Vulnerability emotions bpd
Emotion Vulnerability and Self-Invalidation | DBT
Emotion Vulnerability and Self-Invalidation
Uncategorized
In previous blogs, I’ve touched on some of the secondary targets or “dialectical dilemmas” in DBT. Today, I’ll talk about the last one: Emotion vulnerability versus self-invalidation. Emotion vulnerability is considered a core characteristic of people with borderline personality disorder (BPD) and has three different aspects: Emotional sensitivity, reactivity, and slow return to baseline. People with BPD often have a low threshold for emotional responses, meaning that it doesn’t take much to bring on an emotional response. Just a look on someone’s face, someone’s voicetone, a sad commercial, a seemingly minor slight or frustration, can elicit an emotional response, whereas other people might seem oblivious to these triggers. This is what we call
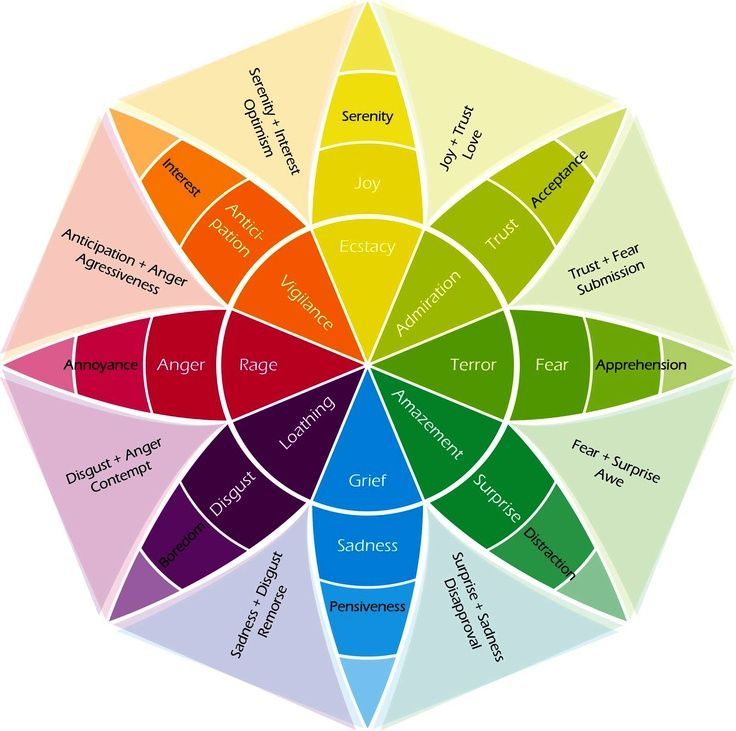
emotional sensitivity. Another aspect of emotion vulnerability is emotional reactivity, or the tendency to experience very strong emotional responses. Some of the research suggests that people with BPD tend to have strong emotional responses, particularly when the emotional triggers are interpersonal or related to social rejection. We all have some degree of emotional reactivity in various situations and with various emotions. Some of us feel anger particularly strongly, whereas others struggle with intense experiences of anxiety, fear, sadness, or shame. Some people are seemingly impervious to criticism, whereas others feel swallowed up by shame, embarrassment, or anger when someone provides negative feedback. For people with BPD, having such strong emotions places great demand on coping resources. It’s harder and sometimes takes a lot more effort and skill to manage very intense emotions, compared with mild emotions. Intense emotions interfere with our ability to think, plan, problem solve, consider others’ perspectives.
 Further, it can be hard to control our behaviour when we experience very strong emotions. Studies have shown that, when emotions are intense, our main priority is to escape them, even through behaviours that might cause us problems (e.g., overeating fattening snacks) (Tice et al., 2001).
Further, it can be hard to control our behaviour when we experience very strong emotions. Studies have shown that, when emotions are intense, our main priority is to escape them, even through behaviours that might cause us problems (e.g., overeating fattening snacks) (Tice et al., 2001).
The third part of emotion vulnerability is slow return to emotional baseline. People with BPD often have difficulty getting back to what we call physiological baseline arousal – basically, a “resting” emotional state. Baseline might be how you feel when nothing particularly emotional is happening, you’re going for a walk down the block, sitting quietly reading a book, and so on. For people with BPD, it can be very hard to get back to baseline, and some of the research suggests biological reasons for this. Some of these biological reasons include a particularly strong physiological stress response system, differences in the parasympathetic and sympathetic nervous system, and brain differences in areas having to do with emotions and self-regulation.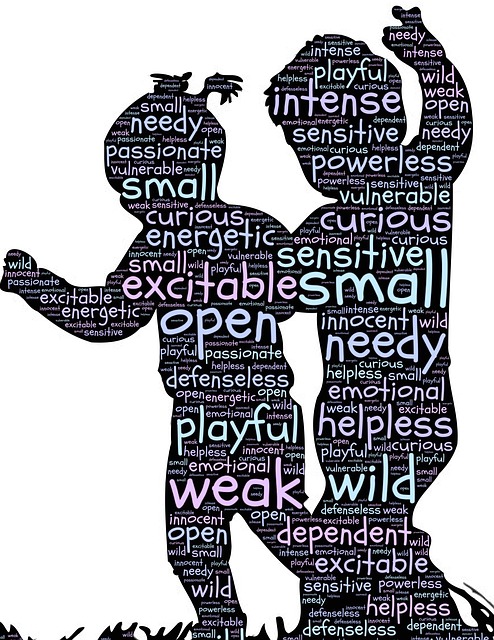 Some people with BPD also may tend to ruminate about emotional events, which amplifies emotions and makes it hard to get back to baseline. Often, people with BPD haven’t learned the skills (e.g., emotion regulation, self-soothing) to get themselves back to baseline. In either case, a slow return to baseline can make you chronically vulnerable to emotional situations. Let’s say you had a conflict with a coworker, your anger and frustration were at 80/100, and you could only get down to 60 or 70 by the time you got home, noticed the house is a mess and there’s no food in the fridge. Your emotions were already high from the incident at work, so you’re probably going to go up to 80 or 90. Then, your partner comes home and wonders why you’re so irritable about seemingly small things (the messy house and bare fridge). In reality, you’re not overreacting to the stuff around the house; you were just unable to get back to baseline after the incident at work. To be continued… Stay tuned for more on emotion vulnerability and self-invalidation next time.
Some people with BPD also may tend to ruminate about emotional events, which amplifies emotions and makes it hard to get back to baseline. Often, people with BPD haven’t learned the skills (e.g., emotion regulation, self-soothing) to get themselves back to baseline. In either case, a slow return to baseline can make you chronically vulnerable to emotional situations. Let’s say you had a conflict with a coworker, your anger and frustration were at 80/100, and you could only get down to 60 or 70 by the time you got home, noticed the house is a mess and there’s no food in the fridge. Your emotions were already high from the incident at work, so you’re probably going to go up to 80 or 90. Then, your partner comes home and wonders why you’re so irritable about seemingly small things (the messy house and bare fridge). In reality, you’re not overreacting to the stuff around the house; you were just unable to get back to baseline after the incident at work. To be continued… Stay tuned for more on emotion vulnerability and self-invalidation next time. ~ Alexander L. Chapman, Ph.D., R.Psych
~ Alexander L. Chapman, Ph.D., R.Psych
The Emotional Vulnerability of Borderline Personality Disorder
Medically reviewed by Scientific Advisory Board — By Margarita Tartakovsky, MS on May 17, 2016
Imagine you have a cut. The skin around your cut heals. But it heals all wrong. The scarred tissue is extra sensitive. So much so that every time you simply touch the area, it’s like the wound tears open again, and again, and again; and the pain peaks every single time. Now imagine this wound represents your emotional sensitivity and how you deal with the world every day. This is akin to the emotional susceptibility of borderline personality disorder (BPD).
As Shari Y. Manning, Ph.D, writes in her excellent book Loving Someone with Borderline Personality Disorder, “People with BPD have an exquisite vulnerability to emotions.” And this susceptibility is hardwired.
For instance, Manning cites one interesting study where researchers tickled infants on their noses with a feather. Their responses ranged widely: Some infants didn’t react at all, others moved around and still others started crying and it was tough to calm them down. These babies were seen as “sensitive to emotional stimuli.”
Their responses ranged widely: Some infants didn’t react at all, others moved around and still others started crying and it was tough to calm them down. These babies were seen as “sensitive to emotional stimuli.”
Like other disorders, BPD also involves an environmental component. (Not everyone who’s emotionally sensitive goes on to have BPD.) Individuals with BPD aren’t just genetically vulnerable to emotions; they’ve also grown up in an “invalidating environment.” So they might’ve never learned how to regulate their emotions, or their emotions were continuously ignored or dismissed.
What It Means To Be “Emotional”
According to Manning, being emotional isn’t a lack of control; it has more to do with “three separate tendencies that cause emotional arousal in different ways.” These are:
- “Emotional Sensitivity.” Loved ones aren’t the only ones confused when someone with BPD has an emotional reaction seemingly out of nowhere. People with BPD may be unaware of the trigger, too.
 But they still have a strong reaction. “Emotional sensitivity wires people to react to cues and to react to their reactions.” Manning explains that: “To understand emotional sensitivity, think of the person with BPD as being ‘raw.’ His emotional nerve endings are exposed, and so he is acutely affected by anything emotional.”
But they still have a strong reaction. “Emotional sensitivity wires people to react to cues and to react to their reactions.” Manning explains that: “To understand emotional sensitivity, think of the person with BPD as being ‘raw.’ His emotional nerve endings are exposed, and so he is acutely affected by anything emotional.” - “Emotional Reactivity.” A person with BPD not only reacts with extreme emotion (“what would be sadness in most becomes overwhelming despair. What would be anger becomes rage”), but their behavior also is intense and doesn’t fit the situation. They might sleep for days, scream in public or self-harm. Manning points out that emotional reactivity isn’t self-indulgent or manipulative, which is an unfortunate myth attached to BPD. Instead, research has suggested that people with BPD have a higher emotional baseline. If most people’s emotional baseline is 20 on a 0 to 100 scale, then people with BPD are continuously at 80. What can intensify their reactions are the secondary emotions of shame and guilt because they know “their emotions are out of control,” Manning writes.
 Let’s say your loved one is angry. “On top of the original anger, these secondary emotions feel intolerable, and their fear of all this emotion, ironically, tends to fire off another series of emotions—perhaps anger that is now shifted to you, for ‘not helping’ your loved one or for some unexpressed reason.”
Let’s say your loved one is angry. “On top of the original anger, these secondary emotions feel intolerable, and their fear of all this emotion, ironically, tends to fire off another series of emotions—perhaps anger that is now shifted to you, for ‘not helping’ your loved one or for some unexpressed reason.” - “Slow Return to Baseline.” People with BPD also have a hard time calming down and stay upset longer than others without the disorder. And there’s interesting evidence to back this up. “In a person with average emotional intensity, an emotion fires in the brain for around 12 seconds. There is evidence that in people with BPD emotions fire for 20 percent longer.”
An Exercise in Understanding
In Loving Someone with Borderline Personality Disorder, Manning also helps readers better understand what it’s like to be emotionally vulnerable. She suggests thinking about an extended period of time when you were very emotional.
For Manning her emotional explosion happened when the company she’d worked for was going bankrupt.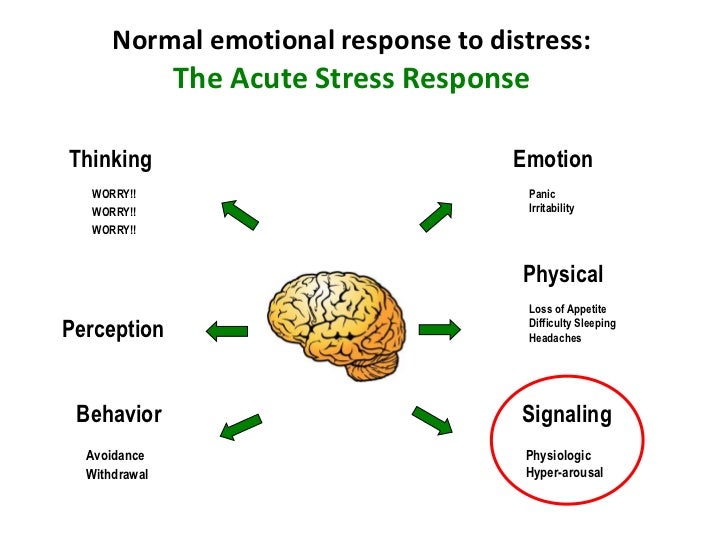 Not only was everyone upset and Manning barely sleeping but then her friend passed away. “At that point I felt like every emotion that I had was at the surface of my skin. I physically felt like I would explode with emotion if one more thing happened.” She notes that she was “an emotional sponge.” She didn’t even want sympathy because she felt like this would put her over the edge.
