A common symptom in schizophrenia is
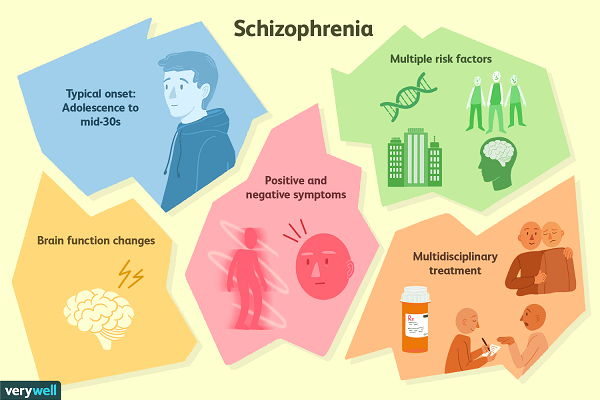
Schizophrenia - Symptoms and causes
Overview
Schizophrenia is a serious mental disorder in which people interpret reality abnormally. Schizophrenia may result in some combination of hallucinations, delusions, and extremely disordered thinking and behavior that impairs daily functioning, and can be disabling.
People with schizophrenia require lifelong treatment. Early treatment may help get symptoms under control before serious complications develop and may help improve the long-term outlook.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
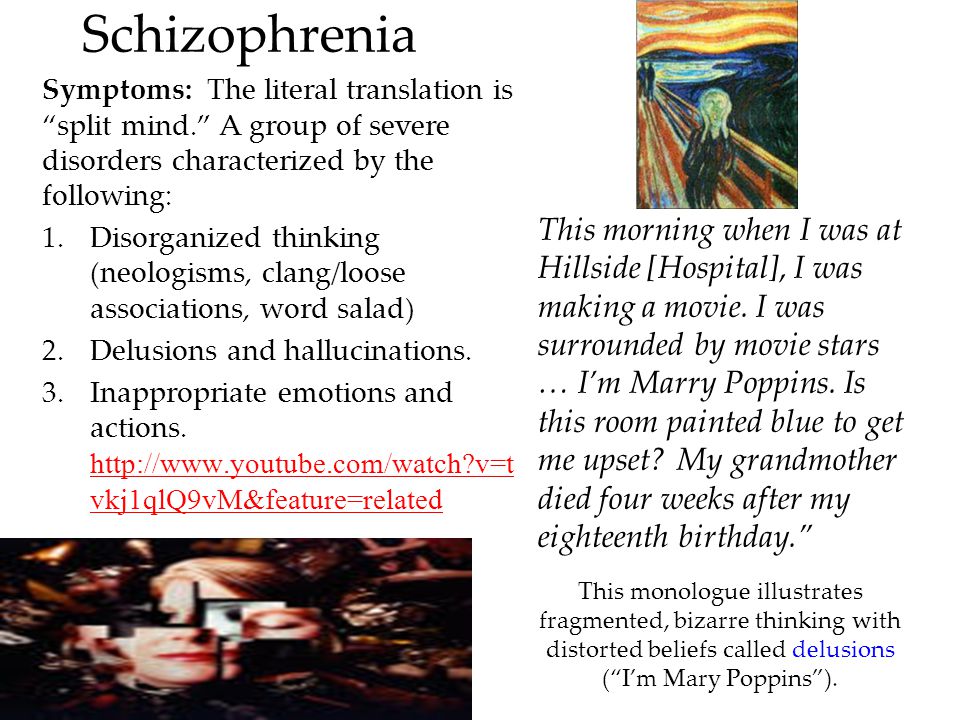
Schizophrenia involves a range of problems with thinking (cognition), behavior and emotions. Signs and symptoms may vary, but usually involve delusions, hallucinations or disorganized speech, and reflect an impaired ability to function. Symptoms may include:
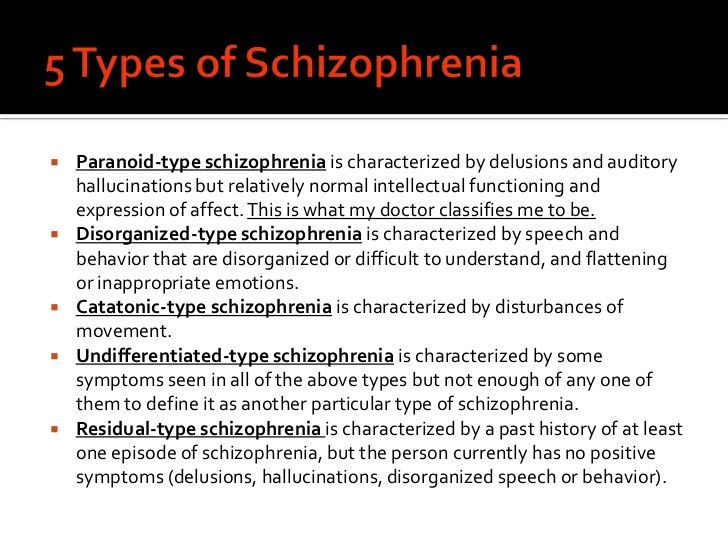
- Delusions. These are false beliefs that are not based in reality.
For example, you think that you're being harmed or harassed; certain gestures or comments are directed at you; you have exceptional ability or fame; another person is in love with you; or a major catastrophe is about to occur. Delusions occur in most people with schizophrenia.
- Hallucinations. These usually involve seeing or hearing things that don't exist. Yet for the person with schizophrenia, they have the full force and impact of a normal experience. Hallucinations can be in any of the senses, but hearing voices is the most common hallucination.
- Disorganized thinking (speech). Disorganized thinking is inferred from disorganized speech. Effective communication can be impaired, and answers to questions may be partially or completely unrelated. Rarely, speech may include putting together meaningless words that can't be understood, sometimes known as word salad.
- Extremely disorganized or abnormal motor behavior.
 This may show in a number of ways, from childlike silliness to unpredictable agitation. Behavior isn't focused on a goal, so it's hard to do tasks. Behavior can include resistance to instructions, inappropriate or bizarre posture, a complete lack of response, or useless and excessive movement.
This may show in a number of ways, from childlike silliness to unpredictable agitation. Behavior isn't focused on a goal, so it's hard to do tasks. Behavior can include resistance to instructions, inappropriate or bizarre posture, a complete lack of response, or useless and excessive movement. - Negative symptoms. This refers to reduced or lack of ability to function normally. For example, the person may neglect personal hygiene or appear to lack emotion (doesn't make eye contact, doesn't change facial expressions or speaks in a monotone). Also, the person may lose interest in everyday activities, socially withdraw or lack the ability to experience pleasure.
Symptoms can vary in type and severity over time, with periods of worsening and remission of symptoms. Some symptoms may always be present.
In men, schizophrenia symptoms typically start in the early to mid-20s. In women, symptoms typically begin in the late 20s. It's uncommon for children to be diagnosed with schizophrenia and rare for those older than age 45.
Symptoms in teenagers
Schizophrenia symptoms in teenagers are similar to those in adults, but the condition may be more difficult to recognize. This may be in part because some of the early symptoms of schizophrenia in teenagers are common for typical development during teen years, such as:
- Withdrawal from friends and family
- A drop in performance at school
- Trouble sleeping
- Irritability or depressed mood
- Lack of motivation
Also, recreational substance use, such as marijuana, methamphetamines or LSD, can sometimes cause similar signs and symptoms.
Compared with schizophrenia symptoms in adults, teens may be:
- Less likely to have delusions
- More likely to have visual hallucinations
When to see a doctor
People with schizophrenia often lack awareness that their difficulties stem from a mental disorder that requires medical attention. So it often falls to family or friends to get them help.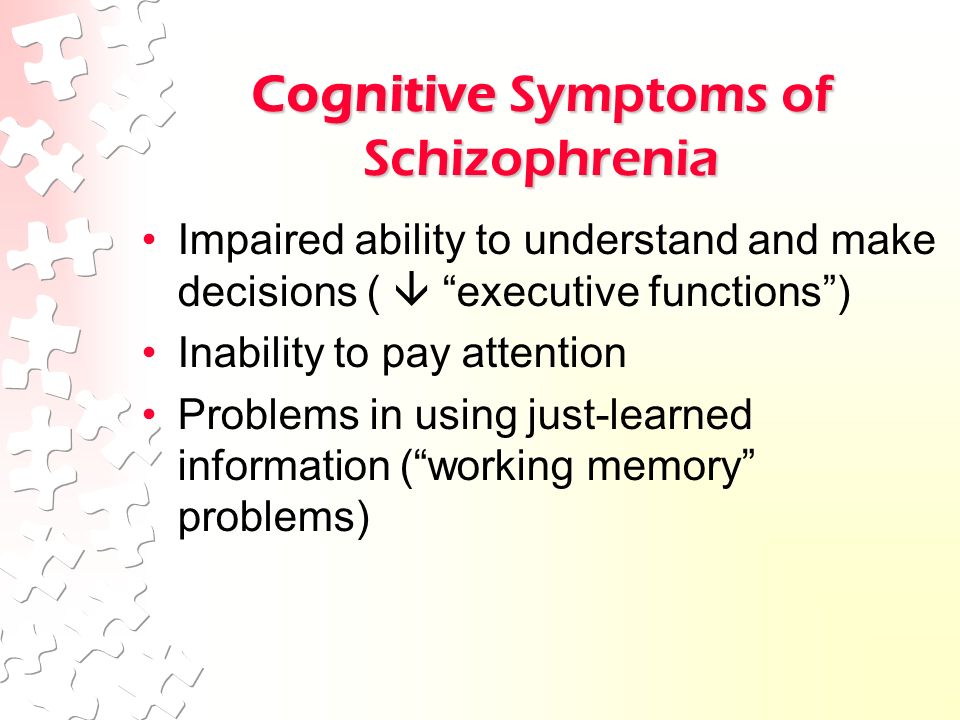
Helping someone who may have schizophrenia
If you think someone you know may have symptoms of schizophrenia, talk to him or her about your concerns. Although you can't force someone to seek professional help, you can offer encouragement and support and help your loved one find a qualified doctor or mental health professional.
If your loved one poses a danger to self or others or can't provide his or her own food, clothing, or shelter, you may need to call 911 or other emergency responders for help so that your loved one can be evaluated by a mental health professional.
In some cases, emergency hospitalization may be needed. Laws on involuntary commitment for mental health treatment vary by state. You can contact community mental health agencies or police departments in your area for details.
Suicidal thoughts and behavior
Suicidal thoughts and behavior are common among people with schizophrenia. If you have a loved one who is in danger of attempting suicide or has made a suicide attempt, make sure someone stays with that person.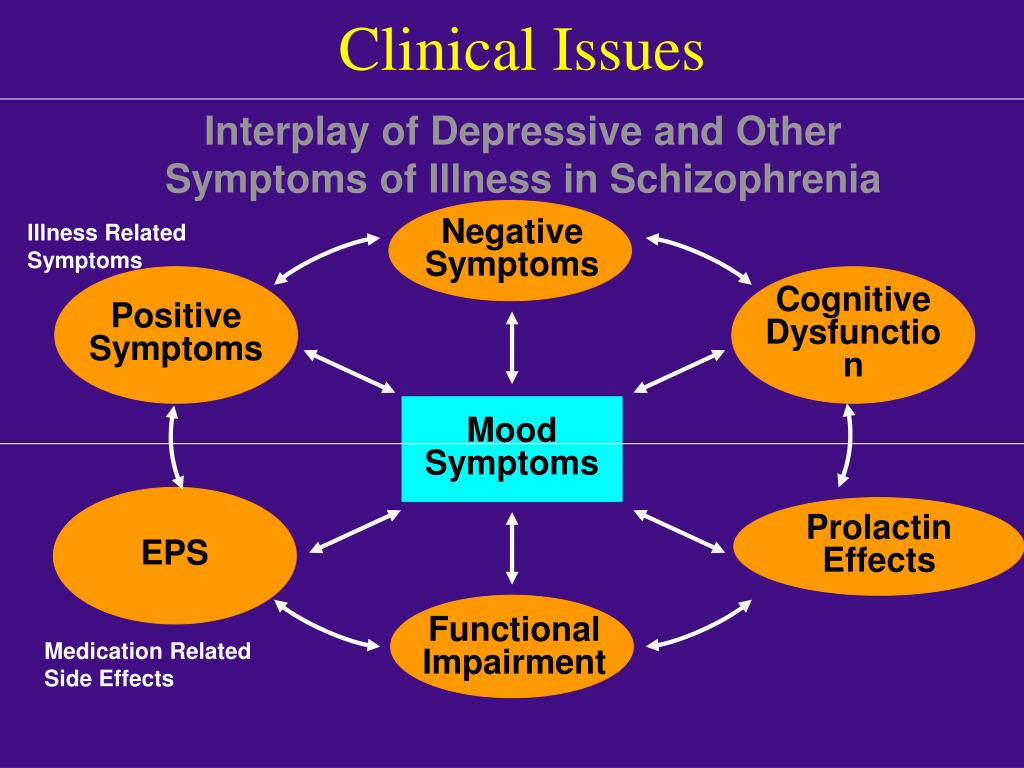 Call 911 or your local emergency number immediately. Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
Call 911 or your local emergency number immediately. Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
It's not known what causes schizophrenia, but researchers believe that a combination of genetics, brain chemistry and environment contributes to development of the disorder.
Problems with certain naturally occurring brain chemicals, including neurotransmitters called dopamine and glutamate, may contribute to schizophrenia. Neuroimaging studies show differences in the brain structure and central nervous system of people with schizophrenia. While researchers aren't certain about the significance of these changes, they indicate that schizophrenia is a brain disease.
Risk factors
Although the precise cause of schizophrenia isn't known, certain factors seem to increase the risk of developing or triggering schizophrenia, including:
- Having a family history of schizophrenia
- Some pregnancy and birth complications, such as malnutrition or exposure to toxins or viruses that may impact brain development
- Taking mind-altering (psychoactive or psychotropic) drugs during teen years and young adulthood
Complications
Left untreated, schizophrenia can result in severe problems that affect every area of life.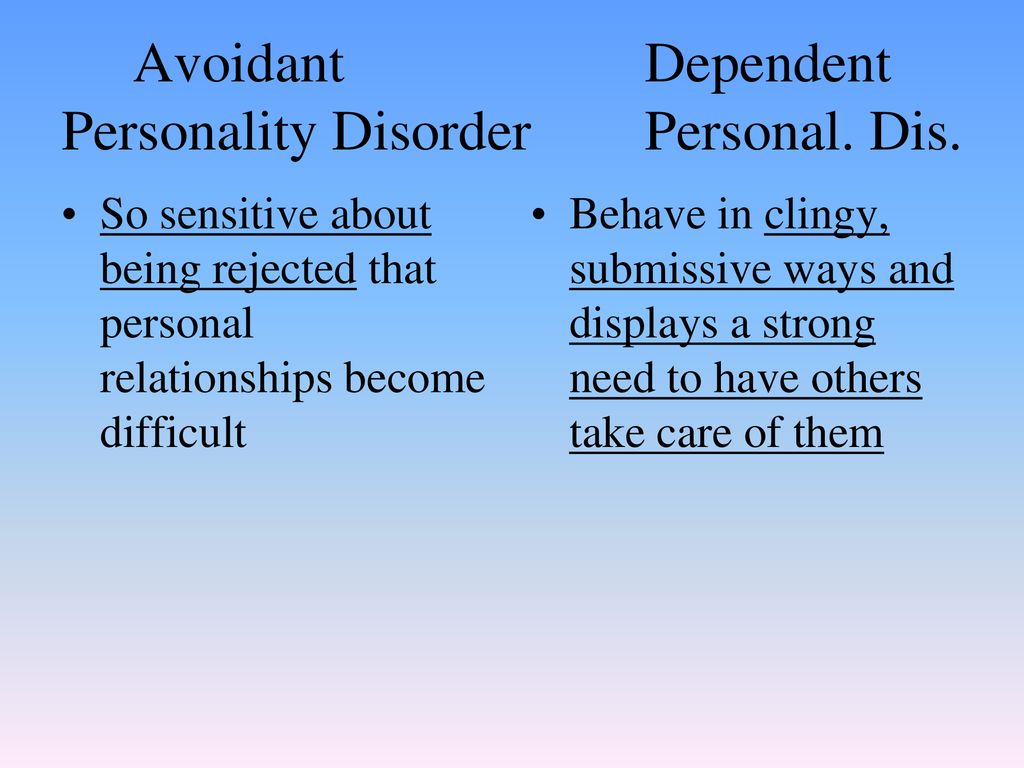 Complications that schizophrenia may cause or be associated with include:
Complications that schizophrenia may cause or be associated with include:
- Suicide, suicide attempts and thoughts of suicide
- Anxiety disorders and obsessive-compulsive disorder (OCD)
- Depression
- Abuse of alcohol or other drugs, including nicotine
- Inability to work or attend school
- Financial problems and homelessness
- Social isolation
- Health and medical problems
- Being victimized
- Aggressive behavior, although it's uncommon
Prevention
There's no sure way to prevent schizophrenia, but sticking with the treatment plan can help prevent relapses or worsening of symptoms. In addition, researchers hope that learning more about risk factors for schizophrenia may lead to earlier diagnosis and treatment.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
NIMH » Schizophrenia
Overview
Schizophrenia is a serious mental illness that affects how a person thinks, feels, and behaves.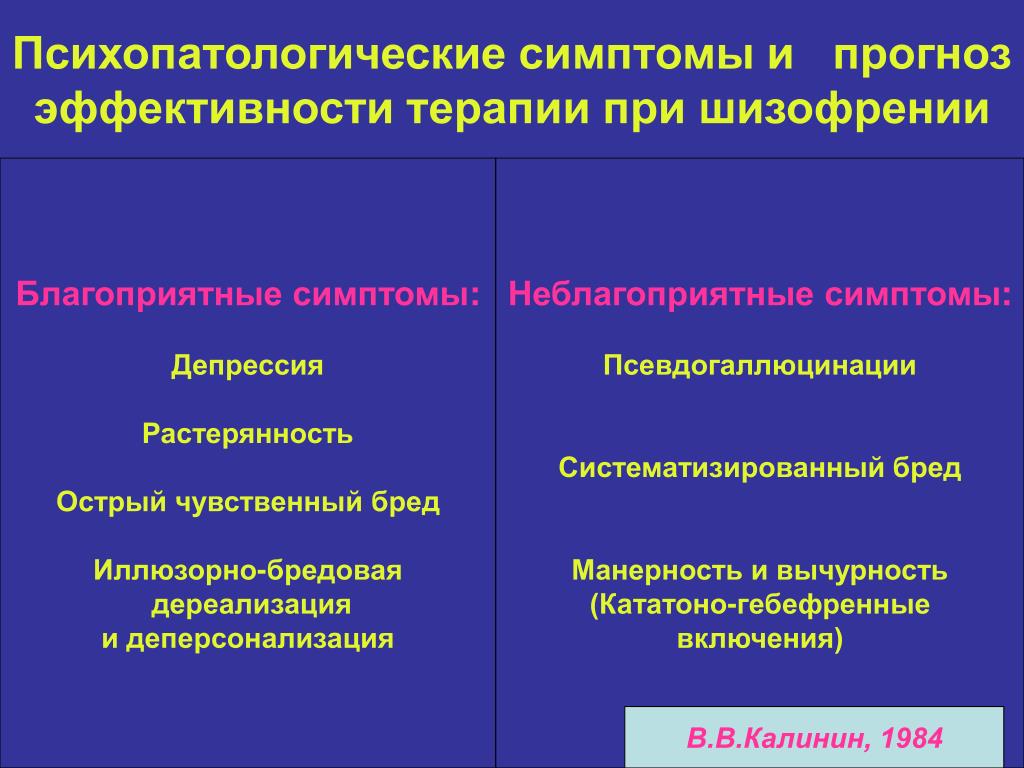 People with schizophrenia may seem like they have lost touch with reality, which can be distressing for them and for their family and friends. The symptoms of schizophrenia can make it difficult to participate in usual, everyday activities, but effective treatments are available. Many people who receive treatment can engage in school or work, achieve independence, and enjoy personal relationships.
People with schizophrenia may seem like they have lost touch with reality, which can be distressing for them and for their family and friends. The symptoms of schizophrenia can make it difficult to participate in usual, everyday activities, but effective treatments are available. Many people who receive treatment can engage in school or work, achieve independence, and enjoy personal relationships.
Onset and Symptoms
The Centers for Disease Control and Prevention (CDC) has recognized that having certain mental disorders, including depression and schizophrenia, can make people more likely to get severely ill from COVID-19. Learn more about getting help and finding a health care provider on NIMH's Help for Mental Illnesses webpage.
