Switching antidepressants withdrawal
Strategies, Side Effects, and More
People may need to switch antidepressants if their existing medication isn’t working as intended. Several strategies can help ease this transition.
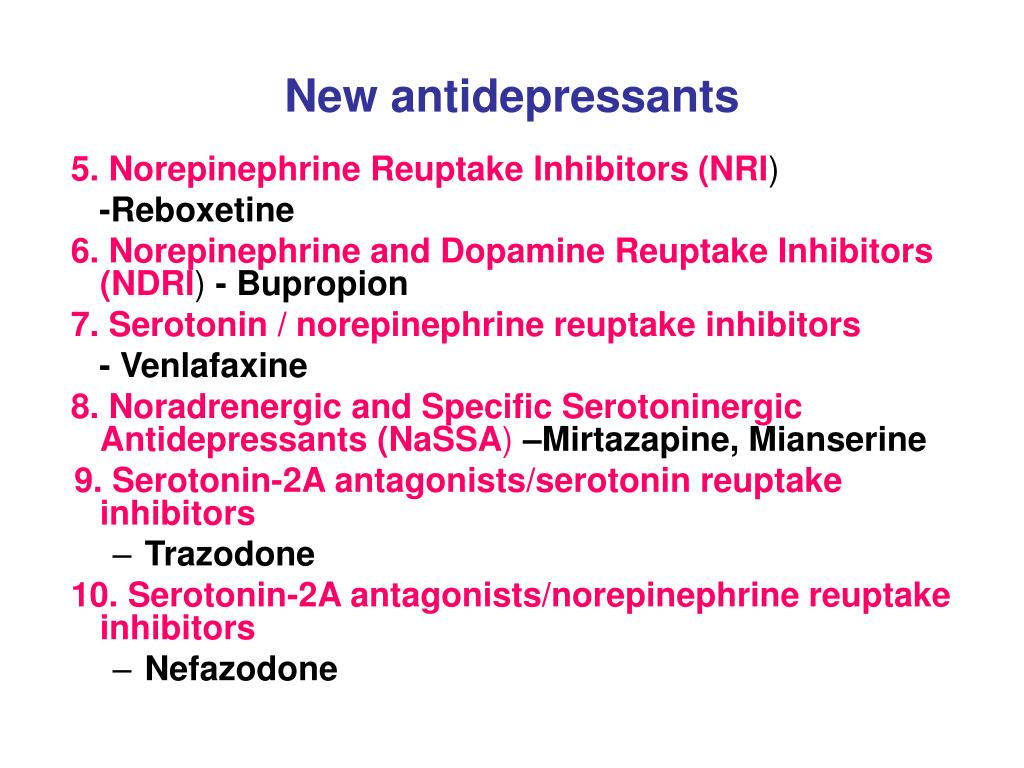
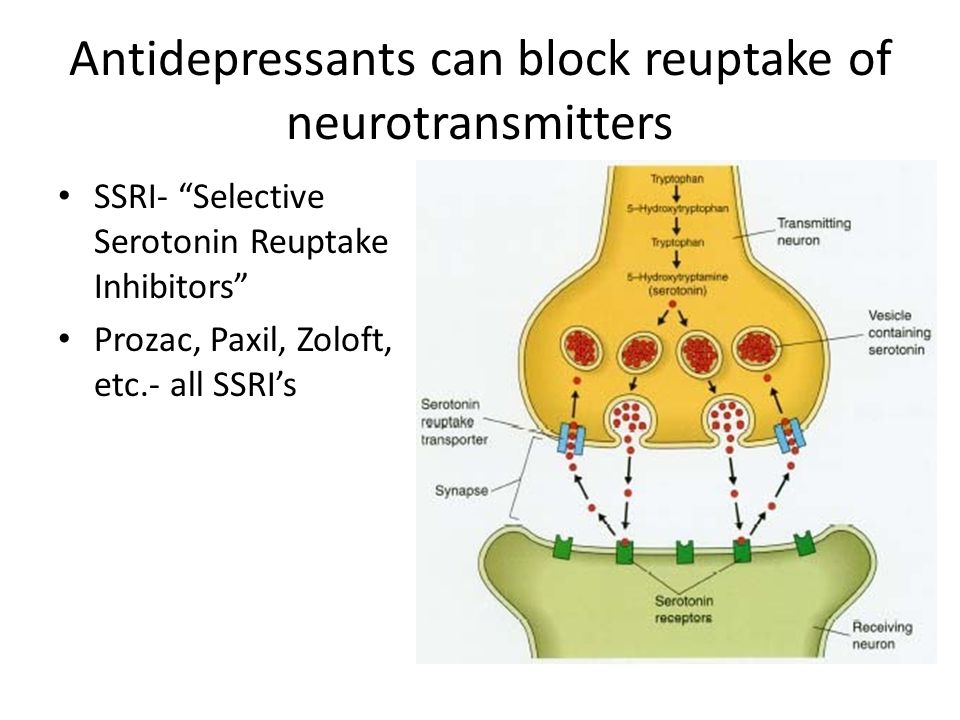
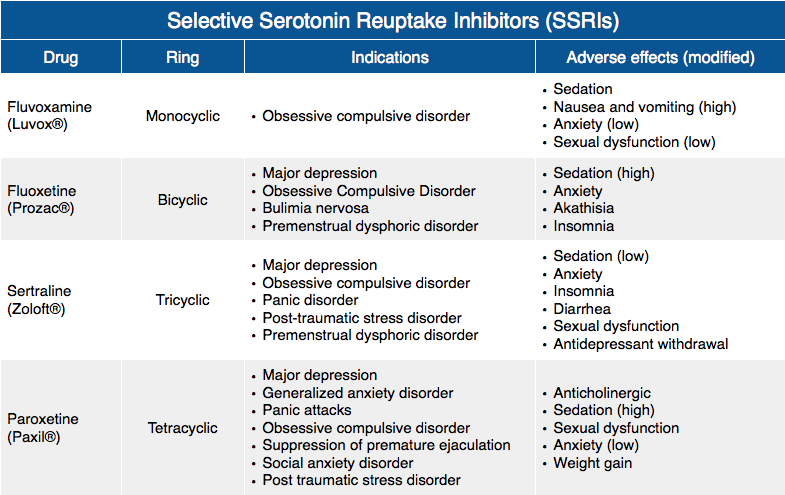
If you’re living with depression, your doctor will likely start you on a treatment plan of antidepressants such as a selective serotonin reuptake inhibitor (SSRI) or serotonin-norepinephrine reuptake inhibitor (SNRI).
