What are the withdrawal symptoms of seroquel
How Long Does Withdrawal From Seroquel Last?
Seroquel is a prescription medication that is commonly used to treat various mood disorders such as depression. While it’s intended for short-term use, individuals can develop a dependency to the medication over time. With the onset of Seroquel abuse or addiction, a host of health risks can arise. For those seeking to safely stop Seroquel use they may wonder about the process. How long does withdrawal from Seroquel last and are there drastic health concerns to consider?
If you or someone you know is experiencing any of these symptoms, you should seek help and treatment.
AspenRidge is one of Colorado’s leading providers of dual diagnosis treatment for substance abuse and mental health. We provide outpatient programs for those who suffer from addiction and their families. Find out more about our prescription drug addiction treatment program options.
Important Seroquel Withdrawal Information
If you suddenly stop taking Seroquel, there is a risk that you will begin to experience Seroquel withdrawal symptoms. These can be either severe or mild and vary from one person to the next. One thing is for certain, experiencing these withdrawal symptoms is not easy. Some individuals may experience restlessness, vomiting, or nausea while others can suffer from withdrawal dyskinesia. These are uncontrollable and erratic movements in the face, arms, legs, or torso.
Read on as we discuss what Seroquel is in further detail, the risks of misusing antidepressant medications, and what to expect with the withdrawal process.
What is Seroquel?
Seroquel, also known as Quetiapine, is a psychotropic medication that is taken to treat mood disorders such as depression and bipolar disorder. It is also widely used to treat schizophrenia but is only available for adults and children who are over the age of 13.
Belonging to the antipsychotic class of drugs, Seroquel is categorized as an atypical antipsychotic and second-generation antipsychotic.
Seroquel works to alter certain activities of natural substances within the brain. It is approved for sale and use by the FDA, as long as it is under a medical professional’s prescription.
Although this medication is not considered to be a controlled substance, it can be misused and abused in some circumstances.
Some studies conducted by the National Health Institute have found that Seroquel is the most abused of all antipsychotic medications.
The potential for this drug to be misused is exaggerated when there is no prescription. Even with medical guidance, many people take Seroquel in higher doses and for longer periods than they are advised to.
You may recognize Seroquel through its various street names such as Squirrel, Susie Q, Quell, and Baby Heroin. When not prescribed, many abusers misuse the substance by crushing and inhaling it. Some will mix it with water and then proceed to administer the drug intravenously.
Such misuse tends to lead to Seroquel addiction and abuse which, in turn, leads to a higher likelihood of overdosing.
Seroquel Withdrawal Symptoms
How long does withdrawal from Seroquel last, though? Seroquel is taken for numerous reasons. Some take it to treat anxiety and bipolar disorder while others may take it to treat schizophrenia. Although intended as a short-term medication for such disorders, withdrawal symptoms can become severe in some cases.
Withdrawal is usually experienced by those who have become addicted to the medication. Some Seroquel withdrawal symptoms include:
- Dizziness
- Nausea
- Vomiting
- Insomnia
- Increases sweating
- An increased heart rate
- Agitation
- Restlessness
- Muscle rigidity
- Abdominal pain
If you experience withdrawal symptoms, they can last from only a few hours to several weeks in extreme cases.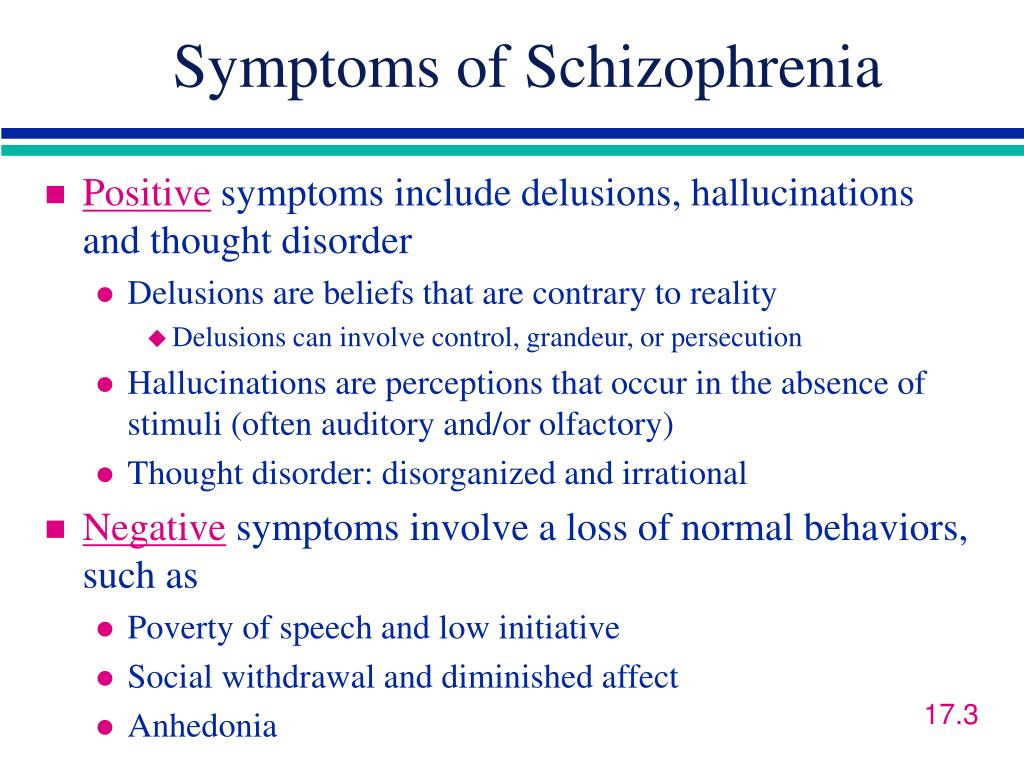 This withdrawal timeline can include new withdrawal, rebound withdrawal, and post-withdrawal.
This withdrawal timeline can include new withdrawal, rebound withdrawal, and post-withdrawal.
How Long Does Withdrawal Last?
So, how long does withdrawal from Seroquel last? New withdrawal symptoms usually begin between the first and fourth day after ceasing the medication but the symptoms can last for up to a week. In some circumstances, the symptoms can last for up to six weeks.
Rebound withdrawal symptoms tend to begin around the same time (one to four days after ceasing medication). However, some of these symptoms are not always associated with Seroquel withdrawal. Nevertheless, these symptoms may last for six weeks. If they persist longer than this, an individual will be experiencing persistent post-withdrawal.
Certain factors determine the severity of the withdrawal symptoms. Examples are:
- The duration of Seroquel use
- The age of the medicine user
- Pre-existing mental health disorders
- Lack of support
Lack of support is not something you will experience with AspenRidge.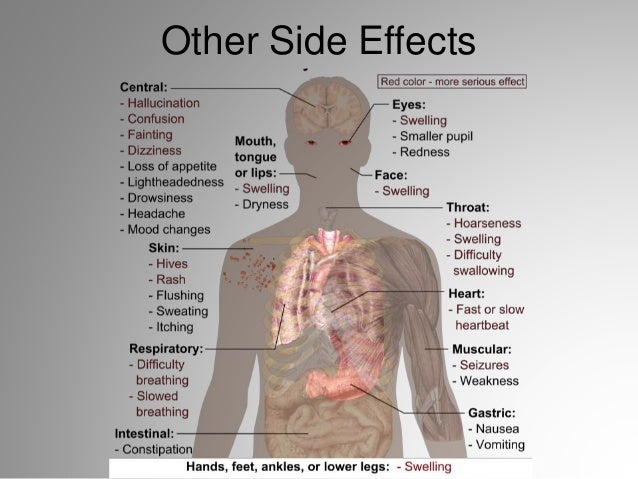 We have a team of fully qualified counselors ready to help you on your road to recovery.
We have a team of fully qualified counselors ready to help you on your road to recovery.
Our dual diagnosis programs aim to treat those who suffer from addiction and mental health issues.
Find out more here.
Risks of misusing anti-depressant medication
One key question to consider is whether depression or substance abuse comes first. Mental health and addiction are so entwined but both can impact an individual’s life and recovery. We cover this in greater detail via this page – What Comes First Depression or Substance Abuse?
Co-occurring disorders can also have significant consequences on how medications are received and whether someone has a higher chance of abusing a drug.
Studies have discovered that the rate of prescription drug abuse has reached “epidemic proportions.” Antidepressants have become one of the misused prescription drugs in the last few decades.
According to a study by Elizabeth A Evans and Maria A Sullivan in 2014, the main motivation behind the abuse of antidepressant medication is to achieve a psychostimulant-like effect. Unlike many other drugs, antidepressants can be easier to come by. Therefore, they are abused in higher doses through various means of administration such as intravenously or intranasally.
Unlike many other drugs, antidepressants can be easier to come by. Therefore, they are abused in higher doses through various means of administration such as intravenously or intranasally.
The negative consequences of this misuse and addiction tend to vary depending on the class of antidepressants and pharmacology. However, some common side effects include confusion, seizures, and psychotic-like episodes.
Those most vulnerable to anti-depressant abuse usually have a history of substance abuse and/or live in a controlled environment.
Coming Off Seroquel:
When coming off Seroquel, there are some warning signs of antidepressant addiction and abuse such as:
- Aberrant behaviors
- Bloodshot eyes
- A diminished appearance
- A change in appetite
- Poor or odd sleeping patterns
- Slurred speech
- Financial hardship
When antidepressant abuse is detected, a treatment plan would be sought as soon as possible.
Seroquel Withdrawal Anxiety
There is a lot of Seroquel withdrawal anxiety among both people taking the medication, and their friends and family members. Many even ask with great concern: “Can Seroquel withdrawal kill you?”. That is an extreme question, but you must exercise immense caution when stopping a medication such as this one.
