When does sad start
Seasonal affective disorder (SAD) - Symptoms and causes
Overview
Seasonal affective disorder (SAD) is a type of depression that's related to changes in seasons — SAD begins and ends at about the same times every year. If you're like most people with SAD, your symptoms start in the fall and continue into the winter months, sapping your energy and making you feel moody. These symptoms often resolve during the spring and summer months. Less often, SAD causes depression in the spring or early summer and resolves during the fall or winter months.
Treatment for SAD may include light therapy (phototherapy), psychotherapy and medications.
Don't brush off that yearly feeling as simply a case of the "winter blues" or a seasonal funk that you have to tough out on your own. Take steps to keep your mood and motivation steady throughout the year.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
In most cases, seasonal affective disorder symptoms appear during late fall or early winter and go away during the sunnier days of spring and summer. Less commonly, people with the opposite pattern have symptoms that begin in spring or summer. In either case, symptoms may start out mild and become more severe as the season progresses.
Signs and symptoms of SAD may include:
- Feeling listless, sad or down most of the day, nearly every day
- Losing interest in activities you once enjoyed
- Having low energy and feeling sluggish
- Having problems with sleeping too much
- Experiencing carbohydrate cravings, overeating and weight gain
- Having difficulty concentrating
- Feeling hopeless, worthless or guilty
- Having thoughts of not wanting to live
Fall and winter SAD
Symptoms specific to winter-onset SAD, sometimes called winter depression, may include:
- Oversleeping
- Appetite changes, especially a craving for foods high in carbohydrates
- Weight gain
- Tiredness or low energy
Spring and summer SAD
Symptoms specific to summer-onset seasonal affective disorder, sometimes called summer depression, may include:
- Trouble sleeping (insomnia)
- Poor appetite
- Weight loss
- Agitation or anxiety
- Increased irritability
Seasonal changes and bipolar disorder
People who have bipolar disorder are at increased risk of seasonal affective disorder. In some people with bipolar disorder, episodes of mania may be linked to a specific season. For example, spring and summer can bring on symptoms of mania or a less intense form of mania (hypomania), anxiety, agitation and irritability. They may also experience depression during the fall and winter months.
In some people with bipolar disorder, episodes of mania may be linked to a specific season. For example, spring and summer can bring on symptoms of mania or a less intense form of mania (hypomania), anxiety, agitation and irritability. They may also experience depression during the fall and winter months.
When to see a doctor
It's normal to have some days when you feel down. But if you feel down for days at a time and you can't get motivated to do activities you normally enjoy, see your health care provider. This is especially important if your sleep patterns and appetite have changed, you turn to alcohol for comfort or relaxation, or you feel hopeless or think about suicide.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
The specific cause of seasonal affective disorder remains unknown. Some factors that may come into play include:
- Your biological clock (circadian rhythm). The reduced level of sunlight in fall and winter may cause winter-onset SAD. This decrease in sunlight may disrupt your body's internal clock and lead to feelings of depression.

- Serotonin levels. A drop in serotonin, a brain chemical (neurotransmitter) that affects mood, might play a role in SAD. Reduced sunlight can cause a drop in serotonin that may trigger depression.
- Melatonin levels. The change in season can disrupt the balance of the body's level of melatonin, which plays a role in sleep patterns and mood.
Risk factors
Seasonal affective disorder is diagnosed more often in women than in men. And SAD occurs more frequently in younger adults than in older adults.
Factors that may increase your risk of seasonal affective disorder include:
- Family history. People with SAD may be more likely to have blood relatives with SAD or another form of depression.
- Having major depression or bipolar disorder. Symptoms of depression may worsen seasonally if you have one of these conditions.
- Living far from the equator. SAD appears to be more common among people who live far north or south of the equator. This may be due to decreased sunlight during the winter and longer days during the summer months.
- Low level of vitamin D. Some vitamin D is produced in the skin when it's exposed to sunlight. Vitamin D can help to boost serotonin activity. Less sunlight and not getting enough vitamin D from foods and other sources may result in low levels of vitamin D in the body.
Complications
Take signs and symptoms of seasonal affective disorder seriously. As with other types of depression, SAD can get worse and lead to problems if it's not treated. These can include:
- Social withdrawal
- School or work problems
- Substance abuse
- Other mental health disorders such as anxiety or eating disorders
- Suicidal thoughts or behavior
Prevention
There's no known way to prevent the development of seasonal affective disorder. However, if you take steps early on to manage symptoms, you may be able to prevent them from getting worse over time. You may be able to head off serious changes in mood, appetite and energy levels, as you can predict the time of the year in which these symptoms may start. Treatment can help prevent complications, especially if SAD is diagnosed and treated before symptoms get bad.
However, if you take steps early on to manage symptoms, you may be able to prevent them from getting worse over time. You may be able to head off serious changes in mood, appetite and energy levels, as you can predict the time of the year in which these symptoms may start. Treatment can help prevent complications, especially if SAD is diagnosed and treated before symptoms get bad.
Some people find it helpful to begin treatment before symptoms would normally start in the fall or winter, and then continue treatment past the time symptoms would normally go away. Other people need continuous treatment to prevent symptoms from returning.
By Mayo Clinic Staff
Related
Associated Procedures
News from Mayo Clinic
Products & Services
NIMH » Seasonal Affective Disorder
What is seasonal affective disorder?
Many people go through short periods of time where they feel sad or not like their usual selves. Sometimes, these mood changes begin and end when the seasons change. People may start to feel “down” when the days get shorter in the fall and winter (also called “winter blues”) and begin to feel better in the spring, with longer daylight hours.
Sometimes, these mood changes begin and end when the seasons change. People may start to feel “down” when the days get shorter in the fall and winter (also called “winter blues”) and begin to feel better in the spring, with longer daylight hours.
In some cases, these mood changes are more serious and can affect how a person feels, thinks, and handles daily activities. If you have noticed significant changes in your mood and behavior whenever the seasons change, you may be suffering from seasonal affective disorder (SAD), a type of depression.
In most cases, SAD symptoms start in the late fall or early winter and go away during the spring and summer; this is known as winter-pattern SAD or winter depression. Some people may experience depressive episodes during the spring and summer months; this is called summer-pattern SAD or summer depression and is less common.
What are the signs and symptoms of SAD?