It can take a few weeks on one of these drugs to see an improvement. However, not everyone will feel better with the first antidepressant they try.
When an antidepressant doesn’t work as intended, doctors can increase the dose or add other treatments such as cognitive behavioral therapy. These strategies sometimes work — but not always.
In other cases, a change of antidepressants is necessary.
Only one in three people will be symptom-free after taking one type of antidepressant. People who don’t respond to the first drug they try may need to switch to a different antidepressant.
You may also need to switch medications if the first drug you try causes side effects you can’t tolerate, such as weight gain or lowered sex drive.
Don’t stop taking your medication without first checking with your doctor. Switching treatment is a careful process. Stopping your current medication too quickly can lead to withdrawal symptoms or cause your depression symptoms to return. Your doctor must monitor you for side effects or problems during the switch.
Doctors use four different strategies to switch people from one antidepressant to another:
- Direct switch: In a direct switch, you stop taking your current drug and start on a new antidepressant the next day. It’s possible to make a direct switch if you’re going from an SSRI or SNRI to another drug in the same class.
- Taper and immediate switch: In this switching method, you gradually taper off your current drug. As soon as you’ve fully stopped the first drug, you start taking the second drug.
- Taper, washout, and switch: This is a conservative method of switching in which you gradually taper off the first drug and wait for it to leave your system before switching to the new medication.
- Cross taper: You gradually taper off the first drug while increasing the second dose. This can be beneficial when switching to a drug in a different antidepressant class.
The strategy your doctor will choose will depend on factors such as:
- The severity of your symptoms: It isn’t safe for some people to go off their antidepressants for
several days or weeks. - Concerns over symptoms: Cross-tapering can help prevent you from having withdrawal symptoms.
- Which drugs you take: Certain antidepressants can interact in dangerous ways and
can’t be cross-tapered. For example, doctors won’t combine clomipramine (Anafranil) with SSRIs, duloxetine (Cymbalta), or venlafaxine (Effexor XR).
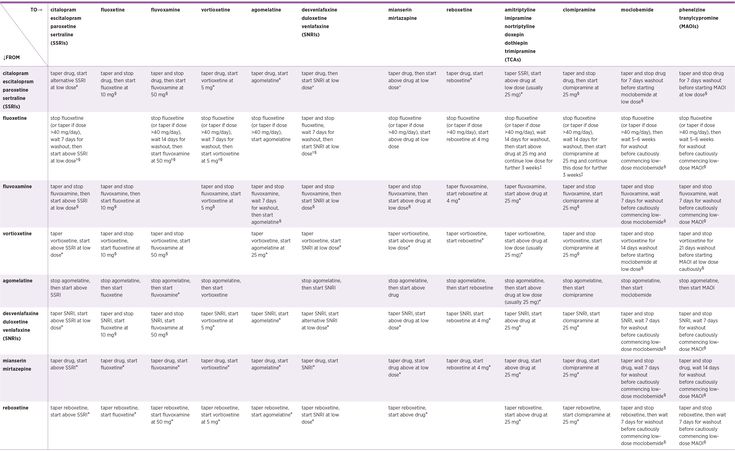
Here’s a chart with information about how your doctor may switch your drugs.
| From | To | How to switch |
|---|---|---|
| SSRI or SNRI | SSRI or SNRI | • Direct switch • Cross taper • Taper, washout, switch • Taper and switch |
| SSRI or SNRI | Tricyclic antidepressant (TCA) | • Cross taper • Taper, washout, switch • Taper and switch |
| SSRI or SNRI | Non-SSRI, non-SNRI, non-TCA | • Cross taper • Taper, washout, switch • Taper and switch |
| TCA | Any antidepressant | Cross taper |
| Monoamine oxidase inhibitors (MAOI) | Any antidepressant | Taper, washout, switch |
| Any antidepressant | MAOI | Taper, washout, switch |
| Bupropion | Any antidepressant | Cross taper |
Changing from one antidepressant to another can cause side effects.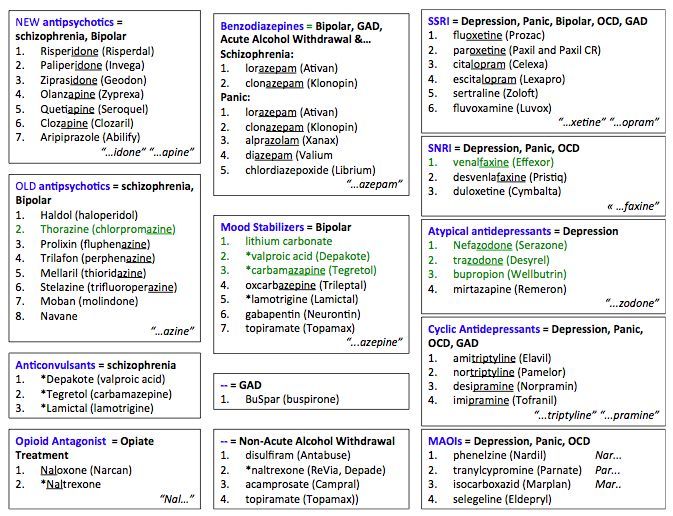
Withdrawal
Reducing your antidepressant dose or stopping medication entirely can cause withdrawal symptoms, including:
- restlessness
- trouble sleeping
- stomach problems
- sweating
- unsteadiness
Serotonin syndrome
If you start taking a new medication before the old one is out of your system, you can develop a rare but serious condition called serotonin syndrome.
Certain antidepressants work by increasing the amount of the chemical serotonin in your brain. The added effects of more than one antidepressant can lead to an excess of serotonin in your body.
Symptoms of serotonin syndrome include:
- agitation
- nervousness
- tremor
- shivering
- heavy sweating
- diarrhea
- fast heart rate
- confusion
More severe cases can cause symptoms such as:
- hyperthermia
- coma
- seizures
- delirium
- muscle rigidity
Call your doctor or go to an emergency room right away if you have any of these symptoms.
