What is an enabler in alcoholism
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.
-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly.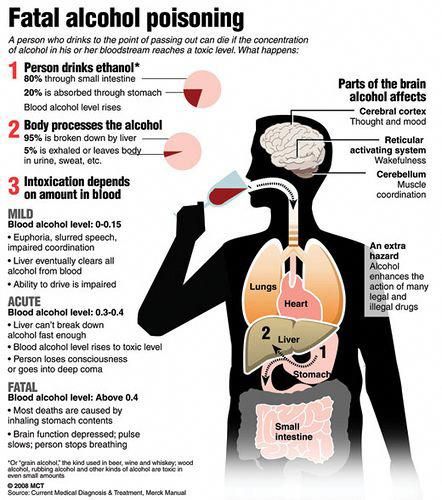 Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Is it possible to create an effective drug for the treatment of alcoholism
November 7, 2017 12:33
A source: RIA News
Alcoholism, as you know, is a huge socially significant problem. In our country, the alcoholization of the population, according to some estimates, has acquired the character of a national disaster and has the scale of a humanitarian catastrophe. Therefore, in many laboratories of the world and, in particular, in Russian institutes, work is underway to invent an effective drug for the treatment of alcohol dependence. nine0008
nine0008
The problem of creating such a drug has been standing for many centuries, which indicates its non-triviality. The fact is that alcohol interacts with the neurotransmitter dopamine, one of the chemical factors of internal reinforcement, which is involved in the reward system of the brain. It is with dopamine that the feeling of pleasure is associated, it affects the processes of motivation and learning. Therefore, almost all drugs that correct the process of alcohol consumption affect dopamine in one way or another. nine0003
There are two ways to "work" with the regulation of dopamine: you can reduce its production - that is, the pleasure that provokes excessive alcohol consumption, or you can replace the dopamine obtained from alcohol with an alternative one - for example, produced with the help of a drug.
In the first case, a depressive state will be a side effect of exposure, since the effect extends to other sources of pleasure. In the second, the patient receives, in fact, the same drug, with the subsequent development of dependence on the drug. nine0003
When asked whether it is possible to somehow bypass the regulation of dopamine and at the same time reduce alcohol consumption, scientists answer in different ways.
The creator of the innovative drug for alcoholism, Academician of the Academy of Sciences of Latvia Ivars Kalvins, comments: "I think dopamine can still be "bypassed." The regulatory mechanism is very complex, it consists of a dozen different receptors - that is, it is a large symphony orchestra. There is a chief conductor - central nervous system, but there are a lot of instruments. The loudest of them, of course, is dopamine - it causes happiness in high concentrations. But there are a number of other small molecules that do the same.
, is the will of a person. Treatment of alcoholism, in which the patient does not want it, cannot lead to anything good. " nine0008
At the moment, only a few drugs are used in the world to treat alcoholism. For example, in the United States, the Food and Drug Administration (FDA) only approved three drugs, and one of them (Disulfiram) is already considered obsolete, as it causes many side effects. It does not work with dopamine, but with the feeling of disgust after drinking alcohol. All it takes to evoke this feeling is to disrupt the ethanol absorption chain, the basis of all alcoholic beverages. nine0003
When alcohol enters the bloodstream, it is metabolized by two enzymes. Alcohol dehydrogenase acts first, it converts ethanol into acetaldehyde, a toxic substance that makes a person sick. And the second enzyme, aldehyde dehydrogenase, “improves” everything with its action.
Disulfiram destroys the second enzyme, so the toxin accumulates in the body, causing headaches and vomiting.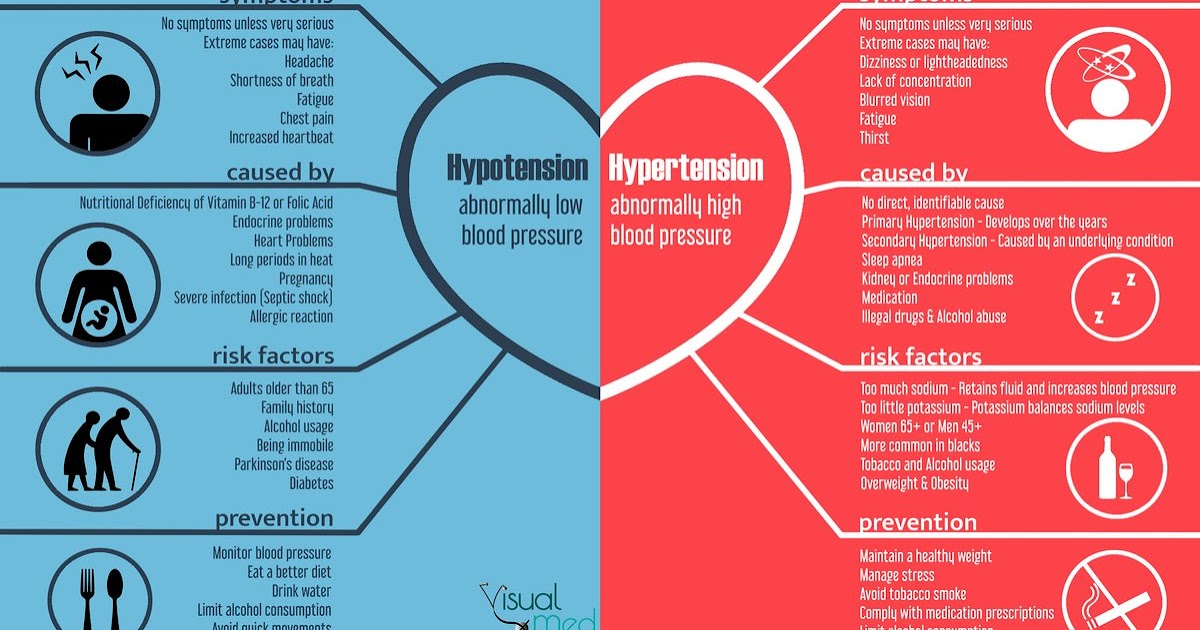 It is clear that an alcoholic, on his own initiative, will not take a drug that causes such consequences. Therefore, this drug is being withdrawn from practice. nine0003
It is clear that an alcoholic, on his own initiative, will not take a drug that causes such consequences. Therefore, this drug is being withdrawn from practice. nine0003
Two other drugs somehow "work" with the dopamine system. This is the drug "Acamprosate", which normalizes the balance of excitatory (glutamate) and inhibitory (gamma-aminobutyric acid, GABA) neurotransmitters of the central nervous system
person. And "Naltrexone" is a substance that blocks opiate receptors. Both of these agents are indirectly related to the regulation of dopamine.