SAD is not considered a separate disorder but is a type of depression characterized by its recurrent seasonal pattern, with symptoms lasting about 4 to 5 months per year. Therefore, the signs and symptoms of SAD include those associated with major depression, and some specific symptoms that differ for winter-pattern and summer-pattern SAD. Not every person with SAD will experience all of the symptoms listed below.
Therefore, the signs and symptoms of SAD include those associated with major depression, and some specific symptoms that differ for winter-pattern and summer-pattern SAD. Not every person with SAD will experience all of the symptoms listed below.
Symptoms of major depression may include:
- Feeling depressed most of the day, nearly every day
- Losing interest in activities you once enjoyed
- Experiencing changes in appetite or weight
- Having problems with sleep
- Feeling sluggish or agitated
- Having low energy
- Feeling hopeless or worthless
- Having difficulty concentrating
- Having frequent thoughts of death or suicide
For winter-pattern SAD, additional specific symptoms may include:
- Oversleeping (hypersomnia)
- Overeating, particularly with a craving for carbohydrates
- Weight gain
- Social withdrawal (feeling like “hibernating”)
Specific symptoms for summer-pattern SAD may include:
- Trouble sleeping (insomnia)
- Poor appetite, leading to weight loss
- Restlessness and agitation
- Anxiety
- Episodes of violent behavior
Get Immediate Help
If you or someone you know is in immediate distress or is thinking about hurting themselves, call the National Suicide Prevention Lifeline toll-free at 1-800-273-TALK (8255). You also can text the Crisis Text Line (HELLO to 741741) or use the Lifeline Chat on the National Suicide Prevention Lifeline website.
You also can text the Crisis Text Line (HELLO to 741741) or use the Lifeline Chat on the National Suicide Prevention Lifeline website.
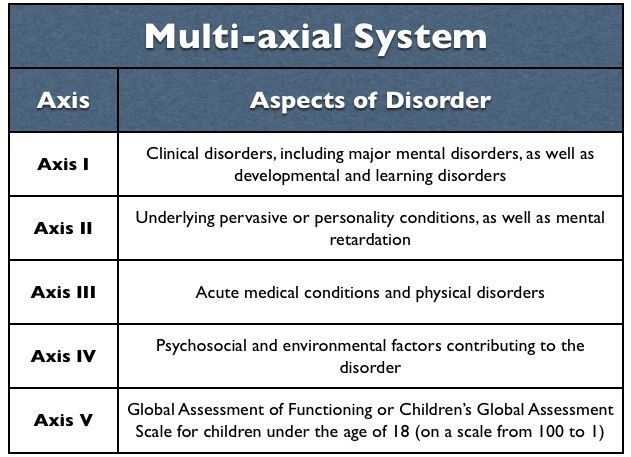
How is SAD diagnosed?
If you think you may be suffering from SAD, talk to your health care provider or a mental health specialist about your concerns. They may have you fill out specific questionnaires to determine if your symptoms meet the criteria for SAD.
To be diagnosed with SAD, a person must meet the following criteria:
- They must have symptoms of major depression or the more specific symptoms listed above.
- The depressive episodes must occur during specific seasons (i.e., only during the winter months or the summer months) for at least 2 consecutive years. However, not all people with SAD do experience symptoms every year.
- The episodes must be much more frequent than other depressive episodes that the person may have had at other times of the year during their lifetime.
Who develops SAD?
Millions of American adults may suffer from SAD, although many may not know they have the condition. SAD occurs much more often in women than in men, and it is more common in those living farther north, where there are shorter daylight hours in the winter. For example, people living in Alaska or New England may be more likely to develop SAD than people living in Florida. In most cases, SAD begins in young adulthood.
SAD is more common in people with major depressive disorder or bipolar disorder, especially bipolar II disorder, which is associated with recurrent depressive and hypomanic episodes (less severe than the full-blown manic episodes typical of bipolar I disorder). Additionally, people with SAD tend to have other mental disorders, such as attention-deficit/hyperactivity disorder, an eating disorder, an anxiety disorder, or panic disorder. Learn more about these disorders by visiting the NIMH Mental Health Information page.
SAD sometimes runs in families. SAD is more common in people who have relatives with other mental illnesses, such as major depression or schizophrenia.
SAD is more common in people who have relatives with other mental illnesses, such as major depression or schizophrenia.
What causes SAD?
Scientists do not fully understand what causes SAD. Research indicates that people with SAD may have reduced activity of the brain chemical (neurotransmitter) serotonin, which helps regulate mood. Research also suggests that sunlight controls the levels of molecules that help maintain normal serotonin levels, but in people with SAD, this regulation does not function properly, resulting in decreased serotonin levels in the winter.
Other findings suggest that people with SAD produce too much melatonin—a hormone that is central for maintaining the normal sleep-wake cycle. Overproduction of melatonin can increase sleepiness.
Both serotonin and melatonin help maintain the body’s daily rhythm that is tied to the seasonal night-day cycle. In people with SAD, the changes in serotonin and melatonin levels disrupt the normal daily rhythms. As a result, they can no longer adjust to the seasonal changes in day length, leading to sleep, mood, and behavior changes.
As a result, they can no longer adjust to the seasonal changes in day length, leading to sleep, mood, and behavior changes.
Deficits in vitamin D may exacerbate these problems because vitamin D is believed to promote serotonin activity. In addition to vitamin D consumed with diet, the body produces vitamin D when exposed to sunlight on the skin. With less daylight in the winter, people with SAD may have lower vitamin D levels, which may further hinder serotonin activity.
Negative thoughts and feelings about the winter and its associated limitations and stresses are common among people with SAD (as well as others). It is unclear whether these are "causes" or "effects" of the mood disorder, but they can be a useful focus of treatment.
How is SAD treated?
Treatments are available that can help many people with SAD. They fall into four main categories that may be used alone or in combination:
- Light therapy
- Psychotherapy
- Antidepressant medications
- Vitamin D
Talk to your health care provider about which treatment, or combination of treatments, is best for you. For tips for talking with your health care provider, refer to the NIMH fact sheet, Taking Control of Your Mental Health: Tips for Talking With Your Health Care Provider.
For tips for talking with your health care provider, refer to the NIMH fact sheet, Taking Control of Your Mental Health: Tips for Talking With Your Health Care Provider.
Light Therapy
Since the 1980s, light therapy has been a mainstay for the treatment of SAD. It aims to expose people with SAD to a bright light every day to make up for the diminished natural sunshine in the darker months.
