Depersonalization derealization syndrome
Depersonalization/Derealization Disorder - Mental Health Disorders
By
David Spiegel
, MD, Stanford University School of Medicine
Last full review/revision Mar 2021| Content last modified Sep 2022
CLICK HERE FOR THE PROFESSIONAL VERSION
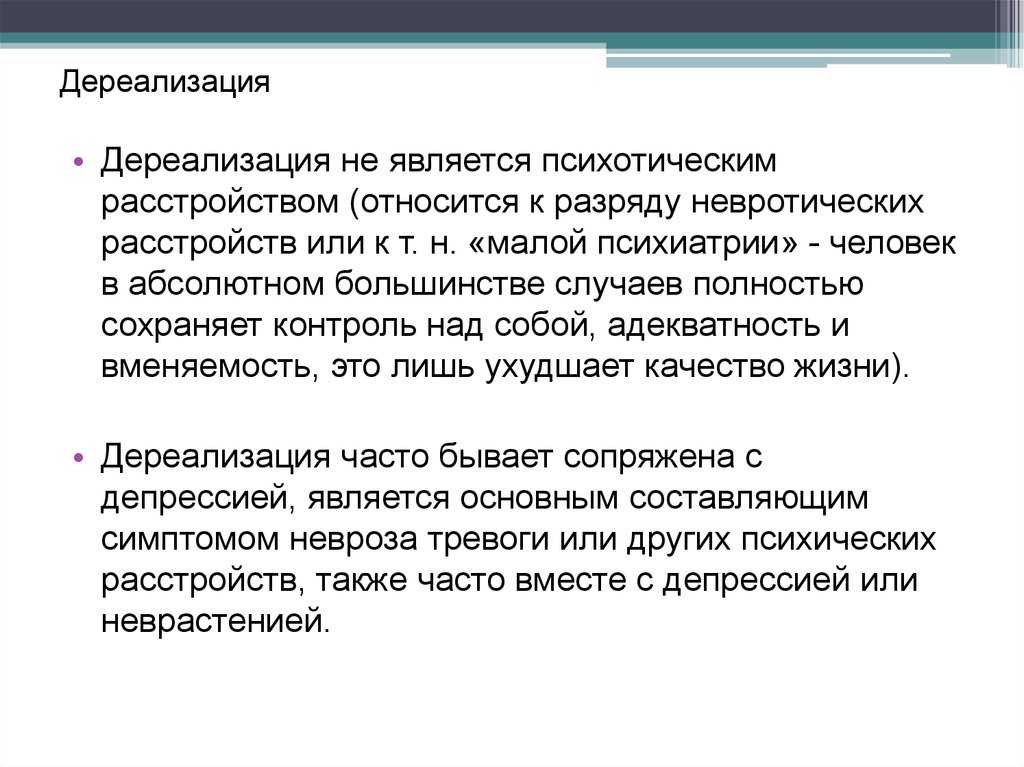
Depersonalization/derealization disorder involves a persistent or recurring feeling of being detached from one’s body or mental processes, like an outside observer of one's life (depersonalization), and/or a feeling of being detached from one's surroundings (derealization).
The disorder is usually triggered by severe stress, particularly emotional abuse or neglect during childhood, or other major stresses (such as experiencing or witnessing physical abuse).
Feelings of detachment from self or the surroundings may occur periodically or continuously.
After tests are done to rule out other possible causes, doctors diagnose the disorder based on symptoms.
Psychotherapy Psychotherapy Extraordinary advances have been made in the treatment of mental illness. As a result, many mental health disorders can now be treated nearly as successfully as physical disorders. Most treatment... read more , especially cognitive-behavioral therapy, is often helpful.
(See also Overview of Dissociative Disorders Overview of Dissociative Disorders Occasionally everyone has minor problems integrating their memories, perceptions, identity, and consciousness. For example, people may drive somewhere and then realize that they do not remember... read more .)
Temporary feelings of depersonalization and/or derealization are common. About one half of people have felt detached from themselves (depersonalization) or from the surroundings (derealization) at one time or another. This feeling often occurs after people
Experience life-threatening danger
Take certain drugs (such as marijuana Marijuana Marijuana (cannabis) is a drug made from the plants Cannabis sativa and Cannabis indica that contain a psychoactive chemical called delta-9-tetrahydrocannabinol (THC).