New drugs are also being developed. "Faccex" - the creation of the "father of meldonium" Ivars Kalvins - is a well-balanced mixture of herbs: leuzea root powder, creeping thyme aerial part, reishi mushroom dry extract, milk thistle seeds and lemon balm leaves. But it is unlikely that this composition will be able to curb alcoholism in a severe stage, since the drug does not contain mechanisms to combat addiction. nine0003
Another development is carried out at the National Medical Research Center for Psychiatry and Narcology named after V. P. Serbsky. In the project Petr Konstantinovich Anokhin, candidate of biological sciences , supported by the Russian Science Foundation, a search is being made for an alcohol dependence therapy that acts by stimulating one of the five types of dopamine receptors.
P. Serbsky. In the project Petr Konstantinovich Anokhin, candidate of biological sciences , supported by the Russian Science Foundation, a search is being made for an alcohol dependence therapy that acts by stimulating one of the five types of dopamine receptors.
Scientists have shown that in the brain of rats that consume large amounts of alcohol, there is a decrease in the activity of the gene encoding the synthesis of the D2-dopamine receptor. nine0003
The idea arose to use a selective activator of this subtype of receptors - cabergoline, in order to stimulate their functions, suppressed by alcohol. It turned out that the drug not only significantly reduces alcohol consumption, but also restores the disturbed synthesis of dopamine receptors.
It is possible that Russian scientists will be able to create a new drug that will start recovery processes inside the body of patients, without initiating a new addiction, now from the drug. nine0003
Tags
Media about the Foundation, Medicine
Liver damage in alcoholism (literature review)
The problem of alcoholism has been extremely urgent all over the world for many years. According to the World Health Organization (WHO), more than 90% of the adult population drink alcohol, with 10% of men and 3-5% of women daily. Alcohol abuse is one of the most important medical, social and economic problems facing society, having a sharp negative impact on it [1-4]. The current situation with alcohol consumption in Russia is recognized by all researchers as an emergency [1, 5-7]. The number of people who abuse alcohol, as well as patients with alcoholism in general, is 14-17% of the population [8, 9]. According to some data, the possible number of alcoholics in Russia at the beginning of the 21st century is about 5 million people, or 3.4% of the country's population, and 15-17 million people who abuse alcohol. At the same time, 20-30% of the adult population consume 60-80% of alcoholic beverages. Mortality from causes associated with alcohol consumption is 10.42% of the number of deaths aged 18-70 years, or 5.42% of the total number of deaths per year. Some authors [6, 10], using their own calculation methods, attribute up to 17.
According to the World Health Organization (WHO), more than 90% of the adult population drink alcohol, with 10% of men and 3-5% of women daily. Alcohol abuse is one of the most important medical, social and economic problems facing society, having a sharp negative impact on it [1-4]. The current situation with alcohol consumption in Russia is recognized by all researchers as an emergency [1, 5-7]. The number of people who abuse alcohol, as well as patients with alcoholism in general, is 14-17% of the population [8, 9]. According to some data, the possible number of alcoholics in Russia at the beginning of the 21st century is about 5 million people, or 3.4% of the country's population, and 15-17 million people who abuse alcohol. At the same time, 20-30% of the adult population consume 60-80% of alcoholic beverages. Mortality from causes associated with alcohol consumption is 10.42% of the number of deaths aged 18-70 years, or 5.42% of the total number of deaths per year. Some authors [6, 10], using their own calculation methods, attribute up to 17. 4% of cases to “alcohol mortality” in Russia, and according to some data, up to 37%. nine0003
4% of cases to “alcohol mortality” in Russia, and according to some data, up to 37%. nine0003
In a large case-control study of 48,557 residents, 52% of all deaths in the 15-54 age group were attributable to the consequences of alcohol abuse (59% and 33% of deaths among men and women, respectively). In older age groups, the effect of alcohol was less pronounced, although still significant (18% of all deaths at the age of 55-74 years) [11].
Analysis of data on mortality and alcohol consumption in Russia since 1980 to 2007, presented in the report of the Civic Chamber of the Russian Federation in 2009, showed that the total mortality associated with alcohol consumption is 23.4% of all deaths per year [12].
According to the results of numerous studies, chronic alcohol intoxication (CHAI) is the cause of a large number of somatic diseases, such as kidney pathology (alcoholic hematuric nephritis, urate nephropathy), pathology of the cardiovascular system (alcoholic cardiomyopathy, alcoholic arterial hypertension), pathology of the endocrine system (diabetes mellitus) [13-17]. nine0003
nine0003
Alcoholism has a high comorbidity with tuberculosis, viral hepatitis, HIV infection, cancer, lung infection, immune system pathology [14, 18-28].
In many works [29, 30] it is noted that the consumption of more than 80 g of pure ethanol per day, which is equivalent to 1 liter of wine, 3.6 liters of beer, 0.25 liters of strong alcoholic beverages, leads to severe hepatopathology in men.
In women, the risk of liver damage occurs with the use of 30 g of ethanol per day. Systematic alcoholization is more pathogenic for the liver than episodic, even at relatively high doses [31]. nine0003
The factors contributing to the development of alcoholic liver disease (ALD), most researchers include systematic alcoholism, hereditary predisposition, prenatal intoxication, female gender, viral hepatitis, underweight or obesity, long-term use of drugs metabolized in the liver, toxic environmental impact [32-38].
It is recognized that the risk of developing ALD is determined by the polymorphism of genes coordinating alcohol dehydrogenase (ADH) type 2, aldehyde dehydrogenase (ADH) type 2 and cytochrome 2E1.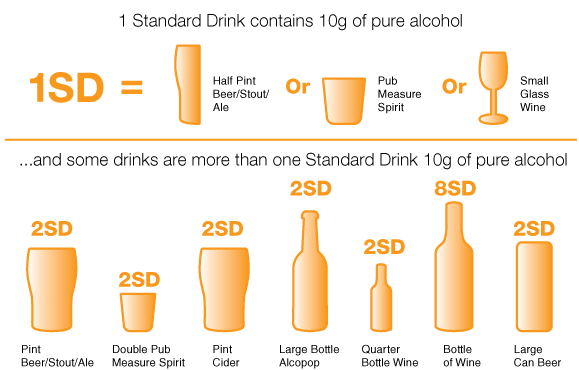 The unfavorable course of ALD is determined by the ADH 2-2 allele, which encodes the synthesis of highly active ADH. The risk of liver cirrhosis in carriers of this allele in CAI is increased by 3 times, and in combination with viral hepatitis - by 4 times. nine0003
The unfavorable course of ALD is determined by the ADH 2-2 allele, which encodes the synthesis of highly active ADH. The risk of liver cirrhosis in carriers of this allele in CAI is increased by 3 times, and in combination with viral hepatitis - by 4 times. nine0003
The second mechanism that determines the genetic predisposition to the development of ALD is the polymorphism of genes encoding proteins that determine the body's immune response to the effects of alcohol. These are CD-14, IL-10, tumor necrosis factor-α (TNF-α) and CTLA-4, which determine the increased sensitivity of the body to alcohol [29, 39].
