Ssdi major depressive disorder
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs.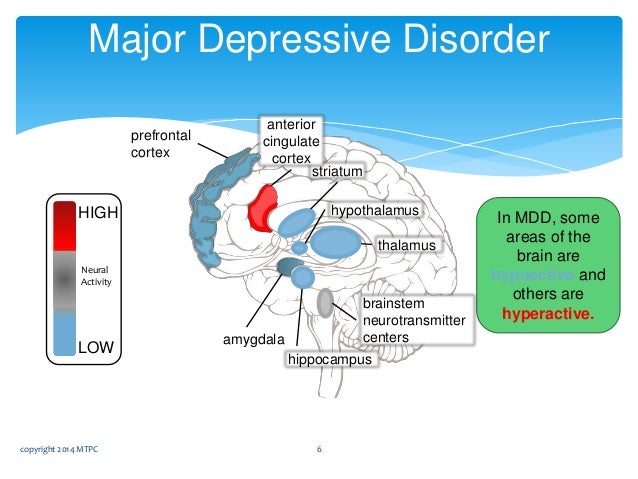 In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).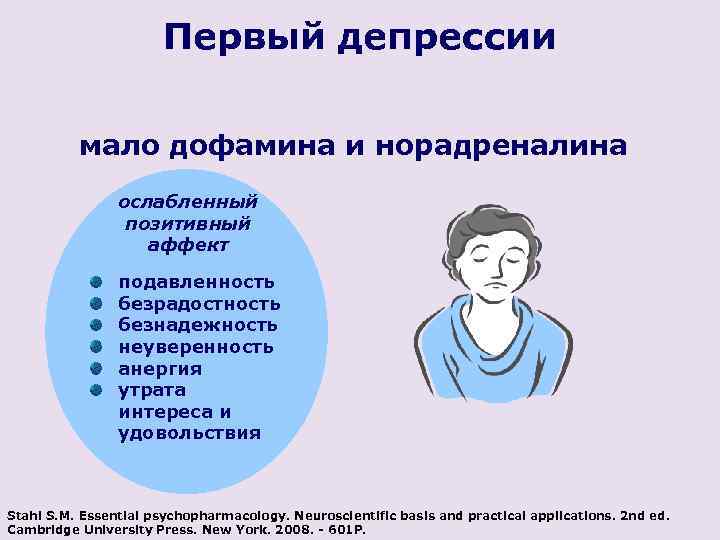
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers. The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
- Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.
 4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH) - The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk.
 They Hear You.
They Hear You. - Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
- Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses.
 The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States - The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month. The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
- Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.
 4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH) - Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 01/05/2023
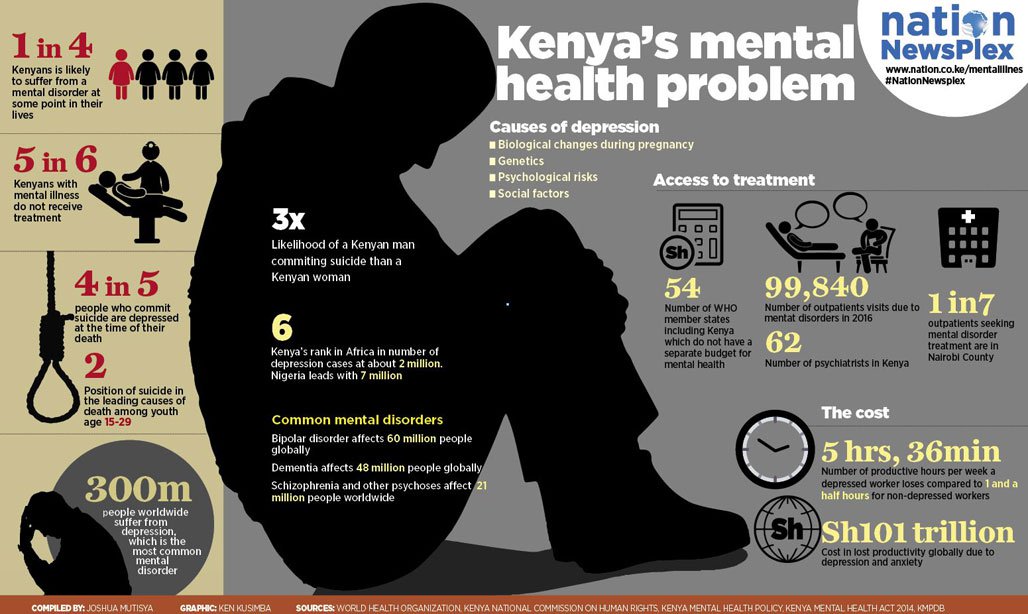
Major depressive disorders (clinical depression)
Depression is different from normal mood swings and short-term emotional responses to everyday problems. Prolonged moderate to severe depression can become a serious illness. This results in patients suffering greatly and doing poorly at work, at school and have problems in their families. At its worst, depression can lead to suicide.
Depression is a common illness worldwide, affecting more than 264 million people.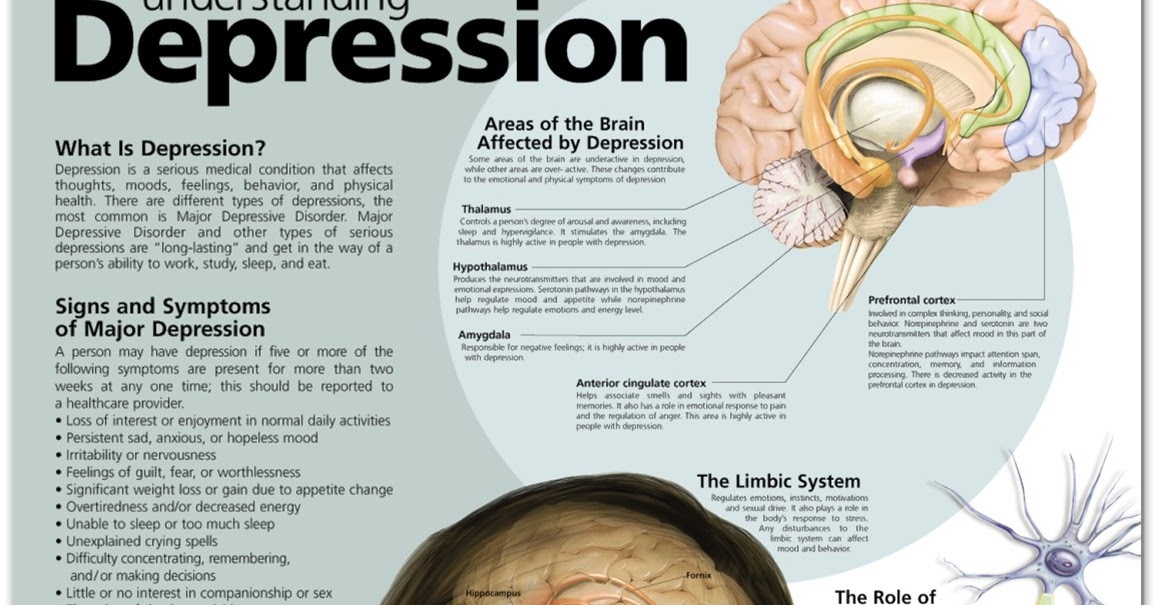 Major depressive disorder is one of the most common forms of mental illness, affecting approximately one in six men and one in four women in their lives.
