Stomach rejecting everything
What Happens When Your Gut Starts Rejecting Food
Smoking and obesity can be bad for your gut health
Highlights
- Risk factors for GERD are direct consequences of lifestyle and diet
- Medication like mild antacids may be prescribed in mild to severe cases
- Extreme cases may require surgery (Fundoplication) and stronger medicines
We all have had someone tell us to always 'follow our gut feeling' when we're anxious or stressed. While most of us have perceived the phrase as something emotional, you'd be surprised to know that it also applies in terms of your physical well-being. The gastrointestinal system is not only the body's prime site of absorbing nutrients, but it also acts as a communication center to and from the brain, and functions as one of the body's frontlines in the fight against disease. However, with increasing urbanisation and a highly competitive environment, the day-to-day healthy routine of majority of the people have changed drastically leading to them falling prey to various disorders.
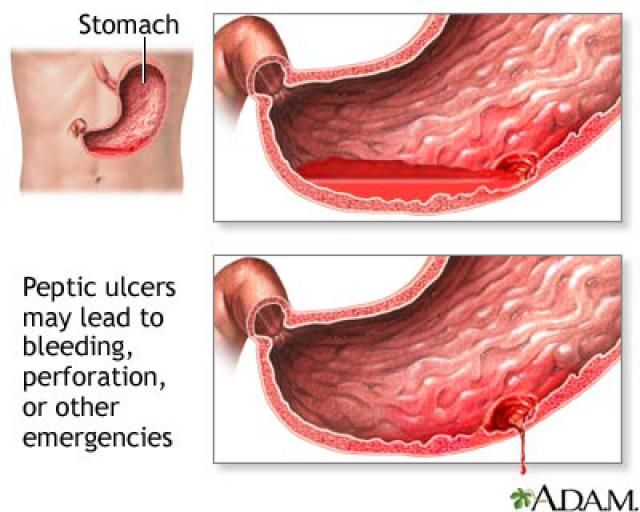
One such serious digestive disorder is acid reflux or gastro oesophageal reflux disease (GERD). GERD is typically defined as the phenomena when acidic liquid contents from stomach frequently back up into the food pipe leading to injury or inflammation in the lining of the food pipe (oesophagus). It is caused either by increased acid output or when the junction of the food pipe and stomach has a loose/weak muscle valve due to which the LES (lower oesophageal sphincter) doesn't close properly or tightly enough resulting in the food content to rise back up into the oesophagus. If the sphincter relaxes abnormally or weakens, stomach acid can flow back up into your oesophagus.
One can easily confuse the symptoms of GERD for a simple case of gastric problem. Some of them are burning sensation in your chest, usually after eating, have difficulty in swallowing or regurgitation (bringing up) of food. Apart from these, other symptoms to look out for are a lump in your throat, chronic cough, laryngitis, new or worsening asthma and disrupted sleep.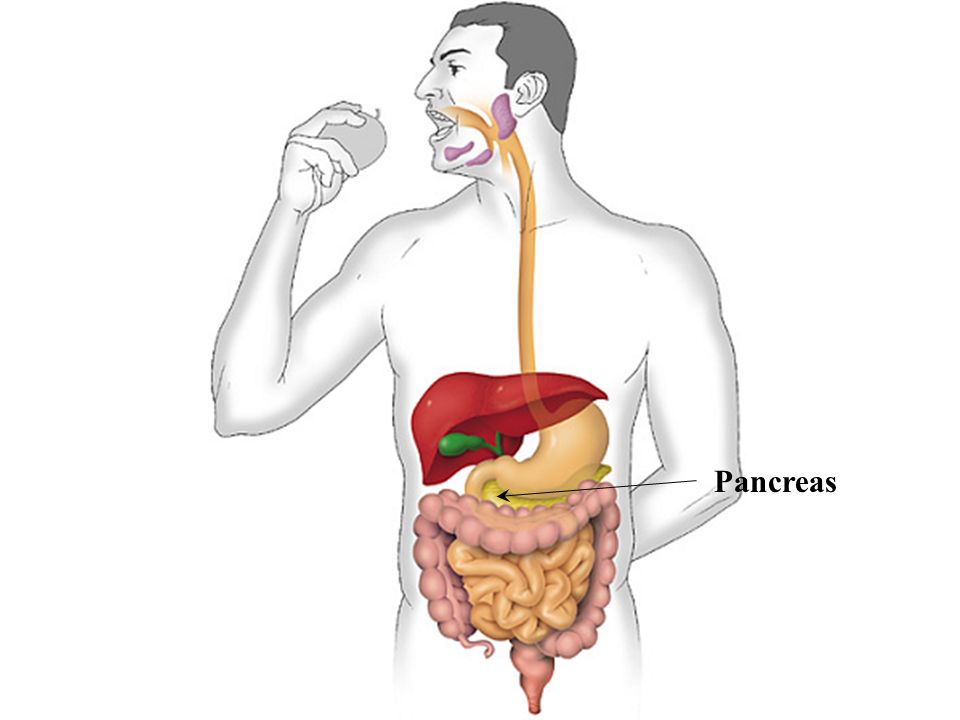
According to recent studies carried out by The Indian Society of Gastroenterology the prevalence of GERD in India is likely to be between 8% and 19%, which is comparable to GERD prevalence rates published in western countries. Additionally, these studies highlight that the risk factors for GERD are related to diet and lifestyle choice; which are both modifiable risk factors such as:
- Obesity
- Smoking
- Delayed stomach emptying
- Having large meals or eating late at night
- Eating trigger foods rich in fat or fried
- Consumption of alcohol, carbonated drinks, coffee, tea and caffeine rich energy drinks.
