Antidepressants how do they work
Overview - Antidepressants - NHS
Antidepressants are a type of medicine used to treat clinical depression.
They can also be used to treat a number of other conditions, including:
- obsessive compulsive disorder (OCD)
- generalised anxiety disorder
- post-traumatic stress disorder (PTSD)
Antidepressants are also sometimes used to treat people with long-term (chronic) pain.
Read more about when antidepressants are used.
How antidepressants work
It's not known exactly how antidepressants work.
It's thought they work by increasing levels of chemicals in the brain called neurotransmitters. Certain neurotransmitters, such as serotonin and noradrenaline, are linked to mood and emotion.
Neurotransmitters may also affect pain signals sent by nerves, which may explain why some antidepressants can help relieve long-term pain.
While antidepressants can treat the symptoms of depression, they do not always address its causes. This is why they're usually used in combination with therapy to treat more severe depression or other mental health conditions.
How effective are antidepressants?
Research suggests that antidepressants can be helpful for people with moderate or severe depression.
They're not usually recommended for mild depression, unless other treatments like talking therapy have not helped.
Doses and duration of treatment
Antidepressants are usually taken in tablet form. When they're prescribed, you'll start on the lowest possible dose thought necessary to improve your symptoms.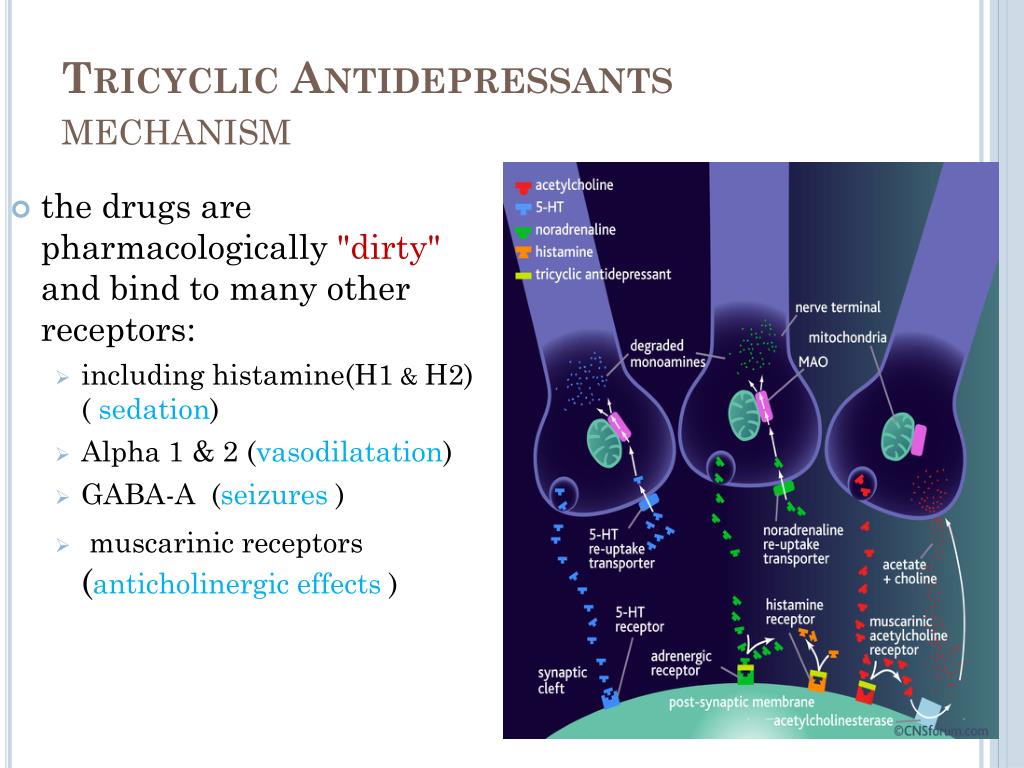
Antidepressants usually need to be taken for 1 or 2 weeks (without missing a dose) before the benefit starts to be felt. It's important not to stop taking them if you get some mild side effects early on, as these effects usually wear off quickly.
If you take an antidepressant for 4 weeks without feeling any benefit, speak to your GP or mental health specialist. They may recommend increasing your dose or trying a different medicine.
A course of treatment usually lasts for at least 6 months after you start to feel better. Some people with recurrent depression may be advised to take them indefinitely.
Read more about antidepressant dosages.
Side effects
Different antidepressants can have a range of different side effects. Always check the information leaflet that comes with your medicine to see what the possible side effects are.
The most common side effects of antidepressants are usually mild. Side effects should improve within a few days or weeks of treatment, as the body gets used to the medicine.
Read more about:
- possible side effects of antidepressants
- cautions and interactions of antidepressants
Coming off antidepressants
Talk to your doctor before you stop taking antidepressants. It's important that you do not stop taking antidepressants suddenly.
Once you're ready to come off antidepressants, your doctor will probably recommend reducing your dose gradually over several weeks – or longer, if you have been taking them for a long time.
This is to help prevent any withdrawal symptoms you might get as a reaction to coming off the medicine.
Read more about stopping or coming off antidepressants.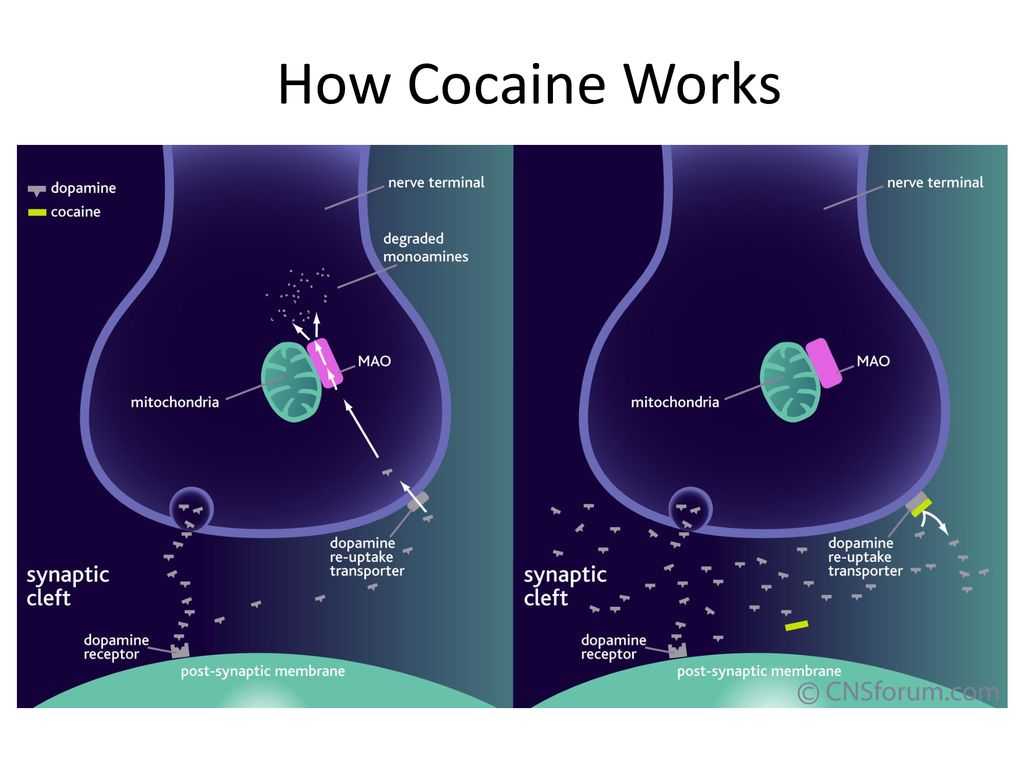
Types of antidepressants
There are several different types of antidepressants.
Selective serotonin reuptake inhibitors (SSRIs)
SSRIs are the most widely prescribed type of antidepressants. They're usually preferred over other antidepressants, as they cause fewer side effects. An overdose is also less likely to be serious.
Fluoxetine is probably the best known SSRI (sold under the brand name Prozac). Other SSRIs include citalopram (Cipramil), escitalopram (Cipralex), paroxetine (Seroxat) and sertraline (Lustral).
