What does anticholinergic mean
List, Side Effects, Uses, Warnings, and More
Anticholinergics: List, Side Effects, Uses, Warnings, and MoreMedically reviewed by Alan Carter, Pharm.D. — By Jacquelyn Cafasso — Updated on December 9, 2019
About anticholinergics
Anticholinergics are drugs that block the action of acetylcholine. Acetylcholine is a neurotransmitter, or a chemical messenger. It transfers signals between certain cells to affect how your body functions.
Anticholinergics can treat a variety of conditions, including:
- urinary incontinence
- overactive bladder (OAB)
- chronic obstructive pulmonary disorder (COPD)
- certain types of poisoning
They also help block involuntary muscle movements associated with certain diseases such as Parkinson’s disease. Sometimes, they’re used before surgery to help maintain body functions while a person is treated with anesthesia.
Read on for:
- a list of anticholinergic drugs
- information about how they work
- what you should know about their risks and side effects
Anticholinergics are only available with a doctor’s prescription. Examples of these drugs include:
- atropine (Atropen)
- belladonna alkaloids
- benztropine mesylate (Cogentin)
- clidinium
- cyclopentolate (Cyclogyl)
- darifenacin (Enablex)
- dicylomine
- fesoterodine (Toviaz)
- flavoxate (Urispas)
- glycopyrrolate
- homatropine hydrobromide
- hyoscyamine (Levsinex)
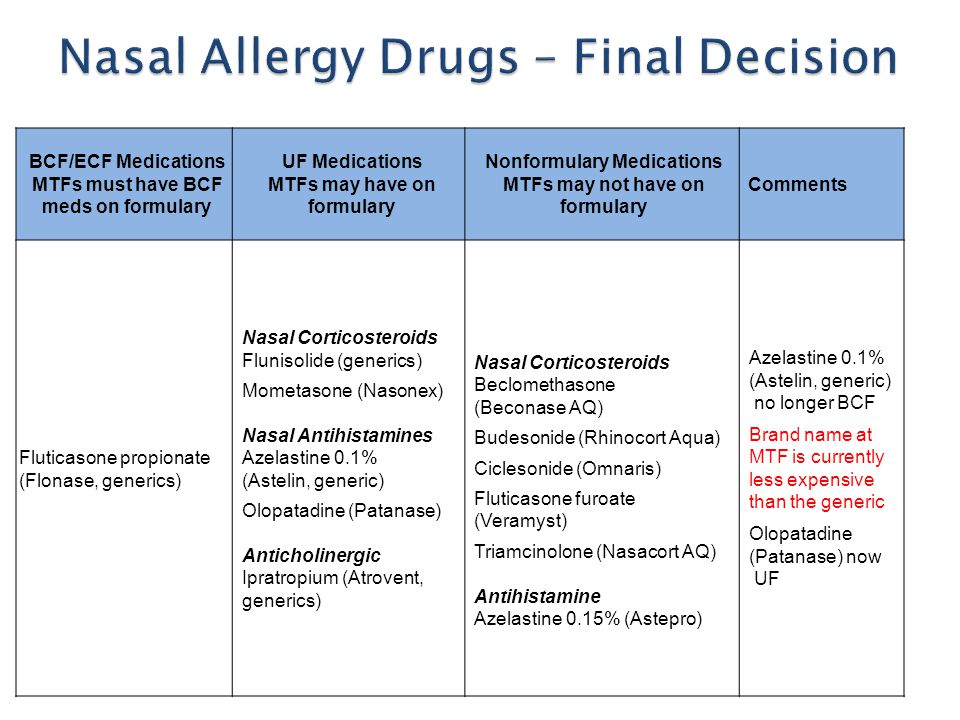
- ipratropium (Atrovent)
- orphenadrine
- oxybutynin (Ditropan XL)
- propantheline (Pro-banthine)
- scopolamine
- methscopolamine
- solifenacin (VESIcare)
- tiotropium (Spiriva)
- tolterodine (Detrol)
- trihexyphenidyl
- trospium
On March 21, 2022, Sandoz issued a voluntary recall of 13 lots of the drug orphenadrine citrate 100mg ER tablets due to the presence of nitrosamine. Nitrosamine, a known carcinogen with the potential to cause cancer, was found to exist in the drug at levels greater than the acceptable daily intake (ADI) as determined by the FDA. This recall is specific only to a handful of lot numbers and does not affect all orphenadrine tablets made by Sandoz. If you take orphenadrine citrate 100mg ER tablets, talk with your pharmacist or doctor and they will help you determine if your medication has been impacted by the recall.
This recall is specific only to a handful of lot numbers and does not affect all orphenadrine tablets made by Sandoz. If you take orphenadrine citrate 100mg ER tablets, talk with your pharmacist or doctor and they will help you determine if your medication has been impacted by the recall.
Although classified as an antihistamine to be taken for allergies and as a sleep aid, diphenhydramine (Benadryl) also has anticholinergic effects.
Each of these drugs works to treat specific conditions. Your doctor will choose the best drug for your condition.
DID YOU KNOW?Some anticholinergics are derived from plants of the deadly nightshade family called Solanaceae. Burning the roots, stems, and seeds of these plants releases the anticholinergics. Inhalation of the smoke has been used for hundreds of years to treat obstructive airway disease.
Anticholinergics block acetylcholine from binding to its receptors on certain nerve cells. They inhibit actions called parasympathetic nerve impulses.