- Frequent use of medications like aspirin, painkillers
Having an empty stomach for too long can cause GERD
Photo Credit: iStock
Also read: Facing Gastrointestinal Issues? You Could Be Depressed
Mild GERD (acid reflux occurring only once a week) is quite common and may be managed with some lifestyle changes and mild over the counter medicines, however, severe GERD (Acid reflux once a day) may need stronger medications or in refractory situations even surgery to ease symptoms.
Doctors usually diagnose GERD based on symptoms and physical examination. Sometimes a short duration of treatment with mild antacids may be advised to see for response specially in the absence of any worrying symptoms. Further evaluation for diagnosis confirmation or for refractory symptoms includes upper gastrointestinal endoscopy, 24 hour ambulatory acid (ph) and impedance probe test, oesophageal manometry and an x-ray of your upper digestive system.
The first step in management of GERD is lifestyle modification which includes eating on time, increasing physical activity, avoiding fatty and fried food, not smoking or consuming alcohol and/or carbonated drinks. Cutting down significantly on tea and coffee also helps.
Also read: Are You Taking Pills For Heartburn, Acid Reflux Too Frequently? Take Note As It May Lead To Early Death Due To These Diseases, Says Study
In case the above remedies do not work, the below medications also help, however, should be taken for a short duration of time:
1. Liquid antacids: Antacids, such as Digene, Mucaine gel and Gaviscon etc. may provide quick relief. But antacids alone won't heal an inflamed oesophagus damaged by stomach acid. Overuse of some antacids can cause side effects, such as diarrhoea or sometimes kidney problems.
Liquid antacids: Antacids, such as Digene, Mucaine gel and Gaviscon etc. may provide quick relief. But antacids alone won't heal an inflamed oesophagus damaged by stomach acid. Overuse of some antacids can cause side effects, such as diarrhoea or sometimes kidney problems.
2. Medications to reduce acid production: These medications - known as H-2-receptor blockers - include famotidine and ranitidine. H-2-receptor blockers don't act as quickly as antacids, but they provide longer relief and may decrease acid production from the stomach for up to 12 hours.
3. Medications that block acid production and heal the oesophagus: These medications - known as proton pump inhibitors - are stronger acid blockers than H-2-receptor blockers and allow time for damaged oesophageal tissue to heal. Examples are Omeprazole, Pantoprazole, Rabeprazole etc. Although these medications bring quick relief they should not be used indiscriminately and long term as that can lead to serious infections and deficiencies.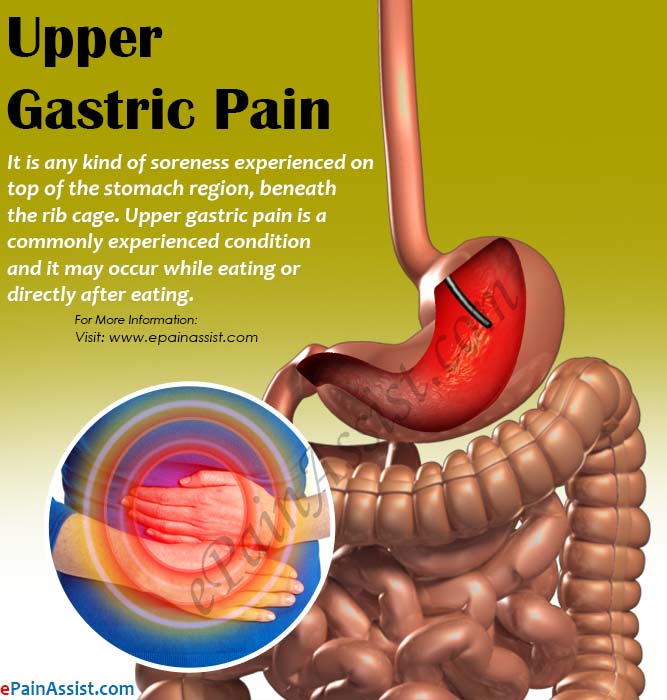
4. Medication to strengthen the lower oesophageal sphincter: Baclofen may ease GERD by decreasing the frequency of relaxations of the lower oesophageal sphincter. Serious side effects might include fatigue or nausea and even loss of consciousness. This medicine should strictly be taken only under medical supervision and in very selected situations.
Also read: What Is Acid Reflux? What Are The Best Foods To Have If You Have Acid Reflux? Our Expert Nutritionist Tells It All
5. Fundoplication (Surgery): While, GERD can usually be controlled with medication. But if medications don't help or you wish to avoid long-term medication use, your doctor might recommend Fundoplication. The surgeon wraps the top of your stomach around the lower oesophageal sphincter, to tighten the muscle and prevent reflux. Fundoplication is usually done with a minimally invasive (laparoscopic) procedure. The wrapping of the top part of the stomach can be partial or complete.
