What to do if you have a binge eating disorder
Binge Eating Disorder: Symptoms, Causes, and Treatment
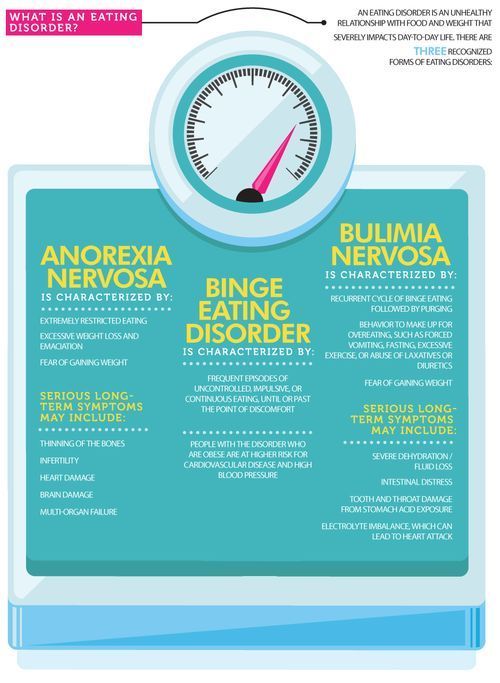
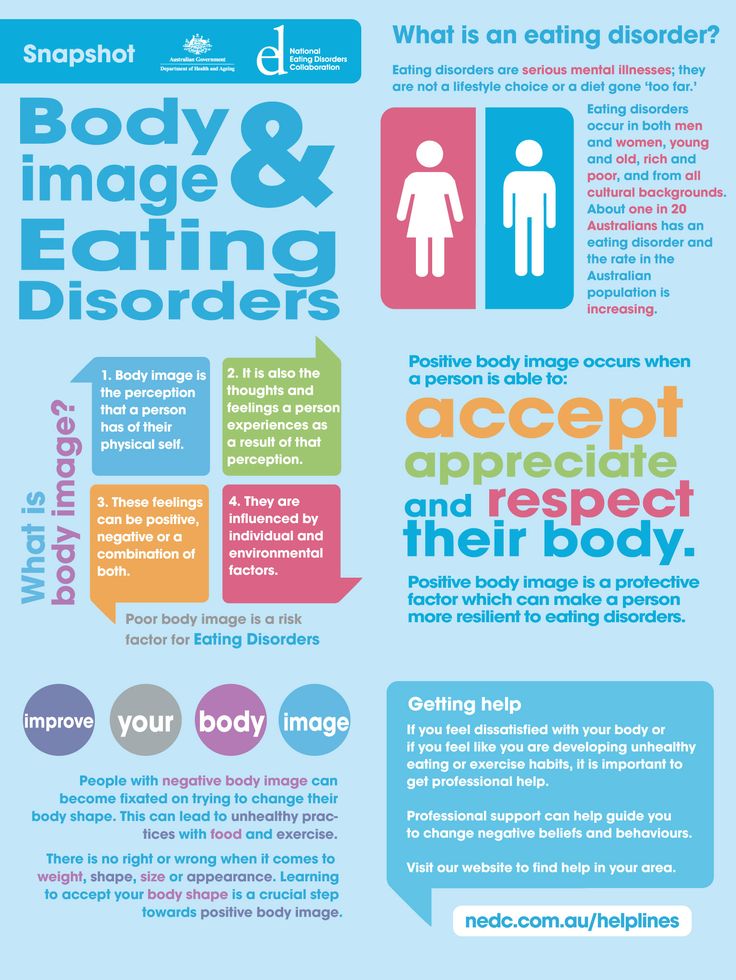
Binge eating disorder (BED) is a type of feeding and eating disorder that’s now recognized as an official diagnosis. It affects almost 2% of people worldwide and can cause additional health issues linked to diet, such as high cholesterol levels and diabetes.
Feeding and eating disorders are not about food alone, which is why they’re recognized as psychiatric disorders. People typically develop them as a way of dealing with a deeper issue or another psychological condition, such as anxiety or depression.
This article looks at the symptoms, causes, and health risks of BED, as well as how to get help and support to overcome it.
People with BED may eat a lot of food in a short amount of time, even if they aren’t hungry. Emotional stress or destress often plays a role and might trigger a period of binge eating.
A person might feel a sense of release or relief during a binge but experience feelings of shame or loss of control afterward (1, 2).
For a healthcare professional to diagnose BED, three or more of the following symptoms must be present:
- eating much more rapidly than normal
- eating until uncomfortably full
- eating large amounts without feeling hungry
- eating alone due to feelings of embarrassment and shame
- feelings of guilt or disgust with oneself
People with BED often experience feelings of extreme unhappiness and distress about their overeating, body shape, and weight (1, 2, 3).
SummaryBED is characterized by repeated episodes of uncontrolled intake of unusually large amounts of food in a short period of time. These episodes are accompanied by feelings of guilt, shame, and psychological distress.
The causes of BED are not well understood but likely due to a variety of risk factors, including:
- Genetics. People with BED may have increased sensitivity to dopamine, a chemical in the brain that’s responsible for feelings of reward and pleasure.
 There is also strong evidence that the disorder is inherited (1, 4, 5, 6).
There is also strong evidence that the disorder is inherited (1, 4, 5, 6). - Gender. BED is more common in women than in men. In the United States, 3.6% of women experience BED at some point in their lives, compared with 2.0% of men. This may be due to underlying biological factors (4, 7).
- Changes in the brain. There are indications that people with BED may have changes in brain structure that result in a heightened response to food and less self-control (4).
- Body size. Almost 50% of people with BED have obesity, and 25–50% of patients seeking weight loss surgery meet the criteria for BED. Weight problems may be both a cause and result of the disorder (5, 7, 8, 9).
- Body image. People with BED often have a very negative body image. Body dissatisfaction, dieting, and overeating contribute to the development of the disorder (10, 11, 12).
- Binge eating. Those affected often report a history of binge eating as the first symptom of the disorder.
 This includes binge eating in childhood and the teenage years (4).
This includes binge eating in childhood and the teenage years (4). - Emotional trauma. Stressful life events, such as abuse, death, separation from a family member, or a car accident, are risk factors. Childhood bullying due to weight may also contribute (13, 14, 15).
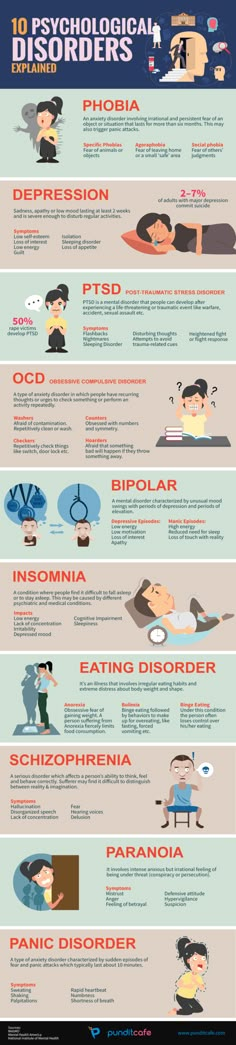
- Other psychological conditions. Almost 80% of people with BED have at least one other psychological disorder, such as phobias, depression, post-traumatic stress disorder (PTSD), bipolar disorder, anxiety, or substance abuse (1, 8).