These nerve impulses are responsible for involuntary muscle movements in the:
- gastrointestinal tract
- lungs
- urinary tract
- other parts of your body
The nerve impulses help control functions such as:
- salivation
- digestion
- urination
- mucus secretion
Blocking acetylcholine signals can decrease:
- involuntary muscle movement
- digestion
- mucus secretion
That’s why these drugs can cause certain side effects, such as:
- retaining urine
- having a dry mouth
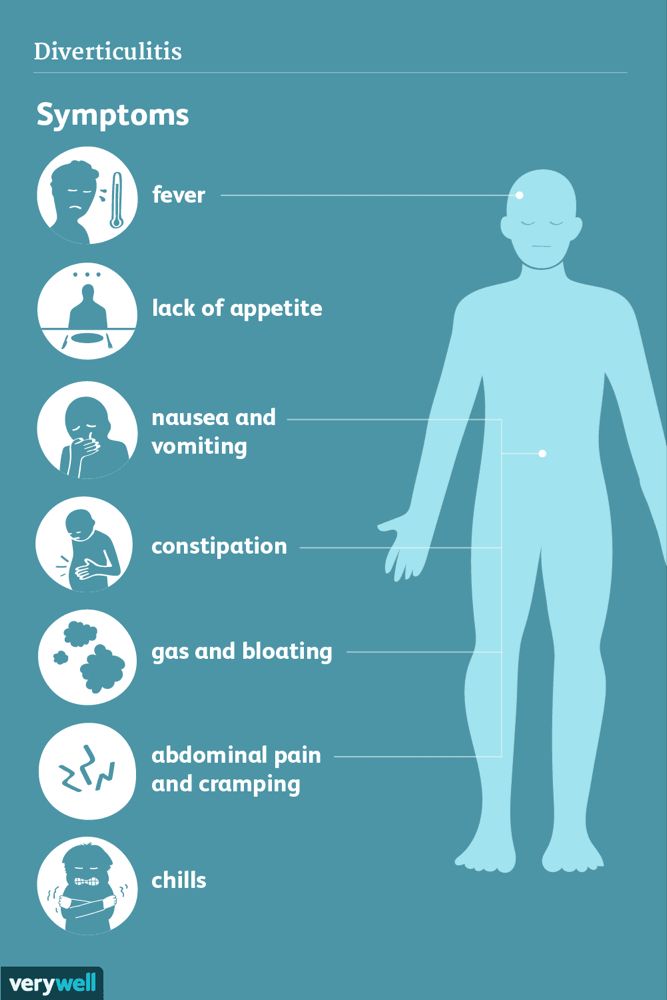
Anticholinergics are used to treat a variety of conditions. These include:
- chronic obstructive pulmonary disease (COPD)
- overactive bladder and incontinence
- gastrointestinal disorders, such as diarrhea
- asthma
- dizziness and motion sickness
- poisoning caused by toxins such as organophosphates or muscarine, which may be found in some insecticides and poisonous mushrooms
- symptoms of Parkinson’s disease, such as abnormal involuntary muscle movement
Anticholinergics can also be used as muscle relaxants during surgery to assist with anesthesia. They help:
They help:
- keep the heartbeat normal
- relax the person
- decrease saliva secretions
Some doctors prescribe anticholinergics for off-label use to help decrease excessive sweating. The anticholinergics used most for this treatment are:
- glycopyrrolate cream
- oxybutynin oral tablets
As do many drugs, anticholinergics come with several warnings.
Heat exhaustion and heat stroke
Anticholinergics decrease how much you sweat, which can cause your body temperature to rise. While taking one of these drugs, be extra careful not to become overheated during:
- exercise
- hot baths
- hot weather
Decreased sweating can put you at risk of heat stroke.
Overdose and alcohol
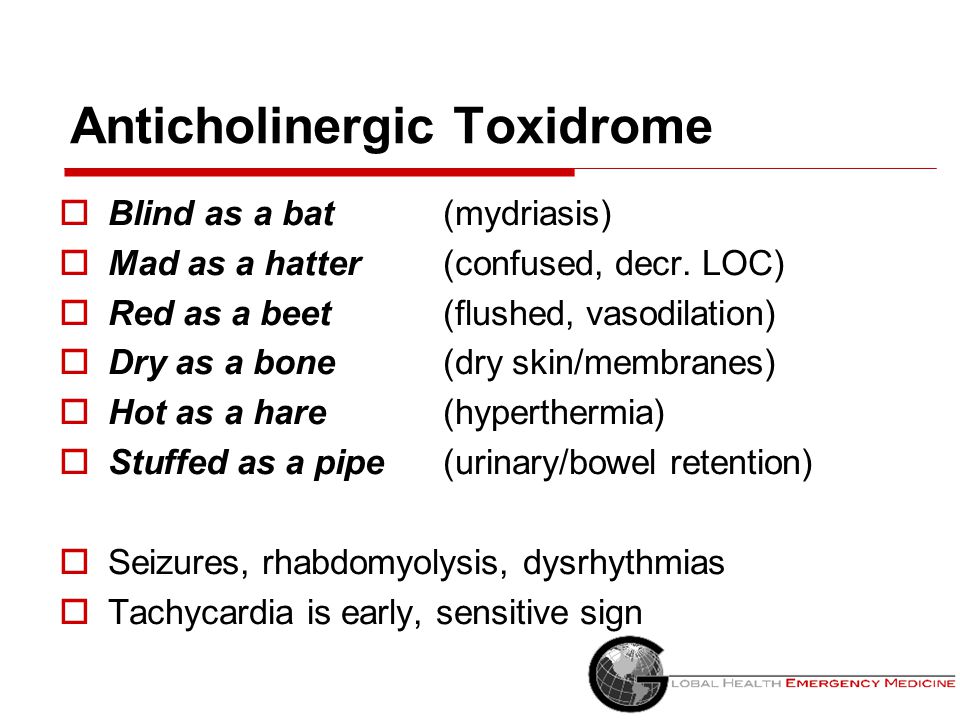
Using too much of an anticholinergic drug can result in unconsciousness or even death. These effects can also happen if you take anticholinergics with alcohol. Signs of an overdose include:
- dizziness
- severe drowsiness
- fever
- severe hallucinations
- confusion
- trouble breathing
- clumsiness and slurred speech
- fast heartbeat
- flushing and warmth of the skin
If you think you or someone you know has taken too much of this drug, call your doctor or seek guidance from the American Association of Poison Control Centers at 1-800-222-1222 or through their online tool.
If your symptoms are severe, call 911 or go to the nearest emergency room right away.
Conflicting conditions
Anticholinergics can be used to treat many conditions, but they aren’t for everyone. For example, these drugs aren’t usually prescribed for older people.
Anticholinergics are known to cause confusion, memory loss, and worsening mental function in people who are older than 65 years. In fact, recent studies have linked use of anticholinergics with increased risk of dementia.