Serotonin-noradrenaline reuptake inhibitors (SNRIs)
SNRIs are similar to SSRIs. They were designed to be a more effective antidepressant than SSRIs. However, the evidence that SNRIs are more effective in treating depression is uncertain. It seems that some people respond better to SSRIs, while others respond better to SNRIs.
It seems that some people respond better to SSRIs, while others respond better to SNRIs.
Examples of SNRIs include duloxetine (Cymbalta and Yentreve) and venlafaxine (Efexor).
Noradrenaline and specific serotonergic antidepressants (NASSAs)
NASSAs may be effective for some people who are unable to take SSRIs. The side effects of NASSAs are similar to those of SSRIs, but they're thought to cause fewer sexual problems. However, they may also cause more drowsiness at first.
The main NASSA prescribed in the UK is mirtazapine (Zispin).
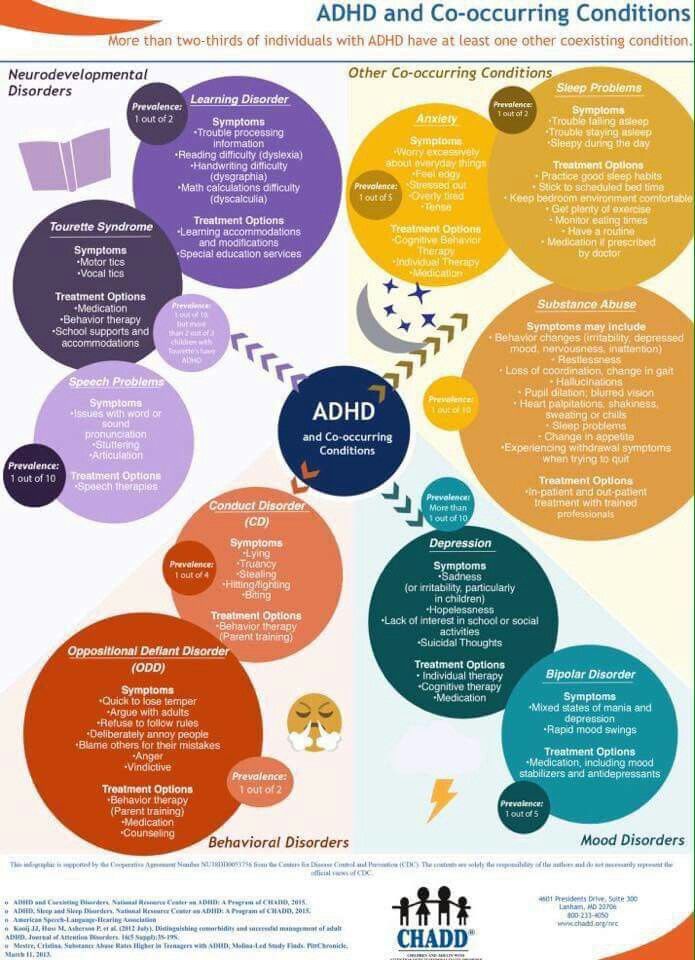
Tricyclic antidepressants (TCAs)
TCAs are an older type of antidepressant. They're no longer usually recommended as the first treatment for depression because they can be more dangerous if an overdose is taken. They also cause more unpleasant side effects than SSRIs and SNRIs.
Exceptions are sometimes made for people with severe depression that fail to respond to other treatments.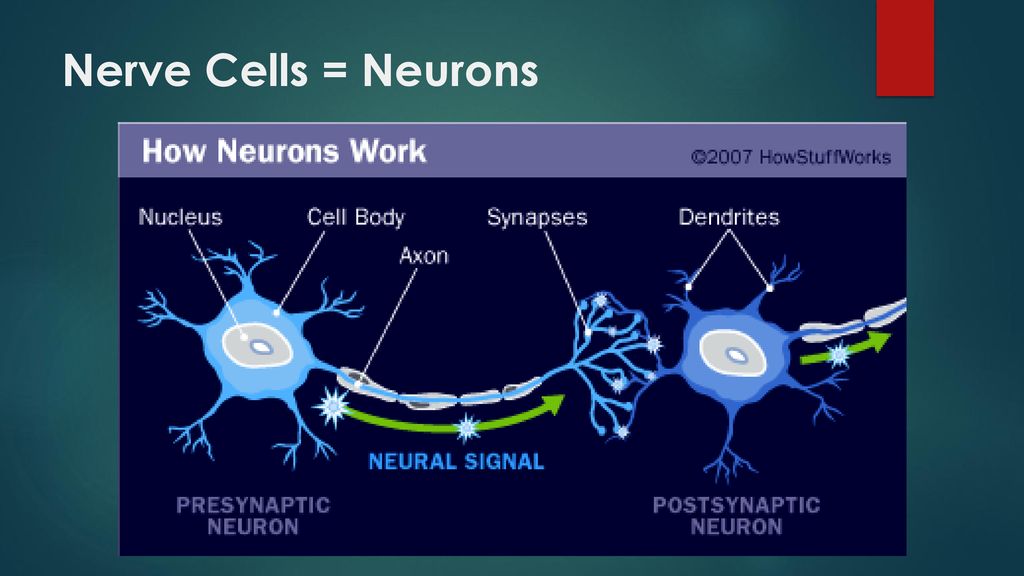 TCAs may also be recommended for other mental health conditions, such as OCD and bipolar disorder.
TCAs may also be recommended for other mental health conditions, such as OCD and bipolar disorder.
Examples of TCAs include amitriptyline, clomipramine, dosulepin, imipramine, lofepramine and nortriptyline.
Some types of TCAs, such as amitriptyline, can also be used to treat chronic nerve pain.
Serotonin antagonists and reuptake inhibitors (SARIs)
SARIs are not usually the first choice of antidepressant, but they may be prescribed if other antidepressants have not worked or have caused side effects.
The main SARI prescribed in the UK is trazodone (Molipaxin).
Monoamine oxidase inhibitors (MAOIs)
MAOIs are an older type of antidepressant that are rarely used nowadays.
They can cause potentially serious side effects so should only be prescribed by a specialist doctor.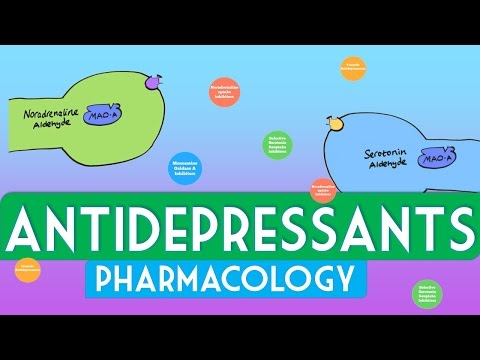
Examples of MAOIs include tranylcypromine, phenelzine and isocarboxazid.
Other treatments for depression
Other treatments for depression include talking therapies such as cognitive behavioural therapy (CBT).
People with moderate to severe depression are usually treated using a combination of antidepressants and CBT. Antidepressants work quickly in reducing symptoms, whereas CBT takes time to deal with causes of depression and ways of overcoming it.
Regular exercise has also been shown to be useful for those with mild depression.
Read more about alternatives to antidepressants.
