Treatment for manic depressive
Bipolar disorder - Diagnosis and treatment
Diagnosis
To determine if you have bipolar disorder, your evaluation may include:
- Physical exam. Your doctor may do a physical exam and lab tests to identify any medical problems that could be causing your symptoms.
- Psychiatric assessment. Your doctor may refer you to a psychiatrist, who will talk to you about your thoughts, feelings and behavior patterns. You may also fill out a psychological self-assessment or questionnaire. With your permission, family members or close friends may be asked to provide information about your symptoms.
- Mood charting. You may be asked to keep a daily record of your moods, sleep patterns or other factors that could help with diagnosis and finding the right treatment.
- Criteria for bipolar disorder. Your psychiatrist may compare your symptoms with the criteria for bipolar and related disorders in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association.
Diagnosis in children
Although diagnosis of children and teenagers with bipolar disorder includes the same criteria that are used for adults, symptoms in children and teens often have different patterns and may not fit neatly into the diagnostic categories.
Also, children who have bipolar disorder are frequently also diagnosed with other mental health conditions such as attention-deficit/hyperactivity disorder (ADHD) or behavior problems, which can make diagnosis more complicated. Referral to a child psychiatrist with experience in bipolar disorder is recommended.
Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your bipolar disorder-related health concerns Start Here
More Information
- Bipolar disorder care at Mayo Clinic
- Bipolar disorder in children: Is it possible?
- Urinalysis
Treatment
Treatment is best guided by a medical doctor who specializes in diagnosing and treating mental health conditions (psychiatrist) who is skilled in treating bipolar and related disorders.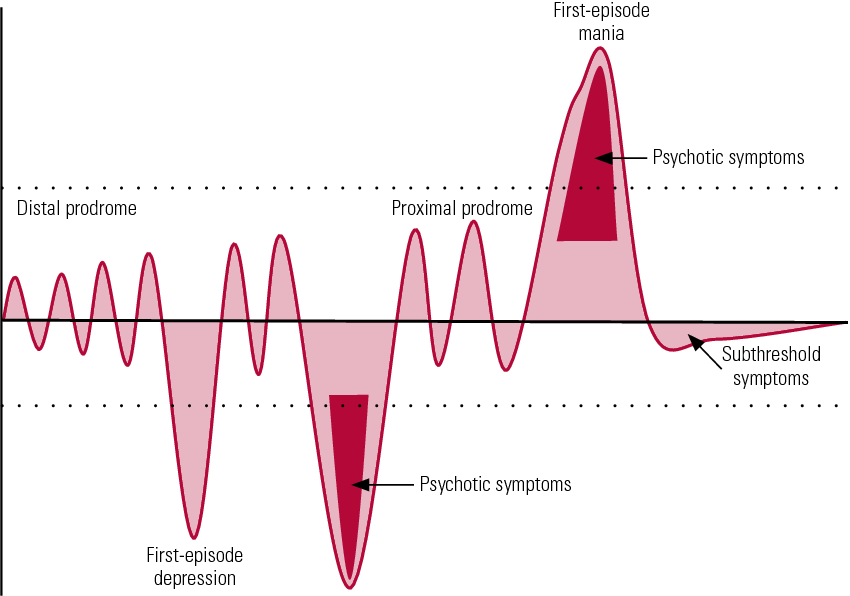 You may have a treatment team that also includes a psychologist, social worker and psychiatric nurse.
You may have a treatment team that also includes a psychologist, social worker and psychiatric nurse.
Bipolar disorder is a lifelong condition. Treatment is directed at managing symptoms. Depending on your needs, treatment may include:
- Medications. Often, you'll need to start taking medications to balance your moods right away.
- Continued treatment. Bipolar disorder requires lifelong treatment with medications, even during periods when you feel better. People who skip maintenance treatment are at high risk of a relapse of symptoms or having minor mood changes turn into full-blown mania or depression.
- Day treatment programs. Your doctor may recommend a day treatment program. These programs provide the support and counseling you need while you get symptoms under control.
- Substance abuse treatment.
If you have problems with alcohol or drugs, you'll also need substance abuse treatment.
 Otherwise, it can be very difficult to manage bipolar disorder.
Otherwise, it can be very difficult to manage bipolar disorder. - Hospitalization. Your doctor may recommend hospitalization if you're behaving dangerously, you feel suicidal or you become detached from reality (psychotic). Getting psychiatric treatment at a hospital can help keep you calm and safe and stabilize your mood, whether you're having a manic or major depressive episode.
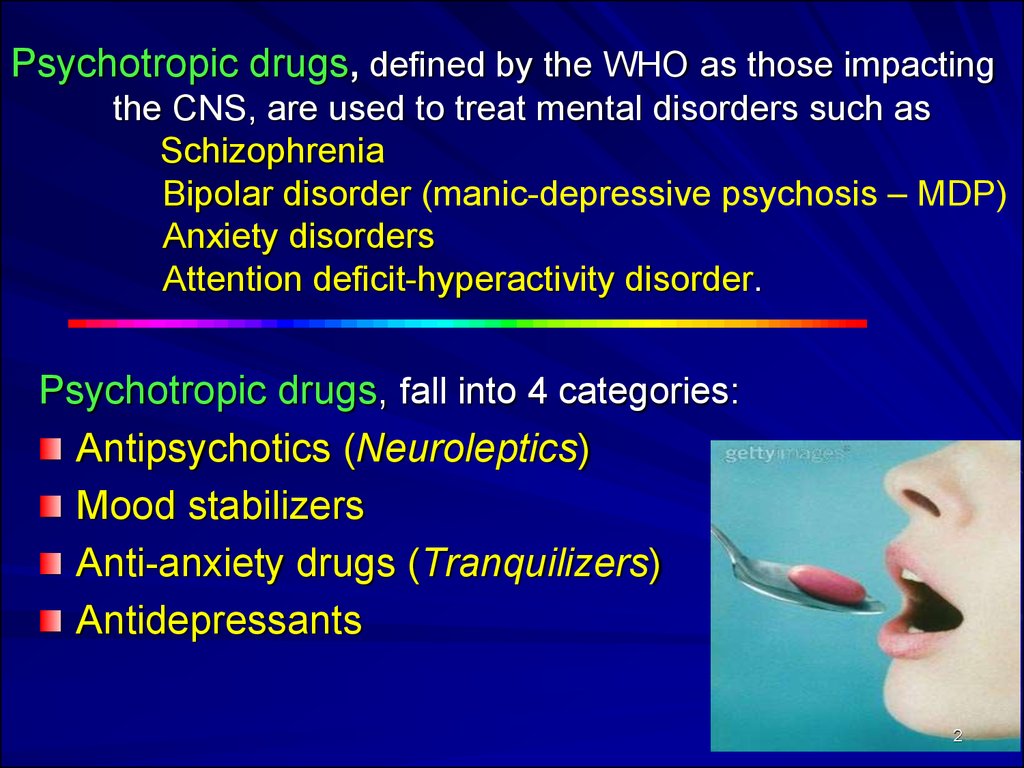
The primary treatments for bipolar disorder include medications and psychological counseling (psychotherapy) to control symptoms, and also may include education and support groups.
Medications
A number of medications are used to treat bipolar disorder. The types and doses of medications prescribed are based on your particular symptoms.
Medications may include:
- Mood stabilizers. You'll typically need mood-stabilizing medication to control manic or hypomanic episodes. Examples of mood stabilizers include lithium (Lithobid), valproic acid (Depakene), divalproex sodium (Depakote), carbamazepine (Tegretol, Equetro, others) and lamotrigine (Lamictal).
- Antipsychotics. If symptoms of depression or mania persist in spite of treatment with other medications, adding an antipsychotic drug such as olanzapine (Zyprexa), risperidone (Risperdal), quetiapine (Seroquel), aripiprazole (Abilify), ziprasidone (Geodon), lurasidone (Latuda) or asenapine (Saphris) may help. Your doctor may prescribe some of these medications alone or along with a mood stabilizer.
- Antidepressants. Your doctor may add an antidepressant to help manage depression. Because an antidepressant can sometimes trigger a manic episode, it's usually prescribed along with a mood stabilizer or antipsychotic.
- Antidepressant-antipsychotic. The medication Symbyax combines the antidepressant fluoxetine and the antipsychotic olanzapine. It works as a depression treatment and a mood stabilizer.
- Anti-anxiety medications. Benzodiazepines may help with anxiety and improve sleep, but are usually used on a short-term basis.

Finding the right medication
Finding the right medication or medications for you will likely take some trial and error. If one doesn't work well for you, there are several others to try.