For this treatment, the person sits in front of a very bright light box (10,000 lux) every day for about 30 to 45 minutes, usually first thing in the morning, from fall to spring. The light boxes, which are about 20 times brighter than ordinary indoor light, filter out the potentially damaging UV light, making this a safe treatment for most. However, people with certain eye diseases or people taking certain medications that increase sensitivity to sunlight may need to use alternative treatments or use light therapy under medical supervision.
Psychotherapy or “Talk Therapy”
Cognitive behavioral therapy (CBT) is a type of talk therapy aimed at helping people learn how to cope with difficult situations; CBT also has been adapted for people with SAD (CBT-SAD). It is typically conducted in two weekly group sessions for 6 weeks and focuses on replacing negative thoughts related to the winter season (e.g., about the darkness of winter) with more positive thoughts. CBT-SAD also uses a process called behavioral activation, which helps individuals identify and schedule pleasant, engaging indoor or outdoor activities to combat the loss of interest they typically experience in the winter.
It is typically conducted in two weekly group sessions for 6 weeks and focuses on replacing negative thoughts related to the winter season (e.g., about the darkness of winter) with more positive thoughts. CBT-SAD also uses a process called behavioral activation, which helps individuals identify and schedule pleasant, engaging indoor or outdoor activities to combat the loss of interest they typically experience in the winter.
When researchers directly compared CBT with light therapy, both treatments were equally effective in improving SAD symptoms. Some symptoms seemed to get better a little faster with light therapy than with CBT. However, a long-term study that followed SAD patients for two winters found that the positive effects of CBT seemed to last longer over time.
Medications
Because SAD, like other types of depression, is associated with disturbances in serotonin activity, antidepressant medications called selective serotonin reuptake inhibitors (SSRIs) are also used to treat SAD when symptoms occur. These agents can significantly enhance patients' moods. Commonly used SSRIs include fluoxetine, citalopram, sertraline, paroxetine, and escitalopram.
These agents can significantly enhance patients' moods. Commonly used SSRIs include fluoxetine, citalopram, sertraline, paroxetine, and escitalopram.
The U.S. Food and Drug Administration (FDA) also has approved another type of antidepressant, bupropion, in an extended-release form, that can prevent recurrence of seasonal major depressive episodes when taken daily from the fall until the following early spring.
All medications can have side effects. Talk to your doctor about the possible risk of using these medications for your condition. You may need to try several different antidepressant medications before finding one that improves your symptoms without causing problematic side effects. For basic information about SSRIs, bupropion, and other mental health medications, visit the NIMH Mental Health Medications page. Also, visit the FDA website for the most up-to-date information on medications, side effects, and warnings.
Vitamin D
Because many people with SAD often have vitamin D deficiency, nutritional supplements of vitamin D may help improve their symptoms. However, studies testing whether vitamin D is effective in SAD treatment have produced mixed findings, with some results indicating that it is as effective as light therapy but others detecting no effect.
However, studies testing whether vitamin D is effective in SAD treatment have produced mixed findings, with some results indicating that it is as effective as light therapy but others detecting no effect.
Can SAD be prevented?
Because the timing of the onset of winter pattern-SAD is so predictable, people with a history of SAD might benefit from starting the treatments mentioned above before the fall to help prevent or reduce the depression. To date, very few studies have investigated this question, and existing studies have found no convincing evidence that starting light therapy or psychotherapy ahead of time could prevent the onset of depression. Only preventive treatment with the antidepressant bupropion prevented SAD in study participants, but it also had a higher risk of side effects. Therefore, people with SAD should discuss with their health care providers if they want to initiate treatment early to prevent depressive episodes.
Are there clinical trials studying SAD?
NIMH supports a wide range of research, including clinical trials that look at new ways to prevent, detect, or treat diseases and conditions—including SAD. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct clinical trials with patients and healthy volunteers. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you. For more information about clinical research and how to find clinical trials being conducted around the country, visit the NIMH Clinical Trials page.
Reprints
This publication is in the public domain and may be reproduced or copied without permission from NIMH. Citation of NIMH as a source is appreciated. To learn more about using NIMH publications, refer to our reprint guidelines.
Citation of NIMH as a source is appreciated. To learn more about using NIMH publications, refer to our reprint guidelines.
For More Information
MedlinePlus (En español)
ClinicalTrials.gov (En español)
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
National Institutes of Health
NIH Publication No. 20-MH-8138
I am constantly sad in the evening. Everything is fine with me?
Evening depression is a phenomenon that has nothing to do with your usual mood in life. We tell you why it is sad in the evening and whether something can be done about it.
Depression is a serious condition, which is characterized by mood swings, despondency, unreasonable sadness. Even if a person does not suffer from ordinary depression, he probably notices how the mood sometimes deteriorates in the evening. This often results in insomnia or sleep problems. A person breaks down on relatives or, conversely, closes in on himself and can sit and stare at the wall for an hour.
There are several reasons for evening sadness. First, banal fatigue. After a busy day, people sometimes feel overwhelmed and empty - and that's okay. The brain signals that it is time to stop, lie down and rest. Secondly, there are fewer events in the evening. All day long, a person works, chats with colleagues, plans things, listens to podcasts while riding the subway. In general, there is no time to be sad. And in the evening there is free time to delve into yourself, think about problems and do other unpleasant things. Thirdly, disturbed regimen and bad habits loosen the nervous system. A glass of alcohol or coffee after work increases the likelihood that you will suddenly be attacked by sadness at home.
Rumination often leads to a bad mood in the evening. In psychology, this is what they call “chewing mental gum”, that is, endless scrolling of past events in the head. For example, a difficult situation that happened the day before, or an unpleasant dialogue that ended in defeat for you. The only way to overcome rumination is through awareness. Allow yourself to feel, but don't dwell on the emotions.
The only way to overcome rumination is through awareness. Allow yourself to feel, but don't dwell on the emotions.
Walk with friends. After work, instead of sitting in a cafe, go for a walk in the park or look at paintings in the museum. If your friends are busy, invite your parents for a walk together.
Go to the cinema. Only for a positive film. Drama or horror will not work.
Do not drink alcohol or coffee at night. These drinks excite the nervous system, and in the evening it needs calmness. It's no secret that caffeine can interfere with sleep, so try to drink your last cup of coffee no later than 3-4 pm.
