Anxiety medicines safe for pregnancy
List of Anxiety Medications Safe During Pregnancy
Learn about the risk associated with taking anxiety medications while pregnant, including birth defects and minor respiratory problems after delivery.
Article at a Glance:
- Anxiety is common during pregnancy, yet the safety of anxiety medication varies from one drug to the next.
- Research shows that benzodiazepines and SSRIs have mild or moderate effects on a pregnancy.
- Babies can be born addicted to benzodiazepine anxiety medications.
- Non-drug cognitive behavioral therapy can help expectant mothers cope with anxiety as an alternative to medication.
- If you find out you are pregnant, do not stop taking an anxiety medication that you currently take without taking to your doctor first.
People often wonder what anxiety meds you can take while pregnant if any. Anxiety can even worsen during pregnancy, which can be a concern for women who are unsure about the safety of certain medications. Overall, the safety of anxiety medications during pregnancy can vary a lot, depending on the specific medication.
For the most part, studies show that anxiety medications including benzodiazepines and serotonin reuptake inhibitors aren’t going to have a huge impact on a baby during pregnancy. There can be some mild effects, based on current research. For example, both benzodiazepines and SSRIs are associated with shorter pregnancies, and babies more likely to require minor respiratory assistance after delivery. Even though some research studies haven’t shown major effects from anxiety medications during pregnancy, that doesn’t mean they’re absolutely safe.
First, benzodiazepines like Xanax and Valium and category D drugs according to the FDA. This indicates the FDA believes there is positive evidence of human fetal risk based on studies or investigations. Some benzodiazepines are believed to be linked to fetal effects like a cleft lip and palate, particularly when they’re used during the first trimester, although the risk is fairly low. Something else that needs to be considered is the risk of maternal toxicity stemming from the use of benzodiazepines, and how that could affect the fetus. For example, if a mother takes a benzodiazepine as an anxiety treatment and experiences side effects, the baby may as well. Side effects of benzodiazepine toxicity can include not only breathing problems, but also sedation and floppiness or decreased muscle tone. This is again a relatively low risk but is more common in women who take high doses of benzodiazepines. However, a category D drug may also have more benefits than risks when used during pregnancy for some women. While benzodiazepines are category D, long-term anxiety medications like Prozac and Zoloft are often described as “probably safe.” Tricyclic antidepressants and buspirone may be safe during pregnancy as well.
Something else that needs to be considered is the risk of maternal toxicity stemming from the use of benzodiazepines, and how that could affect the fetus. For example, if a mother takes a benzodiazepine as an anxiety treatment and experiences side effects, the baby may as well. Side effects of benzodiazepine toxicity can include not only breathing problems, but also sedation and floppiness or decreased muscle tone. This is again a relatively low risk but is more common in women who take high doses of benzodiazepines. However, a category D drug may also have more benefits than risks when used during pregnancy for some women. While benzodiazepines are category D, long-term anxiety medications like Prozac and Zoloft are often described as “probably safe.” Tricyclic antidepressants and buspirone may be safe during pregnancy as well.
Babies Born Addicted to Anxiety Medications
Since most anti-anxiety medications fall into two main categories, benzodiazepines and long-term daily treatments like SSRIs, it’s worth looking at both. Babies can be born technically addicted or dependent on both types of medications. With benzodiazepines, if they’re taken near the time of delivery, the baby may experience withdrawal symptoms. Newborn benzodiazepine withdrawal symptoms can include breathing problems, muscle weakness, crying, irritability, tremors, jitters, and problems with sleep. These symptoms will usually dissipate after a few weeks. Neonatal withdrawal from benzodiazepine will not typically create any long-term effects. As far as SSRIs, an infant can also experience mild withdrawal symptoms from these anxiety medications. With SSRI withdrawal, infants usually have very mild symptoms that disappear within 48 hours. Most SSRI withdrawal symptoms in infants don’t require medical intervention.
Babies can be born technically addicted or dependent on both types of medications. With benzodiazepines, if they’re taken near the time of delivery, the baby may experience withdrawal symptoms. Newborn benzodiazepine withdrawal symptoms can include breathing problems, muscle weakness, crying, irritability, tremors, jitters, and problems with sleep. These symptoms will usually dissipate after a few weeks. Neonatal withdrawal from benzodiazepine will not typically create any long-term effects. As far as SSRIs, an infant can also experience mild withdrawal symptoms from these anxiety medications. With SSRI withdrawal, infants usually have very mild symptoms that disappear within 48 hours. Most SSRI withdrawal symptoms in infants don’t require medical intervention.
