What is impulsive adhd
ADHD Hyperactive-Impulsive Type: Symptoms, Causes, and Treatment
Written by Stephanie Watson
In this Article
- Signs of Hyperactive-Impulsive ADHD
- Inattentive ADHD
- What Causes Hyperactive-Impulsive ADHD?
- ADHD Treatments
Your child can't sit still. They are talking a mile a minute. Are they just a high-energy kid? Or do they have ADHD?
Hyperactivity is just one sign of ADHD. Kids who have it seem to always be on the move.
Kids who are hyperactive also tend to be impulsive. They may interrupt conversations. They may play out of turn.
Adults can also have this type of ADHD, called hyperactive-impulsive. But it’s less common because hyperactivity tends to lessen with age.
So how do you know whether your child has hyperactive-impulsive ADHD? And if your child does, what treatments can help?
Signs of Hyperactive-Impulsive ADHD
No single test can confirm that your child has this type of ADHD. Your doctor will first try to rule out other things that can cause hyperactivity. It could be stress or emotional issues. The behavior might simply be appropriate for their age. Sometimes vision problems or learning disabilities can make it hard for a child to sit still.
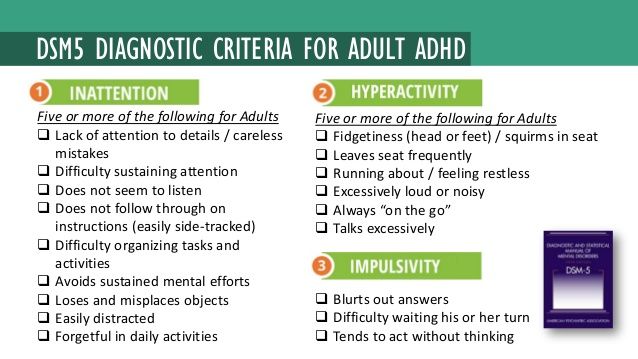
The doctor will also look for at least six of these symptoms of hyperactivity and impulsivity:
- Fidgeting or squirming (not being able to sit still)
- Nonstop talking
- Trouble sitting still and doing quiet tasks, such as reading
- Running from place to place; acting like they are driven by a motor
- Constantly leaving their seat, jumping or climbing on furniture and other inappropriate places
- Not having patience
- Blurting out comments at inappropriate times
- Interrupting conversations or speaking out of turn
- Trouble waiting for a turn or standing in line
Many children who like to run and jump may be high-energy. But that doesn’t mean they are hyperactive.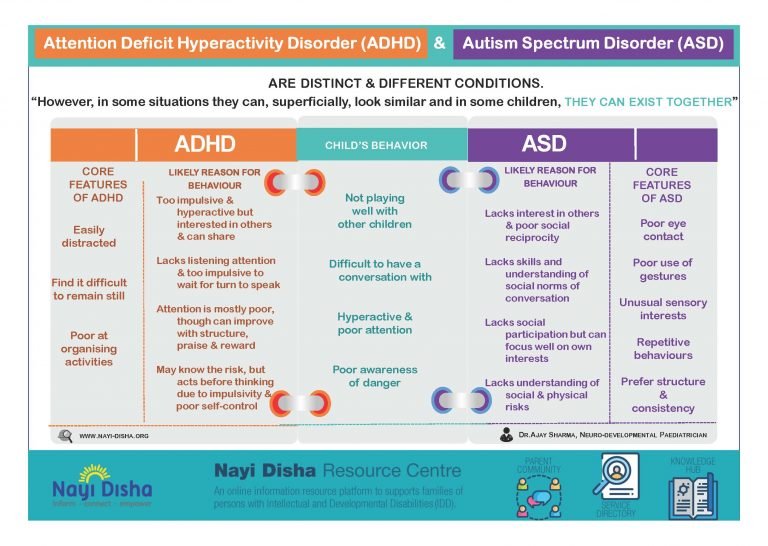 To count as ADHD, symptoms have to be on the extreme side and have to cause problems in the child’s life. Also, they have to have been doing this for at least 6 months.
To count as ADHD, symptoms have to be on the extreme side and have to cause problems in the child’s life. Also, they have to have been doing this for at least 6 months.
Inattentive ADHD
There is another type of ADHD called inattentive ADHD. Children who have inattentive ADHD have trouble focusing. They are also easily distracted.
A child with hyperactive-impulsive ADHD may not always show many signs of inattention. They may not necessarily have trouble focusing or becoming easily distracted.
But many kids have a combination of hyperactive-impulsive and inattentive ADHD (called the "combined type"). They may be always on the go and have trouble focusing.
What Causes Hyperactive-Impulsive ADHD?
The causes of ADHD aren't clear. Scientists say it is due in large part to genes that are passed down from parent to child. But experts aren't sure yet which specific genes make it more likely to get ADHD. A child is more likely to have ADHD if a close family member has it.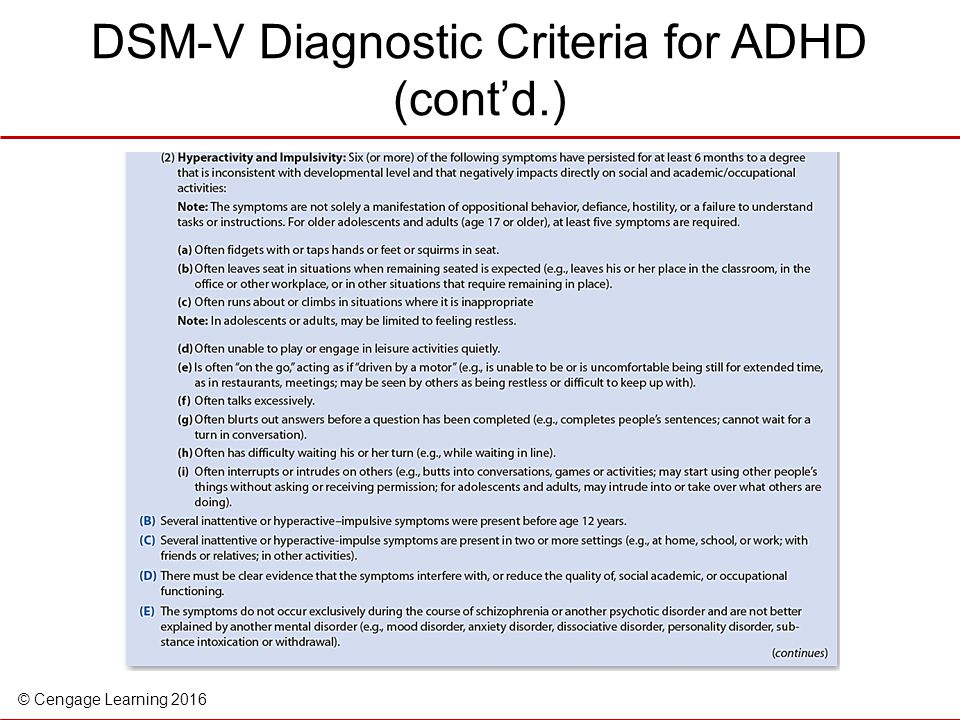
Other things that may influence ADHD risk include:
- Cigarette smoking and alcohol use during pregnancy
- Being born premature
- Low birth weight
- Being exposed to lead during early childhood
- Brain injuries
Many parents claim sugar makes their child hyperactive. But there is no evidence that refined sugar causes ADHD or makes it worse.
There may be a link between ADHD and food additives such as artificial colors and preservatives. But that has not been confirmed.
ADHD Treatments
Once your child is diagnosed with hyperactive-impulsive ADHD, the next step is to treat it. Every child’s treatment plan can be different. Sometimes it takes trying a few things to find the right one.
ADHD treatment usually starts with medication. A few ADHD medicines are available.
Stimulant drugs. Despite their name, stimulant drugs don’t rev up or excite kids with ADHD. They calm them down. These medications include:
They come in different forms, including:
- Pills (tablets and chewables)
- Capsules
- Liquids
- Skin patches
No stimulant has been proven to work better than others.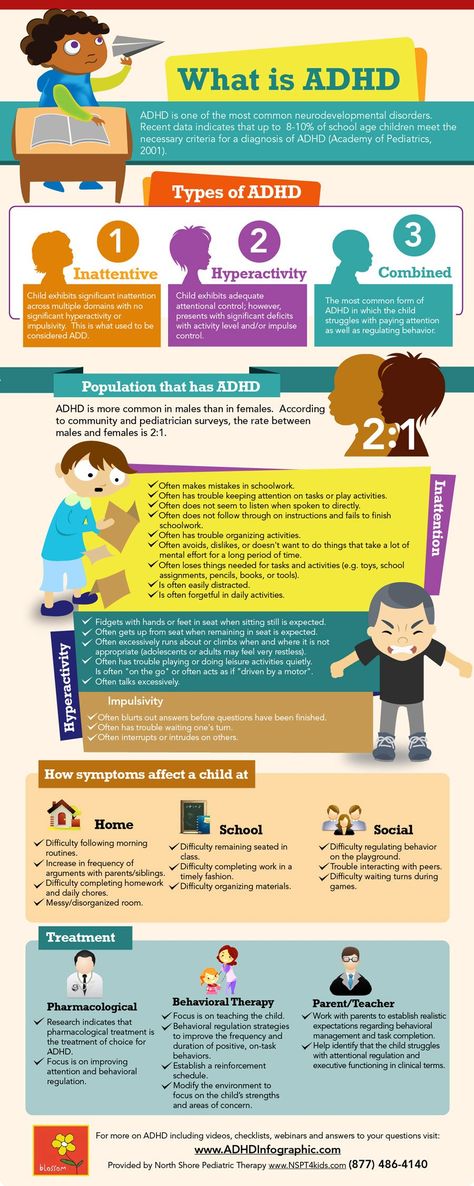 Each child responds differently to these medicines.