 Marijuana... read more , hallucinogens Hallucinogens Hallucinogens are a class of drugs that cause profound distortions in people's perceptions. Hallucinogens distort and intensify sensations, but the actual effects are variable and highly unpredictable... read more , ketamine Ketamine and Phencyclidine (PCP) Ketamine and phencyclidine are chemically similar drugs used for anesthesia but are sometimes used recreationally. Ketamine is available in powder and liquid form. The powder can be snorted... read more , or Ecstasy Hallucinogens Hallucinogens are a class of drugs that cause profound distortions in people's perceptions. Hallucinogens distort and intensify sensations, but the actual effects are variable and highly unpredictable... read more )
Marijuana... read more , hallucinogens Hallucinogens Hallucinogens are a class of drugs that cause profound distortions in people's perceptions. Hallucinogens distort and intensify sensations, but the actual effects are variable and highly unpredictable... read more , ketamine Ketamine and Phencyclidine (PCP) Ketamine and phencyclidine are chemically similar drugs used for anesthesia but are sometimes used recreationally. Ketamine is available in powder and liquid form. The powder can be snorted... read more , or Ecstasy Hallucinogens Hallucinogens are a class of drugs that cause profound distortions in people's perceptions. Hallucinogens distort and intensify sensations, but the actual effects are variable and highly unpredictable... read more )Become very tired
-
Are deprived of sleep or sensory stimulation (as may occur when they are in an intensive care unit)
Depersonalization or derealization can also occur as a symptom in many other mental disorders, as well as in general medical disorders, such as seizure disorders Seizure Disorders In seizure disorders, the brain's electrical activity is periodically disturbed, resulting in some degree of temporary brain dysfunction. Many people have unusual sensations just before a seizure... read more .
Many people have unusual sensations just before a seizure... read more .
Depersonalization/derealization feelings are considered a disorder when the following occur:
Depersonalization or derealization occurs on its own (that is, it is not caused by drugs or another mental disorder), and it persists or recurs.
The symptoms are very distressing to the person or make it difficult for the person to function at home or at work.
Depersonalization/derealization disorder occurs in about 2% of the population and affects men and women equally.
The disorder may begin during early or middle childhood. It rarely begins after age 40.
Depersonalization/derealization disorder often develops in people who have experienced severe stress, including the following:
Being emotionally abused or neglected during childhood
Being physically abused
Witnessing domestic violence
Having had a severely impaired or mentally ill parent
Having had a loved one die unexpectedly
Symptoms can be triggered by severe stress (for example, due to relationships, finances, or work), depression Depression A short discussion of prolonged grief disorder. Depression is a feeling of sadness and/or a decreased interest or pleasure in activities that becomes a disorder when it is intense enough to... read more , anxiety Overview of Anxiety Disorders Anxiety is a feeling of nervousness, worry, or unease that is a normal human experience. It is also present in a wide range of psychiatric disorders, including generalized anxiety disorder,... read more , or use of illegal or recreational drugs Recreational Drugs and Intoxicants . However, in 25 to 50% of cases, stresses are relatively minor or cannot be identified.
Depression is a feeling of sadness and/or a decreased interest or pleasure in activities that becomes a disorder when it is intense enough to... read more , anxiety Overview of Anxiety Disorders Anxiety is a feeling of nervousness, worry, or unease that is a normal human experience. It is also present in a wide range of psychiatric disorders, including generalized anxiety disorder,... read more , or use of illegal or recreational drugs Recreational Drugs and Intoxicants . However, in 25 to 50% of cases, stresses are relatively minor or cannot be identified.
Symptoms of depersonalization/derealization disorder may start gradually or suddenly. Episodes may last for only hours or days or for weeks, months, or years. Episodes may involve depersonalization, derealization, or both.
The intensity of symptoms often waxes and wanes. But when the disorder is severe, symptoms may be present and remain at the same intensity for years or even decades.
Depersonalization symptoms involve
People may also say they feel unreal or like an automaton, with no control over what they do or say. They may feel emotionally or physically numb. Such people may describe themselves as an outside observer of their own life or the “walking dead.”
They may feel emotionally or physically numb. Such people may describe themselves as an outside observer of their own life or the “walking dead.”
Derealization symptoms involve
People may feel as if they are in a dream or a fog, or as if a glass wall or veil separates them from their surroundings. The world seems lifeless, colorless, or artificial. The world may appear distorted to them. For example, objects may appear blurry or unusually clear, or they may seem flat or smaller or larger than they are. Sounds may seem louder or softer than they are. Time may seem to be going too slow or too fast.
The symptoms almost always cause great discomfort. Some people find them intolerable. Anxiety and depression are common. Many people are afraid that the symptoms result from irreversible brain damage. Many worry about whether they really exist or repeatedly check to determine whether their perceptions are real.
Stress, worsening depression or anxiety, new or overstimulating surroundings, and lack of sleep can make symptoms worse.
Symptoms are often persistent. They may
Recur in episodes (in about one third of people)
Occur continuously (in about one third)
Become continuous (in about one third)
People often have great difficulty describing their symptoms and may fear or believe that they are going crazy. However, people always remain aware that their experiences of detachment are not real but rather are just the way that they feel. This awareness is what separates depersonalization/derealization disorder from a psychotic disorder. People with a psychotic disorder always lack such insight.
Doctors suspect the disorder based on symptoms:
People have episodes of depersonalization, derealization, or both that last a long time or recur.
People know that their dissociative experiences are not real.
People are very distressed by their symptoms or their symptoms make them unable to function in social situations or at work.