Also, people with the following conditions shouldn’t use anticholinergics:
- myasthenia gravis
- hyperthyroidism
- glaucoma
- enlarged prostate
- hypertension (high blood pressure)
- urinary tract blockage
- increased heart rate (tachycardia)
- heart failure
- severe dry mouth
- hiatal hernia
- severe constipation
- liver disease
- Down syndrome
Tell your doctor if you have any of these conditions.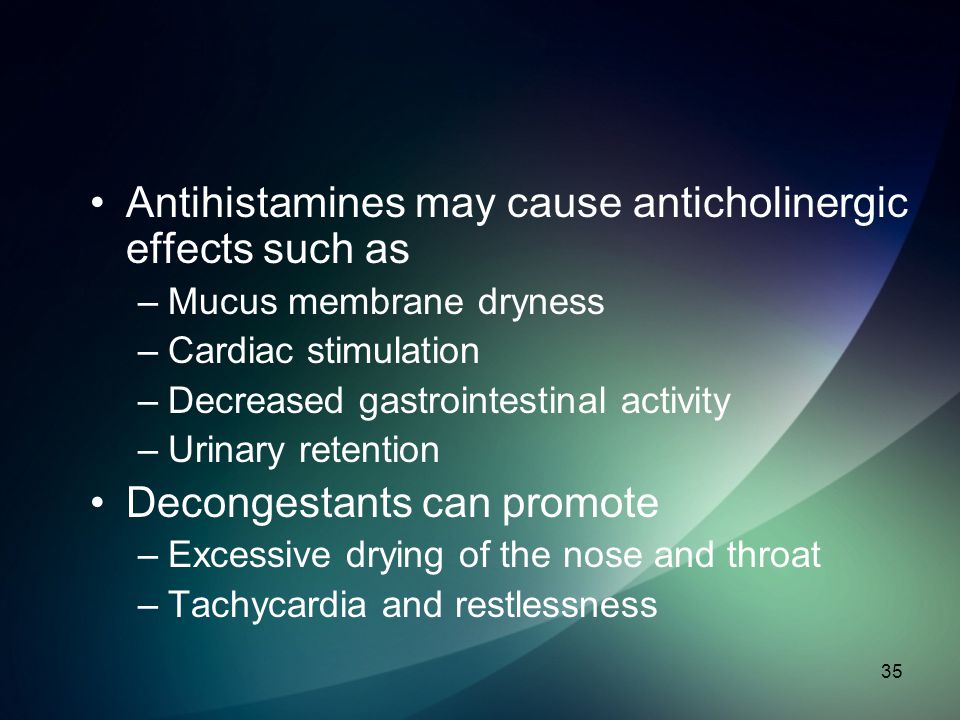 Also, tell your doctor if you have a history of allergies to anticholinergics.
Also, tell your doctor if you have a history of allergies to anticholinergics.
AVOIDING USE IN OLDER ADULTSThe American Geriatrics Society strongly recommends avoiding the use of anticholinergic medications in older adults. This is because seniors may be more likely to experience unwanted side effects than younger people.
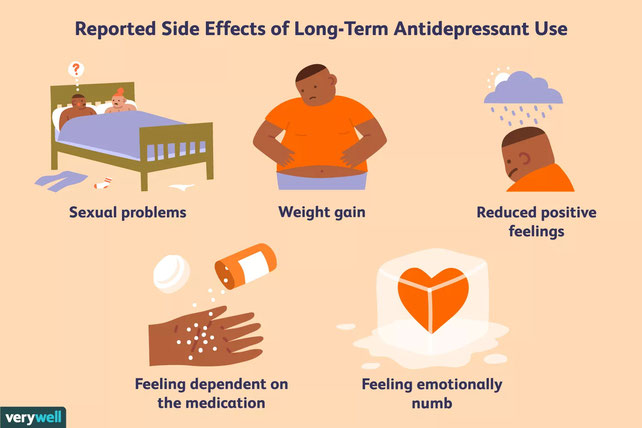
Even when using this drug properly, side effects can happen. The possible side effects of anticholinergics depend on the specific drug and dosage you take.
Side effects can include:
- dry mouth
- blurry vision
- constipation
- drowsiness
- sedation
- hallucinations
- memory problems
- trouble urinating
- confusion
- delirium
- decreased sweating
- decreased saliva
DEMENTIA WARNINGLong-term use of anticholinergics, as well as use of these drugs in older people, has been linked with an increased risk of dementia.
If you’ve been prescribed one of these drugs and have concerns about this risk, be sure to talk to your doctor.
Anticholinergics can be used to treat a variety of conditions. If you think one of these drugs could help you, talk to your doctor.
Your doctor can determine if treatment with an anticholinergic would be a good option for you. They can also answer any questions you have about:
- risks
- side effects
- what to expect with treatment
Anticholinergic drugs block the action of a neurotransmitter called acetylcholine. This inhibits nerve impulses responsible for involuntary muscle movements and various bodily functions.
These drugs can treat a variety of conditions, from overactive bladder to chronic obstructive pulmonary disorder.
Last medically reviewed on August 9, 2019
How we vetted this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Acetylcholine. (2001). Neuroscience. 2nd edition.
ncbi.nlm.nih.gov/books/NBK11143/ - American Geriatrics Society 2015 updated Beers Criteria for potentially inappropriate medication use in older adults. (2015). DOI:
10.1111/jgs.13702 - Anticholinergics. (2015).
parkinsons.org.uk/content/anticholinergics - Diphenhydramine. (n.d.).
pubchem.ncbi.nlm.nih.gov/compound/Diphenhydramine#section=Interactions - Gray SL, et al. (2015). Cumulative use of strong anticholinergics and incident dementia: A prospective cohort study.
- Gray SL, et al. (2018). Anticholinergic drugs and dementia in older adults. DOI:
10.1136/bmj.k1722 - Rochon PA, et al. (2019). Drug prescribing for older adults.
uptodate.com/contents/drug-prescribing-for-older-adults?search=anticholinergic&source=search_result&selectedTitle=5~150&usage_type=default&display_rank=5 - Scullion JE.
 (2007). The development of anticholinergics in the management of COPD.
(2007). The development of anticholinergics in the management of COPD.
ncbi.nlm.nih.gov/pmc/articles/PMC2692120/
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Dec 9, 2019
By
Jacquelyn Cafasso
Edited By
Aline (Ren) Dias
Aug 9, 2019
Medically Reviewed By
Alan Carter, PharmD
Share this article
Medically reviewed by Alan Carter, Pharm.D. — By Jacquelyn Cafasso — Updated on December 9, 2019
related stories
What Are the Best Medications for an Overactive Bladder?
What Are the First-Line Treatments for COPD?
Treatment Options for Waldenstrom Macroglobulinemia
How Does Menopause Affect OAB?
Hyperhidrosis Disorder (Excessive Sweating)
Read this next
What Are the Best Medications for an Overactive Bladder?
Medically reviewed by Alan Carter, Pharm.
 D.
D.Some people need drugs to treat symptoms of overactive bladder. Weigh your options, and check out which treatment may be right for you.
READ MORE
What Are the First-Line Treatments for COPD?
Medically reviewed by Judith Marcin, M.D.
If you’ve been diagnosed with COPD, your doctor will work with you to determine the best treatment options. Read about first-line treatments for COPD.
READ MORE
Treatment Options for Waldenstrom Macroglobulinemia
Waldenstrom macroglobulinemia (WM) is a rare blood cancer. There’s no cure for WM, but many different treatments are available to help manage symptoms.