Yellow Card Scheme
The Yellow Card Scheme allows you to report suspected side effects from any type of medicine you're taking.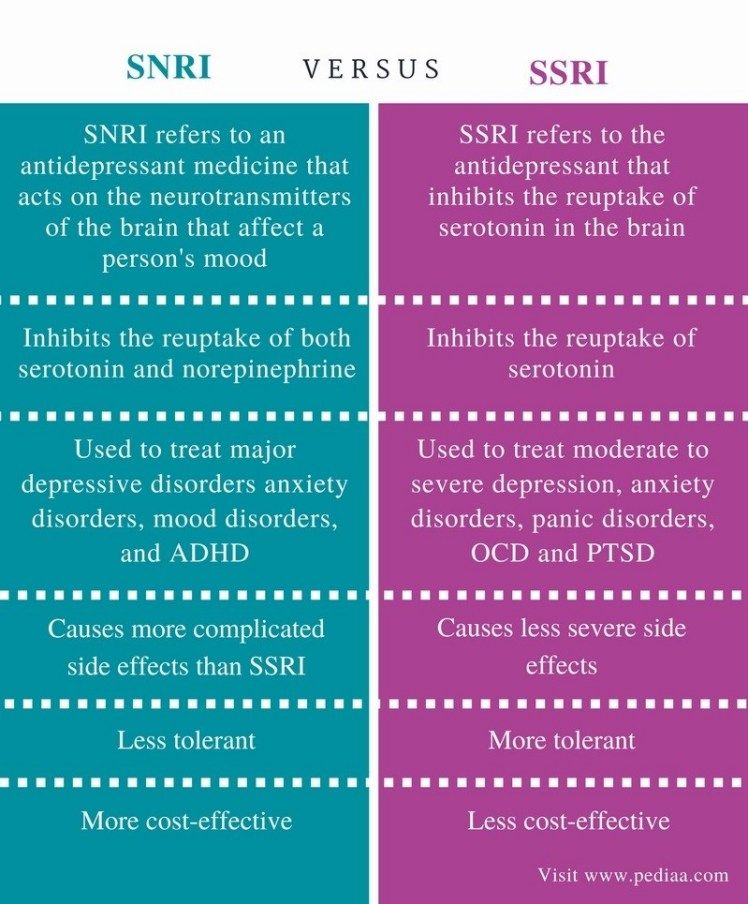 It's run by a medicines safety watchdog called the Medicines and Healthcare products Regulatory Agency (MHRA).
It's run by a medicines safety watchdog called the Medicines and Healthcare products Regulatory Agency (MHRA).
See the Yellow Card Scheme website for more information.
Community content from HealthUnlockedSide effects - Antidepressants - NHS
The side effects of antidepressants can cause problems at first, but they generally improve with time.
It's important to continue treatment, even if you're affected by side effects, as it will take several weeks before you begin to benefit from treatment. With time, you should find that the benefits of treatment outweigh any problems from side effects.
During the first few months of treatment, you'll usually see your doctor or a specialist nurse at least once every 2 to 4 weeks to see how well the medicine is working.
For more information about your specific medicine, see the patient information leaflet that comes with it.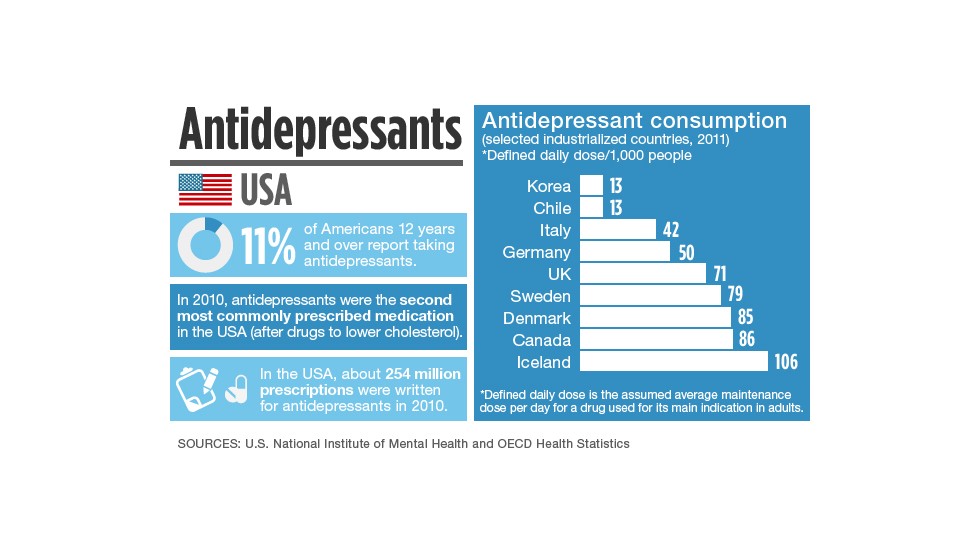
SSRIs and SNRIs
Common side effects of selective serotonin reuptake inhibitors (SSRIs) and serotonin-noradrenaline reuptake inhibitors (SNRIs) can include:
- feeling agitated, shaky or anxious
- feeling and being sick
- indigestion and stomach aches
- diarrhoea or constipation
- loss of appetite
- dizziness
- not sleeping well (insomnia), or feeling very sleepy
- headaches
- loss of libido (reduced sex drive)
- difficulties achieving orgasm during sex or masturbation
- difficulties obtaining or maintaining an erection (erectile dysfunction)
These side effects should improve within a few weeks, although some can occasionally persist.
Tricyclic antidepressants (TCAs)
Common side effects of TCAs can include:
- dry mouth
- slight blurring of vision
- constipation
- problems passing urine
- drowsiness
- dizziness
- weight gain
- excessive sweating (especially at night)
- heart rhythm problems (arrhythmia), such as noticeable palpitations or a fast heartbeat (tachycardia)
The side effects should ease after a couple of weeks as your body begins to get used to the medicine.
Potential health risks
Serotonin syndrome
Serotonin syndrome is an uncommon, but potentially serious, set of side effects linked to SSRIs and SNRIs.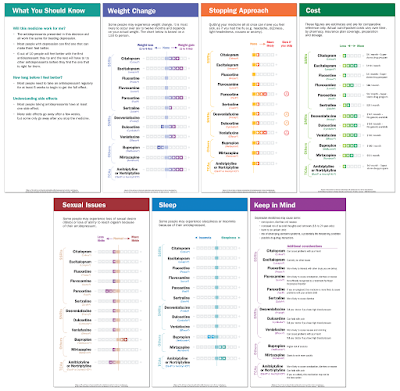
Serotonin syndrome occurs when the levels of a chemical called serotonin in your brain become too high. It's usually triggered when you take an SSRI or SNRI in combination with another medicine (or substance) that also raises serotonin levels, such as another antidepressant or St John's wort.
Symptoms of serotonin syndrome can include:
- confusion
- agitation
- muscle twitching
- sweating
- shivering
- diarrhoea
If you experience these symptoms, you should stop taking the medicine and get immediate advice from your GP or specialist. If this is not possible, call NHS 111.
Symptoms of severe serotonin syndrome include:
- seizures (fits)
- irregular heartbeat (arrhythmia)
- unconsciousness
If you experience symptoms of severe serotonin syndrome, get emergency medical help immediately by dialling 999 to ask for an ambulance.
Hyponatraemia
Elderly people who take antidepressants, particularly those who take SSRIs, may experience a severe fall in sodium (salt) levels, known as hyponatraemia. This may lead to a build-up of fluid inside the cells of the body, which can be potentially dangerous.
This can happen because SSRIs can block the effects of a hormone that regulates levels of sodium and fluid in the body. Elderly people are vulnerable because fluid levels become more difficult for the body to regulate as people age.
Mild hyponatraemia can cause symptoms similar to depression or side effects of antidepressants, such as:
- feeling sick
- headache
- muscle pain
- reduced appetite
- confusion
More severe hyponatraemia can cause:
- feeling listless and tired
- disorientation
- agitation
- psychosis
- seizures (fits)
The most serious cases of hyponatraemia can cause you to stop breathing or enter a coma.
If you suspect mild hyponatraemia, you should call your GP for advice and stop taking SSRIs for the time being.
If you suspect severe hyponatraemia, call 999 and ask for an ambulance.
Hyponatraemia can be treated by feeding a sodium solution into the body through an intravenous drip.
Diabetes
Long-term use of SSRIs and TCAs has been linked to an increased risk of developing type 2 diabetes, although it's not clear if the use of these antidepressants directly causes diabetes to develop.
It may be that the weight gain some people using antidepressants experience increases the risk of them developing type 2 diabetes.
