When pain becomes too much
What To Do When Chronic Pain Becomes Too Much
How Do You Know When Chronic Pain Becomes Too Much To Handle?People with chronic pain can be incredibly resilient after facing daily discomfort for long periods of time. We quickly build a new kind of tolerance to the typical aches and pains. Plus, we have to get creative with how we do day-to-day activities through or around the pain. Chronic pain survivors are often tough because we have no other choice but to be. But all this said, there’s no hiding the impact that living with chronic pain can have on our lives.
So, what do you do when chronic pain becomes too much? Below, we’ve put together some suggestions on what you can do when chronic pain becomes too much to function as you normally would. From self-care to self-advocacy, there are resources to lean on in the times when the pain goes off the scale.
How Do You Know When Chronic Pain Becomes Too Much To Handle?
There are different types of pain that people can experience. Some people might only ever have instances of acute pain while others deal with the long-term effects of chronic pain.
- Advertisement -
The main difference when it comes to acute pain is that this type of pain usually happens suddenly and does not last longer than four weeks. Acute pain usually is the result of an injury, surgery, illness, or other types of strain. Any type of pain, acute or chronic, can disrupt somebody’s abilities. However, chronic pain usually has a longer impact on somebody’s life because it’s not something that resolves after time.
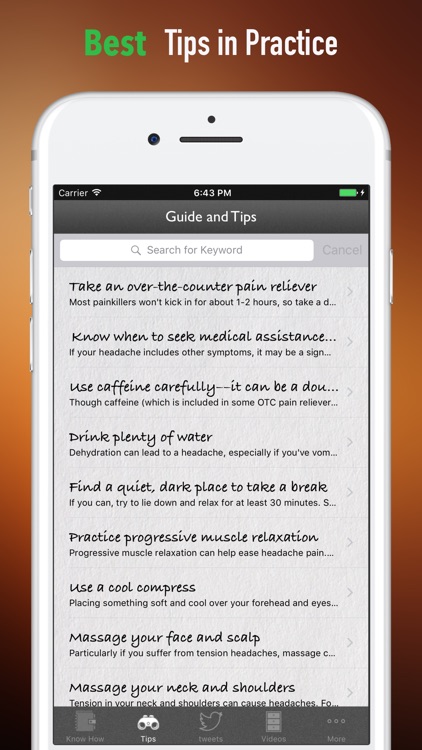
Those with acute pain might have an action plan to work toward eliminating the discomfort. People with chronic pain might have similar methods, such as:
- Taking pain medication
- Applying heat or ice
- Doing physical therapy or other tolerated, gentle movements
- Using distractions (seeing friends, watching movies, reading books, etc.
 )
) - Eating well/avoiding certain foods
- Stress management
But people living with chronic pain might not always find success in these traditional methods. One sign of when chronic pain becomes too much to handle is when there is no relief from the pain, despite these attempts.
Additionally, an indicator that chronic pain has become too much to handle is when it begins to greatly impact one’s quality of life. This means that the pain is so severe that the person experiencing it is unable to work, socialize, find joy in going out, care for themselves independently, or function in other ways.
- Advertisement -
When this happens, people living with chronic pain can face a whole new onslaught of challenges. Not only is it incredibly frustrating to have one’s day-to-day life greatly impacted, but the side effects of pain can be detrimental to one’s overall well-being—including physical and mental health.
Chronic Pain and Mental Health Support
One of the most important resources when chronic pain becomes too much to cope with is to get mental health assistance. The physical experiences of chronic pain are a lot to handle on their own, but there is also an emotional component that comes with this as well.
The physical experiences of chronic pain are a lot to handle on their own, but there is also an emotional component that comes with this as well.
Research shows that people living with chronic pain are at an increased risk of having anxiety and depression as well. When chronic pain becomes too much for a person, it can leave them feeling isolated, stuck, and dependent on others. Sometimes, this leads to a negative self-image.
Even just worrying about when you’ll feel pain next or how you’ll do day-to-day things when the pain flares up can cause a harmful impact on your mental health. Feelings of sadness, helplessness, and loneliness are all common to experience with chronic pain—but nobody should have to deal with these feelings alone.
Attending counseling, practicing mindfulness, and getting help from chronic pain support groups are all useful resources when chronic pain becomes too much. Support groups can be particularly helpful when people living with chronic pain feel as though nobody else understands their struggle. In reality, many people face similar issues when it comes to chronic pain. While this might not make the pain any less severe, it can help lessen the emotional side effects that come with chronic pain.
In reality, many people face similar issues when it comes to chronic pain. While this might not make the pain any less severe, it can help lessen the emotional side effects that come with chronic pain.