A number of experimental studies have shown that prenatal ethanol intoxication causes oxidative stress and leads to the depletion of the reserves of the antioxidant system (albumin, transferrin, ceruloplasmin, a decrease in the pool of reduced glutathione, and a decrease in the activity of glutathione-mediated enzymes in the offspring liver [40, 41].
One of the extremely dangerous social trends is the systematic increase in the number of women suffering from alcoholism.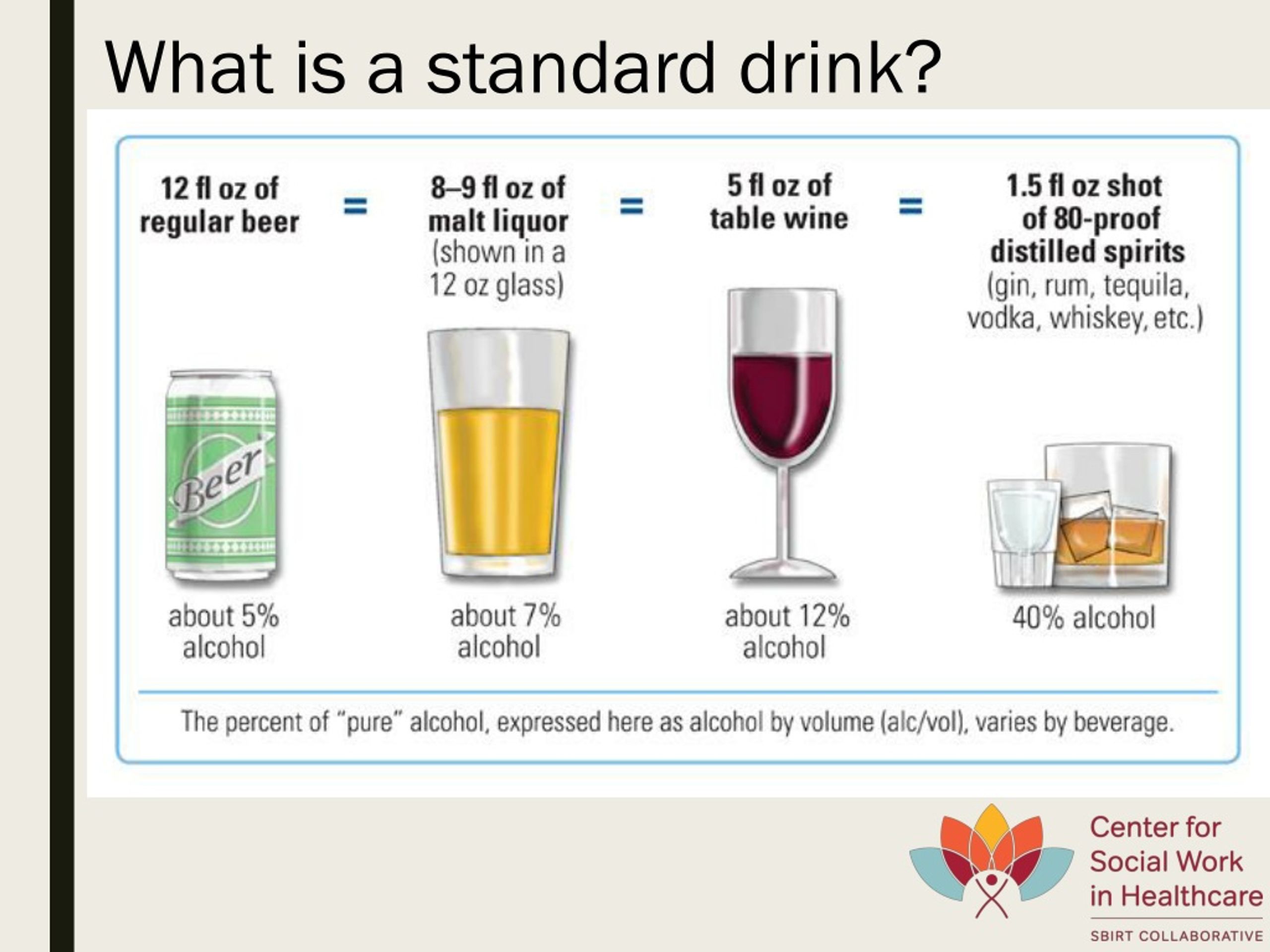 The ratio of women and men among patients with alcohol dependence in developed countries ranges from 1:5 to 1:2. In Russia, this ratio was quite recently 1:12, and in recent years it has been 1:5 [42, 43]. The malignant development of alcoholism in women [32, 33, 35] is also accompanied by the advanced (compared to men) development of ALD in them [35, 72], which is probably associated with a lower activity of hepatic ADH in them and activation of the mechanism of lipid peroxidation (LPO) [44, 45]. The female body is more sensitive to the toxic effects of alcohol and its metabolites. With the development of alcoholic hepatitis, the outcome in cirrhosis of the liver in women is noted more often. ALD in women progresses even during the period of remission of alcoholism. Sex differences explain the lower activity of the gastric fraction of ADH in women. nine0003
The ratio of women and men among patients with alcohol dependence in developed countries ranges from 1:5 to 1:2. In Russia, this ratio was quite recently 1:12, and in recent years it has been 1:5 [42, 43]. The malignant development of alcoholism in women [32, 33, 35] is also accompanied by the advanced (compared to men) development of ALD in them [35, 72], which is probably associated with a lower activity of hepatic ADH in them and activation of the mechanism of lipid peroxidation (LPO) [44, 45]. The female body is more sensitive to the toxic effects of alcohol and its metabolites. With the development of alcoholic hepatitis, the outcome in cirrhosis of the liver in women is noted more often. ALD in women progresses even during the period of remission of alcoholism. Sex differences explain the lower activity of the gastric fraction of ADH in women. nine0003
A number of authors explain the accelerated development of ALD in comparison with men by sex differences in the metabolism of fatty acids. So, if fatty acids accumulate in liver cells as a result of impaired β-oxidation, without being converted into triglycerides, then they can cause liver damage. This is due to the inclusion of alternative metabolic pathways - mediated omega-hydroxylation with the participation of cytochrome P 459A 1. In the course of experimental studies, it was found that this variant of fatty acid metabolism in females is reduced compared to that in men, and the deficiency of fatty acid binding mechanisms acids causes a hepatotoxic effect [46]. nine0003
So, if fatty acids accumulate in liver cells as a result of impaired β-oxidation, without being converted into triglycerides, then they can cause liver damage. This is due to the inclusion of alternative metabolic pathways - mediated omega-hydroxylation with the participation of cytochrome P 459A 1. In the course of experimental studies, it was found that this variant of fatty acid metabolism in females is reduced compared to that in men, and the deficiency of fatty acid binding mechanisms acids causes a hepatotoxic effect [46]. nine0003
According to most authors, overweight and obesity are independent risk factors for both steatosis and steatohepatitis. In obese individuals, ALD develops 2-3 times more often than in people with normal body weight. The combination of obesity and CAI factors increase the risk of ALD by 6 times [47-49]. Insufficient nutritional status against the background of CAI is also a risk factor for ALD. Malnutrition in these patients correlates with high mortality within 6 months.