Suicidal thoughts
In rare cases, some people experience suicidal thoughts and a desire to self-harm when they first take antidepressants. Young people under 25 seem particularly at risk.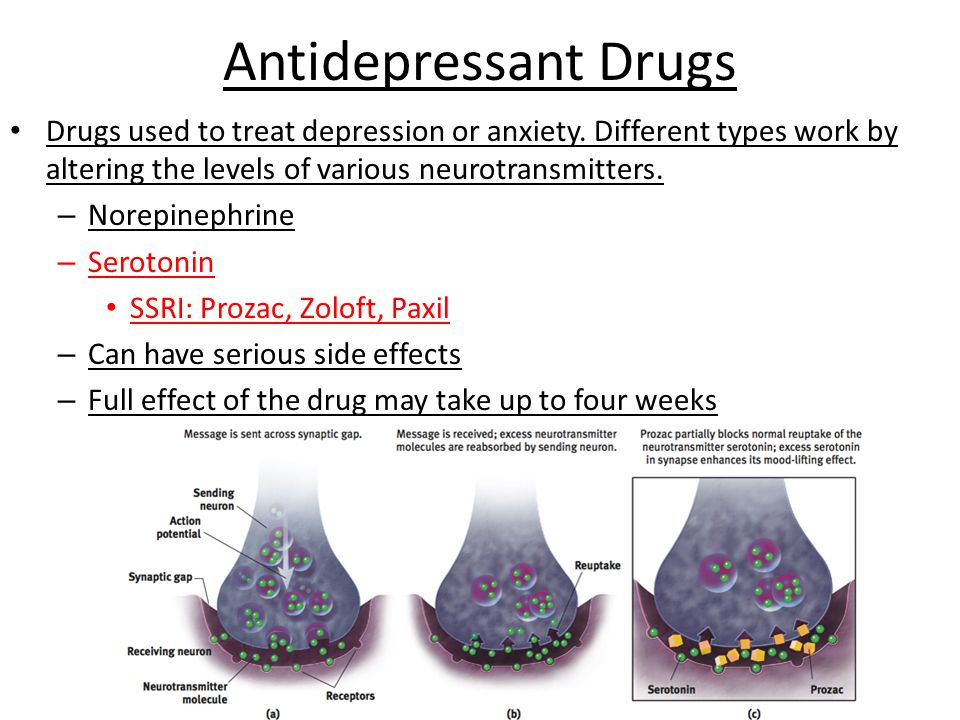
Contact your GP, or go to A&E immediately, if you have thoughts of killing or harming yourself at any time while taking antidepressants.
It may be useful to tell a relative or close friend if you've started taking antidepressants and ask them to read the leaflet that comes with your medicines. You should then ask them to tell you if they think your symptoms are getting worse, or if they're worried about changes in your behaviour.
Page last reviewed: 4 November 2021
Next review due: 4 November 2024
Guide to antidepressants: how do they work?
Treatment
Depression of the Health Guardian Guest
Davydovspid.p.Center
13 JULY 2022
223910
AIDS
“Species Center” is nervous about depression, and, this is a pressing problem.
 This time, with the help of Maria Danina, Candidate of Psychological Sciences, our authors have compiled a short guide to antidepressants. Their types, principles of operation and device. All basic concepts in one text.
This time, with the help of Maria Danina, Candidate of Psychological Sciences, our authors have compiled a short guide to antidepressants. Their types, principles of operation and device. All basic concepts in one text. Depression is quite common: according to WHO, more than 300 million people of all ages and genders suffer from it worldwide.
As defined by the American Psychiatric Association, this serious illness can take many forms, vary in severity from person to person, and coexist with other conditions that cause similar symptoms, such as anxiety disorders.
Since the causes of depression are related to disorders of the brain, it is useless to call on patients with depression to "pull themselves together" - its symptoms cannot be overcome by willpower, just as it is impossible to influence the brain by willpower.
“Mood is our subjective experience, that is, what we can become aware of and what we can give an account of. At the heart of any psychological phenomenon are complex and multi-level processes that take place in our nervous system. In particular, neurochemical ones,” explains Maria Danina, senior researcher at the Laboratory of the Scientific Foundations of Psychotherapy, Candidate of Psychological Sciences.
In particular, neurochemical ones,” explains Maria Danina, senior researcher at the Laboratory of the Scientific Foundations of Psychotherapy, Candidate of Psychological Sciences.
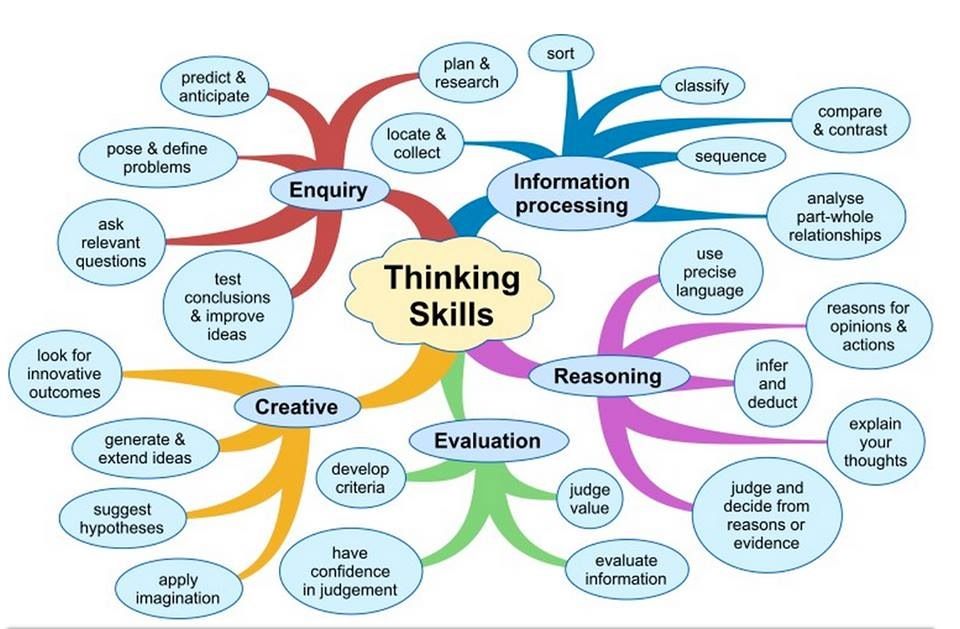
According to her, according to the monoamine theory, three different monoamine neurotransmitters contribute to depressive symptoms. Moreover, neurotransmitters do not "trigger" the disease by themselves, but affect certain processes, which, in fact, lead to depression.
First, it is dopamine, which is involved in the motivation system. A lack of dopamine can lead to anhedonia—that is, the inability to experience pleasure.
Secondly, it is norepinephrine. It is involved in the regulation of our daily activities. Its deficiency is associated with psychomotor retardation (when a person begins to move and speak more slowly than usual).
And thirdly, serotonin. Which is involved in the control of the sensitivity of the pain system, suppresses pain signals and negative emotions.
Lack of serotonin leads to increased pain, negative emotions and anxiety. In addition, due to a lack of serotonin, obsessive states develop, associated with constantly recurring thoughts about the past and the causes of one's current state, which are difficult to get rid of - psychiatrists call this rumination.
In addition, due to a lack of serotonin, obsessive states develop, associated with constantly recurring thoughts about the past and the causes of one's current state, which are difficult to get rid of - psychiatrists call this rumination.
“In addition to lowering the level of neurotransmitters, other groups of biologically active substances, such as glucocorticoids, can contribute to depression,” notes Maria Danina. - Let's say that the level of the famous "stress hormone" cortisol also increases with depression - and this in turn leads to a lack of dopamine. Monoamine levels can be affected by thyroid hormones and the sex hormones estrogen and progesterone.”
However, many factors can trigger clinical depression, such as hereditary predisposition, low self-esteem, difficult life circumstances, severe stress, and chronic diseases. And therefore, we cannot “shift all the blame” only on violations in the brain, emphasizes Maria Danina.
Neurotransmitters and their effects depending on deficiency or excessLife in the “serotonin pit”
An alternative to the monoamine theory, which from the point of view of many scientists can no longer be considered the main one, is the biopsychosocial model of depression. In accordance with it, the development of the disease is influenced not only by biological, but also by psychological factors.
In accordance with it, the development of the disease is influenced not only by biological, but also by psychological factors.
“A person may experience loss (grief) or severe frustration of their needs (stress). As a result, his neurochemistry also changes,” explains Danina. “But this is the so-called normal “mourning process.” Doctors talk about reactive depression only if, even after months, a person continues to experience all the same unpleasant sensations, and over time, his condition only worsens.
