Attention seeking disorder symptoms in children
Attention Seeking Behaviour in Children
Attention is a basic human requirement, which arises from attachment. Thus, every child craves attention, especially from their parents. Due to today’s culture of work and hustle, most parents are unable to spend quality time with their children. As a result, a child can feel left out. Feeling left out leads to attention-seeking behaviour, and it can even strengthen such existing behaviour. Read on to learn about attention-seeking behaviour in children, and how to put an end to it.
Video : Attention Seeking Behaviour in Children – Causes and How to Deal with It
What Is Attention-Seeking Behaviour in a Child?
Have you ever faced problems with your child, such as lying down in the shop because he wants a specific toy, or causing a scene at the park amidst other siblings by stealing ice cream, or bullying other kids? These are examples of attention-seeking behaviour, and sometimes it goes to an extreme, to the point where you get glares and glances from outsiders and other parents.
Other signs of negative attention-seeking behaviour in children are –
- Faking illnesses to get some of your time
- Causing drama or throwing tantrums at home or in public settings
- Causing harm to others and trying to play hero
- Creating problems that make one parent argue with the other
- Playing the victim by magnifying the proportion of simple, everyday problems
- Showing that they are super busy and completing everything on time, or before
How Much Attention Is Enough for Your Child?
How much attention is enough for your child will depend on the child’s personality, behaviour, and daily routine. Your child may feel satisfied with the attention he receives at home, but may be disappointed in the classroom, in which case, you may need to talk to the school counsellor or concerned teachers to make room for opportunity to shine by asking questions and encouraging participation in group discussions.
Giving your child 100% of your attention at home for at least some time of the day, fully and uninterrupted, is highly recommended. The reason behind this is if you don’t spare your attention for your children, they may end up causing temper tantrums or throw fits in other settings to cause a scene.
Types of Attention
There are different types of attention-seeking behaviours. However, just like behaviours, there are ways of approval and rewards that come with adult attention. They are listed below.
1. Positive Attention
If you find your child doing something good, give him words of encouragement, or reinforce that action with positive rewards. This is called positive attention. A pat on the back, a gentle hug, words of praise, and small smiley doodles or notes in their notebooks or lunch boxes work just as well.
2. Negative Attention
When your child misbehaves, and you get upset as a result, you might scold him. This attention that you are now giving your child is called negative attention. This can be in the form of scoldings, lectures, or punishments. If your child is actively seeking attention from you, this type of negative attention will not serve to reduce instances of his misbehaviour, but will instead increase it. Thus, it will turn into a cycle of constant mischief and constant negative attention from you.
This can be in the form of scoldings, lectures, or punishments. If your child is actively seeking attention from you, this type of negative attention will not serve to reduce instances of his misbehaviour, but will instead increase it. Thus, it will turn into a cycle of constant mischief and constant negative attention from you.
3. No Attention
No attention is when you aren’t paying attention when your child is doing something good; it means that you pay attention only when your child is misbehaving, and you are missing his positive-attention behaviour. For example, two brothers who are usually messy or destructive in behaviour are quietly watching TV together. Their parents don’t acknowledge or respond to this positive change. This is an example of paying no attention. On the other hand, if the brothers do misbehave again, the parents are quick to notice and respond with scolding.
Emotional Issues Behind Your Child’s Attention-Seeking Behaviour
The emotional issues or causes of attention-seeking behaviour in children are –
- Your child has trouble making friends at school.
- He doesn’t get enough attention from you at home.
- He feels lonely or left out amidst other siblings.
- He feels ignored due to parents being busy or working too much.
- He doesn’t get enough attention at school or in other social settings.
- Past experiences or trauma.
How to Deal with Attention-Seeking Behaviour in Kids
Here are tips for dealing with attention-seeking behaviour, or learning how to stop this behaviour in children –
- Give more positive attention.
Help your kids lend a hand with your kitchen chores, or praise them for spending time with themselves quietly, like watching TV, or drawing. If they have talents, ask them to practice them, and praise them for putting effort into it.
- Ignore bad behaviour.
Bad behaviour comes with no rewards. Make that known through your ignorance to your child’s whines and tantrums. In time, he will realise that, and slowly change his behaviour for the better.
- Give options.
Giving your child options will make them feel seen by you. Providing options also helps if he throws tantrums during simple tasks, such as dressing himself, or eating his meals. You can ask him what he would like to wear today, or what dessert he would like to eat after he has finished his vegetables.
- Give alone time.
Set aside 5 to 10 minutes of uninterrupted alone time that your child can spend with you and your spouse each, separately. Before bedtime, or any time that both you and your spouse can freely spare, can work.
Do’s and Don’ts for Parents of Children with Attention-Seeking Behaviours
Below we have some do’s and don’ts of dealing with attention-seeking behaviour in kids –
Do’s
- Try to ignore. If your child is screaming or yelling or simply causing a ruckus verbally, don’t be afraid to tell him that he won’t be given chocolate or extra TV time because of his actions, and that you’ll hear him out once he calms down.
- Create a rules list. List out the rules of the house, and consequences for breaking each. For screaming, it could be 10 minutes cut from normal TV time, and for making a mess, it could be going to bed early, and so on. Create this chart with your kid, and hang it up at eye level in a place where he can see it regularly. Stick to this chart no matter what, and you’ll slowly notice your child making changes in his behaviour.
- Give attention mindfully. This is not to say that the rules cut out attention from your side. Come together as a family for dinners, conversations, and bedtime reading. Do little things that bring joy to your child’s daily life, but remember to enforce the rules and be consistent about playing out the consequences when the rules are broken. Your child will only take the rules seriously if you’re consistent and serious from your end.
Don’ts
- Scream. It’s natural to feel angry or frustrated, but never lash out at your kids by screaming or losing emotional control from your end.
 Whenever you feel like you’ll lose your cool, feel free to move away and take a break. Don’t be afraid to tell your child that you’re taking a break because you’re not in a state to handle his whining currently, and will be back after a few minutes after he quietens down. Practice deep breathing exercises, and meditate for a few minutes every day to be calm and composed.
Whenever you feel like you’ll lose your cool, feel free to move away and take a break. Don’t be afraid to tell your child that you’re taking a break because you’re not in a state to handle his whining currently, and will be back after a few minutes after he quietens down. Practice deep breathing exercises, and meditate for a few minutes every day to be calm and composed.
- Guilt-trip your kids. Don’t make them feel guilty, or emotionally blackmail them. If you feel out of it, just tell your child you’re tired after a day’s work, and won’t be able to resolve his situation today since you don’t have the energy to do so. Make it clear that you won’t be able to keep him company on that day if he continues whining or yelling, and move out of the room instead. Even kids have feelings; they will surely understand.
