Theory behind cognitive behavioral therapy
Cognitive Behavior Therapy - StatPearls
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-.
StatPearls [Internet].
Show details
Search term
Suma P. Chand; Daniel P. Kuckel; Martin R. Huecker.
Author Information
Last Update: September 9, 2022.
Continuing Education Activity
In the 1960s, Aaron Beck developed cognitive behavior therapy (CBT) or cognitive therapy. Since then, it has been extensively researched and found to be effective in a large number of outcome studies for psychiatric disorders including depression, anxiety disorders, eating disorders, substance abuse, and personality disorders. It also has been demonstrated to be effective as an adjunctive treatment to medication for serious mental disorders such as bipolar disorder and schizophrenia.
CBT has been adapted and studied for children, adolescents, adults, couples, and families. This activity reviews the efficacy of CBT in both psychiatric and non-psychiatric disorders and the role of the interprofessional team in using it to improve patient outcomes.
Objectives:
Identify the key concepts of cognitive-behavioral therapy.
Describe the indications for cognitive behavioral therapy.
Outline the structure of cognitive behavioral therapy sessions.
Review the clinical significance of cognitive-behavioral therapy and its efficacy in treating common psychiatric illnesses.
Access free multiple choice questions on this topic.
Introduction
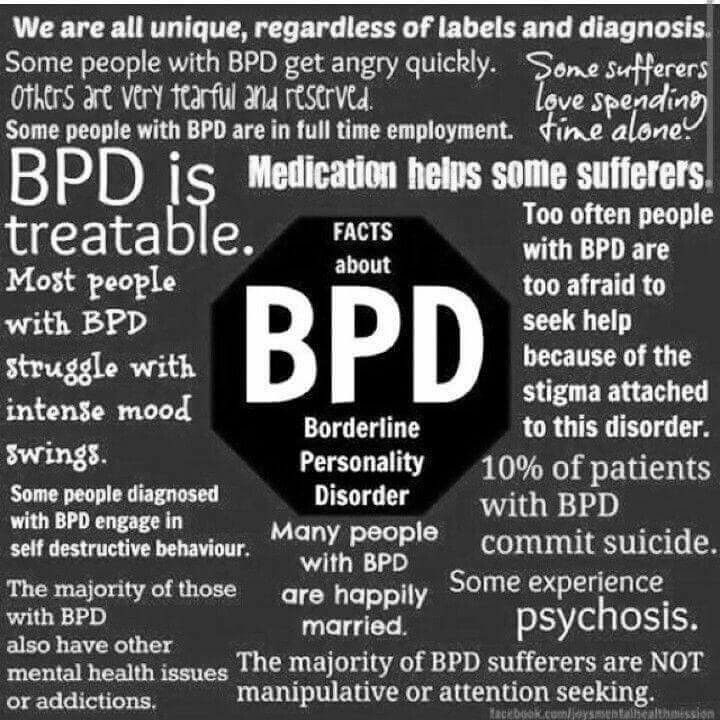
In the 1960s, Aaron Beck developed cognitive behavior therapy (CBT) or cognitive therapy. Since then, it has been extensively researched and found to be effective in a large number of outcome studies for some psychiatric disorders, including depression, anxiety disorders, eating disorders, substance abuse, and personality disorders.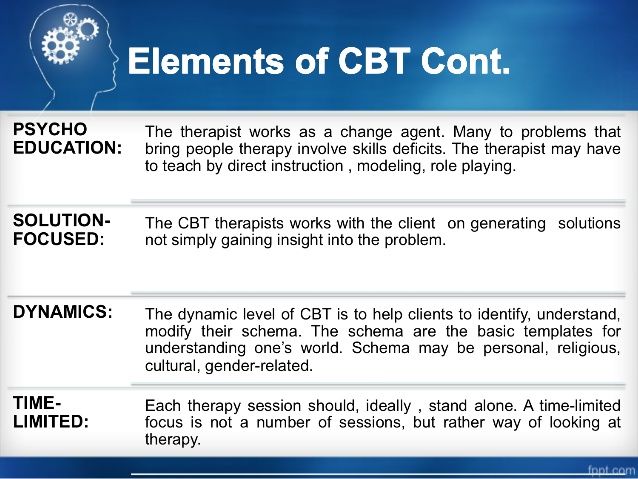 It also has been demonstrated to be effective as an adjunctive treatment to medication for serious mental disorders such as bipolar disorder and schizophrenia. CBT has been adapted and studied for children, adolescents, adults, couples, and families. Its efficacy also has been established in the treatment of non-psychiatric disorders such as irritable bowel syndrome, chronic fatigue syndrome, fibromyalgia, insomnia, migraines, and other chronic pain conditions.[1][2][3]
It also has been demonstrated to be effective as an adjunctive treatment to medication for serious mental disorders such as bipolar disorder and schizophrenia. CBT has been adapted and studied for children, adolescents, adults, couples, and families. Its efficacy also has been established in the treatment of non-psychiatric disorders such as irritable bowel syndrome, chronic fatigue syndrome, fibromyalgia, insomnia, migraines, and other chronic pain conditions.[1][2][3]
Issues of Concern
Origins of Cognitive Behavior Therapy
The idea for developing this form of psychotherapy took root when Aaron Beck began to notice that his patients with depression often verbalized thoughts that were lacking in validity and noted characteristic “cognitive distortions” in their thinking. His empirical observations led him to start viewing depression not so much as a mood disorder but as a cognitive disorder. Based on his clinical observations and empirical findings, Beck outlined a new cognitive theory of depression.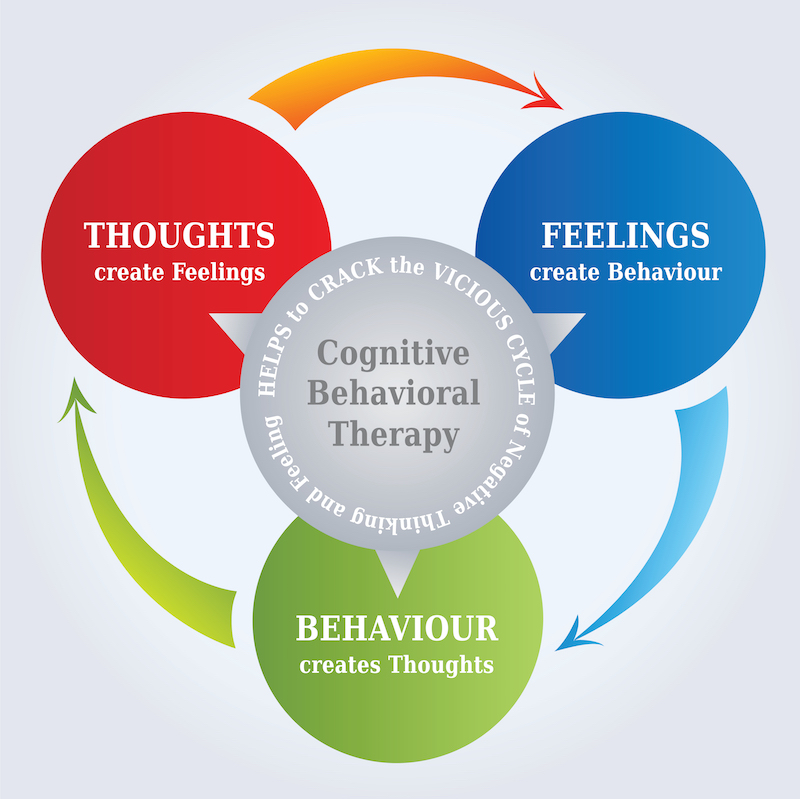 He published Cognitive Therapy for Depression (Beck, Rush, Shaw, and Emery, 1979) after having published a study that evaluated and demonstrated the efficacy of cognitive therapy. The combination of a detailed treatment protocol manual with outcome research was an innovation in psychotherapy practice that had only previously been attempted by behavior therapists in treating discrete behavioral problems. By accomplishing the same feat with a more complex set of clinical interventions that included cognitive, emotional, and behavioral components, Beck pioneered a model for what psychologists many years later defined as an “empirically validated psychological treatment.”
He published Cognitive Therapy for Depression (Beck, Rush, Shaw, and Emery, 1979) after having published a study that evaluated and demonstrated the efficacy of cognitive therapy. The combination of a detailed treatment protocol manual with outcome research was an innovation in psychotherapy practice that had only previously been attempted by behavior therapists in treating discrete behavioral problems. By accomplishing the same feat with a more complex set of clinical interventions that included cognitive, emotional, and behavioral components, Beck pioneered a model for what psychologists many years later defined as an “empirically validated psychological treatment.”
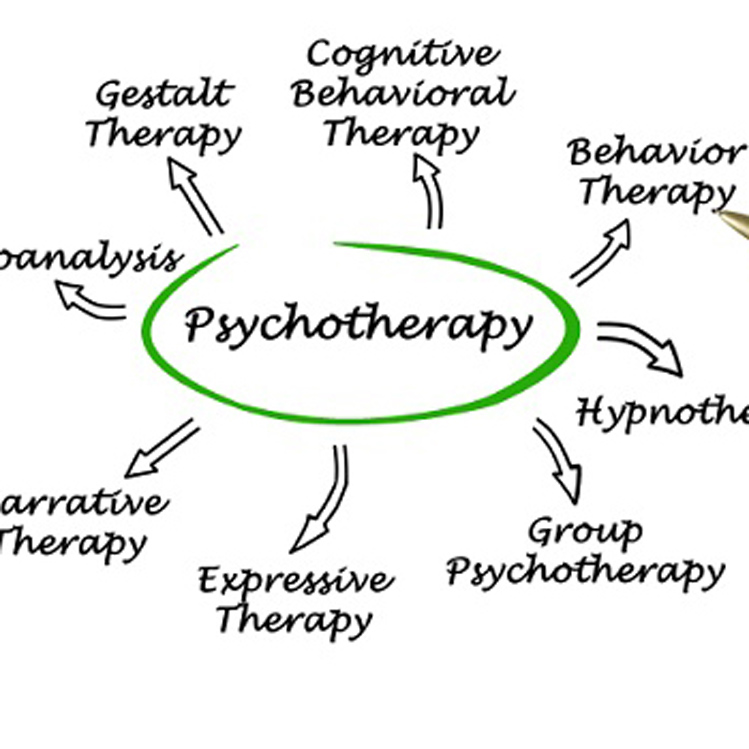
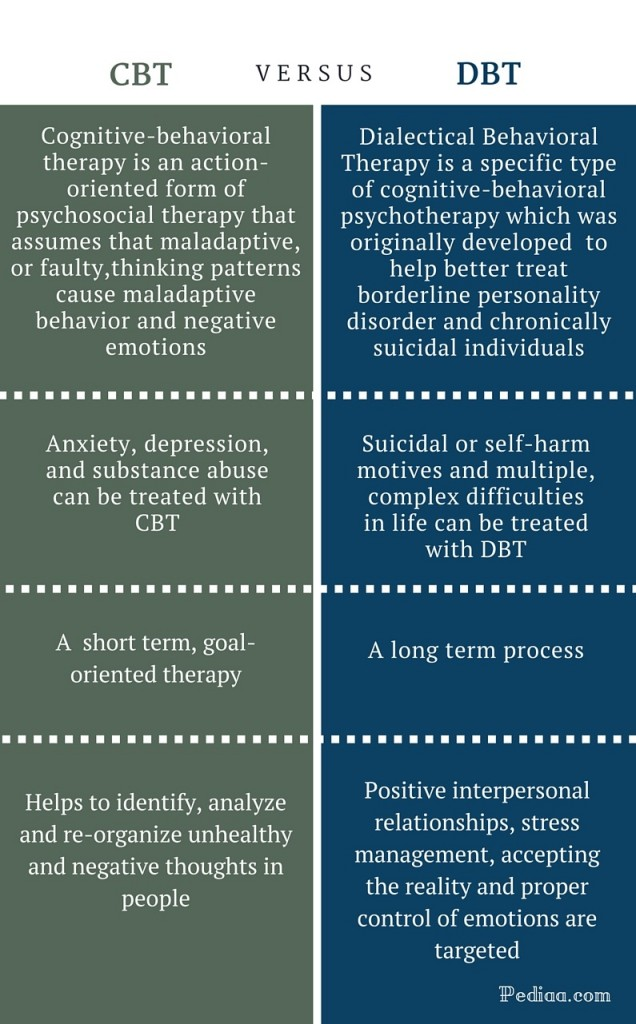
Other clinicians and researchers became interested and began developing CBT treatment protocols and evaluating their efficacy. Specific treatment protocols were developed for some psychiatric disorders. As behavioral strategies were incorporated, the term cognitive therapy changed to cognitive behavior therapy. Today CBT is the most extensively researched of all psychotherapies with several evidence-based treatment protocols.
Today CBT is the most extensively researched of all psychotherapies with several evidence-based treatment protocols.