Advocating for Yourself
Perhaps most importantly, advocating for yourself when chronic pain becomes too much for you to function is absolutely vital to managing your health and happiness. Self-advocacy is the practice of speaking up for your needs. This could mean speaking with your doctor in order to express that the current method of treatment for your pain is not working as effectively as it could be.
Advocating for yourself might also look like asking for accommodations at work. This can be very beneficial to your overall health. Accommodations are very necessary when chronic pain becomes too much to function as you typically would, but they also can help to prevent more pain. For example, if chronic pain makes it challenging for you to take the stairs, having elevator access can reduce the risk of experiencing more pain and might even help you to save the energy that you need to make it through the day.
Moreover, speaking out on the need for digital accessibility can be a useful form of self-advocacy when chronic pain becomes too much to do things physically and leaves you to find other methods of accessing resources or support. Digital access to online support groups, your medical charts, and even using apps to track patterns in your pain are all strategies that might be helpful in better managing the constant discomfort that comes with chronic pain.
When Chronic Pain Becomes Too Much, Don’t Sacrifice Yourself
The biggest takeaway here is that chronic pain can have a significant impact on your quality of life. The trick to living with chronic pain is to find ways to make it more tolerable in the hardest of moments so that you can still find joy and wellness in your day-to-day life. Of course, this is easier said than done.
Pain is complex and people living with chronic pain often have to cope with constant discomfort. There is not a one-size-fits-all solution to what people should do when chronic pain becomes too much to cope with. While some people might find relief in certain remedies like pain medication or physical therapy, others must take the time to practice self-care and tend to their mental health.
While some people might find relief in certain remedies like pain medication or physical therapy, others must take the time to practice self-care and tend to their mental health.
Whatever coping strategies you might turn to when chronic pain becomes too much, just keep in mind that you shouldn’t have to sacrifice yourself or your well-being. Listen to your body’s needs. Sometimes, the different pains can be an indicator that you need to take a break, get those accommodations, or work to advocate for better pain management. Most of all, practice patience and kindness toward yourself.
It’s easy to become frustrated with your body and your abilities when chronic pain becomes too much to handle. Consider making a list of all of the things you can do in spite of the pain. Or use the support of others who understand the struggles of living with chronic pain. You are not alone in this fight—and you are not without hope. Though it may not feel like it, better days are ahead.
What Do You Do When Chronic Pain Becomes Too Much?
Let us know in the comments below.
What topics related to pain management should we cover next?
Email us your ideas at [email protected].
Are you or someone you know living with chronic pain? Looking for a support group?
Join our online community and start building your support network today!
- Pain Resource Giveaway -
JOIN THE CONVERSATION
RELATED
Interventional Spine and Pain Management Physician
When Chronic Pain Becomes Too Much?: Brian K. Rich, MD: Interventional Spine and Pain Management PhysicianNow accepting Telehealth appointments. Schedule a virtual visit.
When Chronic Pain Becomes Too Much?We’ve all experienced pain on some level. Maybe it’s a cooking mishap that caused a 1st-degree burn. Or perhaps it’s much more severe, like major surgery.
This kind of pain is called acute pain. And while all of us know what it’s like to experience acute pain, there’s another level of pain—called chronic pain—that only a select few experiences and can be much harder to treat.
You know the kind of pain that is never-ending? It’s persistent, debilitating, and carries on…and on…and on. It’s often stressful and can prevent those who have it from doing the things they love the most. That’s chronic pain.
More than 1 in 5 adults in the U.S. go through life with chronic pain. It lasts longer than three months, often despite treatment or medication. It can limit movement, strength, flexibility, energy, and physical endurance.
There are many reasons why someone may experience chronic pain. It can be caused by a prior injury, a complication to surgery, or may even seem to appear out of nowhere—and for no reason.
Some common types of chronic pain are:
- Headaches
- Back pain
- Cancer pain
- Arthritic pain
- Pain caused by nerve damage
- Postsurgical pain
- Post-trauma pain
Most people who experience acute pain can heal from an injury in a few days to weeks. Then life resumes back to normal. But when the pain does not go away, it can begin to affect many other aspects of life and can make even the smallest of tasks seem challenging.
Then life resumes back to normal. But when the pain does not go away, it can begin to affect many other aspects of life and can make even the smallest of tasks seem challenging.
Some areas of daily life that chronic pain affects are:
- Mood: Many people experience anxiety, depression, or low mood when dealing with chronic pain. It restricts their ability to live normally, often filling them with a sense of worry or hopelessness.
- Relationships: Because those who experience chronic pain are often limited in their ability to work or go out, it is much harder for them to maintain quality relationships with loved ones. This can affect all relationships, from coworkers to families and close friends. And when relationships are negatively affected, moods are also negatively affected.
