Zoloft and valium
Valium Interactions | Antipsychotics, Sleep Medications, Ssris and More.
Harmful interactions can occur when taking Valium with antipsychotics, sleep medications, SSRIs and more.
Valium (diazepam) is a benzodiazepine prescription drug most frequently recommended for people with anxiety, seizures, muscle spasms or alcohol withdrawal.
Benzodiazepine drugs are Schedule IV drugs, according to the DEA, which means their potential for abuse and addiction is low.
Valium acts on the central nervous system by slowing down electrical impulses in the brain. This results in a calming, soothing and quieting effect. Its tranquilizing effects are also known to assist with seizure prevention, muscle spasms like restless leg syndrome, and abnormal body movement. Additionally, it is sometimes used to help with alcohol withdrawal side effects. Valium makes the individual feel drowsy and can alter moods as well.
When taken as prescribed, Valium is a relatively safe drug with a risk of minor side effects. However, when one combines Valium with drugs or substances that affect the central nervous system, there is a significant increase in the risk of side effects, including drowsiness, memory loss and confusion, breathing problems, hallucinations, depression, rage reactions, overdose, coma and even death.
The most common drug interactions associated with Valium are pharmacodynamic interactions. Here, the effects of one drug are additive to the effects of another. Since Valium is a central nervous system (CNS) depressant, other drugs that are CNS depressants will enhance this effect.
Several drug groups pose significant risk of adverse interactions when taken with Valium.
Phenothiazines
Phenothiazines are a group of medications that can be used to treat nausea or symptoms of psychosis. Common examples include chlorpromazine, thioridazine, fluphenazine and prochlorperazine. When taken with Valium, these drugs pose an extremely high risk of drowsiness, dizziness, falls and memory loss.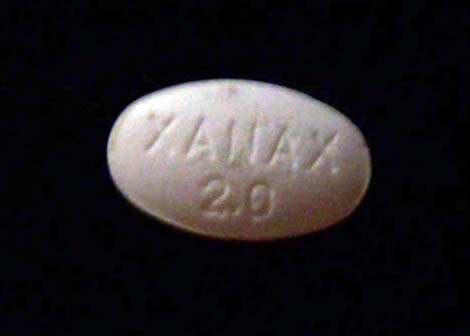
Antipsychotics
Antipsychotics are also known as neuroleptics or major tranquilizers, and they’re prescribed to manage psychosis symptoms of bipolar disorder, schizophrenia and schizoaffective disorder. Examples include haloperidol, aripiprazole, risperidone, paliperidone, olanzapine, clozapine, lurasidone, ziprasidone, quetiapine and paliperidone.
All antipsychotic medications are CNS depressants to a certain extent, with some causing more depressant effects than others. When combined with Valium, side effects can include loss of coordination, confusion, drowsiness and weakness.
Anxiolytics
Anxiolytics are prescribed to treat symptoms of anxiety. There are different groups of medications that can treat anxiety, including SSRIs and SNRIs. Other anxiety medications, like benzodiazepines, should not be mixed with Valium since Valium itself is a benzodiazepine. Examples include Ativan, Xanax, Librium and Klonopin. Combining these drugs may result in extreme CNS depression.
Sleep Medications
Sleep medications can be prescribed or purchased over-the-counter (OTC). Prescription sleep aids include zolpidem, eszopiclone, Dayvigo, Belsomra and zaleplon. OTC sleep medications typically include either doxylamine or diphenhydramine.
Like other drug interactions, combining Valium with sleep medications increases the risk of CNS depression. The only non-sedating sleep medication that is safe to combine with Valium is Ramelteon, by prescription only, and melatonin, available over the counter.
Narcotic Analgesics
Commonly called “narcotics”, this group of medicines includes opiates and opioids. They relieve acute and chronic severe pain by binding to opioid receptors. Drugs include morphine, hydrocodone, codeine, fentanyl, methadone, tramadol, oxycodone and oxymorphone.
It is extremely dangerous to take narcotic pain medications along with benzodiazepines like Valium. The FDA recently required additional boxed warnings to warn the public of the increased risk of overdose and death when combining these two types of drugs.
Sedative Antihistamines
Antihistamines are typically used to manage allergic reactions and sometimes cases of itching. However, a side effect of some of these drugs is that they can have sedative properties. Drugs include diphenhydramine (Benadryl), chlorpheniramine and hydroxyzine. Follow your doctor’s instructions for these drugs cautiously while taking Valium and watch for symptoms of drowsiness, loss of coordination, confusion and sedation.