Cognitive Model
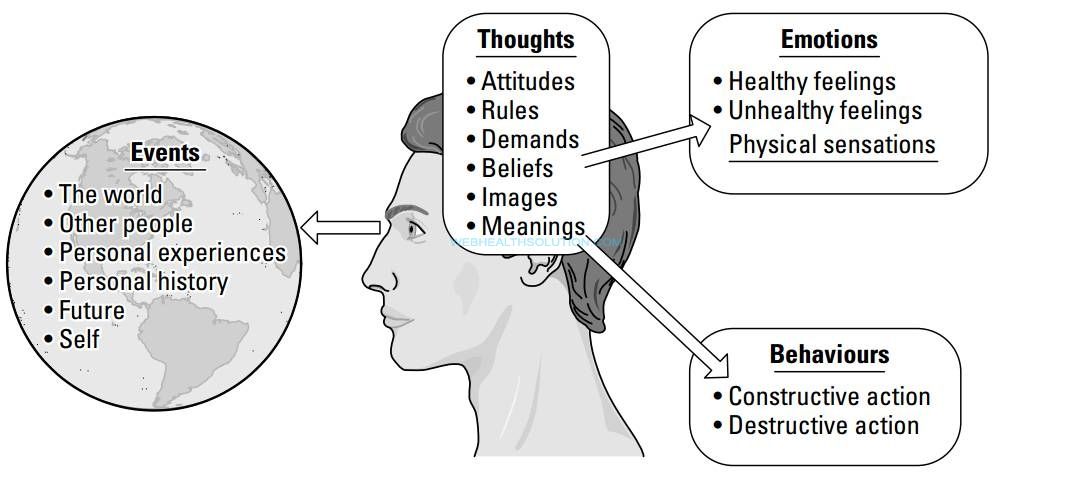
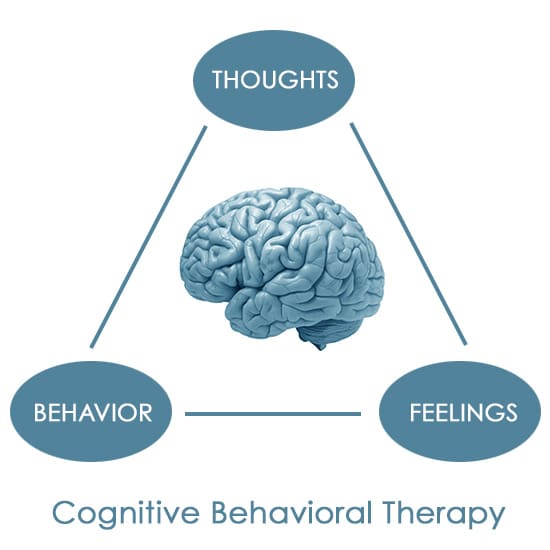
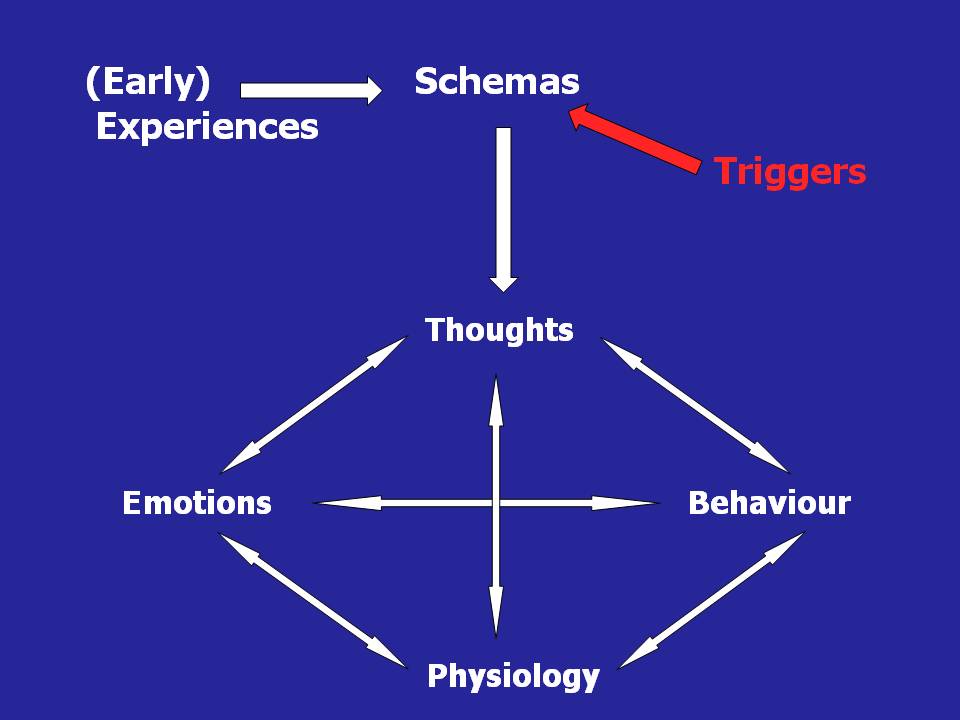
CBT is based on a straightforward, common-sense model of the relationships among cognition, emotion, and behavior.[4][5][6][7]
Three aspects of cognition are emphasized:
Automatic thoughts
Cognitive distortions
Underlying beliefs or schemas
Automatic Thoughts
An individual’s immediate, unpremeditated interpretations of events are referred to as automatic thoughts. Automatic thoughts shape both the individual’s emotions and their actions in response to events. For example, a friend may cross you in the hallway and not say hello to you. If you were to have an automatic thought of “he hates me,” or “I have done something to anger him,” it is likely to impact your mood and cause you to feel upset and also to behave in an avoidant manner when you see him next.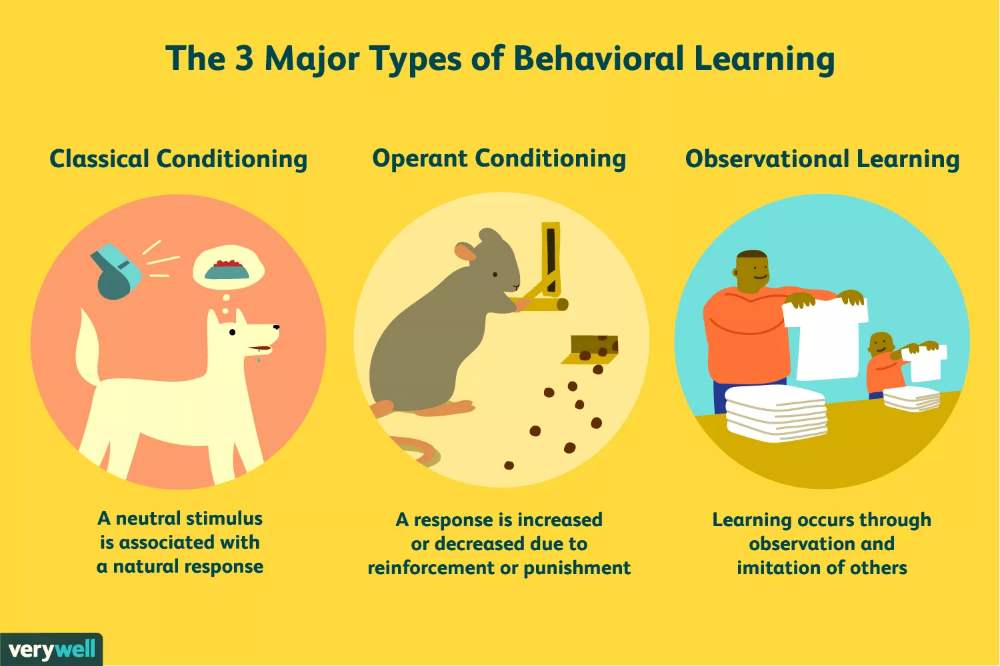 On the other hand, if you had the automatic thought, “he is in a hurry,” you would not be too concerned, and you would not be avoidant when you were to see him next.
On the other hand, if you had the automatic thought, “he is in a hurry,” you would not be too concerned, and you would not be avoidant when you were to see him next.
CBT is based on the observation that dysfunctional automatic thoughts that are exaggerated, distorted, mistaken, or unrealistic in other ways, play a significant role in psychopathology.
Cognitive Distortions
Errors in logic are quite prevalent in patients with psychological disorders. They lead individuals to erroneous conclusions. Below are some cognitive distortions that are commonly seen in individuals with psychopathology:
Dichotomous thinking: Things are seen regarding two mutually exclusive categories with no shades of gray in between.
Overgeneralization: Taking isolated cases and using them to make wide generalizations.
Selective abstraction: Focusing exclusively on certain, usually negative or upsetting, aspects of something while ignoring the rest.
Disqualifying the positive: Positive experiences that conflict with the individual’s negative views are discounted.
Mind reading: Assuming the thoughts and intentions of others.
Fortune telling: Predicting how things will turn out before they happen.
Minimization: Positive characteristics or experiences are treated as real but insignificant.
Catastrophizing: Focusing on the worst possible outcome, however unlikely, or thinking that a situation is unbearable or impossible when it is just uncomfortable.
Emotional reasoning: Making decisions and arguments based on how you feel rather than objective reality.
“Should” statements: Concentrating on what you think “should” or “ought to be” rather than the actual situation you are faced with or having rigid rules which you always apply no matter the circumstances.
Personalization, blame, or attribution: Assuming you are completely or directly responsible for a negative outcome.
 When applied to others consistently, the blame is the distortion.
When applied to others consistently, the blame is the distortion.
Underlying Beliefs
Underlying beliefs shape the perception and interpretation of events. Belief systems or schemas take shape as we go through life experiences. They are defined as templates or rules for information processing that underlie the most superficial layer of automatic thoughts. Beliefs are understood at two levels in CBT:
Core Beliefs
The central ideas about self and the world
The most fundamental level of belief
They are global, rigid, and overgeneralized
Examples of dysfunctional core beliefs:
Intermediate Beliefs
Consist of assumptions, attitudes, and rules
Influenced in their development by the core beliefs
Examples of dysfunctional intermediate beliefs:
“To be accepted, I should always please others.”
“I should be excellent at everything I do to be considered adequate.
 ”
”“It is best to have as little as possible to do with people.”
Clinical Significance
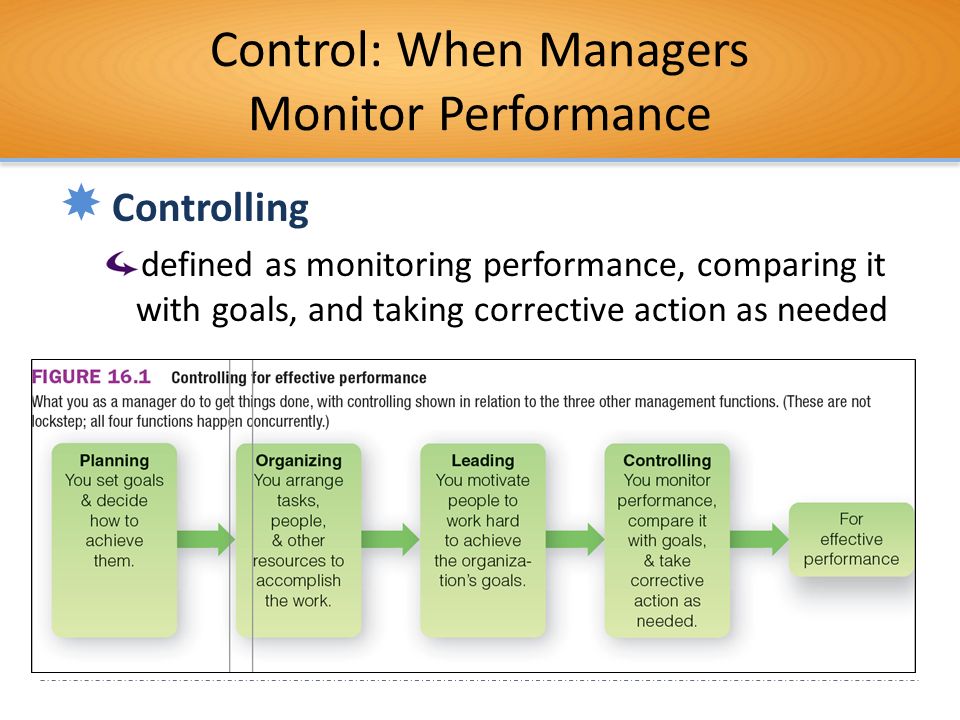
Cognitive behavior therapy is a structured, didactic, and goal-oriented form of therapy. The approach is hands-on and practical wherein the therapist and patient work in a collaborative manner with the goal of modifying patterns of thinking and behavior to bring about a beneficial change in the patient's mood and way of living his/her life. It is used to help a wide range of problems, and appropriate treatment protocols are applied depending on the diagnosis and problems the patient is facing.[8][9][10][11]
Most psychotherapists who practice CBT personalize and customize the therapy to the specific needs of each patient.
The first step is an assessment of the patient and the initiation of developing an individualized conceptualization of him/her. The conceptualization based on the CBT model is built from session to session and is shared with the patient at an appropriate time later in therapy.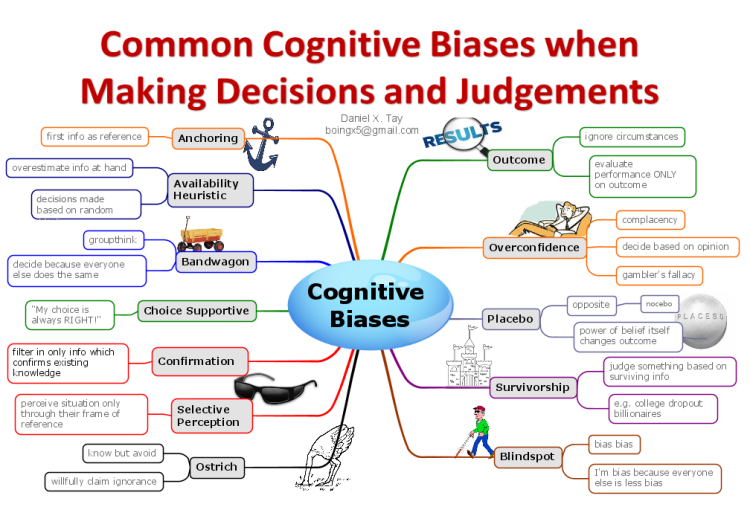 The approach to therapy is explained very early at the start of the therapy. The problems patient would like to work on in therapy, and goals for therapy are decided in the first or second session collaboratively. The prioritized problems are worked on first.
The approach to therapy is explained very early at the start of the therapy. The problems patient would like to work on in therapy, and goals for therapy are decided in the first or second session collaboratively. The prioritized problems are worked on first.
The structure of each session:
The session always starts with a brief update and check on mood. This is followed by bridging from the previous session to establish continuity. The agenda of what will be talked about in the session is set up collaboratively, and the homework the patient had to do between the sessions is reviewed before plunging into talking about any problem. Issues on the agenda are talked about punctuated with feedback and summaries. The session ends with setting up further homework and a final summary.