Not only was everyone upset and Manning barely sleeping but then her friend passed away. “At that point I felt like every emotion that I had was at the surface of my skin. I physically felt like I would explode with emotion if one more thing happened.” She notes that she was “an emotional sponge.” She didn’t even want sympathy because she felt like this would put her over the edge.
When thinking about your own highly emotional experience, Manning writes:
…Remember what it felt like emotionally and physically. Remember how it felt like emotions were just building on each other. Remember the experience of no one understanding how bad the situation was and how emotional you were. Now tell yourself that this is the experience of your loved one every moment of every day.
How Loved Ones Can Help
Manning shared her insight on how family and friends can help in a two-part interview on Psych Central (Part 1 and Part 2). And loved ones can do a lot, especially when it comes to helping the person when they’re upset.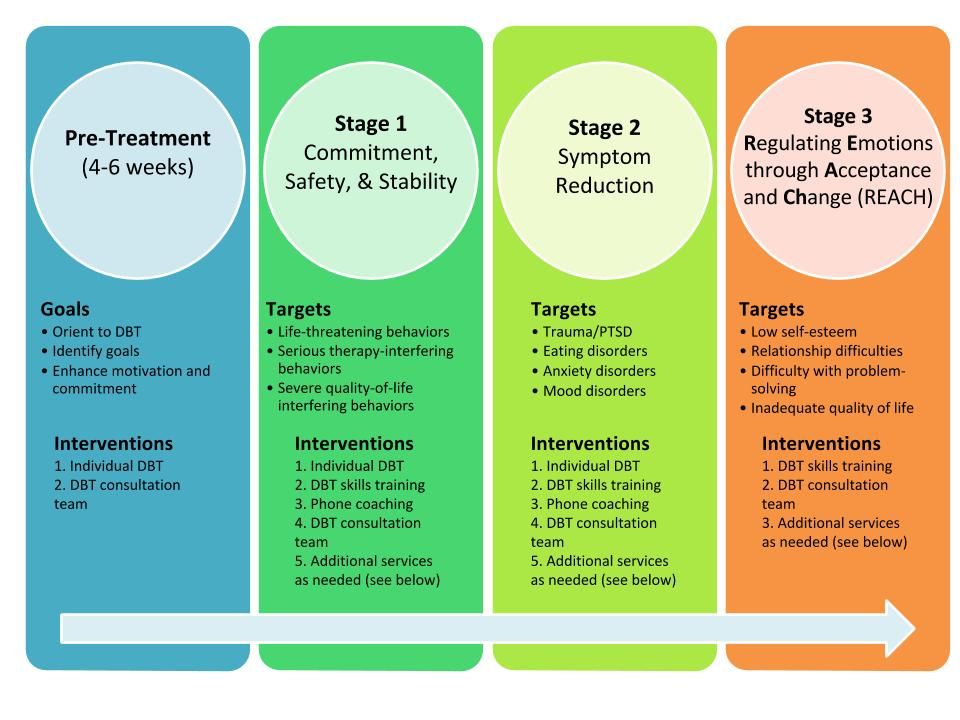
In her book, Manning provides readers with step-by-step strategies and detailed examples. Below is a brief list of suggestions from her book:
- Assess: ask what has happened.
- Listen actively; don’t contradict, judge, or say your loved one is overreacting.
- Validate: find something in what happened that makes sense and is understandable, that you can relate to; say what that is.
- Ask if you can help, not to solve the problem but to get through the moment.
- If your loved one says no, give him or her space and remember the emotions of emotionally vulnerable people last longer.
Also, it’s important to remember that people with BPD do get better and simply need to learn the skills of managing their emotions. While this requires hard work and effort, treatments such as dialectical behavior therapy (DBT) have been shown to be highly effective. You can learn more about DBT here and here.
The impact of biological vulnerability and a disabling environment on the development of borderline personality disorder.
 - Information portal
- Information portal Biological vulnerability and its consequences
Indeed, available data suggest that individuals who meet the criteria for BPD characterized by more frequent, intense and prolonged negative conditions (Stiglmayr et al., 2005), and that biological vulnerability can exacerbate difficulty in regulating emotions (e.g., Juengling et al., 2003; Ebner-Priemer et al., 2005). nine0007
Difficulties in regulating emotions mean difficulties in regulating most aspects of our lives: what we do, and who we are, depends mainly on the stability of mood and adequate emotional regulation. The same action can be perceived as easy or difficult, depending on our mood. For example, let's take the familiar situation of communicating with strangers at a party. If you have great mood, you chat with the most interesting people in the room; if you unsure of yourself and feel insecure, you are standing under the wall, barely looking at people. Or have you put off doing some terrible deed for a few months. And then when you were in a good mood - voila - got it done in half a day. nine0007
And then when you were in a good mood - voila - got it done in half a day. nine0007
Those of us who manage our emotions without significant effort, consider this ability natural. Time From time to time we have situations where our behavior depends on emotions, but in most of the time we get through.
Now imagine that because of your biological vulnerability, on the contrary, your emotions are striking in variety. You cannot predict what mood you will be in. If your behavior varies greatly depending on your mood, can you predict whether you will be a savage or a sociable person in informal communication with people? If you are able to take responsibility for your actions when emotionally focused enough, do you become unconscious and unskilled when emotions get the better of you? Have you been expelled from school or fired from your job? Can you say that your ability to perform any duties is not in your power, but depends on your emotional state? The impact of this unpredictable vulnerability affects all areas of life. As in a nightmare, your efforts are constantly in vain or turn into a disaster. This biological vulnerability is exacerbated, and in some cases even shaped by the interaction between an emotionally vulnerable individual and a persistently disabling social environment. nine0007
As in a nightmare, your efforts are constantly in vain or turn into a disaster. This biological vulnerability is exacerbated, and in some cases even shaped by the interaction between an emotionally vulnerable individual and a persistently disabling social environment. nine0007
Disabling environment and its influence
None of us gets enough flawless optimal environment. Even the best parents can get tired and be under stress. In their essence, they themselves are restless, angry or depressed. In such a depressed mood, they can to punish the expression of primary emotions or make them are minimized. As a result, we learn more or less dysfunctional ways of expressing and understanding our emotions. However, more serious problems arise when educators regularly and consecutively unable to respond to primary emotions and their expression according to our needs. Persistent disability occurs when most cases, educators or parents perceive our initial reactions as wrong, inappropriate, pathological, or not worth taking seriously. Primary reactions of interest are constantly suppressed or ridiculed; the natural need for comfort is regularly ignored or condemned; sincere intentions are questioned or misinterpreted. So Thus, a person learns to avoid, block and control his own natural inclinations and primary emotional reactions. Like a creature closed in a room with an electrically charged grid on the floor, he or she learns to avoid any step that leads to pain and disability. nine0007
Primary reactions of interest are constantly suppressed or ridiculed; the natural need for comfort is regularly ignored or condemned; sincere intentions are questioned or misinterpreted. So Thus, a person learns to avoid, block and control his own natural inclinations and primary emotional reactions. Like a creature closed in a room with an electrically charged grid on the floor, he or she learns to avoid any step that leads to pain and disability. nine0007
In permanent disability environment, the development of a conditioned reflex occurs in connection with the experience of feeling fear - we are not only trying to bypass the electric current of the disability grid, but we also avoid any experience of private events (thoughts, sensations or emotions), able to lead us to this grid. We become extremely sensitized to all external stimuli that can lead to a painful encounter with disability. We are phobically afraid of our own reasonable, natural reactions. Persistent disability not only makes people overly sensitive disabled by others, but also sensitive to their own reactions, justified or not, that can become a reason for disability with sides of others. The natural response to the effect produced can often compared to a spider falling on its knees to a person with arachnophobia. nine0007
The natural response to the effect produced can often compared to a spider falling on its knees to a person with arachnophobia. nine0007
For people with high biological vulnerability to emotional dysregulation even a "normal" level of disability may be enough to create serious problems. Like people with Attention Deficit Disorder, they face with huge but difficult to understand problems.
Child sexual abuse is a classic example of a disabling environment for BPD (Wagner & Linehan, 1997, 2006).
When the environment does not satisfy our needs, biological vulnerability, or persistent disability forces us to internalize a number of problematic emotional regulation strategies. avoidance can be very dexterous: we defend ourselves when we feel the slightest inattention in a friend to our story, with the help of the fact that we say not what we were going to say, but something less risky in terms of revealing information about yourself; unconsciously we we instantly avoid feeling sadness or shame that can hurt us, instead feeling irritated. nine0007
nine0007
Avoidance may be obvious flight with all our might: our emotional state is so disgusting that we unconsciously trying to avoid it or resorting to such desperate methods as deliberately inflicting bodily injury to avoid mental pain. Although such cognitive processes negatively affect all of us, people prone to emotional dysregulation, face more persistent social disability and go so far as to change strategies that over-regulate emotions and their expression, on a strategy, are not enough their regulators. nine0007
Biological vulnerability and persistent disability leads to strong, painful sensitivity. The lightest irritant capable of causing mental pain comparable to receiving a third-degree burn. Because the a person cannot control the occurrence and end of events that cause emotional reaction, he desperately needs anything that can relieve pain. For many feel it is as if their physical body is not able to resist forces rushing violently at him. Even the dysregulation of positive emotions can cause pain.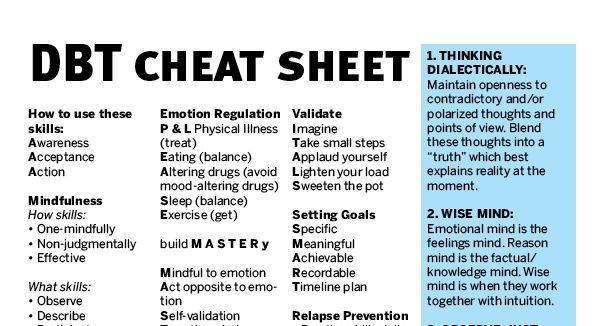 For example, the patient says: “I was so delighted when I saw my friends that he couldn't bear it. I laughed too loud, talked too a lot - everything I did was too much for them. "Emotional Vulnerability" refers to not only painful sensitivity, but also its further consequences in a person’s life, being painfully sensitive. The inevitable daily experiences cause severe mental pain, which eventually leads to the fact that the emotions themselves become traumatic: in this situation, a person cannot tell when emotions take over and harm him. nine0007
For example, the patient says: “I was so delighted when I saw my friends that he couldn't bear it. I laughed too loud, talked too a lot - everything I did was too much for them. "Emotional Vulnerability" refers to not only painful sensitivity, but also its further consequences in a person’s life, being painfully sensitive. The inevitable daily experiences cause severe mental pain, which eventually leads to the fact that the emotions themselves become traumatic: in this situation, a person cannot tell when emotions take over and harm him. nine0007
Behavior becomes completely unpredictable because it is tied to an emotional state that the person cannot control. This unpredictability leads to the disappointment of the expectations of both the patient and others, and in the end everyone feels disappointed. A person despairs because he considers his emotional sensitivity to be biologically integral, part of his character, therefore, something that will never change. The patient feels that he is trapped in a nightmare of discontrol.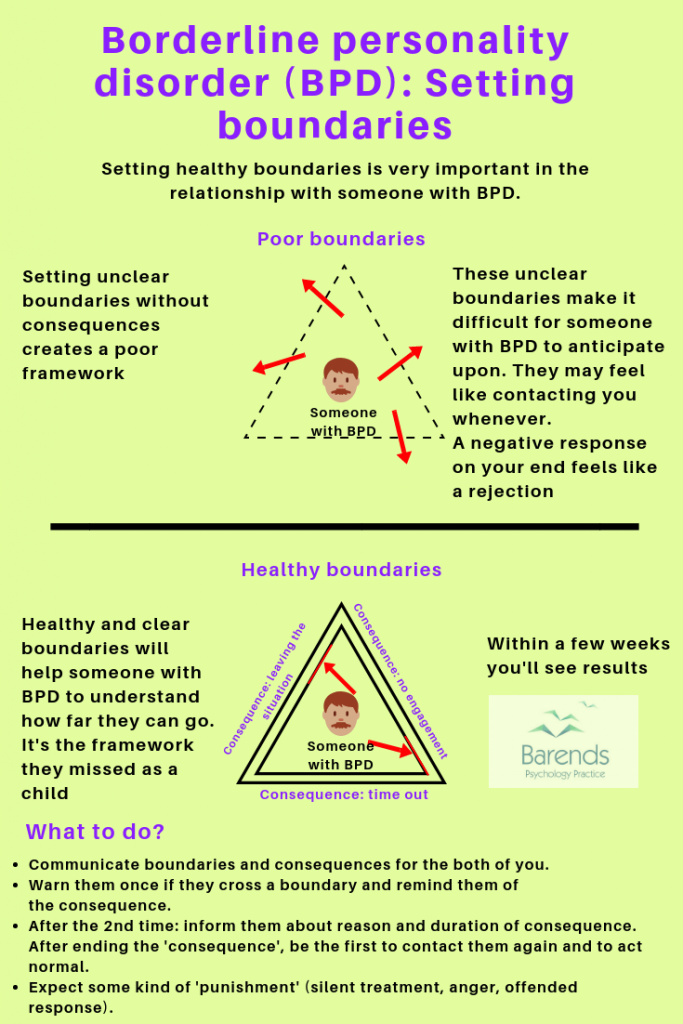 Life has become a constant battle to survive the normal events of the day. In such a situation, suicide may seem like the only way to avoid further excruciating suffering. Suicide can also be other people's last response to their unresponsiveness. nine0007
Life has become a constant battle to survive the normal events of the day. In such a situation, suicide may seem like the only way to avoid further excruciating suffering. Suicide can also be other people's last response to their unresponsiveness. nine0007
Source: Kelly Koerner, Dialectical Behavioral Therapy: A Practical Guide. 2012.