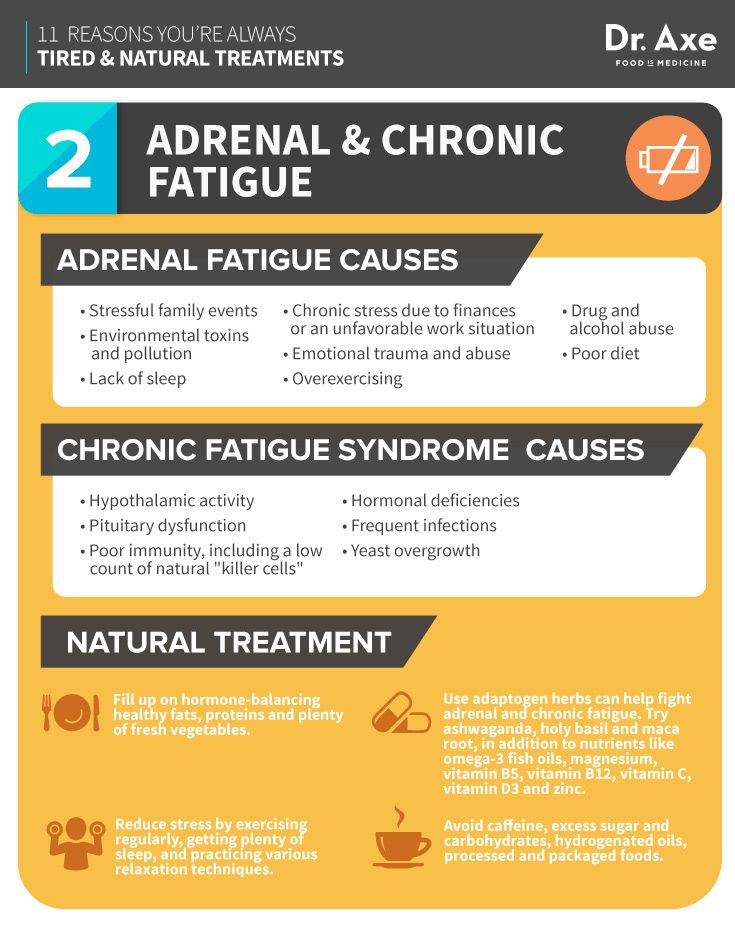
- Sleep: 50-89% of those dealing with chronic pain also experience sleep issues. Lack of sleep can be highly frustrating because rest is necessary for healing, but many people cannot get the hours of sleep they need because of the pain.

- Memory and concentration: Chronic pain can affect one’s ability to remember information—ultimately interfering with long-term memory and concentration. A study at the University of Alberta indicated that two-thirds of tested participants with chronic pain showed impaired memory and concentration.
Many people try to deal with chronic pain by just suffering through it. They tolerate the side effects and put up with an excess of other health problems because of this. Unfortunately, this can cause overwhelm and exhaustion, feeling like it’s all just too much.
So how do you take care of your chronic pain so that it’s manageable?
Thankfully, there are options. There is a way to cope with chronic pain—starting from the comfort of your home—while still maintaining quality of life.
Here are a few essential starting points to help you feel better:Physical exercise: this can be one of the best options for managing your pain.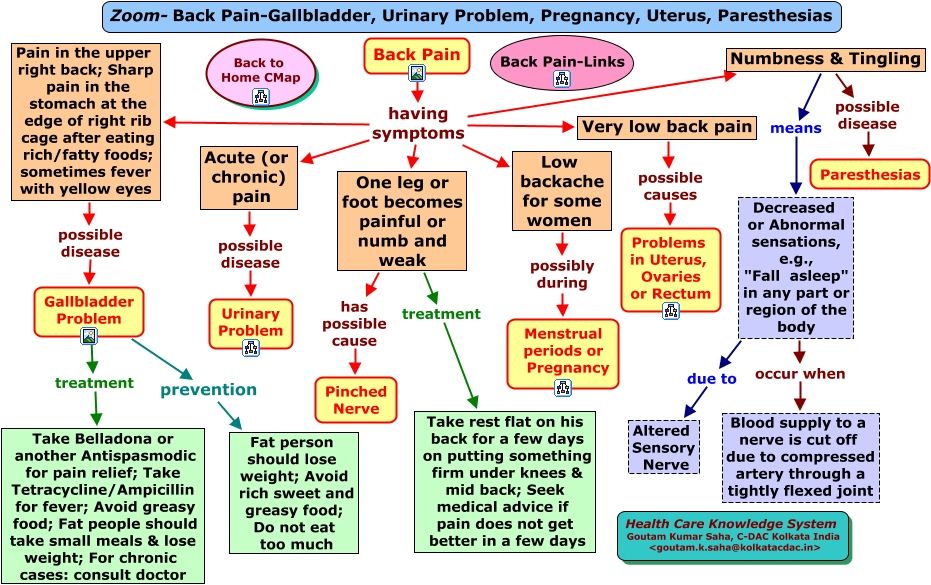 Exercise is known to release endorphins, which can improve your mood while blocking signals that you’re in pain. It also has several other positive side effects, such as strengthening your muscles, preventing injury, maintaining a healthy weight, and improving sleep quality.