READ MORE
How Does Menopause Affect OAB?
Medically reviewed by Kimberly Dishman, MSN, WHNP-BC, RNC-OB
Menopause raises your risk of overactive bladder (OAB).
 Learn about the link between these conditions and how you manage your symptoms.
Learn about the link between these conditions and how you manage your symptoms.READ MORE
Hyperhidrosis Disorder (Excessive Sweating)
Medically reviewed by Xixi Luo, MD
Hyperhidrosis can be uncomfortable. Learn what causes it, and explore treatment options that can provide relief.
READ MORE
Drug Allergy Symptoms
Medically reviewed by Zara Risoldi Cochrane, Pharm.D., M.S., FASCP
Drug allergy symptoms can range from mild to severe. Learn these symptoms and how to react to each type.
READ MORE
How to Treat an Overactive Bladder at Night
Medically reviewed by Graham Rogers, M.D.
If you have an overactive bladder at night, you may have nocturia. Read more about what causes it and how to treat and prevent it.
READ MORE
Vasomotor Rhinitis
Medically reviewed by Graham Rogers, M.
 D.
D.Vasomotor rhinitis, or nonallergic rhinitis, is inflammation of the membranes inside the nose. Learn what causes it and how it's treated.
READ MORE
Understanding Heat Exhaustion: Symptoms, Tips for Self-Care, and More
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
READ MORE
Can Antidepressants Be Used for IBS Treatment?
Medically reviewed by Jennie Olopaade, PharmD, RPH
Antidepressants may be used as a treatment option for IBS in some cases. Learn the types and when they may be recommended.
READ MORE
Side Effects, Dosage, Uses, and More
Highlights for oxybutynin
- Oxybutynin immediate-release oral tablet is available in a generic version only. The extended-release oral tablet is available as a generic and a brand-name drug.
 Brand name: Ditropan XL.
Brand name: Ditropan XL. - In addition to the tablets, oxybutynin comes as an oral syrup. It also comes as a gel and a patch that you apply to your skin.
- Oxybutynin oral tablet is used to treat overactive bladder
- Swelling warning: Oxybutynin can cause angioedema (swelling) around your eyes, lips, genitals, hands, or feet due to an allergic reaction. If you have any of these symptoms, stop taking this drug and seek emergency help right away.
- Central nervous system side effects warning: This drug may cause drowsiness, confusion, agitation, and hallucinations (seeing or hearing things that aren’t real). This is most likely to happen during the first few months you take this medication or after your dosage is increased. If you have these side effects, your doctor may decrease your dosage or have you stop taking this drug.
- Dementia: Research shows this drug can raise your risk of dementia.

Oxybutynin is a prescription drug. It comes as an immediate-release oral tablet, extended-release oral tablet, oral syrup, topical gel, and topical patch.
The oral tablet is available in a generic version only. The extended-release tablet is available as a generic and as the brand-name drug Ditropan XL.
Generic drugs usually cost less than the brand-name version. In some cases, they may not be available in all strengths or forms as the brand-name drug.
Oxybutynin may be used as part of a combination therapy. That means you need to take it with other drugs.
Why it’s used
Oxybutynin is used to treat overactive bladder. Symptoms of this condition can include:
- urinating more often than usual
- feeling like you need to urinate more often
- urinary leakage
- painful urination
- being unable to hold your urine
The extended-release form of this drug is also used to treat children (ages 6 years and older) with overactive bladder caused by a neurological condition such as spina bifida.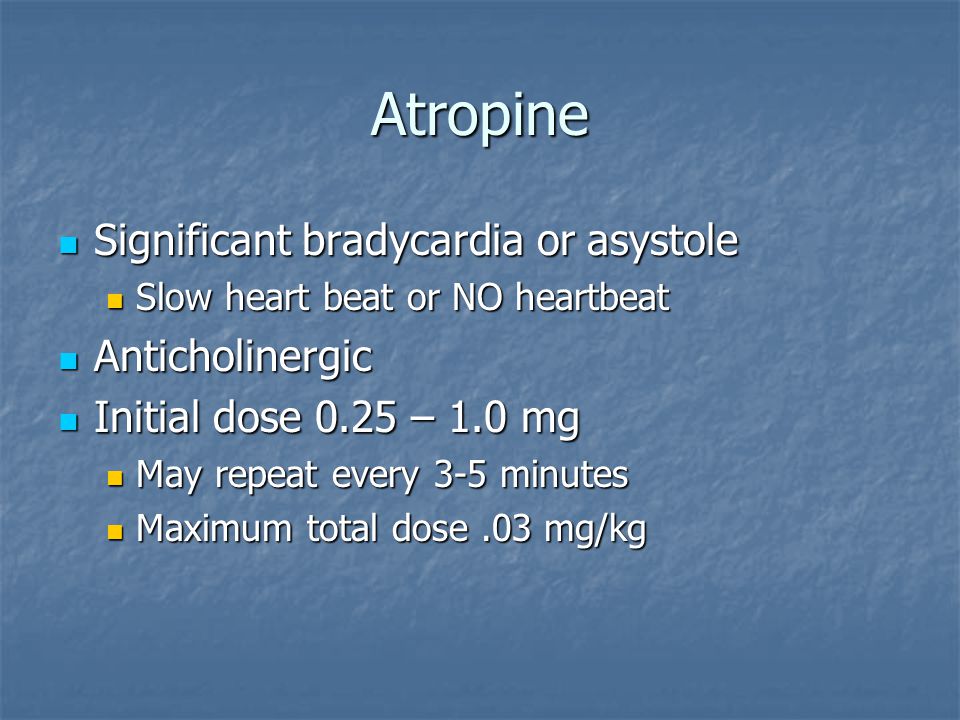
How it works
Oxybutynin belongs to a class of drugs called anticholinergics/antimuscarinics. A class of drugs is a group of medications that work in a similar way. These drugs are often used to treat similar conditions.
Oxybutynin works by relaxing the muscles of your bladder. This decreases your sudden need to urinate, having to urinate often, and leaking in between bathroom visits.
Drowsiness warning
- This drug can cause drowsiness. You shouldn’t drive, use machinery, or do other activities that require alertness until you know how this drug affects you.
Oxybutynin oral tablet may cause drowsiness as well as other side effects.
More common side effects
The more common side effects that can occur with oxybutynin include:
- being unable to urinate
- constipation
- dry mouth
- blurry vision
- dizziness
- drowsiness
- sweating less than usual (raises your risk of overheating, having a fever, or getting heat stroke if you’re in warm or hot temperatures)
- trouble sleeping
- headache
If these effects are mild, they may go away within a few days or a couple of weeks. If they’re more severe or don’t go away, talk to your doctor or pharmacist.
