What does it feel like to be depressed
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.
-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly. Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Depression. How is mental pain born? – Ministry of Health of the PMR
Constant stress, closed borders, self-isolation, increased security measures, statistics of new cases of COVID-19 and frightening thoughts about the future affect mental health. Someone is in a depressed mood or vice versa becomes aggressive. Others lose their appetite, sleep, and taste for life. In this case, we can talk about a real disease, so common and little known at the same time - about depression. The psychiatrist of the Republican Clinical Hospital, psychotherapist Yulia Gromatskaya explained to us what deep problems are hidden behind this word.
- There is an opinion that there is no depression, that these are excuses of weak people who do not want to work on themselves. How would you comment on this?
- Depression is a disease that belongs to affective disorders and is included in the international classification of diseases. It affects the physical state of the body, mood and psyche, affects how a person eats and sleeps, how he treats himself and how he perceives the world around him. It's not the same as being in a bad mood. Depression is not a sign of a person's weakness or a condition that can be overcome by an effort of will or desire. People with depression can't just pull themselves together and get better. At any arbitrary point in time in the human population, clinical depression affects 2–3% of men and 5–9% of% of women. The lifetime risk of getting sick is estimated at 5-12% if you are a man and 10-25% if you are a woman.
- What is depression like?
There are more than seventy classifications of this disease in the world. The simplest and most understandable classification is the division into psychogenic, endogenous and exogenous depressive disorders.
The simplest and most understandable classification is the division into psychogenic, endogenous and exogenous depressive disorders.
- Tell us more about them
Psychogenic depression is a reaction to a traumatic event (reactive depressions, exhaustion depressions). They can be based on long-term or short-term exposure to psychosocial stressors, disruption of interpersonal relationships, labor conflicts.
Endogenous depressions are associated with biological predisposition, little dependent on external triggering factors (manic-depressive psychosis (MDP), cyclothymia, masked depression, involutional melancholia). In their occurrence, of course, the genetic factor is of great importance.
Exogenous depressions occur as a result of organic brain damage (inflammatory processes, traumatic brain injury), intoxication (alcohol, neuroleptic), various types of somatic pathology (arterial hypertension, atherosclerosis).
- What are the symptoms of depression?
Classically, depression is manifested by a disorder of mood, thinking, a decrease in the intensity of sensations. Sleep disturbances may play an important role in the diagnosis of depression. Reduced sleep duration, early awakening, feeling of incomplete “wakefulness” in the morning, difficulty falling asleep, insomnia are combined with frequent awakenings in the middle of the night. In patients with apathy, we can rather talk about increased drowsiness, often with superficial night sleep.
Decreased drives, characteristic of depressive syndrome, are most pronounced in melancholy and apathetic depressions. Loss of appetite is sometimes accompanied by an aversion to the sight, smell of food, patients begin to refuse food, quickly lose weight. It is characteristic of depression and a decrease in sexual desire.
Of particular note is the appearance of suicidal thoughts, reaching in severe cases to an irresistible desire for suicide and self-harm.
- How does a depressed person feel?
When the melancholy affect dominates, patients characterize their mood as sadness, sadness, despondency, depression, depression, grief, melancholy. It is possible to compare these experiences with a special feeling of hopelessness.
Anxiety depression is more characterized by the appearance of internal excitement, anxiety, tension, expectation, despair. Patients talk about a feeling of agonizing expectation of an impending or ongoing disaster, express fears and concerns about the health and well-being of loved ones. These concerns can be both subjective and vague.
Anhedonia observed, i.e. inability to enjoy previously pleasant things, as well as apathy (more often characterized by a feeling of indifference with a narrowing of the circle of interests, or their complete disappearance, reduction or loss of desires, motives and needs). Patients talk about boredom, laziness, lack of will, lack of initiative, mental lethargy, indifference.
- What other difficulties does a sick person face?
Lethargy and slowness of thinking appear up to the feeling of a complete stop of mental activity. Patients complain of thoughtlessness, loss of memory. Speech becomes concise, elementary.
There is also a decrease in the intensity of sensations: the day is perceived as twilight, objects are poorly distinguishable, sounds are muffled, unintelligible, colors and timbre lose their richness and brightness. The world is turning grey.
The perception of time is changing, the temporal vector of experiences with melancholy is directed to the past. Patients do not think about the future, it is closed for them, there is “nothing”, or it is perceived as filled with upcoming trials and troubles. The present worries only as an experience of one's painful state. The day drags on endlessly, languidly, and in the memories the lived day seems short.
- How does depression manifest itself outwardly?
