Can you be manic and depressed at the same time
Is it possible to be hypomanic and depressed at the same time?
Is it possible to be hypomanic and depressed at the same time?
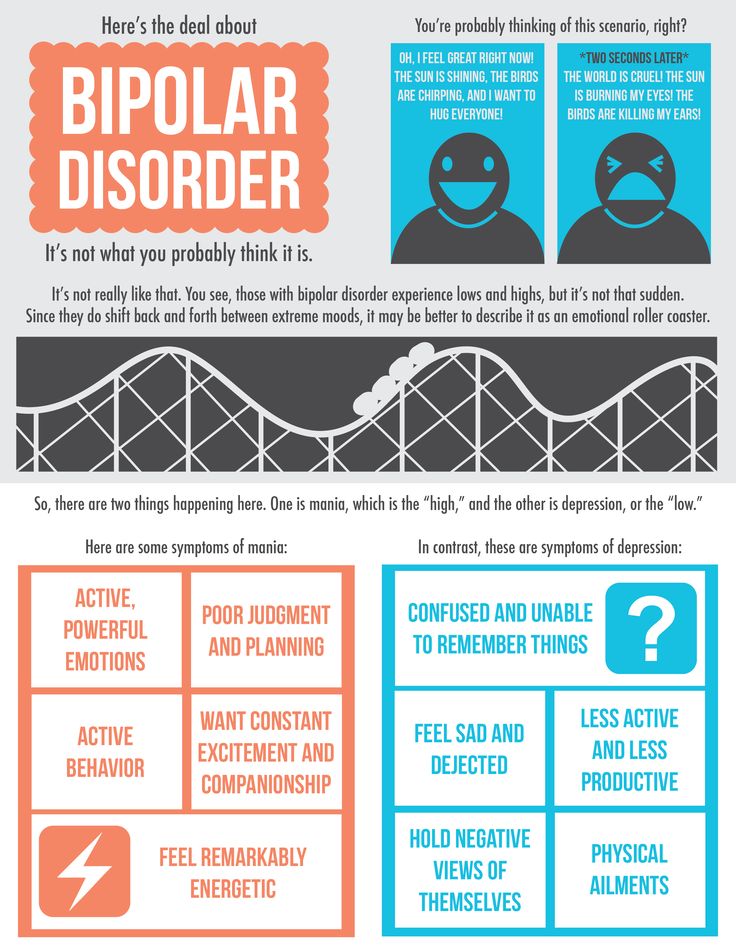
Certainly! Some studies, the most common mood state in bipolar disorder is a mixture of hypomanic/manic and depressed symptoms. In fact, the classic picture of bipolar disorder having a course alternating between the poles of high and low moods is an over-simplification. The very name, bi–polar disorder is probably less accurate than the older term, manic-depressive disorder. How can this be?
Although bipolar disorder has been classified as a “mood” disorder, ample research shows that the core symptom of hypomania and mania is not high mood, but rather hyperactivation
. The mood, as many people have experienced, can either be elevated or irritable. But what always appears in manic or hypomanic episodes is a sense of being “sped up” physically and/or mentally. Racing thoughts, pressured speech, decreased need for sleep, starting lots of projects, and impulsive decision-making all derive from being overly activated, overly driven. Many times this sense of hyperactivation is pleasant—when one is feeling particularly “on my game” the person is self-confident, more likely to act decisively, and often more likely to take risks. However, sometimes being hyperactivated simply is a sense that one’s “motor cannot be turned off.” This can lead to restless irritability, especially if one is confronted by reality or other individuals that do not match expectations. Thus what is common in mania or hypomania is the sense of hyperactivation, or being driven, but the mood can be variable.
What does the DSM, the official naming system for the American Psychiatric Association, have to say about this? Well, there has been some improvement between DSM-IV and DSM-5. In DSM-IV, mixing of manic and depressive symptoms was barely recognized, appearing only in the very limited category of “mixed manic and depressive episodes.” More recent research guided the writers of DSM-5 to rethink this approach, and they came up with this more reasonable and accurate way of describing mixing of hypomanic/manic and depressive symptoms: Mood state is categorized as primarily hypomanic/manic or depressed, but clinicians can add the “modifier” of having depressive features (for hypomanic or manic episodes) or manic features (for depressive episodes). It is also notable that DSM-5 has taken the same approach to recognizing anxiety features in hypomanic, manic, or depressive episodes.