pain, disabling environment, criticism, mood, borderline personality disorder, suicide, vulnerability, emotional dysregulation
On the edge: living with borderline personality disorder
Medical issues
Text: Masha Pushkina,
Ekaterina Tarasova nine0007
Illustrations: Alena Belyakova
October 31, 2017
Borderline personality disorder affects 3% of people on Earth. It would seem that 3% is not much at all, but we are talking about several hundred million people, and this is twice as much as the entire population of Russia. What is BPD and where does it come from, how can a “border guard” live with himself and what should his relatives do, can he be cured and how can he help himself on his own - all this is in our new large material on disorders. Anna Ushkalova, a psychiatrist at the International Medical Center, assisted us in researching the issue. Special thanks to Katya Novikova for collecting comments from people with BPD. nine0064
It would seem that 3% is not much at all, but we are talking about several hundred million people, and this is twice as much as the entire population of Russia. What is BPD and where does it come from, how can a “border guard” live with himself and what should his relatives do, can he be cured and how can he help himself on his own - all this is in our new large material on disorders. Anna Ushkalova, a psychiatrist at the International Medical Center, assisted us in researching the issue. Special thanks to Katya Novikova for collecting comments from people with BPD. nine0064
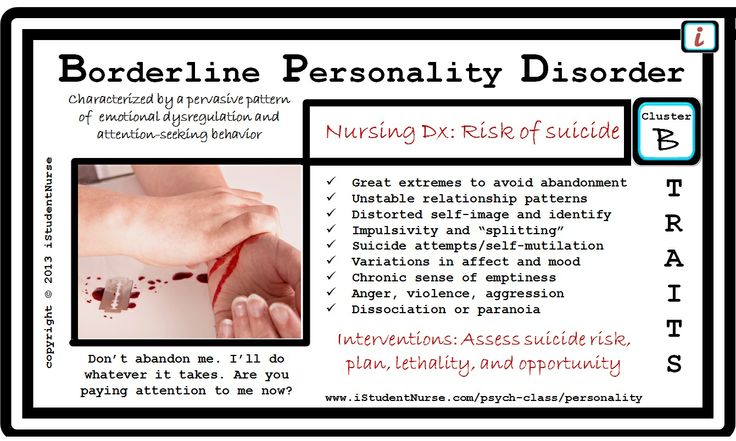
Borderline personality disorder ( BPD, Borderline personality disorder ) is a psychiatric disease characteristic of people who are characterized by instability in interpersonal relationships, self-image, emotional instability, impulsivity. These symptoms occur at a young age, appear regularly in many life situations and lead to maladjustment in society.
Unfortunately, in our country little attention is paid to the problems of people with BPD.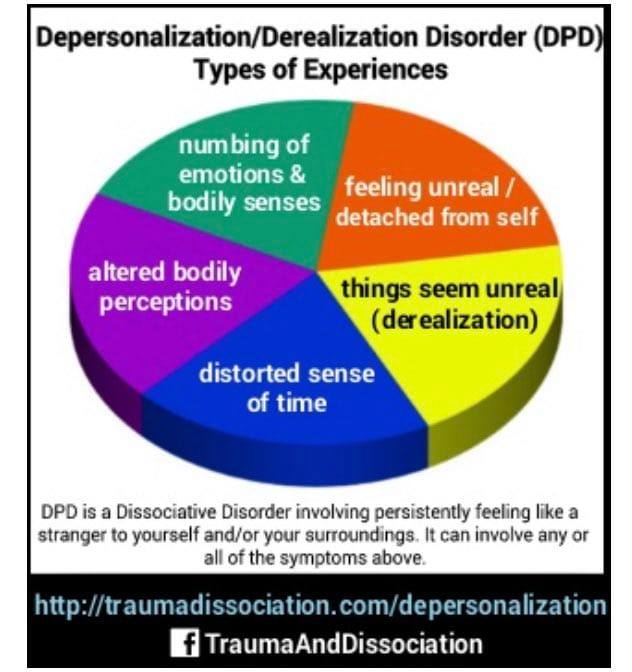 Incorrect diagnosis often complicates the treatment process itself. nine0007
Incorrect diagnosis often complicates the treatment process itself. nine0007
“People with BPD often get the wrong medication, which only makes them worse. But in most cases, “border guards” are unaware of their diagnosis and, accordingly, do not know that their condition can be corrected.
In Russia, acquaintance with the methods of psychotherapy of borderline disorder common in the West is just beginning, there are only a few experienced specialists. But the first psychotherapeutic communities are already opening up where people with BPD can get help, ”says the Resource Center, an information portal for people suffering from borderline disorder. nine0007
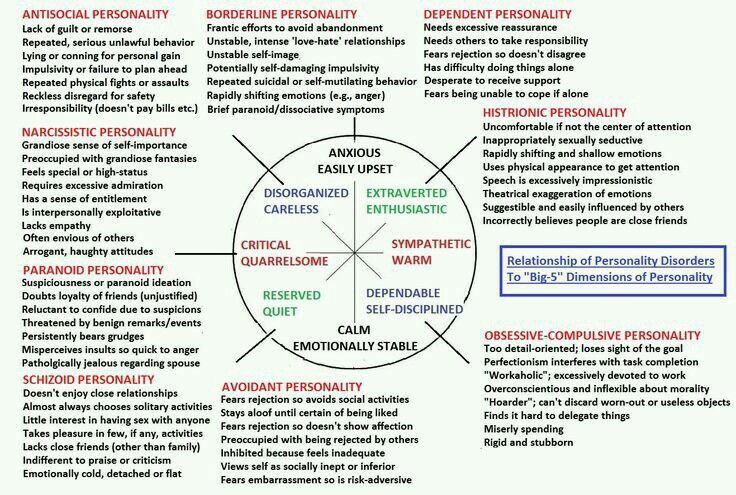
Psychiatry classifies BPD as a personality disorder, a group of diseases that includes various pathologies of character, from dissociative disorders to narcissistic disorders.
Despite the similarity of the name, "borderline personality disorder" has nothing to do with "borderline". Psychologists call the borderline state the degree of severity of character traits on the verge of norm and pathology.
Psychologists call the borderline state the degree of severity of character traits on the verge of norm and pathology.
Diagnosis
nine0087 In order to make a diagnosis of BPD, in addition to general symptoms, at least five other signs from the following list must be present:
1. Strong fear of being alone. The tendency to make excessive efforts to avoid the real or imagined fate of being abandoned.
2. A tendency to intense, tense and unstable relationships, in which extremes alternate - idealization and devaluation of the partner.
3. Identity disorder: instability of the image or feeling of the self. Ups and downs of self-esteem. Fuzzy ideas about myself (who am I? what do I like? what do I want?). nine0007
4. Impulsivity, which manifests itself in at least two areas of dangerous behavior, such as spending money, sexual behavior, substance abuse, risky driving, overeating.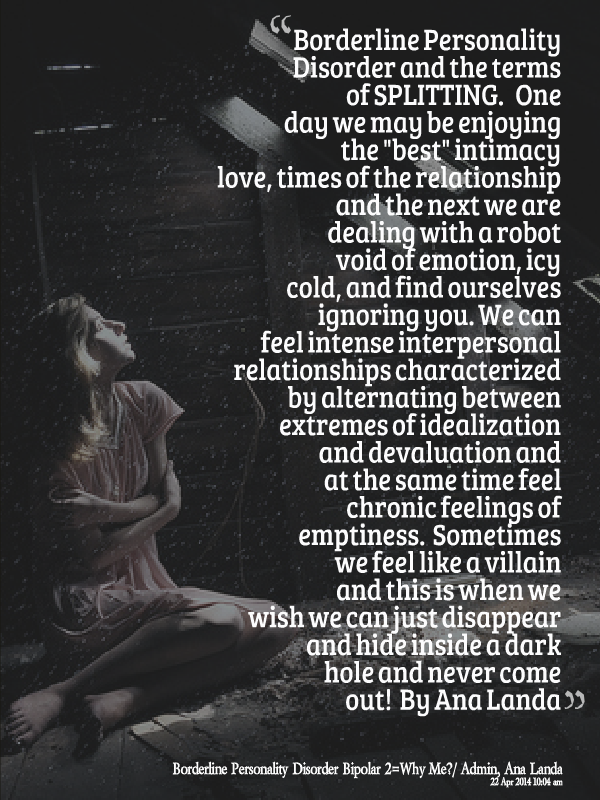
5. Recurrent suicidal behavior, suicide threats, repeated acts of self-harm. Masochistic tendencies in behavior and relationships with people.
6. Affective instability, extremely changeable mood. In this case, periods of intense dysphoria, irritability or anxiety are usually short and last from a few minutes to several days. nine0007
7. Constant feeling of emptiness, senselessness, boredom.
8. Inappropriate displays of intense anger or difficulty in controlling anger (eg frequent irritability, repeated fights).
9. In conditions of severe stress, paranoid ideas and suspicion, dissociative symptoms, derealization, depersonalization may occur.
10. Violations of mentalization, that is, understanding the motives of one's own and other people's actions, difficulty in understanding the emotions and reactions of other people. nine0007
11. Chaotic interpersonal relationships.
To understand what the world of the "border guard" looks like from the inside, I interviewed more than ten people with a diagnosis of "borderline personality disorder. " They talked about the main symptoms of BPD through the prism of personal and very painful experience.
" They talked about the main symptoms of BPD through the prism of personal and very painful experience.