Each child responds differently to these medicines.
Nonstimulant drugs. Although nonstimulant medicines may not work as well as stimulants, they have fewer side effects. This type of medication includes:
High blood pressure medicines are another choice. These drugs can help control impulsivity and hyperactivity symptoms.
- Clonidine (Catapres, Kapvay)
- Guanfacine (Intuniv, Tenex )
Antidepressants. Drugs that affect mood, including bupropion (Wellbutrin), can sometimes help with ADHD symptoms.
Often, a child will need a combination of medicine and other treatments. You may need to work with your doctor to adjust the medicine as your child's symptoms change.
Parents and pediatricians should watch carefully for side effects from medicine. Common ADHD stimulant drug side effects include:
- Loss of appetite
- Weight loss
- Slowed growth
- Disrupted sleep
- Irritability
- Tics
- Anxiety
Stimulant medications have also been linked to more serious side effects, including:
- Heart problems
- Psychiatric problems (such as hallucinations or hearing voices)
Strattera and antidepressant medications also may cause suicidal thoughts in children and teenagers.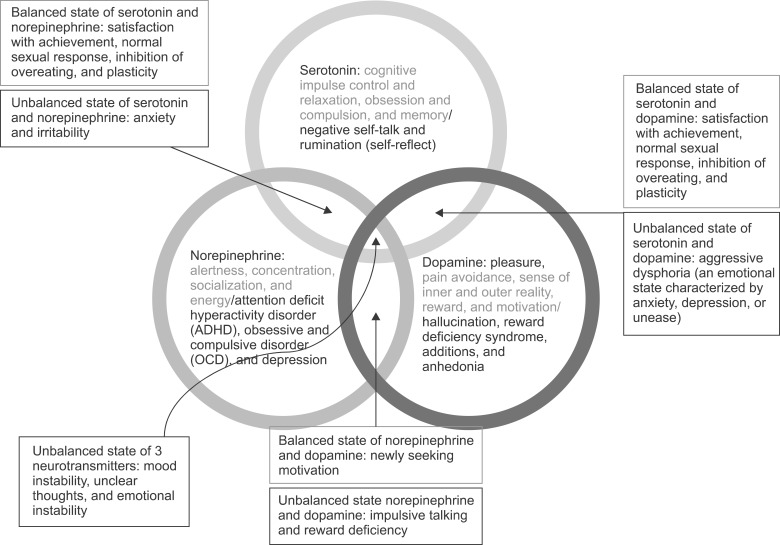
Because of these rare risks, it's important to call your doctor right away if you notice any unusual symptoms in your child. While taking these medicines, kids should have the following carefully checked:
- Height
- Weight
- Blood pressure
- Heart rate
Along with medicine, behavior therapy can help with hyperactivity. A psychologist or therapist can help kids with ADHD learn how to spot and control their hyperactive and impulsive behaviors.
Kids can learn how to create and follow routines. They can also work to improve their social skills. Parents and teachers can use a system of rewards and consequences to reinforce good behaviors.
Here’s What ADHD Impulsivity Is Like
Everyone has a story about That Kid in School from their childhood, right?
Whether it was eating paste, arguing with the teacher, or some manner of a Lovecraftian bathroom nightmare scenario, That Kid in School had scene-stealing outbursts on lock. Sometimes, we all wonder what happened to them, what they’re doing now.
Unless, like me, *you* were That Kid in School because you had impulse control issues from untreated ADHD.
Impulsivity, in the clinical sense, can be neatly defined as “action without foresight.”
I would speak without raising my hand, interrupt the class with emotional outbursts, and get out of my desk so often I’m surprised the use of duct tape was never bandied around the teacher’s lounge.
I would get asked why I was doing any of it and I never had a clear answer — even to myself. I didn’t like drawing that bad sort of attention to myself. It was humiliating.
It’s funny how often suffering in children gets them labelled as merely troublemakers. Part of this is shame-based masking in kids because they’ll do anything to deny they’re different, and part of it is how our school systems aren’t adequately equipped to recognize or act on these circumstances that are ultimately health issues.
But this is a column on ADHD and not on how we’re systemically failing our young people, so let’s keep it pushing!
Let’s go ahead and do our inventory of “jerk-type” behavior.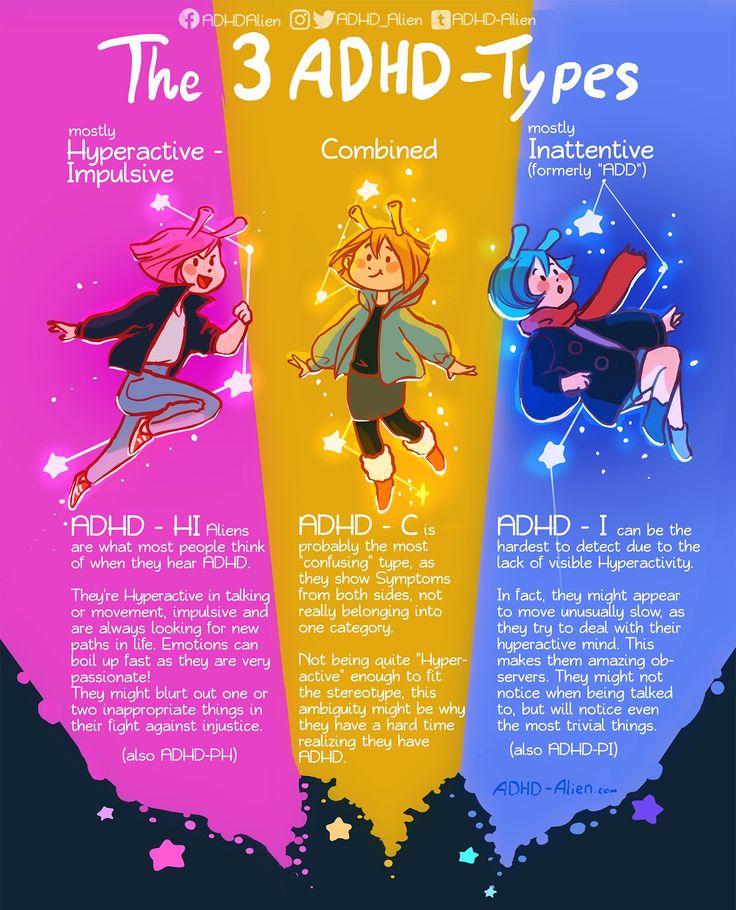
I was an impulsive child and I am a slightly less impulsive adult. We all have our moments of it, but for me it can feel like a dozen controllers are all in charge of my brain at once and nobody is checking in with each other before they’re pushing buttons.
Especially in stressful conditions, I find I tend to move first and then process and deal with my actions second.
It’s not the most efficient or effective process!
I’m not going to lie, impulse control is one of the trickiest parts of ADHD. Even the first step of admitting we’re someone who flies off the handle is tricky because it’s a real struggle session of the ego.
Fortunately, we’ve got a checklist for that — do you do any of the following?
- Interrupt conversations (even when you have nothing of substance to add). Why is it hard to not just shut up and let someone have a word in edgewise?
- Have distractions for your distractions? Often, the most straight-forward tasks can become arduous because the impulsive brain shifts our perception of priority like a spinning slot machine.
 You never know where your attention span is gonna land!
You never know where your attention span is gonna land! - Spend like you make money moves even when you’re broke as hell? We all know about those juicy brain chemicals that get released with the instant gratification of impulsive purchasing, and those with ADHD often find themselves in the trickiest of rabbit holes regarding what is a want and what is a need. I’ve even caught myself trying to justify buying ADHD management tools like planners and calendars and then realized the ones I have work fine. Late stage capitalism, baby!
- Find it hard to resist risky, self-destructive behavior like fighting or unsafe sex? I have a guy in my contacts that has about eight different emojis that all convey “DANGER! DO NOT TEXT HIM!” Anyone else?
- Want to Hulk out at the very thought of standing in a line that takes more than 5 minutes? It’s not (necessarily) that we feel our time is worth more than others, sometimes just the challenge of remaining relatively still and not fidgeting makes standing in a line for a long time positively exhausting! Too bad it’s one of those “part of being in society” things?
If any or all of these resonate, your impatient ass might need some professional intervention to deal with this symptom of ADHD.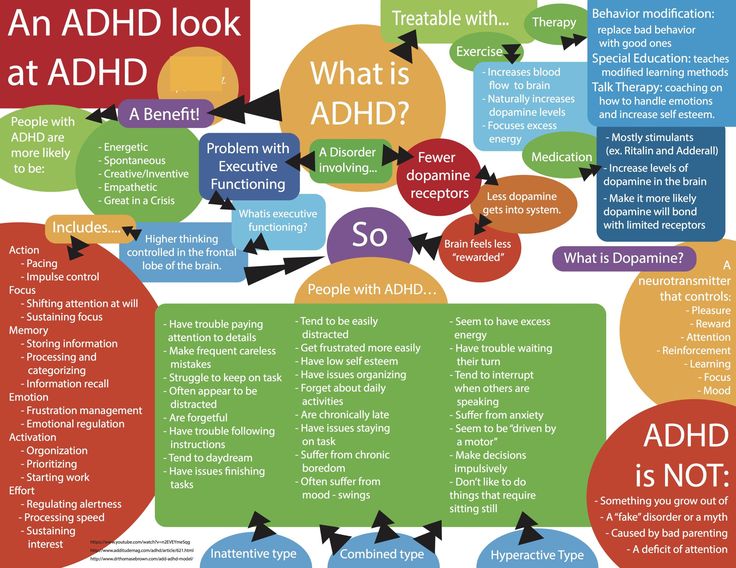
So what can we do about it?