Major depressive disorder is one of the most common forms of mental illness, affecting approximately one in six men and one in four women in their lives.
Major depressive disorder (MDD) is a severe condition characterized by low mood, decreased interests, poor cognitive function, and autonomic symptoms such as disturbed sleep or eating. MDD can develop in one in six adults during their lifetime and affects about twice as many women as men.
Main symptoms of depressive disorder
Symptoms of major depressive disorder (MDD) may include:
- depression almost every day
- loss of interest in activities you once enjoyed
- changes in appetite or weight
- sleep problems
- feeling lazy or restless
- low energy
- feelings of hopelessness or worthlessness
- trouble concentrating
- frequent thoughts of death or suicide
Recurrent depression:
This is a highly relapsing condition: at least 50% of people recovering from a first episode of depression have at least one additional episode in their lifetime, and about 80% of people have a history of two recurrent episodes.
Episodes typically recur within five years of the first episode, and the average person with a history of depression will have five to nine depressive episodes in their lifetime.
Symptoms of recurrent depression:
- difficulty concentrating
- disturbed sleep
- reduced energy level
- constant light alarm
Major depression in adults:
Depression is a common adult disorder that often leads to poor quality of life and impaired role functioning. Depression is also associated with high rates of suicidal behavior and death. When depression occurs in the context of a medical illness, it is associated with increased healthcare costs, longer hospital stays, poor collaboration in treatment, etc.
Causes of depression in adults may be related to the difficulty of changing roles:
- low education and low income
- early pregnancy and childbirth
- divorces
- unstable work
- highly competitive and hard work
Major symptoms of depression in adults include:
- Mostly sad or depressed mood
- Loss of interest or pleasure and avoidance of social gatherings
- Decreased energy and frequent fatigue
- Decreased concentration and attention
- Decreased self-esteem and self-confidence
- Thoughts on guilt and unworthiness
- A gloomy and pessimistic view of the future
- Thoughts or actions of harming oneself or suicidal thoughts
- Sleep disturbance or insomnia
- Pronounced or reduced appetite
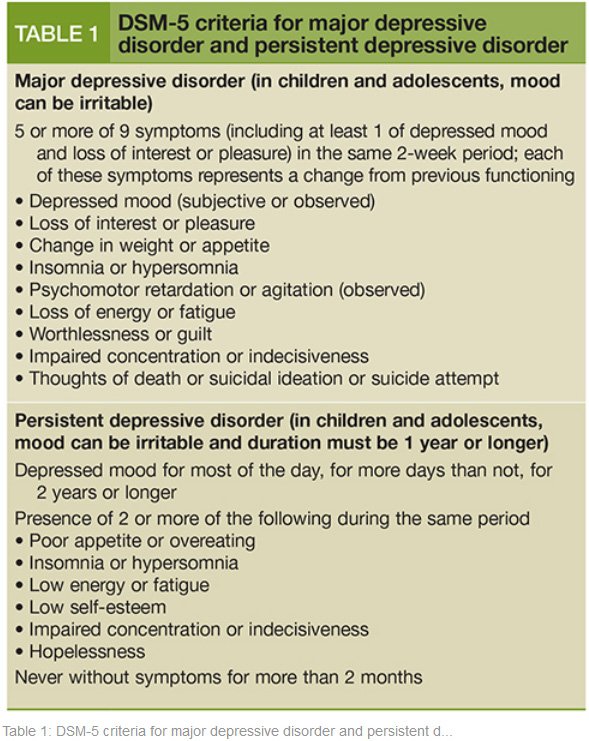
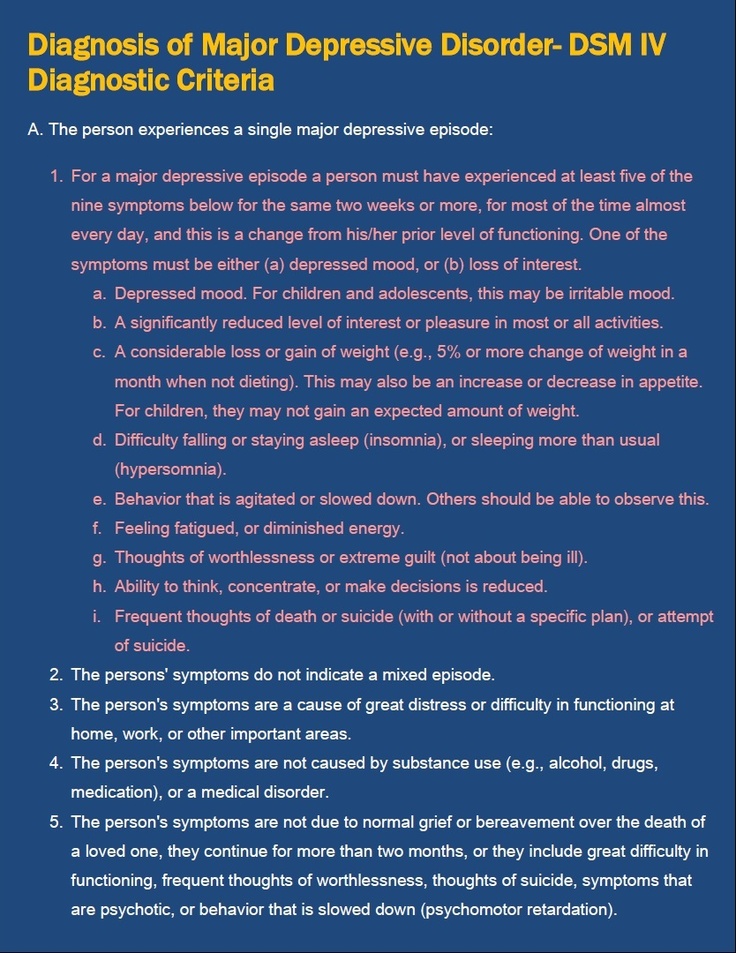
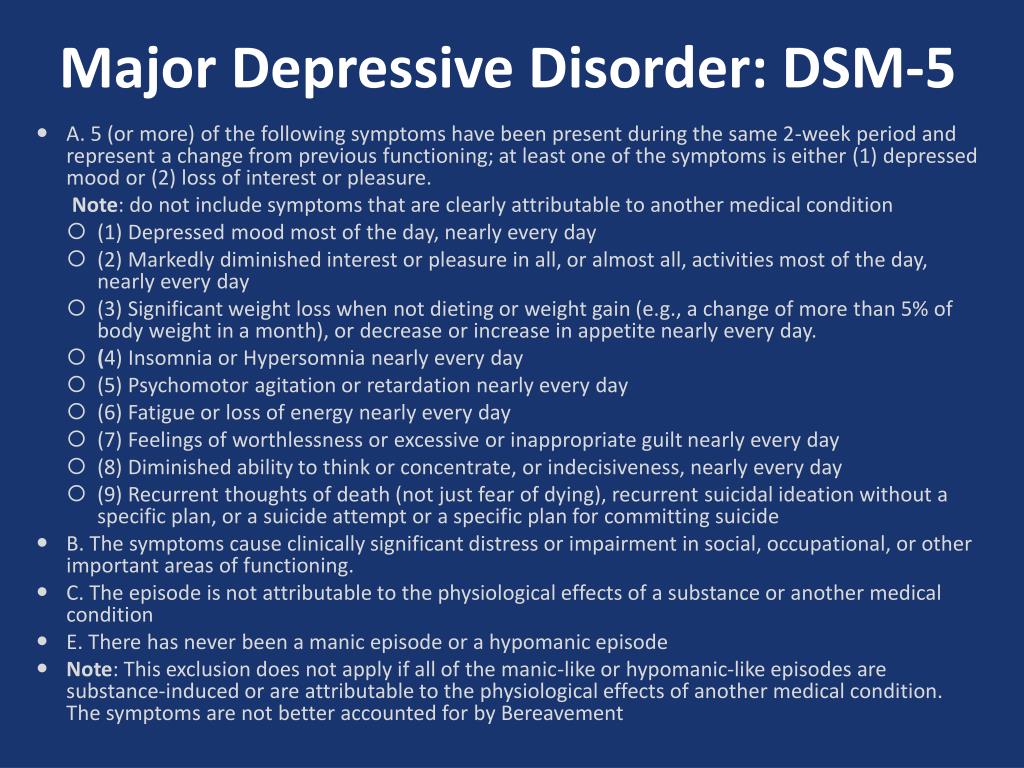
DSM-5 Criteria for Major Depressive Disorder
According to the DSM-5, the following criteria must be met for a diagnosis of major depression:
At least five of the following symptoms must have been present for at least two weeks and reflect a change in previous functionality.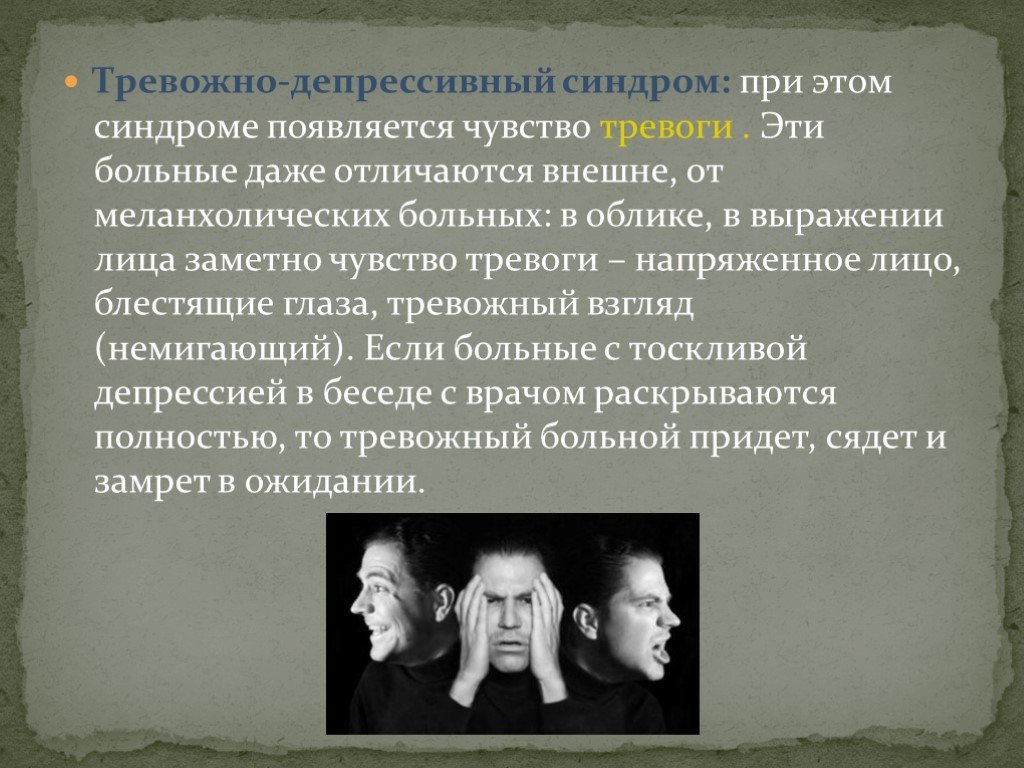 In addition, at least one of the symptoms is a low mood or loss of interest or pleasure.
In addition, at least one of the symptoms is a low mood or loss of interest or pleasure.