Keep an eye out for possible side effects as well. These include:
- Mental confusion
- A lack of emotion
- Uncontrollable shaking
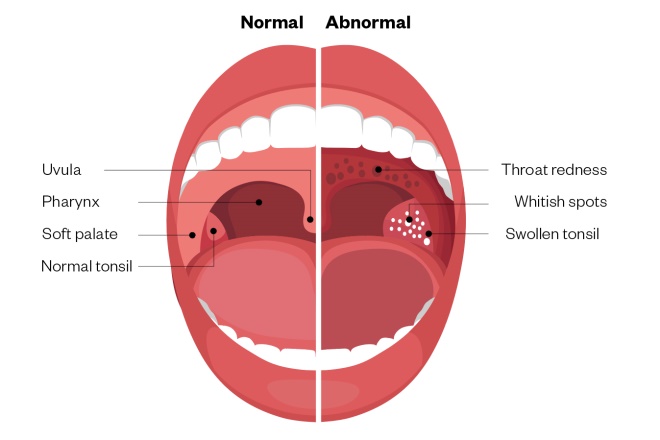
- A sore throat
- Sexual dysfunction/reduced sex drive
- Seizures
- Paranoia
- Hallucinations
- Headaches
- Insomnia
- Irritability
- Blurred vision
- Agitation
- Weight gain
- Loss of appetite
If you or anyone you know is experiencing such symptoms and may have abused antidepressant medication, there are treatment plans in place.
AspenRidge Recovery Can Help
AspenRidge is dedicated to helping those who suffer from the disease of addiction as well as their families. We understand that addiction and mental health treatment is not one size fits all. That is why we have a range of programs to suit each individual’s unique needs. With a lifetime of recovery support programs, AspenRidge is here to help. If you need that help, contact us today.
Seroquel Withdrawal Symptoms | Quetiapine's Questionable Efficacy
Last Updated on September 17, 2022 by Carol Gillette
Alternative to Meds Editorial Team
Medically Reviewed by Dr Samuel Lee MD
Seroquel withdrawal (quetiapine) may be part of a comprehensive treatment program using proven protocols for improved mental health naturally. Seroquel is a commonly prescribed antipsychotic medication used in the treatment of schizophrenia, and mania or depressive episodes of bipolar conditions. As is the case for most psychoactive medications, using Seroquel for several months or longer may lead to physical dependence.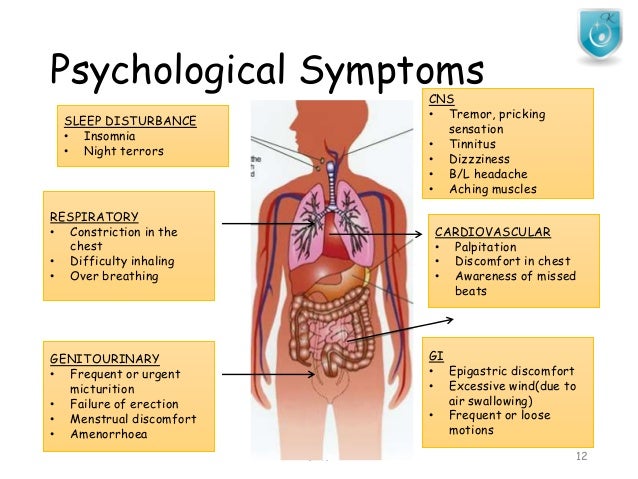
If you or a loved one needs help to navigate Seroquel (quetiapine) withdrawal, this article provides useful information including details about Seroquel (quetiapine) withdrawal symptoms, treatment, withdrawal timeline, and resources for recovery.
Table of Contents:
- What is Seroquel?
- Seroquel (Quetiapine) Side Effects
- Seroquel (Quetiapine) Withdrawal Symptoms
- Seroquel Withdrawal Timeline
- Is It Safe To Quit Seroquel Cold Turkey?
- How Long Does Seroquel Stay in Your System?
- Treatments for Seroquel Withdrawal
- Seroquel Withdrawal Success Stories & Videos
What Is Seroquel?
Seroquel is an atypical antipsychotic drug available as a tablet or extended-release tablet. Its generic name is quetiapine. Seroquel is approved by the U.S. Food and Drug Administration (FDA) to treat schizophrenia and acute manic episodes, and as an adjunctive treatment for major depressive disorder.1
Aside from the FDA-approved guidelines, many off-label uses for Seroquel have developed such as for insomnia, PTSD, OCD, substance abuse and addiction, delirium, anxiety, depression (especially in those who have stopped seeing benefits from SSRIs), and personality disorders. 2 We find a lot of people take Seroquel specifically as a sleep aid, usually at a low dose of 25-150 mg.
2 We find a lot of people take Seroquel specifically as a sleep aid, usually at a low dose of 25-150 mg.
There have been reported uses of Seroquel by crushing and snorting, or used intravenously, sometimes in combination with cocaine.
Is Seroquel Addictive?
While it’s only available by prescription, quetiapine is not on the federal list of controlled substances. In general, it’s not considered addictive. However, a 2013 clinical study conducted on experimental rats by Chinese researchers found clear evidence that quetiapine has the potential to cause psychological dependence in animals.3
In addition, a number of individuals have self-reported a belief that they have become addicted to Seroquel, which is known on the street as “Susie-Q” or “quell.” 4
Seroquel (Quetiapine) Side Effects
There can be a wide range of side effects from this medication, from mild to moderate to severe. Not everyone experiences identical side effects of substance use, such as those listed here. Always discuss changes that occur while on Seroquel with your prescribing physician. The following is not a conclusive list of side effects; if you’re experiencing other reactions to Seroquel, consult your doctor or a medical professional.5
Not everyone experiences identical side effects of substance use, such as those listed here. Always discuss changes that occur while on Seroquel with your prescribing physician. The following is not a conclusive list of side effects; if you’re experiencing other reactions to Seroquel, consult your doctor or a medical professional.5
Common side effects could include:
- Vertigo/dizziness
- Abnormal physical weakness
- Nausea
- Constipation
- Appetite changes
- Weight gain
- Drowsiness/fatigue
- Dryness of the mouth
- Low sodium levels
- Nightmares
- Disturbed sleep
- Sleepwalking, sleep-driving, etc.*
- Lightheadedness
- Tachycardia (elevated heart rate at rest)
Less common, but more severe adverse effects should be carefully monitored and could include suicidality (ideation and behavior; especially noted in younger patients under age 25), tardive dyskinesia, tachycardia, movement disorders, involuntary repeating movements, tremors, cataracts in eyes, slowed heartbeat, sleep apnea, diabetes, abnormal liver function or liver failure, seizures, stroke (especially in elderly patients), pancreatitis, amnesia, hepatitis, and rarely, Neuroleptic Malignant Syndrome.
- Sleepwalking or other normal activities during sleep — sleep-driving, sleep shopping, sleep-texting, etc. — of which the person has no memory can also occur.
- High blood sugar, possibly extreme and associated with diabetic acidosis, coma, or death, has also been reported in patients treated with Seroquel.
Seroquel (Quetiapine) Withdrawal Symptoms
Stopping Seroquel abruptly will frequently evoke a wide range of withdrawal symptoms, generally referred to as Seroquel (Quetiapine) Discontinuation Syndrome.8 If the decision to come off Seroquel is made, stopping should never be done abruptly unless to avert a life-threatening reaction such as NMS. Always seek medical oversight and guidance for safety.
Even when slowly tapering off of the drug, there can still be some significant Seroquel withdrawal symptoms. These symptoms might be more severe if the patient took the medication for a very long time, and at high dosages. Our Seroquel tapering page goes into the nuances of tapering strategies based upon the duration of use.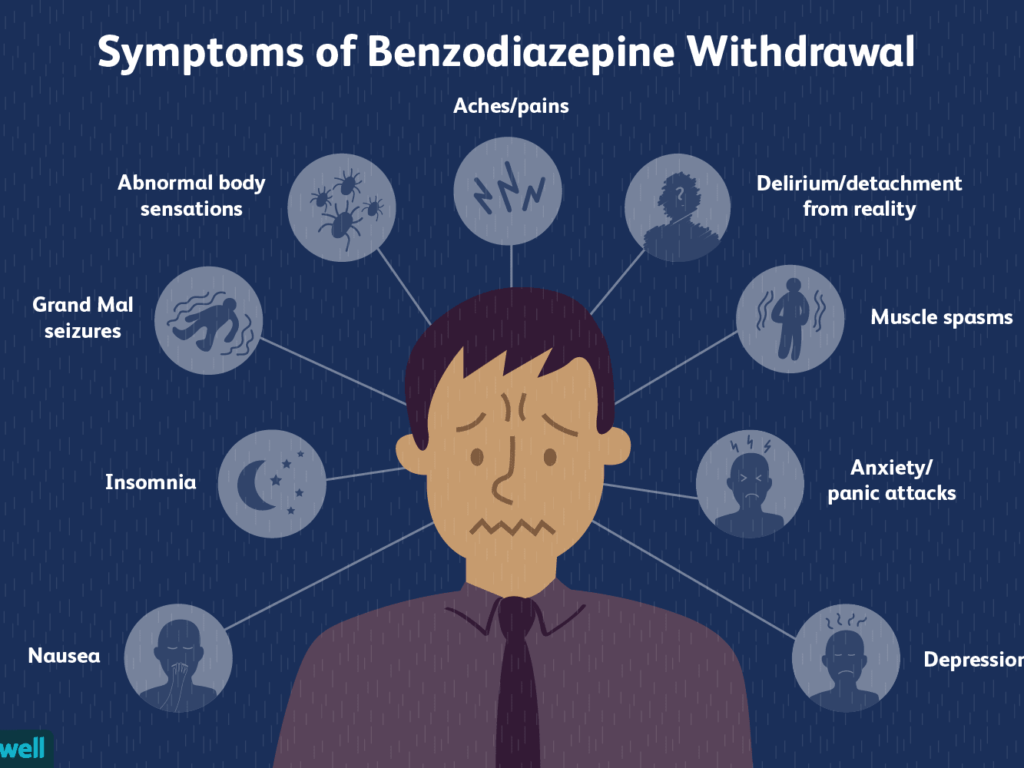 A list of just some of the reported Seroquel withdrawal symptoms follows.