An important factor contributing to the development of comorbid pathology in CAI is a change in the microelement link of homeostasis in patients with alcoholism. Researchers note "various counter-directional and unidirectional, friendly and mismatched changes in a large number of components of micro- and macro-elementary complexes in the blood of alcoholics" [50, 51]. The reasons for this are considered to be a change in the intake of microelements into the body, the influence of endogenously formed toxins, and complex antagonistic and synergistic interactions between elements [52, 53]. Persistent changes in the ratios of chemical elements K/Ca, Ca/Na, Ca/Mg in patients with CAI were revealed. Importance is attached to the violation of calcium metabolism, since it is a universal modulator of neurotransmitter processes (transmission of impulses, transport through membranes), a regulator in the processes of excitation in the nerve centers, tone and vascular permeability. An opinion is expressed that “calcium imbalance can be a leading and at the same time limiting system-forming link in generalized comorbidity in alcoholic disease” [4]. nine0003
nine0003
The balance of trace elements - metals (zinc, copper, iron) in the diet is important. CHAI enhances the absorption of iron from the intestines, increases its reserves in the body. Iron is a catalyst for free radical processes, thereby increasing oxidative stress that contributes to liver damage [54].
Hepatitis C virus infects up to ¼ of all patients with alcoholism and more than 40% of persons with ALD. The combination of CIA and infection with the hepatitis C or B virus accelerates the course of ALD by 8-10 times. Patients with this comorbidity are characterized by high mortality [55]. nine0003
Significant severity and progression of both ABP and chronic alcoholism is observed in patients who, by the nature of their professional activities, have encountered a complex of toxic-chemical hazards, such as organic compounds and heavy metals [4]. Such hepatotoxic substances include dioxin, methyl mercury, nitrogen dioxide, carbon monoxide, sulfur dioxide, tetraethyl lead.
Sources of dioxin are air and water contaminated from the incineration of garbage containing polyvinyl chloride and other polymers; agricultural use of pesticides and herbicides; emissions into the atmosphere and water bodies of waste from chemical, oil refining and pulp enterprises; violations of the technique of utilization of synthetic transformer oils; use of chlorine bleaches and household cleaners. nine0003
Dioxin affects the phospholipids of all cell membranes and disrupts transmembrane transport in both the liver and other organs.
A serious pathogenic effect on the activities of living organisms is caused by mercury contamination of water bodies. Under the influence of microorganisms of the aquatic environment, methylmercury is formed, which accumulates in fish. Methylmercury has a membrane toxic effect, inhibits the activity of cytochrome oxidase, binds glutathione, which prevents the metabolism of xenobiotics in the liver. nine0003
Nitrogen dioxide, carbon monoxide, sulfur dioxide, tetraethyl lead are formed in the environment as a result of vehicle exhaust. In large cities, the concentration of these substances in 1 m 3 air can reach 6-7 mg.
In large cities, the concentration of these substances in 1 m 3 air can reach 6-7 mg.
In Moscow, 3-3.5 thousand people die every year from causes related to air pollution.
The release of lead salts into the environment has reached catastrophic proportions. Up to 650 thousand tons of lead compounds are annually discharged into the oceans. Once in the human body, they accumulate in the liver, kidneys, nervous system, bone marrow, and blood cells [56, 57]. nine0003
In the liver, lead salts disrupt heme synthesis and reduce the activity of microsomal oxidases (C-reductase, CYP 450, CYP 1A2, CYP 3A4, CYP 2A6, 2C19, 2D6, 2E6) located in the endoplasmic reticulum of hepatocytes and responsible for the oxidation of exogenous substrates. Lead blocks mitochondrial ferrochelatase, causing the death of mitochondria and cells, disrupting the transmembrane transport of substances, causing dissonance of metabolic activity in the hepatocyte. Lead salts disrupt the processes of detoxification of xenobiotics, bile acids and LPO products, selectively accumulate cholesterol and lipids in the liver, reducing the synthesis of bile acids from cholesterol.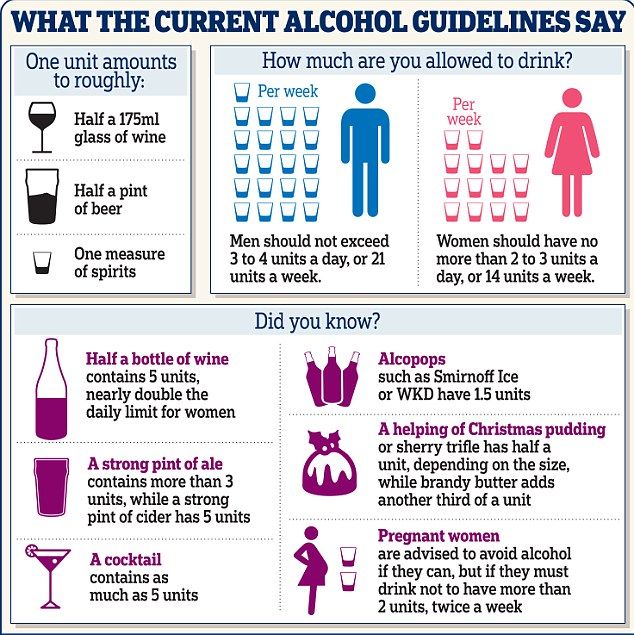 nine0003
nine0003
Pronounced pathogenic factors in the development of fatty degeneration of the liver are the systematic use of various psychoactive substances and drugs, their combined use [50, 51, 58]. Of the drugs, amiodarone, glucocorticoids, verapamil, nifedipine, acetylsalicylic acid, isoniazid, rifampicin, tetracycline have significant hepatotoxicity [59].