An episode of binge eating can be triggered by stress, dieting, negative feelings relating to body weight or body shape, the availability of food, or boredom (1).
SummaryThe causes of BED are not fully known. As with other eating disorders, a variety of genetic, environmental, social, and psychological risks are associated with its development.
While some people may occasionally overeat, such as at Thanksgiving or a party, it does not mean they have BED, despite having experienced some of the symptoms listed above.
BED typically starts in the late teens to early twenties, although it can occur at any age. People generally need support to help overcome BED and develop a healthy relationship with food. If left untreated, BED can last for many years (16).
To be diagnosed, a person must have had at least one binge eating episode per week for a minimum of three months (1, 2).
The severity ranges from mild, which is characterized by one to three binge eating episodes per week, to extreme, which is characterized by 14 or more episodes per week (1, 2).
Another important characteristic is not taking action to “undo” a binge. This means that, unlike bulimia, a person with BED does not throw up, take laxatives, or over-exercise to try and counteract a binging episode.
Like other eating disorders, it’s more common in women than men. However, it’s more common among men than other types of eating disorders (17).
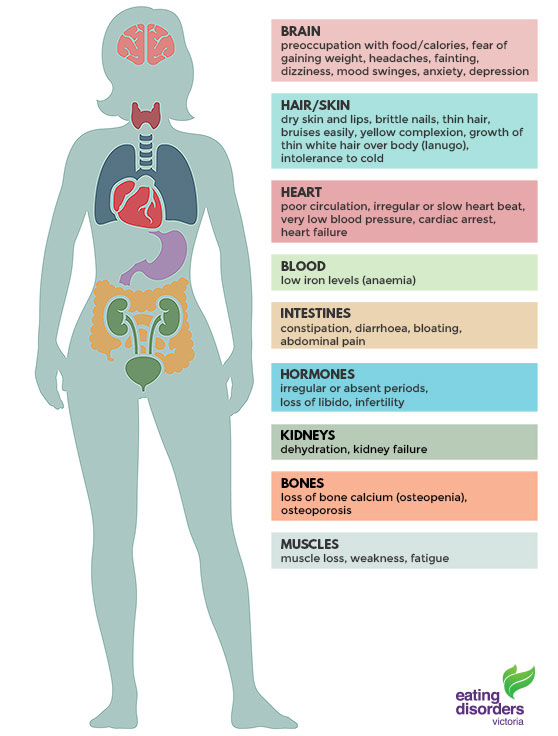
BED is associated with several significant physical, emotional, and social health risks.
Up to 50% of people with BED have obesity. However, the disorder is also an independent risk factor for gaining weight and developing obesity. This is due to the increased calorie intake during binging episodes (8).
On its own, obesity increases the risk of heart disease, stroke, type 2 diabetes, and cancer (18).
However, some studies have found that people with BED have an even greater risk of developing these health problems, compared with people with obesity of the same weight who don’t have BED (16, 18, 19).
Other health risks associated with BED include sleep problems, chronic pain conditions, asthma, and irritable bowel syndrome (IBS) (16, 17, 20).
In women, the condition is associated with a risk of fertility problems, pregnancy complications, and the development of polycystic ovary syndrome (PCOS) (20).
Research has shown that people with BED report challenges with social interactions, compared with people without the condition (21).
Additionally, people with BED have a high rate of hospitalization, outpatient care, and emergency department visits, compared with those who don’t have a feeding or eating disorder (22).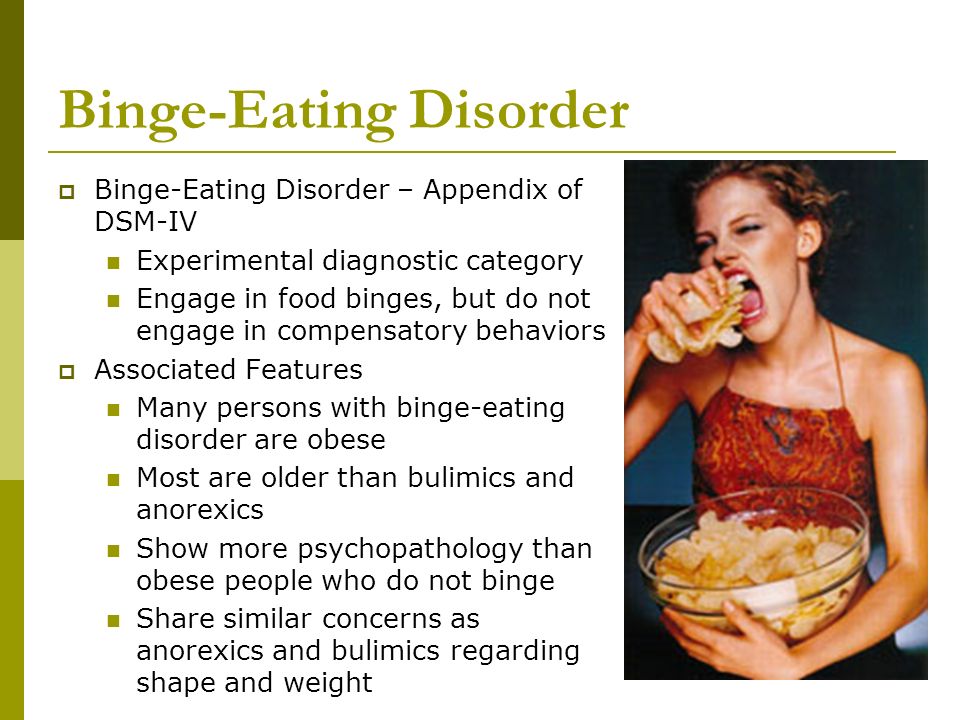
Although these health risks are significant, there are a number of effective treatments for BED.
SummaryBED is linked to an increased risk of weight gain and obesity, as well as associated diseases like diabetes and heart disease. There are also other health risks, including sleep problems, chronic pain, mental health problems, and reduced quality of life.
The treatment plan for BED depends on the causes and severity of the eating disorder, as well as individual goals.
Treatment may target binge eating behaviors, excess weight, body image, mental health issues, or a combination of these.
Therapy options include cognitive behavioral therapy, interpersonal psychotherapy, dialectical behavior therapy, weight loss therapy, and medication. These may be carried out on a one-to-one basis, in a group setting, or in a self-help format.
In some people, just one type of therapy may be required, while others may need to try different combinations until they find the right fit.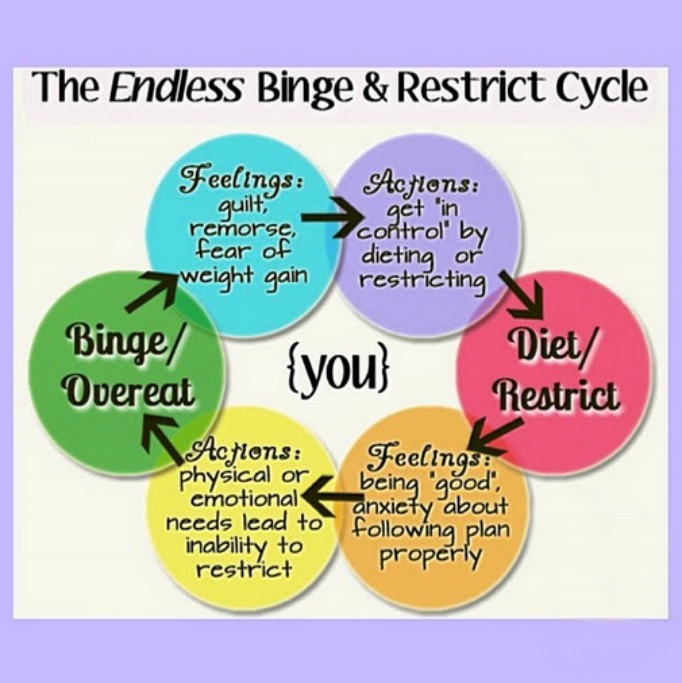
A medical or mental health professional can provide advice on selecting an individual treatment plan.