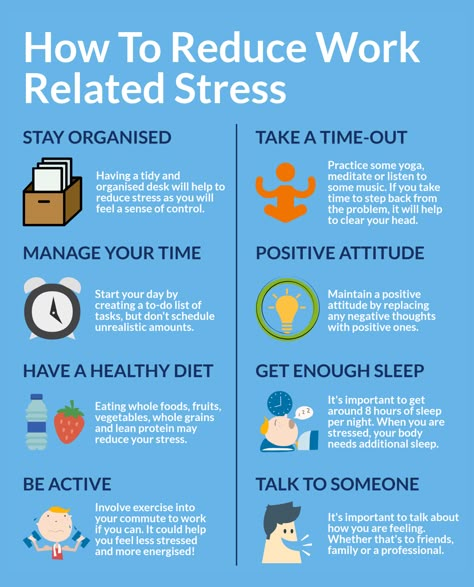
Alternatives to Anxiety Medications While Pregnant
When someone is pregnant and has anxiety, the general medical advice is to try other options for treatment before taking medications. This is true even if an anxiety medicine is considered to be “probably safe. ” Some alternatives to anxiety medications while pregnant can include cognitive behavioral therapy or another type of non-drug therapy. Some people may benefit from alternatives like yoga, meditation or massage. Another option would be herbal therapy, although herbs and supplements can be unsafe during pregnancy, so they should also only be taken under medical supervision. If a doctor does determine that the risks of a pregnant woman’s anxiety being untreated are greater than the risks of medication, they will then work to find the right option. Since some options are safer than others, doctors may, for example, recommend an SSRI over a benzodiazepine. If you’re currently using anxiety medication and you’re pregnant, you shouldn’t suddenly stop using it without speaking to your physician first.
” Some alternatives to anxiety medications while pregnant can include cognitive behavioral therapy or another type of non-drug therapy. Some people may benefit from alternatives like yoga, meditation or massage. Another option would be herbal therapy, although herbs and supplements can be unsafe during pregnancy, so they should also only be taken under medical supervision. If a doctor does determine that the risks of a pregnant woman’s anxiety being untreated are greater than the risks of medication, they will then work to find the right option. Since some options are safer than others, doctors may, for example, recommend an SSRI over a benzodiazepine. If you’re currently using anxiety medication and you’re pregnant, you shouldn’t suddenly stop using it without speaking to your physician first.
If you’re concerned about prescription drugs, or other substances you or a loved one may be taking, we encourage you to reach out to our team at The Recovery Village today.
Related: Taking Anxiety Medications During Breastfeeding: What You Need to Know
If you’re pregnant and looking for healthy ways to manage anxiety, without using potentially harmful medications, the Nobu app can help. It is free and for anyone that is looking to reduce anxiety, work through depression, build self-esteem, get aftercare following treatment, attend teletherapy sessions and so much more. Download the Nobu app today!
It is free and for anyone that is looking to reduce anxiety, work through depression, build self-esteem, get aftercare following treatment, attend teletherapy sessions and so much more. Download the Nobu app today!
Medical Disclaimer
The Recovery Village aims to improve the quality of life for people struggling with substance use or mental health disorder with fact-based content about the nature of behavioral health conditions, treatment options and their related outcomes. We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.
Are Depression and Anxiety Meds OK During Pregnancy?
Written by Lisa Marshall
Reviewed by Nivin Todd, MD on October 22, 2019
Is it safe to take medications for mood disorders when you’re pregnant?
Worried mothers-to-be are increasingly asking this question in the wake of a flurry of new studies linking antidepressants and anti-anxiety drugs with everything from heightened risk of miscarriage to birth defects and autism.
The answer, experts say, is complicated.
“I try to stay away from the ‘safe or not safe’ discussion and frame it in terms of risks vs. risks,” says Mary Kimmel, MD, assistant professor and medical director of the Perinatal Psychiatry Inpatient Unit at University of North Carolina. “There is a risk to taking medication, but there is also a risk to not treating.”
Maternal Mental Health Issues on the Rise
As many as one in four pregnant women have depression, and about one in 10 meet the criteria for generalized anxiety disorder.