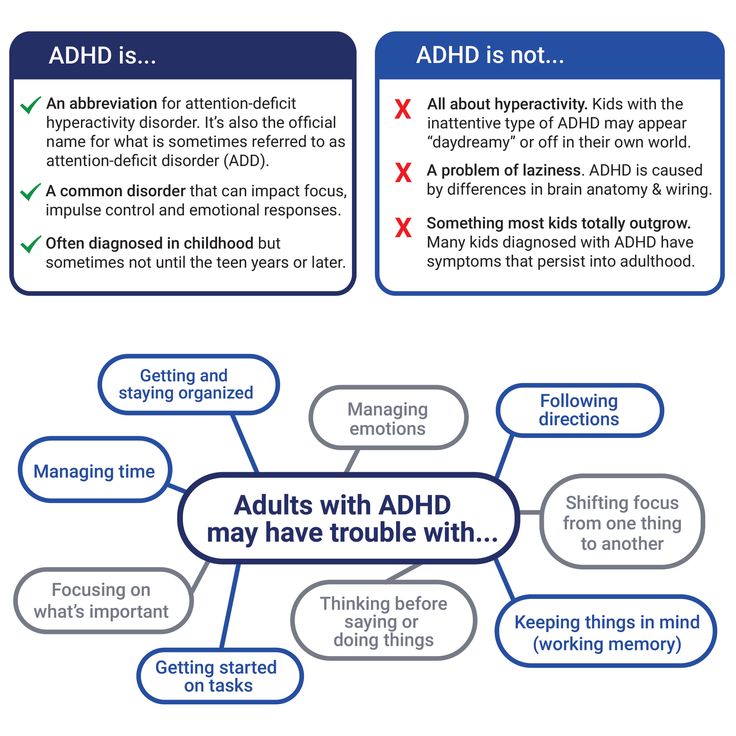
- Think that it’s a clinical disorder. Most parents think that their kids’ temper tantrums are linked to ADHD or other medical disorders.
 Don’t assume that. Sometimes it’s perfectly normal for kids to scream and yell, since they are at that stage of development in their lives. However, if your child is cutting himself or participating in dangerous situations, or causing harm, then seek out a medical specialist for help.
Don’t assume that. Sometimes it’s perfectly normal for kids to scream and yell, since they are at that stage of development in their lives. However, if your child is cutting himself or participating in dangerous situations, or causing harm, then seek out a medical specialist for help.
And, that’s it! Just try out the tips above, and keep these pointers in mind to fix attention seeking behaviour in children in school and home, and we’re sure you’ll notice positive changes soon. And remember the magic word – time!
Also Read: Common Toddler Behavior Problems & Solutions
Child Who's Acting Out: Causes and What to Do
Behavior is communication. If you have a child acting out for attention, what are they trying to say?
When children seek attention, they might not express this need in ways you’d expect. Instead, sometimes they behave as if they’re trying to push you away. This can be a sign that they need your support more than ever.
Understanding the root of your child’s attention-seeking behavior can make it easier for you to help them.
Children depend on adults for care and security, so it’s only natural they seek your attention. While good behavior is the goal, sometimes they act out depending on their age and level of development.
There are many reasons for a child’s behavior to escalate, such as an issue with their environment or past. Or they could have a brain-based difference affecting their behavior.
Examples include:
- boredom
- loneliness or irritability
- attention deficit hyperactivity disorder (ADHD)
- trauma
- a mental health condition
What if your behaviors are causing your child to act out?
Research from 2017 suggests that parents’ use of technology can interrupt their interactions with their children. These interruptions are connected to children’s behavioral issues.
Technology is so weaved into many aspects of life that it’s inevitable children will see their parents using devices. You could skip social media for a day, but you still might need to read email or do some urgent banking.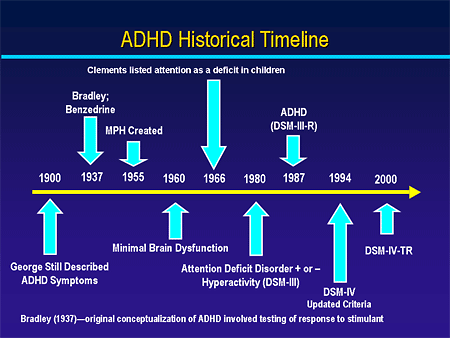
You’re not alone. This type of media use is common.
Research published in 2019 suggests that multitasking with technology while parenting may be connected to:
- less parental responsiveness, attention, and sensitivity
- increased hostility
- harmful behaviors in children
- behavior in children that’s less attentive
- interruptions to parent-child interactions
If a child must compete with technology for their parent’s attention, acting out might be a strategy that gets results.
Signs of negative attention-seeking behavior
Your child exhibits signs of negative attention-seeking behavior when they:
- raise their voice
- interrupt, defy, or ignore adults
- yell, cry
- run away
- push, shove, hit, kick
- destroy items accidentally or deliberately
The cause of your child’s behavior can help you decide how to respond. Not all behaviors should be handled the same way.
For example, your child might cry because you’ve said “no” to eating ice cream before dinner. They might also cry the day their best friend moves away. You’d handle these two situations quite differently.
Understanding the cause of your child’s behavior can help you decide how to respond.
Bored, understimulated, or unchallenged
Signs of boredom, like doodles all over a math worksheet, might not be simply a lack of interest. It can be avoidance behavior for work that’s too difficult. Or, they have difficulty with focus because work is too easy.
They could also question the relevance of homework with, “Why do I have to learn this?”
Boredom during play can also be connected to a lack of stimulation or challenge. Maybe your child has outgrown their toys or needs more exercise.
Scheduling time with your child
If your child seems to be yearning for focused connected time with you, consider scheduling “special time” with your child for 10 to 20 minutes each day. Consider allowing them to choose an activity with you, such as reading or playing their favorite game.
Consider allowing them to choose an activity with you, such as reading or playing their favorite game.
You could check in with your child to see whether they need help with their homework. Also, you could find fun ways to incorporate more daily movement.
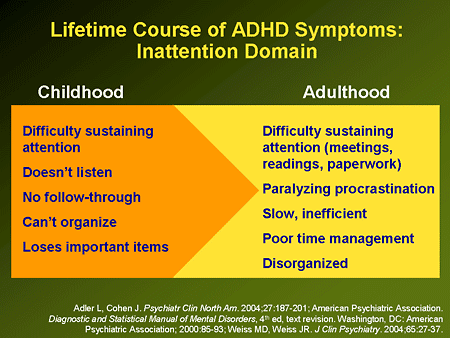
ADHD
Attention-seeking behavior is a symptom of ADHD. It’s often the first clue for parents that their child might have this condition.
You may have heard comments from friends and family members. Or maybe you’ve already had your child assessed and have a diagnosis and treatment plan in place.
In either case, ADHD can cause children to act out. Children with ADHD can experience difficulties with:
- sustained attention
- impulse control
- hyperactivity
All of these are part of attention-seeking behavior.
Knowing that your child has this neurodevelopmental diagnosis can make a difference in how you interpret and respond to them.