Anticonvulsants
Anticonvulsants are used to treat or prevent seizures in people with seizure disorders. Valium itself can be used to treat seizures, so sometimes it will be prescribed in combination with these types of drugs, but Valium can often be used safely if managed by a healthcare professional. Examples of anticonvulsants include gabapentin, valproic acid, barbiturates, benzodiazepines, carbamazepine, oxcarbazepine, tiagabine, topiramate, phenytoin, fosphenytoin, primidone, ethosuximide and zonisamide.
If you are taking anticonvulsants, you should speak with your healthcare provider about the potential risks of drug interactions with Valium.
Monoamine Oxidase (MAO) Inhibitors
MAOIs are antidepressant drugs that elevate the levels of norepinephrine, serotonin and dopamine in the brain. Drugs include Parnate, Nardil, Marplan and Emsam. While MAOIs have an extremely high number of drug interactions, they do not interact with Valium. However, anyone taking MAOIs should use caution before changing their drug regimen.
Selective Serotonin Reuptake Inhibitors (SSRIs)
SSRIs are commonly prescribed to treat anxiety and depression. Common examples include fluoxetine (Prozac), citalopram (Celexa), sertraline (Zoloft), paroxetine (Paxil) and escitalopram (Lexapro).
Most SSRIs have no interactions with Valium and can be used safely at the same time. However, fluoxetine can cause an increased potency of Valium when taken together. There is an increased risk of sedation, confusion and loss of coordination when taking Valium and fluoxetine together.
Serotonin Norepinephrine Reuptake Inhibitors (SNRIs)
There are two commonly prescribed SNRIs: venlafaxine (Effexor) and duloxetine (Cymbalta). SNRIs can be used to treat anxiety or depression and can also be used to treat certain types of nerve pain.
SNRIs can be used to treat anxiety or depression and can also be used to treat certain types of nerve pain.
There are no known interactions between SNRIs and Valium.
Noradrenergic and Specific Serotonergic Antidepressants (NaSSAs)
The only NaSSA available by prescription in the United States is mirtazapine (Remeron). Mirtazapine is indicated for the treatment of depression, but may also be used for anxiety in some people.
Mirtazapine causes a significant level of CNS depression, so it can increase the risk of drowsiness, loss of coordination, confusion and somnolence when taken with Valium.
Alcoholic Beverages
Alcoholic beverages should never be combined with benzodiazepines like Valium. Alcohol, like many other drugs on this list, is a CNS depressant. However, the risk of overdose is significantly increased when taking Valium and alcohol together.
Signs and symptoms of overdose may include:
- Cold or clammy skin
- Confusion
- Low body temperature
- Trouble breathing or irregular breathing
- Slowed heart rate
- Slow responses
- Vomiting
Harmful interactions can occur when using Valium and any of the drugs listed above. Additionally, combining these drugs with Valium presents a greater chance of developing a chemical dependence and addiction.
Additionally, combining these drugs with Valium presents a greater chance of developing a chemical dependence and addiction.
If you or a loved one are concerned about Valium use in combination with other medications or substances, speak with your doctor, who can address any concerns and help mitigate risk associated with your unique situation. If you suspect signs of a substance use disorder, contact us at The Recovery Village, where we have all the tools you need for long-term recovery.
Editor – Erica Weiman
Erica Weiman graduated from Pace University in 2014 with a master's in Publishing and has been writing and editing ever since. Read more
Medically Reviewed By – Dr. Conor Sheehy, PharmD, BCPS, CACP
Dr. Sheehy completed his BS in Molecular Biology at the University of Idaho and went on to complete his Doctor of Pharmacy (PharmD) at the University of Washington in Seattle. Read more
Drug Enforcement Agency (DEA). “Benzodiazepines.” April 2020. Accessed November 9, 2021.
Accessed November 9, 2021.
Food and Drug Administration (FDA). “FDA requiring boxed warning updated t[…]epine drug class.” September 2020. Accessed November 9, 2021.
Food and Drug Administration (FDA). “Valium Package Insert.” 2016. Accessed November 9, 2021.
Drugs.com. “Valium (diazepam) Interactions.” Accessed November 9, 2021.