If they’re more severe or don’t go away, talk to your doctor or pharmacist.
Serious side effects
Call your doctor right away if you have serious side effects. Call 911 if your symptoms feel life-threatening or if you think you’re having a medical emergency. Serious side effects and their symptoms can include the following:
- not being able to empty your bladder
- swelling around your eyes, lips, genitals, hands, or feet
Disclaimer: Our goal is to provide you with the most relevant and current information. However, because drugs affect each person differently, we cannot guarantee that this information includes all possible side effects. This information is not a substitute for medical advice. Always discuss possible side effects with a healthcare provider who knows your medical history.
Oxybutynin oral tablet can interact with other medications, vitamins, or herbs you may be taking. An interaction is when a substance changes the way a drug works. This can be harmful or prevent the drug from working well.
This can be harmful or prevent the drug from working well.
To help avoid interactions, your doctor should manage all of your medications carefully. Be sure to tell your doctor about all medications, vitamins, or herbs you’re taking. To find out how this drug might interact with something else you’re taking, talk to your doctor or pharmacist.
Examples of drugs that can cause interactions with oxybutynin are listed below.
Depression drugs
Oxybutynin may affect how these drugs are absorbed by your body. Taking these drugs with oxybutynin may also increase your risk of side effects. Examples of these drugs include:
- amitriptyline
- nortriptyline
Allergy drugs
Oxybutynin may affect how these drugs are absorbed by your body. Taking these drugs with oxybutynin may also increase your risk of side effects. Examples of these drugs include:
- chlorpheniramine
- diphenhydramine
Psychosis and schizophrenia drugs
Oxybutynin may affect how these drugs are absorbed by your body. Taking these drugs with oxybutynin may also increase your risk of side effects. Examples of these drugs include:
Taking these drugs with oxybutynin may also increase your risk of side effects. Examples of these drugs include:
- chlorpromazine
- thioridazine
Antifungal drugs
Certain antifungal drugs will increase the level of oxybutynin in your body. This will raise your risk of side effects. Examples of these drugs include:
- ketoconazole
- itraconazole
Dementia drugs
Oxybutynin may worsen your dementia symptoms if you take it with certain dementia drugs. These drugs, called cholinesterase inhibitors, include:
- donepezil
- galantamine
- rivastigmine
Disclaimer: Our goal is to provide you with the most relevant and current information. However, because drugs interact differently in each person, we cannot guarantee that this information includes all possible interactions. This information is not a substitute for medical advice. Always speak with your healthcare provider about possible interactions with all prescription drugs, vitamins, herbs and supplements, and over-the-counter drugs that you are taking.
This drug comes with several warnings.
Allergy warning
Oxybutynin may cause a severe allergic reaction. Symptoms can include:
- trouble breathing
- swelling of your throat or tongue
- hives
- severe skin reactions
Don’t take this drug again if you’ve ever had an allergic reaction to it before. Taking it a second time after an allergic reaction could be fatal.
Alcohol warning
You shouldn’t drink alcohol while taking oxybutynin. Alcohol raises your risk of serious side effects, such as drowsiness and dizziness. Alcohol can also worsen your overactive bladder symptoms.
Warnings for certain groups
For people with autonomic neuropathy: Oxybutynin can make your stomach problems worse. Use this drug with caution if you have this condition.
For people with bladder outlet obstruction: Oxybutynin may increase your risk of not being able to empty your bladder.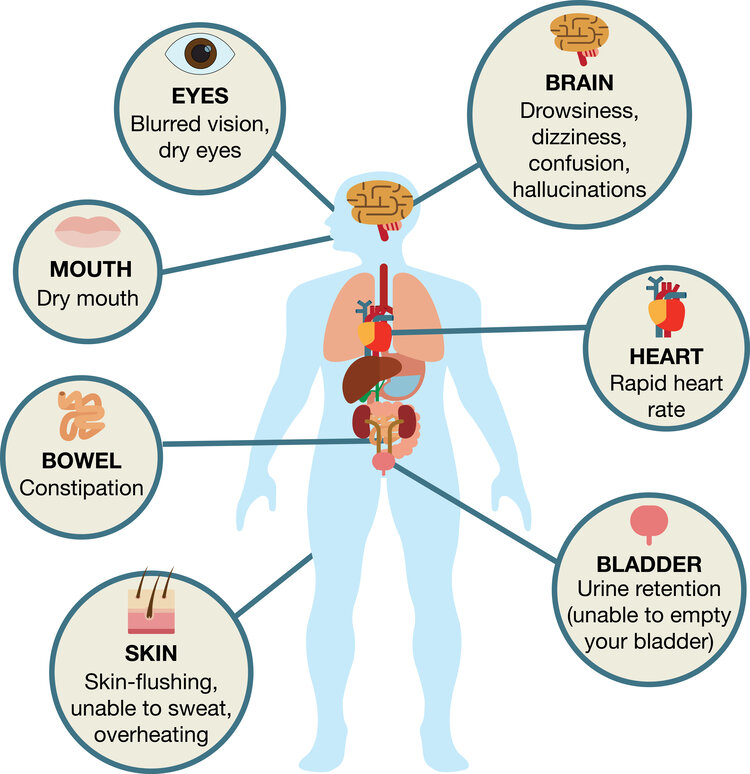
For people with stomach problems: Oxybutynin may cause more stomach problems if you have a history of ulcerative colitis, stomach pain, or reflux.
For people with myasthenia gravis: Oxybutynin may make your symptoms worse.
For people with dementia: If you’re treating your dementia with a drug called a cholinesterase inhibitor, oxybutynin may worsen your dementia symptoms. Your doctor can tell you more.
For pregnant women: Oxybutynin is a pregnancy category B drug. That means two things:
- Research in animals has not shown a risk to the fetus when the mother takes the drug.
- There aren’t enough studies done in humans to show if the drug poses a risk to the fetus.