Cognitive behavioral therapy
Cognitive behavioral therapy (CBT) for BED focuses on analyzing the relationships between negative thoughts, feelings, and behaviors related to eating, body shape, and weight (2, 23).
Once the causes of negative emotions and patterns have been identified, strategies can be developed to help people change them (2).
Specific interventions include setting goals, self-monitoring, achieving regular meal patterns, changing thoughts about self and weight, and encouraging healthy weight-control habits (23).
Therapist-led CBT has been demonstrated to be the most effective treatment for people with BED. One study found that after 20 sessions of CBT, 79% of participants were no longer binge eating, with 59% of them still successful after one year (23).
Alternatively, guided self-help CBT is another option. In this format, participants are usually given a manual to work through on their own, along with the opportunity to attend some additional meetings with a therapist to help guide them and set goals (23).
The self-help form of therapy is often cheaper and more accessible, and there are websites and mobile apps that offer support. Self-help CBT has been shown to be an effective alternative to traditional CBT (24, 25).
SummaryCBT focuses on identifying the negative feelings and behaviors that cause binge eating and helps put strategies in place to improve them. It is the most effective treatment for BED and may be done with a therapist or in a self-help format.
Interpersonal psychotherapy
Interpersonal psychotherapy (IPT) is based on the idea that binge eating is a coping mechanism for unresolved personal problems such as grief, relationship conflicts, significant life changes, or underlying social problems (23).
The goal is to identify the specific problem linked to the negative eating behavior, acknowledge it, and then make constructive changes over 12–16 weeks (2, 26).
Therapy may either be in a group format or on a one-to-one basis with a trained therapist, and it may sometimes be combined with CBT.
There is strong evidence that this type of therapy has both short- and long-term positive effects on reducing binge eating behavior. It is the only other therapy with long-term outcomes as good as CBT (23).
It may be particularly effective for people with more severe forms of binge eating and those with lower self-esteem (23).
SummaryIPT views binge eating as a coping mechanism for underlying personal problems. It addresses binge eating behaviors by acknowledging and treating those underlying problems. It is a successful therapy, particularly for severe cases.
Dialectical behavior therapy
Dialectical behavior therapy (DBT) views binge eating as an emotional reaction to negative experiences that the person has no other way of coping with (23).
It teaches people to regulate their emotional responses so that they can cope with negative situations in daily life without binging (23).
The four key areas of treatment in DBT are mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness (23).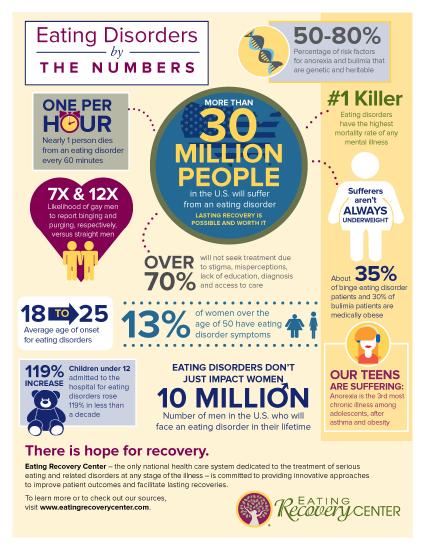
A study including 44 women with BED who underwent DBT showed that 89% of them stopped binge eating by the end of therapy, although this dropped to 56% by the 6-month follow-up (27).
However, there is limited information on the long-term effectiveness of DBT and how it compares with CBT and IPT.
While research on this treatment is promising, more studies are needed to determine if it could be applied to all people with BED.
SummaryDBT sees binge eating as a response to negative experiences in daily life. It uses techniques like mindfulness and the regulation of emotions to help people cope better and stop binging. It is unclear if it is effective in the long term.
Weight loss therapy
Behavioral weight loss therapy aims to help people lose weight, which may reduce binge eating behavior by improving self-esteem and body image.
The intent is to make gradual healthy lifestyle changes in regards to diet and exercise, as well as monitor food intake and thoughts about food throughout the day. Weight loss of about 1 pound (0.5 kg) per week is expected (23).
Weight loss of about 1 pound (0.5 kg) per week is expected (23).
While weight loss therapy may help improve body image and reduce weight and the health risks associated with obesity, it has not been shown to be as effective as CBT or IPT at stopping binge eating (23, 25, 28, 29).
As with regular weight loss treatment for obesity, behavioral weight loss therapy has been shown to help people achieve only short-term, moderate weight loss (25).
However, it may still be a good option for people who were not successful with other therapies or are primarily interested in losing weight (23).
SummaryWeight loss therapy aims to improve binge eating symptoms by reducing weight in hopes that this will improve body image. It is not as successful as CBT or interpersonal therapy, but it may be useful for some individuals.
Medications
Several medications have been found to treat binge eating and are often cheaper and faster than traditional therapy.
However, no current medications are as effective at treating BED as behavioral therapies.
Available treatments include antidepressants, antiepileptic drugs like topiramate, and drugs traditionally used for hyperactive disorders, such as lisdexamfetamine (2).
Research has found that medications have an advantage over a placebo for the short-term reduction of binge eating. Medications have been shown to be 48.7% effective, while placebos have been shown to be 28.5% effective (30).
They may also reduce appetite, obsessions, compulsions, and symptoms of depression (2).
Although these effects sound promising, most studies have been conducted over short periods, so data on the long-term effects is still needed (30).
In addition, side effects of treatment may including headaches, stomach problems, sleep disturbances, increased blood pressure, and anxiety (17).
Because many people with BED have other mental health conditions, such as anxiety and depression, they may also receive additional medications to treat these.
SummaryMedications may help improve binge eating in the short term. However, long-term studies are needed. Medications are generally not as effective as behavioral therapies and can have side effects.
The first step in overcoming binge eating is speaking to a medical professional. This person can help with a diagnosis, determine the severity of the disorder, and recommend the most appropriate treatment.
In general, the most effective treatment is CBT, but a range of treatments exists. Depending on individual circumstances, just one therapy or a combination may work best.
No matter which treatment strategy is used, it is important to also make healthy lifestyle and diet choices when possible.
Here are some additional helpful strategies:
- Keep a food and mood diary. Identifying personal triggers is an important step in learning how to control binge impulses.
- Practice mindfulness.