In some cases, a pregnancy is unintended, leading to complicated emotions. In others, shifting hormones and a predisposition to depression collide to worsen existing mood disorders or bring previously undiagnosed ones to the surface. Often, women are ashamed to speak up, says Shoshana Bennett, PhD, a perinatal psychologist, and author of Beyond the Blues: Understanding and Treating Prenatal and Postpartum Depression and Anxiety (2019 Updated Edition).
“There is an expectation that you are supposed to be happy and excited,” she says. “The reality is, women are not always happy that they are pregnant.” Counseling can be helpful; medications are not the only option.
As attention to prenatal mood disorders has risen, so has the number of women taking medication for it, with about 10% of pregnant U.S. women taking antidepressants and 1% taking benzodiazepines. That concerns some clinicians, who say that while medication is key for severe cases, other options -- like nutritional interventions, better sleep, and psychotherapy -- may work as well or better for mild to moderate cases.
“Is it wonderful that this is now being regarded as something real and needing treatment? Yes,” says Bennett, who often starts with nondrug options, before recommending medication. “Do we jump to medication too quickly some time? Yes. I believe we do.”
Risks Can Be Small, but Real
Anick Berard, PhD, professor, and a perinatal pharmacology researcher at the University of Montreal, notes that because it is considered unethical to ask a healthy pregnant woman to take a drug for a research study, clinical trials on risks and benefits for mom-to-be and baby are hard to find.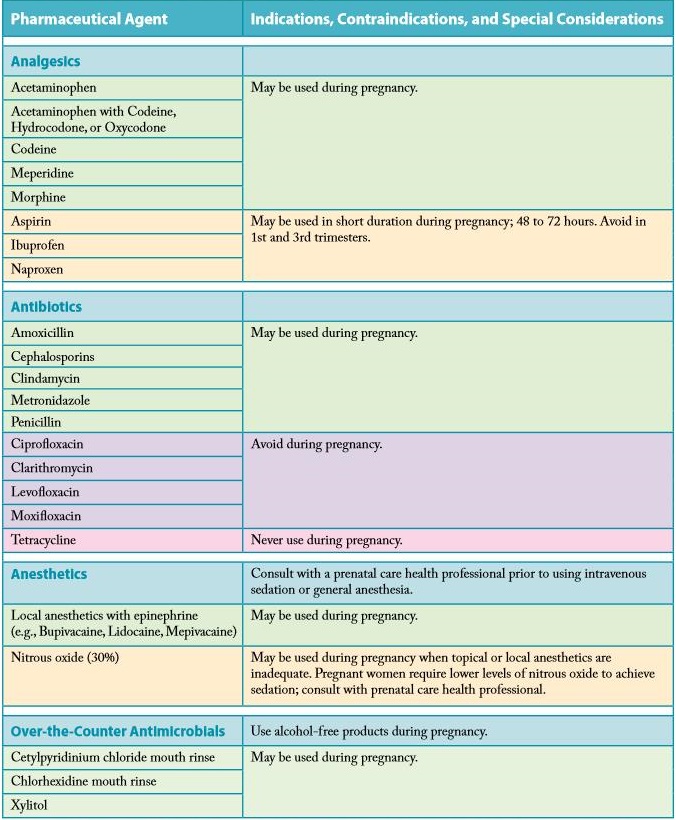
To fill the gap, she’s followed pregnancies in Quebec for 17 years, looking at birth outcomes for nearly 450,000 mothers, and published dozens of studies.
One, published last year in the journal JAMA Psychiatry, found that women who take benzodiazepines like Xanax or Ativan for anxiety in early pregnancy are anywhere from 60% to three times more likely to have a miscarriage, depending on which one they’re taking.
Another, published in 2017, found that those who took certain antidepressants (selective serotonin reuptake inhibitors, or SSRIs) in the first trimester were more slightly more likely to have children with defects of the heart, lungs, digestive system, face, and other organs.
Other large studies have linked antidepressant use during pregnancy with an increased risk of preterm birth and gestational hypertension (high blood pressure). One, published in the journal Pediatrics, found that boys with autism spectrum disorder were three times as likely to have been exposed to SSRIs in utero.
“Serotonin is essential for musculoskeletal, organ and brain development, and SSRIs work by blocking this molecule,” Berard says. “As a result, it has the potential to lead to a wide range of birth defects.”