Some of us treat our ADHD with medications, but the jury still seems to be out on how effective they are alone for this issue in particular.
Therapy, like cognitive behavioral therapy, may be useful if you’re going proactive on impulsivity issues.
Active mindfulness is like working out a muscle. You might start working out after a scenario of feeling particularly weak, and progress might feel impossibly slow at the start. Just like with getting physically active, I want to remind you to literally be patient with yourself as you try to be patient with others.
The more you flex that self-restraint and compassion, the easier it will come to you. And the better your results will be long-term!
Now if you’ll excuse me, this former Weird Kid in School is going to resist the impulse to look up Natalie from sixth grade who TOTALLY framed me for the bathroom horror story. That was your IBS, Natalie, YOUR IBS!
Reed Brice is a writer and comedian based in Los Angeles.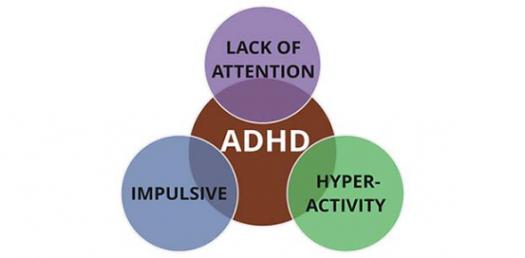 Brice is an alum of UC Irvine’s Claire Trevor School of the Arts and was the first transgender person to ever be cast in a professional revue with The Second City. When not talking the tea of mental illness, Brice also pens our love & sex column, “U Up?”
Brice is an alum of UC Irvine’s Claire Trevor School of the Arts and was the first transgender person to ever be cast in a professional revue with The Second City. When not talking the tea of mental illness, Brice also pens our love & sex column, “U Up?”
Impulsivity in adolescents with attention deficit hyperactivity disorder
There is evidence that adolescents suffering from ADHD are at risk for the development of addictive disorders - alcoholism and drug addiction [1-3]. Therefore, the issue of diagnosis, clinical differentiation and treatment of ADHD in this age group is so important, which is the subject of this study.
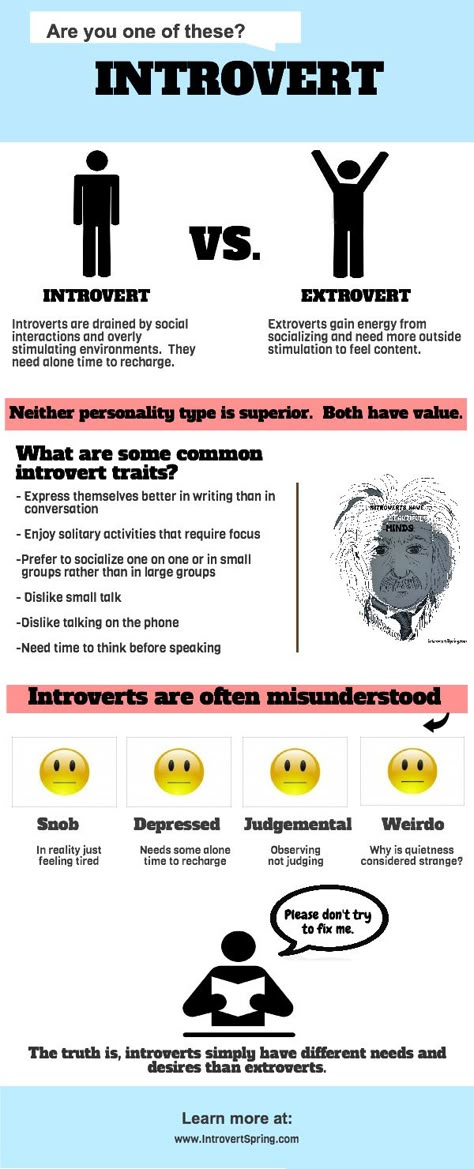
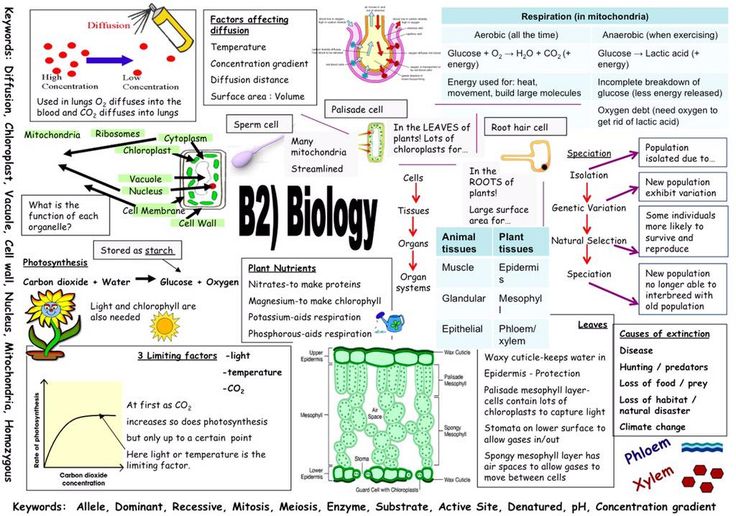
Clinical manifestations of ADHD are defined by three main symptoms: inattention, hyperactivity and impulsivity. When describing ADHD, researchers most often mean inattention (increased distractibility and reduced concentration) and hyperactivity (increased motor activity). At the same time, manifestations of impulsivity play a much smaller role.
Impulsivity is understood as the impossibility of controlling one's impulses. There are cognitive impulsivity (reflecting hasty thinking) and behavioral impulsivity (reflecting difficulties in controlling and suppressing behavioral reactions) [4]. Impulsive children cannot wait for their turn when playing, in a learning situation they have an “impulsive work style”: they shout out answers in the lesson without fully answering them, interrupting other students or teachers [5]. Because of impulsiveness, children often get into dangerous situations without thinking about the consequences. The propensity to take risks causes injuries and accidents. Impulsivity is often combined with aggressive and oppositional behavior.
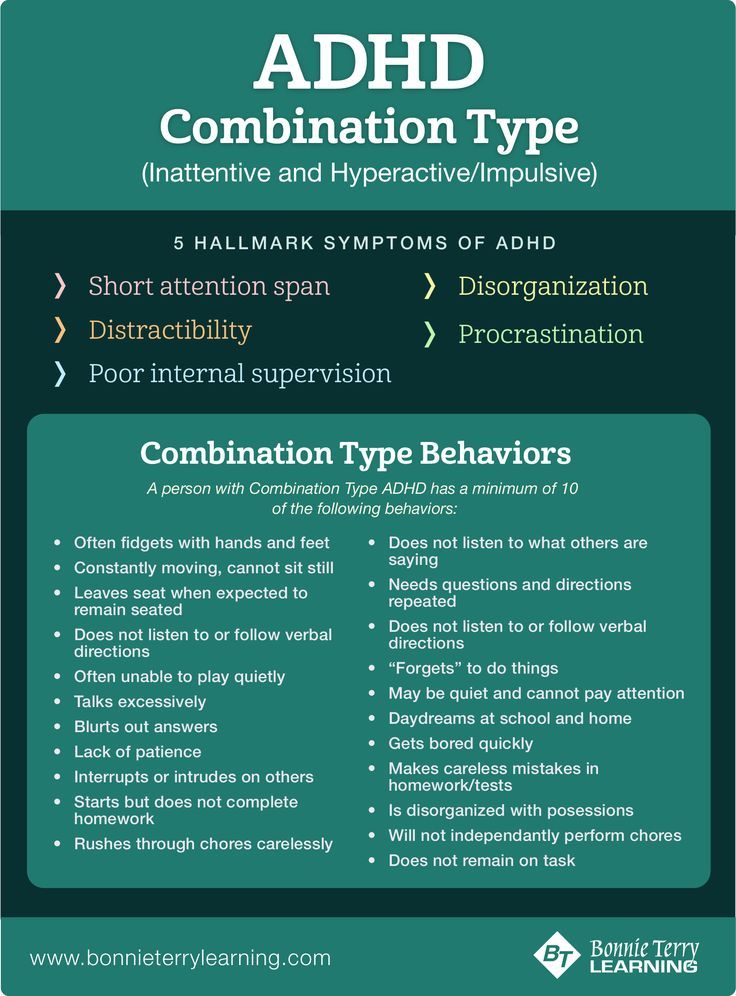
There are forms of ADHD with a predominance of inattention (ADHD-N), ADHD with a predominance of hyperactivity (ADHD-H) and a combined type of disease (ADHD-C) .