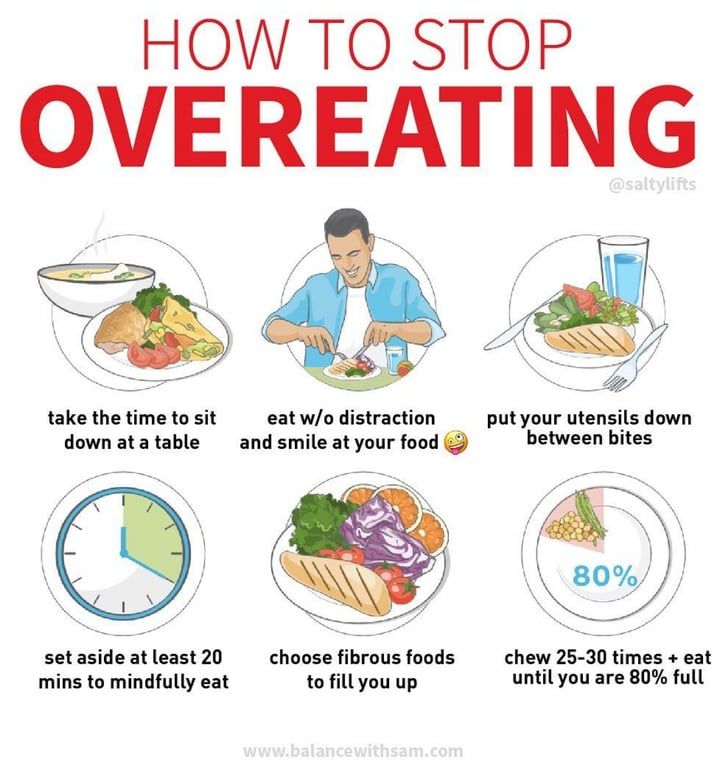 This can help increase awareness of binging triggers while helping increase self-control and maintaining self-acceptance (31, 32, 33).
This can help increase awareness of binging triggers while helping increase self-control and maintaining self-acceptance (31, 32, 33). - Find someone to talk to. It is important to have support, whether it is through a partner, family, a friend, binge eating support groups, or online (34).
- Choose healthy foods. A diet consisting of foods high in protein and healthy fats, regular meals, and whole foods will help satisfy hunger and provide needed nutrients.
- Start exercising. Exercise can help enhance weight loss, improve body image, reduce anxiety symptoms, and boost mood (35, 36).
- Get enough sleep. Lack of sleep is associated with higher calorie intake and irregular eating patterns. It’s recommended to get at least 7–8 hours of good sleep per night (37).
SummaryCBT and IPT are the best treatment options for BED. Other strategies include keeping a food and mood diary, practicing mindfulness, finding support, choosing healthy foods, exercising, and getting enough sleep.

BED is a common feeding and eating disorder that, if not treated, can seriously affect a person’s health.
It’s characterized by repeated, uncontrolled episodes of eating large amounts of food and often accompanied by feelings of shame and guilt.
It can have negative effects on overall health, body weight, self-esteem, and mental health.
Fortunately, very effective treatments are available for BED, including CBT and IPT. There are also many healthy lifestyle strategies that can be incorporated into everyday life.
The first step in overcoming BED is to ask for help from a medical professional.
Editor’s note: This piece was originally published on Dec. 16, 2017. Its current publication date reflects an update, which includes a medical review by Timothy J. Legg, PhD, PsyD.
Binge Eating Disorder: Symptoms, Causes, and Treatment
Binge eating disorder (BED) is a type of feeding and eating disorder that’s now recognized as an official diagnosis.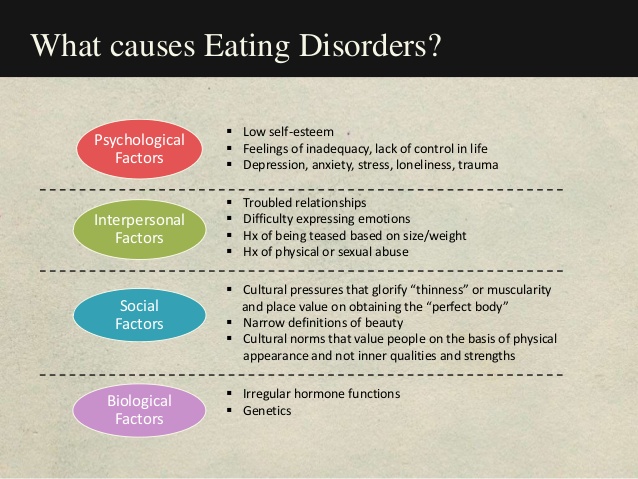 It affects almost 2% of people worldwide and can cause additional health issues linked to diet, such as high cholesterol levels and diabetes.
It affects almost 2% of people worldwide and can cause additional health issues linked to diet, such as high cholesterol levels and diabetes.
Feeding and eating disorders are not about food alone, which is why they’re recognized as psychiatric disorders. People typically develop them as a way of dealing with a deeper issue or another psychological condition, such as anxiety or depression.
This article looks at the symptoms, causes, and health risks of BED, as well as how to get help and support to overcome it.
People with BED may eat a lot of food in a short amount of time, even if they aren’t hungry. Emotional stress or destress often plays a role and might trigger a period of binge eating.
A person might feel a sense of release or relief during a binge but experience feelings of shame or loss of control afterward (1, 2).
For a healthcare professional to diagnose BED, three or more of the following symptoms must be present:
- eating much more rapidly than normal
- eating until uncomfortably full
- eating large amounts without feeling hungry
- eating alone due to feelings of embarrassment and shame
- feelings of guilt or disgust with oneself
People with BED often experience feelings of extreme unhappiness and distress about their overeating, body shape, and weight (1, 2, 3).
SummaryBED is characterized by repeated episodes of uncontrolled intake of unusually large amounts of food in a short period of time. These episodes are accompanied by feelings of guilt, shame, and psychological distress.
The causes of BED are not well understood but likely due to a variety of risk factors, including:
- Genetics. People with BED may have increased sensitivity to dopamine, a chemical in the brain that’s responsible for feelings of reward and pleasure. There is also strong evidence that the disorder is inherited (1, 4, 5, 6).
- Gender. BED is more common in women than in men. In the United States, 3.6% of women experience BED at some point in their lives, compared with 2.0% of men. This may be due to underlying biological factors (4, 7).
- Changes in the brain. There are indications that people with BED may have changes in brain structure that result in a heightened response to food and less self-control (4).

- Body size. Almost 50% of people with BED have obesity, and 25–50% of patients seeking weight loss surgery meet the criteria for BED. Weight problems may be both a cause and result of the disorder (5, 7, 8, 9).
- Body image. People with BED often have a very negative body image. Body dissatisfaction, dieting, and overeating contribute to the development of the disorder (10, 11, 12).
- Binge eating. Those affected often report a history of binge eating as the first symptom of the disorder. This includes binge eating in childhood and the teenage years (4).
- Emotional trauma. Stressful life events, such as abuse, death, separation from a family member, or a car accident, are risk factors. Childhood bullying due to weight may also contribute (13, 14, 15).
- Other psychological conditions. Almost 80% of people with BED have at least one other psychological disorder, such as phobias, depression, post-traumatic stress disorder (PTSD), bipolar disorder, anxiety, or substance abuse (1, 8).

An episode of binge eating can be triggered by stress, dieting, negative feelings relating to body weight or body shape, the availability of food, or boredom (1).
SummaryThe causes of BED are not fully known. As with other eating disorders, a variety of genetic, environmental, social, and psychological risks are associated with its development.
While some people may occasionally overeat, such as at Thanksgiving or a party, it does not mean they have BED, despite having experienced some of the symptoms listed above.