In some people, however, the functional characteristics of their neurons make them more prone to depression. Such patients "start" the process does not require external circumstances. And their depression has a non-reactive "endogenous" character.
In both cases, in addition to psychotherapy, doctors prescribe antidepressants, that is, drugs that can affect neurotransmitters in the brain, as a medical aid.
There are five classes in total. Each of which affects the brain in its own way.
1. Selective serotonin reuptake inhibitors (SSRIs).
SSRI drugs increase serotonin levels. This helps to more accurately regulate mood and gradually overcome moderate to severe depression. These drugs do their job by "forbidding" neurons to absorb serotonin from the synaptic gap between neurons. As a result, neurons are able to communicate better.
SSRIs have fewer side effects than other classes of antidepressants. For example, in case of an overdose, they do not disrupt cardiac conduction and do not lead to convulsions.
However, the side effects are still there and quite serious - from increased suicidal thoughts to sexual dysfunction, drowsiness, dry mouth, dizziness and headache.
In addition, all drugs that increase the level of serotonin in the brain can cause serotonin syndrome - a situation where the neurotransmitter becomes too much.
Serotonin and signal transmission through nerve cells. In serotonin syndrome, the person becomes overexcited, restless, sweats and has an increased heart rate.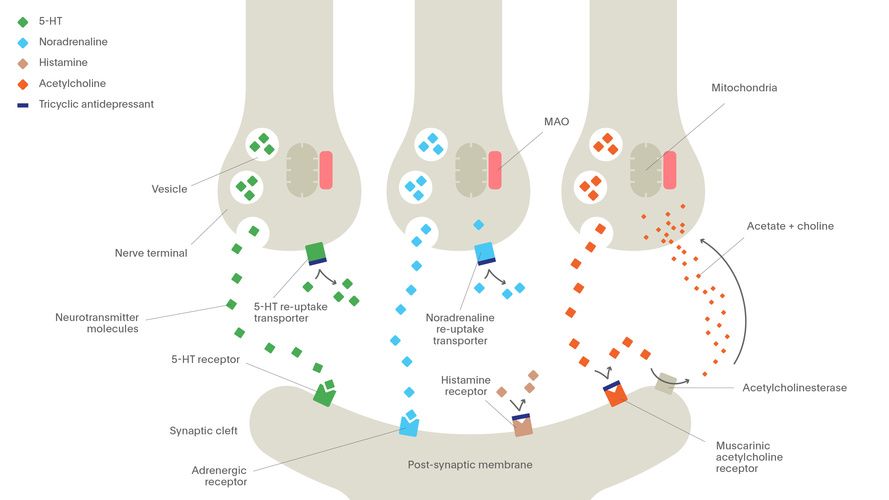 That is why being treated simultaneously with two antidepressants that increase serotonin levels is dangerous to life and health.
That is why being treated simultaneously with two antidepressants that increase serotonin levels is dangerous to life and health.
2. Selective serotonin and norepinephrine reuptake inhibitors (SNRIs).
SNRIs work in much the same way as SSRIs, with one difference. Drugs “forbid” neurons to absorb not only serotonin, but also norepinephrine, a neurotransmitter that is involved in the regulation of emotions and thought processes.
And since norepinephrine works in close conjunction with serotonin and dopamine, SNRIs are thought to increase attention, focus, and improve memory.
The indications and side effects of SNRIs are very similar to those of SSRIs. There are few advantages of this class of drugs over SSRIs, but for some patients they are better suited.
3. Atypical antidepressants.
This class includes drugs with different modes of action that have only one thing in common - these drugs are not like SSRIs and SNRIs.
Although some drugs in this class also "prohibit" neurons from taking up serotonin, like reuptake inhibitors, some of them can act on receptors for other neurotransmitters. This allows you to fine-tune the sensitivity of neurons to one or another substance.
It is worth noting that the components of some atypical antidepressants - say, bupropion - are listed in the note to the list of psychotropic substances subject to control in the Russian Federation. And although this tool is approved by reputable international medical organizations - for example, the US Food and Drug Administration (FDA), it cannot be legally purchased in Russia.
The side effects of this class of drugs depend on the specific drug. For example, some atypical antidepressants make you sleepy, while others, on the contrary, invigorate. To choose the right medicine, the doctor must take into account the peculiarities of the legislation, individual symptoms and the patient's health status.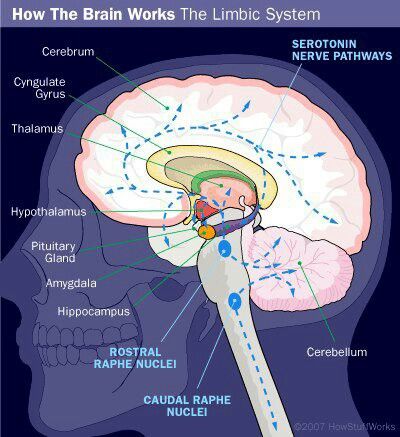
4. Tricyclic antidepressants (TCAs).
All drugs in this class are thought to increase the levels of norepinephrine and serotonin in the brain, much like SNRIs do.
But TCAs have a very important difference - they are able to act on brain receptors that bind to other substances. In overdose, this leads to severe side effects, such as seizures and complete heart block. And although TCAs are quite effective, drugs from this group today are trying to use as little as possible.
5. Monoamine oxidase inhibitors (MAOIs).
This class of drugs "turns off" monoamine oxidase, an enzyme that breaks down norepinephrine, serotonin, and dopamine in the brain. As a result, neurotransmitters are not destroyed and remain in the synaptic cleft for a long time.
Unfortunately, MAOIs have many side effects, including high blood pressure, weight gain, swelling, sexual dysfunction, and suicidal ideation. So today, drugs of this class are used only under strict medical supervision and as a last resort - if other antidepressants have not helped.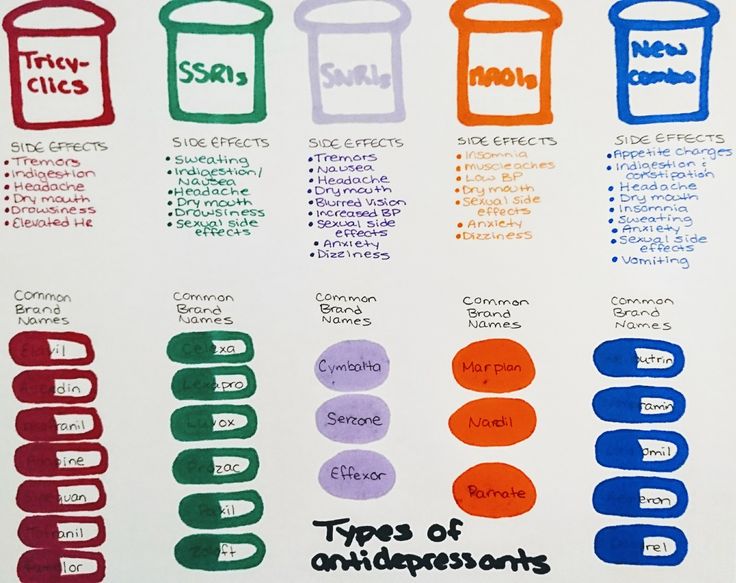
Is it possible to do without antidepressants?
In medicine, there is the concept of a balance of benefits and harms. This is exactly what the old medical saying about medicines says, which "cure one thing - cripple another." When deciding to prescribe an antidepressant (or any other powerful drug), the doctor always thinks about whether it will benefit a particular patient.
related
Society
"You will burn in paradise!" Is depression really permanent?
- DepressionMedicineRussia
Of course, antidepressants are drugs with serious side effects, the abuse of which will not lead to anything good. However, this does not mean that the life of a person with depression without antidepressants will be any better.
What happens if you stop taking the antidepressants prescribed by your doctor? The biggest risk is the return of depression. Moreover, 80% of patients who abruptly stop taking antidepressants develop a withdrawal syndrome. This condition appears within a few days after discontinuation and can last up to two weeks.
Moreover, 80% of patients who abruptly stop taking antidepressants develop a withdrawal syndrome. This condition appears within a few days after discontinuation and can last up to two weeks.
From a medical point of view, it is not too dangerous, but the sensations can be quite unpleasant.