P. Wender and R. Scheider [6] observed a decrease in hyperactivity with age and a change from increased physical activity to a feeling of anxiety.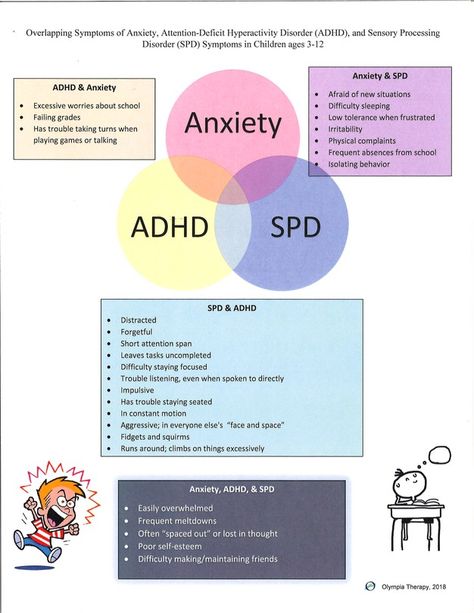 M. Fisher et al. [7] also noted a regression of manifestations of hyperactivity as adolescence approached. Our previous studies [8] showed that in the senior school (adolescent) age, there was a transformation of manifestations of hyperactivity into a significant increase in impulsivity. A. Zuddas et al. [9] noted that sometimes an increase in impulsivity is combined with an increase in aggressiveness. However, A. Clarke et al. [10] found that hyperactivity and impulsivity compared to inattention are more stable clinical components of the disease and less often disappear in adolescence.
M. Fisher et al. [7] also noted a regression of manifestations of hyperactivity as adolescence approached. Our previous studies [8] showed that in the senior school (adolescent) age, there was a transformation of manifestations of hyperactivity into a significant increase in impulsivity. A. Zuddas et al. [9] noted that sometimes an increase in impulsivity is combined with an increase in aggressiveness. However, A. Clarke et al. [10] found that hyperactivity and impulsivity compared to inattention are more stable clinical components of the disease and less often disappear in adolescence.
The purpose of this study is to study impulsivity in adolescents with ADHD and evaluate the effectiveness of the drug noofen in the treatment of this pathology.
Noofen - γ-amino-β-phenylbutyric acid hydrochloride. It is available in 250 mg capsules. A feature of the drug is the combination of the properties of a nootropic and tranquilizing drug. The results of a study conducted by N.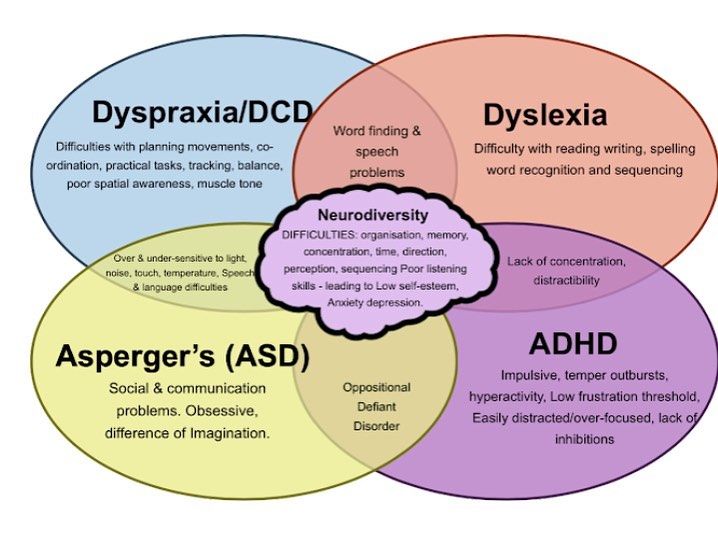 N. Zavadenko and N.Yu. Suvorinova [11], proved the effectiveness of Noofen in the treatment of ADHD. They established a positive effect of noofen on the cognitive sphere, including indicators of attention and auditory-speech memory.
N. Zavadenko and N.Yu. Suvorinova [11], proved the effectiveness of Noofen in the treatment of ADHD. They established a positive effect of noofen on the cognitive sphere, including indicators of attention and auditory-speech memory.
Material and methods
The study included 64 ADHD adolescents, 44 boys and 20 girls, aged 12 to 15 years (mean 13.5±1.4 years).
Diagnosis of clinical manifestations of ADHD was carried out in accordance with the ICD-10 and DSM-5 criteria, according to which the state of adolescents was defined as a combined type of ADHD.
Patients were divided into two groups: the 1st consisted of 38 adolescents with a combined form of ADHD (hereinafter referred to as ADHD-C), the 2nd group consisted of 26 adolescents with ADHD-H, i.e., with a predominance of hyperactivity.
Inclusion criteria for the study were: age 12 to 15 years; compliance of the clinical manifestations of the disease with the diagnostic criteria for ADHD according to DSM-5; the stability of the symptoms of the disease for at least 6 months in such a degree of severity that indicates a poor adaptation of the child; lack of mental retardation; parental and child consent to participate in the study.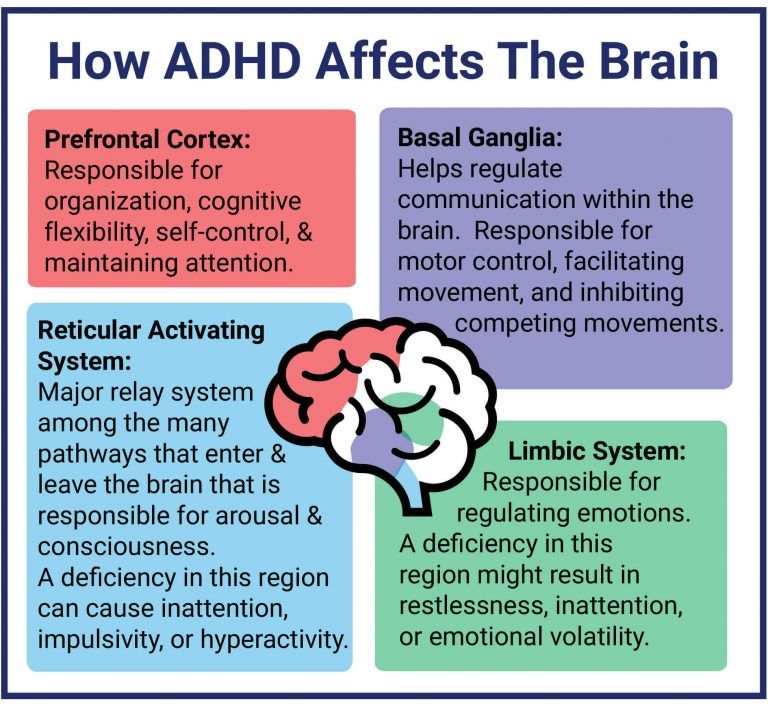
The exclusion criteria were as follows: patients under 12 and over 15 years of age; the presence of severe focal neurological symptoms; a significant decrease in vision and hearing; the occurrence of clinical manifestations of the disease after a traumatic brain injury or neuroinfection; a history of recurrent epileptic seizures; the presence of symptoms of chronic somatic diseases; mental retardation; use for 3 months prior to this study, any nootropic and psychotropic drugs (tranquilizers, antidepressants, sedatives and psychostimulants).
The assessment of the severity of the disease and the effectiveness of therapy was carried out using the SNAP-IV scale, which is a questionnaire for parents, consisting of 43 questions that allow scoring the degree of inattention, hyperactivity and impulsivity of children [12]. This scale, whose name consists of the first letters of the names of the authors (J. Swanson, E. Nolan, W. Palham), was developed in 1992. When filling out the questionnaire, parents must indicate the frequency of each symptom using 4 answer options: “Never”, “Infrequently”, “Quite often”, “Very often”, which were assigned 0, 1, 2 and 3 points respectively. Based on the answers of the parents, indexes of inattention, hyperactivity and impulsivity are calculated (based on the average sum of points for each of the sections). These indexes are then compared with normative data. Patients were examined before treatment (day 0) and after treatment.
Based on the answers of the parents, indexes of inattention, hyperactivity and impulsivity are calculated (based on the average sum of points for each of the sections). These indexes are then compared with normative data. Patients were examined before treatment (day 0) and after treatment.
The level of anxiety was assessed using the Spielberger-Khanin test.
Attention and impulsivity disorders were quantified using the TOVA (The Test of Variables of Attention) psychophysiological test, a test of continuous activity, which is a variant of the GO/NOGO test [13], which allows assessing the number of missed significant stimuli (inattention errors) and the number of false clicks (impulsivity errors) in relation to normative data. The test is based on presenting significant and insignificant stimuli to the subject in the form of geometric shapes. The test is divided into two conditional parts, not separated by a break. In the first part, a significant stimulus is presented in 22.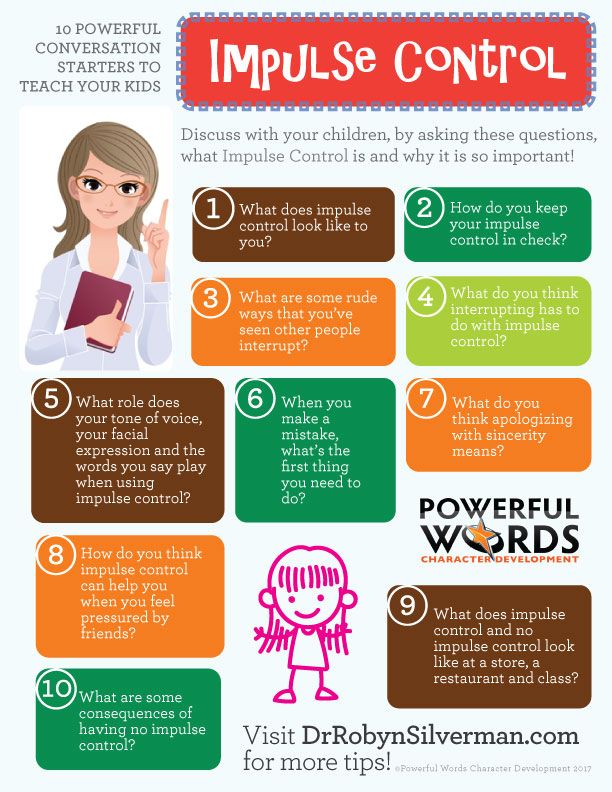 5% of cases; in the second part, a significant stimulus is presented in 77.5%. The test has a normative database. TOVA data included scores for inattention (errors of missing significant stimuli), impulsivity (number of false alarms), reaction time, and reaction time standard deviation. The data were compared before and after the course of treatment using Fisher's nonparametric sign test.