This process requires patience, as some medications need weeks to months to take full effect. Generally only one medication is changed at a time so that your doctor can identify which medications work to relieve your symptoms with the least bothersome side effects. Medications also may need to be adjusted as your symptoms change.
Side effects
Mild side effects often improve as you find the right medications and doses that work for you, and your body adjusts to the medications. Talk to your doctor or mental health professional if you have bothersome side effects.
Don't make changes or stop taking your medications. If you stop your medication, you may experience withdrawal effects or your symptoms may worsen or return. You may become very depressed, feel suicidal, or go into a manic or hypomanic episode. If you think you need to make a change, call your doctor.
If you think you need to make a change, call your doctor.
Medications and pregnancy
A number of medications for bipolar disorder can be associated with birth defects and can pass through breast milk to your baby. Certain medications, such as valproic acid and divalproex sodium, should not be used during pregnancy. Also, birth control medications may lose effectiveness when taken along with certain bipolar disorder medications.
Discuss treatment options with your doctor before you become pregnant, if possible. If you're taking medication to treat your bipolar disorder and think you may be pregnant, talk to your doctor right away.
Psychotherapy
Psychotherapy is a vital part of bipolar disorder treatment and can be provided in individual, family or group settings. Several types of therapy may be helpful. These include:
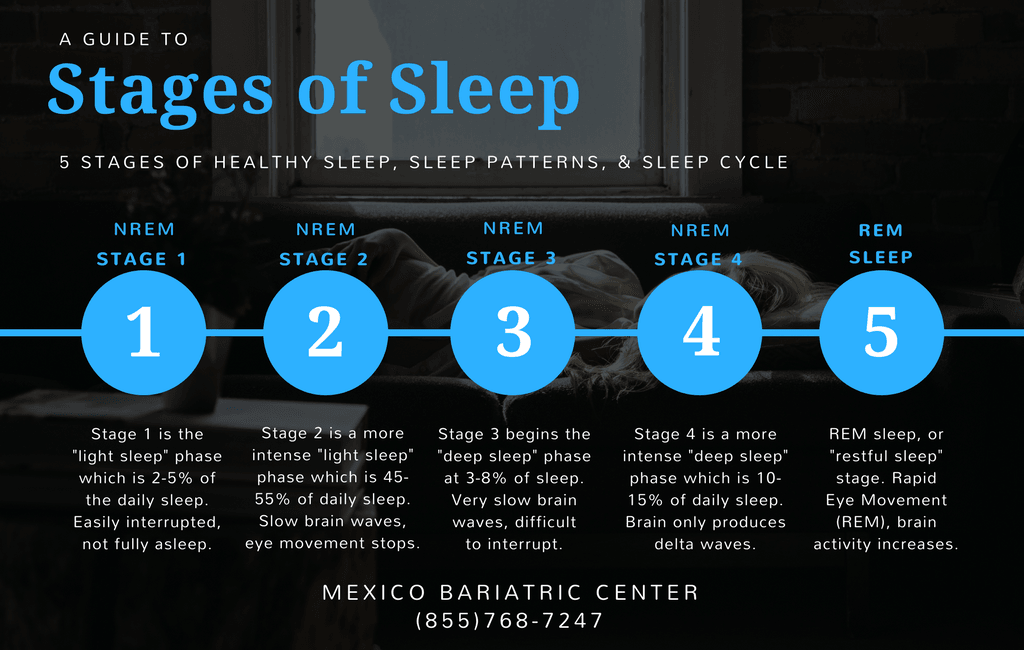
- Interpersonal and social rhythm therapy (IPSRT). IPSRT focuses on the stabilization of daily rhythms, such as sleeping, waking and mealtimes.
 A consistent routine allows for better mood management. People with bipolar disorder may benefit from establishing a daily routine for sleep, diet and exercise.
A consistent routine allows for better mood management. People with bipolar disorder may benefit from establishing a daily routine for sleep, diet and exercise. - Cognitive behavioral therapy (CBT). The focus is identifying unhealthy, negative beliefs and behaviors and replacing them with healthy, positive ones. CBT can help identify what triggers your bipolar episodes. You also learn effective strategies to manage stress and to cope with upsetting situations.
- Psychoeducation. Learning about bipolar disorder (psychoeducation) can help you and your loved ones understand the condition. Knowing what's going on can help you get the best support, identify issues, make a plan to prevent relapse and stick with treatment.
- Family-focused therapy. Family support and communication can help you stick with your treatment plan and help you and your loved ones recognize and manage warning signs of mood swings.
Other treatment options
Depending on your needs, other treatments may be added to your depression therapy.
During electroconvulsive therapy (ECT), electrical currents are passed through the brain, intentionally triggering a brief seizure. ECT seems to cause changes in brain chemistry that can reverse symptoms of certain mental illnesses. ECT may be an option for bipolar treatment if you don't get better with medications, can't take antidepressants for health reasons such as pregnancy or are at high risk of suicide.
Transcranial magnetic stimulation (TMS) is being investigated as an option for those who haven't responded to antidepressants.
Treatment in children and teenagers
Treatments for children and teenagers are generally decided on a case-by-case basis, depending on symptoms, medication side effects and other factors. Generally, treatment includes:
- Medications. Children and teens with bipolar disorder are often prescribed the same types of medications as those used in adults. There's less research on the safety and effectiveness of bipolar medications in children than in adults, so treatment decisions are often based on adult research.
- Psychotherapy. Initial and long-term therapy can help keep symptoms from returning. Psychotherapy can help children and teens manage their routines, develop coping skills, address learning difficulties, resolve social problems, and help strengthen family bonds and communication. And, if needed, it can help treat substance abuse problems common in older children and teens with bipolar disorder.
- Psychoeducation. Psychoeducation can include learning the symptoms of bipolar disorder and how they differ from behavior related to your child's developmental age, the situation and appropriate cultural behavior. Understanding about bipolar disorder can also help you support your child.
- Support. Working with teachers and school counselors and encouraging support from family and friends can help identify services and encourage success.
More Information
- Bipolar disorder care at Mayo Clinic
- Bipolar medications and weight gain
- Bipolar treatment: I vs.
 II
II - Cognitive behavioral therapy
- Electroconvulsive therapy (ECT)
- Family therapy
- Psychotherapy
- Transcranial magnetic stimulation
Request an appointment
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health. Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
You'll probably need to make lifestyle changes to stop cycles of behavior that worsen your bipolar disorder. Here are some steps to take:
- Quit drinking or using recreational drugs. One of the biggest concerns with bipolar disorder is the negative consequences of risk-taking behavior and drug or alcohol abuse. Get help if you have trouble quitting on your own.
- Form healthy relationships. Surround yourself with people who are a positive influence. Friends and family members can provide support and help you watch for warning signs of mood shifts.
- Create a healthy routine.
Having a regular routine for sleeping, eating and physical activity can help balance your moods. Check with your doctor before starting any exercise program. Eat a healthy diet. If you take lithium, talk with your doctor about appropriate fluid and salt intake. If you have trouble sleeping, talk to your doctor or mental health professional about what you can do.
- Check first before taking other medications. Call the doctor who's treating you for bipolar disorder before you take medications prescribed by another doctor or any over-the-counter supplements or medications. Sometimes other medications trigger episodes of depression or mania or may interfere with medications you're taking for bipolar disorder.
- Consider keeping a mood chart. Keeping a record of your daily moods, treatments, sleep, activities and feelings may help identify triggers, effective treatment options and when treatment needs to be adjusted.
Alternative medicine
There isn't much research on alternative or complementary medicine — sometimes called integrative medicine — and bipolar disorder. Most of the studies are on major depression, so it isn't clear how these nontraditional approaches work for bipolar disorder.
If you choose to use alternative or complementary medicine in addition to your physician-recommended treatment, take some precautions first:
- Don't stop taking your prescribed medications or skip therapy sessions. Alternative or complementary medicine is not a substitute for regular medical care when it comes to treating bipolar disorder.
- Be honest with your doctors and mental health professionals. Tell them exactly which alternative or complementary treatments you use or would like to try.
- Be aware of potential dangers. Alternative and complementary products aren't regulated the way prescription drugs are. Just because it's natural doesn't mean it's safe. Before using alternative or complementary medicine, talk to your doctor about the risks, including possible serious interactions with medications.