It’s important to recognize the symptoms of schizophrenia and seek help as early as possible. People with schizophrenia are usually diagnosed between the ages of 16 and 30, after the first episode of psychosis. Starting treatment as soon as possible following the first episode of psychosis is an important step toward recovery.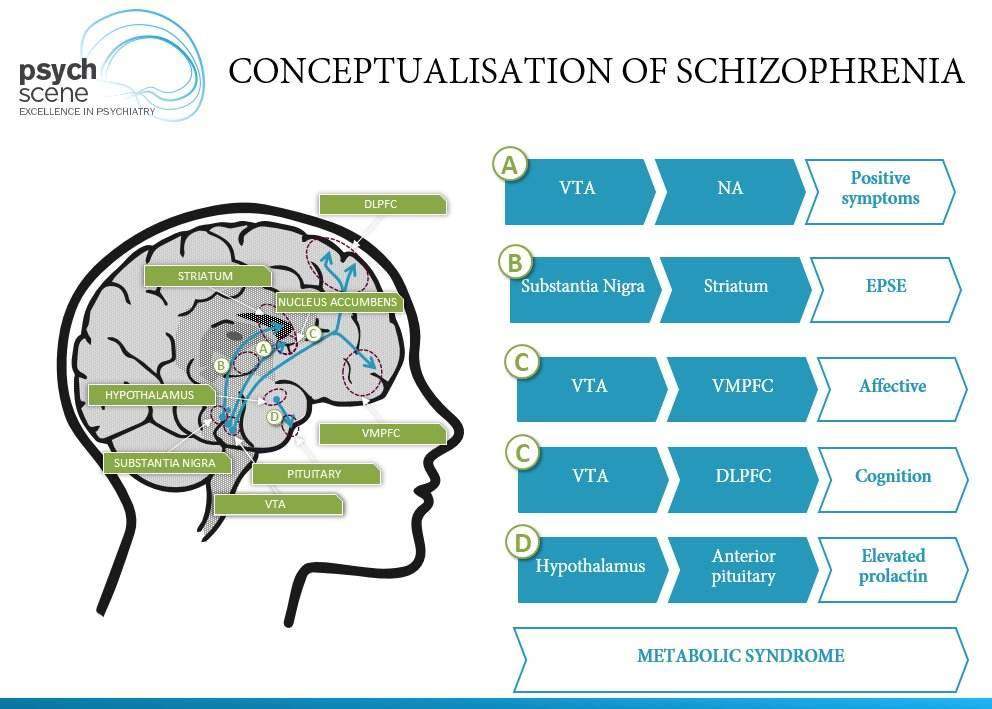 However, research shows that gradual changes in thinking, mood, and social functioning often appear before the first episode of psychosis. Schizophrenia is rare in younger children.
However, research shows that gradual changes in thinking, mood, and social functioning often appear before the first episode of psychosis. Schizophrenia is rare in younger children.
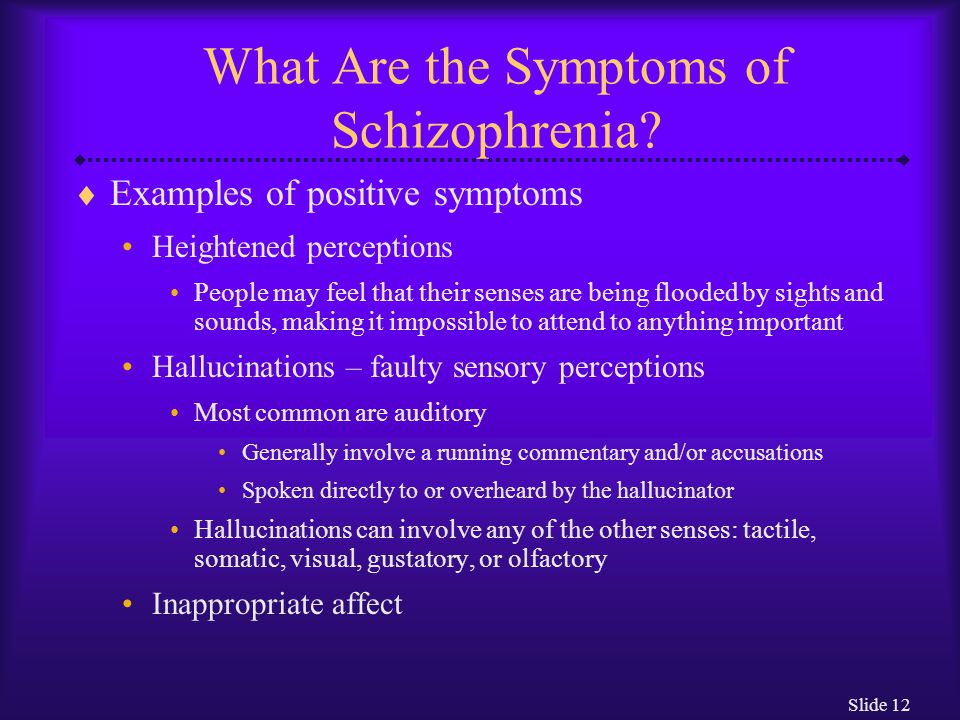
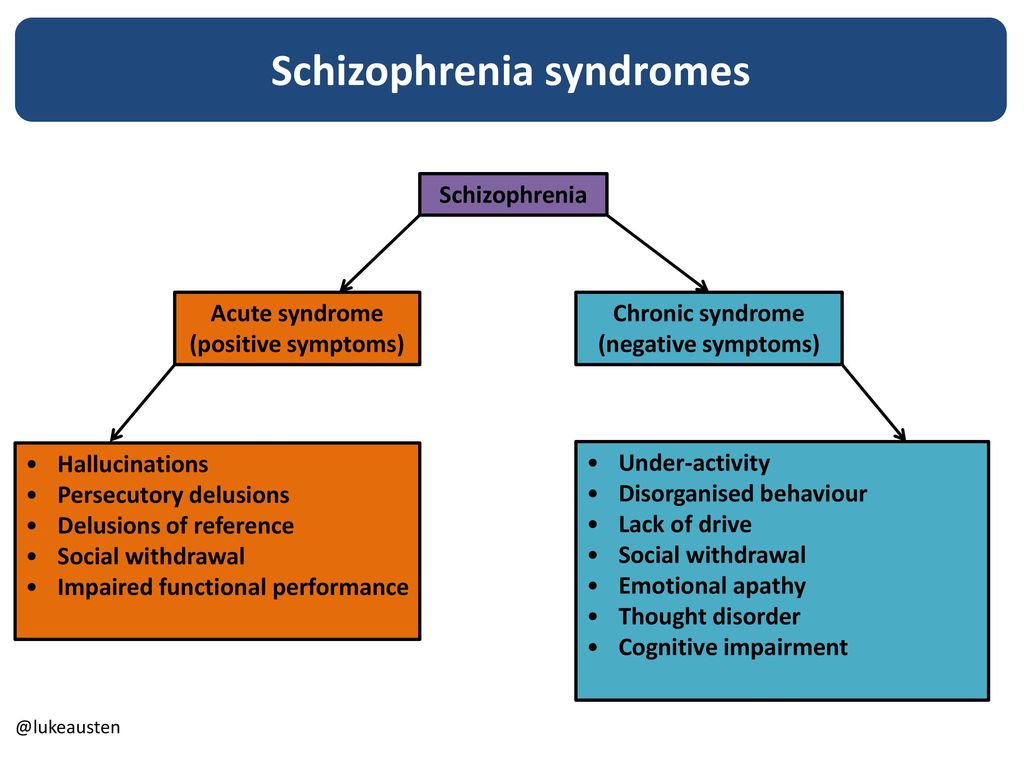
Schizophrenia symptoms can differ from person to person, but they generally fall into three main categories: psychotic, negative, and cognitive.
Psychotic symptoms include changes in the way a person thinks, acts, and experiences the world. People with psychotic symptoms may lose a shared sense of reality with others and experience the world in a distorted way. For some people, these symptoms come and go. For others, the symptoms become stable over time. Psychotic symptoms include:
- Hallucinations: When a person sees, hears, smells, tastes, or feels things that are not actually there. Hearing voices is common for people with schizophrenia. People who hear voices may hear them for a long time before family or friends notice a problem.
- Delusions: When a person has strong beliefs that are not true and may seem irrational to others.
 For example, individuals experiencing delusions may believe that people on the radio and television are sending special messages that require a certain response, or they may believe that they are in danger or that others are trying to hurt them.
For example, individuals experiencing delusions may believe that people on the radio and television are sending special messages that require a certain response, or they may believe that they are in danger or that others are trying to hurt them. - Thought disorder: When a person has ways of thinking that are unusual or illogical. People with thought disorder may have trouble organizing their thoughts and speech. Sometimes a person will stop talking in the middle of a thought, jump from topic to topic, or make up words that have no meaning.
- Movement disorder: When a person exhibits abnormal body movements. People with movement disorder may repeat certain motions over and over.
Negative symptoms include loss of motivation, loss of interest or enjoyment in daily activities, withdrawal from social life, difficulty showing emotions, and difficulty functioning normally. Negative symptoms include:
- Having trouble planning and sticking with activities, such as grocery shopping
- Having trouble anticipating and feeling pleasure in everyday life
- Talking in a dull voice and showing limited facial expression
- Avoiding social interaction or interacting in socially awkward ways
- Having very low energy and spending a lot of time in passive activities.
 In extreme cases, a person might stop moving or talking for a while, which is a rare condition called catatonia.
In extreme cases, a person might stop moving or talking for a while, which is a rare condition called catatonia.
These symptoms are sometimes mistaken for symptoms of depression or other mental illnesses.
Cognitive symptoms include problems in attention, concentration, and memory. These symptoms can make it hard to follow a conversation, learn new things, or remember appointments. A person’s level of cognitive functioning is one of the best predictors of their day-to-day functioning. Cognitive functioning is evaluated using specific tests. Cognitive symptoms include:
- Having trouble processing information to make decisions
- Having trouble using information immediately after learning it
- Having trouble focusing or paying attention
Risk of Violence
Most people with schizophrenia are not violent. Overall, people with schizophrenia are more likely than those without the illness to be harmed by others.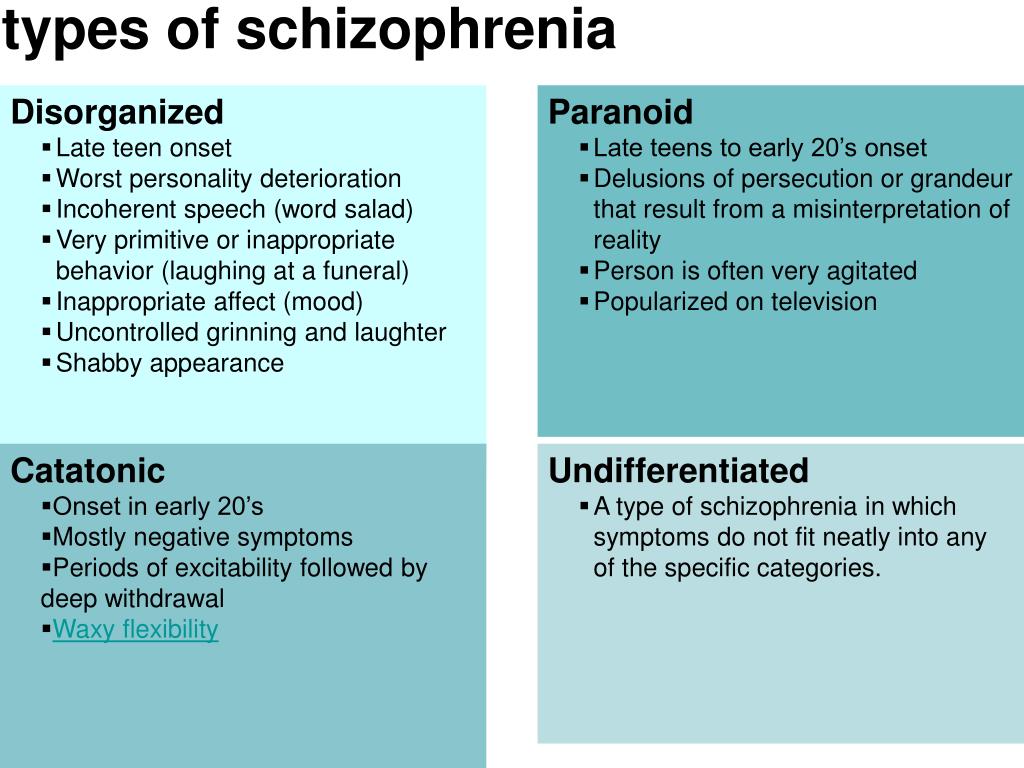 For people with schizophrenia, the risk of self-harm and of violence to others is greatest when the illness is untreated. It is important to help people who are showing symptoms to get treatment as quickly as possible.
For people with schizophrenia, the risk of self-harm and of violence to others is greatest when the illness is untreated. It is important to help people who are showing symptoms to get treatment as quickly as possible.
Schizophrenia vs. Dissociative Identity Disorder
Although some of the signs may seem similar on the surface, schizophrenia is not dissociative identity disorder (which used to be called multiple personality disorder or split personality). People with dissociative identity disorder have two or more distinct identities that are present and that alternately take control of them.
Risk Factors
Several factors may contribute to a person’s risk of developing schizophrenia, including:
Genetics: Schizophrenia sometimes runs in families. However, just because one family member has schizophrenia, it does not mean that other members of the family also will have it. Studies suggest that many different genes may increase a person’s chances of developing schizophrenia, but that no single gene causes the disorder by itself.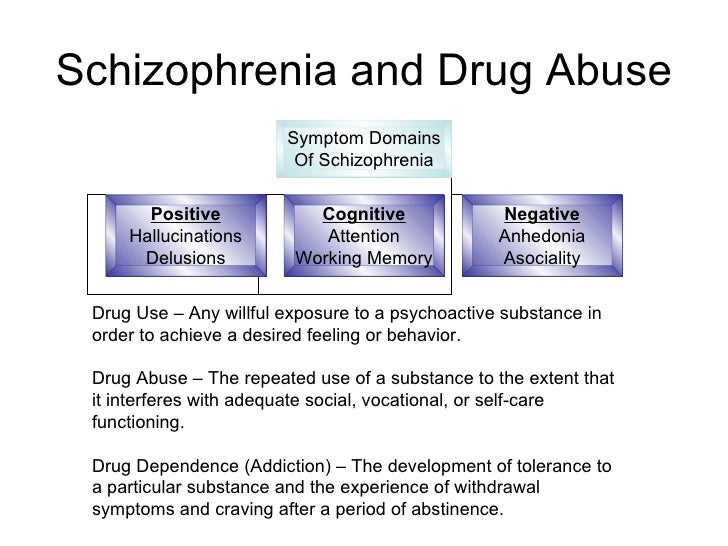
Environment: Research suggests that a combination of genetic factors and aspects of a person’s environment and life experiences may play a role in the development of schizophrenia. These environmental factors that may include living in poverty, stressful or dangerous surroundings, and exposure to viruses or nutritional problems before birth.
Brain structure and function: Research shows that people with schizophrenia may be more likely to have differences in the size of certain brain areas and in connections between brain areas. Some of these brain differences may develop before birth. Researchers are working to better understand how brain structure and function may relate to schizophrenia.
Treatments and Therapies
Current treatments for schizophrenia focus on helping individuals manage their symptoms, improve day-to-day functioning, and achieve personal life goals, such as completing education, pursuing a career, and having fulfilling relationships.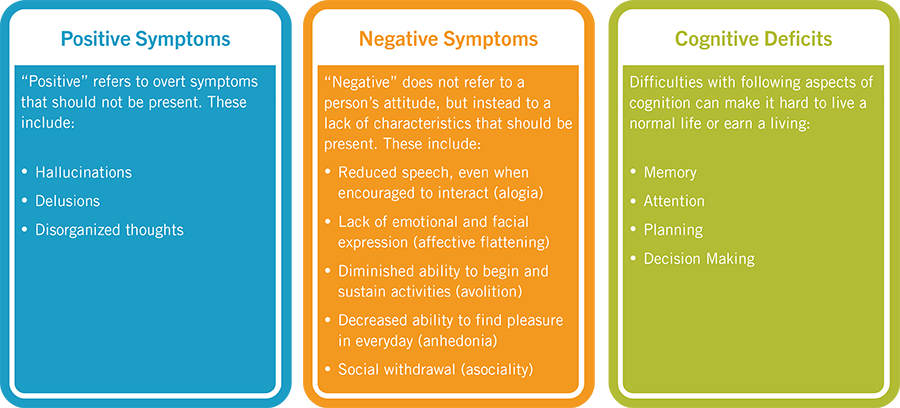
Antipsychotic Medications
Antipsychotic medications can help make psychotic symptoms less intense and less frequent. These medications are usually taken every day in a pill or liquid forms. Some antipsychotic medications are given as injections once or twice a month.
If a person’s symptoms do not improve with usual antipsychotic medications, they may be prescribed clozapine. People who take clozapine must have regular blood tests to check for a potentially dangerous side effect that occurs in 1-2% of patients.
People respond to antipsychotic medications in different ways. It is important to report any side effects to a health care provider. Many people taking antipsychotic medications experience side effects such as weight gain, dry mouth, restlessness, and drowsiness when they start taking these medications. Some of these side effects may go away over time, while others may last.
Shared decision making between doctors and patients is the recommended strategy for determining the best type of medication or medication combination and the right dose.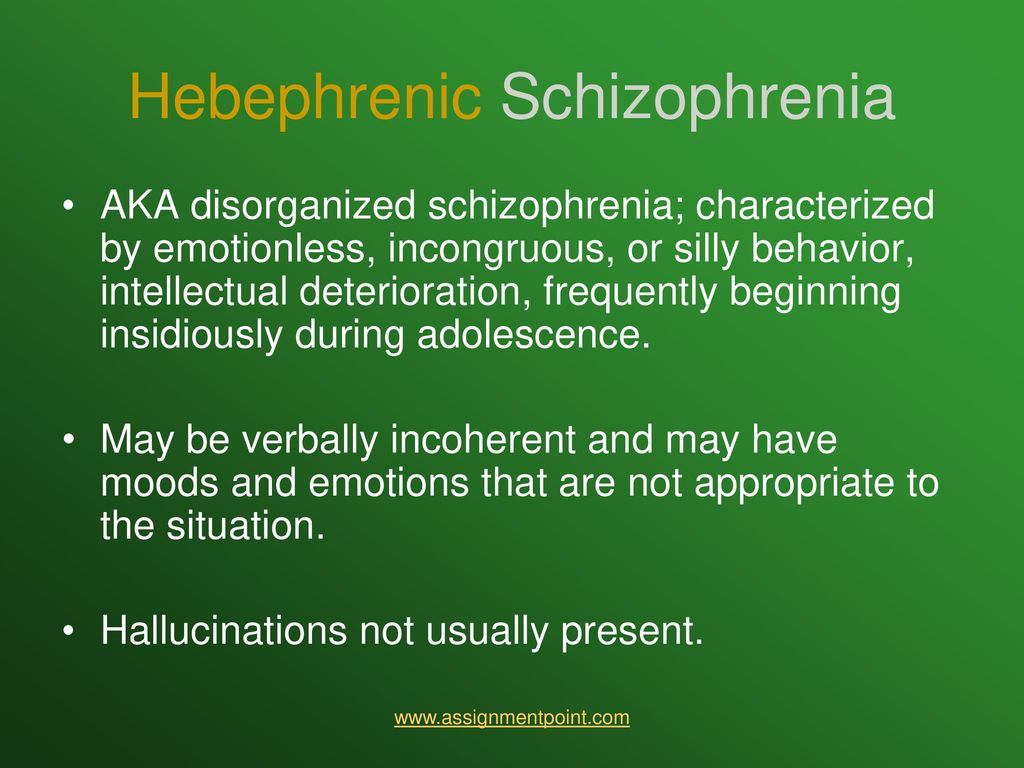 You can find the latest information on warnings, patient medication guides, or newly approved medications on the U.S. Food and Drug Administration (FDA) website.
You can find the latest information on warnings, patient medication guides, or newly approved medications on the U.S. Food and Drug Administration (FDA) website.
Psychosocial Treatments
Psychosocial treatments help people find solutions to everyday challenges and manage symptoms while attending school, working, and forming relationships. These treatments are often used together with antipsychotic medication. People who participate in regular psychosocial treatment are less likely to have symptoms reoccur or to be hospitalized.
Examples of this kind of treatment include cognitive behavioral therapy, behavioral skills training, supported employment, and cognitive remediation interventions.
You can find information about psychosocial treatments on the National Institute of Mental Health (NIMH) psychotherapies webpage.
Family Education and Support
Educational programs can help family and friends learn about symptoms of schizophrenia, treatment options, and strategies for helping loved ones with the illness.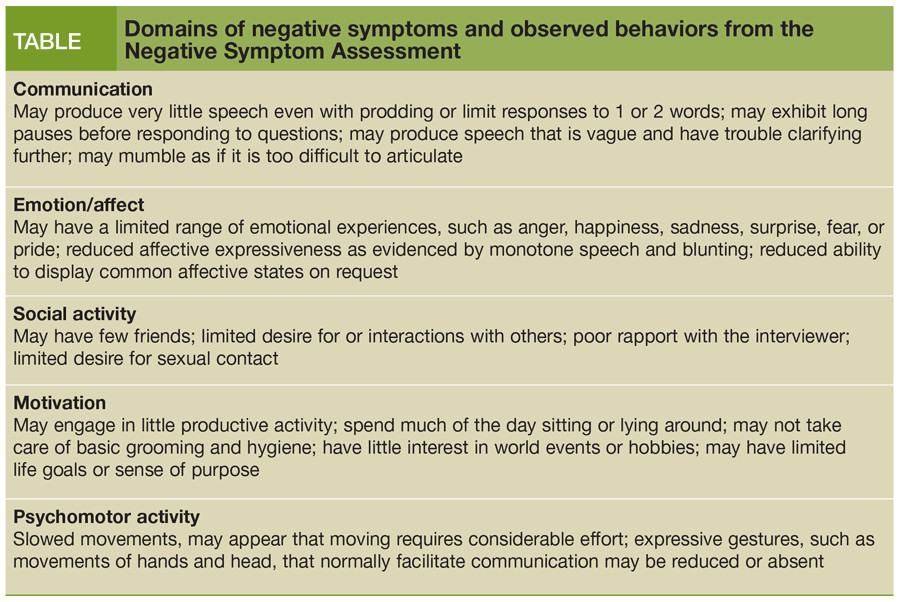 These programs can help friends and family manage their distress, boost their own coping skills, and strengthen their ability to provide support. For more information about family-based services in your area, you can visit the family education and support groups page on the National Alliance on Mental Illness website.