Meanwhile, some studies suggest that for women with mild to moderate depression antidepressant efficacy is questionable. About 13% of women who take antidepressants during pregnancy remain depressed.
“Given that antidepressants don’t do that well for women with mild to moderate depression and that there is some risk, I think it leans to the side of more risky than not for them,” Berard says. “That being said, every woman should talk to her doctor to see what’s right for her.”
The Risks of Doing Nothing
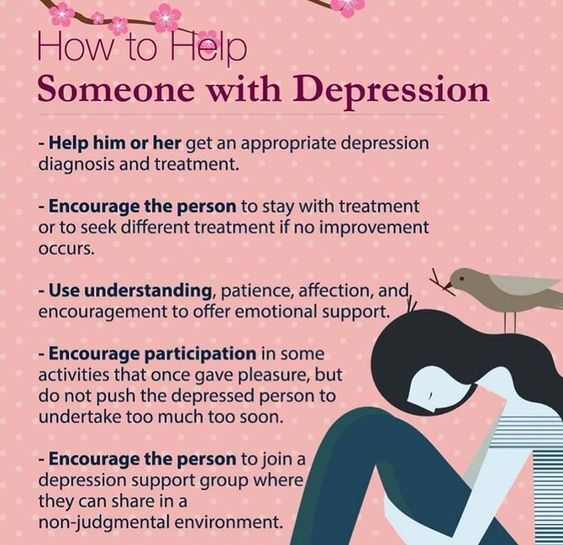
Kimmel stresses that untreated depression and anxiety come with their own risks.
Depressed mothers are less likely to attend prenatal visits or take their prenatal vitamins and more likely to smoke, drink and use drugs -- all factors that can lead to preterm and low-birth weight babies.
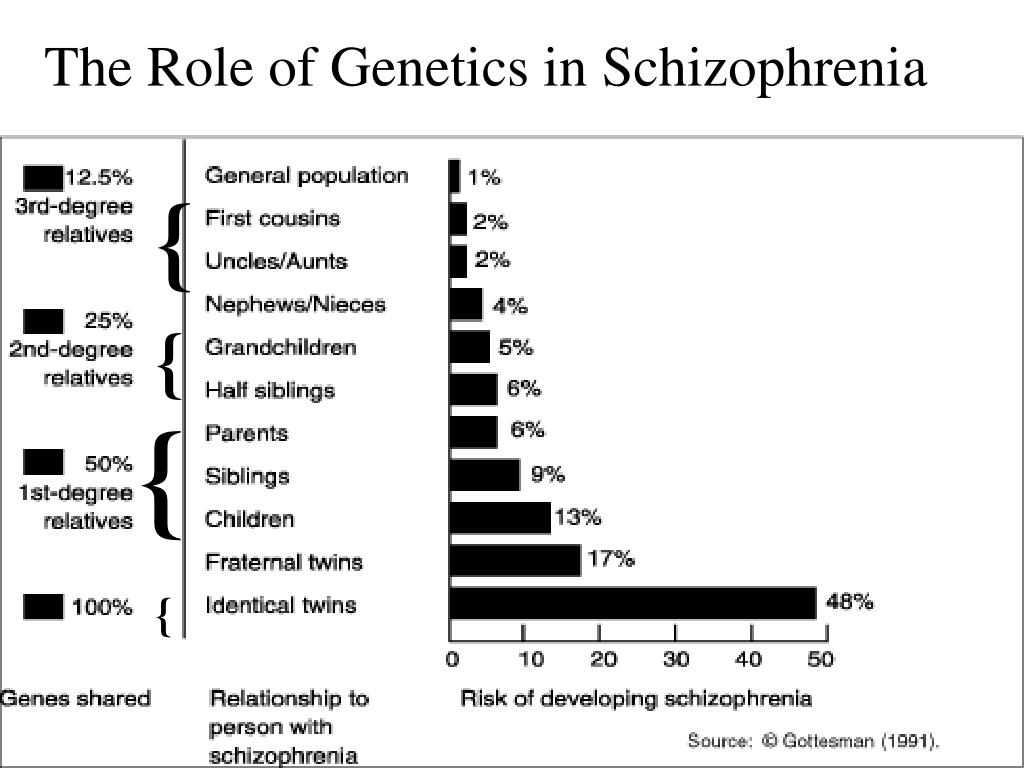
“We also know that depression and anxiety during pregnancy is associated with a child being more likely to have depression and anxiety and other psychiatric disorders later in life,” Kimmel says.