Coping and support
Coping with bipolar disorder can be challenging. Here are some strategies that can help:
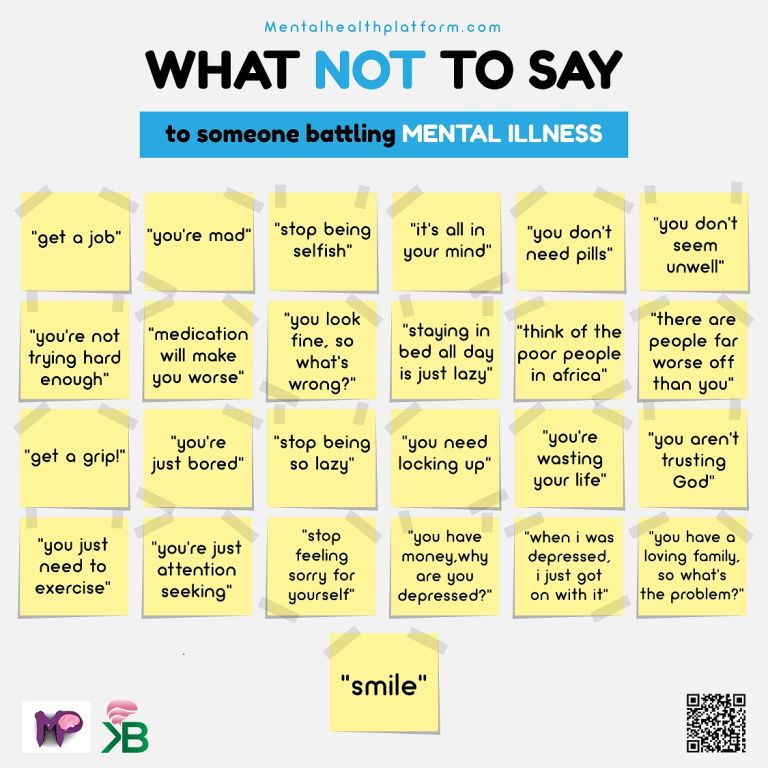
- Learn about bipolar disorder. Education about your condition can empower you and motivate you to stick to your treatment plan and recognize mood changes. Help educate your family and friends about what you're going through.
- Stay focused on your goals. Learning to manage bipolar disorder can take time. Stay motivated by keeping your goals in mind and reminding yourself that you can work to repair damaged relationships and other problems caused by your mood swings.
- Join a support group. Support groups for people with bipolar disorder can help you connect to others facing similar challenges and share experiences.
- Find healthy outlets. Explore healthy ways to channel your energy, such as hobbies, exercise and recreational activities.
- Learn ways to relax and manage stress.
Yoga, tai chi, massage, meditation or other relaxation techniques can be helpful.
Preparing for your appointment
You may start by seeing your primary care doctor or a psychiatrist. You may want to take a family member or friend along to your appointment, if possible, for support and to help remember information.
What you can do
Before your appointment, make a list of:
- Any symptoms you've had, including any that may seem unrelated to the reason for the appointment
- Key personal information, including any major stresses or recent life changes
- All medications, vitamins, herbs or other supplements you're taking, and the dosages
- Questions to ask your doctor
Some questions to ask your doctor may include:
- Do I have bipolar disorder?
- Are there any other possible causes for my symptoms?
- What kinds of tests will I need?
- What treatments are available? Which do you recommend for me?
- What side effects are possible with that treatment?
- What are the alternatives to the primary approach that you're suggesting?
- I have these other health conditions.
How can I best manage these conditions together?
- Should I see a psychiatrist or other mental health professional?
- Is there a generic alternative to the medicine you're prescribing?
- Are there any brochures or other printed material that I can have?
- What websites do you recommend?
Don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Your doctor will likely ask you a number of questions. Be ready to answer them to reserve time to go over any points you want to focus on. Your doctor may ask:
- When did you or your loved ones first begin noticing your symptoms?
- How frequently do your moods change?
- Do you ever have suicidal thoughts when you're feeling down?
- Do your symptoms interfere with your daily life or relationships?
- Do you have any blood relatives with bipolar disorder or depression?
- What other mental or physical health conditions do you have?
- Do you drink alcohol, smoke cigarettes or use recreational drugs?
- How much do you sleep at night? Does it change over time?
- Do you go through periods when you take risks that you wouldn't normally take, such as unsafe sex or unwise, spontaneous financial decisions?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
By Mayo Clinic Staff
Related
Associated Procedures
News from Mayo Clinic
Products & Services
Bipolar disorder - Symptoms and causes
Overview
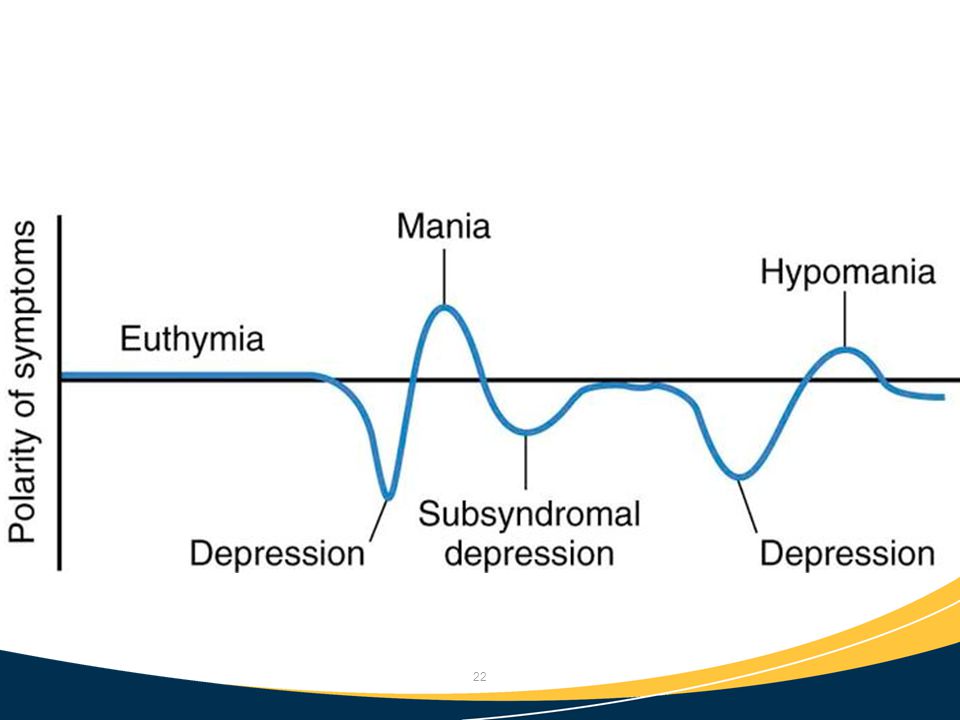
Bipolar disorder, formerly called manic depression, is a mental health condition that causes extreme mood swings that include emotional highs (mania or hypomania) and lows (depression).
When you become depressed, you may feel sad or hopeless and lose interest or pleasure in most activities. When your mood shifts to mania or hypomania (less extreme than mania), you may feel euphoric, full of energy or unusually irritable. These mood swings can affect sleep, energy, activity, judgment, behavior and the ability to think clearly.
Episodes of mood swings may occur rarely or multiple times a year. While most people will experience some emotional symptoms between episodes, some may not experience any.
Although bipolar disorder is a lifelong condition, you can manage your mood swings and other symptoms by following a treatment plan. In most cases, bipolar disorder is treated with medications and psychological counseling (psychotherapy).
Bipolar disorder care at Mayo Clinic
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
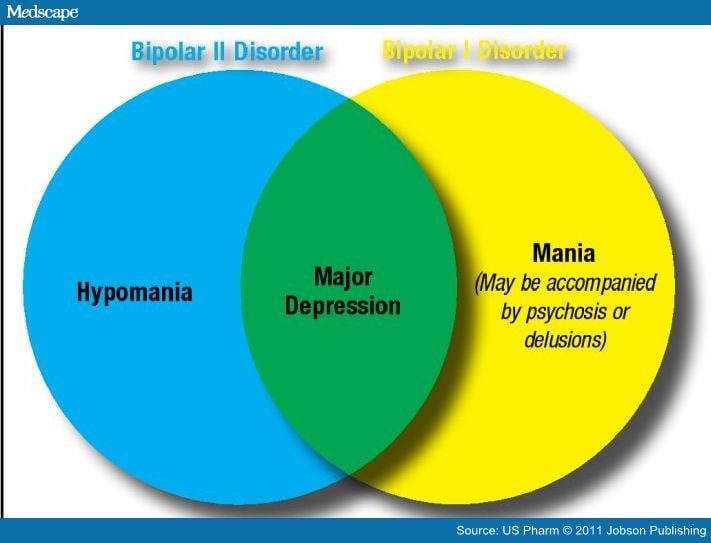
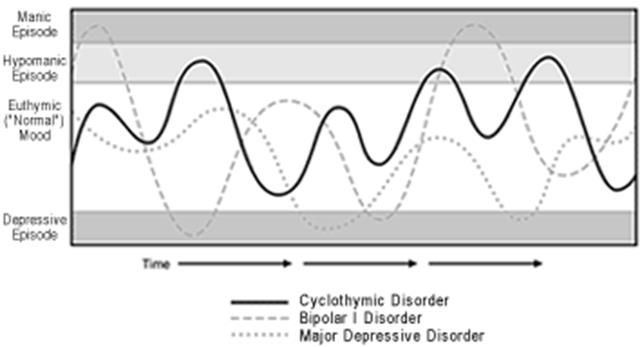
There are several types of bipolar and related disorders. They may include mania or hypomania and depression. Symptoms can cause unpredictable changes in mood and behavior, resulting in significant distress and difficulty in life.