Therefore, if your gut starts rejecting food, please do not try to self-diagnose, instead visit a medical expert. Adding to that, you should immediately see a doctor in case you're experiencing frequent GERD symptoms, taking medicines for heartburn more than twice a week or getting severe chest pain with breathlessness.
Promoted
Listen to the latest songs, only on JioSaavn.com
(Dr. Shanti Swaroop Dhar, Principal Consultant - Gastroenterology, Max MultiSpeciality Centre, Panchsheel Park)
Disclaimer: The opinions expressed within this article are the personal opinions of the author. NDTV is not responsible for the accuracy, completeness, suitability, or validity of any information on this article. All information is provided on an as-is basis. The information, facts or opinions appearing in the article do not reflect the views of NDTV and NDTV does not assume any responsibility or liability for the same.
Gastroparesis: Causes, Symptoms, and Diagnosis
Gastroparesis is a disorder that occurs when the stomach takes too long to empty food. This disorder leads to a variety of symptoms that can include nausea, vomiting, feeling easily full, and a slow emptying of the stomach, known as delayed gastric emptying.
This disorder leads to a variety of symptoms that can include nausea, vomiting, feeling easily full, and a slow emptying of the stomach, known as delayed gastric emptying.
Gastroparesis can be due to a variety of issues. There’s no known cure for gastroparesis, but medical treatment can help you manage your symptoms. Here’s what you need to know.
The symptoms of gastroparesis can range from mild to severe. They occur more often in some people than others.
The symptoms of gastroparesis can include:
- upper abdominal pain
- nausea
- vomiting
- loss of appetite
- bloating
- feeling full
- malnutrition
- unintended weight loss
While the exact cause of gastroparesis isn’t known, it’s thought to have something to do with disrupted nerve signals in the stomach.
It’s believed that when the nerves to the stomach become affected by a variety of factors, food can move through it too slowly.
Other problems, such as the stomach being overly sensitive to signals from the nervous system and the stomach not being able to react to a meal, are believed to also have a role in this condition.
Most types of gastroparesis fit into one of these categories:
- idiopathic, or unknown
- diabetes-related
- postsurgical
Nearly 36 percent of gastroparesis cases aren’t linked to an identifiable cause. This is known as idiopathic. Many times this condition occurs after a viral illness, but it’s not fully understood.
Surgeries that involve the stomach or other digestive organs can also change signals to the stomach. About 13 percent of people with gastroparesis have the type known as postsurgical.
A common cause of damage to the nervous system that affects the digestion is diabetes, specifically diabetes that isn’t well-controlled.
This is because high blood sugar can damage nerves over time, including the vagus nerve, which controls the movement of food through the digestive system.
Maintaining healthy blood sugar levels by making changes to your diet and lifestyle is an effective way to help control symptoms of gastroparesis for people with diabetes.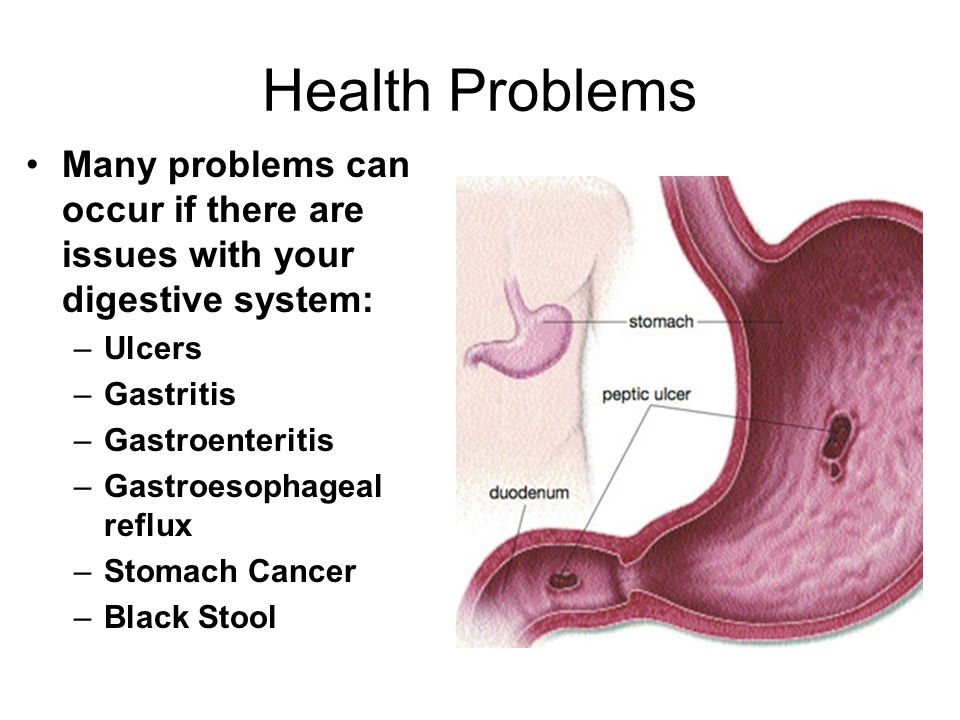
Other health conditions are also associated with gastroparesis but are less common. These include:
- viral infections
- some cancers
- cystic fibrosis
- Parkinson’s disease
- autoimmune diseases
- amyloidosis, a condition that causes an abnormal protein buildup in organs
- medications that make the stomach empty more slowly
- thyroid disorders
The symptoms associated with gastroparesis, such as vomiting and decreased appetite, can cause dehydration and malnutrition. Dehydration and malnutrition can cause numerous problems, including:
- electrolyte imbalances
- decreased blood pressure
- increased heartbeat
- rapid breathing
- decreased urine output
- a weakened immune system
- poor wound healing
- muscle weakness
Since gastroparesis causes food to stay in the stomach for too long, it can also cause an overgrowth of bacteria. The food can also harden into masses called bezoars that cause nausea, vomiting, and obstruction in the stomach.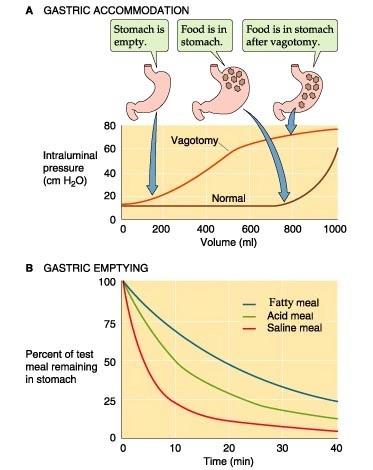
Managing blood glucose levels is essential for people with diabetes. Gastroparesis can make it harder to manage those levels.
