Types of paranoid personality disorder
Paranoia - Better Health Channel
Actions for this page
Summary
Read the full fact sheet- Paranoia is the irrational and persistent feeling that people are ‘out to get you’.
- The three main types of paranoia include paranoid personality disorder, delusional (formerly paranoid) disorder and paranoid schizophrenia.
- Treatment aims to reduce paranoia and other symptoms and improve the person’s ability to function.
What is paranoia?
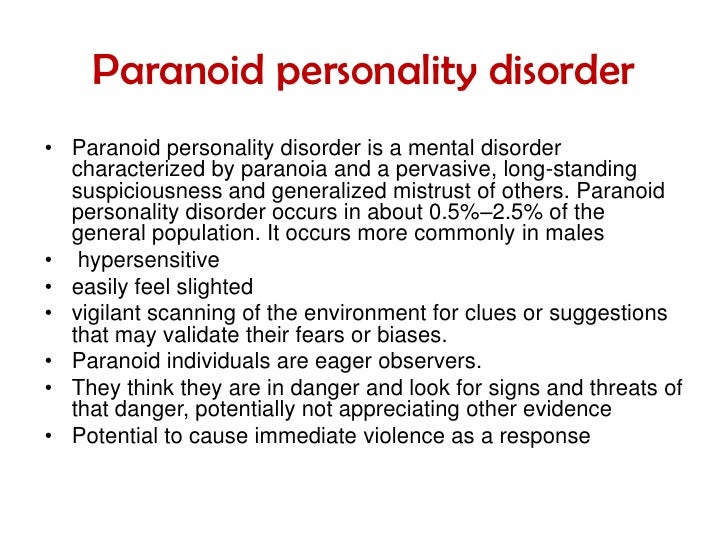
Paranoia is the irrational and persistent feeling that people are ‘out to get you’ or that you are the subject of persistent, intrusive attention by others. This unfounded mistrust of others can make it difficult for a person with paranoia to function socially or have close relationships. Paranoia may be a symptom of a number of conditions, including paranoid personality disorder, delusional (paranoid) disorder and schizophrenia.
The cause of paranoia is unknown but genetics are thought to play a role. Treatment depends on the condition diagnosed as its cause, and may include treatment by psychological therapy or medication.
Symptoms
Paranoid symptoms may range from mild to severe. They depend on the cause but, generally, a person who is paranoid may:
- be easily offended
- find it difficult to trust others
- not cope with any type of criticism
- assign harmful meanings to other people’s remarks
- be always on the defensive
- be hostile, aggressive and argumentative
- not be able to compromise
- find it difficult, if not impossible, to ‘forgive and forget’
- assume that people are talking ill of them behind their back
- be overly suspicious – for example, think that other people are lying or scheming to cheat them
- not be able to confide in anyone
- find relationships difficult
- consider the world to be a place of constant threat
- feel persecuted by the world at large
- believe in unfounded ‘conspiracy theories’.
Three main types of paranoia
Paranoia is associated with three principal conditions:
- Paranoid personality disorder – considered the mildest type. Most people with paranoid personality disorder function well despite their mistrust of the world. The attitudes and behaviours associated with this disorder, when they become obvious, are often discovered to have been present for much of the person’s life.
- Delusional (paranoid) disorder – characterised by the dominance of one delusion (false belief) without any other sign of mental illness. The person’s behaviour depends on which delusion they have. For example, a person who has a delusion of persecution believes that other people are spying on them or plotting to harm them in some way. Stalking can be the result of delusional (paranoid) disorder – for example, the person believes they are in a relationship with a movie star they have never met. In another case, a person may imagine they have a terrible illness, despite repeated reassurance from doctors.
- Paranoid schizophrenia – considered the most severe type. It is characterised by strange delusions, such as believing that one’s thoughts are being broadcast over the radio. Hallucinations, especially bizarre ones, are also common to the condition. A person with paranoid schizophrenia often finds the world confusing and functions poorly without treatment.
Causes are unclear
The causes of paranoia are unclear and depend on the condition with which it is associated. Theories include:
- Genes – research is scanty and inconclusive. Some studies suggest a genetic link while others don’t. It is also unclear whether genetic predisposition to paranoia – if it exists – is inherited or not.
- Brain chemistry – brain chemicals (neurotransmitters) form the basis of thoughts and feelings. Certain drugs such as cocaine, marijuana and amphetamines alter brain chemistry and can bring on paranoid thoughts, feelings and behaviours.
 This leads some researchers to believe that paranoia may be a biochemical disorder of the brain. The causes of this possible disorder are unknown.
This leads some researchers to believe that paranoia may be a biochemical disorder of the brain. The causes of this possible disorder are unknown. - Traumatic life events – for example, abuse in childhood may distort the way a person thinks and feels throughout life.
- Stress reaction – some studies have found that paranoia is more common in people who have experienced severe and ongoing stress – for example, prisoners of war. How stress can trigger paranoia is unclear.
- A combination of factors – it may be that a number of genetic and environmental factors working in combination cause paranoia.
Diagnosis
The condition causing the paranoia can be difficult to diagnose because an exaggerated sense of mistrust is common to a range of mental disorders and also occurs in some people with dementia. Another difficulty is that a person who has paranoia may avoid doctors, hospitals and other medical settings for fear of being harmed.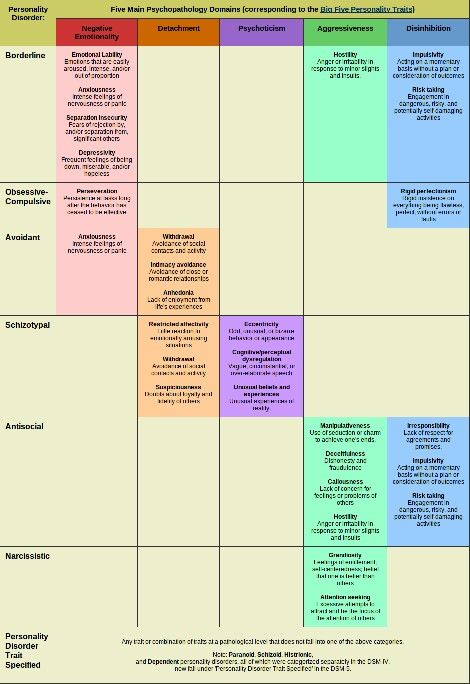
Diagnosis may include:
- medical history
- physical examination
- assessment of symptoms
- psychological tests
- tests to rule out other psychiatric disorders that may be causing the symptoms.
Treatment
While there is no absolute cure for the conditions that cause paranoia, treatment can help the person cope with their symptoms and live a happier, more productive life. Treatment depends on the type and severity of the condition but may include:
- Medications – anti-anxiety drugs or antipsychotic drugs can ease some of the symptoms. However, a person with paranoia may often refuse to take medication because they are afraid it will harm them.
- Therapy – this can help the person to cope with their symptoms and may improve their ability to function. However, a person with paranoia is unlikely to talk openly and freely to a therapist, so progress can be extremely slow.
- Coping skills – other treatments aim to improve the person’s ability to function socially.
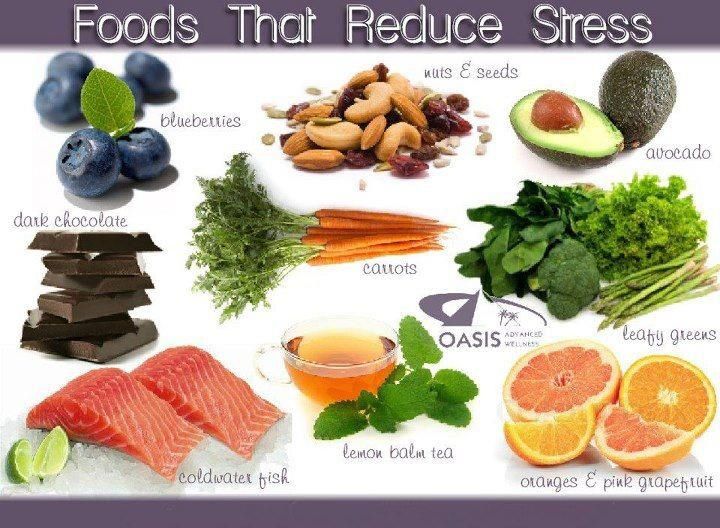
 Options may include relaxation therapy, techniques to reduce anxiety, and behaviour modification.
Options may include relaxation therapy, techniques to reduce anxiety, and behaviour modification. - Hospital admission – in severe cases, the person may need to stay in hospital until the condition causing paranoia stabilises.
Where to get help
- Your GP (doctor)
- Psychiatrist
- Public hospital
- Community health centre
- Mental Health Foundation of Australia (Victoria)Tel. 1300 643 287 (1300 MHF AUS)
- SANE HelplineTel. 1800 187 263
- Paranoia and delusional disorders, Mental Health America.
This page has been produced in consultation with and approved by:
This page has been produced in consultation with and approved by:
Give feedback about this page
Was this page helpful?
More information
Content disclaimer
Content on this website is provided for information purposes only. Information about a therapy, service, product or treatment does not in any way endorse or support such therapy, service, product or treatment and is not intended to replace advice from your doctor or other registered health professional. The information and materials contained on this website are not intended to constitute a comprehensive guide concerning all aspects of the therapy, product or treatment described on the website. All users are urged to always seek advice from a registered health care professional for diagnosis and answers to their medical questions and to ascertain whether the particular therapy, service, product or treatment described on the website is suitable in their circumstances. The State of Victoria and the Department of Health shall not bear any liability for reliance by any user on the materials contained on this website.
Information about a therapy, service, product or treatment does not in any way endorse or support such therapy, service, product or treatment and is not intended to replace advice from your doctor or other registered health professional. The information and materials contained on this website are not intended to constitute a comprehensive guide concerning all aspects of the therapy, product or treatment described on the website. All users are urged to always seek advice from a registered health care professional for diagnosis and answers to their medical questions and to ascertain whether the particular therapy, service, product or treatment described on the website is suitable in their circumstances. The State of Victoria and the Department of Health shall not bear any liability for reliance by any user on the materials contained on this website.
Reviewed on: 18-10-2022
Paranoid Personality Disorder (PPD): Symptoms & Treatment
Overview
What is paranoid personality disorder (PPD)?
Paranoid personality disorder (PPD) is a mental health condition marked by a long-term pattern of distrust and suspicion of others without adequate reason to be suspicious (paranoia). People with PPD often believe that others are trying to demean, harm or threaten them.
People with PPD often believe that others are trying to demean, harm or threaten them.
People with paranoid personality disorder often don’t think their behavior and way of thinking are problematic.
