Always tired and depressed
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery.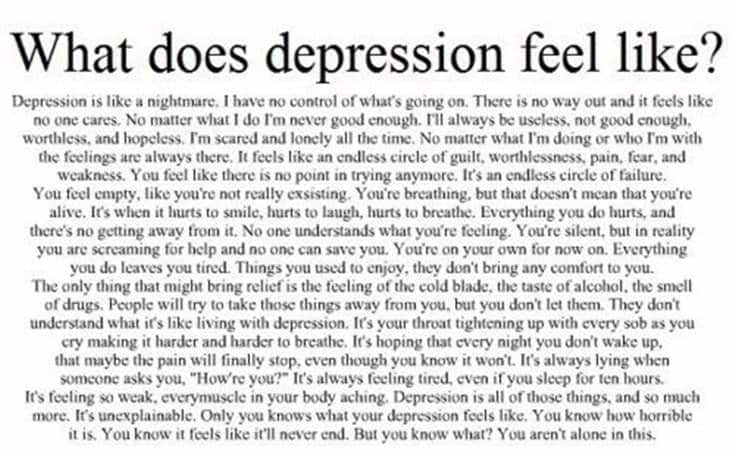 Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. SAMHSA’s 2020 National Survey on Drug Use and Health reports that approximately 19.3 million people aged 18 or older had a substance use disorder in the past year.
Alcohol
Data:
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.
 6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH) - The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
- The 2019 National Survey on Drug Use and Health reports that 139.7 million Americans age 12 or older were past month alcohol users, 65.8 million people were binge drinkers in the past month, and 16 million were heavy drinkers in the past month
- About 2.3 million adolescents aged 12 to 17 in 2019 drank alcohol in the past month, and 1.2 million of these adolescents binge drank in that period (2019 NSDUH)
- Approximately 14.5 million people age 12 or older had an alcohol use disorder (2019 NSDUH)
- Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired.
 The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk. They Hear You.
- Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.7% of people aged 12 or older (or 57.
 3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH) - Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Data from the 2019 NSDUH reports that 58.1 million people were current (i.e., past month) tobacco users. Specifically, 45.9 million people aged 12 or older in 2019 were past month cigarette smokers (2019 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses. The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
- The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey.
 Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018 - E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year.
 Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH) - An estimated 745,000 people had used heroin in the past year, based on 2019 NSDUH data
- In 2019, there were 10.1 million people age 12 or older who misused opioids in the past year. The vast majority of people misused prescription pain relievers (2019 NSDUH)
- An estimated 1.6 million people aged 12 or older had an opioid use disorder based on 2019 NSDUH data
- Opioid use, specifically injection drug use, is a risk factor for contracting HIV, Hepatitis B, and Hepatitis C. The CDC reports that people who inject drugs accounted for 9 percent of HIV diagnoses in the United States in 2016
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.
 5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH) - 2019 NSDUH data indicates that 48.2 million Americans aged 12 or older, 17.5 percent of the population, used marijuana in the past year
- Approximately 4.8 million people aged 12 or older in 2019 had a marijuana use disorder in the past year (2019 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 04/27/2022
Personal experience: a psychologist from St. Petersburg on how to cope with the constant feeling of fatigue and depression
Health
With dysthymia, you almost always feel tired and quite depressed. These symptoms are not so pronounced as to speak of depression, but they can seriously increase during exacerbations. Cognitive-behavioral psychologist of the Quality of Life Center Victoria Tsebrenko spoke about her personal experience of living with a condition similar to dysthymia and ways to help herself.
How dysthymia manifests itself and its exacerbations
According to the latest estimates, 3.3% of the population suffers from dysthymia. This disorder is officially included in the ICD-10 (International Classification of Diseases 10th Revision), it can be found in the section "persistent mood disorders". Even if you have not been diagnosed with this by a doctor, but you often feel depressed and tired, it is important to know how to prevent your condition from worsening. For example, I do not have an official diagnosis of dysthymia, but its manifestations are as close as possible to what I feel.
In a person with dysthymia, a feeling of depression and fatigue in a blurred form is almost always present, and at some moments it becomes more noticeable. This is a fairly constant condition, the symptoms of which may overlap with those of depressive episodes. Their severity is not so strong as to speak of depression. But noticeable enough to impair the quality of life. Due to the blurring of symptoms, a person may consider dysthymia as part of his personality, character, or feature of the rhythm of life. And when, against such a background, even greater declines in activity and mood occur (periods of exacerbations), a person simply cannot understand that something is wrong with him. Although at these moments he needs to take care of himself, seek help.