BED typically starts in the late teens to early twenties, although it can occur at any age. People generally need support to help overcome BED and develop a healthy relationship with food. If left untreated, BED can last for many years (16).
To be diagnosed, a person must have had at least one binge eating episode per week for a minimum of three months (1, 2).
The severity ranges from mild, which is characterized by one to three binge eating episodes per week, to extreme, which is characterized by 14 or more episodes per week (1, 2).
Another important characteristic is not taking action to “undo” a binge. This means that, unlike bulimia, a person with BED does not throw up, take laxatives, or over-exercise to try and counteract a binging episode.
Like other eating disorders, it’s more common in women than men. However, it’s more common among men than other types of eating disorders (17).
BED is associated with several significant physical, emotional, and social health risks.
Up to 50% of people with BED have obesity. However, the disorder is also an independent risk factor for gaining weight and developing obesity. This is due to the increased calorie intake during binging episodes (8).
On its own, obesity increases the risk of heart disease, stroke, type 2 diabetes, and cancer (18).
However, some studies have found that people with BED have an even greater risk of developing these health problems, compared with people with obesity of the same weight who don’t have BED (16, 18, 19).
Other health risks associated with BED include sleep problems, chronic pain conditions, asthma, and irritable bowel syndrome (IBS) (16, 17, 20).
In women, the condition is associated with a risk of fertility problems, pregnancy complications, and the development of polycystic ovary syndrome (PCOS) (20).
Research has shown that people with BED report challenges with social interactions, compared with people without the condition (21).
Additionally, people with BED have a high rate of hospitalization, outpatient care, and emergency department visits, compared with those who don’t have a feeding or eating disorder (22).
Although these health risks are significant, there are a number of effective treatments for BED.
SummaryBED is linked to an increased risk of weight gain and obesity, as well as associated diseases like diabetes and heart disease. There are also other health risks, including sleep problems, chronic pain, mental health problems, and reduced quality of life.
The treatment plan for BED depends on the causes and severity of the eating disorder, as well as individual goals.
Treatment may target binge eating behaviors, excess weight, body image, mental health issues, or a combination of these.
Therapy options include cognitive behavioral therapy, interpersonal psychotherapy, dialectical behavior therapy, weight loss therapy, and medication. These may be carried out on a one-to-one basis, in a group setting, or in a self-help format.
In some people, just one type of therapy may be required, while others may need to try different combinations until they find the right fit.
A medical or mental health professional can provide advice on selecting an individual treatment plan.
Cognitive behavioral therapy
Cognitive behavioral therapy (CBT) for BED focuses on analyzing the relationships between negative thoughts, feelings, and behaviors related to eating, body shape, and weight (2, 23).
Once the causes of negative emotions and patterns have been identified, strategies can be developed to help people change them (2).
Specific interventions include setting goals, self-monitoring, achieving regular meal patterns, changing thoughts about self and weight, and encouraging healthy weight-control habits (23).
Therapist-led CBT has been demonstrated to be the most effective treatment for people with BED. One study found that after 20 sessions of CBT, 79% of participants were no longer binge eating, with 59% of them still successful after one year (23).
Alternatively, guided self-help CBT is another option. In this format, participants are usually given a manual to work through on their own, along with the opportunity to attend some additional meetings with a therapist to help guide them and set goals (23).
The self-help form of therapy is often cheaper and more accessible, and there are websites and mobile apps that offer support. Self-help CBT has been shown to be an effective alternative to traditional CBT (24, 25).
SummaryCBT focuses on identifying the negative feelings and behaviors that cause binge eating and helps put strategies in place to improve them.
It is the most effective treatment for BED and may be done with a therapist or in a self-help format.
Interpersonal psychotherapy
Interpersonal psychotherapy (IPT) is based on the idea that binge eating is a coping mechanism for unresolved personal problems such as grief, relationship conflicts, significant life changes, or underlying social problems (23).
The goal is to identify the specific problem linked to the negative eating behavior, acknowledge it, and then make constructive changes over 12–16 weeks (2, 26).
Therapy may either be in a group format or on a one-to-one basis with a trained therapist, and it may sometimes be combined with CBT.
There is strong evidence that this type of therapy has both short- and long-term positive effects on reducing binge eating behavior. It is the only other therapy with long-term outcomes as good as CBT (23).
It may be particularly effective for people with more severe forms of binge eating and those with lower self-esteem (23).
SummaryIPT views binge eating as a coping mechanism for underlying personal problems. It addresses binge eating behaviors by acknowledging and treating those underlying problems. It is a successful therapy, particularly for severe cases.
Dialectical behavior therapy
Dialectical behavior therapy (DBT) views binge eating as an emotional reaction to negative experiences that the person has no other way of coping with (23).
It teaches people to regulate their emotional responses so that they can cope with negative situations in daily life without binging (23).
The four key areas of treatment in DBT are mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness (23).
A study including 44 women with BED who underwent DBT showed that 89% of them stopped binge eating by the end of therapy, although this dropped to 56% by the 6-month follow-up (27).
However, there is limited information on the long-term effectiveness of DBT and how it compares with CBT and IPT.
While research on this treatment is promising, more studies are needed to determine if it could be applied to all people with BED.
SummaryDBT sees binge eating as a response to negative experiences in daily life. It uses techniques like mindfulness and the regulation of emotions to help people cope better and stop binging. It is unclear if it is effective in the long term.
Weight loss therapy
Behavioral weight loss therapy aims to help people lose weight, which may reduce binge eating behavior by improving self-esteem and body image.
The intent is to make gradual healthy lifestyle changes in regards to diet and exercise, as well as monitor food intake and thoughts about food throughout the day. Weight loss of about 1 pound (0.5 kg) per week is expected (23).
While weight loss therapy may help improve body image and reduce weight and the health risks associated with obesity, it has not been shown to be as effective as CBT or IPT at stopping binge eating (23, 25, 28, 29).
As with regular weight loss treatment for obesity, behavioral weight loss therapy has been shown to help people achieve only short-term, moderate weight loss (25).
However, it may still be a good option for people who were not successful with other therapies or are primarily interested in losing weight (23).
SummaryWeight loss therapy aims to improve binge eating symptoms by reducing weight in hopes that this will improve body image. It is not as successful as CBT or interpersonal therapy, but it may be useful for some individuals.
Medications
Several medications have been found to treat binge eating and are often cheaper and faster than traditional therapy.
However, no current medications are as effective at treating BED as behavioral therapies.
Available treatments include antidepressants, antiepileptic drugs like topiramate, and drugs traditionally used for hyperactive disorders, such as lisdexamfetamine (2).
Research has found that medications have an advantage over a placebo for the short-term reduction of binge eating. Medications have been shown to be 48.7% effective, while placebos have been shown to be 28.5% effective (30).
They may also reduce appetite, obsessions, compulsions, and symptoms of depression (2).
Although these effects sound promising, most studies have been conducted over short periods, so data on the long-term effects is still needed (30).
In addition, side effects of treatment may including headaches, stomach problems, sleep disturbances, increased blood pressure, and anxiety (17).
Because many people with BED have other mental health conditions, such as anxiety and depression, they may also receive additional medications to treat these.
SummaryMedications may help improve binge eating in the short term. However, long-term studies are needed. Medications are generally not as effective as behavioral therapies and can have side effects.