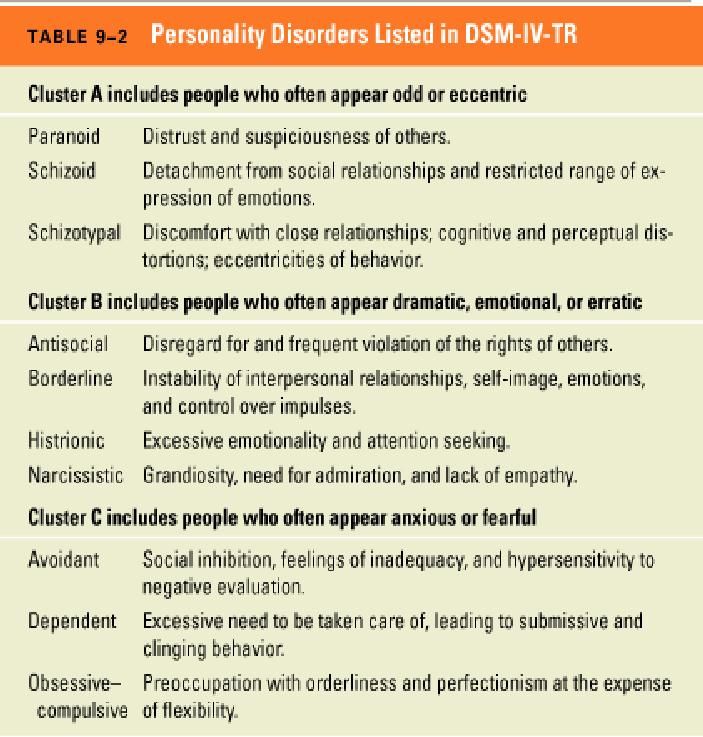
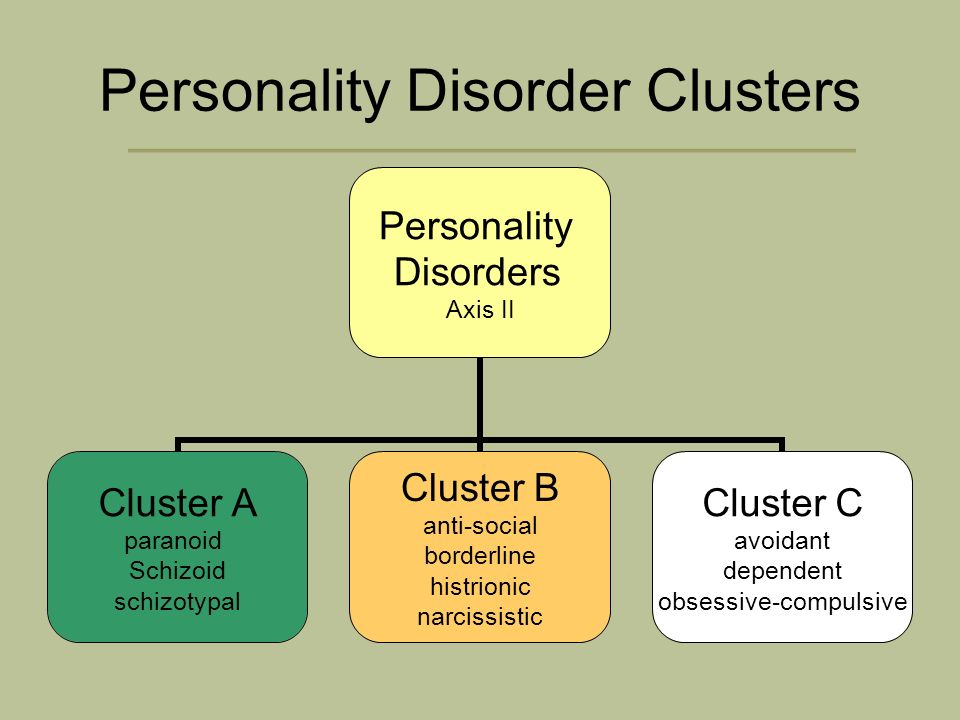
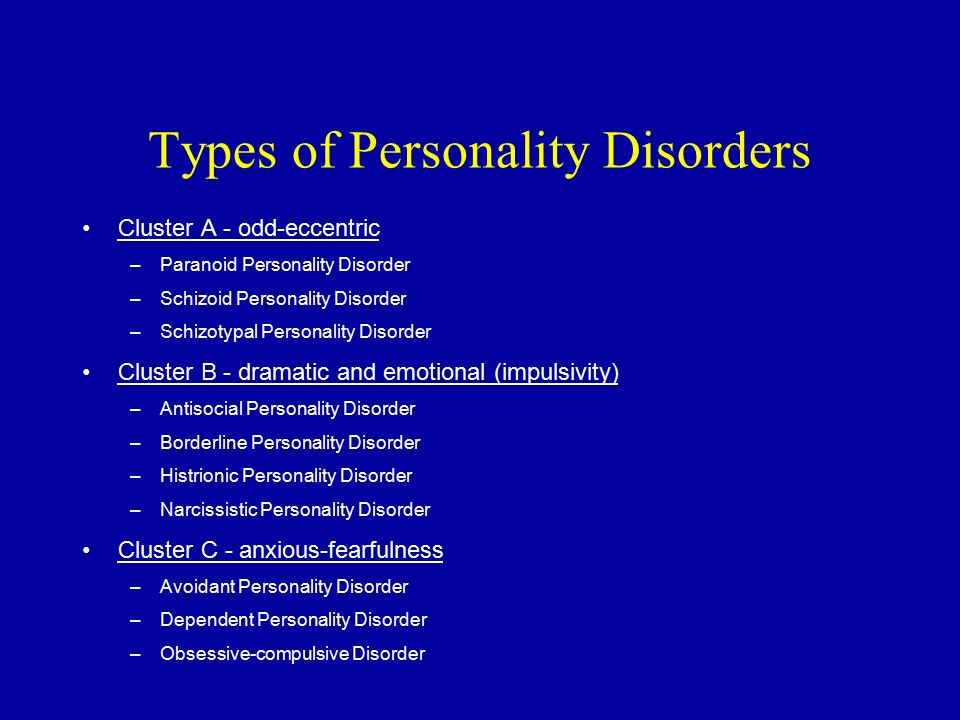
PPD is one of a group of conditions called Cluster A, or eccentric personality disorders. People with these disorders have unusual and eccentric thinking or behavior.
It’s important to note that people with paranoid personality disorder don’t experience delusions or hallucinations with paranoia, as commonly seen in schizophrenia, schizoaffective disorder and severe manic episodes in bipolar disorder.
What age does paranoid personality disorder begin?
People with paranoid personality disorder typically start experiencing symptoms and showing signs of the condition by their late teens or early adult years.
Who does paranoid personality disorder affect?
Overall, research reveals higher rates of paranoid personality disorder (PPD) in people assigned female at birth (AFAB), while samples from hospital records reveal higher rates of PPD in people assigned male at birth (AMAB).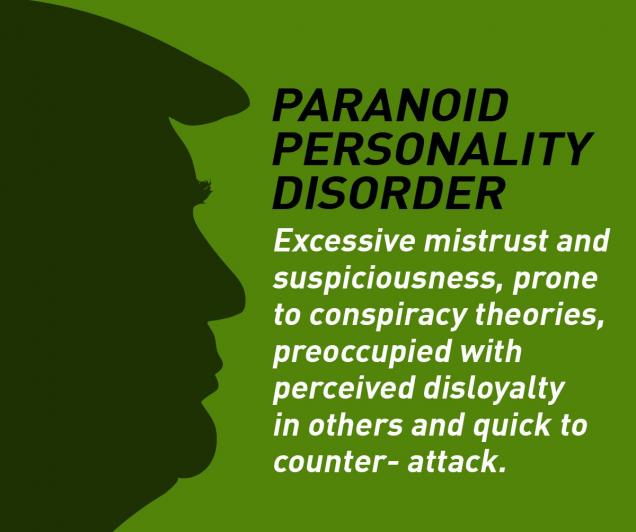
People with PPD are more likely to:
- Live in low-income households.
- Be Black, Native American or Hispanic.
- Be widowed, divorced or separated or never married.
More research is needed to learn more about why these risk factors are associated with PPD and how stress and trauma play a role in its development.
How common is paranoid personality disorder?
Paranoid personality disorder is relatively rare. Researchers estimate that it affects 0.5% to 4.5% of the general U.S. population.
Symptoms and Causes
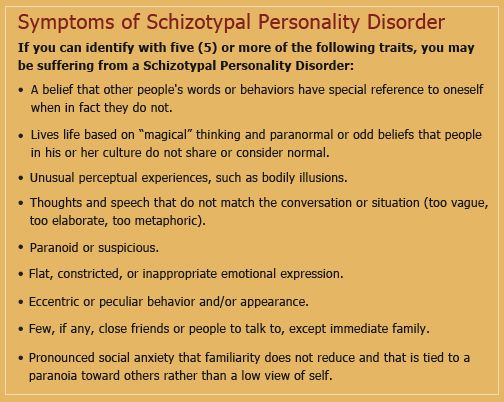
What are the signs and symptoms of paranoid personality disorder?
People with paranoid personality disorder (PPD) are always on guard, believing that others are constantly trying to demean, harm or threaten them. These generally unfounded beliefs, as well as their habits of blame and distrust, interfere with their ability to form close or even workable relationships. People with PPD severely limit their social lives.
People with PPD may:
- Doubt the commitment, loyalty or trustworthiness of others, believing others are exploiting or deceiving them.
- Be reluctant to confide in others or reveal personal information because they’re afraid the information will be used against them.
- Be unforgiving and hold grudges.
- Be hypersensitive and take criticism poorly.
- Read hidden meanings in the innocent remarks or casual looks of others.
- Perceive attacks on their character that aren’t apparent to others.
- Have persistent suspicions, without justified reason, that their spouses or romantic partners are being unfaithful.
- Be cold and distant in their relationships with others and might become controlling and jealous to avoid being betrayed.
- Not see their role in problems or conflicts, believing they’re always right.
- Have difficulty relaxing.
- Be hostile, stubborn and argumentative.
What causes paranoid personality disorder?
Scientists don’t know the exact cause of paranoid personality disorder (PPD), but it likely involves a combination of environmental and biological factors.
Researchers have found that childhood emotional neglect, physical neglect and supervision neglect play a significant role in the development of PPD in adolescence and early adulthood.
Researchers used to think there was likely a genetic link among schizophrenia, schizotypal personality disorder and PPD, but more studies have revealed that this connection isn’t as strong as they once thought.
Diagnosis and Tests
How is paranoid personality disorder diagnosed?
Personality continues to evolve throughout child and adolescent development. Because of this, healthcare providers don’t typically diagnose someone with paranoid personality disorder (PPD) until after the age of 18.
Personality disorders, including PPD, can be difficult to diagnose, as most people with a personality disorder don’t think there’s a problem with their behavior or way of thinking.
