Blue light therapy bipolar disorder
Blue Light, Depression, and Bipolar Disorder
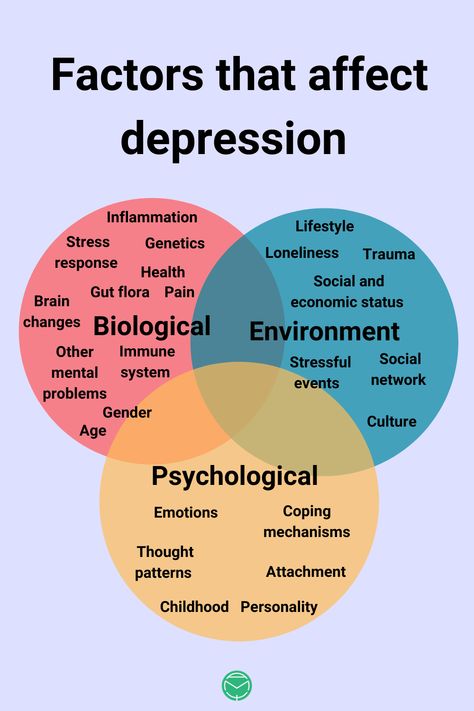
Blue light is associated with a host of physical health maladies, including obesity, diabetes, and cancer. But what does it do to patients with depression or bipolar disorder?
PSYCHPEARLS PODCAST
Blue light is getting blamed for everything from eye strain to cancer lately, but what does it do to our patients with depression and bipolar disorder. A lot, as you will see in this podcast, but it depends on what time of day it is shining.
Welcome to PsychPearls podcast with Psychiatric TimesTM, the Voice of Psychiatry. With thoughtful insights into the world of mental health, this podcast provides timely clinical commentary and practical cutting-edge pearls for you and your practice. We hope you enjoy.
I am Chris Aiken, the Mood Disorders Section Editor for Psychiatric TimesTM and the editor-in-chief of the Carlat Psychiatry Report, and I am Kellie Newsome, a psychiatric NP and the cohost of the Carlat Psychiatry Podcast.
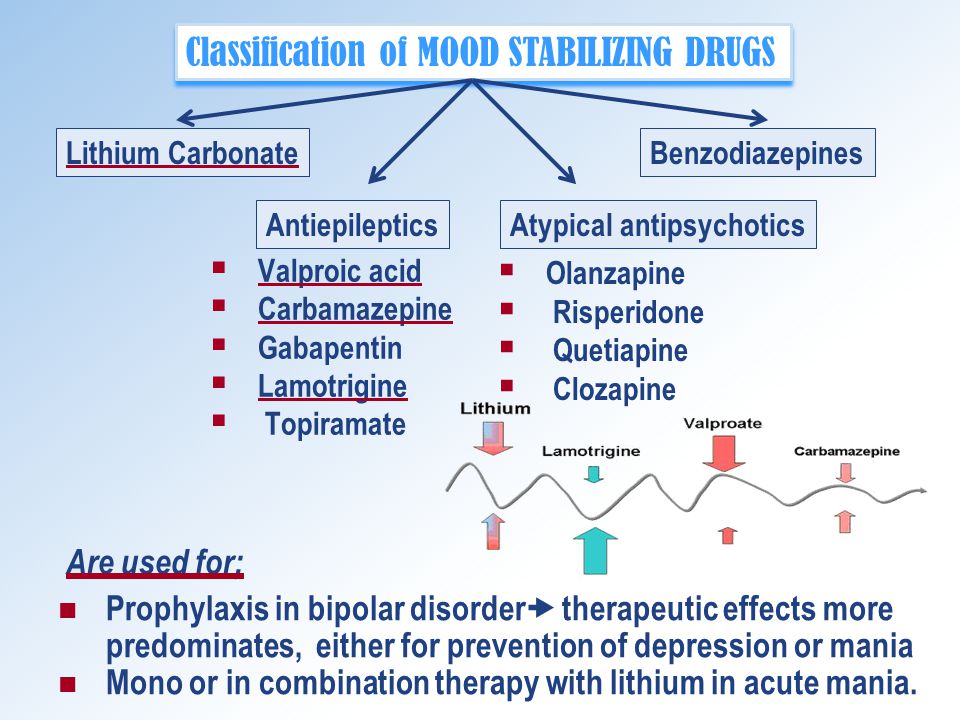
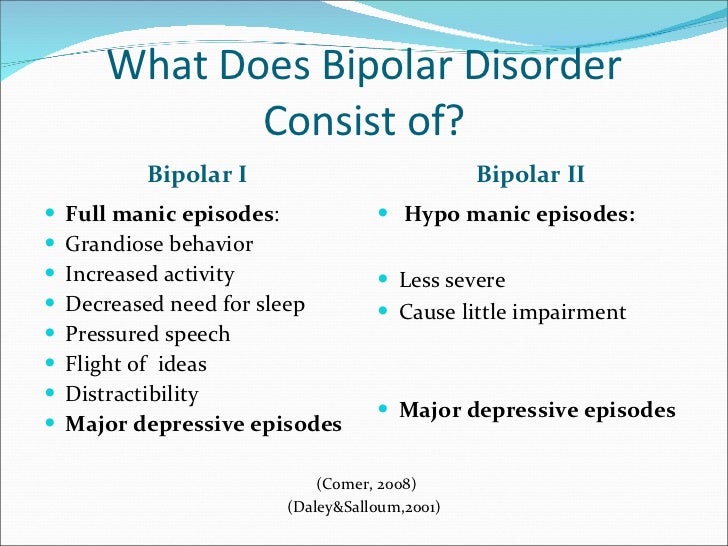
KELLIE NEWSOME: The biological clock is set by the daily rhythms of light and dark – morning sunrise and evening sunset. And this clock is so integral to bipolar disorder that you could almost rename it fragile circadian rhythm disorder. Actually, patients prefer that name over bipolar disorder, and it gets to the heart of the problem. Bipolar is tightly linked to the genes that regulate the biological clock, and lithium actually helps repair the clock by altering the expression of those genes.1 Many of the behavioral therapies for bipolar disorder, like dark therapy and social rhythm therapy, also work through the biological clock, helping patients to keep it running smoothly by regulating their exposure to light, darkness, and the timing of daily activities.
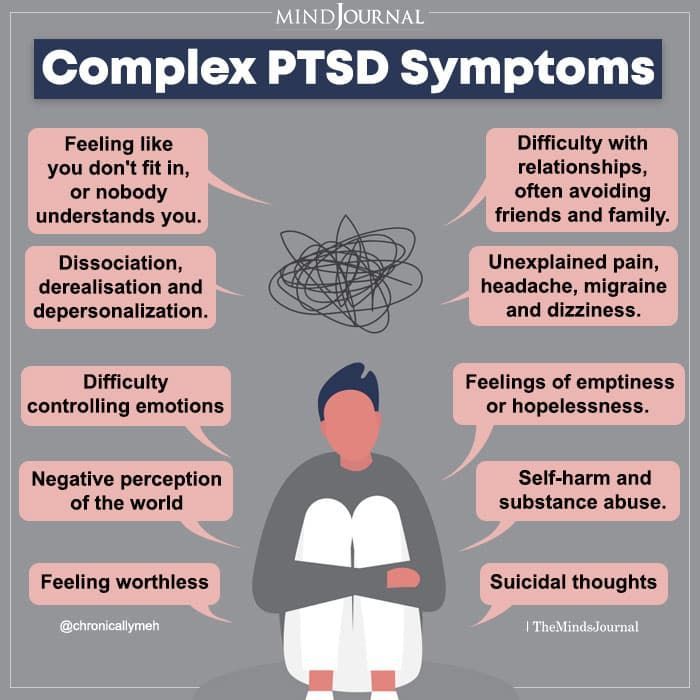
But bipolar is not the only mental illness that is linked to disrupted circadian rhythms. Unipolar depression is as well, though to a lesser extent – for example, rates of circadian rhythm disorders like the phase-delay night owl syndrome are more common in bipolar and unipolar, but they are about 20% less common in unipolar.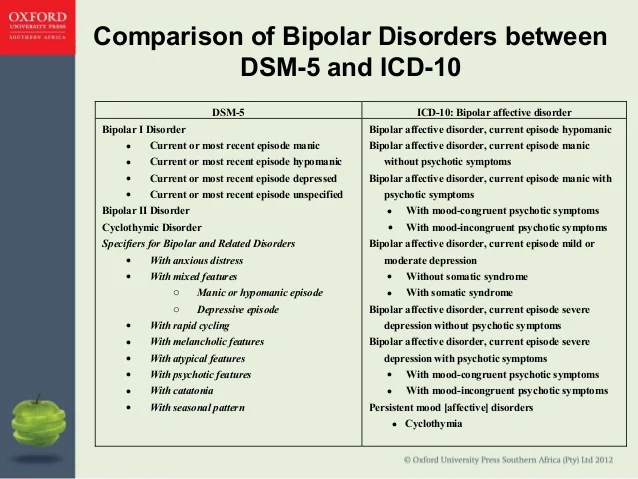 And research is exploring circadian rhythm therapies in borderline personality disorder, substance use disorders, schizophrenia, ADHD, and PTSD.
And research is exploring circadian rhythm therapies in borderline personality disorder, substance use disorders, schizophrenia, ADHD, and PTSD.
But while researching is advancing in the circadian direction, society is moving the other way. Indoor living and nocturnal light are dampening the natural signals that set the biological clock, and there is evidence that this is causing harm in our patients. In this podcast, we will explore those dangers, but first a little background on how light – and in particular blue light – set the biological clock.
Blue Light and Melatonin
KELLIE NEWSOME: Light suppresses melatonin, but not just any light. It is the color that matters here, and blue light in the 460-480 nm range is particularly good at suppressing melatonin and promoting wakefulness. In the 1990s, a new photoreceptor called melanopsin was discovered that only responds to blue light, and it is this receptor that regulates melatonin production through the suprachiasmatic nucleus, the time-keeper of the biological clock. 2
2
What that means is that the body’s internal clock depends on strong shifts in blue-spectrum light at the bookends of the day: morning and night. High levels of evening blue light, and low levels in the morning, disrupt not just circadian rhythms but also the clock genes implicated in bipolar and other psychiatric disorders.3,4
The main source of that blue light are electronic gadgets that were not available 20 years ago. Smart phones, LED screens, and energy-efficient bulbs emit a blue haze of light that is very different from the yellow starlight that we evolved under. This light may look white, like fluorescent bulbs, but white light has a lot of the blue wavelength within it. Distance also matters here. A cell phone close to your face emits about as much blue light as a large screen TV across the living room.
CHRIS AIKEN: The problem is not just psychiatric. Blue light is associated with physical health risks including obesity, diabetes, cancer, cardiovascular and neurologic diseases, gastrointestinal ulcers, and adverse reproductive outcomes. 5 The American Medical Association released a position statement calling for reductions in nocturnal blue light, and psychiatry is catching on as well. The American Academy of Child and Adolescent Psychiatry updated their pediatric sleep recommendations in 2018. They no longer recommend night lights for anxious children and instead emphasize elimination of blue-light sources in the bedroom. Child psychiatrists in Canada have even stronger recommendations.
5 The American Medical Association released a position statement calling for reductions in nocturnal blue light, and psychiatry is catching on as well. The American Academy of Child and Adolescent Psychiatry updated their pediatric sleep recommendations in 2018. They no longer recommend night lights for anxious children and instead emphasize elimination of blue-light sources in the bedroom. Child psychiatrists in Canada have even stronger recommendations.
KELLIE NEWSOME: It is the young and old that are most vulnerable to these light changes, as we will see in the research here.6,7 But they are also the patients who are more likely to sleep with some lights on. So, if your patient needs a light at night – whether because of a childhood phobia or a fall risk – they can purchase amber nightlights that do not emit the blue wavelength.
A Slightly Broken Biological Clock
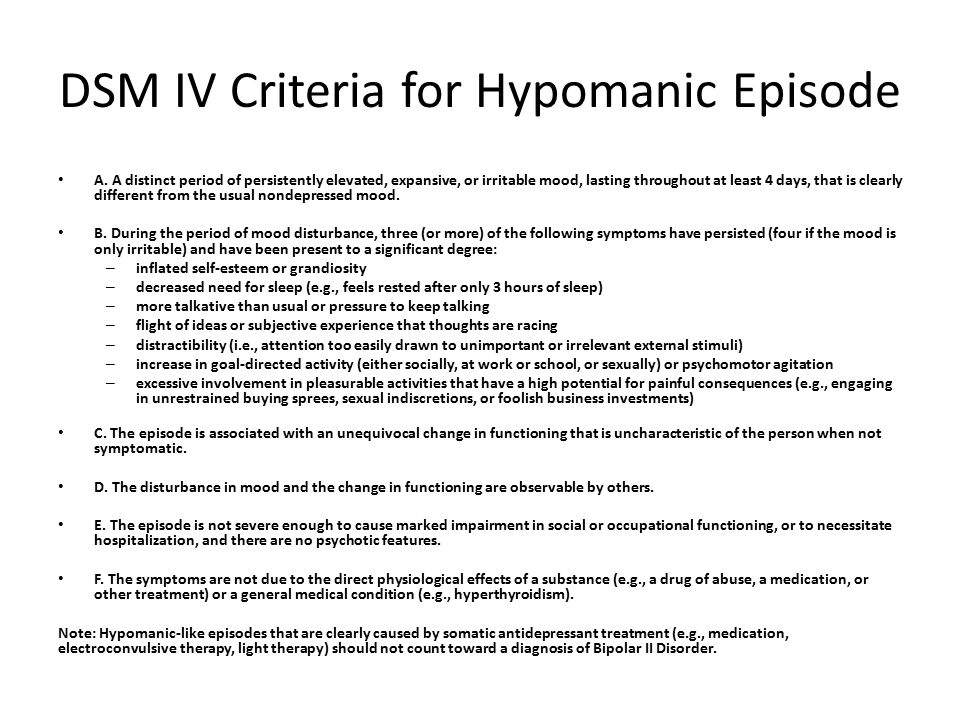
CHRIS AIKEN: Psychiatric patients in general are more sensitive to the circadian disrupting effects of evening blue light, particularly patients with bipolar disorder.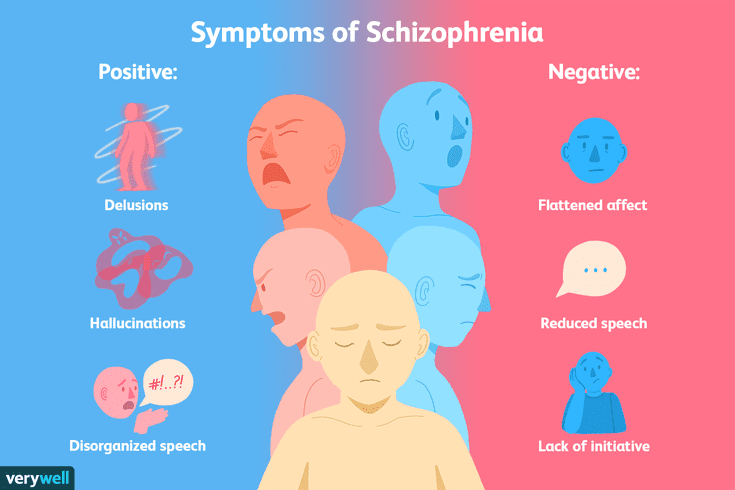 Melatonin is delayed, diminished, and more easily suppressed by blue light in these patients.6 Circadian disruptions often trigger new episodes of mania and depression, such as shift work, seasonal changes, and travel across multiple time zones.8
Melatonin is delayed, diminished, and more easily suppressed by blue light in these patients.6 Circadian disruptions often trigger new episodes of mania and depression, such as shift work, seasonal changes, and travel across multiple time zones.8
KELLIE NEWSOME: Travel across time zones is only a problem with air travel, because the clock has time to adjust when you travel by land or sea unless you are driving at 300 miles per hour. And on average it only causes problems when patients travel across 2 or more time zones. Mania is more common with west to east travel, and depression more likely when travelling east to west. A simple rhyme can help you remember it – west is depressed – because travelling westbound can trigger depression.