- The person is depressed most of the day, almost every day, as noted by himself or others.
- He or she is not interested in all or most activities most of the day, almost every day.
- Every day a person gains or loses a large amount of weight or has a decreased or increased appetite.
- Almost every day he or she suffers from insomnia or hypersomnia.
- Every day a person experiences psychomotor disturbances that are visible to others and can also be reported.
- Almost every day he or she feels exhausted or tired.
- Almost every day a person has thoughts of worthlessness or guilt.
- Every day a person's ability to think, concentrate, or make judgments deteriorates.
- He or she has recurrent suicidal thoughts, suicidal thoughts (without a definite plan), a suicide attempt, or a definite plan to commit suicide.
- Symptoms listed above cause clinical distress or interfere with daily activities.
- The episode of depression is not associated with the physiological effect of the drug or other disease.
- The onset of the episode is not better explained by specific or unspecified schizophrenia spectrum illness or other psychotic disorders.
- The person has never had a manic or hypomanic episode.
The diagnostic code for major depressive disorder is based on the frequency of recurrent episodes, the severity of the episodes, the presence of psychotic characteristics, and the state of remission. Below are the varieties of depression:
Severity of depression:
- Minor
- Moderate
- Heavy
- Psychotic
- In partial remission
- In complete remission
- Undefined
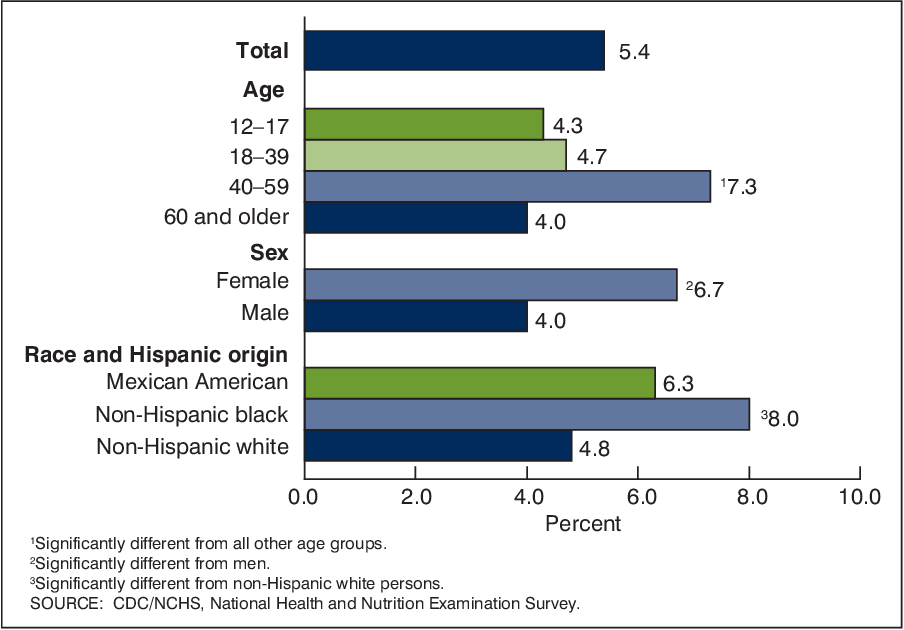
Epidemiology
Major depressive illness is a common mental illness. Its lifetime prevalence ranges from 5 to 17 percent. The incidence in women is about twice as high as in men. This is due to hormonal variations, the consequences of childbearing, different psychological pressures in men and women, and a behavioral model of learned helplessness. Although the median age of onset is around 40 years old, new studies show an increase in the incidence among younger populations due to the use of alcohol and other psychoactive substances.
The incidence in women is about twice as high as in men. This is due to hormonal variations, the consequences of childbearing, different psychological pressures in men and women, and a behavioral model of learned helplessness. Although the median age of onset is around 40 years old, new studies show an increase in the incidence among younger populations due to the use of alcohol and other psychoactive substances.
MDD is more common in divorced, separated, or bereaved individuals who do not have meaningful interpersonal interactions. There is no difference in the prevalence of MDD between races or socioeconomic status. People with MDD often have comorbidities such as substance abuse, panic disorder, social anxiety disorder, and obsessive-compulsive disorder.
The presence of these comorbidities in people with MDD increases the risk of suicide. Depression is more common in older people with underlying medical problems. Depression is more common in rural areas than in cities.
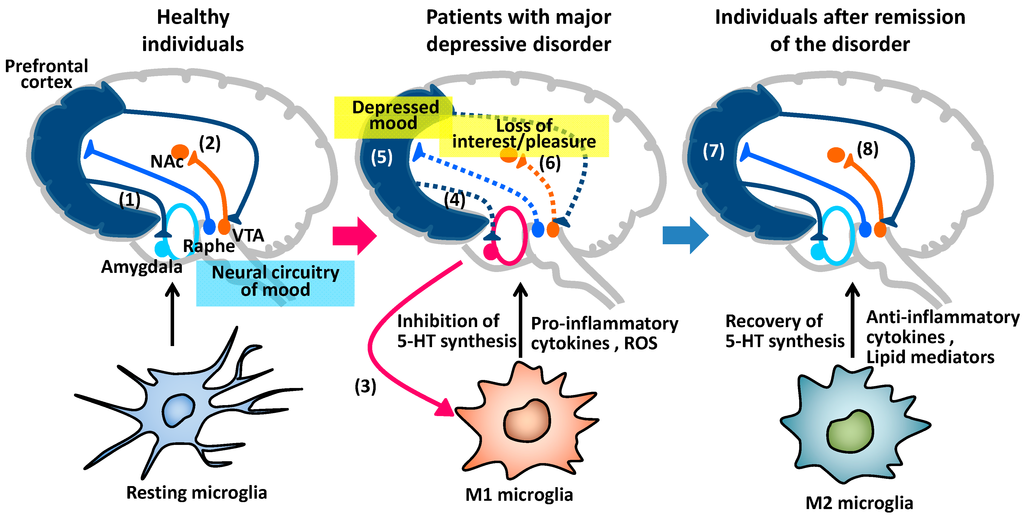
Pathophysiology of major depressive disorder
The genesis of major depressive disorder is believed to be multifaceted, with biological, genetic, environmental and psychological factors at play. It used to be thought that MDD was caused mainly by abnormalities in neurotransmitters, especially serotonin, norepinephrine, and dopamine.