When they do seek help, it’s often related to conditions such as anxiety or depression due to the problems created by their personality disorder, such as divorce or lost relationships, not the disorder itself.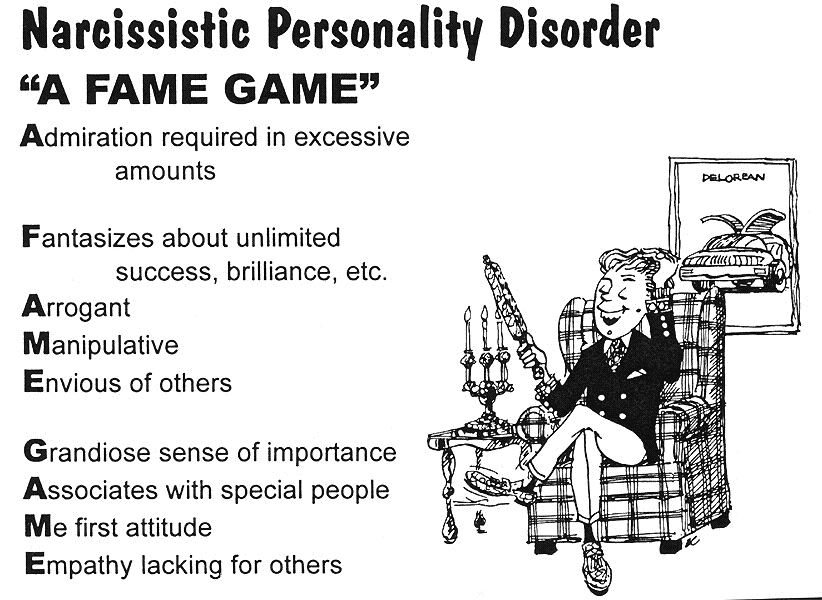
When a mental health professional, such as a psychologist or psychiatrist, suspects someone might have paranoid personality disorder, they often ask broad, general questions that won’t create a defensive response or hostile environment. They ask questions that will shed light on:
- Past history.
- Relationships.
- Previous work history.
- Reality testing.
- Impulse control.
Mental health providers base a diagnosis of paranoid personality disorder on the criteria for the condition in the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders.
Are other medical conditions associated with paranoid personality disorder?
Yes, approximately 75% of people with paranoid personality disorder (PPD) have another personality disorder. The most common personality disorders to co-occur with PPD include:
- Avoidant personality disorder.
- Borderline personality disorder (BPD).
- Antisocial personality disorder (ASPD).
People with PPD are also more likely to have substance use disorder and panic disorder than the general U.S. population.
Management and Treatment
How is paranoid personality disorder treated?
People with paranoid personality disorder (PPD) rarely seek treatment on their own. Family members, coworkers or employers usually refer them.
When someone with PPD does seek treatment, psychotherapy (talk therapy), such as cognitive behavioral therapy (CBT) or dialectical behavior therapy (DBT), is the treatment of choice. Therapy focuses on increasing general coping skills, especially trust and empathy, as well as on improving social interaction, communication and self-esteem.
As people with PPD often distrust others, it poses a challenge for healthcare professionals because trust and rapport-building are important factors of psychotherapy. As a result, many people with PPD may not follow their treatment plan and may even question the motives of the therapist.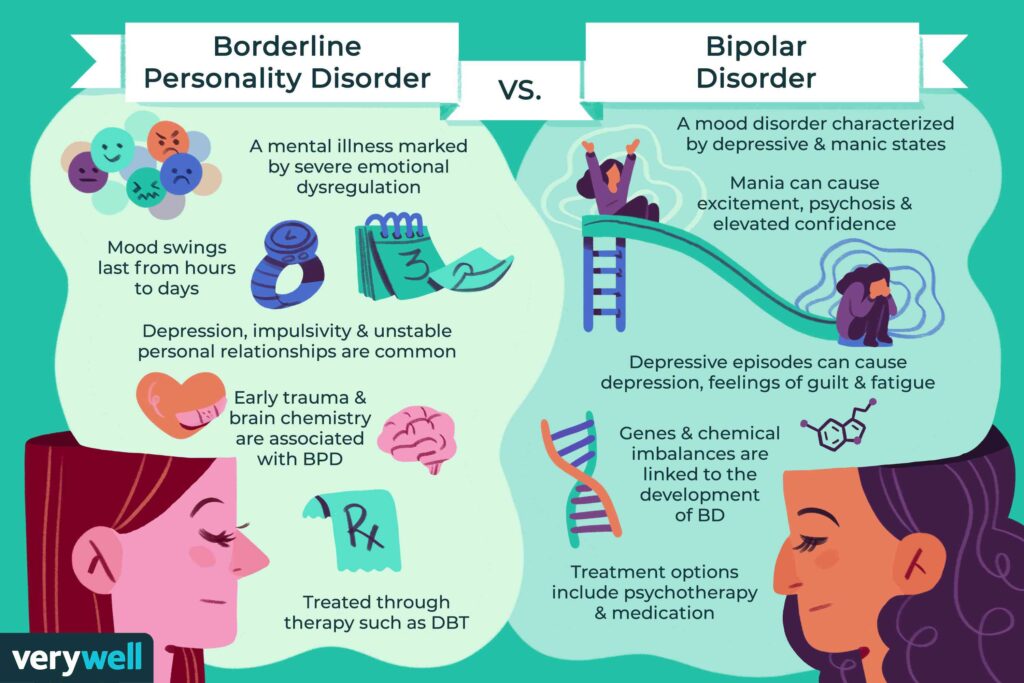
Healthcare providers generally don’t prescribe medication to treat PPD. However, medications — such as anti-anxiety, antidepressant or antipsychotic drugs — might be prescribed if the person’s symptoms are extreme or if they have an associated psychological condition, such as anxiety or depression.
Prevention
Can paranoid personality disorder be prevented?
While paranoid personality disorder generally can’t be prevented, treatment can allow someone with PPD to learn more productive ways of dealing with triggering thoughts and situations.
Outlook / Prognosis
What is the prognosis (outlook) for paranoid personality disorder?
The prognosis (outlook) for paranoid personality disorder (PPD) typically depends on whether someone with PPD is willing to accept and commit to treatment. Talk therapy can sometimes reduce paranoia and limit its impact on daily functioning.
Left untreated, PPD can interfere with a person’s ability to form and maintain relationships, as well as their ability to function socially and in work situations.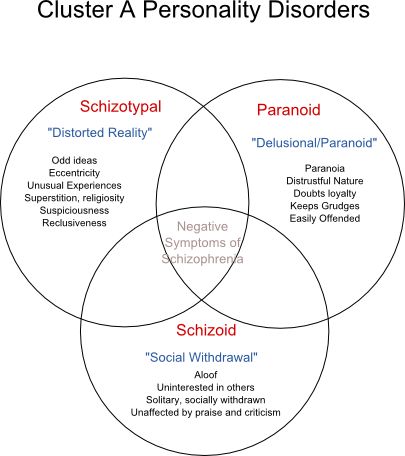 People with PPD are more likely to stop working earlier in their lives than people without personality disorders.
People with PPD are more likely to stop working earlier in their lives than people without personality disorders.
In addition, PPD is one of the strongest predictors of aggressive behavior in a hospital setting. PPD is also associated with stalking and excessive litigation (lawsuits).
A note from Cleveland Clinic
It’s important to remember that paranoid personality disorder (PPD) is a mental health condition. As with all mental health conditions, seeking help as soon as symptoms appear can help decrease disruptions to a person’s life. Mental health professionals can offer treatment plans that can help manage thoughts and behaviors of people with PPD.
Family members of people with paranoid personality disorder often experience stress, depression, grief and isolation. It’s important to take care of your mental health and seek support if you’re experiencing these symptoms.
FGBNU NTsPZ. ‹‹Borderline mental disorders››
Isolation of paranoid personality disorder, or paranoid type of psychopathy (the first name corresponds to ICD-10, the second - to the domestic classification), as an independent constitutional type is associated with the need to distinguish from constitutional anomalies of other types, as well as psychogenic and procedurally conditioned conditions.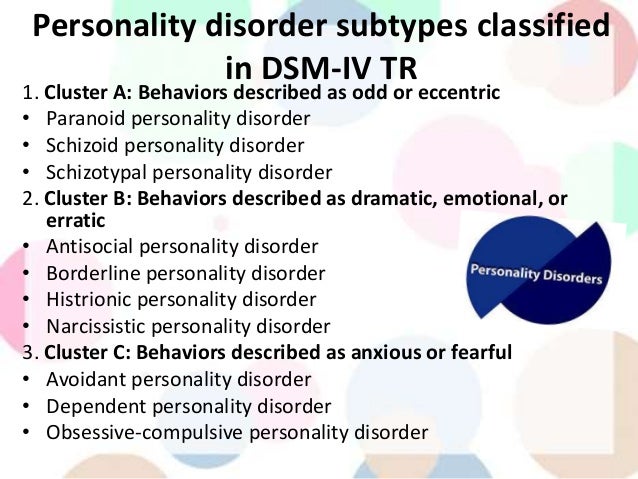 There are transitional states between paranoid psychopathy and other types of personality disorders (narcissistic, dissocial). Paranoid psychopathy is especially closely linked (as shown clinically and confirmed by psychometric studies by W. J. Livesley and M. L. Schneider (1990) with a group of schizoids of both the expansive and sensitive poles. Some authors [Gannushkin P. B., 1933; Molokhov A.N., 1934; Shostakovich B.V., 1971] share the point of view, according to which readiness for paranoid development and delusional formation can arise not only on the basis of a personal predisposition of the same name, but also on the basis of other constitutions. Difficulties in isolating the group of paranoid psychopathy are also due to the complexity of the clinical distinction between constitutional forms and delusional states of a different etiology. The absence of such a distinction or, conversely, the identification of paranoid psychopathy with paranoia and some other endogenously or psychogenically caused protracted delusional psychoses (as R.
There are transitional states between paranoid psychopathy and other types of personality disorders (narcissistic, dissocial). Paranoid psychopathy is especially closely linked (as shown clinically and confirmed by psychometric studies by W. J. Livesley and M. L. Schneider (1990) with a group of schizoids of both the expansive and sensitive poles. Some authors [Gannushkin P. B., 1933; Molokhov A.N., 1934; Shostakovich B.V., 1971] share the point of view, according to which readiness for paranoid development and delusional formation can arise not only on the basis of a personal predisposition of the same name, but also on the basis of other constitutions. Difficulties in isolating the group of paranoid psychopathy are also due to the complexity of the clinical distinction between constitutional forms and delusional states of a different etiology. The absence of such a distinction or, conversely, the identification of paranoid psychopathy with paranoia and some other endogenously or psychogenically caused protracted delusional psychoses (as R. Gaupp and some of his followers do) lead, according to T. I. Yudin, to the qualification of symptoms of an already pronounced disease , and not the features of the constitution, on the basis of which the disease develops.
Gaupp and some of his followers do) lead, according to T. I. Yudin, to the qualification of symptoms of an already pronounced disease , and not the features of the constitution, on the basis of which the disease develops.
