Dissociative identity disorder is most commonly found in
Dissociative Disorders | NAMI: National Alliance on Mental Illness
Dissociative disorders are characterized by an involuntary escape from reality characterized by a disconnection between thoughts, identity, consciousness and memory. People from all age groups and racial, ethnic and socioeconomic backgrounds can experience a dissociative disorder.
Up to 75% of people experience at least one depersonalization/derealization episode in their lives, with only 2% meeting the full criteria for chronic episodes. Women are more likely than men to be diagnosed with a dissociative disorder.
The symptoms of a dissociative disorder usually first develop as a response to a traumatic event, such as abuse or military combat, to keep those memories under control. Stressful situations can worsen symptoms and cause problems with functioning in everyday activities. However, the symptoms a person experiences will depend on the type of dissociative disorder that a person has.
Treatment for dissociative disorders often involves psychotherapy and medication. Though finding an effective treatment plan can be difficult, many people are able to live healthy and productive lives.
Symptoms
Symptoms and signs of dissociative disorders include:
- Significant memory loss of specific times, people and events
- Out-of-body experiences, such as feeling as though you are watching a movie of yourself
- Mental health problems such as depression, anxiety and thoughts of suicide
- A sense of detachment from your emotions, or emotional numbness
- A lack of a sense of self-identity
The symptoms of dissociative disorders depend on the type of disorder that has been diagnosed. There are three types of dissociative disorders defined in the Diagnostic and Statistical Manual of Mental Disorders (DSM):
- Dissociative Amnesia. The main symptom is difficulty remembering important information about one’s self. Dissociative amnesia may surround a particular event, such as combat or abuse, or more rarely, information about identity and life history.
 The onset for an amnesic episode is usually sudden, and an episode can last minutes, hours, days, or, rarely, months or years. There is no average for age onset or percentage, and a person may experience multiple episodes throughout her life.
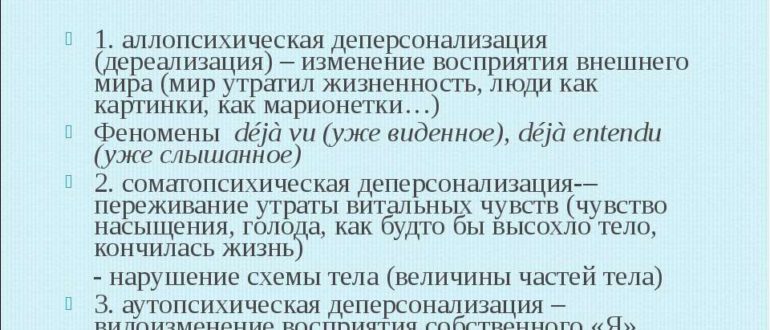
The onset for an amnesic episode is usually sudden, and an episode can last minutes, hours, days, or, rarely, months or years. There is no average for age onset or percentage, and a person may experience multiple episodes throughout her life. - Depersonalization disorder. This disorder involves ongoing feelings of detachment from actions, feelings, thoughts and sensations as if they are watching a movie (depersonalization). Sometimes other people and things may feel like people and things in the world around them are unreal (derealization). A person may experience depersonalization, derealization or both. Symptoms can last just a matter of moments or return at times over the years. The average onset age is 16, although depersonalization episodes can start anywhere from early to mid childhood. Less than 20% of people with this disorder start experiencing episodes after the age of 20.
- Dissociative identity disorder.
Formerly known as multiple personality disorder, this disorder is characterized by alternating between multiple identities.
 A person may feel like one or more voices are trying to take control in their head. Often these identities may have unique names, characteristics, mannerisms and voices. People with DID will experience gaps in memory of every day events, personal information and trauma. Women are more likely to be diagnosed, as they more frequently present with acute dissociative symptoms. Men are more likely to deny symptoms and trauma histories, and commonly exhibit more violent behavior, rather than amnesia or fugue states. This can lead to elevated false negative diagnosis.
A person may feel like one or more voices are trying to take control in their head. Often these identities may have unique names, characteristics, mannerisms and voices. People with DID will experience gaps in memory of every day events, personal information and trauma. Women are more likely to be diagnosed, as they more frequently present with acute dissociative symptoms. Men are more likely to deny symptoms and trauma histories, and commonly exhibit more violent behavior, rather than amnesia or fugue states. This can lead to elevated false negative diagnosis.
Causes
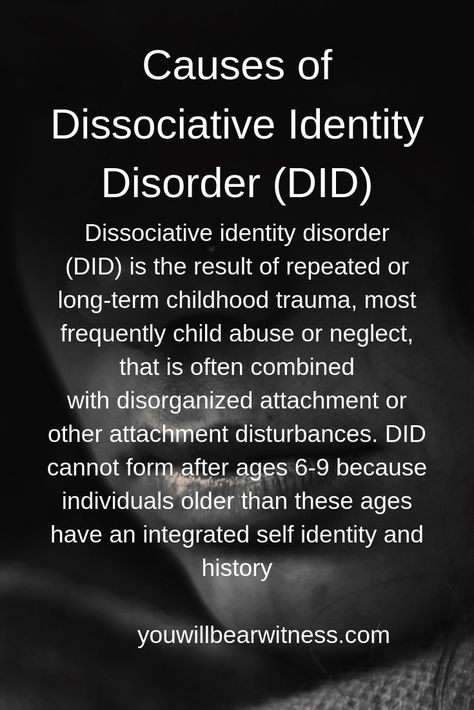
Dissociative disorders usually develop as a way of dealing with trauma. Dissociative disorders most often form in children exposed to long-term physical, sexual or emotional abuse. Natural disasters and combat can also cause dissociative disorders.
Diagnosis
Doctors diagnose dissociative disorders based on a review of symptoms and personal history. A doctor may perform tests to rule out physical conditions that can cause symptoms such as memory loss and a sense of unreality (for example, head injury, brain lesions or tumors, sleep deprivation or intoxication).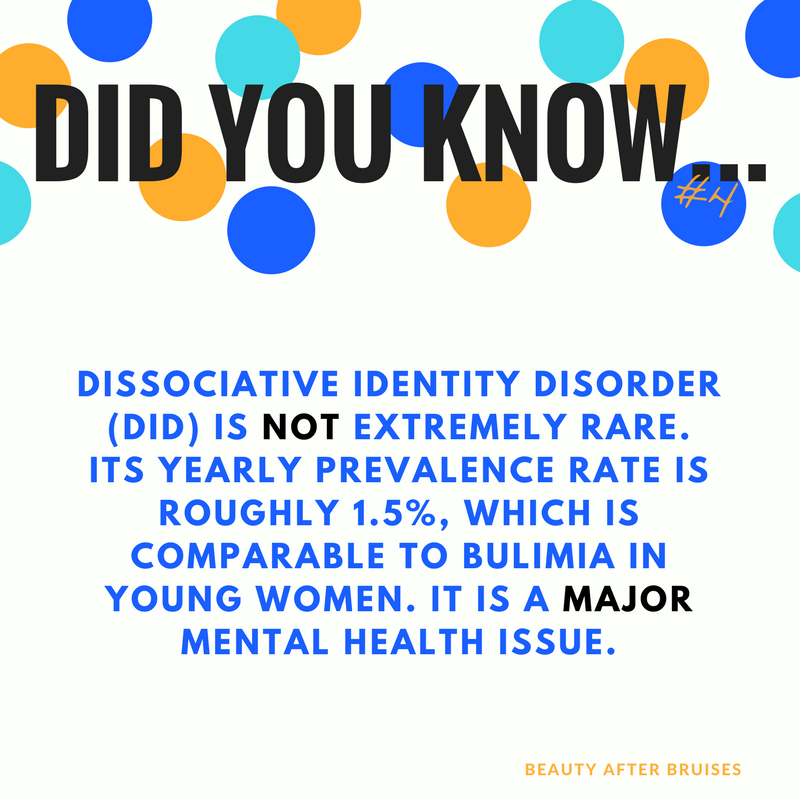 If physical causes are ruled out, a mental health specialist is often consulted to make an evaluation.
If physical causes are ruled out, a mental health specialist is often consulted to make an evaluation.