CHRIS AIKEN: We can add nocturnal blue light and ambient bedroom light to that list of circadian disruptors. Evening use of smartphones delays and reduces melatonin secretion, and impairs sleep and cognition with a medium effect size (0.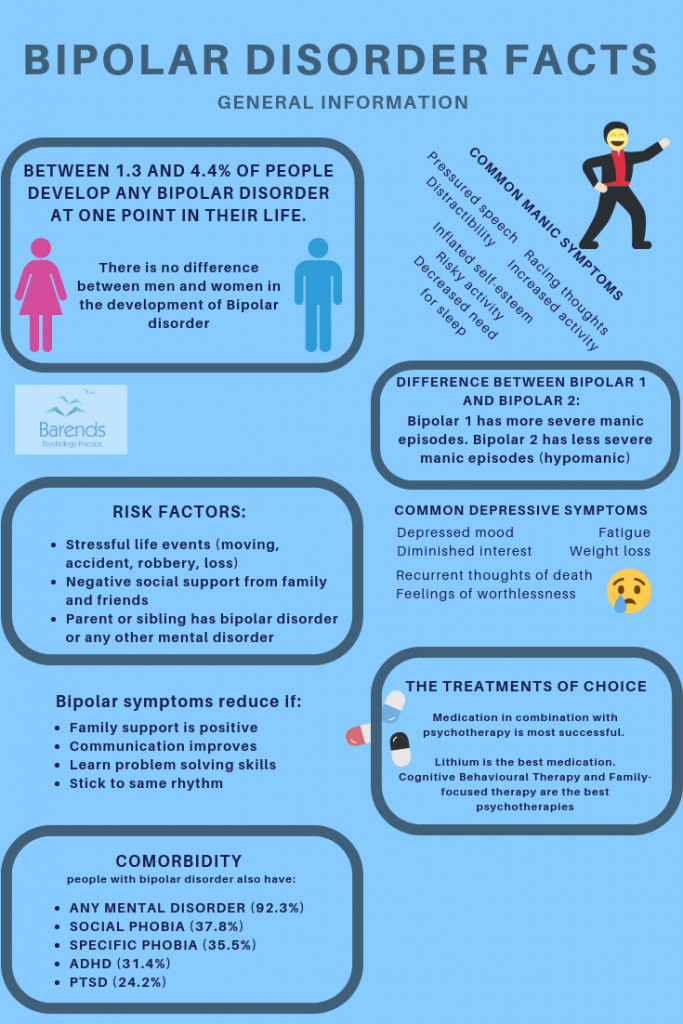 5), which means the effect should be noticeable to the casual observer.9 A viscous cycle is at play here, as evening-types (night owls) have a greater tendency to use electronics at night, and that use independently shifts circadian rhythms toward the evening type (phase delay).6,10 The evening chronotype is prominent in adolescents, and being a night owl is a risk factor for bipolar disorder, depression, and substance abuse.8,10
5), which means the effect should be noticeable to the casual observer.9 A viscous cycle is at play here, as evening-types (night owls) have a greater tendency to use electronics at night, and that use independently shifts circadian rhythms toward the evening type (phase delay).6,10 The evening chronotype is prominent in adolescents, and being a night owl is a risk factor for bipolar disorder, depression, and substance abuse.8,10
Ambient bedroom light is also a problem, as it passes through the eyelids and suppresses melatonin during sleep. In controlled animal studies, ambient nocturnal light causes depression, impedes learning, and has detrimental effects on the brain. It lowers BDNF and shortens the dendritic spines that are essential for learning and cognition.11
The circadian system is also involved in critical periods of brain development, and disruptions of light signals may play a role in the onset of psychiatric illnesses as well as their exacerbation. 12 When mice are exposed to nocturnal dim light as infants, they grow up to have more anxiety as adults.13 Human studies have found a strong link between rapid flux of spring sunlight and earlier onset of bipolar disorder.14
12 When mice are exposed to nocturnal dim light as infants, they grow up to have more anxiety as adults.13 Human studies have found a strong link between rapid flux of spring sunlight and earlier onset of bipolar disorder.14
A study from Japan illustrates the problem for our patients.15 They followed 863 older adults for several years, carefully measuring how much light they were exposed to in their bedrooms. On follow up, the risk of depression was directly correlated with how much light they were exposed to in their bedrooms. Those who slept in pitch darkness had the lowest risk, but what is interesting is how little light was necessary to accomplish the shift: 5 lux – which is equivalent to a night light – was the cut off. Those who slept with at least 5 lux in their bedroom had double the risk of depression 2 years later.
That study was not controlled, although they attempted to control for confounders that might otherwise explain the association.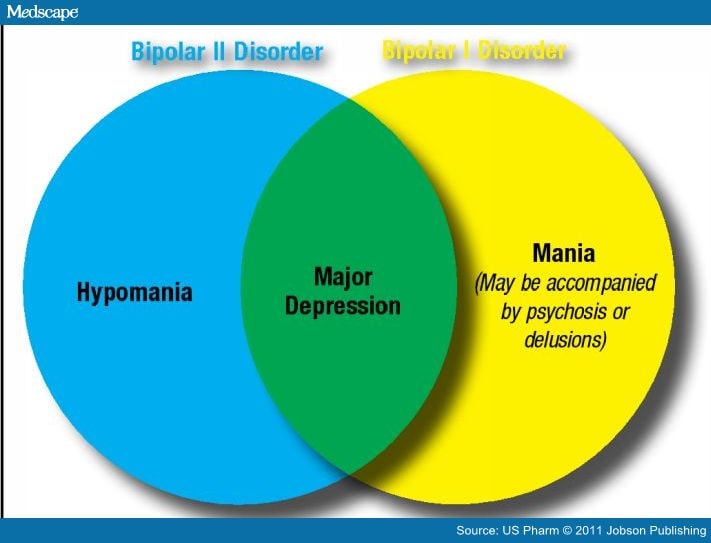 But buried in the discussion was a sentence that struck me. The authors believed that the health risks of evening light are so well documented in animal and epidemiologic human studies that a controlled trial would be unethical in humans. In other words, we already know too much to learn anymore.15
But buried in the discussion was a sentence that struck me. The authors believed that the health risks of evening light are so well documented in animal and epidemiologic human studies that a controlled trial would be unethical in humans. In other words, we already know too much to learn anymore.15
Instead, it is time for action, to educate our patients to follow the natural flow of day and night. That means bright light in the morning, low levels of blue light in the evening, and pitch dark in the bedroom. Those steps are not easy to follow in the modern world, and in a future podcast we will review new technologies that can ease those changes.
KELLIE NEWSOME: Join us then on PsychPearls, and you can also catch us every Monday on the Carlat Psychiatry Podcast.
Chris Aiken, MD, is the Mood Disorders Section Editor for Psychiatric TimesTM, the Editor in Chief of The Carlat Psychiatry Report, and the director of the Mood Treatment Center. He has written several books on mood disorders, most recently The Depression and Bipolar Workbook. He can be heard in the weekly Carlat Psychiatry Podcast with his cohost Kellie Newsome, PMH-NP. The author does not accept honoraria from pharmaceutical companies but receives royalties from PESI for The Depression and Bipolar Workbook and from W.W. Norton & Co. for Bipolar, Not So Much. Kellie L. Newsome, PMH-NP, is the cohost of the Carlat Psychiatry Podcast and is also a practicing psychiatric mental health nurse practitioner in Winston Salem, NC, at the Mood Treatment Center. Raised in Tasmania, Australia, Kellie moved to the United States in 1998.
He has written several books on mood disorders, most recently The Depression and Bipolar Workbook. He can be heard in the weekly Carlat Psychiatry Podcast with his cohost Kellie Newsome, PMH-NP. The author does not accept honoraria from pharmaceutical companies but receives royalties from PESI for The Depression and Bipolar Workbook and from W.W. Norton & Co. for Bipolar, Not So Much. Kellie L. Newsome, PMH-NP, is the cohost of the Carlat Psychiatry Podcast and is also a practicing psychiatric mental health nurse practitioner in Winston Salem, NC, at the Mood Treatment Center. Raised in Tasmania, Australia, Kellie moved to the United States in 1998.
References
1. Moreira J, Geoffroy PA. Lithium and bipolar disorder: Impacts from molecular to behavioural circadian rhythms. Chronobiol Int. 2016;33(4):351-373.
2. Charrier A, Olliac B, Roubertoux P, et al. Clock genes and altered sleep-wake rhythms: their role in the development of psychiatric disorders. Int J Mol Sci. 2017;18(5).
Clock genes and altered sleep-wake rhythms: their role in the development of psychiatric disorders. Int J Mol Sci. 2017;18(5).
3. Olliac B, Ouss L, Charrier A. Suicide attempts in children and adolescents: The place of clock genes and early rhythm dysfunction. J Physiol Paris. 2016;110(4 Pt B):461-466.
4. Lunn RM, Blask DE, Coogan AN, et al. Health consequences of electric lighting practices in the modern world: A report on the National Toxicology Program's workshop on shift work at night, artificial light at night, and circadian disruption. Sci Total Environ. 2017;607-608:1073-1084.
5. Touitou Y, Touitou D, Reinberg A. Disruption of adolescents' circadian clock: The vicious circle of media use, exposure to light at night, sleep loss and risk behaviors. J Physiol Paris. 2016;110(4 Pt B):467-479.
6. Abreu T, Bragança M. The bipolarity of light and dark: A review on bipolar disorder and circadian cycles. J Affect Disord. 2015;185:219-29.
2015;185:219-29.
7. Takaesu Y. Circadian rhythm in bipolar disorder: A review of the literature. Psychiatry Clin Neurosci. 2018 Jun 5.
8. Heo JY, Kim K, Fava M, et al. Effects of smartphone use with and without blue light at night in healthy adults: A randomized, double-blind, cross-over, placebo-controlled comparison. J Psychiatr Res. 2017;87:61-70.
9. Vollmer C, Michel U, Randler C. Outdoor light at night (LAN) is correlated with eveningness in adolescents. Chronobiol Int. 2012;29(4):502-508.
10. Kivelä L, Papadopoulos MR, Antypa N. Chronotype and psychiatric disorders. Curr Sleep Med Rep. 2018;4(2):94-103.
11. Bedrosian TA, Vaughn CA, Galan A, et al. Nocturnal light exposure impairs affective responses in a wavelength-dependent manner. J Neurosci. 2013;33(32):13081-13087.
12. Kobayashi Y, Ye Z, Hensch TK. Clock genes control cortical critical period timing. Neuron. 2015;86(1):264-275.
13. Borniger JC, McHenry ZD, Abi Salloum BA, et al. Exposure to dim light at night during early development increases adult anxiety-like responses. Physiol Behav. 2014;133:99-106.
Borniger JC, McHenry ZD, Abi Salloum BA, et al. Exposure to dim light at night during early development increases adult anxiety-like responses. Physiol Behav. 2014;133:99-106.
14. Bauer M, Glenn T, Alda M, et al. Solar insolation in springtime influences age of onset of bipolar I disorder. Acta Psychiatr Scand. 2017;136:571-582.
15. Obayashi K, Saeki K, Kurumatani N. Bedroom light exposure at night and the incidence of depressive symptoms: a longitudinal study of the heijo-kyo cohort. Am J Epidemiol. 2018;187(3):427-434.
