Advocate mentally ill
What Does It Mean to Be a Mental Health Advocate?
JUN. 24, 2020
By Kristen Fuller, M.D.
Mental health encompasses our emotional health, cognitive health and relationships. It includes taking care of and protecting ourselves so we can succeed in everyday life, taking care of others when they need us the most and overcoming obstacles. In other words, mental health is essential, and worth advocating for.
If we want to be advocates for those who are struggling with their mental health, we must first learn to be advocates for ourselves. This means being true to ourselves, loving ourselves and honoring ourselves, regardless of what our struggles are.
What is a mental health advocate?
Mental health advocates are heroes — individuals who do not wear capes, but who work tirelessly every day to share their stories and help those who are struggling. They take risks and show their vulnerability by telling their truth in hopes of encouraging someone else.
Whether it is through a blog, social media, a book or a speaking engagement, these advocates stand up for others who do not have a voice. They remind us that we are not alone in our struggles. They remind us that we are not at fault. They remind us that there is light, healing and hope throughout this journey. They shatter stereotypes and stigma associated with mental illness.
As an example, my dear friend Daisy Martinez wrote a letter to herself on her social media account about her struggles with mental illness, and how she found the strength and courage to get help and love herself.
“What would I tell this 18-year-old Daisy holding her almost one-month-old baby next to her mom at her high school graduation?
You’re going to be alright. I know you’re scared. I know you’re hurt. I wish I could tell you that the upcoming years will get easier, but they will actually be your toughest years. However, you will get through it all and grow so much.
You will find the courage to leave the abusive relationship you’re currently in. You will find a way to thrive as a single parent. Your grades will drop. You will actually get into academic probation. You will get very depressed and start doing drugs. You will attempt suicide a few times, but this will [lead you] to receiving help.
You will find a way to thrive as a single parent. Your grades will drop. You will actually get into academic probation. You will get very depressed and start doing drugs. You will attempt suicide a few times, but this will [lead you] to receiving help.
You start to see a therapist. You stop doing drugs. You start to get your grades back up. You actually graduate from college and get into graduate school. You even start a non-profit. You will feel lost and like something is missing. That missing part is the love you need to give yourself.
You are loved so much and worthy of so many great things. You are beautiful, and I love you so much for your strength and courage. I wish I could hug you and tell you how amazing you are. Believe it! Believe in yourself. And please stop being so hard on yourself. Take it all one day at a time.
Take care of your health both physically and mentally. Surround yourself with people that help you grow and make you better. You don’t have to have it all figured out. You don’t have to have a plan for everything. Be free and let life flow. Be grateful for all that comes your way good or bad, it all comes for a reason.”
You don’t have to have a plan for everything. Be free and let life flow. Be grateful for all that comes your way good or bad, it all comes for a reason.”
Daisy is a shining example of an everyday hero: a mental health advocate. She speaks for others who do not have a voice.
How can I become an advocate?
You do not have to share your deepest darkest secrets on social media to become an advocate. You can stand up for others by sharing your story privately with a friend, neighbor or loved one. You also don’t have to share your story if you’re not yet ready. You can also:
- Support someone who needs help
- Volunteer for a local mental health organization
- Attend an awareness walk or other event benefitting the mental health movement
- Encourage your local politicians to prioritize mental health
- Correct those who use stigmatizing language
Together, we can change how the world views mental health. We can continue the mental health movement by speaking out, sharing our stories and showing others that they are not alone. Our societal perception of mental health, including mental illness, will not change if we do not take action to change it ourselves.
Our societal perception of mental health, including mental illness, will not change if we do not take action to change it ourselves.
Kristen Fuller M.D. is a family medicine physician with a passion for mental health. She spends her days writing content for a well-known mental health and eating disorder treatment facility, treating patients in the Emergency Room and managing an outdoor women's blog. To read more of Dr. Fuller's work visit her Psychology Today blog and her outdoor blog, GoldenStateofMinds.
We’re always accepting submissions to the NAMI Blog! We feature the latest research, stories of recovery, ways to end stigma and strategies for living well with mental illness. Most importantly: We feature your voices.
Check out our Submission Guidelines for more information.
LEARN MORE
Protection & Advocacy for Individuals with Mental Illness (PAIMI) Program
The PAIMI grant program is intended to protect and advocate for the rights of adults with Significant (Serious) Mental Illness (SMI) and children with Significant (Serious) Impairment or Emotional Disturbances (SED) through activities to ensure the enforcement of the Constitution, and Federal and State statutes.