Many features of dissociative disorders can be influenced by a person’s cultural background. In the case of dissociative identity disorder and dissociative amnesia, patients may present with unexplained, non-epileptic seizures, paralyses or sensory loss. In settings where possession is part of cultural beliefs, the fragmented identities of a person who has DID may take the form of spirits, deities, demons or animals. Intercultural contact may also influence the characteristics of other identities. For example, a person in India exposed to Western culture may present with an “alter” who only speaks English. In cultures with highly restrictive social conditions, amnesia is frequently triggered by severe psychological stress such as conflict caused by oppression. Finally, voluntarily induced states of depersonalization can be a part of meditative practices prevalent in many religions and cultures, and should not be diagnosed as a disorder.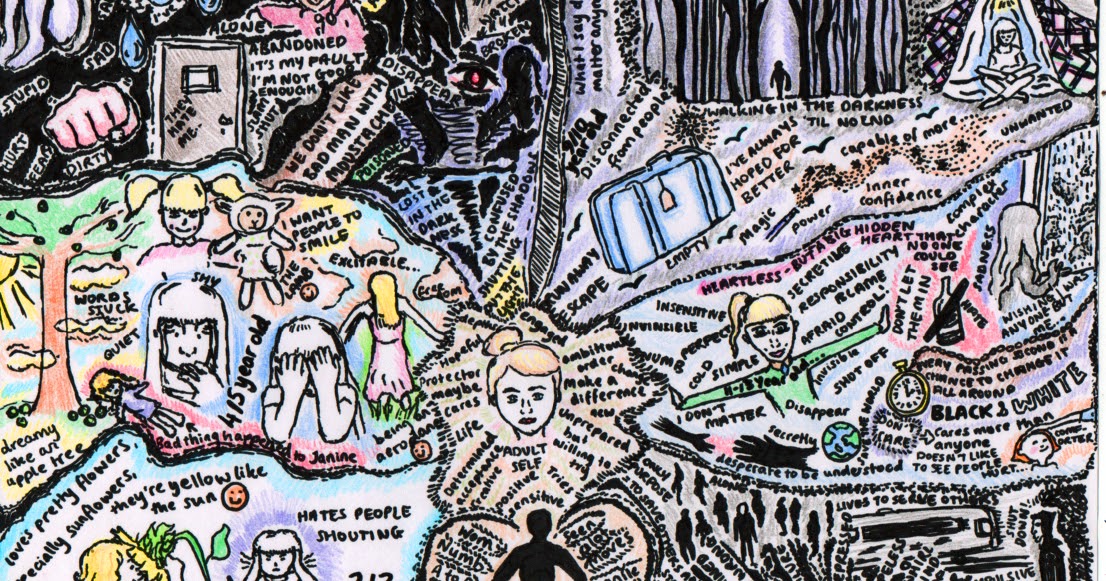
Dissociative disorders are managed through various therapies including:
- Psychotherapies such as cognitive behavioral therapy (CBT) and dialectical behavioral therapy (DBT)
- Eye movement desensitization and reprocessing (EMDR)
- Medications such as antidepressants can treat symptoms of related conditions
Related Conditions
Because dissociative disorders appear on the trauma spectrum, many patients may have conditions associated with trauma, as well as additional trauma-based conditions.
- Posttraumatic stress disorder (PTSD)
- Borderline personality disorder (BPD)
- Substance use disorders / Dual Diagnosis
- Depression
- Anxiety
Dissociative Identity Disorder Statistics, Facts, Prevalence and Diagnosis
Read the latest statistics on dissociative identity disorder and how to get help for this condition.
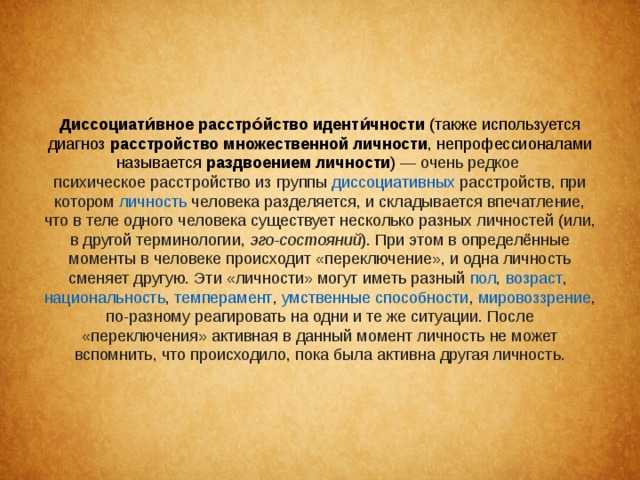
Dissociative identity disorder, previously known as multiple personality disorder, is a psychological state that is characterized by a disconnect between a person’s thoughts, emotions and behaviors. Dissociative identity disorder is a complicated condition that develops from numerous factors, namely early and severe childhood trauma, abuse and neglect. The dissociative features of the disorder are believed to be used as a complex coping strategy, allowing individuals to separate themselves from past traumatic experiences. These experiences are thought to be too upsetting for people to integrate into their conscious thoughts.
Dissociative identity disorder occurs when two or more separate identities are present, each playing a distinctive role and having control over a person’s actions, memories and feelings. Life experiences and situational factors seemingly trigger shifts between identities.
Conclusive facts and statistics on dissociative identity disorder are not readily available due to lack of research and controversy linked to the disorder.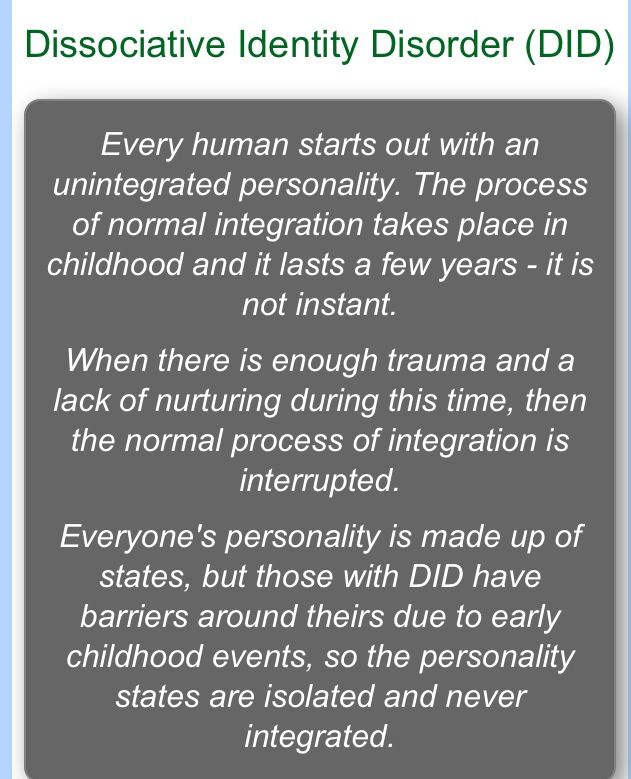 However, available dissociative identity disorder documentation conveys that the disorder was initially believed to be quite rare, with less than 100 diagnosed cases by 1944. Current dissociative identity disorder facts now show that the prevalence of the disorder is beginning to rise, perhaps due to greater understanding and more accurate diagnosis processes.
However, available dissociative identity disorder documentation conveys that the disorder was initially believed to be quite rare, with less than 100 diagnosed cases by 1944. Current dissociative identity disorder facts now show that the prevalence of the disorder is beginning to rise, perhaps due to greater understanding and more accurate diagnosis processes.
How Common is DID?
Dissociative identity disorder prevalence varies widely in different studies. Dissociative identity disorder has been identified in 4 percent to 7.5 percent of patients in psychiatric residences and 2-6 percent of patients in outpatient settings. DID is otherwise very rare, with rates of 0.4 percent to three and one-tenth percent of individuals not linked with mental health services. Dissociative identity disorder is also believed to be widely undiagnosed or misdiagnosed, making it difficult to determine exactly how many people are affected by dissociative identity disorder.