Due to the blurring of symptoms, a person may consider dysthymia as part of his personality, character, or feature of the rhythm of life. And when, against such a background, even greater declines in activity and mood occur (periods of exacerbations), a person simply cannot understand that something is wrong with him. Although at these moments he needs to take care of himself, seek help.
How does this smooth transition from a conditionally normal, background state of depression to a more severe one take place? In the background, you almost always feel sleepy, especially if you slept less than 7 hours. There is little interest and motivation in even the most beloved things, but there are flashes of high interest. Ordinary situations can trigger painful thoughts, such as: "I'm not doing well, I'm doing everything wrong." However, in a conditionally normal state, these thoughts are easier to track and stop so as not to plunge into a dangerous, depressogenic thought pattern.
It happens that a person is a little sad for most of his life, with “beaten” emotions. Against this background, even greater declines in strength and self-confidence occur.
Against this background, even greater declines in strength and self-confidence occur.
During episodes of dysthymia, you begin to experience physical fatigue and exhaustion, regardless of the amount of rest and sleep. You can lie in bed all day and watch a series that makes you sick. Much more situations cause a painful assessment of yourself and your actions: if you experienced hopelessness, felt weak and stupid in a normal state, then during the period of exacerbation this seriously intensifies, it is much harder to suppress such thoughts. You often experience irritation, it is difficult for you to empathize with other people, even those closest to you.
When you feel tired and overwhelmed, this inevitably leads to a deterioration in the quality of your work. You negatively evaluate yourself and your work, trying to solve the problem with the help of processing. Symptoms in the form of fatigue and depression add up in a vicious cycle, support each other and reinforce. This cycle looks like this: “Tired and depressed - Fewer tasks done - I don't work well. I'm not doing well. I should do better. - Start working harder. “Fatigue and depression.”
This cycle looks like this: “Tired and depressed - Fewer tasks done - I don't work well. I'm not doing well. I should do better. - Start working harder. “Fatigue and depression.”
The workhorse mode, as a rule, is turned on in relation to areas that require you to be as hyper-responsible as possible. You turn a blind eye to everything else - it is dangerous that, first of all, what brings you real pleasure, gives you a feeling of a full life. Communication with loved ones, hobbies, playing sports - all this you sacrifice, trying to make time for "really important things." Because of fatigue and depression, it begins to seem that you basically don’t like anything. Here is another closed loop. "Fatigue and depression - Leave only the most necessary, reduce pleasant activities - Mood and strength decrease - Negative forecasts increase "I will not like this, I will get even more tired" - Fatigue and depression. In order to help yourself cope with dysthymia, it is important to break the vicious circles: on the one hand, do not overload yourself with tasks, on the other hand, do not refuse entertainment, communication and a pleasant stay. Do not trust too much the feeling of tiredness and sadness: return to life activity and pleasant rest, even if there is less joy from them now.
Do not trust too much the feeling of tiredness and sadness: return to life activity and pleasant rest, even if there is less joy from them now.
People during depression and exacerbation of dysthymia often turn on mental chewing gum, which consists in painful, unproductive thinking. Often a person is too fixated on his well-being, on feelings of fatigue and sadness. This adds even more suffering, leads to the fact that you merge even more into a state of depression. It is important to train attention switching. Yes, you should pay attention to the symptoms of dysthymia, but don't get too stuck in them. Remember that episodes of aggravation end and even with limited strength, we can still do a lot.
So, here's how to notice the worsening of dysthymia in order to help yourself in time: Follow our news on Telegram Author: Katerina Reznikova, NewsHealth  Spend more hours in bed.
Spend more hours in bed. What to do
 Mindfulness techniques can help you with this. Don't trust fatigue and bad thoughts too much: you may actually be able to do less and worse right now, but still quite a lot.