This has been demonstrated by the use of several antidepressants in the treatment of depression, such as selective serotonin receptor inhibitors, serotonin-norepinephrine receptor inhibitors, and dopamine-norepinephrine receptor inhibitors. Serotonin metabolites have been found to decrease in people who have had suicidal thoughts. However, recent hypotheses suggest that this is largely due to more complex neuroregulatory systems and brain circuits, leading to subsequent disruption of the neurotransmitter systems.
GABA, an inhibitory neurotransmitter, as well as glutamate and glycine, important excitatory neurotransmitters, have been shown to play a role in the genesis of depression.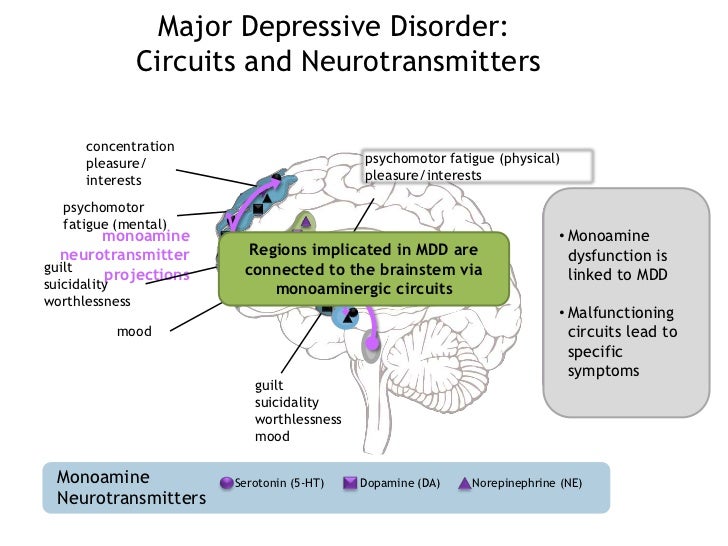 Depressed people have reduced plasma, cerebrospinal fluid, and brain levels of GABA. GABA is believed to act as an antidepressant by blocking the ascending monoamine pathways, including the mesocortical and mesolimbic systems.
Depressed people have reduced plasma, cerebrospinal fluid, and brain levels of GABA. GABA is believed to act as an antidepressant by blocking the ascending monoamine pathways, including the mesocortical and mesolimbic systems.
The antidepressant properties of drugs that oppose NMDA receptors have been investigated. Thyroid and growth hormone imbalances have also been linked to mood disorders. Numerous adversity and trauma in childhood have been linked to the development of depression later in life.
Severe early stress can cause dramatic changes in neuroendocrine and behavioral responses, leading to anatomical abnormalities in the cerebral cortex and severe depression later in life. Structural functional tomography of the brain in people with depression revealed greater hyperintensity in the subcortical regions and a decrease in the metabolism of the anterior brain regions on the left.
Family, adoption and twin studies have shown that genes play a role in the risk of depression. According to genetic studies, twins with MDD have a very high level of concordance, especially monozygotic twins. Life experience and personal qualities also have an impact.
According to genetic studies, twins with MDD have a very high level of concordance, especially monozygotic twins. Life experience and personal qualities also have an impact.
According to the theory of learned helplessness, the onset of depression is associated with the experience of uncontrollable events. Depression, according to cognitive theory, results from cognitive errors in those who are predisposed to depression.
Somatic illnesses associated with depression
Somatic sensations are especially common in depression and other mental illnesses. Although somatic symptoms are common in depressed individuals, they are of much lesser importance than major depressive symptoms in the diagnosis of depression.
The clinical stages of sad mood are characterized by both painful and non-painful bodily symptoms.
Major depressive disorder diagnosis
Major depressive disorder is a clinical diagnosis; this is mainly determined by the patient's medical history and assessment of mental status. Along with symptomatology, the clinical interview should include medical history, family history, social history, and history of drug use. Related information from the patient's family/friends is an important component of the psychiatric evaluation.
Along with symptomatology, the clinical interview should include medical history, family history, social history, and history of drug use. Related information from the patient's family/friends is an important component of the psychiatric evaluation.
Although there are no objective tests to diagnose depression, routine laboratory tests such as CBC with a differential diagnosis, a comprehensive metabolic panel, thyroid-stimulating hormone, free T4, vitamin D, urinalysis, and toxicology screening are done to rule out organic or medical diseases. causes of depression.
People with depression often see their primary care physicians for medical problems related to their depression rather than seeking a mental health professional. In nearly half of the cases, patients deny experiencing depressive symptoms and are often referred to therapy by family members or sent by employers to be tested for social isolation and decreased activity. At each visit, it is critical to assess the patient for thoughts of suicide or murder.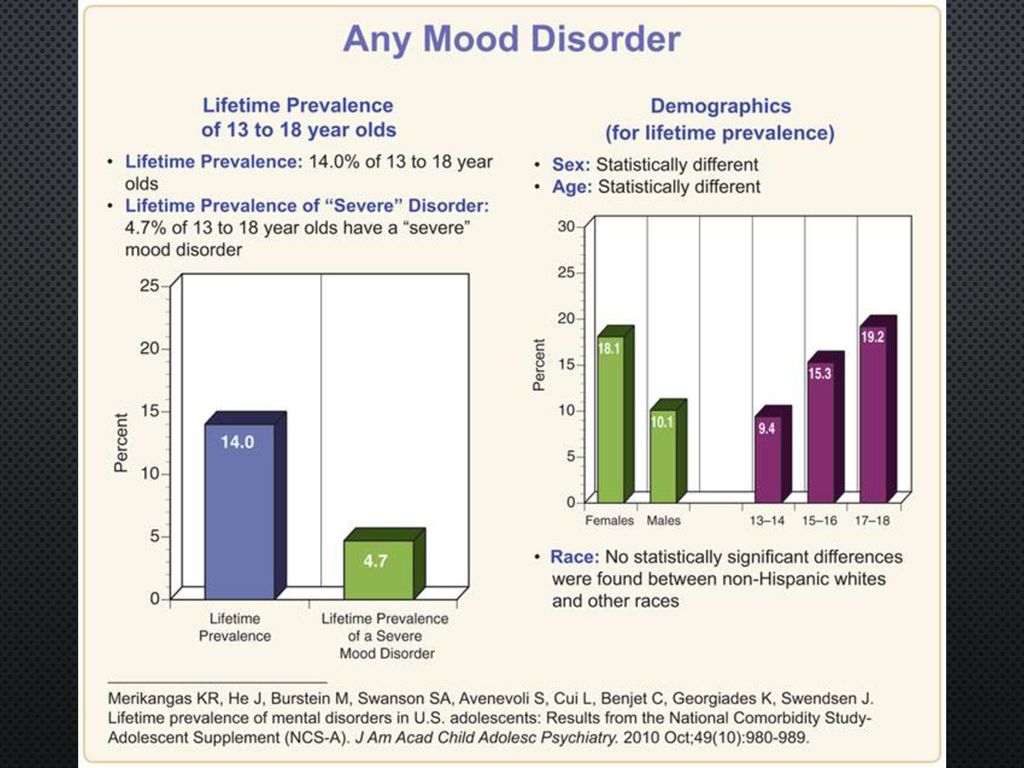
Being in a bad mood or feeling tense is common for all of us. When these feelings persist, you may suffer from depression or anxiety—or both. The self-assessment quizzes contain relevant questions to help you assess your current situation and develop a strategy to help you feel better sooner.