Blue Light Blocking Treatment for the Treatment of Bipolar Disorder: Directions for Research and Practice
1. Ham W.T., Mueller H.A., Ruffolo J.J., Clarke A.M. Sensitivity of the retina to radiation damage as a function of wavelength. Photochem. Photobiol. 1979;29:735–743. doi: 10.1111/j.1751-1097.1979.tb07759.x. [PubMed] [CrossRef] [Google Scholar]
2. Jaadane I., Boulenguez P., Chahory S., Carré S., Savoldelli M.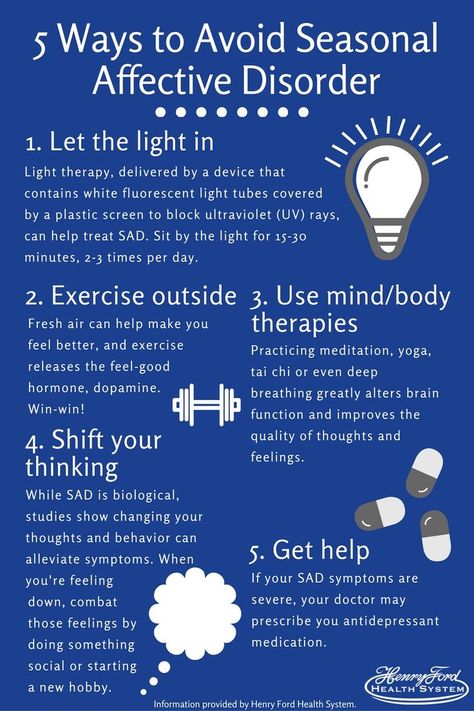 , Jonet L., Behar-Cohen F., Martinsons C., Torriglia A. Retinal damage induced by commercial light emitting diodes (LEDs) Free Radic. Biol. Med. 2015;84:373–384. doi: 10.1016/j.freeradbiomed.2015.03.034. [PubMed] [CrossRef] [Google Scholar]
, Jonet L., Behar-Cohen F., Martinsons C., Torriglia A. Retinal damage induced by commercial light emitting diodes (LEDs) Free Radic. Biol. Med. 2015;84:373–384. doi: 10.1016/j.freeradbiomed.2015.03.034. [PubMed] [CrossRef] [Google Scholar]
3. Van der Lely S., Frey S., Garbazza C., Wirz-Justice A., Jenni O.G., Steiner R., Wolf S., Cajochen C., Bromundt V., Schmidt C. Blue blocker glasses as a countermeasure for alerting effects of evening light-emitting diode screen exposure in male teenagers. J. Adolesc. Health. 2015;56:113–119. doi: 10.1016/j.jadohealth.2014.08.002. [PubMed] [CrossRef] [Google Scholar]
4. Henriksen T.E., Skrede S., Fasmer O.B., Hamre B., Grønli J., Lund A. Blocking blue light during mania–markedly increased regularity of sleep and rapid improvement of symptoms: A case report. Bipolar Disord. 2014;16:894–898. doi: 10.1111/bdi.12265. [PubMed] [CrossRef] [Google Scholar]
5. Sarzetto A., Cavallini M.C., Fregna L., Attanasio F., Pacchioni F., Barbini B., Franchini L. , Colombo C. Blue blocking glasses for the treatment of mania in an elderly patient: A case report with polysomnographic findings. Bipolar Disord. 2021;23:367–639. doi: 10.1111/bdi.13051. [PubMed] [CrossRef] [Google Scholar]
, Colombo C. Blue blocking glasses for the treatment of mania in an elderly patient: A case report with polysomnographic findings. Bipolar Disord. 2021;23:367–639. doi: 10.1111/bdi.13051. [PubMed] [CrossRef] [Google Scholar]
6. Kaufman K., Trenton A., Campeas M., Aziz R., Coluccio M. Blue light mania and trigeminal neuralgia: Case analysis with literature review in the context of organ donation. Bipolar Disord. 2017;19:118. [Google Scholar]
7. Phelps J. Dark therapy for bipolar disorder using amber lenses for blue light blockade. Med. Hypotheses. 2008;70:224–229. doi: 10.1016/j.mehy.2007.05.026. [PubMed] [CrossRef] [Google Scholar]
8. Esaki Y., Takeuchi I., Tsuboi S., Fujita K., Iwata N., Kitajima T. A double-blind, randomized, placebo-controlled trial of adjunctive blue-blocking glasses for the treatment of sleep and circadian rhythm in patients with bipolar disorder. Bipolar Disord. 2020;22:739–748. doi: 10.1111/bdi.12912. [PubMed] [CrossRef] [Google Scholar]
9. Henriksen T.E., Skrede S., Fasmer O.B., Schoeyen H., Leskauskaite I., Bjørke-Bertheussen J., Assmus J., Hamre B., Grønli J., Lund A. Blue-blocking glasses as additive treatment for mania: A randomized placebo–controlled trial. Bipolar Disord. 2016;18:221–232. doi: 10.1111/bdi.12390. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Henriksen T.E., Skrede S., Fasmer O.B., Schoeyen H., Leskauskaite I., Bjørke-Bertheussen J., Assmus J., Hamre B., Grønli J., Lund A. Blue-blocking glasses as additive treatment for mania: A randomized placebo–controlled trial. Bipolar Disord. 2016;18:221–232. doi: 10.1111/bdi.12390. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
10. Lamb T.D., Collin S.P., Pugh E.N. Evolution of the vertebrate eye: Opsins, photoreceptors, retina and eye cup. Nat. Rev. Neurosc. 2007;8:960–976. doi: 10.1038/nrn2283. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
11. Fu Y., Liao H.-W., Do M.T.H., Yau K.-W. Non-image-forming ocular photoreception in vertebrates. Curr. Opin. Neurobiol. 2005;15:415–422. doi: 10.1016/j.conb.2005.06.011. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
12. Shuboni D., Cramm S., Yan L., Nunez A., Smale L. Acute behavioral responses to light and darkness in nocturnal Mus musculus and diurnal Arvicanthis niloticus. J. Biol. Rhythm. 2012;27:299–307.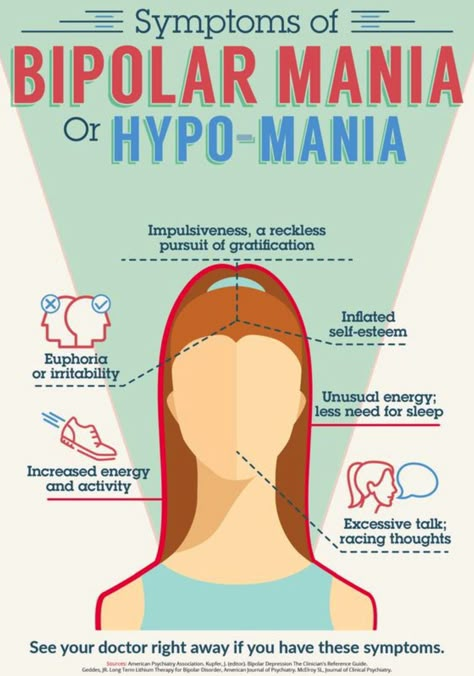 doi: 10.1177/0748730412449723. [PubMed] [CrossRef] [Google Scholar]
doi: 10.1177/0748730412449723. [PubMed] [CrossRef] [Google Scholar]
13. Yokoyama S. Molecular evolution of vertebrate visual pigments. Prog. Retin. Eye Res. 2000;19:385–419. doi: 10.1016/S1350-9462(00)00002-1. [PubMed] [CrossRef] [Google Scholar]
14. Wahl S., Engelhardt M., Schaupp P., Lappe C., Ivanov I.V. The inner clock—Blue light sets the human rhythm. J. Biophotonics. 2019;12:e201900102. doi: 10.1002/jbio.201900102. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
15. Do M.T.H. Melanopsin and the intrinsically photosensitive retinal ganglion cells: Biophysics to behavior. Neuron. 2019;104:205–226. doi: 10.1016/j.neuron.2019.07.016. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
16. Esaki Y., Kitajima T., Takeuchi I., Tsuboi S., Furukawa O., Moriwaki M., Fujita K., Iwata N. Effect of blue-blocking glasses in major depressive disorder with sleep onset insomnia: A randomized, double-blind, placebo-controlled study. Chronobiol. Int. 2017;34:753–761.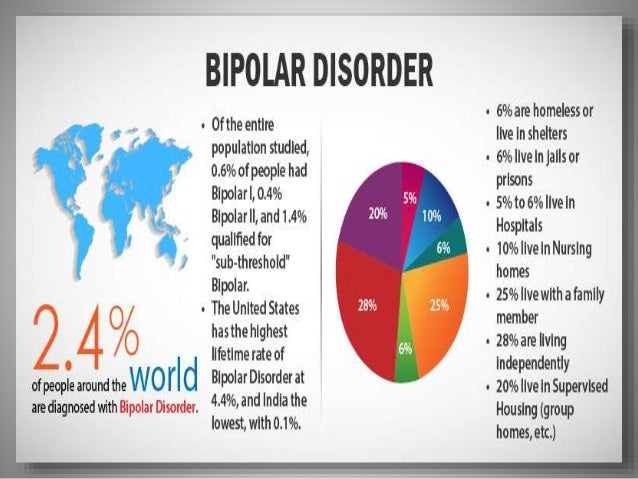 doi: 10.1080/07420528.2017.1318893. [PubMed] [CrossRef] [Google Scholar]
doi: 10.1080/07420528.2017.1318893. [PubMed] [CrossRef] [Google Scholar]
17. Bender A., Werthner P., Samuels C. Sleep optimization improves mood differently between Canadian national team curlers and rowers. Sleep. 2017;40:A293. doi: 10.1093/sleepj/zsx050.791. [CrossRef] [Google Scholar]
18. Bennett S., Alpert M., Kubulins V., Hansler R.L. Use of modified spectacles and light bulbs to block blue light at night may prevent postpartum depression. Med. Hypotheses. 2009;73:251–253. doi: 10.1016/j.mehy.2009.01.049. [PubMed] [CrossRef] [Google Scholar]
19. Çabej N. Epigenetic Principles of Evolution. Elsevier; London, UK: 2012. [Google Scholar]
20. Hedrick P.W. What is the evidence for heterozygote advantage selection? Trends Ecol. Evol. 2012;27:698–704. doi: 10.1016/j.tree.2012.08.012. [PubMed] [CrossRef] [Google Scholar]
21. Soria V., Martínez-Amorós È., Escaramís G., Valero J., Pérez-Egea R., García C., Gutiérrez-Zotes A., Puigdemont D., Bayés M., Crespo J.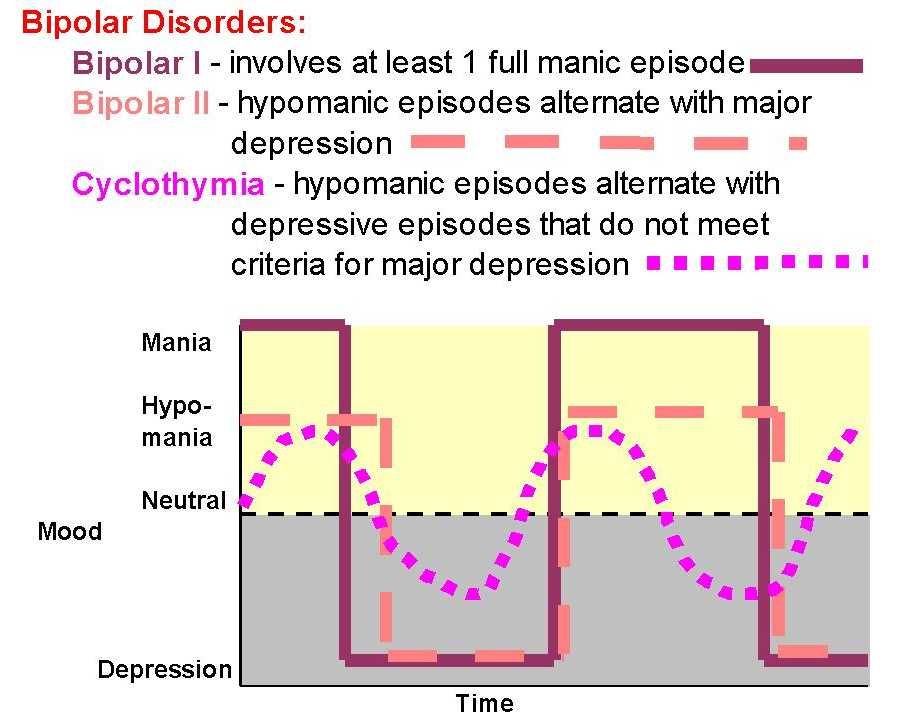 M., et al. Differential Association of Circadian Genes with Mood Disorders: CRY1 and NPAS2 are Associated with Unipolar Major Depression and CLOCK and VIP with Bipolar Disorder. Neuropsychopharmacology. 2010;35:1279–1289. doi: 10.1038/npp.2009.230. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
M., et al. Differential Association of Circadian Genes with Mood Disorders: CRY1 and NPAS2 are Associated with Unipolar Major Depression and CLOCK and VIP with Bipolar Disorder. Neuropsychopharmacology. 2010;35:1279–1289. doi: 10.1038/npp.2009.230. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
22. Partch C.L., Green C.B., Takahashi J.S. Molecular architecture of the mammalian circadian clock. Trends Cell Biol. 2014;24:90–99. doi: 10.1016/j.tcb.2013.07.002. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
23. Loh D.H., Dragich J.M., Kudo T., Schroeder A.M., Nakamura T.J., Waschek J.A., Block G.D., Colwell C.S. Effects of vasoactive intestinal peptide genotype on circadian gene expression in the suprachiasmatic nucleus and peripheral organs. J. Biol. Rhythm. 2011;26:200–209. doi: 10.1177/0748730411401740. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
24. Lewis K.S., Gordon-Smith K., Forty L., Di Florio A., Craddock N., Jones L., Jones I. Sleep loss as a trigger of mood episodes in bipolar disorder: Individual differences based on diagnostic subtype and gender. Br. J. Psychiatry. 2017;211:169–174. doi: 10.1192/bjp.bp.117.202259. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Br. J. Psychiatry. 2017;211:169–174. doi: 10.1192/bjp.bp.117.202259. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
25. Geoffroy P., Scott J., Boudebesse C., Lajnef M., Henry C., Leboyer M., Bellivier F., Etain B. Sleep in patients with remitted bipolar disorders: A meta-analysis of actigraphy studies. Acta Psychiatry Scand. 2015;131:89–99. doi: 10.1111/acps.12367. [PubMed] [CrossRef] [Google Scholar]
26. Sebela A., Kolenic M., Farkova E., Novak T., Goetz M. Decreased need for sleep as an endophenotype of bipolar disorder: An actigraphy study. Chronobiol. Int. 2019;36:1227–1239. doi: 10.1080/07420528.2019.1630631. [PubMed] [CrossRef] [Google Scholar]
27. Lightman S.L., Birnie M.T., Conway-Campbell B.L. Dynamics of ACTH and cortisol secretion and implications for disease. Endocr. Rev. 2020;41:470–490. doi: 10.1210/endrev/bnaa002. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
28. Ellenbogen M.A., Santo J.B., Linnen A.-M., Walker C.-D., Hodgins S.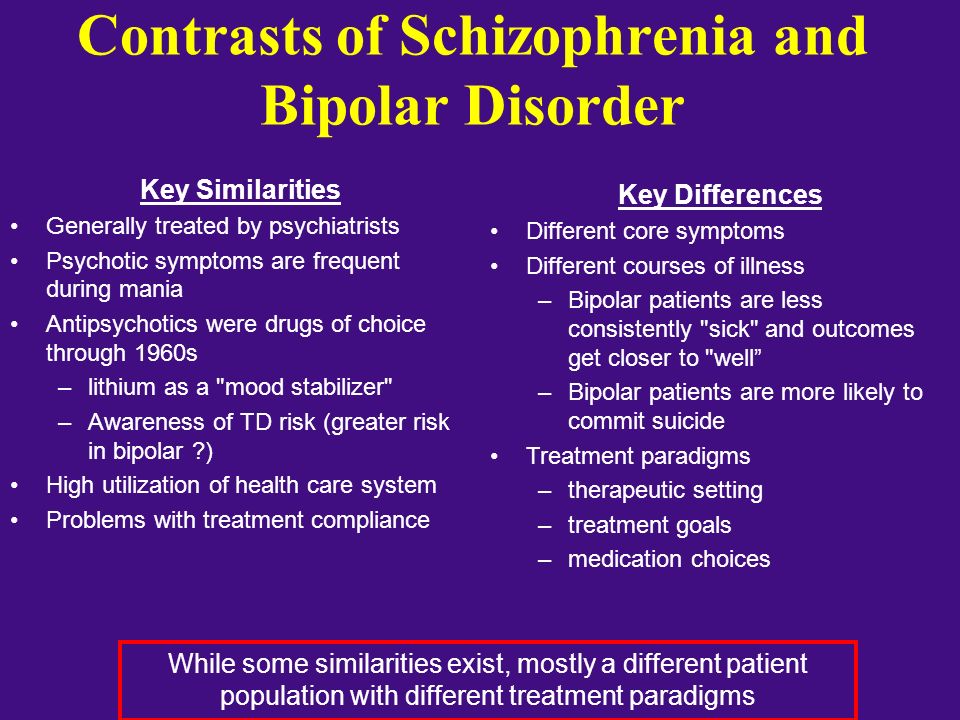 High cortisol levels in the offspring of parents with bipolar disorder during two weeks of daily sampling. Bipolar Disord. 2010;12:77–86. doi: 10.1111/j.1399-5618.2009.00770.x. [PubMed] [CrossRef] [Google Scholar]
High cortisol levels in the offspring of parents with bipolar disorder during two weeks of daily sampling. Bipolar Disord. 2010;12:77–86. doi: 10.1111/j.1399-5618.2009.00770.x. [PubMed] [CrossRef] [Google Scholar]