Exercise is known to release endorphins, which can improve your mood while blocking signals that you’re in pain. It also has several other positive side effects, such as strengthening your muscles, preventing injury, maintaining a healthy weight, and improving sleep quality.
Mindfulness: Try deep breathing and meditation exercises. They not only help your body to relax, but they help distract you from the pain and instead focus on mindfulness. Incorporate these techniques into your bedtime routine. Relaxing the body before bed helps one sleep better.
Healthy eating habits: A healthy, balanced diet not only fuels your body but can also cure a whole list of health issues. Aim for various healthy foods, such as whole grains, fish, poultry, beans, nuts, and of course fruits and vegetables. If you use tobacco or drink an excess of alcohol, begin to cut that out of your diet as well.
Non-invasive help: Although these options can all be practiced from home, it’s essential that you also seek resources outside of your home.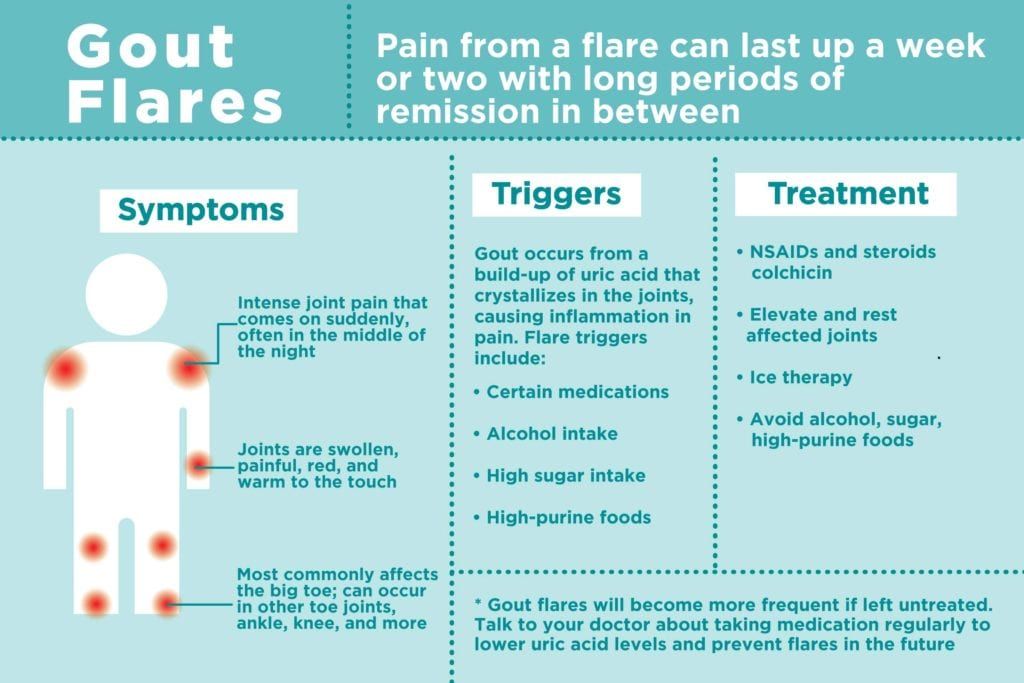 Get a massage, try out acupuncture, and see an interventional pain management specialist. Thankfully, there are many treatments available that will help you regain your quality of life.
Get a massage, try out acupuncture, and see an interventional pain management specialist. Thankfully, there are many treatments available that will help you regain your quality of life.
There is hope! And you don’t need to live in constant pain. Begin by making small changes that will manage your stress, help you sleep better, and gain control over your health. Your chronic pain can be treated.
At Accelerated Interventional Orthopedics, we help our patients manage chronic pain—without opioid usage—by finding minimally invasive and non-operative ways to control their pain. Dr. Rich and his team work to uncover the root of your pain while providing a targeted treatment pathway.
Stop the effects of chronic pain and get your life back. Request an appointment today.
Key Takeaways- Chronic pain affects only a select few and is much harder to treat than acute pain.
- Chronic pain can be caused by a prior injury, a complication to surgery, or may even seem to appear out of nowhere.
