Therapy for depersonalization
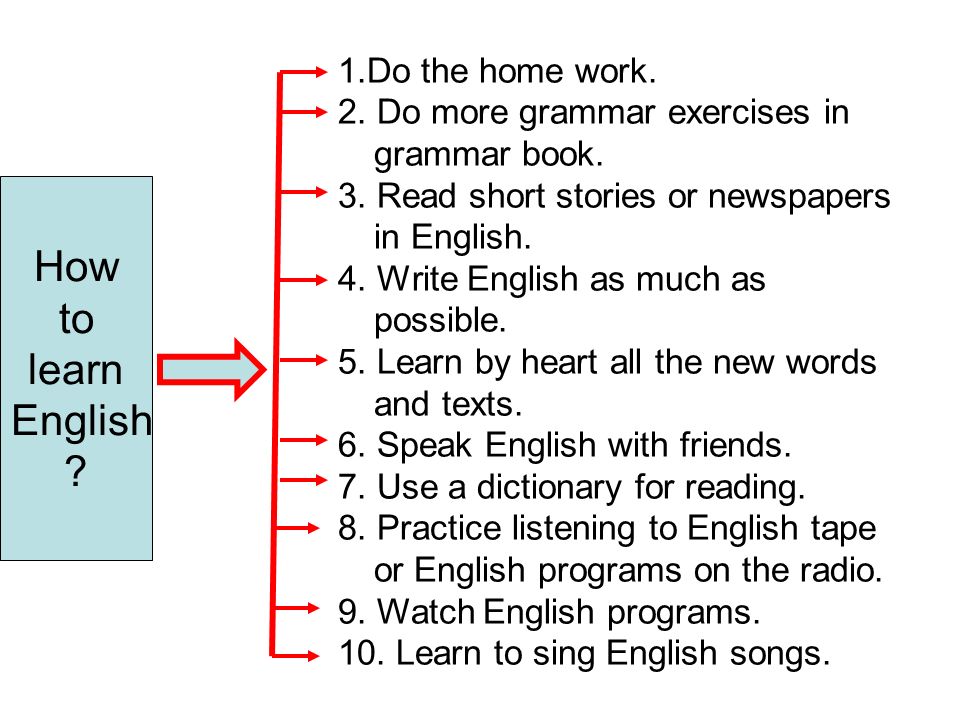
How to Stop Depersonalization: 10 Methods
Do you frequently feel detached from reality, like you’re watching yourself in a movie? If so, you may want to know how to feel some relief from depersonalization.
Depersonalization can be a frightening or confusing experience. The good news is, learning what causes depersonalization, as well as using a few self-care tools, can help make it more manageable.
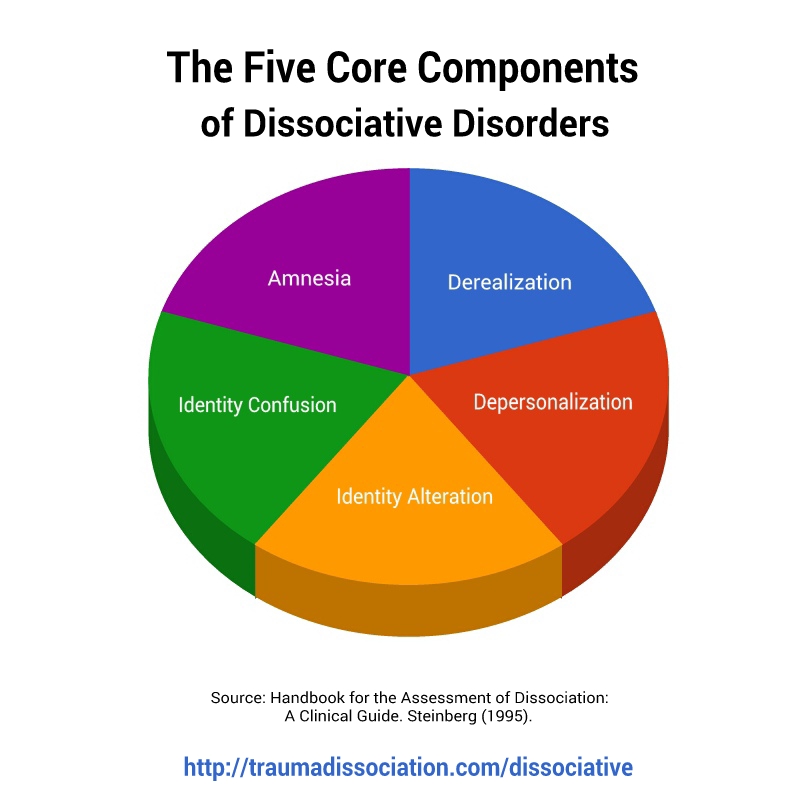
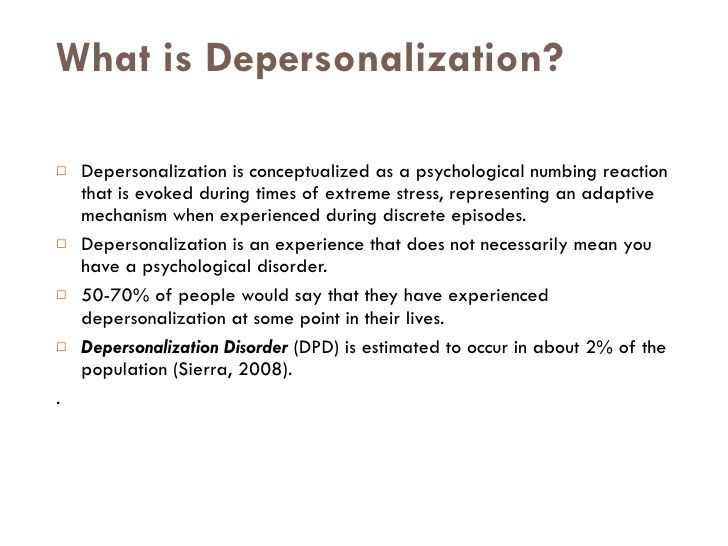
Depersonalization is a complex topic, and researchers still don’t know a lot about it. What they do know is that it’s a type of dissociation, often caused by traumatic or stressful events like a panic attack, an accident, abuse, or assault. Sometimes, depersonalization is caused by a negative experience with cannabis or other substances.
Additional symptoms of depersonalization can include memory loss and out-of-body experiences. In addition, anxiety or depression can often occur alongside depersonalization, which can make your experience more intense.
If you’ve experienced any of these symptoms, you’re not alone. Various types of support may help ease your distress around depersonalization — from self-care and online groups, to therapy and education. With that in mind, here are several resources that you may find helpful.
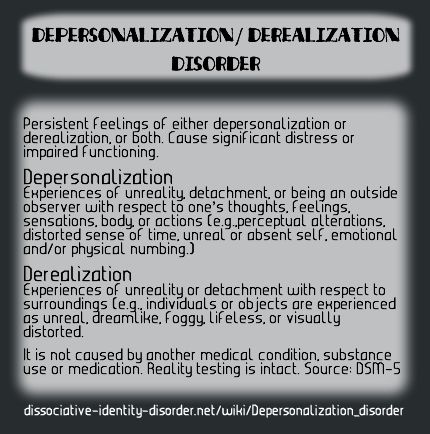
About 75% of people experience feelings of depersonalization at some point in their lives. For 2% of the population, the symptoms become more frequent. This can result in a diagnosis of depersonalization/derealization disorder (DPDR).
Dissociation can also occur with post-traumatic stress disorder (PTSD) and borderline personality disorder (BPD), so you may not necessarily be diagnosed with DPDR separately.
Many theorists believe that dissociation is your body’s way of protecting you from extreme trauma or stress. Others assert that it’s less of a protective function and more like a scar from the traumatic event (or set of events) itself.
While depersonalization symptoms can interfere with your quality of life, managing the distress caused by them is possible. It’s important to work with a mental health professional who’s able to support you with the best treatment plan for your symptoms.
It’s important to work with a mental health professional who’s able to support you with the best treatment plan for your symptoms.
Many tools can help you manage feelings of anxiety, depression, or distress about living with depersonalization. Treatments for PTSD and BPD may also have a beneficial effect on depersonalization symptoms.
First things first: When symptoms arise, try to remind yourself that you’re OK and that you’re safe. Naming your feelings, practicing deep breathing, or listening to music can also help you feel calmer. In addition, challenging your intrusive thoughts and reaching out to close friends may help you feel grounded.
1. Acknowledge your feelings
According to many psychology researchers, depersonalization may be an adaptive way to cope with stress. Some believe that it’s your brain’s way of protecting you from danger. When your body and mind distance you from intense emotional pain, overwhelming feelings may decrease, which may help you feel safe at that moment.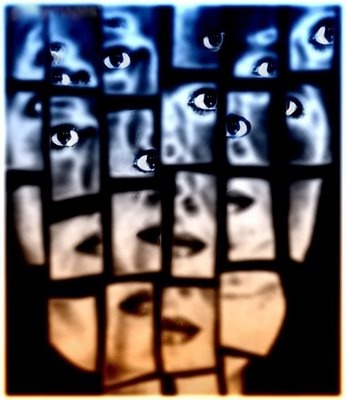
If your body and mind ignore your feelings for too long, symptoms of depersonalization may drag on. In these cases, your brain misreads danger, and feelings of depersonalization increase.