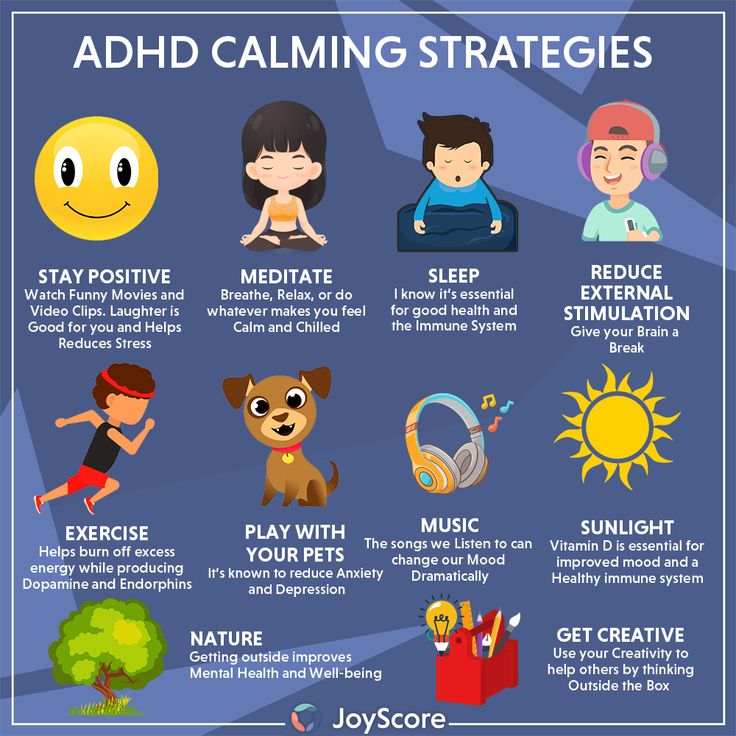
A supportive environment for kids with ADHD
Children with ADHD benefit from a supportive environment that includes clear expectations and structure. Parents who remain calm and understanding in the face of meltdowns can help their children get past them faster.
Parents who remain calm and understanding in the face of meltdowns can help their children get past them faster.
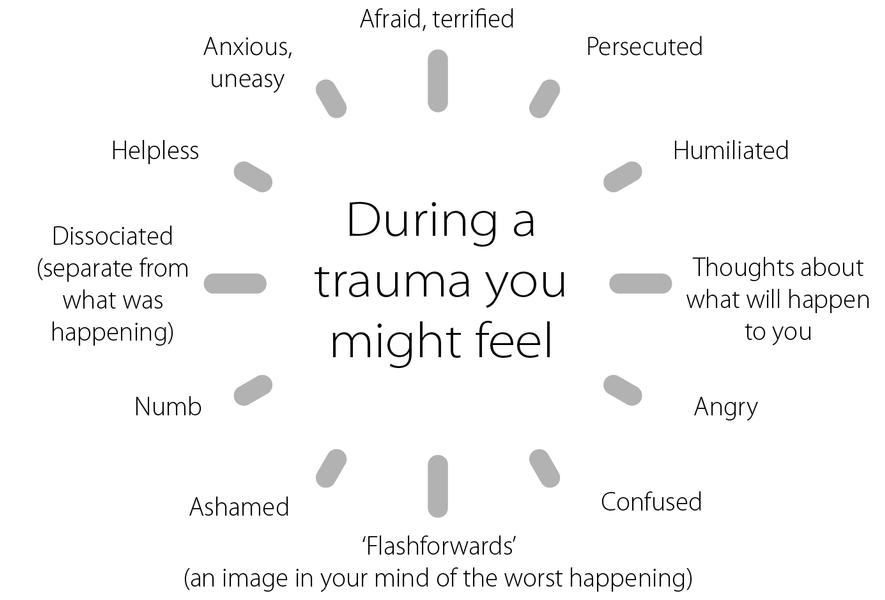
Trauma
Sometimes bad behavior is a response to trauma a child has experienced. This could be from something as common as a household divided by a marital breakup.
Other examples of adverse childhood experiences (ACEs) include:
- poverty
- neglect
- living in the same household as someone with a mental health disorder
- loss
- witnessing or experiencing abuse
According to the Centers for Disease Control and Prevention (CDC), about 61% of adults from across 25 states have experienced at least one type of ACE.
Research published in 2019 suggests that these experiences can double a person’s risk of having mental health conditions. A history of ACEs can also increase the chance of cardiovascular issues in adults, as shown in an Amsterdam study that included 22,165 participants.
Recognizing ACEs and helping children recover not only supports their mental and physical health but also reduces how often they’ll act out.
Building nurturing relationships
If your child has had ACEs, you can offer positive attention through empathetic listening and prioritize building a nurturing and stable relationship. Regardless of the type of ACE, therapy can also help. Research supports therapy as an important intervention when a child’s ACEs include abuse.
Mood shifts due to mental health condition
Sometimes children experience big emotions because they have a mood or behavior disorder. Examples include:
- Oppositional defiant disorder (ODD). In children with ODD, brain differences due to psychological, genetic, and social factors lead to unruly behavior toward authority figures.
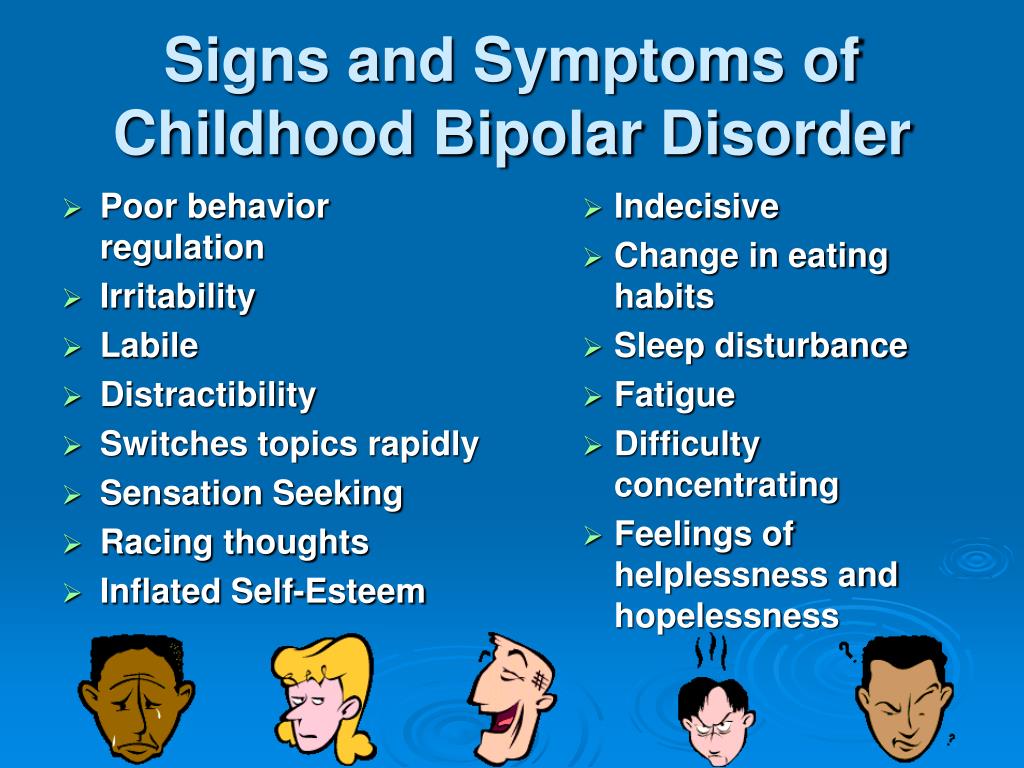
- Bipolar disorder. Both the manic and depressive episodes of bipolar disorder can feature attention-seeking behavior. The child experiencing the changes in mood that come with bipolar disorder may feel out of control and unable to control their behavior.