These programs can help friends and family manage their distress, boost their own coping skills, and strengthen their ability to provide support. For more information about family-based services in your area, you can visit the family education and support groups page on the National Alliance on Mental Illness website.
Coordinated Specialty Care
Coordinated specialty care (CSC) programs are recovery-focused programs for people with first episode psychosis, an early stage of schizophrenia. Health professionals and specialists work together as a team to provide CSC, which includes psychotherapy, medication, case management, employment and education support, and family education and support. The treatment team works collaboratively with the individual to make treatment decisions, involving family members as much as possible.
Compared with typical care, CSC is more effective at reducing symptoms, improving quality of life, and increasing involvement in work or school. Check here for more information about CSC programs.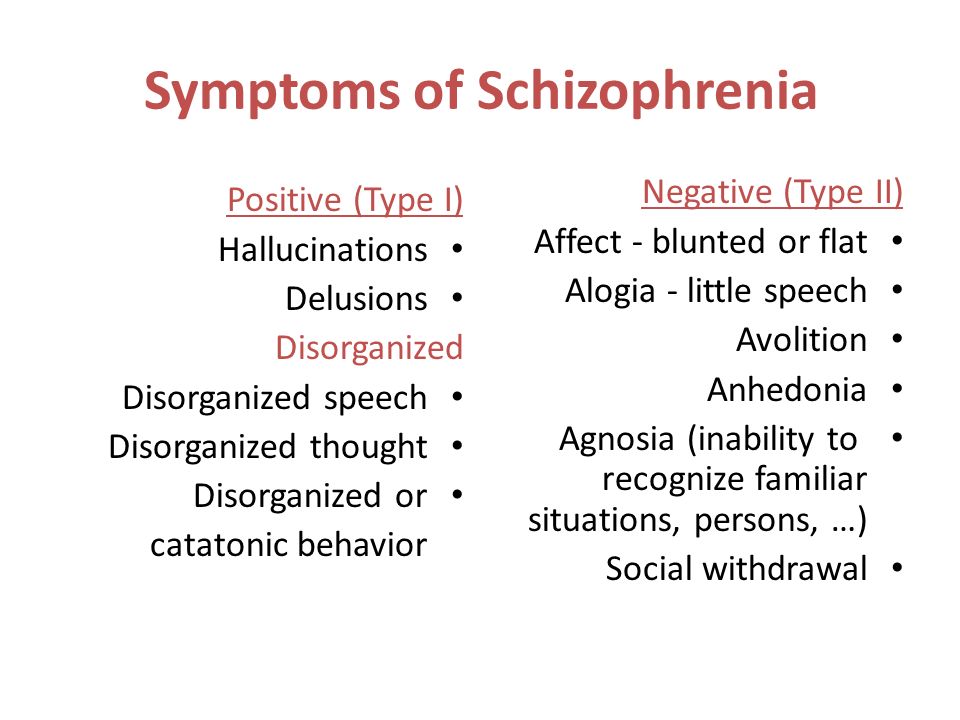
Assertive Community Treatment
Assertive Community Treatment (ACT) is designed especially for individuals with schizophrenia who are likely to experience multiple hospitalizations or homelessness. ACT is usually delivered by a team of health professionals who work together to provide care to patients in the community. Check here for more information about ACT programs.
Treatment for Drug and Alcohol Misuse
It is common for people with schizophrenia to have problems with drugs and alcohol. A treatment program that includes treatment for both schizophrenia and substance use is important for recovery because substance use can interfere with treatment for schizophrenia.
How can I help a friend or relative with schizophrenia?
It can be difficult to know how to help someone who is experiencing psychosis.
Here are some things you can do:
- Help them get treatment and encourage them to stay in treatment.
- Remember that their beliefs or hallucinations seem very real to them.
- Be respectful, supportive, and kind without tolerating dangerous or inappropriate behavior.
- Look for support groups and family education programs, such as those offered by the National Alliance on Mental Illness.
Some symptoms require immediate emergency care. If your loved one is thinking about attempting suicide or otherwise harming themselves or others, seek help right away:
- Call 911 for emergency services or go to the nearest emergency room.
- Call the National Suicide Prevention Lifeline (Lifeline) at 1-800-273-TALK (8255) or text the Crisis Text Line (text HELLO to 741741).
Finding Help
If you’re not sure where to get help, your health care provider is a good place to start. Your health care provider can refer you to a qualified mental health professional, such as a psychiatrist or psychologist who has experience treating schizophrenia. You can learn more about getting help on NIMH's Help for Mental Illness webpage.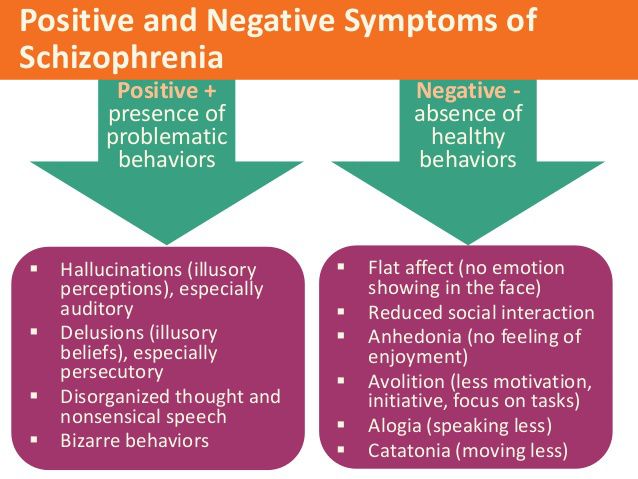
The Substance Abuse and Mental Health Services Administration (SAMHSA) provides the Behavioral Health Treatment Services Locator, an online tool to help you find mental health services in your area. You can find information about treatment facilities that offer coordinated specialty care by using SAMHSA’s Early Serious Mental Illness Treatment Locator.
For tips on talking with your health care provider about your mental health and getting the most out of your visit, read NIMH’s fact sheet, Taking Control of Your Mental Health: Tips for Talking With Your Health Care Provider.
Join a Study
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions. The goal of clinical trials is to determine if a new test or treatment works and is safe. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.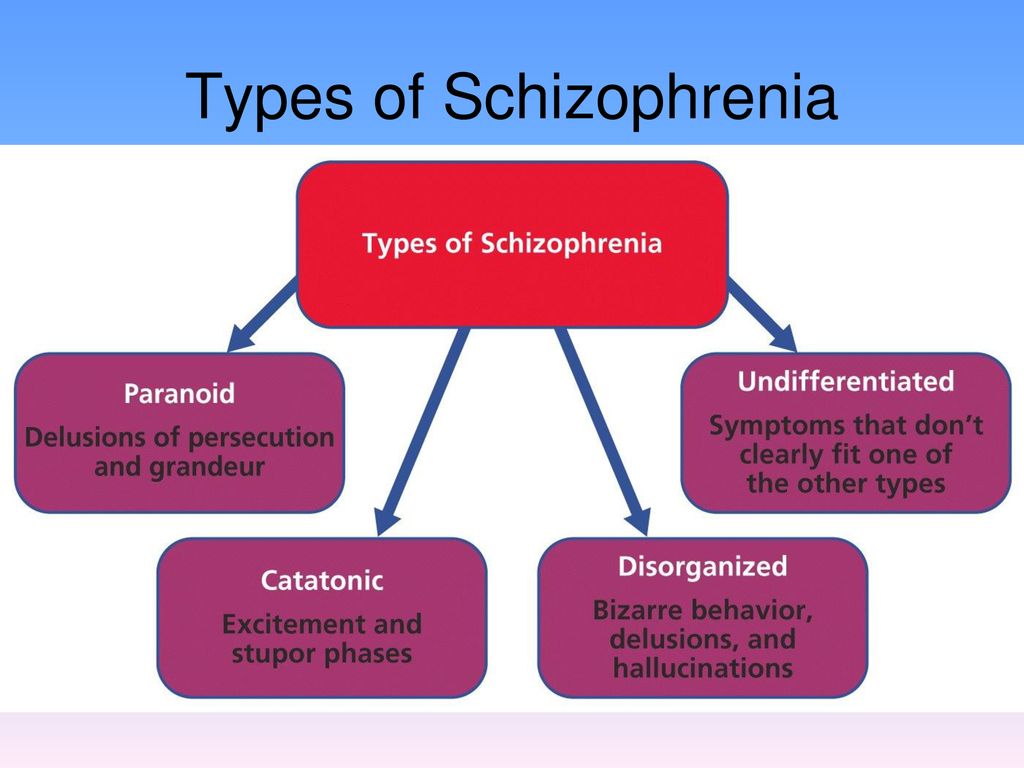
Researchers at NIMH and around the country conduct many studies with patients and healthy volunteers. We have new and better treatment options today because of what clinical trials uncovered years ago. Be part of tomorrow’s medical breakthroughs. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you.
To learn more or find a study, visit:
- NIMH’s Clinical Trials webpage: Information about participating in clinical trials
- Clinicaltrials.gov: Current Studies on Schizophrenia: List of clinical trials funded by the National Institutes of Health (NIH) being conducted across the country
- Join a Study: Schizophrenia: List of studies being conducted on the NIH Campus in Bethesda, MD
Learn More
Free Brochures and Shareable Resources
- Schizophrenia: A brief brochure on schizophrenia that offers basic information on signs and symptoms, treatment, and finding help.
 Also available en español.
Also available en español. - Understanding Psychosis: A fact sheet that presents information on psychosis, including causes, signs and symptoms, treatment, and resources for help. Also available en español.
- Shareable Resources on Schizophrenia: Help support schizophrenia awareness and education in your community. Use these digital resources, including graphics and messages, to spread the word about schizophrenia.
Research and Statistics
- Accelerating Medicines Partnership® Program - Schizophrenia (AMP® SCZ): This AMP public-private collaborative effort aims to promote the development of effective, targeted treatments for those at risk of developing schizophrenia. More information about the program is also available on the AMP SCZ website.
- Early Psychosis Intervention Network (EPINET): This broad research initiative aims to develop models for the effective delivery of coordinated specialty care (CSC) services for early psychosis.
- Journal Articles: This webpage provides information on references and abstracts from MEDLINE/PubMed (National Library of Medicine).
- Psychotic Disorders Research Program: This program supports research into the origins, onset, course, and outcome of schizophrenia spectrum disorders and other psychotic illnesses.
- Recovery After an Initial Schizophrenia Episode (RAISE): The NIMH RAISE research initiative included two studies examining different aspects of coordinated specialty care treatments for people who were experiencing early psychosis.
- Schizophrenia Statistics: This webpage provides information on the best statistics currently available on the prevalence and treatment of schizophrenia in the U.S.
Last Reviewed: May 2022
Unless otherwise specified, NIMH information and publications are in the public domain and available for use free of charge.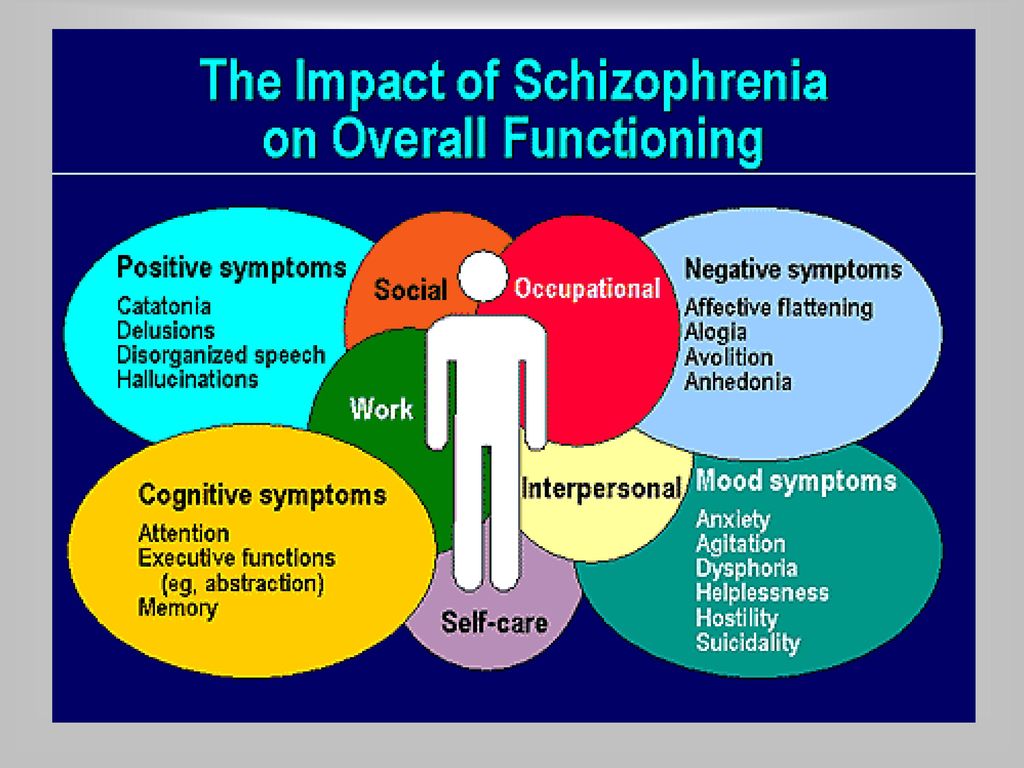 Citation of NIMH is appreciated. Please see our Citing NIMH Information and Publications page for more information.
Citation of NIMH is appreciated. Please see our Citing NIMH Information and Publications page for more information.
PKB No. 5 - Schizophrenia
Moscow State Budgetary Institution of Healthcare
Psychiatric Clinical Hospital No. 5 of the Moscow City Health Department
+7 (495) 445-55-25, +7 (496) 724-33 -33
Moscow region, Chekhov, s. Troitskoe, 5
Medical Tourism
Site search
Schizophrenia is a chronic mental illness, which is characterized by a violation of the unity of thought processes, with a relatively intact intellect, which is combined with significant emotional impoverishment and a decrease in will. Often hallucinatory and delusional disorders join.
The term "schizophrenia" itself is made up of two Greek words - "schizo" - splitting and "freni" - mind reason.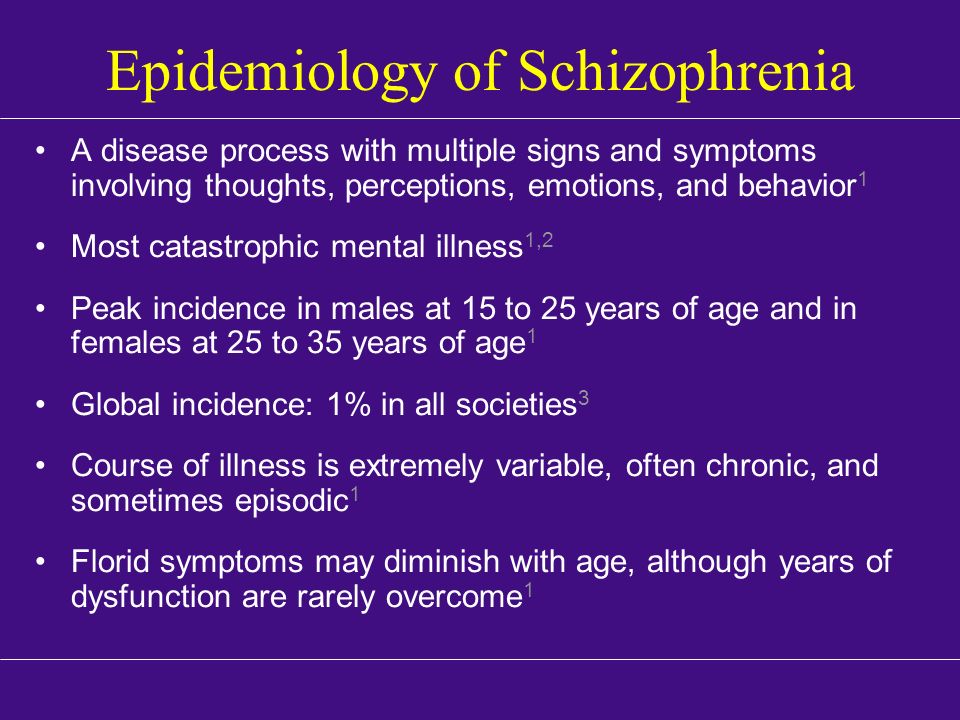
This term was first used by the Swiss psychiatrist Eigen Bleuler in 1908y. Schizophrenia, of course, existed before, but only by the beginning of the 20th century did the idea of it as a special kind of psychosis mature.
In the mass consciousness there is an unreasonable identification of schizophrenia with a "split personality" - that is, in fact, with a very rare mental disorder in which different "I"s are alternately activated in one person.
Schizophrenia, unfortunately, is quite common. Its prevalence among the Russian population is 35 per 10,000 people, with no significant difference between the sexes. Thus, in Russia there are at least half a million patients with this serious pathology.
Schizophrenia refers to endogenous mental illness, which means that it is an internal breakdown of the psyche. It cannot be caused by any factors acting on the brain from the outside (trauma, intoxication, severe stress). Of course, these factors can affect the rate of development of schizophrenia, but not its occurrence. However, the mechanism of development of the schizophrenic process has not yet been established with certainty. There are several hypotheses about this. Thus, there is evidence of a relationship between schizophrenia and a violation of the distribution of dopamine in the central nervous system.
However, the mechanism of development of the schizophrenic process has not yet been established with certainty. There are several hypotheses about this. Thus, there is evidence of a relationship between schizophrenia and a violation of the distribution of dopamine in the central nervous system.
The role of heredity is very great. So, if one of the twins fell ill with schizophrenia, then the risk of getting sick for the other twin is 17% in a fraternal couple and 48% in an identical one. However, it is believed that in half of the cases of schizophrenia arises from a random mutation, that is, on the basis of genetic changes that were absent in the parents and appeared after conception.
Symptoms can develop at any age (possibly even in utero), but usually its onset is timed to coincide with the third pubertal crisis, that is, by the age of 12-18 years or several years later (up to about 30 years).
Most often, the disease begins with negative symptoms associated with the loss of normal functioning - a person changes in character for no apparent reason, becomes closed, fenced off, loses social contacts, emotional warmth in relation to relatives disappears.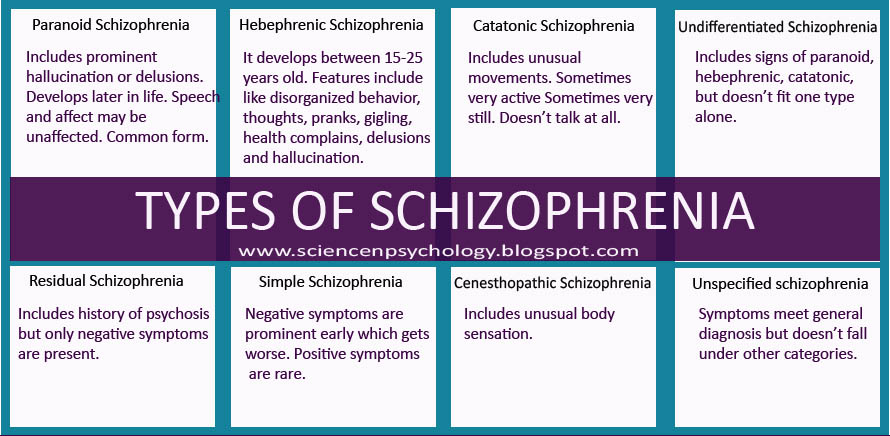 Former interests disappear, school or university performance drops sharply, or official duties are not fulfilled. Thus, from the very beginning of clinical manifestations there is a very high risk of disability. In the most unfavorable variant, which is designated as simple schizophrenia, the patient can lie for days on end, staring at the ceiling, and with a clear mind and normal physical strength, he is not able to simply serve himself. Even with more favorable options, thinking disorders increase, which are expressed in the influx of thoughts or in the feeling that there are no thoughts at all. Reasoning becomes unproductive, unfocused, an ambivalent attitude to life phenomena (ambivalence) is formed. Speech is distinguished by ornateness, sometimes with neologisms that the patient himself comes up with. During the conversation, there are distractions from his topic (sliding), and not to specific details and circumstances, but to the “bad” attitude of certain characters towards the patient, or to global philosophical topics.
Former interests disappear, school or university performance drops sharply, or official duties are not fulfilled. Thus, from the very beginning of clinical manifestations there is a very high risk of disability. In the most unfavorable variant, which is designated as simple schizophrenia, the patient can lie for days on end, staring at the ceiling, and with a clear mind and normal physical strength, he is not able to simply serve himself. Even with more favorable options, thinking disorders increase, which are expressed in the influx of thoughts or in the feeling that there are no thoughts at all. Reasoning becomes unproductive, unfocused, an ambivalent attitude to life phenomena (ambivalence) is formed. Speech is distinguished by ornateness, sometimes with neologisms that the patient himself comes up with. During the conversation, there are distractions from his topic (sliding), and not to specific details and circumstances, but to the “bad” attitude of certain characters towards the patient, or to global philosophical topics.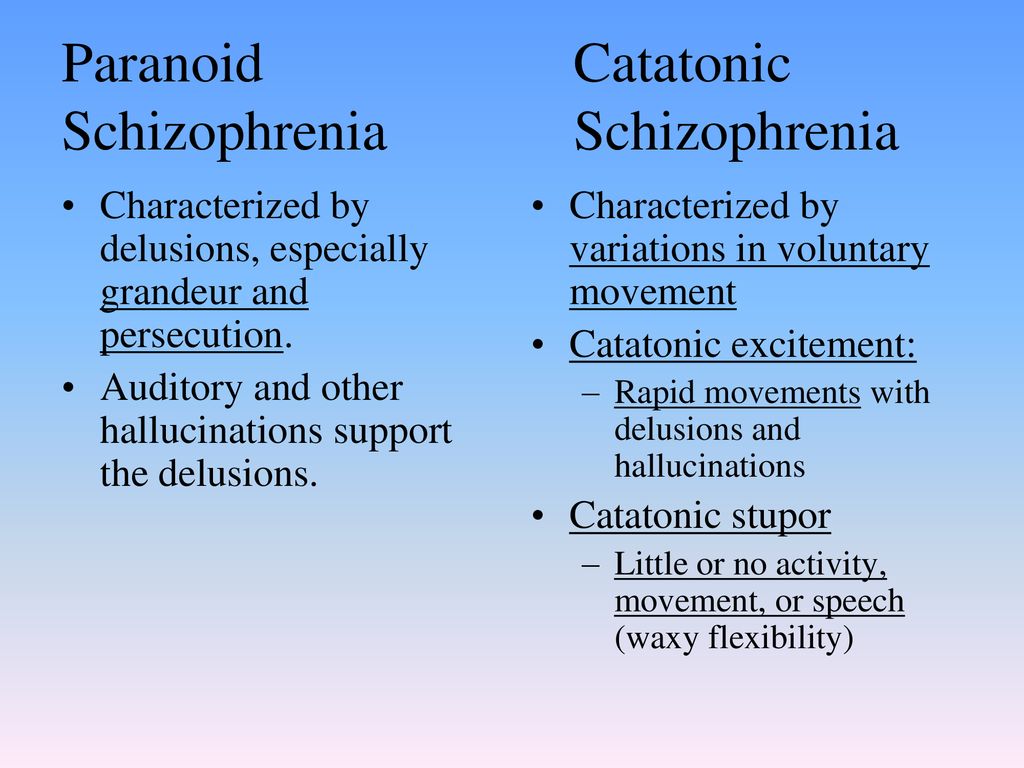 People with schizophrenia tend to be somewhat cynical about many aspects of their environment.
People with schizophrenia tend to be somewhat cynical about many aspects of their environment.
Patients have a painful feeling that everything around is somehow changed, devoid of naturalness, harmony (- derealization), the same feelings can arise in relation to their personality (- depersonalization). With depersonalization, the consciousness (but not the personality!) seems to split in two: one part of it looks at what is happening from the side, and the other is horrified by the realization of the loss of control over oneself.
One's own thoughts and ideas begin to be perceived as alien. According to modern views, this is why schizophrenia has verbal hallucinations (“voices”), and it is not surprising that the sound of “voices” inside the head is typical for this disease. For the same reason, it seems to the patient that someone controls him from the outside, up to the control of movements and the work of internal organs. Visions are less common.
Such a growing wave of unusual sensations is very painful.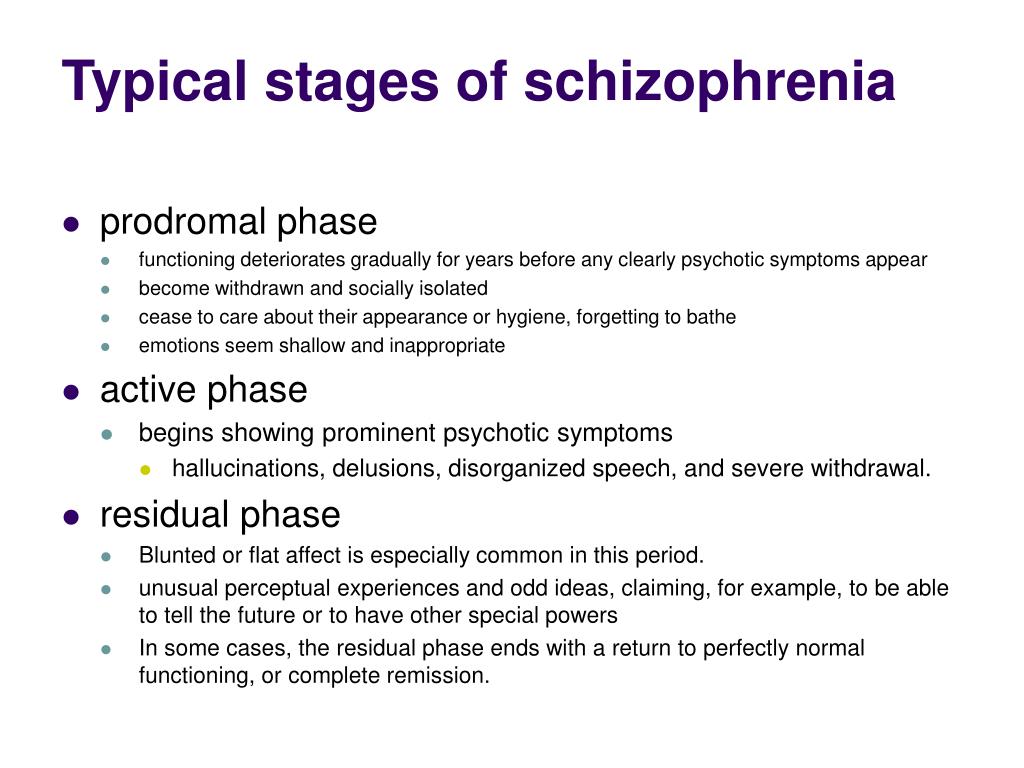 In many cases, internal tension is somewhat relieved by the formation of delusional ideas (quickly - like an insight - the crystallization of delirium occurs). It suddenly becomes “clear” to the patient that what is happening to him is, for example, the “intrigues” of some “organization”, which, with the help of modern equipment, “influences” him from the outside (delusions of persecution, influence). There is also delusions of jealousy, damage. It is clear that the plot of experiences is influenced by the level of development of society, including the plots of popular works of literature and cinema.
In many cases, internal tension is somewhat relieved by the formation of delusional ideas (quickly - like an insight - the crystallization of delirium occurs). It suddenly becomes “clear” to the patient that what is happening to him is, for example, the “intrigues” of some “organization”, which, with the help of modern equipment, “influences” him from the outside (delusions of persecution, influence). There is also delusions of jealousy, damage. It is clear that the plot of experiences is influenced by the level of development of society, including the plots of popular works of literature and cinema.
This whole clinical picture often develops acutely, in the form of an attack that lasts from several days to several months, and then may recur. Attack-like forms of schizophrenia are more favorable, in terms of prognosis, than continuous ones. The intervals between attacks are very long (sometimes - tens of years), and between them the person looks almost the same as before, before the illness.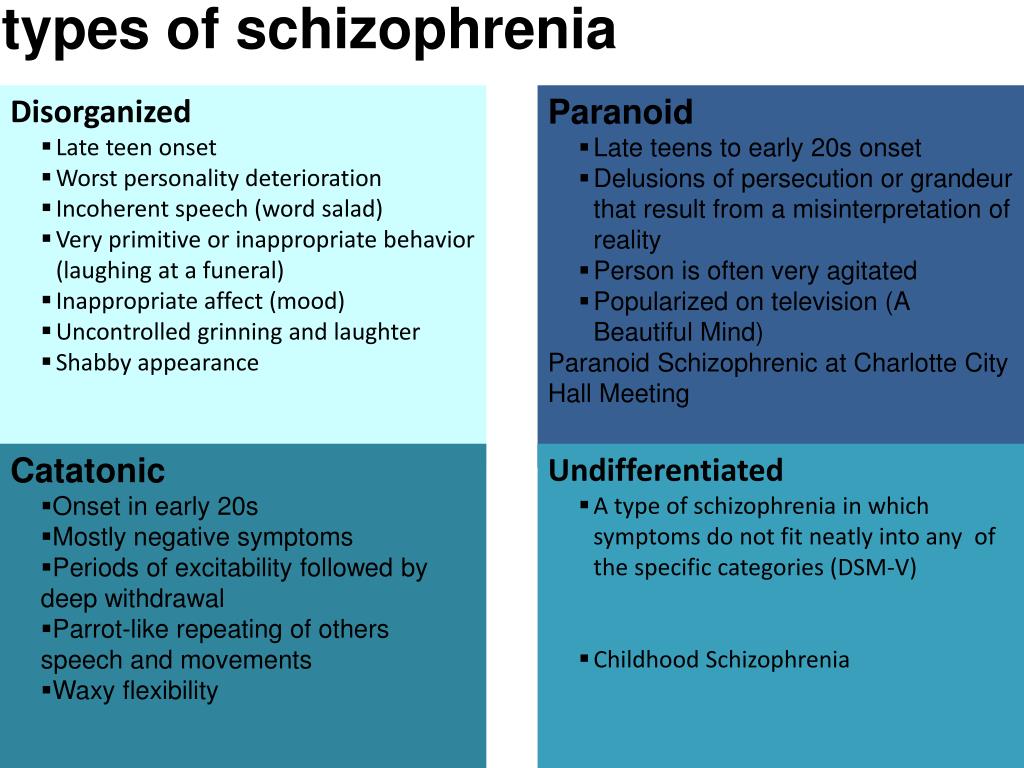 But this is rather an exception. Much more often, exacerbations of symptoms are repeated annually or several times a year, and after each new attack, it turns out that the will has become even weaker and emotions have faded even more. Gradually, over many years, hallucinatory experiences become less relevant. Parallel, but also very slowly, delirium is falling apart as a system of pseudo-logical conclusions - separate fragments of delirium remain. As a result, a state of defect develops, which resembles simple schizophrenia.
But this is rather an exception. Much more often, exacerbations of symptoms are repeated annually or several times a year, and after each new attack, it turns out that the will has become even weaker and emotions have faded even more. Gradually, over many years, hallucinatory experiences become less relevant. Parallel, but also very slowly, delirium is falling apart as a system of pseudo-logical conclusions - separate fragments of delirium remain. As a result, a state of defect develops, which resembles simple schizophrenia.
Patients either do not recognize themselves as ill or have conflicting thoughts about it. As a rule, they negatively meet the persuasion of relatives about the need to contact a psychiatrist. There are attempts to alleviate their condition with alcohol and drugs, which only complicates the clinical picture and leads to further social maladaptation.
Under the influence of orders "voices" and against the background of delusional experiences, the risk of socially dangerous actions of patients increases. For example, cases of attacks on imaginary "persecutors" are known. But much more often, patients with endogenous mental pathology commit OOD through other mechanisms, including when their behavior is influenced by alcohol or drug intoxication, which is superimposed on negative symptoms.
For example, cases of attacks on imaginary "persecutors" are known. But much more often, patients with endogenous mental pathology commit OOD through other mechanisms, including when their behavior is influenced by alcohol or drug intoxication, which is superimposed on negative symptoms.
Schizophrenia is the most common disease among patients in the Clinical Hospital No. 5 in Moscow.
Common diagnosis: Paranoid schizophrenia, episodic course with progressive defect, incomplete remission. The clinical picture with this diagnosis includes delusions and hallucinations (usually delusions of persecution and verbal hallucinations - "voices").
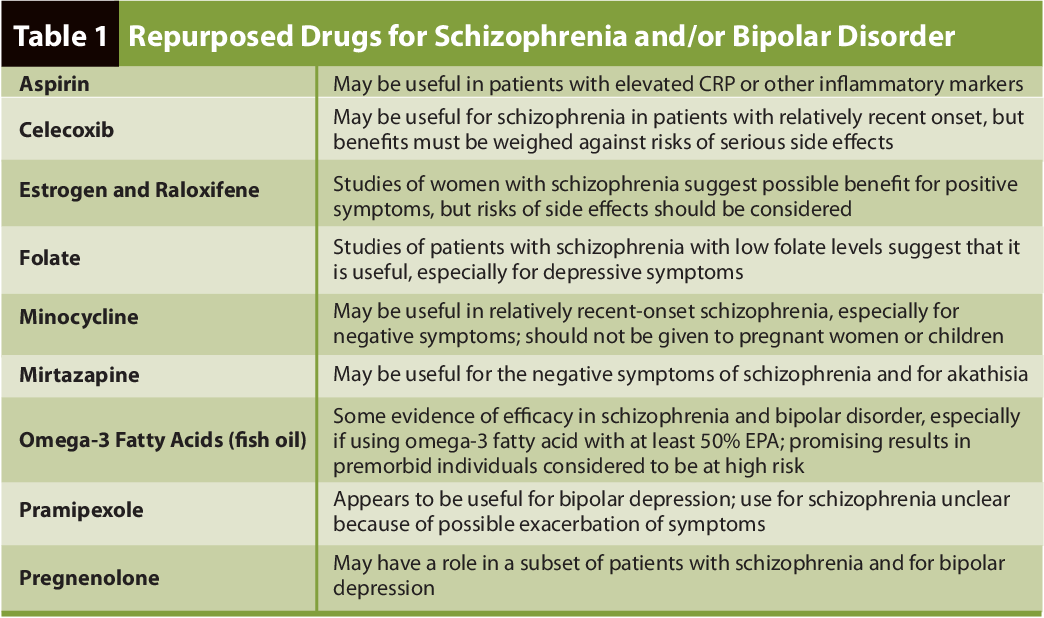
Treatment of schizophrenia includes antipsychotics, antidepressants, nootropics. The leading role belongs to antipsychotics, the action of which is aimed primarily at combating delusions and hallucinations. Against the background of treatment, at first, as a rule, the patient's affective reaction to his own experiences is dulled - he becomes calmer, psychomotor agitation passes.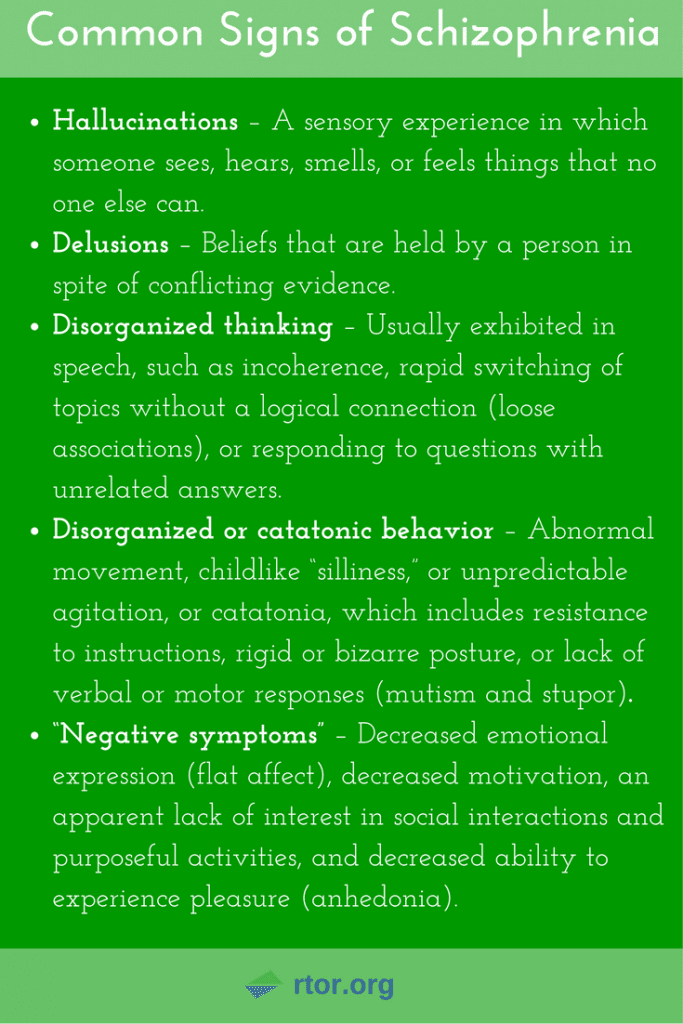 Then the hallucinations decrease in intensity or completely disappear. All these positive changes become noticeable already in the first days of the use of neuroleptics. But the plot (that is, the plot) of delirium can linger for a long time, although in the picture of internal experiences it fades significantly in relevance. After the relief of acute symptoms, the task comes to the fore: how to reduce negative symptoms and eliminate psychopathic (that is, as in psychopathy) behavioral disorders. This is helped by neuroleptics of the latest generations, such as olanzapine, paliperidone, risperidone. Already at this stage, it is worth thinking about the rehabilitation of the patient. Contrary to the earlier opinion, psychotherapy is indicated for these patients, and it helps to strengthen remission and resocialization. A good prognostic sign is the participation of the patient in physical labor, which, in itself, brings a significant therapeutic effect.
Then the hallucinations decrease in intensity or completely disappear. All these positive changes become noticeable already in the first days of the use of neuroleptics. But the plot (that is, the plot) of delirium can linger for a long time, although in the picture of internal experiences it fades significantly in relevance. After the relief of acute symptoms, the task comes to the fore: how to reduce negative symptoms and eliminate psychopathic (that is, as in psychopathy) behavioral disorders. This is helped by neuroleptics of the latest generations, such as olanzapine, paliperidone, risperidone. Already at this stage, it is worth thinking about the rehabilitation of the patient. Contrary to the earlier opinion, psychotherapy is indicated for these patients, and it helps to strengthen remission and resocialization. A good prognostic sign is the participation of the patient in physical labor, which, in itself, brings a significant therapeutic effect.
Although schizophrenia is a very formidable disease, it is not a death sentence.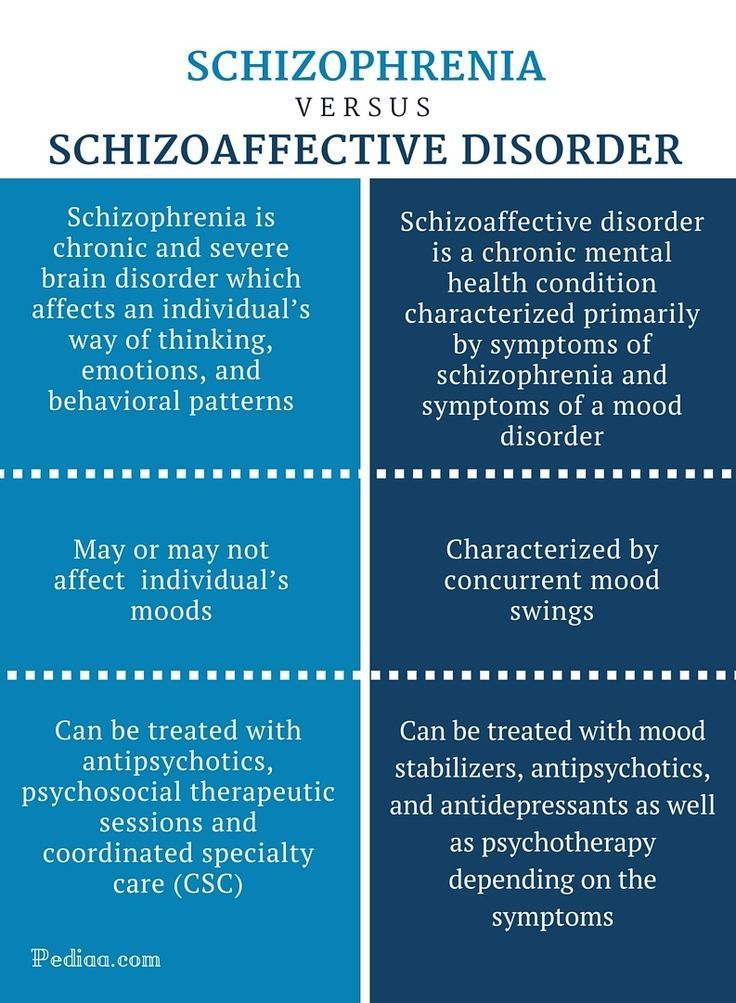 Due to the partial preservation of certain abilities (especially intellectual ones) and non-standard thinking, many of these patients have significant creative potential, which can be seen, among other things, from the works presented at the Ariadne's Thread festival of arts.
Due to the partial preservation of certain abilities (especially intellectual ones) and non-standard thinking, many of these patients have significant creative potential, which can be seen, among other things, from the works presented at the Ariadne's Thread festival of arts.
- Back
- Forward
- Are you here:
- Main page GBUZ "PKB No. 5 DZM" /
- For visitors /
- About mental disorders /
- Schizophrenia
"Primary", "main" and "secondary" symptoms of schizophrenia in the concept of E. Bleiler
The appearance of changes in E.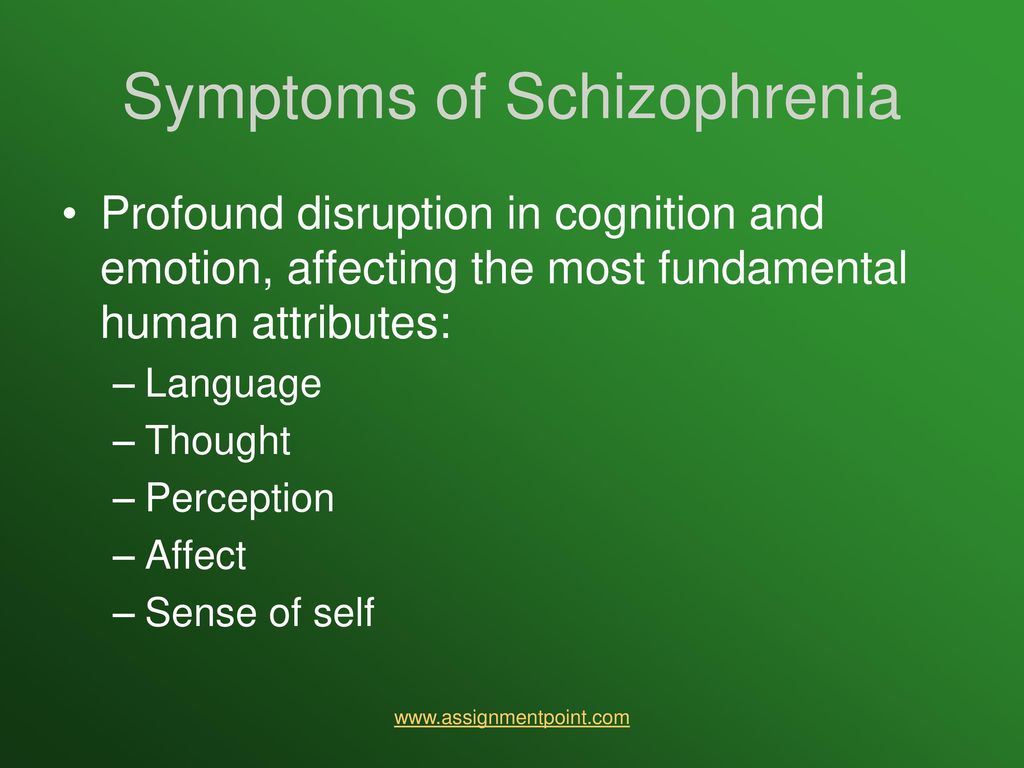 Kretschmer's concept of psychopathic constitutions 1 , presented in the book "Body structure and character" [1] - when compared with the previous monograph "Sensitive delusions of attitude" [2] - cannot be explained without referring to concept dementia praecox , "schizophrenia" developed by E. Bleuler (1908, 1911, 1916, 1920) [3-7].
Kretschmer's concept of psychopathic constitutions 1 , presented in the book "Body structure and character" [1] - when compared with the previous monograph "Sensitive delusions of attitude" [2] - cannot be explained without referring to concept dementia praecox , "schizophrenia" developed by E. Bleuler (1908, 1911, 1916, 1920) [3-7].
Some French psychiatrists [8, 9] cite the widespread opinion that the concept of "degenerative insanity" has been destroyed by the concept dementia praecox E. Kraepelin. This is not entirely true. Rejecting the genetic scheme of B. Morel [10, 11], E. Kraepelin [12—16] did not deny the clinical aspects of the theory of degeneration in the form of the significance for manifest mental disorders of various deviations from the “normal” personality type, constitutional “nervousness” and a tendency to reactive states.
The diagnosis "dementia praecox" in German-speaking psychiatry was first used in the classification of mental illness in 1886 by H.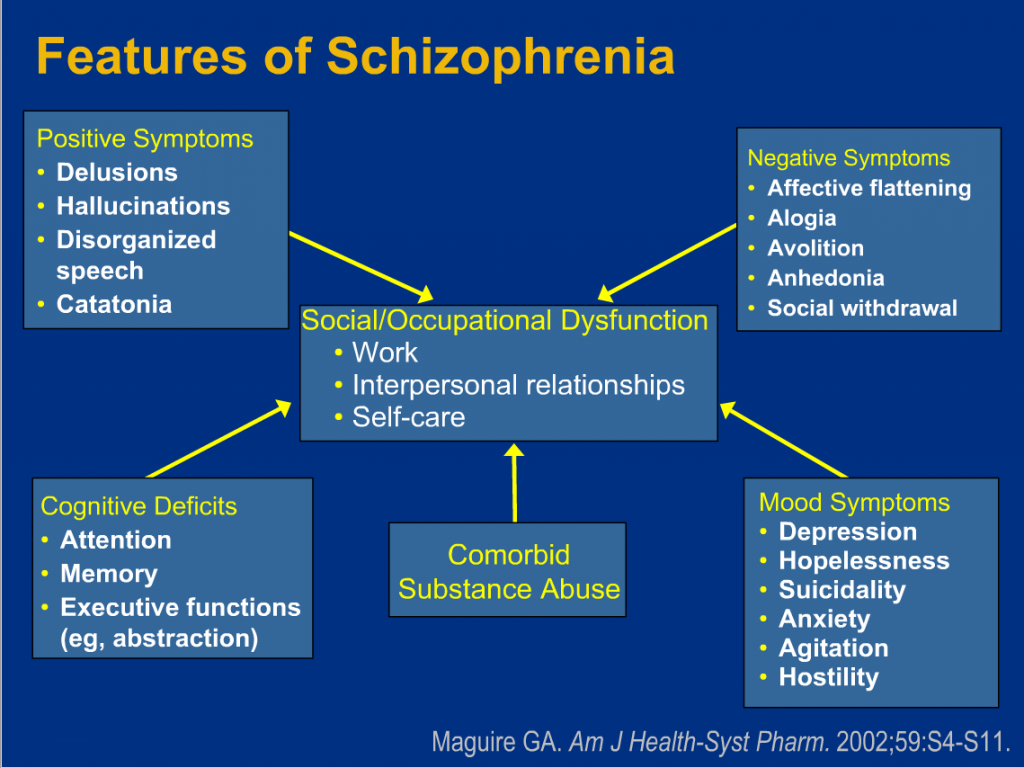 Schuele [17], then in 1893 E. Kraepelin [13] in the 4th edition of the "Textbook" in the heading "processes of degeneration" (corresponding to the concept of "degenerative insanity") identified three subheadings: "Dementia praecox" (a variant of which was considered "hebephrenia" by E. Hecker [ 18]), "Catatonia" [19] and "Dementia paranoidales". Only in the famous 5th edition of the textbook, published in 1896, dementia praecox , catatonia and dementia paranoidales were united under the heading "dementia processes" and classified by E. Kraepelin [14] as acquired psychosis with inclusion in the group of "psychoses due to metabolic disorders". And finally, in the 6th edition of the textbook (1899) [15] dementia praecox becomes a separate rubric combining hebephrenic, catatonic and paranoid forms. Kraepelin's classification of "dementia praecox" remained unchanged in the 7th edition of the textbook (1904) [16], and only in the last lifetime edition - the 8th (1913) [20] - underwent significant changes (note that the 6th and The 7th editions were rated by his fellow psychiatrists as "the best" [21]).
Schuele [17], then in 1893 E. Kraepelin [13] in the 4th edition of the "Textbook" in the heading "processes of degeneration" (corresponding to the concept of "degenerative insanity") identified three subheadings: "Dementia praecox" (a variant of which was considered "hebephrenia" by E. Hecker [ 18]), "Catatonia" [19] and "Dementia paranoidales". Only in the famous 5th edition of the textbook, published in 1896, dementia praecox , catatonia and dementia paranoidales were united under the heading "dementia processes" and classified by E. Kraepelin [14] as acquired psychosis with inclusion in the group of "psychoses due to metabolic disorders". And finally, in the 6th edition of the textbook (1899) [15] dementia praecox becomes a separate rubric combining hebephrenic, catatonic and paranoid forms. Kraepelin's classification of "dementia praecox" remained unchanged in the 7th edition of the textbook (1904) [16], and only in the last lifetime edition - the 8th (1913) [20] - underwent significant changes (note that the 6th and The 7th editions were rated by his fellow psychiatrists as "the best" [21]).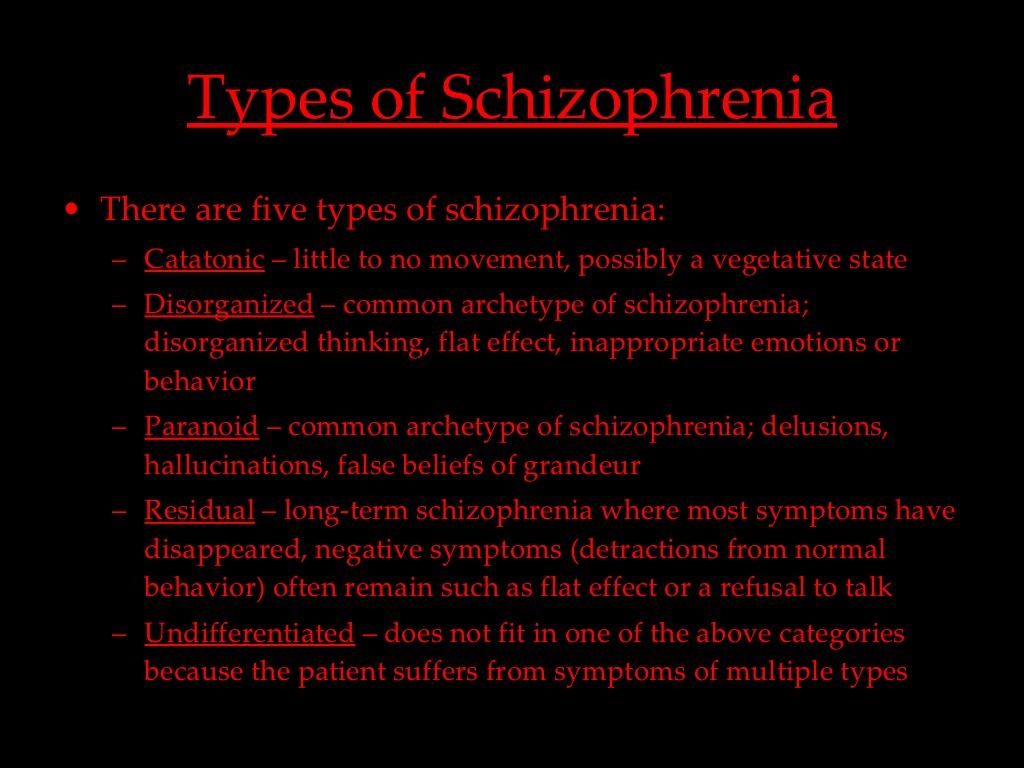
Revision of ideas about dementia praecox was carried out by E. Kraepelin partly under the influence of the new concept of this concept that had appeared by that time by the Swiss psychiatrist E. Bleuler [3, 4], who first presented his views to German psychiatrists at a congress in Berlin in 1908. And precisely the concept of dementia praecox E. Bleuler began to absorb the vast space from the field of various psychopathological pictures of "degenerative insanity". Already in the report “Forecast dementia praecox (groups of schizophrenia)" E. Bleuler [3] announced a new name for the disorder - "schizophrenia". One of the reasons for the renaming, he calls an outstanding symptom of the entire group of "schizophrenia": the fragmentation ("Zerreissung"), or splitting ("Spaltung"), of mental functions. E. Bleuler and his students (Wolfsohn and Zablocka [22]) formulated their observations on the basis of a survey of 647 patients with schizophrenia hospitalized at the Burghoelzli clinic over an 8-year period.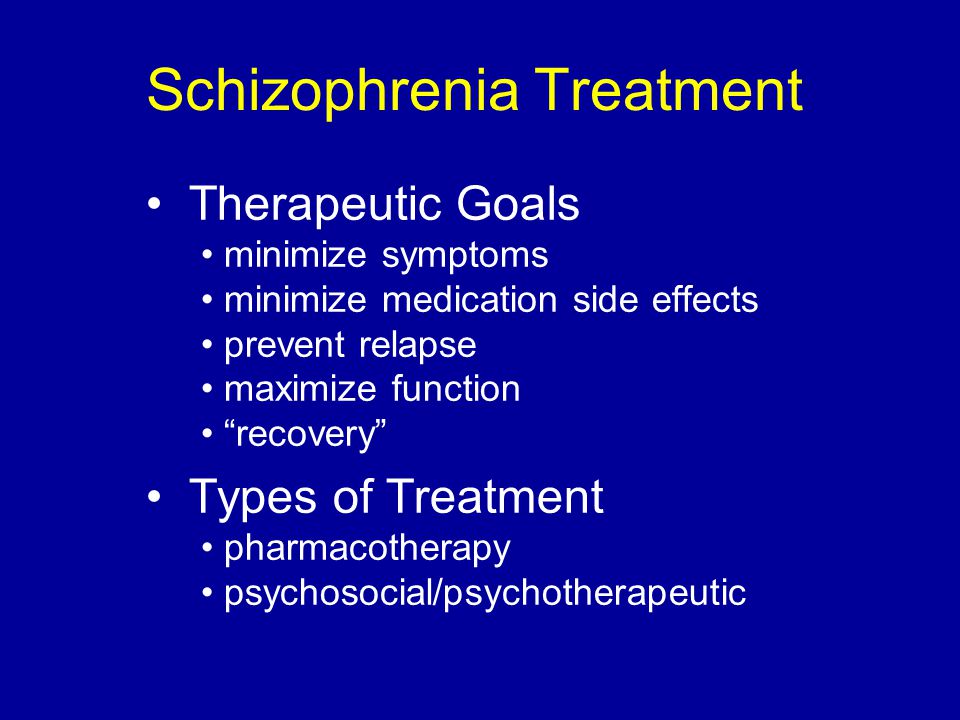 At the same time, E. Bleuler [3] concluded that “abnormal” characters have a greater tendency to a severe course of the disease and less to a mild one than “normal” and “nervous” ones (see table). It should be noted that, based on the concept of "degenerative insanity", in abnormal personalities, on the contrary, psychoses should proceed more favorably.
At the same time, E. Bleuler [3] concluded that “abnormal” characters have a greater tendency to a severe course of the disease and less to a mild one than “normal” and “nervous” ones (see table). It should be noted that, based on the concept of "degenerative insanity", in abnormal personalities, on the contrary, psychoses should proceed more favorably.
The ratio of the nature of patients with schizophrenia to the severity of dementia (according to E. Bleuler [3]) Note. Severe dementia meant patients who needed outside help and usually remained in psychiatric hospitals, mild dementia meant those who adapted to life outside the hospital, maintained working capacity and created families, and moderate dementia meant “something in between these two groups” [22].
An essential feature of the anomalous nature of M.-E. Zablocka [22] found "isolation", E. Bleuler [3] explained that the concept of "abnormal character" is a "pot" in which a wide variety of deviations from the norm are placed, including "latent, chronically current schizophrenia", which and may adversely affect the overall prognosis.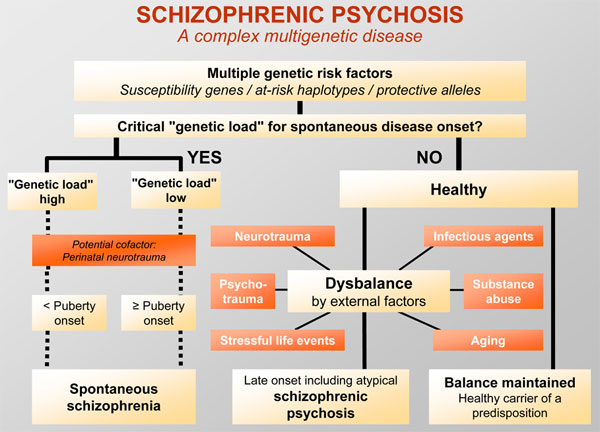 In the report preceding Bleuler's report, M. Jahrmaerker [23] “Final states at dementia praecox "latent" dementia praecox means such minor changes "in the direction of dementia", which are not detected during a normal, not thorough examination. E. Bleuler [3] noted in turn that if an acute attack does not make the disease manifest, such cases of schizophrenia remain latent. He already then believed that latent cases of schizophrenia were very frequent, especially judging by outpatient appointments and meetings in life, as well as a large number of schizophrenic patients who are "considered healthy." He emphasized that many of the "manyan degenerates" and "paranoid constitutions" of other authors are "unrecognized schizophrenics".
In the report preceding Bleuler's report, M. Jahrmaerker [23] “Final states at dementia praecox "latent" dementia praecox means such minor changes "in the direction of dementia", which are not detected during a normal, not thorough examination. E. Bleuler [3] noted in turn that if an acute attack does not make the disease manifest, such cases of schizophrenia remain latent. He already then believed that latent cases of schizophrenia were very frequent, especially judging by outpatient appointments and meetings in life, as well as a large number of schizophrenic patients who are "considered healthy." He emphasized that many of the "manyan degenerates" and "paranoid constitutions" of other authors are "unrecognized schizophrenics".
From the point of view of E. Bleuler [3], with schizophrenia there can be no recovery according to the Restitutio ad integrum type, because he “did not see a single patient in whom no signs of the disease could be detected at discharge”, although in life former patients can achieve outstanding success.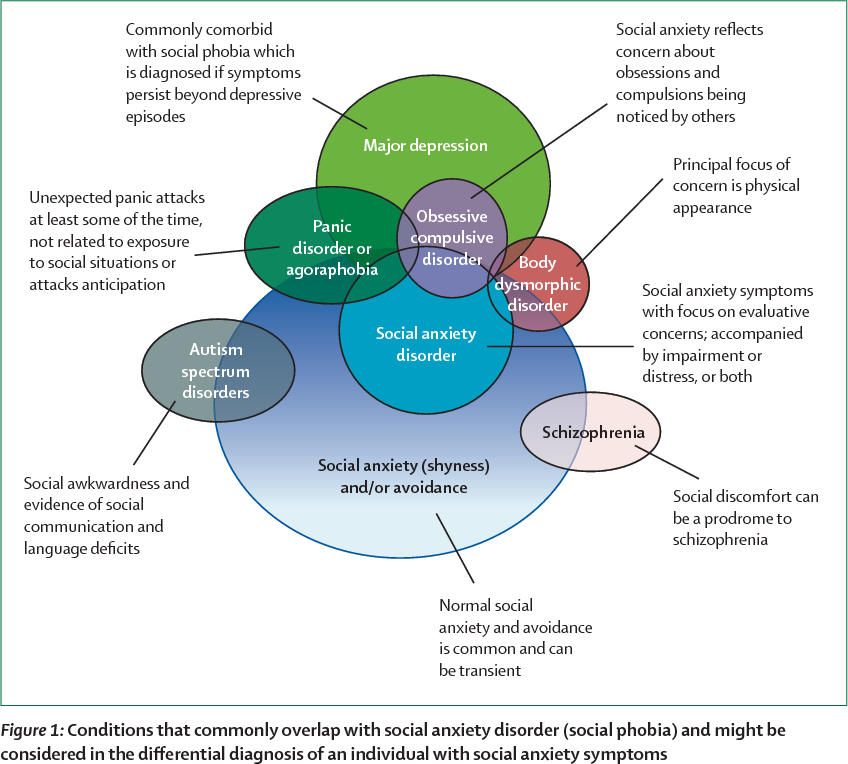 He pointed out: "It is possible with great pleasure to talk with the patient about scientific subtleties, although he continues to suffer from delusional ideas." If, in a conversation with a patient, the “complex” that played a role in his mental illness is touched upon, the patient immediately begins to make gross logical errors. Therefore, E. Bleuler refused to talk about a complete recovery, since as a result of the disease, complexes of ideas remain split off from logic. Other evidence of the "incurability" of schizophrenia according to E. Bleuler is the constant gradual increase in dementia in chronically hospitalized patients, the tendency of acute attacks to relapse and frequent abnormal reactions to alcohol and affective arousal. During exacerbation of the process, a repeated actualization of the ideas developed in the previous attack is also noticeable, which, according to E. Bleuler, indicates "incomplete overcoming of the remnants of the disease." Therefore, at 19In 1908, he proposed to talk essentially not about relapses of schizophrenia, but about “fur coats” of the disease, although he considered it possible to retain the definition of “relapse” for attacks that did not reach the significance of fur coats.
He pointed out: "It is possible with great pleasure to talk with the patient about scientific subtleties, although he continues to suffer from delusional ideas." If, in a conversation with a patient, the “complex” that played a role in his mental illness is touched upon, the patient immediately begins to make gross logical errors. Therefore, E. Bleuler refused to talk about a complete recovery, since as a result of the disease, complexes of ideas remain split off from logic. Other evidence of the "incurability" of schizophrenia according to E. Bleuler is the constant gradual increase in dementia in chronically hospitalized patients, the tendency of acute attacks to relapse and frequent abnormal reactions to alcohol and affective arousal. During exacerbation of the process, a repeated actualization of the ideas developed in the previous attack is also noticeable, which, according to E. Bleuler, indicates "incomplete overcoming of the remnants of the disease." Therefore, at 19In 1908, he proposed to talk essentially not about relapses of schizophrenia, but about “fur coats” of the disease, although he considered it possible to retain the definition of “relapse” for attacks that did not reach the significance of fur coats. The value of heredity for schizophrenia E. Bleuler rejected at that time.
The value of heredity for schizophrenia E. Bleuler rejected at that time.
E. Bleuler [3] emphasized that a patient with schizophrenia is weak-minded not simply, but in relation to certain issues, time and complexes. Specific to schizophrenia, he found disorders of association and affectivity: the more pronounced they are in manic or even more frequent melancholic attacks, the worse the prognosis and the weaker the hope for their reverse development. E. Bleuler attached somewhat less importance to catatonic symptoms, although he noted that their degree tends to correspond to the intensity and danger of the schizophrenic process. However, even in long-term chronic cases, the potential for significant improvement remains.
To study the pathological and prognostic significance of schizophrenic symptoms, E. Bleuler considered it necessary to turn to the doctrine of primary and secondary symptoms, which had already been sufficiently developed in German psychiatry [23-28], but presented primary and secondary symptoms in its own way in relation to schizophrenia.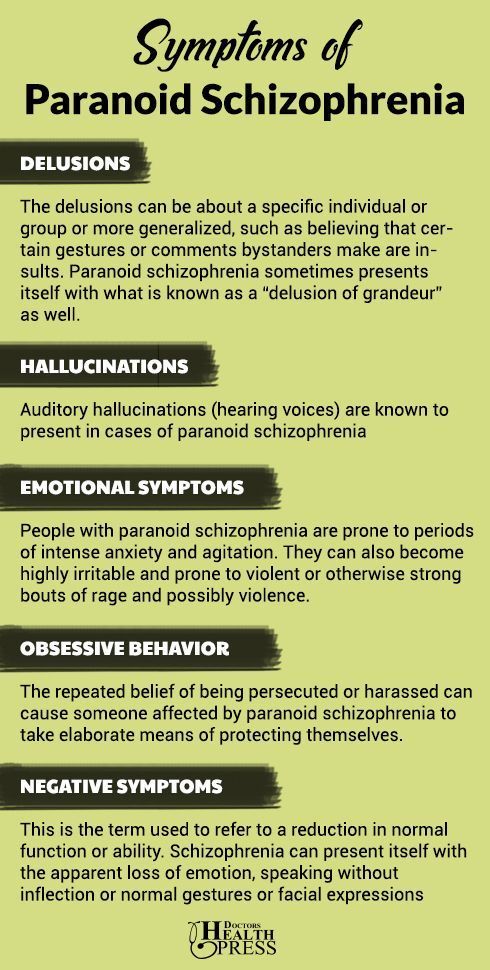 Primary symptoms are a direct manifestation of the disease process, and secondary - occur as a result of the reaction of the sick psyche to the influence of the environment and one's own aspirations. To represent the primary and secondary symptoms in schizophrenia, E. Bleuler refers to a medical metaphor from the field of somatic medicine - osteoporosis. Osteoporosis can be very advanced, yet remain asymptomatic. The disease itself and the prognostic emphasis are bone fragility, which, depending on external circumstances, manifests itself or does not manifest itself in symptoms. Bone fragility is the primary symptom, fracture with minor trauma is secondary. Similarly, paralysis of the abducens eye muscle will be the primary symptom, and contracture of the internal muscle of the eye will be secondary.
Primary symptoms are a direct manifestation of the disease process, and secondary - occur as a result of the reaction of the sick psyche to the influence of the environment and one's own aspirations. To represent the primary and secondary symptoms in schizophrenia, E. Bleuler refers to a medical metaphor from the field of somatic medicine - osteoporosis. Osteoporosis can be very advanced, yet remain asymptomatic. The disease itself and the prognostic emphasis are bone fragility, which, depending on external circumstances, manifests itself or does not manifest itself in symptoms. Bone fragility is the primary symptom, fracture with minor trauma is secondary. Similarly, paralysis of the abducens eye muscle will be the primary symptom, and contracture of the internal muscle of the eye will be secondary.
In schizophrenia, there are symptoms caused by external influences: attacks of swearing and anger (as purely mental reactions of the patient to external circumstances), hysteroform twilight states (including the Ganser symptom complex).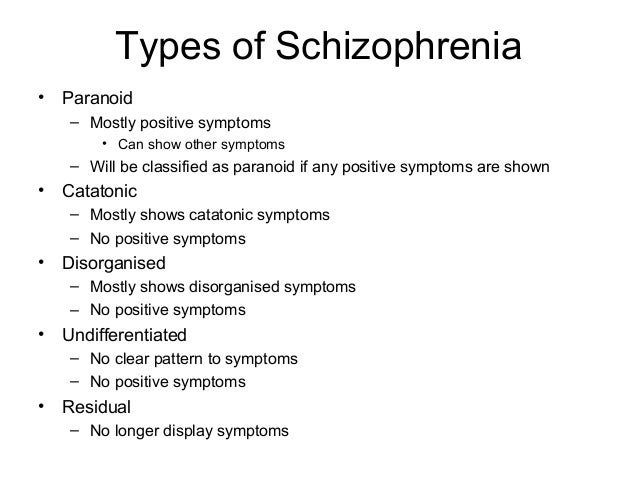 This is not the disease itself, but its signs, and twilight states usually have a good prognosis (an accidental episode, but not the coats of the disease). Whether patients close up, work or not, is not the primary symptom of the disease, but the result of many mental processes and external influences. E. Bleuler then still used not the term "autism", but the word "Abschliessung" - closing in on oneself, and noted that "closure" can be very changeable: in relation to one person and in certain places, patients may look completely detached, and in other circumstances behave as normal. Dementia, according to E. Bleuler [3], is also mainly a secondary symptom, hence the sudden improvements in schizophrenia. First of all, this applies to affective dementia. Affects, according to the observations of E. Bleuler, can revive again after many years. Such a wide recovery with initially detuned associative functions never occurs. Catatonic symptoms in the bulk are also not considered by E. Bleuler as primary.
This is not the disease itself, but its signs, and twilight states usually have a good prognosis (an accidental episode, but not the coats of the disease). Whether patients close up, work or not, is not the primary symptom of the disease, but the result of many mental processes and external influences. E. Bleuler then still used not the term "autism", but the word "Abschliessung" - closing in on oneself, and noted that "closure" can be very changeable: in relation to one person and in certain places, patients may look completely detached, and in other circumstances behave as normal. Dementia, according to E. Bleuler [3], is also mainly a secondary symptom, hence the sudden improvements in schizophrenia. First of all, this applies to affective dementia. Affects, according to the observations of E. Bleuler, can revive again after many years. Such a wide recovery with initially detuned associative functions never occurs. Catatonic symptoms in the bulk are also not considered by E. Bleuler as primary. Primary can only be a "disposition" to catatonic symptoms and stereotypes.
Primary can only be a "disposition" to catatonic symptoms and stereotypes.
But actually bodily symptoms (fibrillar twitches, increased ideomuscular excitability, uneven pupils) E. Bleuler [3] assessed as a direct sign of damage to the nervous system in schizophrenia. With regard to other bodily symptoms (vasomotor disorders, disorders of secretion, nutrition, body temperature, menstruation), he believed that "we still understand them little."
In the psychic sphere, association disorders are primary, in acute cases they break into such pieces that the thought is not thought out to the end, mental synthesis is not carried out. There are also such types of stupefaction and slow flow of all mental processes that cannot be explained by other phenomena, they produce an "organic" impression. E. Bleuler supposedly associated such stupor with swelling of the brain and its membranes, usually found in cases of lethal catatonia. Also primary, "organic", he considered some catatonic seizures with loss of consciousness and convulsions (sometimes accompanied by slight paresis), some states of confusion. Even fluctuations in affect can sometimes be caused directly by a disease process, while states of fear, according to E. Bleuler, are secondary symptoms based on schizophrenic thought disorders.
Even fluctuations in affect can sometimes be caused directly by a disease process, while states of fear, according to E. Bleuler, are secondary symptoms based on schizophrenic thought disorders.
With regard to the prognosis of schizophrenia, E. Bleuler emphasized that a prognosis based on the “feeling” (“Gefuehlsprognose”) of an experienced psychiatrist is more accurate than a deductive prediction made “according to all the rules of art”. However, general schizophrenic association disorder, once chronic, rarely tends to regress. The same applies to very pronounced affective dementia. Although the regression of purely psychically conditioned (“secondary”) symptoms seems to be taken for granted, in some cases the regression does not occur. And in the mentally healthy, some experiences leave a trace. So, religious ideas or superstitions acquired in youth can manifest themselves again and again, despite the change in the carrier's attitude towards them. Similarly, once overcome delusional ideas in schizophrenia do not completely lose their influence on logic and affectivity.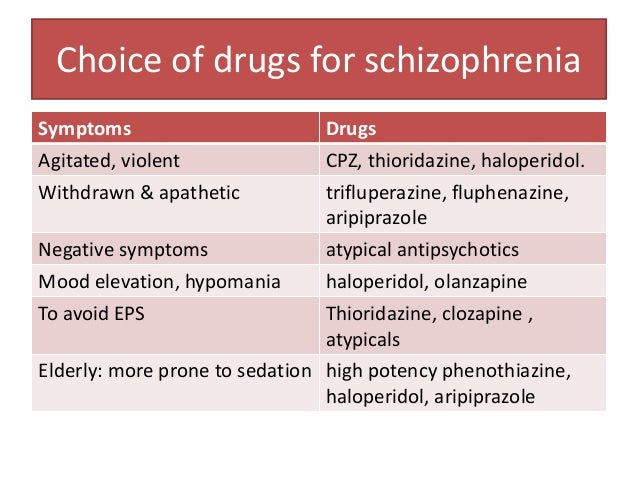 They are never completely corrected in the same way as a healthy error is corrected that is not charged with affect. Thus, according to E. Bleuler [3], one should not speak with full confidence about the mandatory regression of purely functional mental symptoms.
They are never completely corrected in the same way as a healthy error is corrected that is not charged with affect. Thus, according to E. Bleuler [3], one should not speak with full confidence about the mandatory regression of purely functional mental symptoms.
Conditions caused by passion - twilight and fits of anger - cease, since in both the healthy and the sick the affect is eventually exhausted. Most often, according to E. Bleuler [3], the mental “remnants” of a stopped process are split off from the personality. So, crazy ideas are not corrected, but "forgotten". When reminded of them in a conversation, the onset of a new fur coat, the same crazy ideas unfold with renewed vigor. The mechanism of "cleavage" is promoted by external distracting stimulation, therefore E. Bleuler recommended employment therapy and immediate discharge to improve the prognosis. According to E. Bleuler, one can only assume that the intensity of the schizophrenic process is somehow related to the degree of associative fragmentation and stupor; it is difficult to assume this with respect to other symptoms.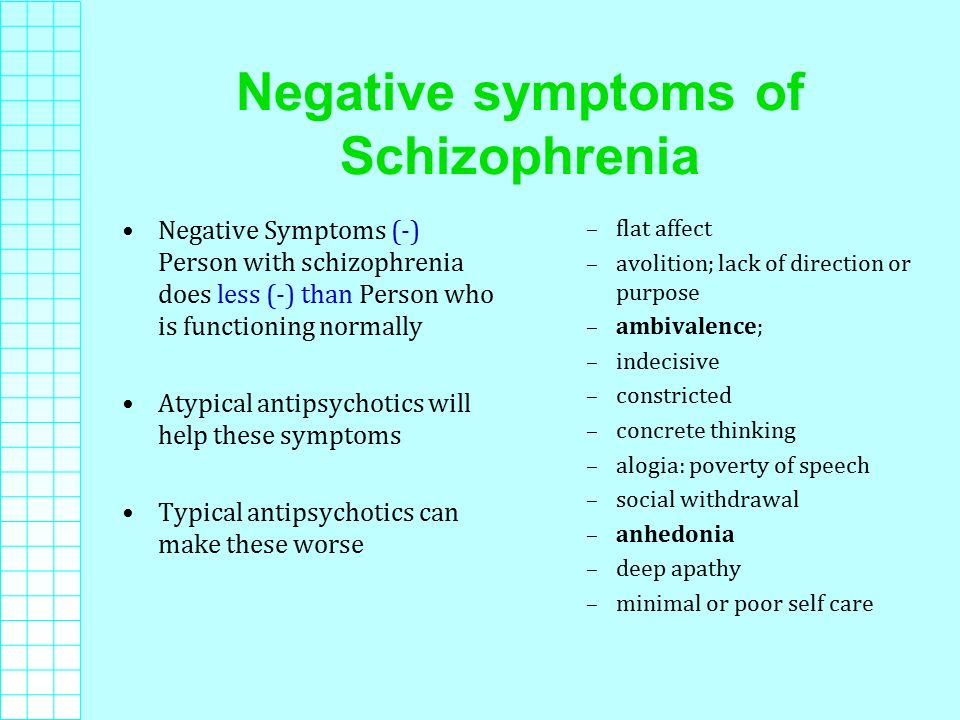 For only primary symptoms are not capable of significant regression. And a new fur coat can develop after any period of time, even decades of a “calm” state. The dating of the disease by relatives is rarely correct. Typically, a worsening or occasional acute symptom leads to a psychiatric hospital visit after the patient has had years of "mild" schizophrenia. Acute onset, according to E. Bleuler, is actually rarely observed.
For only primary symptoms are not capable of significant regression. And a new fur coat can develop after any period of time, even decades of a “calm” state. The dating of the disease by relatives is rarely correct. Typically, a worsening or occasional acute symptom leads to a psychiatric hospital visit after the patient has had years of "mild" schizophrenia. Acute onset, according to E. Bleuler, is actually rarely observed.
Later, in a monograph published in 1911, E. Bleuler [4] added a fourth form of schizophrenia: the “simple” dementia form [ 29] or schizo phrenia simplex . In the preface to this monograph, E. Bleuler noted that the whole grouping and selection of individual symptoms dementia praecox are the merit of E. Kraepelin, and his own psychopathological concept of schizophrenia is based on the application of the ideas of S. Freud [30—32] to dementia praecox , including also the ideas of other psychoanalysts - F.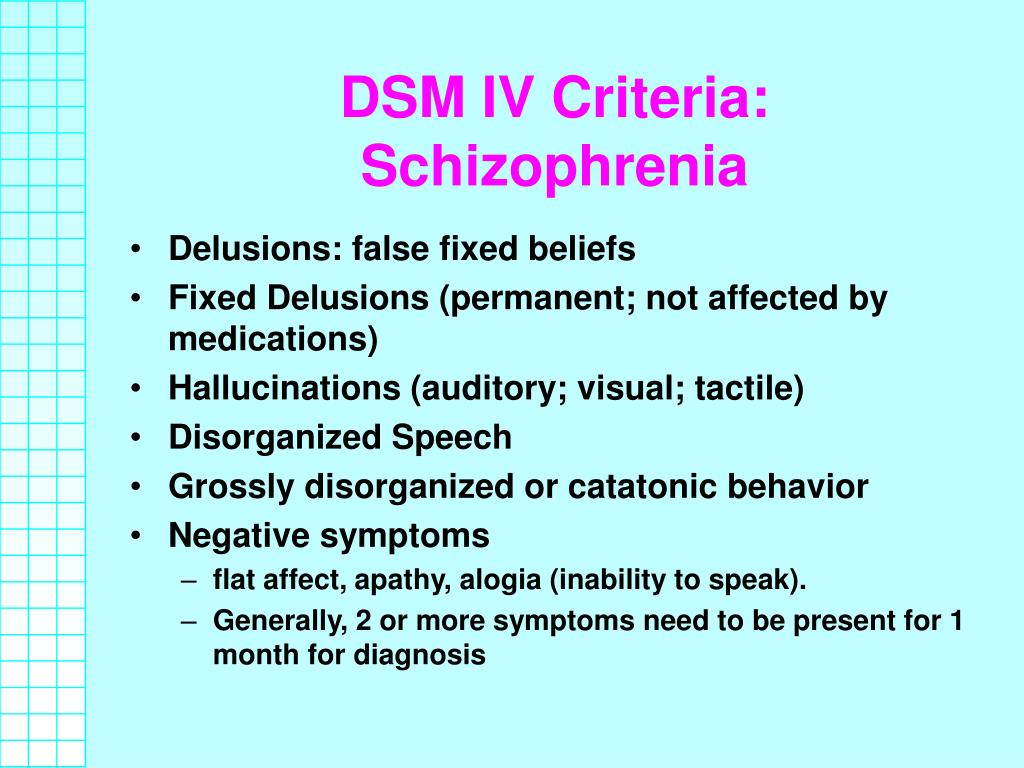 Riklin [33], K. Abraham [34, 35] and C. Jung [36].
Riklin [33], K. Abraham [34, 35] and C. Jung [36].
In a report made in 1908 [3], and in a more detailed and detailed monograph in 1911, E. Bleuler [3, 4] expanded the boundaries of the concept by their authors from dementia praecox E. Kraepelin and most often referred to the category of "degenerative insanity". In the report mentioned above, E. Bleuler noted that “degenerates” V. Magnan [37, 38] and abnormal personalities (psychopathic personalities in the understanding of E. Kraepelin [16]) may include a significant proportion of patients with latent schizophrenia. The symptoms observed in "degenerative insanity", according to E. Bleuler [4], are very common in schizophrenia. For example, described by K. Birnbaum [39, 40] “delusional fantasies of degenerates” can be “schizophrenic” down to the smallest nuances, as well as “crazy sudden ideas” by K. Bonhoeffer [41]. "Eknoyu", allocated by Th. Ziehen [42, 43], E. Bleuler attributed to schizophrenia. The "nonsense of masturbators", later distinguished by E.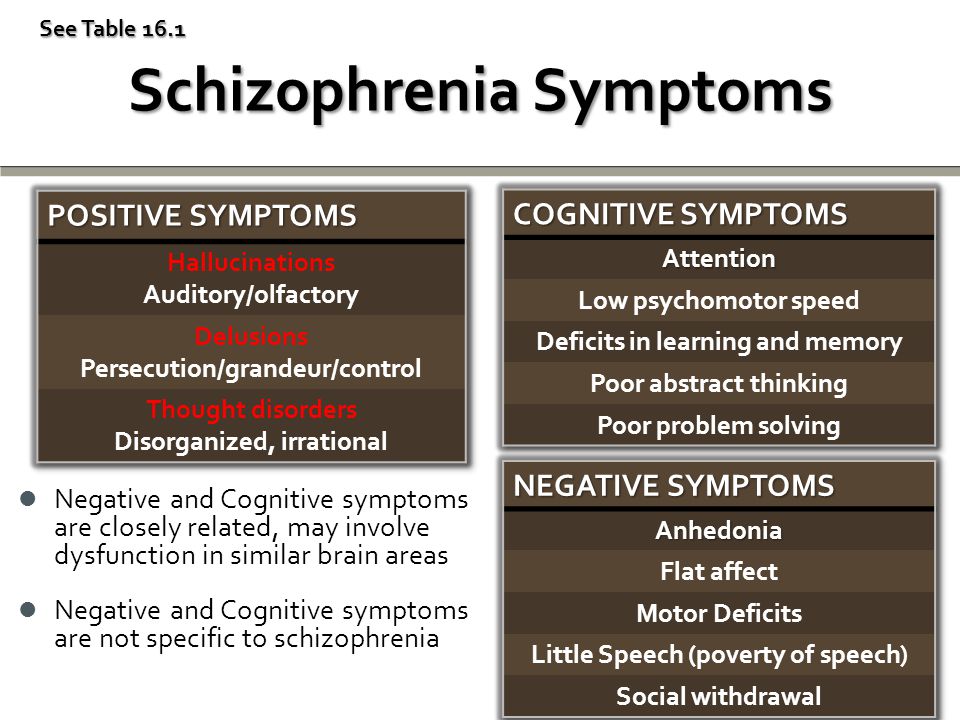 Kretschmer [1] from dementia praecox , according to E. Bleuler also "dissolves" in schizophenia. And the typical Ganzer symptom complex develops on a "schizophrenic basis."
Kretschmer [1] from dementia praecox , according to E. Bleuler also "dissolves" in schizophenia. And the typical Ganzer symptom complex develops on a "schizophrenic basis."
"Moral insanity" does not apply to schizophrenia only when the lack of ethical feelings is permanent and the character remains unchanged from early years. The paranoia described by E. Kraepelin [16] remains independent of schizophrenia only at the absence of delusions of "internal influence", periods of massive hallucinations, loss of external self-control and violation of customs. Most of the cases of hysteria and neurasthenia (attributed by many authors to "degenerative insanity") turn out to be, according to E. Bleuler, schizophrenia. In substantiating this view, he relied on the fact that "there is not a single hysterical and neurasthenic symptom that would be alien to schizophrenia." Therefore, if symptoms “specific” to schizophrenia are found in the hysterical or neurasthenic picture of the disease, then this is schizophrenia, and mild (“leichte”) schizophrenia can “hide” behind the symptoms of “nervousness” for a long time.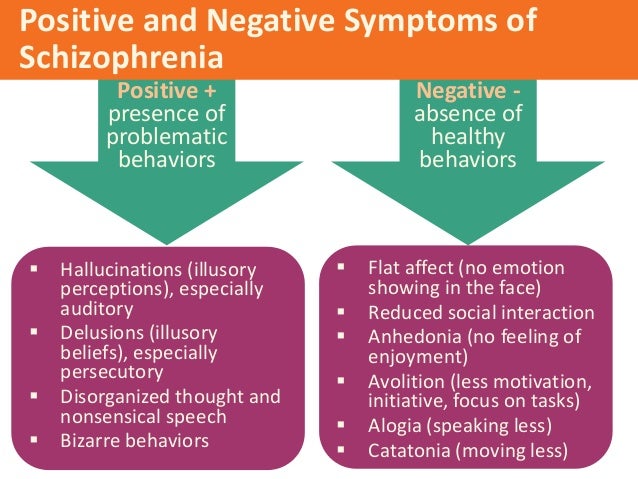 According to E. Bleuler, differences in the affective area can serve as the main differential sign: affective autism is expressed in the fact that patients do not feel the need to speak out. He emphasized that “if a doctor talks with a patient about his illness for an hour, then a “personal relationship” is established between the doctor and the patient, hostile or friendly, and such an affective rapprochement is not observed with a patient with schizophrenia.
According to E. Bleuler, differences in the affective area can serve as the main differential sign: affective autism is expressed in the fact that patients do not feel the need to speak out. He emphasized that “if a doctor talks with a patient about his illness for an hour, then a “personal relationship” is established between the doctor and the patient, hostile or friendly, and such an affective rapprochement is not observed with a patient with schizophrenia.
A considerable part of cases of alcoholism, according to the concept of E. Bleuler [4], develops on the basis of schizophrenia: it predisposes to delirium tremens ; the development of alcoholic delirium in persons younger than 25 years of age with relatively moderate alcohol consumption for several years is possible only with schizophrenia. Chronic "alcohol paranoia" is entirely "common schizophrenia developed in a drinking patient." Paranoid predisposition in alcoholism E. Bleuler called latent schizophrenia.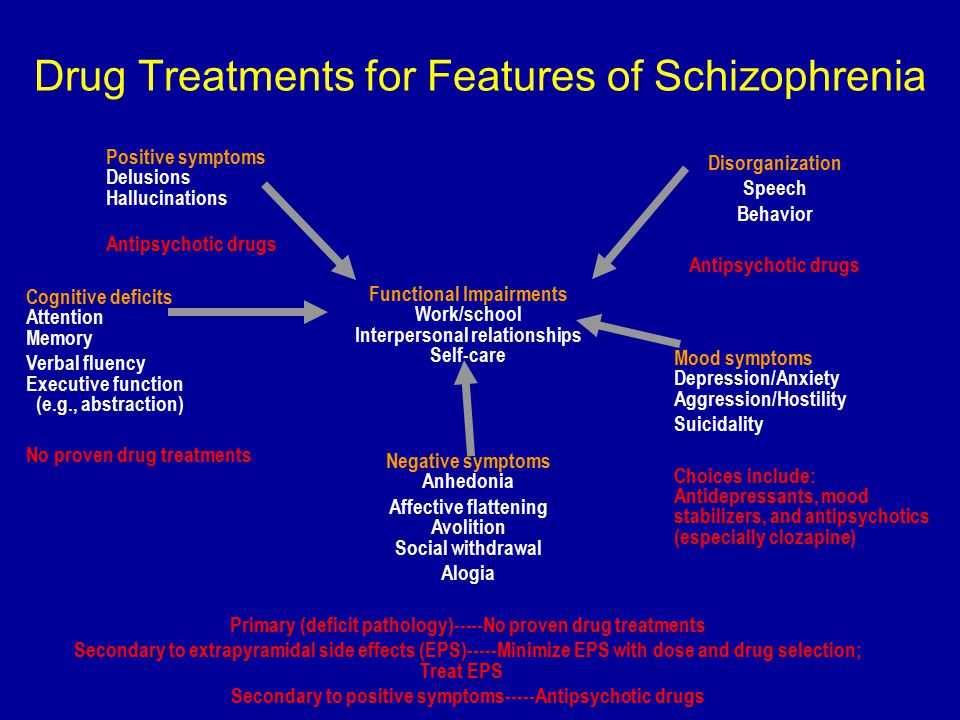 Kraepelin's presenile delirium of damage [16] E. Bleuler attributed to the late paranoid form of schizophrenia.
Kraepelin's presenile delirium of damage [16] E. Bleuler attributed to the late paranoid form of schizophrenia.
E. Bleuler emphasized that the concept of schizophrenia is based not on relative, but on absolute criteria, meaning by "absolute" that if they are proved, the diagnosis of schizophrenia is determined in all circumstances. At the same time, in mild cases of schizophrenia, its symptoms may not be detected at the present level of research (hence the diagnosis of “schizophrenia sine schizophreniae” (“schizophrenia sine schizophreniae”) subsequently arose.0089 in the monograph by E. Bleuler [4] carried out, based on the doctrine he developed about the main and additional schizophrenic symptoms, the inclusion in the classification of schizophrenia of the fourth, “simple” form (which E. Kraepelin [16] did not do before him until the 7th edition of the textbook, inclusive), as well as on the basis of the conviction that latent forms of schizophrenia are much more common than manifest ones.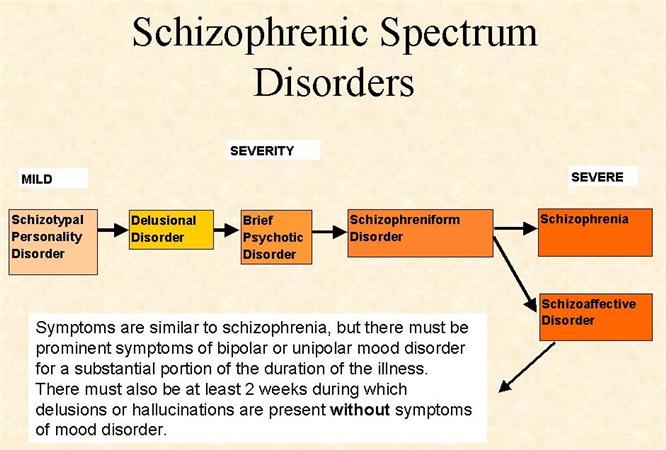 E. Bleuler [7] also argued the last aspect by direct comparison of schizophrenia and tuberculosis.
E. Bleuler [7] also argued the last aspect by direct comparison of schizophrenia and tuberculosis.
In the "symptomatology" of schizophrenia, E. Bleuler [4] said that the only symptom always inherent in schizophrenia is a peculiar disorder of associations. Based on the doctrine of the primary and secondary symptoms of schizophrenia, he tried to create criteria for the prognosis of the disease. Later, he realized reflections on primary and secondary symptoms in the “theory” of symptoms, and for the diagnosis of schizophrenia in “symptomatology” he created a system of “basic” and “additional” (or accessory) symptoms. The main symptoms are characteristic of schizophrenia, additional symptoms can also be observed in other mental illnesses, may be absent in schizophrenia, however, according to E. Bleuler, additional symptoms in most cases of schizophrenia have a “specific” color. At the same time, he emphasized that for all the "basic" symptoms he describes, there are all sorts of transitions to the norm , and in mild cases of schizophrenia, which he calls "latent schizophrenia", they are generally "little distinct. " Moreover, given the large fluctuations in the schizophrenic picture of the disease, "it is impossible to prove the presence of every symptom at every moment of the disease."
" Moreover, given the large fluctuations in the schizophrenic picture of the disease, "it is impossible to prove the presence of every symptom at every moment of the disease."
To the main symptoms E. Bleuler [4] ranked "schizophrenic" disorder of associations, affectivity, ambivalence and autism, understanding by the latter the tendency to put one's own fantasy above reality and fence oneself off from it.
Among the various associative disorders (discontinuity, “strangeness, strangeness of associations, associations by consonance, condensation (“Verdichtung”) of associations, stereotyping, monoideism, distractibility, viscosity of thinking, perseveration, impoverishment of thinking, etc.) E. Bleuler [4] named two forms that he found especially specific to schizophrenia: “influx of thoughts” and “sperrung 3 ” - a complete break in the train of thought. At the end of the "sperrung", the occurrence of which may be associated with "complexes 4 ”, ideas that are not related to the previous ones usually arise.
The palette of affective symptoms of schizophrenia according to E. Bleiler [4] is extremely diverse. On the one hand, the affective life of patients is characterized by stupefaction, indifference, reduction of the drive to self-preservation. In mild cases, indifference may be absent or masked. In the beginning of the disease, on the contrary, hypersensitivity is often found, due to which patients tend to isolation. Patients latent schizophrenia may seem labile in their affects, sanguine. But they lack the depth of affect, there is a "partial" indifference. On the other hand, as noted by E. Bleuler [4], there are many patients with schizophrenia who have “live” affects in certain areas, including active ones: writers, “improvers” of peace and health, founders of religious sects. Their main mood can be euphoric, sad, anxious. The transition from a euphoric mood to an indifferent one or their mixture is often observed in patients with hebephrenia in the form of a special emotional state of "sausage" ("Wurstigkeit" 5 ): patients are satisfied with themselves and the world around them, undesirable events are not perceived as unpleasant, and in their answers they easily become impudent and impudent.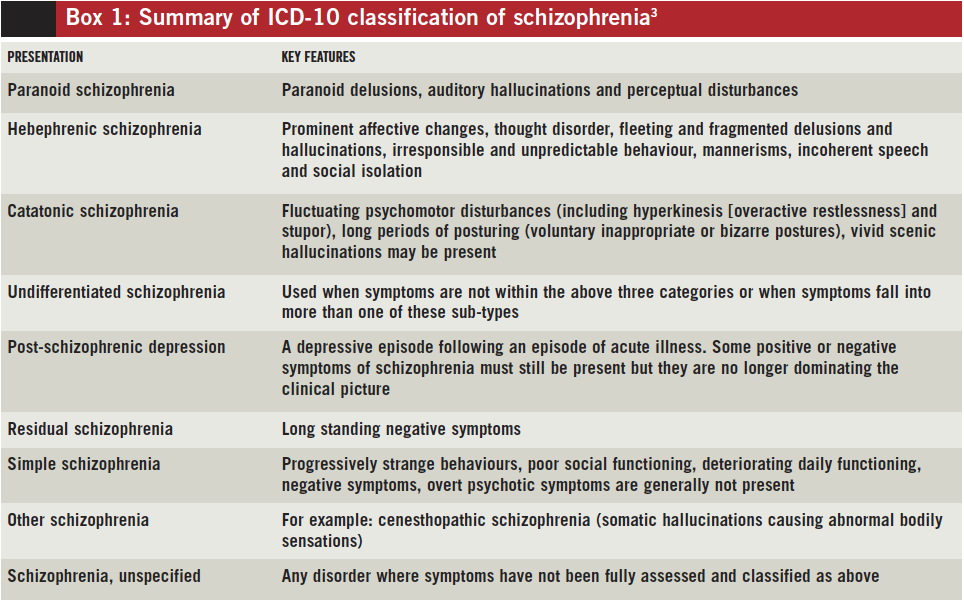
An essential feature of the affective status of patients with schizophrenia according to E. Bleuler [4] is the frequent lack of unity in the expression of affect: words do not fit the tone of voice, movements. Facial expressions also lack unity: the forehead rises as if in the affect of surprise, smile wrinkles scatter from the corners of the eyes, and the corners of the mouth sadly fall (a variant of "paramimia"). There is also a defect in the ability to modulate: the insufficiency of the correspondence of affect to the changing content of thinking. It happens that in the presence of distinct fluctuations of affect, there is still a “frozen” affect: even if the corners of the mouth rise with one affect and fall with another, both affects have something in common. Also, people with schizophrenia tend to experience anger and discontent longer than healthy people. And patients with schizophrenia sometimes manage to retain long-standing affective memories much better and longer than healthy ones (“preservation” of affect).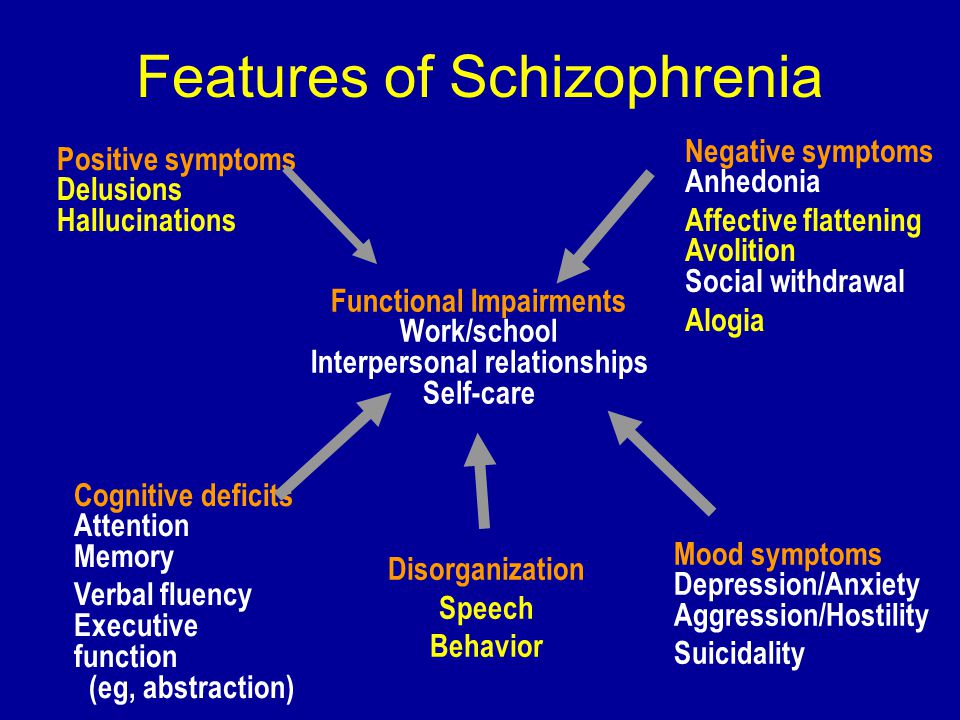 It happens that the only expression of feelings in patients with schizophrenia, except for irritability, is parental love, but sympathy for others does not always “extinguish”, in the hospital some patients with schizophrenia can very well feel into the position of other patients, among them there are those capable of such a “Samaritan care that no healthy person is capable of. Patients with schizophrenia, poets and musicians are able to feel into others through art.
It happens that the only expression of feelings in patients with schizophrenia, except for irritability, is parental love, but sympathy for others does not always “extinguish”, in the hospital some patients with schizophrenia can very well feel into the position of other patients, among them there are those capable of such a “Samaritan care that no healthy person is capable of. Patients with schizophrenia, poets and musicians are able to feel into others through art.
Although, on the whole, in moral terms, schizophrenic patients can be trusted no more and no less than healthy people, yet patients steal and cheat less than healthy people. E. Bleuler [4] noted that in schizophrenia there are also defects in the senses "regulating the communication of people with each other." So, whether patients speak with a higher or lower status, a man or a woman, it makes no difference to them. Often there is no sense of shame in patients who are otherwise quite well preserved. Such patients may, without any reason, begin to say shameful things, to speak in an extremely rude way about their sexual relations.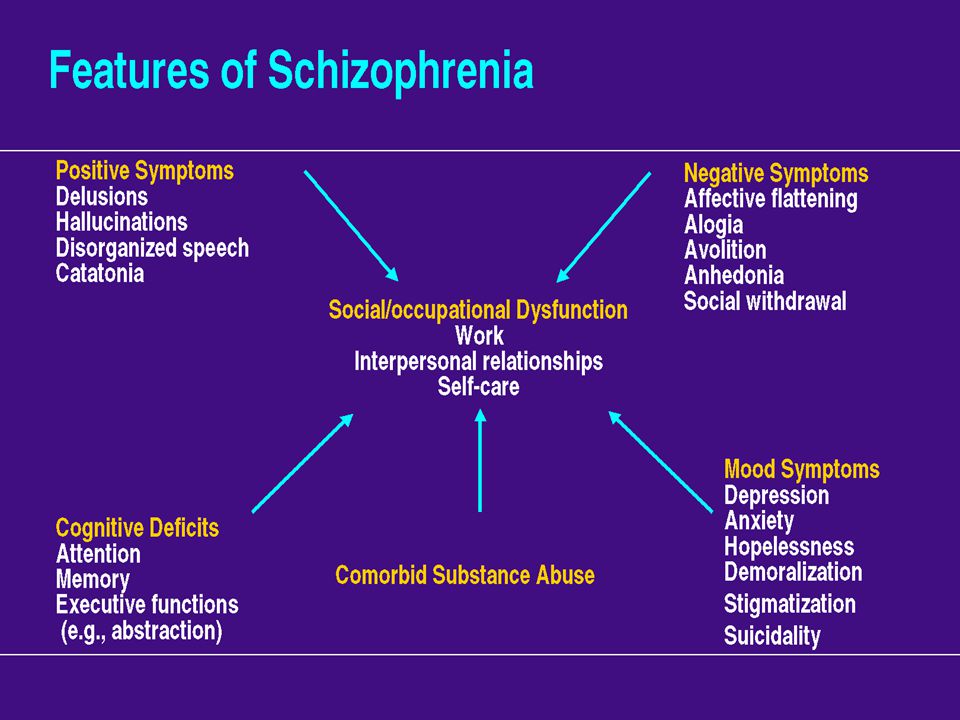 Contrasts in feelings are also possible: with a severe defect in some of the senses, there is a lively sensual emphasis on any trifles: for example, an old maid is embarrassed to tell the doctor her age, but eats her excrement.
Contrasts in feelings are also possible: with a severe defect in some of the senses, there is a lively sensual emphasis on any trifles: for example, an old maid is embarrassed to tell the doctor her age, but eats her excrement.
As a prominent affective main symptom of schizophrenia, apart from those listed above, E. Bleuler [4] described the phenomenon of "parathymia": the ability of patients to respond to sad news with gaiety or laughter, to pleasant or indifferent to others - sadness or irritability. Sometimes patients attach erotic feelings to something or someone who seems clearly unsuitable for this: they can fall in love with neighboring patients without regard to their gender and external deformity. E. Bleuler also attributed loud laughter for no reason to parathymia. In the field of taste and smell, parathymia can manifest itself in the fact that patients swallow with pleasure things that would only cause discomfort in healthy people: beetles, sawdust, wires, spoons, earth, gasoline, and often their own excrement. E. Bleuler also mentioned possible dissociations in individual components of facial expressions: voice, posture, movements of arms and legs.
E. Bleuler also mentioned possible dissociations in individual components of facial expressions: voice, posture, movements of arms and legs.
As a direct consequence of schizophrenic disorder of associations, E. Bleuler considered another important "basic" symptom of schizophrenia - " ambivalence" , which he defined as "the tendency of the schizophrenic psyche to supply various "psychisms" with both negative and positive signs." At the same time, he singled out three forms of ambivalence: affective (while emphasizing the presentation with pleasant and unpleasant feelings), strong-willed , or ambivalence (for example, the patient wants and does not want to eat, seeks to be discharged from the hospital and resists being discharged, etc.), and intellectual (when almost the same words are given the opposite meaning in two sentences). E. Bleuler noted that affective and volitional ambivalence cannot be sharply separated from each other, since they represent “sides of a single function”, just as, however, it is difficult to distinguish intellectual “opposites” from affective ones.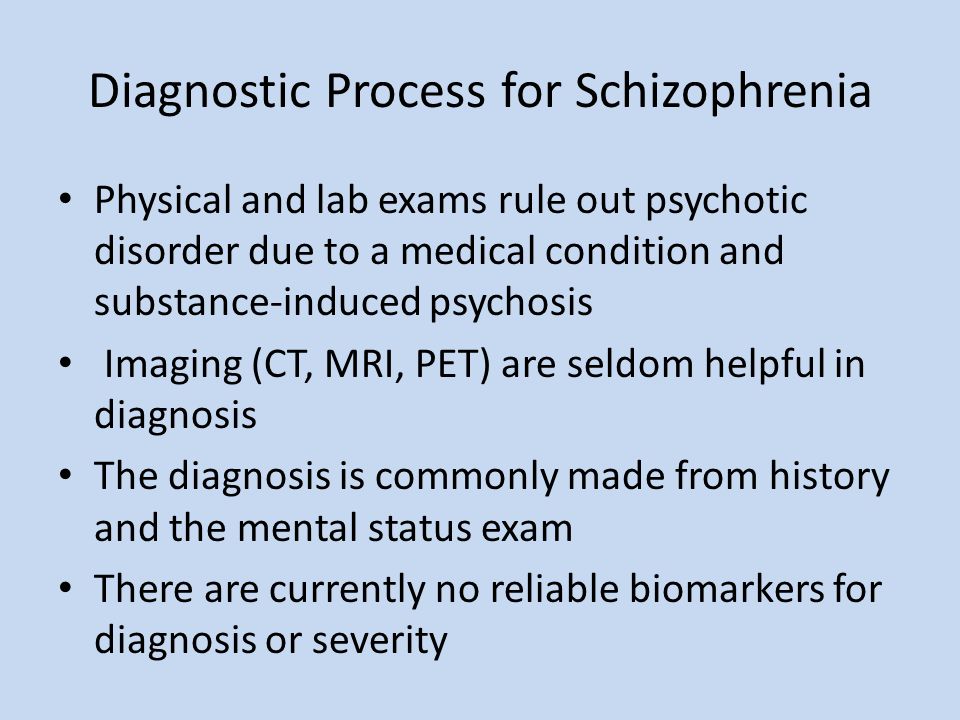
E. Bleuler [4] called the painful predominance of the inner world over the outer one " autism ", considered it as a disorder of consciousness 6 and unlike elementary "basic" disorders of associations and affectivity - as a "basic" disorder complex mental functions. Conceptually, E. Bleuler compared autism with the concept of "autoeroticism" by S. Freud and "loss of the sense of the real" by P. Janet [44]. The latter comparison gives rise to some modern authors [45] to assert that the concept of "psychasthenia", presented by P. Janet, had a much greater influence on E. Bleuler in the psychological analysis of the symptoms of schizophrenia than the psychoanalysis of neuroses by S. Freud. However, E. Bleuler himself [4] emphasized the influence of S. Freud and the psychoanalytic school, especially since the followers of S. Freud (C. Jung, F. Riklin and K. Abraham) worked under the direction of E. Bleuler at the Burghoelzli clinic. At the same time, P. Janet's "loss of a sense of reality", according to E. Bleuler, represents the "negative" side of what the term "autism" defines mainly "positively". The severe cases of "psychasthenia" described by P. Janet are, from the point of view of E. Bleuler, schizophrenia. Although the sense of reality never "denies completely in patients with schizophrenia, but only in relation to phenomena that are in conflict with their" complexes ". In cases where reality becomes identical to the patient's morbid formations, it is often ignored: for example, a schizophrenic patient loves a certain person, but when it appears before him in reality, he remains indifferent; the patient's desires revolve around being discharged from the hospital, although the actual discharge does not affect his feelings at all.
Janet's "loss of a sense of reality", according to E. Bleuler, represents the "negative" side of what the term "autism" defines mainly "positively". The severe cases of "psychasthenia" described by P. Janet are, from the point of view of E. Bleuler, schizophrenia. Although the sense of reality never "denies completely in patients with schizophrenia, but only in relation to phenomena that are in conflict with their" complexes ". In cases where reality becomes identical to the patient's morbid formations, it is often ignored: for example, a schizophrenic patient loves a certain person, but when it appears before him in reality, he remains indifferent; the patient's desires revolve around being discharged from the hospital, although the actual discharge does not affect his feelings at all.
E. Bleuler [4] emphasizes that autism is invisible at first sight, the patient's behavior may not be unusual at first. Patients with schizophrenia may maintain a good daily connection with the outside world, but keep their "complexes" in themselves, not wanting anyone from the outside to touch them.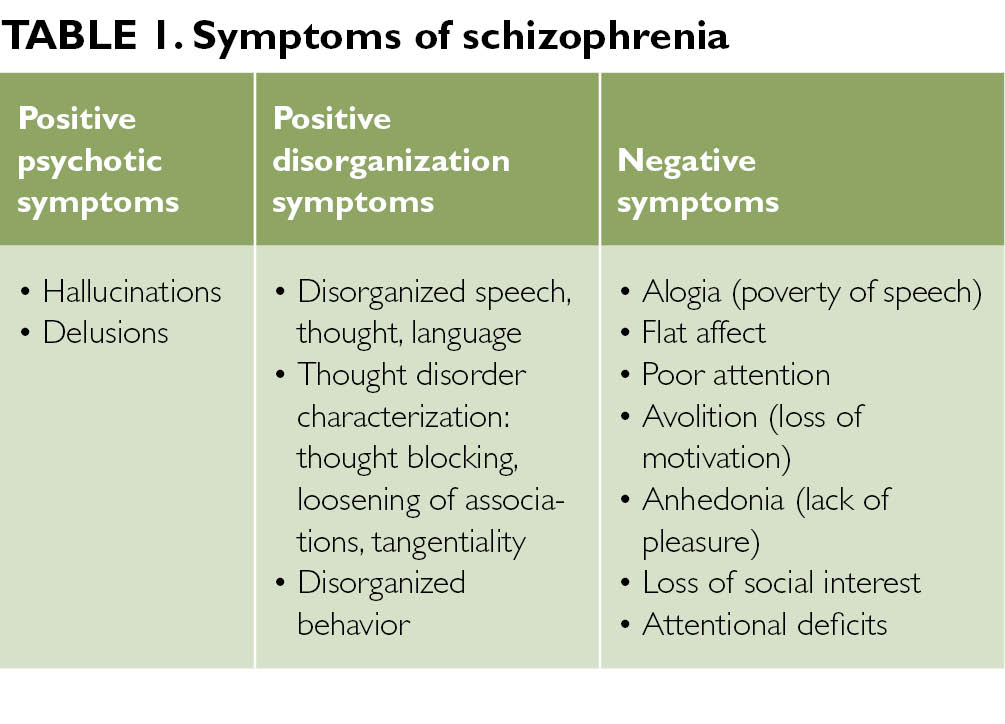 In other patients, autism also manifests itself outwardly: they usually sit with their backs turned, looking at empty walls, close their senses, pull a blanket over themselves, etc. There may be a poor distinction between autistic ideas and reality, and sometimes a clear preference for the autistic world (“another reality”) with subjective assessment of reality as a hallucination. E. Bleuler [4] gave another definition of autism - "inability to reckon with reality" and also considered autism an inappropriate reaction to external influences (irritability) and a lack of resistance to any ideas and drives. At the same time, he noted that many patients may appear less autistic than they are, due to the fact that they suppress autistic thinking and act according to reality. Autistic thinking uses the laws of logic as long as they suit it, since it is controlled by affective needs. The same patient has realistic and autistic thinking, from autistic thinking come delusions, gross logical inconsistencies and other painful symptoms.
In other patients, autism also manifests itself outwardly: they usually sit with their backs turned, looking at empty walls, close their senses, pull a blanket over themselves, etc. There may be a poor distinction between autistic ideas and reality, and sometimes a clear preference for the autistic world (“another reality”) with subjective assessment of reality as a hallucination. E. Bleuler [4] gave another definition of autism - "inability to reckon with reality" and also considered autism an inappropriate reaction to external influences (irritability) and a lack of resistance to any ideas and drives. At the same time, he noted that many patients may appear less autistic than they are, due to the fact that they suppress autistic thinking and act according to reality. Autistic thinking uses the laws of logic as long as they suit it, since it is controlled by affective needs. The same patient has realistic and autistic thinking, from autistic thinking come delusions, gross logical inconsistencies and other painful symptoms. In some patients the patterns of thought are well separated, in others they are mixed. The employment of patients with hebephrenia with "higher issues" E. Bleuler also attributed to autistic thinking. Note that E. Bleuler, referred to in modern psychiatry as “depersonalization” disorders, also partially considered them as a manifestation of autism, referring to “unconscious” autistic thinking: “intelligent patients can feel the difference with the previous, pre-morbid period for years, often experience it as something unpleasant (less than pleasant). They complain that reality looks different than before, things and people no longer mean what they used to mean, that people are different, “strangers” and have nothing to do with them. According to E. Bleuler [4], autistic thinking (as well as realistic thinking) can be conscious and unconscious. There are also autistic feeling that turns away from reality.
In some patients the patterns of thought are well separated, in others they are mixed. The employment of patients with hebephrenia with "higher issues" E. Bleuler also attributed to autistic thinking. Note that E. Bleuler, referred to in modern psychiatry as “depersonalization” disorders, also partially considered them as a manifestation of autism, referring to “unconscious” autistic thinking: “intelligent patients can feel the difference with the previous, pre-morbid period for years, often experience it as something unpleasant (less than pleasant). They complain that reality looks different than before, things and people no longer mean what they used to mean, that people are different, “strangers” and have nothing to do with them. According to E. Bleuler [4], autistic thinking (as well as realistic thinking) can be conscious and unconscious. There are also autistic feeling that turns away from reality.
In The Theory of Symptoms, E. Bleuler [4] developed the concept of "primary" symptoms of schizophrenia in more detail, emphasizing their difference from the "basic" ones.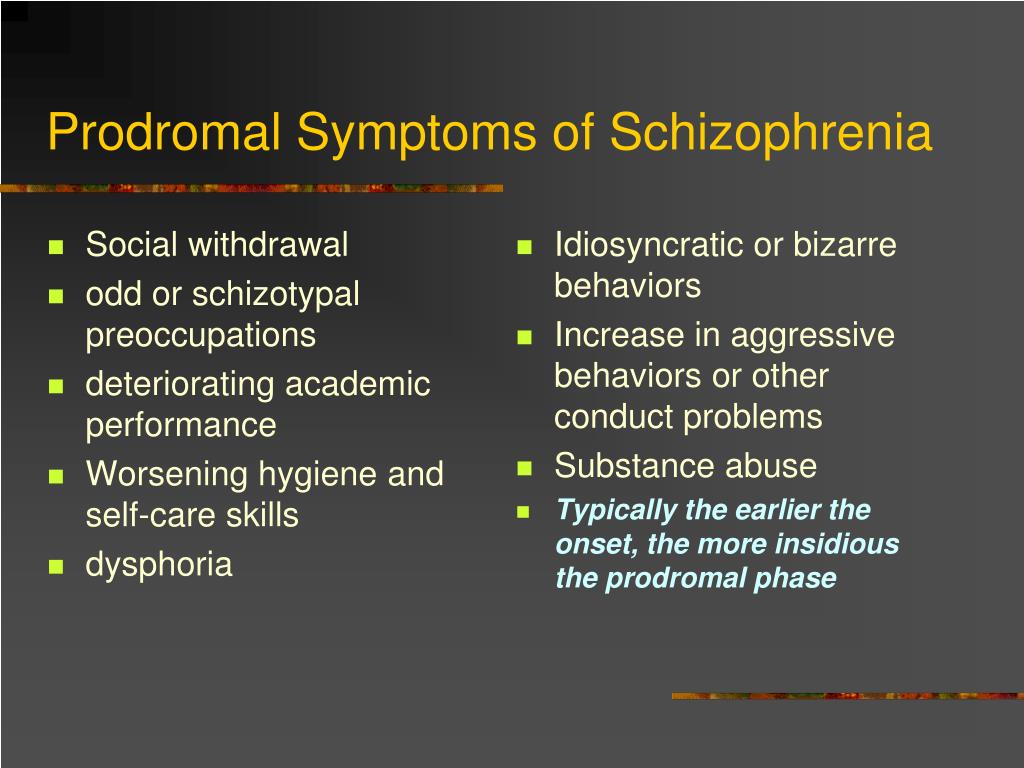 Unfortunately, the confusion in understanding Bleuler's "basic" and "primary" symptoms, even in highly professional manuals on psychiatry, as noted by the French psychiatrist P. Pichot [46], continues for many decades.
Unfortunately, the confusion in understanding Bleuler's "basic" and "primary" symptoms, even in highly professional manuals on psychiatry, as noted by the French psychiatrist P. Pichot [46], continues for many decades.
Thus, according to E. Bleuler [4], the primary symptoms are a direct expression of schizophrenic brain damage (of an organic nature). With a high probability, a part of “simple phenomena” belongs to them, first of all, a part of associative disorders. Sometimes such associative disorders are accompanied by somatic symptoms characteristic of an infection or autointoxication: coated dry tongue, indigestion, weight loss, weakness, severe tremor, periodic fever, leukocytosis. Associative disorder, in which we are talking about the reduction and leveling of affinity (habitual) associative paths (from a small degree of associative splitting to confusion in acute schizophrenic attacks with a complete breakdown of the train of thought, when even the concepts of "father" and "mother" are blurred), is, according to E.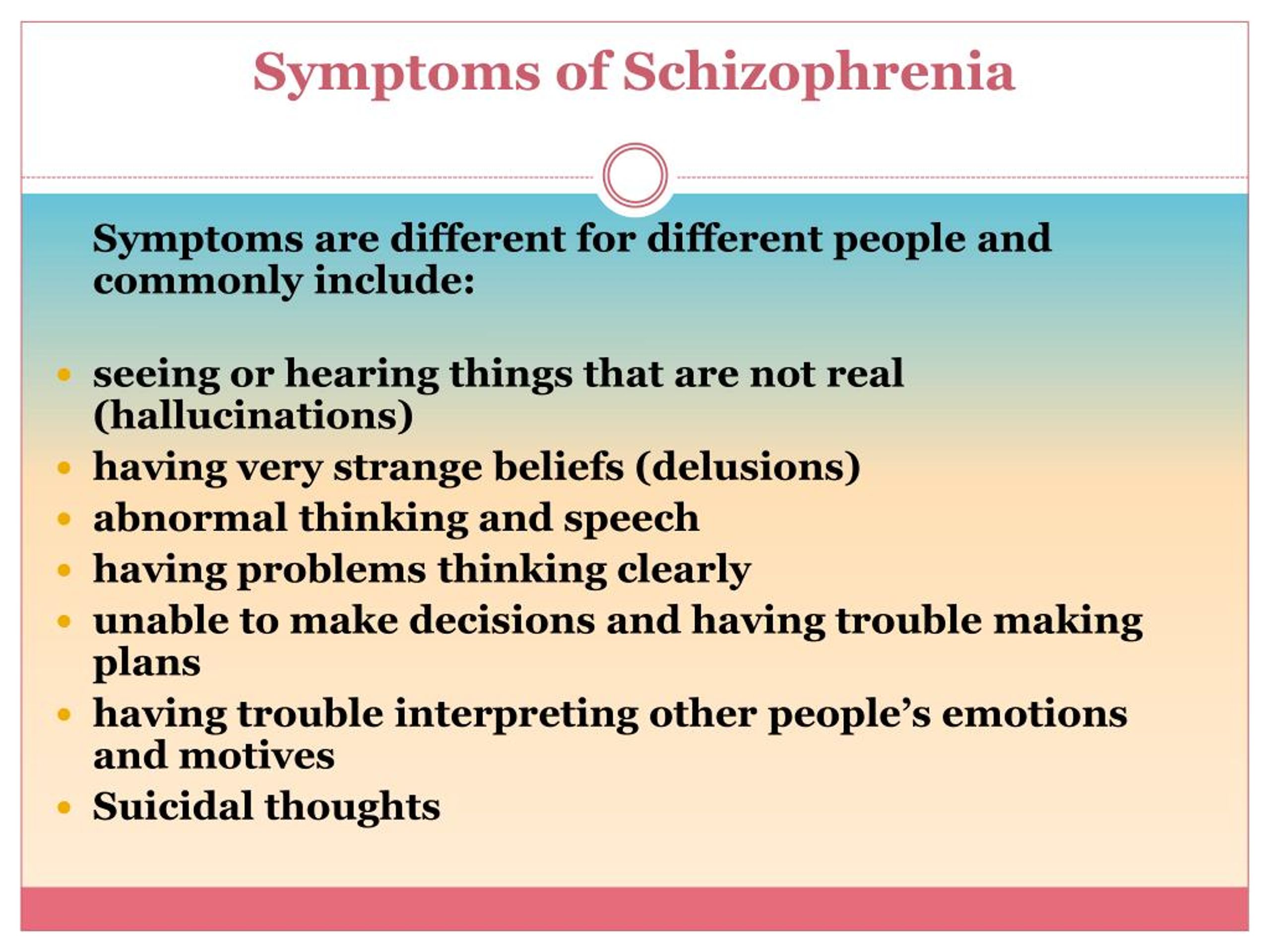 Bleuler [4], a “primary” (direct) symptom, and sperrings and systematic splittings are “secondary”. At the same time, sperrungs are the most specific "basic" symptoms of schizophrenia. Secondary (indirect) symptoms do not indicate a simultaneous change in the organic disease process, and a change in the intensity of the primary symptoms to a certain extent reflects changes in the intensity of the organic schizophrenic process. As E. Bleuler emphasizes, all the described symptomatology dementia praecox is secondary, "accidental". Therefore, the disease can be asymptomatic for a long time.
Bleuler [4], a “primary” (direct) symptom, and sperrings and systematic splittings are “secondary”. At the same time, sperrungs are the most specific "basic" symptoms of schizophrenia. Secondary (indirect) symptoms do not indicate a simultaneous change in the organic disease process, and a change in the intensity of the primary symptoms to a certain extent reflects changes in the intensity of the organic schizophrenic process. As E. Bleuler emphasizes, all the described symptomatology dementia praecox is secondary, "accidental". Therefore, the disease can be asymptomatic for a long time.
E. Bleuler [4] also believed that the “impression of primary” symptoms is created by states of “stupefaction”. Usually, even with them, a relatively rough tremor, loss of strength and a certain awkwardness of movements are observed. Possibly the stupefaction is also a "direct" symptom of the cerebral schizophrenic process. Similarly, melancholic and manic episodes, which are not "basic", but always "accessory" symptoms, can at the same time be "primary" symptoms of schizophrenia.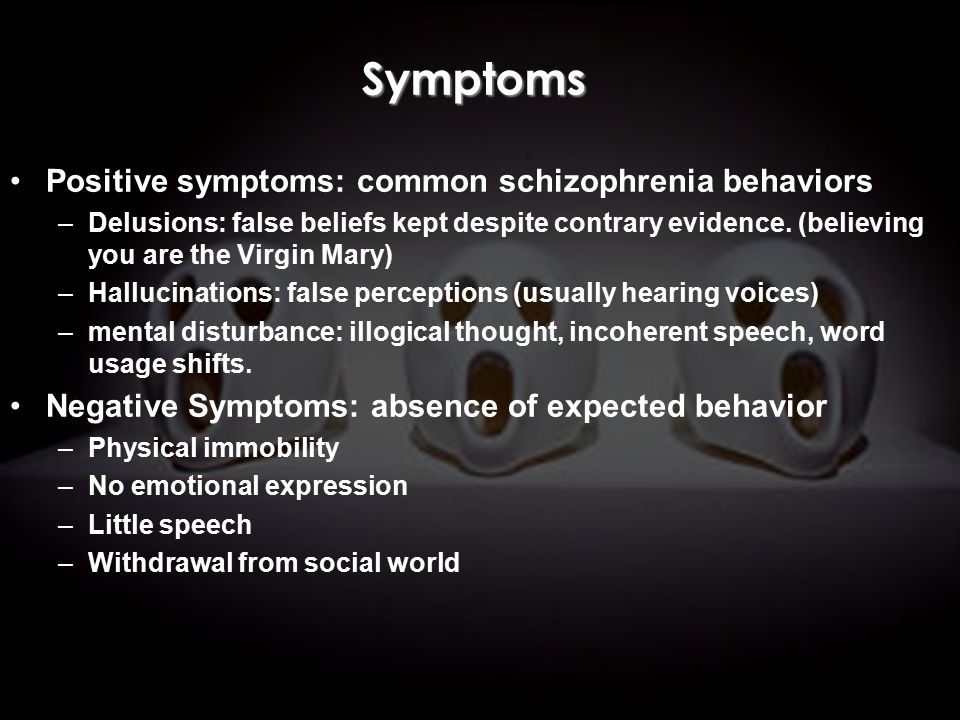 "The affective waves in schizophrenia are conditioned in some organic way." This is especially true for manic attacks, since melancholic states can also develop secondarily (i.e., psychogenic) - as a reaction to the consciousness of an illness or a state of fear.
"The affective waves in schizophrenia are conditioned in some organic way." This is especially true for manic attacks, since melancholic states can also develop secondarily (i.e., psychogenic) - as a reaction to the consciousness of an illness or a state of fear.
Unlike M. Jahrmaerker [23], E. Bleuler [3, 4] did not attribute the disposition to hallucinations to the primary symptoms in schizophrenia, but assumed its existence in any psyche, which is confirmed by dreams, hallucinations during poisoning, other organic brain processes, obliteration of representation and perception in people of art. In schizophrenia, the reduction in the difference between reality and representation is also due to splitting.
Part of the catatonic symptoms, namely chronic catatonic symptoms, which E. Bleuler [4] considered as an "undoubted" bad prognostic sign, and catatonic attacks, especially accompanied by the development of paresis in certain muscle groups (organic symptoms), are also primary.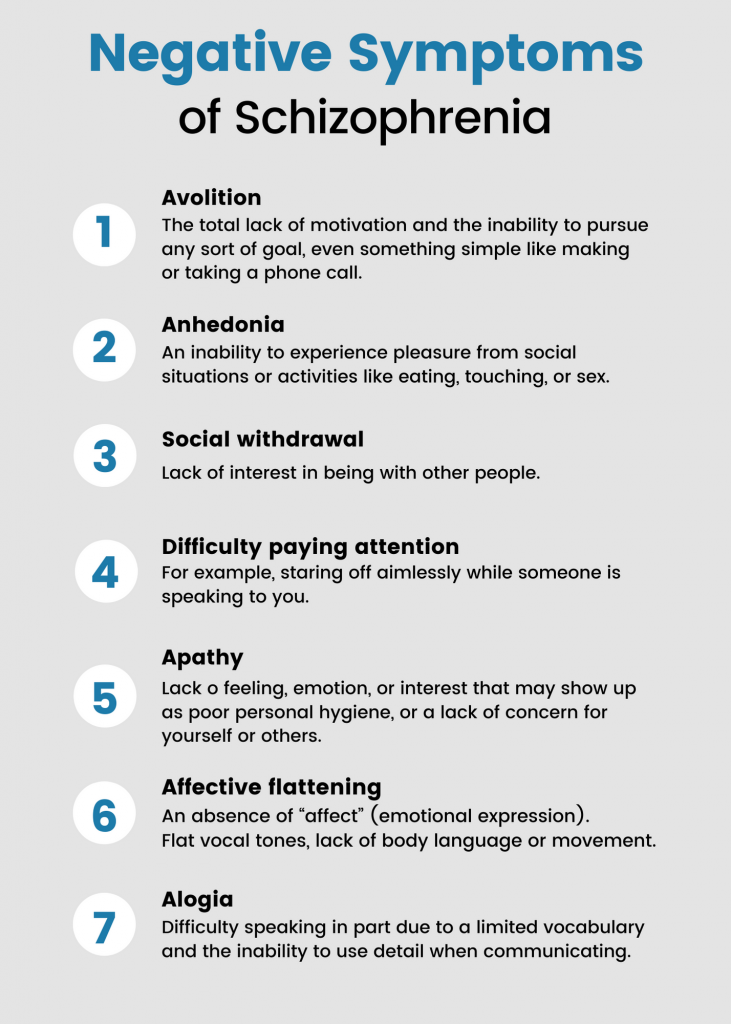 Their psychogenic origin is ruled out in most cases, even if one does not take into account that catatonic seizures are often indistinguishable from apoplectic and epileptic ones. Also, the primary symptom is a disposition to stereotypes.
Their psychogenic origin is ruled out in most cases, even if one does not take into account that catatonic seizures are often indistinguishable from apoplectic and epileptic ones. Also, the primary symptom is a disposition to stereotypes.
According to E. Bleuler [4], from the actual “bodily” to the primary symptoms in schizophrenia, “phenomena of paralysis and metabolic disorders” in fatal cases of schizophrenia, “organic”, primary symptoms may also include anisocoria (difference in pupil size) , which is indirectly confirmed by the data of M.-E. Zablocka [22] about the worst prognosis in anisocoria. Tremor, not dependent on excitation and tension, and fibrillar twitches E. Bleuler unequivocally attributed to organic symptoms; they are also likely to include an increase in ideomuscular excitability, as well as persistent headaches and dizziness, the latter not only often accompany the manifestation of the disease, but also precede it. Vasomotor disorders may be secondary, but without showing any connection with affectivity or limited to only certain parts of the body, they can be a direct symptom of a disorder of the nervous system (ie, primary).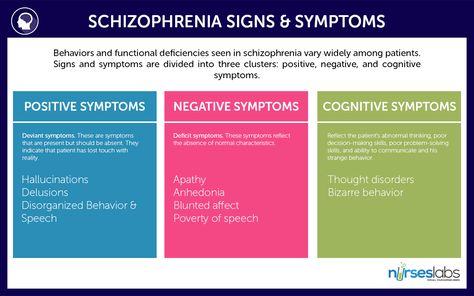 Part of the edema can also be a direct expression of the disease process.
Part of the edema can also be a direct expression of the disease process.
Secondary or secondary symptoms are a direct consequence of the loosening ("Lockerung") of associations: this is the use of "pieces" of concepts in thinking with incorrect results, displacement, symbolization, condensation and fragmentation of thinking. Sperrungs are also a secondary symptom, since they depend on psychic influences both in occurrence and termination.
E. Bleuler [4] sometimes assessed systematic splitting as a secondary symptom, and sometimes as a primary one (capable of being in direct connection with the disease process), and the “organic” character is more pronounced in acute cases. However, in his opinion, a completely different split ("Spaltung") is much more striking: the decomposition of complex mental formations in an irregular way. For example, associations concerning scientific problems flow flawlessly, while elementary ones are suppressed. This is a splitting of a purely mental genesis (secondary, secondary, symptom): the functions that come into conflict with the known affective needs of the patient are upset.