The PAIMI grants are authorized under the PAIMI Act of 1986 [42 U.S.C. 10801(b)(1), et seq., as amended in 2000].
PAIMI Program resources are to serve eligible individuals who meet the definitions of mental illness as defined by the authorizing legislation [42 U.S.C. 10802(4)(A)&(B) and 10804(d)].
Purpose of the PAIMI Program
- Provide legal-based advocacy services
- Protect and advocate for the rights of individuals with SMI for adults and SED for children
- Investigate abuse, neglect, and rights violations
PAIMI Program Grantees
57 state Protection and Advocacy (P&A) systems:
- 50 States
- District of Columbia
- 5 Territories (American Samoa, Guam, Northern Marianas, Puerto Rico, and Virgin Islands)
- American Indian Consortium for Native Americans
The 57 state P&A systems are comprised of 52 Governor-designated non-profit organizations and 5 state-operated agencies (Alabama, American Samoa, Kentucky, North Dakota, and Puerto Rico).
PAIMI Program Performance Reports (PPR)
Each PAIMI grantee is required to transmit an annual report that describes its program activities, accomplishments, and expenditures during the most recently completed FY by January 1.
All PAIMI approved annual grant applications are compared to the PPR submitted for the same fiscal year. Per the PAIMI Act [42 U.S.C. 10824], SAMHSA summarizes state P&A activities and accomplishments as mandated under the PAIMI Act, as amended in 2000, 42 U.S.C. 10801 et. seq. at 10805(a)(7).
PAIMI Program Biennial Reports
Section 105 of The Developmental Disabilities Assistance and Bill of Rights Act of 1975 (DD Act) requires the submission of a report at least once every two years to the President, the Congress, and the National Council on Disability describing the goals and outcomes of the programs carried out under the DD Act.
The PAIMI Biennial report is included in the Appendix to the Secretary’s biennial report on federal disability activities, which is prepared by the Administration for Community Living and sent to the President, Congress, and National Council on Disability in accordance with the DD Act of 2000 [42 U. S.C. 15005] and the PAIMI Act of 2000 [42 U.S.C. 10824]).
S.C. 15005] and the PAIMI Act of 2000 [42 U.S.C. 10824]).
Links to the approved PAIMI Program Biennial Reports:
- FY 2019-2020 (PAIMI Activities Only) (PDF | 2.7 MB)
- FY 2017-2018 (PAIMI Activities Only) (PDF | 2 MB)
- FY 2015-2016 (PDF | 1.8 MB)
- FY 2013-2014 (See Appendix pages 49-138) (PDF | 2.2 MB)
Article 5. Rights of persons suffering from mental disorders \ ConsultantPlus
Article 5. Rights of persons suffering from mental disorders
(1) Persons suffering from mental disorders have all the rights and freedoms of citizens provided for by the Constitution of the Russian Federation and federal laws. Restriction of the rights and freedoms of citizens associated with a mental disorder is permissible only in cases provided for by the laws of the Russian Federation.
(as amended by Federal Law No. 122-FZ of August 22, 2004)
(see the text in the previous edition)
(2) All persons suffering from mental disorders, in the provision of psychiatric care, are entitled to:
respectful and humane treatment, excluding humiliation of human dignity;
receive information about their rights, as well as in a form accessible to them and taking into account their mental state, information about the nature of their mental disorders and the methods of treatment used;
psychiatric care in the least restrictive conditions, if possible at the place of residence;
stay in a medical organization providing psychiatric care in inpatient settings, only for the period necessary to provide psychiatric care in such conditions;
(as amended by Federal Law No. 317-FZ of November 25, 2013)
317-FZ of November 25, 2013)
(see the text in the previous edition)
all types of treatment (including spa treatment) for medical reasons;
providing psychiatric care in conditions that meet sanitary and hygienic requirements;
prior consent and refusal at any stage to use as an object of testing methods of prevention, diagnosis, treatment and medical rehabilitation, medicinal products for medical use, specialized medical foods and medical devices, scientific research or education, from photo, video, or filming;
(as amended by Federal Laws No. 185-FZ of 02.07.2013, No. 317-FZ of 25.11.2013)
(see the text in the previous version)
invitation, at their request, of any specialist involved in the provision of psychiatric care, with the consent of the latter, to work in a medical commission on matters regulated by this Law;
assistance of a lawyer, legal representative or other person in the manner prescribed by law.