Dissociative identity disorders are not overly common, but aren’t entirely rare, either.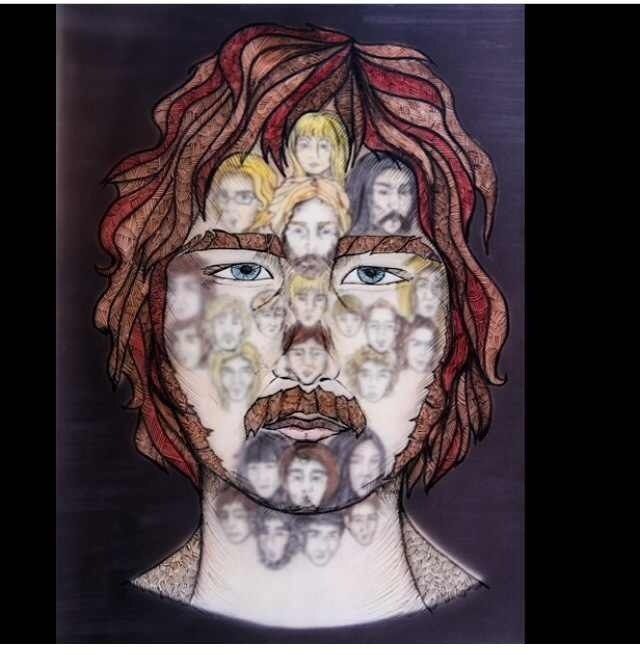 Statistics on alternate personalities have risen over time, which may come from better knowledge and understanding of the condition along with fewer cases of misdiagnosis.
Statistics on alternate personalities have risen over time, which may come from better knowledge and understanding of the condition along with fewer cases of misdiagnosis.
The average number of personalities in dissociative identity disorder is two to four upon initial diagnosis. The average number of personalities in someone with multiple personality disorder is 13 to 15 over the entire course of treatment. It is unusual, but there have been cases in which more than 100 personalities have been reported.
Who Is Affected by Dissociative Identity Disorder?
Dissociative identity disorder statistics vary but show that the condition occurs in anywhere from one-half percent to two percent of the population. Other dissociative identity disorder facts suggest that about seven percent of the general population may have the disorder, but remain undiagnosed.
Dissociative identity disorder is a relatively rare and controversial condition, making it complicated to study and research.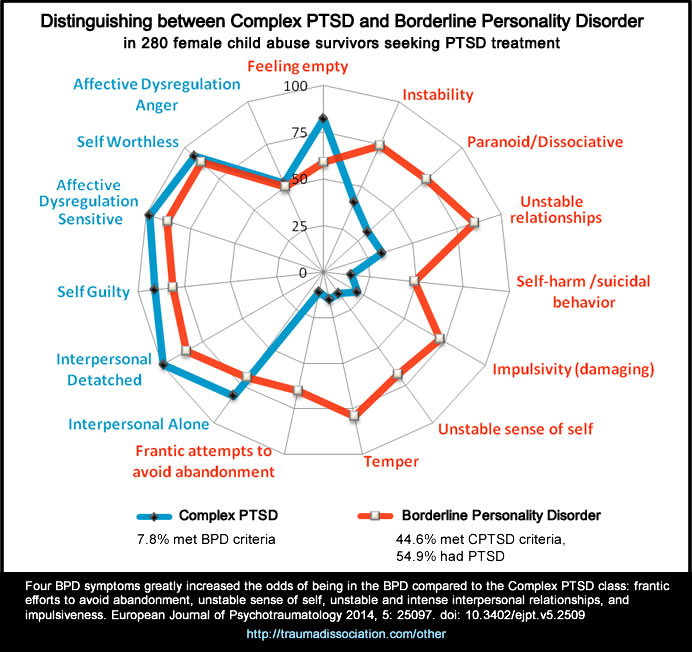 Researchers continue to assess how common dissociative identity disorder is in the population. Available research indicates that approximately two percent of people in the world experience dissociative disorders and they are more commonly diagnosed in women.
Researchers continue to assess how common dissociative identity disorder is in the population. Available research indicates that approximately two percent of people in the world experience dissociative disorders and they are more commonly diagnosed in women.
Research has sought to investigate why dissociative identity disorder is more common in females. Studies have found that women have symptoms more regularly than males, as males are more apt to hide symptoms and traumatic histories. Men also display more aggressive behavior and less memory loss than females do, resulting in less diagnosis. Females face childhood abuse more frequently than males, also making dissociative identity disorder more likely to occur in the female population.
Individuals who are victims of past violence and mistreatment are at elevated risk of developing dissociative identity disorder. Dissociative symptoms originate to help a person to deal with distressing and traumatic memories. Risk factors for dissociative identity disorder include severe abuse, recurrent neglect, natural disasters and past trauma in childhood. In reported cases in the United States, Canada and Europe, approximately 90 percent of people with this condition had experienced abuse and neglect in childhood.
In reported cases in the United States, Canada and Europe, approximately 90 percent of people with this condition had experienced abuse and neglect in childhood.
Rates of DID and Substance Abuse
There is a direct relationship between substance abuse and dissociative identity disorder, as people may use drugs or alcohol to numb symptoms and separate from reality. People may use substances as a way to cope with their victimization and past trauma. Individuals with dissociative identity disorder and co-occurring addictions contend with added difficulties on top of original issues that led to the dissociation. Dissociation and addiction are both chronic, recurring conditions that are complex to treat. In one study of people in an inpatient substance abuse treatment program, 17.2 percent of people had a dissociative disorder.
Misdiagnosis of Dissociative Identity Disorder
Dissociative identity disorder misdiagnosis is common, as symptoms are similar to symptoms of other mental health disorders. Many psychological conditions share symptoms of anxiety, depression and substance abuse. Some individuals with dissociative identity disorder may receive several diagnoses before being given a correct dissociative identity disorder diagnosis. To further complicate matters, one personality may present symptoms of a mental health condition that is not shared by the primary “host” personality.
Many psychological conditions share symptoms of anxiety, depression and substance abuse. Some individuals with dissociative identity disorder may receive several diagnoses before being given a correct dissociative identity disorder diagnosis. To further complicate matters, one personality may present symptoms of a mental health condition that is not shared by the primary “host” personality.
Some common dissociative identity disorder misdiagnosis cases include borderline personality disorder, schizophrenia and bipolar disorder. It is unclear whether these misdiagnoses arise from actual misdiagnosis or whether these diagnoses are present in conjunction with dissociative identity disorder. Misdiagnosis can result in incorrect treatments, worsening of symptoms or no improvement.
Dissociative identity disorder treatment concentrates on integrating “alter” personalities into one functional personality structure. Dissociative identity disorder recovery is long-term, multi-staged and consists mainly of talk therapy, hypnotherapy and other psychotherapeutic treatment interventions. Medications are not used to treat the disorder itself but may be prescribed to treat specific symptoms.
Medications are not used to treat the disorder itself but may be prescribed to treat specific symptoms.
Psychotherapy can span from five to seven years. Individuals who do not receive treatment for dissociative disorders tend to get worse, as alternate personalities cannot integrate on their own. Untreated dissociative identity disorder makes an individual susceptible to further exploitation and mistreatment by others. Typical treatment approaches attempt to stabilize an individual, process trauma and integrate personalities. Although statistics depict that dissociative identity disorder is rare, it is also a commonly misdiagnosed or undiagnosed condition.
Check out the Nobu app to learn more about dissociative identity disorder and a variety of other mental health topics. It is free and for anyone that is looking to reduce anxiety, work through depression, build self-esteem, get aftercare following treatment, attend teletherapy sessions and so much more. Download the Nobu app today!
Editor – Camille Renzoni
Cami Renzoni is a creative writer and editor for The Recovery Village. As an advocate for behavioral health, Cami is certified in mental health first aid and encourages people who face substance use disorders to ask for the help they deserve. Read more
As an advocate for behavioral health, Cami is certified in mental health first aid and encourages people who face substance use disorders to ask for the help they deserve. Read more
Medically Reviewed By – Tracy Smith, LPC, NCC, ACS
Tracy Smith is a Licensed Professional Counselor, a Nationally Certified Counselor, an Approved Clinical Supervisor, and a mental health freelance and ghostwriter. Read more
American Association for Marriage and Family Therapy. “Dissociative Identity Disorder.” AAMFT, 2019. Accessed February 18, 2019.
Johnson, Karen. “The Problem of Prevalence-How Common Is DID?” PODS, May 1, 2011 Accessed January 13, 2019.
Matulewicz, Crystalie. “Why Dissociative Identity Disorder (DID)[…]s Often Misdiagnosed.” Healthy Place, November 4, 2015. Accessed January 13, 2019.
National Alliance on Mental Illness. “Dissociative Disorders.” (n.d.) Accessed February 2019.