Talk with a doctor if you have side effects that don’t improve. You might need to make another medication switch.
Once you’ve been on antidepressants, your body gets used to the drug. When you try to stop taking the antidepressant, you can experience withdrawal symptoms. Slowly tapering off your antidepressant can help you avoid these symptoms.
Doctors will typically lower your antidepressant dose over the course of 4 or more weeks.
A washout period is the waiting time of a few days or weeks after stopping the old drug before starting the new one. This lets your body clear the old drug out of your system. This often takes 2 to 5 days.
Once the washout period is over, you’ll usually start with a low dose of the new drug. Your doctor will slowly increase the dose, titrating up until it starts to relieve your symptoms.
There are different types of antidepressants, and people respond to them differently. Only one-third of people experience symptoms remission from their first course of antidepressants.
If your antidepressants don’t work, you may need to switch medications.
When switching antidepressants, it’s common to taper down your medications before switching, and doctors may also require you to wait days or weeks before taking a new medication. These strategies can help lower the risk of adverse drug interactions.
Strategies, Side Effects, and More
People may need to switch antidepressants if their existing medication isn’t working as intended. Several strategies can help ease this transition.
If you’re living with depression, your doctor will likely start you on a treatment plan of antidepressants such as a selective serotonin reuptake inhibitor (SSRI) or serotonin-norepinephrine reuptake inhibitor (SNRI).
It can take a few weeks on one of these drugs to see an improvement. However, not everyone will feel better with the first antidepressant they try.
When an antidepressant doesn’t work as intended, doctors can increase the dose or add other treatments such as cognitive behavioral therapy.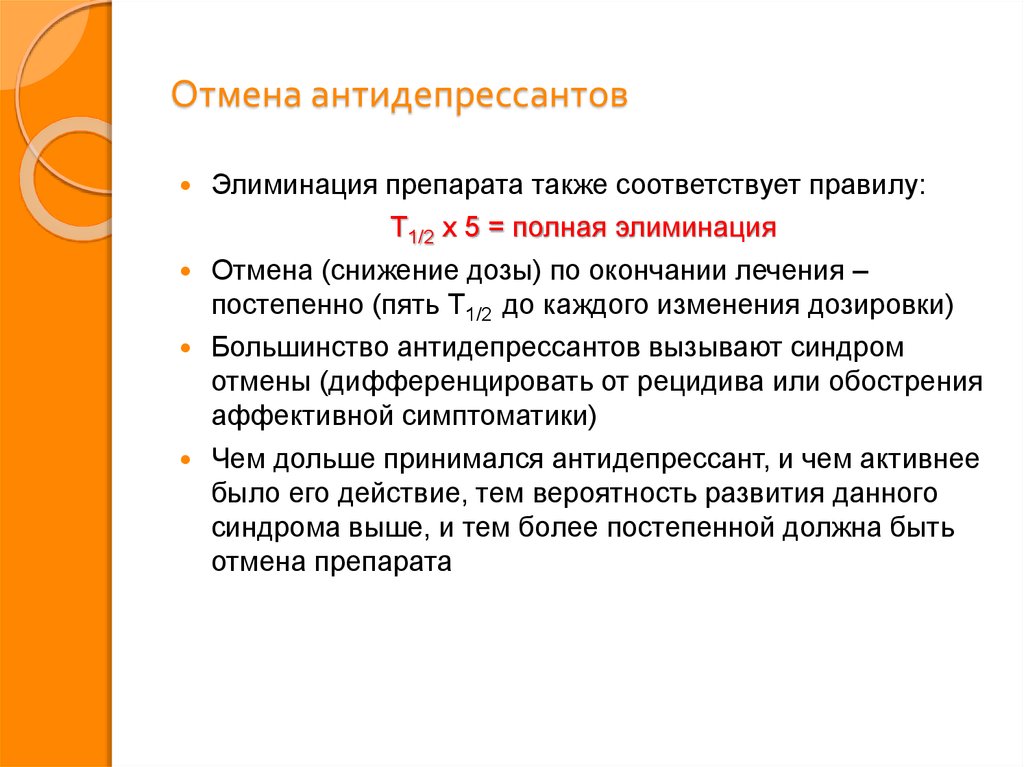 These strategies sometimes work — but not always.
These strategies sometimes work — but not always.
In other cases, a change of antidepressants is necessary.
Only one in three people will be symptom-free after taking one type of antidepressant. People who don’t respond to the first drug they try may need to switch to a different antidepressant.
You may also need to switch medications if the first drug you try causes side effects you can’t tolerate, such as weight gain or lowered sex drive.
Don’t stop taking your medication without first checking with your doctor. Switching treatment is a careful process. Stopping your current medication too quickly can lead to withdrawal symptoms or cause your depression symptoms to return. Your doctor must monitor you for side effects or problems during the switch.
Doctors use four different strategies to switch people from one antidepressant to another:
- Direct switch: In a direct switch, you stop taking your current drug and start on a new antidepressant the next day.
 It’s possible to make a direct switch if you’re going from an SSRI or SNRI to another drug in the same class.
It’s possible to make a direct switch if you’re going from an SSRI or SNRI to another drug in the same class. - Taper and immediate switch: In this switching method, you gradually taper off your current drug. As soon as you’ve fully stopped the first drug, you start taking the second drug.
- Taper, washout, and switch: This is a conservative method of switching in which you gradually taper off the first drug and wait for it to leave your system before switching to the new medication.
- Cross taper: You gradually taper off the first drug while increasing the second dose. This can be beneficial when switching to a drug in a different antidepressant class.
The strategy your doctor will choose will depend on factors such as:
- The severity of your symptoms: It isn’t safe for some people to go off their antidepressants for
several days or weeks. - Concerns over symptoms: Cross-tapering can help prevent you from having withdrawal symptoms.
- Which drugs you take: Certain antidepressants can interact in dangerous ways and
can’t be cross-tapered. For example, doctors won’t combine clomipramine (Anafranil) with SSRIs, duloxetine (Cymbalta), or venlafaxine (Effexor XR).