National Institute on Alcohol Abuse and Alcoholism (NIAAA). “Understanding the Dangers of Alcohol Overdose.” May 2021. Accessed November 9, 2021.
Medical Disclaimer
The Recovery Village aims to improve the quality of life for people struggling with substance use or mental health disorder with fact-based content about the nature of behavioral health conditions, treatment options and their related outcomes. We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.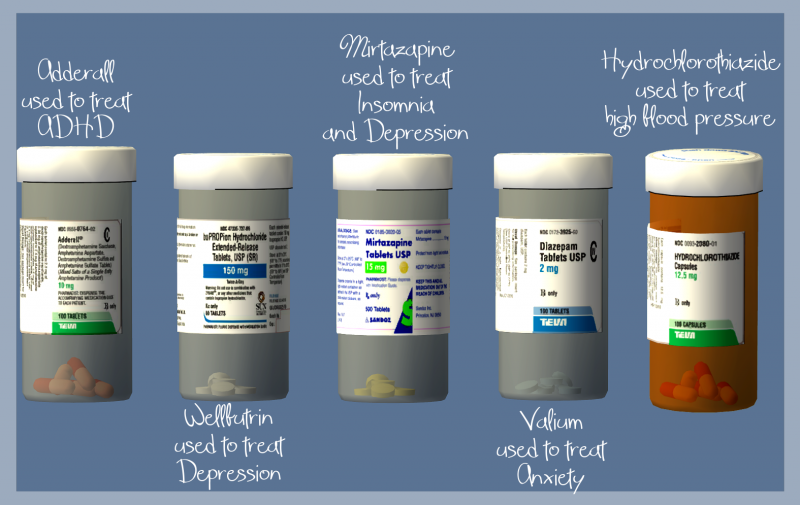
Can You Take Sertraline And Valium Together?
In this blog post, we are going to talk about the safety and efficacy of the concomitant use of sertraline and valium. Both of these medicines are used for a number of mental health conditions.
This blog will cover the possible interactions between these two drugs and we will also discuss some warnings that come with both sertraline and valium.
Can you take sertraline and valium together?
Counseling is Key to a Healthy Marr...
Please enable JavaScript
Counseling is Key to a Healthy Marriage
Yes, you can use sertraline and valium together, but only if your healthcare provider has prescribed this combination. In some conditions, the combination therapy of sertraline and valium is preferred as compared to the monotherapy.
Several research studies have come forward to explain how the use of valium can be helpful, especially during the first few weeks of your treatment with sertraline.
Sertraline is an antidepressant. It is a selective serotonin reuptake inhibitor (SSRI) and is used to treat mild to severe episodes of depression and generalised anxiety disorder.
Sertraline inhibits the reuptake of serotonin by blocking serotonin transporters (SERT). This results in increased serotonergic activity. However, the drug takes time to make these changes in your system, but it starts to produce the side effects right away.
The most common early side effect of sertraline is anxiety. This anxiety can get so bad that some people stop using the antidepressant before it even kicks in. This is a major problem with sertraline use and this is where valium comes into the picture.
Valium and other benzodiazepines can be used to control early anxiety caused by sertraline. The treatment is usually continued till your antidepressant kicks in. These meds together can control multiple overlapping symptoms of anxiety and depression. These symptoms include:
- Restlessness
- Extreme distress
- Irritability
- Suicidal behavior
- Inability to engage in daily life activities
- Weight loss or gain, depending on the effect of the condition on eating habits
- Excessive sweating
- An urge to get isolated
- Hopelessness
- Worthlessness
- Confusion
- Social disconnection
Valium is a benzodiazepine, which is an anti-anxiety medication. Individually, it is used for the treatment of anxiety, convulsions and panic attacks. This medication basically mimics inhibitory chemicals in your brain, like GABA, to control the excessive neuronal activity.
Individually, it is used for the treatment of anxiety, convulsions and panic attacks. This medication basically mimics inhibitory chemicals in your brain, like GABA, to control the excessive neuronal activity.
The onset of action of valium is much quicker than sertraline. Valium typically takes a few hours to work and its effects last longer, as it is considered a long acting benzodiazepine.
A few studies indicate that benzodiazepines may play an important role in the management of depression and can be used in combination with antidepressants for the treatment of major depressive disorder (MDD).
The same study revealed that GABA can make an impact on your depression through GABA depression theory and benzodiazepines can control this effect.
