
Submit an application for diagnosis and treatment
I confirm that I accept the terms of consent to the processing of personal data.
Bipolar disorder, manic-depressive psychosis manifests itself in intense mood swings: mania and depression, which can follow each other or alternate with periods of remission, the frequency, duration and change of episodes depends on the individual characteristics of the person. Approximately one percent of the population suffers from bipolar disorder. The disease, as a rule, develops in adolescence or socially active age (15-30 years), although cases of the onset of the disease at 40 years and older have sometimes been recorded.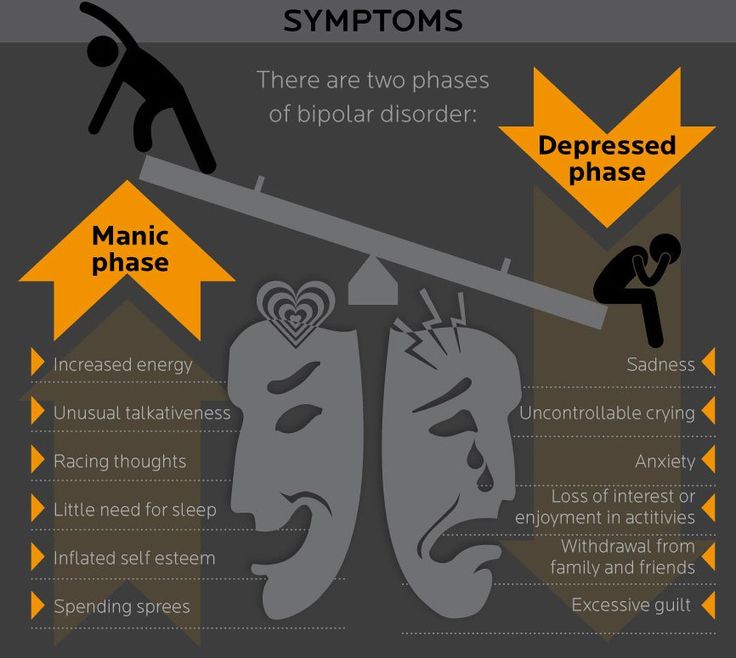 Episodes of mania or depression last approximately 3-7 months, with depressive phases much longer than manic phases. The change of phases can be correct or incorrect, they can alternate with periods of intermission, in addition, the disorder can be expressed in only one episode: manic or depressive. nine0003
Episodes of mania or depression last approximately 3-7 months, with depressive phases much longer than manic phases. The change of phases can be correct or incorrect, they can alternate with periods of intermission, in addition, the disorder can be expressed in only one episode: manic or depressive. nine0003
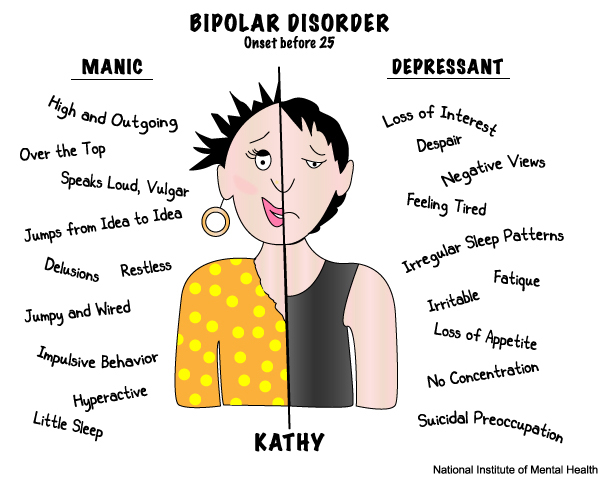
Manic phase
There is a so-called "triad of signs" of the manic phase: increased motor activity, ideational-psychic excitement and elevated mood. The manic stage of bipolar disorder in its development goes through the following stages:
- Hypomanic, during which a person feels an emotional and physical uplift, motor excitation increases, speech accelerates, appetite increases, the amount of sleep decreases. nine0018
- Severe mania. Symptoms grow and worsen, speech becomes faster, patients laugh, joke, sometimes there are outbursts of anger, a series of ideas. The distractibility increases, and therefore it is problematic to maintain a conversation with the patient.
 Delusions of grandeur develop, the patient often invests in unprofitable projects. Due to increased excitability, a person cannot sleep, and the amount of sleep is reduced to 3-4 hours a day.
Delusions of grandeur develop, the patient often invests in unprofitable projects. Due to increased excitability, a person cannot sleep, and the amount of sleep is reduced to 3-4 hours a day. - Manic frenzy. The peak of the increase in manic symptoms: incoherent, fragmentary, meaningless speech, abrupt and erratic movements. nine0018
- Motor sedation. Motor excitation subsides, although speech excitation and elevated mood, laughter remain at the same level.