5% of cases; in the second part, a significant stimulus is presented in 77.5%. The test has a normative database. TOVA data included scores for inattention (errors of missing significant stimuli), impulsivity (number of false alarms), reaction time, and reaction time standard deviation. The data were compared before and after the course of treatment using Fisher's nonparametric sign test.
At the next stage of the study, 30 patients from the study group (19 patients with ADHD-C and 11 adolescents with ADHD-H) received Noofen at a dose of 500 mg per day (250 mg 2 times a day - day and evening) for 45 days . Evaluation of the effectiveness of therapy in this group was carried out 15 days after the end of treatment (day 60 from the start of treatment).
The control group consisted of 30 practically healthy teenagers.
Results
In tab. Figure 1 shows the values of the SNAP-IV scores in the study groups, indicating that the level of inattention in the study groups was approximately the same, while the level of hyperactivity and impulsivity in adolescents with ADHD-H was significantly higher.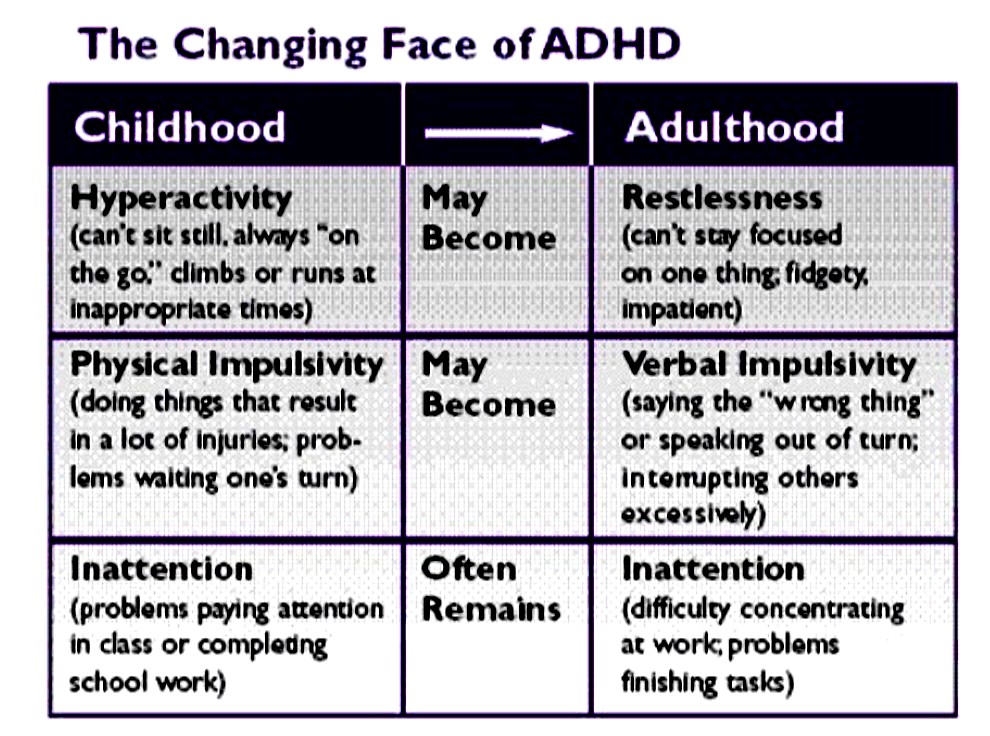 Parents especially often noted the following points on the scale: “begins to act without thinking”, “experiences difficulties in group games when it is necessary to wait for their turn”, “begins to answer questions without listening to them to the end”.
Parents especially often noted the following points on the scale: “begins to act without thinking”, “experiences difficulties in group games when it is necessary to wait for their turn”, “begins to answer questions without listening to them to the end”.
Table 1. Average clinical and psychological indicators in the studied groups of patients Note. * — р<0.05 — significance of differences in comparison with the control group; ** — р<0.01 — significance of differences in comparison with the control group; # — р<0.05 — significance of differences in comparison with ADHD-K; ## - p<0.01 - significance of differences in comparison with ADHD-K.
Compared with the control group, children with ADHD showed a significant increase in the average level of anxiety (both reactive and personal), while in adolescents with ADHD-H, these indicators were significantly higher than in patients with ADHD-C (see Table 1). Table 1).
The TOVA psychophysiological study showed that the majority of patients in the study groups had a marked increase in inattention scores compared to patients in the control group, with no significant differences found between the study groups.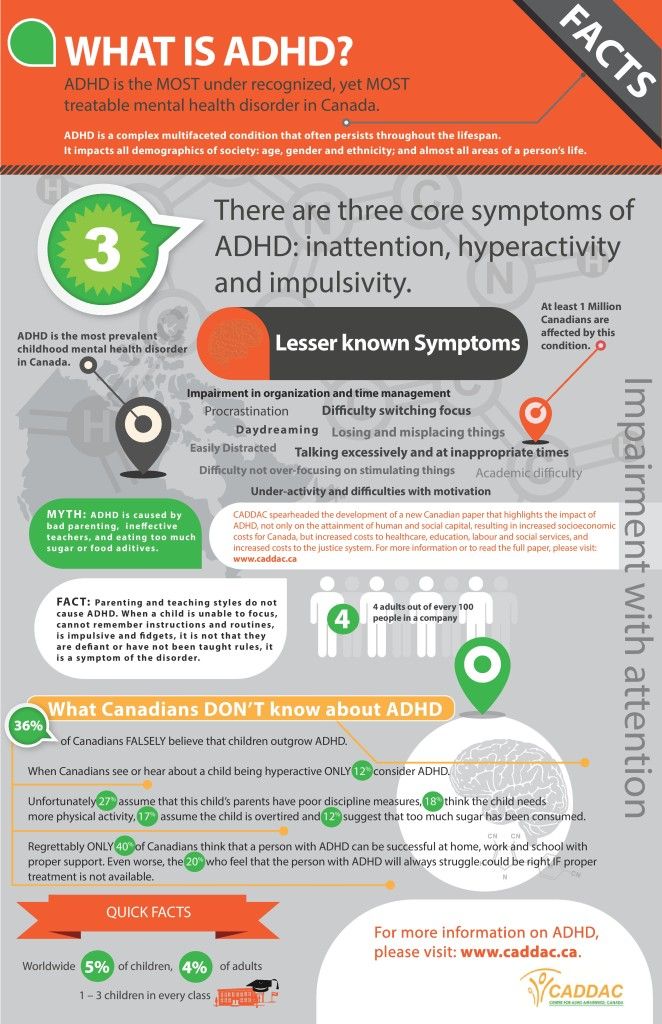 Attention is drawn to a significant increase in the number of false alarms (indicator of impulsivity) in all the subjects, however, in adolescents with ADHD-H, this indicator was significantly higher than in adolescents with ADHD-C (Table 2).
Attention is drawn to a significant increase in the number of false alarms (indicator of impulsivity) in all the subjects, however, in adolescents with ADHD-H, this indicator was significantly higher than in adolescents with ADHD-C (Table 2).
Table 2. Indicators of the TOVA test in the study groups of patients Note. * — р<0.05 — significance of differences in comparison with the control group; ** — р<0.01 — significance of differences in comparison with the control group; # — р<0.05 — significance of differences in comparison with ADHD-K.
After treatment, improvement was noted in 19 (63.3%) adolescents. Among them were 12 teenagers with ADHD-C and 7 teenagers with ADHD-H. Positive dynamics was not observed in 11 (36.7%) patients.
According to parents, after therapy, children became more diligent during school and homework, were less distracted during lessons, and completed tasks faster. Assessment of the condition using the SNAP-IV scale showed that the treatment led to a significant decrease in inattention and a pronounced, but not significant, decrease in impulsivity and hyperactivity (Table 3).
Table 3. Mean clinical parameters and results of the Spielberger-Khanin test before and after treatment, n=30 Note. * — р<0.05 — significance of differences in comparison with the index before treatment.
Re-examination of patients according to the Spielberger-Khanin test after treatment with Noofen showed a significant decrease in reactive anxiety, while personal anxiety did not change (see Table 3).
A repeat study after Noofen treatment using the TOVA test revealed a statistically significant decrease in inattention, false alarms (impulsivity), and response time (Table 4).