Another 2019 research study monitored the effects of this combination of antianxiety and antidepressants for the treatment of MDD.
The study used various standardisation techniques and concluded that it is indeed an effective combination and can significantly help to reduce the early anxiety caused by antidepressants.
What are the possible interactions between sertraline and valium?
Sertraline and valium may interact with each other and cause the following side effects:
- Increased sedation
- Dizziness
- Fatigue
- Impaired senses
- Impairment of motor coordination
- Difficulty in concentrating
- Blackouts
These side effects can vary from person to person and they depend on the doses of this combination. If you are at low doses, the most common thing you can experience is dizziness and sleepiness. However, higher doses cause much more damage.
Elderly patients are more susceptible to the interactions between sertraline and valium. They may also suffer from additional effects like memory loss, impairment of motor coordination and troubled judgement.
What are the side effects associated with the use of sertraline and valium?
Both sertraline and valium are associated with some side effects that may range from mild to severe. It totally depends on the doses of these two meds.
It totally depends on the doses of these two meds.
Side effects of sertraline
- Loss of appetite
- Tiredness
- Feeling angry or agitated
- Weight gain
- Inability to digest food
- Nausea
- Diarrhoea
- Loss of libido
- Sweating/Night sweats
- Tremors or shaking
- Insomnia
- Decreased sex drive
- Impotence
- Inability to ejaculate
Some serious and rare side effects include:
- Allergic reactions, like rash, hives are common. It also includes wheezing, difficulty in breathing, tightness in the chest, trouble breathing, swallowing, or swelling of the mouth, face, lips, tongue, or throat.
- Convulsions
- The inability to have an erection
- Hypothyroidism (low thyroid gland function)
- Bone marrow failure associated with low blood counts
- Thrombocytopenia
- Neutropenia
- Abnormal behaviour/mania
- Suicidal thoughts
- Feeling guilty all the time
- Extrapyramidal symptoms
Side effects of valium
- Dizziness
- Tiredness or fatigue
- Drowsiness
- Muscle pain
- Vision problems
- Headache
- Hypersomnia
- Forgetfulness
- Troubled or intrusive thoughts
- Impairment of motor coordination
- Constipation or diarrhoea
- Nausea
- Vomiting
- Increased or decreased appetite
Serious side effects include:
- Allergic reaction associated with symptoms like redness of skin, itching, painful blisters, blue-purple patches, burning sensation etc.

- Serious respiratory depression which lowers down breathing rate and can decrease the availability of oxygen in the blood. It could be life-threatening for people suffering from asthma or chronic obstructive pulmonary disease (COPD)
- Dementia
- Abnormal behaviour
- Blackouts
How to ensure the proper use of sertraline and valium?
Immediately talk to your healthcare provider if you experience unusual side effects while taking valium and sertraline together. Do not recommend this combination to someone else and use it as long as your doctor has advised.
Inform your doctor if you’re pregnant, trying to conceive. Valium should not be used by pregnant women and sertraline can also be dangerous for the fetus, especially when used in the third trimester.
Inform your doctor if you’re a breastfeeding mother. Both of these drugs are capable of passing into the breastmilk and may cause side effects in newborns.
Sertraline comes with a black-box warning as it may induce suicidal behavior in users younger than 24 years of age. If you have someone who shows suicidal behavior or you see hopelessness in them, make sure you keep an eye on them and get medical attention as soon as you can.
If you have someone who shows suicidal behavior or you see hopelessness in them, make sure you keep an eye on them and get medical attention as soon as you can.
One of the side effects of valium include respiratory depression, which is dose dependent.
A person with normal respiratory function might not even notice this side effect on the normal therapeutic dose, but people with chronic breathing disorders like asthma, chronic obstructive pulmonary disease (COPD) and emphysema etc, can suffer from significant breathing difficulties.
Similarly, sertraline is considered safe to be used in cardiac patients, but it could cause QT elongation and make pre-existing arrhythmia even worse. Valium is also known for causing an addiction, which is why it is not suitable for prolonged use.
Doctors usually recommend using it as long as your antidepressant kicks in. After that, both anxiety and depression can be managed by sertraline and valium is slowly tapered off because it is not safe to use benzodiazepines for a long period of time.
Do not stop valium or sertraline abruptly. If it’s time for you to stop one or both of these meds, your doctor will simply recommend a taper schedule for you, which should be followed vigilantly if you wish to keep withdrawal symptoms at bay.