A physical examination and sometimes tests are done to rule out other disorders that could cause the symptoms, including other mental health disorders, seizure disorders Seizure Disorders In seizure disorders, the brain's electrical activity is periodically disturbed, resulting in some degree of temporary brain dysfunction. Many people have unusual sensations just before a seizure... read more , and substance abuse Overview of Substance-Related Disorders Medications and other substances, whether used for legitimate medical purposes, as a habit (for example, caffeine), or recreationally, are an integral part of everyday life for many people ... read more . Tests may include magnetic resonance imaging (MRI), computed tomography (CT), electroencephalography (EEG), and blood and urine tests to check for drugs.
Psychologic tests and special structured interviews and questionnaires can also help doctors with the diagnosis.
Complete recovery is possible for many people with depersonalization/derealization disorder, especially if the symptoms result from stresses that can be dealt with during treatment. Other people do not respond well to treatment, and the disorder becomes chronic. In some people, depersonalization/derealization disorder disappears on its own.
Other people do not respond well to treatment, and the disorder becomes chronic. In some people, depersonalization/derealization disorder disappears on its own.
Symptoms, even those that persist or recur, may cause only minor problems if people can keep their mind busy and focus on other thoughts or activities, rather than think about their sense of self. However, some people become disabled because they feel so disconnected from their self and their surroundings or because they also have anxiety or depression.
Depersonalization/derealization disorder may disappear without treatment. People are treated only if the disorder persists, recurs, or causes distress.
Psychodynamic psychotherapy Psychotherapy Extraordinary advances have been made in the treatment of mental illness. As a result, many mental health disorders can now be treated nearly as successfully as physical disorders. Most treatment... read more and cognitive-behavioral therapy have been effective for some people. Depersonalization/derealization disorder is often associated with or triggered by other mental health disorders (such as anxiety Overview of Anxiety Disorders Anxiety is a feeling of nervousness, worry, or unease that is a normal human experience. It is also present in a wide range of psychiatric disorders, including generalized anxiety disorder,... read more or depression Depression A short discussion of prolonged grief disorder. Depression is a feeling of sadness and/or a decreased interest or pleasure in activities that becomes a disorder when it is intense enough to... read more ), which require treatment. Any stresses that triggered the symptoms or that may have contributed to development of depersonalization/derealization disorder must also be addressed.
Depersonalization/derealization disorder is often associated with or triggered by other mental health disorders (such as anxiety Overview of Anxiety Disorders Anxiety is a feeling of nervousness, worry, or unease that is a normal human experience. It is also present in a wide range of psychiatric disorders, including generalized anxiety disorder,... read more or depression Depression A short discussion of prolonged grief disorder. Depression is a feeling of sadness and/or a decreased interest or pleasure in activities that becomes a disorder when it is intense enough to... read more ), which require treatment. Any stresses that triggered the symptoms or that may have contributed to development of depersonalization/derealization disorder must also be addressed.
Techniques that can help include the following:
Cognitive techniques can help block obsessive thinking about the unreal state of being.
Behavioral techniques can help people become absorbed in tasks that distract them from the depersonalization.
Grounding techniques use the five senses (hearing, touch, smell, taste, and sight) to help people feel more connected to themselves and the world. For example, loud music is played or a piece of ice is put in the hand. These sensations are difficult to ignore, making people aware of themselves in the present moment.
Psychodynamic techniques focus on helping people work through intolerable conflicts, negative feelings, and experiences that people feel they must detach themselves from.
Moment-to-moment tracking and labeling of dissociation and affect (the outward expression of emotions and thoughts) teaches people to recognize and identify their feelings of dissociation. Such recognition helps some people. This technique also helps people focus on what is actually happening in the moment.
Various drugs have been used to treat depersonalization/derealization disorder, but none has been proved to be effective. Antianxiety drugs Treatment Anxiety is a feeling of nervousness, worry, or unease that is a normal human experience. It is also present in a wide range of psychiatric disorders, including generalized anxiety disorder,... read more and antidepressants Drug Treatment for Depression Agomelatine, a new type of antidepressant, is a possible treatment for major depressive episodes. Several types of drugs can be used to treat depression: Selective serotonin reuptake inhibitors... read more sometimes help, mainly by relieving anxiety or depression, which are present in many people with depersonalization/derealization disorder. However, antianxiety drugs may also increase depersonalization or derealization, so doctors carefully monitor use of these drugs.
Antianxiety drugs Treatment Anxiety is a feeling of nervousness, worry, or unease that is a normal human experience. It is also present in a wide range of psychiatric disorders, including generalized anxiety disorder,... read more and antidepressants Drug Treatment for Depression Agomelatine, a new type of antidepressant, is a possible treatment for major depressive episodes. Several types of drugs can be used to treat depression: Selective serotonin reuptake inhibitors... read more sometimes help, mainly by relieving anxiety or depression, which are present in many people with depersonalization/derealization disorder. However, antianxiety drugs may also increase depersonalization or derealization, so doctors carefully monitor use of these drugs.
| Generic Name | Select Brand Names |
|---|---|
ketamine |
KETALAR |
 DOCTORS:
CLICK HERE FOR THE PROFESSIONAL VERSION
DOCTORS:
CLICK HERE FOR THE PROFESSIONAL VERSION
CLICK HERE FOR THE PROFESSIONAL VERSION
Copyright © 2022 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Test your knowledge
Take a Quiz!Depersonalization Disorder - NORD (National Organization for Rare Disorders)
Depersonalization Disorder
Synonyms of Depersonalization Disorder
- Depersonalization Neurosis
Signs & Symptoms
Causes
The exact cause of depersonalization disorder is not known. A traumatic event such as military combat, a car accident, or being a victim of a violent crime may trigger an episode of depersonalization disorder. Substance use may cause depersonalization episodes, but not the disorder.