Other medications stimulate the stomach muscles and help with digestion. These include:
- metoclopramide (Reglan)
- erythromycin (EES)
- domperidone (Motilin)
However, these drugs can cause side effects. Talk with your doctor to weigh the pros and cons of each medication to find out which one is right for you.
Your doctor will perform a physical exam and ask you questions about your medical history. In order to rule out other possible causes of your symptoms, your doctor will probably want to run some tests. These might include:
- An ultrasound. Ultrasounds use sound waves to create an image of your organs. It can be used to rule out liver disease, pancreatitis, and gallbladder disease.
- Blood tests. Blood tests can check for diabetes and other conditions.
- An upper endoscopy.
 In an upper endoscopy procedure, your doctor guides a long, thin scope down your esophagus and into your stomach to check for blockages in the stomach and other conditions.
In an upper endoscopy procedure, your doctor guides a long, thin scope down your esophagus and into your stomach to check for blockages in the stomach and other conditions.
Once your doctor has ruled out other possible causes of your symptoms, they’ll order tests to evaluate how well your stomach empties. These tests can include a:
- gastric emptying scintigraphy test. A gastric emptying scan involves eating a small amount of food with a harmless radioactive substance so your doctor can see how fast food is being digested and emptied from your stomach.
- SmartPill. A SmartPill is a capsule that contains a device to track how fast food moves through your digestive tract.
- carbon breath test. In this test, carbon dioxide production is tracked through the digestive system.
If your gastroparesis is caused by a condition like diabetes, the first step is to improve control of that underlying condition. After that, your doctor may recommend medications, diet changes, and even surgery in some cases.
After that, your doctor may recommend medications, diet changes, and even surgery in some cases.
Medication
Your doctor may prescribe one or more medications to treat your gastroparesis.
Medications to control nausea and vomiting caused by gastroparesis can include:
- prochlorperazine (Compro)
- ondansetron (Zofran)
- promethazine (Phenergan)
Surgery
If your malnutrition or vomiting remains an issue even with the use of medications, your doctor may decide surgery is necessary. The goal of surgery for gastroparesis is to help your stomach empty more effectively.
A stomach stimulator known as a GES (gastric electrical stimulator) can be implanted into the stomach. This device is FDA-approved for use if medications don’t work.
One study of 33 people showed that in the first year after this surgery, up to 97 percent of people with a GES have less nausea and vomiting and are able to gain weight. The device may also improve life expectancy related to gastroparesis.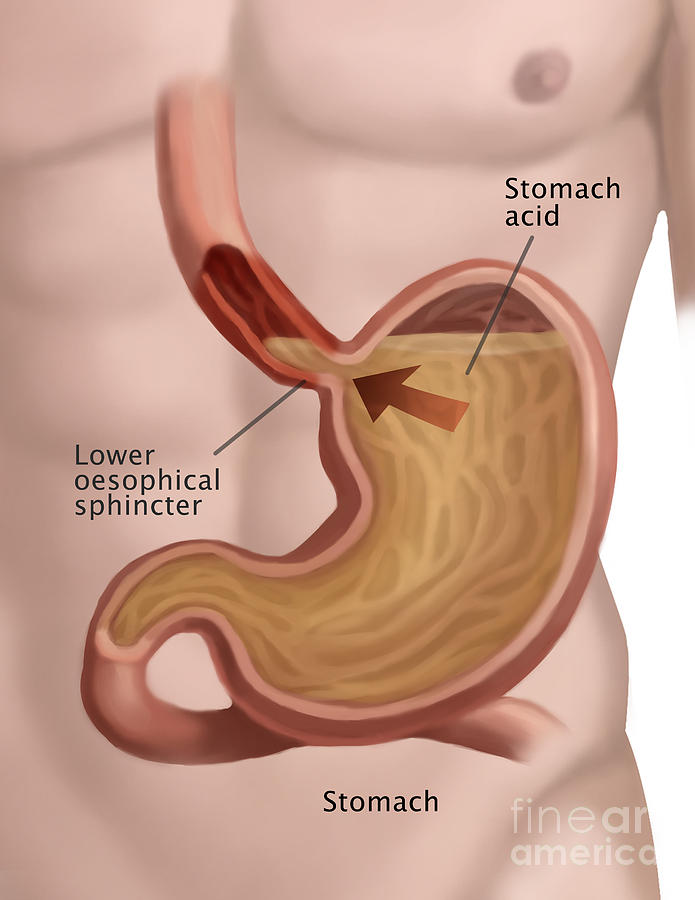
Diet changes
Seeing a dietitian — an expert on food and nutrition — is a common part of treatment for gastroparesis. A dietitian can suggest foods that your body can digest more easily, allowing your body to absorb more nutrients.