Paranoid personalities are people of a special disposition, wayward, frank, devoid of a sense of humor, capricious, irritable, with one-sided but persistent affects that take precedence over logic and reason. They are characterized by increased activity, often combined with high spirits, excessive accuracy, conscientiousness and intolerance of injustice. As a rule, they are rigid, prone to "getting stuck", fixing on certain ideas and ideas, which is largely facilitated by the great emotional tension of experiences that are significant to them. They are distinguished by a narrow outlook, one-sidedness and limited interests. They do not set themselves big tasks, but objectively insignificant problems can obscure the whole world for them. Their judgments are immature, too straightforward, extremely specific, primitive and not always consistent.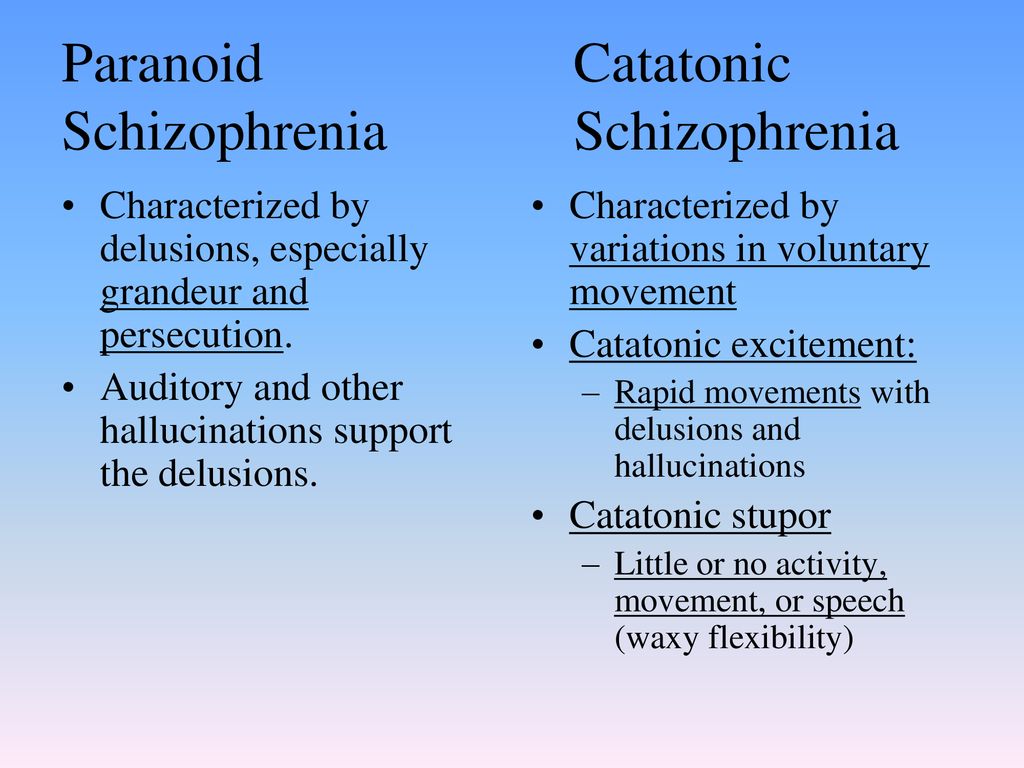 S. A. Sukhanov (1912), who referred such persons to the group of “logopaths”, emphasizes their characteristic tendency from their youthful years to reasoning and flaws in thinking in the form of an abundance of one-sided and logically incorrect (paralogical) conclusions.
S. A. Sukhanov (1912), who referred such persons to the group of “logopaths”, emphasizes their characteristic tendency from their youthful years to reasoning and flaws in thinking in the form of an abundance of one-sided and logically incorrect (paralogical) conclusions.
Paranoid psychopaths are distinguished by increased conceit, a heightened sense of self-worth, combined with "hypersensitivity" to failures, to a negative assessment from others. For the paranoid, everything that is somehow connected with his own personality and affects his interests acquires special meaning and significance. They are deeply indifferent to phenomena outside the sphere of "attraction" of their "I", simply excluding them from the field of active attention. “Everything that is not closely related to his “I” seems to the paranoid little worthy of attention” [Gannushkin P. B., 1964].
In this aspect, it is necessary to emphasize one more feature of the paranoid, hardly noticeable in everyday life, but distinctly acting in the conditions of a somatic hospital - egodistonism in relation to one's own bodily sphere.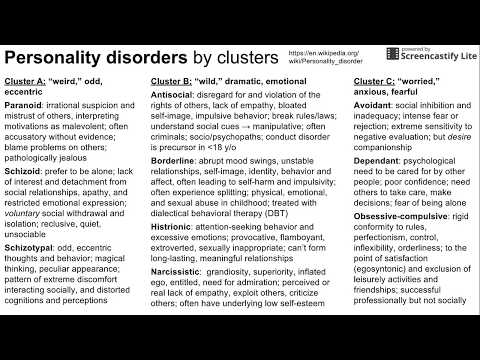 Psychopathic personalities of this circle are not only indifferent to a number of events in external life, but also to the problems of their somatic state. The news of a severe somatic illness often leaves them indifferent - it does not entail anxiety, fears of the detrimental consequences of the disease, fear of death, a decrease in mood that remains within the constitutionally characteristic hyperthymia. Such resistance to severe physical illness, defined in the psychoanalytically oriented literature by the term "resilience", is sometimes interpreted in a positive way as a well-developed ability to self-control. However, often a defect in bodily self-awareness is revealed by hypo- or even anosognosic reactions with inadequate, sometimes self-destructive behavior (neglect of medical recommendations, refusal to take medication, life-threatening exercises and physical activity).
Psychopathic personalities of this circle are not only indifferent to a number of events in external life, but also to the problems of their somatic state. The news of a severe somatic illness often leaves them indifferent - it does not entail anxiety, fears of the detrimental consequences of the disease, fear of death, a decrease in mood that remains within the constitutionally characteristic hyperthymia. Such resistance to severe physical illness, defined in the psychoanalytically oriented literature by the term "resilience", is sometimes interpreted in a positive way as a well-developed ability to self-control. However, often a defect in bodily self-awareness is revealed by hypo- or even anosognosic reactions with inadequate, sometimes self-destructive behavior (neglect of medical recommendations, refusal to take medication, life-threatening exercises and physical activity).
The constant opposition of oneself to others, the perception of the world as an opposite and even hostile phenomenon is manifested in paranoids by such features as “hyper vigilance” (constant search for a threat from the outside, readiness to respond to any alarm signal) and distrust of people.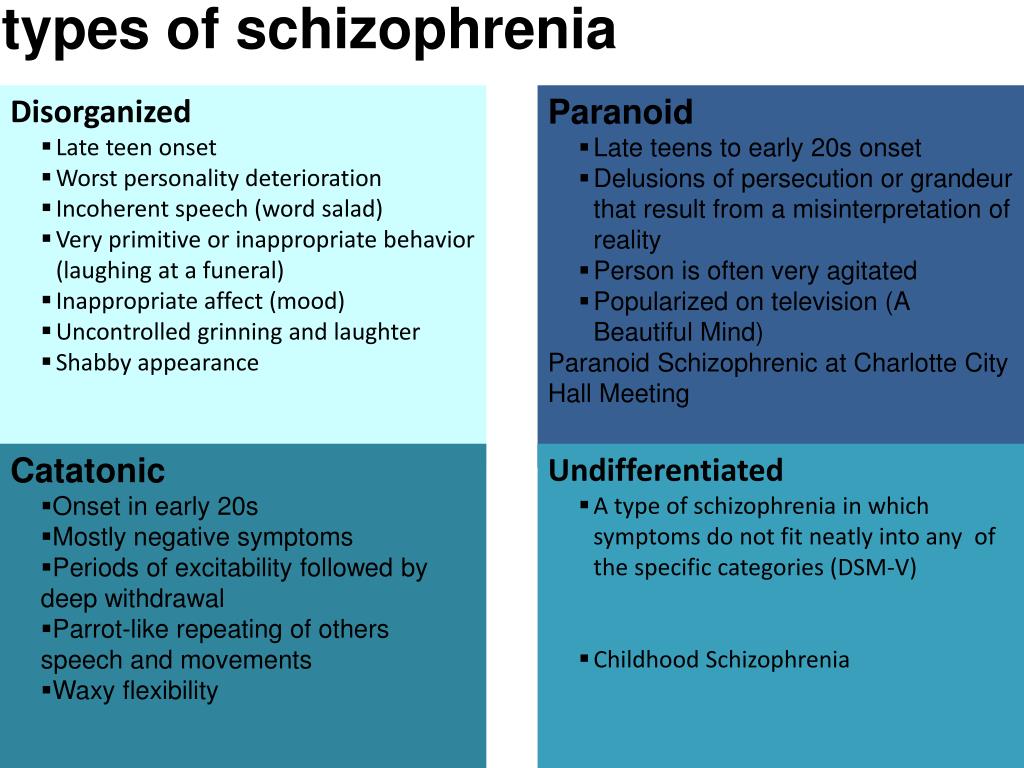 Often, the fear of infringement on their rights, their property, their spouse or sexual partner is at the forefront. Such distrust of the intentions of others easily turns into suspicion in paranoid individuals. There are thoughts that others treat them unfairly, without due respect, envy or even want to humiliate, insult; under them "undermining", infringe on their authority. An incorrect, one-sided interpretation of the words and actions of others leads the paranoid to unfounded and mostly devoid of even the slightest reason for suspicion. Any trifle that is not directly related to them can be interpreted as a manifestation of bad intentions, a negative (or even hostile) attitude of others (more often relatives and colleagues).
Often, the fear of infringement on their rights, their property, their spouse or sexual partner is at the forefront. Such distrust of the intentions of others easily turns into suspicion in paranoid individuals. There are thoughts that others treat them unfairly, without due respect, envy or even want to humiliate, insult; under them "undermining", infringe on their authority. An incorrect, one-sided interpretation of the words and actions of others leads the paranoid to unfounded and mostly devoid of even the slightest reason for suspicion. Any trifle that is not directly related to them can be interpreted as a manifestation of bad intentions, a negative (or even hostile) attitude of others (more often relatives and colleagues).
In many cases, starting from early adolescence, throughout the life of a paranoid personality, the described manifestations remain persistent and change little in intensity. However, in some abnormal personalities, the character traits do not essentially change, but give, according to the definition of S. A. Sukhanov (1912), "pathological growths" of one or another sign characteristic of this individual. According to J. Lange (1927), in such cases there is a biologically fixed readiness for a pathological response. The key to understanding such more pronounced mental anomalies lies in the clinical definition of paranoid psychopathy, which belongs to P. B. Gannushkin. The most typical, according to P. B. Gannushkin, property of paranoids is the tendency to form overvalued ideas, in the power of which they then find themselves. Overvalued ideas subordinate the whole personality to themselves, determine the behavior of the individual; it is not the paranoid person who controls his thoughts, but his thoughts control him.