Withdrawal symptoms can be divided into four groups:
- gastrointestinal: nausea, vomiting, diarrhea and abdominal cramps;
- somatic: headaches, lethargy and sweating;
- sleep-related: insomnia or excessive sleepiness, nightmares;
- affective: restlessness, agitation and bad mood.
To avoid withdrawal syndrome, the physician should gradually reduce the dose of antidepressants. This may take several weeks or even several months.
Moreover, not only giving up antidepressants on your own, but also “prescribing” them to yourself without consulting a specialist is harmful.
“If you have symptoms of depression that do not go away for more than two weeks, this is a reason to consult a psychiatrist.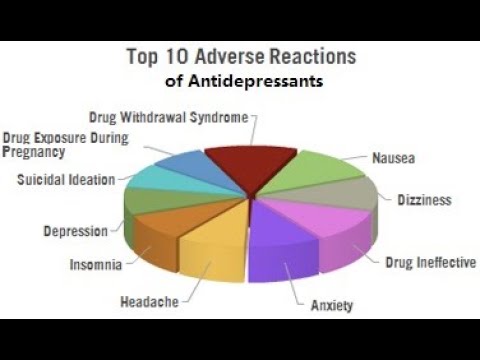 The sooner the better, because early treatment gives a better prognosis,” Maria Danina sums up.
The sooner the better, because early treatment gives a better prognosis,” Maria Danina sums up.
Doctors sometimes have to try several different antidepressants to find the right one for you. But it will not be possible to do without a specialist: only during a personal examination, the doctor can confirm the diagnosis and prescribe treatment, she emphasizes.
Where to go for depression?
There are several exits:
- neuropsychiatric dispensary at the place of residence (free of charge),
- psychiatric hospital (free of charge),
- private clinic (extra charge),
- private doctor (for a fee).
Of all the options described for the treatment of depression, the last three options are preferred.
Also, whether you have a confirmed diagnosis of depression, are on medication, or only suspect you have an illness, you may need support - informational or emotional.
At the time of publication of the article for people who suspect depression, there are:
- 24-hour hotline of the Moscow Service for Psychological Assistance to the Population: from a landline for Moscow residents - 051, free of charge; from a mobile phone - 8-495-051 *, only the services of a telecom operator are paid according to the tariff plan.

- Emergency medical and psychological assistance in crisis situations - (495) 205-05-50.
- Emergency psychological help - (495) 575-87-70.
- Hotline of the Psychological Assistance Ministry of Emergencies of Russia - (499) 216-50-50.
This material was prepared for you by the editors of the AIDS.CENTER Foundation. We exist thanks to your help.
You can support our work at this link.
let's be friends?
- read
- read
- enter
- read
read also
Society "Injured people remember too little and too much at the same time." Why do we remember insults and how to live with it?
- Psychology
EpidemicCure Everyone: what is happening in Russia with the treatment of hepatitis C
- Hepatitis
SocietyHormones, psychology and DNA: six books about love from psychologists, neuroscientists and anthropologists
- WomenArtHistory
Daniil Davydov
medical journalist
Author profile
At the same time, the cures for this disease are surrounded by many myths. Antidepressants are accused of ineffectiveness and severe side effects, but often the problem is not with the drugs themselves, but with their misuse.
Antidepressants are accused of ineffectiveness and severe side effects, but often the problem is not with the drugs themselves, but with their misuse.
We collected 8 myths about antidepressants and found out how close they are to the truth.
Go see a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
Myth 1
Antidepressants almost never helpMost likely, this myth arose due to the fact that antidepressants do not work in all patients - so even some doctors and scientists doubt their effectiveness. However, antidepressants cannot be called ineffective, there are just important nuances in the use of these drugs.
Antidepressants are a class of drugs that normalize the level of neurotransmitters, that is, chemicals that help nerve cells in the brain exchange information.
What are Antidepressants - International Drug Database RxLis
What Medications Help Clinical Depression in Adults - International Primer for Physicians UpToDate
How Antidepressants Help Pain - Mayo Clinic Bulletin
All antidepressants used to treat depression in adults Adults Working - The Lancet
Who Antidepressants Work and Who Don't - Clinical Guidelines for British PhysiciansPDF, 141KB
These medicines help people whose problems are due to a deficiency or excess of neurotransmitters. Antidepressants reduce symptoms of depression, obsessive-compulsive disorder, generalized anxiety disorder, post-traumatic stress disorder, and bipolar affective disorder.
There is evidence that antidepressants are effective for chronic pain. Antidepressants increase the amount of neurotransmitters in the spinal cord, which reduces pain signals.
Most specialists have no doubts that antidepressants work. For example, according to the British Royal College of Psychiatry, 50-65% of people with depression who take antidepressants feel better - compared with 25-30% of those who take a placebo.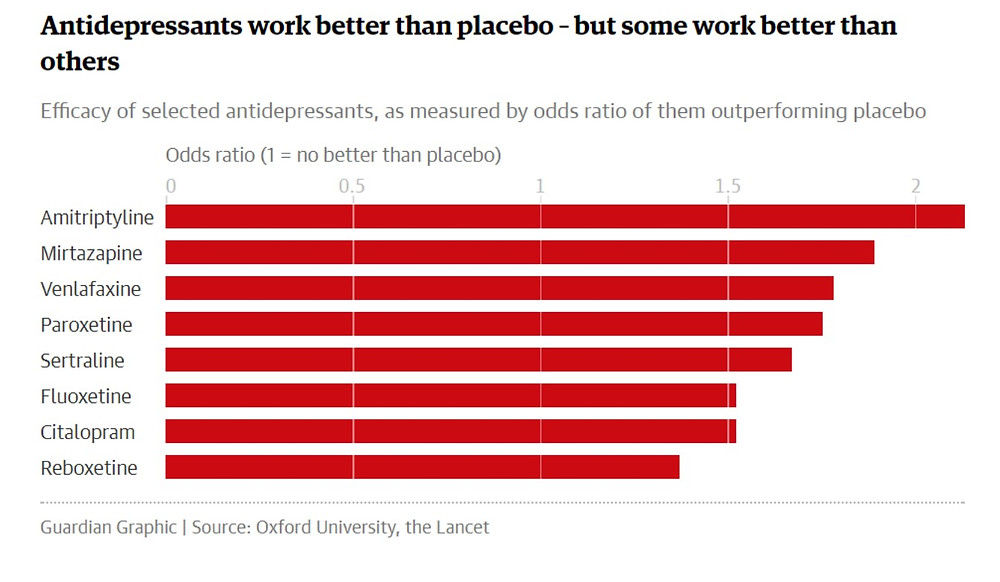
However, there are situations where the benefit of antidepressants is questionable. For example, antidepressants are good for treating moderate to severe depression, but do not work well for people with mild depression - psychotherapy is more suitable for them.
And there are situations when these medicines were prescribed by mistake. Then antidepressants really won't help.
When antidepressants don't help
Sergey Divisenko
psychotherapist
There are three cases when antidepressants most often cause problems.
The antidepressant didn't work because the doctor prescribed the wrong dose. Minimum doses of these drugs do not help in half of the cases. Then competent doctors increase the doses to those recommended in clinical guidelines, while illiterate ones refuse them.
Sometimes, in order for antidepressants to work, they need to be augmented—i.e., enhanced—with other classes of drugs. For example, second-generation antipsychotics, or normothymics, that is, drugs that stabilize mood.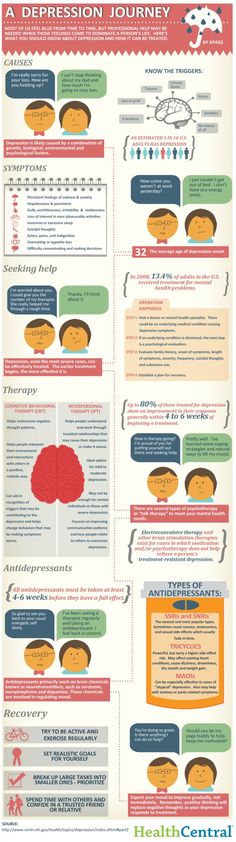 If this is not done, the person taking antidepressants will not feel relief.