Your dietitian might make suggestions, including:
- eating four to six meals per day
- drinking high-calorie liquids
- limiting alcohol and carbonated beverages
- taking a daily multivitamin, if tolerated
- limiting certain meats and dairy
- eating well-cooked vegetables and fruit to lower the amount of fiber they contain
- eating mostly low-fat foods
- avoiding high-fiber foods, like broccoli and oranges
- not lying down for bed immediately after a meal
- substituting solid foods for puréed or liquid foods
A change in diet could be preferable to taking medication, as medicine tends to have undesirable side effects. If you have a severe case of gastroparesis, you might not be able to eat solid foods and drink liquids. In this case, you may need a feeding tube until your condition improves.
In this case, you may need a feeding tube until your condition improves.
Botulinum toxin type A
Botulinum toxin type A is a toxin that reduces muscle activity. It’s been studied in gastroparesis and other gastrointestinal tract disorders.
Injection of the medication into the pyloric sphincter muscle improved this condition in some studies. However, due to contradictory results and the small size of most studies, scientists state that more research is needed before it can be recommended.
Vagal nerve stimulation
The vagus nerve is important to digestion. In 2018, research was underway to study the use of vagal nerve stimulation for people with gastroparesis. This study was looking at the effectiveness of self-administered nerve stimulation twice a day.
The hope is that vagal nerve stimulation will help reduce inflammation and nerve problems associated with gastroparesis.
If you suspect you have gastroparesis, talk to your doctor. They’ll do a thorough exam before diagnosing the condition.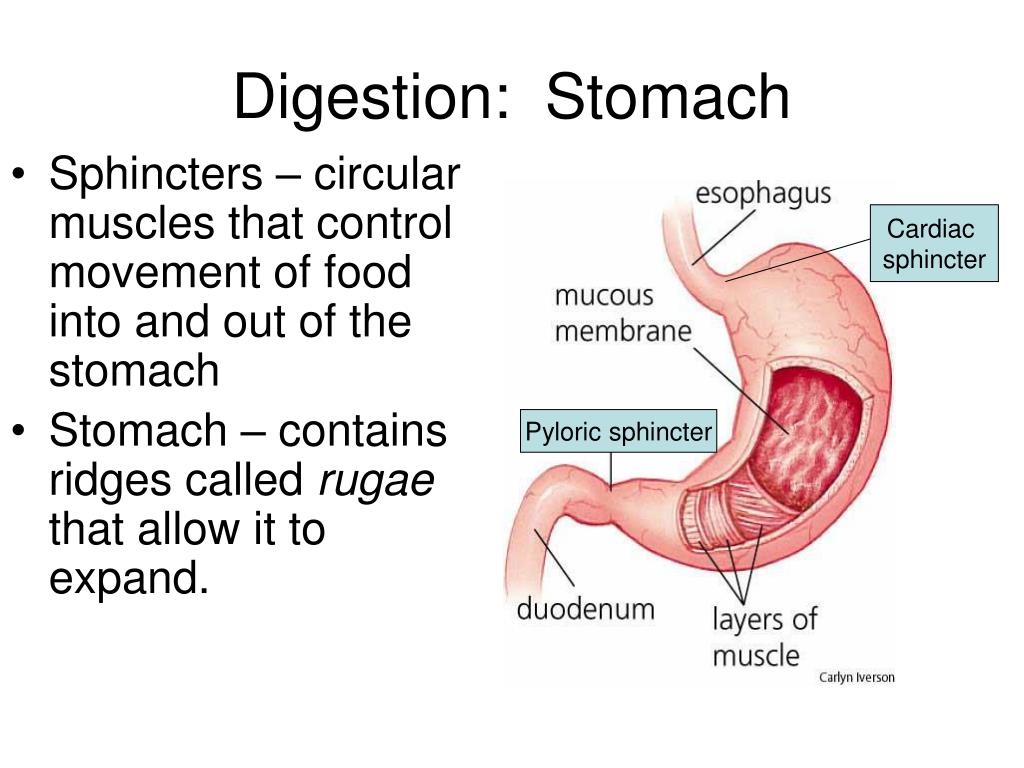 If you do have gastroparesis, work with your doctor to develop a treatment plan based on your particular health needs.