Table 4. TOVA scores before and after treatment, n=30 Note. * — р<0.05 — significance of differences in comparison with the index before treatment; ** - p<0.01 - significance of differences compared with the index before treatment.
Tolerability of therapy can be described as good. Side effects in the form of transient daytime sleepiness were observed in 2 (6.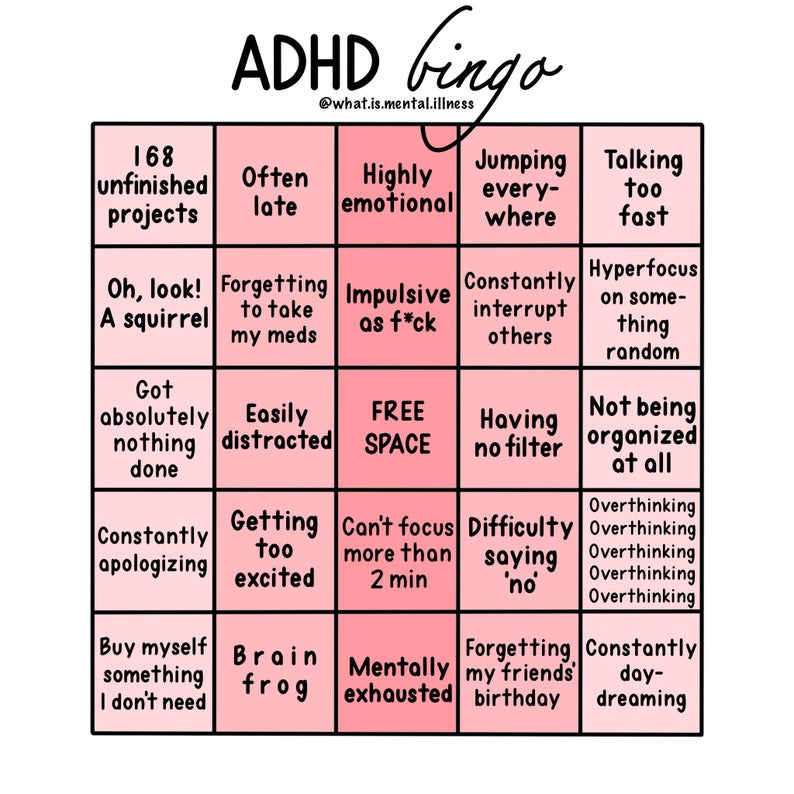 7%) adolescents, in 1 case parents noted an increase in physical activity. These undesirable symptoms appeared at the beginning of treatment and disappeared during treatment after 2 weeks, without leading to interruption of therapy.
7%) adolescents, in 1 case parents noted an increase in physical activity. These undesirable symptoms appeared at the beginning of treatment and disappeared during treatment after 2 weeks, without leading to interruption of therapy.
Discussion
Impairment of the system of emotional and motor control in patients with ADHD should be considered as one of the manifestations of executive dysfunction [14]. M. Lezak et al. [15] identified four main components of executive functions: the ability to form a goal, planning, purposeful actions and effective execution [15]. According to the model of K. Cicerone et al. [16], four areas are distinguished as part of control functions: 1) control cognitive functions associated with control and planning, purposefulness of activity; 2) the functions of behavioral self-regulation associated with emotional reinforcement; 3) functions regulating activation, i.e., providing initiative and activation of behavior; 4) metacognitive processes.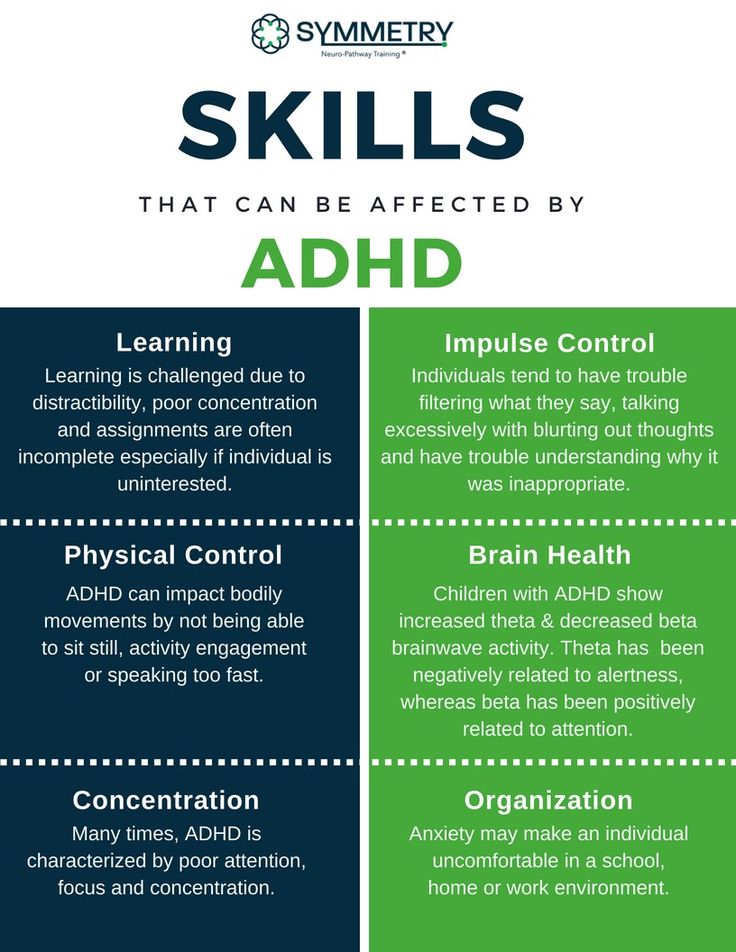
T. Robbins et al. [17], A. Aron et al. [18] showed the essential role of the prefrontal cortex in the process of controlling impulsivity. P. Petrovic and F. Castellanos [19] distinguish between "cold" (not associated with emotions) and "hot" (associated with emotions) performing functions. According to R. Barkley [20], performance dysfunction is noted in the combined type of ADHD (ADHD-C) and does not occur in ADHD-N.
Our study showed the presence of impulsivity in both ADHD-C and ADHD-H. In the latter, impulsivity is especially pronounced. Its degree is significantly higher, both according to clinical and psychophysiological studies. It should be noted that impulsivity in adolescents with ADHD is combined with an increased level of anxiety.
The high therapeutic efficacy of Noofen in ADHD has been established. After treatment, there is a marked decrease in impulsivity, hyperactivity and anxiety. These changes can be explained by the tranquilizing effect of Noofen, associated with its ability to enhance the controlling function of cortical structures over subcortical ones, including limbic ones, due to the pathogenetic effect: improvement of GABAergic neurotransmitter transmission [21].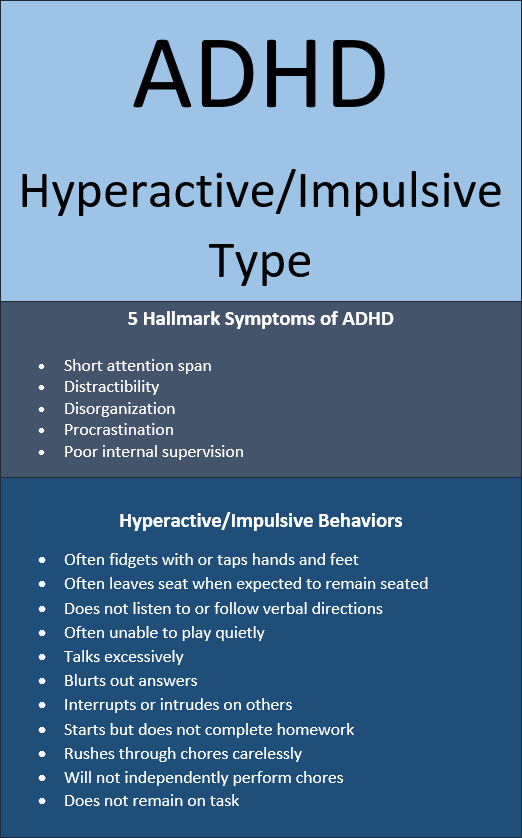 The decrease in inattention can be explained by the nootropic effect of Noofen. Noofen (as a derivative of phenylethylamine) has dopamine-positive properties that enhance its anti-asthenic effect. An important feature of the drug is the rarity of side effects.
The decrease in inattention can be explained by the nootropic effect of Noofen. Noofen (as a derivative of phenylethylamine) has dopamine-positive properties that enhance its anti-asthenic effect. An important feature of the drug is the rarity of side effects.
In conclusion, we emphasize that the treatment of children with ADHD is of great social importance, as it is a means of preventing addictive disorders.
No conflict of interest.
Hyperactivity and inattention (ADHD) | Encyclopedia of Early Childhood Development
To distinguish between restlessness and attention deficit hyperactivity disorder (ADHD), we need to understand the root causes of ADHD, its development, the myths and prejudices associated with it, how to recognize it, and what are the most effective remedial measures.