- Bipolar I disorder. You've had at least one manic episode that may be preceded or followed by hypomanic or major depressive episodes. In some cases, mania may trigger a break from reality (psychosis).
- Bipolar II disorder. You've had at least one major depressive episode and at least one hypomanic episode, but you've never had a manic episode.
- Cyclothymic disorder. You've had at least two years — or one year in children and teenagers — of many periods of hypomania symptoms and periods of depressive symptoms (though less severe than major depression).
- Other types. These include, for example, bipolar and related disorders induced by certain drugs or alcohol or due to a medical condition, such as Cushing's disease, multiple sclerosis or stroke.
Bipolar II disorder is not a milder form of bipolar I disorder, but a separate diagnosis. While the manic episodes of bipolar I disorder can be severe and dangerous, individuals with bipolar II disorder can be depressed for longer periods, which can cause significant impairment.
Although bipolar disorder can occur at any age, typically it's diagnosed in the teenage years or early 20s. Symptoms can vary from person to person, and symptoms may vary over time.
Mania and hypomania
Mania and hypomania are two distinct types of episodes, but they have the same symptoms. Mania is more severe than hypomania and causes more noticeable problems at work, school and social activities, as well as relationship difficulties. Mania may also trigger a break from reality (psychosis) and require hospitalization.
Both a manic and a hypomanic episode include three or more of these symptoms:
- Abnormally upbeat, jumpy or wired
- Increased activity, energy or agitation
- Exaggerated sense of well-being and self-confidence (euphoria)
- Decreased need for sleep
- Unusual talkativeness
- Racing thoughts
- Distractibility
- Poor decision-making — for example, going on buying sprees, taking sexual risks or making foolish investments
Major depressive episode
A major depressive episode includes symptoms that are severe enough to cause noticeable difficulty in day-to-day activities, such as work, school, social activities or relationships. An episode includes five or more of these symptoms:
- Depressed mood, such as feeling sad, empty, hopeless or tearful (in children and teens, depressed mood can appear as irritability)
- Marked loss of interest or feeling no pleasure in all — or almost all — activities
- Significant weight loss when not dieting, weight gain, or decrease or increase in appetite (in children, failure to gain weight as expected can be a sign of depression)
- Either insomnia or sleeping too much
- Either restlessness or slowed behavior
- Fatigue or loss of energy
- Feelings of worthlessness or excessive or inappropriate guilt
- Decreased ability to think or concentrate, or indecisiveness
- Thinking about, planning or attempting suicide
Other features of bipolar disorder
Signs and symptoms of bipolar I and bipolar II disorders may include other features, such as anxious distress, melancholy, psychosis or others. The timing of symptoms may include diagnostic labels such as mixed or rapid cycling. In addition, bipolar symptoms may occur during pregnancy or change with the seasons.
Symptoms in children and teens
Symptoms of bipolar disorder can be difficult to identify in children and teens. It's often hard to tell whether these are normal ups and downs, the results of stress or trauma, or signs of a mental health problem other than bipolar disorder.
Children and teens may have distinct major depressive or manic or hypomanic episodes, but the pattern can vary from that of adults with bipolar disorder. And moods can rapidly shift during episodes. Some children may have periods without mood symptoms between episodes.
The most prominent signs of bipolar disorder in children and teenagers may include severe mood swings that are different from their usual mood swings.
When to see a doctor
Despite the mood extremes, people with bipolar disorder often don't recognize how much their emotional instability disrupts their lives and the lives of their loved ones and don't get the treatment they need.
And if you're like some people with bipolar disorder, you may enjoy the feelings of euphoria and cycles of being more productive. However, this euphoria is always followed by an emotional crash that can leave you depressed, worn out — and perhaps in financial, legal or relationship trouble.
If you have any symptoms of depression or mania, see your doctor or mental health professional. Bipolar disorder doesn't get better on its own. Getting treatment from a mental health professional with experience in bipolar disorder can help you get your symptoms under control.
When to get emergency help
Suicidal thoughts and behavior are common among people with bipolar disorder. If you have thoughts of hurting yourself, call 911 or your local emergency number immediately, go to an emergency room, or confide in a trusted relative or friend. Or contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline, available 24 hours a day, seven days a week. Or use the Lifeline Chat. Services are free and confidential.
If you have a loved one who is in danger of suicide or has made a suicide attempt, make sure someone stays with that person. Call 911 or your local emergency number immediately. Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
Request an appointment
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health. Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Causes
The exact cause of bipolar disorder is unknown, but several factors may be involved, such as:
- Biological differences. People with bipolar disorder appear to have physical changes in their brains. The significance of these changes is still uncertain but may eventually help pinpoint causes.
- Genetics. Bipolar disorder is more common in people who have a first-degree relative, such as a sibling or parent, with the condition. Researchers are trying to find genes that may be involved in causing bipolar disorder.
Risk factors
Factors that may increase the risk of developing bipolar disorder or act as a trigger for the first episode include:
- Having a first-degree relative, such as a parent or sibling, with bipolar disorder
- Periods of high stress, such as the death of a loved one or other traumatic event
- Drug or alcohol abuse
Complications
Left untreated, bipolar disorder can result in serious problems that affect every area of your life, such as:
- Problems related to drug and alcohol use
- Suicide or suicide attempts
- Legal or financial problems
- Damaged relationships
- Poor work or school performance
Co-occurring conditions
If you have bipolar disorder, you may also have another health condition that needs to be treated along with bipolar disorder. Some conditions can worsen bipolar disorder symptoms or make treatment less successful. Examples include:
- Anxiety disorders
- Eating disorders
- Attention-deficit/hyperactivity disorder (ADHD)
- Alcohol or drug problems
- Physical health problems, such as heart disease, thyroid problems, headaches or obesity
More Information
- Bipolar disorder care at Mayo Clinic
- Bipolar disorder and alcoholism: Are they related?
Prevention
There's no sure way to prevent bipolar disorder. However, getting treatment at the earliest sign of a mental health disorder can help prevent bipolar disorder or other mental health conditions from worsening.
If you've been diagnosed with bipolar disorder, some strategies can help prevent minor symptoms from becoming full-blown episodes of mania or depression:
- Pay attention to warning signs. Addressing symptoms early on can prevent episodes from getting worse. You may have identified a pattern to your bipolar episodes and what triggers them. Call your doctor if you feel you're falling into an episode of depression or mania. Involve family members or friends in watching for warning signs.
- Avoid drugs and alcohol. Using alcohol or recreational drugs can worsen your symptoms and make them more likely to come back.
- Take your medications exactly as directed. You may be tempted to stop treatment — but don't. Stopping your medication or reducing your dose on your own may cause withdrawal effects or your symptoms may worsen or return.
By Mayo Clinic Staff
Related
Associated Procedures
News from Mayo Clinic
Products & Services
Treatment of manic-depressive psychosis in St. Petersburg
- Main
- Psychiatry
- TIR treatment
We treat manic-depressive psychosis (F31, ICD-10) in teenagers and adults. The treatment of MDP in adolescents is carried out by the head physician of the clinic, a certified child psychiatrist, a recognized expert in the pharmacotherapy of mental disorders. In particular, we take on difficult cases and cases with therapeutic resistance.
Keeping a diary of mood swings on your own, including before seeking help, will help the doctor make a diagnosis (a long process) and will also effectively prevent episodes of the disease (Rasim Somer Diler, Boris Birmaher).
The selection of pharmacotherapy is more expedient to carry out in the clinic, especially in the presence of a pronounced depressive state and suicidal intentions/behavior. Due to the intensification of treatment, we are able to force a complex algorithm for the biological therapy of manic and mixed states, thereby reducing the patient's stay in the hospital.
In addition to drug therapy, the treatment of manic-depressive psychosis includes individual work with a psychotherapist, and, if necessary, within the framework of family and / or group sessions. After discharge, it is important not to neglect control visits to the doctor and preventive sessions with a psychotherapist, since the disease is chronic, with a high probability of relapse.
Test: "Altman scale for self-assessment of mania"
Choose the answer that most accurately reflects your state of mind over the past week.