For some women, she says, better self-care and therapy can go a long way to ease mental health problems during pregnancy.
“But there are times when someone may be doing all the right things and still be depressed or even suicidal,” she says, noting that there can be underlying biological reasons. “In that case medication may be really important.”
The Right Medication at the Right Dose
Kimmel suspects that some women may not respond well to antidepressants, because they are not taking enough or not taking the right one. Due to changes in blood volume and metabolism during pregnancy, women already taking antidepressants may have to take a higher dose to maintain the same effect.
While she generally does not recommend benzodiazepines for pregnant women, she warns that abruptly halting them is not advised.
And she stresses that some medications come with more risks than others.
For instance, one recent study found that while paroxetine (Paxil) and fluoxetine were strongly linked to birth defects, including cardiac defects, sertraline (Zoloft) was not.
“If you do need medication, our objective is to use the right medication and the lowest effective dose to get you well,” she says.
Her advice to those mulling this tough question: “Talk to your doctor about it and keep talking with your doctor about it. Different decisions can be made at different times to be sure you are doing all you can for your mental health.”
Dos and Don’ts
Do talk to your doctor if you are already on medication and considering pregnancy.
Don't suddenly go off your medication because you are pregnant. Rapid withdrawal can come with its own risks to both you and your baby.
Do make sure you are taking the right dose. Some medication doses must be increased to work effectively during pregnancy.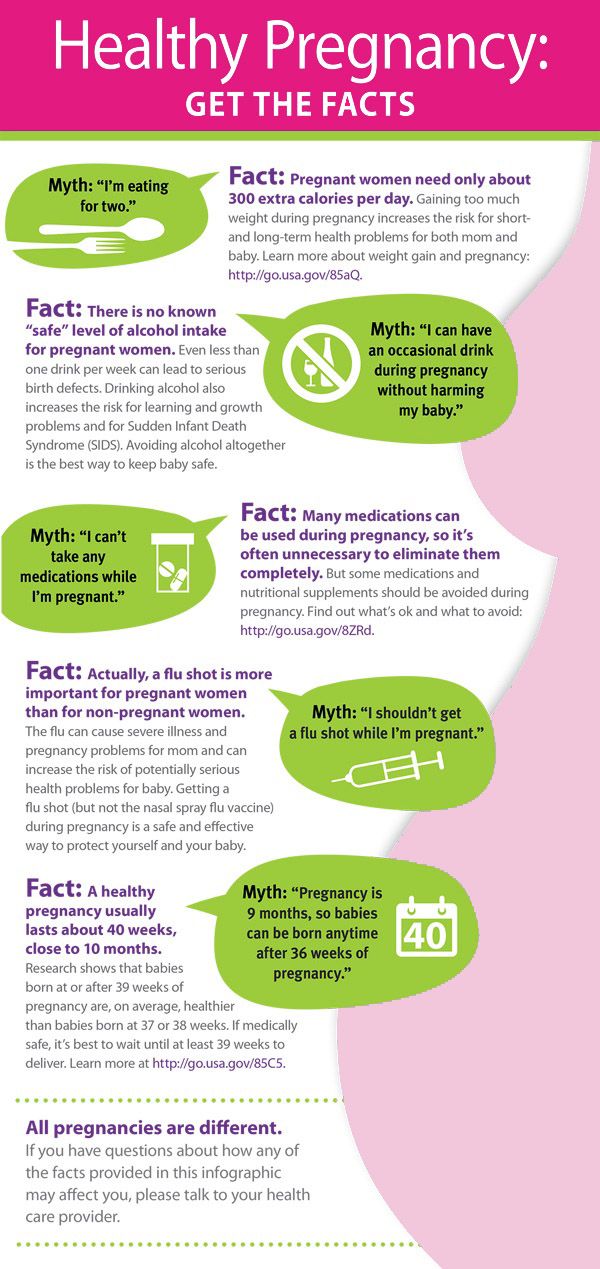
Do ask your doctor about your medication’s safety profile. Some are safer during pregnancy than others.
Do ask your doctor what other steps you can take to prevent depression. Some psychotherapies have been shown to help.