Examples of CBT in practice:
Anxiety: CBT often focuses on replacing negative automatic thoughts that can occur in generalized anxiety disorder and may be used alone or in combination with medications such as selective serotonin reuptake inhibitors, which are typically first-line as benzodiazepines have a greater risk of adverse outcomes.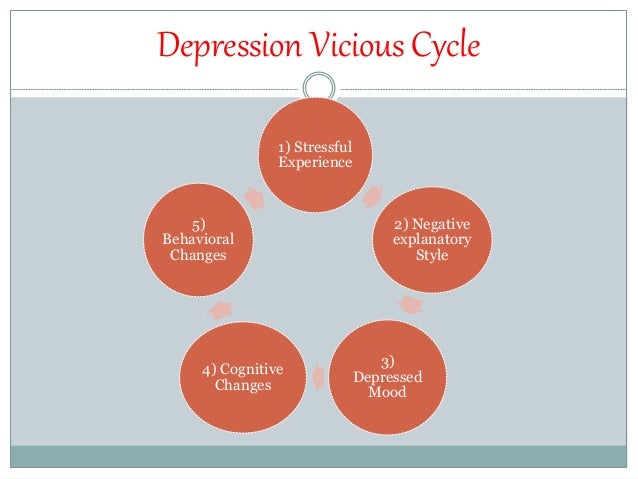 In treating panic disorder, CBT may include desensitization to triggers that provoke anxiety; it is important to note, however, that a potential adverse effect of this technique is a temporary mild increase in anxiety.[12]
In treating panic disorder, CBT may include desensitization to triggers that provoke anxiety; it is important to note, however, that a potential adverse effect of this technique is a temporary mild increase in anxiety.[12]
Depression: In patients with chronic depression, the combination of CBT and antidepressant medication is more effective than either intervention alone. In patients who are no longer taking part in activities that typically bring them pleasure, CBT may initially focus on reinitiating positive activities to overcome inertia.[13]
Attention deficit hyperactivity disorder (ADHD): Behavioral therapy is the initial recommended treatment for children younger than 6 years old, while stimulant medications are the recommended initial intervention for ADHD in children 6 years and older. Behavioral treatments are also recommended for older children, especially if they have a poor response or adverse effects on medication. Behavioral therapy interventions include parent training and behavioral classroom management with a focus on setting clear rules and expectations for the child with appropriate rewards and punishments and daily feedback.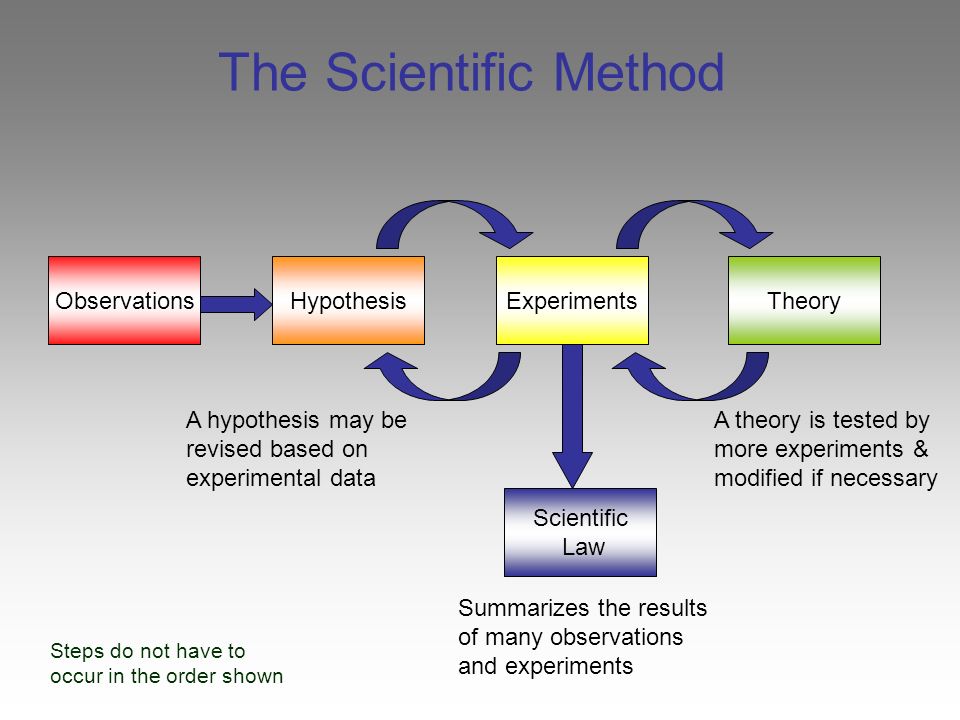 [14][15]
[14][15]
Typical CBT treatments involve approximately 60-minute sessions occurring weekly for 8 to 12 weeks.[15]
Enhancing Healthcare Team Outcomes
CBT is a valid and proven form of psychological therapy for a range of mental health disorders. It is important for physicians and nurses to understand that CBT is often used in conjunction with pharmacological therapy to achieve the best outcomes. Moreover, CBT has been shown to provide additional benefits or similar outcomes compared to medication alone. Patients with psychiatric disorders should be referred to a mental health nurse who can educate the patient on treatment options. Primary care physicians are encouraged to develop collaborative relationships with behavior therapists and introduce and monitor the progress of cognitive-behavioral therapy. An interprofessional team approach will result in the best outcomes.[16][17][15]
Review Questions
Access free multiple choice questions on this topic.

Comment on this article.
References
- 1.
van den Berk Clark C, Moore R, Secrest S, Tuerk P, Norman S, Myers U, Lustman PJ, Schneider FD, Barnes J, Gallamore R, Ovais M, Plurad JA, Scherrer JF. Factors Associated With Receipt of Cognitive-Behavioral Therapy or Prolonged Exposure Therapy Among Individuals With PTSD. Psychiatr Serv. 2019 Aug 01;70(8):703-713. [PMC free article: PMC6702958] [PubMed: 31010409]
- 2.
Keefe JR, Chambless DL, Barber JP, Milrod BL. Treatment of anxiety and mood comorbidities in cognitive-behavioral and psychodynamic therapies for panic disorder. J Psychiatr Res. 2019 Jul;114:34-40. [PubMed: 31015099]
- 3.
Zilcha-Mano S, Eubanks CF, Muran JC. Sudden gains in the alliance in cognitive behavioral therapy versus brief relational therapy. J Consult Clin Psychol. 2019 Jun;87(6):501-509. [PMC free article: PMC6533161] [PubMed: 31008637]
- 4.
de Jonge M, Bockting CLH, Kikkert MJ, van Dijk MK, van Schaik DJF, Peen J, Hollon SD, Dekker JJM.
 Preventive cognitive therapy versus care as usual in cognitive behavioral therapy responders: A randomized controlled trial. J Consult Clin Psychol. 2019 Jun;87(6):521-529. [PubMed: 31008635]
Preventive cognitive therapy versus care as usual in cognitive behavioral therapy responders: A randomized controlled trial. J Consult Clin Psychol. 2019 Jun;87(6):521-529. [PubMed: 31008635]- 5.
Tolin DF, Wootton BM, Levy HC, Hallion LS, Worden BL, Diefenbach GJ, Jaccard J, Stevens MC. Efficacy and mediators of a group cognitive-behavioral therapy for hoarding disorder: A randomized trial. J Consult Clin Psychol. 2019 Jul;87(7):590-602. [PubMed: 31008633]
- 6.
Heenan A, Pipe A, Lemay K, Davidson JR, Tulloch H. Cognitive-Behavioral Therapy for Insomnia Tailored to Patients With Cardiovascular Disease: A Pre-Post Study. Behav Sleep Med. 2020 May-Jun;18(3):372-385. [PubMed: 31007057]
- 7.
Janse A, Bleijenberg G, Knoop H. Prediction of long-term outcome after cognitive behavioral therapy for chronic fatigue syndrome. J Psychosom Res. 2019 Jun;121:93-99. [PubMed: 31006534]
- 8.
Webb CA, Stanton CH, Bondy E, Singleton P, Pizzagalli DA, Auerbach RP.
 Cognitive versus behavioral skills in CBT for depressed adolescents: Disaggregating within-patient versus between-patient effects on symptom change. J Consult Clin Psychol. 2019 May;87(5):484-490. [PMC free article: PMC6506214] [PubMed: 30998049]
Cognitive versus behavioral skills in CBT for depressed adolescents: Disaggregating within-patient versus between-patient effects on symptom change. J Consult Clin Psychol. 2019 May;87(5):484-490. [PMC free article: PMC6506214] [PubMed: 30998049]- 9.
Cuijpers P, Noma H, Karyotaki E, Cipriani A, Furukawa TA. Effectiveness and Acceptability of Cognitive Behavior Therapy Delivery Formats in Adults With Depression: A Network Meta-analysis. JAMA Psychiatry. 2019 Jul 01;76(7):700-707. [PMC free article: PMC6583673] [PubMed: 30994877]
- 10.
O'Cleirigh C, Safren SA, Taylor SW, Goshe BM, Bedoya CA, Marquez SM, Boroughs MS, Shipherd JC. Cognitive Behavioral Therapy for Trauma and Self-Care (CBT-TSC) in Men Who have Sex with Men with a History of Childhood Sexual Abuse: A Randomized Controlled Trial. AIDS Behav. 2019 Sep;23(9):2421-2431. [PMC free article: PMC7271561] [PubMed: 30993478]
- 11.
Sahranavard S, Esmaeili A, Salehiniya H, Behdani S.
 The effectiveness of group training of cognitive behavioral therapy-based stress management on anxiety, hardiness and self-efficacy in female medical students. J Educ Health Promot. 2019;8:49. [PMC free article: PMC6432834] [PubMed: 30993142]
The effectiveness of group training of cognitive behavioral therapy-based stress management on anxiety, hardiness and self-efficacy in female medical students. J Educ Health Promot. 2019;8:49. [PMC free article: PMC6432834] [PubMed: 30993142]- 12.
Locke AB, Kirst N, Shultz CG. Diagnosis and management of generalized anxiety disorder and panic disorder in adults. Am Fam Physician. 2015 May 01;91(9):617-24. [PubMed: 25955736]
- 13.
Rupke SJ, Blecke D, Renfrow M. Cognitive therapy for depression. Am Fam Physician. 2006 Jan 01;73(1):83-6. [PubMed: 16417069]
- 14.
Felt BT, Biermann B, Christner JG, Kochhar P, Harrison RV. Diagnosis and management of ADHD in children. Am Fam Physician. 2014 Oct 01;90(7):456-64. [PubMed: 25369623]
- 15.
Coffey SF, Banducci AN, Vinci C. Common Questions About Cognitive Behavior Therapy for Psychiatric Disorders. Am Fam Physician. 2015 Nov 01;92(9):807-12. [PubMed: 26554473]
- 16.
Wu CY, Rodakowski JL, Terhorst L, Karp JF, Fields B, Skidmore ER. A Scoping Review of Nonpharmacological Interventions to Reduce Disability in Older Adults. Gerontologist. 2020 Jan 24;60(1):e52-e65. [PMC free article: PMC7182004] [PubMed: 31002312]
- 17.
Ngamkham S, Holden JE, Smith EL. A Systematic Review: Mindfulness Intervention for Cancer-Related Pain. Asia Pac J Oncol Nurs. 2019 Apr-Jun;6(2):161-169. [PMC free article: PMC6371675] [PubMed: 30931361]
Copyright © 2022, StatPearls Publishing LLC.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.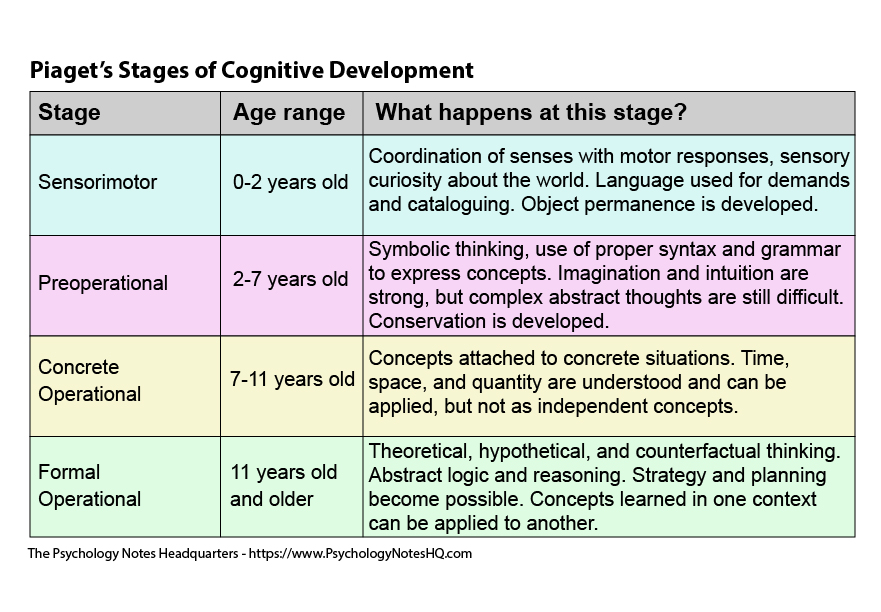
Bookshelf ID: NBK470241PMID: 29261869
Cognitive Behavior Therapy - StatPearls
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-.
StatPearls [Internet].
Show details
Search term
Suma P. Chand; Daniel P. Kuckel; Martin R. Huecker.
Author Information
Last Update: September 9, 2022.
Continuing Education Activity
In the 1960s, Aaron Beck developed cognitive behavior therapy (CBT) or cognitive therapy. Since then, it has been extensively researched and found to be effective in a large number of outcome studies for psychiatric disorders including depression, anxiety disorders, eating disorders, substance abuse, and personality disorders. It also has been demonstrated to be effective as an adjunctive treatment to medication for serious mental disorders such as bipolar disorder and schizophrenia.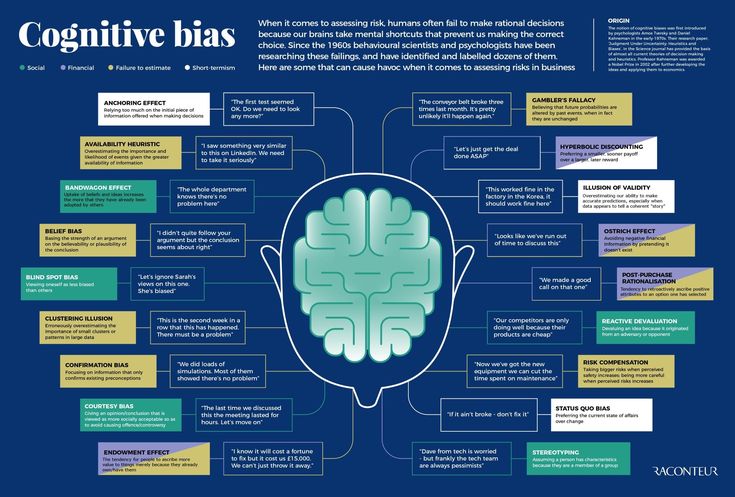 CBT has been adapted and studied for children, adolescents, adults, couples, and families. This activity reviews the efficacy of CBT in both psychiatric and non-psychiatric disorders and the role of the interprofessional team in using it to improve patient outcomes.