The risk of fatty degeneration of the liver increases with the simultaneous use of drugs that compete for cytochrome P 450 enzymes or transporters that ensure the entry of substances into the hepatocyte or their movement in the cytosol. nine0003
Activation of the sympathetic division of the autonomic nervous system (SNS), caused by a stressful situation, smoking, the use of psychostimulants, cannabinoids, eating in large quantities, leads to the activation of lipolysis, an increase in the concentration of fatty acids, an increase in the synthesis of cholesterol, phospholipids, steroids and bile acids. This increases the content of all lipoprotein fractions in the blood.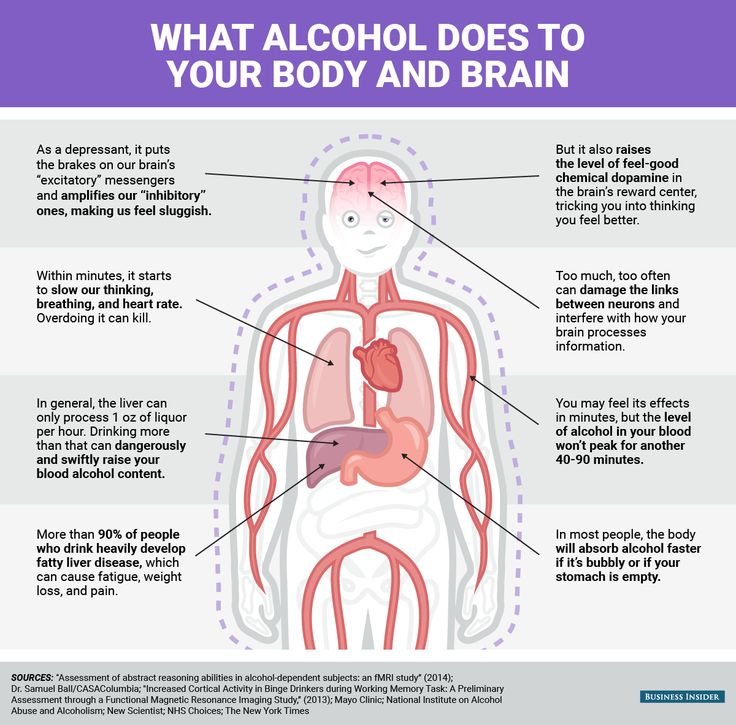 After the elimination of the sympathicotonic factor, excess lipids are utilized or excreted from the body. nine0003
After the elimination of the sympathicotonic factor, excess lipids are utilized or excreted from the body. nine0003
Activation of the SNS also forms eating behavior aimed at eating foods high in fat and cholesterol. Prolonged activation of the SNS can lead to atherogenic dyslipidemia and fatty degeneration of the liver [56].
Ethanol is metabolized in the liver due to the enzyme systems of ADH, cytochrome P 450 2V1 and catalase, but the role of the latter is insignificant.
ADH are cytoplasmic enzymes that exist as isoforms in the human liver. They are responsible for the metabolism of alcohol when its concentration in tissues is low. In case of alcoholic excesses or in the conditions of CAI, the cytochrome CYP 2E1 system is activated. The latter, together with ADH, converts alcohol into acetaldehyde. Then, with the help of AlDH, aldehyde oxidase and xanthine oxidase, it is converted to acetate. Acetaldehyde is a highly active and toxic metabolite of alcohol, but a healthy liver breaks down this compound fairly quickly. However, if its ability to eliminate acetaldehyde is impaired, it accumulates in the liver and blood [29, 46, 60].
However, if its ability to eliminate acetaldehyde is impaired, it accumulates in the liver and blood [29, 46, 60].
ADH-associated ethanol oxidation is associated with the reduction of oxidized nicotinamide adenine dinucleotide (NAD+) to reduced (NADH). An excess amount of NADH leads to a shift in the redox potential of the hepatocyte and a disruption in the metabolism of lipids and carbohydrates. There is a stimulation of the synthesis of fatty acids, suppression of β-oxidation in mitochondria, dissociation of gluconeogenesis processes due to a decrease in its substrates (oxaloacetate, pyruvate and dihydroxyacetate phosphate). In the cytoplasm of the hepatocyte, fatty acids accumulate, which, transforming into triglycerides, lead to the development of hepatic steatosis [18, 29].
Oxidation of ethanol by the cytochrome CYP 2E1 system leads to the formation of free radicals in the liver. These include the hydroxyethyl radical, the superoxide anion O2–, and the hydroxyl radical OH–. They cause various damage to intracellular structures. Interacting with unsaturated lipids, free radicals trigger the LPO process in the liver, which causes tissue damage and the development of fibrosis [44]. They also damage cellular DNA, primarily mitochondrial, which leads to mitochondrial dysfunction. nine0003
They cause various damage to intracellular structures. Interacting with unsaturated lipids, free radicals trigger the LPO process in the liver, which causes tissue damage and the development of fibrosis [44]. They also damage cellular DNA, primarily mitochondrial, which leads to mitochondrial dysfunction. nine0003
Ethanol, being metabolized in the liver, disrupts antioxidant protection. CAI causes deficiency of vitamins A and E, as well as glutathione. Vitamin E deficiency enhances LPO processes, and vitamin A deficiency contributes to lysosome damage. A lack of glutathione disrupts mitochondrial function and makes the cell susceptible to apoptosis [29, 46, 54, 61].
CAI causes activation of metabolic processes in the liver, which is associated with an increase in oxygen consumption by hepatocytes. This, in turn, increases the portocentral oxygen gradient, leaving pericentral hepatocytes in a state of relative hypoxia, which leads, along with damage to mitochondria, to ATP depletion and exacerbates liver damage [29, 46].
In patients with alcoholism, the process of metabolization of acetaldehyde is slowed down. When it is oxidized with the participation of xanthine oxidase and aldehyde oxidase, free radicals are also formed. Acetaldehyde disrupts the β-oxidation of fatty acids in mitochondria and interacts with specific amino acid residues on cellular proteins to form acetaldehyde-protein complexes. The latter cause the formation of neoantigens, which initiate the immune response of the body and at the same time enhance the synthesis of collagen in the liver. Acetaldehyde, interacting with tubulin, disorganizes the association of microtubules, which disrupts the transport processes in the hepatocyte and protein synthesis. The result of these processes is balloon dilatation of hepatocytes, one of the characteristic features of ALD [60]. nine0003
HAI activates inflammatory processes in the liver. Kupffer cells, being liver macrophages, synthesize oxidants and cytokines that normally perform protective functions. When released in large quantities, these substances cause liver damage. The main role in this is played by TNF-α, transforming growth factor (TGF-β) and superoxide. Under CAI conditions, the influence of these substances leads to apoptosis of hepatocytes [44, 62, 63].
When released in large quantities, these substances cause liver damage. The main role in this is played by TNF-α, transforming growth factor (TGF-β) and superoxide. Under CAI conditions, the influence of these substances leads to apoptosis of hepatocytes [44, 62, 63].
Hepatocellular proteins, combining with acetaldehyde and hydroxyethyl radical, form the so-called neo-proteins, which interact with the proteins of tubulin- and lysine-dependent enzyme systems and lead to the formation of secondarily modified proteins that act as neoantigens. These protein complexes are associated with acidaldehyde, malonaldehyde, 4-hydroxyphenol dialdehyde, and hydroxyl ethyl radicals [30, 64]. nine0003
Severe and irreversible consequence of CAI is liver fibrosis, which is recorded in 10-15% of patients with alcoholism. Its pathophysiological basis is considered to be the activation of the growth of stellate cells. Normally, these cells are located in the spaces of Disse between hepatocytes and vascular endothelium and are the depot of vitamin A in the body. In CAI, they proliferate, migrate to areas of inflammation, transform into myofibroblastic cells, and produce collagen. The starting factors of this process are considered to be acetaldehyde, aldehyde-protein complexes, oxidants, LPO process and TFR-β. Under the action of the latter, the intracellular matrix (ECM) is activated. The balance that exists normally between the profibrotic factors of the liver (tissue inhibitors of matrix metalloproteases) and antifibrotic factors (collagenases, gelatinases, stromolysins) is disturbed. This causes an increase in ECM components by 3-20 times and a change in its content, where collagen types I and III predominate. Expansion of the ECM and the ongoing capillarization of the sinusoids disrupt the metabolism between hepatocytes and the bloodstream, leading to blood shunting due to the development of false lobules and liver fibrosis [29, 46, 60, 65, 66].