-Step-1.jpg/aid12430596-v4-728px-Treat-B.E.D.-(Binge-Eating-Disorder)-Step-1.jpg)
The first step in overcoming binge eating is speaking to a medical professional. This person can help with a diagnosis, determine the severity of the disorder, and recommend the most appropriate treatment.
In general, the most effective treatment is CBT, but a range of treatments exists. Depending on individual circumstances, just one therapy or a combination may work best.
No matter which treatment strategy is used, it is important to also make healthy lifestyle and diet choices when possible.
Here are some additional helpful strategies:
- Keep a food and mood diary. Identifying personal triggers is an important step in learning how to control binge impulses.
- Practice mindfulness. This can help increase awareness of binging triggers while helping increase self-control and maintaining self-acceptance (31, 32, 33).
- Find someone to talk to. It is important to have support, whether it is through a partner, family, a friend, binge eating support groups, or online (34).
- Choose healthy foods. A diet consisting of foods high in protein and healthy fats, regular meals, and whole foods will help satisfy hunger and provide needed nutrients.
- Start exercising. Exercise can help enhance weight loss, improve body image, reduce anxiety symptoms, and boost mood (35, 36).
- Get enough sleep. Lack of sleep is associated with higher calorie intake and irregular eating patterns. It’s recommended to get at least 7–8 hours of good sleep per night (37).
SummaryCBT and IPT are the best treatment options for BED. Other strategies include keeping a food and mood diary, practicing mindfulness, finding support, choosing healthy foods, exercising, and getting enough sleep.
BED is a common feeding and eating disorder that, if not treated, can seriously affect a person’s health.
It’s characterized by repeated, uncontrolled episodes of eating large amounts of food and often accompanied by feelings of shame and guilt.
It can have negative effects on overall health, body weight, self-esteem, and mental health.
Fortunately, very effective treatments are available for BED, including CBT and IPT. There are also many healthy lifestyle strategies that can be incorporated into everyday life.
The first step in overcoming BED is to ask for help from a medical professional.
Editor’s note: This piece was originally published on Dec. 16, 2017. Its current publication date reflects an update, which includes a medical review by Timothy J. Legg, PhD, PsyD.
Medical treatment of compulsive overeating by a psychologist, treat the disease by a psychotherapist
Sometimes it happens that delicious food, appetizing appearance of dishes cause a person to get up from the table with a feeling of a full stomach. If such situations occur rarely, overeating can be controlled, then there is nothing to worry about. If we are talking about causeless and uncontrolled appetite, which is preceded by stress or negative emotions, then we can suspect a dangerous eating disorder - compulsive or uncontrolled overeating.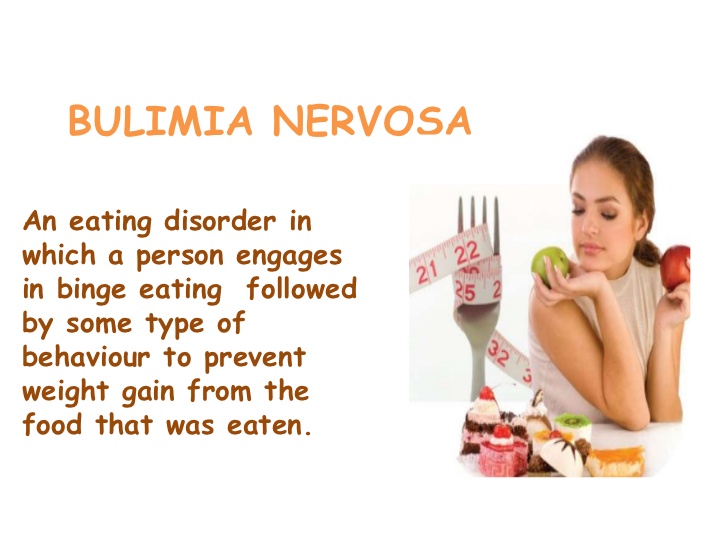 It is important not to miss the moment and turn to a psychotherapist in time. nine0003
It is important not to miss the moment and turn to a psychotherapist in time. nine0003
Article content:
- Disease description
- Causes
- Psychological aspect of the problem
- Methods of psychotherapy in the treatment of illness
- Possible complications
Seek medical attention if symptoms occur. The information on the page is for reference only and cannot be used for self-diagnosis and self-treatment.
Description of disease
Compulsive overeating (CP) is a dangerous pathological condition. The patient is unable to control his appetite due to stress. The essence and nature of a compulsive disease is well explained by its second name - psychogenic overeating, since the causes of the development of an eating disorder should be sought not in the physiological, but in the mental sphere.
Any stressful situation can provoke a painful condition: the loss of a loved one, the loss of keys, a conversation with superiors in a raised tone, and other unpleasant situations.
nine0003
Bouts of psychogenic overeating may recur from time to time. As with other eating disorders, the patient considers himself healthy. The exception is excess weight, which accompanies psychogenic overeating. Uncontrolled appetite has clear differences from other diseases of a food nature:
- if with anorexia the patient ceases to adequately perceive his own body, then with compulsive overeating the problem of excess weight becomes obvious and is the root cause of contacting a psychologist, psychotherapist, other doctors; nine0010
- The binge patient usually does not seek to get rid of food by inducing artificial vomiting, while the symptoms of bulimia are characterized by obligatory cleansing procedures, which the patient cannot refuse.
Causes
It is a normal physiological need to eat exactly when the feeling of hunger arises. If food intake is reduced to nervous chewing, no attention is paid to the amount eaten, it is worth considering that it is bulimia or uncontrolled overeating that can cause increased weight, the appearance of extra centimeters in volume. nine0003
nine0003
Physiological factors can provoke compulsive overeating - dysfunction of the hypothalamus and genetic predisposition. Genetic scientists have identified three genes whose presence in the genetic code leads to obesity and can provoke the development of an eating disorder.
The psychological aspect of the problem of psychogenic overeating
Physiological and genetic causes may be a consequence of the development of an eating disorder, but the psyche plays a central role. nine0003
Leading psychotherapists in the description of clinical cases of compulsive overeating note that the onset of the disease is preceded by negative life events. Such stress can be caused by social and physiological factors.
To understand whether you have a problem, whether you need the help of a psychotherapist, you should honestly answer a number of questions.
- Have you noticed that your diet is difficult to control? nine0009 all your thoughts are related to food?
- Do you prefer to eat alone?
- Do you tend to overeat when stressed out, distracted from current problems?
- Do you experience guilt that affects your enjoyment of eating?
- How often do you start eating without feeling hungry?
- Do you find it difficult to refuse food if you are treated?
If you answered yes to 4 or more questions, it makes sense to contact a medical institution for advice and clarification of the causes of the food problems that have arisen. nine0003
nine0003
Methods of psychotherapy in the treatment of illness
The solution in the fight against food addiction is to seek help from a specialist. Only a psychologist is able to help find the causes of binge eating disorder and form a healthy model of dealing with stress.
The Center for the Study of Eating Disorders uses the latest psychotherapy techniques accepted in the international medical community.
Depending on the severity of the condition, a treatment algorithm is selected. It can be done on an outpatient or inpatient basis under the supervision of a psychotherapist. The following areas of psychotherapy are used to treat patients with compulsive psychogenic overeating, bulimia, anorexia and other eating disorders:
- CBT - cognitive behavioral therapy;
- DBT - Dialectical Behavioral Psychotherapy;
- FBT - Family Involved Therapy.