Report any problems with bleeding or bruising to your doctor. If you see any unexplained blisters or rashes on your body, or experience any problems with urination, or if you feel changes in your vision, immediately report to your healthcare provider.
If the combination of valium and sertraline makes you sleepy, make sure you avoid the following activities:
- Do not drive when you’re feeling tired or drowsy. Driving requires your full physical and mental alertness and it’s in your best interest to avoid it when you’re tired and have low energy levels.
- If you’re an employee in some factory where you are supposed to operate heavy machinery, don’t! Your drowsiness might cause an accident and can make you or others around you severely injured.
- Make sure you’re not taking any other medication that might be contributing to your drowsiness. Do not drink alcohol, or you’ll end up dulling your senses even more.
Conclusion
In this blog post, we have discussed the concomitant use of sertraline and valium. These may interact with each other and increase the risk of sedation, dizziness, fatigue, impaired senses and difficulty in concentrating.
Elderly patients are more susceptible to these side effects and may suffer from additional effects like memory loss, impairment of motor coordination and troubled judgement. However, these two meds are still used together.
The dose at which you take these two drugs can make a huge impact on your health. Make sure you use these two meds only when the combination treatment is preferred by your mental healthcare professional. Do not start any other medication along with your prescribed antidepressant.
FAQs:Sertraline and valium
Is sertraline the same as Valium?
No, valium and sertraline are not the same.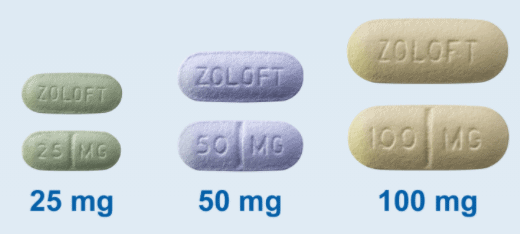 Valium is a benzodiazepine. It is used to help control anxiety, convulsions and panic attacks. This medication basically mimics inhibitory chemicals in your brain, like GABA, to control the excessive neuronal activity.
Valium is a benzodiazepine. It is used to help control anxiety, convulsions and panic attacks. This medication basically mimics inhibitory chemicals in your brain, like GABA, to control the excessive neuronal activity.
Sertraline, on the other hand, is an antidepressant. It is a selective serotonin reuptake inhibitor (SSRI). This med inhibits the reuptake of serotonin by blocking serotonin transporters (SERT). This results in increased serotonergic activity which can treat mild to severe episodes of depression and generalised anxiety disorder.
What medications can you not take with Valium?
- Other anti-anxiety medications or sleeping pills. The concomitant use can dangerously increase the sedation and may cause confusion.
- Antipsychotic medications
- Opioid drugs, including painkillers and anti-tussive (cough relieving) medications. The concomitant use can cause serious psychological side effects and respiratory depression.
- Alcohol
What drugs should not be taken with sertraline?
- Monoaminoxidase inhibitors (MAOIs).
 The combination use can increase the risk of serotonin syndrome.
The combination use can increase the risk of serotonin syndrome. - Non-steroidal anti-inflammatory drugs (NSAIDS). The combination use can increase the risk of bleeding.
- Pimozide. The concomitant use can increase the plasma concentration(availability of a drug in the blood) of pimozide to much higher levels. It can result in life-threatening arrhythmia.
- Controlled substances, including all narcotic analgesics. The concomitant use can cause severe psychological side effects.
- Mood stabilisers
- Alcohol
Can you take diazepam with antidepressants?
Yes, you can take diazepam with antidepressants if your healthcare provider has prescribed these meds together. Valium and other benzodiazepines can be used to control early anxiety caused by antidepressants.
The treatment is usually continued till your antidepressant kicks in. These meds are also used together for the treatment of comorbid anxiety and depression.
Is Valium good for anxiety?
Yes, valium is good for anxiety. In fact, it is known as an anti-anxiety medication because it is specially used to treat anxiety. It belongs to the class of benzodiazepines and it starts working soon after taking the first ever dose. It not only treats your anxiety, but also helps you sleep better. However, it is not recommended to use these agents for a long period of time because they cause addiction.
In fact, it is known as an anti-anxiety medication because it is specially used to treat anxiety. It belongs to the class of benzodiazepines and it starts working soon after taking the first ever dose. It not only treats your anxiety, but also helps you sleep better. However, it is not recommended to use these agents for a long period of time because they cause addiction.