- Chronic pain can have some significant, long-term effects on those living with it.
- There are ways to reduce some of these long-term effects and live a quality life.
Summary
Article Name
When Chronic Pain Becomes Too Much?
Description
It’s common for those who suffer from chronic pain to feel like it’s just too much to handle. But there are proven steps you can take to help manage the pain.
Author
Brian Rich
How to Relieve Knee Pain Without Surgery
Don't let knee pain hold you back. Discover nonsurgical treatment options that can help improve the pain, function, and mobility of your knee.
Lifestyle Habits That Can Cause Neck Pain
Waking up with a stiff neck is common, but when the pain doesn’t resolve, it’s possible that lifestyle habits are to blame. Breaking these habits can restore spine health and relieve neck pain.
Breaking these habits can restore spine health and relieve neck pain.
How Do Pinched Nerves Occur in My Back?
Living with back pain from a pinched nerve can have a major impact on your ability to fully enjoy your life, making it difficult to work and pursue hobbies. Don’t put off seeking help for back pain. Treatment can help restore quality of life.
When Is Radiofrequency Ablation Recommended?
Radiofrequency ablation is a relatively new and advanced pain management technique. It targets specific nerves that are causing pain and provides relief by disabling pain-causing nerves.
The 3 Main Benefits of a Sacroiliac Joint Fusion
Chronic low back pain can not only take the zest out of life, it can make daily life excruciatingly painful and challenging. For patients with sacroiliac joint pain, fusion surgery offers hope in restoring a life with less pain.
For patients with sacroiliac joint pain, fusion surgery offers hope in restoring a life with less pain.
What to Expect the First Few Days After Getting a Nerve Stimulator Placed
Millions of Americans are living with the daily reminder of chronic pain. Treatments like nerve stimulation can ease pain when other treatments have failed. Our experts share what happens after your nerve stimulator is placed and on the job.
Pain. What is this? How can you help someone in pain? — Health Olympus
Pain has been known to the world since the beginning of life. Every living organism, when exposed to excessive environmental factors (high and low temperatures, trauma, chemical damage, etc.), must react and defend itself. It is pain that is the red flag that the body throws out so that the human consciousness reacts and reduces the volume or strength of the damaging effect. Thus, pain is a shield that reduces damage. After all, if we did not feel that we burned our finger, we would burn out completely. But, unfortunately, pain is not only protective.
Thus, pain is a shield that reduces damage. After all, if we did not feel that we burned our finger, we would burn out completely. But, unfortunately, pain is not only protective.
Let's touch on a few definitions of "pain".
Pain is an unpleasant or painful sensation, an experience of physical or emotional suffering. Serves as a signal of real or perceived tissue damage or psychological distress; pain can also be caused by disorders in the functioning of the nervous system. It is one of the symptoms of a number of diseases.
Pain is a kind of mental state of a person, determined by a combination of physiological processes in the central nervous system caused by a strong stimulus.
These definitions show that pain is always subjective. Only the sufferer feels it, and no one, even an experienced doctor, can see it and fully appreciate it.
Personally, I like this definition. Pain is a psychosocial phenomenon that disrupts a person's habitual lifestyle and is associated with unpleasant subjective sensations.
Pain is often caused by a disease or injury. Having cured this condition, the doctor, according to the logic of things, should remove the pain. But some diseases are not completely reversible (curvature of the spine, chronic herpetic neuropathy, cicatricial deformities, amputations of body parts) and lead to chronic pain or, in simple words, to a constant sensation of pain of varying degrees of intensity. In this case, pain is no longer one of the symptoms of a causative disease, it itself manifests itself as a powerful damaging factor and leads to serious changes in the physiology of the body, as well as in the psychosocial background of the individual. The work of all human organs and systems is changing (sleep disorder, intestinal disorders, fluctuations in blood pressure, increased stress on the heart). The psyche of the individual changes significantly. People lose their jobs, family relationships are disorganized.
In this situation, the pain itself needs to be treated. The red flag has already been thrown away, the person has realized where and how it hurts. Perhaps even the cause that provoked the pain disappeared.
The red flag has already been thrown away, the person has realized where and how it hurts. Perhaps even the cause that provoked the pain disappeared.
Everyone knows the names of drugs for pain relief. They are available in tablet and injectable form and belong to the group of non-steroidal anti-inflammatory drugs (NSAIDs). The drugs act on the entire body, regardless of the form of administration. The mechanism of action is associated with blocking the enzyme COX 1 and COX 2 and reducing the inflammatory response.
In ordinary acute conditions (bruises, injuries), these drugs are successfully used. However, complications rarely occur. Painkillers do not always help in an acute process, for example, in radicular syndrome, the cause of which is the infringement and injury of a large nerve trunk that exits through narrow foraminal openings. There is severe back pain that is not amenable to conventional treatment.