29. Ostiguy C.S., Ellenbogen M.A., Walker C.D., Walker E.F., Hodgins S. Sensitivity to stress among the offspring of parents with bipolar disorder: A study of daytime cortisol levels. Psychol. Med. 2011;41:2447–2457. doi: 10.1017/S0033291711000523. [PubMed] [CrossRef] [Google Scholar]
30. Scheiermann C., Kunisaki Y., Frenette P.S. Circadian control of the immune system. Nat. Rev. Immunol. 2013;13:190–198. doi: 10.1038/nri3386. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
31. Orozco-Solis R., Aguilar-Arnal L. Circadian Regulation of Immunity through Epigenetic Mechanisms. Front. Cell. Infect. Microbiol. 2020;10:96. doi: 10.3389/fcimb.2020.00096. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
32. Brod S., Rattazzi L., Piras G., D’Acquisto F.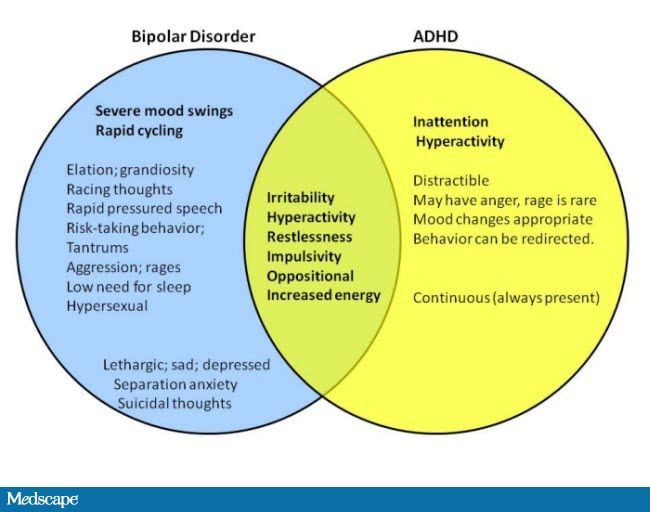 ‘As above, so below’ examining the interplay between emotion and the immune system. Immunology. 2014;143:311–318. doi: 10.1111/imm.12341. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
‘As above, so below’ examining the interplay between emotion and the immune system. Immunology. 2014;143:311–318. doi: 10.1111/imm.12341. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
33. Pietruczuk K., Lisowska K.A., Grabowski K., Landowski J., Witkowski J.M. Proliferation and apoptosis of T lymphocytes in patients with bipolar disorder. Sci. Rep. 2018;8:3327. doi: 10.1038/s41598-018-21769-0. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
34. Pietruczuk K., Lisowska K.A., Grabowski K., Landowski J., Cubała W.J., Witkowski J.M. Peripheral blood lymphocyte subpopulations in patients with bipolar disorder type II. Sci. Rep. 2019;9:5869. doi: 10.1038/s41598-019-42482-6. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
35. Snijders G., Mesman E., de Wit H., Wijkhuijs A., Nolen W.A., Drexhage H.A., Hillegers M.H.J. Immune dysregulation in offspring of a bipolar parent. Altered serum levels of immune growth factors at adolescent age. Brain Behav. Immun. 2017;64:116–123. doi: 10.1016/j.bbi.2017.04.004. [PubMed] [CrossRef] [Google Scholar]
2017;64:116–123. doi: 10.1016/j.bbi.2017.04.004. [PubMed] [CrossRef] [Google Scholar]
36. Koch C.E., Leinweber B., Drengberg B.C., Blaum C., Oster H. Interaction between circadian rhythms and stress. Neurobiol. Stress. 2017;6:57–67. doi: 10.1016/j.ynstr.2016.09.001. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
37. Grandin L.D., Alloy L.B., Abramson L.Y. The social zeitgeber theory, circadian rhythms, and mood disorders: Review and evaluation. Clin. Psychol. Rev. 2006;26:679–694. doi: 10.1016/j.cpr.2006.07.001. [PubMed] [CrossRef] [Google Scholar]
38. Shen G.H., Alloy L.B., Abramson L.Y., Sylvia L.G. Social rhythm regularity and the onset of affective episodes in bipolar spectrum individuals. Bipolar Disord. 2008;10:520–529. doi: 10.1111/j.1399-5618.2008.00583.x. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
39. Frank E., Kupfer D.J., Thase M.E., Mallinger A.G., Swartz H.A., Fagiolini A.M., Grochocinski V., Houck P., Scott J., Thompson W., et al. Two-Year Outcomes for Interpersonal and Social Rhythm Therapy in Individuals with Bipolar I Disorder. Arch. Gen. Psychiatry. 2005;62:996–1004. doi: 10.1001/archpsyc.62.9.996. [PubMed] [CrossRef] [Google Scholar]
Two-Year Outcomes for Interpersonal and Social Rhythm Therapy in Individuals with Bipolar I Disorder. Arch. Gen. Psychiatry. 2005;62:996–1004. doi: 10.1001/archpsyc.62.9.996. [PubMed] [CrossRef] [Google Scholar]
40. Soreca I. Circadian rhythms and sleep in bipolar disorder: Implications for pathophysiology and treatment. Curr. Opin. Psychiatry. 2014;27:467–471. doi: 10.1097/YCO.0000000000000108. [PubMed] [CrossRef] [Google Scholar]
41. Gold A.K., Sylvia L.G. The role of sleep in bipolar disorder. Nat. Sci. Sleep. 2016;8:207–214. doi: 10.2147/NSS.S85754. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
42. Pagani L., St. Clair P.A., Teshiba T.M., Service S.K., Fears S.C., Araya C., Araya X., Bejarano J., Ramirez M., Castrillón G., et al. Genetic contributions to circadian activity rhythm and sleep pattern phenotypes in pedigrees segregating for severe bipolar disorder. Proc. Natl. Acad. Sci. USA. 2016;113:E754–E761. doi: 10.1073/pnas.1513525113. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
43. Roybal K., Theobold D., Graham A., DiNieri J.A., Russo S.J., Krishnan V., Chakravarty S., Peevey J., Oehrlein N., Birnbaum S. Mania-like behavior induced by disruption of CLOCK. Proc. Natl. Acad. Sci. USA. 2007;104:6406–6411. doi: 10.1073/pnas.0609625104. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Roybal K., Theobold D., Graham A., DiNieri J.A., Russo S.J., Krishnan V., Chakravarty S., Peevey J., Oehrlein N., Birnbaum S. Mania-like behavior induced by disruption of CLOCK. Proc. Natl. Acad. Sci. USA. 2007;104:6406–6411. doi: 10.1073/pnas.0609625104. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
44. Rizzo L.B., Costa L.G., Mansur R.B., Swardfager W., Belangero S.I., Grassi-Oliveira R., McIntyre R.S., Bauer M.E., Brietzke E. The theory of bipolar disorder as an illness of accelerated aging: Implications for clinical care and research. Neurosci. Biobehav. Rev. 2014;42:157–169. doi: 10.1016/j.neubiorev.2014.02.004. [PubMed] [CrossRef] [Google Scholar]
45. Fries G.R., Zamzow M.J., Andrews T., Pink O., Scaini G., Quevedo J. Accelerated aging in bipolar disorder: A comprehensive review of molecular findings and their clinical implications. Neurosci. Biobehav. Rev. 2020;112:107–116. doi: 10.1016/j.neubiorev.2020.01.035. [PubMed] [CrossRef] [Google Scholar]
46. Timothy J.W.S., Klas N., Sanghani H.R., Al-Mansouri T., Hughes A.T.L., Kirshenbaum G.S., Brienza V., Belle M.D.C., Ralph M.R., Clapcote S.J., et al. Circadian Disruptions in the Myshkin Mouse Model of Mania Are Independent of Deficits in Suprachiasmatic Molecular Clock Function. Biol. Psychiatry. 2018;84:827–837. doi: 10.1016/j.biopsych.2017.04.018. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Timothy J.W.S., Klas N., Sanghani H.R., Al-Mansouri T., Hughes A.T.L., Kirshenbaum G.S., Brienza V., Belle M.D.C., Ralph M.R., Clapcote S.J., et al. Circadian Disruptions in the Myshkin Mouse Model of Mania Are Independent of Deficits in Suprachiasmatic Molecular Clock Function. Biol. Psychiatry. 2018;84:827–837. doi: 10.1016/j.biopsych.2017.04.018. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
47. Parekh P.K., Becker-Krail D., Sundaravelu P., Ishigaki S., Okado H., Sobue G., Huang Y., McClung C.A. Altered GluA1 (Gria1) Function and Accumbal Synaptic Plasticity in the ClockΔ19 Model of Bipolar Mania. Biol. Psychiatry. 2018;84:817–826. doi: 10.1016/j.biopsych.2017.06.022. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
48. Albrecht U. Molecular Connections Between Circadian Clocks and Mood-related Behaviors. J. Mol. Biol. 2020;432:3714–3721. doi: 10.1016/j.jmb.2019.11.021. [PubMed] [CrossRef] [Google Scholar]
49. Verma V. Classic studies on the interaction of cocaine and the dopamine transporter. Clin. Psychopharmacol. Neurosci. 2015;13:227. doi: 10.9758/cpn.2015.13.3.227. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Clin. Psychopharmacol. Neurosci. 2015;13:227. doi: 10.9758/cpn.2015.13.3.227. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
50. Kokkinou M., Ashok A.H., Howes O.D. The effects of ketamine on dopaminergic function: Meta-analysis and review of the implications for neuropsychiatric disorders. Mol. Psychiatry. 2018;23:59–69. doi: 10.1038/mp.2017.190. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
51. Willner P., Hale A.S., Argyropoulos S. Dopaminergic mechanism of antidepressant action in depressed patients. J. Affect. Dis. 2005;86:37–45. doi: 10.1016/j.jad.2004.12.010. [PubMed] [CrossRef] [Google Scholar]
52. Engert V., Pruessner J.C. Dopaminergic and noradrenergic contributions to functionality in ADHD: The role of methylphenidate. Curr. Neuropharm. 2008;6:322–328. doi: 10.2174/157015908787386069. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
53. Roberts R.J., Repass R., El-Mallakh R.S. Effect of dopamine on intracellular sodium: A common pathway for pharmacological mechanism of action in bipolar illness.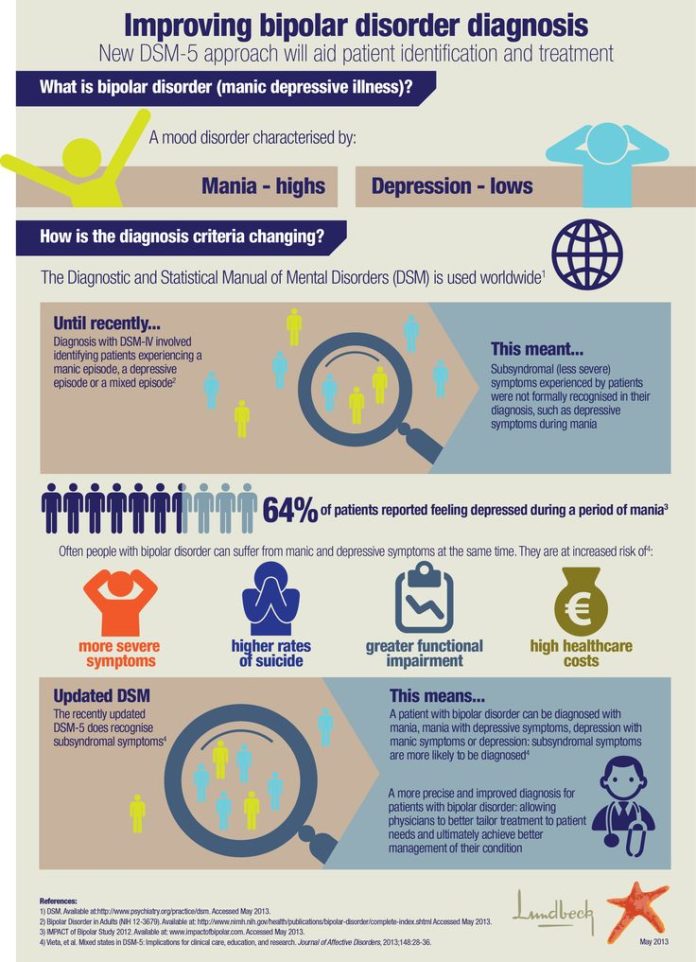 World J. Biol. Psychiatry. 2010;11:181–187. doi: 10.3109/15622970902718774. [PubMed] [CrossRef] [Google Scholar]
World J. Biol. Psychiatry. 2010;11:181–187. doi: 10.3109/15622970902718774. [PubMed] [CrossRef] [Google Scholar]
54. Lau P., Hawes D.J., Hunt C., Frankland A., Roberts G., Mitchell P.B. Prevalence of psychopathology in bipolar high-risk offspring and siblings: A meta-analysis. Eur. Child Adolesent Psychiatry. 2018;27:823–837. doi: 10.1007/s00787-017-1050-7. [PubMed] [CrossRef] [Google Scholar]
55. Wu M.-J., Mwangi B., Passos I.C., Bauer I.E., Cao B., Frazier T.W., Zunta-Soares G.B., Soares J.C. Prediction of vulnerability to bipolar disorder using multivariate neurocognitive patterns: A pilot study. Int. J. Bipolar Disord. 2017;5:1–7. doi: 10.1186/s40345-017-0101-9. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
56. Morin L.P. Serotonin and the regulation of mammalian circadian rhythmicity. Ann. Med. 1999;31:12–33. doi: 10.3109/07853899909019259. [PubMed] [CrossRef] [Google Scholar]
57. Daut R.A., Fonken L.K. Circadian regulation of depression: A role for serotonin. Front. Neuroendocrinol. 2019;54:100746. doi: 10.1016/j.yfrne.2019.04.003. [PubMed] [CrossRef] [Google Scholar]