Swartz, A. “Dissociative Identity Disorder.” All Psych, December 10, 2001.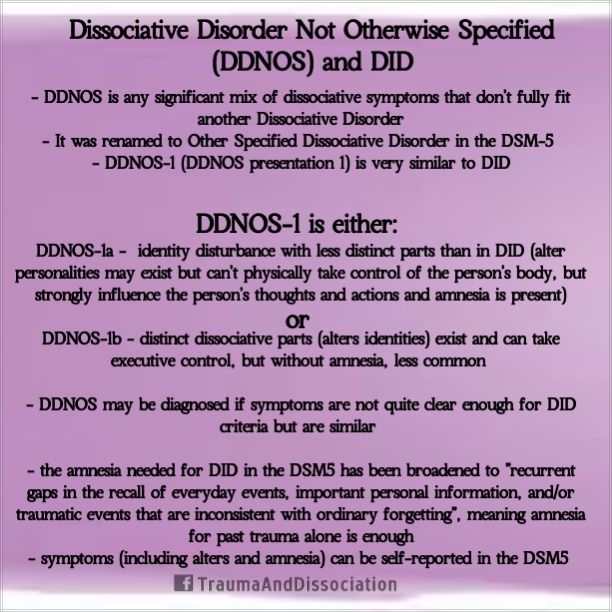 Accessed January 13, 2019.
Accessed January 13, 2019.
Tracy, Natasha. “Dissociative Identity Disorder (DID) Statistics and Facts.” Healthy Place, October 16, 2018. Accessed January 13, 2019.
Wang, P. (2018, August). “Dissociative Disorders.” Psychiatry.Org, August 2018. Accessed January 13, 2019.
Medical Disclaimer
The Recovery Village aims to improve the quality of life for people struggling with substance use or mental health disorder with fact-based content about the nature of behavioral health conditions, treatment options and their related outcomes. We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.
Dissociative Identity Disorder | Rehab Family Clinic
Dissociative identity disorder is a mental disorder in which a person self-identifies with multiple personalities. They seem to exist in him alone; each of them periodically dominates, determining his views, behavior and attitude towards himself as if other personalities were absent.
They seem to exist in him alone; each of them periodically dominates, determining his views, behavior and attitude towards himself as if other personalities were absent.
They may be of different genders, different ages and belong to different nationalities, each of them usually has its own name and biography. During the period of dominance of one of the personalities, the patient does not remember his original personality and is not aware of the existence of others. There is a tendency for a sudden transition from the dominance of one personality to another.
This disorder is also known as dissociative identity disorder, multiple personality disorder, split personality disorder, and multiple personality disorder. There are many names, but the essence is the same - a person with this disease may not even suspect that several characters live in his body at the same time.
In fact, this is a group of mental disorders, which are characterized by changes or disturbances in a number of mental functions - consciousness, memory, a sense of personal identity, awareness of the continuity of one's own identity. Dissociative disorder manifests itself involuntarily. The choice of this or that personality by the patient cannot be controlled.
Dissociative disorder manifests itself involuntarily. The choice of this or that personality by the patient cannot be controlled.
Symptoms of a dissociative disorder
The nature of the occurrence of this mental disorder most often comes down to a traumatic event in the past. It can be a terrorist act, an accident, military operations or violence. The splitting of the personality in this case becomes a manifestation of the body's defense mechanism.
Patients with a disorder feel as if they have become witnesses to the actions of others, observers from the outside. They perceive themselves and their bodies differently.
In general, there are two main features of a dissociative disorder:
- The presence of at least two personalities who would regularly take turns controlling the behavior of the individual.
- Memory loss that goes beyond normal forgetfulness and is described as a "switch".
Usually, memory loss in a disorder is not long-term and ends with a complete recovery. The disorder is more common in young women. Symptoms and signs of dissociative identity disorder should be a reason for a person to see a doctor.
The disorder is more common in young women. Symptoms and signs of dissociative identity disorder should be a reason for a person to see a doctor.
Causes of dissociative disorder
In most cases, the causes of this disorder are severe emotional trauma in early childhood, repeated physical, sexual or emotional abuse.
The human mind builds dissociations as a defense - this helps to separate traumatic memories and thoughts. No matter how hard a person tries to forget an unpleasant event, it pops up in the subconscious under the influence of triggers. Some things, people, events that bring back memories of psychological trauma can act in their role.
The causes of dissociative disorder can be:
- the influence of parents or other relatives who had a split personality;
- predisposition to multiple personality;
- abuse of others, lack of support;
- physical, emotional or sexual abuse.
It is important to note that children are not born with a holistic personality - it is formed into a single whole under the influence of biological and social factors. If the child grows up in an atmosphere of cruelty, then dissociative personality disorder may manifest itself at an older age.
If the child grows up in an atmosphere of cruelty, then dissociative personality disorder may manifest itself at an older age.
Other reasons include traumatic events at a conscious age (even if a person grew up in a healthy environment). For example, assault, car and plane crashes, natural disasters, war, participation in hostilities, rape.
Patients with an unstable psyche are also at risk - those who are diagnosed with incurable diseases, as well as people who abuse psychotropic substances. Dissociative mental disorders are not uncommon in people taking hallucinogens.
Classification of dissociative disorder
There are two main forms of mental disorder - possessed and unpossessed.
The first is characterized by a sudden change in behavior that is noticeable to the naked eye by those who know the person well. Each of the third-party personalities has a whole story - the patient may not introduce himself by his own name, behave in an unusual way. The clearest example is demonic possession. From the outside, it seems that someone has moved into the patient, he speaks in a different voice, performs non-standard actions. The possessed form very often has religious overtones.
Each of the third-party personalities has a whole story - the patient may not introduce himself by his own name, behave in an unusual way. The clearest example is demonic possession. From the outside, it seems that someone has moved into the patient, he speaks in a different voice, performs non-standard actions. The possessed form very often has religious overtones.
The second type of dissociative disorder is not as clearly distinguishable as the first. According to patients, they observe themselves as if from the outside, they cannot interfere with the behavior of an outsider and control their body as they want. At the same time, there is a clear feeling of a change in gender, age. Thoughts and feelings are also observed that were not previously characteristic of a person. There may be a temper tantrum in a temperamentally calm person or a sudden desire to change appearance. These are all the initial signs of a plurality of personality.
The more traditional form includes 7 states, each of which has its own characteristics.
- dissociative fugue. It is marked by complete depersonalization of the subject - a person can leave home, completely forget about who he is. There are two options for the development of events - either a state of confusion, a misunderstanding of what is happening, or a complete identification of oneself with a new personality. In the advanced form of fugue, patients can form a new family, get another job, or move to a new place of residence. When the true identity returns, the person suddenly finds himself in an unfamiliar place, next to strangers. Interestingly, during the period of personality change, the patient does not suspect that something has changed, he feels organic, and he turns to the doctor only when the memory of the original personality is restored.
- dissociative amnesia. It is more common than other forms of dissociative disorders. With it, the patient may partially or completely lose memory. At the same time, the person is quite clearly aware that he is in a state of amnesia.
 Usually it is caused by stressful or tragic situations. Patients are well oriented in their own personality, but cannot restore the events that have occurred.
Usually it is caused by stressful or tragic situations. Patients are well oriented in their own personality, but cannot restore the events that have occurred. - Trance and possession. This type of disorder is diagnosed in clergy, mediums. A person experiences confusion, as if he falls into a stupor, does not understand where he is and who he is. These are usually short episodes. They can occur with monotony and in situations that involve a loss of orientation in space. For example, aircraft pilots, drivers.
- Dissociative identity disorder. With this type of dissociative mental disorder, individuals of a different gender and age make themselves felt. For example, an adult has the behavior of a child. This form is connected with childhood - mistreatment, violence affects. In this case, many personalities come together to protect the original one. The transition to it occurs abruptly, and the patient cannot remember what happened during that period of time when side personalities predominated.
- Depersonalization disorder. Here a personality is manifested that cannot be defined as a specific person with a history. The patient may associate himself with a robot, extraterrestrial intelligence, or feel like a hero of a dream. This acute dissociative disorder destabilizes all spheres of life - a person cannot control his thoughts, body, feels like an outside observer.
- dissociative convulsions. These are similar to epileptic seizures, which are an imitation of a brain disease. The patient may twitch as if in convulsions, but unlike epilepsy, he will not bite his tongue and lose consciousness.
- Dissociative disorders of movement and sensation. The patient has a complete or partial loss of mobility, he does not respond to external stimuli, but consciousness is preserved.