CBT has been adapted and studied for children, adolescents, adults, couples, and families. This activity reviews the efficacy of CBT in both psychiatric and non-psychiatric disorders and the role of the interprofessional team in using it to improve patient outcomes.
Objectives:
Identify the key concepts of cognitive-behavioral therapy.
Describe the indications for cognitive behavioral therapy.
Outline the structure of cognitive behavioral therapy sessions.
Review the clinical significance of cognitive-behavioral therapy and its efficacy in treating common psychiatric illnesses.
Access free multiple choice questions on this topic.
Introduction
In the 1960s, Aaron Beck developed cognitive behavior therapy (CBT) or cognitive therapy. Since then, it has been extensively researched and found to be effective in a large number of outcome studies for some psychiatric disorders, including depression, anxiety disorders, eating disorders, substance abuse, and personality disorders.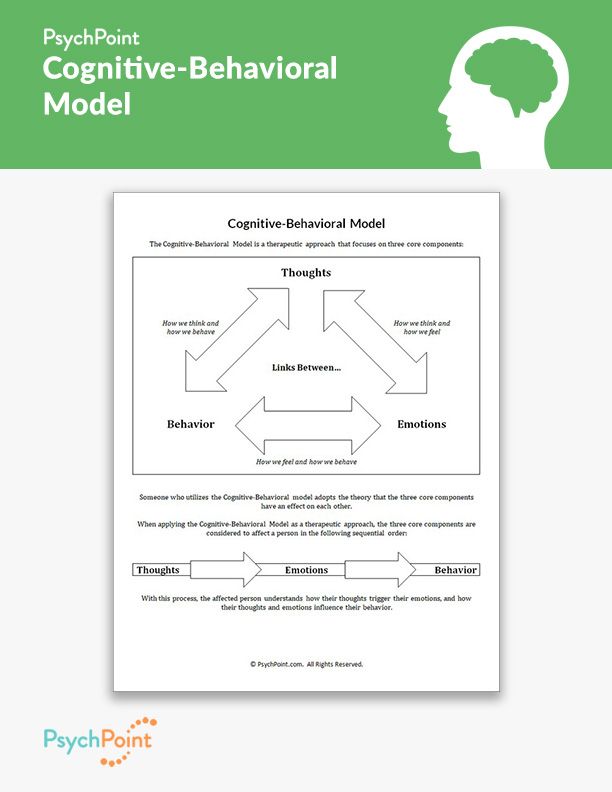 It also has been demonstrated to be effective as an adjunctive treatment to medication for serious mental disorders such as bipolar disorder and schizophrenia. CBT has been adapted and studied for children, adolescents, adults, couples, and families. Its efficacy also has been established in the treatment of non-psychiatric disorders such as irritable bowel syndrome, chronic fatigue syndrome, fibromyalgia, insomnia, migraines, and other chronic pain conditions.[1][2][3]
It also has been demonstrated to be effective as an adjunctive treatment to medication for serious mental disorders such as bipolar disorder and schizophrenia. CBT has been adapted and studied for children, adolescents, adults, couples, and families. Its efficacy also has been established in the treatment of non-psychiatric disorders such as irritable bowel syndrome, chronic fatigue syndrome, fibromyalgia, insomnia, migraines, and other chronic pain conditions.[1][2][3]
Issues of Concern
Origins of Cognitive Behavior Therapy
The idea for developing this form of psychotherapy took root when Aaron Beck began to notice that his patients with depression often verbalized thoughts that were lacking in validity and noted characteristic “cognitive distortions” in their thinking. His empirical observations led him to start viewing depression not so much as a mood disorder but as a cognitive disorder. Based on his clinical observations and empirical findings, Beck outlined a new cognitive theory of depression.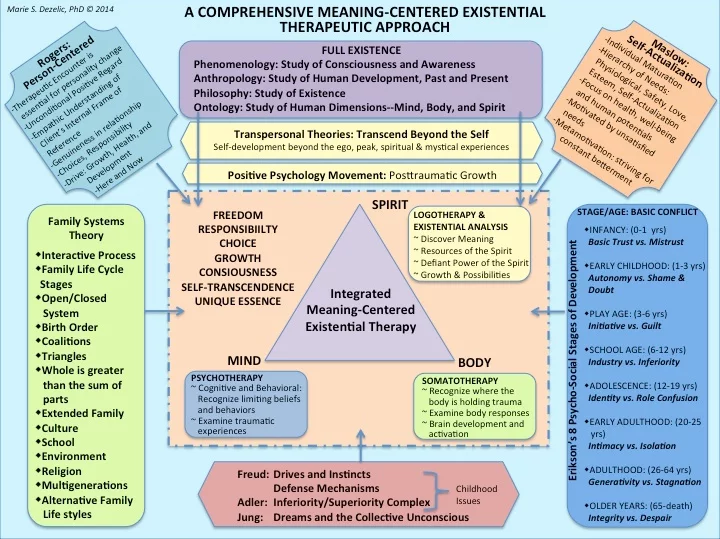 He published Cognitive Therapy for Depression (Beck, Rush, Shaw, and Emery, 1979) after having published a study that evaluated and demonstrated the efficacy of cognitive therapy. The combination of a detailed treatment protocol manual with outcome research was an innovation in psychotherapy practice that had only previously been attempted by behavior therapists in treating discrete behavioral problems. By accomplishing the same feat with a more complex set of clinical interventions that included cognitive, emotional, and behavioral components, Beck pioneered a model for what psychologists many years later defined as an “empirically validated psychological treatment.”
He published Cognitive Therapy for Depression (Beck, Rush, Shaw, and Emery, 1979) after having published a study that evaluated and demonstrated the efficacy of cognitive therapy. The combination of a detailed treatment protocol manual with outcome research was an innovation in psychotherapy practice that had only previously been attempted by behavior therapists in treating discrete behavioral problems. By accomplishing the same feat with a more complex set of clinical interventions that included cognitive, emotional, and behavioral components, Beck pioneered a model for what psychologists many years later defined as an “empirically validated psychological treatment.”
Other clinicians and researchers became interested and began developing CBT treatment protocols and evaluating their efficacy. Specific treatment protocols were developed for some psychiatric disorders. As behavioral strategies were incorporated, the term cognitive therapy changed to cognitive behavior therapy. Today CBT is the most extensively researched of all psychotherapies with several evidence-based treatment protocols.
Today CBT is the most extensively researched of all psychotherapies with several evidence-based treatment protocols.
Cognitive Model
CBT is based on a straightforward, common-sense model of the relationships among cognition, emotion, and behavior.[4][5][6][7]
Three aspects of cognition are emphasized:
Automatic thoughts
Cognitive distortions
Underlying beliefs or schemas
Automatic Thoughts
An individual’s immediate, unpremeditated interpretations of events are referred to as automatic thoughts. Automatic thoughts shape both the individual’s emotions and their actions in response to events. For example, a friend may cross you in the hallway and not say hello to you. If you were to have an automatic thought of “he hates me,” or “I have done something to anger him,” it is likely to impact your mood and cause you to feel upset and also to behave in an avoidant manner when you see him next.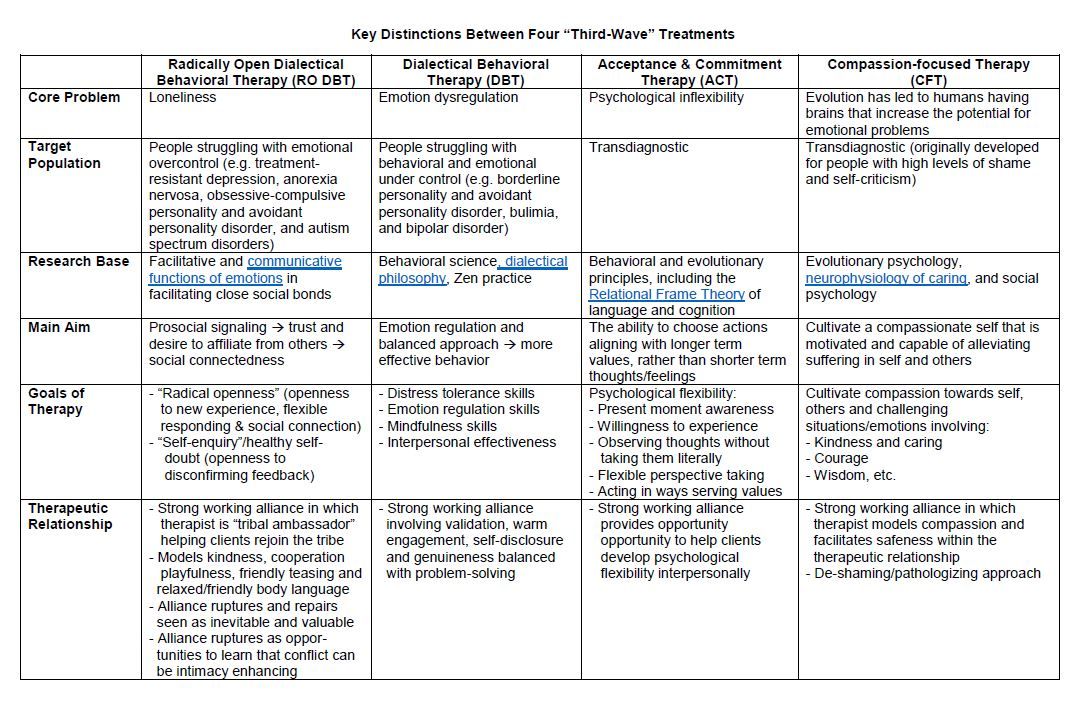 On the other hand, if you had the automatic thought, “he is in a hurry,” you would not be too concerned, and you would not be avoidant when you were to see him next.
On the other hand, if you had the automatic thought, “he is in a hurry,” you would not be too concerned, and you would not be avoidant when you were to see him next.
CBT is based on the observation that dysfunctional automatic thoughts that are exaggerated, distorted, mistaken, or unrealistic in other ways, play a significant role in psychopathology.
Cognitive Distortions
Errors in logic are quite prevalent in patients with psychological disorders. They lead individuals to erroneous conclusions. Below are some cognitive distortions that are commonly seen in individuals with psychopathology:
Dichotomous thinking: Things are seen regarding two mutually exclusive categories with no shades of gray in between.
Overgeneralization: Taking isolated cases and using them to make wide generalizations.
Selective abstraction: Focusing exclusively on certain, usually negative or upsetting, aspects of something while ignoring the rest.
Disqualifying the positive: Positive experiences that conflict with the individual’s negative views are discounted.
Mind reading: Assuming the thoughts and intentions of others.
Fortune telling: Predicting how things will turn out before they happen.
Minimization: Positive characteristics or experiences are treated as real but insignificant.
Catastrophizing: Focusing on the worst possible outcome, however unlikely, or thinking that a situation is unbearable or impossible when it is just uncomfortable.
Emotional reasoning: Making decisions and arguments based on how you feel rather than objective reality.
“Should” statements: Concentrating on what you think “should” or “ought to be” rather than the actual situation you are faced with or having rigid rules which you always apply no matter the circumstances.
Personalization, blame, or attribution: Assuming you are completely or directly responsible for a negative outcome.
 When applied to others consistently, the blame is the distortion.
When applied to others consistently, the blame is the distortion.
Underlying Beliefs
Underlying beliefs shape the perception and interpretation of events. Belief systems or schemas take shape as we go through life experiences. They are defined as templates or rules for information processing that underlie the most superficial layer of automatic thoughts. Beliefs are understood at two levels in CBT:
Core Beliefs
The central ideas about self and the world
The most fundamental level of belief
They are global, rigid, and overgeneralized
Examples of dysfunctional core beliefs:
Intermediate Beliefs
Consist of assumptions, attitudes, and rules
Influenced in their development by the core beliefs
Examples of dysfunctional intermediate beliefs:
“To be accepted, I should always please others.”
“I should be excellent at everything I do to be considered adequate.
 ”
”“It is best to have as little as possible to do with people.”
Clinical Significance
Cognitive behavior therapy is a structured, didactic, and goal-oriented form of therapy. The approach is hands-on and practical wherein the therapist and patient work in a collaborative manner with the goal of modifying patterns of thinking and behavior to bring about a beneficial change in the patient's mood and way of living his/her life. It is used to help a wide range of problems, and appropriate treatment protocols are applied depending on the diagnosis and problems the patient is facing.[8][9][10][11]
Most psychotherapists who practice CBT personalize and customize the therapy to the specific needs of each patient.
The first step is an assessment of the patient and the initiation of developing an individualized conceptualization of him/her. The conceptualization based on the CBT model is built from session to session and is shared with the patient at an appropriate time later in therapy. The approach to therapy is explained very early at the start of the therapy. The problems patient would like to work on in therapy, and goals for therapy are decided in the first or second session collaboratively. The prioritized problems are worked on first.
The structure of each session:
The session always starts with a brief update and check on mood. This is followed by bridging from the previous session to establish continuity. The agenda of what will be talked about in the session is set up collaboratively, and the homework the patient had to do between the sessions is reviewed before plunging into talking about any problem. Issues on the agenda are talked about punctuated with feedback and summaries. The session ends with setting up further homework and a final summary.