A list of just some of the reported Seroquel withdrawal symptoms follows.
Seroquel withdrawal symptoms may include:
- Suicidal ideation or behavior
- Seroquel Withdrawal Rebound Psychosis
- Rebound mania
- Psychotic symptoms that did not exist prior to taking antipsychotics
- Insomnia
- Hypersensitivity to light, sound, temperature, all sensory perceptions
- Vomiting
- Headaches
- Racing heart, tachycardia, hypertension
- Unusual mood swings that can change rapidly
- Loss of appetite
- Nausea
- Dizziness
- Anxiety
- Agitation
- Loss of concentration
- Depression
- Excessive sweating
- Dysphoric unease with life
- Some limited reports of withdrawal dyskinesia
Abrupt or fast Seroquel withdrawal can cause a rebound psychosis. Ample caution and patience for a slow withdrawal are warranted.
Everyone has a different set of withdrawal symptoms, and in that way, there is no one-size-fits-all description.
However, the most consistent symptoms we have seen at Alternative to Meds Center are:
- Seroquel Withdrawal Rebound Psychosis
- Rebound mania
- Insomnia
- Loss of appetite
Suddenly not sleeping, not eating, and acting manic when enduring Seroquel withdrawal is a sure sign that things are most likely going too fast and that the rate of withdrawal needs to be slowed down.
There are instances where people without prior psychotic symptoms experienced withdrawal psychosis when stopping neuroleptics such as Seroquel.
Seroquel Withdrawal Timeline
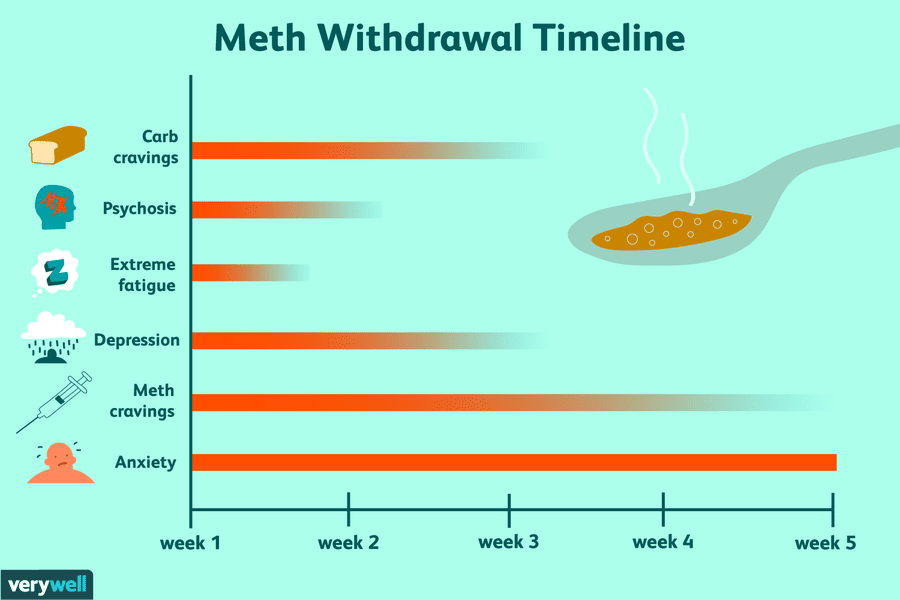
Seroquel withdrawal symptoms are different for everyone. Withdrawal can be broken into three phases: new withdrawal, rebound withdrawal, and Post-Acute Withdrawal Syndrome.
Phase 1: New Withdrawal
Studies indicate that most withdrawal symptoms occur during the first four weeks of stopping antipsychotic drugs.8 They often start one to four days after discontinuing medication and last up to six weeks, sometimes lessening during that period.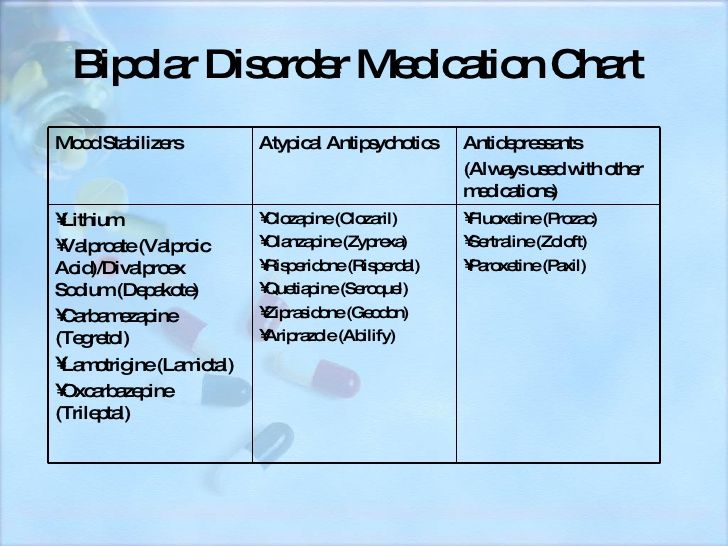 Symptoms associated with cessation of quetiapine can include interruptions in sleep and insomnia, paresthesia (burning or prickling sensations), nausea, vomiting, diarrhea, dizziness, hypertension (high blood pressure), an increased heart rate, agitation, anxiety, sweating, anorexia, and myalgia. Though rare, movement disorders can emerge upon abrupt withdrawal of neuroleptic medications. Restlessness or hyperkinesia may last longer, sometimes months.6,7,25
Symptoms associated with cessation of quetiapine can include interruptions in sleep and insomnia, paresthesia (burning or prickling sensations), nausea, vomiting, diarrhea, dizziness, hypertension (high blood pressure), an increased heart rate, agitation, anxiety, sweating, anorexia, and myalgia. Though rare, movement disorders can emerge upon abrupt withdrawal of neuroleptic medications. Restlessness or hyperkinesia may last longer, sometimes months.6,7,25
Phase 2: Rebound Withdrawal
Rebound withdrawal can occur concurrently with or last beyond the new withdrawal phase.8 The symptoms exhibited in rebound withdrawal are understudied and can vary greatly from individual to individual. It may not always be clear unless a comprehensive patient history is available whether symptoms are newly emerging as a result of drug withdrawal, or whether pre-medication symptoms are recurring. Research has suggested that the symptoms in rebound withdrawal are frequently more severe than symptoms experienced pre-medication. 23
23
Phase 3: Post-Acute Withdrawal Syndrome
Post-Acute Withdrawal Syndrome (PAWS) is a term used to describe withdrawal symptoms that can persist weeks or even months after discontinuing certain drugs.9 PAWS is thought to occur because virtually all drugs can cause physiologic and neuroadaptive changes. During drug use, the brain and CNS adapt to accommodate changes in available neurotransmitters. When you discontinue the drug, neurotransmitters can change again, increasing excitability or causing other reactions.
Symptoms can include things like irritability, anxiety, obsessive-compulsive behaviors, difficulty maintaining social relationships, pessimism, disturbed sleep patterns, and greater sensitivity to stress.9
How Long Does Seroquel Stay in Your System?
The half-life of Seroquel is six hours. Theoretically, it takes approximately six hours to clear 50 percent of the active drug from your system after you stop taking it and 24 to 48 hours to completely clear it after cessation.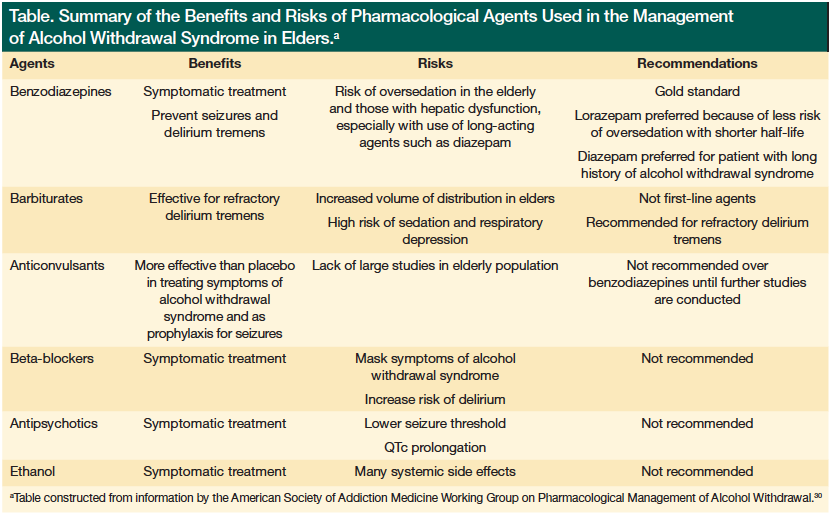 10
10
However, the body adapts to the presence of medications. The longer Seroquel is taken, the more adaptations are likely to develop. As a result, it may take considerably longer for your body to recalibrate back to pre-medication states and reverse the antipsychotic-induced dopamine supersensitivity or other neuroadaptive changes.
Changing neuroadaptive states, often called “Seroquel withdrawal syndrome,” can continue to plague patients for weeks, months, or even years. A precisely calibrated diet and supplement regimen can be designed to provide the essential neurotransmitter precursors needed to repair and normalize, and possibly shorten these after-effects.
Is It Safe To Quit Seroquel Cold Turkey?
