Unipolar depression symptoms
SAMHSA’s National Helpline | SAMHSA
Solr Mobile Search
Share Buttons
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs.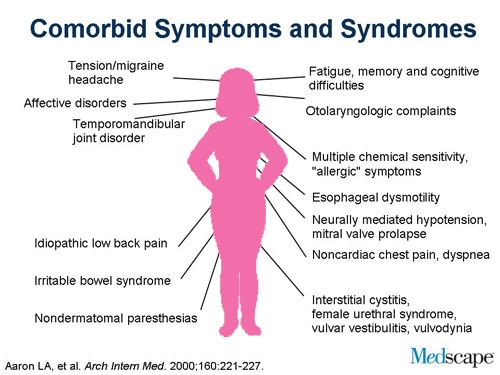 In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems.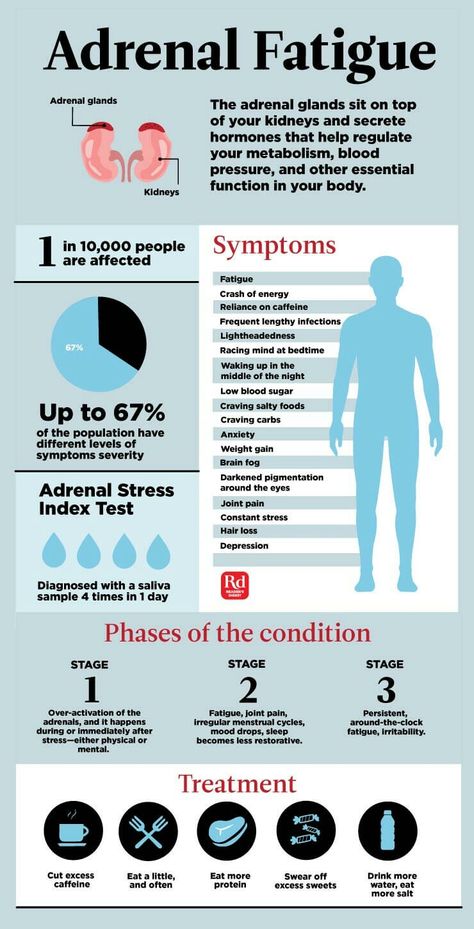 Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.For additional resources, please visit the SAMHSA Store.
Last Updated
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Solr Mobile Search
Share Buttons
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers. The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
- Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.
 4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH) - The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk.
 They Hear You.
They Hear You. - Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
- Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses.
 The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States - The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month. The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
- Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.
 4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH) - Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medications for Substance Use Disorders
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated
Last Updated: 03/22/2023
Unipolar depression - diagnosis, treatment
Unipolar depression is a type of endogenous depressive disorder that occurs in bipolar disorder without manic phases. Characterized by a chronic course with periodic exacerbations lasting several months and light intervals, averaging 3-7 years. In an unfavorable variant, the duration of the episodes increases or the symptoms persist permanently. The diagnosis is established taking into account the data of the anamnesis, conversation and special tests. Medical treatment.
Medical treatment.
Contact our operator by phone 8(969)060-93-93 and choose a convenient time for a consultation.
General information
Depression is a large and varied group of conditions that present with similar symptoms: depression of mood, slowing of thinking and motor retardation. May be independent diseases or be observed as part of other mental pathologies. An example of the second option is unipolar depression in bipolar affective disorder.
In classic BAD, depression alternates with mania. In atypical, depressive symptoms occur intermittently, but there are no manic episodes. This type of disease is more often detected in women, it can develop primarily. Sometimes the typical form of bipolar disorder transforms into a unipolar form with age.
Along with involutional melancholia, the unipolar form is one of the endogenous depressions - pathologies caused by neurochemical rather than psycho-emotional factors, that is, genetic predisposition and hormonal changes in the aging process.