- Perfectionism.
 Having exacting standards isn’t a mental health disorder, but it can be connected to anxiety and obsessive-compulsive disorder (OCD). Perfectionism can also trigger meltdowns in children.
Having exacting standards isn’t a mental health disorder, but it can be connected to anxiety and obsessive-compulsive disorder (OCD). Perfectionism can also trigger meltdowns in children. - Depression. According to 2017 research, depression in children can sometimes present as irritability.
Self-regulation skills
Children with mood and behavior disorders can benefit from learning self-regulation skills. Therapy can teach these skills to children and their parents.
Attention-seeking behavior is part of childhood. Some young children act out because they haven’t learned calmer ways to communicate their needs. Others have underlying causes for their behavior, but you can help them manage.
One of the most important ways you can meet the needs of your child is to pay attention to your relationship with them. Building a stable and nurturing connection will be their foundation for a healthy life.
Types of attention disorders in children and related behavioral disorders
The function of attention and its role in the regulation of behavior is one of the most urgent problems of both fundamental (psychology and psychophysiology) and clinical (neurology and psychiatry) sciences.
One of the pillars of Russian psychology L.S. Vygotsky wrote: "The history of a child's attention is the history of the organization of his behavior" [1]. K. Buhler considered attention as the driving force in the development of the child [2]. Attention, as one of the most important cognitive functions, provides control and organization of information processing processes [3, 4]. The role of attention in the organization of cognitive activity is especially high in children of primary school age, which is characterized by the beginning of systematic schooling, which requires a change in the level of voluntary organization of mental processes [5]. nine0003
According to A.R. Luria [6], attention is a factor that ensures the selectivity and direction of mental processes. He wrote that attention is both a process of isolating elements essential for mental activity and a process of maintaining control over other areas of mental activity.
D.N. Uznadze [7] did not consider attention only in the context of cognitive functions. In his opinion, attention is significantly related to behavior and determines its success. nine0003
In his opinion, attention is significantly related to behavior and determines its success. nine0003
M. Rothbart et al. [8] suggested that good attention development helps to carry out emotional regulation, and a high level of attention control is associated with a low level of negative affects. According to N. Eisenberg and M. Sulik [9], the ability to control the level of attention is an index of emotional regulation. In this regard, it is interesting to note the studies by S. Calkins and N. Fox [10], the results of which showed that children with greater ability to control attention better control emotions and behavior. According to A. Diamond [11], attention together with working memory and cognitive flexibility are the three main components underlying the organization of executive functions. nine0003
In 1975, M. Posner introduced the term “cognitive control” in his book “Attention and cognitive control” [12]. Currently, cognitive control is understood as the ability for cognitive analysis, anticipation and planning of activities. E.A. Sergienko formulated the main functions of cognitive control: “Cognitive control is responsible for switching between activities, maintaining current activities, and suppressing external impulses” [13].
E.A. Sergienko formulated the main functions of cognitive control: “Cognitive control is responsible for switching between activities, maintaining current activities, and suppressing external impulses” [13].
Problems associated with impaired attention are one of the most common reasons for parents to visit a pediatric neurologist. Given the extreme importance of the development of attention for children and the high frequency of disorders of this function, we attempted to create a typology of attention disorders in childhood. nine0003
Types of attention/disorder in childhood
The following types of attention development in children were distinguished: normal, borderline and pathological.
Normal type
"Ideal" children. They are characterized by the absence of disturbances in attention and behavior and do not require drug therapy and psychotherapeutic correction. nine0003
nine0003
Features of temperament . Temperament is currently defined as biologically determined individual differences in reactivity and self-regulation [14, 15]. Children with a normal type of attention demonstrate excessive activity without significant impairment of attention. At the same time, such hyperactivity usually does not lead to significant difficulties in learning and communicating with peers.
M. Rothbart et al. [16] distinguish three factors (scales) of temperament, each of which includes a number of psychological traits: the first factor is “extraversion” (positive emotionality), it is expressed by the desire for communication, pleasure from new situations, a high level of activity, impulsiveness; the second factor - "negative emotionality", includes shyness, a feeling of discomfort from new situations, fear, anxiety; the third factor - "volitional regulation" ("self-control"), is described by the authors as the ability to suppress the dominant reaction in order to implement a subdominant one, which is more adequate in a given situation. Persons with a high level on the “volitional regulation” scale are characterized by diligence, perseverance, reliability and responsibility. nine0003
Persons with a high level on the “volitional regulation” scale are characterized by diligence, perseverance, reliability and responsibility. nine0003
Attention disorders due to competing motivation : an intellectually gifted child does not receive sufficient stimulation, as he may be occupied with other (more interesting or important) thoughts or activities [17, 18]. Excessive stimulation : the receipt of too much information, improperly organized educational process can cause situational hyperactivity in a child [18].
Frontier Type
"Low cognitive tempo" (sluggish cognitive tempo). Such children are characterized by a general decrease in activity, a tendency to daytime sleepiness, immersion in their thoughts and fantasies [19-21]. This condition can also be observed in healthy children during periods of excessive stress, and in some pathological conditions, such as asthenic disorders, attention deficit disorder (ADD) without hyperactivity. Educational activity in such children is characterized by difficulties in entering the task, rapid exhaustion, fluctuations in working capacity, etc. [19, 22].
Educational activity in such children is characterized by difficulties in entering the task, rapid exhaustion, fluctuations in working capacity, etc. [19, 22].