In CAI, they proliferate, migrate to areas of inflammation, transform into myofibroblastic cells, and produce collagen. The starting factors of this process are considered to be acetaldehyde, aldehyde-protein complexes, oxidants, LPO process and TFR-β. Under the action of the latter, the intracellular matrix (ECM) is activated. The balance that exists normally between the profibrotic factors of the liver (tissue inhibitors of matrix metalloproteases) and antifibrotic factors (collagenases, gelatinases, stromolysins) is disturbed. This causes an increase in ECM components by 3-20 times and a change in its content, where collagen types I and III predominate. Expansion of the ECM and the ongoing capillarization of the sinusoids disrupt the metabolism between hepatocytes and the bloodstream, leading to blood shunting due to the development of false lobules and liver fibrosis [29, 46, 60, 65, 66].
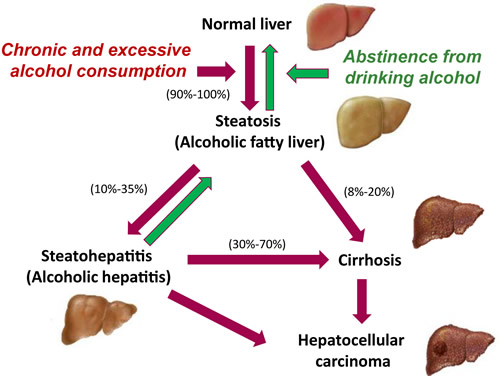
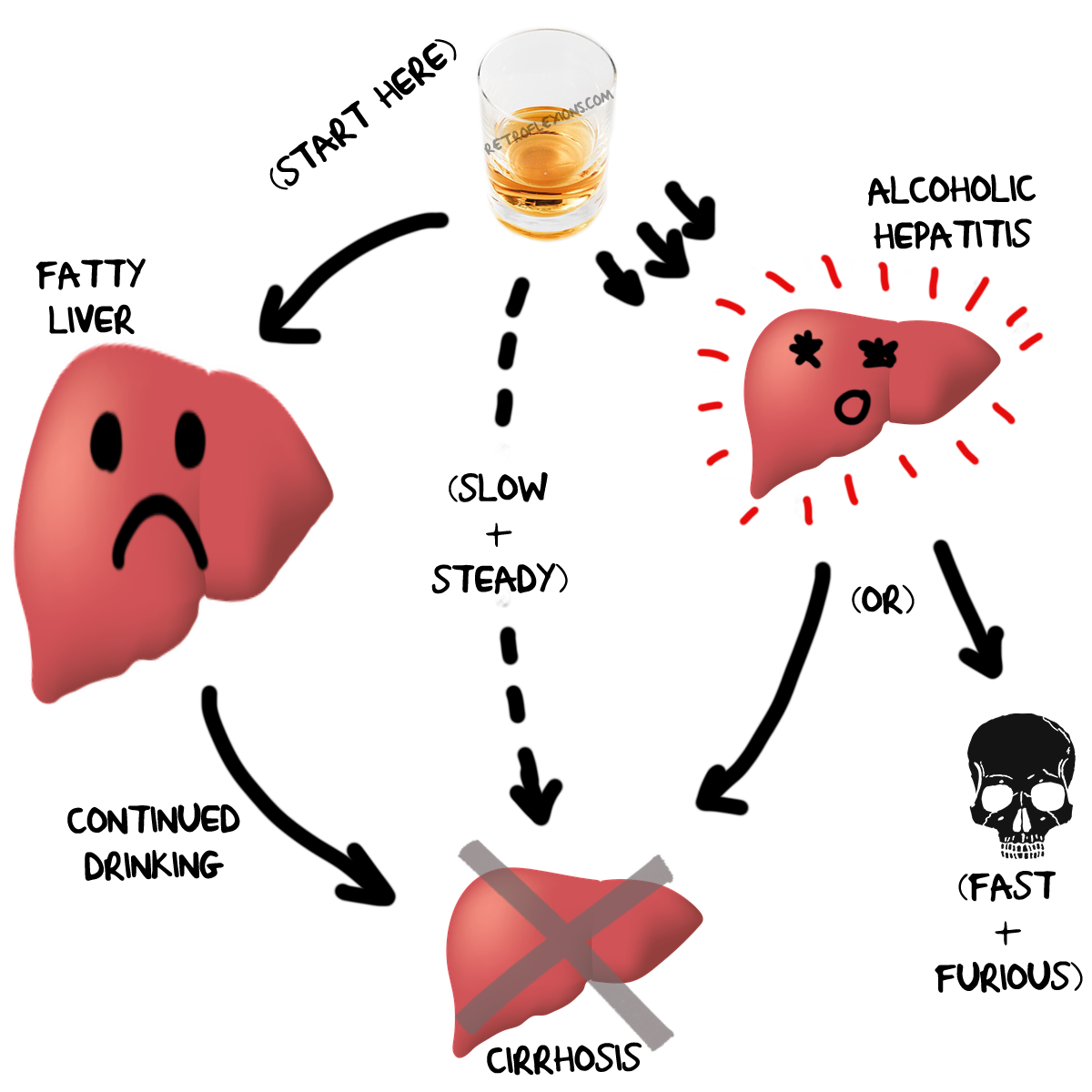
ABP proceeds in stages. To stage I of alcoholic liver damage include fatty degeneration (fatty hepatosis, steatosis). It occurs most often in practice - in about 60% of people with alcoholism. Patients complain of nausea, a feeling of bitterness in the mouth, unstable stools. Palpation reveals an increase in the liver by 3-4 cm, while its surface is smooth, the edge is rounded. In a biochemical blood test, a slight increase in alanine aminotransferase (ALT), aspartate aminotransferase (AST) and gamma-glutamyl transpeptidase (GGT) is detected. Histologically, macrovesiculatory obesity (large drops of fat in hepatocytes) is noted. nine0003
It occurs most often in practice - in about 60% of people with alcoholism. Patients complain of nausea, a feeling of bitterness in the mouth, unstable stools. Palpation reveals an increase in the liver by 3-4 cm, while its surface is smooth, the edge is rounded. In a biochemical blood test, a slight increase in alanine aminotransferase (ALT), aspartate aminotransferase (AST) and gamma-glutamyl transpeptidase (GGT) is detected. Histologically, macrovesiculatory obesity (large drops of fat in hepatocytes) is noted. nine0003
This form of the disease may be reversible with prolonged abstinence from alcohol.