All methods have scientifically proven effectiveness, are actively used in practice by psychotherapists and other doctors of "CIRPP" in the fight against overeating.
Family Therapy
Successful Family Psychological Therapy, which was developed for the treatment of patients with eating disorders by the leading specialists of the Maudsley Clinic. nine0003
A multi-family group has been organized in CIRP, where not only patients, but also their relatives, as co-dependent persons, receive therapy. In the course of group therapy, the psychotherapist helps to jointly develop the right adaptation tactics, build the right behavior model, and provides the necessary support to parents whose children suffer from eating disorders.
Cognitive behavioral therapy
The program is aimed at finding the causes of eating disorders (bulimia, anorexia, compulsive uncontrolled overeating, etc.). It is important to find out the root cause of the disease, this will help in choosing the right tactics. nine0003
DBT - Dialectical Behavior Therapy
The use of Dialectical Behavior Therapy has a positive effect in the treatment of patients with compulsive overeating.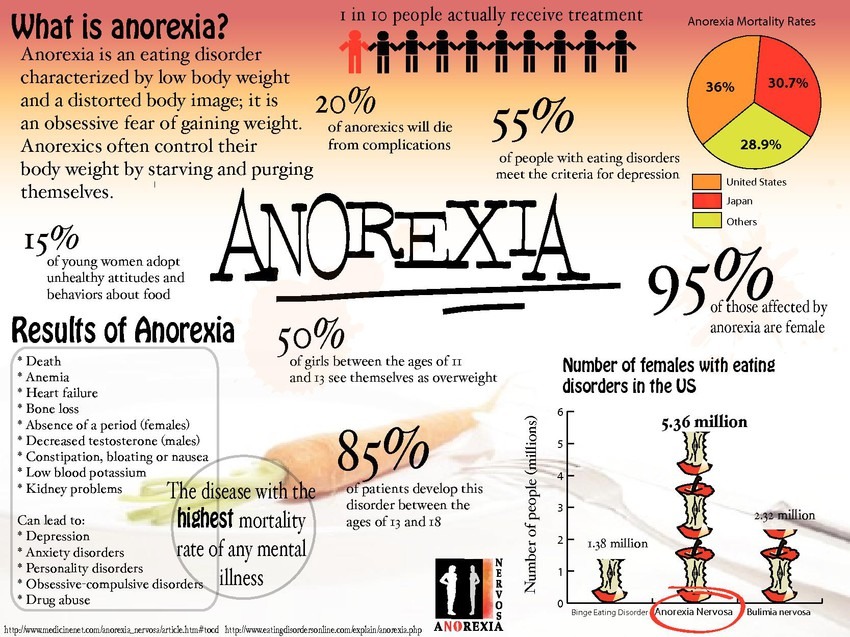 The method is aimed at finding new ways to deal with stress, teaching effective emotional regulation techniques that are not related to eating or deliberately refusing it.
The method is aimed at finding new ways to deal with stress, teaching effective emotional regulation techniques that are not related to eating or deliberately refusing it.
At the end of the treatment phase, the patient will be able to painlessly give up destructive ways of dealing with stress, strict weight control and dietary regimens. Bouts of uncontrolled overeating will be left behind. nine0003
Psychologists "CIRPP" use the latest methods of work with people suffering from eating disorders, psychogenic overeating. In addition to providing basic medical care, resuscitation, developing an individual diet, the DBT program includes the work of online psychotherapy groups, art therapy, dance therapy led by a psychotherapist, and other eating behavior adjustment programs.
Possible complications
Delayed treatment of eating disorders can adversely affect the condition of a patient suffering from regular overeating. If there is no treatment, then there is a high probability of developing other complications:
- decrease or increase in blood pressure;
- aggressive or lethargic behaviour;
- metabolic disorder;
- obesity;
- depression;
- alcohol or drug addiction; nine0010
- diseases of the cardiovascular system;
- type 2 diabetes and others.
Gradually, complications can become chronic, which reduces the chances of a full recovery. It is not difficult to avoid such a scenario - it is enough to be attentive to your own health, pay attention to alarming symptoms and consult a doctor in time.
Getting help from a psychologist, nutritionist or psychotherapist is easy: sign up for an initial medical consultation by calling +7(499) 703-20-51 or through the online form.
Author: Maksim Borisovich Sologub
Head Physician of TsIRPP,
psychiatrist, psychotherapist.
How to deal with compulsive overeating - Here and Now
Author of the article: Alexandra Igorevna Naumenko Family psychologist, child psychologist.
Practical experience: 8 years.
Are you upset about something, feeling lonely and insecure? As a result, you return home, open the refrigerator and choose what to eat (certainly something that does not fit into the framework of a healthy diet). The choice stops at your favorite biscuit cake - exactly what you need. A couple of bites and you'll feel happy again. You eat the first and then the second piece with pleasure, and after only 15 minutes only crumbs remain from the cake. A feeling of guilt covers you: another breakdown, you feel bad and ashamed of yourself. But nothing! Another hard day is left behind, tomorrow you will certainly go on a diet and you will be able to overcome overeating forever. nine0003
The choice stops at your favorite biscuit cake - exactly what you need. A couple of bites and you'll feel happy again. You eat the first and then the second piece with pleasure, and after only 15 minutes only crumbs remain from the cake. A feeling of guilt covers you: another breakdown, you feel bad and ashamed of yourself. But nothing! Another hard day is left behind, tomorrow you will certainly go on a diet and you will be able to overcome overeating forever. nine0003
Half an hour later you are still feeling mental and physical discomfort from having eaten too much, but against all odds you are back in the kitchen. And the situation repeats itself. Feelings of guilt, shame, feeling unwell are covered with renewed vigor, and in a fit of emotions you throw away all the food - this will not happen again. However, after just a couple of minutes you are about to go to the store...