When you are going through a difficult moment, it is natural to feel depressed for a while; feelings like melancholy and loss help define who we are. However, if you feel sad or uncomfortable most of the time for an extended period of time, you may be suffering from depression.
Take a self-test to see if you are showing any warning signs of depression. This won't give you a diagnosis, but it will help you determine what to do next.
Major depressive disorder with psychotic features
Psychotic depression, also known as major depressive disorder with psychotic features, is a serious medical or mental illness that requires prompt treatment and constant monitoring by a physician or mental health professional.
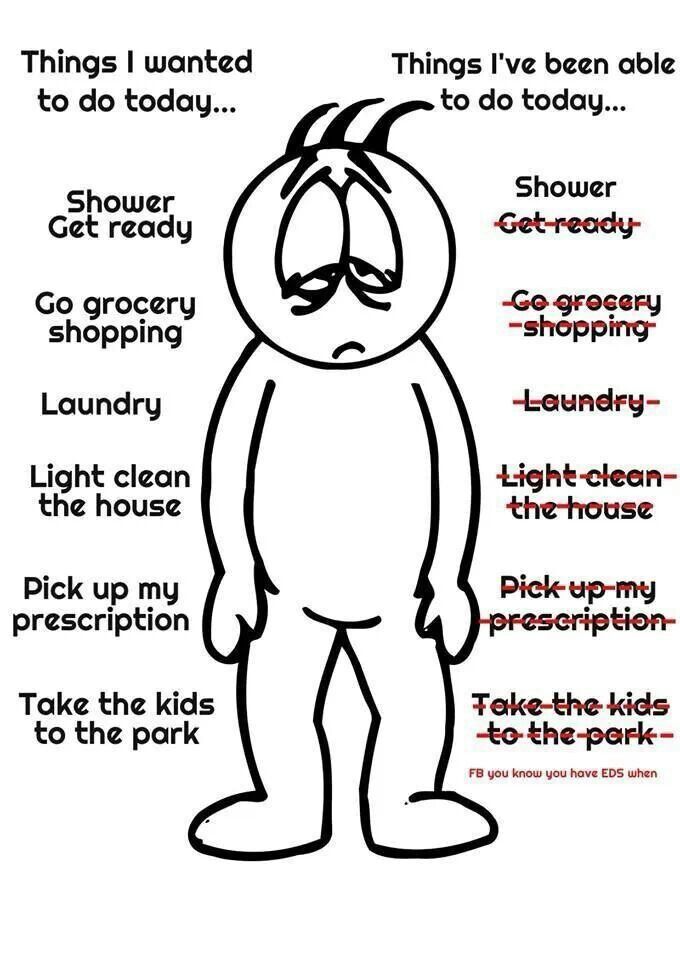
Major depression is a common mental condition that can have a detrimental effect on many aspects of a person's life. It affects mood and behavior as well as various bodily processes such as eating and sleeping. People who are severely depressed often lose interest in things they used to love and have difficulty doing daily activities. Sometimes they may even feel that life is not worth living.
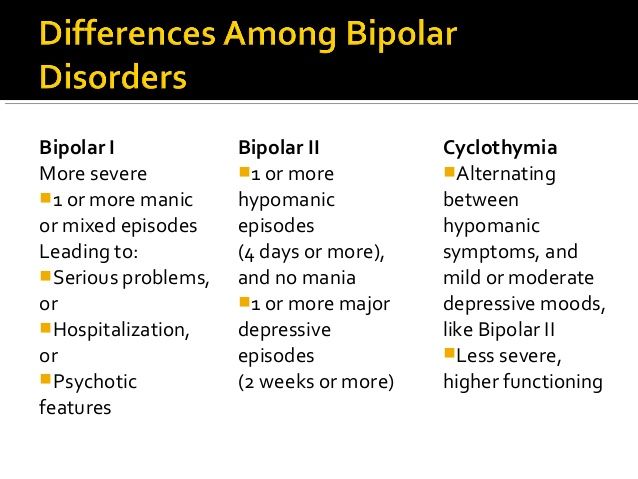