Features of "border guards"
Psychiatrists call it identity disorder, psychopathy, sluggish schizophrenia - because BPD only exists in the DSM-4 foreign classification of diseases. "Border guards" are so dependent on the attitude of other people towards them and their own emotional outbursts that they hardly understand what they really are and what they want from life. These are solipsists in reverse: they consider the world around them to be a figment of their imagination, while people with BPD often doubt their own reality. nine0065
Who am I?
Anya: “The hardest thing is the complete fragmentation of the world and oneself. Every day or several times a day you are a completely different person, and you are strongly influenced by the people around you and events.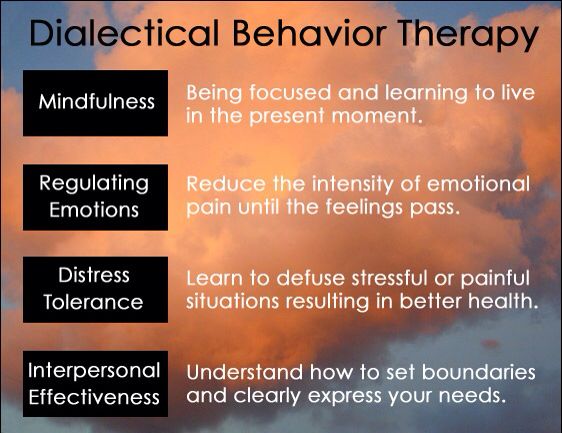 Either you are tough and distant, then you are deeply dependent and extremely emotional, then you are straight, then you are lesbian, then you are generally asexual. You can react radically differently to the same thing, depending on which part of your personality you find yourself in at that moment. And each of the states seems to be absolute, you are not able to remember yourself at this moment. nine0007
Either you are tough and distant, then you are deeply dependent and extremely emotional, then you are straight, then you are lesbian, then you are generally asexual. You can react radically differently to the same thing, depending on which part of your personality you find yourself in at that moment. And each of the states seems to be absolute, you are not able to remember yourself at this moment. nine0007
It's almost a split personality, and your parts are barely connected. The hardest part is the feeling that you don't really exist. It's like you only exist while someone is looking at you and talking to you, while someone else is reflecting you. Sometimes these fluctuations leave you so isolated that you want to go outside and pester passers-by, asking if they see me at all.”
Anastasia, 18 years old, actress in the experimental theater and physics student: "I still don't clearly understand who I am. A feeling of inner emptiness that has been progressing since childhood, an extremely unstable self-esteem.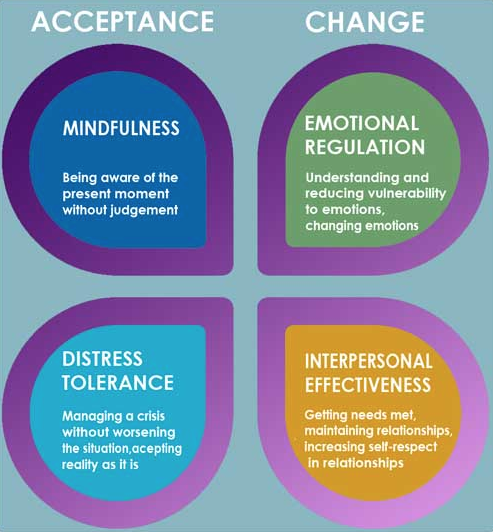 But it's not that disturbing yet. But after I was visited by depersonalization and dissociation, it became not fun at all. And when there was a constant desire to harm myself, I was not the only one who got scared. Poisoning, cuts, blows, blackouts, bulimia - an incomplete list of my adventures.
But it's not that disturbing yet. But after I was visited by depersonalization and dissociation, it became not fun at all. And when there was a constant desire to harm myself, I was not the only one who got scared. Poisoning, cuts, blows, blackouts, bulimia - an incomplete list of my adventures.
Existence with such a fragmented self-perception is very painful. The life of a "border guard" during periods of deterioration is a constant fear of being rejected and mental pain; what Freud called the word "Angst". nine0065
Lois , aged 23: “My brain hurts. Every time I experience hell like the first time. During the next episode, it always seems that it has never been worse, now it’s definitely an apocalypse. The memory of what was bad before and then disappeared disappears.
Even answering the question “How are you?” is problematic. Immediately a swarm of questions arises: how are you when? now or today? Or maybe you're hinting with your question that you don't like me? what answer do you want to get? nine0007
Fear sends me into a vicious circle, when all options for action are bad: not talking about what I feel, keeping everything in myself is bad for me. I speak out - people take it personally, even if I clarify that these are just my feelings. Friends get angry and upset, which makes me even worse. And I can talk in a bad state endlessly. The more I talk, the more I regret what I said."
I speak out - people take it personally, even if I clarify that these are just my feelings. Friends get angry and upset, which makes me even worse. And I can talk in a bad state endlessly. The more I talk, the more I regret what I said."
But a few people noted positive aspects in their condition. For example, the ability to empathize (although other people have said the opposite: that obsession with their feelings prevents them from taking the place of another). nine0065
Ksenia, 25 years old, social media manager: “I think I feel everything much brighter and deeper than others. It is very difficult for me to be alone on the streets and especially in the metro, where there are a lot of people. Grandmothers begging, a sad girl, a stray dog, a tired driver - they all give me an uncontrollable pity and a feeling of empathy that is almost impossible to cope with. Crying three times on the way from home to work is a common thing. nine0007
Illness has expanded the boundaries of my perception, growing such a huge range of feelings that it allows me to easily enter into the position of others.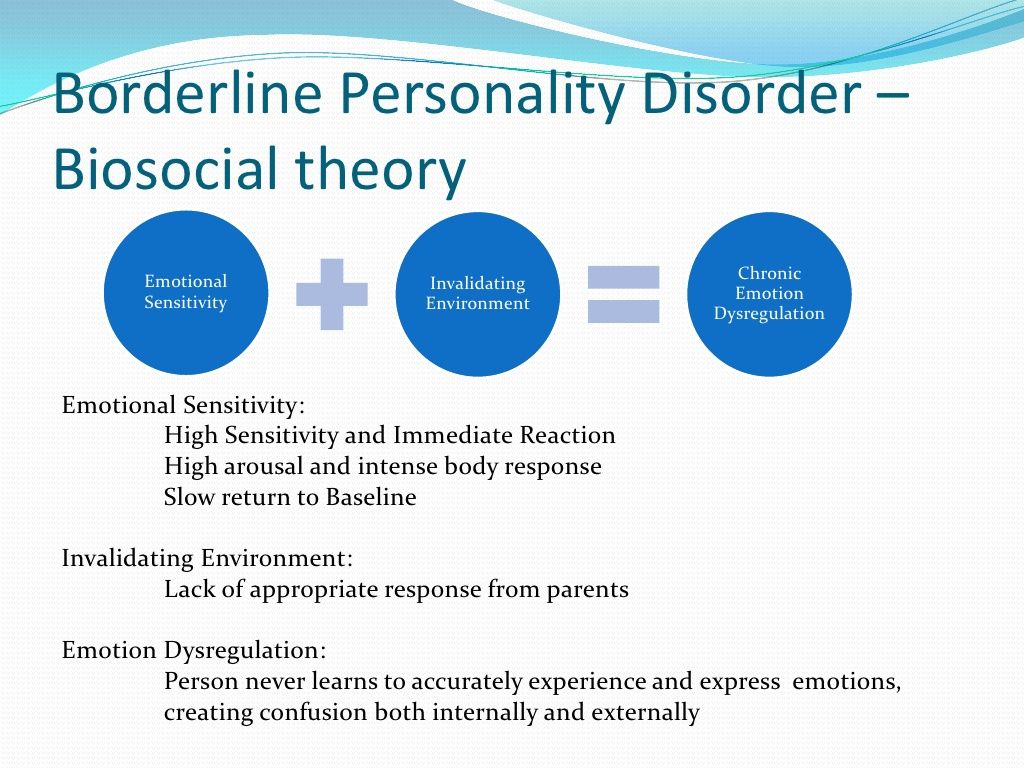 My young man says that sometimes he himself does not have time to understand himself and understand some of his inner experiences, as I already feel the slightest changes in him and anticipate events.
My young man says that sometimes he himself does not have time to understand himself and understand some of his inner experiences, as I already feel the slightest changes in him and anticipate events.
It is important to understand that the condition of a border guard is not a continuous series of suffering. There are periods of improvement, and quite long ones. At this time, they can experience "brighter, richer and more interesting feelings, sharpening in perception, the ability to notice and enjoy such things in the world around them that ordinary people simply pass by." nine0007
Max: “During episodes of good mood, you want to communicate with everyone, you become very friendly and there is a lot of energy that is easy to direct to any business, just give it a push. But everything is fine only until something hits the switch. Even one ridiculous thing - say, the death of a dove - can cause the world to abruptly change its tone to black.
Don't leave me - leave immediately!
nine0002 The void needs to be filled with something, and the fragmented consciousness needs to be glued together. Most often - strong feelings and emotions of other people, which the "border guard" needs like air.A feature that distinguishes all people with BPD is the difficulty in building stable relationships. On the one hand, they strive for dependence and complete merging, but at the same time they are afraid of intimacy, feeling danger in it. After all, if a loved one rejects you, it will be tantamount to losing yourself. Therefore, such people try to leave first, often suddenly and for no apparent reason. nine0007
Xenia: “People with BPD have such a concept as Favorite Person (FP). This is the one who replaces you all and everything. To some extent, this is reminiscent of the relationship between the dog and the owner, when the dog was left at home alone, and he trashed the whole apartment and whined at the door for several hours, waiting for the owner.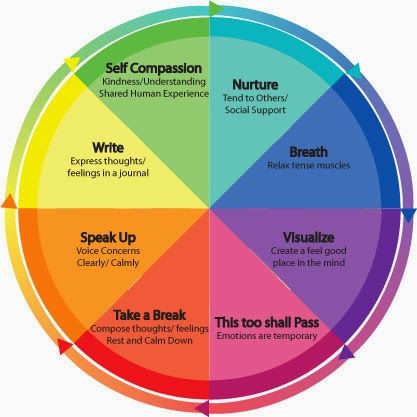 Most of the time I cannot be alone with myself, I am corroded by emptiness and at the same time a storm of emotions.
Most of the time I cannot be alone with myself, I am corroded by emptiness and at the same time a storm of emotions.
Rina, 25 years old, philologist: “I am constantly waiting for rejection. You may not be aware of this, live in peace, and then one of your friends will express himself incorrectly, say, for example, “Let's say goodbye” - and your world will immediately collapse. You start to think that the person doesn't want to see you again. You delve into yourself, trying to figure out what you did wrong, until you plunge into the abyss of sadness and thoughts about death. And a friend just wanted to say that he needs to go home now, we'll meet tomorrow. Always like this". nine0065
Being close to a "border guard" is risky. In his love, idealization is always replaced by depreciation, and the one who yesterday was a “handsome prince”, after a couple of unsuccessful phrases, can turn into a “terrible tyrant”.