Talk to your doctor if you’re pregnant or planning to become pregnant. Animal studies do not always predict the way humans would respond. Therefore, this drug should only be used during pregnancy if clearly needed.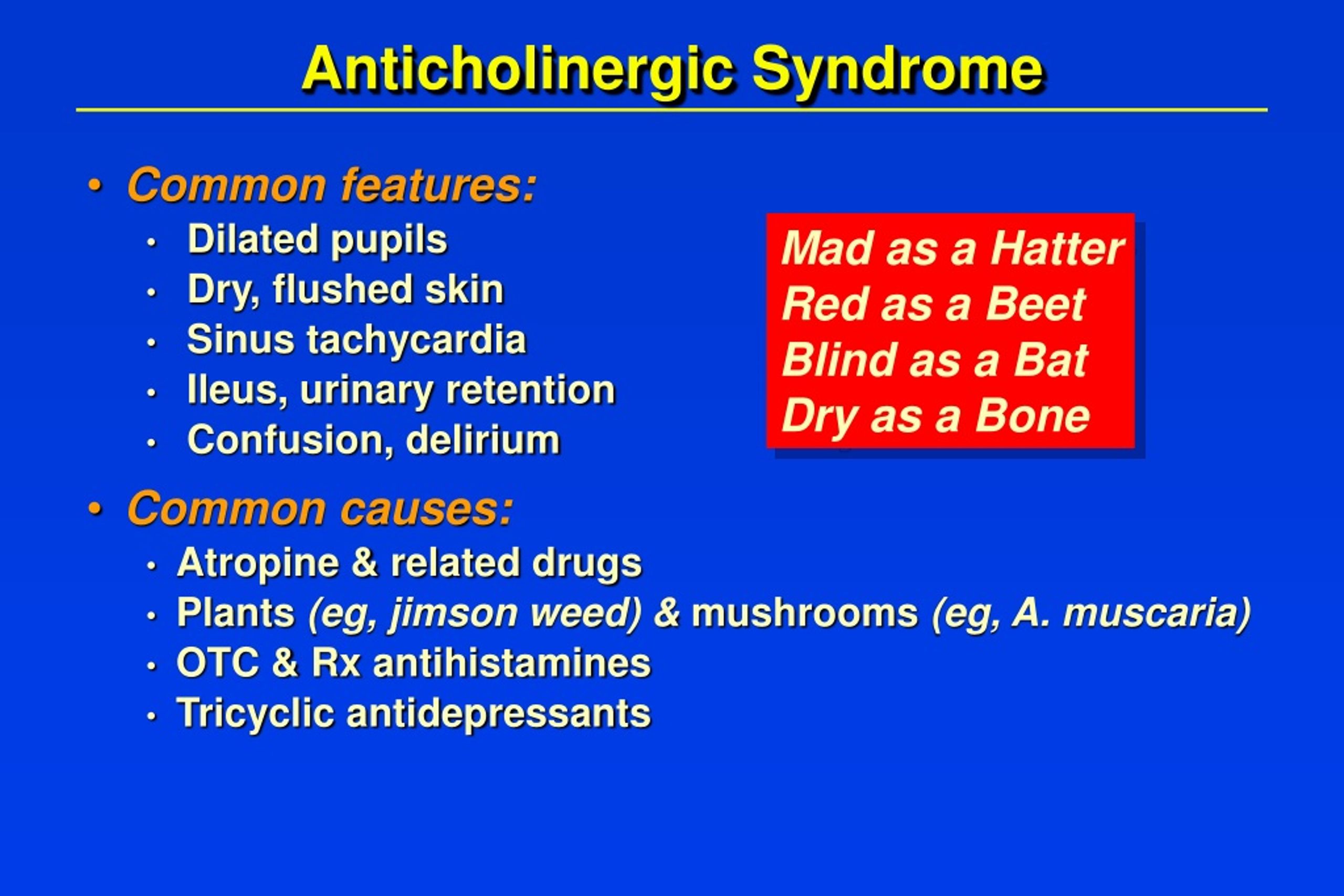
For women who are breastfeeding: It isn’t known if oxybutynin passes into breast milk. If it does, it may cause side effects in a child who is breastfed. Talk to your doctor if you breastfeed your baby. You may need to decide whether to stop breastfeeding or stop taking this medication.
For children: The safety and effectiveness of oxybutynin in children younger than 6 years haven’t been established.
All possible dosages and forms may not be included here. Your dose, form, and how often you take it will depend on:
- your age
- the condition being treated
- how severe your condition is
- other medical conditions you have
- how you react to the first dose
Forms and strengths
Generic: oxybutynin
- Form: immediate-release oral tablet
- Strength: 5 mg
- Form: extended-release oral tablet
- Strengths: 5 mg, 10 mg, 15 mg
Brand: Ditropan XL
- Form: extended-release oral tablet
- Strengths: 5 mg, 10 mg, 15 mg
IMMEDIATE-RELEASE ORAL TABLET
Adult dosage (ages 18–64 years)
- Typical starting dosage: 5 mg taken by mouth two to three times per day.

- Maximum dosage: 5 mg taken by mouth four times per day.
Child dosage (ages 6–17 years)
- Typical starting dosage: 5 mg taken by mouth two times per day.
- Maximum dosage: 5 mg taken by mouth three times per day.
Senior dosage (ages 65 years and older)
Typical starting dosage: Your doctor may start your dosage at 2.5 mg taken two to three times per day.
EXTENDED-RELEASE ORAL TABLET
Adult dosage (ages 18 years and older)
- Typical starting dosage: 5–10 mg taken by mouth one time per day at the same time each day.
- Dosage increases: Your doctor may increase your dosage by 5 mg at a time on a weekly basis, up to a maximum of 30 mg per day.
Child dosage (ages 6–17 years)
- Typical starting dosage: 5 mg taken by mouth one time per day at the same time each day.
- Dosage increases: Your doctor may increase your dosage by 5 mg at a time, up to a maximum of 20 mg per day.

Dosage for overactive bladder associated with a neurological condition
EXTENDED-RELEASE ORAL TABLET
Adult dosage (ages 18 years and older)
- Typical starting dosage: 5–10 mg taken by mouth one time per day at the same time each day.
- Dosage increases: Your doctor may increase your dosage by 5 mg at a time on a weekly basis, up to a maximum of 30 mg per day.
Child dosage (ages 6–17 years)
- Typical starting dosage: 5 mg taken by mouth one time per day at the same time each day.
- Dosage increases: Your doctor may increase your dosage by 5 mg at a time, up to a maximum of 20 mg per day.
Disclaimer: Our goal is to provide you with the most relevant and current information. However, because drugs affect each person differently, we cannot guarantee that this list includes all possible dosages. This information is not a substitute for medical advice. Always speak with your doctor or pharmacist about dosages that are right for you.
Always speak with your doctor or pharmacist about dosages that are right for you.
Oxybutynin is used for long-term treatment. It comes with serious risks if you don’t take it as prescribed.
What to do if you miss a dose: If you forget to take your dose, take it as soon as you remember. If it’s just a few hours before the time of your next dose, then wait and only take one dose at that time. Never try to catch up by taking two doses at once. This could result in toxic side effects.