(3) Restriction of the rights and freedoms of persons suffering from mental disorders only on the basis of a psychiatric diagnosis, facts of being under dispensary observation or stay in a medical organization providing psychiatric care in inpatient conditions, as well as in an inpatient social service organization intended for persons those suffering from mental disorders are not allowed. Officials guilty of such violations are liable in accordance with the legislation of the Russian Federation and the constituent entities of the Russian Federation.
Officials guilty of such violations are liable in accordance with the legislation of the Russian Federation and the constituent entities of the Russian Federation.
(as amended by Federal Laws No. 122-FZ of 22.08.2004, No. 185-FZ of 02.07.2013, No. 317-FZ of 25.11.2013, No. 358-FZ of 28.11.2015)
(see text) in the previous edition)
Information for families with mentally ill people
We, psychiatrists, often ask relatives of people with "our" diseases what they most often lack in their situation. Often I hear answers: “Information”, “Understanding”.
The family has always existed in the social environment that every person needs, whether he is healthy or ill (even with a mental disorder). At the same time, he often falls out of it. And every individual (healthy or sick) in this environment has rights and obligations. The sick person has a special claim to help and a precautionary attitude, like other members of his family, who also have the same, but they cannot be left unattended for a long time, unless he (the sick person) does not want to risk the breakdown of family ties. In such a special situation, help from outside is required, and then we will talk about overcoming crises, about treatment, about rehabilitation, about the social security of the patient, or about the financial and moral hardships of relatives.
In such a special situation, help from outside is required, and then we will talk about overcoming crises, about treatment, about rehabilitation, about the social security of the patient, or about the financial and moral hardships of relatives.
The common notion that "a person, once mentally ill, remains ill forever" is erroneous. It often happens that the disease disappears again, or at least it can be successfully overcome.
It is also encouraging that in recent decades significant progress has been made in the research and treatment of mental illness, thanks to the emergence of new drugs.
Erroneous sentences include the idea that patients with mental (mental) disorders should be equated with "mentally retarded persons" and during fascism they were exterminated by the thousands. This is also completely false. As one look at the many mentally ill and yet talented people who have made outstanding contributions to art and achieved success in other fields shows: Fyodor Dostoevsky, Hans Christian Andersen, Franz Schubert, Alfred Schnittke, Salvador Dali, Leonardo da Vinci, Nicolo Paganini, Johann Sebastian Bach, Sigmund Freud, Rudolf Diesel, Johann Wolfgang Goethe, Claude Henri Saint-Simon, Immanuel Kant, Charles Dickens, Albrecht Dürer, Sergei Rachmaninoff, Wolfgang Amadeus Mozart, Lope de Vega, Nostradamus, Jean Baptiste Molière, Francisco Goya, Honore de Balzac, Friedrich Nietzsche and others
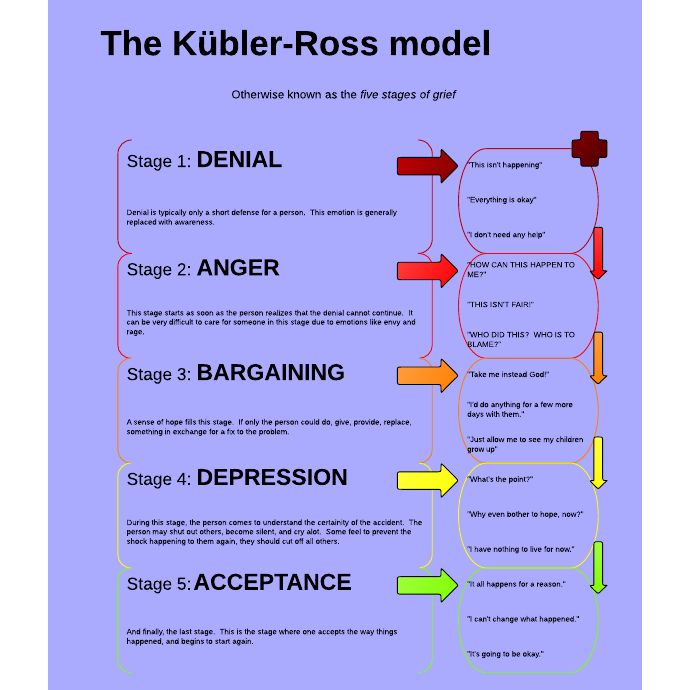
Today, the concept of "mentally ill" is no longer used, but it is said about "mental illness" and "mentally ill" in order to clarify the change of views, knowledge. Despite the existing, fortunately, positive processes, a relatively high percentage of patients suffer from relapses or remain impaired for a long time. This means that the lives of families where there are such people proceed differently than expected, and plans and desires remain in the background, and all participants must go through painful processes of adaptation, learning, until eventually, perhaps, balance is restored.