When this happens, you might try to name your feelings. Some research suggests that by acknowledging certain emotions (in this case, fatigue), you can lessen stress. It’s possible that this concept may work on other painful emotions as well. In turn, this may decrease symptoms of derealization, though more research is obviously needed.
Self-compassion exercises may help you accept whatever feelings arise at that moment.
2. Take deep breaths
When stress arises, your body’s nervous system fires up. For people living with depersonalization disorder, this can disrupt brain functioning and lead to feelings of depersonalization.
Breathing exercises, like taking deep belly breaths, may help against this stress.
If you want some guidance from a meditation teacher, consider downloading a mindfulness app or look for a free guided meditation on YouTube or TikTok. If deep breathing is helpful, you might consider practicing your exercises for a few minutes each day. Like exercise, deep breathing can become easier with practice.
If deep breathing is helpful, you might consider practicing your exercises for a few minutes each day. Like exercise, deep breathing can become easier with practice.
3. Listen to music
Feelings of derealization can be more intense when your brain focuses on them. A grounding technique, like listening to music, may help you feel less anxious about the experience.
Research shows that music can help reduce cortisol levels, a stress hormone, in your system.
You might consider making a playlist of your favorite songs and keep the playlist on your phone. When symptoms arise, even if you’re at work or waiting for the bus, you can pop in your earbuds, press play, and let the music soothe you.
4. Read a book
If you enjoy reading, it may help with depression and the anxious thoughts that often occur alongside depersonalization. Try picking up an old favorite book, or a story that brings you comfort. You might find that you’re able to concentrate on the words and their meanings enough to quiet intrusive thoughts.
5. Challenge your intrusive thoughts
For some, depersonalization involves a lack of intrusive thoughts. For others who live with depersonalization as well as anxiety or PTSD, intrusive thoughts can pose a real challenge.
Cognitive psychologists point out that a tool called psychological distancing can help quiet intrusive thoughts. Psychological distancing means finding some space between the upsetting thoughts and painful emotions.
Taking a few deep breaths can help quiet intrusive thoughts. As odd as it might sound, talking to yourself out loud can also help. You might ask yourself, “What evidence do I have that my worry is real?”
Basically, when your mind focuses on something else, intrusive thoughts often go away.
6. Call a friend
When you’re anxious and symptoms of depersonalization arise, you might be tempted to isolate. But at times like these, talking to a trusted friend or family member can really help.
Opening up can make you feel vulnerable. But talking gives you a chance to receive empathy from someone who cares about you. If you’re not sure who to lean on, try to identify two or three loved ones that you can text or keep on speed dial, no matter what.
But talking gives you a chance to receive empathy from someone who cares about you. If you’re not sure who to lean on, try to identify two or three loved ones that you can text or keep on speed dial, no matter what.
Self-care tools can help relieve symptoms of depersonalization. In addition, psychotherapy, education, nutrition, and exercise can help you maintain a sense of well-being in the long run.
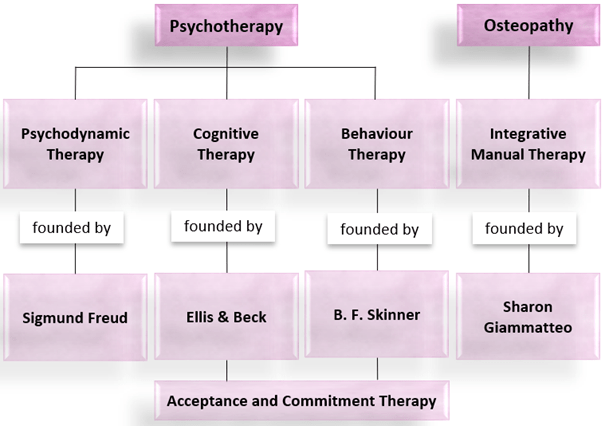
7. Talk therapy
If your symptoms of depersonalization are caused by a stressful or traumatic experience, talking with a therapist may really help.
Several types of therapy can work. Cognitive-behavioral therapy (CBT) can teach you to challenge intrusive thoughts and manage symptoms of depersonalization. Trauma-focused therapy like eye-movement desensitization and reprocessing therapy (EMDR) can help you process traumatic memories.
Once your trauma heals, symptoms of depersonalization may lessen.
8. Education
Learning more about the symptoms and causes of depersonalization disorder can also help. The National Alliance on Mental Illness (NAMI) has resources and information. Finding out how depersonalization affects your brain can make symptoms less frightening. In addition, reading about other people’s experiences is one way to feel less alone.
The National Alliance on Mental Illness (NAMI) has resources and information. Finding out how depersonalization affects your brain can make symptoms less frightening. In addition, reading about other people’s experiences is one way to feel less alone.
9. Sleep
Going to bed when your body feels tired can help you manage stress and decrease anxiety. The Centers for Disease Control and Prevention (CDC) recommends going to bed and waking up at the same time each day.
If you’d like to improve your sleep, you might also consider banning your phone and other electronics from your bedroom. If possible, try to keep your sleep space as dark as you can. Darkness helps regulate the body’s circadian rhythms, which can improve the quality of your sleep.
10. Exercise
Like getting enough rest, exercise can also help you manage stress. One study found that aerobic exercise can help decrease burnout, and one symptom of burnout is depersonalization.
If you’re interested in exercise but aren’t sure what to choose, walking could be a good option. Walking can help lower your body’s cortisol, which can help decrease stress.
Walking can help lower your body’s cortisol, which can help decrease stress.
If you’re living with depersonalization disorder, finding the right type of support can be an essential part of self-care.
If you’d like to find a mental health professional, the American Psychiatric Association (APA) has a searchable database that can help you find a therapist. If you’re looking for a local support group, you might contact your local National Alliance on Mental Health (NAMI) chapter.
If you’d like to read about other people’s experiences with depersonalization, you can check out the NAMI blog post, “The Scariest Panic Symptoms People Don’t Talk About,” which is one person’s story about living with depersonalization disorder. You can find other blog posts here and here.
If you’re interested in checking out some mental health podcasts, The Anxiety Podcast seeks to support anyone struggling with anxiety, stress, and panic attacks. The Spin Cycle is another mental health podcast that features interviews with mental health professionals.
Maybe you’re ready to check out meditation, but you aren’t sure where to start. Meditation Minis is a podcast that includes several types of guided meditations. And if you’re on Clubhouse, meditation teacher Lisa Abramson leads mindfulness classes every day.
Finally, know that taking care of your mental health takes courage! Sure, it can feel frustrating at times, and that’s OK. No one expects you to be perfect. With more mental health resources and tools available, living with depersonalization disorder is much easier.
How to Stop Depersonalization: 10 Methods
Do you frequently feel detached from reality, like you’re watching yourself in a movie? If so, you may want to know how to feel some relief from depersonalization.
Depersonalization can be a frightening or confusing experience. The good news is, learning what causes depersonalization, as well as using a few self-care tools, can help make it more manageable.
Depersonalization is a complex topic, and researchers still don’t know a lot about it. What they do know is that it’s a type of dissociation, often caused by traumatic or stressful events like a panic attack, an accident, abuse, or assault. Sometimes, depersonalization is caused by a negative experience with cannabis or other substances.
What they do know is that it’s a type of dissociation, often caused by traumatic or stressful events like a panic attack, an accident, abuse, or assault. Sometimes, depersonalization is caused by a negative experience with cannabis or other substances.
Additional symptoms of depersonalization can include memory loss and out-of-body experiences. In addition, anxiety or depression can often occur alongside depersonalization, which can make your experience more intense.
If you’ve experienced any of these symptoms, you’re not alone. Various types of support may help ease your distress around depersonalization — from self-care and online groups, to therapy and education. With that in mind, here are several resources that you may find helpful.
About 75% of people experience feelings of depersonalization at some point in their lives. For 2% of the population, the symptoms become more frequent. This can result in a diagnosis of depersonalization/derealization disorder (DPDR).
Dissociation can also occur with post-traumatic stress disorder (PTSD) and borderline personality disorder (BPD), so you may not necessarily be diagnosed with DPDR separately.
Many theorists believe that dissociation is your body’s way of protecting you from extreme trauma or stress. Others assert that it’s less of a protective function and more like a scar from the traumatic event (or set of events) itself.
While depersonalization symptoms can interfere with your quality of life, managing the distress caused by them is possible. It’s important to work with a mental health professional who’s able to support you with the best treatment plan for your symptoms.
Many tools can help you manage feelings of anxiety, depression, or distress about living with depersonalization. Treatments for PTSD and BPD may also have a beneficial effect on depersonalization symptoms.
First things first: When symptoms arise, try to remind yourself that you’re OK and that you’re safe. Naming your feelings, practicing deep breathing, or listening to music can also help you feel calmer. In addition, challenging your intrusive thoughts and reaching out to close friends may help you feel grounded.
Naming your feelings, practicing deep breathing, or listening to music can also help you feel calmer. In addition, challenging your intrusive thoughts and reaching out to close friends may help you feel grounded.