PDF summary All materials on the topic PDFInformation sheets
Download free PDF here or buy the paper version from our webshop (English and French only).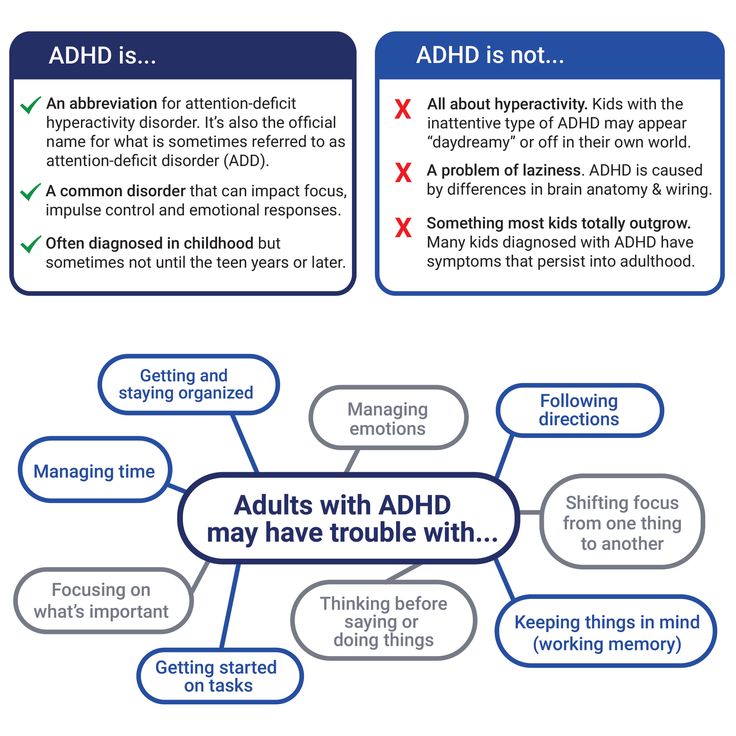
Generalization
Theme Editor: Russell Shakhar, MD, University of Toronto, Canada
Theme was developed with financial support from:
How important is this?
Attention-deficit/hyperactivity disorder (ADHD) is a neuropsychiatric disorder characterized by age-related, persistent and debilitating anxiety, impulsivity, and inattention from an early age. ADHD can be divided into three subtypes based on the type of behavior that is most noticeable: 1) the attention-impaired type; 2) hyperactive-impulsive type; and 3) combined type, depending on the nature of the symptoms. This syndrome is diagnosed when the symptoms appear and cause difficulty for the child in more than one life setting, such as school, home, or away from home.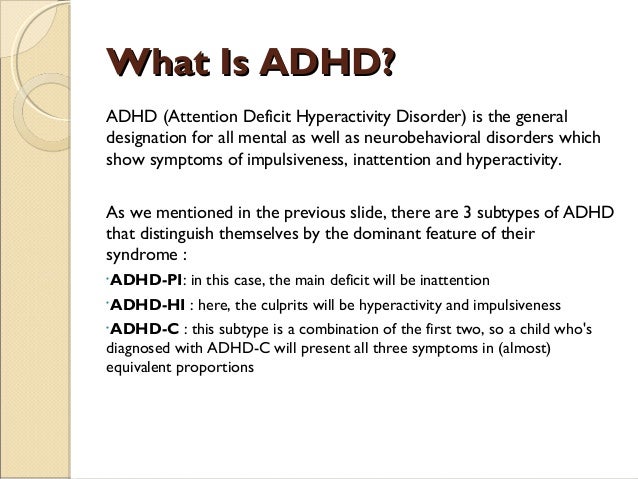 By some estimates, ADHD affects between 3 and 7% of school-age children worldwide, with boys showing higher levels of ADHD than girls. ADHD typically co-occurs with other psychiatric or developmental disorders (eg, anxiety, mood disorder, learning or speech disorders, conduct disorder, and sleep disorders) in 50-66% of cases. ADHD persists into adulthood in more than half of affected children. The symptoms of ADHD and its accompanying disorders interfere with learning and appropriate behavior in school, so the percentage of children with ADHD who graduate from school is lower. As they get older, they are also more likely to experience difficulty finding employment. Other negative consequences associated with ADHD include interpersonal difficulties and an increased incidence of accidental injuries, car accidents, and teenage pregnancies. In general, ADHD is one of the major health problems and can lead to significant losses both in the lives of individuals and society.
By some estimates, ADHD affects between 3 and 7% of school-age children worldwide, with boys showing higher levels of ADHD than girls. ADHD typically co-occurs with other psychiatric or developmental disorders (eg, anxiety, mood disorder, learning or speech disorders, conduct disorder, and sleep disorders) in 50-66% of cases. ADHD persists into adulthood in more than half of affected children. The symptoms of ADHD and its accompanying disorders interfere with learning and appropriate behavior in school, so the percentage of children with ADHD who graduate from school is lower. As they get older, they are also more likely to experience difficulty finding employment. Other negative consequences associated with ADHD include interpersonal difficulties and an increased incidence of accidental injuries, car accidents, and teenage pregnancies. In general, ADHD is one of the major health problems and can lead to significant losses both in the lives of individuals and society.
What do we know?
ADHD is believed to be caused by an interaction of genetic and environmental factors.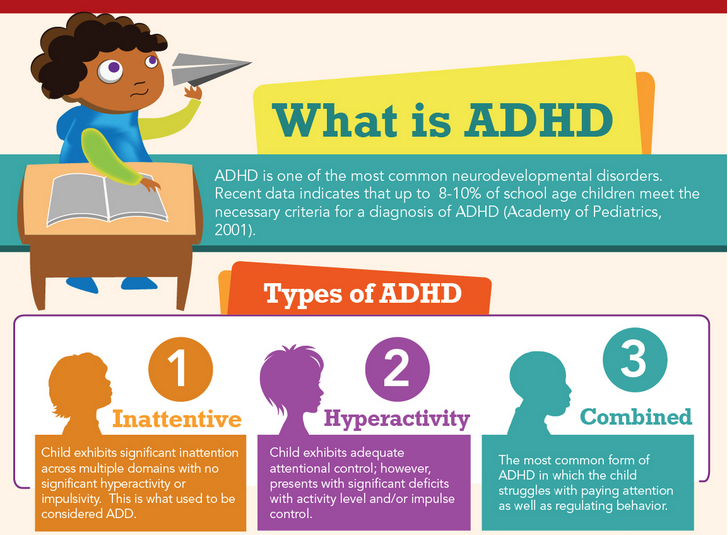 Symptoms of ADHD are highly heritable (76%), but the nature of the genetic influence is still undiscovered. According to the results of published studies, genetic factors leading to ADHD are also associated with other disorders. Thus, common genetic influences were found in the case of dyslexia and symptoms of inattention, symptoms of hyperactivity-impulsivity and oppositional conduct disorders, ADHD and symptoms of autism. Moreover, genes responsible for cell division, cell adhesion, and neuronal migration have been suggested to be related to the onset of ADHD. In terms of environmental risk factors, here the researchers noted the negative impact of smoking and drinking by the mother during the prenatal period, maternal depression, low birth weight of the newborn, poor parenting practices, and living in disadvantaged areas.
Symptoms of ADHD are highly heritable (76%), but the nature of the genetic influence is still undiscovered. According to the results of published studies, genetic factors leading to ADHD are also associated with other disorders. Thus, common genetic influences were found in the case of dyslexia and symptoms of inattention, symptoms of hyperactivity-impulsivity and oppositional conduct disorders, ADHD and symptoms of autism. Moreover, genes responsible for cell division, cell adhesion, and neuronal migration have been suggested to be related to the onset of ADHD. In terms of environmental risk factors, here the researchers noted the negative impact of smoking and drinking by the mother during the prenatal period, maternal depression, low birth weight of the newborn, poor parenting practices, and living in disadvantaged areas.
Children with ADHD experience more learning difficulties than their classmates due to neurocognitive impairment and behaviour. ADHD is often associated with deficits in executive functions (eg, planning, organization, attention to important details, and impulse inhibition).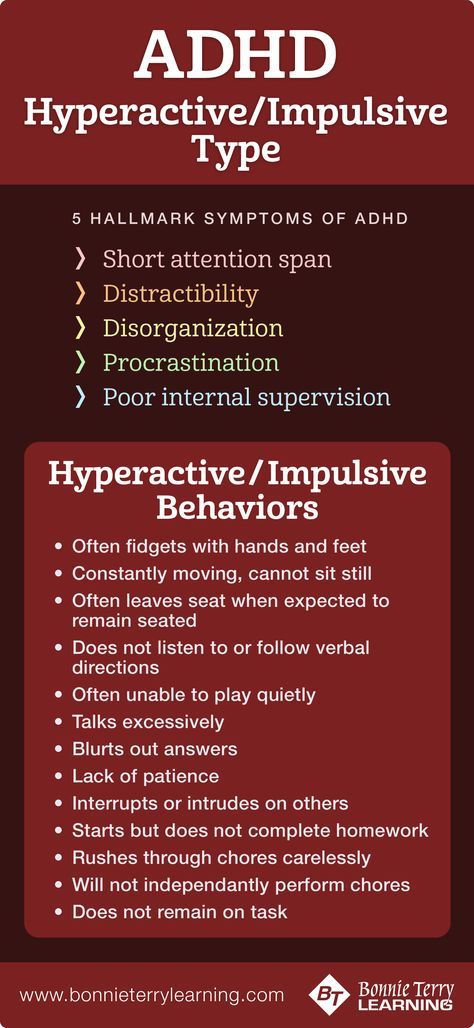 Accordingly, children diagnosed with this disorder are more likely to experience learning and/or speech difficulties. The results of neurophysiological studies suggest that ADHD is associated with atypical activity in the frontal cortex, the area of the brain responsible for cognitive processes. However, it is important to note that only a certain proportion of school-age children with ADHD (30%) have weak executive functions, which makes it possible to consider them neither as a necessary nor as a sufficient cause of the disorder.