Separately, it is worth highlighting organic dissociative disorder. With it, all the same symptoms are observed as with other forms of the disorder, but the reason for its occurrence is traumatic situations that are accompanied by damage to the brain. It can be provoked by traumatic brain injury, damage to brain neurons, and women during menopause are also susceptible to this type.
Complications of the disease
A patient with a disease may primarily harm himself during a change of personality. It is not known what qualities the new entity may have - perhaps it is suicidal.
Among the complications of dissociative disorder, it can be noted that the patient becomes potentially dangerous to society. It is not known what strategy of behavior the new personality will choose. She may be prone to overeating (this is fraught with disruption of the gastrointestinal tract), strive for extreme sports (this is traumatic, an unprepared person can easily get fractures and bruises), and convulsions with certain varieties can also cause injury - a person involuntarily twitches, falls to the floor .
Against the background of DID, depression can develop, which will lead to sleep disturbance, followed by malfunctions in the work of all systems and organs.
When to see a doctor
In the ICD, dissociative personality disorder occupies an entire section (F 44.8), which means that a specialist should deal with this violation. The slightest deviation from normal behavior (even according to close people) is a reason to visit a specialist.
If a person notices non-standard behavior, feels like an observer in his own body, or cannot remember some segments of his life, then it is likely that he is diagnosed with DID.
It is important to listen to loved ones who notice changes in the person's habitual state, and not try to cope with dissociative conversion disorders on their own.
Disease diagnosis
The initial task of a specialist in the diagnosis of DID is to exclude any organic brain damage. To do this, after clarifying the symptoms, the patient is sent for an MRI and CT scan of the brain. The same study helps the doctor rule out schizophrenia, epilepsy, dementia, and bipolar disorder.
It is also important to determine whether a person is faking or not. To do this, the survey must necessarily include an anamnesis and a survey that helps to establish the presence of traumatic situations and assess the patient's family relationships in childhood.
Also, for the diagnosis of dissociative disorder, constant monitoring of a person is necessary. At this point, it is also important to take into account the feedback of the patient's close people, because in a state of amnesia, a person himself is not able to remember whether personality splits occurred at some moments.
Diagnosis of the disease in children also includes a mandatory survey. If a child has fictitious friends, then this may be just a fantasy game. But observation at this age is also important.
Some doctors use hypnosis, during the dive they can discover other personalities in themselves, or the person himself recalls a situation in which he behaved outside the box. Amytal-caffeine disinhibition helps to achieve the same effect.
Treatment
Treatment for dissociative disorder does not have an established regimen. However, most specialists focus on psychotherapy, and the direction is chosen depending on the type of DID. It can be family, group, cognitive therapy or the already mentioned hypnosis.
During the sessions, the doctor aims to change the patient's thinking, work out stereotypes and eliminate them.
Medications help to alleviate the condition - tranquilizers and antidepressants, which are prescribed only in advanced cases. Medicines relieve depression, if necessary, restore sleep. They are selected for each patient individually.
Physiotherapy may be prescribed as maintenance therapy in the treatment of dissociative identity disorder.
Unfortunately, it is believed that DID is not completely cured, but some forms can still be corrected, and in patients with fugue and amnesia, recovery occurs quite quickly. The main thing is to ensure that the acute form does not turn into a chronic one.
+7 (495) 121-48-31
Prevention of disorder
To date, there are no measures that can prevent this mental disorder. Therefore, it is so important to track the disease in time at the initial stage.
Recommendations for dissociative disorder include regular visits to the doctor if there are predisposing factors for DID and, if possible, maintaining mental health.
References:
- Abolin L.M. Psychological mechanisms of human emotional stability. Kazan: Ed. Kazan University, 1987
- Gilligen S. Therapeutic trances. Guide to Ericksonian therapy. M.: Independent firm "Class", 1997
- Grof S. Beyond the Brain. M.: Ed. Transpersonal Institute, 1993
- Jones E. The Life and Works of Sigmund Freud. M.: Humanitarian, 1997
- Diekman H. Methods in analytical psychology. M.: LLC "TsGL "RON", 2001
- Dmitrieva T.B. (ed.) Clinical Psychiatry. M.: GOETAR MEDICINE, 1998
- Enikolopov S.
 N. Psychotherapy for psychotraumatic stress disorders. // Russian Psychiatric Journal, 1998, No. 3, S. 5056.
N. Psychotherapy for psychotraumatic stress disorders. // Russian Psychiatric Journal, 1998, No. 3, S. 5056. - Kannabikh Yu. History of psychiatry. M.: TsTR MGP VOS, 1994
- Kantorovich N.V. Psychogeny. T .: Medicine, 1967
general information, causes, symptoms, treatment
Dissocial personality disorder (sociopathy, unstable psychopathy, antisocial psychopathy) is a mental personality disorder characterized by ignoring social norms and the rights of other people, a tendency to illegal actions.
According to the ICD-10 classification, dissocial personality disorder (F60.2) belongs to the group of specific personality disorders (F60). In accordance with the ICD, specific personality disorders are classified as severe disorders, with marked behavioral abnormalities. They are not a direct consequence of disease or any damage to the brain. The disorder is almost always associated with social breakdown and negatively affects several areas of a person's life.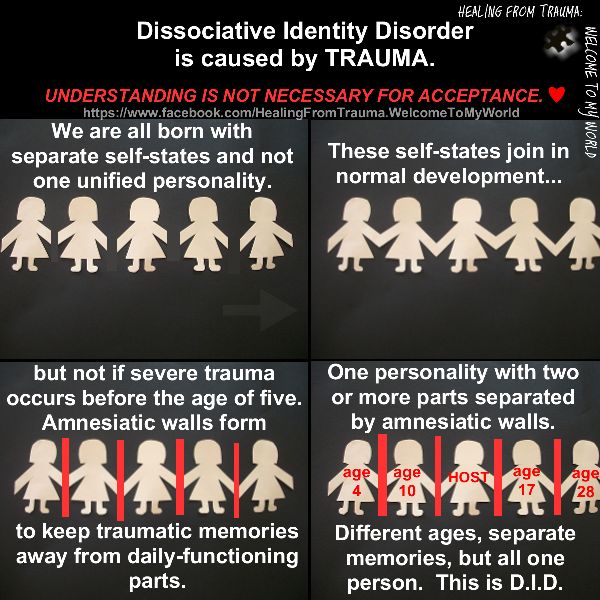 They begin in childhood and adolescence and last for many years. The disorder is detected in 1% of women and 3% of men. Residents of cities, children from large families, people from low-income segments of the population are most susceptible to the emergence of sociopathy.
They begin in childhood and adolescence and last for many years. The disorder is detected in 1% of women and 3% of men. Residents of cities, children from large families, people from low-income segments of the population are most susceptible to the emergence of sociopathy.
Researchers claim that patients with antisocial disorder make up to 75% of the contingent of places of detention. But not all sociopaths become criminals - some people commit socially condemned, but not formally punishable actions.
There are two types of people with antisocial personality disorder: passive and active. "Passive" sociopaths do not have internal moral restrictions, but are repelled by the norms of external authorities (religion, legislation). Such behavior protects them from open conflicts with society and allows them to formally meet the requirements of society.
"Active" sociopaths have no internal and external restrictions. If necessary, they can demonstrate to others their responsibility, decency and readiness to abide by the rules of society, but at any opportunity they stop limiting themselves and return to antisocial behavior. "Active" sociopaths often demonstrate criminal behavior, passive - hidden, formally unpunished (lie, manipulation, neglect of duties).
"Active" sociopaths often demonstrate criminal behavior, passive - hidden, formally unpunished (lie, manipulation, neglect of duties).
Clinically, sociopathy is manifested by a complete lack of guilt and responsibility for one's actions, an inability to learn from negative experiences. The person is prone to lies and hypocrisy, self-centered, aggressive, lacks empathy and affection. As with other psychotic conditions, the person acts impulsively, but sociopaths are aware that they violate the norms of society, unlike people with psychosis.
People with antisocial disorder commit illegal actions in order to obtain profit or pleasure (fraud, exploitation, etc.), they do not cope well with failures. A person justifies and rationalizes his actions, is indifferent to the negative consequences of his actions for others.