1. Acknowledge your feelings
According to many psychology researchers, depersonalization may be an adaptive way to cope with stress. Some believe that it’s your brain’s way of protecting you from danger. When your body and mind distance you from intense emotional pain, overwhelming feelings may decrease, which may help you feel safe at that moment.
If your body and mind ignore your feelings for too long, symptoms of depersonalization may drag on. In these cases, your brain misreads danger, and feelings of depersonalization increase.
When this happens, you might try to name your feelings. Some research suggests that by acknowledging certain emotions (in this case, fatigue), you can lessen stress. It’s possible that this concept may work on other painful emotions as well. In turn, this may decrease symptoms of derealization, though more research is obviously needed.
In turn, this may decrease symptoms of derealization, though more research is obviously needed.
Self-compassion exercises may help you accept whatever feelings arise at that moment.
2. Take deep breaths
When stress arises, your body’s nervous system fires up. For people living with depersonalization disorder, this can disrupt brain functioning and lead to feelings of depersonalization.
Breathing exercises, like taking deep belly breaths, may help against this stress.
If you want some guidance from a meditation teacher, consider downloading a mindfulness app or look for a free guided meditation on YouTube or TikTok. If deep breathing is helpful, you might consider practicing your exercises for a few minutes each day. Like exercise, deep breathing can become easier with practice.
3. Listen to music
Feelings of derealization can be more intense when your brain focuses on them. A grounding technique, like listening to music, may help you feel less anxious about the experience.
Research shows that music can help reduce cortisol levels, a stress hormone, in your system.
You might consider making a playlist of your favorite songs and keep the playlist on your phone. When symptoms arise, even if you’re at work or waiting for the bus, you can pop in your earbuds, press play, and let the music soothe you.
4. Read a book
If you enjoy reading, it may help with depression and the anxious thoughts that often occur alongside depersonalization. Try picking up an old favorite book, or a story that brings you comfort. You might find that you’re able to concentrate on the words and their meanings enough to quiet intrusive thoughts.
5. Challenge your intrusive thoughts
For some, depersonalization involves a lack of intrusive thoughts. For others who live with depersonalization as well as anxiety or PTSD, intrusive thoughts can pose a real challenge.
Cognitive psychologists point out that a tool called psychological distancing can help quiet intrusive thoughts. Psychological distancing means finding some space between the upsetting thoughts and painful emotions.
Psychological distancing means finding some space between the upsetting thoughts and painful emotions.
Taking a few deep breaths can help quiet intrusive thoughts. As odd as it might sound, talking to yourself out loud can also help. You might ask yourself, “What evidence do I have that my worry is real?”
Basically, when your mind focuses on something else, intrusive thoughts often go away.
6. Call a friend
When you’re anxious and symptoms of depersonalization arise, you might be tempted to isolate. But at times like these, talking to a trusted friend or family member can really help.
Opening up can make you feel vulnerable. But talking gives you a chance to receive empathy from someone who cares about you. If you’re not sure who to lean on, try to identify two or three loved ones that you can text or keep on speed dial, no matter what.
Self-care tools can help relieve symptoms of depersonalization. In addition, psychotherapy, education, nutrition, and exercise can help you maintain a sense of well-being in the long run.
7. Talk therapy
If your symptoms of depersonalization are caused by a stressful or traumatic experience, talking with a therapist may really help.
Several types of therapy can work. Cognitive-behavioral therapy (CBT) can teach you to challenge intrusive thoughts and manage symptoms of depersonalization. Trauma-focused therapy like eye-movement desensitization and reprocessing therapy (EMDR) can help you process traumatic memories.
Once your trauma heals, symptoms of depersonalization may lessen.
8. Education
Learning more about the symptoms and causes of depersonalization disorder can also help. The National Alliance on Mental Illness (NAMI) has resources and information. Finding out how depersonalization affects your brain can make symptoms less frightening. In addition, reading about other people’s experiences is one way to feel less alone.
9. Sleep
Going to bed when your body feels tired can help you manage stress and decrease anxiety. The Centers for Disease Control and Prevention (CDC) recommends going to bed and waking up at the same time each day.
The Centers for Disease Control and Prevention (CDC) recommends going to bed and waking up at the same time each day.
If you’d like to improve your sleep, you might also consider banning your phone and other electronics from your bedroom. If possible, try to keep your sleep space as dark as you can. Darkness helps regulate the body’s circadian rhythms, which can improve the quality of your sleep.
10. Exercise
Like getting enough rest, exercise can also help you manage stress. One study found that aerobic exercise can help decrease burnout, and one symptom of burnout is depersonalization.
If you’re interested in exercise but aren’t sure what to choose, walking could be a good option. Walking can help lower your body’s cortisol, which can help decrease stress.
If you’re living with depersonalization disorder, finding the right type of support can be an essential part of self-care.
If you’d like to find a mental health professional, the American Psychiatric Association (APA) has a searchable database that can help you find a therapist. If you’re looking for a local support group, you might contact your local National Alliance on Mental Health (NAMI) chapter.
If you’re looking for a local support group, you might contact your local National Alliance on Mental Health (NAMI) chapter.
If you’d like to read about other people’s experiences with depersonalization, you can check out the NAMI blog post, “The Scariest Panic Symptoms People Don’t Talk About,” which is one person’s story about living with depersonalization disorder. You can find other blog posts here and here.
If you’re interested in checking out some mental health podcasts, The Anxiety Podcast seeks to support anyone struggling with anxiety, stress, and panic attacks. The Spin Cycle is another mental health podcast that features interviews with mental health professionals.
Maybe you’re ready to check out meditation, but you aren’t sure where to start. Meditation Minis is a podcast that includes several types of guided meditations. And if you’re on Clubhouse, meditation teacher Lisa Abramson leads mindfulness classes every day.
Finally, know that taking care of your mental health takes courage! Sure, it can feel frustrating at times, and that’s OK. No one expects you to be perfect. With more mental health resources and tools available, living with depersonalization disorder is much easier.
No one expects you to be perfect. With more mental health resources and tools available, living with depersonalization disorder is much easier.
FGBNU NTsPZ. Dissertations. Ilyina Natalya Alekseevna. Depersonalization depression (psychopathology, dynamics, therapy) ..
Ilyina Ilyina
Depersonalization depression (psychopathology, dynamics, therapy)
Author of the discord -degree of candidate of medical sciences 9000 9000 9000 9000 9000 CHARACTERISTICS OF THE RESEARCH
Relevance of the study
The paramount importance of the study of depression already follows from the results of epidemiological studies. According to modern data, the prevalence of this pathology in the population is at least 5.5%, and taking into account dysthymia - 9% [Reiger D., Boyd J., 1988] and even 9.5 - 11.3% [Judd L.L., 1996] . The urgency of the problem is growing in view of the increase in the prevalence of depression over the past decades, which, according to the WHO forecast, will take second place among ten disabling diseases by the beginning of the 21st century.
According to a number of researchers, the increase in the number of patients with affective diseases occurs mainly due to atypical, protracted, intractable forms, which primarily include depersonalization depression [Petrilowitsch N., 1976; Smulevich A.B. et al., 1971; Kielholz P., 1973; Robinson D.S. et al., 1974; Avrupkiy G.Ya., 1976; Vovin R.Ya., Aksenova I.O., 1982; Zisook V. et al., 1985; Pies R., 1988; Liebowitz M.R. et al., 1988].
It must be emphasized that this group of depressions occurring with depersonalization phenomena has not yet received a clear clinical definition.
Modern classifications (ICD-10) do not distinguish depersonalization depression as an independent category. The only rubric that combines depression symptoms with separate signs of alienation phenomena ("loss of emotional reactivity to the environment or events that are normally pleasant") and belongs to section F30-F39 "Mood (affective) disorders" contains the interpretation of these disorders of self-awareness as somatic symptoms of depression . At the same time, the classic melancholic symptom - "feeling of lack of feelings" is not included in the section of affective disorders, but is only mentioned among other symptoms of depersonalization in section F4 - "Neurotic, stress-related and somatoform disorders". The category of these disorders also includes other manifestations of depersonalization, often observed in clinical practice together with affective pathology, and considered among neurotic disorders only with an indication of their most frequent occurrence within the framework of depressive, phobic and obsessive-compulsive disorder.
At the same time, the classic melancholic symptom - "feeling of lack of feelings" is not included in the section of affective disorders, but is only mentioned among other symptoms of depersonalization in section F4 - "Neurotic, stress-related and somatoform disorders". The category of these disorders also includes other manifestations of depersonalization, often observed in clinical practice together with affective pathology, and considered among neurotic disorders only with an indication of their most frequent occurrence within the framework of depressive, phobic and obsessive-compulsive disorder.