If you do have gastroparesis, work with your doctor to develop a treatment plan based on your particular health needs.
What is the life expectancy for someone with gastroparesis?
Though gastroparesis is not a life threatening condition, it can cause serious complications, including malnutrition and dehydration.
However, if symptoms are managed effectively, people with gastroparesis can expect to have a normal life expectancy.
How should I handle a flare-up of gastroparesis?
Making changes to your diet and lifestyle is an effective way to manage symptoms of gastroparesis.
Eating several smaller meals per day, limiting foods that are hard to digest, and swapping solid foods for liquid or pureed ingredients can all be beneficial.
Your doctor may also prescribe medications to help control symptoms like nausea or vomiting during a flare-up.
What are the symptoms of slow digestion?
Gastrointestinal issues like nausea, vomiting, bloating, and stomach pain are some of the most common symptoms of slow digestion.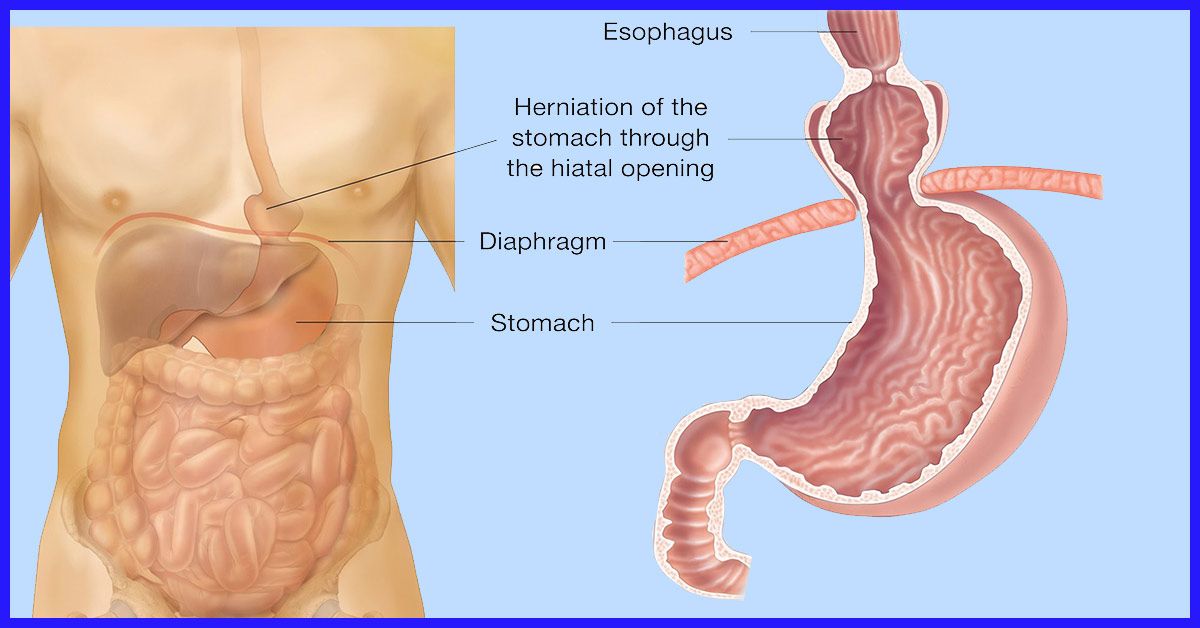
Other symptoms may include loss of appetite, unintentional weight loss, or feeling full after eating only a small amount.
Can gastroparesis go away?
Gastroparesis is a chronic condition and there is currently no known cure.
However, symptoms can be managed effectively for many people using a combination of treatments, including medications, surgical procedures, and diet and lifestyle changes.
What foods should you avoid if you have gastroparesis?
People with gastroparesis should limit their intake of hard-to-digest foods to help reduce symptoms.
This includes foods high in fiber, such as raw fruits and vegetables, nuts, seeds, and whole grains.
You should also limit fried foods, high-fat meat and dairy products, alcohol, and carbonated beverages to help manage symptoms.
Nausea and vomiting after eating - causes, symptoms and treatment, how to relieve nausea
Co-author, editor and medical expert - Klimovich Elina Valerievna.
Number of views: 86 794
Date last updated: 12/20/2021
Average reading time: 5 minutes
are violated. And instead of moving food to the intestines, where the digestive processes will continue and end, it pushes it up - into the esophagus and oral cavity.
Symptoms
Nausea is manifested by an unpleasant sensation in the upper abdomen, often described as a "sucking", "pulling" feeling. This may be accompanied by weakness, dizziness, increased salivation, pallor of the skin. And as nausea develops, it often ends with vomiting - the involuntary eruption of stomach contents out through the mouth.
Nausea after eating, ending with emptying of the stomach, followed by a feeling of relief, most often indicates malnutrition or overeating.
Causes of nausea and vomiting
Food allergies
Some foods tend to cause nausea and vomiting if a person has an individual intolerance to these foods or an increased sensitivity of the immune system (allergy).
Improper nutrition
Nausea is a natural consequence of overeating (both constant and episodic). This symptom can be especially pronounced when eating fatty, fried, spicy foods. In this case, the inability of the digestive juices to process the “heavy” food joins the overflow of the stomach with an excessively large portion.