If this is not done, the person taking antidepressants will not feel relief.
The antidepressant didn't work because the doctor misdiagnosed and was trying to treat a condition that these drugs don't work for. To help a person, one had to either use other drugs or use non-drug methods of treatment: for example, psychotherapy, transcranial stimulation, or electroconvulsive therapy.
For example, in bipolar disorder, symptoms can be very similar to depression or anxiety. But with bipolar disorder, antidepressants help only if they are used together with other drugs - mood stabilizers. By themselves, they will either work for a short time, or they will not work, or they can cause a phase inversion - that is, a person will switch from a depressive phase to a manic one.
The patient was not helped by a particular antidepressant, but another might. Antidepressants differ in the principle of action - on this basis they are divided into classes. It happens that one antidepressant does not work, but another from the same or another class helps. If the treatment does not work, you should not stop drug therapy, but continue to look for a drug that will help this particular patient.
It happens that one antidepressant does not work, but another from the same or another class helps. If the treatment does not work, you should not stop drug therapy, but continue to look for a drug that will help this particular patient.
Myth 2
Antidepressants only relieve symptoms, but do not eliminate the cause of the disorderIn most cases, this is not a myth. However, in some situations, antidepressants act on the cause of the disorder.
Depression is a heterogeneous disease. Experts identify a different number of subtypes of depression - from 4 to 12. But for our purposes, depression can be divided into two large subtypes.
American Criteria for Depressive Disorders - A Handbook for Psychiatrists DSM-5PDF, 32 MB
What Depression Is - An International Primer for Physicians UpToDate
associated with depression. Disorders that can be attributed to this group are more common.
If these causes affect a person long enough and he does not understand how to deal with them, depression may develop.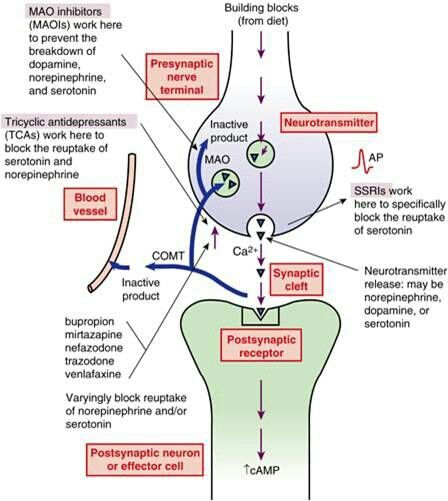 In this situation, antidepressants act as drugs that alleviate the symptoms of the disease. To influence the cause of the problem, psychotherapy is needed.
In this situation, antidepressants act as drugs that alleviate the symptoms of the disease. To influence the cause of the problem, psychotherapy is needed.
Depression provoked by internal causes. Approximately 7% of people with depression have the correct way of thinking, there are no internal conflicts and injuries, and there are no serious illnesses. In this situation, the cause of depression is the lack of neurotransmitters: serotonin, norepinephrine and dopamine in the synapses of brain nerve cells. In such people, the antidepressant acts precisely on the cause of the disease, that is, it corrects the production of serotonin in neuronal synapses.
Myth 3
As soon as it gets better, you can stop taking the antidepressantThis is also not entirely a myth - it would be more correct to call it a belief that is true only for some, but not for all patients with depression.
It is generally advised to continue taking antidepressants for at least six months after remission.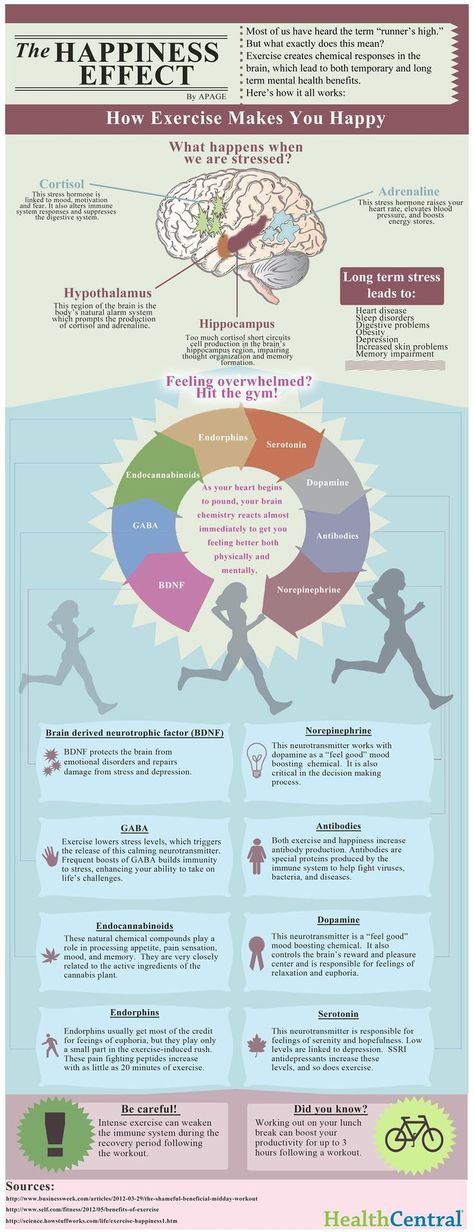 If the duration of the disease is short, that is, the person was ill for about two weeks, then for the onset of remission, one or two months usually need to take medication. If the duration of the disease is long, from several months or years, then more time is required for the onset of remission. It’s impossible to say exactly how much: different people with depression have different recovery times.
If the duration of the disease is short, that is, the person was ill for about two weeks, then for the onset of remission, one or two months usually need to take medication. If the duration of the disease is long, from several months or years, then more time is required for the onset of remission. It’s impossible to say exactly how much: different people with depression have different recovery times.
Some people have recurrent depression. In this case, the period during which you need to take the medicine depends on how many bouts of depression have already been during your life. If more than three, it is recommended to take antidepressants for several years or for life.
Myth 4
Antidepressants cause addiction Perhaps the roots of this myth are that some people need to take depression medication for life. And at the beginning of treatment, some patients have to increase the dose. But in fact, antidepressants do not cause either true physical or drug dependence.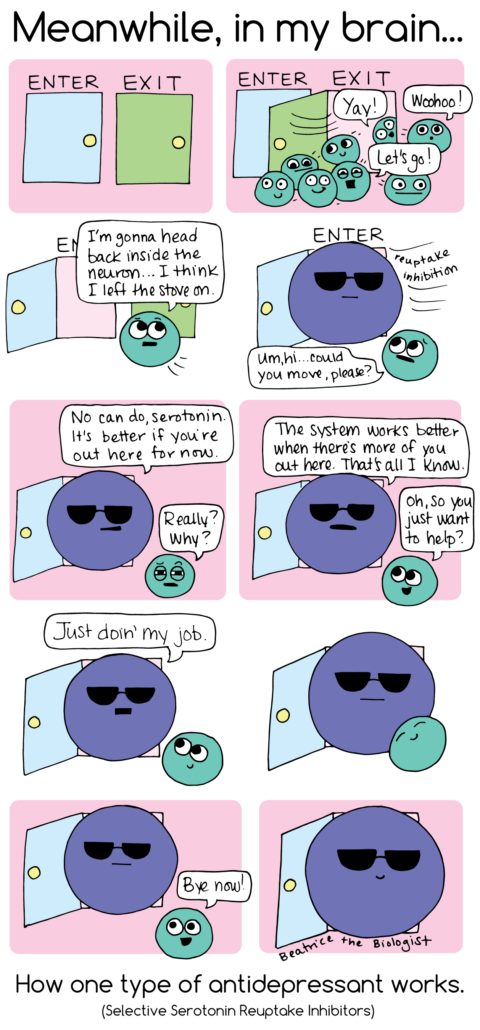
True physical dependence on a drug is a situation where a person becomes so addicted to the drug that when it is withdrawn, the symptoms of the disease sharply increase. People who are dependent on the drug have to increase the dosage, otherwise the drug stops helping.
What is True Drug Addiction - Bulletin of the National Institute for the Study of Drug AbusePDF, 7 MB
What is Drug Addiction - Bulletin of the American Psychiatric Association
Drug dependence may include physical dependence on a drug. But this addiction has a unique feature. Dependence can also develop in a healthy person who used the drug not to recover, but to enjoy it. But when he tries to quit the drug, he still experiences physical suffering, which is called the withdrawal syndrome. As a result, a person is forced to look for a new dose of a drug.