Most researchers refer to depersonalization depressions as typologically heterogeneous affective states, including, along with the classical one - melancholia anaesthetica - and other options, anesthetic manifestations in which are not limited to the painful sensation of loss of all feelings (anaesthesia psychica dolorosa), but cover a wide range of self-consciousness disorders that are realized within the framework of neurotic, somatovegetative and other types of depersonalization. At the same time, the traditional idea of a protracted, unfavorable course of these conditions and their resistance to therapy dominates [Khvilivitsky T.Ya., 1966; Tiganov A.S. 1975; 1997; Krasnov V.N., 1978, 1980; Bovin R.Ya., Aksenova M.O., 1982; Nuller Yu.L., Mikhalenko I.N., 1988; Bondar V.V., 1992; Akhapkina M.V., 1993].
At the same time, the traditional idea of a protracted, unfavorable course of these conditions and their resistance to therapy dominates [Khvilivitsky T.Ya., 1966; Tiganov A.S. 1975; 1997; Krasnov V.N., 1978, 1980; Bovin R.Ya., Aksenova M.O., 1982; Nuller Yu.L., Mikhalenko I.N., 1988; Bondar V.V., 1992; Akhapkina M.V., 1993].
However, such an assessment of the prognosis of depersonalization depression, as shown by clinical observations, does not seem to be the only possible one. In some cases, affective disorders of this range are characterized by a favorable course and outcome [Smulevich A.B. et al., 1997].
Thus, depersonalization depressions are a heterogeneous group, the clinical assessment of which, when comparing data from a number of modern studies, is ambiguous and is the subject of further analysis.
Purpose and objectives of the study
The purpose of this study is a clinical (with the involvement of follow-up data) study of the structure of depressive-depersonalization states, aimed at their typological differentiation, analysis of dynamics and outcomes, which allows developing new approaches to optimize therapeutic and rehabilitation programs.
Accordingly, the following tasks are solved in the work:
— typological differentiation of depersonalization depressions, taking into account the psychopathological structure of the components of the syndrome;
- determination of the mechanisms of occurrence of alienation phenomena and comorbid affective disorders;
— analysis of the dynamics and outcomes of affective disorders with a predominance of depersonalization phenomena;
— optimization of treatment and rehabilitation programs differentiated according to the typology of depersonalization depressions.
Scientific novelty
For the first time, taking into account the clinical mechanisms of the occurrence of depersonalization disorders and their interaction with the affective component of the syndrome, variants of depersonalization depressions were identified: with phenomena of hysterical and defective depersonalization. Relationships between the psychopathological structure and the clinical prognosis of the studied affective pathology were established; the possibility of not only a malignant course, but also a favorable outcome of depressive states with a predominance of depersonalization phenomena has been proved. It has been shown for the first time that the response to the effects of psychotropic drugs is associated with the typological structure of depersonalization depressions. The information content of these data as predictors of effectiveness has been confirmed, which allows solving the issues of differentiated psychopharmacological effects and the choice of tactics for rehabilitation measures. Within the framework of depressions with the phenomena of hysterical depersonalization, a special form of self-awareness disorders in the cognitive sphere, designated by the term "apperceptive anesthesia", was singled out.
It has been shown for the first time that the response to the effects of psychotropic drugs is associated with the typological structure of depersonalization depressions. The information content of these data as predictors of effectiveness has been confirmed, which allows solving the issues of differentiated psychopharmacological effects and the choice of tactics for rehabilitation measures. Within the framework of depressions with the phenomena of hysterical depersonalization, a special form of self-awareness disorders in the cognitive sphere, designated by the term "apperceptive anesthesia", was singled out.
The practical significance of the results of the study
The psychopathological differentiation of depersonalization depression presented in the work contributes to the solution of complex diagnostic problems associated with the clinical assessment of alienation phenomena in the structure of affective disorders.
Developed taking into account the psychopathological heterogeneity of depersonalization depressions and the stereotype of their development, methods of phased therapeutic effects, as well as recommendations for the use of psychotropic drugs, in
including the latest generation of antidepressants, allow you to optimize the possibilities of psychopharmacotherapy.
The established regularities of the course and outcomes of depersonalization depressions make it possible to provide an adequate choice of measures for clinical and social rehabilitation aimed at compensating for painful disorders.
Publication of research results
The main results of the research are reflected in 5 scientific publications, the list of which is given at the end of the abstract. The generalized data of the dissertation work were reported at the Conference of Young Scientists held at the NTSPZ RAMS (May 1997), at the scientific and practical conference with international participation "Affective and schizoaffective psychoses" (Moscow, April 1998), the conference "Modern methods of diagnosis and treatment of schizophrenia" (Smolensk, October, 1998), as well as at the interdepartmental scientific conference NTsPZ RAMS (March 29, 1999).
Scope and structure of the work
The dissertation is presented on . .. pages of typewritten text (main text - .... literature index - ...) and consists of an introduction, 5 chapters (Review of literature;
.. pages of typewritten text (main text - .... literature index - ...) and consists of an introduction, 5 chapters (Review of literature;
Characteristics of the material and research methods; Psychopathology of depersonalization depressions; Depersonalization depression, course and outcome;
Issues of therapy and social rehabilitation), conclusions and conclusions. The bibliographic index contains ... names (of which domestic - ..., foreign - ...). The dissertation is illustrated with 11 tables, 5 figures and 4 clinical observations.
Research materials and methods
When planning and conducting the study, clinical and clinical follow-up methods were chosen as the main methods.
Based on the nosological and syndromic qualification of the studied conditions, the features currently used in the official classifications of mental disorders (ICD-9 and ICD-10) were chosen, supplemented in such a way that already during the formation of the sample, conditions were created for a verified psychopathological assessment of both coexisting in the clinical picture of the components of the syndrome under study: hypothymic and depersonalization. Particular attention in the psychopathological analysis of the clinical picture was paid to the assessment of the depersonalization component of the studied syndrome, carried out taking into account a wide range of alienation phenomena, assessed according to the criteria of heading F 48.1 (“Depersonalization-derealization syndrome”) of the International Classification of Mental Diseases of the 10th revision. For the syndromic assessment of the disorder under study, the most common systematics of depersonalization (depressive, neurotic, defective) was additionally used.
Particular attention in the psychopathological analysis of the clinical picture was paid to the assessment of the depersonalization component of the studied syndrome, carried out taking into account a wide range of alienation phenomena, assessed according to the criteria of heading F 48.1 (“Depersonalization-derealization syndrome”) of the International Classification of Mental Diseases of the 10th revision. For the syndromic assessment of the disorder under study, the most common systematics of depersonalization (depressive, neurotic, defective) was additionally used.
The study material consisted of patients whose affective disorders at the time of the examination met the definition of non-psychotic depression, with a duration of depersonalization depression of at least 6 months; subject to the possibility of studying the dynamics of the states under study through long-term direct or follow-up observation (at least 2 years).
The study did not include patients whose condition at the time of the examination showed signs of manifest schizophrenic (schizoaffective) psychosis, organic CNS damage, severe disabling somatic disease, alcoholism, drug addiction.
The study sample included 91 patients with depressive-depersonalization conditions (37 men and 54 women aged 17 to 60 years; mean age 29.6 ± 9.1 years).
The criteria for exclusion from the study group were signs of overt schizophrenic (schizoaffective) psychosis, organic damage to the central nervous system, severe disabling somatic disease, alcoholism, drug addiction.
According to the nosological affiliation (ICD-9), patients were distributed as follows: schizophrenia (slow-flowing — 57 cases, residual — 4 cases), cyclothymia (monopolar type of course — 15 cases, bipolar — 15 cases).
In the course of treatment of depressive-depersonalization states, the depression (Hamilton) and general clinical impression (CGI) scales were tested for standardized processing of information, assessment of the initial severity of depression and control of the dynamics of psychopathological disorders.
RESULTS OF THE STUDY
The analysis of the studied conditions is based on the concept of clinical heterogeneity of depersonalization depressions. The mechanisms of their occurrence, the psychopathological structure of alienation phenomena, as well as comorbid affective disorders are considered as typologically differentiating signs of the affective-depersonalization syndrome.
The mechanisms of their occurrence, the psychopathological structure of alienation phenomena, as well as comorbid affective disorders are considered as typologically differentiating signs of the affective-depersonalization syndrome.
Analysis of affective states with a predominance of alienation phenomena made it possible to distinguish two variants of depersonalization depressions — with the phenomena of hysterical (ID) and defective (DD) depersonalization.
Typological differences between the two variants of affective disorders are based on polar psychopathological mechanisms associated with the nature of alienation phenomena.
Depression with symptoms of hysterical depersonalization [Jane P., 1911] — first variant — 67 observations (22 men and 45 women).
Disorders of self-awareness in this variant of depression reflect the lightest level of mental dissociation related to the pathology of imagination - neurotic (hysterical). This is evidenced by a tendency to dramatize, exaggeratedly expressive expression of attitudes towards painful manifestations. The connection between the phenomena of alienation and the mechanisms of hysterical dissociation is also confirmed by the occurrence of conditions considered within the framework of hysterical response, as well as by the lability of psychopathological symptoms in relation to psychogenic influences.
This is evidenced by a tendency to dramatize, exaggeratedly expressive expression of attitudes towards painful manifestations. The connection between the phenomena of alienation and the mechanisms of hysterical dissociation is also confirmed by the occurrence of conditions considered within the framework of hysterical response, as well as by the lability of psychopathological symptoms in relation to psychogenic influences.