Affected Populations
Depersonalization disorder is believed to affect women twice as much as men. The disorder most commonly affects individuals between the ages of 15 and 30. It is rarely seen in those over the age of 40.
Diagnosis
The diagnosis of depersonalization disorder can be suspected after a complete physical examination and laboratory tests have ruled out any substance or geneal medical condition. A complete psychiatric evaluation should also be conducted.
Standard Therapies
Treatment
Treatment of depersonalization disorder involves psychotherapy. The antidepressant drug desipramine may be beneficial. The drugs dextroamphetamines and amobarbital (Amytal) combined with chlorpromazine (Thorazine) may be beneficial if anxiety is experienced. Other treatment is symptomatic and supportive.
Investigational Therapies
Information on current clinical trials is posted on the Internet at www.clinicaltrials. gov. All studies receiving U.S. government funding, and some supported by private industry, are posted on this government website.
gov. All studies receiving U.S. government funding, and some supported by private industry, are posted on this government website.
For information about clinical trials being conducted at the National Institutes of Health (NIH) in Bethesda, MD, contact the NIH Patient Recruitment Office:
Tollfree: (800) 411-1222
TTY: (866) 411-1010
Email: [email protected]
For information about clinical trials sponsored by private sources, contact:
www.centerwatch.com
A study to determine the effects of fluoxetine on patients with depersonalization disorder was recently (2005) completed. This study was sponsored by the National Institute of Mental Health and Mount Sinai School of Medicine. Further information is available on the www.clinicaltrials.gov web site.
References
Comprehensive Textbook of Psychiatry/V, 5th Ed.: Harold I. Kaplan and Benjamin J. Sadock, Editors; Williams & Wilkins, 1989. Pp. 1038-43.
Diagnostic and Statistical Manual of Mental Disorders: DSM IV, 4th Ed. : A. Frances et. al., Editors; American Psychiatric Association, 1994. Pp. 488-90.
: A. Frances et. al., Editors; American Psychiatric Association, 1994. Pp. 488-90.
Treatments of Psychiatric Disorders, 2nd Ed.: Glen O. Gabbard, M.D., Editor; American Psychiatric Association, 1995. Pp. 1634-53.
Desipramine: A Possible Treatment for Depersonalization Disorder. R. Noyes, Jr. et al.; Canadian Journal Psychiatry (Dec 1987; 32(9)). Pp. 782-84.
Depersonalization in a Nonclinical Population. D. Trueman; Journal Psychol (Jan 1984; 116 (1st half)). Pp. 107-12.
Depersonalization and Agoraphobia Associated with Marijuana Use. C. Moran; British Journal Med Psychol (Jun 1986; 59(pt 2)). Pp. 187-96.
Feelings Unreal: 30 Cases of DSM-III-R Depersonalization Disorder. D. Simeon et al.; Am J Psychiatry (Aug 1997; 154(8)). Pp. 1107-13.
Depersonalization Disorder and Self-Injurious Behavior. D. Simeon et al.; J Clin Psychiatry (1995; 56(suppl 4)). Pp. 36-39.