Examples of CBT in practice:
Anxiety: CBT often focuses on replacing negative automatic thoughts that can occur in generalized anxiety disorder and may be used alone or in combination with medications such as selective serotonin reuptake inhibitors, which are typically first-line as benzodiazepines have a greater risk of adverse outcomes. In treating panic disorder, CBT may include desensitization to triggers that provoke anxiety; it is important to note, however, that a potential adverse effect of this technique is a temporary mild increase in anxiety.[12]
In treating panic disorder, CBT may include desensitization to triggers that provoke anxiety; it is important to note, however, that a potential adverse effect of this technique is a temporary mild increase in anxiety.[12]
Depression: In patients with chronic depression, the combination of CBT and antidepressant medication is more effective than either intervention alone. In patients who are no longer taking part in activities that typically bring them pleasure, CBT may initially focus on reinitiating positive activities to overcome inertia.[13]
Attention deficit hyperactivity disorder (ADHD): Behavioral therapy is the initial recommended treatment for children younger than 6 years old, while stimulant medications are the recommended initial intervention for ADHD in children 6 years and older. Behavioral treatments are also recommended for older children, especially if they have a poor response or adverse effects on medication. Behavioral therapy interventions include parent training and behavioral classroom management with a focus on setting clear rules and expectations for the child with appropriate rewards and punishments and daily feedback.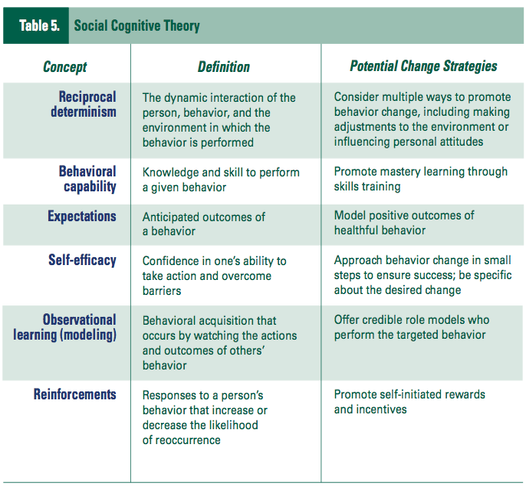 [14][15]
[14][15]
Typical CBT treatments involve approximately 60-minute sessions occurring weekly for 8 to 12 weeks.[15]
Enhancing Healthcare Team Outcomes
CBT is a valid and proven form of psychological therapy for a range of mental health disorders. It is important for physicians and nurses to understand that CBT is often used in conjunction with pharmacological therapy to achieve the best outcomes. Moreover, CBT has been shown to provide additional benefits or similar outcomes compared to medication alone. Patients with psychiatric disorders should be referred to a mental health nurse who can educate the patient on treatment options. Primary care physicians are encouraged to develop collaborative relationships with behavior therapists and introduce and monitor the progress of cognitive-behavioral therapy. An interprofessional team approach will result in the best outcomes.[16][17][15]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
van den Berk Clark C, Moore R, Secrest S, Tuerk P, Norman S, Myers U, Lustman PJ, Schneider FD, Barnes J, Gallamore R, Ovais M, Plurad JA, Scherrer JF. Factors Associated With Receipt of Cognitive-Behavioral Therapy or Prolonged Exposure Therapy Among Individuals With PTSD. Psychiatr Serv. 2019 Aug 01;70(8):703-713. [PMC free article: PMC6702958] [PubMed: 31010409]
- 2.
Keefe JR, Chambless DL, Barber JP, Milrod BL. Treatment of anxiety and mood comorbidities in cognitive-behavioral and psychodynamic therapies for panic disorder. J Psychiatr Res. 2019 Jul;114:34-40. [PubMed: 31015099]
- 3.
Zilcha-Mano S, Eubanks CF, Muran JC. Sudden gains in the alliance in cognitive behavioral therapy versus brief relational therapy. J Consult Clin Psychol. 2019 Jun;87(6):501-509. [PMC free article: PMC6533161] [PubMed: 31008637]
- 4.
de Jonge M, Bockting CLH, Kikkert MJ, van Dijk MK, van Schaik DJF, Peen J, Hollon SD, Dekker JJM.
 Preventive cognitive therapy versus care as usual in cognitive behavioral therapy responders: A randomized controlled trial. J Consult Clin Psychol. 2019 Jun;87(6):521-529. [PubMed: 31008635]
Preventive cognitive therapy versus care as usual in cognitive behavioral therapy responders: A randomized controlled trial. J Consult Clin Psychol. 2019 Jun;87(6):521-529. [PubMed: 31008635]- 5.
Tolin DF, Wootton BM, Levy HC, Hallion LS, Worden BL, Diefenbach GJ, Jaccard J, Stevens MC. Efficacy and mediators of a group cognitive-behavioral therapy for hoarding disorder: A randomized trial. J Consult Clin Psychol. 2019 Jul;87(7):590-602. [PubMed: 31008633]
- 6.
Heenan A, Pipe A, Lemay K, Davidson JR, Tulloch H. Cognitive-Behavioral Therapy for Insomnia Tailored to Patients With Cardiovascular Disease: A Pre-Post Study. Behav Sleep Med. 2020 May-Jun;18(3):372-385. [PubMed: 31007057]
- 7.
Janse A, Bleijenberg G, Knoop H. Prediction of long-term outcome after cognitive behavioral therapy for chronic fatigue syndrome. J Psychosom Res. 2019 Jun;121:93-99. [PubMed: 31006534]
- 8.
Webb CA, Stanton CH, Bondy E, Singleton P, Pizzagalli DA, Auerbach RP.
 Cognitive versus behavioral skills in CBT for depressed adolescents: Disaggregating within-patient versus between-patient effects on symptom change. J Consult Clin Psychol. 2019 May;87(5):484-490. [PMC free article: PMC6506214] [PubMed: 30998049]
Cognitive versus behavioral skills in CBT for depressed adolescents: Disaggregating within-patient versus between-patient effects on symptom change. J Consult Clin Psychol. 2019 May;87(5):484-490. [PMC free article: PMC6506214] [PubMed: 30998049]- 9.
Cuijpers P, Noma H, Karyotaki E, Cipriani A, Furukawa TA. Effectiveness and Acceptability of Cognitive Behavior Therapy Delivery Formats in Adults With Depression: A Network Meta-analysis. JAMA Psychiatry. 2019 Jul 01;76(7):700-707. [PMC free article: PMC6583673] [PubMed: 30994877]
- 10.
O'Cleirigh C, Safren SA, Taylor SW, Goshe BM, Bedoya CA, Marquez SM, Boroughs MS, Shipherd JC. Cognitive Behavioral Therapy for Trauma and Self-Care (CBT-TSC) in Men Who have Sex with Men with a History of Childhood Sexual Abuse: A Randomized Controlled Trial. AIDS Behav. 2019 Sep;23(9):2421-2431. [PMC free article: PMC7271561] [PubMed: 30993478]
- 11.
Sahranavard S, Esmaeili A, Salehiniya H, Behdani S.
 The effectiveness of group training of cognitive behavioral therapy-based stress management on anxiety, hardiness and self-efficacy in female medical students. J Educ Health Promot. 2019;8:49. [PMC free article: PMC6432834] [PubMed: 30993142]
The effectiveness of group training of cognitive behavioral therapy-based stress management on anxiety, hardiness and self-efficacy in female medical students. J Educ Health Promot. 2019;8:49. [PMC free article: PMC6432834] [PubMed: 30993142]- 12.
Locke AB, Kirst N, Shultz CG. Diagnosis and management of generalized anxiety disorder and panic disorder in adults. Am Fam Physician. 2015 May 01;91(9):617-24. [PubMed: 25955736]
- 13.
Rupke SJ, Blecke D, Renfrow M. Cognitive therapy for depression. Am Fam Physician. 2006 Jan 01;73(1):83-6. [PubMed: 16417069]
- 14.
Felt BT, Biermann B, Christner JG, Kochhar P, Harrison RV. Diagnosis and management of ADHD in children. Am Fam Physician. 2014 Oct 01;90(7):456-64. [PubMed: 25369623]
- 15.
Coffey SF, Banducci AN, Vinci C. Common Questions About Cognitive Behavior Therapy for Psychiatric Disorders. Am Fam Physician. 2015 Nov 01;92(9):807-12. [PubMed: 26554473]
- 16.
Wu CY, Rodakowski JL, Terhorst L, Karp JF, Fields B, Skidmore ER. A Scoping Review of Nonpharmacological Interventions to Reduce Disability in Older Adults. Gerontologist. 2020 Jan 24;60(1):e52-e65. [PMC free article: PMC7182004] [PubMed: 31002312]
- 17.
Ngamkham S, Holden JE, Smith EL. A Systematic Review: Mindfulness Intervention for Cancer-Related Pain. Asia Pac J Oncol Nurs. 2019 Apr-Jun;6(2):161-169. [PMC free article: PMC6371675] [PubMed: 30931361]
Copyright © 2022, StatPearls Publishing LLC.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.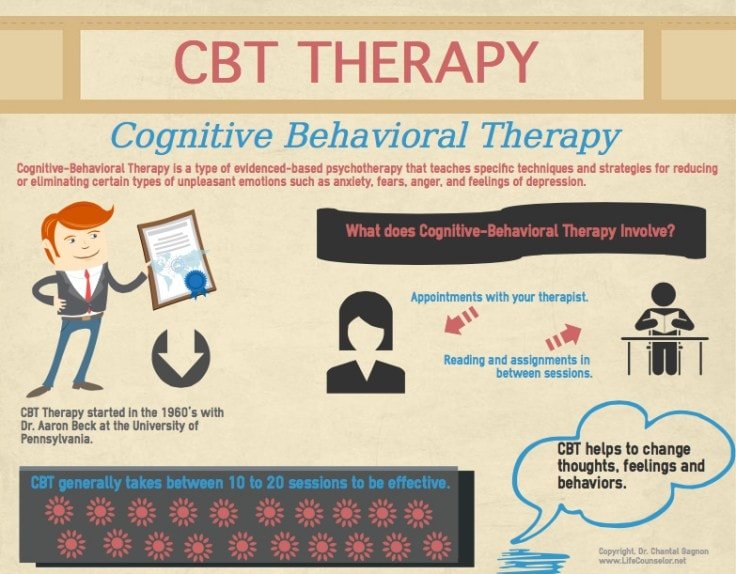
Bookshelf ID: NBK470241PMID: 29261869
Cognitive Behavioral Therapy (CBT) or Cognitive Behavioral Psychotherapy (CBT)
FIND A PSYCHOLOGIST
We tell you how one of the most popular psychotherapy techniques works, which allows you to correct thinking and emotional reactions.
alter
DIRECTION GUIDE
Contents
Behaviorism and cognitivism
Basic concepts
Techniques and exercises
When will CBT help?
Course duration
Evidence-based medicine and CBT
Medical therapy and CBT
Case studies
What to read
What is CBT?
Cognitive Behavioral Therapy (or CBT) is a technique that highlights a person's unconscious motivations, transfers them to a conscious level, helps to change beliefs and behavior that cause neurotic and other pathological conditions. nine0003
From the name it is clear that CBT combines two scientific psychological approaches: cognitive and behavioral (behavioristic).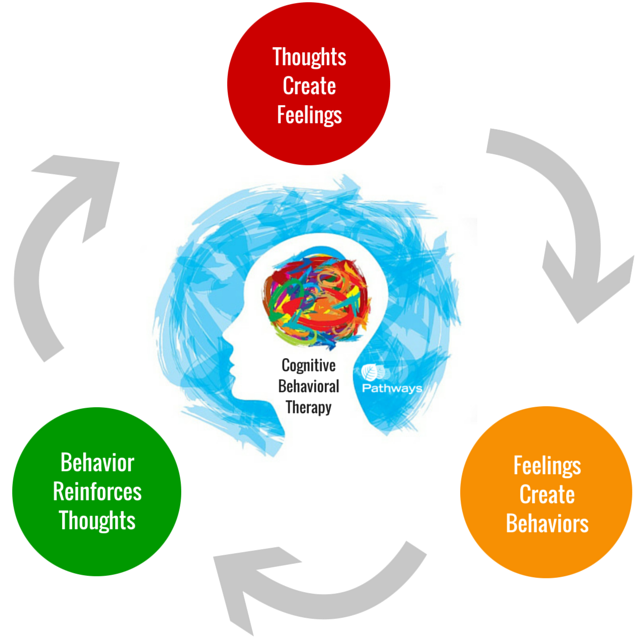 The first states that psychological problems and neuropsychiatric disorders are caused by thoughts and beliefs, stereotypes of thinking acquired during life. The second argues that human (as well as animal) behavior can be changed by encouraging desirable forms of action and not reinforcing undesirable behavior.
The first states that psychological problems and neuropsychiatric disorders are caused by thoughts and beliefs, stereotypes of thinking acquired during life. The second argues that human (as well as animal) behavior can be changed by encouraging desirable forms of action and not reinforcing undesirable behavior.