Alcoholic hepatitis is stage II ALD. The term is found in the International Classification of Diseases, 10th revision (WHO, 1995) and is used to refer to acute degenerative and inflammatory liver lesions caused by alcohol consumption and capable of progressing to cirrhosis of the liver. It develops within 5-7 years of CAI existence, its severity depends on the duration of CAI and the amount of alcohol consumed [67]. nine0003
nine0003
CAI leads to accumulation of cytokines, damage to hepatocyte membranes, inflammatory infiltration in the liver parenchyma. The liver increases by 10-15 cm, it is dense on palpation. Morphologically visualized inflammatory infiltration, degeneration of hepatocytes, alcoholic hyaline (Mallory bodies), collagenosis in the space of Disse, rare foci of necrosis.
It is accepted to allocate acute and chronic hepatitis. Acute alcoholic hepatitis usually develops after prolonged systematic alcohol abuse against the background of formed cirrhosis of the liver. This is an acute progressive degenerative-inflammatory liver disease. There are latent, icteric, cholestatic and fulminant forms. nine0003
The latent variant of acute alcoholic hepatitis does not give a bright clinical picture. Its diagnosis is based on a biochemical blood test, which clearly shows an increase in ALT, AST and GGT. Verification of the diagnosis often requires a liver biopsy.
The icteric variant is more common. Patients complain of weakness, lethargy, fatigue, lack of appetite, nausea, vomiting, diarrhea, weight loss, yellow coloration of the sclera and skin, dull pain in the right hypochondrium, often hyperthermia. On palpation, the liver is enlarged, smooth, dense, painful. Detection of splenomegaly, ascites, telangiectasias, palmar erythema, asterixis indicates the presence of cirrhosis. Characterized by the addition of comorbid infections of the urinary, respiratory systems, as well as peritonitis and septicemia. nine0003
Patients complain of weakness, lethargy, fatigue, lack of appetite, nausea, vomiting, diarrhea, weight loss, yellow coloration of the sclera and skin, dull pain in the right hypochondrium, often hyperthermia. On palpation, the liver is enlarged, smooth, dense, painful. Detection of splenomegaly, ascites, telangiectasias, palmar erythema, asterixis indicates the presence of cirrhosis. Characterized by the addition of comorbid infections of the urinary, respiratory systems, as well as peritonitis and septicemia. nine0003
The cholestatic variant is observed in 5-13% of cases, manifesting itself as jaundice, darkening of urine and lightening of feces, constant pain in the right hypochondrium, skin itching. There may be signs of portal hypertension with the development of ascites. In the biochemical blood test, an increase in GGT and alkaline phosphatase (AP) is clearly visible. Differential diagnosis is carried out with acute cholangitis. This variant is prone to a protracted course [67].
The fulminant form is characterized by severe jaundice and severe course, as well as a combination of encephalopathic, edematous-ascitic, hemorrhagic syndromes, renal failure, cholestasis. Paraclinical examination reveals neutrophilic leukocytosis, increased ESR, bilirubin due to the direct fraction. The level of transaminases can be increased 10 times, GGT and alkaline phosphatase increase significantly, the ratio of AST to ALT exceeds 2; increased concentration of IgA. When combined with cirrhosis, biochemical signs of liver failure appear - an increase in prothrombin time (PT), a decrease in serum albumin concentration, hyperammonemia. Histological examination reveals hepatocytes in the stage of balloon and fatty degeneration, Mallory bodies, fibrosis, massive lobular infiltration with a predominance of polymorphonuclear leukocytes and areas of focal necrosis. nine0003
Chronic alcoholic hepatitis, according to many authors, does not show a specific clinical picture. In its manifestations, including paraclinical ones, it is similar to hepatitis of other etiologies. Patients complain of weakness, lethargy, fatigue, lack of appetite, loose stools, dull aching pain in the right hypochondrium. There are usually no signs of portal hypertension, but symptoms of cholestasis are often present.
In its manifestations, including paraclinical ones, it is similar to hepatitis of other etiologies. Patients complain of weakness, lethargy, fatigue, lack of appetite, loose stools, dull aching pain in the right hypochondrium. There are usually no signs of portal hypertension, but symptoms of cholestasis are often present.
In paraclinical studies, there is a slight increase in transaminase activity, and ALT is always greater than AST. Morphologically visible inflammatory changes without a tendency to cirrhotic process. nine0003
There are two forms of chronic alcoholic hepatitis.
The persistent form is characterized by a mild, sluggish clinical picture and a tendency to reverse the development of symptoms during periods of prolonged abstinence from alcohol. It is often detected only in a laboratory study. In the morphological picture - pericellular and subsinusoidal fibrosis, the presence of Mallory bodies, balloon degeneration of hepatocytes. Symptoms may be stable for a number of years if the course of alcoholism is moderately progressive, with remissions [67].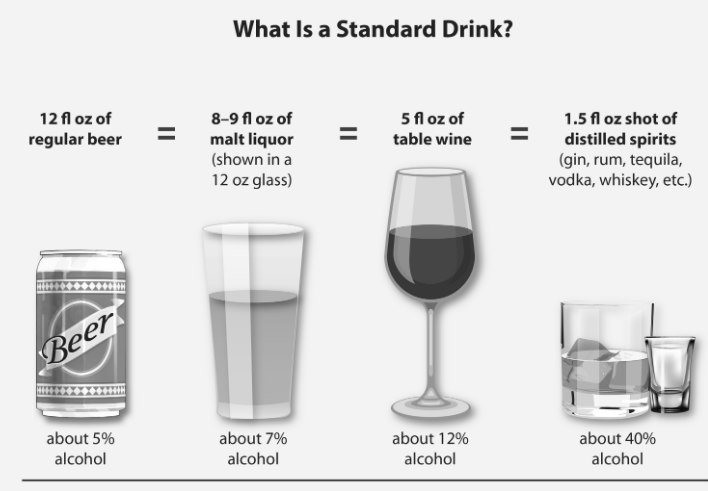 nine0003
nine0003
The progressive form is characterized by foci of small necrosis. Growing, they form a picture of liver cirrhosis. Patients complain of nausea, vomiting, diarrhea, icteric coloration of the sclera and skin, fever, bleeding, aching pain in the right hypochondrium. A biochemical blood test shows a high level of bilirubin, GGT, a moderate increase in transaminases. Hyperimmunoglobulinemia A is characteristic. The thiol test is moderately elevated.