A key feature of the use of NSAIDs is the need for good blood flow in the area of pain. Inflammation and pain go hand in hand. And where inflammation is present, blood flow is always reduced. Accordingly, only a small concentration of the drug will fall into the zone of inflammation and pain. Skin patches also cannot deliver the drug to the focus of pain, since the depth of penetration of drugs through the skin is very low, only 1-2 centimeters. For example, with radicular syndrome, pain is localized at a depth of up to 11 centimeters from the skin. Increasing the dose of the drug in injections or tablets will not have an effect, but will only increase the toxic effect (stomach ulcers, blood clotting disorders, kidney and liver damage).
Inflammation and pain go hand in hand. And where inflammation is present, blood flow is always reduced. Accordingly, only a small concentration of the drug will fall into the zone of inflammation and pain. Skin patches also cannot deliver the drug to the focus of pain, since the depth of penetration of drugs through the skin is very low, only 1-2 centimeters. For example, with radicular syndrome, pain is localized at a depth of up to 11 centimeters from the skin. Increasing the dose of the drug in injections or tablets will not have an effect, but will only increase the toxic effect (stomach ulcers, blood clotting disorders, kidney and liver damage).
The only effective way to deliver the drug to the site of pain in this case is an injection into the area of inflammation itself. For this, deep blockades are used.
Blockades differ in their method and purpose. Some doctors perform therapeutic blockades "blindly", using only the patient's anatomical landmarks. The effectiveness of such a blockade is always low, the likelihood of complications increases and there is no diagnostic value at all. After all, the doctor in such a case does not know where the tip of the needle is and, accordingly, where the drug will be delivered.
The effectiveness of such a blockade is always low, the likelihood of complications increases and there is no diagnostic value at all. After all, the doctor in such a case does not know where the tip of the needle is and, accordingly, where the drug will be delivered.
Modern algology routinely uses visualized (“visible”, not blind, accurate) therapeutic and diagnostic blocks. The doctor performing the procedures has special equipment in his arsenal (ultrasound scanner and / or C-arm X-ray machine, neurostimulator, radiofrequency destruction device), as well as specialized certified training in working with chronic pain. Due to this, the doctor sees the tip of the needle in the deep tissues of the patient at the time of injection and injects the drug right on target. The control of the needle position is carried out in real time, which eliminates complications from manipulation. Due to the local administration of the drug, the effect on the body is reduced to zero. Therefore, these procedures are not contraindicated even for patients with pathology of the gastrointestinal tract, kidneys, liver, cardiovascular and hematopoietic systems of the body. The therapeutic effect is long-lasting and, if necessary, increases with the help of ablation techniques (temporary shutdown of work) of the nerve fiber.
The therapeutic effect is long-lasting and, if necessary, increases with the help of ablation techniques (temporary shutdown of work) of the nerve fiber.
An absolutely important aspect of the procedure is its diagnostic value. The doctor establishes a preliminary diagnosis of the cause of pain, conducts an accurate blockade. The result of the blockade is evaluated, and the doctor, knowing the area of the previous impact, can always change his tactics and the place of impact for the best result with a second blockade. This is especially important in the treatment of chronic (long-term disturbing) pain.
In conclusion, I would like to note that prolonged pain is now in itself a cause of disability. With the right approach, together with the patient and an interdisciplinary team of specialists, it is possible to return a person in pain to a full life, work and joy.
Author of the article:
Vodolazsky Nikolai Yurievich
Head of the Department of Anesthesiology and Intensive Care,
Anesthesiologist-resuscitator
- Rheumatology – interesting and completely unknown 9006
- Department of Radiology
Previous article | Next article
Muscle pain: causes and symptoms.
 Diagnosis, prevention and treatment
Diagnosis, prevention and treatment
Author, editor and medical expert - Klimovich Elina Valerievna.
Pedantine and medical expert - Arutyunyan Mariam Arutyunovna
Views: 487 701
Date of the last update: 02.202
Causes of muscle pain
Muscle fatigue
Physical activity
Injuries
Muscle inflammation
Diseases of the spine and joints
Stress
SARS and influenza
Other causes
Features of myalgia
Diagnosis of muscle pain
Methods of treatment of myalgia
Our whole life is in motion, and movement involves the work of approximately 400 skeletal muscles 1 , which, moreover, make up 40-45% of body weight 3 . Therefore, it is not surprising that every person repeatedly experiences muscle pain and discomfort in different parts of the body - neck, back, lower back and limbs 1 during their life.