Stopping Seroquel should rarely be done abruptly. In the vast majority of cases, antipsychotic withdrawal should be extremely gradual and attended with as much support as possible, including medical supervision, to help ease the person through to a successful outcome.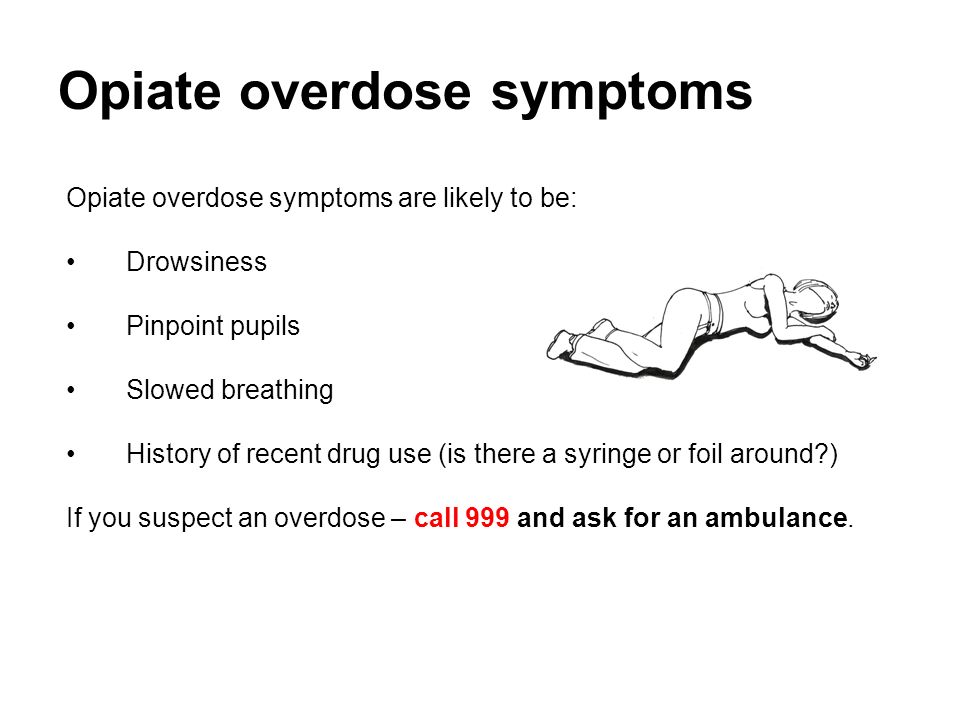
Abrupt cessation should only occur in rare cases where life-threatening reactions to the drug need to be controlled, such as NMS (neuroleptic malignant syndrome).5
Based on 15 years of experience, we suggest that Seroquel withdrawal be done with our team of health professionals in an inpatient setting to help navigate the complexities that may occur.
Does Seroquel Work Long-Term?
We are unable to find research demonstrating the long-term efficacy of antipsychotics like Seroquel.11 While Seroquel has an impressive ability to quickly thwart a psychotic event, and may even be life-saving in certain cases, the long-term use efficacy remains questionable.
Martin Harrow and colleagues recently published a study in the Feb 2021 edition of Psychological Medicine following patients with schizophrenia and schizoaffective psychosis for 20 years.12 Their results showed that those suffering from a severe mental illness who stopped taking medication within the first two years were six times more likely to recover than those who continued the antipsychotics.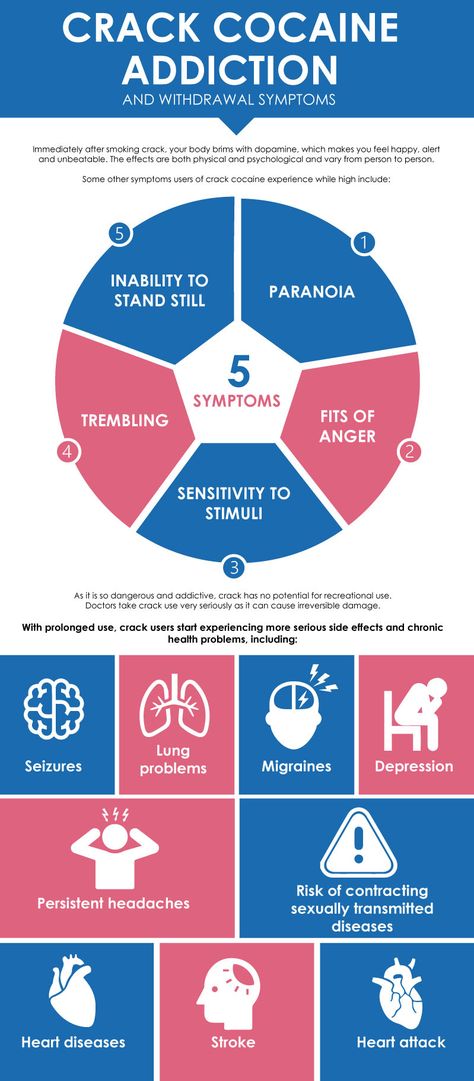
“Even when the confound by indication for prescribing antipsychotic medication is controlled for, participants with schizophrenia and affective psychosis do better than their medicated cohorts.”
“These and previous data indicate that after 2 years, antipsychotics no longer reduce psychotic symptoms and participants not on antipsychotics perform better.” ~Harrow, Jobe & Tong, Journal of Psychological Medicine.12
The reason for the lack of long-term efficacy may be the way that the body adapts to the presence of the drug. According to three different independent researchers — Chouinard, Fallon, Harrow, and respective colleagues — there may be an antipsychotic-induced sensitivity to the dopamine receptors, termed drug-induced supersensitivity psychosis, as they attempt to compensate.13-15 This drug-induced perpetuation of psychosis is also termed tardive psychosis.
It cannot be said that all people do better off of antipsychotics.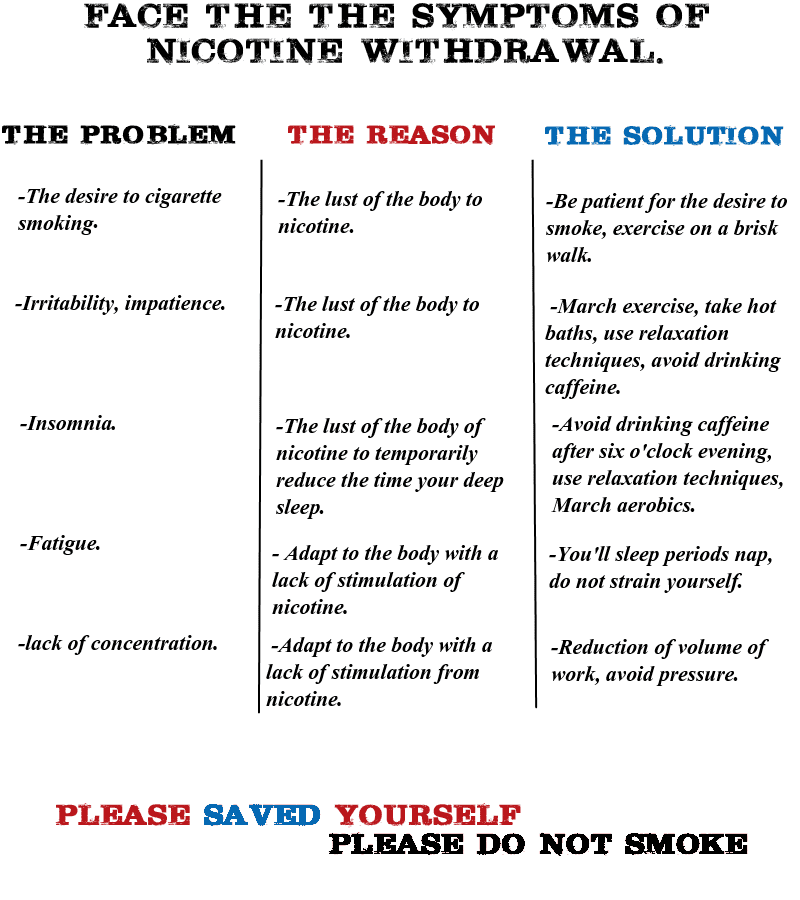 However, the research presents a strong case for investigating safe alternatives to antipsychotics like Seroquel for long-term treatment of symptoms.
However, the research presents a strong case for investigating safe alternatives to antipsychotics like Seroquel for long-term treatment of symptoms.
At Alternative to Meds Center, any persons wishing to undergo Seroquel withdrawal are screened for the probability of a successful outcome.
Treatments for Seroquel Withdrawal
If you or a loved one is considering a treatment program designed to help taper Seroquel safely, the protocols used at Alternative to Meds Center may be helpful to learn more about.
Each client’s program is designed within a holistic scientific context at our treatment center to carefully investigate root causes that may have contributed to your need for prescription medication in the first place.
Natural Remedies
Many symptoms of Seroquel withdrawal can be treated using natural methods. For instance, studies have shown that poor nutrition can lead to depression, and an improved diet can likewise improve mental health.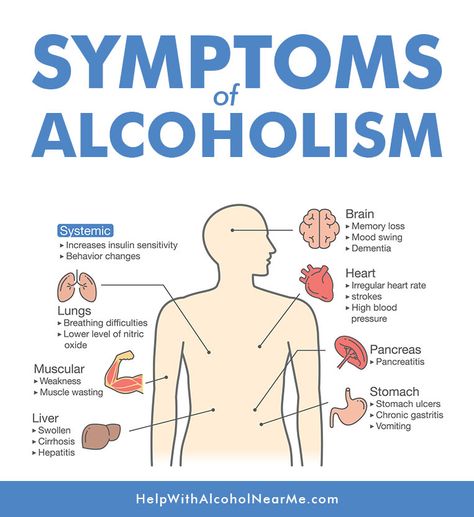 16 Improving nutrition by reducing carbohydrates and adhering to a Mediterranean diet high in Omega-3 fatty acids and other vital nutrients have been clearly associated with improved mental health.24
16 Improving nutrition by reducing carbohydrates and adhering to a Mediterranean diet high in Omega-3 fatty acids and other vital nutrients have been clearly associated with improved mental health.24
Likewise, exercise has proven helpful in preventing depression.17,18 And yoga has been shown to decrease anxiety, depression, and stress significantly.19
Heavy metal toxicity testing and neurotoxin removal are fundamentals that may have been missed in earlier treatments. It is likely for many that toxicity played a role in symptoms for which no other reason was found to explain neurotransmitter imbalances.20 We have found that once the offending pollutants, chemical residues, heavy metals, food preservatives, industrial exposures, etc., have been isolated and gently purged, clients typically experience a resurgence in quality of sleep, appetite, energy, and mood.21
Knowing as much as possible about drugs like Seroquel, medication alternatives, side effects, and withdrawal is vital. This is why we offer a comprehensive education component in our programs.