Alcoholic liver cirrhosis develops in 10-20% of patients with chronic alcoholism [68]. Its formation is hardly noticeable, and the diagnosis, as a rule, is made already at the stage of decompensation. The clinical picture of the disease at the initial stage is manifested by an increase in the liver, but as the disease progresses, its size decreases. The diagnosis is helped by the presence of telangiectasias, gynecomastia, ascites, symptoms of encephalopathy, which are mixed (hepatic and toxic). nine0003
Patients with alcoholism are characterized by an erased course of ALD and late seeking medical help.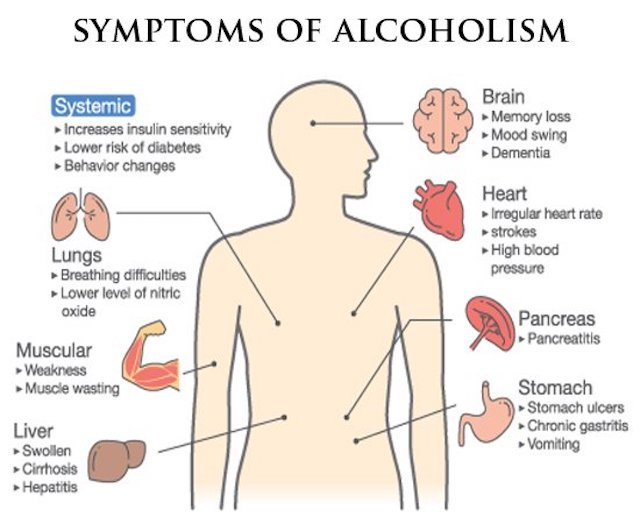 Diagnosis of the disease occurs, as a rule, in somatic hospitals, based on the symptoms of hepatomegaly, macrocytic anemia, leukocytosis, increased levels of ALT, AST, GGT. The predictor of the severity of ALD is the level of bilirubin in the blood serum and PT. To assess this indicator, the Meddrey index (MI) is calculated: MI = 4.6 (PT - PT in control) + bilirubin (mg / dl). PV in the control - in healthy people. nine0174
Diagnosis of the disease occurs, as a rule, in somatic hospitals, based on the symptoms of hepatomegaly, macrocytic anemia, leukocytosis, increased levels of ALT, AST, GGT. The predictor of the severity of ALD is the level of bilirubin in the blood serum and PT. To assess this indicator, the Meddrey index (MI) is calculated: MI = 4.6 (PT - PT in control) + bilirubin (mg / dl). PV in the control - in healthy people. nine0174
With an MI of more than 32, mortality from ALD occurs in approximately 50% of cases within 1 month.
Among the instrumental diagnostic methods, ultrasound of the abdominal organs is used, including to detect ascites and the size of the portal vein, as well as Doppler ultrasound to determine the degree of portal hypertension, and radionuclide hepatosplenoscintigraphy is also used. For diagnosis, it is important to identify multiple organ pathologies comorbid with alcoholism, such as cardiomyopathy, hypertension, pancreatitis, encephalopathy. Latent CAI is detected by determination of mitochondrial AST, carbohydrate-free transferrin, antibodies against acetaldehyde-protein products [69].
Latent CAI is detected by determination of mitochondrial AST, carbohydrate-free transferrin, antibodies against acetaldehyde-protein products [69].
According to the clinical and morphological classification of ALD, there are three main forms - steatosis, hepatitis and cirrhosis. The characteristic histological manifestations of ALD are hepatocyte fatty degeneration, the presence of Mallory bodies (semicircular eosophilic structures, condensed intermediate filaments), neutrophilic infiltration, and perivenular fibrosis.
Steatosis is observed in the vast majority of patients with ALD. Fat inclusions are localized in hepatocytes pericentrally, and in severe cases - panlobularly. Microvesicular steatosis and ballooning degeneration are characteristic (the cytoplasm of the cell is pale, edematous). Alcoholic hepatitis is produced by polymorphonuclear leukocytes (neutrophils), which predominate in the infiltrate. There are also mononuclear cells. nine0003
Fibrosis begins with deposition of connective tissue around the terminal hepatic vein and extends to the hepatic parenchyma.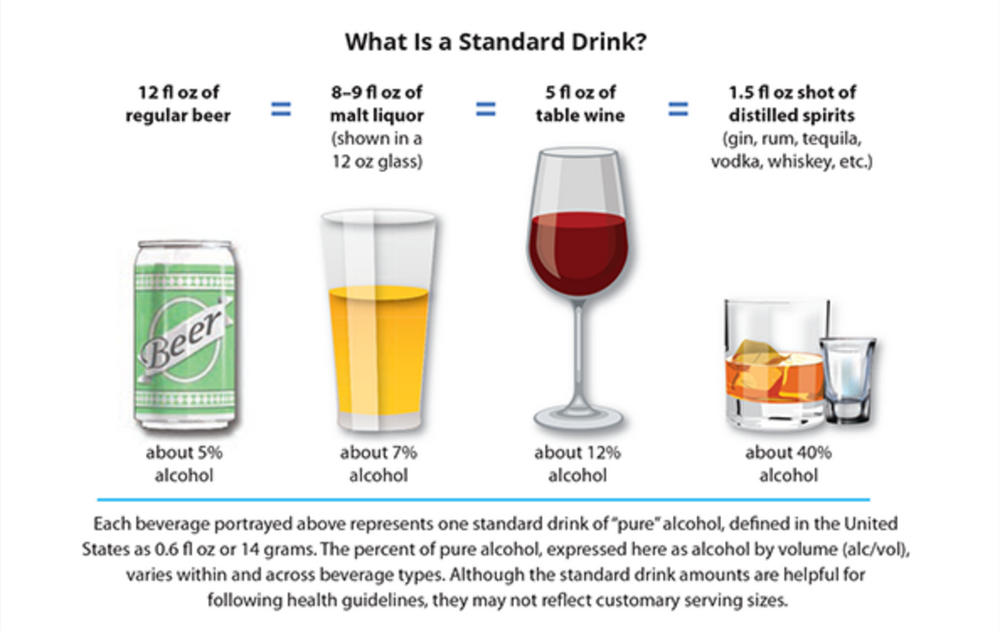 Centro-central and centroportal septa are formed. As a result, predominantly micronodular cirrhosis of the liver develops [29, 30, 46, 54, 60, 70, 71].
Centro-central and centroportal septa are formed. As a result, predominantly micronodular cirrhosis of the liver develops [29, 30, 46, 54, 60, 70, 71].
Complications of ALD include ascites, gastrointestinal bleeding, hypoprothrombinemia, hepatocellular carcinoma, primary liver cancer.
Chronic liver diseases claim about 1.4 million lives per year, of which about 800 thousand cases are accounted for by cirrhosis of the liver. The maximum lethality is noted precisely in ALD, as well as in the combination of alcoholic and viral lesions, and the presence of hepatic encephalopathy, incurable ascites, bleeding from varicose veins of the esophagus and stomach. The predictors of these conditions are a decrease in total protein in the blood of less than 60 g/l in combination with an increase in urea over 15 mmol/l, an increase in AST over 120 U/l and a ratio of AST/ALT more than 2 times, erythrocyturia. nine0003
Esophageal varicose veins of the III degree and portal gastropathy of the III degree testify to the possibility of an early lethal outcome in ALD.