Doctor's consultation on TIR treatment:
+7 (812) 407-18-00
Thank you for your trust!
- Selection of medical treatment
- Outpatient or inpatient treatment
- Psychosocial personality correction
| Service | Price | |
|---|---|---|
| Outpatient treatment | ||
| Psychiatric consultation | 5 000 ₽ | |
| Psychotherapist appointment | 5 000 ₽ | |
| Reception of the chief physician Bocharov A. | 6 000 ₽ | |
| Psychiatric consultation at home | 6 000 ₽ | |
| Treatment in a hospital | ||
| Delivery to hospital | For free | |
| Standard Chamber | 8 900 ₽ | |
| 3-bed superior room | 12 000 ₽ | |
| 2-bed superior room | 15 000 ₽ | |
| 1 local VIP room | 19 500 ₽ | |
| Doctor's appointment 2 weeks after discharge | For free | |
Manic depressive causes
Manic depressive symptoms
Phases of the disease
Treatment of manic-depressive psychosis
Methods of conservative treatment of this disease directly depend on the phase of psychosis. However, to date, scientists have developed a universal remedy that is applicable to any form of the pathological process - these are lithium preparations. Treatment of manic-depressive psychosis in St. Petersburg with the help of the presented drug is carried out under the strict control of laboratory research methods, in particular, clinical and biochemical blood tests. The dose is selected individually and depends on the severity of the disease, duration, age of the patient and the presence of concomitant pathologies.
Antipsychotics or sedatives are also commonly used to treat manic episodes. In the treatment of the depressive phase, antidepressants are most effective.
Treat symptomatic TIR in a hospital. Therefore, patients who pose a danger to themselves and others must be hospitalized. Most often, such people are sent to the intensive care unit or intensive care unit. After a person is taken out of the pathological phase of psychosis, it is important to provide him with social adaptation. Much in the treatment depends on the patient and his relatives.
Medical treatment
When choosing conservative therapy, it is important to choose the right drug. The remedy should have a persistent and lasting effect, and also be designed for a long course of administration.
We use strong antidepressants to eliminate the depressive phase. These drugs are characterized by a rapid effect. However, when prescribing antidepressants, mood stabilizers are also needed. To stop the manic phase in our clinic, therapy with antipsychotics, sedatives and mood stabilizers is carried out. It is important to choose the right drug, dose and determine the course of treatment.
It is also important to diagnose manic-depressive syndrome in time. Treatment of MDP should be aimed not only at stopping seizures, but also at stabilizing the general condition. To date, it is possible to achieve a stable remission of this disease and even its complete cure. Such success is achieved by the appointment of antidepressants, antipsychotics, tranquilizers, sedatives and some other groups of drugs. In many cases, lithium carbonate is used, which effectively stops the excitement.
Psychotherapeutic treatment
Undoubtedly, drug therapy plays an important role in the treatment of manic-depressive psychosis. However, after achieving the desired remission, a person needs the help of a psychotherapist, which will help him adapt to the world around him. The following psychotherapeutic treatment has been developed:
- Cognitive therapy. At this stage, it is important to establish the underlying cause that may lead to TIR. If the main link is found, further attacks can be avoided;
- Family therapy. This stage involves the restoration of a person in the circle of family and friends;
- Social therapy. At this stage, it is important to create a clear daily routine for a person. This will help not only to discipline, but also to distract from your illness. What are bipolar disorders? — https://psychiatry.org
- Depersonalization and derealization
- Suicidal behavior
- Anxiety disorder
- manic-depressive disorder;
- cyclophrenia;
- bipolar disorder;
- circular psychosis;
- sustained elevated mood;
- mental arousal, against which the speed of speech and thinking increases;
- psychomotor agitation, which is expressed by motor restlessness.
- monopolar - periodic mania or periodic depression.
The patient registers phases of a certain type;
- correct-intermittent - the classic course of the disease, in which the manic phase replaces the depressive, and the depressive turns into manic through intermission;
- irregularly intermittent - the manic phase may turn into an intermission, after which the mania begins again. There is no strict sequence of phase changes;
- double - the manic phase without intermission passes directly into depression, after which the interphase begins;
- continual - the manic phase flows into depression and vice versa without intermission.
- genetic - the presence of close relatives with any mental illness increases the risk of bipolar disorder. Genetic causes underlie 70-80% of cases;
- neurochemical - imbalance in the brain of neurotransmitters - dopamine, norepinephrine;
- pathological - changes and shifts in the work of the endocrine system, disturbances in water-salt metabolism and biological rhythms associated with day and night fluctuations.
Brain disorders such as encephalitis or meningitis can lead to bipolar disorder;
- psychological - difficult life situations, such as the death of a loved one, divorce, financial difficulties;
- toxicological - abuse of narcotic drugs, alcoholic beverages.
- emotional blockage - in the intermission phase, a person begins to realize that psychosis limits his functionality, freedom of action, that he cannot fully fulfill his professional duties, communicate normally with his loved ones. This leads to the appearance during the interphase of a state of anxiety and the appearance of an emotional blockade, against which diseases of the internal organs and the nervous system are formed;
- mental blockage - for people who have achieved success in the professional field, for teachers, the presence of psychosis becomes a severe psychological trauma.
The disease is beginning to be blamed for all failures, including in personal life. Waiting for a phase change intensifies depression, against which a mental block occurs. This mental disorder causes severe pathologies of the internal organs and the central nervous system.
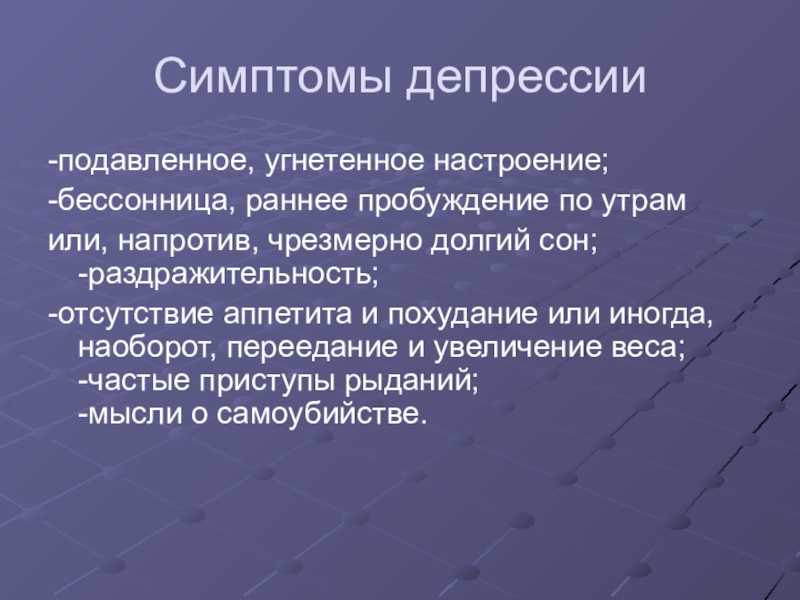
- increased activity accompanied by sleep disturbance;
- an excited state, which is characterized by groundless euphoria and unreasonable self-confidence;
- irritability, flowing into aggressive behavior with rash actions that can lead to dangerous situations;
- low concentration of attention, the patient is often distracted by minor phenomena and events;
- increased speed of speech, thoughts are expressed intermittently, the person becomes more talkative than usual;
- the patient generates ideas that demonstrate his greatness or genius, which leads to adventurous acts;
- motor activity is accompanied by intellectual excitement.
- depressed for most of the day;
- pessimistic reaction to everything that happens around;
- causeless sadness;
- decreased motor and mental activity;
- loss of interest, loss of pleasure in all activities;
- poor appetite;
- sudden weight loss (up to 5% of body weight) or its increase when trying to "seize" the problem;
- insomnia;
- suicidal thoughts.
- magnetic resonance imaging of the brain - allows you to detect the presence of neoplasms, aneurysms, thrombosis, hematomas and areas of increased intracranial pressure;
- electroencephalography - prescribed to detect pathologies of cerebral vessels, foci of inflammatory processes.
Used to diagnose epilepsy and neoplasms;
- measurement of blood pressure to rule out the diagnosis of pheochromocytoma;
- analysis of the level of thyroxine and thyroid-stimulating hormone to exclude hyperthyroidism from the clinical picture;
- X-ray of the brain - helps to identify injuries, bone displacements, pituitary tumors, hematomas and neoplasms;
- blood and urine test for the presence of narcotic drugs.
- Impact treatment - with the help of drug therapy and psychotherapy, the patient's condition is stabilized, controlling the symptoms of the disease.