Here’s a chart with information about how your doctor may switch your drugs.
| From | To | How to switch |
|---|---|---|
| SSRI or SNRI | SSRI or SNRI | • Direct switch • Cross taper • Taper, washout, switch • Taper and switch |
| SSRI or SNRI | Tricyclic antidepressant (TCA) | • Cross taper • Taper, washout, switch • Taper and switch |
| SSRI or SNRI | Non-SSRI, non-SNRI, non-TCA | • Cross taper • Taper, washout, switch • Taper and switch |
| TCA | Any antidepressant | Cross taper |
| Monoamine oxidase inhibitors (MAOI) | Any antidepressant | Taper, washout, switch |
| Any antidepressant | MAOI | Taper, washout, switch |
| Bupropion | Any antidepressant | Cross taper |
Changing from one antidepressant to another can cause side effects.
Withdrawal
Reducing your antidepressant dose or stopping medication entirely can cause withdrawal symptoms, including:
- restlessness
- trouble sleeping
- stomach problems
- sweating
- unsteadiness
Serotonin syndrome
If you start taking a new medication before the old one is out of your system, you can develop a rare but serious condition called serotonin syndrome.
Certain antidepressants work by increasing the amount of the chemical serotonin in your brain. The added effects of more than one antidepressant can lead to an excess of serotonin in your body.
Symptoms of serotonin syndrome include:
- agitation
- nervousness
- tremor
- shivering
- heavy sweating
- diarrhea
- fast heart rate
- confusion
More severe cases can cause symptoms such as:
- hyperthermia
- coma
- seizures
- delirium
- muscle rigidity
Call your doctor or go to an emergency room right away if you have any of these symptoms.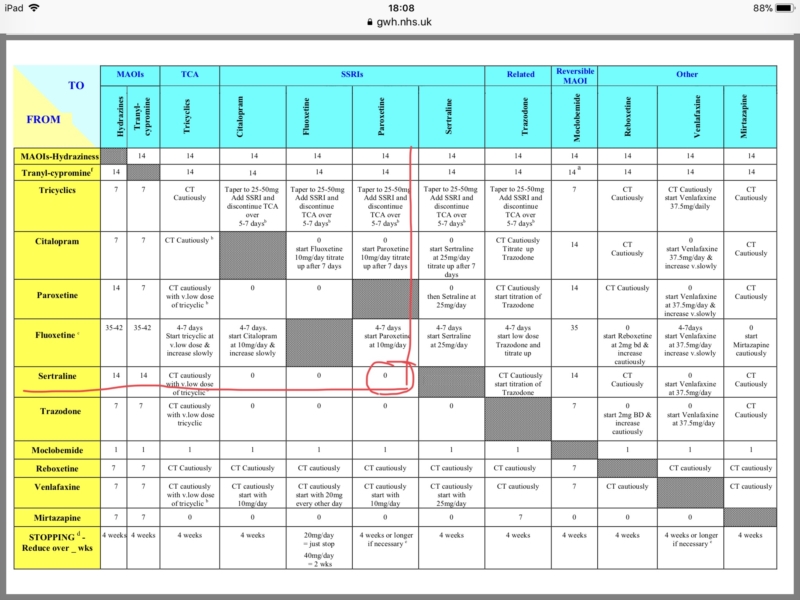
Talk with a doctor if you have side effects that don’t improve. You might need to make another medication switch.
Once you’ve been on antidepressants, your body gets used to the drug. When you try to stop taking the antidepressant, you can experience withdrawal symptoms. Slowly tapering off your antidepressant can help you avoid these symptoms.
Doctors will typically lower your antidepressant dose over the course of 4 or more weeks.
A washout period is the waiting time of a few days or weeks after stopping the old drug before starting the new one. This lets your body clear the old drug out of your system. This often takes 2 to 5 days.
Once the washout period is over, you’ll usually start with a low dose of the new drug. Your doctor will slowly increase the dose, titrating up until it starts to relieve your symptoms.
There are different types of antidepressants, and people respond to them differently. Only one-third of people experience symptoms remission from their first course of antidepressants.
If your antidepressants don’t work, you may need to switch medications.
When switching antidepressants, it’s common to taper down your medications before switching, and doctors may also require you to wait days or weeks before taking a new medication. These strategies can help lower the risk of adverse drug interactions.
Experts have changed the way adults treat depression » Medvestnik
The National Institute for Health and Care Excellence (NICE) has updated guidelines for treating adults with depression. The changes affected the tactics of treating the disease, the possibility of intensifying antidepressant therapy, and ways to cancel drug therapy.
Definition
Depression is a mental disorder characterized by an inability to experience positive emotions (loss of interest in and enjoyment of ordinary things and activities), depressed mood, and a wide range of associated emotional, cognitive, somatic, and behavioral symptoms, according to the NICE document .
Principles of case management
In caring for a patient with depression, the professional should strive to build trust. It is necessary to communicate with the patient openly, without judging him, avoiding stigmatization and discrimination, respecting confidentiality, privacy and respect for his personality. The patient must be given full access to up-to-date, evidence-based recommendations for the treatment of depression, as well as information about local self-help groups.
At the first meeting with the patient, it is necessary to clarify the history of the disease, concomitant mental and somatic pathology, the presence of episodes of elevated mood (for differential diagnosis with bipolar disorder), previous therapy and response to it. It is important to know the patient's strengths, personal resources, difficulties in relationships, lifestyle (eg, diet, physical activity, sleep), the presence of stressful or traumatic life events, current or past (divorce, loss of a loved one, trauma), conditions life, whether he has drug or alcohol abuse. A patient with depression should definitely ask about the presence of suicidal thoughts and intentions.
A patient with depression should definitely ask about the presence of suicidal thoughts and intentions.
If suicidal risk is identified, the patient should be referred to a psychiatrist immediately.
Periods of high risk
When working with depressed patients, special care should be taken during periods of high risk: when starting and changing therapy, when stress increases. It is necessary to advise the patient and his relatives to pay attention to mood swings, anxiety, negative feelings and a sense of hopelessness, the appearance of suicidal thoughts.
It should be remembered that high doses of antidepressants can be toxic, so patients with suicidal risk should limit the amount of medication dispensed at one time on their hands.
The risk of suicidal thoughts, the likelihood of self-harm and suicide increase in the first weeks of antidepressant therapy.