References
- Drug Interactions between Valium and Zoloft https://www.drugs.com/drug-interactions/valium-with-zoloft-862-441-2057-1348.html?professional=1
- J W Tiller et al. Br J Psychiatry. (1989) – Is diazepam an antidepressant? https://pubmed.ncbi.nlm.nih.gov/2692764/
- Valium – Uses, Side Effects, and More https://www.webmd.com/drugs/2/drug-11116/valium-oral/details
- A L McRae et al. Expert Opin Pharmacother. 2001 – Review of sertraline and its clinical applications in psychiatric disorders https://pubmed.ncbi.nlm.nih.gov/11336629/
- Singh HK, Saadabadi A. – Sertraline https://www.
 ncbi.nlm.nih.gov/books/NBK547689/
ncbi.nlm.nih.gov/books/NBK547689/
FGBNU NTsPZ. ‹‹Endogenous anesthetic depressions (psychopathology, therapy) ››
Feedback form
Question about the work of the siteQuestion to a specialistQuestion to the administration of the clinic
email address
Name
Message text
left by Associate Professor of the Department of Psychiatry of the Russian Medical Academy of Postgraduate Education, Cand. honey. Sciences Baranov PA. The manual presents an analysis of psychopathological variants of anesthetic depression. Depending on the clinical structure p ‹‹Endogenous anesthetic depressions (psychopathology, therapy)››
Features of the treatment of anesthetic depression.
- Main
- Library
- Manuals for physicians
- Endogenous anesthetic depressions (psychopathology, therapy)
- Features of the treatment of anesthetic depressions.
Anxiety-anesthetic depression is treated with antidepressants with sedative and anxiolytic action: tricyclic (amitriptyline 150-250 mg/day, clomipramine (anafranil) 150-250 mg/day, trimipramine (gerfonal) 100-150 mg/day) , serotonergic (sertraline (zoloft) 50-300 mg/day and fluvoxamine (fevarin) 100-300 mg/day) and tetracyclic (maprotiline (ludiomil) 250-300 mg/day).
Tranquilizers are prescribed as adjuvants and for anxiolytic purposes in combination therapy: phenazepam 3-6 mg/day, diazepam (seduxen, relanium) 10-30 mg/day, lorazepam (merlit) 2-6 mg/day, alprazolam (Xanax, Cassadan) 2-4 mg/day and neuroleptics: alimemazine (teralen) 30-45 mg/day, thioridazine (sonapax) 30-40 mg/day, chlorprothixene 100-150 mg/day, clozapine (leponex, azaleptin ) 50-100 mg / day.
For anesthetic depression antidepressants with a powerful thymoanaleptic effect are used, as well as drugs with a "balanced" effect. Tricyclic antidepressants are used: imipramine (melipramine) 150-250 mg/day, clomipramine (anafranil) 150-250 mg/day; serotonergic agents: fluoxetine (Prozac, Portal) 20-80 mg/day and sertraline (Zoloft) 50-300 mg/day, as well as maprotiline (Ludiomil) 250-300 mg/day. Antidepressants, if necessary, are combined, while the doses of tricyclic drugs in combination with serotonergic drugs are reduced by half compared to the above. With the ineffectiveness of the described means in some patients, the use of a reversible monoamine oxidase inhibitor, moclobemide (Aurorix) at the maximum daily dose (600 mg / day), is successful.
With the ineffectiveness of the described means in some patients, the use of a reversible monoamine oxidase inhibitor, moclobemide (Aurorix) at the maximum daily dose (600 mg / day), is successful.
Usually it is necessary to add antipsychotics with a stimulating effect: trifluoperazine (stelazine, triftazine) 5-10 mg/day, sulpiride (eglonil) 100-400 mg/day, etaperazine 4-8 mg/day.
It should be noted that anxiety- and dreary-anesthetic depressions do not show marked resistance to therapy in most cases. If resistance is detected, then intravenous drip of antidepressants (amitriptyline, imipramine, clomipramine, maprotiline) is effective, increasing the dose to a maximum of 125-150 mg / day in combination with the above listed tranquilizers and antipsychotics. Usually success brings a course of intravenous drip infusions for 15-20 days. If there is no effect, it is necessary to carry out a one-stage cancellation of therapy according to the proposed G.Ya. Avrutsky method. In some patients, the effect of treatment may be incomplete: depression from a melancholy or anxious anesthetic becomes purely anesthetic, which, however, is subjectively less severe for patients (see below for the treatment of purely anesthetic depression). At the same time, patients become able-bodied and consider the transition to purely anesthetic depression as a "positive" dynamics of their condition.