Front. Neuroendocrinol. 2019;54:100746. doi: 10.1016/j.yfrne.2019.04.003. [PubMed] [CrossRef] [Google Scholar]
58. Fang L., Yu Q., Yin F., Yu J., Zhang Y., Zhang Y., Zhu D., Qin X. Combined cortisol and melatonin measurements with detailed parameter analysis can assess the circadian rhythms in bipolar disorder patients. Brain Behav. 2021;11:e02186. doi: 10.1002/brb3.2186. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
59. Etain B., Dumaine A., Bellivier F., Pagan C., Francelle L., Goubran-Botros H., Moreno S., Deshommes J., Moustafa K., Le Dudal K., et al. Genetic and functional abnormalities of the melatonin biosynthesis pathway in patients with bipolar disorder. Hum. Mol. Genet. 2012;21:4030–4037. doi: 10.1093/hmg/dds227. [PubMed] [CrossRef] [Google Scholar]
60. Alexis Geoffroy P., Etain B., Micoulaud Franchi J.-A., Bellivier F., Ritter P. Melatonin and melatonin agonists as adjunctive treatments in bipolar disorders. Curr. Pharm. Des. 2015;21:3352–3358. doi: 10. 2174/1381612821666150619093448. [PubMed] [CrossRef] [Google Scholar]
2174/1381612821666150619093448. [PubMed] [CrossRef] [Google Scholar]
61. Fornaro M., McCarthy M.J., De Berardis D., De Pasquale C., Tabaton M., Martino M., Colicchio S., Cattaneo C.I., D’Angelo E., Fornaro P. Adjunctive agomelatine therapy in the treatment of acute bipolar II depression: A preliminary open label study. Neuropsychiatry Dis. Treat. 2013;9:243–251. doi: 10.2147/NDT.S41557. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
62. Drews H.J., Scott J., Langsrud K., Vethe D., Kallestad H. Chronobiologically informed inpatient milieu in psychiatric institutions. Lancet Psychiatry. 2020;7:1013–1014. doi: 10.1016/S2215-0366(20)30459-4. [PubMed] [CrossRef] [Google Scholar]
63. Scott J., Langsrud K., Goulding I.R., Kallestad H. Let there be blue-depleted light: In-patient dark therapy, circadian rhythms and length of stay. BJPsych Adv. 2021;27:73–84. doi: 10.1192/bja.2020.47. [CrossRef] [Google Scholar]
64. Vethe D., Scott J., Engstrøm M., Salvesen Ø., Sand T.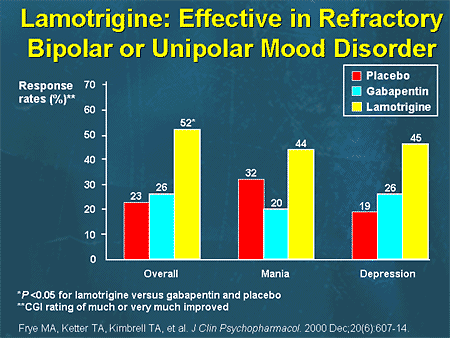 , Olsen A., Morken G., Heglum H.S., Kjørstad K., Faaland P.M. The evening light environment in hospitals can be designed to produce less disruptive effects on the circadian system and improve sleep. Sleep. 2021;44:zsaa194. doi: 10.1093/sleep/zsaa194. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
, Olsen A., Morken G., Heglum H.S., Kjørstad K., Faaland P.M. The evening light environment in hospitals can be designed to produce less disruptive effects on the circadian system and improve sleep. Sleep. 2021;44:zsaa194. doi: 10.1093/sleep/zsaa194. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
65. Cegla-Schvartzman F.B., Ovejero S., López-Castroman J., Baca-García E. Diagnostic Stability in Bipolar Disorder: A Narrative Review. Harv. Rev. Psychiatry. 2019;27:3–14. doi: 10.1097/HRP.0000000000000187. [PubMed] [CrossRef] [Google Scholar]
66. Malhi G.S., Outhred T., Irwin L. Bipolar II Disorder Is a Myth. Can. J. Psychiatry. 2019;64:531–536. doi: 10.1177/0706743719847341. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
67. Bolton S., Warner J., Harriss E., Geddes J., Saunders K.E.A. Bipolar disorder: Trimodal age-at-onset distribution. Bipolar Disord. 2021;23:341–356. doi: 10.1111/bdi.13016. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
68. Herane-Vives A., Arnone D., de Angel V., Papadopoulos A., Wise T., Alameda L., Chua K.-C., Young A.H., Cleare A.J. Cortisol levels in unmedicated patients with unipolar and bipolar major depression using hair and saliva specimens. Int. J. Bipolar Disord. 2020;8:15. doi: 10.1186/s40345-020-0180-x. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Herane-Vives A., Arnone D., de Angel V., Papadopoulos A., Wise T., Alameda L., Chua K.-C., Young A.H., Cleare A.J. Cortisol levels in unmedicated patients with unipolar and bipolar major depression using hair and saliva specimens. Int. J. Bipolar Disord. 2020;8:15. doi: 10.1186/s40345-020-0180-x. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
69. Braun R., Kath W.L., Iwanaszko M., Kula-Eversole E., Abbott S.M., Reid K.J., Zee P.C., Allada R. Universal method for robust detection of circadian state from gene expression. Proc. Natl. Acad. Sci. USA. 2018;115:E9247–E9256. doi: 10.1073/pnas.1800314115. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
70. Anafi R.C., Francey L.J., Hogenesch J.B., Kim J. CYCLOPS reveals human transcriptional rhythms in health and disease. Proc. Natl. Acad. Sci. USA. 2017;114:5312–5317. doi: 10.1073/pnas.1619320114. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
71. Alzahrani H.S., Khuu S.K., Roy M. Modelling the effect of commercially available blue-blocking lenses on visual and non-visual functions.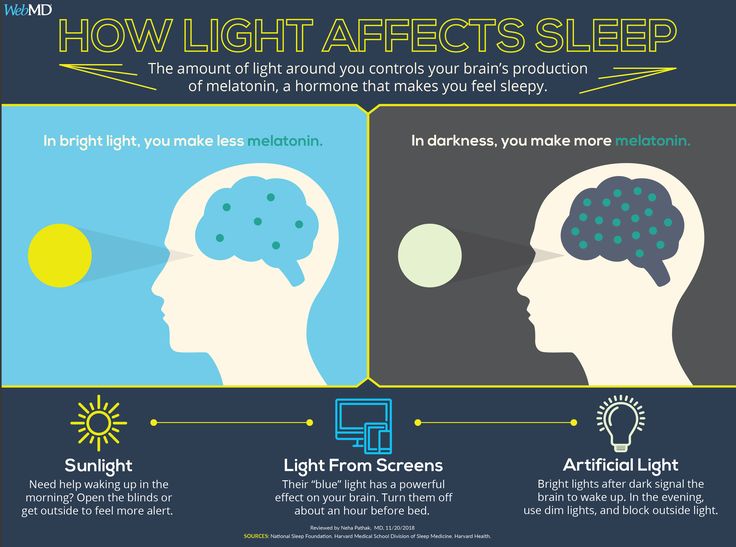 Clin. Exp. Optom. 2020;103:339–346. doi: 10.1111/cxo.12959. [PubMed] [CrossRef] [Google Scholar]
Clin. Exp. Optom. 2020;103:339–346. doi: 10.1111/cxo.12959. [PubMed] [CrossRef] [Google Scholar]
72. Zeitzer J.M., Dijk D.-J., Kronauer R.E., Brown E.N., Czeisler C.A. Sensitivity of the human circadian pacemaker to nocturnal light: Melatonin phase resetting and suppression. J. Physiol. 2000;526:695–702. doi: 10.1111/j.1469-7793.2000.00695.x. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
73. Comparetto R., Farini A. Mitigating retinal damage and circadian rhythm modification by blue-blocking spectacles lenses: Evaluation parameters. Eur. Phys. J. Plus. 2019;134:494. doi: 10.1140/epjp/i2019-12848-x. [CrossRef] [Google Scholar]
Light therapy against depression - Bipolar.su
Ordinary sunlight or a special lamp can improve depression. This is called light therapy. A member of our community has prepared a review of publications on what light therapy is and how it helps with bipolar disorder and seasonal affective disorder.
Personal experience prompted me to write this article.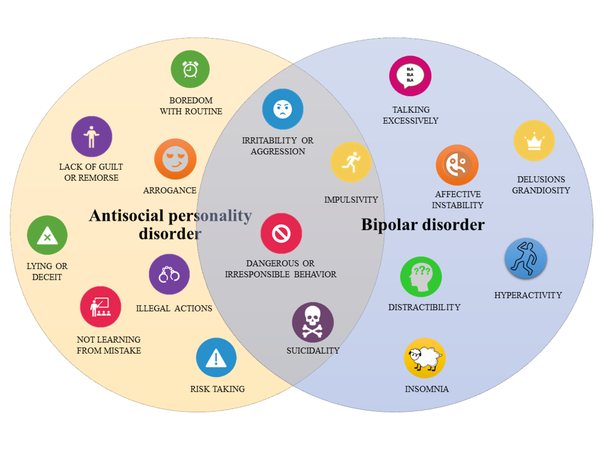 For as long as I can remember, summer has been the best time of my life. As a child, as a student, this could be attributed to the holidays, which everyone enjoys without exception. Then somehow it became more difficult to tie to the holidays - the holidays were no longer with me, but the habit of rejoicing remained. In summer, everything is easy, everything is simple, everything is fast, there is no time to even sleep, and you don’t feel like it. Then comes the golden autumn, then not very golden, and then not golden at all, but slushy, dreary and dark. Everything around becomes dull and gray, meaningless and useless, and you feel that your life is meaningless, useless, so the best thing is to go to the kitchen, have a big snack on buns and go to bed. Preferably until spring, so as not to hear those idiots who offer you to cheer up. nine0003
For as long as I can remember, summer has been the best time of my life. As a child, as a student, this could be attributed to the holidays, which everyone enjoys without exception. Then somehow it became more difficult to tie to the holidays - the holidays were no longer with me, but the habit of rejoicing remained. In summer, everything is easy, everything is simple, everything is fast, there is no time to even sleep, and you don’t feel like it. Then comes the golden autumn, then not very golden, and then not golden at all, but slushy, dreary and dark. Everything around becomes dull and gray, meaningless and useless, and you feel that your life is meaningless, useless, so the best thing is to go to the kitchen, have a big snack on buns and go to bed. Preferably until spring, so as not to hear those idiots who offer you to cheer up. nine0003
It is impossible to force yourself to get up in the morning and start some kind of meaningful activity, everything and everyone around you infuriates. The only good news is the opportunity to go to bed early and try to fall asleep. Then once - and a snowball falls, then another, then everything turns white, and somehow life gets a little better. But soon the snow turns gray, fades, and there, and again, everything acquires a yellow-blue hue, like a boiled yolk. And so on until the summer. And then the cycle repeats. And only many years later I learned that seasonal affective disorder combined with bipolar disorder is not only what I saw in others, but also what I myself have. nine0003
The only good news is the opportunity to go to bed early and try to fall asleep. Then once - and a snowball falls, then another, then everything turns white, and somehow life gets a little better. But soon the snow turns gray, fades, and there, and again, everything acquires a yellow-blue hue, like a boiled yolk. And so on until the summer. And then the cycle repeats. And only many years later I learned that seasonal affective disorder combined with bipolar disorder is not only what I saw in others, but also what I myself have. nine0003
If you recognize yourself in winter, take my word for it - this is not the norm. It's time for you to go to the doctor. You very likely have seasonal affective disorder, as detailed by Dr. Rosenthal in 1984(1). And if in the summer everything is just as wonderful for you as it is for me, then go all the more so, bipolar affective disorder combined with seasonal is no better.