Poisoning
Nausea may be one of the symptoms of food poisoning due to the consumption of stale or poorly prepared food, expired products, tap water, etc.
Excessive alcohol consumption
drinks, is a complex reaction, in the development of which not only the gastrointestinal tract, but also the nervous system is involved. In the stomach, alcohol destroys the protective layer of the mucosa and impairs motility, and the nervous system, reacting to it as a poison, activates processes to remove it from the body, i.e., provokes vomiting.
Smoking
In addition to the fact that the components of tobacco cause disturbances in peristalsis (contractions of the walls of the stomach and intestines), the components of tobacco smoke, swallowed with saliva, irritate the walls of the stomach and can cause nausea.
Psychological factors
Excessive psycho-emotional stress, lack of rest, being in stress mode - all this seriously affects the functioning of the gastrointestinal tract, which can react with constipation, diarrhea, bloating, nausea or vomiting.
Disorders of the digestive system
Feelings of nausea, as well as vomiting, are not independent diseases - these are symptoms that may indicate some kind of digestive system health problems, especially if these symptoms are observed often or regularly.
How to prevent vomiting after eating
Nausea after eating, caused by overeating or heavy food, does not necessarily end with vomiting. To prevent unwanted developments and relieve discomfort, you should follow just a few recommendations.
First of all, it is necessary to ensure the flow of fresh air: open the windows or go out onto the balcony, outside and take a deep breath.
After that, it is advisable to drink a glass of clean non-carbonated water at room temperature. Avoid taking hot drinks or, conversely, chilled ones - high and low temperatures will further disrupt the motor functions of the stomach, exacerbating the feeling of nausea.
Avoid taking hot drinks or, conversely, chilled ones - high and low temperatures will further disrupt the motor functions of the stomach, exacerbating the feeling of nausea.
Now assume a comfortable sitting or reclining position and minimize physical activity for a while until nausea and the threat of vomiting after eating has passed.
Nausea relief
Maintaining a healthy lifestyle
Smoking, alcohol consumption, sedentary lifestyle, non-observance of the daily routine - these factors negatively affect both the health of the gastrointestinal tract, causing indigestion and nausea, and the state of the whole organism as a whole.
Nutrition correction and diet
Healthy eating implies not only the correct selection of products, control of their freshness and quality of preparation, but also eating at strictly defined times, moderate portions, avoiding foods that are harmful to the stomach.
After the acute attack of nausea has passed, think over further food: it should not include fatty, spicy, fried, sweet, too hot and cold dishes. Keep portions small, ideally breaking up the daily amount of food into 5-6 meals.
Keep portions small, ideally breaking up the daily amount of food into 5-6 meals.
When to See a Doctor
Single episodes of vomiting are rarely a cause for concern. But with repeated attacks, when the cause of these symptoms is unknown, you should consult a doctor. Particular attention should be paid to vomiting, which is accompanied by headache, loss of strength, drowsiness, impaired consciousness and deterioration of the general condition. Nausea and vomiting can develop after trauma to the head and internal organs. In this case, it is necessary to consult a doctor and conduct an examination.
Stomach does not take food, vomiting
If the stomach regularly rejects food, this phenomenon very often indicates a disease of the digestive system. The condition when the digestion of food by the stomach suffers is called dyspepsia, which is accompanied by nausea and vomiting after eating. In rare cases, when you feel sick, a single gag reflex can be a symptom associated with a violation of the diet.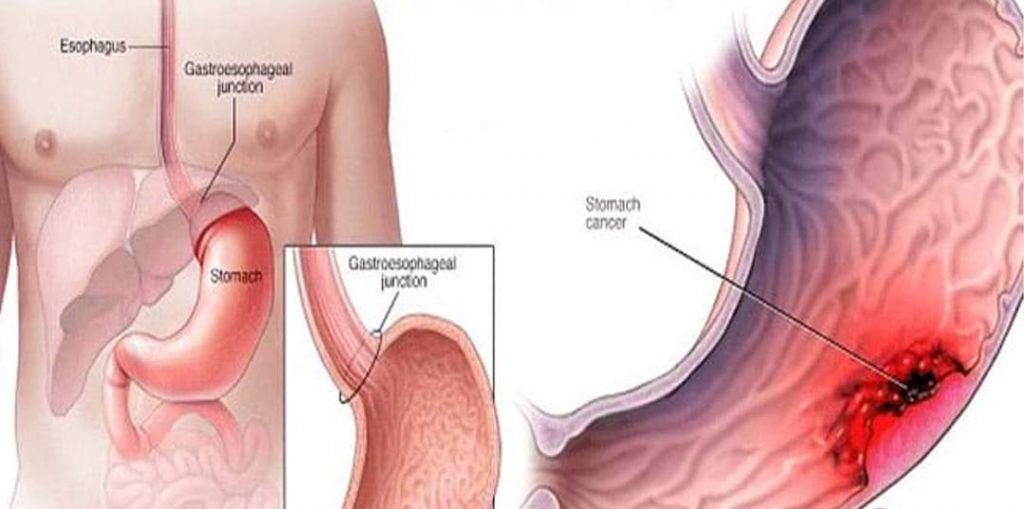
Causes of vomiting
- the use of poor-quality food products - the body is poisoned by toxic substances that have entered the body with food;
- gastritis and peptic ulcer;
- diseases of the pancreas and gallbladder;
- gag reflex after eating in stressful situations - due to a disease of a nervous nature;
- overeating;
- consumption of significant amounts of alcohol;
- stomach reaction to certain medications;
- the presence of a volumetric process in the stomach;
- acute appendicitis with abdominal pain, nausea and vomiting;
- diseases of the central nervous system - volumetric process or brain injury;
- first months of pregnancy;
- diseases of the vestibular apparatus - "motion sickness" when driving in transport;
- viral infections;
- helminthic infestations;
- chemotherapy in oncological diseases.