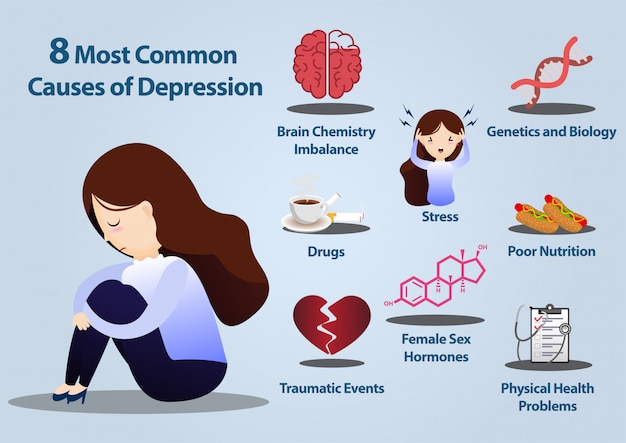
Causes
Causes have not been reliably established, however, researchers point to the polyetiological nature of the disease, the importance of both internal and external factors that are combined with each other. A more significant role is played by endogenous factors - a hereditary predisposition due to the transfer of one or more genes. The disease is more often diagnosed in people with the following personality types:
- Melancholy. Differs in increased emotional sensitivity with rapid fatigue and external restrained manifestation of experiences.
- Schizoid. Feelings are somewhat monotonous, rationalization is the leading defense, people do not like excess communication, they prefer solitude.
- Statothymic. Patients are responsible, pedantic, have a high need for ordering the phenomena of the external world, their own actions and experiences.
Suspiciousness, anxiety and emotional lability are considered predisposing features. Information regarding the sexual distribution is contradictory, but there are indications that monopolar forms are more often found in the fairer sex. The risk of pathology in women increases during periods of endocrine changes - after childbirth and during menopause.
Information regarding the sexual distribution is contradictory, but there are indications that monopolar forms are more often found in the fairer sex. The risk of pathology in women increases during periods of endocrine changes - after childbirth and during menopause.
The average age of bipolar onset is 25–44 years, while the unipolar form often develops after 35–40 years. In every fifth case, the first episode occurs after 50 years of age. The duration of one episode ranges from 1-2 weeks to 1-2 years, more often it is several months. In most cases, then there is a light interval lasting from 3 to 7 years. It is impossible to accurately predict the duration of the phases and the number of exacerbations.