A. Sukhanov (1912), "pathological growths" of one or another sign characteristic of this individual. According to J. Lange (1927), in such cases there is a biologically fixed readiness for a pathological response. The key to understanding such more pronounced mental anomalies lies in the clinical definition of paranoid psychopathy, which belongs to P. B. Gannushkin. The most typical, according to P. B. Gannushkin, property of paranoids is the tendency to form overvalued ideas, in the power of which they then find themselves. Overvalued ideas subordinate the whole personality to themselves, determine the behavior of the individual; it is not the paranoid person who controls his thoughts, but his thoughts control him.
Depending on the subject of overvalued ideas, several types of paranoid personalities are distinguished: jealous people, inventors, querulants, fanatics, etc. However, a systematics based only on the content of overvalued formations cannot reflect the structure of psychopathy as a whole.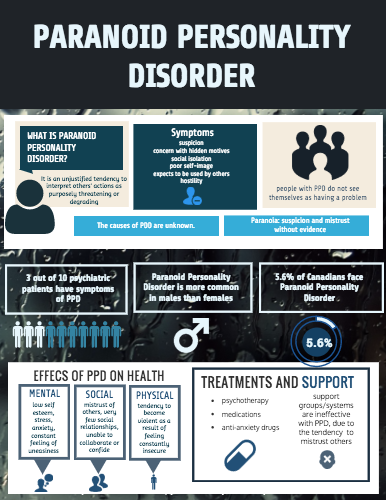
The foundations of the clinical typology of paranoid psychopathy were laid down in the works of O. Bumke (1924), T. I. Yudin (1926), E. Kretschmer (1930), N. Binder (1967). So far, this typology has not been completed, but it seems legitimate to single out (as separately as in the group of schizoids and psychasthenics) at least two polar variants of paranoid psychopathy: expansive and sensitive. Such differentiation to a certain extent coincides with the one proposed by S. Akhtars (1996) division of the paranoid constitution into 2 subtypes: 1) stronger, more active, defiant, angry, litigious; 2) weak, passive, secretive, touchy.
Expansive paranoid personalities are pathological jealous, quarrelsome, persons prone to conflicts, truth-seeking and reformism. From childhood, they are deceitful, vindictive, often slander and complain, notice shortcomings in others, but do not recognize them in themselves. As V.F. Chizh (1902) points out, they are always pleased with themselves, failures do not bother them.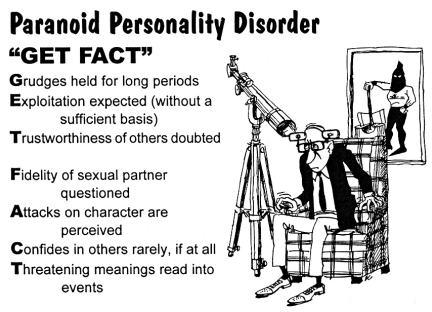 We are convinced that only they know this specialty, only they understand everything perfectly. They do not want to obey, limit themselves to a modest role, usually fight with their personal enemies, and not for a common cause. Having devoted themselves to scientific activity, they in essence do not like science, they are engaged in it only in order to shame their enemies. Fighting opponents and asserting their importance fill their lives. As a rule, these are sthenic and even exalted personalities with an accelerated pace of mental activity and a constantly elevated background of mood. They are energetic, mobile, sometimes fussy, do not know what fatigue is, do not feel the need for rest. A group of fanatics also belongs to expansive paranoid personalities [Schneider K., 1928; Gannushkin P. B., 1933]. Fanatics are people who, with exceptional passion, devote all their interests, activities, time, and, ultimately, their whole life to one cause, one idea. The strength of their obsession is such that they are able to captivate, at least temporarily, other people with their idea.
We are convinced that only they know this specialty, only they understand everything perfectly. They do not want to obey, limit themselves to a modest role, usually fight with their personal enemies, and not for a common cause. Having devoted themselves to scientific activity, they in essence do not like science, they are engaged in it only in order to shame their enemies. Fighting opponents and asserting their importance fill their lives. As a rule, these are sthenic and even exalted personalities with an accelerated pace of mental activity and a constantly elevated background of mood. They are energetic, mobile, sometimes fussy, do not know what fatigue is, do not feel the need for rest. A group of fanatics also belongs to expansive paranoid personalities [Schneider K., 1928; Gannushkin P. B., 1933]. Fanatics are people who, with exceptional passion, devote all their interests, activities, time, and, ultimately, their whole life to one cause, one idea. The strength of their obsession is such that they are able to captivate, at least temporarily, other people with their idea.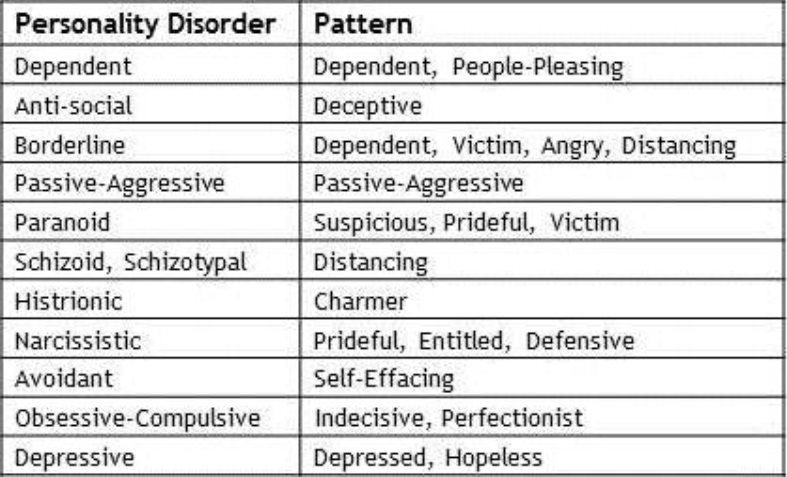 It must be emphasized that we are talking about blind faith (for example, religious fanaticism), which does not require a logical justification. Although fanatics, unlike other paranoid personalities, do not highlight themselves, they are far from true altruism, devoid of immediate love for their neighbor, soulless, and often cruel. When describing a group of fanatics, P. B. Gannushkin emphasizes that such cases are not always easy to distinguish from schizoids and "dreamers", there are many transitional forms between these groups of psychopathy. T. Bilikiewicz (1973) describes this type as a variant of schizoid psychopathy (paranoid schizoids). Such transitional types close to schizoids include, in particular, psychopathic personalities, defined by K. Schneider (1959) as sluggish fanatics. Sluggish fanatics, in contrast to expansive, actively striving to implement their program, are people prone to fantasizing, eccentric, turned away from reality. Their obsession with any idea is very close to autistic hobbies (collecting, vegetarianism) and is realized only in their personal lives.
It must be emphasized that we are talking about blind faith (for example, religious fanaticism), which does not require a logical justification. Although fanatics, unlike other paranoid personalities, do not highlight themselves, they are far from true altruism, devoid of immediate love for their neighbor, soulless, and often cruel. When describing a group of fanatics, P. B. Gannushkin emphasizes that such cases are not always easy to distinguish from schizoids and "dreamers", there are many transitional forms between these groups of psychopathy. T. Bilikiewicz (1973) describes this type as a variant of schizoid psychopathy (paranoid schizoids). Such transitional types close to schizoids include, in particular, psychopathic personalities, defined by K. Schneider (1959) as sluggish fanatics. Sluggish fanatics, in contrast to expansive, actively striving to implement their program, are people prone to fantasizing, eccentric, turned away from reality. Their obsession with any idea is very close to autistic hobbies (collecting, vegetarianism) and is realized only in their personal lives.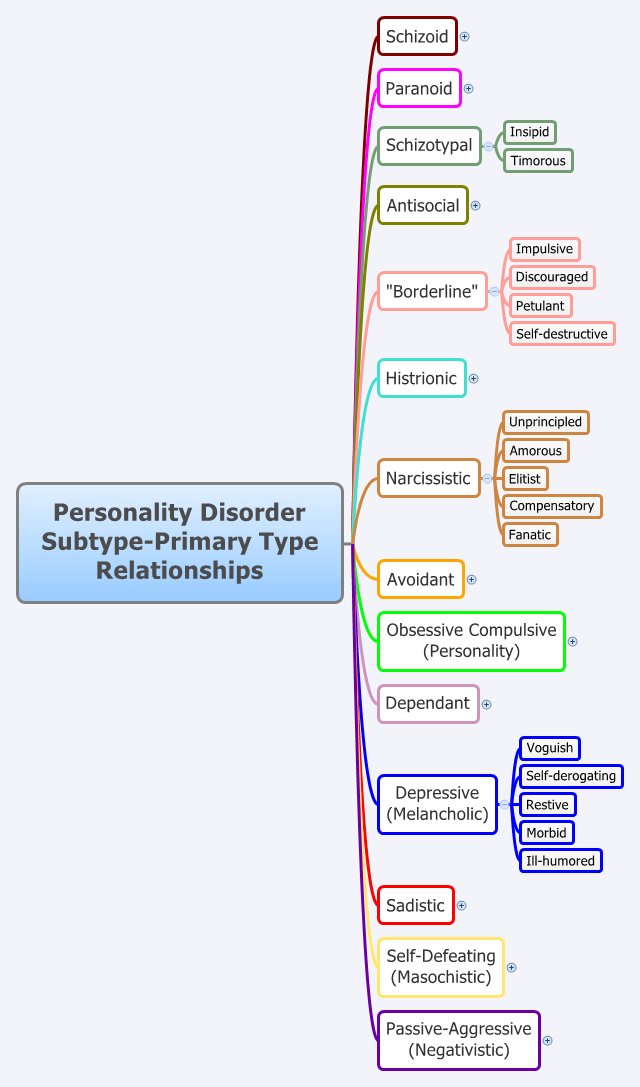 They do not fight to spread their ideas, they do not look for supporters and followers.
They do not fight to spread their ideas, they do not look for supporters and followers.
The description of the paranoid psychopathy of the sensitive pole belongs to E. Kretschmer (1930). A. E. Lichko (1985) distinguishes these rather rare personality anomalies into an independent - sensitive type of psychopathy. According to the personality structure, sensitive paranoids during the period of compensation show similarities with certain variants of sensitive schizoids [Yudin T.I., 1926].
A characteristic feature of the sensitive variant of paranoid psychopathy is a combination of contrasting personality traits: asthenic, sensitive (consciousness of one's own inferiority, vulnerability, false modesty) and sthenic (ambition, increased self-esteem). Sensitive paranoids are no less characterized by an insufficient ability for mental, affective discharge (conduction disturbance, according to E. Kretschmer), leading to stagnation of affect. These people are timid, shy, timid and at the same time suspicious and irritable, prone to introspection, self-criticism and even self-torture. They are distinguished by a heightened sense of inadequacy, humiliating for them, in relation to the standards (professional, worldly, etc.) that they have set for themselves. As E. Kretschmer writes (1930), “the content of their spiritual life is characterized by complexes of shameful ethical insufficiency.” Their most essential property is the deep and long sensitive reactions that arise in connection with certain ethical conflicts. These reactions were defined by E. Kretschmer as an attitude neurosis - a sense of the relationship of everything to oneself, based on internal complexes of insufficiency. Conflicts of conscience or feelings of inferiority, which have certain and typical starting points, lead to sensitive experiences. These can be not only the sexual complexes described by E. Kretschmer (for example, masturbation, carefully concealed and suppressed love of old maids), but also various .. service failures (delayed promotion, etc.), family grievances. The whole surrounding world during this period seems to the sensitive paranoid person to be colored by the traces of that affect, which in reality only he suffers from.