Find more articles, browse back issues, and read the current issue of WebMD Magazine.
Pregnancy and medicines / Obstetrics and gynecology, reproductive medicine / Articles about health / Articles and encyclopedia / madez.ru
We have been actively planning for a baby for a long time, but we never think about the dangers of drugs during pregnancy!
Gynecologist, gynecologist endocrinologist Popova Natalya Vladimirovna will tell you what medicines can be taken during pregnancy, and which ones are categorically not recommended.
One of the most important periods in a woman's life is the period of bearing a child. And in these few months, the expectant mother must do everything in her power to give birth to a healthy baby.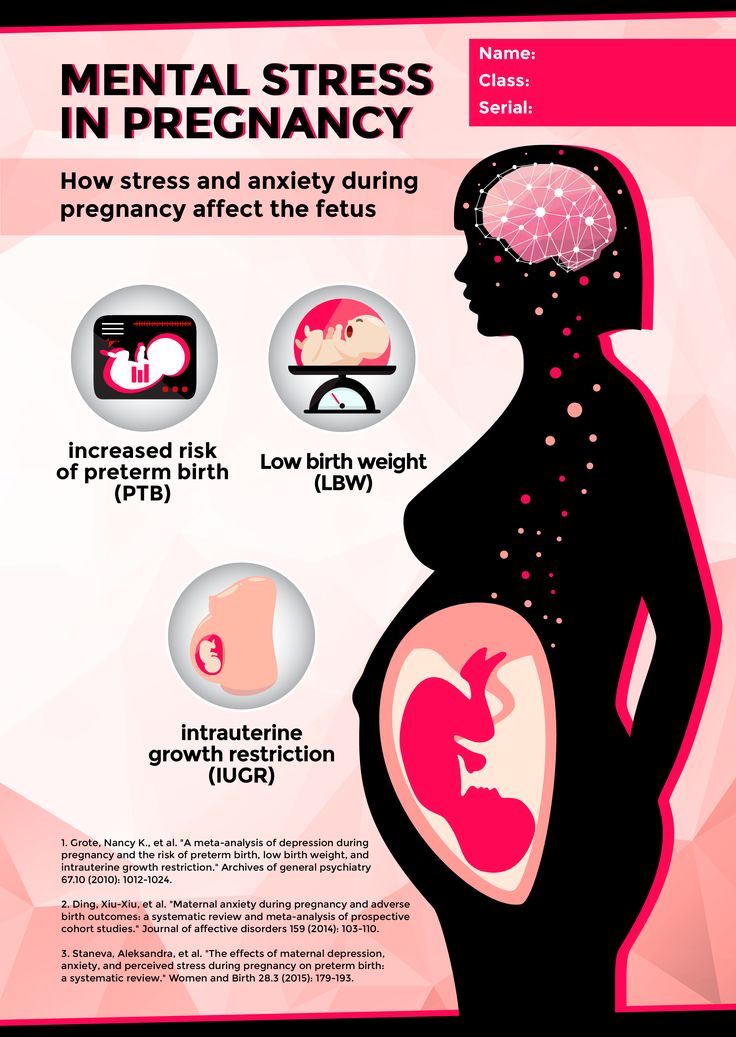 But pregnancy lasts nine calendar months - it is very difficult during this time to never feel any ailments or health problems.
But pregnancy lasts nine calendar months - it is very difficult during this time to never feel any ailments or health problems.
If it is necessary to use any drug during pregnancy, the mother-to-be should remember:
- Any drug during pregnancy (at any stage) can be used only in accordance with the indications and only as prescribed by the attending physician;
- When choosing a medicinal product, preference should be given only to those medicinal products that have proven efficacy;
- Prefer monotherapy, i.e. treatment with only one drug if possible; combined treatment during this period is undesirable;
- Topical treatment is more desirable than systemic (oral, intravenous, intramuscular) administration of the drug.
- A pregnant woman should remember that completely safe and absolutely harmless drugs do not exist.
The most dangerous period for the use of any drugs, both of chemical and natural origin, is considered the first trimester of pregnancy (the first 12 gestational weeks), when all organs and systems are laid in the fetus, which in the future will only develop and form the placenta. It is at this time that the fetus is considered the most vulnerable to any chemical and medicinal substances.
It is at this time that the fetus is considered the most vulnerable to any chemical and medicinal substances.