FROM THE INTERNET
eMedicine – Dissociative Disorders : Article by Idan Sharon, MD
www.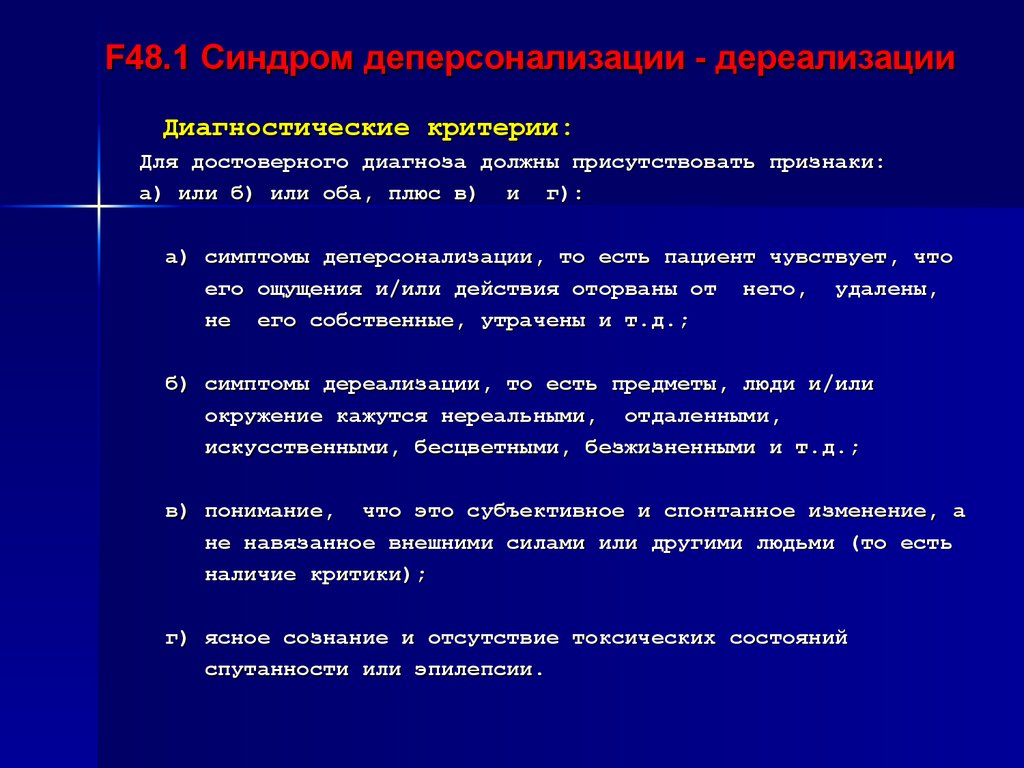 emedicine.com/med/topic3484.htm
emedicine.com/med/topic3484.htm
www.mayoclinic.com/health/dissociative-disorders/DS00574
Years Published
1989, 1998, 2007
The information in NORD’s Rare Disease Database is for educational purposes only and is not intended to replace the advice of a physician or other qualified medical professional.
The content of the website and databases of the National Organization for Rare Disorders (NORD) is copyrighted and may not be reproduced, copied, downloaded or disseminated, in any way, for any commercial or public purpose, without prior written authorization and approval from NORD. Individuals may print one hard copy of an individual disease for personal use, provided that content is unmodified and includes NORD’s copyright.
National Organization for Rare Disorders (NORD)
55 Kenosia Ave., Danbury CT 06810 • (203)744-0100
What is depersonalization and derealization and how to detect them
Perhaps at least once in your life you felt that your body does not belong to you or that what is happening around you seems to be happening not to you and not really.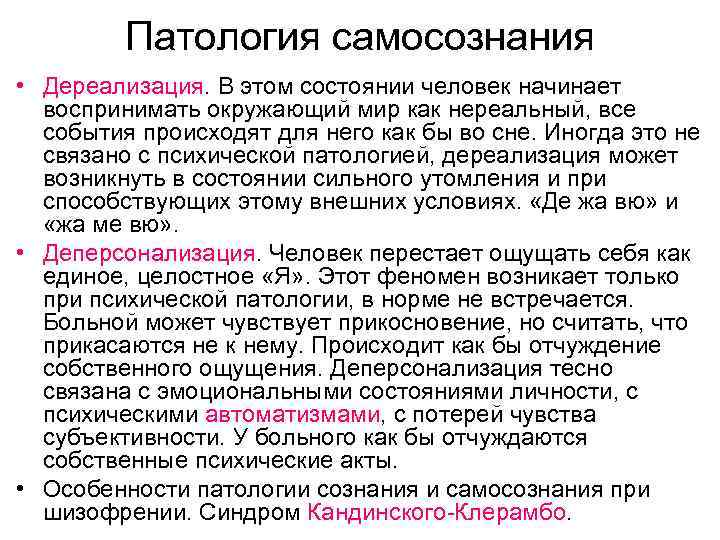 These are quite common in society syndromes of depersonalization and derealization, which can manifest themselves both together and one by one. Due to similarities, the terms are often used together. Zaborona journalist Polina Vernigor figured out what are the signs of these symptoms, when to see a doctor, how to deal with it, and whether it is worth it.
These are quite common in society syndromes of depersonalization and derealization, which can manifest themselves both together and one by one. Due to similarities, the terms are often used together. Zaborona journalist Polina Vernigor figured out what are the signs of these symptoms, when to see a doctor, how to deal with it, and whether it is worth it.
What is depersonalization and derealization?
In themselves they are symptoms. Like headache, dizziness or restlessness. But there is a disorder of depersonalization-derealization, which is already a full-fledged psychiatric diagnosis. The disorder itself occurs in only about 2% of the population, but at least 50% of people experience symptoms at least once in their lives.