It is also notable that DSM-5 has taken the same approach to recognizing anxiety features in hypomanic, manic, or depressive episodes.
Overall, then, it is not surprising that mood in hypomania or mania can sometimes be depressed. In fact, it may be most accurate to think of bipolar disorder not as a condition of alternating too-high and too-low moods, but rather as a condition of recurring depressive periods punctuated by periods of hyperactivation—and sometimes these periods of hyperactivation alternate with slowed down, depressed periods, but at other times they overlap.
Because many people think that bipolar disorder can only be “bi-polar”, they may not talk to mental health providers about feeling both depressed and sped up. Assumptions or labels can sometimes get in the way of understanding.
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.

Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders. This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.
Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Bipolar disorder - Official website of the FGBUZ KB No. 85 FMBA of Russia
General brief information
Bipolar disorder, also known as bipolar affective disorder (BAD) and formerly as manic-depressive psychosis (PMD). It is a set of mood disorders characterized by marked fluctuations in mood, thinking, behaviour, energy and ability to perform daily activities.
A person suffering from this disorder alternates his state of mind between mania or hypomania - a phase of joy, exaltation, euphoria and grandiosity and depression, with sadness, inhibition and ideas of death. nine0005
Four types of bipolar disorder were defined by severity and alternation of moods over time:
- Bipolar I disorder
- Bipolar disorder type II
- Cyclothymia
- Non-specific bipolar disorder
Because bipolar disorder occurs in young people, it has a high social cost. It is the second leading cause of disability worldwide. In addition, those who suffer from it pose a higher risk than the general population of deaths from suicide, homicide, accidents, and natural causes such as cardiovascular disease. nine0005
In type 1, the person alternates between depressive episodes with full manic episodes, and in type 2, he alternates between depressive episodes and hypomanic (less severe) episodes.
The symptoms of this disorder are severe, different from the normal highs and lows of mood. These symptoms can lead to relationship problems, work, school, or even suicide.
These symptoms can lead to relationship problems, work, school, or even suicide.
During the depression phase a person may experience:
- Negative perception of life. nine0014
- Inability to feel the pleasure of life.
- No energy
- Self-criticism.
- In extreme cases, suicide.
During a manic phase a person may experience:
- Denial that there is a problem.
- Sudden change of mood.
- Irrational financial decisions.
- Feeling of great enthusiasm
- Don't think about the consequences of your actions.
- Lack of sleep nine0021
- Persistent sadness
- Lack of interest in engaging in pleasurable activities.
- Apathy or indifference.
- Anxiety or social anxiety.
- Chronic pain or irritability.
- Lack of motivation
- Guilt, hopelessness, social isolation.
- Lack of sleep or appetite. nine0014
- Suicidal thoughts
- In extreme cases, there may be psychotic symptoms: delusions or hallucinations are usually unpleasant.
- Great energy and activity.
- Some people may be more creative, while others may be more irritable. nine0014
- A person may feel so good that he denies that he is experiencing a state of hypomania.
- Talk quickly and smoothly.
- Accelerated thoughts.
- Agitation.
- Light condition. nine0014
- Impulsive and risky behavior.
- Excessive cash expenses
- Hypersexuality.
- A person with mania may also experience lack of sleep and inadequate judgment.
- On the other hand, maniacs may have problems with alcohol or other substance abuse.
- Bipolar I disorder - includes periods of depression and mania
- Bipolar type 2 disorder - characterized by depression in some cases and hypomania (not as pronounced as mania).
- high spirits
- excess energy
- anger and irritation
- reduced need for sleep
- talkativeness
- excessive self-confidence.
- high spirits
- excess energy
- reduced need for sleep nine0013 creative inspiration.
- depressed mood
- alarm
- feelings of emptiness and longing
- reduced appetite
- trouble concentrating
- increased fatigue.
- hyperactivity
- impulsivity
- anger
- problems with concentration.
Although childhood onset occurs, the normal age of onset for type 1 is 18 years and for type 2 is 22 years.
About 10% of bipolar 2 cases develop into type 1.
Although the causes are unclear, genetic and environmental factors (stress, childhood abuse) play a role.
Treatment usually includes psychotherapy, medication, sometimes electroconvulsive therapy may be helpful.
Symptoms
Signs and symptoms of the depressive phase of bipolar disorder include:
Manic symptoms
Mania can occur in varying degrees:
Hypomania
This is the least severe degree of mania and lasts at least 4 days. This does not result in a noticeable decrease in a person's ability to work, communicate, or adapt.
He also does not require hospitalization and does not have psychotic characteristics. nine0005
nine0005
In fact, overall functioning may improve during a hypomanic episode and is considered a natural anti-depression mechanism.
If an event of hypomania is not accompanied by or precedes depressive episodes, it is not considered a problem if the state of mind is uncontrollable.
Symptoms may last from several weeks to several months.
It is characterized by:
Mania
Mania is a period of euphoria and high mood for at least 7 days. If left untreated, a manic episode can last 3 to 6 months.
It is characterized by displaying three or more of the following behaviors:
In extreme cases, they may experience psychosis, so that contact with reality is broken, having a high state of mind.
It is common for a manic person to feel incomparable or indestructible and to feel chosen to realize a goal. nine0005
Approximately 50% of people with bipolar disorder experience hallucinations or delusions, which can lead to violent behavior or admission to a psychiatric hospital.
Mixed episodes
In bipolar disorder, a mixed episode is a condition in which mania and depression occur simultaneously.
People who experience this condition may have thoughts of grandiosity while having depressive symptoms such as suicidal thoughts or feelings of guilt. nine0005
People who are in this state are at high risk of committing suicide because they confuse depressive emotions with mood swings or difficulty controlling impulsivity.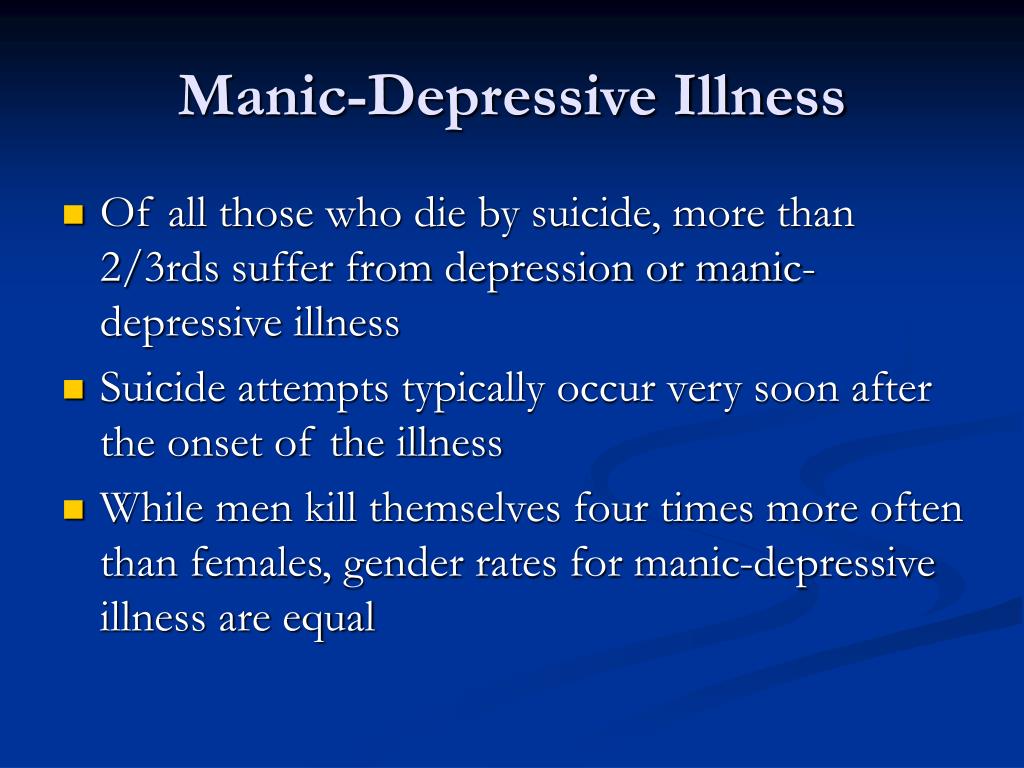
Causes
The exact causes of bipolar disorder are unclear, although they are thought to be largely genetic and environmental.
Genetic factors
It is believed that 60-70% of the risk of developing bipolarity depends on genetic factors. nine0005
Several studies have shown that certain genes and chromosomal regions are associated with susceptibility to develop the disorder, with each gene being more or less important.
The risk of bipolar disorder in people with family members with the same diagnosis is 10 times higher than in the general population.
Studies indicate heterogeneity, meaning that different genes are involved in different families.
Environmental factors
Research shows that environmental factors play an important role in the development of bipolar disorder, and psychosocial variables may interact with genetic dispositions. nine0005
Recent life events and interpersonal relationships contribute to manic and depressive episodes.
30-50% of adults diagnosed with bipolar disorder have been found to report abuse or trauma in childhood, which is associated with an earlier onset of the disorder and more suicide attempts.
Evolutionary factors
From evolutionary theory, one might think that the negative effects that bipolar disorder can have on adaptability cause genes not to be selected by natural selection. nine0005
However, there is still a high incidence of BD in many populations, so there may be some evolutionary benefit.
Doctors of evolutionary medicine suggest that high rates of BR throughout history suggest that the change between depressive and manic states suggested some evolutionary advantage in ancestral humans.
In highly stressed individuals, depressed mood can serve as a defense strategy to escape external stress, store energy, and increase sleep hours. nine0005
Mania could benefit from her relationship with creativity, confidence, high energy levels and greater productivity.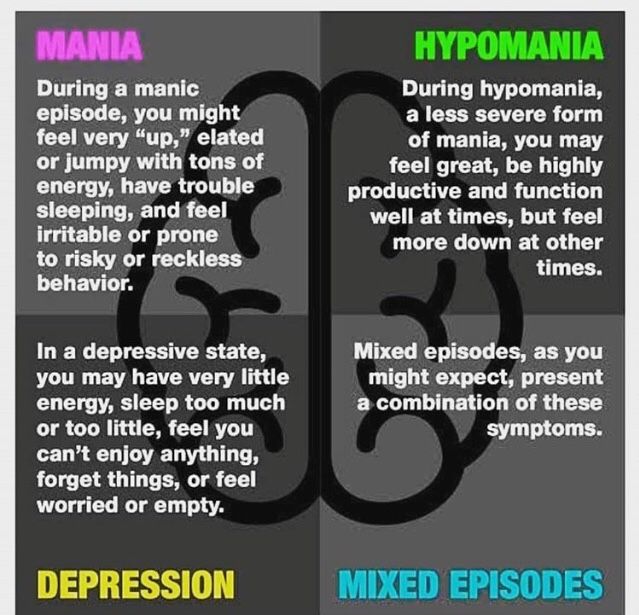
Physiological, neurological and neuroendocrine factors
Brain imaging studies have shown differences in the volume of various brain areas between patients with bipolar disorder and healthy patients.
An increase in the volume of the lateral ventricles and an increase in the rate of white matter hyperintensity were found. nine0005
Magnetic resonance studies have shown that there is an abnormal modulation between the abdominal prefrontal region and the limbic regions, especially the amygdala. This will contribute to poor emotional regulation and mood-related symptoms.
On the other hand, there is evidence of an association between early stressful experiences and dysfunction of the hypothalamic-pituitary-adrenal axis, leading to hyperactivation.