Motor depressive disorders are manifested by slowness, paucity of movements, rapid fatigue, changes in facial expressions - the look is dreary, sad, in severe cases, frozen, motionless with an expression of suffering. Facial expressions - from slowly changing (with a predominance of a sad expression) to a mournful, suffering mask.
Facial expressions - from slowly changing (with a predominance of a sad expression) to a mournful, suffering mask.
- How does depression affect the brain?
Depression involves many neurotransmitters and, more importantly, many different brain structures. The cortex is not able to adequately assess the surrounding reality (and believes that everything is bad, without sufficient objective grounds for this), the hippocampus does not remember anything good, the amygdala is afraid of everything and does not rejoice at anything, the nucleus accumbens does not reward our good deeds with a sense of joy, the hypothalamus allows all sorts of failures in the formation of the desire to eat, sleep or have sex, etc. Depression changes the brain's response to stress, suppressing the activity of the hypothalamus, pituitary gland and adrenal glands.
- Why is depression born?
Some forms of depression run in the family from generation to generation, which suggests that the existing biological predisposition to the disease may be hereditary.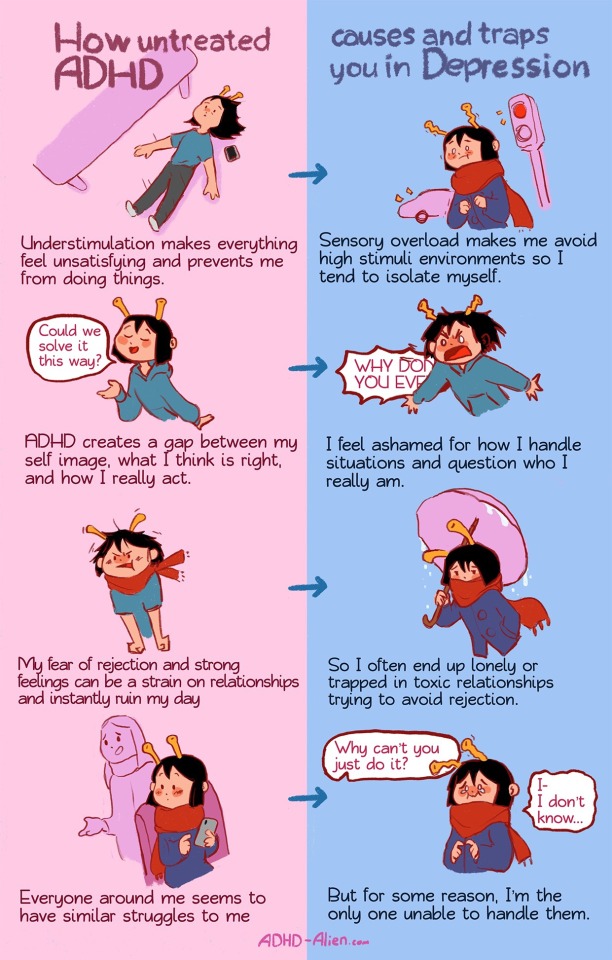 Bipolar disorder seems to be just such a case. However, not every family member with a genetic predisposition to bipolar affective disorder will necessarily develop the disease. Most likely, additional factors, such as stress and anxiety at home, at work or at school, influence the development of the disease. Hereditary or not, clinical depression is often associated with changes in the structure or function of the brain. People with low self-esteem, with a constant pessimistic view of themselves and the world around them, are prone to depression.
Bipolar disorder seems to be just such a case. However, not every family member with a genetic predisposition to bipolar affective disorder will necessarily develop the disease. Most likely, additional factors, such as stress and anxiety at home, at work or at school, influence the development of the disease. Hereditary or not, clinical depression is often associated with changes in the structure or function of the brain. People with low self-esteem, with a constant pessimistic view of themselves and the world around them, are prone to depression.
Recent studies have shown that physical changes in the body can be accompanied by mental changes as well. Diseases such as stroke, heart attack, cancer, Parkinson's disease and hormonal disorders can lead to depressive states, making the patient apathetic and unwilling to take care of their physical needs, thereby delaying the recovery period. In addition, bereavement, difficult relationships, financial problems, or any stressful (unwanted or even desired) lifestyle changes can trigger a bout of depression. Very often, a depressive disorder is triggered by a combination of genetic, psychological, and environmental factors. Subsequent attacks of the disease can be caused by even a little stress or occur for no apparent reason at all.
Very often, a depressive disorder is triggered by a combination of genetic, psychological, and environmental factors. Subsequent attacks of the disease can be caused by even a little stress or occur for no apparent reason at all.