As symptoms, depersonalization and derealization can indicate mental disorders (panic attack, phobias, post-traumatic stress disorder, depression, schizophrenia, borderline personality disorder, etc.) or neurological (convulsions, brain tumor, post-concussion syndrome, metabolic disorders, migraines, Meniere's disease, etc.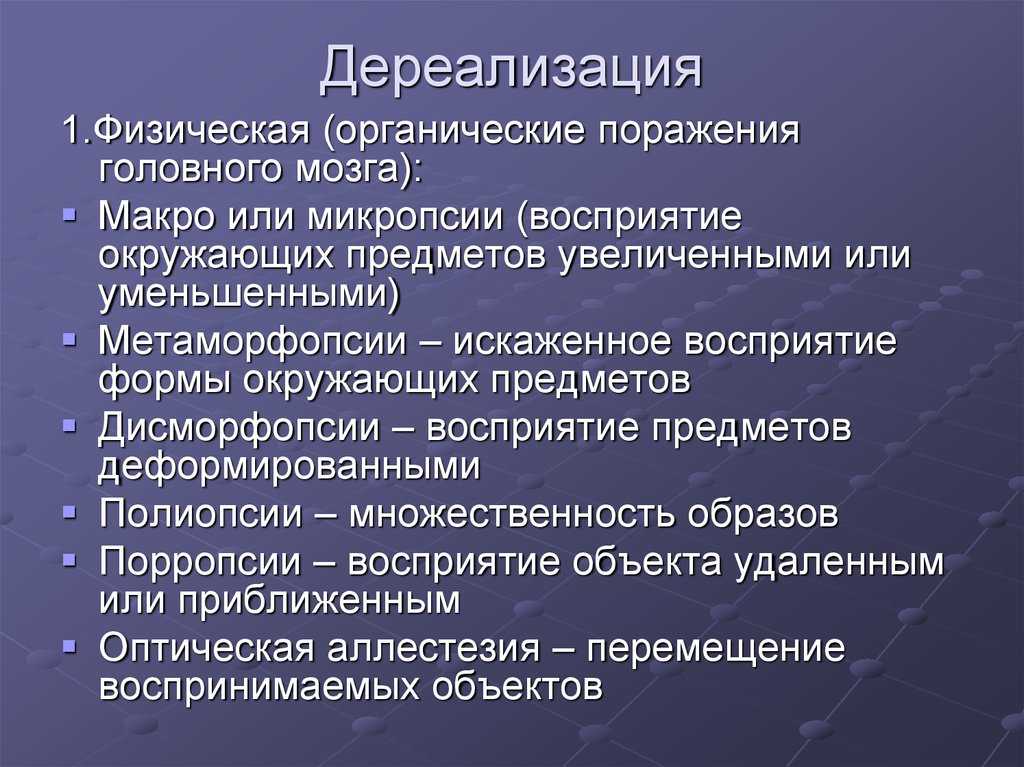 ). They can also occur as a reaction to stress or trauma, and are also found in people with alcohol or drug addiction.
). They can also occur as a reaction to stress or trauma, and are also found in people with alcohol or drug addiction.
Almost always, these symptoms appear either in late childhood or early adulthood. On average, onset occurs at age 16, and 95% of cases are diagnosed before age 25. The first experience of depersonalization can be scary, as patients fear losing control and separating themselves from the rest of society. Most people with these symptoms misinterpret them as signs of severe psychosis or brain dysfunction. This usually leads to an increase in anxiety and obsessions, which contributes to the worsening of symptoms.
- Francisco Goya, Witches' Sabbath (1797-98) / Wikimedia
renamed Depersonalization/Derealization Disorder (DPDR). This diagnosis is classified as a dissociative disorder.
This diagnosis is classified as a dissociative disorder.
The latest International Classification of Diseases (ICD-11) reclassified DPDR as a disorder rather than a syndrome as before, and reclassified it as a dissociative disorder from the list of neurotic disorders. The description that is used in ICD-11 is similar to the criteria found in DSM-5.
How do I know if I have depersonalization or derealization?
You can notice the symptoms yourself, but depersonalization-derealization disorder is a diagnosis that only a doctor can make. No laboratory tests reveal either the symptoms themselves or the disorder. To rule out the physical causes of these conditions, your doctor may order magnetic resonance imaging (MRI), electroencephalography (EEG), x-rays, or a urine test for toxic chemicals. If all these studies turn up nothing, then the cause is most likely mental states.
Signs of depersonalization:
- the feeling that you are watching your thoughts, feelings, body or parts of it from the side - for example, as if you are floating in the air above you;
- feels like a robot and/or has no control over your speech and/or movements;
- your body or parts of it seem distorted, deformed, and your head seems to be wrapped in cotton wool;
- emotional or physical numbness of feelings or reactions to the environment;
- your memories lack emotion, and doubts arise whether they are really your memories.

- Henry Fuseli, Nightmare (1781) / Wikimedia
Signs of derealization:
- a feeling of alienation or ignorance of one's surroundings - for example, as if you are living in a movie or in a dream;
- emotional isolation from people close to you, as if you were separated by a glass wall;
- the environment appears distorted, blurry, colorless, two-dimensional or artificial;
- distortion in the perception of time, for example, recent events are perceived as the distant past;
- distortion of the distance, size and shape of objects.