Treatment
For subthreshold and mild depression, antidepressant therapy should not be the first choice.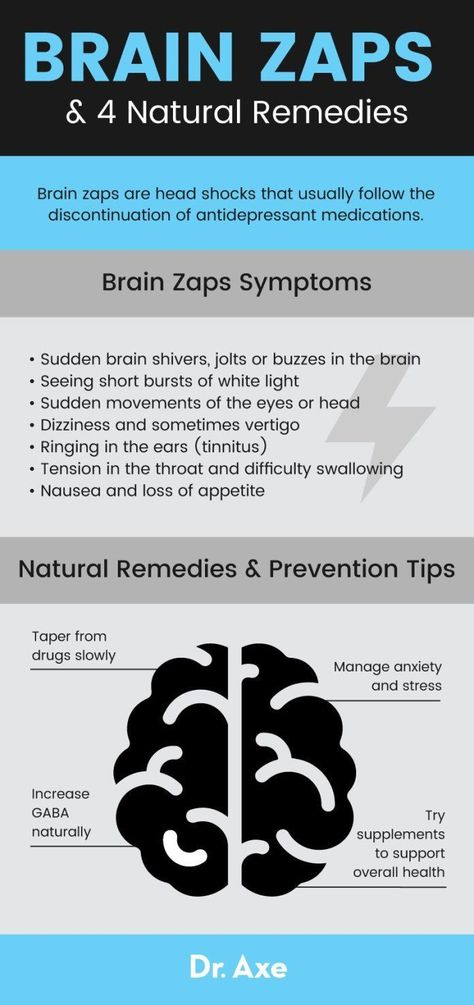 The patient can be offered a wide range of therapeutic techniques: self-help groups, cognitive behavioral therapy, behavioral activation, interpersonal psychotherapy, short-term psychodynamic psychotherapy, group physical education classes specially designed for patients with depression, mindfulness-based cognitive therapy and meditation.
The patient can be offered a wide range of therapeutic techniques: self-help groups, cognitive behavioral therapy, behavioral activation, interpersonal psychotherapy, short-term psychodynamic psychotherapy, group physical education classes specially designed for patients with depression, mindfulness-based cognitive therapy and meditation.
When working with patients with depressive disorders moderate and severe , antidepressant therapy may be required in addition to non-pharmacological methods.
When suggesting drug therapy to a patient, the reasons for prescribing the drug, possible drugs, dosage and options for changing it, expected improvements in therapy, possible side effects and withdrawal should be discussed.
When prescribing an antidepressant, the physician should explain to the patient the possible effects at the start of treatment, the timing of response to therapy (usually 4 weeks), and the need to take drugs for at least 6 months after the onset of remission.

A follow-up appointment should be scheduled after 2 weeks or after 1 week if there is a risk of suicide or if the patient is between 18 and 25 years of age.
Principles of Antidepressant Withdrawal and Dose Reduction
The patient should be aware that antidepressant withdrawal is gradual, gradual and successful in most cases. Abrupt discontinuation of therapy, skipping a dose, or taking an incomplete dose may cause a withdrawal syndrome: dizziness, sensory disturbances (eg, tingling sensation), mental changes (irritability, anxiety, anxiety, low mood, tearfulness, panic attacks, fears, confusion, occasionally suicidal thoughts), sleep disturbance, sweating, gastrointestinal disturbances (eg, nausea), palpitations, fatigue, headaches, joint and muscle pain.
Most often, the withdrawal syndrome is mild and lasts from 1 to 2 weeks, sometimes it can be more severe and last for several weeks, in rare cases - months. Occasionally, the withdrawal syndrome can be severe, especially with abrupt withdrawal of therapy.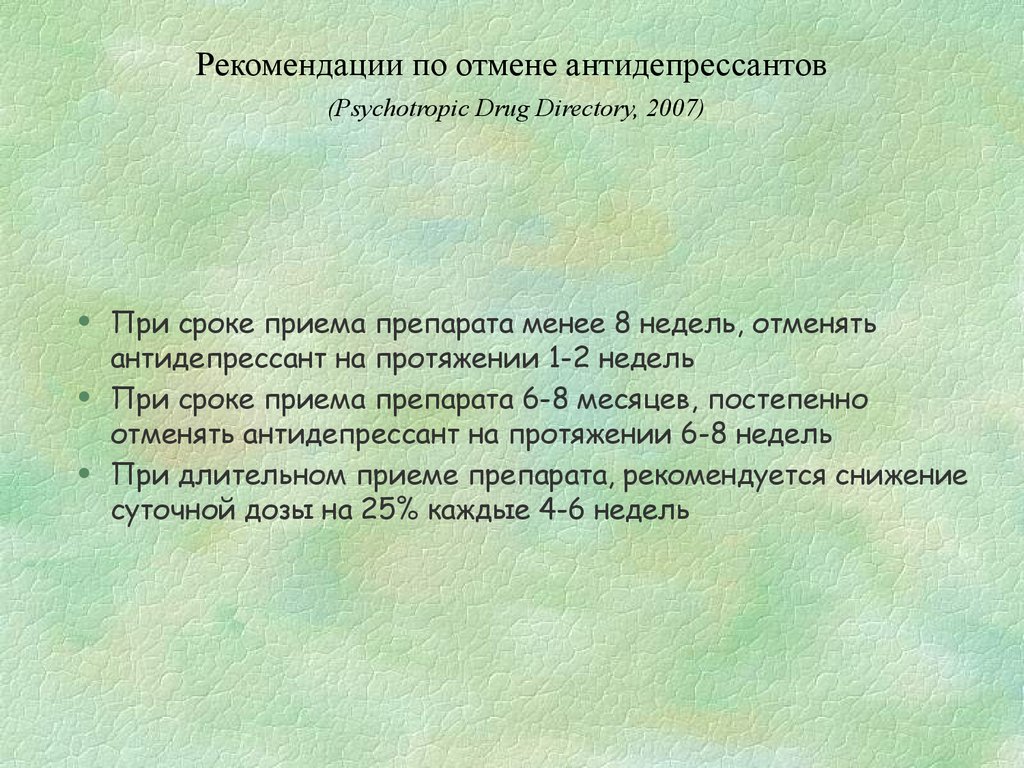
When antidepressants are discontinued, the dose should be reduced in stages, for example by 50%. After that, reduce by another 25%, when small doses are reached, a transition to liquid forms of drugs is possible.