Turn off all glowing gadgets two hours before bedtime. In 2009, scientists from Pittsburgh
proved
that artificial intense light disrupts circadian rhythms and can contribute to depression. The social media feed is here to stay - check it out in the morning.
The social media feed is here to stay - check it out in the morning.
Keep a list of "What I Praise Myself For". Almost every person has endless lists of tasks and tasks, but people rarely praise themselves. Try every night to write down three things that you are proud of. This will help you realize your own worth and reduce the feeling of guilt, if any.
Do nothing. When you feel that you are running out of strength - both moral and physical - just lie down and rest. Set aside gadgets, books, and productivity thoughts. The better you rest, the less likely it is that causeless sadness will attack you. And there will be more strength to conquer the world the next day.
Subscribe to The Challenger!
Share
Depression
Russian Academy of Medical Sciences
SCIENTIFIC CENTER FOR MENTAL HEALTH
DEPRESSION (from hope to certainty).
(INFORMATION FOR PATIENTS AND THEIR FAMILIES)
MOSCOW
2008
Oleichik I.V. - Candidate of Medical Sciences, Leading Researcher of the Department for the Study of Endogenous Mental Disorders and Affective States
© 2008, Oleichik I.V.
© 2008, NTsPZ RAMS
The vast experience accumulated by mankind and reflected in many literary works convincingly shows that sadness (sadness, melancholy) has always gone side by side with people, being one of the natural human emotions. None of us is immune from failures, illness, breakups, loss of loved ones, financial collapse. Each person can face something inevitable and inevitable, when it seems that life loses its meaning, and despair becomes boundless. However, normally, sadness, sadness and melancholy, as natural reactions to traumatic events, weaken over time and the person's condition returns to normal without special treatment. The situation is different with depressions, which are mental disorders that differ from natural physiological reactions in greater intensity, special severity of experiences and persistence of manifestations. True depression rarely goes away on its own, requiring persistent, sometimes long-term treatment.
The situation is different with depressions, which are mental disorders that differ from natural physiological reactions in greater intensity, special severity of experiences and persistence of manifestations. True depression rarely goes away on its own, requiring persistent, sometimes long-term treatment.
A depressive state (from the Latin word depressio - suppression, oppression) is a disease that concerns not only an individual specific sick person, but is also a significant burden of modern society, since it is spreading more and more widely in the world, causing enormous damage to the health of the population and the state. economy. And this applies to all countries, regardless of their level of social development. Every year, at least 200 million people in the world fall ill with depression. Perhaps these figures are even higher, since most victims of depression do not seek help because they are not aware of the painfulness of their condition. Scientists have calculated that almost one in five people who have reached adulthood will experience at least one episode of depression during their lifetime.
In the most general sense, a depressive state is one of the possible forms of a person's response to the impact of stress factors. In some cases, depression can be triggered by external negative influences, for example, mental trauma, excessive educational or work overload, infection or other serious somatic disease, traumatic brain injury, changes in the hormonal background, which is especially important for the female body, regular certain medications, such as hormones, blood pressure medications, alcohol or other drug abuse. In other cases, depressive states develop as a manifestation of such mental illnesses, in which the main influence is heredity or characteristics of the nervous system (cyclothymia, dysthymia, manic-depressive psychosis, schizophrenia, etc.). If, based on the description of depressive symptoms set out later in our brochure, you realize that you have indeed developed a depressive state, do not fall into despair, do not “try to control yourself”, remember that depression is not a manifestation of weakness of will or character, on the contrary, weakening of volitional qualities is one of the main symptoms of depression. Depression is a disease like rheumatism, arthritis or hypertension, it responds well to treatment, resulting in almost always a full recovery. You should not blame yourself for the occurrence of depression, it does not indicate either your fault, or your weakness, or the possible development of a more severe mental pathology. Below we will tell you about the symptoms of depression, which can be extremely diverse.
Depression is a disease like rheumatism, arthritis or hypertension, it responds well to treatment, resulting in almost always a full recovery. You should not blame yourself for the occurrence of depression, it does not indicate either your fault, or your weakness, or the possible development of a more severe mental pathology. Below we will tell you about the symptoms of depression, which can be extremely diverse.
Manifestations of depression
Manifestations of depression can be very different. Depressive states can be manifested by a violation of almost all aspects of mental life: mood, memory, will, activity, which is expressed in the appearance of sadness, sadness, mental and muscle retardation, lasting at least 2 weeks. Depressed mood during depression can manifest itself as mild sadness, sadness, and boundless despair. Often it is accompanied by a feeling of melancholy, unbearable heaviness in the soul, with excruciating pain behind the sternum, a feeling of hopelessness, deep depression, hopelessness, helplessness, despair and uncertainty. At the same time, the patient is completely immersed in his gloomy experiences, and external events, even the most joyful ones, do not affect him, do not affect his mood, and sometimes even worsen the latter. A constant "companion" of a depressive mood is also anxiety of varying severity: from mild anxiety or tension to violent excitement, riot. Anxiety and bad mood arise at the mere thought of the need to make some kind of decision or change your plans due to suddenly changed circumstances. Anxiety can also manifest itself on the physical (bodily) level in the form of belching, intestinal cramps, loose stools, frequent urination, shortness of breath, palpitations, headaches, increased sweating, etc.
At the same time, the patient is completely immersed in his gloomy experiences, and external events, even the most joyful ones, do not affect him, do not affect his mood, and sometimes even worsen the latter. A constant "companion" of a depressive mood is also anxiety of varying severity: from mild anxiety or tension to violent excitement, riot. Anxiety and bad mood arise at the mere thought of the need to make some kind of decision or change your plans due to suddenly changed circumstances. Anxiety can also manifest itself on the physical (bodily) level in the form of belching, intestinal cramps, loose stools, frequent urination, shortness of breath, palpitations, headaches, increased sweating, etc.
The picture of depression is complemented by the disappearance of desires, interests, a pessimistic assessment of everything around, ideas of one's own low value and self-blame. Deficiency of vital impulses is manifested in patients with a variety of symptoms - from lethargy, physical weakness to a state of weakness, loss of energy and complete impotence. Where an important decision is required, a choice between different options, human activity is sharply hampered. Depressed people are well aware of this: they complain that insignificant everyday tasks, small issues that used to be solved almost automatically, take on the significance of complex, painful, insoluble problems. At the same time, a person feels that he began to think, act and speak slowly, notes the suppression of instincts (including food and sexual instincts), the suppression or loss of the instinct of self-preservation and the lack of the ability to enjoy life up to complete indifference to what used to be liked evoked positive emotions.