Behaviorism and cognitivism
The theory of behaviorism (from the English behavior - behavior) was developed in the early twentieth century. It considers behavior as a set of reactions (reflexes) to environmental stimuli. One of the basic concepts of behaviorism is positive and negative reinforcement. Positive reinforcement, or encouragement, is applied when the individual has done the right thing, and helps to reinforce the desired form of behavior. Negative reinforcement implies a negative reaction to the undesirable behavior of the trainee. As a rule, the first form of reinforcement is used in CBT: it works faster, clearly indicates what needs to be achieved.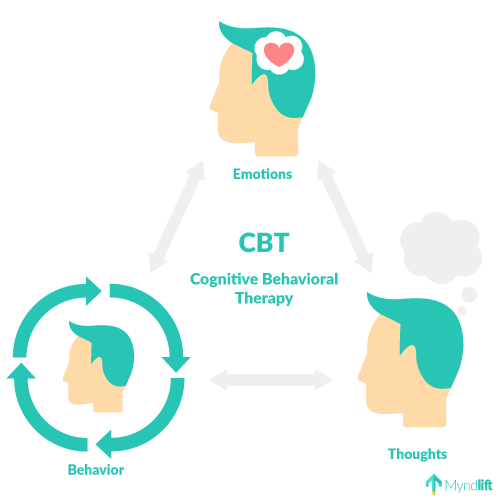 nine0005
nine0005
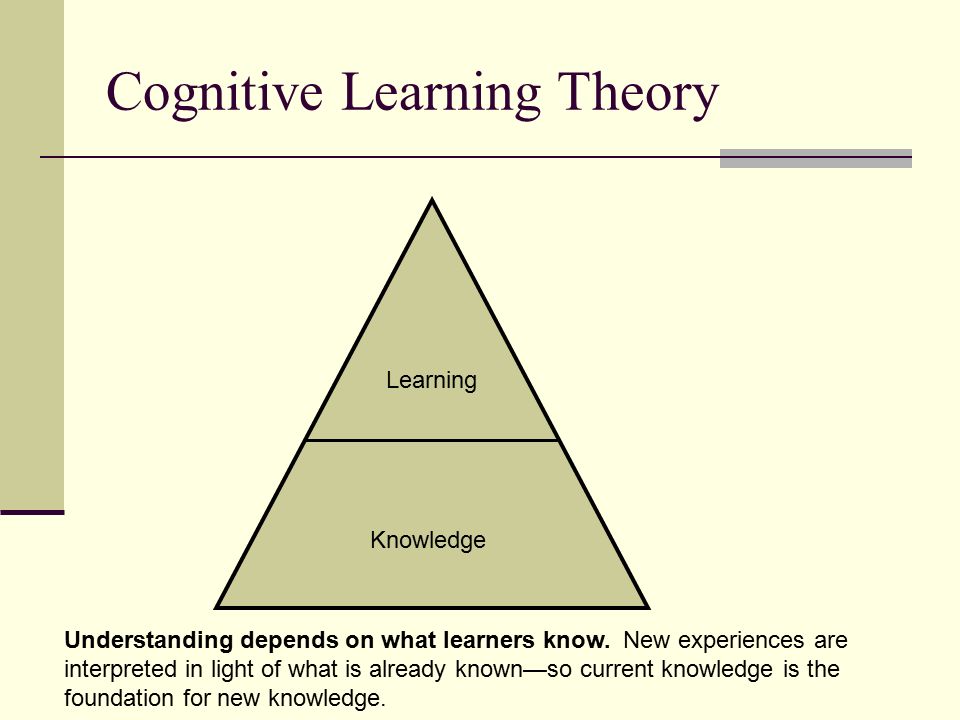
Cognitivism is a scientific movement that originated in the 1960s. It focuses on mental processes: how people perceive, think, remember, learn, solve problems, where they direct their attention. Cognitions are any thoughts and ideas that become the fruits of our thinking. According to the cognitive approach, it is inefficient to work only with a person’s behavior to solve his psychological problems: first, you need to identify beliefs, ideas and thoughts that make him act destructively or feel discomfort, get rid of them, and only then work on the behavioral aspect. nine0005
“Cognitions are basically all mental processes, both adequate and dysfunctional. When children are born, they don't know anything about the world yet. Over time, they begin to encounter people and their ideas about the environment. Parents and society help them formulate both adequate and dysfunctional beliefs. Dysfunctional and maladaptive views make it difficult to adequately assess life situations.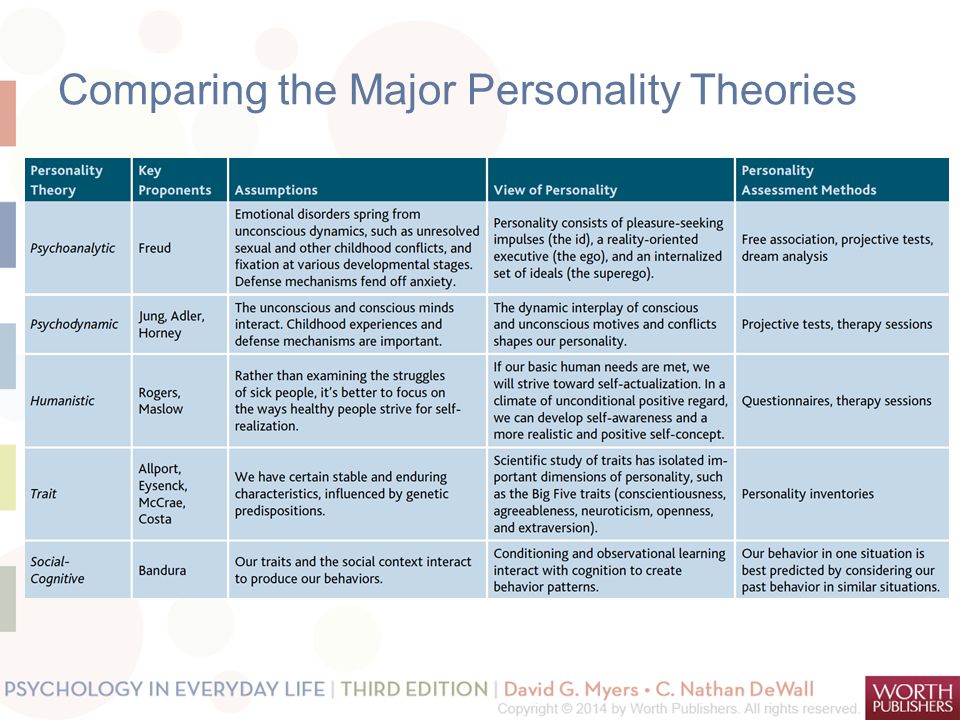 Fears, complexes are formed, the child has a feeling that he is doing something wrong. It is this feeling that in the future leads to neurotic and other psychological problems. nine0005
Fears, complexes are formed, the child has a feeling that he is doing something wrong. It is this feeling that in the future leads to neurotic and other psychological problems. nine0005
Anastasia Afanasyeva, Psychotherapist KPT:
Historically, the development of KPT is divided into 4 waves:
The first wave
(1910s-1950s)
Behavioral therapy
Second wave
(1960s)
Classical approach of CBT and rational-emotive psychotherapy
Third wave
(1990s)
Development of new currents within CBT: dialectical-behavioral psychotherapy, schema therapy, mindfulness therapy, acceptance and obligation therapy (ACT)
The fourth wave
(2010s)
The emerging stage associated with the use of modern technologies in therapy: augmented reality gadgets and software applications
In 1913, the American psychologist John Watson publishes the first articles on behaviorism.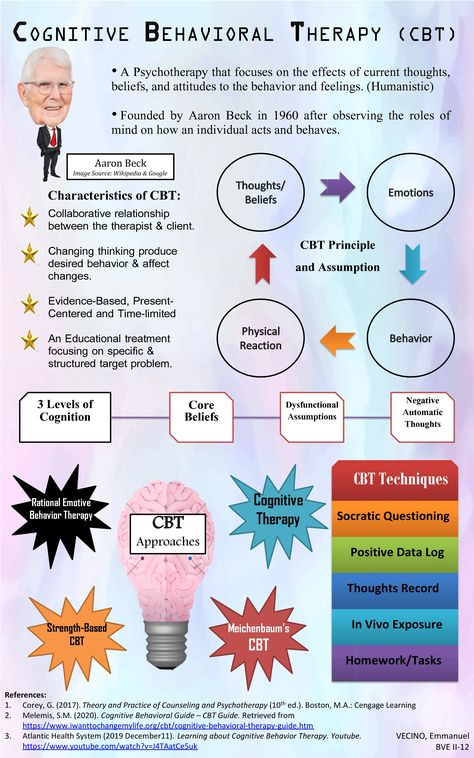 He urges his colleagues to focus exclusively on the study of human behavior, the study of the connection "external stimulus - external reaction (behavior)". Instead of analyzing the structural components of consciousness, behaviorists looked for reproducible connections between observed events, in particular between stimuli (environment) and responses (observed and measured reactions of people or animals to stimuli). Learning theories were the main model in the psychology of that time. Behaviorists have tried to formulate an explanation for how an organism establishes new connections between stimulus and response. Despite its early and sustained success, the behavioral approach placed many limitations on the therapy process. nine0003
He urges his colleagues to focus exclusively on the study of human behavior, the study of the connection "external stimulus - external reaction (behavior)". Instead of analyzing the structural components of consciousness, behaviorists looked for reproducible connections between observed events, in particular between stimuli (environment) and responses (observed and measured reactions of people or animals to stimuli). Learning theories were the main model in the psychology of that time. Behaviorists have tried to formulate an explanation for how an organism establishes new connections between stimulus and response. Despite its early and sustained success, the behavioral approach placed many limitations on the therapy process. nine0003
In 1955, the founder of rational-emotional psychotherapy, Albert Ellis, announced the influence of our thoughts and ideas (cognitions) on mental processes. His colleague Aaron Beck begins to study the field of knowledge. After evaluating the results of various methods of therapy, he comes to the conclusion that our emotions and behavior depend on the way we think.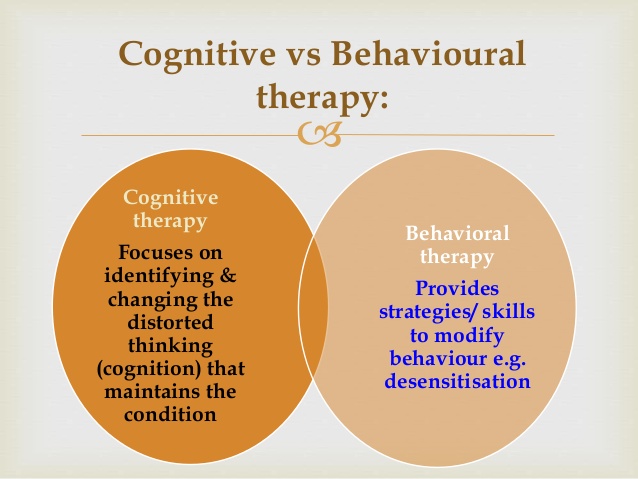
Despite attempts by behavioral therapists to maintain their position in the late 1950s and early 1960s, the ideas of cognitivism became increasingly influential. Publication of the book by A.T. Beck on Cognitive Therapy for Depression (Beck et al., 1979), as well as studies showing that cognitive therapy treats depression as effectively as antidepressants (Rush, Beck, Kovacs & Hollon, 1977), changed psychotherapy forever. In subsequent years, behavioral and cognitive therapy developed together and influenced each other so strongly that they eventually merged into a single cognitive-behavioral approach.
Historical reference
Basic concepts: automatic thoughts, cognitive distortions
Search and awareness automatic thoughts - the basis of the CBT method. About 20 thousand of such quick thoughts arise in our head per day, which are a response to what is happening to us. They are always appreciated. Evolutionarily automatic thoughts are necessary so that we can quickly respond to changes in the environment.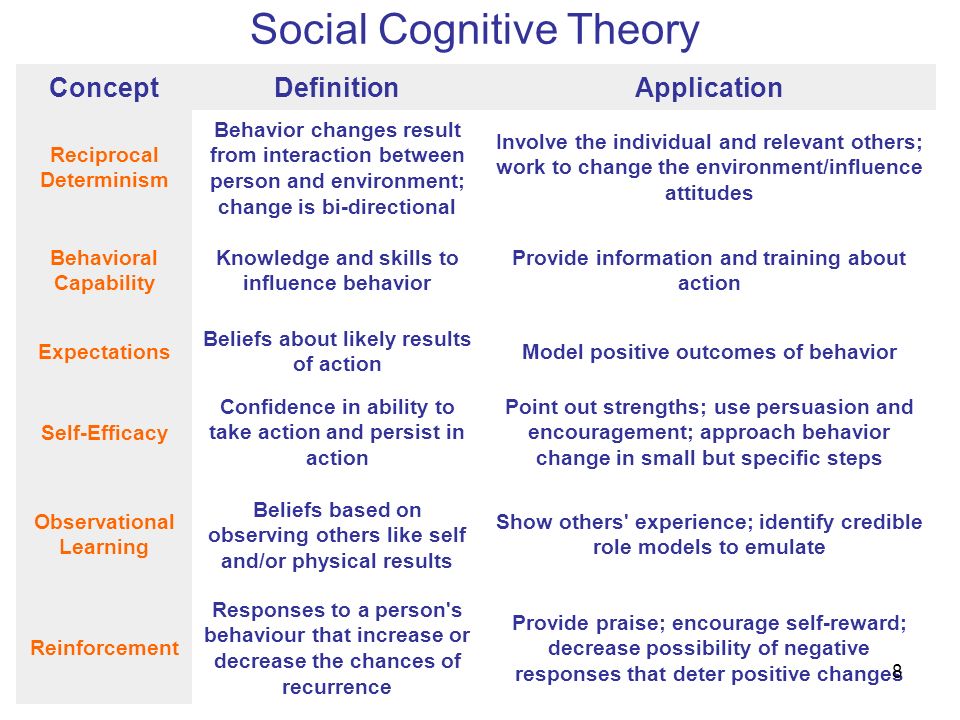 Most of them we do not have time to realize. These thoughts trigger our emotional response. In order to understand why our state has changed (anxiety, fear appeared, mood fell), it is necessary to identify what kind of thought caused this change. CBT suggests looking for quick thoughts in order to process them and translate your judgments into a rational channel. nine0005
Most of them we do not have time to realize. These thoughts trigger our emotional response. In order to understand why our state has changed (anxiety, fear appeared, mood fell), it is necessary to identify what kind of thought caused this change. CBT suggests looking for quick thoughts in order to process them and translate your judgments into a rational channel. nine0005
“There is always a situation that triggers a state change. For example, a person is walking in the dark and hears something rustling in the bushes. He becomes anxious. Most likely, the thought flashed that there was a danger nearby. In response to this thought and feeling of anxiety, the person decides to leave quickly. However, a quick thought and a reaction to it are not always rational. For example, you are doing a work task and realize that you do not have time to complete it on time. A neurotic person may have automatic thoughts: I am not responsible enough, I will be fired. The emotional response to them is anxiety, fear.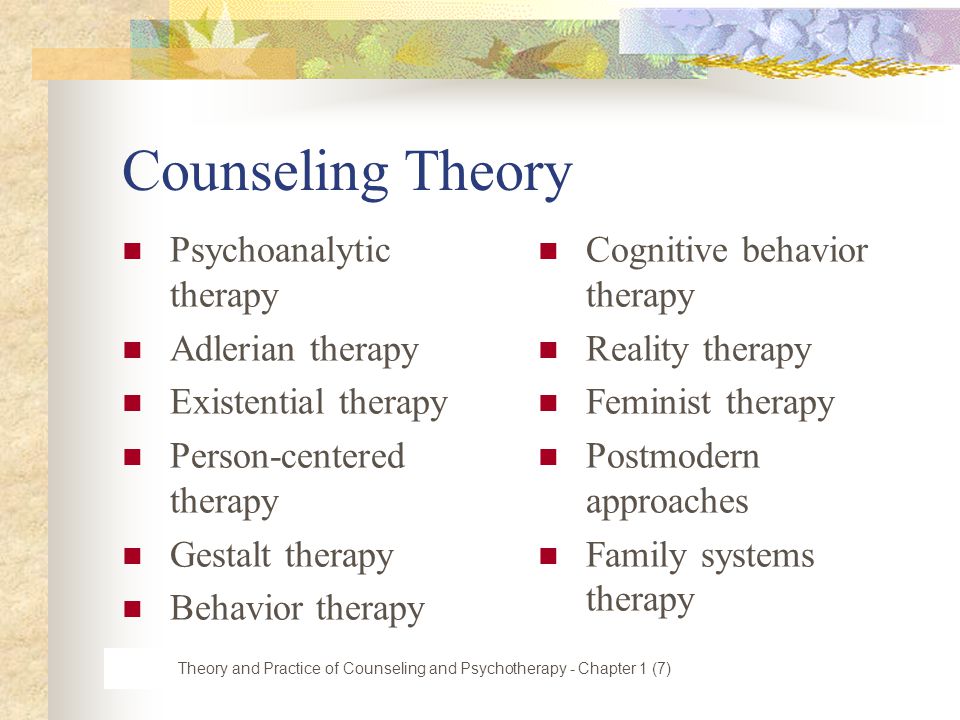 Although if you think rationally, it is unlikely that one missed deadline will negatively affect your entire career. nine0005
Although if you think rationally, it is unlikely that one missed deadline will negatively affect your entire career. nine0005
Anastasia Afanasyeva, psychotherapist CBT:
Cognitive Behavioral Therapy works on cognitive distortions (or errors) that arise from automatic thoughts. Cognitive distortions are erroneous conclusions, irrational ideas that ultimately lead a person to psychological problems. There are over 100 types of cognitive distortions. Here are just a few examples:
Generalization
“I never have relationships”, “I always ruin everything”, “I always have bad luck”. nine0107 A person carries over the characteristics of a single incident for life.