Accordingly, children diagnosed with this disorder are more likely to experience learning and/or speech difficulties. The results of neurophysiological studies suggest that ADHD is associated with atypical activity in the frontal cortex, the area of the brain responsible for cognitive processes. However, it is important to note that only a certain proportion of school-age children with ADHD (30%) have weak executive functions, which makes it possible to consider them neither as a necessary nor as a sufficient cause of the disorder.
What can be done?
Diagnosis
ADHD is usually first detected and treated in school-aged children. However, the presence of symptoms of hyperactivity, impulsivity, and inattention during preschool years is considered a major factor in the diagnosis. Direct observation of the child suggests a diagnosis, but a child with even the most severe symptoms may be calm and attentive in an unusual setting such as a doctor's office. Therefore, the survey should focus on obtaining the entire history of the child's behavior at home, during play and at school from early childhood to the time of the survey. A routine clinical conversation (interview) provides an opportunity to discuss how parents and educators have responded to the child's difficulties and to identify strategies that have worked and those that have not worked. Examination should not be limited to symptoms of ADHD, but should also be asked about associated symptoms that may be present, such as anxiety, mood and behavioral problems, for example. Parents are not always fully aware of how stressful environments can upset a child; this is why talking directly to the child can be an important part of the examination. Comorbid disorders are an important area of treatment, and their presence can affect the effectiveness of therapy.
Therefore, the survey should focus on obtaining the entire history of the child's behavior at home, during play and at school from early childhood to the time of the survey. A routine clinical conversation (interview) provides an opportunity to discuss how parents and educators have responded to the child's difficulties and to identify strategies that have worked and those that have not worked. Examination should not be limited to symptoms of ADHD, but should also be asked about associated symptoms that may be present, such as anxiety, mood and behavioral problems, for example. Parents are not always fully aware of how stressful environments can upset a child; this is why talking directly to the child can be an important part of the examination. Comorbid disorders are an important area of treatment, and their presence can affect the effectiveness of therapy.
Many clinicians recognize that the parent-teacher rating scale is useful in the diagnostic process as a way of obtaining a description of a child's behavior that can be easily compared to age norms.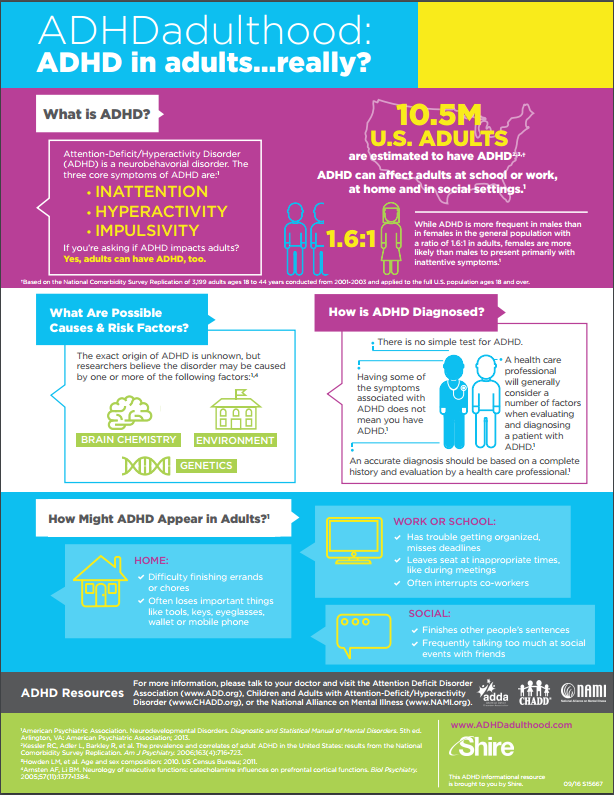 Some children with high levels of restlessness (restlessness), inattention and impulsivity have medical problems or developmental delays that should be identified during the examination. Children with learning difficulties may show symptoms at school and during homework because they have difficulty learning the material. Other children may show symptoms at home, which only indicates some problems in the environment of the child, social difficulties or parenting problems. In the doctor's office, it can be very difficult to determine which children have specific learning problems. Therefore, consultation with an educational psychologist can be very helpful in getting a complete picture of a child's strengths and weaknesses.
Some children with high levels of restlessness (restlessness), inattention and impulsivity have medical problems or developmental delays that should be identified during the examination. Children with learning difficulties may show symptoms at school and during homework because they have difficulty learning the material. Other children may show symptoms at home, which only indicates some problems in the environment of the child, social difficulties or parenting problems. In the doctor's office, it can be very difficult to determine which children have specific learning problems. Therefore, consultation with an educational psychologist can be very helpful in getting a complete picture of a child's strengths and weaknesses.
Corrective intervention
Stimulant medications (such as methylphenidate, Ritalin TM ) in various short-acting and long-acting forms play an important role in the treatment of ADHD. Some time ago, non-stimulant medications such as Atomoxetine became available and play an important role in the treatment.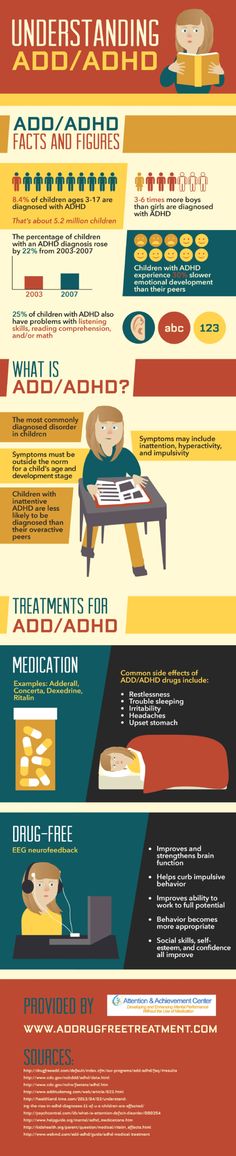 These medications can help a large number of sick people improve their attention, control impulses and reduce their level of activity. Also effective are intensive behavioral interventions that combine teaching the child self-control with teaching parenting strategies. Positive parental attention, rewards for appropriate behavior, and the negative consequences of inappropriate behavior (such as forbidding a child to play with a favorite toy) are recommended methods of behavioral intervention. Educators can also apply similar methods in their classrooms. Available evidence suggests that the best corrective intervention is a combination of medication, behavioral intervention, and school-based behavioral and learning interventions. For optimal effect, these treatments must be intensive and long-term. Direct training of cognitive functions such as working memory (the ability to retain and process information in short-term memory) seems promising as a potentially effective intervention. Some children may have improved behavior when certain foods are removed from their diet, although the universality of this effect has not been proven.
These medications can help a large number of sick people improve their attention, control impulses and reduce their level of activity. Also effective are intensive behavioral interventions that combine teaching the child self-control with teaching parenting strategies. Positive parental attention, rewards for appropriate behavior, and the negative consequences of inappropriate behavior (such as forbidding a child to play with a favorite toy) are recommended methods of behavioral intervention. Educators can also apply similar methods in their classrooms. Available evidence suggests that the best corrective intervention is a combination of medication, behavioral intervention, and school-based behavioral and learning interventions. For optimal effect, these treatments must be intensive and long-term. Direct training of cognitive functions such as working memory (the ability to retain and process information in short-term memory) seems promising as a potentially effective intervention. Some children may have improved behavior when certain foods are removed from their diet, although the universality of this effect has not been proven. Brain electrical activity training can improve alertness and behavior in some children. In this regard, the main problem of such treatment is the generalization of positive dynamics and its transfer to another environment. Further research is needed to explore treatment factors (individual and context-specific) in order to increase the beneficial effects of treating children over time and in different settings.
Brain electrical activity training can improve alertness and behavior in some children. In this regard, the main problem of such treatment is the generalization of positive dynamics and its transfer to another environment. Further research is needed to explore treatment factors (individual and context-specific) in order to increase the beneficial effects of treating children over time and in different settings.
Additional materials
Understanding ADHD: When does normal become abnormal?
Many people claim that true ADHD appears in the preschool years and that the symptoms associated with it are objective, implying that any observer would come to the same conclusion. This view is often, but not always, correct.
Although in preschool children the right to diagnose this disorder is left to specialists, in everyday settings parents are experts on their children. If they notice that their child is restless, inattentive, or impulsive, that he has difficulty controlling his reactions, that he needs to move, or that he has difficulty waiting his turn, then caregivers should listen.
If they notice that their child is restless, inattentive, or impulsive, that he has difficulty controlling his reactions, that he needs to move, or that he has difficulty waiting his turn, then caregivers should listen.
Ideally, the specialist will work with parents to observe the child's behavior in different settings and to assess whether the problem lies elsewhere (for example, parental expectations, coping strategies, stress levels, or socio-economic situation).
In some cases, ADHD symptoms may appear much later in development, after school entry or even later in the school years.
In all cases, the decisive factor in the diagnosis will be the deterioration of the condition - whether on a social, educational or emotional level.
Publications
Children with Attention Deficit Hyperactivity Disorder: Epidemiology, Comorbidity and Diagnosis
How to help a hyperactive child?
ADHD can affect all areas of a person's life.