Features of the depersonalization component of depression - partiality, relatively shallow degree of manifestation of alienation phenomena, dissociation between subjective perception of the severity of the disease and objective assessment.
The phenomena of alienation of cognitive functions are limited to the actual sphere of interpersonal relations, for their definition the term "apperceptive anesthesia" is proposed, reflecting the content characteristics of the leading disorder and emphasizing its connection with the pathology of imagination.
The symptomatology extending beyond the disorders of self-awareness of ideation functions is limited. Among the manifestations of allopsychic alienation, the feeling of a change in emotional involvement in external objects, "existence behind a barrier" dominates. Somatopsychic depersonalization is exhausted by a fluctuating, unstable distortion of bodily perception with a projection onto a separate organ or function. Anesthesia in the emotional sphere does not reach a climax. The only sign of a change in the self-consciousness of vitality [Snezhnevsky A.V., 1983; Jaspers K., 1923] is combined with the phenomena of depressive hyperesthesia and is exhausted by the features of anhedonia, which extends not only to the sphere of somatosensory drives, but also to spiritual values.
Among the manifestations of allopsychic alienation, the feeling of a change in emotional involvement in external objects, "existence behind a barrier" dominates. Somatopsychic depersonalization is exhausted by a fluctuating, unstable distortion of bodily perception with a projection onto a separate organ or function. Anesthesia in the emotional sphere does not reach a climax. The only sign of a change in the self-consciousness of vitality [Snezhnevsky A.V., 1983; Jaspers K., 1923] is combined with the phenomena of depressive hyperesthesia and is exhausted by the features of anhedonia, which extends not only to the sphere of somatosensory drives, but also to spiritual values.
The depressive component itself is characterized by the presence of a relatively mild degree of hypothymia with a predominance of anxiety-apathetic affect [Fanai F. 1973]. An integral part of hypothymia in all cases related to this variant of depression are hystero-dysphoric manifestations integrated into the structure of pathologically reduced affect [Koliutskaya E.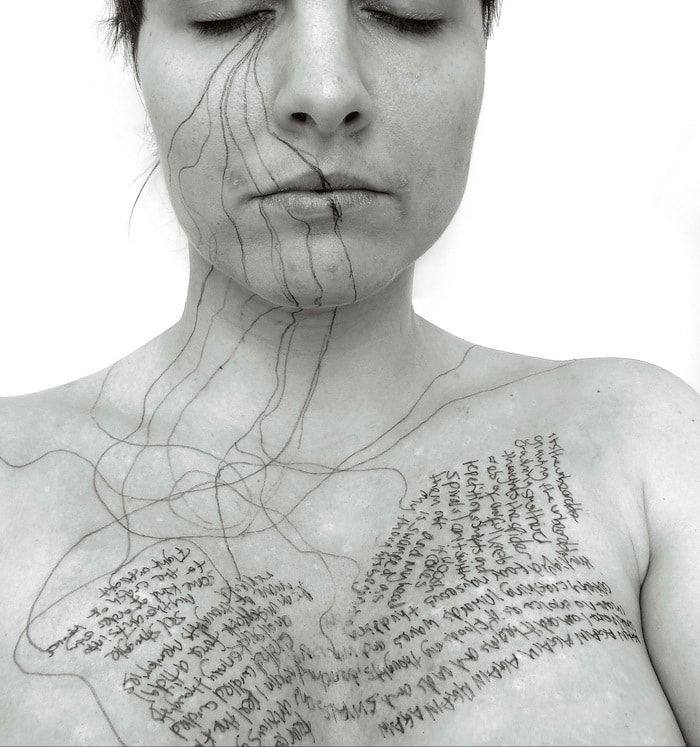 V., 1993; Liebowiz M.R., Yesh D.F., 1979; Akiskal H.S., 1983; Hirsehfeld R., 1990].
V., 1993; Liebowiz M.R., Yesh D.F., 1979; Akiskal H.S., 1983; Hirsehfeld R., 1990].
Demonstrative traits with dramatization and figurative representations of the consequences of the violations that have arisen leave their mark on all the symptoms of depression. Complaints of melancholy, which differ in features of physicality and have a bodily projection (chest area, epigastrium), with an objective assessment, reveal similarities with "bodily fantasies" [Burenina N.I., 1997; Shon z F., 1978, 1985]. Ideas of guilt take the form of ideas of "bad conscience" [Leonhard K., 1957] and are accompanied by "suicidal blackmail" [Miehaux L., 1964]. Somatovegetative disorders are represented by single phenomena, which are among the mildest in depression. Thus, loss of appetite is unstable, selective and rarely accompanied by weight loss. In a number of observations, an inverted daily rhythm is recorded with fluctuations in well-being from depression to "full health". No objectively expressed signs of psychomotor inhibition or agitation are recorded.
Depression with symptoms of defective depersonalization [Haug K., 1939] — second variant — 24 observations (15 men and 9 women).
Anesthetic disorders in this variant of depression, unlike the previous one, reflect not only a feeling of alienation that extends to one or another sphere of mental activity, but also an awareness of the changes that have actually occurred, "a reaction of self-consciousness to a defect or a process leading to a defect" [Haug K., 1939]. According to a number of researchers [Jackson J.H., 1884; Jaspers K., 1913; Bleuler M., 1972], these violations of self-awareness are comparable to pathological manifestations attributed to the so-called "basic disorder" [Berze J., 1926] (and much later - to the basic symptoms [Huber G., 1983]) and defined as "hypotension consciousness" [Berze J., 1926]. If, in the first variant of depression, depersonalization disorders are related to the pathology of the imagination and, accordingly, differ in the partial splitting off of individual mental functions, then in the second, they constitute nuclear manifestations of self-consciousness disorders and are represented by disturbances of self-consciousness of the activity and unity of the Self, characteristic of hypotension of consciousness, acquiring a total character. Another distinctive feature of depersonalization in these cases is the drop in vitality [Huber G., 1983].
Another distinctive feature of depersonalization in these cases is the drop in vitality [Huber G., 1983].
Alienation of cognitive functions, in contrast to the corresponding manifestations in the first variant of depersonalization depression, goes beyond the sphere of interpersonal relations and, acquiring clear forms of self-awareness disorders, is expressed by a feeling of insufficiency of specific, unique features of one's self. Depersonalization disorders that extend to the allopsychic sphere are characterized by "a total experience of existence in a void" [Gebsa el V.E., 1937] and differ from signs of alienation comparable to elementary visual impairments that occur within the framework of hysterical depersonalization. Anesthesia in the somatopsychic sphere, in contrast to similar phenomena of alienation in the first variant of depression, includes not only symptoms of a bifurcation of bodily perception, but covers a wider area, including disorders of the general feeling of the body. Complaints about the lack of feelings are represented by a monotonous statement of the changes that have occurred without the corresponding expression. Vital drives, in contrast to partial, shallow disorders in patients with hysterical depersonalization, are completely alienated.
Complaints about the lack of feelings are represented by a monotonous statement of the changes that have occurred without the corresponding expression. Vital drives, in contrast to partial, shallow disorders in patients with hysterical depersonalization, are completely alienated.
The actual depressive component of the syndrome is characterized by a predominance of apathetic affect with features of anergy. Vital disorders (feeling of melancholy or anxiety) are more pronounced than in the first variant of depression and are of a deep protopathic nature. Manifestations of dysphoria such as "unlus" [Lemke R., 1960] differ from the corresponding symptoms of hysterodysphoria in gross behavioral disorders with malice and aggression.
As shown by the study, the selected variants of depersonalization depressions reflect not only their psychopathological heterogeneity, but also carry information about various trends in the dynamics of affective disorders that are detected during the further development of the disease.
Along with the common features observed in the dynamics of depersonalization depressions (a tendency to a long, protracted course, the predominance of hypothymia over states with the opposite sign of affect, etc.), as noted by many researchers [Nuller Yu.L., Mikhalenko I.N. , 1968; Nuller Yu.L., 1973; Vovin R.Ya., Aksenova M.O., 1982; Krasnov V.N., 1978; Tiganov A.S., 1997], already when assessing quantitative parameters, differences are revealed. In the first variant of depression with ID, a significant proportion of observations recorded periodicity, phasic affective disorders, indicating their reversibility and thus a relatively more favorable prognosis than in the second (depression with DD), where chronic hypothymia is almost twice as common. In addition, differences are also found when assessing the characteristics of the patients' premorbid, as well as when comparing the nosological affiliation of the studied variants of depersonalization depression. Depressive states with ID are distributed between two diagnostic categories - "cyclothymia" (40% of cases) and "schizophrenia" (60% of cases), while the presence of depression with DD in all cases corresponds to the diagnosis of schizophrenia with an unfavorable development of the process.
However, the most significant differences are identified in the analysis of the studied variants, carried out at the clinical level.
Constitutional predisposition, course and outcome of depression with symptoms of hysterical depersonalization
Premorbid features of patients belong to the dramatic cluster. However, the totality of pathocharacterological properties is a feature of unstable affectivity [Livesley W.J. e al., 1994] and signs of a violation of self-identification [Sab M., Kochler, 1983] allow us to consider such constitutional features within the framework of borderline personality disorder (BPD) [Cloninger C.R., Guse S.V., 1975; Links P., 1982; Harrison G. e al., 1983]. This is also evidenced by such personality deviations in patients with affective disorders with ID as a tendency to form transient affective and dissociative disorders, the use of psychoactive substances, intolerance to frustration, accompanied by suicidal behavior, and others.