Catastrophe
“Everything is very bad”, “This is a failure”, “Irreparable happened”. Under the influence of negative judgments and emotions, the feeling of the situation is pumped up to complete hopelessness.
Duty
“I owe”, “They owe me”, “Everything should have turned out this way and not otherwise.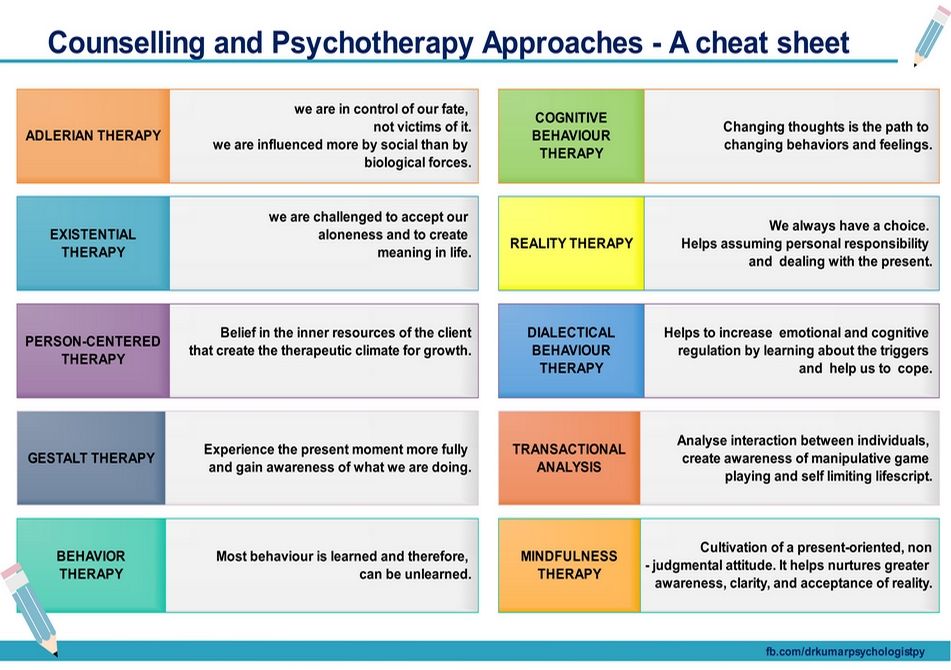 ” Social roles and responsibilities become immutable truths, neither the specifics of the situation, nor the state of the person, nor the complexity of relationships are taken into account. nine0003
” Social roles and responsibilities become immutable truths, neither the specifics of the situation, nor the state of the person, nor the complexity of relationships are taken into account. nine0003
Conformity
“Everyone does/behaves like this. Those who do otherwise are bad/inferior, etc.” Ideas about norms received from outside cause one to stigmatize the slightest deviation in oneself and others.
The task of the CBT therapist is to identify cognitive distortions that negatively affect the client's quality of life and help develop rational, constructive thought patterns in their place.
Techniques and exercises
One of the main techniques of the method is keeping a CBT diary . Usually it is a table in which you need to enter daily events that caused a strong emotional reaction, and analyze them according to the proposed scheme. Further cases are discussed with the therapist at the session.
An example of what columns a CBT diary can contain. Each therapist offers his own diary system.
“After the client has learned to identify his automatic thoughts, he begins to keep a diary for a week. We look at what thoughts most often arise in different situations. This may be the fear that the person will look in someone's eyes as optional (that is, bad), or a feeling that he is not successful, or a feeling that he is vulnerable and will not cope. From the automatic thoughts we recognize, core beliefs begin to emerge. Not quick, superficial thoughts, but the foundation on which the human psyche is based. We are working on changing this array of beliefs in a rational direction.” nine0005
Anastasia Afanasyeva, CBT psychotherapist:
Another important technique for CBT is exposure . It is especially useful in all kinds of phobias. Exposure helps the client learn not to avoid disturbing situations, but to experience them.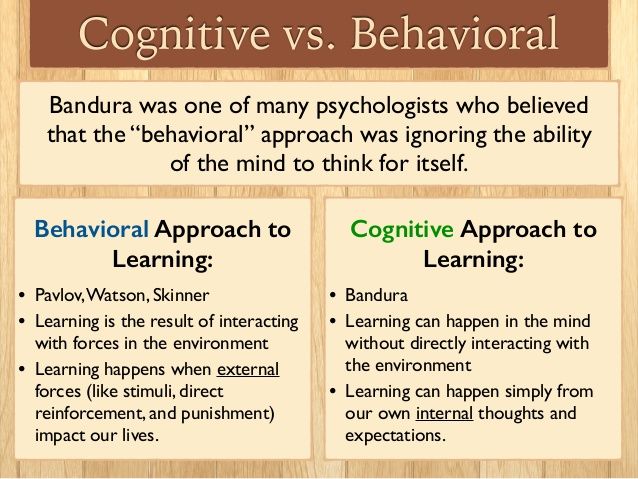
For example, a person is afraid to enter an elevator. When using the exposure technique, the client and therapist approach the booth, stop, and begin to observe the client's reaction. When the anxiety rises, they do exercises with the therapist to help them cope with the anxiety. If the reaction is managed, the client and therapist move on to the next step: they enter the elevator together. The level of anxiety rises again, the therapist again works out with the client his condition. The intensity of the situation gradually increases until the client receives all the necessary skills in order to be aware and rationally assess his condition, to cope with it. nine0005
When will CBT help?
The effectiveness of the CPT is proved for the following states:
All types of phobia
Alarm
Panic disorder and panic attacks
Depression
Occupation and compulsive disorders (OKR)
9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 thoughts, actions, rituals
Psychosomatic disorders
irritable intestine, headaches and another
post -traumatic stress disorder
Eating disorders
Difficulties with communication, building contacts and their maintenance, constancy in the work and family relations
Dependencies 9000,0003
Physical and physical mental
Aggressive behavior
CBT in panic attacks
Panic attacks are spontaneous panic attacks that are accompanied by rapid breathing, palpitations, dizziness, tremor, nausea, sweating and other somatic manifestations. nine0003
nine0003
A panic attack may be the result of other psychiatric disorders rather than a single illness. Recurrent panic attacks without other symptoms may be manifestations of panic disorder. Cognitive behavioral therapy is the proven and most effective treatment for it.
“Panic attacks can occur in depressive disorders, generalized anxiety disorder, and hypochondriacal disorders. This is a very non-specific symptom, such as fever. It is found in various diseases. To make an accurate diagnosis, before starting treatment, you need to be diagnosed by a psychiatrist or psychotherapist. nine0005
Anastasia Afanasyeva, psychotherapist CBT:
The exposure technique mentioned above is very well the main tool for dealing with panic attacks. The psychotherapist teaches the patient to recognize what is happening to him at the time of the attack, how and to what his body reacts. Gradually, the patient learns to cope with his condition.
“First, there is a stage of psycho-education: we tell what happens in the patient's body at the time of the attack.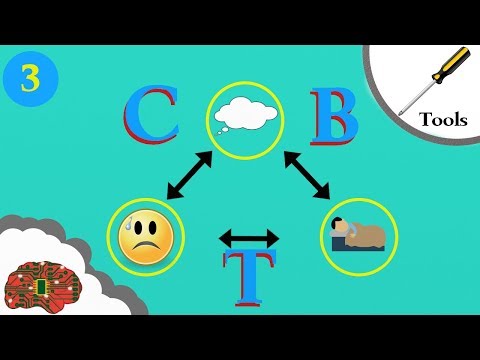 We analyze cycles, thoughts, emotions, behavior, we are looking for the reason that starts the process. Further work is based on the fact that in the office we learn to cause symptoms: dizziness, palpitations, hyperventilation. We practice techniques to endure the anxiety that these symptoms cause. Thus, gradually we build tolerance. Anxiety decreases and eventually disappears. nine0003
We analyze cycles, thoughts, emotions, behavior, we are looking for the reason that starts the process. Further work is based on the fact that in the office we learn to cause symptoms: dizziness, palpitations, hyperventilation. We practice techniques to endure the anxiety that these symptoms cause. Thus, gradually we build tolerance. Anxiety decreases and eventually disappears. nine0003
Shortness of breath can be caused by hyperventilation - rapid shallow breathing. Dizziness - spinning in place. Palpitations - squats or running up the stairs. All exercises are performed together with the therapist. We say that it is not dangerous, the person understands this. When during the session I breathe with the patient, he sees that I normally endure this state. In doing so, he observes what happens to his own sensations.
The essence of a panic attack is that it always goes away. The fear that it will start, most often becomes the trigger for its start. It brings other problems as well, such as avoiding certain situations or carefully checking one's condition.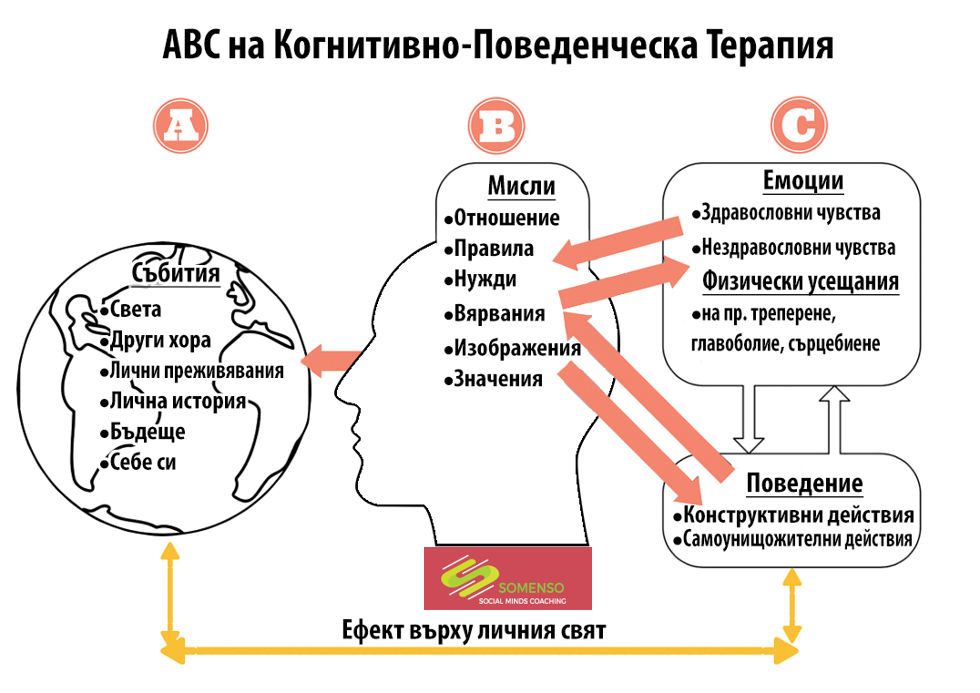 " nine0005
" nine0005
Anastasia Afanasyeva, psychotherapist CBT:
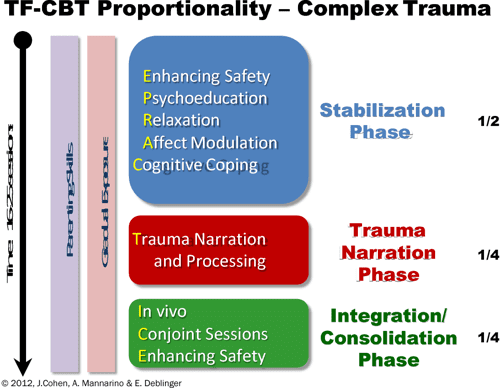
Duration of the course
CBT is considered a short-term therapy, but the duration of the course depends on many factors. For a specific request, such as a phobia or difficulty falling asleep, about 10 sessions are needed. However, this format involves solving only one problem. For multiple problems and more complex conditions, the course will last from a few months to a year. Treating personality disorders will require even longer work. nine0003
Therapy involves a meeting once a week, at a pre-selected time. The duration of the session is 50 minutes. Outside of sessions, the client does homework.
Each session has a structure: agenda, checking homework, discussing specific requests, working through them, debriefing, receiving homework, feedback.