Mindfulness techniques can help you with this. Don't trust fatigue and bad thoughts too much: you may actually be able to do less and worse right now, but still quite a lot. Top 11 reasons why you wake up tired and exhausted every day
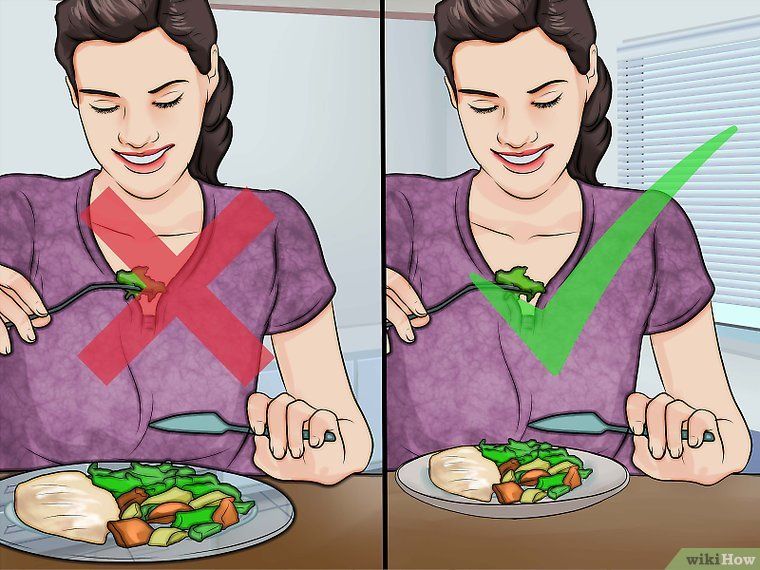
 Waking up early in the morning is hard, especially if you went to bed late, ate too much dinner, or were nervous the day before. But a contrast shower, exercise, a delicious breakfast, a walk with the dog can help cheer up and cheer you up. Yes, getting out of a warm bed is not the easiest task, but pleasant morning rituals really help to feel better.
Waking up early in the morning is hard, especially if you went to bed late, ate too much dinner, or were nervous the day before. But a contrast shower, exercise, a delicious breakfast, a walk with the dog can help cheer up and cheer you up. Yes, getting out of a warm bed is not the easiest task, but pleasant morning rituals really help to feel better.
It's another matter when every morning is a real test for you. You wake up already tired, broken, with a heavy head and complete unwillingness to do anything. Neither your favorite coffee with a delicious breakfast, nor conversations with your family can cheer you up. I want to go back to bed and fall asleep sooner, so as not to live today. Such a condition may indicate disorders and even diseases, says psychotherapist Ekaterina Misevich. For example, people often suffer from asthenia without even realizing it.
Psychotherapist, narcologist
“Asthenia is a state of decline in physical and mental strength with minimal exertion.![]() The feeling of being overwhelmed does not go away after sleeping at night or resting during the day. It is characterized by a subjective feeling of a decrease in the level of vital energy by 30–50 percent. Asthenia can be a sign of an imbalance between work and rest, an adaptation disorder, an organic brain lesion, the doctor told Evening Moscow.
The feeling of being overwhelmed does not go away after sleeping at night or resting during the day. It is characterized by a subjective feeling of a decrease in the level of vital energy by 30–50 percent. Asthenia can be a sign of an imbalance between work and rest, an adaptation disorder, an organic brain lesion, the doctor told Evening Moscow.
The second cause of this condition is depression. This is a serious illness that cannot be dealt with on your own, you need the help of a psychotherapist. Usually people who suffer from depression wake up without an alarm at 3-5 in the morning and cannot fall asleep. They have a depressed mood, especially in the first half of the day, and morning for them is the worst time of the day. A person also constantly feels guilty about all the troubles, he has no motivation to work and do what he loves.
Another cause of morning sickness is an anxiety disorder. It most often develops when one stressful situation is immediately followed by another. The brain gives a signal: “it’s dangerous around”, the autonomic nervous system goes into a mode of increased excitability. Every organ from the top of the head to the tips of the fingers is preparing to activate the person's ability to escape or defend himself. A person cannot relax in any way, he does not sleep well, he may be tormented by nightmares, and in the morning he feels as if he had not slept all night, but was doing hard physical work.
The brain gives a signal: “it’s dangerous around”, the autonomic nervous system goes into a mode of increased excitability. Every organ from the top of the head to the tips of the fingers is preparing to activate the person's ability to escape or defend himself. A person cannot relax in any way, he does not sleep well, he may be tormented by nightmares, and in the morning he feels as if he had not slept all night, but was doing hard physical work.
If you begin to notice that every morning you are looking for an excuse to just get out of bed and start doing things, you are constantly in a bad mood, attacks of aggression, or, conversely, complete indifference to everything, then be sure to make an appointment with a psychotherapist. The specialist will determine the cause and, if necessary, sign you up for therapy.
Pathologies that have nothing to do with your mental health may be to blame for the fact that you wake up hard and feel tired. So, for example, you can develop iron deficiency anemia.