- How quickly does the disease "strike" a person, if we talk about a serious negative event in his biography?
A depressive reaction may develop within a few hours of acute stress, but a depressive disorder can be considered if symptoms persist for at least two weeks.
- What is the treatment for depression?
Treatment takes quite a long time, depending on the type of depression and its severity. The approach is individual, in mild cases it will be possible to get by with psychotherapy, with endogenous depression, the appointment of antidepressants is mandatory.
- How do these medicines work and what do they directly affect?
Not the only, but still important component of brain dysfunction during depression is a decrease in the level of neurotransmitters that transmit signals from one neuron to another, and specifically serotonin and norepinephrine. The first regulates anxiety, joy and is responsible for mood, the second is responsible for performance and motivation.
The first regulates anxiety, joy and is responsible for mood, the second is responsible for performance and motivation.
Historically, the first and still used drugs for depression are drugs that increase the amount of serotonin and norepinephrine in the synaptic cleft. This does not lead to an immediate improvement in the state, but gradually helps the brain to restore the rest of the disturbed systems.
- What other tools are effective in combating depression and depression?
In addition to drug therapy, of course, psychotherapy and aids such as active physical exercise, outdoor walks, light therapy, water treatments are recommended.
- What happens if depression is not treated? What is fraught with this disease, stretched for years?
The main and most severe complication of depression is suicide. From 45 to 60% of all suicides on the planet are committed by patients with depression, 56% of those suffering from depression attempt suicide, and 15% end their lives in this way. This is in addition to social maladjustment, the impact on the quality of life and relationships in the family, since the presence of a mental illness in one of the family members cannot but affect the general atmosphere.
This is in addition to social maladjustment, the impact on the quality of life and relationships in the family, since the presence of a mental illness in one of the family members cannot but affect the general atmosphere.
- Is there an age limit when depression treatment is useless?
There is a common misconception that feeling depressed in old age is normal. In fact, undiagnosed depression in the elderly causes needless suffering for the family and the person himself, who could lead a fruitful life. When the elderly do go to the doctor, they usually complain of physical ailment, they are reluctant to discuss feelings of hopelessness, sadness, loss of interest in activities that usually give pleasure; they are reluctant to talk about endlessly protracted grief after a bereavement. Realizing that the symptoms of depression in the elderly are often blurred, many professionals are learning to recognize and treat latent depression. They recognize that some of the symptoms may be side effects of medications the older person is taking for other illnesses, or may be caused by comorbidities. Once depression is diagnosed, medication and/or psychotherapy can help the person return to a happier, more fulfilling life.
Once depression is diagnosed, medication and/or psychotherapy can help the person return to a happier, more fulfilling life.
- How not to become a victim of depression?
We can prevent situational or somatogenic depression by a healthy lifestyle, avoiding stressful situations, direct the organization of our time and space to strengthen psychological and physical immunity: physical activity, hobbies, meditation, psychotherapy. If we talk about depression that has already manifested itself (especially about endogenous depression, with all of the above signs), one cannot do without a specialist. A change of scenery and walks in the fresh air will no longer help, I would recommend not to waste time and consult a psychiatrist. And, of course, the most important thing in the prevention of depression is the environmentally friendly upbringing of our children, in love, support and care, since the ability to form a depressive reaction is laid in the early stages of growing up. It is due to a lack of attention from significant adults for the child.
It is due to a lack of attention from significant adults for the child.
Just about depression
29 March 2016
Just about depression
Artem Alekseevich Sergeev - psychiatrist of the Consultative Polyclinic No. 1 of the Regional Clinical Hospital No. 1
Depression! How often do we hear this word in everyday life, but it is far from always being used correctly, not every decrease in mood can be considered depression. Currently, a depressive episode is a condition characterized by low mood, loss of interests and pleasures, possibly motor and mental retardation, and lasting at least two weeks. This is an extremely generalized definition, since depression is extremely diverse and manifests itself in different ways in different people and in combination with various factors.
Mankind has long been familiar with mood disorders, in particular depression. This is how Hippocrates described states of depression and mania about 2500 years ago. Gradually ideas about affective disorders evolved. Modern ideas about depression were formulated in the late 19th century by the German psychiatrist Emil Kraepelin. Nowadays, the “monoamine” hypothesis is the most widespread, according to which mood disorders are based on an imbalance in the activity of neurotransmitters (dopamine, norepinephrine, serotonin).