Although a person who takes antidepressants to treat depression gets better, the drugs themselves are neither pleasurable nor addictive.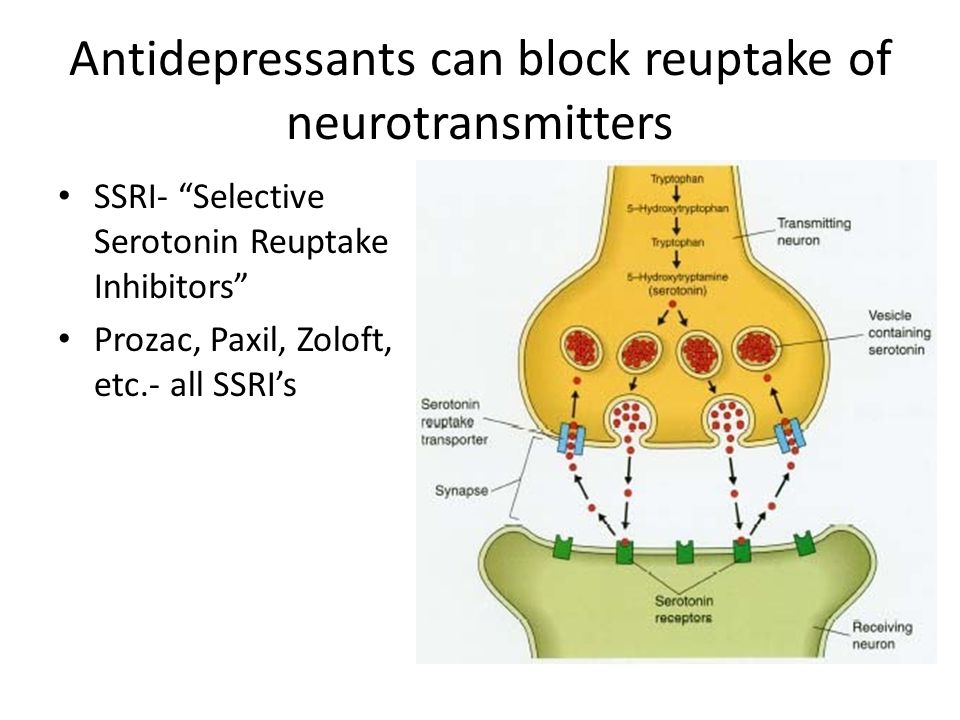 Taking them as drugs is useless.
Taking them as drugs is useless.
Of all the drugs that are used in psychiatry, true physical dependence can only be caused by psychostimulants that activate mental activity and anti-anxiety, that is, benzodiazepine tranquilizers. Antidepressants are not included in this list, because there is no need to increase the dosage of correctly selected drugs from this group.
However, some people who stop taking antidepressants early sometimes experience withdrawal symptoms such as nausea, hand tremors, and some feel “shocks” in the head, similar to the sensations of an electric shock. Depressive symptoms return to patients who need to take the medicine for a very long time.
Antidepressants are sometimes abused, but they cannot cause addiction - Journal of Modern Psychiatry
To avoid unpleasant consequences, stop taking antidepressants only if the attending physician says that they are no longer needed. But even in this situation, it is necessary to cancel antidepressants slowly, that is, gradually reducing the dose. This will help avoid unpleasant side effects.
This will help avoid unpleasant side effects.
Myth 5
A person on antidepressants becomes lethargic and loses interest in lifeThis popular myth is based on real but outdated data.
These mental changes are seen in patients taking first-generation tricyclic antidepressants such as amitriptyline. It has a sedative, that is, a sedative effect. A person who takes high doses of amitriptyline can indeed become sleepy and indifferent to the outside world.
Amitriptyline - Sedative - Drugs.com International Drug Database
SSRIs do not sedate - Drugs.com International Drug Database
Current second-generation antidepressants that are recommended to start treatment with, such as selective serotonin reuptake inhibitors, or SSRIs almost never cause drowsiness and apathy.
On the contrary, in most people with depression they return interest in life.
Sometimes SSRIs do cause drowsiness, but this has not yet been proven
Sergey Divisenko
psychotherapist
It is believed that in rare cases, modern antidepressants can provoke SSRI-induced apathy. But this condition is extremely rare.
But this condition is extremely rare.
And even then psychiatrists still doubt that the cause is precisely in the drugs, and not in the patient's condition. After all, some people during the time of taking antidepressants may develop other adverse mental states in which apathy occurs: for example, schizotypal disorder, which was not noticed before.
Myth 6
Antidepressants have many side effectsThis is partly true: both SSRIs and antidepressants from other groups have side effects. But it is quite possible to deal with them.
At the start of treatment, when people first start taking antidepressants, many complain of increased anxiety, dry mouth, nausea, and trouble sleeping. But after a few days or weeks after the start of the course of treatment, these symptoms usually disappear. If the side effects do not stop, it makes sense to consult a doctor - he will replace the antidepressant.
Dealing with antidepressant side effects - tips from the Mayo Clinic staff
Here's what to do before the side effects go away:
- take your antidepressant with meals, unless the instructions say otherwise, so the antidepressant will be less annoying stomach;
- put a bottle of clean water on the work table - if your mouth is dry, you can take a sip.
 Unsweetened lollipops and chewing gum also help with dry mouth;
Unsweetened lollipops and chewing gum also help with dry mouth; - take a walk for at least half an hour before going to bed to make it easier to fall asleep. If you can’t sleep at all, you can ask your doctor to pick up sleeping pills.
The second most common side effect is increased anxiety at the beginning of antidepressant use. To avoid this problem, psychiatrists resort to two effective methods:
- titrate the dose - that is, start with the minimum dose of the antidepressant, and then gradually increase it;
- at the beginning of the reception, sedatives - tranquilizers are prescribed together with the antidepressant.
The third common side effect of SSRIs, especially sertraline, known as Zoloft, and escitalopram, better known as Cipralex, is decreased libido. Approximately 20-30% of people taking antidepressants from this group experience a decrease in sexual desire to one degree or another. At the same time, it is difficult to say how much the drugs are to blame, because approximately 35-50% of people with depression have already experienced sexual dysfunction.
Many people with depression experience sexual dysfunction before starting antidepressants - Harvard Medical School Bulletin
Switching to another antidepressant usually helps, but many people prefer to wait until the medication can be stopped. In some cases, psychiatrists prescribe antidepressants from other groups in addition to the libido-lowering antidepressant. Sometimes it helps to regain interest in sex.
Myth 7
Weight gain due to antidepressantsThis is not a myth, but a half-truth. There are both antidepressants that contribute to weight gain, and those that do not have a similar effect.
The most common complaint about weight gain during treatment is people taking the tetracyclic antidepressant mirtazapine, which actually increases appetite. Another weight gaining antidepressant is paroxetine, better known by the trade name Paxil. But "Zoloft" and "Cipralex" do not contribute to weight gain.
If a patient feels that an antidepressant is causing them to overeat, it is wise to consult a doctor and discuss a change of medication.
Myth 8
Antidepressants are expensiveTrue, but not for all patients. Most people can cure depression and not go broke.
Antidepressants from different groups vary greatly in price. There are both very expensive drugs and relatively low-cost drugs among them. At the same time, both of them work equally well. However, there are situations when a cheap antidepressant cannot be dispensed with.
On the left - inexpensive "Zoloft" for 327 R, a drug based on sertraline, on the right - the most expensive antidepressant "Ixel" based on milnacipran for 2453 R For example, there is a good antidepressant venlafaxine. The maximum dose of venlafaxine can reach up to 375 mg per day. If these are inexpensive tablets of a domestic manufacturer, then a course of treatment for a month costs about 2000 R. But sometimes inexpensive tablets are not very well tolerated: they cause headache, nausea, sweating, tachycardia, that is, rapid heartbeat. In such cases, you need to switch to a prolonged form of venlafaxine - "Venlafaxine Retard", or "Velaxin XR".