N: “Because I am afraid of being left and abandoned, I have always destroyed all relationships.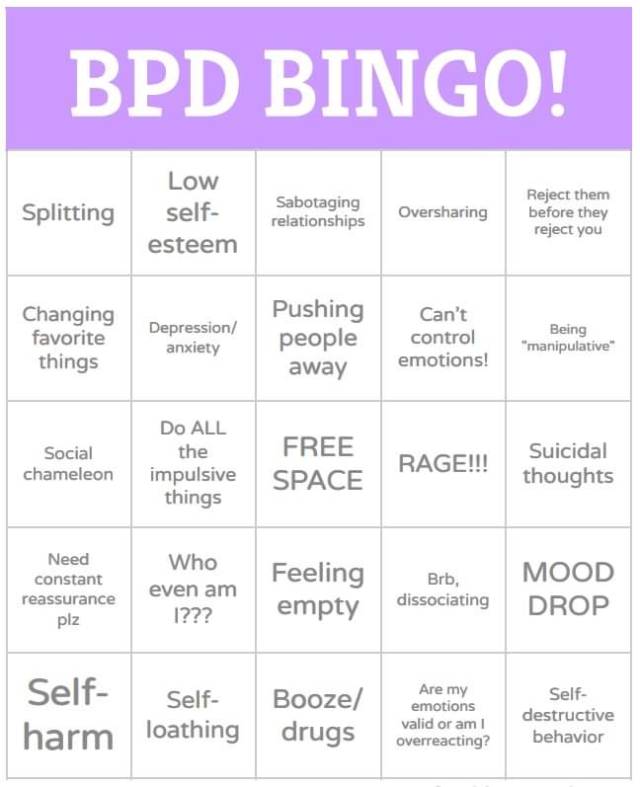 I started seeing a therapist because I was unable to trust the girls I dated. If we didn’t see each other for a day, and sometimes for several hours, I was absolutely sure that she had cheated on me, that everyone around me was deceiving. nine0007
I started seeing a therapist because I was unable to trust the girls I dated. If we didn’t see each other for a day, and sometimes for several hours, I was absolutely sure that she had cheated on me, that everyone around me was deceiving. nine0007
Pain and razor
Many do not believe in the depth and severity of the experiences of BPD sufferers. Their loud suffering from the outside may seem like just a way to attract attention and manipulate. But all these feelings, even if they are objectively inadequate, are completely real in the mind of the patient. Their ignoring and depreciation can end in a real disaster.
Up to 10% of "border guards" die by suicide. These are extreme cases. What happens much more often, at some point in life - with almost everyone, is self-harm, that is, self-harm. Chaos inside and mental pain become so strong that physical pain seems more acceptable. nine0007
My interlocutors named various motives for inflicting physical harm on themselves: it could be a “punishment” for bad behavior, a way to drown out guilt and shame for one’s “abnormality”, and even an attempt to destroy the “monster” inside, which destroys everything around and poisons the lives of loved ones . It can also be a cry for help, a desperate attempt to get support, most often from indifferent parents.
It can also be a cry for help, a desperate attempt to get support, most often from indifferent parents.
To suppress pain, both alcohol and psychotropic substances are used, therefore, borderline disorder gives rise to addictions and codependencies. nine0007
Xenia: “Many harm themselves spontaneously, thoughtlessly. But there are also those who specially, in a special way, prepare for this: they sharpen a knife, sterilize the skin, prepare bandages. Sometimes it is not enough for such people to inflict a wound on themselves, because it will heal anyway. They pour lemon juice over the cuts and cover them with salt.”
D., 20 years old, student: “At five in the morning, I was standing in the dormitory toilet with a knife in my hand. Blood was splattering down my leg. Back then, self-harm was the only reliable way to deal with emotions without losing performance. Then I carried the knife in my bag, kept it on the table next to the laptop at home and even sometimes slept with it, hiding it under the pillow or under the bed. Only then did I realize that it was a disease.” nine0065
Only then did I realize that it was a disease.” nine0065
The greatest risk of suicide in BPD is at a young age (13-15 years)
© Berman A.L., 1985; Friedman R.C., 1987
Aggression can be directed not only at oneself, but also at another. Not so long ago, the Internet was bypassed by a video of schoolgirls who beat each other in a wasteland while friends were filming it. The audience was shocked by girlish aggression: they tried to blame her on television, computer games. It seems that no one then thought that this could be a way to overcome mental pain: “Anya (author's note: the heroine's best friend) backhanded me in the face. We fought: we thrashed with our fists and legs, pulled each other by the hair, scratched, tried to knock each other to the ground and beat each other harder. We smashed our noses and cut our lips, ripped our clothes and tried to release our heartache, like in Fight Club. nine0007
Some manage to channel this need for physical pain into more acceptable channels.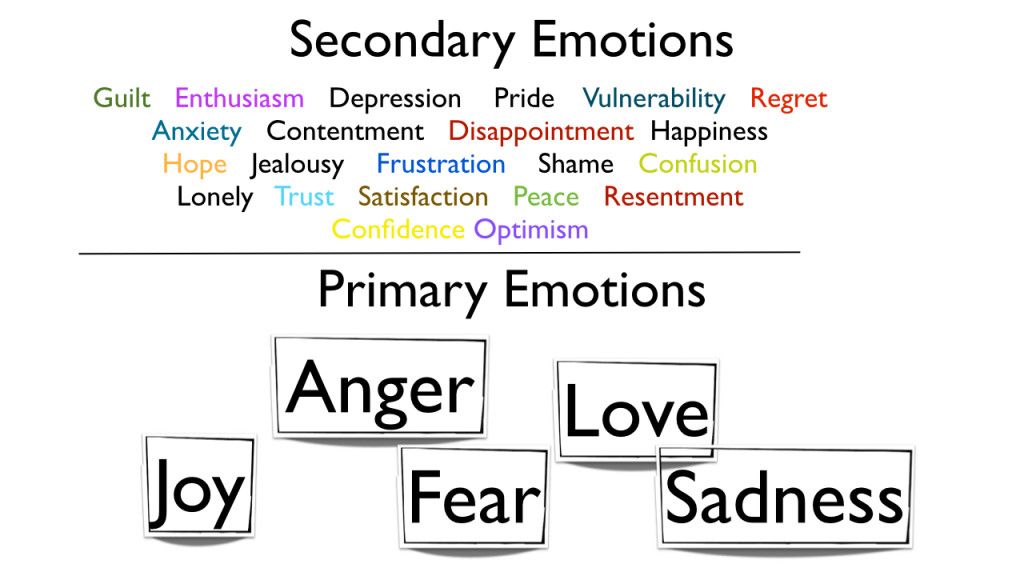 Among the border guards there are many fans of piercings, tattoos, BDSM.
Among the border guards there are many fans of piercings, tattoos, BDSM.
Not all people with BPD cut themselves and abuse alcohol or other substances: borderline disorder can present with relatively "mild" disorders. In borderline disorder, either impulsivity, suicidal attempts, or violations of direct interpersonal relationships may predominate, when, due to emotional instability, relationships with others become negative. There are more severe violations, as in the case of suicide attempts, when psychiatric consultations are necessary. There are such disorders in which you can improve your life with the help of regular psychotherapy and work on yourself. That is, the gradations of symptoms in the manifestation of BPD are very different! Sometimes people seem to be adapted at first glance, everything “seems to be all right” with them: they work, they live well, but in stressful situations they can show impulsive destructive behavior. One hundred and fifty-one different combinations of symptoms are possible in the clinical picture of patients diagnosed with BPD (and some authors give two hundred and fifty-six as a possible number of combinations of symptoms)! nine0007
Self-help
Borderline disorder is by no means a sentence.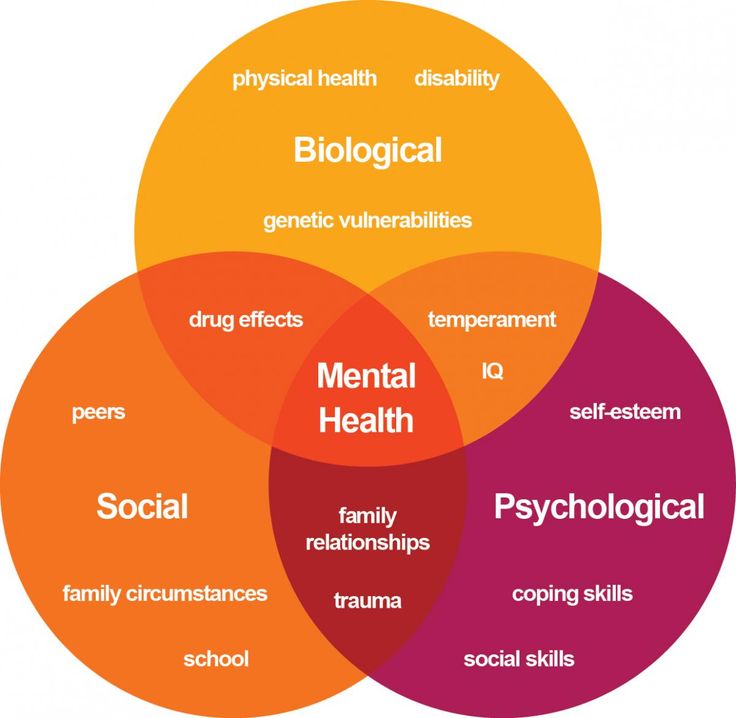 Almost all of my interlocutors were able to recognize their problem and find constructive ways to deal with emotional extremes. In order to perceive the world as it is, and not as dictated by a sick imagination, the "border guard" needs to make great efforts.
Almost all of my interlocutors were able to recognize their problem and find constructive ways to deal with emotional extremes. In order to perceive the world as it is, and not as dictated by a sick imagination, the "border guard" needs to make great efforts.
J: “I have a whole list of self-help methods: meditation, mindfulness exercises, detachment from the situation (I physically interrupt the conversation, leave the apartment, and so on). And, of course, in my head there is always a background process of tracking my thoughts and correcting errors of perception. Regularly do “reality checks”:
1.
in my mind I build a “line of defense” in favor of the person whom I suspect of bad things;
2.
asking a stranger how he would react to the situation;
3.
step back, wait until emotions subside, and only then make a decision;
4.
I try to keep a schedule of work and rest: I am especially unstable during sessions and deadlines, so I try to prepare in advance and always get enough sleep. ”.
”.
N: “The therapist gave me an exercise based on meditation: in an inner voice that expresses self-care, acknowledge my feelings, acknowledge that right now it hurts and is unpleasant, and then imagine a gesture that would express self-care ( like a big hug). It helps a lot. It became incredibly easier for me to live when I realized what was happening, that all these things (a change in the meaning of life every ten minutes, breakdowns and tantrums) are not really me, but my disease.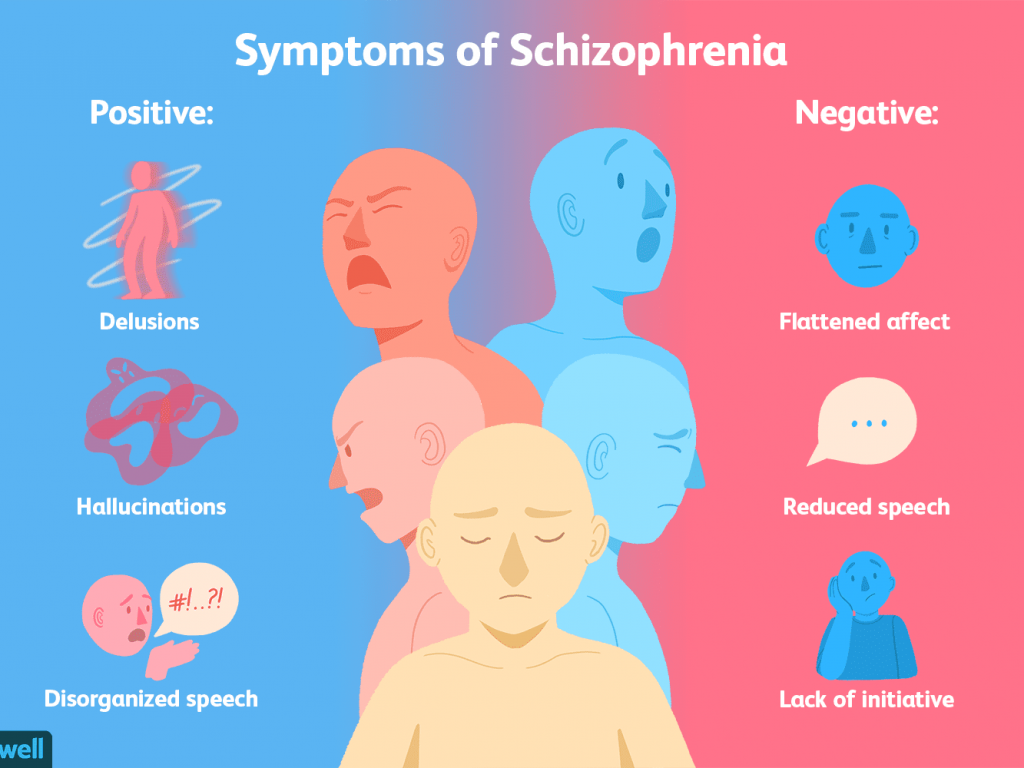
Lois: “Adequate view from the outside is extremely important to us. A friend recently told me what my “borderline” part looks like. And that was the most helpful information I've received in months. She helped me finish a difficult episode. Without a friend, I would never have guessed what it looks like.