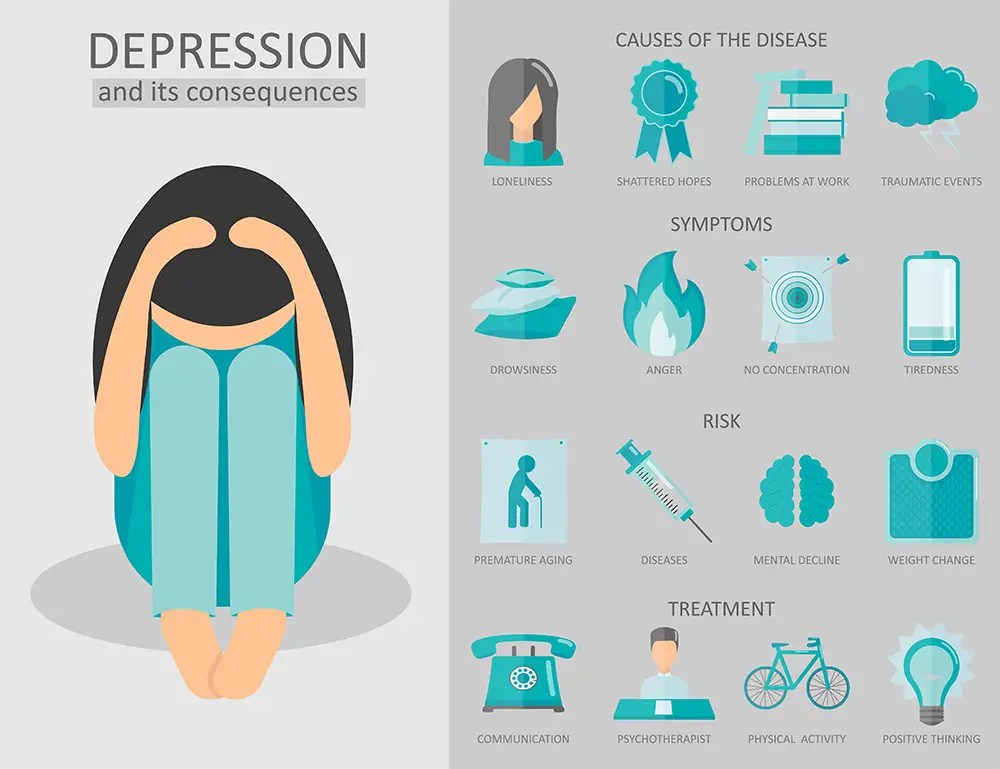
Symptoms
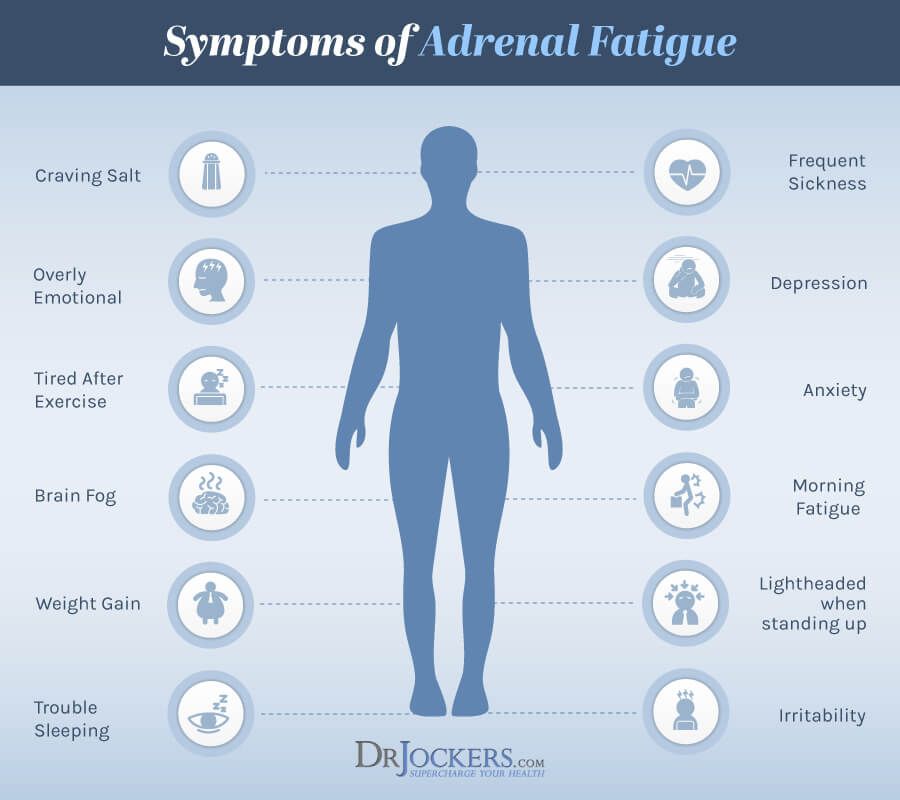
In the simple type, a characteristic triad is formed: steady deterioration in mood, slowing down of movements and mental activity. Loss of appetite and weight loss. Violations in the sexual sphere are revealed: irregularity of menstruation, disappearance of sexual desire. A characteristic feature is diurnal mood changes, worsening in the morning and improving in the evening.
A characteristic feature is diurnal mood changes, worsening in the morning and improving in the evening.
Along with the simple type, the following types of unipolar depression are possible:
- Hypochondriacal. Worries about a non-existent serious illness come to the fore. The patient's conviction reaches the level of delirium or an overvalued idea. The disease may seem shameful or very rare, unknown to specialists and therefore not amenable to diagnosis.
- Agitated. A two-phase flow is observed. The phase of despondency is represented by apathy, melancholy and depression. People spend long hours without moving. Then comes the phase of anxiety, accompanied by motor excitement, crying, attempts to escape. At the peak, raptus can form - a violent emotional explosion with throwing, screaming, suicidal attempts.
- Anesthetic. Painful insensibility predominates. The absence of emotions is perceived as a severe unbearable loss.
 Patients say that they have a "hole inside" in place of previous feelings, and this gives them unbearable suffering.
Patients say that they have a "hole inside" in place of previous feelings, and this gives them unbearable suffering.