The allocation of this type of personality disorder is conditional. Rather, it is the same type of formation of different constitutional forms of personality. Some of the personalities can be attributed to the circle of schizoid psychopathy (emotionally cold expansive schizoids), others - to emotionally unstable and narcissistic personality disorders.
Some of the personalities can be attributed to the circle of schizoid psychopathy (emotionally cold expansive schizoids), others - to emotionally unstable and narcissistic personality disorders.
The main role in the occurrence of antisocial personality disorder is played by heredity and upbringing. With age, some correction of their behavior is possible.
Sociopathies often coexist with other psychiatric illnesses (borderline personality disorder, attention deficit hyperactivity disorder, impulse disorder) and addictions such as substance abuse and alcohol addiction.
Sociopathy is a dynamic personality structure along with masochistic, hysterical and others, which is formed from genetic predisposition and psychogenic factors. Behavior is difficult to treat and correct. Sociopaths are able to be responsible for their actions, they deliberately violate the laws, feeling permissiveness.
Such a person easily endures loneliness, often changes partners, if necessary, create a family, does this in order to better integrate into society. He attracts attention with his charisma and high intelligence.
He attracts attention with his charisma and high intelligence.
Uses the norms of society well for his own purposes, rejects traditional patterns of behavior and thinking, does not listen to medical recommendations, easily gives up his comfort (life in an inappropriate place for this, hitchhiking, vagrancy, etc.) Sociopaths do not believe and do not trust anyone .
Causes of disorder
Genetic and psychogenic factors contribute to the development of antisocial personality disorder. The mechanism of development of impulsivity and aggression towards others may be associated with the pathological functioning of the serotonin carrier gene. The hormonal apparatus of a person with sociopathy produces less serotonin, as a result of which he is not able to take the necessary emotions from communication, to experience empathy.
In close male relatives, sociopathy occurs five times more often than in other relatives. In families of patients with antisocial personality disorder, hysterical disorders are often detected. High criminal activity of family members, the presence of relatives suffering from alcoholism and drug addiction, poverty and unfavorable social conditions are also considered as factors contributing to the development of dissocial disorder.
High criminal activity of family members, the presence of relatives suffering from alcoholism and drug addiction, poverty and unfavorable social conditions are also considered as factors contributing to the development of dissocial disorder.
The presence of mental illness in close relatives increases the risk of the disorder in children. In this case, the role is played by hereditary predisposition and the adoption of a behavior model from parents (quarrels between family members, violence, divorce of parents), and much also depends on the methods of education (if relatives neglect the child, use violence, are inconsistent in discipline, etc.).
Sociopathy, like other personality disorders, can be caused by a lack of parental love and care in childhood, which leads to a lack of trust in people. A person with such an experience is emotionally alienated and is able to establish contact with other people only by force. In some cases, family members can unknowingly instill in a person an antisocial behavior model - they give in to a child in order to maintain good relations, in response to his aggressive behavior or stubbornness.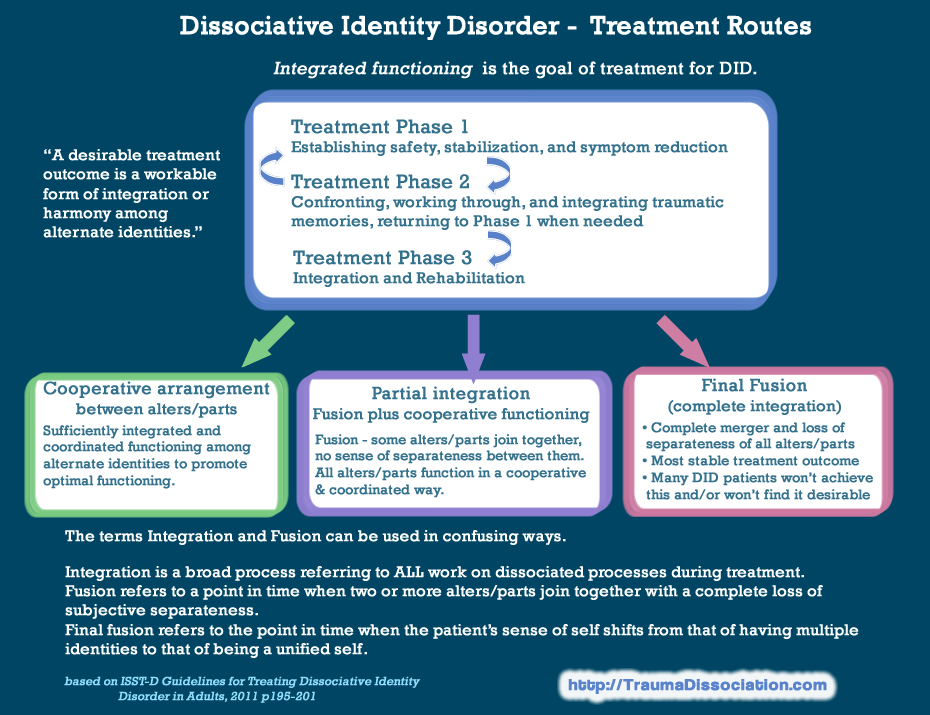 Overprotection or neglect can also affect.
Overprotection or neglect can also affect.
People with antisocial disorder find it difficult to accept any point of view other than their own. Studies have shown that people with this disorder are often less anxious than other people. Individuals with antisocial disorder have been found to be less able than controls to solve laboratory tasks, such as finding a way out of a maze, when the key reinforcers are punishments, such as some sort of shock or monetary fine. When the punishments were made more explicit or brought to the subjects' attention to them, learning improved. It is difficult for a person to learn from his mistakes, this may be due to the lack of an element that is key in the learning process.
Scientists have found that subjects with this disease respond to the expectation of stress by low excitation of the brain (slow excitation of the autonomic nervous system, low-frequency EEG waves). Due to low brain arousal, patients may find it difficult to grasp threatening situations, so they have little effect on them. Perhaps that is why anti-social and risky activities attract people, satisfying the need for more excitement.
Perhaps that is why anti-social and risky activities attract people, satisfying the need for more excitement.
Symptoms of the disorder
Sociopathy can appear as early as early preschool and adolescence, and symptoms in boys usually become visible as early as early school age. In girls, symptoms appear a little later - during the prepubertal period. The symptoms of the disorder are numerous: the child is selfish, hostile, stubborn, cruel (acts evil with peers, tortures animals, skips classes, runs away from home, spoils property, steals). In dealing with people, he is angry, quick-tempered, fits of rage are possible. Has a very high opinion of himself. A distinctive feature of patients with antisocial personality disorder is early opposition to parents. Due to the lack of attachment to their neighbors and a critical assessment of their actions, they neglect family traditions, moral and legal norms.
A person can deceive, speculate or manipulate other people for his own purposes, using his intellectual abilities for this.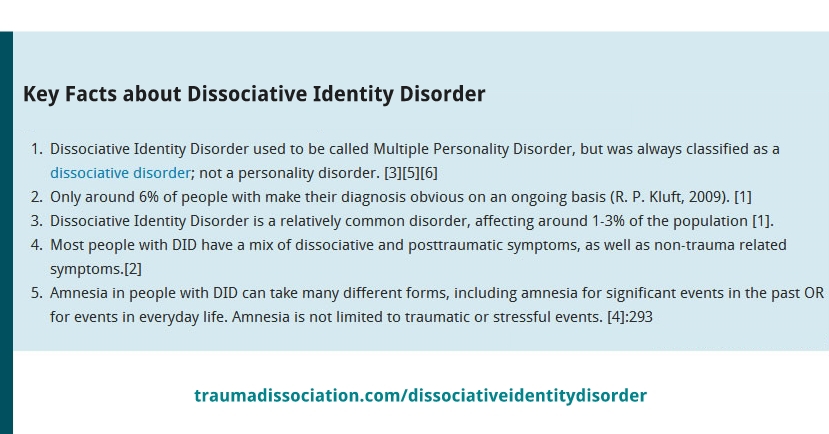 In order to get what they want, they are extremely charming, talkative, and endearing. They constantly crave light entertainment and pleasures, an idle lifestyle, try to avoid any work, study, fulfillment of any duties. From adolescence, they are drawn to asocial companies, alcohol, and drugs. They are indifferent to their future, live in the present. Weak-willed and cowardly - they try to run away from any difficulties and troubles.