Despite the existing, fortunately, positive processes, a relatively high percentage of patients suffer from relapses or remain impaired for a long time. This means that the lives of families where there are such people proceed differently than expected, and plans and desires remain in the background, and all participants must go through painful processes of adaptation, learning, until eventually, perhaps, balance is restored.
This is based on the experience of families with such relatives. Well, if you are a relative only recently and have come into conflict with a mental illness, then you will probably find these descriptions depressing. However, perhaps in this you will gain your own experience, and your suffering will be justified.
We, the specialists, would like to give information and evoke understanding without delusion, and point out the possibilities for assistance that you can seek without hiding problems - sometimes out of shame, more often out of good will, in order to somehow spare the patient or cause greater understanding from the outside world. The flip side of this behavior is that problems and ailments are underestimated and not taken seriously - "it's just the psyche ...", as many say and at the same time believe: this is not so bad and if you pull yourself together, everything will work out . The consequences of such views can be completely unforeseen and are the basis for insufficient assistance, which families usually complain about.
The flip side of this behavior is that problems and ailments are underestimated and not taken seriously - "it's just the psyche ...", as many say and at the same time believe: this is not so bad and if you pull yourself together, everything will work out . The consequences of such views can be completely unforeseen and are the basis for insufficient assistance, which families usually complain about.
It is appropriate to talk about the conflicting feelings of relatives towards the mentally ill. On the one hand, they treat him with understanding and want to protect him, and on the other hand, irritation and dissatisfaction may appear if, as a result of the patient’s behavior, all family life goes haphazardly, although it is known that one must always restrain oneself in illness. Some relatives take the side of the patient and oppose the "rest of the world", others act quite the opposite: they get so upset and nervous that they contribute to the isolation of the sick person, while others hesitate between understanding and sympathy, on the one hand, and refusal, and anger , on the other side.
Patients themselves, doctors, support staff participate in this game, and the "stumbling block" adjoins either one or the other. Everything in this complex and constantly changing situation is understandable, but this certainly does not make it easier for a solution that is acceptable to all participants.
The motto of the German Relatives Association brings this goal together in the thesis: "In order to live together with the mentally ill, it is necessary to be self-confident and in solidarity." However, there is an experience acquired by many relatives before you: “Your most important assistant is yourself!”. Therefore, it is so important that you take care not only of the patient, but also of yourself.
The first step in self-help is gathering information. The one who receives more information about the disease can better manage it and overcome its consequences. Relatives can turn to doctors, read specialized literature, etc. However, when it comes to the numerous and dubious issues that arise in daily communication with the mentally ill, the "expert assessment" of other relatives is an indispensable source of help and Information.
All of the above can be summarized in ten basic rules, such a "game" is worth the candle. Thanks to her, we can all avoid stress and conflict in the family and ensure peace in our relationships with each other.
So, 10 basic rules to avoid stress and conflict in the family and ensure peace in relationships with each other:
1. Try to limit yourself to the most important things and at first close your eyes to some behavioral problems.
2. Leave the patient alone - excessive care will not benefit him or us. Do not protect him or take care of him beyond measure and give him as much independence as possible. However, it is important to let him know that you are at his disposal at any moment when he needs you.
3. Give yourself and the patient time, especially after the acute phase of the disease. Don't wait impatiently for a "quick leap forward" but promote small steps and enjoy them.
4. Match your expectations and aspirations to the situation, avoid overstimulation and do not make excessive demands.
5. If you want to do something (for example, tidy up your room), first think about how to act more delicately and wait for the most favorable moment. Express your thoughts clearly and concisely. If you act with irritation or direct pressure, then the chances of achieving the intended goal decrease, and we create additional stress for ourselves.
6. Consider that the symptoms of illness are not an expression of ill will, but an attempt to cope with a disturbed lifestyle.
7. Reflect on the fact that the sick person himself is trying to protect the still healthy parts of his body from the disease and help him strengthen and develop them.
8. Take care of a quiet way of life - even if it is sometimes difficult. Work hard to minimize conflicts and strained relationships in the family. Ask yourself if a walk in the fresh air will help you get out of a difficult situation or if you need to give free rein to your own feelings.
9. Take a well-thought-out attitude towards medicines.