This is why we offer a comprehensive education component in our programs.
Holistic Medicine
A comprehensive series of steps form a foundation for better health as a client moves through the Alternative to Meds Center program. You may never have been introduced to orthomolecular medicine, nebulized glutathione treatments, clay packs, infrared sauna, and many other gentle yet effective treatments we provide. We invite you to review our services page on the website to learn more about these and other therapies.
You may be surprised by how beneficial these holistic therapies can be. There are many such protocols used before, during, and after the taper is complete. Please contact us to find out more about our program and get answers to any specific questions you may have. Perhaps now is the time to look at a science-based, health-oriented program to assist you in your restorative health goals.
We invite you to learn more about our comfortable, inpatient, retreat-style facility, and how we may be able to help you move confidently toward sustainable and natural mental health.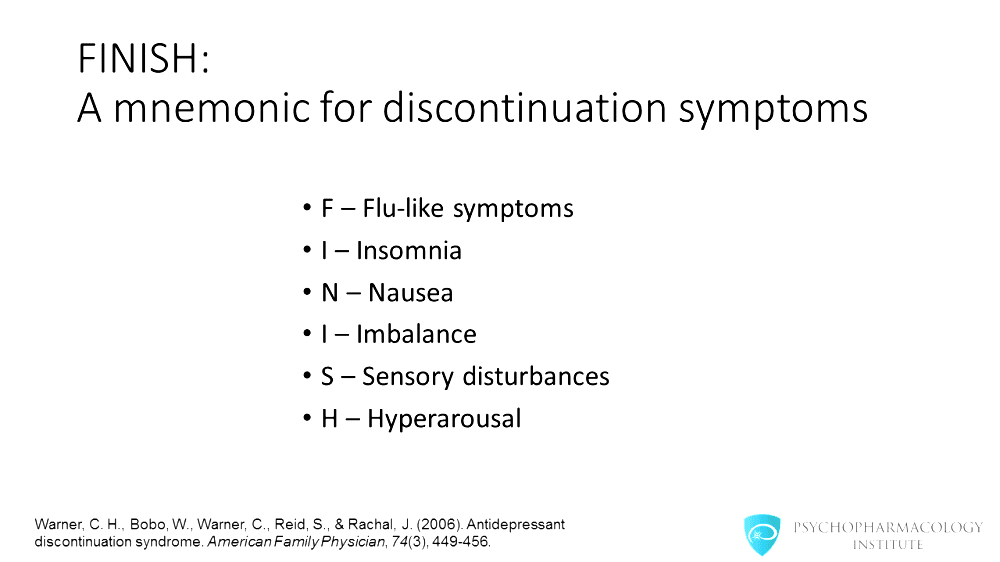 Please ask us all your other questions about Seroquel withdrawal, alternatives, side effects, and other information you may be interested in for yourself or a loved one.
Please ask us all your other questions about Seroquel withdrawal, alternatives, side effects, and other information you may be interested in for yourself or a loved one.
Seroquel Withdrawal Success Stories & Videos
It takes a skilled professional to help navigate Seroquel withdrawal smoothly. Even if antipsychotic medications are warranted at the time of a crisis, it may not be necessary to endure the related debilitating side effects for a lifetime. According to some long-term research, many schizophrenic patients do better in the long run without antipsychotics.22
Alternative to Meds has been the expert on antipsychotic withdrawal for over 15 years. We have published evidence documenting our success. Often we find that patients were put on psychiatric meds for medical conditions, drug-induced psychosis, or other factors that have since changed. A person could have also been misdiagnosed.
A person could have also been misdiagnosed.
This video is of a former schizophrenic who was treated at our center. It was found that his previous diagnosis and treatment did not lead to recovery. Instead, his issues were discovered to be food allergies complicated by recreational drug use. He came off of the medications and became an international speaker, helping others to understand the true components of mental health. This video was taken 10 years after his Alternative to Meds experience.
What is withdrawal syndrome and how to overcome it
December 10, 2019 Likbez Health
Abruptly quitting a bad habit can kill you.
The state of withdrawal Perhaps the term "withdrawal syndrome" does not mean anything to you. But you are probably familiar with the word "breaking". The painful physical sensations experienced by a drug addict who has lost his habitual drug is a well-known thing.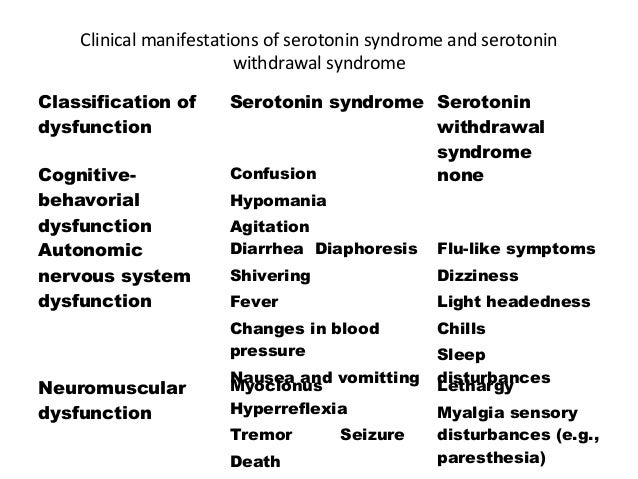
Abstinence (the second name for withdrawal) can also be caused by substances that are much more harmless at first glance, for example, some drugs. nine0003
Lifehacker found out everything about withdrawal syndrome, its possible consequences, and how to get rid of it.
What is the withdrawal syndrome and where does it come from
The withdrawal syndrome is always associated with the formed dependence. At some point, a person decides (or is forced) to give up the usual dose of one or another substance, on which his brain has “hooked” for weeks, months, or even years of use, and a panic begins in the organ. However, not in a vacuum.
Psychoactive substances change the way the brain works. For example, they increase the activity of some receptors, which increases the production of hormones - the same "pleasure hormone" dopamine or exciting adrenaline. There is also an increase in the level of certain neurotransmitters - excitatory or, on the contrary, relaxing. All this, combined with other reactions, leads to a simple thing: the brain, which is constantly fed with a psychoactive substance, stops regulating an adequate amount of hormones and neurotransmitters on its own. nine0003
All this, combined with other reactions, leads to a simple thing: the brain, which is constantly fed with a psychoactive substance, stops regulating an adequate amount of hormones and neurotransmitters on its own. nine0003
Well, really, why work? After all, the owner will drink or take a pill - and with hormones everything will become fine by itself.
When the time comes for regular use of a psychoactive substance, but the coveted powder (conditionally) is not there, everything becomes bad. The body needs the usual doses of hormones and neurotransmitters. But the brain is unable to produce them. This severe imbalance between “I want” and “I can” leads to a whole range of physical and emotional consequences.
What substances cause withdrawal syndrome
It's not just drugs, although you can't do without them. The five most addictive substances are:
- Heroin and other opiates.
- Cocaine.
- Nicotine.
- Barbiturates are sedatives and hypnotics based on barbituric acid.
- Alcohol. By the way, it is called the most dangerous drug in the world - based on the speed of addiction, and on the impact on the body as a whole, and on the severity of withdrawal that occurs when trying to give up alcohol abuse. nine0028
This list is certainly not complete. Some antidepressants, psychostimulants, antipsychotics, benzodiazepine tranquilizers, and “harmless” drugs such as marijuana and ecstasy also cause addiction, which is fraught with withdrawal syndrome.
How to recognize the withdrawal syndrome
The symptoms vary depending on which substance is lacking in the body. Withdrawal of some drugs causes severe physical discomfort. The lack of others makes itself felt not so much physically as mentally. nine0003
In general, there are 10 most common signs of withdrawal.
Mental symptoms of withdrawal syndrome:
- Anxiety. This includes anxiety, irritability, panic attacks.
- Depressed mood. A person suffering from withdrawal wants only one thing: to be left behind.
 It's impossible to cheer him up. He is constantly "too tired".
It's impossible to cheer him up. He is constantly "too tired". - Sleep problems. Any: insomnia, nightmares, the need to sleep for days on end. nine0028
- Cognitive impairment. Memory impairment, inability to concentrate.
Physical withdrawal symptoms:
- Dizziness, headache.
- Chest tightness, labored breathing.
- Heart rhythm disturbances, fast or irregular heartbeat.
- Nausea, vomiting, diarrhea, abdominal pain.
- Muscle tension. Including convulsions, tremor (trembling) of the limbs, muscle pain, as with the flu. nine0028
- Sweating, numbness and tingling of the skin of the hands and feet.