They are distinguished by a heightened sense of inadequacy, humiliating for them, in relation to the standards (professional, worldly, etc.) that they have set for themselves. As E. Kretschmer writes (1930), “the content of their spiritual life is characterized by complexes of shameful ethical insufficiency.” Their most essential property is the deep and long sensitive reactions that arise in connection with certain ethical conflicts. These reactions were defined by E. Kretschmer as an attitude neurosis - a sense of the relationship of everything to oneself, based on internal complexes of insufficiency. Conflicts of conscience or feelings of inferiority, which have certain and typical starting points, lead to sensitive experiences. These can be not only the sexual complexes described by E. Kretschmer (for example, masturbation, carefully concealed and suppressed love of old maids), but also various .. service failures (delayed promotion, etc.), family grievances. The whole surrounding world during this period seems to the sensitive paranoid person to be colored by the traces of that affect, which in reality only he suffers from.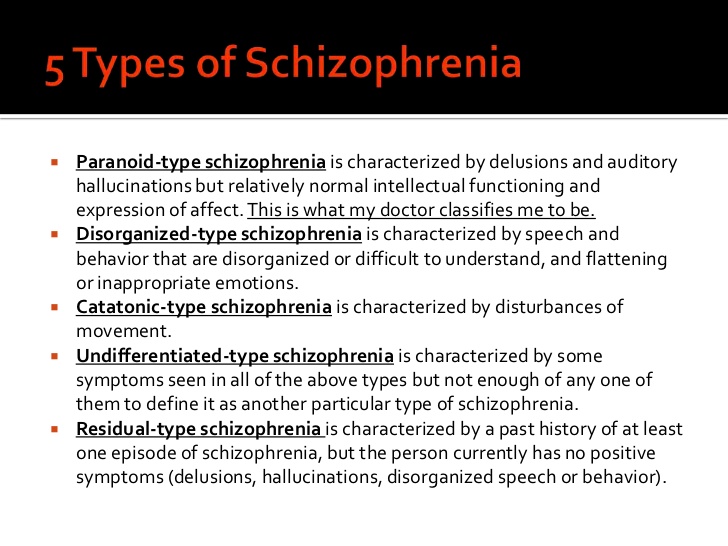 He gets the impression that his shame should become public, that everyone knows about his painful experiences.
He gets the impression that his shame should become public, that everyone knows about his painful experiences.
Types of personality disorders and features of their treatment. Paranoid, schizoid, dissocial, hysterical disorder, obsessive-compulsive, obsessive-compulsive, anxious, narcissistic
The main feature of personality disorders are pronounced maladaptive features of the psyche - such patients do not know how and cannot get along with others, adapt to new conditions. Previously, personality disorders were called psychopathy, but over time, experts adopted a Western point of view - psychopathy is still a separate mental disorder. There are several types of personality disorders, sometimes there are mixed types of the disease. Treatment should only be carried out by experienced professionals, but the main problem with this disorder is that patients for the most part do not recognize their mental problems.
Submit an application for diagnosis and treatment
I confirm that I accept the terms of consent to the processing of personal data.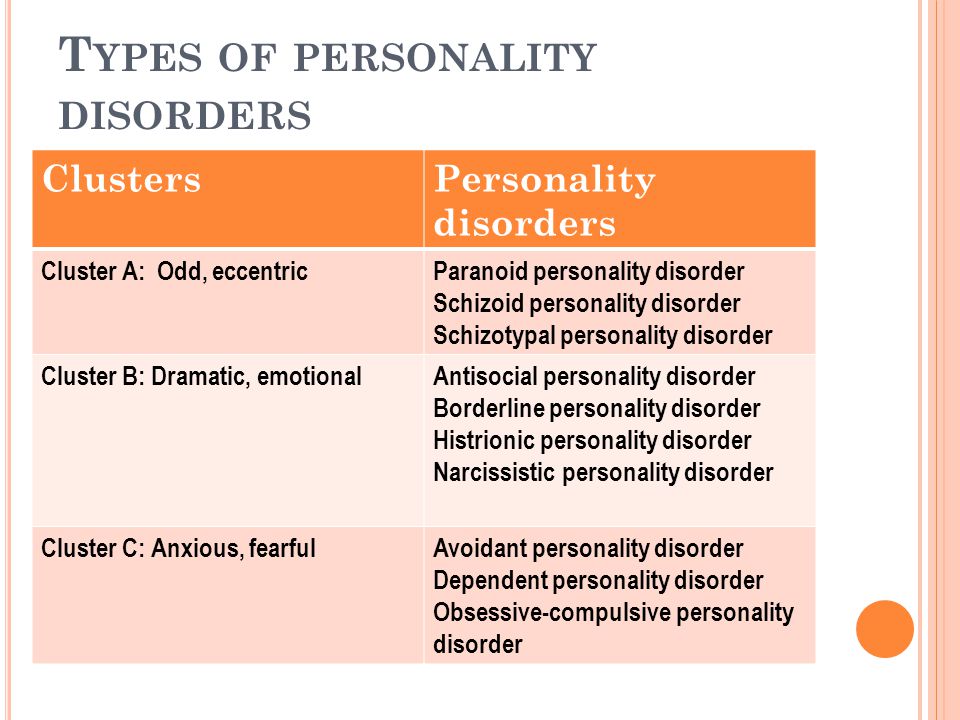
Types of personality disorders and features of their treatment
Every fifteenth inhabitant of our planet suffers from a personality disorder. Moreover, he himself hardly perceives his condition as a disease that requires an appeal to specialists. He will justify all his actions and consider his behavior normal. Treatment denies, and the consequences are unpredictable.
Personality disorder: adjustment difficulties
Personality disorder is a maladaptive pattern of behavior caused by a persistent mental disorder that is not associated with a physical or neurological disease. This pathology is difficult to correct, because the patient does not believe that he needs treatment. There is no motivation, which is a catalyst for positive changes. The individual himself does not seek to get rid of the violation and does not make good contact with psychotherapists. Late appeal to specialists leads to the fact that the patient gets an appointment with a psychiatrist already in the stage of deep neglect of the disease.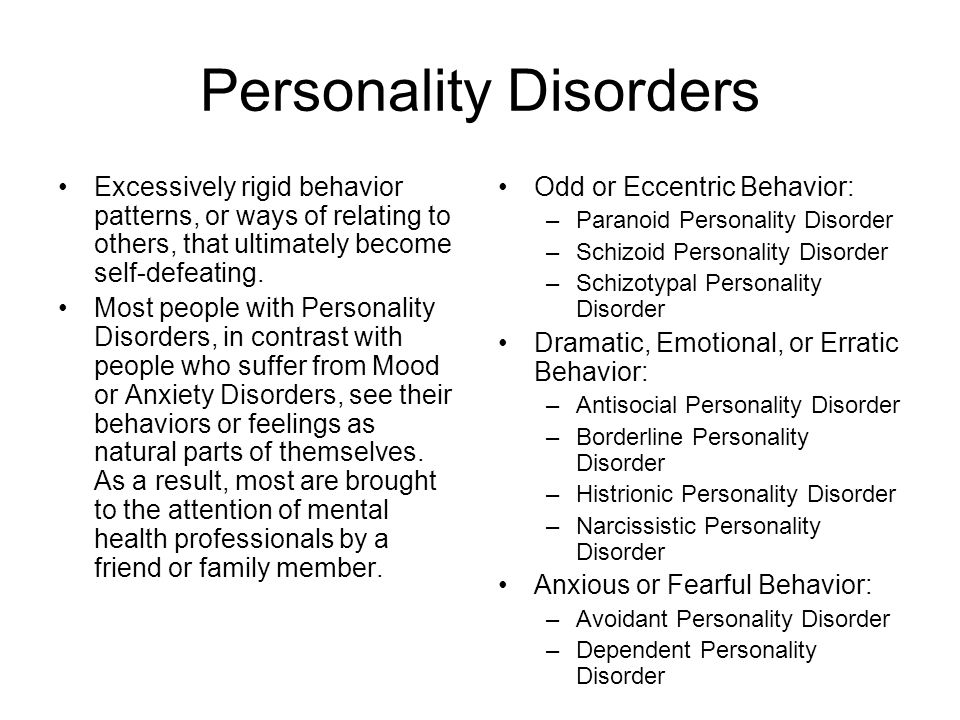 It can be difficult to relieve symptoms and cure. The first signs of the disease are actively manifested in adolescence. Before this period, individual episodes are possible, but only after the period of puberty can we talk about the problem. Individuals with cognitive personality disorder do not understand why others talk about any of their problems. After all, they believe that behavior and actions are normal. People with personality disorders are poorly perceived in society. They often have difficulties in personal communication. But at the same time, patients do not feel pangs of remorse and have no sympathy for others. After a certain time, their relationship with the world is built not according to the principle of personal adaptation to society, but according to the scheme, when the society is forced to accept or not accept a problematic person. The lack of motivation and desire to be treated exacerbates the problem, since not every doctor can find an approach to such a patient, relieve the symptoms of exacerbation and help get rid of the problem.