She (my border side):
1.
requires constant attention;
2.
she needs to explain everything;
3.
her thoughts must be guessed;
4.
she acts like a child.
I am learning to catch and unravel "borderline" thoughts, make them absurd, I try to share them with loved ones in order to jointly refute them. It's a very useful practice."
Polina: “I am a perfectionist and have always strived to be the best. But if I've learned anything during my illness, it's that the world and the people around you are already demanding enough, so it's important to be kind and gentle with yourself. Now I just allow myself to be weak. I allow myself to listen to sad music, cry and whine. I allow myself to take breaks from work. Because I know that if you do not allow yourself weakness, it will be even worse. nine0007
Now I just allow myself to be weak. I allow myself to listen to sad music, cry and whine. I allow myself to take breaks from work. Because I know that if you do not allow yourself weakness, it will be even worse. nine0007
Alexander , poet, journalist: “I am always looking for new, constructive ways. For example, the People Skills To Go app for people with BPD. In times of crisis, without psychotherapists and psychiatrists, I would not have coped. Sometimes people get tired of me and stop talking, but many people stay in relationships for many years, and I think that love overcomes pain.
Many BPD sufferers have a desire for creativity, self-expression through it. And this is also a form of therapy. nine0065
Anastasia: “The theater saves me. If there are no rehearsals, I dance, merge with the music. If there is no physical strength, then I lie on the floor and listen to cello and piano recordings.
Xenia: “The Telegram channel saved me, I wrote everything I felt there, trying to spit out all the lines in a beam between my eyes.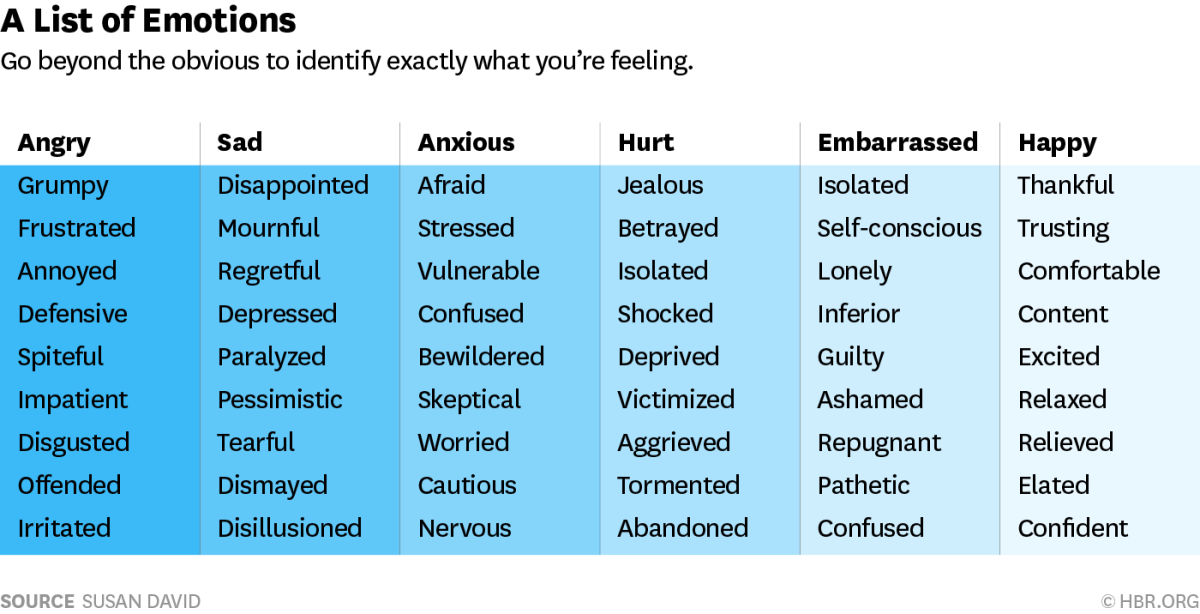 The letters floated in front of me, blocking out the pain for a while. A round dance of unspoken words that flew like canvases to the Internet to thousands of people. nine0065
The letters floated in front of me, blocking out the pain for a while. A round dance of unspoken words that flew like canvases to the Internet to thousands of people. nine0065
Relationships
Many people with BPD are quite happy with their social and personal lives, but this is exactly the case when you cannot rely on feelings and the will of fate alone. A lot of work is needed on oneself and relationships, and on both sides. The “border guard” needs to be aware and pronounce every conflict moment, and, most importantly, learn to express their feelings without aggression. Partner, respectively - to support him and calmly answer even the strangest questions. nine0007
The popular advice for dealing with "tantrums" - to go away and wait until she calms down - is not applicable in any case, because everything can end very badly.
Daria: “I used to have more friends, but it was codependency based on the 'eat my mental waste and I'll eat yours' co-dependency.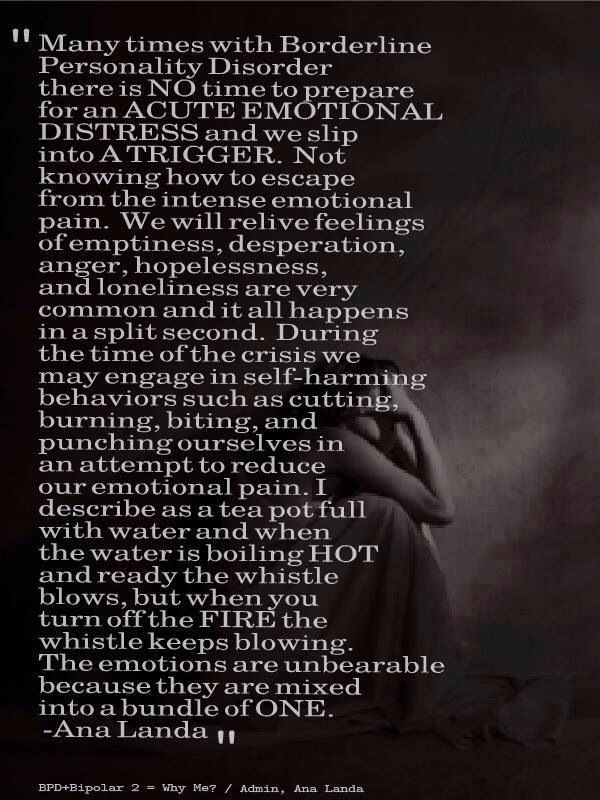 Now I redefine the concept of friendship for myself.
Now I redefine the concept of friendship for myself.
It was hard for my second husband, whom we met at the height of my treatment. He says that he had to calm me down two or three times a day. I was stormy at the sudden appearance of a valuable person whom I tried to simultaneously idealize and completely appropriate, and completely devalue - that is, forever banish from the horror of intimacy. Now, three years later, when I sometimes start to stagger from fatigue and overstrain, I “hang” on my husband - I describe my feelings to him, he gently tells that in reality everything is not so, but much better, and it becomes easier for me. nine0007
Rina: “My friends know my diagnosis. Friends and colleagues consider me an interesting and very eccentric person. I studied so much literature about PHR that I learned how to lecture my friends about what was happening to me. Now they almost see me better when I am carried, and can insure in time.
Polina: “I do not hide my condition from anyone: not so long ago I published a long post on Facebook explaining my diagnosis in detail, and received a lot of support.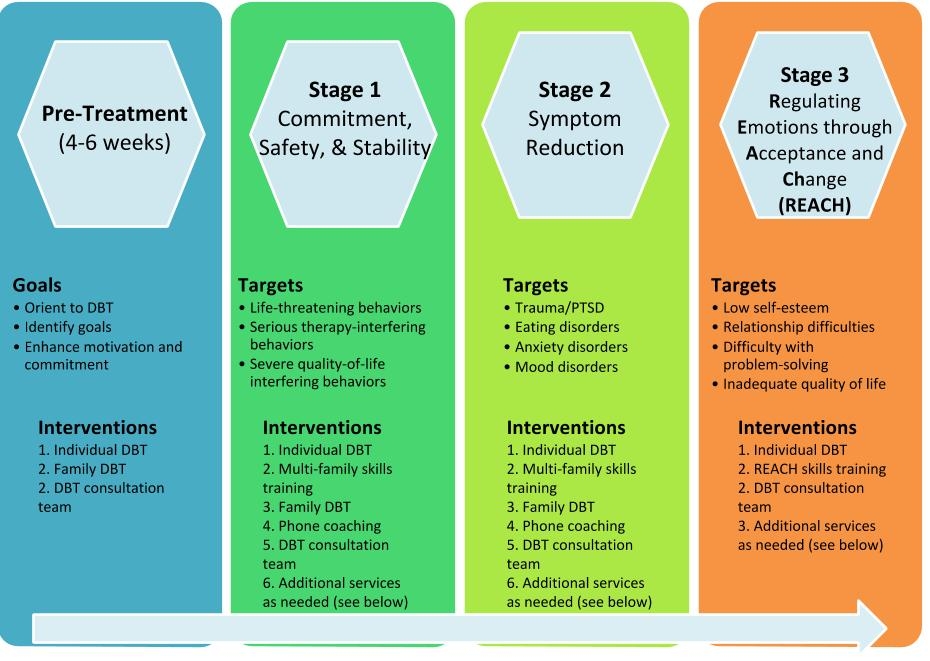 Many relatives are also aware, but not everyone understands how to behave correctly. Even my father, when I told him about BPD, joked: “Go to the village to milk the cows at five in the morning.” Not a very good joke, I think. nine0007
Many relatives are also aware, but not everyone understands how to behave correctly. Even my father, when I told him about BPD, joked: “Go to the village to milk the cows at five in the morning.” Not a very good joke, I think. nine0007
I think it's pointless to hide, because sooner or later my condition will become public - I'm not made of iron. So I try to avoid rumors, discussions behind my back and accusations of a bad temper. I'm really lucky that they accept me, because, perhaps, I myself would not want to be my own friend.
Lois: “Before I couldn't tell when something was going on, now I can say to a new acquaintance, 'Sometimes I react illogically to what's going on around me. If I ask: Are you sure you don't hate me now? “It means that I’m really afraid to hear: yes, I hate you and don’t want to see you ever.” nine0065
Diagnostics in Russia
The cases described above are the exception rather than the rule.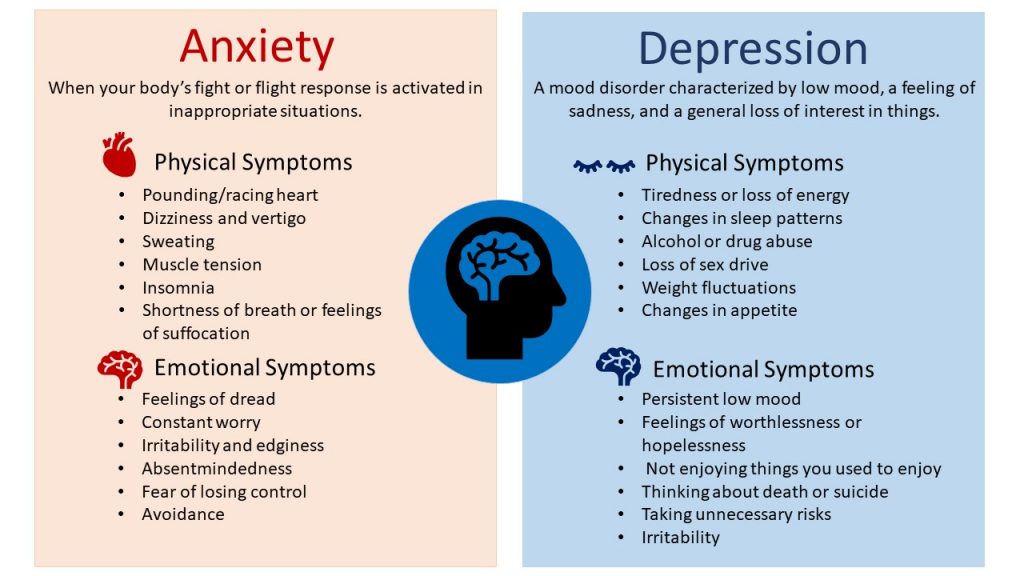 Most people with borderline disorder do not know their diagnosis and do not receive any treatment.