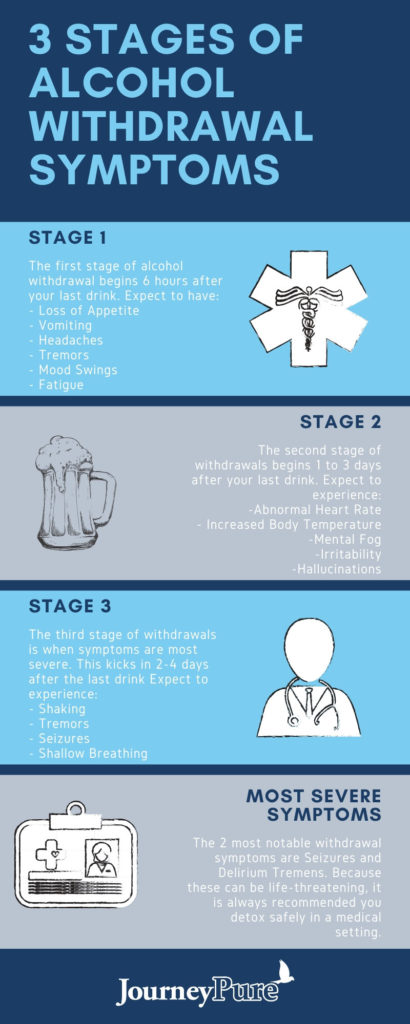
What is the danger of withdrawal syndrome
Sometimes - nothing but a few days (sometimes weeks) of physical malaise and psychological discomfort. For example, this is how quitting antidepressants or smoking manifests itself. But in some cases, withdrawal can be so powerful that it poses a real threat to life.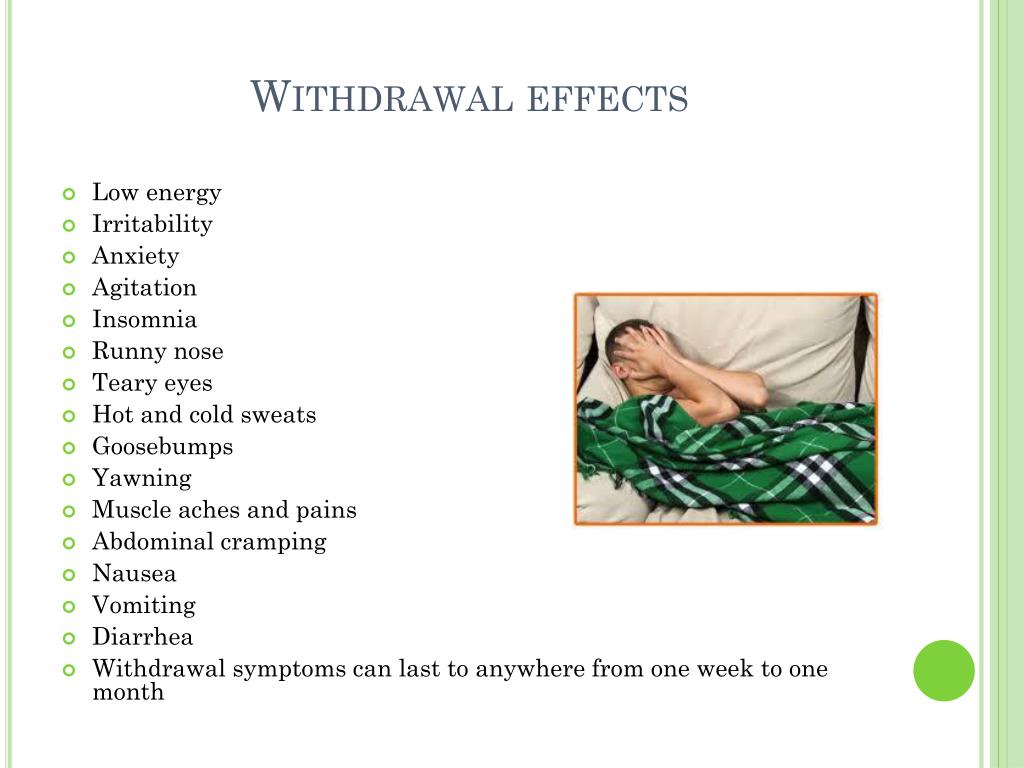
The most dangerous physical symptoms appear with a sharp withdrawal from alcohol and tranquilizers, which were previously taken regularly and in large doses. It can lead to seizures, stroke or heart attack, and in the case of alcohol - even to the development of meth-alcohol psychosis, better known as delirium tremens. nine0003
How to overcome the withdrawal syndrome
Considering the possible consequences, withdrawal from an addictive drug, as well as the “quit I smoke” gestures, should be coordinated with your doctor or at least with a therapist. The doctor will tell you how to go through the withdrawal period with minimal discomfort.
If you don't have serious health problems, just a comfortable environment will most likely help:
- a quiet, peaceful bedroom where you can lie down while your body recovers; nine0028
- soft dimmed lighting;
- limited human contact;
- support from loved ones;
- healthy food and plenty of fluids.
But at the same time, it is necessary to carefully monitor your well-being. If during the withdrawal period blood pressure rises, tachycardia (accelerated, uneven heartbeat) is observed, body temperature rises and, moreover, convulsions and hallucinations appear, call an ambulance. You may need hospital treatment. nine0003
Read also 🧐
- The story of how running helped overcome drug addiction
- How dopamine addiction to technology is formed
- 10 signs that you are addicted
Optimization of antipsychotic therapy switching tactics on the quetiapine model | Tsukarzi E.E.
Optimization of tactics for switching antipsychotic therapy on the quetiapine model
May 12, 2009
Share material print Add to favorites nine0026 For citation: Tsukarzi E.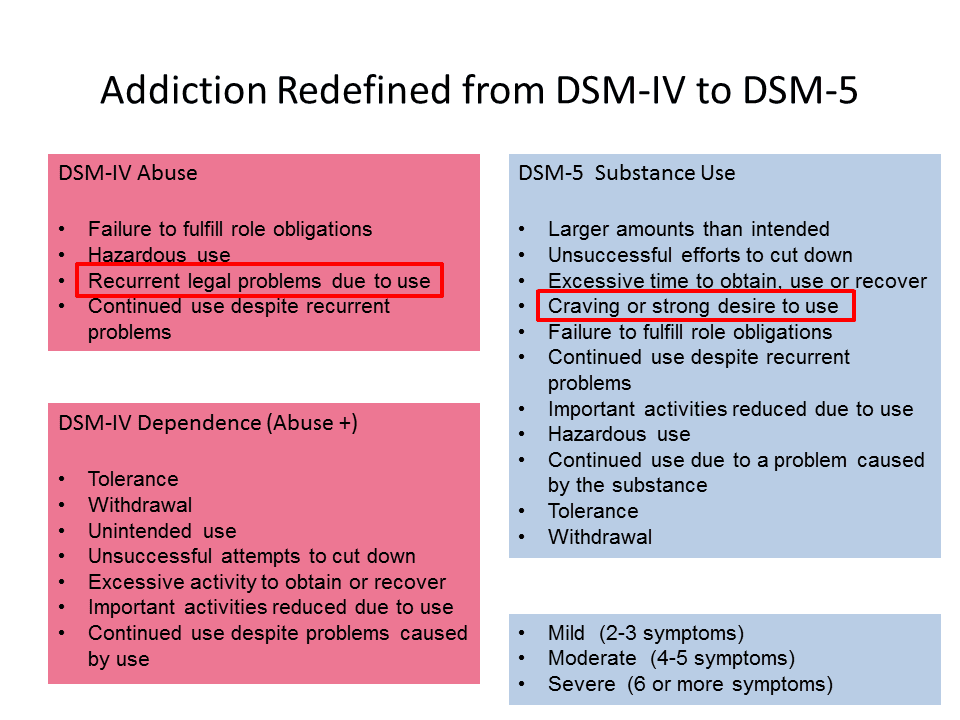 E. Optimization of tactics for changing antipsychotic therapy on the quetiapine model. breast cancer. 2009;11:810.
E. Optimization of tactics for changing antipsychotic therapy on the quetiapine model. breast cancer. 2009;11:810.
Data from observational studies show that changing therapy, unfortunately, is a routine practice, in particular, the replacement of one atypical antipsychotic with another, on average, occurs twice a year [Mahmoud R.A., Engelgart L.M., 2004]. This fact is due to clinical realities and is forced after the development of clinical deterioration or intolerable side effects. It is no coincidence that in modern clinical studies on the use of antipsychotics in long-term therapy, one of the main criteria for effectiveness is the dropout rate, expressed in the duration of treatment and the number of patients remaining on therapy. Of course, the attending physician also bears part of the blame for the frequent change of therapy: we often do not know how to wait and are in too much of a hurry. In this regard, it is important to comply with standards in evaluating the effectiveness of antipsychotic therapy courses. Undoubtedly, the reasons that prompt a doctor to change treatment in each specific case are the object of a special analysis (Table 1). nine0003
Undoubtedly, the reasons that prompt a doctor to change treatment in each specific case are the object of a special analysis (Table 1). nine0003
As we can see, in both cases, the first reason for changing therapy is the lack of effectiveness. It is seen on a continuum of therapeutic response from partial effect to absolute refractoriness. However, there are significant differences between the two classes of antipsychotics in indications for changing therapy. For conversion from typical drugs, the clinical targets are: negative symptoms (predominantly anhedonia and hypobulia), depression, EPS and tardive dyskinesia, and low compliance. While reducing the burden of side effects is an important reason to replace one atypical with another. Primarily these side effects are weight gain and hyperprolactinemia, as well as sedation and sexual dysfunction. It should be noted that the possibility of improving cognitive functions also serves as a motive for prescribing a new second-generation antipsychotic.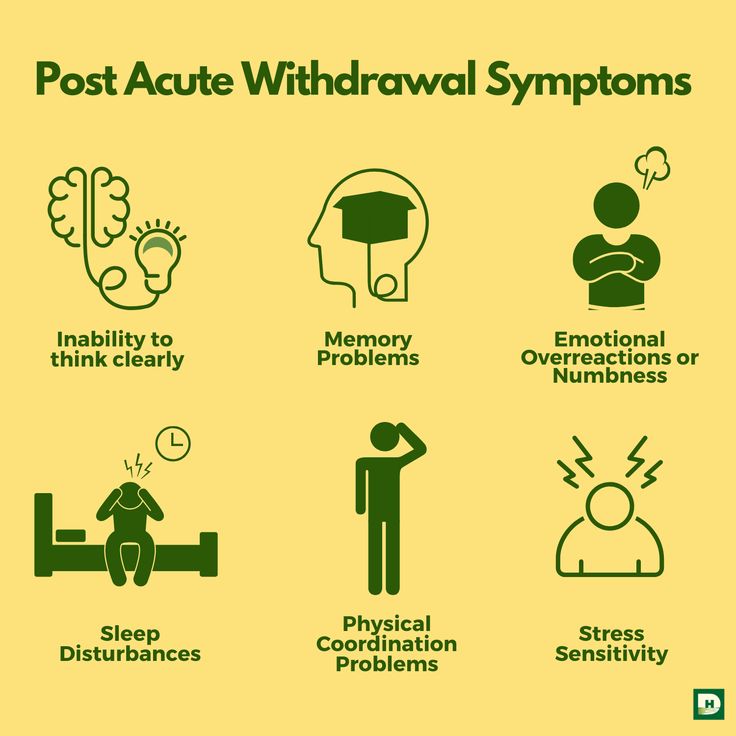 nine0128 However, clinical realities constantly show us that the hopes placed on a new drug often do not have time to be realized. This is largely due to the fact that the transfer process is quite painful for the patient, and sometimes even the transfer itself cannot be completed at all. The reason for this is both the mental state of the patient and the various side effects that develop in this period. On the one hand, the somatic trouble that appears on the shift is associated by the doctor with the new drug and discredits it already in the first days of treatment. On the other hand, sometimes “unusual” somatic complaints presented by the patient, which do not fit into the spectra of side effects of the old and new antipsychotics, are regarded by the doctor as subjective signs of the patient not accepting the new medication. And, as a result, we evaluate that “the drug did not work” and quickly return to the old one or prescribe another, third antipsychotic in a short period of time.