Muscle pain, or, scientifically, myalgia 5 , periodically occurs in 54% of women and 45% of men of working age - from 27 to 50 years, but such a complaint is not uncommon even in children 1 . Myalgia may be mild or very severe, intolerable 1 , depending on its cause.
Causes of muscle pain
Due to the large number of nerve endings, muscle tissue is sensitive to any damage or irritation. In response, it secretes substances that stimulate pain 4.5 . There are a lot of factors that provoke muscle irritation. We will describe the most common below.
Muscle fatigue
In our technological age, many people are gradually forming a new "bad habit". Spending most of the day in front of a computer screen or holding mobile gadgets in our hands, we may not even notice that we are sitting in a completely uncomfortable and unnatural position. Especially "goes" to the muscles of the shoulder girdle, neck, back and right arm, which is constantly on the computer mouse of office workers 1 . Prolonged stay in one position or stereotypical movements can lead to overstrain of the muscles involved in the work, which we feel as soreness 1 .
Prolonged stay in one position or stereotypical movements can lead to overstrain of the muscles involved in the work, which we feel as soreness 1 .
Exercise
Body aches after exercise can occur in both untrained people and professional athletes 8 . And the cause of discomfort is the accumulation of under-oxidized metabolic products in muscle cells, in particular, pain is caused by an excessive amount of lactic acid (lactate) 2 . Less often, microtrauma becomes the cause, but this can only be observed if the training rules are violated 8 .
Muscle soreness due to fatigue does not occur immediately, but after a few hours or within 1-2 days after training or unusual physical activity and disappears within a week 8 .
Injuries
Severe pain can occur when muscle fibers and tendons are torn. This usually happens if the load is excessive, and the muscles are not prepared for it 1 . However, they can also be damaged by sudden movements 3 . In contrast to the "ache" in case of muscle overwork, pain due to injury occurs immediately, at the peak of the load 3 .
However, they can also be damaged by sudden movements 3 . In contrast to the "ache" in case of muscle overwork, pain due to injury occurs immediately, at the peak of the load 3 .
It should be remembered that even a small, but untreated injury can cause even more pronounced sprain 3 . Therefore, if you experience pain during exercise, be sure to consult a doctor to rule out a serious injury.
Back to top
Muscle inflammation
Inflammatory process in muscle tissue (myositis) may occur due to hypothermia, infection or accumulation of toxic substances 16.17 . Sometimes inflammation is limited to one muscle group. When muscles ache all over the body, this can be a sign of autoimmune diseases and other serious illnesses 7 .
Diseases of the spine and joints
Muscles respond to dysfunction of the joints associated with them 4 and vertebrae 5 . Therefore, myalgia is one of the symptoms of diseases of the spine 5.11 and the joints of the extremities 4 . For example, with osteochondrosis or scoliosis (curvature of the spine), pain in the neck, chest or lower back is associated with overstrain of the paravertebral muscles 5.11 . And in advanced cases, when a vertebra compresses the nerve root coming out of the spinal cord, the pain can “radiate” to the arm or leg 11 .
Therefore, myalgia is one of the symptoms of diseases of the spine 5.11 and the joints of the extremities 4 . For example, with osteochondrosis or scoliosis (curvature of the spine), pain in the neck, chest or lower back is associated with overstrain of the paravertebral muscles 5.11 . And in advanced cases, when a vertebra compresses the nerve root coming out of the spinal cord, the pain can “radiate” to the arm or leg 11 .
Often, myalgia in osteochondrosis is combined with a feeling of numbness or "crawling". At the moment of acute pain, the person freezes, taking a forced position 11 .
Stress
Prolonged emotional stress affects the activity of brain regions involved in pain control. No muscle damage can be detected, but nevertheless, the person complains of discomfort or soreness, which is most often chronic 11 .
ARVI and influenza
Aches in muscles and joints with colds and flu 9 - the result of exposure to muscle receptors of bacteria, viruses and substances that are formed in tissues during infection 10 .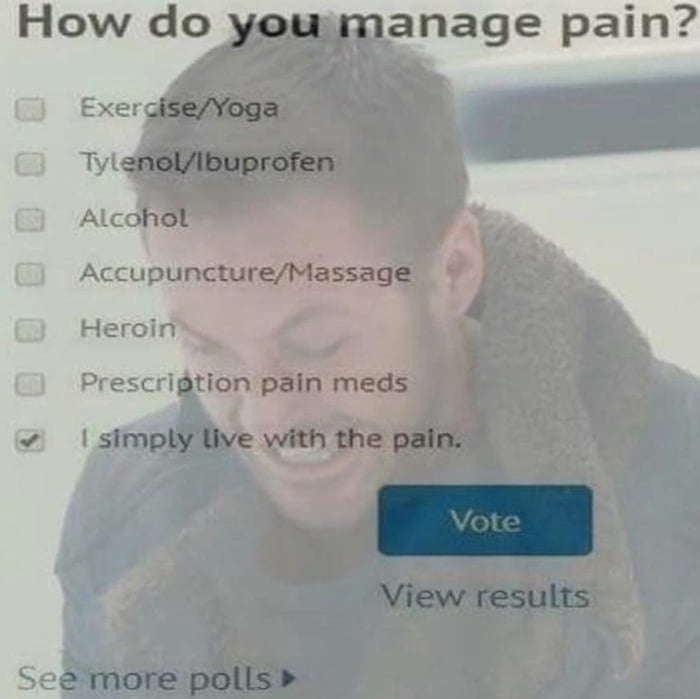 Simultaneously with muscle pain, body temperature usually rises and symptoms of damage to various parts of the respiratory tract occur: runny nose, cough and sore throat 9 .