In order to get what they want, they are extremely charming, talkative, and endearing. They constantly crave light entertainment and pleasures, an idle lifestyle, try to avoid any work, study, fulfillment of any duties. From adolescence, they are drawn to asocial companies, alcohol, and drugs. They are indifferent to their future, live in the present. Weak-willed and cowardly - they try to run away from any difficulties and troubles.
Patients with antisocial personality disorder may rationalize their actions by blaming those they offended that they themselves are to blame or that they deserve such treatment. They do not feel remorse and repentance, they are always sure that they are right, at any cost they do what they consider the best for themselves at the expense of other people. They are guided not only by selfish interests, but also by the desire to annoy and offend others. Any penalty from them is regarded as a manifestation of injustice.
In adulthood, a person with a similar disorder most often looks adequate and socially adapted.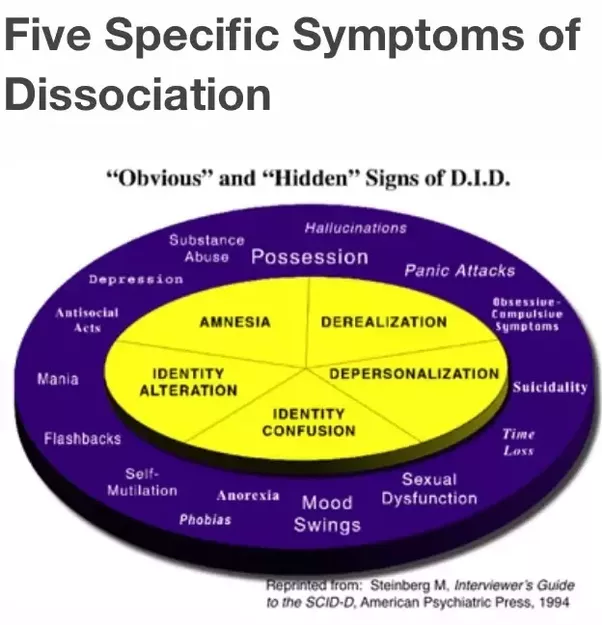 There are no problems in communication - thanks to the charm and ability to win over others, they often make a good impression with superficial contacts. Sociopaths have a special attraction, and people who need to be nurtured and guided like to be around such a “strong” person. It reassures them and gives them confidence. A person with a sociopathy is often sexually attractive, which he takes advantage of. Sexual life is a source of pleasure. Such a person is not able to love, empathize, sympathize, but can imitate love. you will never suspect that he does not feel anything for you.
There are no problems in communication - thanks to the charm and ability to win over others, they often make a good impression with superficial contacts. Sociopaths have a special attraction, and people who need to be nurtured and guided like to be around such a “strong” person. It reassures them and gives them confidence. A person with a sociopathy is often sexually attractive, which he takes advantage of. Sexual life is a source of pleasure. Such a person is not able to love, empathize, sympathize, but can imitate love. you will never suspect that he does not feel anything for you.
A person with a dissocial disorder is a desperate debater who always wins, and if they try to catch him, he will dodge to the end, but will not admit to being wrong or lying and most likely will go on the counterattack. When trying to argue the accusations and his wrongness, the sociopath will respond with accusations that they want to denigrate his honor. You should not compete with such a person, in any situation it is important for him to always win, and he uses any means for this.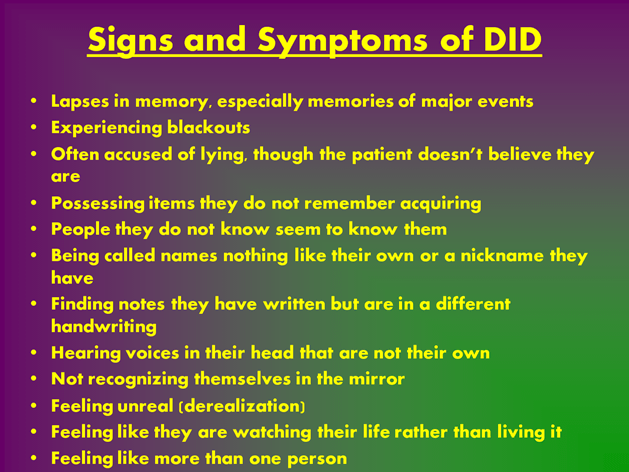
As a result of their impulsiveness, patients do not plan in advance, are socially and financially irresponsible - carelessly handle money, often move, change their place of residence and work, relationships. They may not pay bills, loans, alimony. Very often, sociopaths end up in prison, for many people with this disorder, the criminality of behavior begins to decrease after 40 years. Abuse alcohol and psychoactive substances. In a state of intoxication, conflict and aggressiveness increase.
Antisocial personality disorder persists throughout life, treatment is ineffective, but it helps to slightly correct behavior. Some patients create social groups isolated from society, become leaders of sects or criminal gangs. With age, many patients develop concomitant affective and somatic disorders, alcoholism, and drug addiction.
Diagnosis of disorder
The disorder is diagnosed on the basis of a conversation with a person and the collection of an anamnesis of life.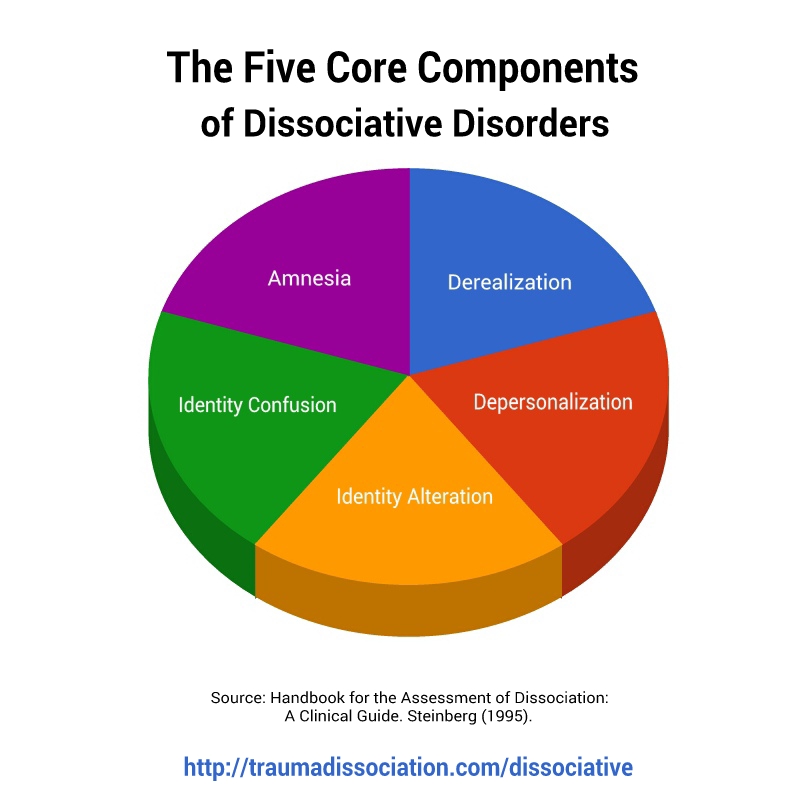 To assess the degree of neglect of duties and neglect of established rules, social conditions and cultural norms of a particular region are taken into account.
To assess the degree of neglect of duties and neglect of established rules, social conditions and cultural norms of a particular region are taken into account.
Antisocial personality disorder is diagnosed in the presence of general manifestations of the disorder and specific symptoms:
- the disorder is initiated at an early age (up to 15 years), there are no alternating periods of exacerbation and recovery;
- constant deliberate violation of social norms, laws, disregard for the rights and feelings of people;
- a person easily loses his temper, is angry, prone to violence;
- there is no sense of guilt and responsibility for their actions;
- a tendency to constant lies, fraud and manipulation;
- condemnation of other people's actions, justification and rationalization of their own;
- there is no planning, impulsiveness of actions, irresponsibility.