nine0128 However, clinical realities constantly show us that the hopes placed on a new drug often do not have time to be realized. This is largely due to the fact that the transfer process is quite painful for the patient, and sometimes even the transfer itself cannot be completed at all. The reason for this is both the mental state of the patient and the various side effects that develop in this period. On the one hand, the somatic trouble that appears on the shift is associated by the doctor with the new drug and discredits it already in the first days of treatment. On the other hand, sometimes “unusual” somatic complaints presented by the patient, which do not fit into the spectra of side effects of the old and new antipsychotics, are regarded by the doctor as subjective signs of the patient not accepting the new medication. And, as a result, we evaluate that “the drug did not work” and quickly return to the old one or prescribe another, third antipsychotic in a short period of time. In this regard, it is necessary to pay attention to the problem of the effects of neuroleptic withdrawal, which has been widely voiced in recent years. Traditionally, withdrawal syndrome in psychopharmacotherapy has been described in relation to tranquilizers and antidepressants. At the same time, turning to this topic, we see a convincing and reasoned attribution of a variety of symptoms when changing / canceling an antipsychotic to withdrawal phenomena. What is it? Under the symptoms of "cancellation" of neuroleptics, predominantly non-specific somatic symptoms are described: nausea, vomiting, diarrhea, increased sweating, sensation of heat / cold, myalgia and paresthesia. In addition, it is also some psychic phenomena. Their maximum severity manifests itself within 1–4 days, followed by resolution in 7–14 days, in some cases up to 3–4 weeks. Withdrawal symptoms are more pronounced with a sharp break in therapy, transfer from low-potency (sedative) AP and simultaneous discontinuation of correctors.
In this regard, it is necessary to pay attention to the problem of the effects of neuroleptic withdrawal, which has been widely voiced in recent years. Traditionally, withdrawal syndrome in psychopharmacotherapy has been described in relation to tranquilizers and antidepressants. At the same time, turning to this topic, we see a convincing and reasoned attribution of a variety of symptoms when changing / canceling an antipsychotic to withdrawal phenomena. What is it? Under the symptoms of "cancellation" of neuroleptics, predominantly non-specific somatic symptoms are described: nausea, vomiting, diarrhea, increased sweating, sensation of heat / cold, myalgia and paresthesia. In addition, it is also some psychic phenomena. Their maximum severity manifests itself within 1–4 days, followed by resolution in 7–14 days, in some cases up to 3–4 weeks. Withdrawal symptoms are more pronounced with a sharp break in therapy, transfer from low-potency (sedative) AP and simultaneous discontinuation of correctors.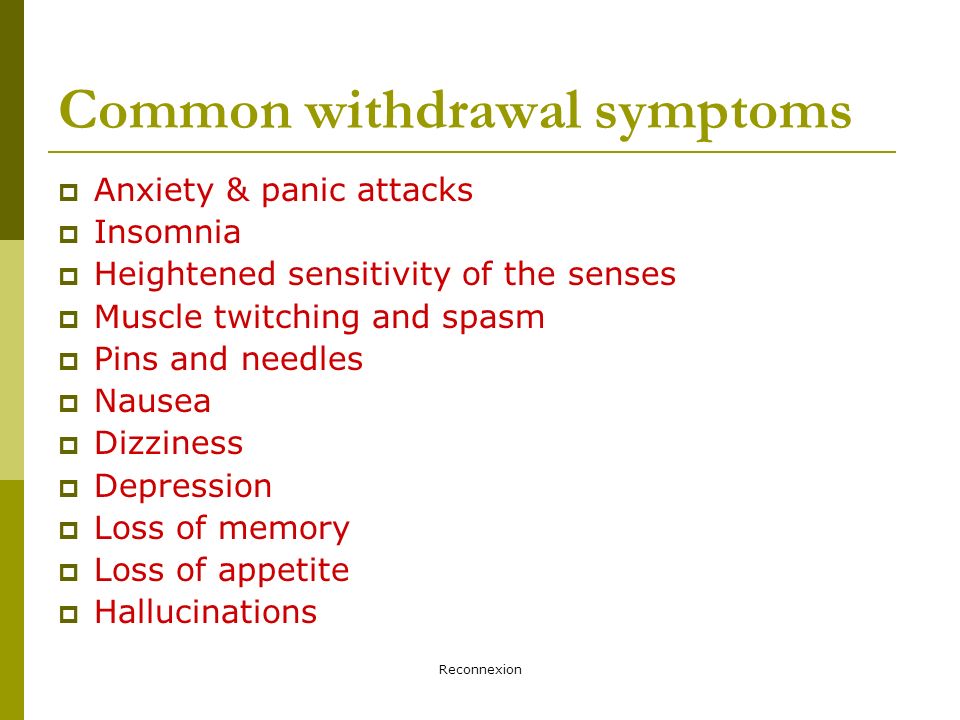 The mechanisms of withdrawal symptoms are based on the development of pharmacodynamic stress against the background of adaptation and hypersensitivity of mediator systems, mainly DA- and HL-ergic ones. Also, a certain effect is associated with the cessation of antiemetic and sedative effects. The connection between the termination of the blockade of individual mediator systems and the development of certain clinical phenomena made it possible to systematize the effects of antipsychotic withdrawal and come to an understanding of the mechanisms of their development (Fig. 1). nine0128 Cholinergic (CL) effects of withdrawal develop when transferred from a drug with high activity against muscarinic receptors. As is known, the leading therapeutic mechanism of the technique of simultaneous withdrawal of therapy, which was widely used earlier, is anticholinergic effects. In this case, we are talking about withdrawal symptoms as an undesirable phenomenon. Clinical manifestations are quite varied.