Most people with borderline disorder do not know their diagnosis and do not receive any treatment.
Because BPD has almost no obvious psychiatric manifestations such as hallucinations and psychosis, it does not occur to the patient or his relatives to see a doctor. Self-harm - the most obvious manifestation of BPD - patients carefully hide. nine0007
Acquaintances consider such a person to be hysterical, self-centered, capricious, with a bad temper and do not believe that he can be changed. He himself, due to the specifics of the disease, is not able to analyze and evaluate his condition, and in his problems he sincerely considers others or external circumstances to be guilty.
Anna Ushkalova, psychiatrist: “Difficulties in diagnosing BPD — like other personality disorders — lie in the fact that, historically, the mental health care system in Russia has been oriented toward inpatient treatment, with an emphasis on acute and emergency conditions.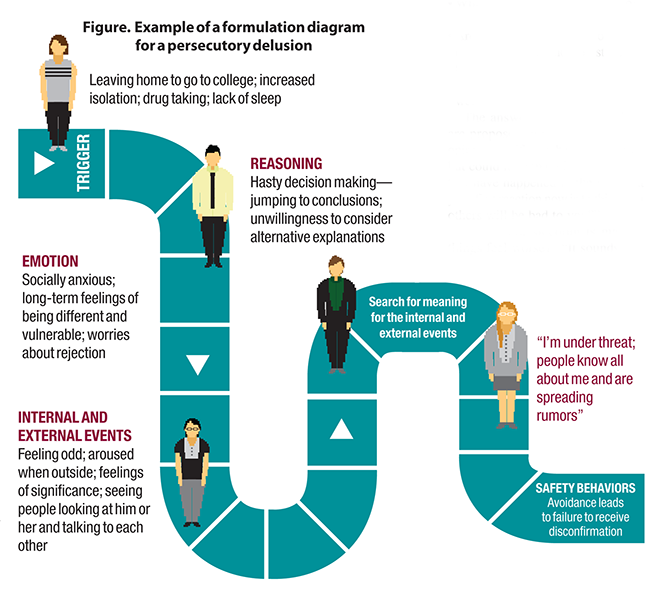 Russian psychiatry paid insufficient attention to personality disorders in general. In addition, psychotherapeutic education in our country is not included in the basic course of psychiatry. Nevertheless, interest in this problem is growing, as is the number of specialists with skills and experience in working with such disorders. nine0069
Russian psychiatry paid insufficient attention to personality disorders in general. In addition, psychotherapeutic education in our country is not included in the basic course of psychiatry. Nevertheless, interest in this problem is growing, as is the number of specialists with skills and experience in working with such disorders. nine0069
The situation is complicated by the fact that in the International Classification of Diseases (ICD-10) adopted in Russia, the diagnosis of "borderline personality disorder" does not exist at all. There is a concept close, but not identical to it - "emotionally unstable personality disorder" (disease code - F60.3).
Daria: “I realized what was happening to me, closer to twenty-five years, when they started writing about BPD on the Internet. I realized that I am not a lazy, inconsistent, irresponsible hysteric, but that what is happening in my body and head has objective reasons. nine0065
Up to a third of all completed suicides are committed by people with BPD
© Kullgren G. et al., 1986; Runesson B. et al., 1991; Links, 2003
et al., 1986; Runesson B. et al., 1991; Links, 2003
Unfortunately, often those with BPD do not see a doctor for the first time until after a suicide attempt. If it does not reach such an extreme, the diagnosis can turn into a whole investigation.
Polina: “The prerequisites were in early childhood, and alarm bells began to be heard in high school, when I unexpectedly started cutting myself, then starving myself and depriving myself of sleep. It took me a long time to figure out what was wrong with me. At first she turned to a private psychotherapist, but she suspected a charlatan in her. Long trips to the doctors began. They didn’t tell me anything worthwhile, they advised me to drink glycine. In the meantime, I suspected that I had bipolar disorder, it seemed to me that I was wasting time with doctors - in general, it was so. The mother of a friend once told me that she was successfully treated in the Clinic of Neurosis. Already at home, in St.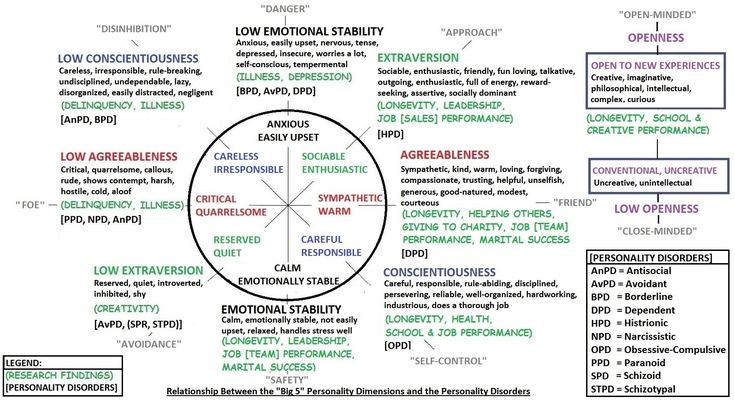 Petersburg, a neurologist in the district clinic wrote me a referral. At the clinic, I was first diagnosed with “bipolar disorder”, but it was not confirmed. The psychiatrist started calling me ‘border guard’.” nine0065
Petersburg, a neurologist in the district clinic wrote me a referral. At the clinic, I was first diagnosed with “bipolar disorder”, but it was not confirmed. The psychiatrist started calling me ‘border guard’.” nine0065
Some of the symptoms of borderline disorder are indeed similar to those of bipolar disorder (mood swings, alternations of agitation and depression, depression), and misdiagnosis is not uncommon.
It is important to remember the differences: in BPD, unlike bipolar affective disorder, mood swings are instantaneous and can occur dozens of times a day, and are most often caused by external events rather than internal processes.
But there are also patients in whom these two diseases are combined: according to a number of studies, such cases are more than 10%. nine0007
Anna Ushkalova, psychiatrist: “In the new, eleventh edition of the International Classification of Diseases, a transition to completely different criteria for all personality disorders, including BPD, is planned.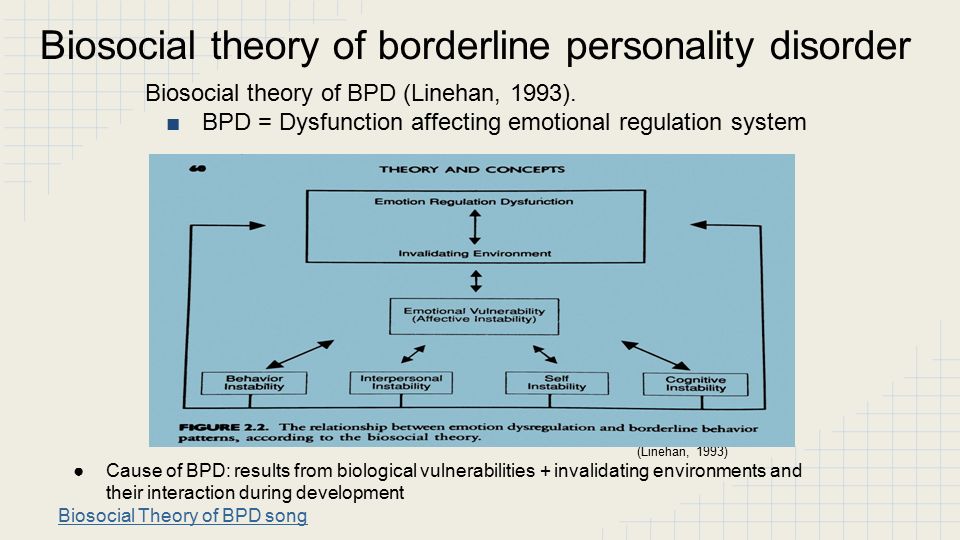 First of all, the degree of maladjustment of a person will be taken into account. If a doctor in the public care system can even determine the very presence of the disorder and send the patient to a psychotherapist, this will be a breakthrough in treatment.”
First of all, the degree of maladjustment of a person will be taken into account. If a doctor in the public care system can even determine the very presence of the disorder and send the patient to a psychotherapist, this will be a breakthrough in treatment.”
Making a diagnosis, no matter how hard it may sound, changes the lives of patients for the better. Understanding what exactly is happening to you, and that you can influence it, gives a sense of control that people with borderline disorder lack so much. nine0065
Xenia: “Before, I constantly thought that other people just didn’t want to understand me, that I didn’t try hard enough, that I should become like everyone else, or vice versa, everyone should become like me. Until the age of twenty-four, I had full confidence that I was special, that I had a completely unique set of qualities, that I did things that were peculiar to me. And then I read an article about BPD and realized that I had lived my whole life as if by a textbook.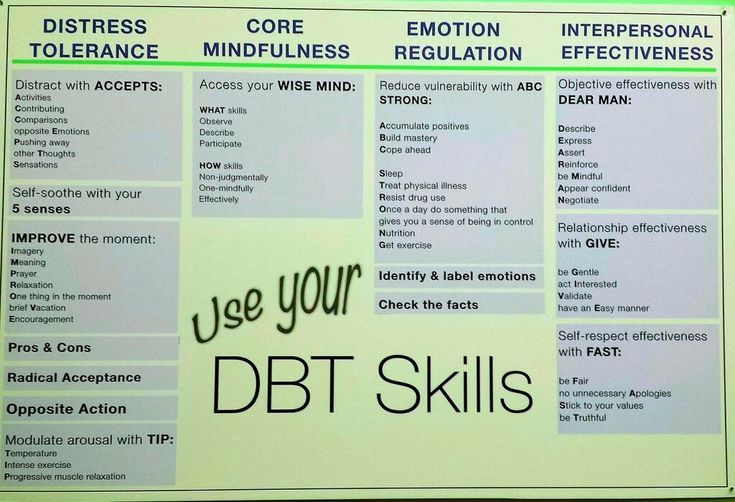 ”
”
Causes of borderline disorder
There is no clear understanding of the causes of borderline disorder.
As with most mental illnesses, both innate predisposition and early trauma seem to play a role. In almost every case history there is an emotional shock: the loss of a very close person, physical or sexual abuse, generally inappropriate behavior of parents.