How to tell if the drug is working: Your symptoms of overactive bladder or bladder instability may get better.
If you don’t take it at all: Your symptoms of overactive bladder or bladder instability won’t improve.
If you skip or miss doses: You may not see the full benefit of this medication.
If you take too much: You may experience more side effects if you take too much of this drug. These include:
- dizziness
- headache
- not being able to urinate
- constipation
- hallucinations (seeing or hearing things that aren’t real)
- confusion
- drowsiness
If you think you’ve taken too much of this drug, call your doctor or local poison control center. If your symptoms are severe, call 911 or go to the nearest emergency room right away.
If your symptoms are severe, call 911 or go to the nearest emergency room right away.
Keep these considerations in mind if your doctor prescribes oxybutynin for you.
General
- You can take oxybutynin with or without food.
- You should take the extended-release tablet at about the same time each day.
- You can cut or crush the immediate-release tablet. However, you must swallow the extended-release tablet whole. Don’t chew, divide, or crush it.
Storage
- Store oxybutynin at a temperature as close to 77°F (25°C) as possible. You can store it briefly at a temperature between 59°F and 86°F (15°C and 30°C).
- Keep this drug away from light.
- Don’t store this medication in moist or damp areas, such as bathrooms.
Refills
A prescription for this medication is refillable. You should not need a new prescription for this medication to be refilled. Your doctor will write the number of refills authorized on your prescription.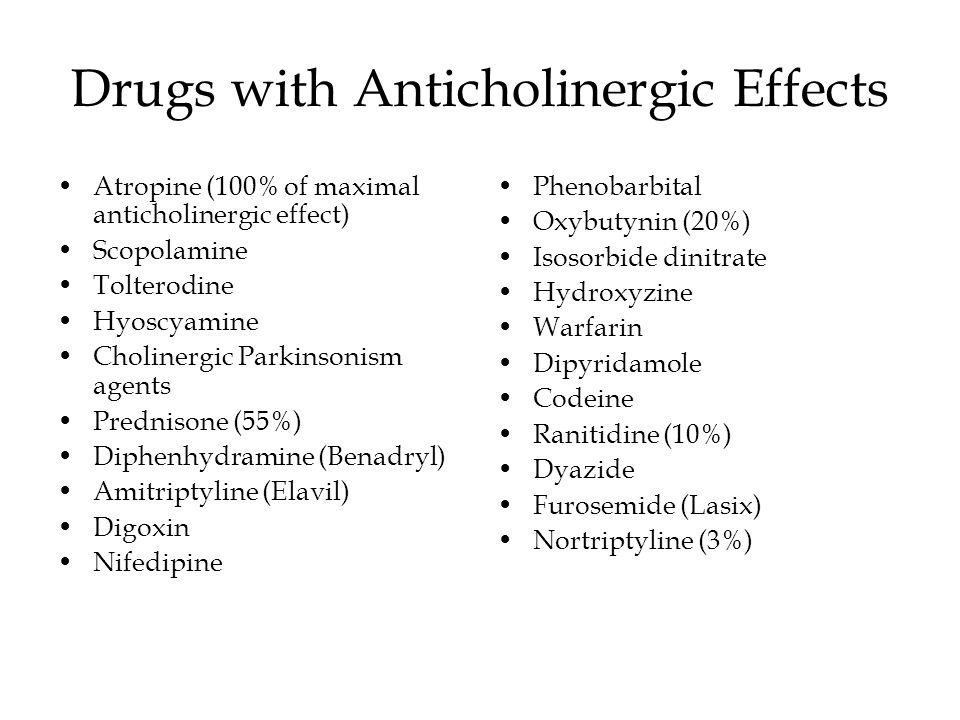
Travel
When traveling with your medication:
- Always carry your medication with you. When flying, never put it into a checked bag. Keep it in your carry-on bag.
- Don’t worry about airport x-ray machines. They can’t hurt your medication.
- You may need to show airport staff the pharmacy label for your medication. Always carry the original prescription-labeled box with you.
- Don’t put this medication in your car’s glove compartment or leave it in the car. Be sure to avoid doing this when the weather is very hot or very cold.
Your diet
Caffeine may worsen your symptoms of overactive bladder. It may make this drug less effective in treating your condition. You should limit your caffeine intake while taking oxybutynin.
Insurance
Many insurance companies require a prior authorization for this drug. This means your doctor will need to get approval from your insurance company before your insurance company will pay for the prescription.
There are other drugs available to treat your condition. Some may be more suitable for you than others. Talk to your doctor about possible alternatives.
Disclaimer: Healthline has made every effort to make certain that all information is factually correct, comprehensive, and up-to-date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or other healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.
Scientists: conventional drugs reduce brain activity
Sign up for our 'Context' newsletter: it will help you understand the events.
The author of the photo,
Photo caption,People who take several drugs with anticholinergic effects are most at risk
diseases - can lead to deterioration of brain function and increase the risk of death.
Nearly half of the world's population over the age of 65 is reported to be taking one or more of these drugs.
Those most at risk are people whose treatment involves taking a whole "cocktail" of pills, according to a study published in the Journal of the American Association of Gerontologists.
At the same time, its authors note that in no case should you immediately stop taking the medicines prescribed for you.
Anticholinergic effect
Researchers focused on drugs that affect acetylcholine, the chemical responsible for signaling from one brain cell to another.
Many of the most common drugs have been found to have anticholinergic side effects, that is, they reduce the ability of brain cells to transmit nerve signals.
The scientists compiled a list of 80 drugs, scoring their anticholinergic effects on a scale of one to three: one for little effect on the brain and three for major.
Gerontologists then calculated the total effect of medications taken by 13,000 volunteers over the age of 65.
So, for example, a patient taking one drug with a strong side effect (3 points) and two with a minor one (another 2 points), in total, reduces the capabilities of his brain quite a lot.
Consequences and side effects
According to a study conducted from 1991 to 1993, one in five patients who took drugs with a total score of more than four died during this period. At the same time, among people who did not take anticholinergic drugs, the mortality rate was only 7%.
Patients with high scores (scores of five or more) experienced a 4% decrease in brain function.
Scientists point out that it is only possible to speak with certainty about the relationship between the use of certain medications and mortality, and not that the drugs themselves lead to the death of patients.
"Physicians should regularly check which medications their elderly patients are taking. And pay attention not only to those that were prescribed by prescription, but also those simply bought in a pharmacy. If possible, we recommend avoiding prescribing patients with several anticholinergic drugs at once. action," said study leader Chris Fox.
"Doctors started prescribing more drugs"
According to the head of the British Royal College of General Practitioners, Claire Gerada, the results of the study should be taken very seriously.