Before each step, you should make sure that there is no or minimal manifestations of the withdrawal syndrome.
Drugs with a short half-life should be discontinued more slowly. Cancellation of fluoxetine, given its prolonged action, can be performed with the transition to taking the drug every other day.
Successful withdrawal of antidepressants can take weeks to months. In severe withdrawal symptoms, the antidepressant should be resumed at full dose and tapered more slowly after symptoms resolve.
Augmentation therapy
Lithium may be used as augmentation therapy for depression. After the appointment and then every 6 months, it is necessary to perform weight control, evaluate the function of the kidneys and thyroid gland, and the level of calcium.
Plasma lithium levels should be assessed 12 hours after the first dose, then 1 week later, and 1 week after each dosage change; further drug monitoring is carried out every 3-6 months, depending on the patient's health status.
The concentration of lithium in the blood plasma should not exceed 1.0 mmol / l (the level required to achieve a therapeutic effect is from 0.4 mmol / l). Cancellation of lithium is carried out within 1-3 months under the supervision of a psychiatrist.
Antipsychotics may also be used to augment therapy, with attention to possible side effects (eg, extrapyramidal symptoms [eg, tremor, parkinsonism], elevated plasma prolactin levels).
When prescribing antipsychotics, it is necessary to monitor the clinical analysis of blood and urine, the concentration of electrolytes, prolactin, glucose and liver enzymes in the blood after 6, 12 weeks and 1 year from the start of therapy, and then annually, and also perform ECG monitoring.
No response to therapy
If there is no response to antidepressants 4 weeks after the start of therapy, the following options for further treatment are possible: combination of medication with psychotherapy or physical education, increasing the dosage or replacing the antidepressant with another.
In particularly resistant forms, a combination with another class of antidepressant, second-generation antipsychotics or lithium is possible.
Selective serotonin reuptake inhibitors, selective serotonin-norepinephrine reuptake inhibitors and tricyclic antidepressants should not be combined with monoamine oxidase inhibitors.
For severe depression, an urgent response to therapy (eg, if the patient is not eating or drinking), and drug resistance, electroconvulsive therapy may be indicated.
Antidepressant withdrawal syndrome: diagnosis, prevention and treatment
04/18/2017
UP TO THE ZMISTU NUMBER
Withdrawal symptoms may occur after discontinuation of any class of antidepressants. The largest number of publications is devoted to selective serotonin reuptake inhibitors (SSRIs), apparently due to the fact that drugs of this class are most often prescribed for the treatment of depressive disorders. Usually these symptoms are mild and disappear on their own after a while. However, some patients may need to resume pharmacotherapy. This review briefly discusses the main clinical aspects of the antidepressant discontinuation syndrome.
The largest number of publications is devoted to selective serotonin reuptake inhibitors (SSRIs), apparently due to the fact that drugs of this class are most often prescribed for the treatment of depressive disorders. Usually these symptoms are mild and disappear on their own after a while. However, some patients may need to resume pharmacotherapy. This review briefly discusses the main clinical aspects of the antidepressant discontinuation syndrome.
This condition is also called antidepressant withdrawal syndrome, although this is not entirely correct. The appearance of symptoms after stopping therapy does not mean that the drug is addictive. Antidepressants do not have addictive potential and do not cause addiction. This is an important positive point that should be communicated to patients, since most people will stop taking the prescribed treatment as soon as possible in case of fear of becoming dependent on the drug.
Why is it important to recognize antidepressant withdrawal syndrome?
There are three reasons: discomfort for the patient, diagnostic problem and possible compliance problems. Although withdrawal symptoms are rarely life-threatening, they are always associated with discomfort and some degree of psychosocial maladjustment. Hence the second problem: having experienced a withdrawal syndrome, the patient hardly agrees to any psychopharmacotherapy in the future. And finally, symptoms that occur in connection with the cessation of the action of an antidepressant can be mistaken for an exacerbation of a depressive disorder, another mental disorder, or a physical illness.
For example, consider two typical scenarios. Convinced of achieving remission of major depressive disorder, the doctor hurries to please the patient that the antidepressant can be stopped, but forgets to tell how to do it correctly. The patient takes everything literally and the next day forgets about the medicine. A week later, he develops withdrawal symptoms, and he addresses his complaints to a) the same psychiatrist who forgets to ask how the antidepressant was withdrawn and perceives the symptoms as a relapse of depression; b) to another specialist, for example, a neurologist, to whom he prefers not to report about treatment with a psychiatrist. And the neurologist interprets these non-specific symptoms according to his competence. As a result, unnecessary examinations and possibly even treatment.
A week later, he develops withdrawal symptoms, and he addresses his complaints to a) the same psychiatrist who forgets to ask how the antidepressant was withdrawn and perceives the symptoms as a relapse of depression; b) to another specialist, for example, a neurologist, to whom he prefers not to report about treatment with a psychiatrist. And the neurologist interprets these non-specific symptoms according to his competence. As a result, unnecessary examinations and possibly even treatment.
In addition, symptoms can be confused with side effects of a newly prescribed drug after discontinuation of an antidepressant, especially when switching between antidepressants with different mechanisms of action, for example, from paroxetine (SSRI) to bupropion (a dopamine and norepinephrine reuptake inhibitor). This can lead to the erroneous conclusion that the patient does not tolerate the new drug well. Symptoms of discontinuation of therapy may also be perceived as failure of therapy, especially irritability and anxiety.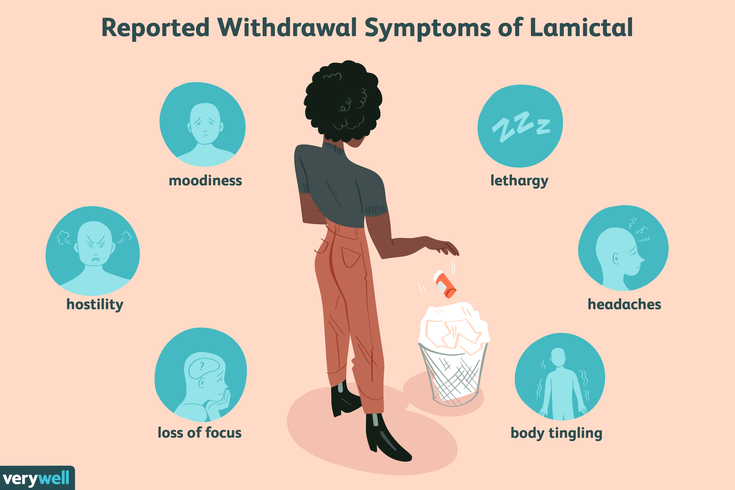
Symptoms of discontinuation of antidepressant therapy can be divided into six categories: sensory symptoms, balance disorders, general somatic, affective, gastrointestinal symptoms, and sleep disorders (Fig.).