In some patients, the effect of treatment may be incomplete: depression from a melancholy or anxious anesthetic becomes purely anesthetic, which, however, is subjectively less severe for patients (see below for the treatment of purely anesthetic depression). At the same time, patients become able-bodied and consider the transition to purely anesthetic depression as a "positive" dynamics of their condition.
The general sequence of therapeutic interventions for anxious and melancholy anesthetic depressions is as follows: oral therapy with one antidepressant in combination with a tranquilizer and (or) neuroleptic (2-3 weeks)! combination of two oral antidepressants or administration of moclobemide (2-3 weeks) ! intravenous drip of an antidepressant (2-3 weeks)! immediate withdrawal of therapy. It should be noted that in some patients, serotonergic drugs and moclobemide are more effective than powerful tricyclic antidepressants.
Against the background of treatment with antidepressants and, especially, after simultaneous withdrawal of therapy, an affect inversion with the development of mania (hypomania) may occur, therefore, in order to prevent the latter and increase the effectiveness of therapy, it is recommended to prescribe normothymic drugs: lithium salts and carbamazepine.
Purely anesthetic depressions , in contrast to anxious and dreary anesthetic depressions, in the vast majority of cases they show a pronounced resistance to therapy, which allows only a slight decrease in the intensity of anesthetic disorders during treatment, but not to stop the symptoms completely. This condition is prone to a protracted long-term course and often develops as part of a schizophrenic process. If purely anesthetic depression is detected, high doses of tricyclic antidepressants (imipramine, clomipramine 300–350 mg/day) should be immediately prescribed or intravenous drip injection of these drugs should be started immediately, reaching maximum dosages (125–150 mg/day). S.N. Mosolov (1995) recommends in such cases the tactics of "rapid thymoanalepsy": anafranil is administered intravenously, starting from 25-50 mg / day with a daily dose increase of 25-50 mg (i.e. 1-2 ampoules) with a rapid achievement maximum daily level of 150 mg. To enhance the effect, 25-75 mg (1-3 ampoules) of maprotiline (Ludiomil) are sometimes added to the infusion system. After 15-20 days, in the absence of an effect, it is recommended to carry out a one-time cancellation of therapy, against which in some patients it is possible to achieve a decrease in the severity of anesthetic disorders. Sometimes it is necessary to resume therapy and 2-3 more sessions of cancellation.
After 15-20 days, in the absence of an effect, it is recommended to carry out a one-time cancellation of therapy, against which in some patients it is possible to achieve a decrease in the severity of anesthetic disorders. Sometimes it is necessary to resume therapy and 2-3 more sessions of cancellation.
In patients with purely anesthetic depression, antidepressants must be combined with antipsychotics of stimulating and anti-negative action (trifluoperazine 5-10 mg/day, etaperazine 4-8 mg/day, sulpiride 100-400 mg/day).
The experience of using electroconvulsive therapy for anesthetic depression is contradictory (both the effectiveness and complete ineffectiveness of this type of treatment and even worsening of the condition after it are described), therefore it is not possible to unambiguously recommend this technique for resistant anesthetic depression.
It should be added that in the event of anesthetic depression against the background of a pronounced progression of the schizophrenic process or in the presence of delusional disorders in the structure of depression, it is mandatory to prescribe powerful antipsychotics in medium doses (trifluoperazine 10-30 mg / day, clozapine 100-150 mg / day) regardless of the psychopathological type of depression.
Prozac generation. How the truth about antidepressants was hidden from us - Snob
Thirty years ago, the introduction of Prozac in American pharmacies revolutionized the treatment of depression. Today, however, scientists say we don't know what depression is or whether Prozac actually works. "Snob" cites theses from Quartz's article on why modern approaches to the treatment of depression can be based on misconceptions and what to do for people who suffer from mental illness
Today it is widely believed that depression is the result of biochemical disorders of the brain. In fact, this is just one of the hypotheses that is so often replicated in the scientific community that it has come to be perceived as a proven truth.