"The main thing is not to worry and be sure to consult your doctor or pharmacist. And in no case should you stop taking your prescribed medications without first consulting a doctor," she notes.
According to Claire Jerada, British doctors understand the dangers of drug cocktails and review their patients' medications every 15 months.
Many doctors note that the data for the current study were obtained in the early 90s, and that since then the situation could have changed, and for the worse.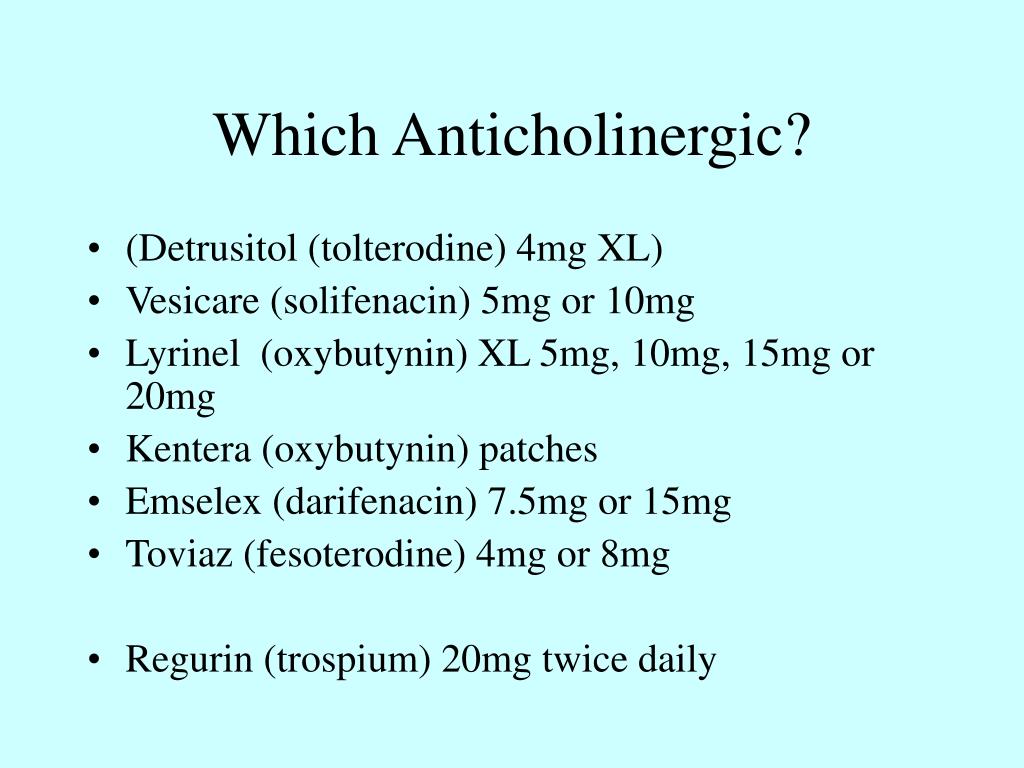
According to pharmacologist Ian Maidment, the use of anticholinergic drugs "probably increased because, in general, doctors began to prescribe more drugs than before."
Anticholinergic load
0064, the topic of drugs that affect the cholinergic system was touched upon. Now let's discuss the concept of anticholinergic load - this is a cumulative effect when several drugs (drugs) with anticholinergic potential are taken simultaneously. These include drugs that interfere with the action of acetylcholine on the corresponding receptors. It is important to understand that when using one drug with anticholinergic activity, there may not be a negative effect, but when several drugs are combined, this effect becomes clinically significant.
The most frequently mentioned in a negative way is the effect on the central nervous system, namely on cognitive functions. This is due to the fact that the cholinergic pathways in the brain are mainly associated with the processes of learning and short-term memory. The problem is especially acute for elderly patients. In this age group, cognitive functions play an important role and significantly affect the quality of life.
The problem is especially acute for elderly patients. In this age group, cognitive functions play an important role and significantly affect the quality of life.
Elderly patients are more susceptible to cognitive anticholinergic effects. There are several reasons for this:
- inhibition of the biotransformation of drugs in the liver and a decrease in renal excretion;
- increased permeability of the blood-brain barrier;
- slowing down and reducing cholinergic transmission.
In Russia, not so many drugs from the group of M-cholinergic blockers are registered, the main pharmacological action of which is associated with the blockade of M-cholinergic receptors. These include low-selective atropine and platifillin; trospium chloride, oxybutynin, and solifenacin for the treatment of overactive bladder; hyoscine butyl bromide, used for spasms of the gastrointestinal tract; trihexyphenidyl - for the treatment of Parkinson's disease. Preparations for local (tropicamide, cyclopentolate hydrochloride in eye drops) and inhalation use (ipratropium bromide, tiotropium bromide, glycopyrronium bromide) are absorbed into the systemic circulation in low concentrations, and therefore their anticholinergic potential is minimal. There are many more drugs for which the effect on M-cholinergic receptors are not the main pharmacological effect. These include: antidepressants (amitriptyline, imipramine, venlafaxine), neuroleptics (clozapine, olanzapine, quetiapine, thioridazine, alimemazine), h2-histamine receptor blockers (clemastine, doxylamine, hydroxyzine, cetirizine, levocetirizine, loratadine, desloratadine), diuretics (furosemide , chlorthalidone), etc. The anticholinergic potential is estimated using special scales: for example, Anticholinergic Cognitive Burden (ACB). It awards drugs from 1 to 3 points, depending on the potential risk of adverse events (such as impaired reaction time, attention, memory). Depending on the total score for this school, the clinician may decide to continue the previously prescribed therapy or its correction.
There are many more drugs for which the effect on M-cholinergic receptors are not the main pharmacological effect. These include: antidepressants (amitriptyline, imipramine, venlafaxine), neuroleptics (clozapine, olanzapine, quetiapine, thioridazine, alimemazine), h2-histamine receptor blockers (clemastine, doxylamine, hydroxyzine, cetirizine, levocetirizine, loratadine, desloratadine), diuretics (furosemide , chlorthalidone), etc. The anticholinergic potential is estimated using special scales: for example, Anticholinergic Cognitive Burden (ACB). It awards drugs from 1 to 3 points, depending on the potential risk of adverse events (such as impaired reaction time, attention, memory). Depending on the total score for this school, the clinician may decide to continue the previously prescribed therapy or its correction.
Polina Litvinenko, clinical pharmacologist
References:
1. Boustani, Malaz & Campbell, Noll & Munger, Stephanie & Fox, Chris. (2008). Impact of anticholinergics on the aging brain: A review and practical application.