The fact that the length of the daylight hours affects our activity has been known since ancient times(2). The Chinese physician Wong Tei wrote 4700 years ago that a person's mood is connected with the season. Hippocrates associated melancholy with winter and mania with summer, and many other physicians, ancient and not so, drew attention to the connection of mood with the seasons. nine0003
The Chinese physician Wong Tei wrote 4700 years ago that a person's mood is connected with the season. Hippocrates associated melancholy with winter and mania with summer, and many other physicians, ancient and not so, drew attention to the connection of mood with the seasons. nine0003
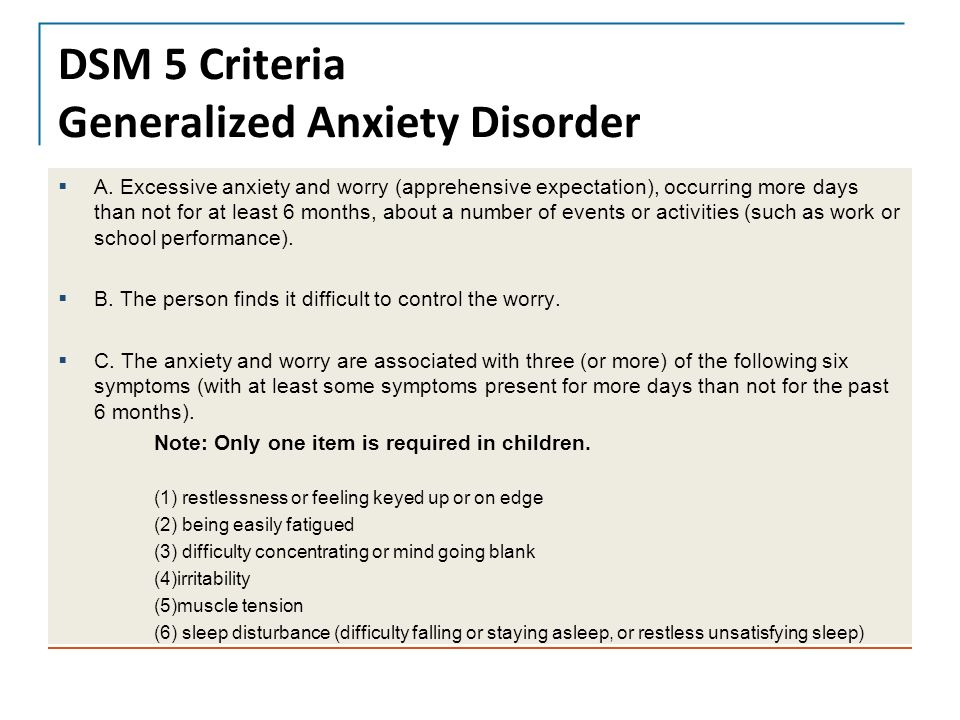
There are many hypotheses for SAD (Seasonal Affective Disorder), but the exact cause is unknown. It is believed that the less sun a person sees, the worse a part of the brain called the hypothalamus works for him. It is responsible for many brain functions, including our emotions. Melatonin is overproduced, causing drowsiness, and serotonin, on the contrary, is produced in smaller amounts, which causes a decrease in mood, and these are just some of the possible mechanisms for the development of SAD. The main reason is the lack of sunlight. nine0003
By the way, not only people suffer from SAD. If animals leading a predominantly diurnal lifestyle (humans, for example, or grass rats) are deprived of bright light for a long time, they will somehow develop a depressive state (3). In grass mice, which were placed in an environment with a dim, “winter” light, memory, learning ability worsened, signs of anxiety and depression appeared. Even mice with a lack of sunlight become depressed. What can we say about a person ... At the same time, in mice, no connection was found with circadian rhythm disorders, on which seasonal depression depends, in this study. nine0003
In grass mice, which were placed in an environment with a dim, “winter” light, memory, learning ability worsened, signs of anxiety and depression appeared. Even mice with a lack of sunlight become depressed. What can we say about a person ... At the same time, in mice, no connection was found with circadian rhythm disorders, on which seasonal depression depends, in this study. nine0003
According to one theory, depression can develop when the circadian rhythm (that is, the change of day and night) and periods of sleep and wakefulness do not match. In other words, a person is forced to go to bed and wake up not in accordance with his biological rhythm, but at an imposed time (not a word about an alarm clock!). This idea is based on the theory of light therapy, which aims to restore the circadian rhythm and thus bring a person out of depression. But the level of illumination, which is necessary for this, turned out to be much higher than in natural conditions. So it's not just about circadian rhythms. But whatever it is, light therapy works well for SAD (4). nine0003
But whatever it is, light therapy works well for SAD (4). nine0003
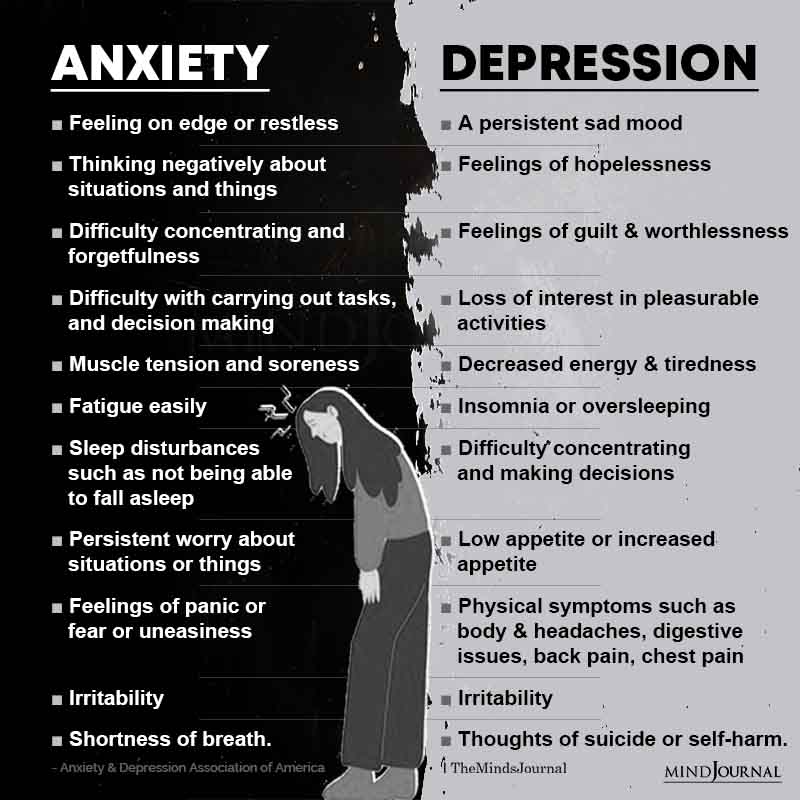
But depression is not limited to SAD. Depression may not be related to the length of daylight hours, and then the question remains: will additional light help such people? And if a person has not just SAD, but bipolar affective disorder?
If he has periods of autumn depression followed by periods of hypo- or manic state in summer? Will he then switch from depression to mania, that is, will the light harm him? In search of answers to these questions, scientists have come to the conclusion that there is no damage due to bright light, but there is a benefit for people with depression. Several studies have recently been published that studied the effect of bright light on depression in bipolar disorder. nine0003
A study was conducted at Chicago Northwestern University where light was used not in the morning but in the afternoon (5). The original plan was to compare morning bright white light with soft red light, but three of the first four patients treated with bright light developed hypomania. The researchers decided that light therapy in the morning might be to blame, and moved the treatment time to the afternoon hours.
The researchers decided that light therapy in the morning might be to blame, and moved the treatment time to the afternoon hours.
They assumed that it would be ineffective, because a person sees the light during the day, unless he lives underground or in the conditions of the polar night. nine0003
It turned out that a bright white lamp significantly alleviated depression in 68% of patients, and a red one only in 22%, which was consistent with the results of other studies with morning light therapy. It is noteworthy that no one developed hypomania during treatment.
Very similar results were obtained in Turkey (6) and China (7), where it was confirmed that bright light in patients with depression increased the effect of antidepressants in both unipolar depression and bipolar disorder, including in patients without seasonality (8) The table below compares the illuminance with different light sources
Although people have known since ancient times that sunlight affects mood, this type of treatment is not fully understood. In Holland, a group of scientists decided to find out whether the effect of light on mood depends on the spectrum of this light (10).
A cloudy day is bad not only because it has little light as such, but also because there is practically no ultraviolet in the radiation. Of course, it is not good for the eyes at all. But was it worth testing the hypothesis of whether dim blue light of just 100 lux is useful for people with depression? nine0003
It turned out that yes, in the study it turned out to be as effective as bright. Unfortunately, there are no definitive recommendations on how and when to properly use a bright lamp. Some people, including psychiatrists and psychotherapists, still have questions about the safety of bright light treatment for the eyes.
Unfortunately, there are no definitive recommendations on how and when to properly use a bright lamp. Some people, including psychiatrists and psychotherapists, still have questions about the safety of bright light treatment for the eyes.
A team from the Free University of Amsterdam reviewed 43 scientific articles reporting various adverse events in patients treated with light therapy for various reasons, including depression and bipolar disorder (11). nine0003
In theory, light therapy can be dangerous to the eyes because it can damage the retina with HEV radiation (HEV radiation, or blue light, high-energy visible light) - this is high-frequency high-energy light in the visible spectrum in the range from 400 to 500 nm. No other parts of the eye (lens, cornea, etc.) are affected. During light therapy, some patients (up to 45%) complained of discomfort and visual disturbances, regardless of the dose of light therapy.
However, in part of the studies, there were more complaints in patients treated with dim red light than in those treated with bright white light.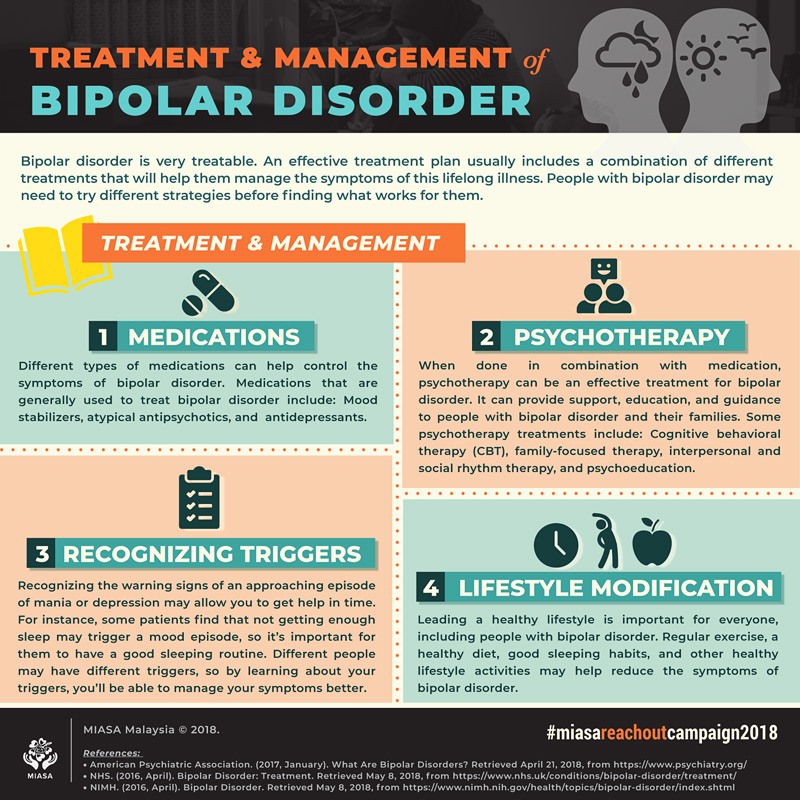 In other experiments, on the contrary, bright light was tolerated worse. In some studies, bright light at 10,000 lux did not cause any discomfort, and in others, people complained of discomfort at an intensity of only 400 lux. nine0003
In other experiments, on the contrary, bright light was tolerated worse. In some studies, bright light at 10,000 lux did not cause any discomfort, and in others, people complained of discomfort at an intensity of only 400 lux. nine0003
Researchers evaluated the effect of light therapy on the eye's light sensitivity and found that exposure to brighter white light temporarily reduced sensitivity to red light, while exposure to less intense red light increased red light sensitivity.