Less common bipolar disorder can result from trauma or a neurological condition: brain injury, stroke, HIV, multiple sclerosis, porphyria, and temporal lobe epilepsy. nine0005
The neurotransmitter responsible for regulating mood, dopamine, has been found to increase its transmission during the manic phase and decrease during the depressive phase.
Glutamate increases in the left dorsolateral prefrontal cortex during the manic phase.
Diagnosis
A patient must have at least two episodes of affective disorder to be diagnosed with bipolar disorder. At the same time, at least one of them must be either manic or mixed. For the correct diagnosis, the psychiatrist must take into account the characteristics of the patient's history, information received from his relatives. Currently, it is believed that the symptoms of bipolar disorder are characteristic of 1% of people, and in 30% of them the disease becomes a severe psychotic form. Determination of the severity of depression is carried out using special scales. The manic phase of bipolar disorder must be differentiated from arousal caused by the use of psychoactive substances, lack of sleep, or other causes, and the depressive phase from psychogenic depression. Psychopathy, neurosis, schizophrenia, as well as affective disorders and other psychoses due to somatic or nervous diseases should be excluded. nine0005
nine0005
Methods of treatment
The main goal of the treatment of bipolar disorder is to normalize the mental state and mood of the patient, to achieve long-term remission. In severe cases of the disease, patients are hospitalized in the psychiatric department. Mild forms of the disorder can be treated on an outpatient basis. Antidepressants are used to relieve a depressive episode. The choice of a specific drug, its dosage and frequency of administration in each case is determined by a psychiatrist, taking into account the age of the patient, the severity of depression, and the possibility of its transition to mania. If necessary, the appointment of antidepressants is supplemented with mood stabilizers or antipsychotics. Antidepressants help to stop depressive states in bipolar disorder. Drug treatment of bipolar disorder in the stage of mania is carried out by normotimics, and in severe cases of the disease, antipsychotics are additionally prescribed. In the stage of remission, psychotherapy (group, family and individual) is shown. nine0005
nine0005
Bipolar disorder - Appotek
Bipolar disorder is characterized by periods of depression and mania or hypomania. Between episodes, a person often has no symptoms at all and can work as usual. The disease can cause psychological distress, but with the right treatment, symptoms can be alleviated—often with a combination of medication, psychotherapy, and education.
General
Symptoms of bipolar disorder often first appear during adolescence, but are sometimes difficult to detect early on because these symptoms may initially be mistaken for some other mental illness. nine0241
There are two types of bipolar disorder. Type 1 was also formerly known as manic depressive disorder
Cyclothymia . This is a condition that causes milder episodes of hypomania and depression. Cyclothymia sometimes develops into bipolar disorder. nine0005
This is a condition that causes milder episodes of hypomania and depression. Cyclothymia sometimes develops into bipolar disorder. nine0005
Symptoms
Bipolar disorder is characterized by recurrent depressive episodes alternating with episodes of mania or hypomania. Mania means, among other things, a sustained elation with euphoria or irritability. Patients tend to ignore inhibitions, behave inappropriately, or even offend others without even realizing it. Hypomania has much in common with mania, but the mood is not as high and the person can function normally. Symptoms can vary from person to person and over time. Mood swings can be fast and strong, and often difficult, not only for the person experiencing them, but also for those around them. Sometimes depressive and manic symptoms can occur at the same time; these are so-called "mixed episodes", with rapid changes between depressive and manic stages within one day. Some only have manic episodes, but these cases are less common. Intermediate periods without depression, mania, or hypomania are called "euthymia." Depressive and manic periods can last for weeks or months. In some people, depression can last for several years and be either clinical depression or melancholic depression. nine0005
Intermediate periods without depression, mania, or hypomania are called "euthymia." Depressive and manic periods can last for weeks or months. In some people, depression can last for several years and be either clinical depression or melancholic depression. nine0005
Examples of manic symptoms:
Examples of hypomanic symptoms:
Examples of depressive symptoms:
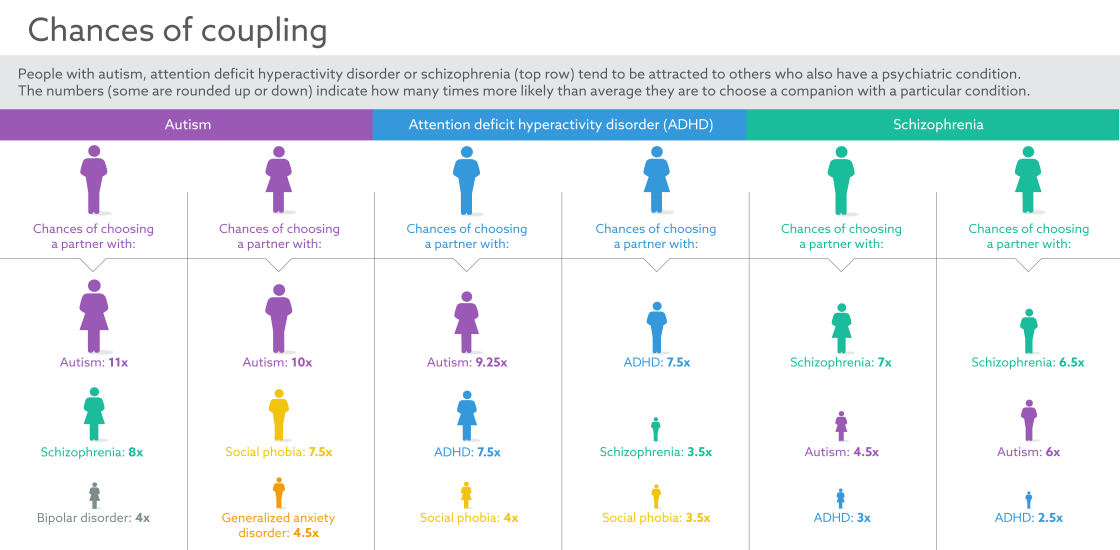
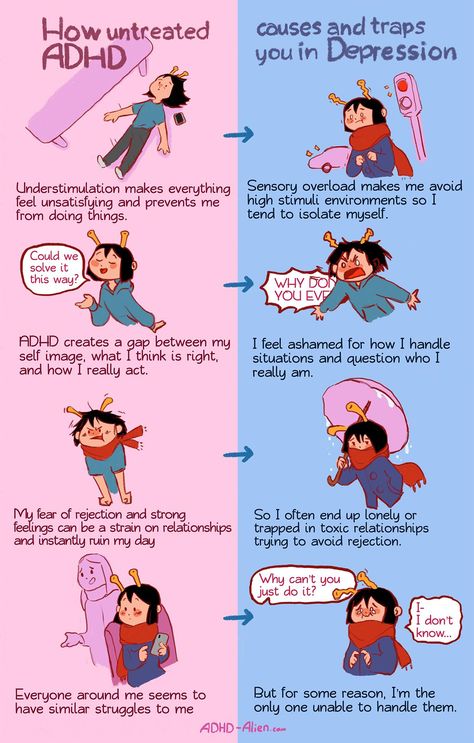
Bipolar disorder can also coexist with other conditions such as various types of anxiety disorders, ADHD and alcohol abuse. nine0005
nine0005
Causes
The word "bipolar" refers to the two states (poles) of mania and depression. In bipolar disorder, heredity plays a big role. Certain factors, such as illness, life events, stress, and sleep problems, can also cause bipolar disorder. Occasionally, hypomania or mania may occur during treatment for depression.
Bipolar disorder in children
Bipolar disorder is rare in children but common in adolescents. Heredity is often a factor contributing to the development of the disease. It can sometimes be difficult to distinguish the symptoms of bipolar disorder from other mental illnesses such as depression. But it is important that the child gets help as soon as possible. nine0005
Children with bipolar disorder may show various symptoms such as:
These symptoms are common, but children with bipolar disorder suffer more often than their peers.
Treatment often includes a medical and psychological-pedagogical approach, including information and strategies to deal with the disease. nine0005
Treatment
Bipolar disorder can cause serious psychological consequences for both patients and their families, as well as potentially serious social and economic costs. Therefore, it is important that the disease be treated, preferably at an early stage, in order to alleviate the problem.
Bipolar disorder is often treated with a combination of medication, psychotherapy, and education. Medications are used to stabilize mood swings and prevent relapses. Cognitive behavioral therapy (CBT) is a form of psychotherapy that can also be used in treatment. Education focuses on learning to recognize and manage relapse symptoms. nine0005
Prevention and protection
If you have already been diagnosed with bipolar disorder, you must actively participate in your treatment. Avoid things that previously triggered episodes and try to learn to recognize the signs of mania, hypomania, or depression.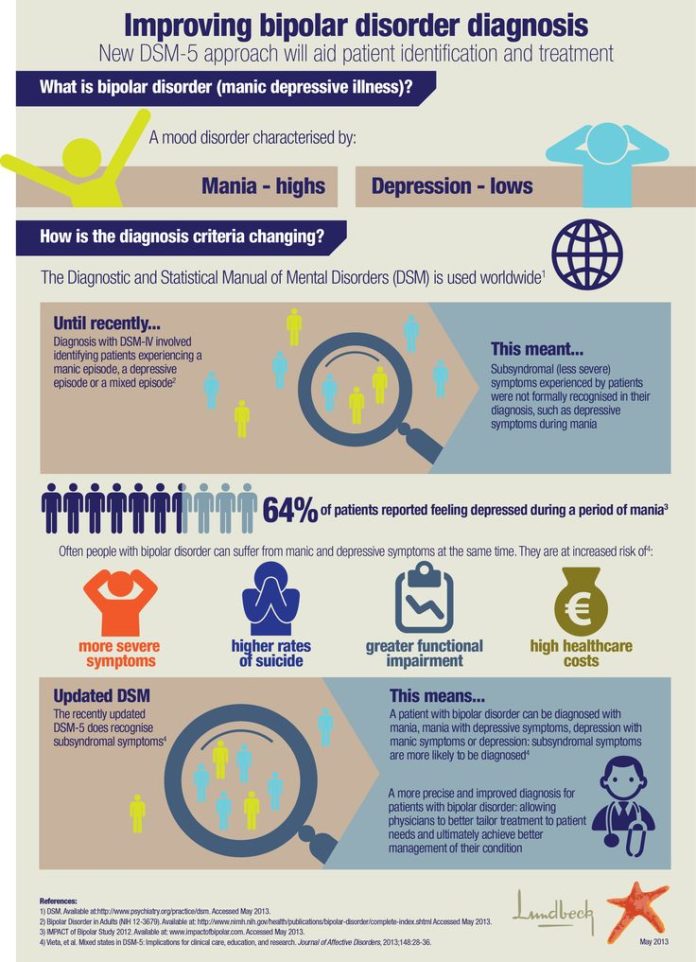 Regular contact with psychiatrists makes it easier to detect early signs of new episodes. Remember to take your medicines on time, control your sleep and be physically active. You should also avoid stress, alcohol and smoking. If you feel unwell and want to stop taking your medication, it is important to discuss this with your doctor rather than adjusting your dosage yourself. For family members and relatives, family therapy can help beat this disorder. There are also various associations that can provide support. nine0005
Regular contact with psychiatrists makes it easier to detect early signs of new episodes. Remember to take your medicines on time, control your sleep and be physically active. You should also avoid stress, alcohol and smoking. If you feel unwell and want to stop taking your medication, it is important to discuss this with your doctor rather than adjusting your dosage yourself. For family members and relatives, family therapy can help beat this disorder. There are also various associations that can provide support. nine0005
When to seek help
If you suspect that you have bipolar disorder, you should seek medical help - see a doctor or mental health clinic. This should also be done if you have severe mood swings that affect your social and daily life.
If you have suicidal thoughts, seek emergency help. Relatives who are concerned that a person wants to commit suicide should also call an ambulance immediately. nine0005
How APPOTEK can help you
If you suspect you have bipolar disorder or have already been diagnosed, you should contact a psychiatric clinic.