Where an important decision is required, a choice between different options, human activity is sharply hampered. Depressed people are well aware of this: they complain that insignificant everyday tasks, small issues that used to be solved almost automatically, take on the significance of complex, painful, insoluble problems. At the same time, a person feels that he began to think, act and speak slowly, notes the suppression of instincts (including food and sexual instincts), the suppression or loss of the instinct of self-preservation and the lack of the ability to enjoy life up to complete indifference to what used to be liked evoked positive emotions.
People suffering from depression often feel "stupid", "mentally retarded", "feeble-minded". Thinking in depression becomes viscous, painful, requires special efforts, one mental image is hardly forced out by the next. The sick person is oppressed by the feeling of his own intellectual insolvency, professional collapse. Depressed patients can hardly describe their painful experiences to the doctor. Only after getting out of depression, many of them say that the mood at that moment was lowered, thinking was slow, all undertakings (including treatment) seemed in vain, and the years lived were empty and useless. However, at the time of the first visit to the doctor, they could not explain this because of the almost complete absence of thoughts in their heads, “para-lich of thinking”. With depression, there are also often complaints of memory loss, which is why those suffering from it assume that they have "Alzheimer's disease", "schizophrenia", "senile dementia", which is not true. Especially often these complaints are found in depressions that develop in adolescence.
Only after getting out of depression, many of them say that the mood at that moment was lowered, thinking was slow, all undertakings (including treatment) seemed in vain, and the years lived were empty and useless. However, at the time of the first visit to the doctor, they could not explain this because of the almost complete absence of thoughts in their heads, “para-lich of thinking”. With depression, there are also often complaints of memory loss, which is why those suffering from it assume that they have "Alzheimer's disease", "schizophrenia", "senile dementia", which is not true. Especially often these complaints are found in depressions that develop in adolescence.
Typical story
Aleksey, 18 years old, 1st year student of a technical university, describes his condition during depression in this way:
“From childhood, I was fond of technology and modeling, I could read special literature for hours, won school and regional olympiads in mathematics and physics. After graduating from school, my dream came true - I brilliantly passed the exams to a prestigious university. Then it seemed to me that the whole world was at my feet, I flew with happiness "as if on wings." In September, I happily began to study. At the beginning, everything worked out well, but after 2 months I began to notice that it was becoming increasingly difficult for me to absorb what I read, I did not remember the simplest text, I could not solve problems that I used to “click like nuts”. Trying to achieve success through many hours of brainstorming or drinking a few cups of coffee led to the fact that I completely stopped thinking about anything. It seemed to me that I was "finally and irreversibly stupid." At night I sobbed, wrapped in a blanket and thought about how best to commit suicide. Luckily, I met a senior in the library and shared my problems with him. My new acquaintance said that he experienced something similar and advised me to contact the psychiatrist of the student clinic. After the examination, I was diagnosed with juvenile depression and sent for treatment to a specialized medical center.
Then it seemed to me that the whole world was at my feet, I flew with happiness "as if on wings." In September, I happily began to study. At the beginning, everything worked out well, but after 2 months I began to notice that it was becoming increasingly difficult for me to absorb what I read, I did not remember the simplest text, I could not solve problems that I used to “click like nuts”. Trying to achieve success through many hours of brainstorming or drinking a few cups of coffee led to the fact that I completely stopped thinking about anything. It seemed to me that I was "finally and irreversibly stupid." At night I sobbed, wrapped in a blanket and thought about how best to commit suicide. Luckily, I met a senior in the library and shared my problems with him. My new acquaintance said that he experienced something similar and advised me to contact the psychiatrist of the student clinic. After the examination, I was diagnosed with juvenile depression and sent for treatment to a specialized medical center. After 2 months, I felt completely healthy, returned to my studies and caught up with my classmates.
After 2 months, I felt completely healthy, returned to my studies and caught up with my classmates.
Depression can also be accompanied by real setbacks: for example, a decrease in academic performance, the quality of work, family conflicts, sexual disorders and their consequences for personal relationships. As a rule, the significance of these failures is exaggerated and as a result there is a false sense of the irreparability of what happened, "the collapse of all hopes."
Another generally recognized danger of depression is the possibility of suicidal thoughts, which often lead to suicide attempts. The condition of a person suffering from depression can suddenly deteriorate sharply, which happens either without clear external causes, or under the influence of traumatic situations, unpleasant news. It is during these hours, and sometimes even minutes, that a fatal decision is made. Factors that increase the risk of suicide in depression are past suicide attempts, the severity and duration of the depressive state, the presence of anxiety in its structure, prolonged insomnia, loneliness or alienation in the family, alcohol and drug abuse, loss of work and a sharp change in lifestyle, as well as relatives commit suicide.
Typical story
Eugene E., 35 years old, leading manager of the company.
Almost all my life, my career went “on the ascending”, the goals set were clear, clear and achievable. The marriage was extremely harmonious, two beloved children grew up. He devoted almost all the time to the affairs of the company, occasionally, once every 1-2 months, he escaped with his family out of town, to the country. He often lacked sleep, stayed late at work, took home assignments, and was deeply worried about the affairs of the company. Gradually, irritability, fatigue, insomnia, difficulty concentrating appeared, more and more often he suffered a “fiasco” in intimate life. Thoughts appeared that life was lived in vain, that it is a "chain of tragic mistakes" that led to a dead end. He began to believe that the choice of work, friends, family was wrong, for which now "retribution has come." Analyzing the past years for a long time, he found more and more evidence and examples of his "duplicity, hypocrisy, insincerity, etc. " I realized that the only way to solve all problems is to voluntarily leave this life. At the same time, he believed that by this act he would free the family from the “burden”, “loser”, “loser”. I decided, having locked myself in the garage, to get poisoned by the exhaust gases of the car. However, by chance, in a semi-conscious state, he was discovered by an employee of a garage cooperative. He explained what happened as an "accident". The thought of leaving life did not leave the patient. I decided to shoot myself with a gas pistol, which I had long ago acquired for self-defense. After a shot in the mouth, in a serious condition, he was taken to the Research Institute. Sklifasovsky, from where he was discharged a week later. The alarmed wife, suspecting something was wrong, decided to consult her husband with a psychiatrist. He was admitted to the clinic. He agreed to this only out of respect for family relations, he himself believed that treatment by psychiatrists was completely useless, because.