If in due time the child is not taught to value himself as a person and to understand where the boundary lies between his interests and the interests of others, he will not be able to trust either others or himself in the future. nine0007
Anna Ushkalova, psychiatrist: “Currently, the biosocial model has received the greatest recognition. The pathogenesis of BPD can be represented as follows: against the background of a genetic predisposition, there is a “vulnerability” of individual biological structures (hyperactivity of the limbic system, a decrease in the regulatory function of the prefrontal cortex).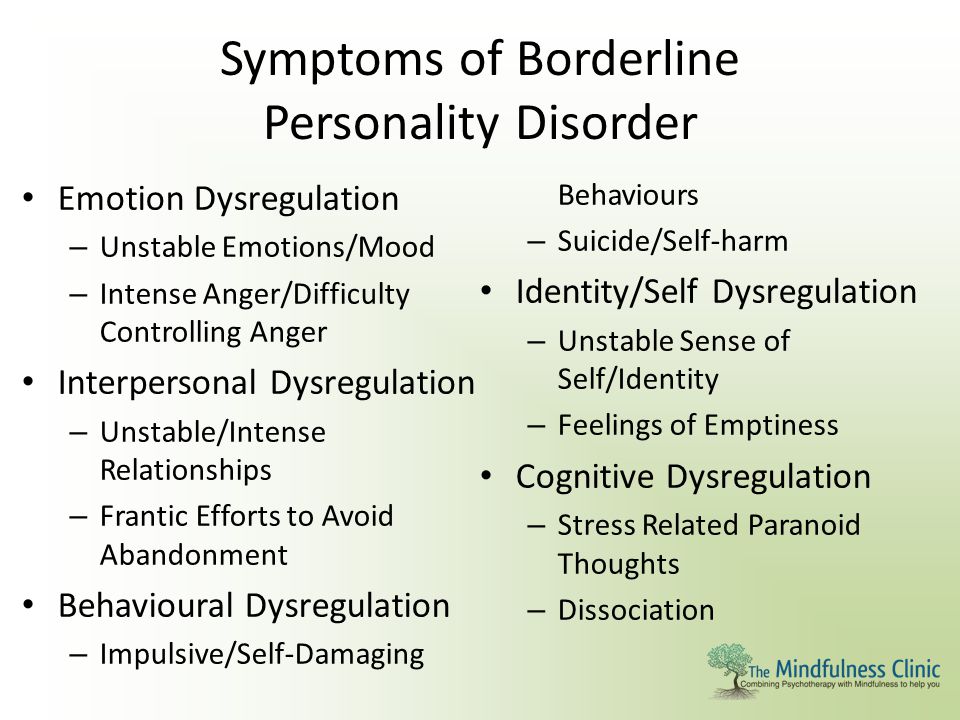 This leads to increased excitation and slower inhibition in response to stress. The combination of these factors with adverse conditions, especially in childhood (such as sexual or physical abuse, neglect) leads to the fact that the patient develops a dysfunctional pattern of emotional response and behavior. nine0069
This leads to increased excitation and slower inhibition in response to stress. The combination of these factors with adverse conditions, especially in childhood (such as sexual or physical abuse, neglect) leads to the fact that the patient develops a dysfunctional pattern of emotional response and behavior. nine0069
Psychological reasons
The most common cause of borderline disorder is considered direct child abuse in the family and chronic childhood trauma.
Xenia: “When I was four years old, I was sexually abused by an elderly man. This situation haunts me to this day and clearly had a great influence on the formation of my personality. Specifically, it blew the roof off me at thirteen or fifteen: alcohol, drugs, the wrong company, fights, hooliganism, running away from home, uncontrolled sexual behavior. nine0007
Lois: “When I was twelve, my stepfather confessed his 'love' to me.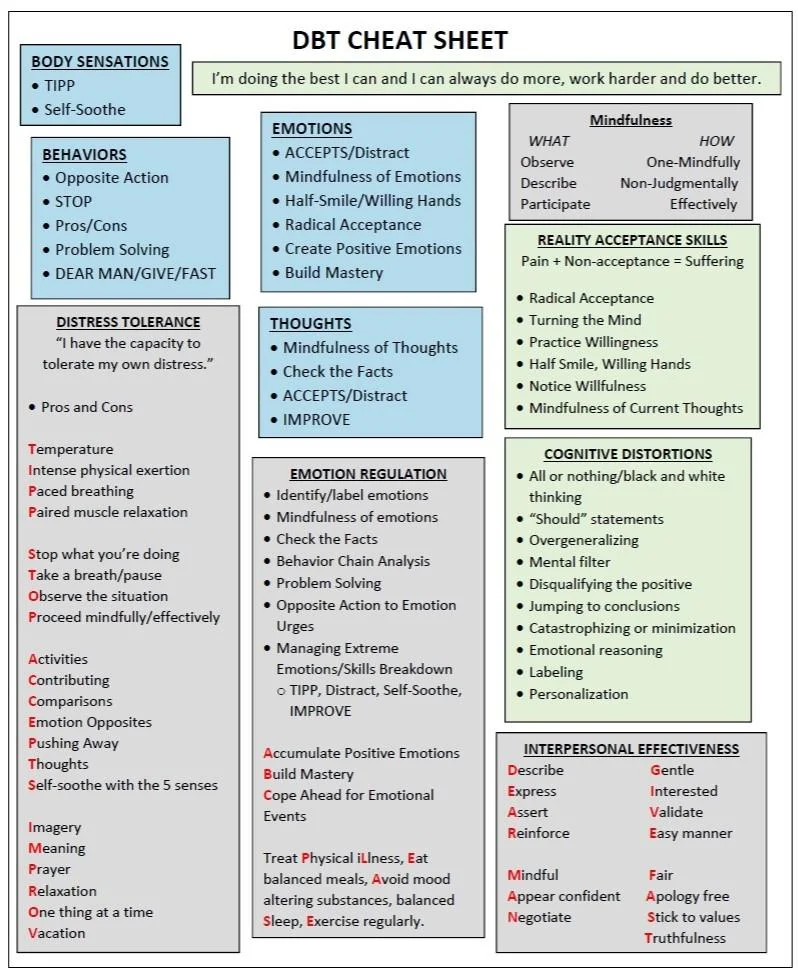 The first "kiss" was with him. At that time, I did not understand so much what was happening that I froze physically, disconnected from all emotions and did not talk to anyone for another two days. Then there was a series of cases of psychological and physical violence, and he constantly said that he loved me and suffered because of such a difficult situation. In addition, he followed all my actions, read correspondence with my friends, communicated with them if he did not like something. I didn’t understand what was going on at all, but he threatened me and I haven’t told my parents anything until now.” nine0065
The first "kiss" was with him. At that time, I did not understand so much what was happening that I froze physically, disconnected from all emotions and did not talk to anyone for another two days. Then there was a series of cases of psychological and physical violence, and he constantly said that he loved me and suffered because of such a difficult situation. In addition, he followed all my actions, read correspondence with my friends, communicated with them if he did not like something. I didn’t understand what was going on at all, but he threatened me and I haven’t told my parents anything until now.” nine0065
However, more often than not, an unfavorable emotional situation is enough: often “borderliness” is brought up by parents with their own mental disorders.
Anya: “Mom has a mental disorder, although she has never seen a psychiatrist. Her contact with reality was clearly broken, she always lived in imaginary worlds, and from my early childhood I was left to myself, there was practically no communication within the family.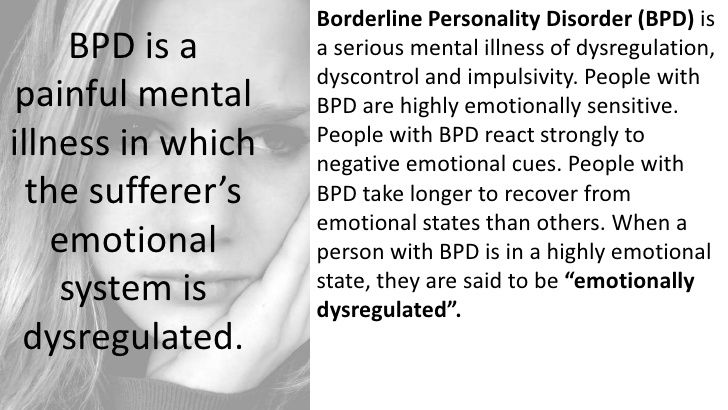
Daria: “The family was middle-income, no one beat or raped me, and for a long time I could not understand what had destroyed me so much. My brother and I had cold, anxious, aggressive, demanding parents, a depressed mother, and a combination of borderline and narcissistic father. It looked like this: something rolled over one of the parents, and they began to bombard my brother and me with demands, accusations, claims against each other - “your neglected mother” and “your crazy father”. It was quite difficult to predict when and whom it would close, so we grew up in an atmosphere of complete chaos, which we attributed not to our parents, but to ourselves. As a result of such an upbringing, I considered myself practically crazy and honestly thought that I would end my life in the garbage, where I belong. nine0065
Some people described their families as outwardly quite normal and, in the opinion of others, prosperous. Often the violence is purely emotional and goes unnoticed by outsiders.
Rina: “All my childhood I diligently fulfilled the function entrusted to me - reconciling my parents when they made scandals.”
V., IT specialist: “There was a conflict in the family. I was a very late child and... I don't know how to explain it - this is a huge gap between the parents' view of life, the way it should be, and the views of other people. I was “that weird kid” who was dressed the wrong way and treated the wrong way. As a result, at the age of eighteen, he ended up in a therapeutic department of psychiatry with hysteria. nine0007
Polina: “My earliest childhood was almost perfect. But in elementary school, my father lost his business and fell into a deep depression. So that I would not see this, I was sent to live with my grandmother. Grandmother is a church-going person, which she instilled in me as well. This had a rather strong influence: I treat each of my mistakes as a terrible sin, I feel guilty about everything.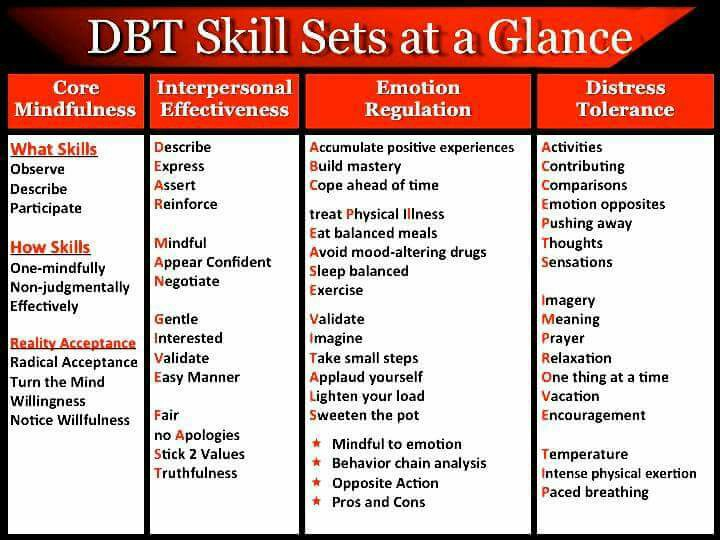 At confession, you pronounce your sins to the priest, and he lets them go for you. My “sins” never let me go, I didn’t feel forgiven by anyone.” nine0065
At confession, you pronounce your sins to the priest, and he lets them go for you. My “sins” never let me go, I didn’t feel forgiven by anyone.” nine0065
Biological causes
Physicians have discovered abnormalities in the functioning of the brain of people with borderline disorder.
Tendency to depression, anxiety and fear of being abandoned were explained by disturbances in the functioning of serotonin receptors. Due to childhood stress, these receptors become less sensitive to stimuli. That is, impulsiveness, weak will and self-control are not the result of promiscuity: it has specific biological causes. nine0007
Using brain mapping techniques, researchers have identified key reasons for the inability of BPD patients to regulate their aggression. BPD sufferers have a strong activation of the amygdala, which is responsible for emotions, which can cause errors in perceiving other people's neutral facial expressions when they appear unfriendly. Moreover, doctors note that distortions in the mental world can be not only a consequence, but also the cause of impaired activity in the amygdala. In addition, patients with BPD produce more of the stress hormone cortisol, so they are in a constant state of hyper-alertness. The prefrontal cortex, which is responsible for self-control, on the contrary, is too weakly activated in such patients: this prevents them from evaluating their actions from the outside. Also, many “border guards” found a decrease in the volume of the hippocampus, which is responsible for memory: it is suggested that this makes it difficult to comprehend the history of relationships with other people. The hormone dopamine, which causes us to enjoy pleasant things and encourages us to seek these pleasures, is often produced in BPD sufferers from relationships that bring negative emotions - hence the desire to repeat unpleasant relationship patterns. nine0007
Moreover, doctors note that distortions in the mental world can be not only a consequence, but also the cause of impaired activity in the amygdala. In addition, patients with BPD produce more of the stress hormone cortisol, so they are in a constant state of hyper-alertness. The prefrontal cortex, which is responsible for self-control, on the contrary, is too weakly activated in such patients: this prevents them from evaluating their actions from the outside. Also, many “border guards” found a decrease in the volume of the hippocampus, which is responsible for memory: it is suggested that this makes it difficult to comprehend the history of relationships with other people. The hormone dopamine, which causes us to enjoy pleasant things and encourages us to seek these pleasures, is often produced in BPD sufferers from relationships that bring negative emotions - hence the desire to repeat unpleasant relationship patterns. nine0007
Useful resources about BPD
In 2017, the first Russian Resource Center was opened - an information portal for people suffering from borderline personality disorder, created on the basis of the experience of colleagues from the USA and Australia.