Simultaneously with muscle pain, body temperature usually rises and symptoms of damage to various parts of the respiratory tract occur: runny nose, cough and sore throat 9 .
Other causes
Almost any disease of the internal organs can lead to myalgia 11 . When any organ is affected, it creates pain impulses, which are partially transmitted to the muscles located nearby 11 .
Myalgia can also be caused by:
- endocrine diseases, for example, deficiency of thyroid hormones 16.7 ;
- vascular pathologies that disrupt the nutrition of the muscles of the limbs 15.16 ;
- chronic fatigue syndrome 7 ;
- imbalance of trace elements in the body 16 ;
- taking cholesterol-lowering drugs 12 .
Back to top
Features of myalgia
Muscle pain, usually deep 6 . Acute myalgia is protective in nature, because it causes reactions aimed at eliminating the damaging factor 11 . Such reactions include, for example, muscle spasm 4 . But despite the protective nature, there is almost always a risk that the pain will become chronic 11 . There are 2 main causes of chronicity:
Such reactions include, for example, muscle spasm 4 . But despite the protective nature, there is almost always a risk that the pain will become chronic 11 . There are 2 main causes of chronicity:
- Hypersensitivity. In response to irritation, substances that support inflammation are released in the muscle. They further irritate the pain receptors in the muscles. In response to frequent signals, the central nervous system lowers the pain threshold, so we can feel pain in the muscle even if it is not strongly irritated 11 .
- Spasm. When pain and spasm persist, a vicious circle is formed: pain causes spasm, and spasm maintains pain 1.5, 11 .
Diagnosis of muscle pain
Determining why myalgia occurs is not always easy. Only a doctor can understand the causes and choose a treatment that helps get rid of the disturbing symptoms or alleviate them. To find out the cause of myalgia, the doctor conducts a comprehensive examination, including a neurological examination, prescribes laboratory tests, ultrasound, computed tomography and other research methods 3 .
Myalgia is treated by different specialists. Depending on its cause, a traumatologist, rheumatologist, neurologist or endocrinologist can help you.
Treatments for myalgia
Treatment of muscle pain includes non-drug and drug treatments 5.13 . In each case, the doctor selects individual methods of therapy.
One of the main tasks is pain relief 5.13 . In the fight against pain, doctors are guided by the "pain ladder" developed by the World Health Organization (WHO). It recommends the use of non-steroidal anti-inflammatory drugs (NSAIDs) as the first step or step in the treatment of mild to moderate pain 6 such as MOTRIN® 14 . The drug is approved for use in adults and adolescents over 15 years of age 14 .
The active substance of MOTRIN® - naproxen - has analgesic, anti-inflammatory and antipyretic effects. The drug can be used as part of a complex treatment of mild to moderate muscle pain associated with trauma, inflammation and diseases of the musculoskeletal system 14 . One dose of MOTRIN® is enough for up to 12 hours 14 . The drug can be used up to 5 days 14 .
The drug can be used as part of a complex treatment of mild to moderate muscle pain associated with trauma, inflammation and diseases of the musculoskeletal system 14 . One dose of MOTRIN® is enough for up to 12 hours 14 . The drug can be used up to 5 days 14 .
It is imperative that you consult your doctor, since symptomatic treatment and taking painkillers do not replace the main treatment of the disease 5 . If acute pain persists, your doctor may use other methods of pain relief 13 .
Non-drug treatments for myalgia include 13 :
- manual therapy;
- massage;
- acupuncture;
- transcutaneous electrical stimulation;
- post-isometric relaxation;
- physiotherapy exercises.
These treatments aim to relax tight muscles and relieve the spasm that causes pain, breaking the vicious cycle 13 .
Myalgia can disrupt the usual rhythm of life, interfere with work and rest.