Depersonalization-derealization disorder can be considered if these symptoms recur frequently and for a long time and are not the result of some other disease or disorder.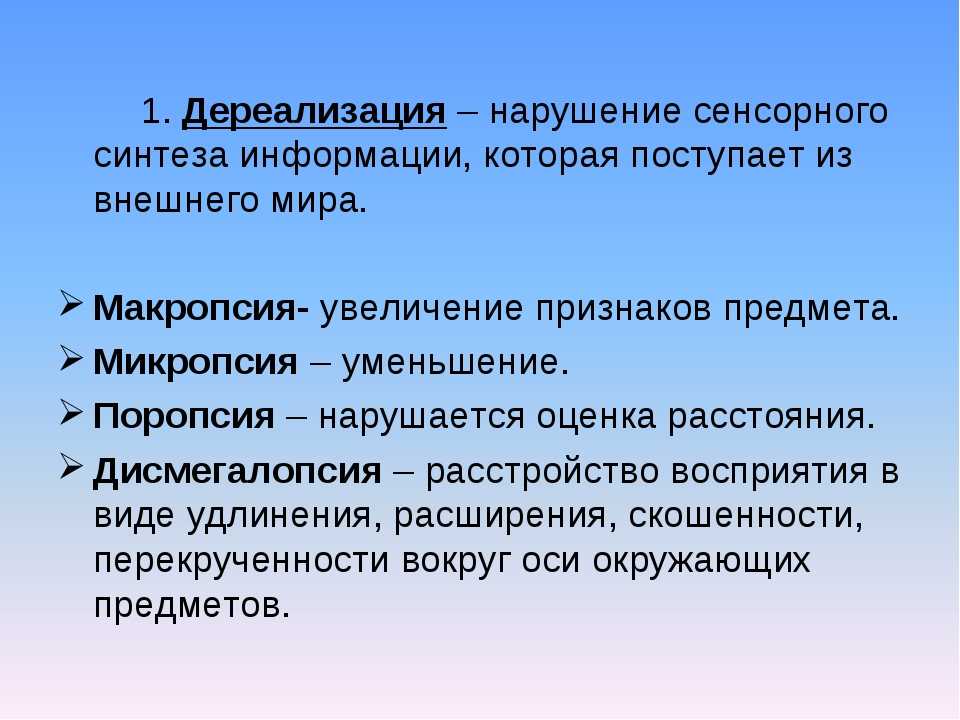 In any case, if it drains you emotionally or interferes with your life, contact a specialist.
In any case, if it drains you emotionally or interferes with your life, contact a specialist.
What to do about it?
Very often, both the symptoms and the disorder do not require special treatment and go away on their own. But it depends on their nature and how much they bother you. For many patients, a full recovery is possible, especially if the symptoms are related to another disorder/disease that is being treated, or to stress that is being relieved. In other cases, depersonalization and derealization become more chronic and less noticeable. Even persistent or recurring symptoms can cause only minimal disturbance if you learn to perceive them correctly - for example, to focus on other thoughts or actions.
- Mikhail Vrubel, “Demon Defeated” (1901-02) / Wikimedia
If we still talk about the treatment of depersonalization-derealization disorder, then psychotherapy helps here. Treatment should take into account all the stresses associated with the onset of the disorder, as well as earlier traumas (eg, childhood abuse or neglect, physical, psychological or sexual abuse, etc.) that may cause patients to have a late onset of depersonalization and/or derealization. .
Treatment should take into account all the stresses associated with the onset of the disorder, as well as earlier traumas (eg, childhood abuse or neglect, physical, psychological or sexual abuse, etc.) that may cause patients to have a late onset of depersonalization and/or derealization. .
Different psychotherapeutic methods are successful for different patients. Cognitive techniques can help block intrusive thoughts about an unreal state of being. Behavioral techniques can help patients perform tasks that distract them from depersonalization and derealization. Grounding Techniques use various senses (such as playing loud music or holding a block of ice) to help patients feel more real in the moment and more connected to the body and surroundings. Psychodynamic Therapy helps patients cope with negative feelings, hidden conflicts or experiences that, due to accumulation, provoke symptoms.
Various drugs are also used, but none of them has been clearly proven to be effective.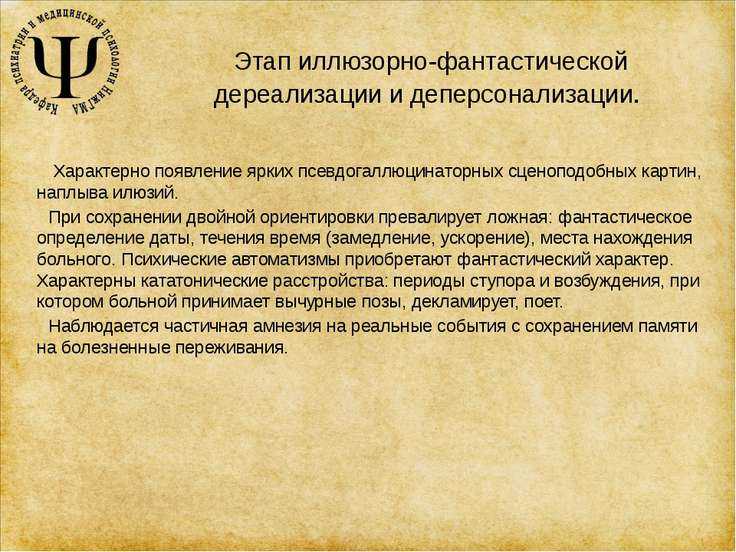 However, some patients benefit from selective serotonin reuptake inhibitors (SSRIs), opioid antagonists, anxiolytics, and stimulants. However, these drugs may work primarily by targeting other psychiatric disorders (eg, anxiety, depression) that cause depersonalization and/or derealization.