The disorder can be differentially diagnosed with the following diseases:
Narcissistic Personality Disorder .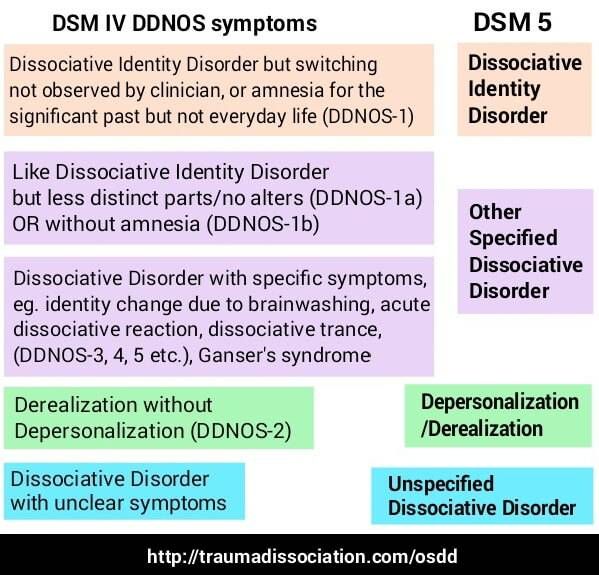 The person is not capable of empathy, tends to exploit others for their own purposes, but is not aggressive. Patients with narcissistic disorder have difficulty managing their self-esteem, it is important for them to hear praise and belong to special groups of people. To maintain their sense of superiority, they devalue other people and their achievements. They overestimate their abilities and exaggerate their achievements. Patients with antisocial personality disorder exploit others for material gain, while those with narcissistic personality disorder exploit others to maintain their self-esteem.
The person is not capable of empathy, tends to exploit others for their own purposes, but is not aggressive. Patients with narcissistic disorder have difficulty managing their self-esteem, it is important for them to hear praise and belong to special groups of people. To maintain their sense of superiority, they devalue other people and their achievements. They overestimate their abilities and exaggerate their achievements. Patients with antisocial personality disorder exploit others for material gain, while those with narcissistic personality disorder exploit others to maintain their self-esteem.
Borderline Personality Disorder . BPD patients are prone to manipulative behavior, the goal of manipulation is to gain attention and support, not material gain. Patients experience intense fear or anger when they feel ignored or rejected, afraid of being abandoned, left alone. Often and abruptly change the point of view, there is a phase of idealization and devaluation. They empathize only if they are sure that this person will come to their aid at any moment and will not leave them alone. After the end of the outburst of anger, he feels guilt and shame, convinces himself how much he himself is a bad person.
They empathize only if they are sure that this person will come to their aid at any moment and will not leave them alone. After the end of the outburst of anger, he feels guilt and shame, convinces himself how much he himself is a bad person.
Conduct disorders . Destructive patterns of behavior, in violation of norms and laws, occur before the age of 15 and stop with adulthood. In about a third of cases, they persist, the symptoms consistent with antisocial personality disorder. The disorders are characterized by persistent uncommunicative, aggressive, defiant patterns of behavior. Diagnosis is based on behavior patterns, including excessive conflict, deceit, cruelty to other people and animals, damage to property, etc. The presence of such pronounced signs is sufficient for diagnosis, but specific actions are evaluated only in conjunction with other factors.
Psychopathy . A disease with pronounced antisocial behavior, with complete preservation of thinking. Sociopathy is a milder form of psychopathy. With a normal existence in society, but a complete disregard for the rules and laws, we are talking about sociopathy. Psychopaths also know how to manipulate others, do not form attachments, other people are needed only to achieve their goals and entertainment. But if the psychopath is inclined to build and implement his plans in cold blood, then the sociopath acts spontaneously, often commits risky acts.
Sociopathy is a milder form of psychopathy. With a normal existence in society, but a complete disregard for the rules and laws, we are talking about sociopathy. Psychopaths also know how to manipulate others, do not form attachments, other people are needed only to achieve their goals and entertainment. But if the psychopath is inclined to build and implement his plans in cold blood, then the sociopath acts spontaneously, often commits risky acts.
Substance dependence . Impulsivity and irresponsibility can be the result of substance use. The analysis is based on the patient's history. Dependence can accompany a dissocial disorder, or be an independent disease.
Heboid schizophrenia . The presence of pronounced emotional changes and early onset emotional dullness is often a sign of slowly developing schizophrenia with heboid manifestations or chronic mania. The leading place in the manifestations of the heboid state in schizophrenia in adolescence is occupied by psychopathological disorders that contribute to a strong distortion and exaggeration of the typical manifestations of puberty (the desire to assert oneself, a tendency to oppose, contradict others).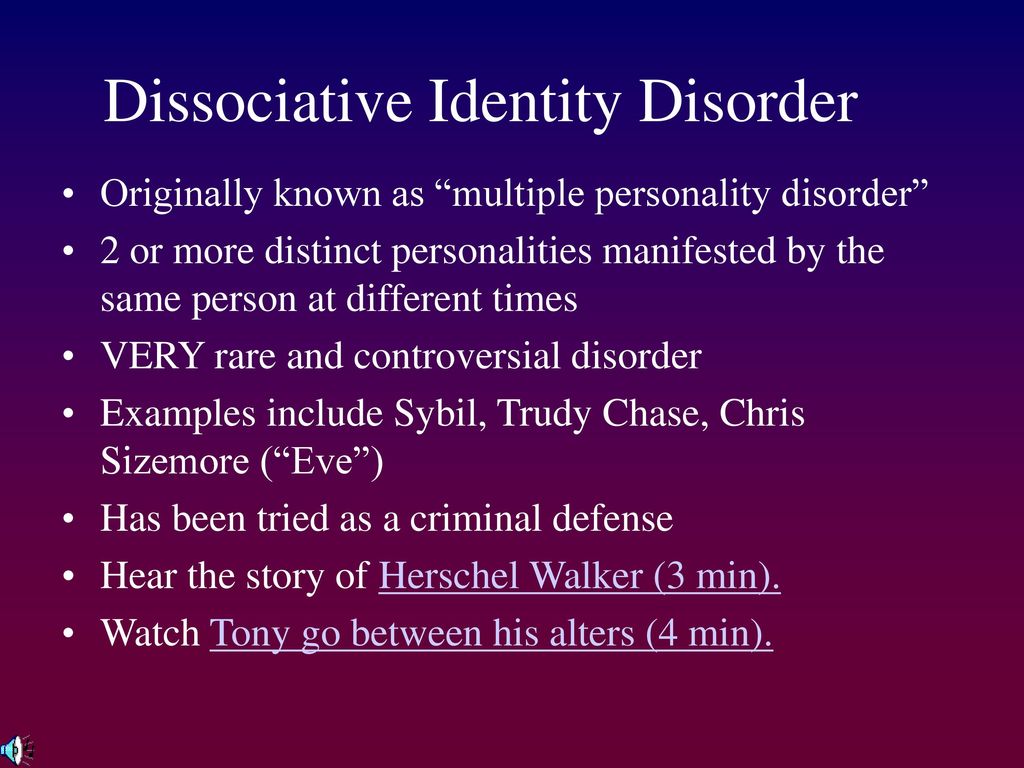 Under the influence of the disorder, the usual manifestations become psychopathological, total negativism and opposition to others and discipline develop.
Under the influence of the disorder, the usual manifestations become psychopathological, total negativism and opposition to others and discipline develop.
Dissociative Identity Disorder . A type of dissociative (conversion) disorder. It is characterized by the presence of two or more alternating personalities (alter-personality, ego-state or identity). Dissociative identity disorder is accompanied by an involuntary escape from reality, derealization, depersonalization. Inability to recall events from daily life, certain personal information, traumatic events, or severe stress. The cause of conversion disorder is almost always a trauma in childhood or adulthood. As a result of an identity disorder, a person finds himself in one or more personalities at the same time or in turn. At such moments, a person disconnects from himself and stops feeling his own body, may not see himself from the outside. Personalities within a person can have different ages, genders, nationalities, mental abilities, temperaments, and have completely different behaviors and habits.
Emotionally unstable personality disorder . Such people are prone to impulsive actions, are not afraid of consequences, are unpredictable, conflict and capricious. They tend to have emotional outbursts and are unable to control their temper tantrums. There are two types of disorder: impulsive type (emotional instability and lack of emotional control) and borderline type (characterized by a disorder of self-perception, goals and aspirations, a constant feeling of emptiness, tension and instability of interpersonal relationships, self-destructive behavior, suicidal attempts are possible).
Treatment of antisocial disorder in Alter
Individuals with antisocial disorder almost never seek psychiatric help. But many sociopaths feel the inner emptiness that is formed due to the lack of attachments and harmonious relationships with others, and they want to correct this.
Treatment of antisocial disorder is carried out with the help of a course of individual psychotherapy, sometimes methods of cognitive behavioral therapy and situational management.