This happened because in medical science psychiatry for a long time did not have the weight of and, as a rule, was associated with the Hippocratic theory of four types of temperament and phrenology (pseudo-science about the connection of the psyche with the shape of the skull). For doctors, Freud's psychoanalytic theory was not convincing either. Under these conditions, the hypothesis that mental illness is a consequence of organic disorders of the brain sounded very attractive. This version was most often discussed as the main one, however, significant studies confirming it have not appeared.
For doctors, Freud's psychoanalytic theory was not convincing either. Under these conditions, the hypothesis that mental illness is a consequence of organic disorders of the brain sounded very attractive. This version was most often discussed as the main one, however, significant studies confirming it have not appeared.
One of the first drugs to "capitalize" the hypothesis of mental illness as a result of biochemical brain disorders was Prozac (fluoxetine). The drug appeared in American pharmacies 30 years ago, and we still do not know how it works and whether it is really effective in treating depression.
Psychiatrists, who benefit from arguing that depression is a disease of the brain and not a mental illness, insist on medication. Left behind are various social factors that can also provoke depression: isolation, poverty, tragic events in life, and much more. Psychotherapy as a method of treatment is secondary to pills. This distorts not only our understanding of depression, but even our experience of it.
Various types of depressive disorders* have been described today. For example, major depressive disorder, drug-induced depressive disorder, organic mood disorders resulting from an organic disease. They all differ in etiology and duration, but the symptoms described are generally the same. Patients with different depressive states are treated with the same drugs, although there is no question of the same violations of the biochemical processes of the brain.
In the 1950s and 1970s, some pretty dangerous drugs were available in American pharmacies to treat depression. Even a slight overdose of these drugs - Butisol (barbiturate) and Valium (diazepam) - could be fatal, which deterred many buyers. The introduction of Prozac made a big difference because it was a new generation of antidepressants, safer and with fewer unpleasant side effects.
Antidepressants that exist today work more or less the same way. So says Anthony Rothschild, Professor of Psychiatry at the University of Massachusetts Medical School. What's more, over the past three decades of Prozac's use in the treatment of depression, the choice of antidepressants in pharmacies has grown significantly. However, nothing more effective than imipramine, the main drug of tricyclic antidepressants, has not been created.
What's more, over the past three decades of Prozac's use in the treatment of depression, the choice of antidepressants in pharmacies has grown significantly. However, nothing more effective than imipramine, the main drug of tricyclic antidepressants, has not been created.
All this time, antidepressant manufacturers have been able to claim that depression is a brain disorder that can be corrected with pills: , both Paroxetine and Zoloft (sertraline) were marketed as "chemical rebalancing" drugs. Meanwhile, there are still no convincing, scientifically proven versions of the causes of depression.
According to modern research, depression is inherited in 37 percent of cases , so obviously genetics and biology play a significant role. But since neuroscientists still don't have a precise way to determine what brain function is considered "normal" and what is not, it's impossible to test some of the hypotheses.
If serotonin levels were the cause of depression, then SSRIs would work instantly instead of requiring a long cycle of dosing**. In addition, a decrease in the level of serotonin in the brain should provoke depression, but studies show that this is not the case. This does not mean that antidepressants aimed at restoring serotonin levels do not work. But we don't know if they ultimately address the root cause of depression or just combat its effects.
Our ideas about diseases and their nature influence their course. For example, the symptoms of anorexia in patients in Hong Kong have changed as people in the region become more aware of how the disease works in Western countries. It is possible that our current understanding of depression and the medical approach are leading to the fact that the disease covers more people: psychiatry calls mental illness even those conditions that were previously considered stress or emotional decline.
According to this study, the placebo effect in treating depression is almost as good as taking antidepressants. The difference is so small that it practically does not affect the clinical picture. The author of the study, director of the placebo study program at Harvard Medical School, Irwin Kirsch, is a staunch supporter of non-drug treatments for depression. Studies show that pills and psychotherapy are effective in the short term, but patients treated without medication feel better over a longer period of time and have a significantly lower relapse rate. Kirsch, of course, is full of opponents who, on the contrary, are convinced that drugs are necessary.
The truth, as is often the case, is somewhere in between: severely depressed patients who are unable to go to psychotherapy should definitely be prescribed medication. Those who are able to undergo psychotherapy should definitely do this, especially since drug treatment does not help all patients.