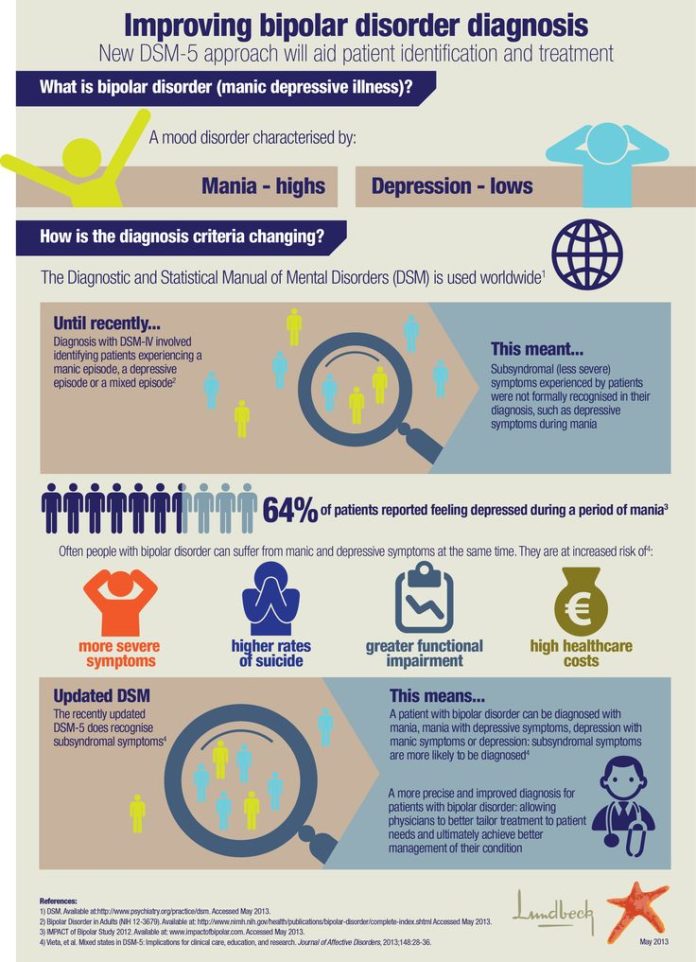
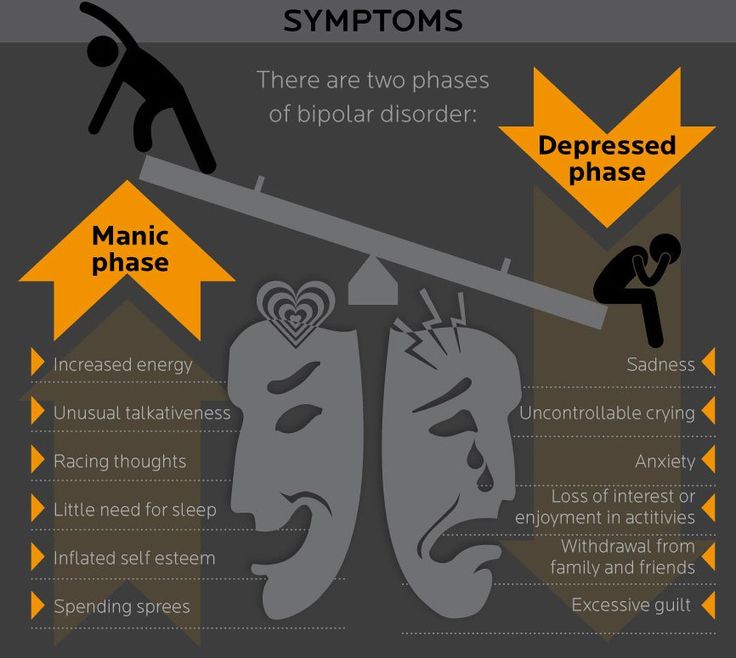
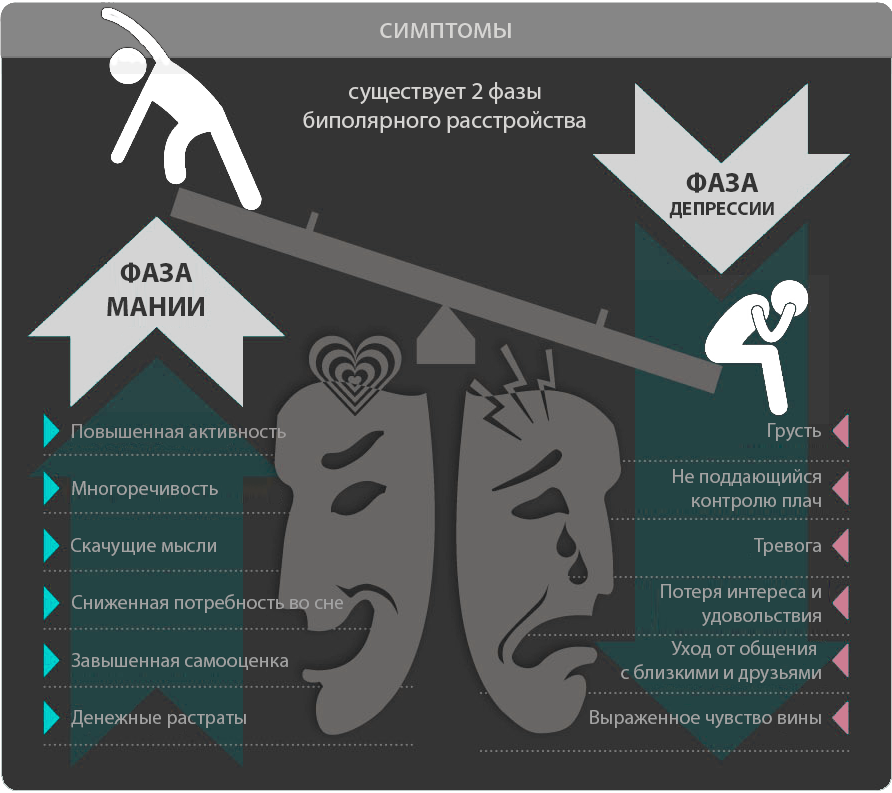
Bipolar disorder (BD)
Depression in patients with bipolar disorder (BD) is a significant clinical problem. Since schizophrenia dominates even in the treatment of BD, depression is associated not only with schizophrenia, but also with BD and comorbid medical disorders with a high risk of suicide.
Diagnosis of bipolar disorder (BD) and risk factors:
Approximately 12-17% of cases of bipolar disorder are not recognized until the mood "transforms" into hypomania or mania, either spontaneously or under the influence of substances uplifting mood.
Factors suggesting a diagnosis of BD:
- Family mania, psychosis, "nervous breakdown" or psychiatric hospitalization
- Early onset, often with depressive symptoms
- Cyclothymic mood
- Multiple relapses (eg 4 episodes of depression in 10 years)
- Depression with characteristic agitation, anger, insomnia, irritability, talkativeness.
- Other features are "mixed" or hypomanic or psychotic symptoms.
- Clinically "worsens", especially with mixed properties, during antidepressant treatment.