Among the obligate properties is the presence of an accentuation of the sphere of self-consciousness with a tendency to transform abnormal personality traits into transient depersonalization phenomena, which is realized in different periods of age development.
Depression with symptoms of hysterical depersonalization, despite the relapsing and sometimes protracted course, correlates with a favorable prognosis and the possibility of complete reduction of clinical manifestations.
Manifest depression, which marks the onset of the disease, falls on the age of 16 to 46 years (average 32.4±7.2). In more than half of the observations, the debut of affective disorders is preceded by provocative influences, mainly psychogenic ones. At the stage of formation of developed depressive symptoms, in most cases, panic attacks are noted.
The formation of depressive-depersonalization disorders occurs, as a rule, rather quickly (in 1-4 weeks). The duration of recurrent depression varies from 2 to 6 months, dysthymia - from 2. 5-3 years or more. The reverse development of depressive-depersonalization disorders in most cases is characterized by a parallel reduction of both components of the syndrome.
5-3 years or more. The reverse development of depressive-depersonalization disorders in most cases is characterized by a parallel reduction of both components of the syndrome.
The greatest number of remissions has a duration of 6 to 12 months. In all cases related to this variant of the studied conditions, after the depersonalization depression has passed, remissions are formed with the restoration of professional activity and social activity at the pre-morbid level inherent in patients or close to it. At the same time, in those cases where cyclothymia is diagnosed, phase affective disorders end with either complete or thymopathic remission, in which residual affective symptoms can persist for up to several months with a tendency to a complete reduction of positive disorders with lengthening of light intervals. In cases of schizophrenia, there is a tendency for the occurrence of recurrent or chronic affective disorders. As the extensive depressive symptoms are reduced, remissions are formed with signs of autochthonous lability, irritable weakness and asthenia.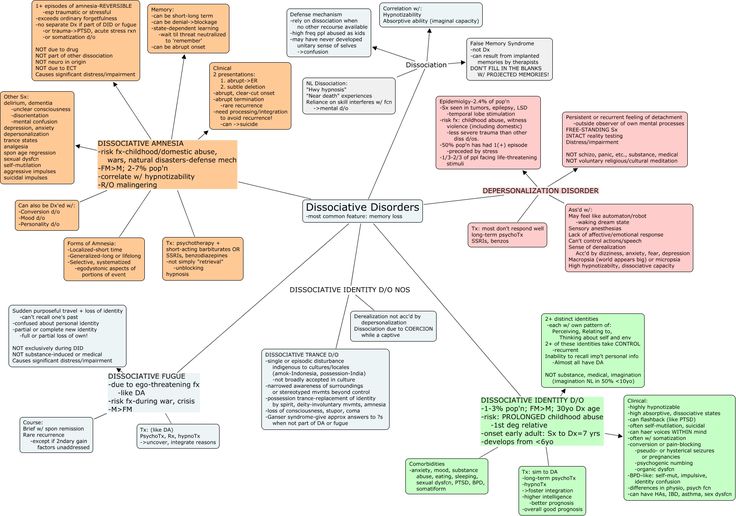 After repeated affective phases, relatively shallow deficient disorders of the schizoid spectrum become more distinct in the form of an increase in isolation, emotional leveling, eccentricity, and a decrease in activity. Signs of a psychopathic defect are also characterized by the appearance of a tendency to magical thinking, the aggravation of the premorbid inherent features of demonstratively, capriciousness.
After repeated affective phases, relatively shallow deficient disorders of the schizoid spectrum become more distinct in the form of an increase in isolation, emotional leveling, eccentricity, and a decrease in activity. Signs of a psychopathic defect are also characterized by the appearance of a tendency to magical thinking, the aggravation of the premorbid inherent features of demonstratively, capriciousness.
Alienation phenomena in the absence of extensive affective manifestations acquire the properties of subsyndromal psychopathological formations. As in the period preceding the onset of an affective illness, self-awareness disorders retain lability in relation to provocative influences, without revealing a tendency to generalization, modification and complication.
Constitutional predisposition, course and outcome of depression with symptoms of defective depersonalization
The constitutional properties of patients show significant differences from the premorbid of depressed patients with symptoms of hysterical depersonalization and are mainly limited to schizoid features.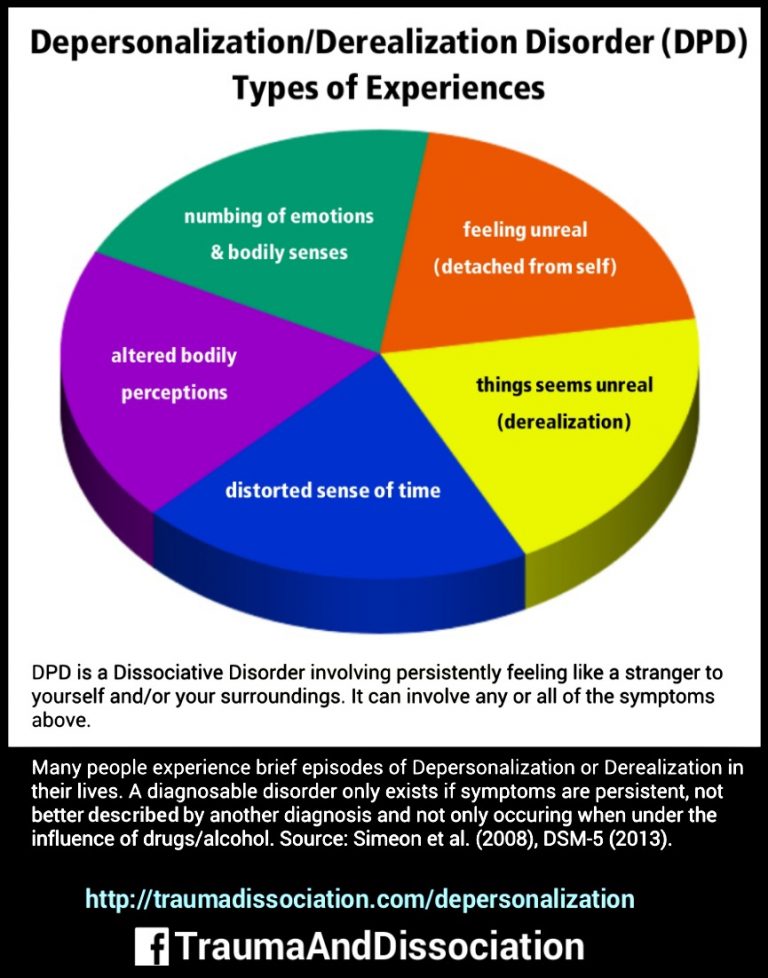 Shyness, shyness, sensitivity, introspection with detachment from life - in some, and perseverance, emotional coldness with arrogance and perseverance in achieving the goal - in others, is combined with a reduced need for contacts and painful pride.
Shyness, shyness, sensitivity, introspection with detachment from life - in some, and perseverance, emotional coldness with arrogance and perseverance in achieving the goal - in others, is combined with a reduced need for contacts and painful pride.
The onset of full-blown depressive symptoms occurs, as a rule, at an earlier age (17-20 years) than in the first variant of depression. Moreover, if in patients referred to the first variant of depersonalization depressions, the occurrence of clinically defined affective manifestations coincides with the onset of the disease, then depression with DD is formed already against the background of a growing disorder of mental activity in the form of erased deficient symptoms (a decrease in mental activity, impaired thinking with a weakening of the ability to concentration of attention) and is a reflection of the generalization of the disease process [Morozov V.M., 1969]. Negative changes preceding the manifestation of depressive-depersonalization disorders occur during the period of a pathologically occurring pubertal crisis, which marks the beginning of a procedural disease and is manifested by psychopathic (heboid) disorders with the formation of a personality shift.
In contrast to affective disorders comorbid with ID, the role of provoking factors in the onset of depressive disorders in this variant is insignificant;
Psychogenic traumas that have taken place are most often opportunistic in nature.
The development of hypothymia is usually gradual. The emergence of manifest affective disorders, in contrast to the variant of depression with ID (often accompanied by panic attacks), in some cases is preceded by the appearance of senesto-hypochondriac symptoms.
After the affective phases pass, in a number of cases, shallow manifestations of hypothymia persist, in another part of the observations, a transition to a continual course is noted.
Depersonalization disorders that form in the structure of depression with DD are irreversible, acquire a persistent character with subsequent modification and transformation into a defect structure. Manifesting a sense of change, incomplete perception of the environment, one's own body, which dominates at the initial stages of the development of the disease, self-consciousness disorders are gradually stereotyped, lose their brightness, which was previously characteristic of the tragic awareness of the changes that have taken place, acquire a "resonant" [Krasnov V. N., 1980] character and are reduced to monotonous registration of objectively observed deficient changes.
N., 1980] character and are reduced to monotonous registration of objectively observed deficient changes.