« Terms are always individual and depend on the severity of the condition. For panic attacks or depression, this is six months to a year. For complex diseases or personality disorders, therapy can be very long. In addition to the form and severity of the disease, the ability and desire of a person to get involved in work play a role. There are people who are more prone to reflection, it is easier for them to realize their own mental processes. There are people who find it harder. nine0003
For panic attacks or depression, this is six months to a year. For complex diseases or personality disorders, therapy can be very long. In addition to the form and severity of the disease, the ability and desire of a person to get involved in work play a role. There are people who are more prone to reflection, it is easier for them to realize their own mental processes. There are people who find it harder. nine0003
As with any therapy, one should not expect miracles from CBT. You cannot change in a couple of months, and even in six months. But you can learn to see the relationship between your thoughts, emotions and behavior, and this will allow you to weed out unnecessary thoughts, change reactions, not be led by your beliefs left by your parents and the outside world, and not let anxiety and fear rule your life.
Anastasia Afanasyeva, CBT psychotherapist:
Evidence-based medicine and CBT
Cognitive Behavioral Therapy (CBT) is one of the most researched methods of psychotherapy.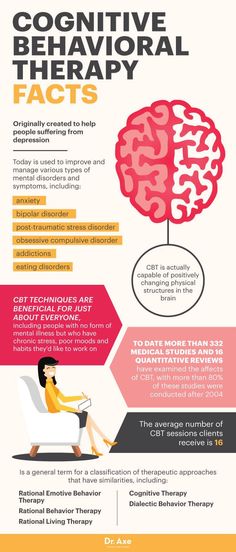 In 2012, a Boston University Department of Psychology Working Group released a seminal systematic review of meta-analyses (1) of various studies, which is the most comprehensive scientific paper on the effectiveness of CBT to date. Based on 269 papers, the researchers concluded that the referral was extremely effective in dealing with anxiety and mood disorders, highly effective in treating phobias, insomnia, and significantly effective in reducing workplace stress. The full text of the review in English can be found here. nine0005
In 2012, a Boston University Department of Psychology Working Group released a seminal systematic review of meta-analyses (1) of various studies, which is the most comprehensive scientific paper on the effectiveness of CBT to date. Based on 269 papers, the researchers concluded that the referral was extremely effective in dealing with anxiety and mood disorders, highly effective in treating phobias, insomnia, and significantly effective in reducing workplace stress. The full text of the review in English can be found here. nine0005
1 Meta-analysis is a type of data analysis in which the results of a number of randomized clinical trials are combined and analyzed as a single large study. In evidence-based medicine, meta-analysis is assigned the highest level of evidence (IA).
Medication and CBT
There are a number of conditions that can be treated with non-medicated CBT, such as mild generalized anxiety disorder, panic disorder, mild OCD, mild depression.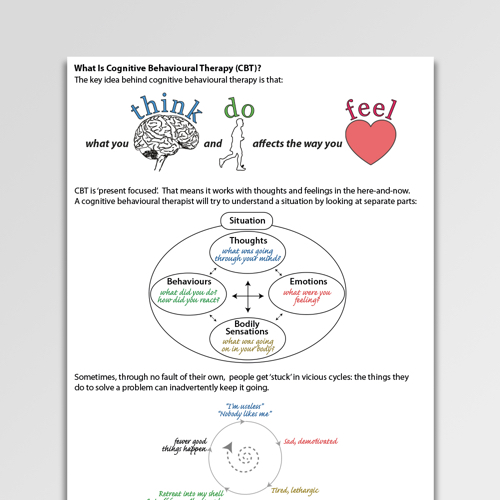 However, in a number of conditions, it is recommended to combine psychotherapy with pharmacotherapy. These include moderate depression and severe depression. nine0005
However, in a number of conditions, it is recommended to combine psychotherapy with pharmacotherapy. These include moderate depression and severe depression. nine0005
« Fear of pharmacotherapy is quite common and I deal with it regularly. I can say that many fears are unfounded. There is a myth that antidepressants are addictive. According to all studies, no antidepressant causes either mental or physical dependence.
If you have a fear of medication, see a qualified doctor who is trained in psychotherapy and pharmacotherapy. He will conduct a medical diagnosis, decide whether it is really necessary to carry out drug therapy, and help work through your fear using CBT techniques.” nine0005
Anastasia Afanasyeva, psychotherapist CBT:
Case reports
“A young man asked for help: after breaking up with a girlfriend, he suffered from depressed mood, anxiety, difficulty falling asleep, obsessive thoughts before going to bed, loss of appetite . In the course of therapy, we uncovered the hidden beliefs that generated these reactions. He believed that if he could not "keep" the relationship, then this indicates his unreliability, if he failed to choose an "adequate" partner, this indicates weakness. Also, the client could not understand what he needed, he relied on ideas about how "should be". nine0003
In the course of therapy, we uncovered the hidden beliefs that generated these reactions. He believed that if he could not "keep" the relationship, then this indicates his unreliability, if he failed to choose an "adequate" partner, this indicates weakness. Also, the client could not understand what he needed, he relied on ideas about how "should be". nine0003
During three months of work, the client has learned to be aware of his needs, desires, track thoughts and engage in polemics with them. The young man was able to emotionally distance himself from obsessive thoughts, the mood background leveled off. He built his schedule in accordance with his own goals and values, acquired awareness skills.
Anastasia Afanasyeva, psychotherapist CBT:
What to read?
Cognitive Behavioral Therapy for Anxiety, Fear, Worry and Panic. Michelle Skin, Matthew McKay, Patrick Fanning
This book is for those who are already in therapy and want to understand the basics of the method and get the most out of CBT. The authors dwell on techniques and exercises that help to cope with the manifestations of anxiety and symptoms of panic attacks.
The authors dwell on techniques and exercises that help to cope with the manifestations of anxiety and symptoms of panic attacks.
Cognitive Behavioral Therapy for Dummies. Rena Branch, Rob Wilson
A book from practicing therapists that explains CBT principles, concepts and how to deal with various disorders in simple language. In addition to practical advice and exercises, you will find many examples from the practice of the authors in it. nine0005
FIND A CBT PSYCHOLOGIST
Did you find the material helpful? Share it:
Cognitive Behavioral Therapy (CBT) - Origins
What is Cognitive Behavioral Therapy (CBT)?
What processes led to the emergence of cognitive behavioral therapy (CBT).
What is the place of cognitive behavioral therapy (CBT) among modern psychotherapeutic techniques?
Freud's Theory
At the end of the 19th century, Freud presented to the public his view of the human psyche, its components, the causes of the formation of psychopathology and the principles of its treatment - psychoanalysis.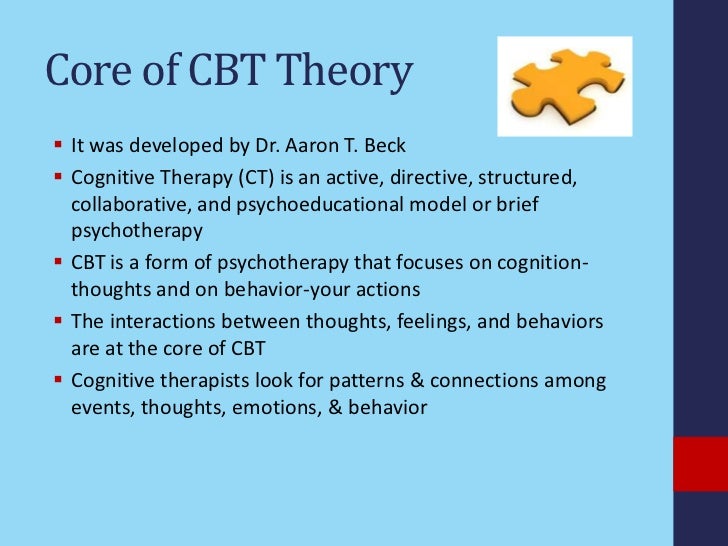 Freud made the main emphasis in his theory on the study of unconscious mental processes, presenting them as the main source of both psychopathology and daily behavioral acts.
Freud made the main emphasis in his theory on the study of unconscious mental processes, presenting them as the main source of both psychopathology and daily behavioral acts.
See also
Myths about the diagnosis of mental illness nine0003
Behavioral Theory and Behavioral Therapy
At the same end of the 19th century, a behavioral theory began to develop - behaviorism (behaviorism), originating with Pavlov and Bekhterev and presented as a well-formed theory in the works of Skinner and Bandura by the middle of the 20th century. Skinner preferred to explain the human psyche, his personality, behavior and psychopathology in behavioral terms, arguing that one should operate only with those concepts that can be empirically measured. Behaviorists argued that only stimulus and behavior are objectively measurable concepts. At the same time, it was argued that the human brain is a “black box” (black box) - a kind of black hole in which objectively unmeasurable and unknowable processes take place.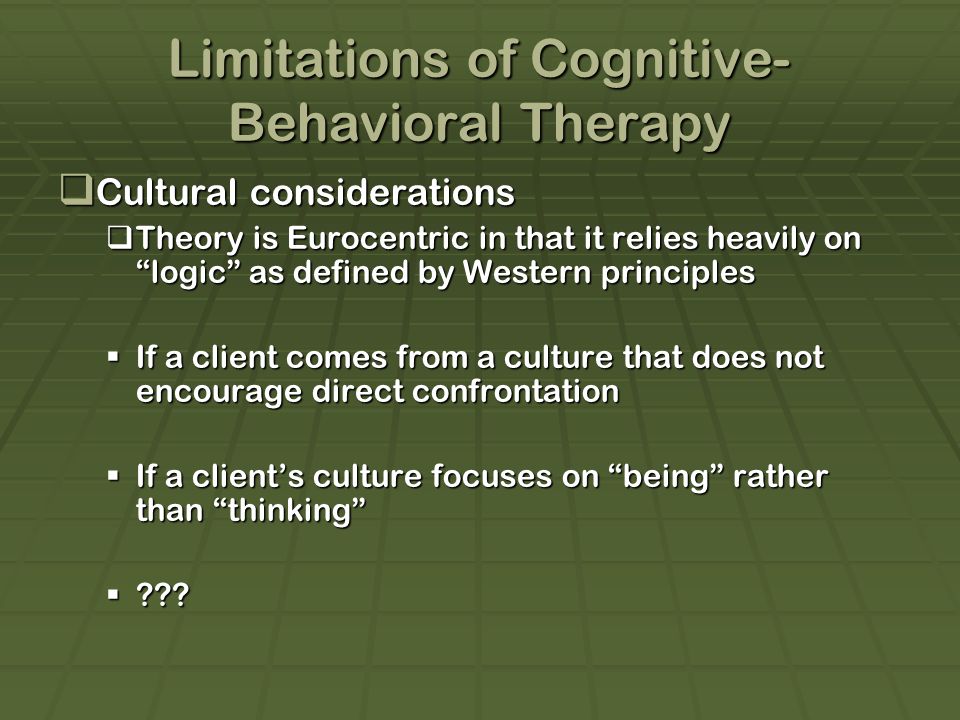 Therefore, behaviorists in their work addressed only the stimulus and behavior. nine0003
Therefore, behaviorists in their work addressed only the stimulus and behavior. nine0003
New brain data and cognitive behavioral therapy
In the 60s-70s. In the 20th century, new data about the brain and cognitive processes appear. Computer science is developing (knowledge about the brain and cognitive processes is the basis for compiling computer programs, in turn, the brain and cognition are explained by analogy with a computer) and now it becomes impossible to treat the brain as a black hole.
As a consequence, the work of Piaget and his students, describing cognitive processes, occupy an increasing place in the work of a psychologist. Vygotsky's works are being actively translated into other languages and occupy a firm place in Western academic psychology. In psychotherapy, Aron Beck develops cognitive theory and Albert Ellis rational-emotive theory, later merged into cognitive behavioral therapy (CBT). The main emphasis in these theories is on cognitive processes that largely determine the human psyche, his personality, behavior and psychopathology.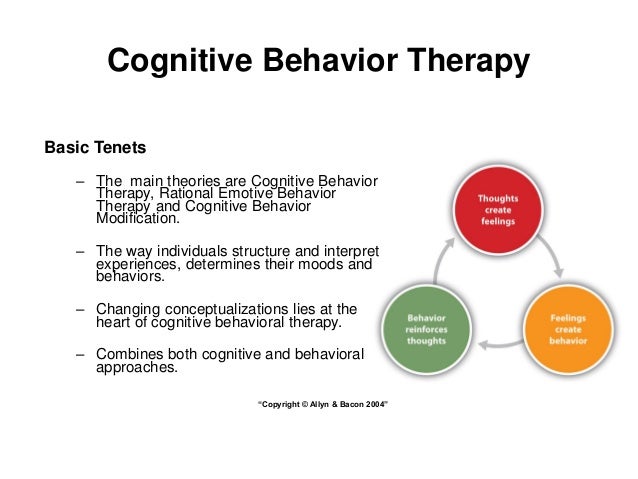 nine0003
nine0003
Cognitive behavioral therapy at the tip of a knife
CBT explains psychopathological processes by the influence of parasitic thoughts on human behavior. Thoughts-parasites are thoughts that negatively affect human self-esteem, perception of the external and internal world. Such thoughts have different colors: mind-reading (“I know what others think of me”), self-flagellation (“I am to blame for everything”), negative perception of reality, timeline, self or other, called the 'Beck Triad', by name Aaron Beck, who first pointed out this kind of parasitic thought (“everything is bad, it always has been, is and will be, and I will never get out of this hole”). Thoughts-parasites negatively affect the feelings of a person and the interpretation of sensations perceived by human senses (I was specially pushed, the whole world is against me and I feel extremely bad). Such a chain closes with appropriate behavior (if I feel so bad and everyone is against me, then I have no reason to live, I don’t want to leave the house). Accordingly, our actions and our feelings affect our way of thinking. nine0003
Accordingly, our actions and our feelings affect our way of thinking. nine0003
See also
What are cognitive biases?
Treatment with cognitive behavioral therapy (CBT)
There are many approaches and techniques emerging from the theoretical developments of cognitive behavioral therapy (CBT). A cognitive behavioral therapy (CBT) psychotherapist will offer to identify parasitic thoughts and change their direction with the help of the so-called Socratic questions: who said that everything is bad?; where did you get the idea that it will be like this forever? etc. Many other cognitive techniques allow you to change the negative train of thought. But just changing the way you think is not enough to alleviate mental pain or build relationships. A certain cognitive-behavioral therapy is required (auto-training, meditative techniques, communication training, etc.), the use of which leads the patient both to change negative thinking to a more optimistic one, and to acquire more adaptive behavior patterns.