It can be difficult to relieve symptoms and cure. The first signs of the disease are actively manifested in adolescence. Before this period, individual episodes are possible, but only after the period of puberty can we talk about the problem. Individuals with cognitive personality disorder do not understand why others talk about any of their problems. After all, they believe that behavior and actions are normal. People with personality disorders are poorly perceived in society. They often have difficulties in personal communication. But at the same time, patients do not feel pangs of remorse and have no sympathy for others. After a certain time, their relationship with the world is built not according to the principle of personal adaptation to society, but according to the scheme, when the society is forced to accept or not accept a problematic person. The lack of motivation and desire to be treated exacerbates the problem, since not every doctor can find an approach to such a patient, relieve the symptoms of exacerbation and help get rid of the problem.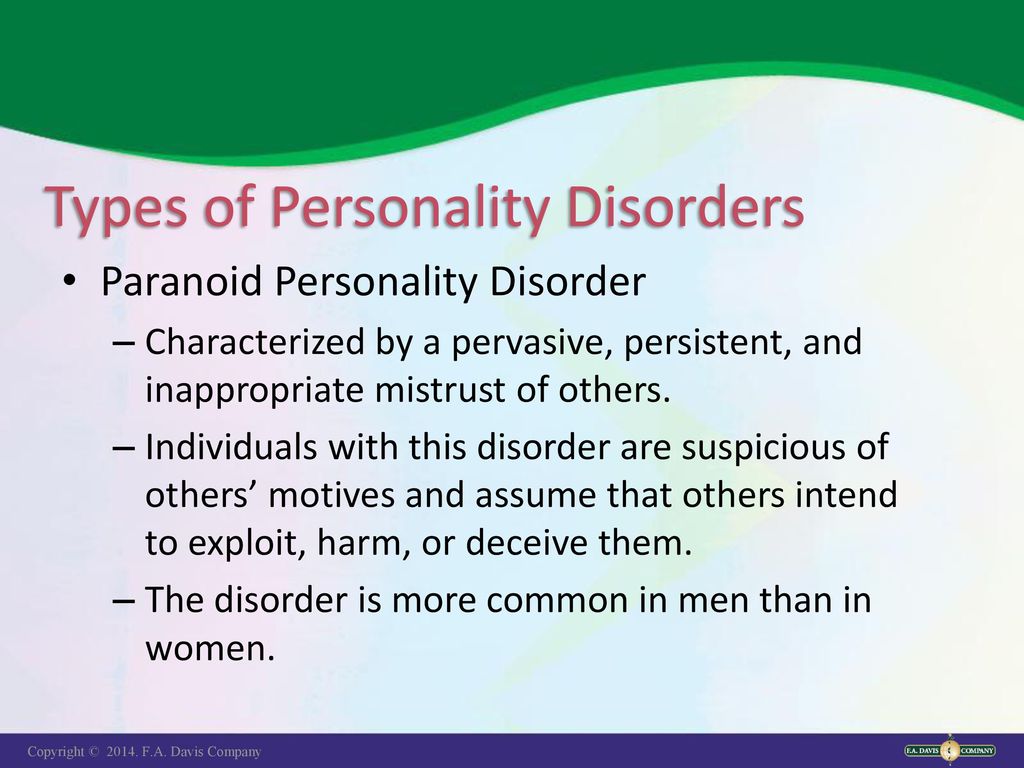
Specific personality disorders
In Soviet times, overly emotional individuals were often called psychopaths. Such a characterization and classification was not inherent in Western psychiatry. Psychopathy is a serious violation of a behavioral nature, in which, against the background of underdevelopment of a number of personality traits, one clearly dominates. This includes a number of deviations. Types of personality disorders:
- § Paranoid - the patient is dominated by overvalued ideas. He attaches special importance to his personality. But he treats others with hostility, suspecting them of malicious intent. A person with a pathology does not recognize its presence. When relatives or friends pay attention to a cognitive deviation and try to take him to a specialist, he will assure that everything is in order with him and deny the existence of a problem. Very sensitive to criticism.
- § Schizoid - this diagnosis is characterized by introversion, isolation, decreased interest in life's things.
 The patient does not perceive the accepted norms of social behavior, often behaves eccentrically. Schizoid personality disorders are associated with a great passion for some kind of activity in which the individual succeeds. For example, he may be pathologically addicted to various health systems, to the point of attracting other people to his interests. Experts believe that in this way a certain asociality is replaced. Also, such patients may have problems with alcohol, drugs or other types of addiction.
The patient does not perceive the accepted norms of social behavior, often behaves eccentrically. Schizoid personality disorders are associated with a great passion for some kind of activity in which the individual succeeds. For example, he may be pathologically addicted to various health systems, to the point of attracting other people to his interests. Experts believe that in this way a certain asociality is replaced. Also, such patients may have problems with alcohol, drugs or other types of addiction. - § Dissocial - a characteristic feature of this personality disorder is the patient's cognitive defiant behavior in order to get what he wants. With all this, such patients are able to win over people, including doctors. This type is especially pronounced in late adolescence.
- § Hysterical - the main goal of such patients is to draw attention to their person in any way, including defiant behavior. The diagnosis is more typical for women. Atypical capriciousness, inconstancy of desires, extravagance, deceit are observed.
 In order to attract attention, the patient invents non-existent diseases for himself, the symptoms of which can be given out by the autonomic system and which is difficult to remove.
In order to attract attention, the patient invents non-existent diseases for himself, the symptoms of which can be given out by the autonomic system and which is difficult to remove. - § Obsessive-compulsive - patients with this type of personality disorder pathologically strive for order and perfection. They have no sense of humor, they try to be perfect in everything. When the set ideal goals are not achieved, they can fall into depressive states.
- § Anxious - such a personality disorder is characterized by the cultivation of a personal inferiority complex. Patients are in a state of perpetual anxiety and uncertainty. From childhood, such patients are shy and timid. Often suspect others of hostility. They are prone to depression.
- § Narcissistic - a deviation in which a person manifests self-admiration from childhood, a desire to be constantly admired. Such a patient does not accept criticism: he reacts to it either with resentment or with aggression. Indifferent to the feelings of other people, prone to exploiting them to achieve their own goals.

Different forms of psychopathy require an individual approach to treatment. Personality disorders should not be confused with character accentuation. In the latter case, a person also has behavioral features, but they lie within the upper limit of the norm. In addition, it is adapted to social conditions. The classification of classical psychopathy is inappropriate here. Diagnosis and types are different.
Causes that cause personality and behavioral disorders
All specific personality disorders are usually divided into three clusters. Their classification:
- § types of cluster A psychopathy: paranoid and schizoid;
- § Cluster B psychopathy: hysterical, asocial, narcissistic;
- § Types of cluster B psychopathy: obsessive-compulsive, depressive.
The causes of cluster A psychopathy are considered to be genetic and hereditary.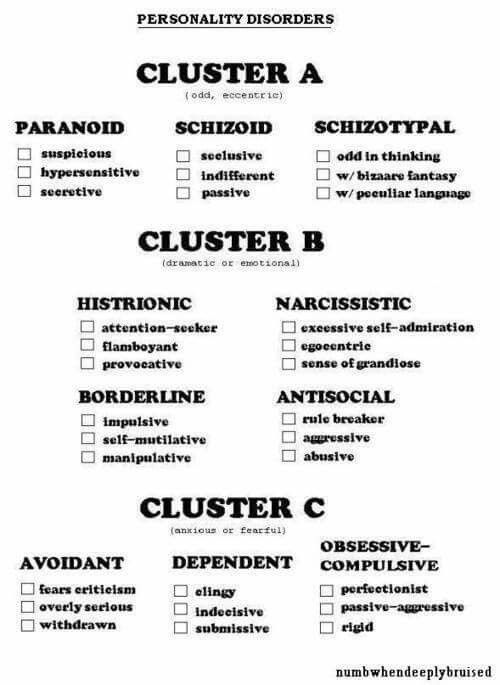 The fact is that among the relatives of patients who have a personality disorder, as a rule, there is at least one with schizophrenia. A hereditary predisposition to pathologies can also be traced in cluster B and C psychopathy. The first option can also be aggravated by problems with alcohol: in families of people who drink, children often develop with disorders. There is a version that cognitive specific personality disorders may be associated with hormonal disorders in the body. If a person has elevated levels of testosterone, estrone and estradiol, the consequences of this are manifested in the form of aggression. In addition, he does not produce enough endorphins, which, in turn, leads to depressive disorders. The social factor also plays an important role in the formation of the psychotype. For active children, space is important. If they are forced to be brought up in a closed space, small areas, this leads to the appearance of hyperactivity. Anxious babies from birth can become balanced if they are raised by emotionally stable parents.
The fact is that among the relatives of patients who have a personality disorder, as a rule, there is at least one with schizophrenia. A hereditary predisposition to pathologies can also be traced in cluster B and C psychopathy. The first option can also be aggravated by problems with alcohol: in families of people who drink, children often develop with disorders. There is a version that cognitive specific personality disorders may be associated with hormonal disorders in the body. If a person has elevated levels of testosterone, estrone and estradiol, the consequences of this are manifested in the form of aggression. In addition, he does not produce enough endorphins, which, in turn, leads to depressive disorders. The social factor also plays an important role in the formation of the psychotype. For active children, space is important. If they are forced to be brought up in a closed space, small areas, this leads to the appearance of hyperactivity. Anxious babies from birth can become balanced if they are raised by emotionally stable parents.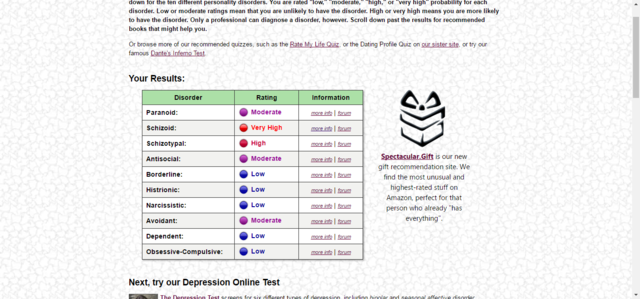 A calm mother can help a child become confident, and an anxious one can not remove, but increase his personal anxiety state. Character traits become noticeable already in early childhood. In adolescence, they can already develop as a personality disorder. Cognitive impairment is manifested in a decrease in memory, increased fatigue. Pathologies of the nervous system are observed more often in people with an asocial temperament.
A calm mother can help a child become confident, and an anxious one can not remove, but increase his personal anxiety state. Character traits become noticeable already in early childhood. In adolescence, they can already develop as a personality disorder. Cognitive impairment is manifested in a decrease in memory, increased fatigue. Pathologies of the nervous system are observed more often in people with an asocial temperament.