Thus, the feeling of alienation of intellectual abilities, being transformed during the formation of a defect, is realized by a drop in the productivity of mental activity, and subsequently by a persistent intellectual decline. The phenomena of somatopsychic depersonalization, initially associated with asthenic manifestations and alienation of one's own activity, acting in the structure of depression, in the process of further transformation acquire the properties of an objectively recorded persistent decrease in working capacity. Complaints about the lack of feelings as the disease progresses become a reflection of a real-life emotional deficit.
Modifications of depersonalization disorders that occur in the course of an unfavorable current schizophrenia are complemented by a phenomenon characteristic of the outcome of DD - "moral hypochondria" [Falre J., 1866]. Patients are entirely fixated on the state of their mental functioning. Some stenically seek from specialists a complete restoration of their former intellectual abilities, the use of the latest methods of treatment, and independently develop a whole system of measures. Others, stating the onset of mental
Some stenically seek from specialists a complete restoration of their former intellectual abilities, the use of the latest methods of treatment, and independently develop a whole system of measures. Others, stating the onset of mental
inferiority, take a passive position, protecting themselves from overwork and correlate their actions with the situation of the disabled, people with disabilities due to illness.
Methods for optimizing the treatment of depression with a predominance of alienation phenomena are presented in a number of publications [Megrabyan AA, 1962; Khvilivitsky T.Ya., 1966; Nuller Yu.L., Mikhalenko I.N., 1988; Bovin R. Ya, Aksenova M. O., 1983; Mosolov S.N., 1995]. The study of the modification of the clinical picture of depersonalization depressions occurring in the process of psychopharmacotherapy, carried out in the framework of this study, indicates the presence of a close relationship between the psychopathological structure and the nature of the comorbid ratios of affective and depersonalization disorders in each of the selected variants of depression, on the one hand, and the different susceptibility of these conditions to therapeutic effects - with another.
Analysis of the results of treatment of patients in the studied sample showed that the proportion of patients with depersonalization depression with a complete reduction of psychopathological disorders in general was 33.3%, which corresponds to the data of other researchers [Avrutsky G.Ya. et al., 1991; Mosolov S.N., 1995].
However, evaluation of the effectiveness of therapy for affective disorders, differentiated depending on comorbidity with ID and DD, showed that the data presented do not fully reflect the therapeutic potential of psychotropic drugs in depersonalization depression.
The clinical effect of psychopharmacotherapy in depression with ID is much higher than that in affective disorders with symptoms of DD.
Analysis of the results of treatment according to the parameters: "complete reduction of the syndrome", "splitting of the syndrome", "resistance of the syndrome to therapy" indicates the following.
In depression with ID, a complete reduction of psychopathological symptoms was observed in more than 2/3 of patients (80. 3% of cases) and was not recorded in patients with DD. The effect of treatment in DD was reflected only in a decrease in the severity of manifestations of hypothymia (37.5% of cases). At the same time, in 62.5% of cases, DD therapy for depression was ineffective.
3% of cases) and was not recorded in patients with DD. The effect of treatment in DD was reflected only in a decrease in the severity of manifestations of hypothymia (37.5% of cases). At the same time, in 62.5% of cases, DD therapy for depression was ineffective.
Given the complexity of the treatment of depersonalization depressions, antidepressants of all main groups were used for their treatment: tricyclic (amitriptyline, imipramine, clomipramine), tetracyclic (maprotiline), as well as new generation drugs (fluoxetine, sertraline; selective reversible MAO inhibitor type A - myjubemide) . Tranquilizers (benzodiazepine derivatives - phenazepam, diazepam, etc., as well as piperazine - hydroxyzine), antipsychotics (aliphatic phenothiazine derivatives - alimemazine, trifluoperazine, periciazine; thioxanthene - chlorprothixene; butyrophenones - haloperidol, atypical antipsychotic risperidone, etc.).
New generation antidepressants (fluoxetine, sertraline, moclobemide) are preferred for relief of depression with ID, and only in some cases traditional tricyclic antidepressants (TCAs), used in medium therapeutic doses, administered intravenously in combination with antipsychotics (sulpiride, alimemazine).
In case of depression that occurs within the framework of an unfavorable course of schizophrenia with depersonalization, reflecting pronounced and growing negative changes, a more intensive intervention is needed to achieve a therapeutic effect - the appointment of high doses (up to 400 mg / day) of TCAs. The therapeutic effect is achieved in these patients only with prolonged psychopharmacological exposure, followed by repeated courses of intravenous drip infusions of antidepressants.
For the relief of anxiety symptoms in depression with ID, benzodiazepine tranquilizers are mainly used in minimal or moderate doses, and in depression with DD, antipsychotics (chlorprothixene, clozapine) and high doses of tranquilizers are preferred.
Treatment of depressive conditions with depersonalization phenomena is carried out in three stages. At the first stage, tablet forms of drugs are used - antidepressants, as well as tranquilizers and antipsychotics. At the second stage - with the absence of the effect of the previous treatment - a transition is made to parenteral methods of administering thymoleptics with a course of 12-15 infusions. At the third stage - in cases of depression with DD, resistant to psychopharmacotherapy - ECT is prescribed.
At the third stage - in cases of depression with DD, resistant to psychopharmacotherapy - ECT is prescribed.
Due to the fact that in depersonalization depressions, the reverse development of psychopathological disorders in the process of using psychotropic drugs occurs gradually and unevenly with frequent fluctuations in the severity of painful manifestations, the success of thymoleptic treatment is ensured only under the condition of continuous and prolonged drug exposure [Mosolov S.N., 1995], including maintenance therapy. For the prevention of relapse, the addition of drugs from the group of normotimics (lithium salts, carbamazepine (finlepsin, tegretol)) is indicated.
When carrying out rehabilitation measures, one should take into account the different levels of social and labor adaptation of patients attributed to each of the studied variants of depersonalization depression.
Since in patients with ID, social adaptation is not significantly disturbed and affects the sphere of interpersonal communication to a greater extent, which is manifested by work conflicts and unstable marital status, rehabilitation measures are mainly aimed at maintaining existing professional stereotypes, stabilizing intra-family relationships.
In the presence of a persistent decrease in the professional standard, up to the loss of ability to work, observed in patients with DD, the emphasis in rehabilitation measures is shifted to achieving independence in self-service and versatile activation of patients - employment with a light regimen, in medical and labor workshops, institutions that use the work of disabled people, as well as the expansion of contacts with the external environment. Taking into account the need for sequential appointment of several courses of treatment and the associated long-term social isolation, for the prevention of the phenomena of hospitalism, it seems appropriate to limit the length of stay in the hospital by the period of time necessary for active therapy.
CONCLUSIONS
Clinical (using follow-up data) study of a representative sample of patients with depersonalization depression made it possible to establish the following relationships.
1. Depersonalization depressions with phenomena of alienation in the auto-, allo- and somatopsychic spheres are heterogeneous in the psychopathological structure of both depersonalization phenomena and comorbid affective disorders and are divided into two polar variants - with phenomena of hysterical and defective depersonalization.
Depersonalization depressions with phenomena of alienation in the auto-, allo- and somatopsychic spheres are heterogeneous in the psychopathological structure of both depersonalization phenomena and comorbid affective disorders and are divided into two polar variants - with phenomena of hysterical and defective depersonalization.
1.1. Depression with hysterical depersonalization (hystero-hypochondriac hypothymia with anxiety-apathetic affect and vital anhedonia).
Disorders of self-awareness refer to the pathology of the imagination with a partial splitting off of mental functions.
1.1.1. Cognitive alienation affects only the structure of actual interpersonal relationships.
1.1.2. Alienation in the allopsychic realm is limited to a sense of change in emotional involvement with external objects.
1.1.3. Somatopsychic depersonalization is exhausted by an unstable distortion of bodily perception with a projection on individual organs.
1. 2. Depression with defective depersonalization (dysphoria of the "Unlus" type with apathy and vital anguish).
2. Depression with defective depersonalization (dysphoria of the "Unlus" type with apathy and vital anguish).
Disorders of self-awareness refer to the basic (basic disorder Berze J., 1926) manifestations of the endogenous process and are accompanied by a total violation of self-awareness of the activity and unity of the Self.
1.2.1. Cognitive alienation is associated with a feeling of insufficiency of both communicative functions and specific, unique features of one's Self.
1.2.2. Allopsychic depersonalization covers the main manifestations (integrity, completeness, volume) of the external world.
1.2.3. Somatopsychic depersonalization extends to all areas of bodily sensitivity, including the general feeling of the body.
2. The selected options reflect not only psychopathological heterogeneity, but also carry information about differences in premorbidity, nosological affiliation and trends in the dynamics of affective disorders.
2.1. For depression with ID, manifesting in individuals with BPD as part of cyclothymia and neurosis-like schizophrenia, a phase course is characteristic, long-term remissions with the formation (in cases of schizophrenia) of negative changes in the asthenic circle.
Depersonalization disorders that debut after psychogenic or somatogenic provocation within the framework of PA are reversible and are reduced together with manifestations of pathological affect.