The mechanisms of withdrawal symptoms are based on the development of pharmacodynamic stress against the background of adaptation and hypersensitivity of mediator systems, mainly DA- and HL-ergic ones. Also, a certain effect is associated with the cessation of antiemetic and sedative effects. The connection between the termination of the blockade of individual mediator systems and the development of certain clinical phenomena made it possible to systematize the effects of antipsychotic withdrawal and come to an understanding of the mechanisms of their development (Fig. 1). nine0128 Cholinergic (CL) effects of withdrawal develop when transferred from a drug with high activity against muscarinic receptors. As is known, the leading therapeutic mechanism of the technique of simultaneous withdrawal of therapy, which was widely used earlier, is anticholinergic effects. In this case, we are talking about withdrawal symptoms as an undesirable phenomenon. Clinical manifestations are quite varied.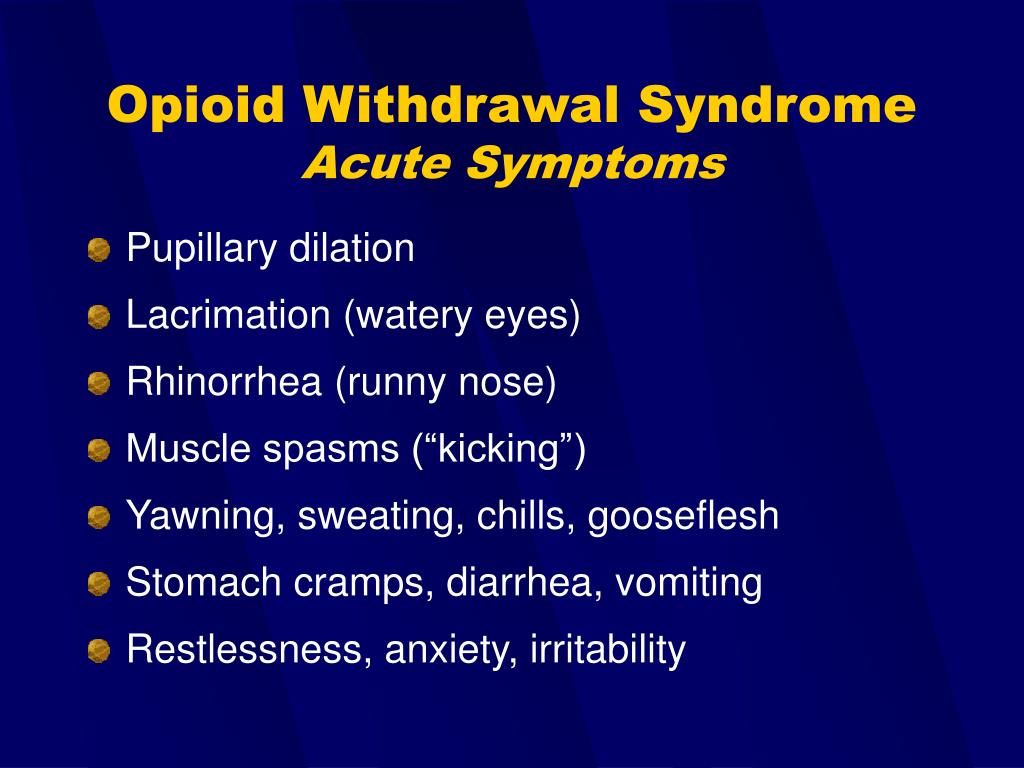 First of all, this is the so-called flu-like syndrome, gastrointestinal symptoms (nausea, vomiting, diarrhea), as well as insomnia, anxiety, anxiety, agitation, confusion and EPS. Most often, CL effects are described when anticholinergic therapy is discontinued (in 50–90% of cases), as well as sedative antipsychotics and some atypical antipsychotics (clozapine and olanzapine). They appear faster in drugs with a short half-life. It is based on the same phenomenon of hypersensitivity, in this case - cholinergic. The therapeutic tactic to prevent the development of withdrawal symptoms is to titrate from low doses with a gradual decrease in the dose of the previous drug ("Start low and go slow"). With the development of symptoms, a “step back” in the process of transferring to the previous dose of the drug being withdrawn and its slower withdrawal, if necessary, the appointment of correctors and benzodiazepines. nine0128 Psychoses (phenomena)
First of all, this is the so-called flu-like syndrome, gastrointestinal symptoms (nausea, vomiting, diarrhea), as well as insomnia, anxiety, anxiety, agitation, confusion and EPS. Most often, CL effects are described when anticholinergic therapy is discontinued (in 50–90% of cases), as well as sedative antipsychotics and some atypical antipsychotics (clozapine and olanzapine). They appear faster in drugs with a short half-life. It is based on the same phenomenon of hypersensitivity, in this case - cholinergic. The therapeutic tactic to prevent the development of withdrawal symptoms is to titrate from low doses with a gradual decrease in the dose of the previous drug ("Start low and go slow"). With the development of symptoms, a “step back” in the process of transferring to the previous dose of the drug being withdrawn and its slower withdrawal, if necessary, the appointment of correctors and benzodiazepines. nine0128 Psychoses (phenomena)
"hypersensitivity"
Clinically, psychoses of hypersensitivity are manifested by an exacerbation or worsening of the symptoms of psychosis when prescribing or changing an antipsychotic.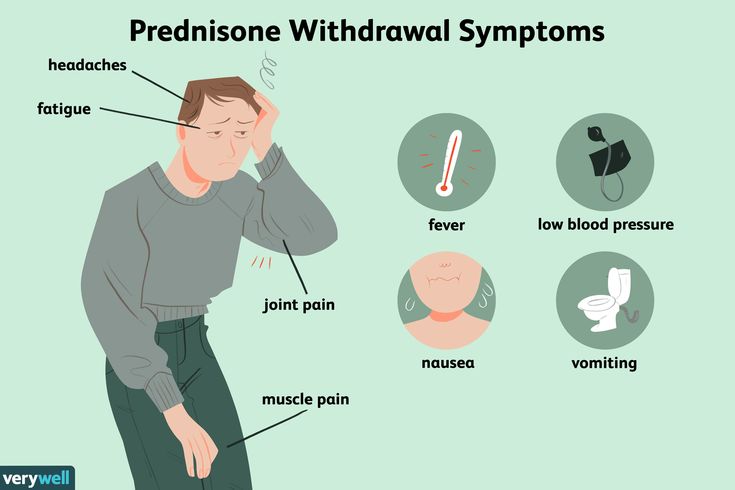 The first clinical descriptions date back to the beginning of the 60s of the last century, when at the beginning of antipsychotic therapy at the stage of dose titration in some patients, mainly with organically defective soil and the elderly, there was a sharp increase in psychosis. At the same time, in the future, with an increase in the dose, the condition, as a rule, quickly stabilized. This phenomenon is based on an artifactual increase in dopamine transmission due to hypersensitivity of postsynaptic D2 receptors and an increase in their density. In recent years, this clinical phenomenon has also been recorded when switching from a conventional antipsychotic (D2 receptor antagonist) to partial dopamine agonists. In this case, the mechanism of the hypersensitivity phenomenon is somewhat different: a high affinity for this type of receptor and a slightly different activity profile determine the involvement of new, previously unused receptors and a partial increase in synaptic transmission at the beginning of therapy.
The first clinical descriptions date back to the beginning of the 60s of the last century, when at the beginning of antipsychotic therapy at the stage of dose titration in some patients, mainly with organically defective soil and the elderly, there was a sharp increase in psychosis. At the same time, in the future, with an increase in the dose, the condition, as a rule, quickly stabilized. This phenomenon is based on an artifactual increase in dopamine transmission due to hypersensitivity of postsynaptic D2 receptors and an increase in their density. In recent years, this clinical phenomenon has also been recorded when switching from a conventional antipsychotic (D2 receptor antagonist) to partial dopamine agonists. In this case, the mechanism of the hypersensitivity phenomenon is somewhat different: a high affinity for this type of receptor and a slightly different activity profile determine the involvement of new, previously unused receptors and a partial increase in synaptic transmission at the beginning of therapy.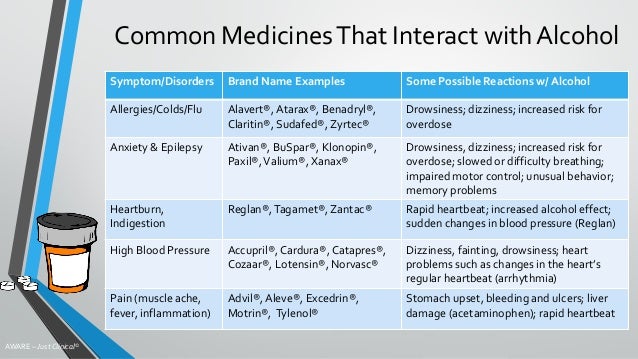 nine0128 Of course, not every increase in psychotic symptoms after switching to a new drug is a hypersensitivity phenomenon. Clear differentiation with exacerbation of psychosis is certainly necessary. One of the hallmarks may be the fact that the risk of exacerbation in stable patients is low in the first 2–3 weeks after withdrawal/transfer and increases in subsequent months. According to numerous observational studies, risk factors for exacerbation include: male gender, young age, the presence of organic soil, addictions. There is also a higher risk of exacerbation in inpatients and recently stabilized patients, with a sharp interruption of therapy, previous therapy with high doses of AP and clozapine. nine0128 Therapeutic tactics for hypersensitivity psychoses is to increase antipsychotic therapy with a rapid dose increase. While when transferring from a D2 antagonist to a partial agonist, the tactics should be fundamentally different, with a slower change in antipsychotic.
nine0128 Of course, not every increase in psychotic symptoms after switching to a new drug is a hypersensitivity phenomenon. Clear differentiation with exacerbation of psychosis is certainly necessary. One of the hallmarks may be the fact that the risk of exacerbation in stable patients is low in the first 2–3 weeks after withdrawal/transfer and increases in subsequent months. According to numerous observational studies, risk factors for exacerbation include: male gender, young age, the presence of organic soil, addictions. There is also a higher risk of exacerbation in inpatients and recently stabilized patients, with a sharp interruption of therapy, previous therapy with high doses of AP and clozapine. nine0128 Therapeutic tactics for hypersensitivity psychoses is to increase antipsychotic therapy with a rapid dose increase. While when transferring from a D2 antagonist to a partial agonist, the tactics should be fundamentally different, with a slower change in antipsychotic.
"Early activation" of patient
when changing antipsychotic
“Early activation” (RA) is a definition quite often used recently in the literature. It should be noted, along with the "unfamiliarity" of the term for psychiatrists, also the lack of a clear clinical definition. In general, RA is understood as the development in a patient at the beginning of a new antipsychotic therapy of excess energy, increased activity, and insomnia. Traditionally, this symptomatology was considered as a stimulating effect of a new drug, which is rightly perceived as an undesirable phenomenon in psychotic patients or as signs of worsening psychosis. However, the clinical phenomenon of RA is associated with the withdrawal of the previous antipsychotic and is considered solely as a withdrawal effect. It is associated with the cessation of the blockade of type 1 histamine receptors (h2) and develops with the abrupt withdrawal of drugs whose pharmacological profile is characterized by high activity for this type of receptor. These drugs include most sedative (low-potency) antipsychotics (chlorpromazine, levomepromazine, etc.), as well as olanzapine and clozapine.
It should be noted, along with the "unfamiliarity" of the term for psychiatrists, also the lack of a clear clinical definition. In general, RA is understood as the development in a patient at the beginning of a new antipsychotic therapy of excess energy, increased activity, and insomnia. Traditionally, this symptomatology was considered as a stimulating effect of a new drug, which is rightly perceived as an undesirable phenomenon in psychotic patients or as signs of worsening psychosis. However, the clinical phenomenon of RA is associated with the withdrawal of the previous antipsychotic and is considered solely as a withdrawal effect. It is associated with the cessation of the blockade of type 1 histamine receptors (h2) and develops with the abrupt withdrawal of drugs whose pharmacological profile is characterized by high activity for this type of receptor. These drugs include most sedative (low-potency) antipsychotics (chlorpromazine, levomepromazine, etc.), as well as olanzapine and clozapine.