Both are normal. There are practically no complications from light therapy in people who do not have eye diseases. An exception is complications when taking photosensitizing drugs (photosensitization is an increase in the sensitivity of the body, more often the skin and mucous membranes, to the action of light radiation when taking certain drugs, such as antibiotics). nine0003
The only reliable case of damage to the retina during light therapy was recorded in a patient who took the antidepressant clomipramine (anafranil), among the side effects of which is photosensitivity.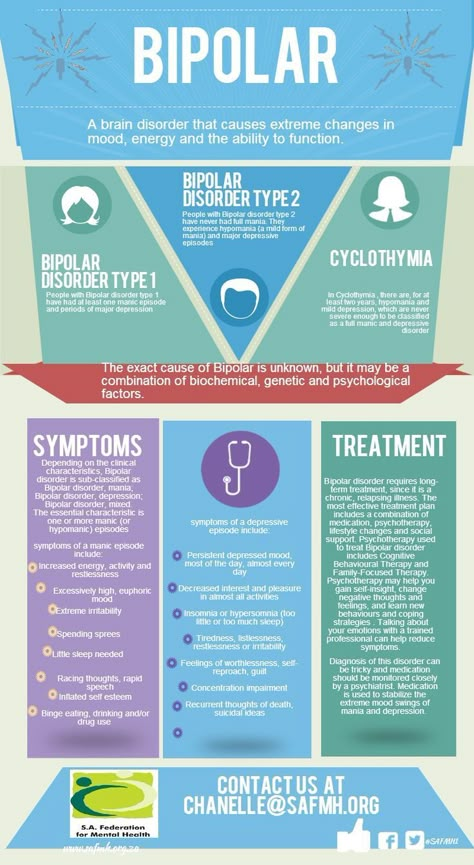
It is safe to say that bright light treatment is safe for the eyes. Dr. Carl Aiken, director of the Center for Mood Disorders at Wake Forest University (USA), recommends the use of large lamps with a brightness of at least 2,000 lux with a UV filter to protect the eyes 12. The session is best done during the day, from 12 to 14 hours. It is better to sit half a meter from the lamp, but not directly opposite it, but obliquely, at an angle of 45 degrees. At the same time, you can do the usual things (eat, work, watch TV). The lamp should be changed every three years. nine0003
In any case, you should only start light therapy after consulting your doctor. Although sunlight is beneficial for health, light therapy for bipolar disorder is not fully understood and should be approached with caution. 1. Rosenthal, N. E. et al. Seasonal affective disorder. A description of the syndrome and preliminary findings with light therapy. nine0129 Arch. Gen. Psychiatry 41, 72–80 (1984).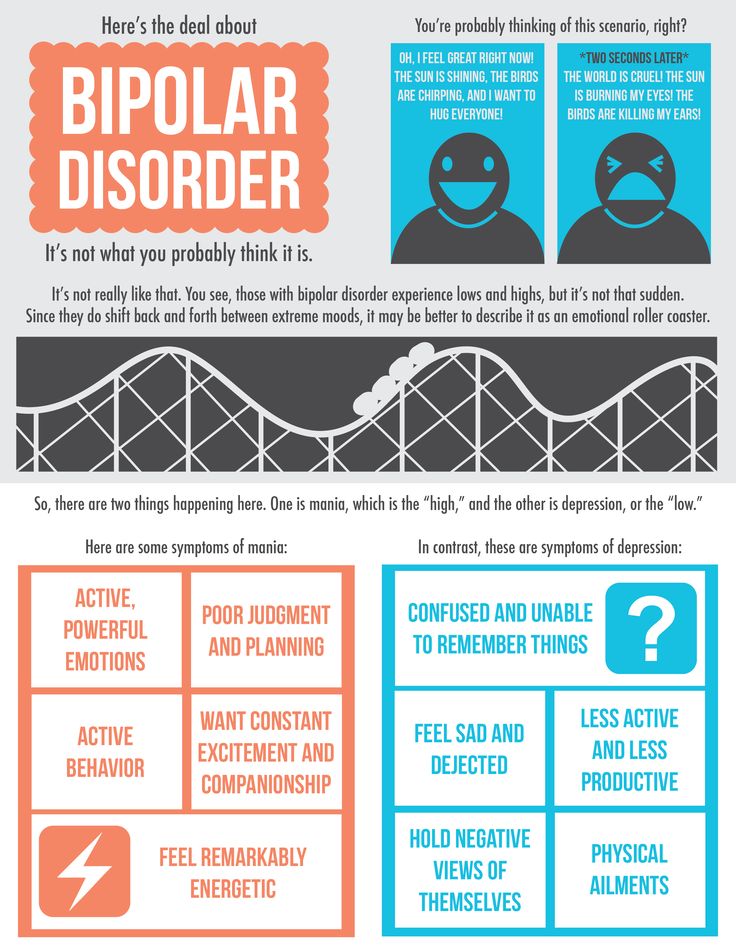
2. Geoffroy, P. A., Schroder, C. M. & Bourgin, P. Light treatment in depression: An antique treatment with new insights. Sleep Med. Rev. 40, 218–219 (2018).
3. Yan, L., Lonstein, J. S. & Nunez, A. A. Light as a modulator of emotion and cognition: Lessons learned from studying a diurnal rodent. Horm. behavior. (2018). doi:10.1016/j.yhbeh.2018.09.003
4. Nussbaumer, B. et al. nine0130 Light therapy for preventing seasonal affective disorder. Cochrane Database Syst. Rev. (2015). doi:10.1002/14651858.CD011269.pub2
5. Sit, D.K. et al. Adjunctive Bright Light Therapy for Bipolar Depression: A Randomized Double-Blind Placebo-Controlled Trial. Am. J. Psychiatry 175, 131–139 (2018).
6. Yorguner Kupeli, N., Bulut, N. S., Carkaxhiu Bulut, G., Kurt, E. & Kora, K. Efficacy of bright light therapy in bipolar depression. nine0129 Psychiatry Res. 260, 432–438 (2018).
7. Zhou, T. et al. Clinical efficacy, onset time and safety of bright light therapy in acute bipolar depression as an adjunctive therapy: A randomized controlled trial.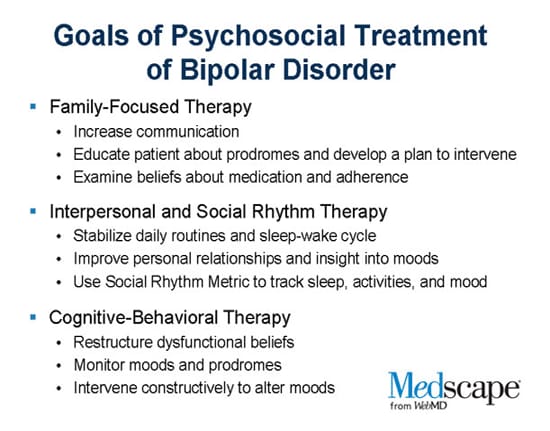 J. Affect. Discord. 227, 90–96 (2018).
J. Affect. Discord. 227, 90–96 (2018).
8. Penders, T. M. et al. Bright Light Therapy as Augmentation of Pharmacotherapy for Treatment of Depression: A Systematic Review and Meta-Analysis. Prim. Care Companion CNS Disord. nine0130 18, (2016).
9. Leahy, L. G. Overcoming Seasonal Affective Disorder. J. Psychosoc. Nurs. Ment. Health Service 55, 10–14 (2017).
10. Meesters, Y., Duijzer, W. B. & Hommes, V. The effects of low-intensity narrow-band blue-light treatment compared to bright white-light treatment in seasonal affective disorder. J. Affect. Discord. 232, 48–51 (2018).
11. Brouwer, A. et al. Light therapy: is it safe for the eyes? Acta Psychiatr. Scand. 136, 534–548 (2017).
12. Aiken, C. How to Use Light Therapy in Bipolar Disorder | Psychiatric Times. Available at: http://www.psychiatrictimes.com/. (Accessed: 17th December 2018)
Light therapy
Light therapy is treatment with artificial light sources that mimic the effects of sunlight on the human body. Light treatment includes two directions. The first is based on the action of ultraviolet and infrared rays on the skin, the second on the action of the visible part of the spectrum on the eyes. In this article you will learn:
Light treatment includes two directions. The first is based on the action of ultraviolet and infrared rays on the skin, the second on the action of the visible part of the spectrum on the eyes. In this article you will learn:
- what is chronobiology and circadian rhythms;
- how light affects our "biological clock" and what happens if it becomes out of sync with actual time;
- development history of light therapy;
- when visible light treatment is indicated and how it is done;
- are there any contraindications and side effects;
- what types of lamps are used for light therapy.
Light therapy mimics natural sunlight
What is chronobiology and what is the importance of light in it
Chronobiology is a science that studies daily cyclic physiological and biochemical changes in the human body. These changes, called circadian rhythms, are controlled by our "biological clock". Illumination plays a crucial role in synchronizing the work of the biological clock with the time of day.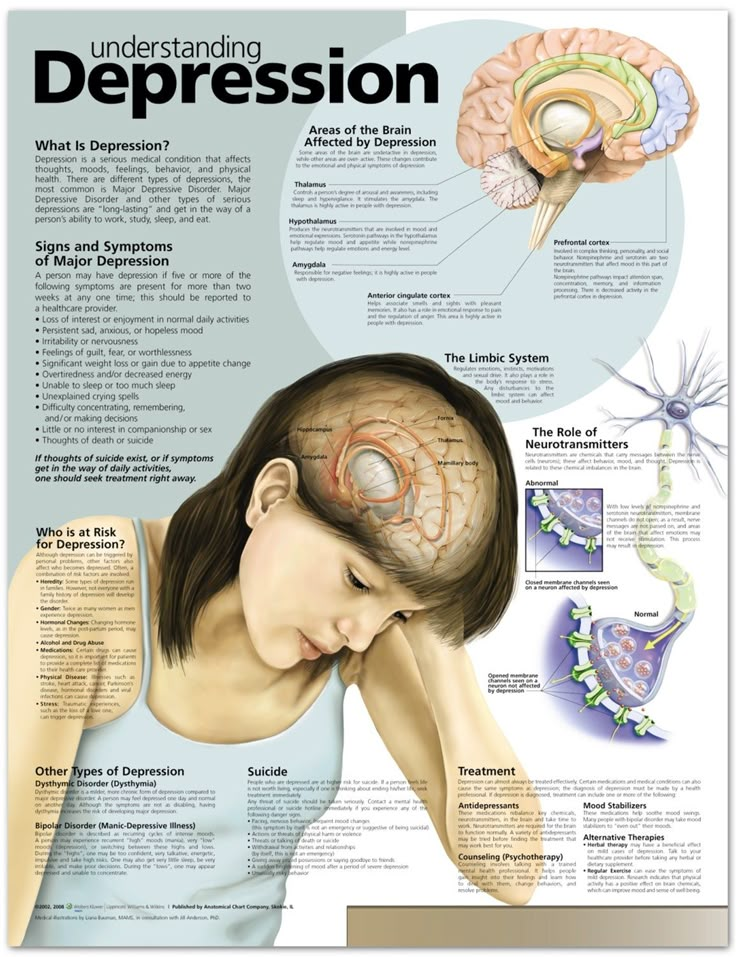
During the daytime, special receptors in our eyes - pigment ganglion cells - react to light and send signals to the "control center" of the biological clock in the brain. From there, organs and systems are "instructed" to work in wakefulness, which is accompanied by the production of cortisol, serotonin, adrenaline - hormones responsible for vivacity, activity, quick reaction, clear thinking, good mood, intellectual abilities, increased muscle tone and blood vessels. nine0003
At night, the biological clock does not receive signals from the eye receptors and "commands" the body to rest. At the same time, the production of the “sleep hormone” melatonin increases, the tone of muscles and blood vessels, body temperature, and heart rate decrease.
Unfortunately, our way of life often leads to a malfunction of the biological clock. We are confusing and prevent us from falling asleep with the lights on, the TV or computer turned on, the illumination outside the window, circadian rhythms are disturbed due to work at night, time zone changes and a number of other factors. nine0003
nine0003
When our internal clock is out of sync with the actual time, there are problems with sleeping, waking up and feeling well. We do not sleep well at night, it is difficult to wake up in the morning, we become irritable, lethargic, drowsy, our reaction and memory, working capacity decrease. Long-term imbalance of the "biological clock" leads to hypertension, myocardial ischemia and cardiac arrhythmias, the development of diabetes, the "start" of oncological diseases.
The work of the biological clock is synchronized with the time of day nine0003
In the autumn-winter period, our circadian rhythms are also affected by a chronic lack of sunlight - during the daytime, the production of cortisol and serotonin decreases, processes occurring during wakefulness are inhibited, and seasonal depression can develop.
Light treatment restores normal circadian rhythms, resulting in improved psychological and physical health.
History of the method
At the beginning of the 20th century, the Dane Niels Reiberg Finsen included blue light in the treatment of immunocompromised patients and proved that it stimulates the immune defense and allows you to successfully fight diseases such as tuberculosis, etc.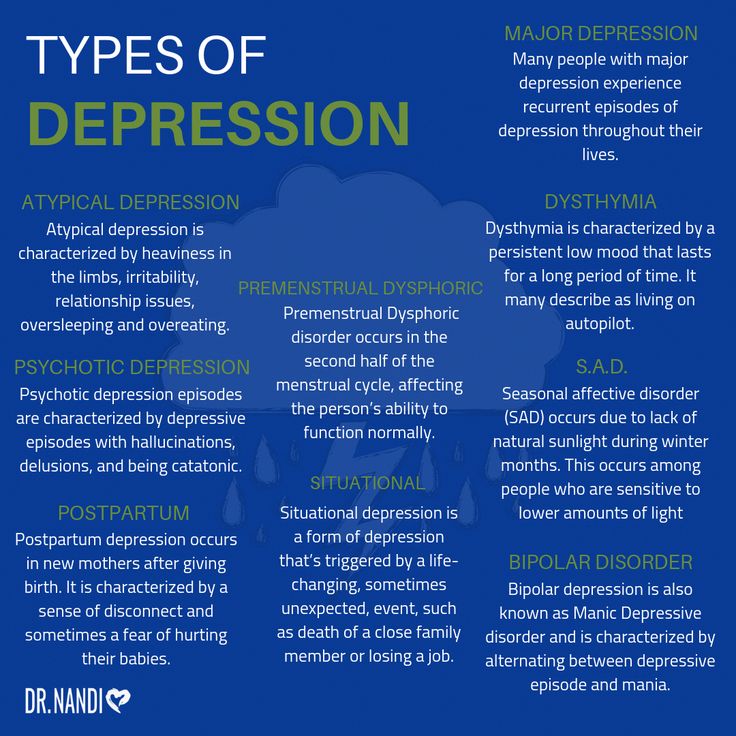
Almost 80 years later, Norman Rosenthal, a South African physician living in Washington, drew attention to the connection between a lack of sunlight and seasonal mood and well-being disorders, the so-called autumn blues. With the advent of autumn, he felt depressed and tired. Together with his colleagues at the National Institute of Mental Health, Rosenthal conducted a series of studies. Their results showed that autumn blues can be treated with exposure to artificial light, similar in spectrum to sunlight. Thus light therapy was born. nine0003
After the discovery in 2002 of pigment cells in the retina of the eye and evidence of the positive effect of light therapy sessions on the imbalance of the biological clock, the scope of therapeutic light in the visible range has been significantly expanded.