" I realized that the only way to solve all problems is to voluntarily leave this life. At the same time, he believed that by this act he would free the family from the “burden”, “loser”, “loser”. I decided, having locked myself in the garage, to get poisoned by the exhaust gases of the car. However, by chance, in a semi-conscious state, he was discovered by an employee of a garage cooperative. He explained what happened as an "accident". The thought of leaving life did not leave the patient. I decided to shoot myself with a gas pistol, which I had long ago acquired for self-defense. After a shot in the mouth, in a serious condition, he was taken to the Research Institute. Sklifasovsky, from where he was discharged a week later. The alarmed wife, suspecting something was wrong, decided to consult her husband with a psychiatrist. He was admitted to the clinic. He agreed to this only out of respect for family relations, he himself believed that treatment by psychiatrists was completely useless, because. his situation is hopeless and no medicines will help here, but will only "stupefy" his psyche. However, after two weeks of taking a modern antidepressant, the patient's point of view changed. Everything began to look not so bleak and hopeless, interest in work and life in general returned, I began to feel more cheerful, more energetic, interest in intimate life appeared. He took work to the clinic, called up colleagues. After two months of treatment, he fully returned to his usual life. With bewilderment, he recalled his thoughts about insolvency, the collapse of life, suicide. He took the drug prophylactically for about six months, then, on the recommendation of a doctor, he gradually reduced the dose and stopped taking it. Over the next two years, the condition remained stable, career growth continued, another child was born.
his situation is hopeless and no medicines will help here, but will only "stupefy" his psyche. However, after two weeks of taking a modern antidepressant, the patient's point of view changed. Everything began to look not so bleak and hopeless, interest in work and life in general returned, I began to feel more cheerful, more energetic, interest in intimate life appeared. He took work to the clinic, called up colleagues. After two months of treatment, he fully returned to his usual life. With bewilderment, he recalled his thoughts about insolvency, the collapse of life, suicide. He took the drug prophylactically for about six months, then, on the recommendation of a doctor, he gradually reduced the dose and stopped taking it. Over the next two years, the condition remained stable, career growth continued, another child was born.
Depression is also characterized by sleep disturbances, occurring in approximately 80% of patients. As a rule, these are early awakenings with the inability to fall asleep, lack of a sense of sleep, difficulty falling asleep. These disorders, as well as restless sleep with unpleasant dreams, are often the very first symptoms of incipient depression.
These disorders, as well as restless sleep with unpleasant dreams, are often the very first symptoms of incipient depression.
If the depression is not deep, it is sometimes difficult to recognize it. This is due to the fact that people are ashamed to tell others about their problems, to admit to "weaknesses". Quite often, especially in Russia, depressive states are masked by alcohol abuse (“vodka heals”). In addition, often patients suffering from depression, in order to "shake themselves up", "throw into all serious", engage in casual sex, are fond of gambling or extreme sports, leave to serve on a contract in "hot spots", lead an idle lifestyle with constant attendance at entertainment events. Surrounding people, relatives who do not have psychiatric knowledge, often accuse them of debauchery, drunkenness, riotous lifestyle, parasitism. Meanwhile, this behavior is a kind of “cry for help”, an attempt to fill the spiritual emptiness brought by depression with new acquaintances and impressions.
Depressive conditions can occur in shallow forms that are easily treatable, but at least a third of depressions are more severe. Characteristics for such depressions are:
- ideas of guilt, sometimes reaching the degree of delirium, i.e. unshakable conviction in their sinfulness, low value (patients consider themselves great sinners, believe that because of them all relatives and Mankind will die, that they are “moral freaks” from birth, supposedly deprived of the foundations of morality and a sense of empathy for other people that they have no place on earth They find in their past numerous "confirmations" of what has been said above, they believe that the doctor and other patients are aware of these transgressions and express contempt and indignation with their facial expressions and gestures, but in the words “they hide, deny the obvious.” Both the patients themselves and their relatives must remember this in order to prevent the impending threat in time: remove all firearms, piercing and cutting objects, ropes, potent drugs and poisonous close household fluids, close windows or shutters, do not let the patient go anywhere alone. If these ideas become persistent and cannot be dissuaded, it is urgent to seek advice from a psychiatrist. neurological institution or call a psychiatrist at home.
If these ideas become persistent and cannot be dissuaded, it is urgent to seek advice from a psychiatrist. neurological institution or call a psychiatrist at home.
- mood swings during the day: in typical cases, the patient, waking up, immediately feels longing. Sometimes, even before full awakening, through a dream he experiences a painful premonition of a heavy coming morning. In the evening, the state of health improves somewhat.
- the patient may experience a feeling of unmotivated hostility towards relatives, friends, constant internal discontent and irritation, which makes him unbearable for the family.
- in a number of people suffering from depression, constant doubts, fear for the health and well-being of loved ones, obsessive ones, come to the fore. arising against the will, ideas about the misfortunes and troubles of family members.
Typical story
Dmitry Petrovich, 58 years old, teacher.
“After minor troubles at work, I began to feel incomprehensible anxiety and agitation. Unpleasant thoughts came into my head that I did something wrong at work, because of which I double-checked everything many times and went home later than everyone else. But even at home, the anxiety did not let go: as soon as the daughter or wife lingered for at least half an hour, terrible pictures of traffic accidents or violence were drawn in the imagination. I fell asleep only in the morning, got up broken and felt sleepy all day. I took Valerian, Corvalol, but it practically did not help. At work, they hinted whether I should take a vacation. Friends advised me to consult a neuropathologist, but he did not find his pathology and sent me to a psychiatrist. I was diagnosed with anxiety depression. After a course of outpatient treatment, I completely recovered.”
Unpleasant thoughts came into my head that I did something wrong at work, because of which I double-checked everything many times and went home later than everyone else. But even at home, the anxiety did not let go: as soon as the daughter or wife lingered for at least half an hour, terrible pictures of traffic accidents or violence were drawn in the imagination. I fell asleep only in the morning, got up broken and felt sleepy all day. I took Valerian, Corvalol, but it practically did not help. At work, they hinted whether I should take a vacation. Friends advised me to consult a neuropathologist, but he did not find his pathology and sent me to a psychiatrist. I was diagnosed with anxiety depression. After a course of outpatient treatment, I completely recovered.”