Mixed personality disorder
This type of psychopathy is less studied than others. The classification has no special criteria. The patient manifests forms of one or the other type of disorders that are not persistent. Therefore, this type of disorder is also called mosaic psychopathy. But it is also difficult for a person with a mixed type of disorder to get along in society because of the peculiarities of their behavior. Instability of character is often the basis that contributes to the development of various types of addiction.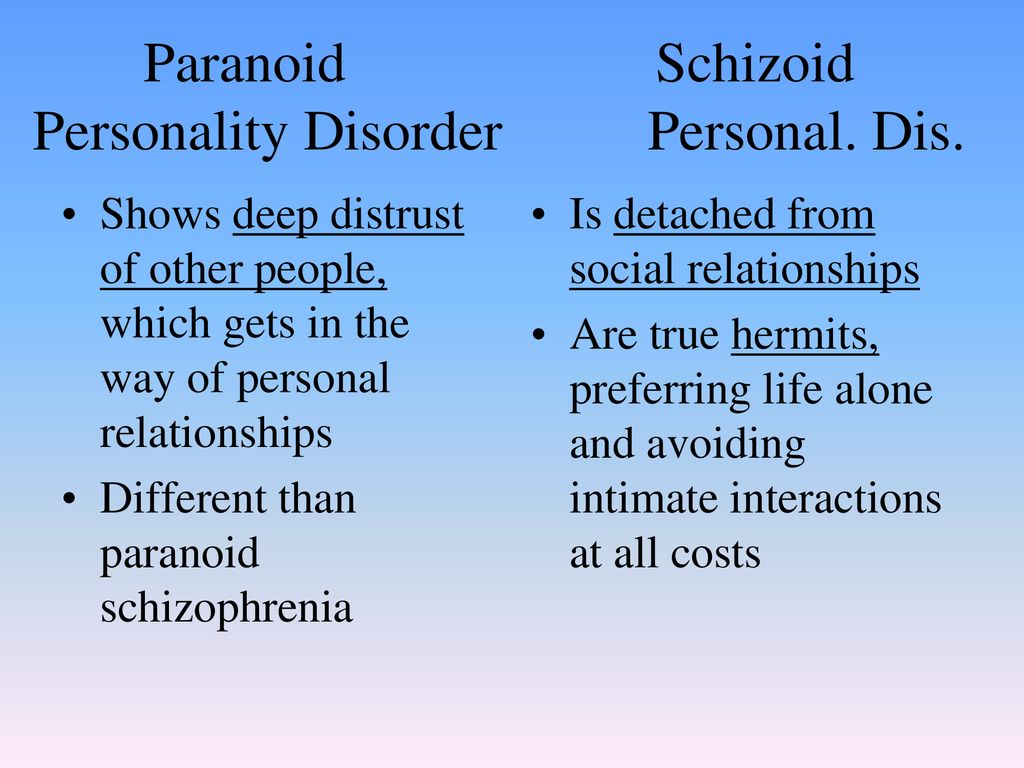 Mixed personality disorder may be accompanied by alcoholism, drug addiction, gambling addiction. Mosaic psychopathy can combine symptoms of the schizoid and paranoid types. Such people do not know how to build social contacts in society, they are obsessed with overvalued ideas. With the predominance of paranoid symptoms, patients suffer from increased suspicion. They are prone to scandals, threats, like to write angry complaints about everyone and everything. Specialists are alarmed if signs (classification) of several disorders coexist in one patient: schizoid, hysterical, asthenic, excitable. In this case, there is a high risk of developing schizophrenia. Brain injuries or complications after a number of diseases can lead to mosaic types of pathology. This mixed personality disorder is considered acquired. If we consider the situation in detail, it will look like this: a person already has an innate tendency to mosaic psychopathy, which, due to certain circumstances, is superimposed by organic pathology.
Mixed personality disorder may be accompanied by alcoholism, drug addiction, gambling addiction. Mosaic psychopathy can combine symptoms of the schizoid and paranoid types. Such people do not know how to build social contacts in society, they are obsessed with overvalued ideas. With the predominance of paranoid symptoms, patients suffer from increased suspicion. They are prone to scandals, threats, like to write angry complaints about everyone and everything. Specialists are alarmed if signs (classification) of several disorders coexist in one patient: schizoid, hysterical, asthenic, excitable. In this case, there is a high risk of developing schizophrenia. Brain injuries or complications after a number of diseases can lead to mosaic types of pathology. This mixed personality disorder is considered acquired. If we consider the situation in detail, it will look like this: a person already has an innate tendency to mosaic psychopathy, which, due to certain circumstances, is superimposed by organic pathology.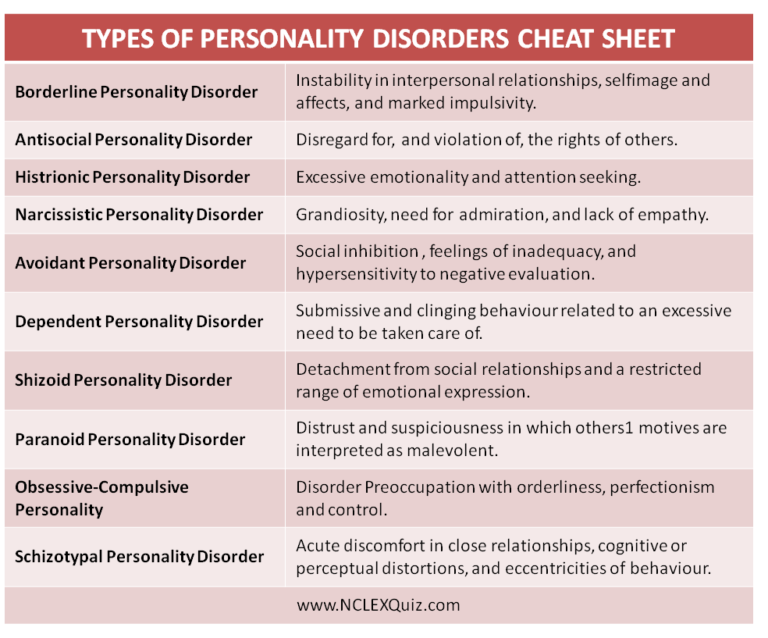 Mosaic disorder requires specific treatment only when symptoms worsen, or if there is organic build-up. Then neuroleptics, tranquilizers, vitamins can be prescribed by a specialist.
Mosaic disorder requires specific treatment only when symptoms worsen, or if there is organic build-up. Then neuroleptics, tranquilizers, vitamins can be prescribed by a specialist.
Infantile personality disorder
With this type of psychopathy, signs of social immaturity are pronounced. A person is not able to withstand stressful situations and relieve tension. In difficult circumstances, he does not control his emotions in the same way as children do. Infantile personality disorders for the first time clearly declare themselves in adolescence. Hormonal storms that occur at this time with a person cause changes in the psycho-emotional sphere. As you get older, the diagnosis can only progress. It is possible to finally talk about the presence of the disease only after reaching 16-17 years. In stressful circumstances, the patient manifests himself immature, poorly controls aggression, anxiety, fear. Such a person is not hired for military service, they are denied employment in law enforcement agencies.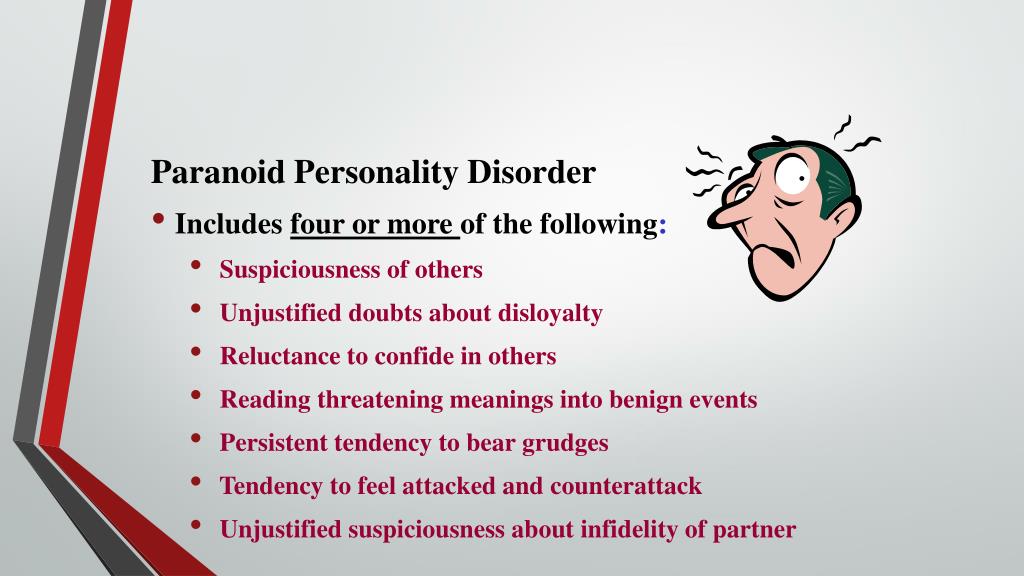 Permits to carry weapons or obtain a driver's license are decided on a limited and strictly case-by-case basis, according to an assessment of signs and condition.
Permits to carry weapons or obtain a driver's license are decided on a limited and strictly case-by-case basis, according to an assessment of signs and condition.
Transient personality disorder
This diagnosis refers to borderline conditions, when the symptoms of deviation are difficult to attribute to any type of personality disorder. The main causes of psychopathy are long-term stressful situations. In the modern world, a person is surrounded by many unfavorable factors: troubles at work, military operations, difficult family circumstances, financial failures, moving... All this disrupts the usual way of life and unbalances. If such circumstances last too long, the human psyche does not always have a reserve to survive and overcome them. Transient personality disorder has its own characteristics:
- § disorientation;
- § hallucinations;
- § nonsense;
- § inhibition of verbal and motor functions.
Even one of the symptoms can already signal a disorder. This diagnosis is special in that the disease does not last too long: sometimes only a day, and sometimes a month. It suddenly arises and just as it passes. Sometimes a person can go to sleep with a disturbance, and get up in a normal emotional state with residual effects in the form of increased anxiety or sleep disturbances. With each new stress, a spontaneous return of pathology is possible. Such a diagnosis does not pass without a trace. In the event that there are signs of delirium or hallucinations, such a person requires special treatment, because his condition can also threaten those around him. In the period between exacerbations, the patient experiences emotional burnout, in which nerve cells are also destroyed. Therefore, even for preventive purposes, it is recommended to take vitamins and herbal remedies. As historical examples show, partial transient personality disorder is not a benign condition. Many of the famous serial killers and maniacs had this diagnosis. They led a normal life, had families, work, but during the period of exacerbations they committed crimes.
This diagnosis is special in that the disease does not last too long: sometimes only a day, and sometimes a month. It suddenly arises and just as it passes. Sometimes a person can go to sleep with a disturbance, and get up in a normal emotional state with residual effects in the form of increased anxiety or sleep disturbances. With each new stress, a spontaneous return of pathology is possible. Such a diagnosis does not pass without a trace. In the event that there are signs of delirium or hallucinations, such a person requires special treatment, because his condition can also threaten those around him. In the period between exacerbations, the patient experiences emotional burnout, in which nerve cells are also destroyed. Therefore, even for preventive purposes, it is recommended to take vitamins and herbal remedies. As historical examples show, partial transient personality disorder is not a benign condition. Many of the famous serial killers and maniacs had this diagnosis. They led a normal life, had families, work, but during the period of exacerbations they committed crimes. When Western experts studied the brains of executed criminals, they did not find significant changes in it. All its parts corresponded to the norm of a healthy person. And only stressful conditions could lead to the appearance of signs of a personality disorder, which entailed antisocial acts. Perhaps, if during the period when the first signs of the disease appeared, there would have been a person nearby who noticed this and helped to contact a specialist, such consequences could have been avoided. Being face-to-face with continuous stressful situations, the psyche simply could not stand it. The mechanism of the development of the disease was launched.
When Western experts studied the brains of executed criminals, they did not find significant changes in it. All its parts corresponded to the norm of a healthy person. And only stressful conditions could lead to the appearance of signs of a personality disorder, which entailed antisocial acts. Perhaps, if during the period when the first signs of the disease appeared, there would have been a person nearby who noticed this and helped to contact a specialist, such consequences could have been avoided. Being face-to-face with continuous stressful situations, the psyche simply could not stand it. The mechanism of the development of the disease was launched.
Treatment for personality disorders
When a person is diagnosed with psychopathy, they rarely agree with it. The peculiarity of this disease is that the patient does not see problems in himself, but looks for them in others. Treatment in this case is always difficult. According to statistics, only one in five of them agree to accept help.