In 2005, light therapy was officially recognized by the American Psychiatric Association as a first-line treatment for seasonal depression, also known as seasonal affective disorder.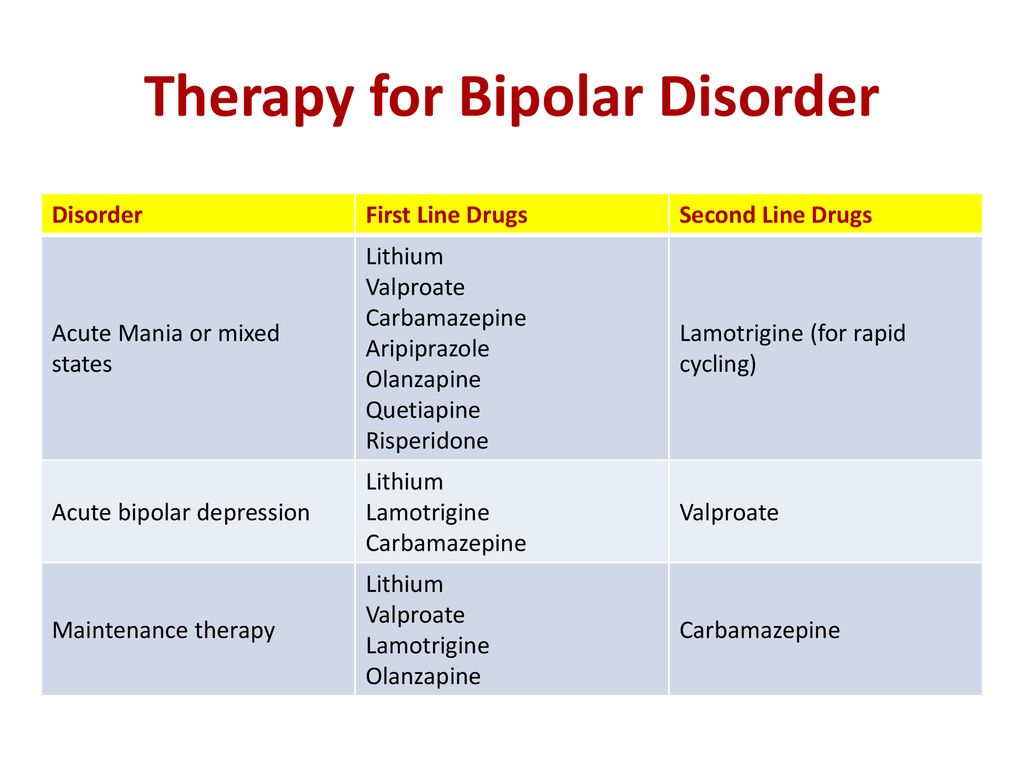
Since then, new studies have been reported each year showing the positive effects of light on Parkinson's and Alzheimer's symptoms, the effects of brain injury, quitting smoking or alcohol, and more. nine0003
It is safe to assume that light therapy will eventually find its place in the arsenal of every doctor.
When is light therapy indicated and how does it work?
Treatment with this method is based on the therapeutic properties of visible light waves and is indicated in cases where:
- people live in a region where sunlight is not enough in late autumn and winter;
- work schedule includes night shifts or work is carried out on a rotational basis; nine0192
- there is a sharp change in the time zone (from 3 or more time zones).
Light therapy is also used for sleep disorders of various origins, postpartum depression, chronic fatigue.
Light therapy helps to get rid of chronic fatigue
Light therapy lamps are available in all sizes and designs.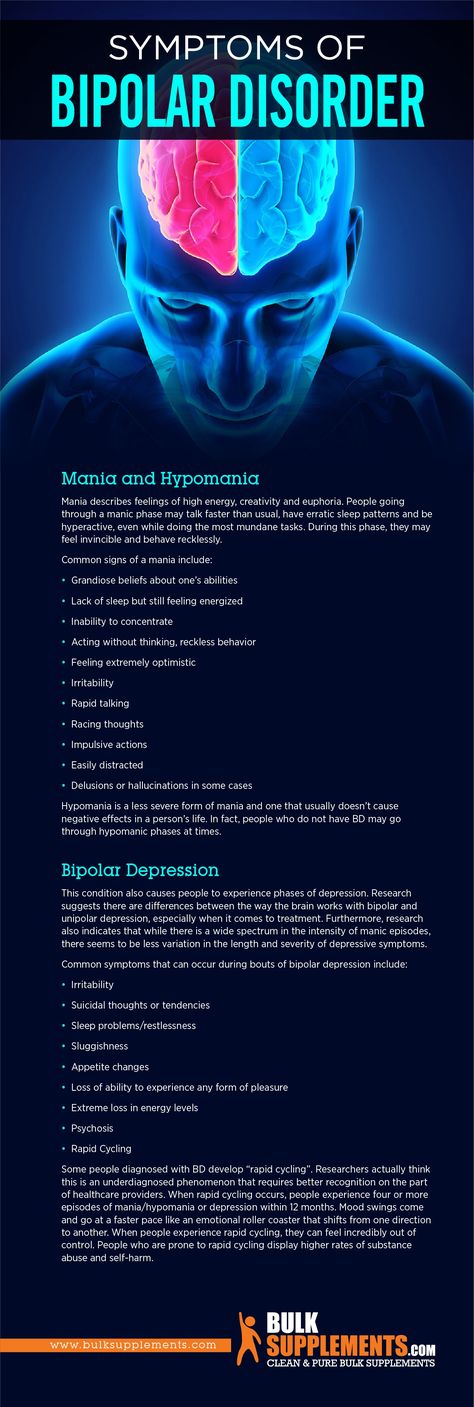 They emit light close in spectrum to the sun, but for safety reasons completely devoid of ultraviolet and infrared rays. nine0003
They emit light close in spectrum to the sun, but for safety reasons completely devoid of ultraviolet and infrared rays. nine0003
Depending on the nature of the problem and the individual characteristics of a person, a mode, spectrum, intensity, duration of sessions and a course of treatment are selected. So, for example, it takes 2-3 weeks to restore normal sleep and eliminate other manifestations of autumn depression, and you can adapt to a new time zone in 2-3 days.
Treatment regimen and its results are determined by the following main factors:
Daily routine. Conducting a session in the morning, immediately after waking up, allows you to adjust the sleep-wake cycle in unison with the time of day and recharge your batteries for the whole working day. A session in the daytime has a stimulating effect comparable to the effect of coffee - such a regimen may be a priority for teachers, doctors and other specialists working on the second shift. The evening session is carried out before night work. If a person works at night for more than 7 days in a row, he may be shown an additional session of light therapy in the middle of the shift. After the end of the night shift until going to bed, it is recommended to protect your eyes from sunlight with blue filter glasses or regular sunglasses, you need to sleep in a room with thick dark curtains. nine0003
If a person works at night for more than 7 days in a row, he may be shown an additional session of light therapy in the middle of the shift. After the end of the night shift until going to bed, it is recommended to protect your eyes from sunlight with blue filter glasses or regular sunglasses, you need to sleep in a room with thick dark curtains. nine0003
Artificial "sunshine" before the start of the night shift will charge you with vigor and energy
The spectrum of light waves and their intensity. Photoreceptors are especially sensitive to the blue part of the visible spectrum. The enrichment of white light with blue makes it possible to reduce the light intensity of the light therapy lamp to a minimum. The use of such a device with high efficiency of treatment completely eliminates the risk of damage to the eyes.
Contraindications and side effects
Light therapy is a gentle method of exposure, so the method has very few contraindications and limitations.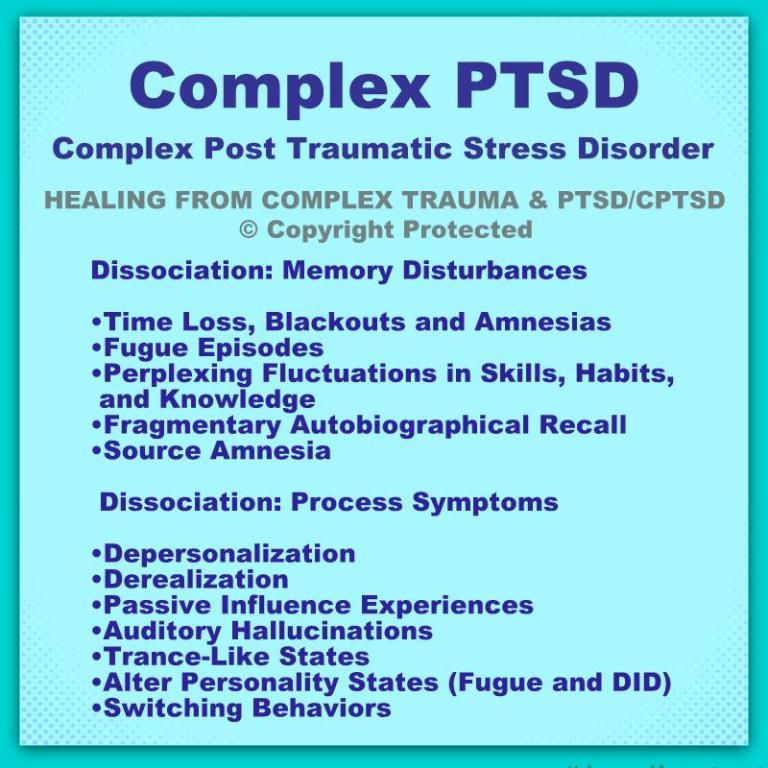 However, in certain cases it is necessary to consult a doctor.
However, in certain cases it is necessary to consult a doctor.
Discuss light treatment with an ophthalmologist if you have been diagnosed with retinal damage, diabetic retinopathy, retinitis pigmentosa, macular degeneration (age-related macular degeneration), glaucoma.
We add that none of the above ophthalmic diseases is an absolute contraindication and is only a reason for increased caution. nine0003
If you have ophthalmic diseases, do not start light treatment without first consulting your doctor.
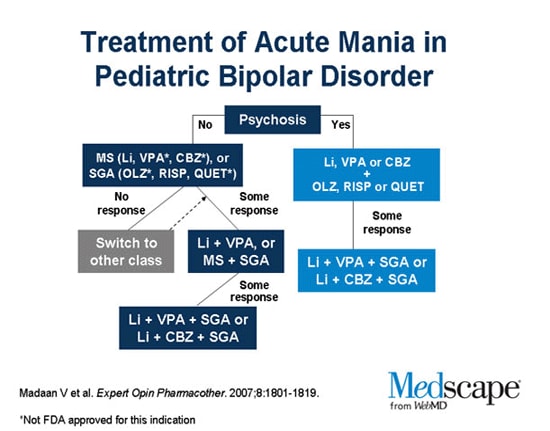
Another relative contraindication is bipolar disorder. During the manic phase, treatment with light can cause an increase in symptoms. At the same time, light therapy has a beneficial antidepressant effect during the depressive phase of the disease. Patients with bipolar disorder in the depressive phase are usually advised to have a session at noon rather than in the morning - this avoids the transition to the manic phase. Also, in such patients, light treatment is recommended to be combined with medication. nine0003
nine0003
Mild side effects sometimes occur during light therapy:
- headaches;
- eye fatigue and dry eyes;
- nausea.
Their appearance is due to the fact that our brain has to manage more light than usual. And he needs time to adapt.
Side effects are extremely rare and quickly disappear - either on their own or after adjusting the parameters. Only in rare cases, light treatment has to be abandoned. nine0003
The following simple rules will help reduce the risk of occurrence, intensity and duration of side effects:
- the device must be used in a well-lit room;
- if any adverse reactions occur, reduce the light intensity or increase the distance from the device to the eyes;
- in the event of any discomfort, it is advisable to interrupt the course of treatment for a few days, and then try again. nine0192
To prevent side effects, conduct a light therapy session in a lit room.
Types of light therapy lamps
Stationary light therapy lamps can be floor and wall (light panel).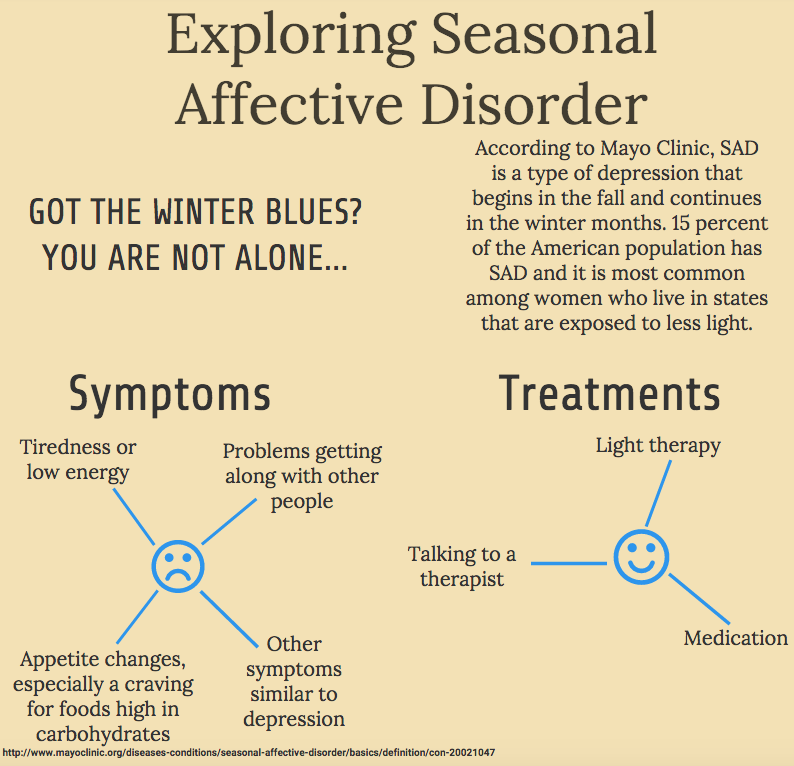 Such emitters have high power and can be used for group therapy. During the session, the patient is located on a chair, at a distance of 20-50 cm from the device. The optimal distance depends on the intensity of the radiation - the higher it is, the further you need to be from the light source. nine0003
Such emitters have high power and can be used for group therapy. During the session, the patient is located on a chair, at a distance of 20-50 cm from the device. The optimal distance depends on the intensity of the radiation - the higher it is, the further you need to be from the light source. nine0003
The main advantage of large lamps is the feeling of a “light bath”, which has a beneficial effect on well-being and mood.
Light therapy with large stationary lamps requires time and immobility
The disadvantages include:
- bulky;
- the possibility of adverse effects on the environment;
- too bright light.
Compact table lamps for individual use. The intensity of white light in such emitters is low, but the enrichment of the spectrum with blue waves allows you to get the desired therapeutic effect. Small appliances are less harmful to the environment. nine0003
Lumie table lamp with flexible emitter position adjustment
Disadvantages compared to a large emitter:
- the focus of the light stream, which can be annoying;
- no "light bath" effect.