Pronounced mutagenic hazard:
1. in industry - asbestos, acetaldehyde, vinyl chloride, dimethyl sulfate; factors of metallurgical and rubber industries;
Metals: copper, nickel, lead, zinc, cadmium, mercury, chromium, arsenic, styrene, formaldehyde, chloroprene, epichlorohydrin, ethylene oxide.
2. agriculture - a mixture of defoliants, pesticides, insectiosides, repellents, fungicides, pesticides, methylpartion, phthalaphos, chlorophos, gardona, DDT, contan.
If you work in a hazardous industry and come into contact with these chemicals, from early pregnancy, switch to "light work".
Global trends in early pregnancy from the point of view of evidence-based medicine are unambiguous: the need for rational diet therapy , intake of folic acid at least 400 mcg/day and potassium iodide 200 mg/day.
After 12-14 weeks of pregnancy, with an inadequate diet, the use of vitamin preparations during pregnancy and lactation is recommended as a way to improve the health of the mother and fetus . Vitamin complexes intended for other groups of the population (including children) are contraindicated for pregnant women!
Medicines during pregnancy
In existing classifications, it is customary to subdivide drugs during pregnancy into groups - safe, relatively safe, relatively unsafe and dangerous. Moreover, the list of drugs is periodically updated.
- Category A - safe drugs. Controlled trials have shown no risk to the fetus for the first 12 weeks of pregnancy. Regarding them, there is no evidence of a harmful effect on the fetus in late pregnancy. These are folic acid, levothyroxine sodium, paracetamol, magnesium sulfate.

- Category B - relatively safe drugs. Experimental studies have generally not shown their teratogenic effects in animals and children whose mothers took such drugs. These are amoxicillin, heparin, insulin, aspirin, metronidazole (except for the first trimester)
- Category C - relatively unsafe drugs. When testing these drugs on animals, their teratogenic or embryotoxic effects were revealed. Controlled trials have not been conducted or the effect of the drug has not been studied (isoniazid, fluoroquinolones, gentamicin, antidepressants, antiparkinsonian drugs). These drugs should only be used if the potential benefit outweighs the potential risk.
- Caregory D - dangerous drugs. The use of drugs in this group is associated with a certain risk to the fetus, but despite this, it is possible to use the drug for health reasons (anticonvulsants, doxycycline, kanamycin, diclofenac).

- Category X - dangerous drugs that are contraindicated for use.
The teratogenic effect of drugs in this group has been proven, their use is contraindicated during pregnancy, as well as when planning a pregnancy.
Although almost 1000 chemicals are known to be teratogenic in animals, only a few chemicals have been proven to be permanently teratogenic in humans. These include a number of narcotic analgesics, chemotherapeutic drugs (antimetabolites, alkylating agents), anticonvulsants (trimethadione, valproic acid, fenithione, carbamazepine), androgens, warfarin, danazol, lithium, retinoids, thalidomide.
The safest drugs
(Larimore W.L., Petrie K.A., 2000)
| Drug groups | The safest drugs |
| Analgesics | Paracetamol, narcotic analgesics (short courses), NSAIDs (except due date) |
| Antibiotics | Aminopenicillins, macrolides (Vilprafen), azithromycin, cephalosporins, clindamycin, erythromycin, metronidazole (except 1st trimester), penicillins, trimethoprim (except 1st trimester) |
| Antidepressants | Venlafaxine, fluoxetine, trazodone |
| Antidiarrheals | Loperamide |
| Antiemetics | Andacids, doxylamine, prochlorperazine, promethazine, vitamin B |
| Antihypertensives | B-blockers, hydralazine, methyldopa, prazosin |
| Antiparasitics | Permethrin |
| Antituberculous drugs | Ethambutol, isoniazid |
| Antivirals | Amantadine, acyclovir |
| Antihistamines | Cetirizine, loratadine |
| Anti-asthma/anti-allergy products | Epinephrine, inhaled bronchodilators, theophylline |
| Cardiovascular medicines | B-blockers, calcium channel blockers, digoxin, nitroglycerin |
| Constipation products | Bisacodyl, methylcellulose |
| Antidiabetics | Insulin |
| Gastrointestinal drugs | Sucralfate, metoclopramide |
| Thyroid hormones | Levothyroxine, liothyronine |
Terminals
It is very important that every pregnant woman remember that any drug during pregnancy can bring not only benefits, but also considerable harm, therefore, any self-administration during this period is not permissible, since their consequences are unpredictable and in many cases can cause irreparable harm to the developing fetus.