- Ongoing treatment - in addition to drugs, physiotherapy methods are involved in the treatment.
- Maintenance treatment - reduce the dosage of drugs, continue psychotherapy, add exercise therapy complexes to the program, which help maintain a stable remission.
- antidepressants - have a therapeutic effect in depression, correct the level of neurotransmitters - dopamine, serotonin, norepinephrine. Assign "Olanzapine", "Lurazidon", "Quetialin", "Fluoxetine", "Bupropion". When choosing a medicine, the doctor takes into account the main symptoms of depression;
- antiepileptic drugs - stop muscle cramps of any origin, normalize mood. Prescribe medications based on valproic acid, "Carbamazepine", "Lamotrigine";
- preparations containing lithium - prescribed for severe manic symptoms, used for long-term treatment.
Use "Lithium carbonate";
- normotimics - psychotropic drugs that can stabilize mood. Used for the treatment of "Quetiapin", "Finlepsin";
- neuroleptics - antipsychotics that suppress higher mental activity. Effective in short phases of manic type. Use "Haloperidol", "Chlorpromazine", "Ziprasidone", "Aripiprazole", "Lurazidol", "Risperidone".
- social adaptation;
- professional functioning;
- symptom management training;
- formation of the ability to withstand stress factors;
- medication control training.
- cognitive-behavioral – aimed at changing the patient's emotional reactions by changing behavior or thoughts. The doctor changes the stereotypes of the patient's thinking, which are not functional and lead to non-adaptive reactions to what is happening. Desired reactions in psychotherapy sessions are reinforced by encouragement, undesirable ones are not reinforced, which leads to a change in the stereotype of thinking and other emotions;
- interpersonal - aimed at solving specific interpersonal relationships that lead to maladaptive emotional reactions.
It is a narrowly focused method that helps to cope with difficult personal experiences, role conflicts, change or lack of interpersonal relationships. Effective in the treatment of depression;
- family - all family members are involved in therapy, who are taught to jointly experience sudden changes in the patient's mood, they are taught to distinguish the symptoms of the disorder. The family must accept the fact that episodes of mood swings are inevitable in the future, that medication will have to be constantly taken to prevent and relieve symptoms. The psychiatrist forms in the group the ability to cope with family-specific stressful situations that provoke bipolar disorder;
- social support - performed as part of group therapy, during the sessions, patients exchange information about their emotional reactions, learn from each other to cope with problems. This improves the socialization of patients, simplifies the return to the team;
- compliance therapy - teaches you to act in accordance with a strict instruction or request.
The technique is used to teach the patient to use drugs in the amount prescribed by the doctor;
- social rhythm therapy - patients are taught to form a daily routine and strictly follow it. Lack of sleep can have a profound effect on people with bipolar disorder. The doctor teaches to observe the regime of rest and sleep, keep records during the week, which help to form the routine. The patient necessarily fixes the time of awakening, the first interpersonal contact during the day, the beginning of work or study. This diary takes into account the degree of participation of other people in the affairs of the patient, the mood is assessed. The diary helps the doctor to assess the dynamics of the development of the disease or its remission.
- electroshock therapy - used in the treatment of severe depression, consists in the impact of electric current on the brain;
- phototherapy - used in the treatment of seasonal bipolar disorder.
The patient takes sun baths or is irradiated with bright light with a certain wavelength. Phototherapy stimulates the production of positive emotions, has a calming effect;
- deep transcranial magnetic stimulation - affects the deep areas of the brain with electromagnetic radiation. Affects the synthesis of neurohormones, such as dopamine.
- omega-3-acids - relieve the symptoms of the disease, fatty acids can be purchased in the form of nutritional supplements, but it is better to add foods such as fish oil, nuts, eggs to the diet;
- magnesium - a microelement that has a strong effect on mood stabilization, has a calming effect similar to that of lithium.
Foods rich in magnesium can reduce the dosage of sodium carbonate, but you should not completely abandon this drug. Magnesium is found in beans, spinach, grains;
- table salt - in case of manic-depressive disorder, the usual amount of salt is used, without reducing its volume in products. This is due to the need to normalize the electrolyte balance and maintain the required level of therapeutic drugs in the blood;
- vegetable fats - help maintain a feeling of satiety, do not overeat, which is typical for manic and depressive states. Positive effect on metabolism. Healthy foods high in vegetable fats include olive oil and avocados.
- caffeine - found in coffee and tea, energy drinks, Pepsi Cola and Coca Cola. It has a stimulating effect on the nervous system, can provoke an attack of mania.
Instead of the usual drinks with caffeine, it is recommended to switch to dried fruit compote, rosehip broth, clean water;
- sugar - is a destabilizing factor, with an increase in blood levels, it makes the mood chaotic. It is better to replace ordinary sugar with sweet fruits or honey: when using these products, the glucose content in the blood does not increase abruptly;
- simple carbohydrates - found in fast food, homemade cakes, canned juices. Contribute to a sharp increase in weight, since bipolar disorder is characterized by an imbalance of serotonin;
- grapefruit - not recommended in the treatment of antiepileptic drugs;
- alcohol - not combined with mental illness, not only because of the unpredictable effect. After drinking, sleep is disturbed, and the risk of becoming dependent on alcohol in patients with bipolar disorder increases dramatically.
- genetic - the doctor prescribes mood stabilizers, anticonvulsants, a combination of antipsychotic drugs. After shock treatment, psychotherapy sessions begin, a complex of exercise therapy is prescribed;
- neurochemical - psychiatrist prescribes antidepressants that regulate the imbalance of neurotransmitters. The patient undergoes a course of phototherapy, psychotherapy, diet is adjusted;
- pathological - an endocrinologist or therapist is involved in the treatment, who prescribes drugs that normalize the endocrine system, water-salt metabolism, and stabilize biological rhythms. Encephalitis or meningitis is treated by a neurologist. After curing the underlying disease, they begin to eliminate the symptoms of bipolar disorder with the help of mood stabilizers or antidepressants, adjust the diet;
- psychological - prescribe psychotherapy, a course of drug therapy, exercise therapy complexes;
- toxicological - before starting treatment, the body is detoxified, removing alcohol, narcotic substances and decay products.
Treatment with antidepressants, lithium preparations, psychotherapy. A psychologist is actively working with the patient, social adaptation is being carried out;
- psychosomatic - exacerbation is relieved by mood stabilizers, antidepressants, antipsychotic drugs. In individual sessions of psychotherapy, the causes that led to the disease are clarified. The doctor explains to the patient that life does not end with negative events. Lack of attention from parents in the distant past, it is necessary to live a full life. All those who hurt many years ago must be forgiven. There are many positive, interesting events ahead that can and should be sympathized with those who are nearby today. The psychologist corrects personal self-esteem, teaches you to set new goals and achieve them yourself and with the help of others.
- access to doctors from specialized clinics, metropolitan medical institutions;
- doctors with a narrow specialization are involved in consultations;
- you can use the help at any convenient time;
- there is no need to go to the clinic, which optimizes personal time.
- people whose close relatives suffer from mental illness;
- patients with disorders of the endocrine system;
- who received a traumatic brain injury;
- recovered from meningitis and encephalitis;
- representatives of professions who regularly face stressful situations;
- alcohol and drug addicts;
- people who underwent brain surgery;
- people who have lost loved ones.
- people with a genetic predisposition are advised to visit a psychotherapist regularly;
- patients with disorders of the endocrine system need to follow a diet, undergo a course of treatment, regularly visit an endocrinologist;
- patients with traumatic brain injury need a full course of treatment; after recovery, follow-up by a psychotherapist is required;
- who have recovered from meningitis and encephalitis, a preventive course of lithium salts is recommended;
- representatives of professions who regularly face stressful situations need to follow the regime, have a good rest, play sports, periodically visit a psychotherapist;
- alcohol and drug addicts need to give up bad habits, undergo a course of treatment;
- people who underwent brain surgery are prescribed a course of preventive treatment;
- people who have lost loved ones should not neglect the help of a psychologist.