Rare episodes of the gag reflex that occur when overeating or eating certain foods require a mandatory adjustment of the diet.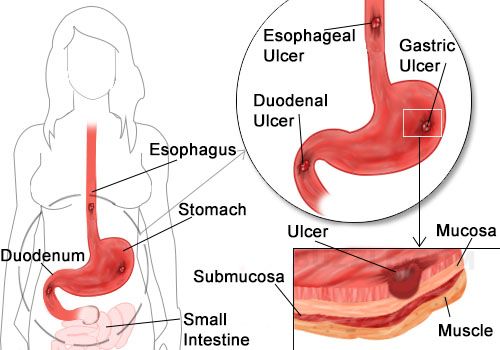 But if the stomach does not accept high-quality food, after which nausea appears, and then a gag reflex, this is already a direct indicator for contacting a doctor. It is necessary to find out the cause of this phenomenon and treat it.
But if the stomach does not accept high-quality food, after which nausea appears, and then a gag reflex, this is already a direct indicator for contacting a doctor. It is necessary to find out the cause of this phenomenon and treat it.
Important! Vomiting after eating, which takes on a systematic character, is a symptom that signals a disease of the digestive system. A mandatory examination by a gastroenterologist is necessary in order to exclude diseases of the stomach or intestines.
Characterization of vomit
An important indicator of the state of the digestive system is the characteristics of vomit, by the nature of which the doctor can already determine a preliminary diagnosis. Vomit, depending on the disease, can be:
- with streaks of fresh blood - such a clinical picture gives gastric bleeding due to rupture of a blood vessel in peptic ulcer, malignant tumor of the stomach, cirrhosis of the liver, polyps, as a complication in the treatment of hormonal drugs.
This is an acute condition that threatens the life of the patient and requires immediate hospitalization of the patient;
- Dark-colored vomit - vomiting occurs when there are problems in the assimilation of certain dark-colored foods or medications, such as activated charcoal. It occurs quite rarely. Sometimes the dark color of the vomit is a reaction to general anesthesia;
- vomit of undigested food - characteristic of food poisoning, allergic reactions to a food allergen;
- vomit mixed with bile - characteristic of cholecystitis and pancreatitis;
- natural color of gastric contents - typical for overeating, or if the gag reflex is provoked by a stressful situation.
Symptoms of vomiting
Vomiting occurs as a reflex when the body rejects food eaten:
- there is a continuous contraction of the muscular walls of the stomach, abdominal wall and diaphragm;
- food bolus under pressure moves through the esophagus into the mouth and is thrown out.

As a rule, the gag reflex is preceded by nausea, accompanied by weakness, "lightheadedness", tachycardia. But sometimes this reflex can occur spontaneously, without previous nausea, for example, during pregnancy.
Bile vomiting
In the vomit, regardless of the type and nature of vomiting, bile is necessarily present in a small amount, which has a bitter taste after the removal of gastric contents from the mouth. But if copious vomit is yellow and there is pronounced bitterness in the mouth, then in this case it will be vomiting of bile.
This symptom most often indicates gallbladder disease, ie cholecystitis or the initial manifestations of pancreatitis.
Treatment of vomiting
The gag reflex is a symptom of some disease. Therefore, in order for the digestive system of the body to work well, first of all, it is necessary to find out the cause of this unpleasant phenomenon, and why the stomach does not accept food. Only by eliminating the cause, that is, the disease, the work of the stomach will be restored.
Only by eliminating the cause, that is, the disease, the work of the stomach will be restored.
Any pathology accompanied by vomiting requires mandatory examination and treatment by a doctor. Compliance with the daily regimen and diet are an integral part of the treatment process.
Depending on the pathological process that causes the gag reflex, the following drugs are used:
- pathology of the vestibular apparatus, accompanied by nausea and vomiting when riding in public transport or pitching at sea, is stopped by taking Meterazine;
- Food poisoning, accompanied by nausea and gag reflex, is removed by the use of adsorbing drugs that bind toxins that have entered the body with poor-quality products. The most accessible and commonly used is activated carbon;
- treatment of vomiting, which is a symptom of a disease of the stomach or intestines, is carried out comprehensively and is aimed primarily at eliminating the main cause of the pathological process;
- inflammatory processes in the body, accompanied by a gag reflex, require anti-inflammatory drug treatment prescribed by a doctor;
- the rejection of food by the stomach against the background of neurotic manifestations requires treatment of neurosis, which is prescribed by a neuropathologist.