Keywords
Dentist examination during pregnancy | Forest Balsam
Almost every future mother has a question: how are the oral health of a woman planning a pregnancy and the health of the unborn baby interrelated? What dentists say about this - we will tell in this article.
Pregnancy is a unique and difficult period in a woman's life, when her body has to grow a full-fledged person from a couple of cells. The hormonal background of the expectant mother is significantly rebuilt, bringing changes to the work of the body. And almost every expectant mother has a question: how are dental health interrelated.
During pregnancy, a woman is more vulnerable to various oral diseases such as caries, gingivitis, stomatitis, and other infections that may well harm the baby. Therefore, p , a visit to the dentist during pregnancy is mandatory, and if there are any problems with the health of teeth and gums, then you should definitely not limit yourself to one visit.
As you know, diseases of the teeth and gums develop rather slowly, but pregnancy serves as a kind of catalyst that significantly speeds up the detection of hidden oral problems.
One of the reasons for a sharp change in the condition of teeth and gums is a change in nutrition . As a rule, during pregnancy, appetite increases and a higher amount of carbohydrates enters the oral cavity. Changing the regimen and composition of nutrition serves as an impetus for an increase in the number of microorganisms in plaque, and, accordingly, increases the risk of developing or complicating oral problems.
Toxicosis in the first trimester of pregnancy increases the acidity of saliva, which makes the oral cavity even more comfortable environment for the growth of bacteria. Together, these factors create conditions for the active formation of plaque, which, in the absence of proper hygiene, quickly turns into tartar. Tartar leads to inflammation and bleeding of the gums.
Another problem during pregnancy is lack of calcium , which plays an important role in the formation of bones and internal organs of the baby, and also affects the course of pregnancy itself. If there is not enough calcium in the woman’s blood, then the body “transfers” it to the baby from the bone tissue and teeth of the expectant mother. Accordingly, the supply of microelements to the teeth is disrupted, they become brittle and more prone to destruction.
As a rule, a dental examination during pregnancy is prescribed by gynecologists without fail. In the normal course of pregnancy, a visit to the dentist is usually scheduled at 14-16 weeks, and then at 30-32 weeks.
In general, when asked whether or not to treat teeth during pregnancy, anesthetic drugs are a concern for women. In modern dentistry, for the treatment of teeth in pregnant women, safe hypoallergenic anesthetics are used, which do not penetrate the placental barrier, do not pose any danger to the baby and are excreted from the body in natural ways. Moreover, dental treatment without anesthesia for a baby can be much more dangerous, because the fear, pain and discomfort of the expectant mother can lead to unpleasant consequences for the fetus.
Moreover, dental treatment without anesthesia for a baby can be much more dangerous, because the fear, pain and discomfort of the expectant mother can lead to unpleasant consequences for the fetus.
During pregnancy, a woman can:
- treat caries;
- treat inflammation of the gums;
- extract teeth;
- install braces;
- to carry out hygienic cleaning of teeth.
Dental procedures not recommended:
- prosthodontics;
- implantation;
- whitening;
- X-ray of teeth.
Forest Balsam products are recommended by dentists during pregnancy and lactation.
Forte Active Tea Tree Oil Toothpaste and Rinse is the best choice for oral care during pregnancy. They contain a high content of herbal decoction and phyto-extracts, help maintain oral immunity, normalize the balance of microflora, and protect gums from inflammation and bleeding*.
To make a visit to the dentist during pregnancy as comfortable as possible, we recommend that you pay increased attention to preventive measures:
Carry out hygienic cleaning of teeth from tartar. Professional cleaning is carried out using ultrasound and special toothpastes. This procedure is safe for the baby and painless for the expectant mother.
Don't forget about good oral hygiene. Brush your teeth not less than 2 times per day for 2-3 minutes , be sure to use mouthwash and floss to clean the interdental spaces.
Optimal visit the dentist while planning pregnancy and treat all existing oral diseases
* Supports oral immunity by improving the quality of hygiene, according to clinical trials, Russia 2015. Not a drug. Application does not exempt from visiting the dentist. Recommendation of dentists of the state institution of the Ministry of Health of the Russian Federation.