Analysis of the relationship between age of onset, family history and clinical outcome in 1665 patients with type I bipolar disorder — https://psychiatr. ru
Update date: 01/20/2023
Make an appointment
Date and time: (not set)
Make an appointment with a psychiatrist
Make an appointment with a psychiatrist
Select the date and time of your appointment
Today
April 24
Tomorrow
April 25
Wednesday
April 26
Thursday
April 27
Friday
April 28
Saturday
April 29
Sunday
April 30
Monday
01 May
Tuesday
02 May
Wednesday
03 May
Thursday
04 May
Friday
05 May
Monday
08 May
Tuesday
09 May
Wednesday
May 10
Thursday
May 11
Friday
May 12
Sunday
May 14
Monday
May 15
Tuesday
May 16
Wednesday
May 17
Thursday
May 18
Friday
May 19
Sunday
May 21
Monday
May 22
Tuesday
May 23
Wednesday
May 24
Thursday
May 25
Friday
May 26
Monday
May 29
Tuesday
May 30
Wednesday
31 May
TIR treatment is carried out
Bocharov Alexey
Viktorovich
Psychiatrist, psychotherapist
Head physician of clinic
Experience 42 years
Psychiatrist, psychotherapist, sexologist, child psychiatrist
Work experience 42 years
Sinenchenko Andrey
Georgievich
Psychiatrist, psychotherapist
PhD
Work experience 23 years
Psychiatrist, psychotherapist, narcologist
Work experience 23 years
Zun Sergey
Andreevich
Psychiatrist, narcologist
PhD
Experience 34 years
Psychiatrist, narcologist, psychotherapist
Work experience 34 years
Lisitsyna Elena Alekseevna
Psychiatrist
Top category
Experience 34 years
Psychiatrist
Work experience 34 years
Buchelnikova Victoria
Viktorovna
Psychiatrist
Head of amb. branch
Work experience 16 years
Psychiatrist
Work experience 16 years
Voronina Elvira
Vladimirovna
Psychiatrist
First category
Experience 28 years
Psychiatrist
Work experience 28 years
Gorobets Elena
Vasilievna
Psychiatrist
First category
Experience 17 years
Psychiatrist
Work experience 17 years
Travnikova Oksana
Mikhailovna
Psychiatrist
First category
Experience 22 years
Psychiatrist
Work experience 22 years
Kurochkina Nadezhda
Pavlovna
Psychiatrist
First category
Experience 20 years
Psychiatrist
Experience 20 years
Suslennikova Elena
Viktorovna
Psychiatrist, psychotherapist
First category
Experience 26 years
Psychiatrist, psychotherapist
Work experience 26 years
Chuban Olga
Ivanovna
Psychiatrist, psychotherapist
First category
Work experience 14 years
Psychiatrist, psychotherapist, psychologist
Work experience 14 years
Popov Andrey
Petrovich
Psychiatrist
Top category
Experience 36 years
Psychiatrist
Work experience 36 years
Stetsiv Ludmila
Gennadievna
Psychiatrist, psychotherapist
PhD
Experience 32 years
Psychiatrist, psychotherapist
Work experience 32 years
Prokhorchev Konstantin
Sergeevich
Psychiatrist, psychotherapist
First category
Work experience 13 years
Psychiatrist, psychotherapist
Work experience 13 years
Gulevsky Roman
Aleksandrovich
Psychiatrist, narcologist
Head of hospital
Experience 26 years
Psychiatrist, narcologist
Work experience 26 years
Konoplin Dmitry
Alekseevich
Narcologist, psychiatrist
PhD
Experience 25 years
Narcologist, psychiatrist
Experience 25 years
Stavitskaya Svetlana
Yurievna
Psychiatrist
Top category
Work experience 25 years
Psychiatrist
Experience 25 years
Pylskaya Anna
Nikolaevna
Psychiatrist
Second category
Experience 8 years
Psychiatrist
Work experience 8 years
Trofimova Alexandra
Olegovna
Psychiatrist, child psychiatrist
First category
Experience 29 years
Psychiatrist, child psychiatrist
Work experience 29years
Zhelobetskaya Maria
Sergeevna
Psychiatrist, psychotherapist
Top category
Work experience 23 years
Psychiatrist, psychotherapist
Work experience 23 years
Endrzheevskaya Diana
Vadimovna
Psychiatrist, psychotherapist
Second category
Work experience 15 years
Psychiatrist, child psychiatrist, psychotherapist
Work experience 15 years
Usov Grigory
Mikhailovich
Psychiatrist, psychotherapist
MD
Experience 25 years
Psychiatrist, psychotherapist
Experience 25 years
Ivanov Alexander
Nikolaevich
Psychiatrist, narcologist
Top category
Experience 21 years
Psychiatrist, narcologist
Work experience 21 years
Leave a request for a call:
+7 (812) 407-18-00
Manic-depressive psychosis - causes, symptoms, diagnosis, prevention and treatment
Synonyms
In modern medical practice, manic-depressive psychosis is called bipolar affective disorder. The symptoms of the disease were first noticed in the middle of the 19th century. The disease was called circulation psychosis, but it was not isolated as a separate disease. The generally accepted name of manic-depressive psychosis was received only in 1896 year. Among other synonyms of the disease:
The boundaries of manic disorder in modern psychiatry are not clearly limited, which causes numerous additions to the name of the disease indicating the phase of the ongoing psychosis.
General information
Each person undergoes psycho-physiological processes that are the background for motivating action, regulation of behavior, reflecting subjectively what is happening around. These processes are called mood, unlike emotions, feelings and affects, they are characterized by low intensity, but they are quite long. A natural change of mood is not distinguished by bursts of psychophysical activity. Processes can proceed smoothly, slightly lower or increase the emotional background. Mood expresses the general attitude of a person to a certain situation, and not to a certain object. Mood changes in a mentally healthy person may not have external manifestations.
Mood can change dramatically, and two opposite states are fixed - mania and depression. In case of manic syndrome, the following states are registered:
In manic syndrome, a person's instinctive actions increase - sexual desire increases, appetite increases. At the peak of the aggravation of the state, a reassessment of the personality occurs, ideas about one's own greatness arise. The patient may experience a hypomanic state, which can be called a mild degree of mania. In this state, a person has a constantly high mood, which can be observed for several days. Unlike mania, hypomania does not have psychosomatic symptoms.
The opposite state of psychophysical processes is depression. This syndrome is characterized by depression and loss of the ability to enjoy. Motor processes in depression are inhibited, mood is lowered, and thought processes are slowed down.
In bipolar disorder, mania and depression intermittently replace each other, while the process is not influenced by external factors. Episodes may follow each other or through normal mental health conditions, which are called intermissions.
The American classification of mental disorders distinguishes two types of illness. The second type differs from the first in the absence of a manic stage: depression is replaced by hypomanic episodes. Regardless of the type of bipolar disorder, a person's mental health is fully restored during an intermission.
Depending on the course of the disease, the following types of disorders are distinguished:
Most cases of psychosis are characterized by a regular alternation of phases.
Manic depressive illness is not contagious. The main role in its manifestation belongs to hereditary and neurochemical factors. Despite the external safety of psychosis, pathology can cause serious mental illness.
Statistics
Estimates of the criteria for diagnosing manic-depressive psychosis vary not only in different countries, but are also subjective. For this reason, the number of cases of the disease varies from 0.05 to 7%. The probability of falling ill with the classic form of bipolar disorder is 2%, with other types of this pathology - 4%. Men and women suffer from bipolar disorder in different proportions, but some experts believe that women have it more often - in 65-67% of cases.
The statistics of manic-depressive psychosis does not depend on ethnicity, geographical and urban factors. Data on gender factors are contradictory, especially in adolescence. Up to 40% of boys and girls experience depression, which is associated with puberty and the formation of the psyche. Only a psychiatrist can determine with high accuracy whether this condition is part of a bipolar disorder.
Most often, manic-depressive psychosis is formed between the ages of 25 and 45, during this period the pathology occurs in 47-48% of patients. In young people from 25 to 30 years old, the bipolar form of the disorder is more often recorded. In patients older than 30 years, psychosis is formed in a unipolar form. The first manifestation of the disease is often recorded after 50 years - up to 20% of cases.
Bipolar disorder is a completely incurable disease, treatment is aimed at reducing the severity of the mental disorder, restoring the ability to control mood swings. People who have undergone a course of treatment acquire the ability to socialize, can live normally and work productively.
Causes of occurrence
The exact causes of the disease have not been established, but the following groups of factors influence the pathogenesis:
Manic-depressive illness can be caused by head trauma or brain surgery.
Separately, it is necessary to single out the psychosomatic causes that lead to bipolar disorder. In patients in childhood, an emotional blockage is formed, associated with the fact that the parent of the opposite sex does not pay due attention to the child. In adults, the cause of this type of mental disorder is an internal struggle with one's desires, when a person stops wanting to be who he is and makes attempts to go beyond his own "I". An emotional blockage can also form against the background of a refusal to help that a person is offered in a difficult life situation. The patient begins to shift the responsibility for what is happening to others and he likes that someone becomes to blame for his problems.
The cause of bipolar disorder can be a mental block, which is formed against the background of experienced mental suffering, depression. A person cannot forgive the guilty, withdraws into himself and against this background a mental disorder develops.