Gradually ideas about affective disorders evolved. Modern ideas about depression were formulated in the late 19th century by the German psychiatrist Emil Kraepelin. Nowadays, the “monoamine” hypothesis is the most widespread, according to which mood disorders are based on an imbalance in the activity of neurotransmitters (dopamine, norepinephrine, serotonin).
The prevalence of "pure" (unipolar) depression is extremely high and ranges from 4% to 6%, according to WHO, while the risk of getting sick during life is 15-20%. Of this number, only 20% seek medical attention, and 2% require hospitalization. Up to 60-80% of depressions do not fall into the field of view of a psychiatrist and, at best, are treated by doctors of other specialties. Up to 25-30% of all patients seeking medical care in the outpatient department (polyclinics) show signs of a depressive disorder. Recurrent depressive disorder (“recurrent” depressive episodes) is the leading cause of disability worldwide, accounting for approximately 10. 5% of all cases. For comparison, such a reason as a fall and its consequences gives 4.6% of the total.
5% of all cases. For comparison, such a reason as a fall and its consequences gives 4.6% of the total.
There is no exhaustive data on the causes of mood disorders. However, certain risk factors for the development of depression are known, which include: early episodes of depression, the presence of mood disorders among relatives, especially close ones, suicidal attempts, female gender, the postpartum period, lack of social support (unfavorable financial circumstances), stressful life events (for example, divorce , death of a loved one), loneliness, severe physical illness, other mental illness. There is a very high risk of developing depression in people with one or another type of addiction (alcohol, drug, gaming). There are also many psychological theories of the risk of developing depression, for example, the famous psychoanalyst Z. Freud believed that a predisposition to depression is laid down in infancy as a result of a violation of the relationship between mother and child.
What are the manifestations of depression, what symptoms to look for in ourselves or people close to us? As mentioned above, depression is extremely multifaceted and can occur as a single disease or combined with other bodily and mental ailments. Here is a list of the most common symptoms, but it is far from exhaustive: low mood independent of the situation for most of the day. Decrease or loss of interest in activities that previously could bring satisfaction. Decrease in activity, drop in vitality and increased fatigue. In severe cases, inhibition of thinking, motor activity can be pronounced. Possible sleep disturbance, early awakening (a few hours before the scheduled time). Deterioration of mood in the morning or an increase in anxiety in the evening. Psychologically, a person can feel his "worthlessness", a decrease in self-esteem, experience ideas of guilt. Libido decreases, frigidity appears. When depression worsens, thoughts of suicide often join. Recently, so-called "somatized" depressions have often been encountered, which are not characterized by direct complaints of low mood, but melancholy, various tingling, constriction, pain throughout the body, difficulty breathing, loss of appetite. The functioning of the internal organs and systems of the body (often the gastrointestinal tract, cardiovascular system, etc.) may be disrupted.
The functioning of the internal organs and systems of the body (often the gastrointestinal tract, cardiovascular system, etc.) may be disrupted.
So, what to do if you find symptoms of depression. Of course, you need to contact a specialist, it is better if it is a psychiatrist. If you ignore your state of postponing "for later", it is possible that mild depression will gradually pass on its own, but this is the "ideal" option, and even in this case, delayed "side effects" may appear. If you look at the whole layer of the problem, it turns out that untreated depression is a risk factor for the development of a recurrent depressive episode in the future, dementia (dementia), significantly worsens the course of concomitant somatic diseases (for example, arterial hypertension, diabetes mellitus, etc.). Depression is dangerous with the risk of developing suicidal behavior, developing dependence on alcohol, drugs, leaving the family, from work, social exclusion. And in itself, a depressive state can hardly be called a pleasant episode in life, therefore, the sooner timely and qualified assistance is provided, the better the further prognosis.
In recent years, the treatment of depression has ceased to be the isolated prescription of psychotropic drugs. The so-called concept of rehabilitation treatment has been formed, the purpose of which is to restore the initial level of human functioning, restore cognitive functions, readapt the patient in the family and society. Modern antidepressants have long appeared, which have a good tolerability profile, significantly less side effects compared to the "old" generation. Not only antidepressants are used, but also anti-anxiety drugs, drugs that improve brain metabolism and help restore the structure of brain nerve cells. Diagnosis and treatment of concomitant diseases is carried out. Far from last in the treatment of depression is the “non-drug” side of the issue. So it is desirable to consult a psychotherapist (cognitive-behavioral methods are widely used), consultations of a physiotherapist (use of TRANSAIR methods, electrosleep). It is important to build the correct daily routine, sufficient rest, regular physical exercises with the appropriate level of load for each person.