At first, information about the listed manifestations was accumulated from reports of clinical cases. Then this problem was studied in prospective double-blind clinical trials in which patients were specifically randomized to the abolition of antidepressant therapy.
In English literature, a mnemonic device is used to memorize the spectrum of antidepressant withdrawal syndrome: the main symptoms are encrypted in the word FINISH.
F for "flu-like" - flu-like symptoms;
I - insomnia;
N - from "nausea" - nausea;
I - from "imbalance" - imbalance;
S - sensory symptoms;
H - from "hyperarousal" - increased excitability, which reflects affective disorders.
It should be noted that the symptoms presented in the figure are mainly associated with discontinuation of SSRIs and serotonin and norepinephrine reuptake inhibitors.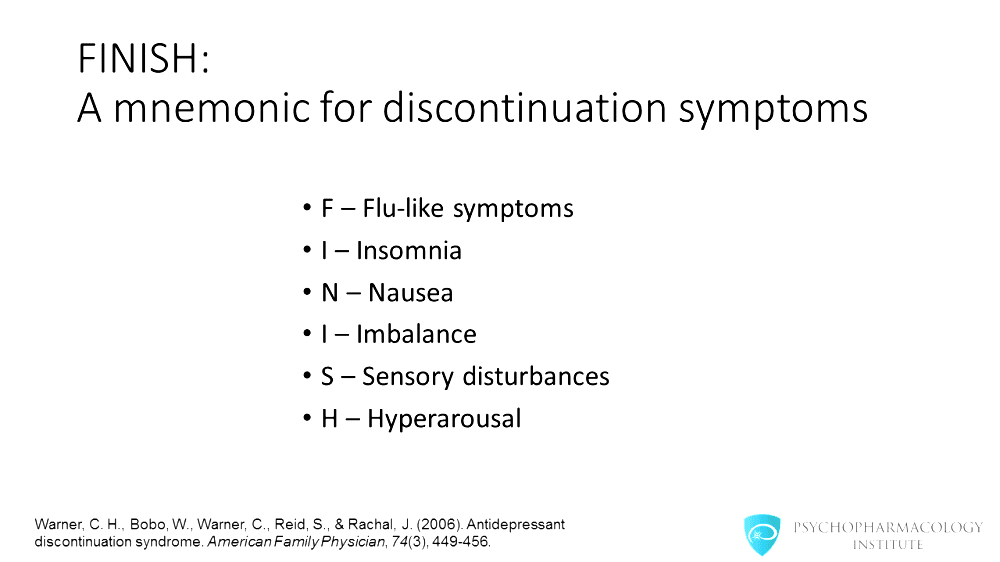 The spectrum of symptoms during withdrawal of monoamine oxidase inhibitors (MAOIs) and tricyclic antidepressants has its own specifics. Thus, in the event of discontinuation of tricyclic antidepressants, sensory symptoms and balance disorders, as a rule, are not observed. With the abolition of MAO inhibitors, symptoms may be more pronounced than after the abolition of SSRIs. Patients may experience a worsening of depressive and anxiety symptoms, an acute impairment of consciousness up to catatonia.
The spectrum of symptoms during withdrawal of monoamine oxidase inhibitors (MAOIs) and tricyclic antidepressants has its own specifics. Thus, in the event of discontinuation of tricyclic antidepressants, sensory symptoms and balance disorders, as a rule, are not observed. With the abolition of MAO inhibitors, symptoms may be more pronounced than after the abolition of SSRIs. Patients may experience a worsening of depressive and anxiety symptoms, an acute impairment of consciousness up to catatonia.
When do withdrawal symptoms appear and how long do they last?
They usually appear within the first week after stopping the antidepressant; according to studies, on average on the second day. Spontaneous resolution occurs at different times - from 1 day to 3 weeks, on average, patients continue to experience symptoms for 10 days.
What causes withdrawal syndrome?
The syndrome occurs when antidepressants of all classes are discontinued.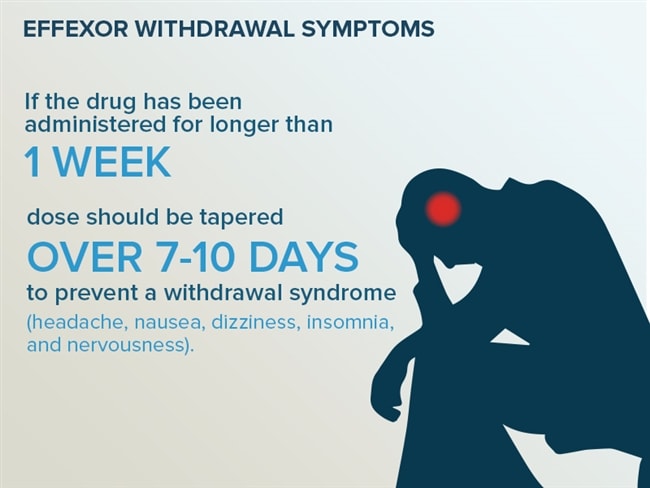 The largest number of reports was recorded for paroxetine. The half-life of the drug from blood plasma is the indicator that correlates more than others with the risk of developing a withdrawal syndrome. In other words, the shorter the residual effect of the drug after the last dose, the higher the likelihood of symptoms.
The largest number of reports was recorded for paroxetine. The half-life of the drug from blood plasma is the indicator that correlates more than others with the risk of developing a withdrawal syndrome. In other words, the shorter the residual effect of the drug after the last dose, the higher the likelihood of symptoms.