Overfocused attention. These children are characterized by a lack of flexibility in their psychological attitude, difficulties in switching and focusing attention [18, 23]. They have difficulty adapting to new requirements and situations, the desires of other children, which makes them stand out during social contacts. This entails perseveration, slowness, avoidance of contact and seriously affects the child's behavior in society. Children with overfocused attention are more prone to anxiety and affective (depression) disorders than to behavioral and asocial ones [18]. nine0003
Primary learning difficulties. In such cases, the child is not able to cope with cognitive tasks that are difficult for him. At preschool age, these children do not show problems associated with insufficient attention.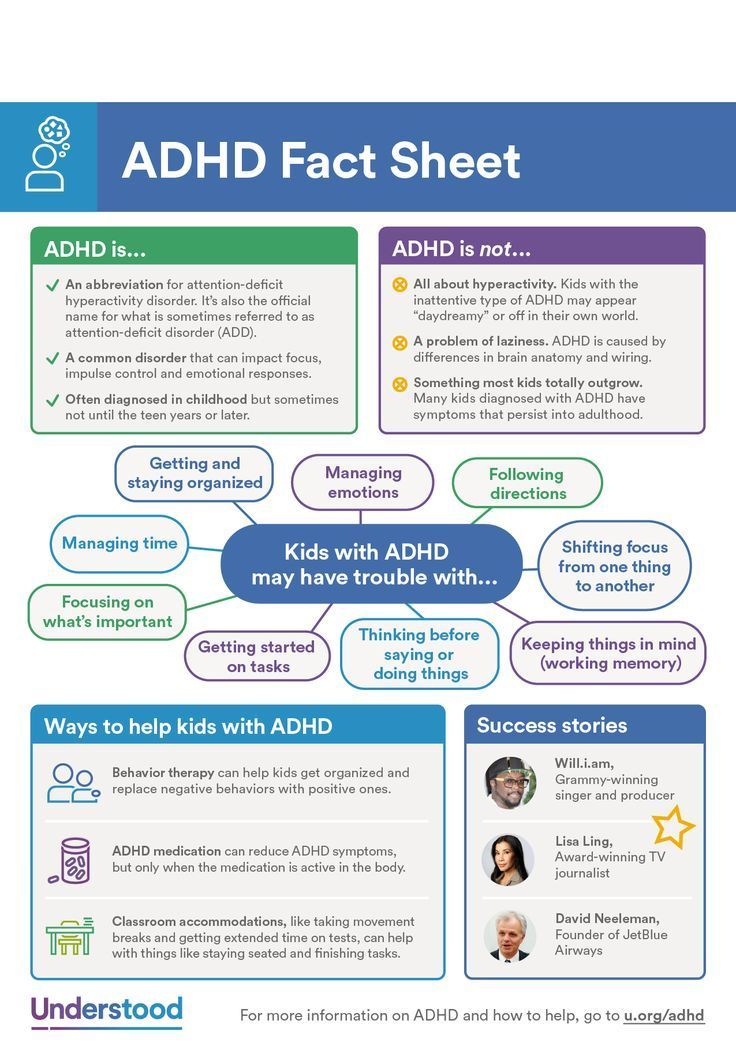
Pathological type
Such children do not have significant developmental disorders, except for the development of attention and associated regulatory and behavioral disorders.
nine0002 ADD with hyperactivity (ADHD). According to the literature [24-26], this syndrome occurs in 5-7% of children, significantly more often in males. So, M. Skounti et al. [27] identified signs of ADHD in 8% of the examined schoolchildren and only in 3.8% of schoolgirls. It should be noted that some "blurring" in the existing criteria for making this diagnosis sometimes leads to overdiagnosis of ADHD [28, 29]. Clinical manifestations of ADHD are defined by three main symptoms: inattention, hyperactivity and impulsivity. Impulsivity is understood as the impossibility of controlling one's impulses. There are cognitive impulsivity (reflecting hasty thinking) and behavioral impulsivity (reflecting difficulty in suppressing reactions).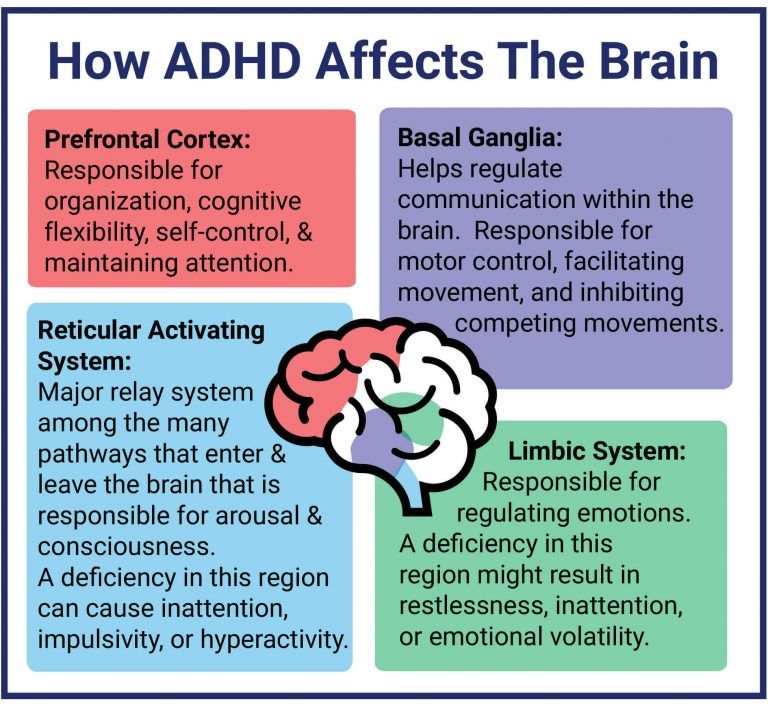 An interesting work is V. Douglas [30], who put forward the theory of “four major deficits” at the heart of the disease: 1) reduced ability to maintain attention; 2) weakness of inhibition of impulsive behavior; 3) weakness of modulation of the level of activating influences during a situational request; 4) an unusually strong propensity for immediate reward. nine0003
An interesting work is V. Douglas [30], who put forward the theory of “four major deficits” at the heart of the disease: 1) reduced ability to maintain attention; 2) weakness of inhibition of impulsive behavior; 3) weakness of modulation of the level of activating influences during a situational request; 4) an unusually strong propensity for immediate reward. nine0003
Children with ADHD have a lack of continuous (supported) attention, which manifests itself in the impossibility of long-term performance of an uninteresting task. In this regard, it is necessary to note the studies by P. Leung and K. Conolly [31], who did not find a pronounced deficit of sustained attention in children with this pathology and noted that children with ADHD are more likely to have a deficit of selective attention, which is manifested by increased distractibility to extraneous stimuli, especially if these stimuli are bright, interesting. nine0003
According to R. Barkley's model [32], ADHD is characterized not so much by attention disorders as by a deficit in inhibition (inhibition), i.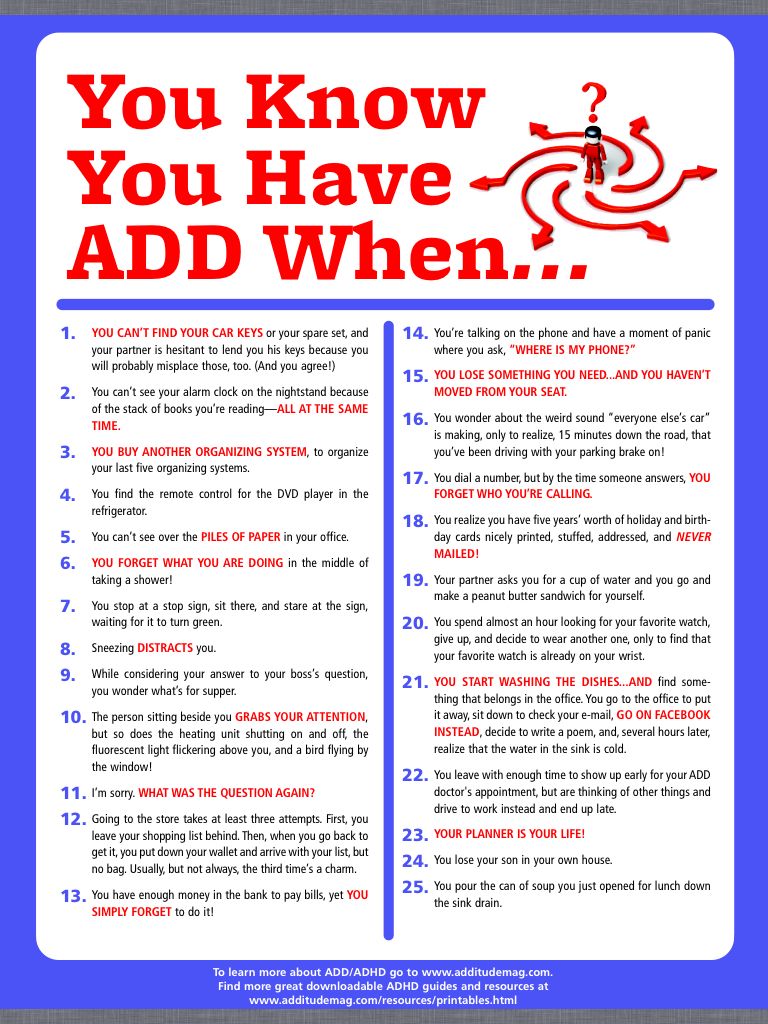 e., a person's ability to control impulsive or automatic reactions. In his opinion, the basis of the disease is a disorder of executive functions (executive desfunction), the implementation of which is carried out mainly by the prefrontal sections of the cerebral cortex. Inhibition deficiency contributes to increased distractibility and impairs sustained attention. Along with this, violations of executive functions lead to hyperactivity and behavioral disorders. nine0003
e., a person's ability to control impulsive or automatic reactions. In his opinion, the basis of the disease is a disorder of executive functions (executive desfunction), the implementation of which is carried out mainly by the prefrontal sections of the cerebral cortex. Inhibition deficiency contributes to increased distractibility and impairs sustained attention. Along with this, violations of executive functions lead to hyperactivity and behavioral disorders. nine0003
ADD (without hyperactivity) with a predominance of inattention
According to R. Milich et al. [33], this disorder is a completely independent disease. Such children give the impression of inhibited, drowsy, timid, shy. They perceive information more slowly than their peers, they remember worse. They are characterized by the state of low cognitive pace described above. There is evidence in the literature [32] that this type occurs in 30–50% of children with ADHD. The results of our studies indicate that this subtype is detected in 16.6% of children with ADHD [34]. Patients with this type of ADHD are characterized by severe manifestations of inattention and minor manifestations of hyperactivity. At the same time, their impulsiveness indicators remain within the age norm. In our studies, the severity of asthenic symptoms in ADHD was greater than in ADHD [35]. In addition, data from a psychophysiological study indicate a significantly higher level of attention deficit in children with ADHD compared to children with ADHD. At the same time, the level of impulsivity was significantly higher in children with ADHD [35]. nine0003
The results of our studies indicate that this subtype is detected in 16.6% of children with ADHD [34]. Patients with this type of ADHD are characterized by severe manifestations of inattention and minor manifestations of hyperactivity. At the same time, their impulsiveness indicators remain within the age norm. In our studies, the severity of asthenic symptoms in ADHD was greater than in ADHD [35]. In addition, data from a psychophysiological study indicate a significantly higher level of attention deficit in children with ADHD compared to children with ADHD. At the same time, the level of impulsivity was significantly higher in children with ADHD [35]. nine0003
According to A.R. Agris et al. [36], if disturbances in frontostriate interactions play a leading role in the pathogenesis of ADHD, then ADD is characterized by weakness of frontoparietal interactions. The leading cognitive impairment for ADD is a deficit in working memory, another component of executive functions. Thus, according to these authors, ADD can be described as a regulatory-activation deficit with a weakness in working memory, while ADHD can be described as a regulatory-motor deficit with difficulties in voluntary inhibition [36]. N. Ahmadi et al. [37] observed that children with ADHD are characterized by more pronounced impairment of executive functions than children with ADHD. nine0003
N. Ahmadi et al. [37] observed that children with ADHD are characterized by more pronounced impairment of executive functions than children with ADHD. nine0003
Secondary attention disorders. These disorders are associated with marked cognitive, socio-emotional, sensory and neurological deficits. This group includes children with various types of mental retardation, mental retardation, asthenic disorders.
Recently, the attention of researchers has been drawn to the question of the possibility of a combination of ADHD and autism spectrum disorders (ASD) [38–40]. It should be noted that children with ASD have not only a deficit of attention, but also a wider range of pronounced cognitive impairments. In our opinion, in this case we can rather speak not of primary, but of secondary attention disorders. nine0003
Treatment of attention disorders
In Russia, nootropic drugs have traditionally been used to treat cognitive impairments, i. e., drugs that positively affect the higher integrative functions of the brain, the main manifestation of which is the improvement of learning and memory processes in case of their impairment [41]. A common neurophysiological correlate of the pharmacological effect of nootropics is their facilitating effect on glutamatergic transmission, enhancement and lengthening of long-term potentiation. Nootropic and neuroprotective drugs used in the treatment of cognitive impairment in children include Cortexin, Pantogam, Nooklerin, Phenibut (Noofen, Anvifen), Picamilon, etc.
e., drugs that positively affect the higher integrative functions of the brain, the main manifestation of which is the improvement of learning and memory processes in case of their impairment [41]. A common neurophysiological correlate of the pharmacological effect of nootropics is their facilitating effect on glutamatergic transmission, enhancement and lengthening of long-term potentiation. Nootropic and neuroprotective drugs used in the treatment of cognitive impairment in children include Cortexin, Pantogam, Nooklerin, Phenibut (Noofen, Anvifen), Picamilon, etc.
Peptide bioregulator Cortexin, included in this group of drugs, is a complex of polypeptides isolated from the cerebral cortex of calves and pigs not older than 12 months of age by the method of acetic acid extraction. Cortexin improves memory and learning under the action of amnesic agents in animals, which indicates its nootropic activity. T.N. Platonov et al. [42] showed the high efficiency of Cortexin in the treatment of various cognitive impairments in children.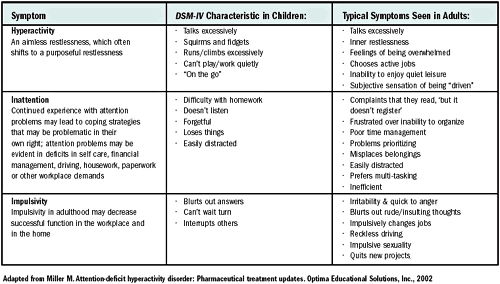 nine0003
nine0003
In our previous studies [43], it was found that after a course of Cortexin, clinical improvement occurred in approximately 72% of patients with ADHD. The best result was obtained in the treatment of children with ADD. These data were confirmed by an objective reduction in inattention and a reduction in reaction time, which were registered using a psychophysiological study. The results of the repeated neuropsychological study showed a significant improvement in the performance of Ozeretsky's neuropsychological tests and finger counting. In addition, positive clinical dynamics was accompanied by an improvement in electroencephalographic parameters. Only in 2.0% of cases there was a slight increase in impulsivity after the course of treatment. Other side effects are not registered. The obtained results make it possible to recommend Cortexin for the treatment of children with various forms of ADHD. nine0003
The authors declare no conflict of interest.
The authors declare no conflicts of interest.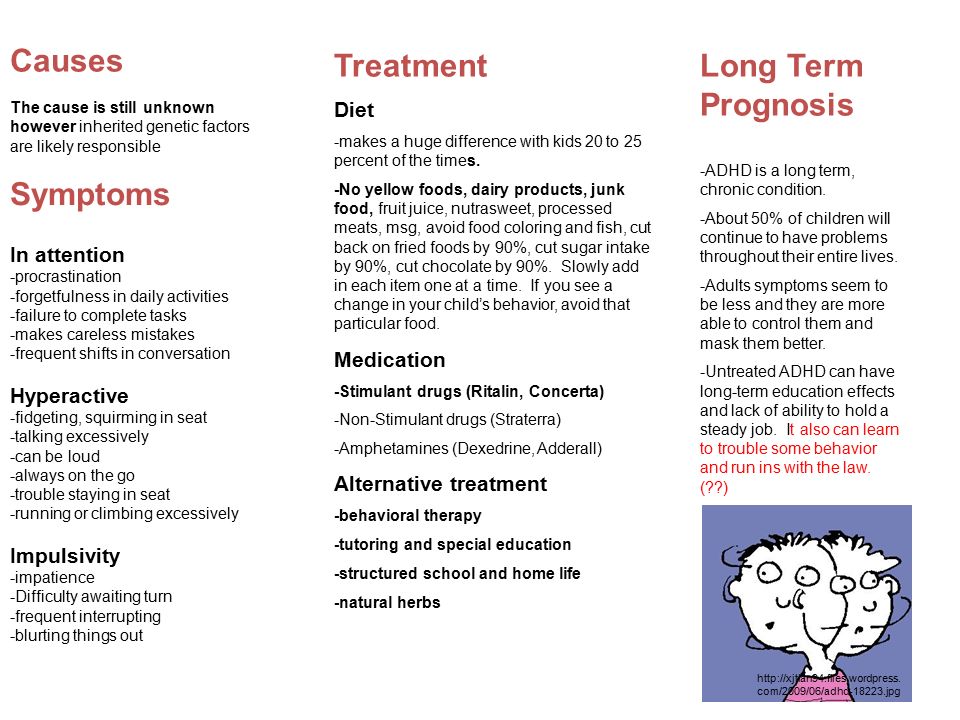
Credits
Chutko L.S. — https://orcid.org/0000-0002-1065-9859; e-mail: [email protected]
Surushkina S.Yu. — https://orcid.org/0000-0001-9510-7182; e-mail: [email protected]
Corresponding author: Chutko Leonid Semenovich — e-mail: [email protected]
causes, symptoms, signs, diagnosis, treatment of attention deficit hyperactivity disorder in children and adults
Symptoms of ADHD in children
Causes of pathology
Diagnosis
Treatment methods for ADHD
Prevention
Today, more and more children are being diagnosed with ADHD (Attention Deficit Hyperactivity Disorder). As a rule, it is diagnosed in children aged 6-8 years, when the child goes to school. It is at this time that it becomes obvious that the child has pronounced problems with behavior and perception of information. nine0003
ADHD is a neurological-behavioral developmental disorder.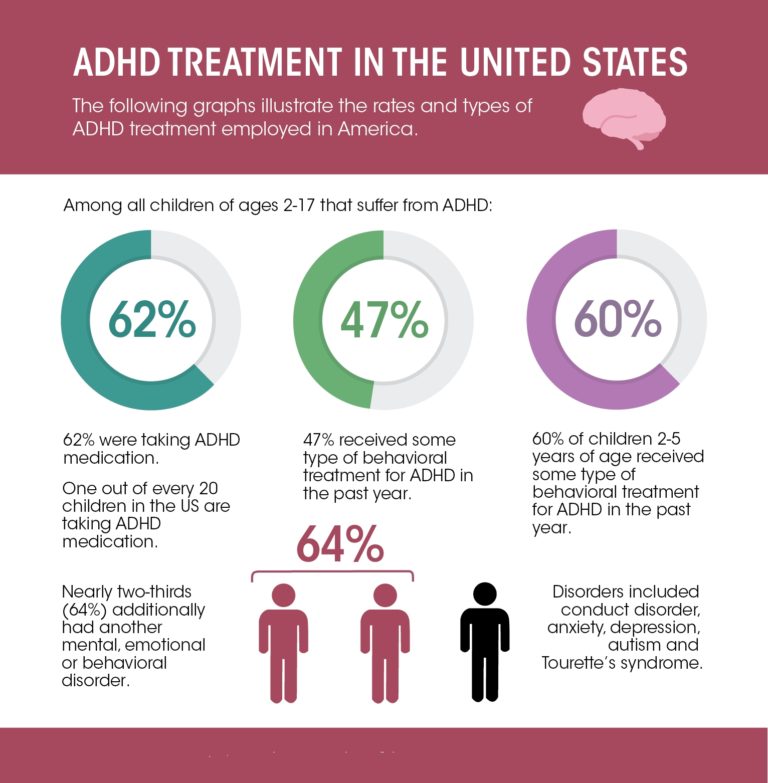 Pathology makes itself felt in childhood, but in the absence of timely therapy, it can persist into adulthood. According to statistics, ADHD is most common in boys, but can also occur in girls. If the pathology is not diagnosed and treated in a timely manner, this is fraught with poor school performance, the child may develop serious social problems, which increases the risk of substance abuse in the future. nine0003
Pathology makes itself felt in childhood, but in the absence of timely therapy, it can persist into adulthood. According to statistics, ADHD is most common in boys, but can also occur in girls. If the pathology is not diagnosed and treated in a timely manner, this is fraught with poor school performance, the child may develop serious social problems, which increases the risk of substance abuse in the future. nine0003
Symptoms of ADHD in children
Consider some of the signs that may signal ADHD in children:
- The child is constantly distracted, inattentive, when communicating with him there is a feeling that he is not listening to you.
- It is difficult for him to keep his attention on the teacher's words for a long time, because of which the understanding of information also suffers.
- Increased activity is observed - the child literally cannot sit in one place. Even during school hours, he can get up and walk around the classroom. nine0155
- The child is impatient, cannot wait for his turn, constantly interrupts, answers questions without waiting for them to finish.

- Children with ADHD are characterized by emotional instability, which can be manifested by frequent mood swings: a child can suddenly become irritable, whiny, and restless for no reason.
- Lack of concentration is characteristic - children with this diagnosis often lose their belongings (for example, school supplies, money, keys). nine0154 Problems with sleep and appetite, with daily routine.
Additionally, some neurological abnormalities may be observed. For example, a child with ADHD may have poor motor coordination, resulting in some clumsiness. Also, in some cases, twitching of the facial muscles and trembling of the limbs are observed.
The first signs of attention deficit hyperactivity disorder are observed at the age of 2-3 years, but at this age it is difficult to determine whether they are a manifestation of pathology or normal age-related features. nine0003
However, if by the age of 6-8 years the child has not become more attentive and collected, this is an alarming sign that makes it possible to assume ADHD with a high degree of probability. That is why, if you have the above symptoms, you should definitely consult a doctor and start treatment.
That is why, if you have the above symptoms, you should definitely consult a doctor and start treatment.
Causes of pathology
There is no single reason for the development of ADHD. Many experts agree that the most common cause may be genetic mutations that lead to a disruption in the production of dopamine and the work of dopamine receptors. nine0003
Also, the causes of the development of attention deficit hyperactivity disorder may be the following factors:
- Severe pregnancy, complicated delivery, including prolonged or rapid.
- Use by the expectant mother during pregnancy of potent drugs, alcoholic beverages, toxic substances.
- Serious pathologies suffered by a child at an early age, including craniocerebral trauma. nine0155
- Psychological trauma in a child.
- Fetal asphyxia.
It is also worth noting that this pathology has a hereditary predisposition. It was found that the presence of ADHD in parents significantly increases the likelihood of developing this syndrome in a child.
Diagnostics
The diagnosis of ADHD is not established only on the basis of existing complaints. To accurately confirm the diagnosis, it is necessary to conduct some examinations. First of all, you need to visit a neurologist, psychiatrist and psychologist. nine0003
During the consultation, the doctor collects an anamnesis, conducts various tests, conversations, and diagnostic surveys.
In order to identify the cause of the development of ADHD, consultations with other specialists may also be required, as well as instrumental and laboratory examination methods, such as: EEG, MRI of the brain, general and biochemical blood tests.
ADHD treatments
It should be noted that attention deficit hyperactivity disorder most often has a favorable prognosis (provided that therapy is started in a timely manner).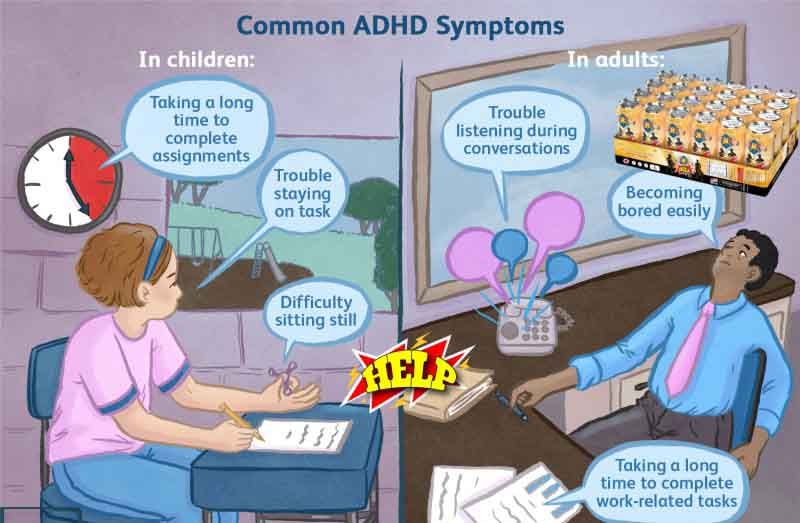 It is possible to significantly improve the behavior and learning of the child. nine0003
It is possible to significantly improve the behavior and learning of the child. nine0003
Depending on the severity of the pathological process and the causes of its occurrence, the doctor may prescribe such types of treatment as:
- Drug treatment: the patient may be prescribed sedatives, antidepressants, neurostimulants.
- Cognitive behavioral therapy.
- A clear daily routine: a balanced diet, good sleep.
- Family therapy: if there are conflicts in the family, ADHD often develops against this background. nine0155
- Biofeedback therapy: this method of treatment is aimed at training the child's ability to self-regulate their conditions with the help of computer game tasks.
- Physiotherapy techniques, eg massage, exercise, kinesiotherapy.
Additionally, other methods of treatment can be used.
Prophylaxis
Unfortunately, it is not always possible to prevent the development of ADHD. However, there are some factors that significantly reduce the risk of developing pathology. For example, the expectant mother should follow a healthy lifestyle, eat a balanced diet, give up bad habits. Before conception, it is desirable to undergo a complete examination, if necessary, to pre-treat existing pathologies. nine0003
For example, the expectant mother should follow a healthy lifestyle, eat a balanced diet, give up bad habits. Before conception, it is desirable to undergo a complete examination, if necessary, to pre-treat existing pathologies. nine0003
Also, as a prevention of ADHD, the following recommendations should be observed:
- The child should be active, walk in the fresh air more often.
- The regimen of the day and nutrition should be clear.
- Monitor the child's behavior, immediately stop unacceptable behavior on his part.
- It is very important to build a trusting relationship between parents and children.
- Family conflicts should be avoided. nine0155
At the first signs of ADHD, it is recommended to contact specialists who will help minimize the risk of developing more serious pathologies in the future.
You can learn more about the treatment of attention deficit hyperactivity disorder at a face-to-face appointment with a doctor. Be healthy!
Be healthy!
Author of the article:
Markelov Gleb Vladimirovich
neurologist, online consultations
work experience 4 years
reviews Leave a review
Clinic
m. Sukharevskaya
Reviews
Services
- Title
- Appointment, consultation of a neurologist primary
- Appointment, consultation of a neurologist repeated900
Health articles
All articlesAllergologistGastroenterologistHematologistGynecologistDermatologistImmunologistInfectionistCardiologistENT doctor (otolaryngologist)MammologistNeurologistNephrologistOncologistOphthalmologistProctologistPsychotherapistPulmonologistRheumatologistTraumatologistTrichologistUrologistPhlebologistSurgeonEndocrinologist nine05 years. Red Gates. AvtozavodskayaPharmacy. Glades. Sukharevskaya. st. Academician Yangelam. Frunzenskaya Zelenograd
Frunzenskaya Zelenograd Dmitrieva Olga Nikolaevna
Chief physician of "Polyclinika.ru" on Frunzenskaya, neurologist, ENMG specialist
reviews
Clinic
m. Frunzenskaya
Sumina Evgenia Yurievna
Head doctor "Polyanka.ru" on Polyanka, neurologist
reviews
Clinic
m. Polyanka
Demina Evgenia Sergeevna
neurologist, reflexologist, ENMG specialist
reviews Make an appointment
Clinic
m. Sukharevskaya
Kuzmina Irina Vladimirovna
neurologist, reflexologist, hirudotherapist
reviews Make an appointment
Clinic
m.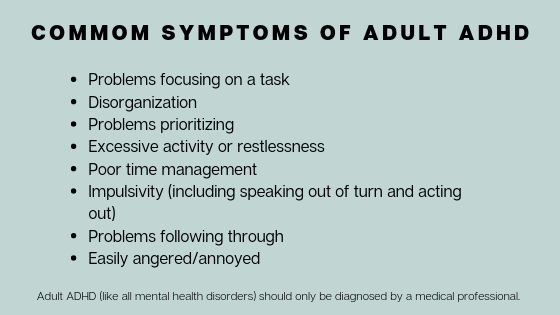 Street 1905 Goda
Street 1905 Goda
Shcherbenkova Alina Lvovna
neurologist, specialist in ENMG, KMN
reviews Make an appointment nine0003
Clinic
m. Frunzenskaya
Aleksandrova Tatyana Sergeevna
neurologist
reviews Make an appointment
Clinic
m. Sukharevskaya
Apevalova Anastasia Romanovna
neurologist
reviews Make an appointment nine0003
Clinic
m. st. Academician Yangel
Arkhireeva Lyudmila Vladimirovna
neurologist
reviews Make an appointment
Clinic
m.