Manic-depressive psychosis can cause a reverse psychosomatic effect. Against the background of this disease, the following disorders may develop:
Symptoms
The symptoms of bipolar disorder depend on the phase the patient is in. Periods differ not only in the clinical picture, but also in duration. The manic phase lasts from several days to several months, the patient has the following symptoms:
In the manic phase, the patient may become addicted to gambling, extreme sports, and begin to lead a promiscuous and active sex life. A person makes inexplicable financial investments, sharply increases expenses, cannot engage in professional activities or studies. Domineering manners appear in behavior, the patient begins to dress brightly and illogically, in conversations he constantly jumps from one topic to another.
The depressive phase of bipolar disorder can last from a few weeks to one and a half to two years. The average duration is 6-7 months. Main symptoms:
During the depressive phase of bipolar disorder, the number of suicide attempts increases 15 times. This is largely due to the feeling of unjustified guilt. The risk of suicide increases if phases are mixed during bipolar disorder.
When symptoms of manic-depressive psychosis appear, the patient can rarely diagnose himself as having a problem. If relatives, friends observe a change in phases, focus on a change in behavior, and the patient refuses to admit it, then it is necessary to urgently seek medical help.
Which specialist should I contact?
Manic-depressive psychosis is treated by a psychiatrist. Special preparation for the visit is not required. The presence of one of the close people is necessary, who would objectively describe the symptoms of the disease and answer the doctor's questions. An appointment with a psychiatrist begins with an anamnesis. The doctor specifies when the symptoms of bipolar disorder first appeared, how they manifest themselves, what is the frequency between changes in mood phases, and whether they are seasonal.
During the interview, the psychiatrist finds out whether there were patients with mental illness among close relatives. The doctor clarifies the lifestyle, the presence of bad habits, chronic pathologies. After collecting the anamnesis, the psychiatrist conducts an examination of the patient. The doctor studies the reaction to questions, motor activity, conducts tests, fills out a questionnaire for behavioral disorders. The psychiatrist specifies what psychoactive substances the patient is taking, whether he does it as prescribed by the doctor. When making a diagnosis, it is necessary to reject the likelihood of diseases such as panic attack, social phobia, schizoaffective disorder.
Contact the right specialist right now
Titova Elena Alekseevna
Experience 29 years
Therapist
Contact
Kosmodemyansky Leonid Vladimirovich
Therapist
Doctor of Medical Sciences
11
Contact
Borisov Evgeny Nikolaevich
Experience 9 years
Therapist
Rheumatologist
Contact
Nazarenko Natalya Nikolaevna
Experience 43 years
Therapist
Gastroenterologist
Cardiologist
Contact
Varlakova Natalya Nikolaevna
Experience 44 years
Therapist
Gastroenterologist
Cardiologist
Contact
Bezprozvanny Andrey Borisovich
Experience 46 years
Therapist
Cardiologist
Contact
Diagnosis
The following instrumental and laboratory methods are used to accurately diagnose bipolar disorder:
Diagnosis allows the psychiatrist to exclude schizophrenic-type disorders from the diagnosis, which are treated with powerful antipsychotics in depot form. For a patient with manic-depressive psychosis, such treatment can lead to disability.
Treatment
I use combined methods to treat bipolar disorder. Drug therapy is combined with psychotherapy, a favorable background is created with the help of physiotherapy, a balanced diet and a complex of exercise therapy. Treatment consists of three main stages:
Mild cases of bipolar disorder are treated as outpatients, patients with severe mania and depression are hospitalized.
Drug therapy
In the treatment of bipolar disorder, the following drugs are used:
For outpatient treatment, the dosage must be strictly adhered to. The use of a large number of lithium preparations leads to impaired articulation, dyspepsia, and thyroid pathologies. An overdose of antipsychotics causes vomiting, can cause leukocytosis and menstrual irregularities. The use of a large number of antidepressants can be fatal.
To protect the liver from a large number of drugs used, the doctor may prescribe hepatoprotectors - Essentiale, Gepabene, Karsil.
Psychotherapeutic methods of treatment
In the treatment of manic-depressive psychosis, the following tasks are solved:
Knowledge of the main stress factors that lead to the aggravation of the disorder is an advantage. Information about the main life problems, difficult situations, conflicts at work and in the family, obtained in the process of collecting an anamnesis, allows the patient to form an adaptive mechanism. This contributes to the absence of relapses and sustainable remission of bipolar disorder.
The following methods of psychotherapy are used in the treatment of manic-depressive psychosis:
In the course of psychotherapeutic sessions, the true causes of mood swings are effectively revealed, which makes it possible to learn how to regulate the condition.
Physiotherapy in the treatment of bipolar disorder
The following methods are used:
Physiotherapy methods are complementary in the treatment of bipolar affective disorder. When choosing electroshock therapy, the written consent of the patient is required, as there is a risk of memory loss. At the same time, the method is highly effective treatment.
Therapeutic exercise
Physical exercise increases the level of endorphins, relieves psychological stress, improves mood. Exercise therapy helps fight depression and stress, but is not always helpful for manic symptoms. You can use any set of exercises that are practiced daily for 25-30 minutes. In good physical shape, you can do any amateur sport. A good effect is given by classes in the gym and swimming pool. In case of poor physical shape, they do a complex of health-improving gymnastics or replace it with walks in the fresh air, which take place at a calm pace for 30-40 minutes every day. Physical therapy classes should take place at the same time, end at least two hours before bedtime. This will help stabilize the daily routine, which has a positive effect on the treatment of bipolar disorder.
Diet for manic-depressive psychosis
Trace elements, vitamins, complex organic substances that are part of the products affect not only metabolism, but also mood changes. With bipolar disorder, the following substances must be in the diet:
Meals should be portioned, regular, 4-5 times a day. The last meal should not be heavy, as this will have a negative effect on sleep.
Doctors recommend avoiding the following foods:
The diet should be balanced, exclude smoked meats, a large number of marinades, spices.
Treatment scheme and causes of manic-depressive psychosis
When choosing a treatment for bipolar disorder, the psychiatrist takes into account the causes of the disease:
The course of treatment is long, but drug therapy and psychotherapy lead to stable remission. This allows you to avoid disability, return to your family and work.
Left untreated
Left untreated, bipolar disorder can lead to more severe mental illness. A person without medical assistance is steadily declining intellectual abilities, reduced efficiency, he can not cope with professional duties. At the depressive stage, the risk of suicide increases sharply, which causes death or severe physical consequences for the body. When symptoms of manic-depressive psychosis appear, it is recommended to immediately seek medical help.
If there is no psychiatrist in the nearest medical institution or if you need not to make public the presence of a mental illness, you can use the services of online medicine. To do this, you need access to the Internet, computer equipment - a laptop, tablet, stationary PC with a video camera or a smartphone. Through videoconferencing, the patient or a family member can contact a psychiatrist who will take an anamnesis, make a diagnosis based on tests, prescribe treatment, and make recommendations if inpatient treatment is needed.
Online medicine has important advantages:
During the consultation, it is possible to confirm or refute an already diagnosed diagnosis, adjust the course of treatment, and receive dietary recommendations.
How to help yourself
Manic-depressive disorder should be treated by doctors, but in their absence, you should try to help yourself. To stabilize the emotional state will help the rejection of alcoholic beverages, coffee and tea. It is necessary to reduce the level of anxiety, normalize sleep. Help in this tincture of motherwort or valerian. Good sedatives are herbal preparations based on lemon balm leaves, nettle, lily of the valley, chamomile, burdock root. For depression, saffron tincture is recommended. Warm baths with the addition of medicinal herbs will help stabilize the mood: mint, lemon balm, oak bark.
Aromatherapy gives good results, this is due to the fact that the centers of the brain responsible for the perception of smells are in close connection with the departments that regulate the emotional sphere. Essential oils of juniper, citrus fruits, lavender will help relieve anxiety and irritability. In depressive states - oils of rose, violet and tea tree.
With manic-depressive psychosis, which is caused by psychosomatic causes, it is necessary to do auto-training. During the sessions, you need to inspire yourself with thoughts of forgiveness for all those who have hurt in the past. It is worth concentrating on positive emotions, setting goals for yourself for the near future and the distant future, developing a plan for the implementation of your plans. It is best to connect the execution of projects with your family members, friends. This will help in socialization, will allow you to learn how to cope with anxiety.
Risks
Manic-depressive illness is not a contagious disease, but anyone can experience this pathology. The risk groups include:
High risk of developing bipolar disorder in people who have experienced psychological humiliation in childhood or grew up in dysfunctional families.
Prevention
For the prevention of manic-depressive psychosis, it is recommended to control your emotions, get enough sleep, go for walks regularly and play sports at an amateur level. In risk groups, the following preventive measures are recommended: