When the pain is too much
5 Truths To Hold Onto When Your Pain Feels Like Too Much
Have you ever felt like your pain was too much? The past two years have been a period of incredible hardship for me as I stumbled through this eating disorder recovery journey.
While I would never wish pain on anyone, it is, unfortunately, universal. Every single one of us will experience pain at some point in our lives.
I’m still learning to manage the hurt. I won’t sugarcoat the amount of time and energy it takes for the power of pain to subside. However, over the past two years, I have also learned so much about myself through my pain. And these lessons are important.
Some days I have to remind myself of these lessons over and over, while other days I believe them with ease.
What do you do when it feels like the pain in recovery is too much? That’s what I want to help you with.
Here are 5 powerful facts to remember when the pain feels like too much.
I want every single one of you to remember that these statements are true for all of you.
Take them in. Repeat them. Learn to believe them.
1. You will be okay
I know that when I’m experiencing extreme pain or any intense emotion for that matter, it feels like it will never end. It is truly a horrible feeling.
Sometimes the circumstances causing the emotions are permanent – maybe it’s the loss of a loved one, a trauma that can’t be undone, or a person who simply won’t change. Things like that are truly sad, and your pain is valid.
However, the intensity of your pain will not last forever.
I know that sounds cliché, but it’s true, I know from experience.
Now, this isn’t to say it’s all sunshine and rainbows. The pain in recovery doesn’t just “go away.” Sometimes a past hurt comes back like a dagger to the heart, but it doesn’t last as long as it once did. I have the skills to manage it, and people I can go to for support.
I have the skills to manage it, and people I can go to for support.
Other kinds of pain are always there, lingering in the back of my mind, but they no longer consume me – and that’s okay.
2. You are
not too muchThe pain I felt was BIG. And sometimes that pain got expressed in very big ways – ways that overwhelmed me.
Sometimes I broke down into seemingly uncontrollable tears; other times I exploded with anger that I had let simmer for far too long. I often fell into a stubborn mindset where nothing anyone could say would change my mind. The pain felt too much.
I think these manifestations of my pain scared people sometimes. My peers didn’t know what to do or say. This made me feel like others didn’t care, and that I was simply too much. What I have learned, however, is that I am not too much.
Sometimes my pain and the expression of that pain may have been too much for certain people to handle at the time, but that is not a reflection of me.

And that’s okay – sometimes our pain in recovery is extreme and we need professionals to help us manage it. Our friends and family simply may not be equipped to help us in those moments.
This does not mean that our friends don’t care; in fact, they probably care very deeply and simply feel helpless to handle the situation.
But know that you, as a person, are never too much.
3. You are brave
Sometimes being in pain can make you feel helpless. It would be easy to remain in that helpless place, feeling like you’re suffocating; drowning.
I understand the desire to do so. Making a change can seem overwhelming and unbearable. The thing is, staying in the hurt and the helplessness keeps you stuck. It disables you from facing the deep-rooted source of that pain.
For me, there was a situation I had been trying to escape from for 18 years. The pain of remaining stuck in that situation kept me depressed and anxiety-ridden. But in facing those feelings, I realized that the deeper source of my hurt was the desire to be rescued. This also meant coming to terms with the reality that, after 18 years, that wish would never be granted.
But in facing those feelings, I realized that the deeper source of my hurt was the desire to be rescued. This also meant coming to terms with the reality that, after 18 years, that wish would never be granted.
Though enlightening, this realization brought on an entirely new level of hurt.
However, it also allowed me to wiggle myself out of that stuck, helpless place.
I realized that I had to save myself.
But that wasn’t what I wanted. Nor was it without pain, but it was a solution. I would never have discovered my bravery had I not had to fight pain head-on.
4. Sometimes the impossible happens
Pain can make you feel hopeless especially when it feels like it is too much. I can’t tell you how many times it left me on my bedroom floor crying, thinking that my dreams were shattered and my life was over. I thought that my mental illnesses and multiple stints in treatment had robbed me of all opportunities.
There was a point, not too long ago, when I was told that I would never get into another graduate school again – that it was simply an impossibility.
It was impossible because I had withdrawn from school too many times, choosing to put my health first. My emotional pain had temporarily disabled me from participating in “real life”.
I felt defeated – I had done nothing wrong other than experience the pain inflicted on me by others (if you can even consider that “wrong”) and I was punished for that.
Yet somehow, in the depths of my pain, I realized the injustice of my situation. So I picked myself up off the floor and used my pain to advocate for myself.
I cannot explain how vulnerable and heartbreaking it feels to fight a seemingly impossible battle. However, I also cannot explain the joy and pride when the impossible happens – like getting into graduate school when you were told it would never happen.
My point is, extreme pain has the capacity to leave you paralyzed on the floor. But it can also be used for good, if you let it.
5. It changes you
I would argue that nobody goes through pain unscathed. It can leave you broken, depressed, damaged, angry, lonely, and anxiety-ridden.
But the pain in recovery that feels like it is too much can also leave you stronger, braver, more confident, resilient – changed.
Most of the time, that change isn’t black and white. I still oscillate between feeling brave and broken pretty frequently. However, in the past I simply felt broken; the progress is in allowing the feelings of bravery to slowly seep into my soul and alter my beliefs.
The journey is slow, difficult, and incredibly scary, but it’s also remarkable. Allow the change to happen.
So feel your pain in recovery, Warrior. Even when it feels like it is too much. Talk about it. Learn from it. But don’t let it overtake you.
Learn from it. But don’t let it overtake you.
Interventional Spine and Pain Management Physician
When Chronic Pain Becomes Too Much?: Brian K. Rich, MD: Interventional Spine and Pain Management PhysicianNow accepting Telehealth appointments. Schedule a virtual visit.
When Chronic Pain Becomes Too Much?We’ve all experienced pain on some level. Maybe it’s a cooking mishap that caused a 1st-degree burn. Or perhaps it’s much more severe, like major surgery.
This kind of pain is called acute pain. And while all of us know what it’s like to experience acute pain, there’s another level of pain—called chronic pain—that only a select few experiences and can be much harder to treat.
What is chronic pain?You know the kind of pain that is never-ending? It’s persistent, debilitating, and carries on…and on…and on. It’s often stressful and can prevent those who have it from doing the things they love the most. That’s chronic pain.
That’s chronic pain.
More than 1 in 5 adults in the U.S. go through life with chronic pain. It lasts longer than three months, often despite treatment or medication. It can limit movement, strength, flexibility, energy, and physical endurance.
There are many reasons why someone may experience chronic pain. It can be caused by a prior injury, a complication to surgery, or may even seem to appear out of nowhere—and for no reason.
Some common types of chronic pain are:
- Headaches
- Back pain
- Cancer pain
- Arthritic pain
- Pain caused by nerve damage
- Postsurgical pain
- Post-trauma pain
Most people who experience acute pain can heal from an injury in a few days to weeks. Then life resumes back to normal. But when the pain does not go away, it can begin to affect many other aspects of life and can make even the smallest of tasks seem challenging.
Some areas of daily life that chronic pain affects are:
- Mood: Many people experience anxiety, depression, or low mood when dealing with chronic pain. It restricts their ability to live normally, often filling them with a sense of worry or hopelessness.
- Relationships: Because those who experience chronic pain are often limited in their ability to work or go out, it is much harder for them to maintain quality relationships with loved ones. This can affect all relationships, from coworkers to families and close friends. And when relationships are negatively affected, moods are also negatively affected.
- Sleep: 50-89% of those dealing with chronic pain also experience sleep issues. Lack of sleep can be highly frustrating because rest is necessary for healing, but many people cannot get the hours of sleep they need because of the pain.
- Memory and concentration: Chronic pain can affect one’s ability to remember information—ultimately interfering with long-term memory and concentration.
 A study at the University of Alberta indicated that two-thirds of tested participants with chronic pain showed impaired memory and concentration.
A study at the University of Alberta indicated that two-thirds of tested participants with chronic pain showed impaired memory and concentration.
Many people try to deal with chronic pain by just suffering through it. They tolerate the side effects and put up with an excess of other health problems because of this. Unfortunately, this can cause overwhelm and exhaustion, feeling like it’s all just too much.
So how do you take care of your chronic pain so that it’s manageable?
Thankfully, there are options. There is a way to cope with chronic pain—starting from the comfort of your home—while still maintaining quality of life.
Here are a few essential starting points to help you feel better:Physical exercise: this can be one of the best options for managing your pain. Exercise is known to release endorphins, which can improve your mood while blocking signals that you’re in pain. It also has several other positive side effects, such as strengthening your muscles, preventing injury, maintaining a healthy weight, and improving sleep quality.
It also has several other positive side effects, such as strengthening your muscles, preventing injury, maintaining a healthy weight, and improving sleep quality.
Mindfulness: Try deep breathing and meditation exercises. They not only help your body to relax, but they help distract you from the pain and instead focus on mindfulness. Incorporate these techniques into your bedtime routine. Relaxing the body before bed helps one sleep better.
Healthy eating habits: A healthy, balanced diet not only fuels your body but can also cure a whole list of health issues. Aim for various healthy foods, such as whole grains, fish, poultry, beans, nuts, and of course fruits and vegetables. If you use tobacco or drink an excess of alcohol, begin to cut that out of your diet as well.
Non-invasive help: Although these options can all be practiced from home, it’s essential that you also seek resources outside of your home. Get a massage, try out acupuncture, and see an interventional pain management specialist. Thankfully, there are many treatments available that will help you regain your quality of life.
Thankfully, there are many treatments available that will help you regain your quality of life.
There is hope! And you don’t need to live in constant pain. Begin by making small changes that will manage your stress, help you sleep better, and gain control over your health. Your chronic pain can be treated.
At Accelerated Interventional Orthopedics, we help our patients manage chronic pain—without opioid usage—by finding minimally invasive and non-operative ways to control their pain. Dr. Rich and his team work to uncover the root of your pain while providing a targeted treatment pathway.
Stop the effects of chronic pain and get your life back. Request an appointment today.
Key Takeaways- Chronic pain affects only a select few and is much harder to treat than acute pain.
- Chronic pain can be caused by a prior injury, a complication to surgery, or may even seem to appear out of nowhere.
- Chronic pain can have some significant, long-term effects on those living with it.
- There are ways to reduce some of these long-term effects and live a quality life.
Summary
Article Name
When Chronic Pain Becomes Too Much?
Description
It’s common for those who suffer from chronic pain to feel like it’s just too much to handle. But there are proven steps you can take to help manage the pain.
Author
Brian Rich
The 3 Main Benefits of a Sacroiliac Joint Fusion
Chronic low back pain can not only take the zest out of life, it can make daily life excruciatingly painful and challenging. For patients with sacroiliac joint pain, fusion surgery offers hope in restoring a life with less pain.
What to Expect the First Few Days After Getting a Nerve Stimulator Placed
Millions of Americans are living with the daily reminder of chronic pain. Treatments like nerve stimulation can ease pain when other treatments have failed. Our experts share what happens after your nerve stimulator is placed and on the job.
Treatments like nerve stimulation can ease pain when other treatments have failed. Our experts share what happens after your nerve stimulator is placed and on the job.
All About Rotator Cuff Tendonitis
Rotator cuff tendonitis can make it difficult and painful to reach up for your favorite mug in the cupboard. If you’re plagued with shoulder pain, an orthopedic specialist can help.
Key Benefits of Interspinous Fusion
Spinal stenosis can cause significant pain and interfere with your quality of life. If you still have pain after trying nonsurgical therapies, maybe it’s time to consider surgical options.
When to Consider Radiofrequency Ablation for Lower Back Pain
You might be a candidate for a radiofrequency ablation if you experience recurrent pain and have had success with a nerve block injection. Meet with our pain management specialist to find out if it’s an option for you.
Meet with our pain management specialist to find out if it’s an option for you.
Four Common Causes of Chronic Knee Pain
Knee pain can begin gradually at first and evolve into persistent discomfort that starts to interfere with your life. Rely on a knee specialist to get things back on track so that you can get back to living fully.
12 mysteries and paradoxes of pain
- Yana Litvinova
- BBC London
Image copyright, Getty Images
Image caption,We all know that pain is an objective reality, but its perception is deeply subjective. Pain can be a symptom, a disease, mental or physical. How close are we to understanding what it is?
Acute, dull, sudden, chronic, aching, throbbing, blinding. .. This is not a complete list of epithets that we use without hesitation when talking about the sensation that we all have experienced and continue to experience: pain.
.. This is not a complete list of epithets that we use without hesitation when talking about the sensation that we all have experienced and continue to experience: pain.
- Why is pain so difficult to measure and relieve?
- Medicine of the future: how bioglass will revolutionize surgery
- Why paper cuts are so painful
She doesn't care about skin color, eye shape, or social status. It doesn't care what level of evolution this or that creature is at. People, dogs, cats, dolphins, whales, birds, frogs, and even, according to scientists, earthworms experience pain.
At the same time, if scientists say that the mechanism of pain is more or less clear to them, then what is it: a signaling system of malfunctions, an obligatory part of being, without which it is impossible to understand physical and mental well-being, a purely physiological process or a result complex chemical processes in the brain, neither doctors nor even the clergy came to a unanimous agreement.
Image copyright, Getty Images
Image caption,We know how the signaling system works from neurons to the brain and back, but many questions remain unanswered
In addition, there is a group of people who, due to a genetic anomaly, do not experience pain at all.
In fact, they do not need to envy, because they can easily miss the onset of some disease, and die, although painlessly, but completely in vain.
All our knowledge of pain is based on paradoxes.
1. Our brain registers pain signals, but does not feel pain itself
Photo author, Getty Images
Photo caption,The brain registers and processes pain signals from all other parts of the body, but does not feel pain itself
Let's say you twisted your ankle or burned your finger. The nerve fibers immediately send a signal to your brain that interprets the sensation as pain.
No wonder modern surgery became possible only after the discovery of anesthesia.
However, if the brain itself is the object of the operation, then pain medication is useless.
Nerve cells in the brain send themselves the same signals as in a broken limb, only there is no data center for them.
The brain, accustomed to being responsible for the whole organism, does not understand at all when it should hurt itself.
It's kind of creepy, but patients are often fully awake during brain surgery, allowing surgeons to see if they've dug too deep into our body's main processing unit.
2. We all feel pain in different ways
Photo by DanielVilleneuve
Photo caption,Pain is subjective: for some it is agony, but for others it is a slight inconvenience.
The fact that, after, for example, a natural childbirth, one woman says that she was a little uncomfortable, but that's okay, and the other needs pain relief at the very beginning of the contractions, does not mean at all that one of them is stoic, and the other is weak slur.
How we feel pain is influenced by many factors: what chemical reactions are taking place in your brain at that time, whether an inflammatory process is taking place somewhere in your body, and how much you "remember" pain sensations that you experienced before .
As Kenneth Hansraj, head of the New York Spine Center, once said: “Someone can drill a tibia without anesthesia, and he will calmly tell you, they say, buddy, pull that thing out! the skin of a thin needle."
3. Pain can be distracted
Photo author, Portra
Photo caption,Pain can be fooled: if you start shaking a bruised finger, it becomes easier
Our brain, of course, is the most complex computer ever or created by nature, but at the same time he is a little blunt.
The fact is that it is difficult for him to analyze several sensations at the same time.
Let's say you've been bitten by a mosquito and the bite is itchy. Attach an ice cube to it, and suddenly you will realize that you still feel the cold, but the itching is gone.
Attach an ice cube to it, and suddenly you will realize that you still feel the cold, but the itching is gone.
That's why we instinctively rub a bruised area or frantically shake a finger that is accidentally pinched in a door.
0008 Redheads have a hard time: fiery hair color is accompanied by a non-standard attitude to painkillers
It's hard to believe, but in 2009 an article appeared in the Journal of the American Dental Association, according to which redheads really do not like to visit the dentist.
The fact is that the same genetic combination that gives them a fiery hair color makes them less susceptible to certain painkillers.
And sometimes they need a dose that is twice what would be enough for some brunette.
It is also possible that their body reacts to anesthesia in a way that is not entirely trivial. Some doctors, by the way, make adjustments for the patient's hair color.
5. Sex relieves pain
Image copyright, Getty Images
Image captionHaving sex can reduce migraine pain... if you have the energy to do it, of course
Well, objectively speaking, if you have a migraine attack, then sex in such a situation seems to be somewhat doubtful.
However, there are some statistics that show that 60% of migraine sufferers feel much better if they do it during an attack.
Sexual arousal releases endorphins in the brain, which are natural pain relievers.
By the way, things are not so simple with migraine patients. It is suspected that the same gene variant that bestows migraine sufferers at the same time significantly increases their libido.
6. We are mercilessly divided into women and men
The author of the photo, Getty Images
Image caption,We all feel the same way, only men believe that we should endure
Actually, there is no scientific evidence that that men and women experience pain differently.
Although doctors note that, in general, women are more likely to admit that they are in pain.
Perhaps this is due to a social stereotype that requires "real" men to endure with clenched teeth.
7. Those who don't feel pain
Image copyright, Getty Images
Image captionThose who don't feel pain don't do so well: just touching a hot stove can result in a third-degree burn
This is a very rare genetic anomaly. So rare that in the entire history of medicine it has met only a few dozen times.
Those who are very unlucky to be born with it can, for example, feel whether an object is hot or cold, but they do not feel pain.
And that, by the way, is really bad. For example, accidentally touching a hot stove might result in a third-degree burn, instead of the small blister that would result if they quickly figured out what was happening and pulled their hand away.
According to available statistics (which, for quite obvious reasons, are extremely small), the average life expectancy of such insensitive people is significantly below the average.
8. The most common pain
Image copyright Getty Images
Image caption,The most common pain in developed countries is pain in the lower back.
This is back pain. Approximately 27% of people in developed countries claim to suffer from low back pain.
Whereas from constant headaches or migraines - only 15%. Experts advise not to disdain physical exercises and not to gain excess weight.
However, this is a consequence of our evolutionary successes. Bipedalism is not at all conducive to spinal health. Quadrupeds, in which the weight is distributed much more evenly, do not face back pain.
9. What hurt kings and dinosaurs
Photo copyright, Getty Images
Image caption, Both kings and dinosaurs suffered from gout.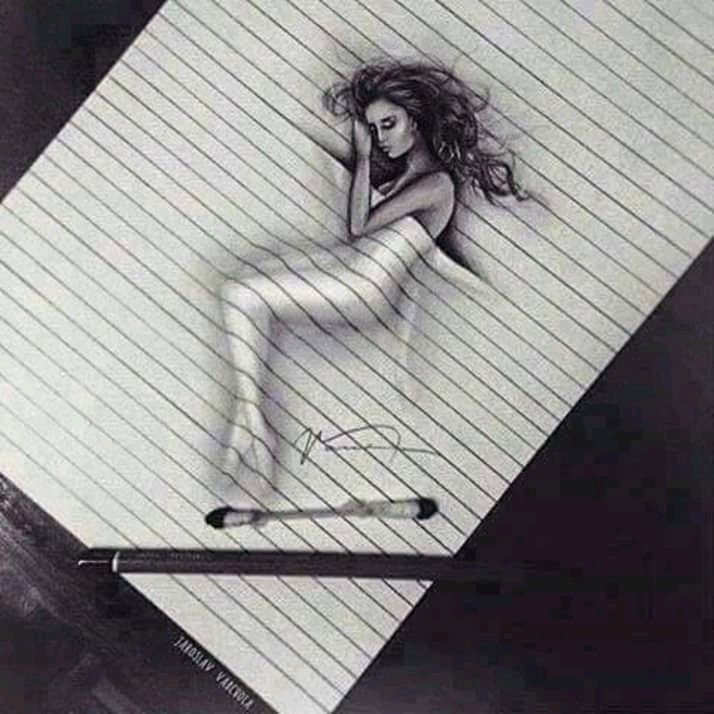 True, there is a dragon here, but it is probably a close relative of the Tyrannosaurus rex
True, there is a dragon here, but it is probably a close relative of the Tyrannosaurus rex
Gout, also known as arthritis, used to be called the disease of kings, since it was allegedly the result of excessive consumption of fatty foods and alcohol.
It is clear that in the distant Middle Ages only very wealthy people could afford it. We now know that gout pain is caused by the formation of sharp uric acid crystals inside the joints.
Examination of the skeletal upper limb of a female Tyrannosaurus rex (which palaeontologists named Sue) showed that this particular Jurassic predator also suffered from gout, and in a very advanced form. It is likely that Sue suffered from chronic pain throughout the last years of her life.
10. The nature of pain is not at all unambiguous
The author of the photo, Getty Images
Image caption, Sometimes pain turns from a symptom into a disease. It hurts everywhere, and why is not clear
It hurts everywhere, and why is not clear
Pain is a symptom, which, however, gives only a general idea that something is wrong, but does not give any specifics.
And in patients suffering from central pain syndrome, the pain itself becomes the disease, not its symptom.
Such patients complain of pain throughout the body, with sensations ranging from "pins and needles" to "strong pressure". In this case, the brain is not just a registrar and processor of pain sensations, but also their main generator.
11. Don't underestimate your brain
Image copyright, Getty Images evaluates the signals it receives, deciding how serious the danger is and whether immediate action should be taken.
Having received an alarm signal, the brain immediately tries to answer the main question: "How dangerous is this all really?"
In assessing the situation, our central processor uses all the information it has at its disposal: from subjective, coming from our past experience, to objective, obtained from the whole complex of physical and chemical parameters of the organism.
And having received a signal, it sends "instructions" to the nerve endings on how to behave. Canadian physician Paul Ingram described the process in this imaginary dialogue:
Image copyright, Getty Images
Image caption,The brain commands neurons as it wants, and they have to obey
Nerves: Problem! Problem! Huge! Big! Red alert! Turn on immediately!
Brain: Mmmmm, right? Okay, I took note. But guys, I have a database here, sorry, it's strictly secret, so take my word for it: it's not all that scary. Relax.
Nerves : No, no, listen, this is all very serious!
Brain: Nope, I don't believe it.
Nerves: Look, maybe we don't have access to this "information" that you talk about all the time, but we know very well what tissue damage is! And we're not playing games here. We won't shut up until you take action!
Brain (in the voice of a hypnotist): You no longer remember what it was. There is absolutely no need to send me signals. Everything is absolutely fine, breathe deeply…
There is absolutely no need to send me signals. Everything is absolutely fine, breathe deeply…
Nerves: Ah, yes… What are we talking about? Damn, it looks like they just wanted to report something important... Well, okay, we'll be back later.
12. The ultimate boss
Photo credit, Getty Images
Photo caption,The brain decides how to regulate the pain button in our body, and why sometimes it stops at six and sometimes at ten, we are up to we still don't know for sure
The brain can really twirl its peripheral nerve endings as it pleases.
If he doesn't like something, he can ask for more information. Or maybe order his subordinates not to fuss.
In recent years, a lot of information has appeared, according to which nerves in the periphery can actually change both physically and chemically, possibly following a command coming from the brain.
As the same Paul Ingram noted: "The brain can not only turn the button that controls the sound, but easily change all the equipment, changing the signal itself long before it enters the speakers. "
"
Conclusion
The final nature of pain, despite the fact that it is an integral part of the existence of all living beings, is still not known to us.
Stomach pain
As you know, pain in the abdominal cavity can cause diseases of the organs that are located in it. Unlike, for example, from a heart attack, in this case, pain does not require urgent measures, although here the correct diagnosis is no less important. If your life after the first heart attack will never be the same as before, then if the surgeon removes your gallbladder or inflamed appendix, he will thereby destroy the disease itself. And men who experience abdominal pain are usually very afraid of appendicitis, ulcers. Though they better be worried about their gallstones or diverticula, as ulcers and appendicitis are not as common these days.
Also, unlike chest pain, acute abdominal pain almost never requires an immediate response, even with a perforated ulcer, a slight delay of a couple of hours is not at all fatal. However, if a couple of days are late, usually patients either die or the doctors are sued. But fortunately, abdominal pain in many cases is a symptom of a completely minor disorder. And in order to better understand them, you can use the following tips.
However, if a couple of days are late, usually patients either die or the doctors are sued. But fortunately, abdominal pain in many cases is a symptom of a completely minor disorder. And in order to better understand them, you can use the following tips.
The first step is to determine exactly where your pain is. So the navel serves as the border between the lower and upper sections of your digestive tract (although the large intestine runs higher, however, serious pain is usually localized there at the bottom). And the small intestine, coiled in loops, is located in the center of your abdomen behind the navel. He is usually very rarely exposed to serious diseases. The most common sources of pain in your abdomen can be:
- The duodenum is the first section of the small intestine, about 25 cm long. Food enters it directly from the stomach and ulcers usually occur more often than in the stomach, but bowel pain is indistinguishable from stomach pain.
- Stomach - located above the horizontal line, which under the arc of the ribs of the chest passes through the navel (the so-called epigastric region).
 Back in school, we were taught that the stomach digests and mixes food, and its main function is its storage and accumulation. However, a person deprived of a stomach can also digest food normally, only if it is consumed in large quantities, then unpleasant sensations may appear.
Back in school, we were taught that the stomach digests and mixes food, and its main function is its storage and accumulation. However, a person deprived of a stomach can also digest food normally, only if it is consumed in large quantities, then unpleasant sensations may appear. - The liver is the largest organ in the abdominal cavity. The liver is located in its upper right part. It should be noted that quite rarely, liver diseases are a source of acute abdominal pain.
- The gallbladder is a small sac located at the bottom of the chest on the right side. Thus, oily bile continuously enters the gallbladder from the liver, where it accumulates and concentrates. And after eating, the gallbladder delivers it to the duodenum in order to improve the absorption of food fats. Pain in the gallbladder can occur for completely different reasons. The most common cause is stones formed from hardening bile. This is due to the appearance of cholesterol in bile, which precipitates first at high concentrations, as well as dehydration of bile.
 However, stones are completely harmless as long as they lie motionless in the gallbladder. And problems can begin when they move, blockage of the bile duct, which leads to the small intestine. And the pain that can occur when pushing a stone through the duct can last up to several hours.
However, stones are completely harmless as long as they lie motionless in the gallbladder. And problems can begin when they move, blockage of the bile duct, which leads to the small intestine. And the pain that can occur when pushing a stone through the duct can last up to several hours. - Large intestine. Most often, pain in it occurs somewhere in the lower left side of the abdomen (cramps, diverticulitis, diarrhea, constipation), and sometimes even in the lower right side of the abdomen (appendicitis). However, the most serious diseases in the colon can rarely cause pain above the navel. But we must not forget about the pain in the left upper abdomen, which occurs with the syndrome of accumulation of gases in the splenic flexure. Also, the colon on the right under the liver has a different 90° turn, but with a much smoother radius, and so gas pain is not so often noted here.
- Pancreas - located in the abdominal cavity quite deep behind the duodenum, stomach. It produces a certain secret, which contains many enzymes, which then enters the small intestine through a separate duct.
 With inflammation of the pancreas (pancreatitis), pain usually occurs in the epigastric region, which can be felt on the left.
With inflammation of the pancreas (pancreatitis), pain usually occurs in the epigastric region, which can be felt on the left.
After you determine the nature of your pain (aching pain, burning, gas pain), try very hard to somehow abstract from it. In some textbooks, the pain of an ulcer is described as burning, and the pain from blockage of the duct by a stone is described as colic, which increases to a maximum and immediately subsides. And gas pains are usually compared there with a certain movement of a large ball through the insides. All these descriptions may sometimes not correspond to your feelings, since the nerves that transmit pain signals from the internal organs, unlike the nerve endings of the skin, are too primitive. Sometimes your life depends on many subtle sensations, but the signals inside the body can only serve as a rude warning. A burn of the stomach with acid can cause both aching, dull, gnawing, sharp pain, and not cause any pain at all.
When exactly do you feel pain?
The pain that woke you up in the middle of the night deserves special attention. Usually, pain at night in the stomach area can signal an ulcer, since after midnight the stomach is usually empty, and acid secretion increases after about 2 hours. Such pains sometimes appear with almost any violation of the functions of the stomach, as well as with various indigestions and dyspepsia.
Usually, pain at night in the stomach area can signal an ulcer, since after midnight the stomach is usually empty, and acid secretion increases after about 2 hours. Such pains sometimes appear with almost any violation of the functions of the stomach, as well as with various indigestions and dyspepsia.
You can think about the relationship of pain with your food. Often with an ulcer, "hunger pains" are felt because the food neutralizes the acid, but they usually disappear immediately after eating, but not always. And gas pains usually occur after eating after 1-2 hours, but not because their food releases when it enters the stomach, but precisely because when digesting food, the intestines contract intensively, thereby compressing the gases already there .
Symptoms associated with pain
Infections can sometimes be accompanied by fever. Also, with catarrh of the stomach, diverticula, appendicitis, the temperature may rise. However, with stones in the gallbladder, gases, ulcers, this is not observed. And the absence, presence, even a slight rise in temperature cannot accurately indicate the severity of the violation.
And the absence, presence, even a slight rise in temperature cannot accurately indicate the severity of the violation.
Vomiting can start when the gastric outlet is blocked, and even with a chronic ulcer. And blocking the exit from the stomach sometimes requires surgical intervention. Often, vomiting is accompanied by severe pain with gallstones, exacerbation of an ulcer, but in general, vomiting is not a specific signal about some kind of malfunction in your digestive tract. The same applies to diarrhea.
Degree of risk
A small hernia (diverticulum) often occurs in the colon in middle-aged and older people, because after prolonged use of food that is poor in coarse fibers, its walls weaken, the weakest parts of the colon sag, thereby bulging outwards as diverticula sacs. Usually, in older people, you can find dozens of diverticula that do not bother them at all, but until they begin to bleed a little or tear the wall of the colon. A break (perforation) usually causes a very painful infection (diverticulitis), which is usually treated with antibiotics, a liquid diet, but can sometimes require surgery.
If you constantly ate a large amount of coarse fiber food and did not suffer from constipation, then your colon experienced little stress, and your risk of diverticulitis is quite small.
It is worth noting that appendicitis at any age is dangerous, but usually this disease is characteristic of people in adolescence or early adulthood. And pain in the lower right side of the abdomen, which is accompanied by nausea, a slight temperature, a general painful condition, can usually indicate appendicitis.
Also severe pain in the same area, while the general state of health is normal, usually associated with intestinal irritation, gas.
Gallbladder stones are twice as common in women as in men.
How bad is your pain?
More often than not, moderate pain may indicate a minor illness. And excruciating pain, too, may not necessarily be a symptom of a disease that threatens your life, since it can accompany even simple gastroenteritis (gastric catarrh), but you should still pay attention to it.