2.2. Depressions with phenomena of defective depersonalization develop in schizoid individuals within the framework of unfavorable juvenile schizophrenia and acquire a protracted, chronic course with the formation of a Verschrobene-type defect.
Depersonalization disorders arise autochthonously, are accompanied by the phenomena of "moral hypochondria", are irreversible, as the disease develops, they take the form of negative changes.
3. Psychopharmacotherapy of depersonalization depression involves long-term (inpatient and outpatient stages) treatment using the main classes of psychotropic drugs (antidepressants, tranquilizers, antipsychotics).
The method of treatment is determined by the psychopathological structure of affective disorders.
3. 1. In depression with ID, showing high sensitivity to psychotropic drugs (a positive effect is noted in 80.3% of cases), new generation thymoleptics (fluoxetine, sertraline, moclobemide) are indicated, and only in resistant cases - TCA in combination with benzodiazepine derivatives.
1. In depression with ID, showing high sensitivity to psychotropic drugs (a positive effect is noted in 80.3% of cases), new generation thymoleptics (fluoxetine, sertraline, moclobemide) are indicated, and only in resistant cases - TCA in combination with benzodiazepine derivatives.
3.2. In depression with DD, resistant to the effects of psychotropic drugs (decrease in the severity of hypothymia in 37.5% of cases), TCAs are indicated in combination with neuroleptics (repeated courses of intravenous drip infusions), as well as ECT.
4. Rehabilitation measures - adequate organization of therapeutic tactics, determination of optimal terms of hospitalization, as well as employment are differentiated depending on the variant of depersonalization depression.
4.1. In case of depression with ID, taking into account an insignificant violation of social adaptation, rehabilitation measures are aimed at maintaining professional stereotypes, the level of intra-family relationships and interpersonal communication.
4.2. In case of depression with DD, due to the tendency to a persistent, up to disability, decrease in the professional standard, measures are shown to activate patients, expand contacts with the external environment, restore self-service skills, and get a job with a light regimen.
LIST OF WORKS published on the topic of the dissertation
1. The phenomena of depersonalization in depressive states. // Modern Psychiatry. P.B. Gannushkina, 1998. - №2. - pp. 19-21.
2. Depressive depersonalization syndrome. // Journal of neuropathology and psychiatry. S.S. Korsakov, 1998. - No. 8. - With. 19-22.
3. To psychopathological differentiation of anesthetic depressions. // In the book:
Affective and schizoaffective psychoses (the current state of the problem) (Materials of a scientific and practical conference with international participation on April 7-8, 1998). M, 1998r.-c.l95.196.
4. Therapy of depersonalization depressions in patients with schizophrenia (experience with Aurorix). // In the book: Schizophrenia and schizophrenia spectrum disorders. M., 1999. - pp. 275-277.
// In the book: Schizophrenia and schizophrenia spectrum disorders. M., 1999. - pp. 275-277.
5. Differentiation of the syndrome of depressive depersonalization (to the psychopathological characteristic of the phenomenon of "moral anesthesia"). (Accepted for publication in the Journal of Neuropathology and Psychiatry named after S.S. Korsakov).
Treatment of depersonalization and derealization in St. Petersburg
- Home
- Psychiatry
- Treatment of depersonalization and derealization
Depersonalization and derealization are treated in our clinic. To start the treatment of the syndrome, a face-to-face consultation with a psychiatrist and a differential examination are necessary to clarify the diagnosis and exclude / confirm diseases that cause a similar condition against the background of the course (for example, OCD, phobic and depressive disorders, delusional and dissociative disorders, early dementia).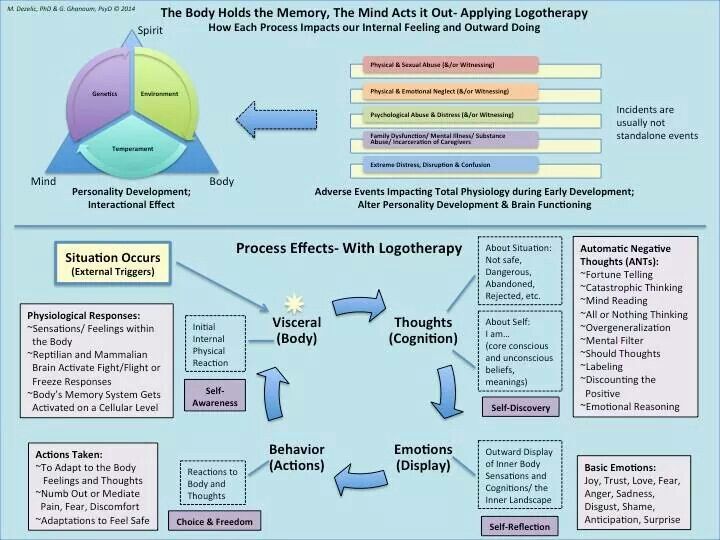
About half of the world's population has experienced a state of depersonalization-derealization at least once in their lives. But only 2% of them fully meet the diagnostic criteria for the syndrome.
In order to shorten the period of selection of pharmacotherapy in the treatment of depersonalization and derealization, hospitalization (4–6 weeks) is required. The conditions of the hospital allow you to monitor the patient's condition in dynamics and promptly adjust drug treatment. Also, in the hospital of the clinic, patients are provided with psychotherapeutic assistance, which precedes individual and / or group sessions after discharge, adapting to a full life in the family and society.
In particular, if the disease has caused intra-family conflicts, they can be resolved in family therapy sessions. In addition, participation in a group of open problems will allow you to get rid of internal experiences, restore lost communication skills. In parallel with outpatient treatment (taking prescribed drugs), one should not forget about visits to the attending physician, who should be informed of any conditions that cause anxiety or seem unusual.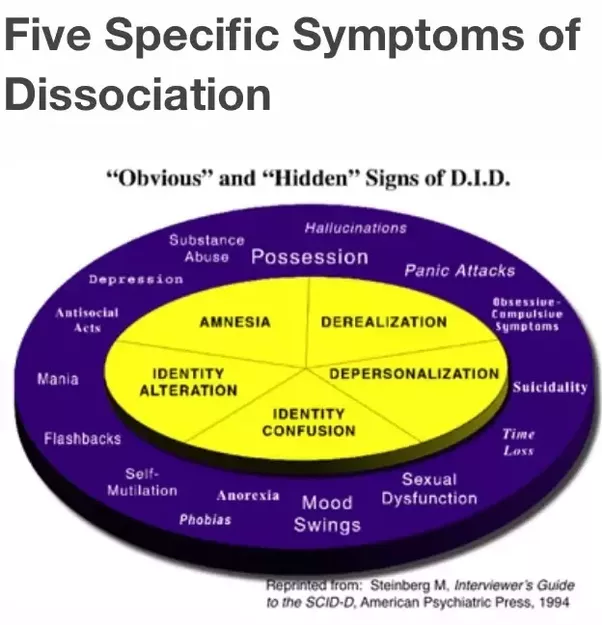 Such an approach to the treatment of depersonalization and derealization will make it possible to correct drug treatment in a timely manner, get rid of addictive attitudes and, as a result, prevent a relapse of the disease.
Such an approach to the treatment of depersonalization and derealization will make it possible to correct drug treatment in a timely manner, get rid of addictive attitudes and, as a result, prevent a relapse of the disease.
Doctor's consultation on the treatment of depersonalization:
+7 (812) 407-18-00
Thank you for your trust!
- Assistance in resocialization
- Safe drug therapy
- Psychologists with clinical experience
| Service | Price | |
|---|---|---|
| Psychotherapist appointment | 5 000 ₽ | |
| Family Therapy | 10 000 ₽ | |
| Hypnotherapy | 8 000 ₽ | |
| Psychiatric consultation | 5 000 ₽ Depersonalization under academic stress — https://pubmed. Update date: 12/28/2020
Make an appointment Date and time: (not set) Make an appointment with a psychiatrist Make an appointment with a psychiatrist Select the date and time of your appointment Today October 31 Tomorrow November 01 Wednesday November 02 Thursday November 03 Friday November 04 Saturday November 05 Sunday November 06 Monday November 07 Tuesday November 08 Wednesday November 09 Thursday November 10 Friday November 11 Saturday November 12 Sunday November 13 Monday November 14 Tuesday November 15 Wednesday November 16 Thursday November 17 Friday November 18 Saturday November 19 Sunday November 20 Monday November 21 Tuesday November 22 Wednesday November 23 Thursday November 24 Friday November 25 Saturday November 26 Sunday November 27 Monday November 28 Tuesday November 29 Wednesday November 30 Treatment of depersonalization and derealization is carried out on Bocharov Alexey Psychiatrist, psychotherapist Psychiatrist, psychotherapist, sexologist, child psychiatrist Work experience 41 years Sinenchenko Andrey Psychiatrist, psychotherapist Psychiatrist, psychotherapist, narcologist Work experience 22 years Zun Sergey Psychiatrist, narcologist Psychiatrist, narcologist, psychotherapist Work experience 33 years Lisitsyna Elena Psychiatrist Psychiatrist Work experience 33 years Buchelnikova Victoria Psychiatrist |
 ncbi.nlm.nih.gov
ncbi.nlm.nih.gov