However, some patients benefit from selective serotonin reuptake inhibitors (SSRIs), opioid antagonists, anxiolytics, and stimulants. However, these drugs may work primarily by targeting other psychiatric disorders (eg, anxiety, depression) that cause depersonalization and/or derealization.
Treatment of depersonalization and derealization in St. Petersburg
- Home
- Psychiatry
- Treatment of depersonalization and derealization
We treat depersonalization and derealization in our clinic. To start the treatment of the syndrome, a face-to-face consultation with a psychiatrist and a differential examination are necessary to clarify the diagnosis and exclude / confirm diseases that cause a similar condition against the background of the course (for example, OCD, phobic and depressive disorders, delusional and dissociative disorders, early dementia).
About half of the world's population has experienced a state of depersonalization-derealization at least once in their lives. But only 2% of them fully meet the diagnostic criteria for the syndrome.
In order to shorten the period of selection of pharmacotherapy in the treatment of depersonalization and derealization, hospitalization (4–6 weeks) is required. The conditions of the hospital allow you to monitor the patient's condition in dynamics and promptly adjust drug treatment. Also, in the hospital of the clinic, patients are provided with psychotherapeutic assistance, which precedes individual and / or group sessions after discharge, adapting to a full life in the family and society.
In particular, if the disease has caused intra-family conflicts, they can be resolved in family therapy sessions. In addition, participation in a group of open problems will allow you to get rid of internal experiences, restore lost communication skills. In parallel with outpatient treatment (taking prescribed drugs), one should not forget about visits to the attending physician, who should be informed of any conditions that cause anxiety or seem unusual. Such an approach to the treatment of depersonalization and derealization will make it possible to correct drug treatment in a timely manner, get rid of addictive attitudes and, as a result, prevent a relapse of the disease.
Such an approach to the treatment of depersonalization and derealization will make it possible to correct drug treatment in a timely manner, get rid of addictive attitudes and, as a result, prevent a relapse of the disease.
Doctor's consultation on the treatment of depersonalization:
+7 (812) 407-18-00
Thank you for your trust!
- Assistance in resocialization
- Safe drug therapy
- Psychologists with clinical experience
| Service | Price | |
|---|---|---|
| Psychotherapist appointment | 5 000 ₽ | |
| Family Therapy | 10 000 ₽ | |
| Hypnotherapy | 8 000 ₽ | |
| Psychiatric consultation | 5 000 ₽ |
Causes //psychiatr.
 ru
ru Vestibular function and depersonalization/derealization symptoms — https://pubmed.ncbi.nlm.nih.gov
Depersonalization under academic stress — https://pubmed.ncbi.nlm.nih.gov
Update date: 12/28/2020
- Depersonalization and derealization
- Suicidal behavior
- Anxiety disorder
Make an appointment
Date and time: (not set)
Make an appointment with a psychiatrist
Make an appointment with a psychiatrist
Select the date and time of your appointment
Today
October 31
Tomorrow
November 01
Wednesday
November 02
Thursday
November 03
Friday
November 04
Saturday
November 05
Sunday
November 06
Monday
November 07
Tuesday
November 08
Wednesday
November 09
Thursday
November 10
Friday
November 11
Saturday
November 12
Sunday
November 13
Monday
November 14
Tuesday
November 15
Wednesday
November 16
Thursday
November 17
Friday
November 18
Saturday
November 19
Sunday
November 20
Monday
November 21
Tuesday
November 22
Wednesday
November 23
Thursday
November 24
Friday
November 25
Saturday
November 26
Sunday
November 27
Monday
November 28
Tuesday
November 29
Wednesday
November 30
Treatment of depersonalization and derealization is carried out on
Bocharov Alexey
Viktorovich
Psychiatrist, psychotherapist
Head physician of clinic
Experience 41 years
Psychiatrist, psychotherapist, sexologist, child psychiatrist
Work experience 41 years
Sinenchenko Andrey
Georgievich
Psychiatrist, psychotherapist
PhD
Work experience 22 years
Psychiatrist, psychotherapist, narcologist
Work experience 22 years
Zun Sergey
Andreevich
Psychiatrist, narcologist
PhD
Experience 33 years
Psychiatrist, narcologist, psychotherapist
Work experience 33 years
Lisitsyna Elena
Alekseevna
Psychiatrist
Top category
Experience 33 years
Psychiatrist
Work experience 33 years
Buchelnikova Victoria
Viktorovna
Psychiatrist
Head of amb.