The delusional unipolar form is especially difficult. Auditory hallucinations appear. Voices convince the patient of the insignificance and necessity of suicide. The theme of delusions is always self-incriminating, pessimistic, derogatory, possible motives include the belief in one's own economic or physical insolvency, committing an unforgivable act, worthlessness, guilt.
Cotard's syndrome may develop, accompanied by derealization, depersonalization and negativistic hypochondriacal delusions. A conviction is found in the presence of an incurable disease, transformation into a corpse, rotting of internal organs, lack of need for water and food. Sometimes people consider themselves the greatest villains, talk about the coming universal catastrophe and the death of civilization. Due to pronounced suicidal tendencies, patients pose a threat to themselves.
Diagnostics
The nature of the pathology is determined by a psychiatrist. Diagnosis requires at least two affective episodes. Along with this, anamnestic data, features of the clinical picture, a possible connection with endocrine changes and other circumstances are taken into account. The severity of unipolar depression is assessed using special tests and scales.
Differential diagnosis with other types of depressive disorder. In the presence of anxiety, the distinction with the GAD is relevant. With delusional and hallucinatory symptoms, schizophrenia and organic mental disorders that have arisen against the background of somatic or neurological diseases are required to be excluded.
Treatment
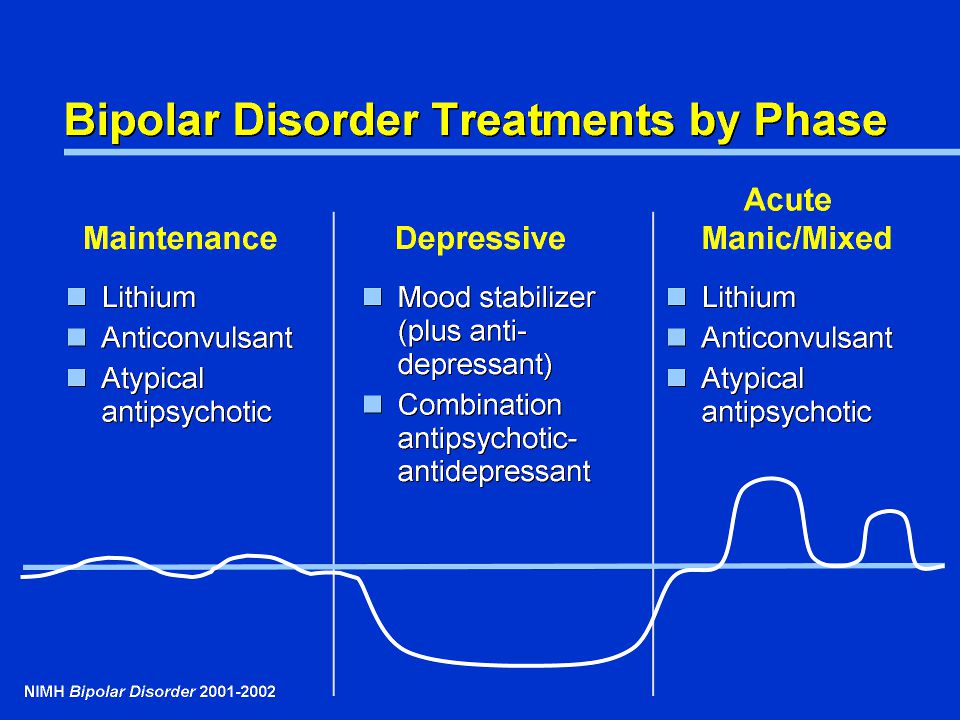
Psychotic symptoms, suicidal thoughts and actions require hospitalization in a psychiatric ward. Patients with mild forms are observed on an outpatient basis. The main role is given to drug treatment.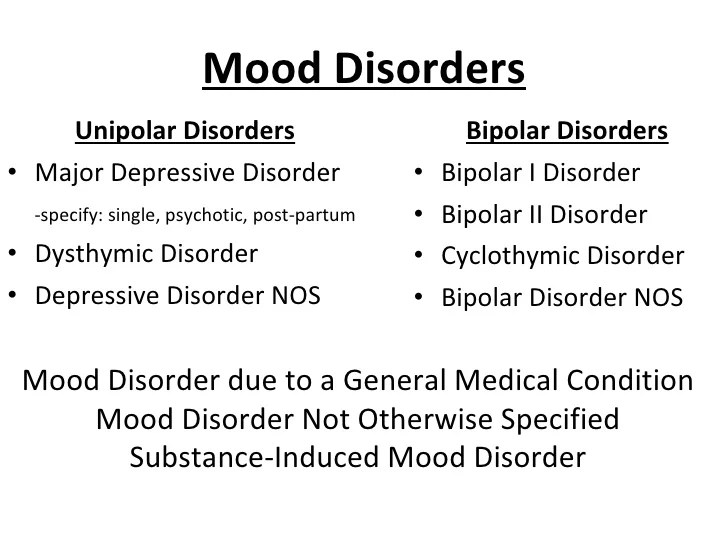 Antidepressants are used, sometimes in combination with mood stabilizers and anti-anxiety drugs. In psychosis, neuroleptics are used.