For example, fluoxetine has a half-life of 7 days, so this SSRI has the lowest risk of withdrawal. Paroxetine has an average half-life of 24 hours, hence the high risk of withdrawal syndrome, especially when the therapeutic dose is abruptly stopped.
Can antidepressant discontinuation syndrome be distinguished from relapse of depression?
Common symptoms include dysphoria, decreased appetite, sleep disturbances and fatigue. But there are also distinctive features—symptoms that are rarely seen in depression, such as sensory phenomena (paresthesias) as well as dizziness, headache, and nausea. In addition, in the case of withdrawal syndrome, a rapid (within 1 day) improvement can be observed when the drug is resumed, while recurrent depression does not respond so quickly to therapy.
Who is at risk for developing antidepressant withdrawal syndrome?
Typically, these are patients who begin to feel better after a few weeks of taking an antidepressant and are not sufficiently informed about the need for long-term maintenance therapy. Women who find out they are pregnant during treatment may also abruptly stop taking the antidepressant for safety reasons.
How to stop antidepressants to minimize the risk of withdrawal?
Patients should be explained in an accessible form the features of the action of the prescribed antidepressant, the rules for increasing and gradually reducing the dose, and warn about a possible deterioration in well-being in the event of an abrupt cessation of therapy. But at the same time, the words "withdrawal syndrome", "addiction", "addiction" should be avoided, since they can be perceived negatively and cause early termination of therapy. Sooner or later, that happy moment comes when it becomes clear that antidepressants can be abandoned. However, the withdrawal process, as a rule, takes several weeks, but in some cases even longer, especially if the patient's health worsens at the first steps of dose reduction. When prescribing fluoxetine, it is possible to cancel the drug without a gradual dose reduction, although it has not been specifically studied in studies.
However, the withdrawal process, as a rule, takes several weeks, but in some cases even longer, especially if the patient's health worsens at the first steps of dose reduction. When prescribing fluoxetine, it is possible to cancel the drug without a gradual dose reduction, although it has not been specifically studied in studies.
If possible, you should also discuss with the patient's relatives the creation of the most favorable conditions for the period of antidepressant withdrawal. Patients with major depressive disorder, as a rule, do not work and are at home, therefore they are not subjected to external psycho-emotional stress. It is optimal if the patient's close environment tries to create a positive atmosphere and tries to involve a family member in some kind of activity in order to distract from the perception of possible withdrawal symptoms.
How to help patients who complain of feeling worse after stopping antidepressants?
If this does happen, explain to the patient that the symptoms are not life-threatening and usually resolve within a few days. If the patient continues to experience symptoms and they reduce quality of life, it is common practice to restart the therapeutic dose of the antidepressant. In the future, you can again try to stop the drug through a very gradual dose reduction. If this does not help, then it is possible to transfer the patient to fluoxetine-SSRI with the lowest risk of withdrawal syndrome, and then cancel it.
If the patient continues to experience symptoms and they reduce quality of life, it is common practice to restart the therapeutic dose of the antidepressant. In the future, you can again try to stop the drug through a very gradual dose reduction. If this does not help, then it is possible to transfer the patient to fluoxetine-SSRI with the lowest risk of withdrawal syndrome, and then cancel it.
Literature
1. Haddad P.M., AndersonI.M. (2007). Recognizing and managing antidepressant discontinuation symptoms. Advances in Psychiatric treatment, 13(6): 447-457.
2. Warner C.H., Bobo W., Warner C., Reid S., Rachal J. (2006). Antidepressant discontinuation syndrome. American Family Physician, 74(3): 449-456.
3. Renoir T. (2013). Selective serotonin reuptake inhibitor antidepressant treatment discontinuation syndrome: a review of the clinical evidence and the possible mechanisms involved. Frontiers in Pharmacology, 4.
Prepared by Dmitry Molchanov
- Number:
- Thematic issue "Neurology, Psychiatry, Psychotherapy" No.
 1 (40), March 2017
1 (40), March 2017
11/25/2022 PsychiatryTherapy and family medicine Treating depressive disorder
In today's world, depression is one of the most widespread mental disorders. Show illness and negative consequences both on the psychological and on the somatic level, and severe depression can become a cause of suicide. In the absence of a decrease in the quality of life of ailments, and a stronger focus on the economic and medical systems of the country, the urgency of this illness is mindful. About modern standards of diagnostics and methods of treating depressive disorder in its dopovіdі at the international neurological conference "XIV Neurosymposium" by Prof. Allan H. Young....
Young....
11/20/2022 Psychiatry Somatically unreasonable syndromes and functional disorders at the sight of a psychiatrist
The conference “Internal medicine in the minds of modern people” was organized by the Department of Internal Diseases of the Faculty of Dentistry of the National Medical University. O.O. Bogomolets (m. Kyiv), community organizations "Academy of Internal Medicine" (m. Kiev) and "Polish Medical Association in Ukraine named after. A.S. Svіncіtskogo” (m. Kiev). Tsya zustrіch bula was dedicated to the nutrition of diagnostics, exaltation, as well as the prevention of illness in the ambush of evidence-based medicine ....
21. 10.2022 Psychiastraita, the bartness of the non-bonds of the unanimous vitrati at the likovanni with antideparests: the results of a systematic look at the Merei Metaaliza of the Ekonomic Modeling
10.2022 Psychiastraita, the bartness of the non-bonds of the unanimous vitrati at the likovanni with antideparests: the results of a systematic look at the Merei Metaaliza of the Ekonomic Modeling
Great Depressive Rosemy of the Glorita, the 13th cause of the 13th reason. sickness [1, 2]. Antidepressants are the main means of treating the great depressive disorder. As previous studies have shown, drugs of the same class may have similar efficacy, but they may also vary significantly in the profile of side effects [3, 6-10]. Such manifestations as anxiety, sleeplessness, sexual dysfunction, changes in body mass, anhedonia (lack of satisfaction), are blamed practically on another patient's skin for depression, which can be overcome by the influx of antidepressants, which often become a cause [4]. Also, current recent data on side effects can help clinicians choose antidepressants to treat their patients.