- in many cases, depression is characterized by unpleasant sensations in the body, disturbances in the activity of internal organs in the absence of objective signs of true somatic, i.e. non-mental illness. At the same time, many patients constantly report pain, internal discomfort. Some complain of headaches, pains in the stomach, joints, lower back, others - of disorders in the intestines: constipation, indigestion, irritation of the colon, others pay attention to a decrease in sexual desire and potency. In women, menstruation often becomes painful and irregular. Approximately 50% of depressed people at the doctor's office complain of such physical ailments, without mentioning the depressed mood or state of mind underlying the depression. Experiencing chronic pain or other unpleasant sensations in the body, patients may not realize that they are suffering from depression, even with severe melancholy, considering the latter a reaction to painful bodily discomfort.
Some complain of headaches, pains in the stomach, joints, lower back, others - of disorders in the intestines: constipation, indigestion, irritation of the colon, others pay attention to a decrease in sexual desire and potency. In women, menstruation often becomes painful and irregular. Approximately 50% of depressed people at the doctor's office complain of such physical ailments, without mentioning the depressed mood or state of mind underlying the depression. Experiencing chronic pain or other unpleasant sensations in the body, patients may not realize that they are suffering from depression, even with severe melancholy, considering the latter a reaction to painful bodily discomfort.
- some patients are convinced that they have some rare and difficult to diagnose disease and insist on numerous examinations in general medical institutions. Doctors call this condition masked (hidden) depression, in which a person may experience pain in the head, in the limbs, behind the sternum, in the abdomen and in any other parts of the body, he may be haunted by anxious fears, he may suffer from insomnia or, on the contrary, too much sleep.
- Patients may experience disturbances in the cardiovascular system, skin itching or lack of appetite. All of these are manifestations of depression.
- the pathological sensations that patients experience during such depressions are quite real, painful, but they are the result of a special mental state, and not an internal disease. It must be remembered that the frequency of latent depressions exceeds the number of explicit ones many times over.
- with such depression, patients, as a rule, also have a changed attitude towards food: they can go without food for a long time and not feel hungry, and sitting down at the table, eat only 1-2 spoons - they have neither strength nor desire for more .
- a sign of depression can serve as a weight loss of more than 5 kg. within a month. In some people, especially women, the appetite for depression, on the contrary, increases, sometimes reaching the level of excruciating hunger, accompanied by severe weakness and pain in the epigastric region. In some cases, food is taken in excess due to an increased craving for sweets or attempts to distract oneself from painful thoughts by frequent eating.
In some cases, food is taken in excess due to an increased craving for sweets or attempts to distract oneself from painful thoughts by frequent eating.
Thus, we see that depression is a disease with many different manifestations that do not go away on their own, requiring special, sometimes long-term, medical intervention. Therefore, when the symptoms described above appear, it is necessary to seek help from a psychiatrist who will prescribe and monitor antidepressant treatment.
TREATMENT OF DEPRESSIVE DISORDERS
To date, it can be argued that the vast majority of cases of depression respond well to treatment. According to modern views, effective treatment of depression consists of a combination of pharmacotherapy, psychotherapy and, if necessary, other types of treatment. At the same time, the main role in therapy, of course, belongs to antidepressants - drugs specially designed for the treatment of various types of depression.
The creation of antidepressants is based on the discovery of scientists that depression develops as a result of a violation of the mechanism of biochemical transmission of nerve impulses in the brain regions responsible for mood, behavior, response to stress, sleep and wakefulness, appetite and some other functions. To ensure the coordination of the work of all these functional divisions, the brain sends special "commands" to them in the form of chemical impulses transmitted from the processes of one nerve cell (neuron) to the processes of another. This transmission is carried out with the help of chemical mediators (neurotransmitters), which, after transmitting a signal, partially return to the original neuron. This process is called neurotransmitter reuptake. Thanks to him, the number of mediators in the microscopic space between the processes of neurons (in the so-called synaptic cleft) decreases, which means that the necessary signals are transmitted worse. Numerous studies have shown that mediators of various structures, in particular, norepinephrine and serotonin, are involved in the transmission of signals that ensure the normal functioning of the nervous system. The first of them has a general activating effect, maintains the level of wakefulness of the body and takes part in the formation of adaptive reactions, and the second has the main antidepressant effect, controls impulsive actions, anxiety, aggressiveness, sexual behavior, falling asleep, feeling of pain, therefore serotonin is called sometimes a "good mood" regulator.
To ensure the coordination of the work of all these functional divisions, the brain sends special "commands" to them in the form of chemical impulses transmitted from the processes of one nerve cell (neuron) to the processes of another. This transmission is carried out with the help of chemical mediators (neurotransmitters), which, after transmitting a signal, partially return to the original neuron. This process is called neurotransmitter reuptake. Thanks to him, the number of mediators in the microscopic space between the processes of neurons (in the so-called synaptic cleft) decreases, which means that the necessary signals are transmitted worse. Numerous studies have shown that mediators of various structures, in particular, norepinephrine and serotonin, are involved in the transmission of signals that ensure the normal functioning of the nervous system. The first of them has a general activating effect, maintains the level of wakefulness of the body and takes part in the formation of adaptive reactions, and the second has the main antidepressant effect, controls impulsive actions, anxiety, aggressiveness, sexual behavior, falling asleep, feeling of pain, therefore serotonin is called sometimes a "good mood" regulator. A decrease in the number of mediators in the synaptic cleft causes symptoms of depression, while an increase, on the contrary, prevents their appearance. The ability of some drugs in one way or another to increase the concentration of mediators in the synaptic cleft allows them to be used as antidepressants.
A decrease in the number of mediators in the synaptic cleft causes symptoms of depression, while an increase, on the contrary, prevents their appearance. The ability of some drugs in one way or another to increase the concentration of mediators in the synaptic cleft allows them to be used as antidepressants.
Now antidepressants are used in Russia, which can be conditionally divided into 4 generations according to the time of creation.
The first antidepressants to find wide clinical use were tricyclic drugs: amitriptyline and imipramine. They have a fairly powerful effect on most depressive states by blocking the reuptake of both norepinephrine and serotonin. However, the real clinical effect of these drugs is significantly offset by their undesirable side effects, which drastically reduce the quality of life of patients during treatment. Side effects of tricyclic antidepressants arise due to the nonspecificity of their effect on receptor structures. Acting in addition to the serotonin and norepinephrine system and other neurotransmitters (acetylcholine, histamine, dopamine), these antidepressants cause side effects such as urinary retention, dry mucous membranes, constipation, palpitations, fluctuations in blood pressure, confusion, tremor, sexual dysfunction. functions, weight gain. In such cases, it is necessary to prescribe other drugs to correct side effects or reduce the therapeutic dose of drugs, which naturally affects the effectiveness of the antidepressant action. It has been observed that up to 50% of patients refuse to take tricyclic antidepressants due to severe side effects. For the same reason, physicians are less likely to prescribe these drugs to patients on an outpatient basis.
functions, weight gain. In such cases, it is necessary to prescribe other drugs to correct side effects or reduce the therapeutic dose of drugs, which naturally affects the effectiveness of the antidepressant action. It has been observed that up to 50% of patients refuse to take tricyclic antidepressants due to severe side effects. For the same reason, physicians are less likely to prescribe these drugs to patients on an outpatient basis.
The situation was somewhat improved by the introduction into practice of drugs of the second generation - tetracyclic antidepressants, which, along with the ability to block the reuptake of norepinephrine and serotonin, could also affect some other receptors. Being analogues of tricyclic compounds, these drugs have antidepressant activity comparable to them, but unlike their predecessors, they are safer, since they cause unwanted side effects much less often. In addition to the antidepressant, mianserin (lerivon) has a clear sedative, anti-anxiety and hypnotic effect. Maprotiline (Ludiamil) has a mild balanced antidepressant effect. In general, these drugs are able to cure mild to moderate depression, but are ineffective in patients with severe depression.
Maprotiline (Ludiamil) has a mild balanced antidepressant effect. In general, these drugs are able to cure mild to moderate depression, but are ineffective in patients with severe depression.
To date, antidepressants of the 3rd generation, such as fluoxetine (Prozac), fluvoxamine (Fevarin), paroxetine (Paxil), sertraline (Zoloft), citalopram (Cipralex) and some other drugs that selectively (selectively) affect the serotonin metabolism system, have received widespread recognition today. , preventing its reuptake in the synaptic cleft. Based on the mechanism of action, these antidepressants are combined into a group of selective serotonin reuptake inhibitors. In addition to treating depression, they are used to correct eating disorders, level panic disorders, so-called social phobias, various obsessive-compulsive disorders and chronic pain symptoms. These drugs have gained popularity due to the possibility of a once-daily intake, concomitant anti-anxiety effect, the presence of a psychostimulant component and a small number of side effects. In addition, they have low toxicity and are well tolerated by elderly patients. However, some researchers note their lack of effectiveness in the treatment of severe forms of depressive states, probably associated with selective activity in relation to only one neurotransmitter - serotonin. It should be noted that in recent years, some American scientists have associated the use of these drugs with an increased risk of suicide, which, however, is not proven.
In addition, they have low toxicity and are well tolerated by elderly patients. However, some researchers note their lack of effectiveness in the treatment of severe forms of depressive states, probably associated with selective activity in relation to only one neurotransmitter - serotonin. It should be noted that in recent years, some American scientists have associated the use of these drugs with an increased risk of suicide, which, however, is not proven.
Considering the high frequency of side effects in some of the above drugs and the insufficient antidepressant activity in others, psychopharmacologists have taken the path of developing more effective antidepressants - IV generation drugs that selectively block the reuptake of both serotonin and noradrenaline, without affecting other mediators. system and with minor side effects. Currently, 3 drugs meet these requirements: milnacipran (Ixel), duloxetine (Cymbalta) and venlafaxine (Effexor). Their antidepressant activity in the treatment of patients with severe and moderate depression has been confirmed in a number of specially conducted studies, which at the same time showed that these drugs are well tolerated.
It should be noted that antidepressants of plant origin (negrustin, gelarium hypericum, deprim, etc.) can be effective in mild depressive states, but there are no reliable data guaranteeing their effectiveness. The opinion of a number of doctors that all depression can be treated with herbs or, say, acupuncture, should be recognized as unfounded.
For extremely severe depressions that do not improve despite the use of the most powerful antidepressants, electroconvulsive therapy (ECT) can be effective, but this situation is extremely rare and requires careful justification by the commission of doctors and the consent of the patient.
An important additional role in antidepressant therapy, especially with concomitant anxiety, is played by tranquilizers - anti-anxiety drugs, such as Xanax, phenazepam, diazepam, nitrazepam, atarax, etc. Drugs that can, when taken systematically, prevent mood swings in various depressive disorders include so-called mood stabilizers or mood stabilizers - lithium preparations, carbamazepine, valproic acid salts, lamotrigine, topiramate. With their systematic intake in most patients, the clinical manifestations of depression either completely disappear or become rare and mild, requiring no hospitalization and not significantly affecting the ability to work.
With their systematic intake in most patients, the clinical manifestations of depression either completely disappear or become rare and mild, requiring no hospitalization and not significantly affecting the ability to work.
Antipsychotics play a significant role in the treatment of certain forms of depression. These include both traditional drugs - fluanxol, triftazin, eglonil, teralen, neuleptil, sonapax, and atypical antipsychotics that are gaining more and more recognition among doctors: seroquel, solian, zeldox, rispolept, abilify, serdolect and others.
In drug therapy of depressive conditions, an unconventional, strictly individual approach is used, with the obligatory provision of fruitful cooperation between the patient and the doctor. Otherwise, there may be a violation of medical recommendations regarding doses and regimens for taking medications. The patient's faith in the possibility of recovery, the absence of prejudice against the "harm" caused by psychotropic drugs, the systematic observance of the prescriptions prescribed by the doctor largely contribute to the achievement of therapeutic success.
Drug treatment of depression takes time. You should not expect a complete cure already in the first days of taking the drug. It must be remembered that all modern antidepressants begin to act on depressive symptoms no earlier than 1-2 weeks after the start of treatment. Cancellation of an antidepressant, as well as its appointment, should be carried out only by a doctor. Cancellation is usually made no earlier than 6 months from the normalization of the mental state. Even after the complete disappearance of all symptoms of depression, do not rush to stop taking the drug yourself, as there is a risk of an exacerbation of the disease. Therefore, doctors recommend continuing to take the antidepressant for a certain period of time. A common mistake is the premature withdrawal of drugs soon after a significant improvement in the condition or due to "forgetfulness". To avoid this, try to include the drug in the list of daily urgent matters - for example, store it in the bathroom and take it after hygiene procedures.