Antidepressants are used, sometimes in combination with mood stabilizers and anti-anxiety drugs. In psychosis, neuroleptics are used.
Psychotherapy is of secondary importance. It is carried out after relief of acute symptoms to eliminate internal conflicts, increase resistance to stressful situations. Patients are taught to recognize early signs of exacerbation for timely referral to a specialist.
The prognosis is relatively unfavorable. Outside of periods of exacerbation, emotional, cognitive and volitional qualities are not impaired, however, there is a high probability of developing repeated episodes, in which 35–50% of patients become disabled. Every third person has a continuous course of illness.
To make an appointment with the specialists of the Summer Center, just call tel. 8(969)060-93-93.
Types of depression - iFightDepression [EN]
There are different types of depression, which are different.
Signs and symptoms vary in number, time, severity and frequency, but are generally very similar. Because different types of depression are treated differently, it is important to pinpoint the type of depression. Depending on gender, age and cultural characteristics, people have different symptoms and severity of depression.
Neurotic, reactive (minor) depression is treated with psychotherapy.
Somatic and psychotic - medication. These terms are used by psychiatrists.
Studies have shown that depression has a phasic course. Periods of normal mood alternate with depressive episodes. Sometimes, instead of a depressive phase,
there may be a manic phase, which is manifested by irritability and high mood. If so, then it is not depression, but bipolar disorder (a more serious illness).
1. Depressive episode
The most common and typical form of depression is the depressive episode. An episode lasts from a few weeks to a year, but is always longer than 2 weeks.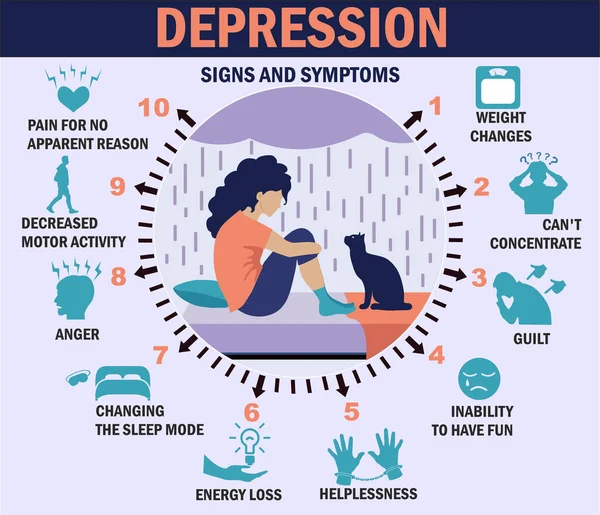 A single depressive episode is called a unipolar episode. Approximately one third of affected people experience only one episode, or "phase", during their lifetime. However, if a person does not receive appropriate treatment for depression, there is a risk of recurrent depressive episodes in the future. Depressive episodes always affect a person's performance to one degree or another.
A single depressive episode is called a unipolar episode. Approximately one third of affected people experience only one episode, or "phase", during their lifetime. However, if a person does not receive appropriate treatment for depression, there is a risk of recurrent depressive episodes in the future. Depressive episodes always affect a person's performance to one degree or another.