Causes and symptoms of compulsive overeating
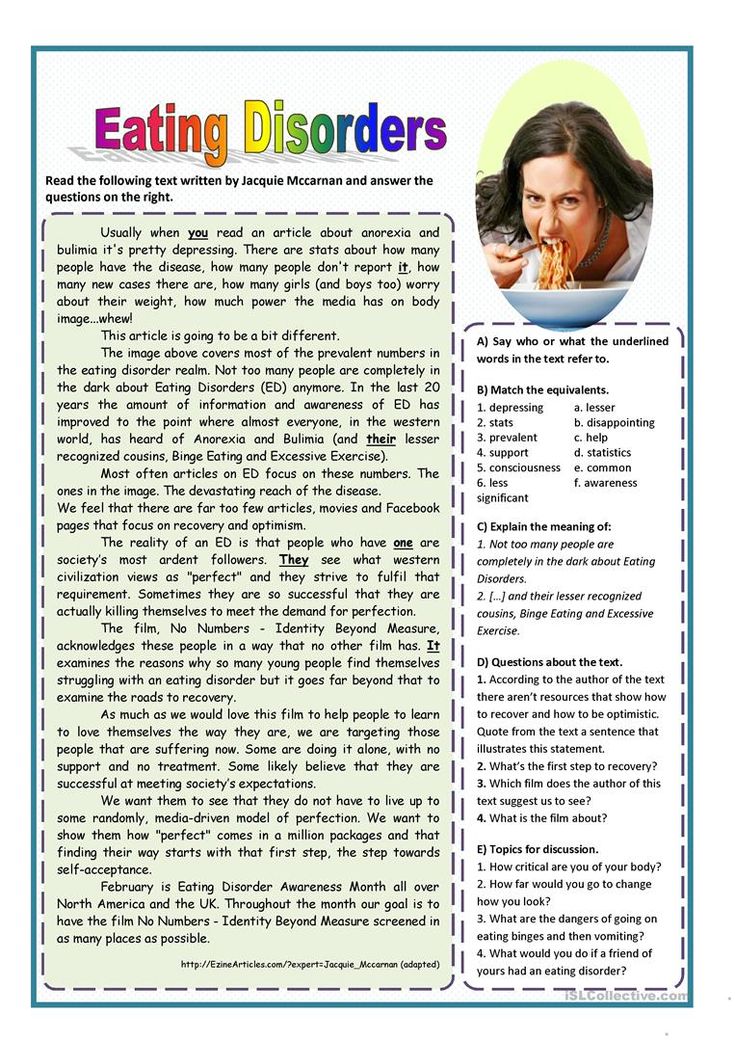
Compulsive overeating is an eating disorder, expressed in the uncontrolled absorption of large amounts of food, despite the moral and physical discomfort experienced. At the same time, it is important not to confuse episodic overeating with compulsive overeating - these are two completely different concepts. If overeating occurs only during a festive feast or rare meetings with friends, it is more likely a lack of discipline in eating behavior - a problem that can be solved with the help of self-control. But attacks of compulsive overeating require the adoption of a whole range of measures: changing both eating habits and the whole lifestyle in general, working with a psychologist. Often, the psychosomatics of overeating is laid down in childhood, which is why it is so difficult for adults to get rid of bad eating habits. nine0003
At the same time, it is important not to confuse episodic overeating with compulsive overeating - these are two completely different concepts. If overeating occurs only during a festive feast or rare meetings with friends, it is more likely a lack of discipline in eating behavior - a problem that can be solved with the help of self-control. But attacks of compulsive overeating require the adoption of a whole range of measures: changing both eating habits and the whole lifestyle in general, working with a psychologist. Often, the psychosomatics of overeating is laid down in childhood, which is why it is so difficult for adults to get rid of bad eating habits. nine0003
Characteristic features of this type of disorder are:
- obsessive thoughts about food;
- feeling of guilt during and after eating;
- disgust for oneself and one's own body;
- eating when not physically hungry;
- continued eating despite physical discomfort;
- high eating rate;
- a combination of absolutely incongruous products and dishes; nine0010
- habit of hiding food;
- frequent meals alone, the desire to hide it from others;
- the absorption of food becomes a reaction to stress, conflict situations and resentment.

If you do not start to fight compulsive overeating in time, it can be fraught with the following complications:
- hypertension;
- hormonal imbalance;
- thromboembolism;
- metabolic syndrome; nine0010
- obesity;
- weak immunity;
- high blood sugar;
- diabetes mellitus;
- cardiovascular diseases.
Compulsive overeating: how to deal with it
Until a “magic pill” was invented that would help solve the problem of overeating once and for all. Dealing with an eating disorder takes time, willpower, and professional help. Among the actions you should take:
- recognize the problem - if you convince yourself that your behavior is absolutely normal, then getting rid of addiction is out of the question;
- find the problem you are trying to seize. Only a deep and clear understanding of the desires that form at the unconscious level will help get rid of overeating;
- stop forbidding yourself anything - do not divide food into “possible” and “impossible”.
 Ultimatums will only harm those who are looking for a way to stop compulsive overeating. Understand: food is not going anywhere from you, it is available at any time. You don't have to eat it unless you're hungry; nine0010
Ultimatums will only harm those who are looking for a way to stop compulsive overeating. Understand: food is not going anywhere from you, it is available at any time. You don't have to eat it unless you're hungry; nine0010 - learn to distinguish between physical and psychological hunger. Physical hunger is accompanied by physical discomfort: rumbling in the stomach, loss of strength, etc. If you feel full, but want to eat something simply because of boredom or loneliness, this is psychological hunger;
- do not drive yourself into the framework of diets and strict nutrition. Often, it is the abuse of diets that becomes fertile ground for the development of compulsive overeating;
- seek professional help - a psychologist will help you understand the cause of overeating and tell you how to cope with overeating. nine0010
Compulsive overeating: treatment
Do not put off solving the problem until later, as this will lead not only to a deterioration in appearance, but also to a negative impact on health.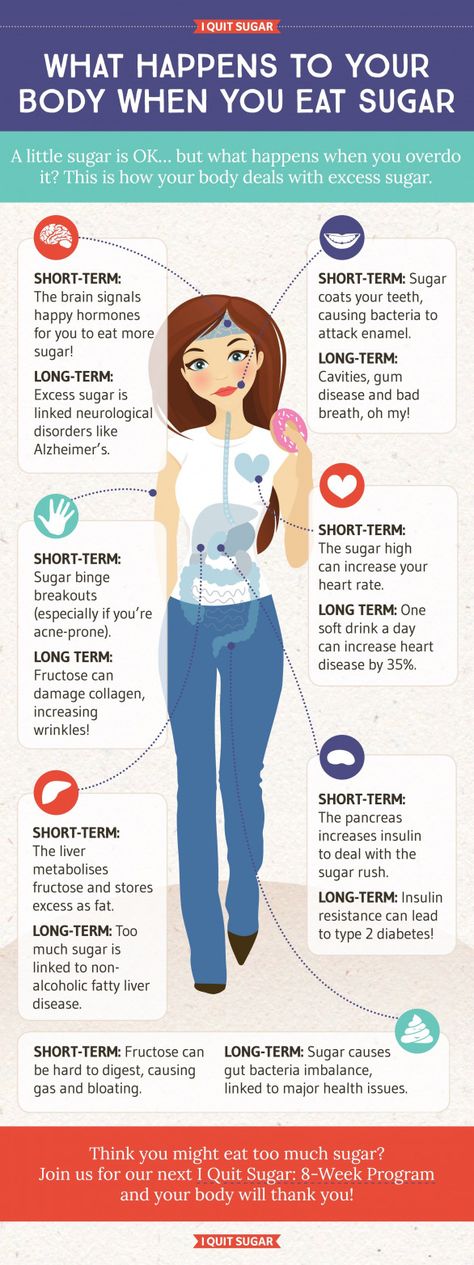 This type of eating disorder can be successfully treated, but only with competent and timely intervention. Working with a psychotherapist will allow you to cope with systematic overeating, say goodbye to bad habits and develop new healthy ones.
This type of eating disorder can be successfully treated, but only with competent and timely intervention. Working with a psychotherapist will allow you to cope with systematic overeating, say goodbye to bad habits and develop new healthy ones.
In the treatment of compulsive overeating, psychotherapists of the Center for Harmony of Soul and Body "Here and Now" use the following types of therapy:
- cognitive - each of the sessions is aimed at solving the problems that caused the development of the disease. Gradually, the patient gains control over his behavior and desires, avoids risk factors;
- behavioral - therapy is aimed at combating the negative perception of one's own body, increasing self-esteem, developing communication skills and solving problems in relationships with others; nine0010
- group therapy is relevant if the cause of overeating lies in insufficient socialization (the patient is dependent on the opinions of others), and its main task is to relieve emotional and nervous tension through communication with people suffering from a similar disorder;
- art therapy - allows patients to throw out their feelings and emotions and visually see what is happening to them.