- Reactive stage. The symptomatology of mania fades and stops at a level slightly below the norm, in connection with which the person feels asthenia, slight motor and ideational retardation, and some episodes of severe mania may be forgotten.
Depending on the severity of symptoms, the following types of mania are distinguished
- Hypomania (mild form), characterized by a slight increase in activity and energy, a slight rise in mood, a sense of mental and physical productivity, increased social activity, talkativeness, familiarity, absent-mindedness, hypersexuality appear.
 Occasionally, instead of an elevated mood, anger and irritability appear. The stage lasts a couple of days.
Occasionally, instead of an elevated mood, anger and irritability appear. The stage lasts a couple of days. - Mania without psychotic symptoms (moderate) is characterized by markedly elevated mood, speech pressure, severe hyperactivity, euphoric mood, insomnia, and ideas of grandeur appear. In some cases, irritation and aggression are manifested. The episode lasts about a week and leads to a complete disruption of social activity and performance. nine0018
- Mania with psychotic features (severe form), characterized by uncontrolled psychomotor agitation with violence and aggression. Delusions of grandeur or persecution develop, speech becomes incomprehensible, jumps of thoughts are observed, hallucinations occur.
Depressive phase
The bipolar depressive phase of manic-depressive disorder has its own triad of symptoms that are exactly the opposite of the manic phase: slow thinking, depressed mood and motor inhibition.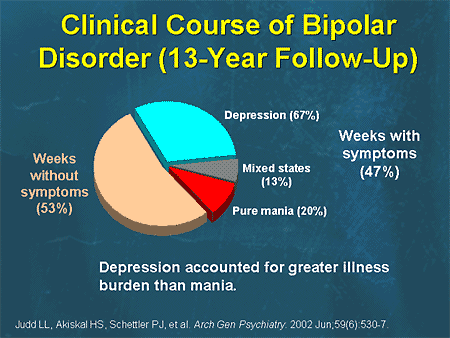 Stages of the depressive phase
Stages of the depressive phase
- Initial. It is characterized by a gradual weakening of working capacity, both mental and physical, a decrease in mood, sleep disorders (insomnia)
- Increasing depression. Symptoms worsen, mood decreases, anxiety, motor retardation, significant loss of appetite appear. Mental and physical performance is sharply reduced. Speech becomes slow and laconic. The insomnia gets worse.
- Severe depression. The triad of depressive symptoms reaches its peak. There are attacks of anxiety and melancholy, which are difficult to tolerate by patients. Speech slows down sharply, becomes quiet, answers to questions are given with a delay and monosyllabic. Appetite is lost, the risk of anorexia increases. Severe motor retardation, often depressive stupor, during which patients can stay in one position for a long time (sit or lie down). Persistent delusional ideas of one's own sinfulness, immorality, self-abasement or self-accusation develop. Suicidal thoughts, suicide attempts or actions may appear, they are most dangerous at the beginning and at the end of the development of this stage, when motor inhibition weakens.
 Sometimes there are auditory hallucinations in the form of accusing voices with recommendations to commit suicide. nine0018
Sometimes there are auditory hallucinations in the form of accusing voices with recommendations to commit suicide. nine0018 - Reactive. Symptoms subside, mood and motor activity increase.
Depending on the severity and composition of symptoms, there are the following options for the development of the depressive stage:
- Simple depression is a classic triad of symptoms, not aggravated by delirium;
- Hypochondriacal - depression, aggravated by hypochondriacal delirium, when a person believes that he is ill, possibly fatally, this is a state of a kind of "falling in love with the disease."
- Delusional depression, or Qatar syndrome - large-scale, grotesque delusions of a hypochondriacal or nihilistic nature, against the background of an anxious and dreary mood. A person believes that he is rotting, that he has infected all of humanity with some kind of disease, that he has no heart, and so on.
- Agitated - a classic triad of signs with mild motor retardation or with a complete absence of motor retardation.
- Anesthetic depression with a symptom of loss of mental sensitivity, when patients claim that they have lost the ability to love, rejoice and have become insensible, in connection with this they feel acute mental pain. nine0018
Bipolar disorder (manic depressive psychosis) diagnosis
Until recently, it was believed that bipolar disorder (manic depressive syndrome) is a very rare disease and difficult to diagnose. In Israel, for the diagnosis of bipolar disorder, the internationally recognized ICD-10 classification is used, according to which an episode of an affective disorder is recognized as a severe mood disorder for 1 week (for mania) and 2 weeks (for depression). Bipolar disorder (manic depressive psychosis), for the diagnosis of which screening tables, questionnaires and tests are used, which allows the doctor to establish an accurate diagnosis and prescribe treatment. nine0003
Bipolar disorder (manic depressive psychosis) treatment methods
Early contact with the center and diagnosis of the disease after the first phase significantly improves the prognosis of the course of the disease and reduces the treatment time.