2. Intermittent (recurrent) depressive disorder
When a depressive episode recurs, it is recurrent depressive disorder or major depressive disorder, which usually begins in adolescence or early adulthood. With this kind of depression, depressive phases, which can last from several months to several years, alternate with phases of normal mood. This type of depressive disorder can seriously affect performance and is unipolar in nature (no manic or hypomanic phase). This is the so-called "classic" or "clinical" depression.
3. Dysthymia
Dysthymia presents with milder and less severe symptoms than a depressive episode or recurrent depression. However, the disorder is permanent, with symptoms lasting much longer, at least 2 years, sometimes decades, which is why it is called "chronic depression". This disorder is unipolar and also affects performance. This type of depression sometimes develops into a more severe form (major depressive episode) and if this happens it is called double depression.
However, the disorder is permanent, with symptoms lasting much longer, at least 2 years, sometimes decades, which is why it is called "chronic depression". This disorder is unipolar and also affects performance. This type of depression sometimes develops into a more severe form (major depressive episode) and if this happens it is called double depression.
4. Bipolar depression, type I
This is the type of depression in bipolar disorder, formerly called manic-depressive illness, and is less common than unipolar depression. It consists of alternating depressive phases, phases of normal mood and so-called manic phases.
Manic phases are characterized by excessively high mood associated with hyperactivity, anxiety, and decreased need for sleep.
Mania affects thinking, judgment and social behavior causing serious problems and difficulties. When a person is in a manic phase, he makes frequent casual unsafe sex, makes unwise financial decisions. After a manic episode, such people often experience depression.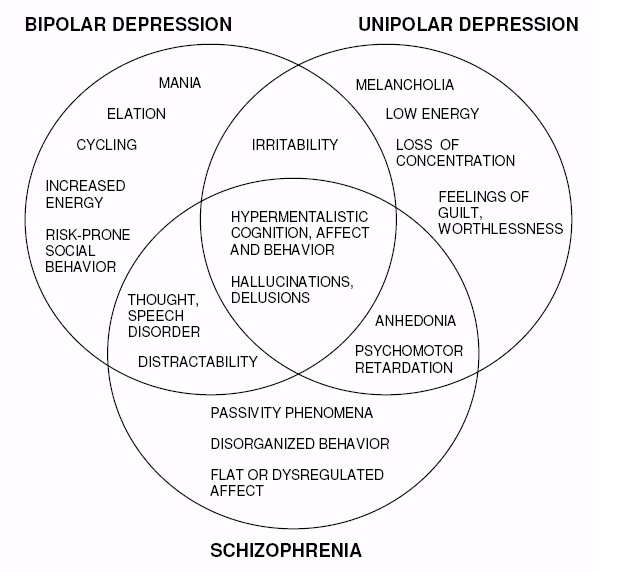
The best way to describe these "emotional upheavals" is "to be on top of the world and fall into the depths of despair".
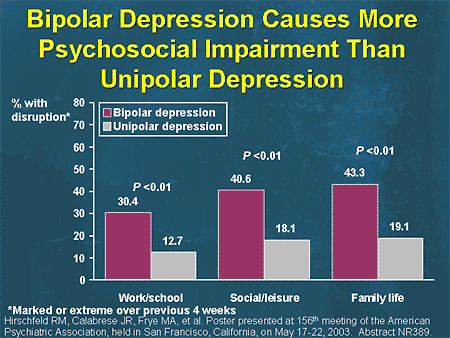
Symptoms of the phases of depression in bipolar disorder are sometimes difficult to distinguish from unipolar depression.
5. Bipolar depression type II
More like recurrent depressive disorder than bipolar disorder. In this disorder, multiple depressive phases alternate with phases of mania, but with less pronounced euphoria. During these phases, family and loved ones may even mistakenly assume that the person is doing well.
6. Mixed anxiety-depressive disorder
In anxiety-depressive disorder, the clinical picture is very similar to depression, however, in depression, depressive syndromes always come first. In this case, both anxious and depressive symptoms are evenly combined.
7. Depressive psychotic episode
A special form of depressive episode is psychotic or delusional depression.