- Suicidal thoughts and actions
- Alcohol or drug abuse
Major depressive disorder in children and adolescents:
Major depressive disorder (MDD) can have a significant impact onset during childhood and adolescence. Associated with this are poor school performance, interpersonal problems later in life, early parenthood, and an increased risk of other psychiatric and substance use disorders.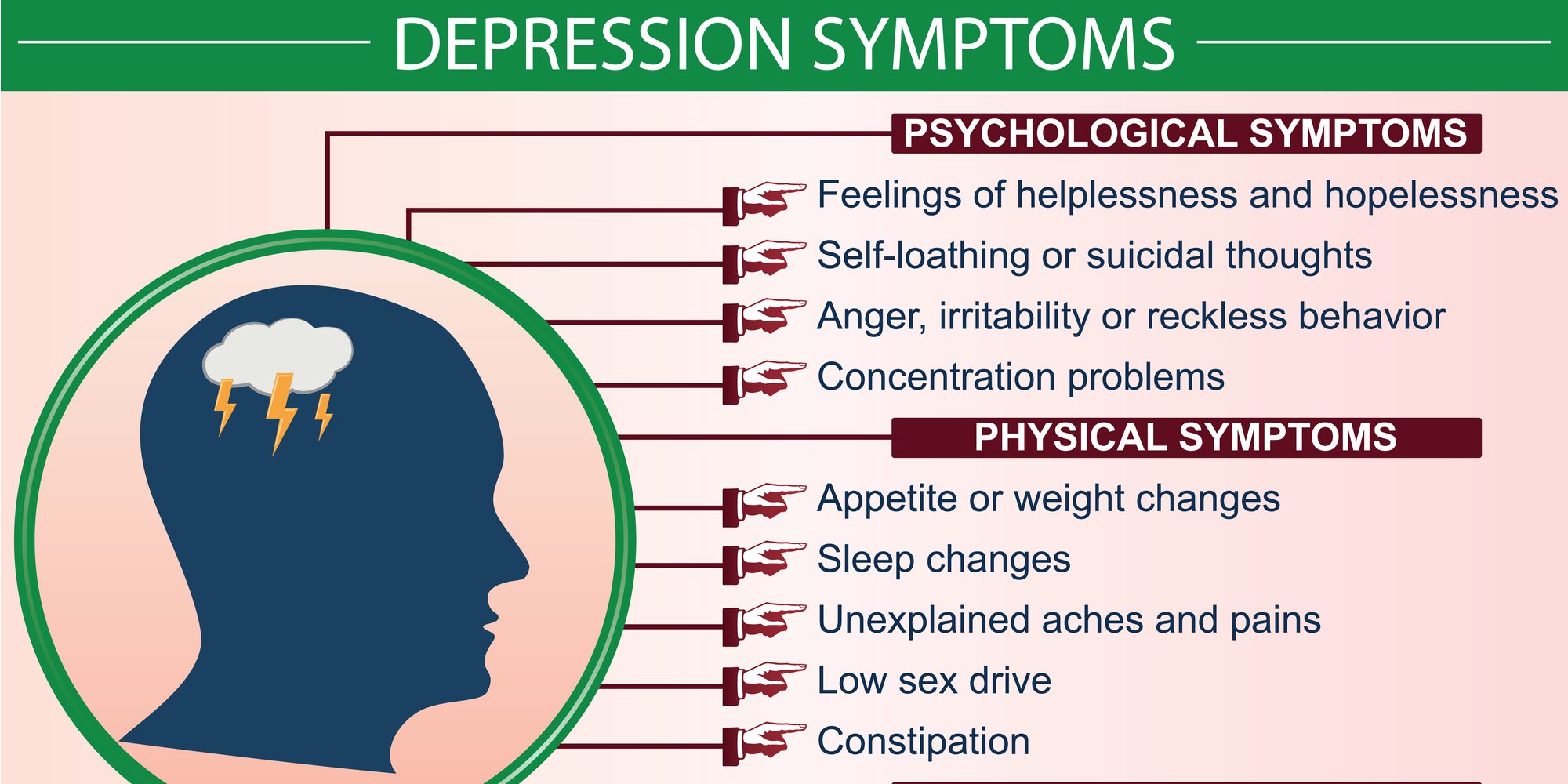 Diagnosing MDD in childhood is difficult. Children with MDD are often underdiagnosed and undertreated, and only 50% of adolescents are diagnosed before reaching adulthood.
Diagnosing MDD in childhood is difficult. Children with MDD are often underdiagnosed and undertreated, and only 50% of adolescents are diagnosed before reaching adulthood.
Symptoms of depression in children aged 3-8 years include:
- unsubstantiated claims.
- irritability
- less signs of depression
- anxiety
- behavioral changes
As the child becomes a teenager and adult, the presentation of symptoms meets the criteria for the Diagnostic and Statistical Manual of Mental Disorders (DSM-5):
- Irritability.
- Expected weight gain.
- Lethargy or inner restlessness.
- May be delusional and not limited to feelings of guilt.
Postpartum depression
Postpartum depression affects one in seven women (PPD). While most women recover quickly from childhood blues, PPD lasts much longer and has a significant impact on women's ability to return to normal activities.
PDD affects the mother and her relationship with the child. PRD impairs maternal brain response and behavior. Postpartum depression most often occurs within 6 weeks after delivery. PDD affects 6.5 to 20% of women. It is more common in teenage girls, mothers who have given birth prematurely, and women living in cities.
In one study, African American and Hispanic mothers reported onset of symptoms within 2 weeks of birth, while white mothers reported onset of symptoms later.
Premenstrual dysphoric disorder
Premenstrual symptoms are a group of psychological, behavioral and physical symptoms that cyclically occur before menstruation and subsequently resolve after menstruation in women of reproductive age. Most women experience relatively mild pain and the symptoms do not interfere with their personal, social, or professional lives; however, 5% to 8% of women experience moderate or severe symptoms that can cause significant distress and functional impairment.
All women of reproductive age, from menarche to menopause, may have premenstrual symptoms. Premenstrual symptoms are a common problem for women of reproductive age. In the United States, 70 to 90 percent of women of reproductive age report at least some premenstrual pain.
Approximately one third of these women have symptoms severe enough to warrant a diagnosis of PMS. PMDD, the most severe type of premenstrual symptom complex, occurs in 3-8% of these women.
Treatment of major depressive disorder
Treatment of major depressive disorder (MDD) in adults:
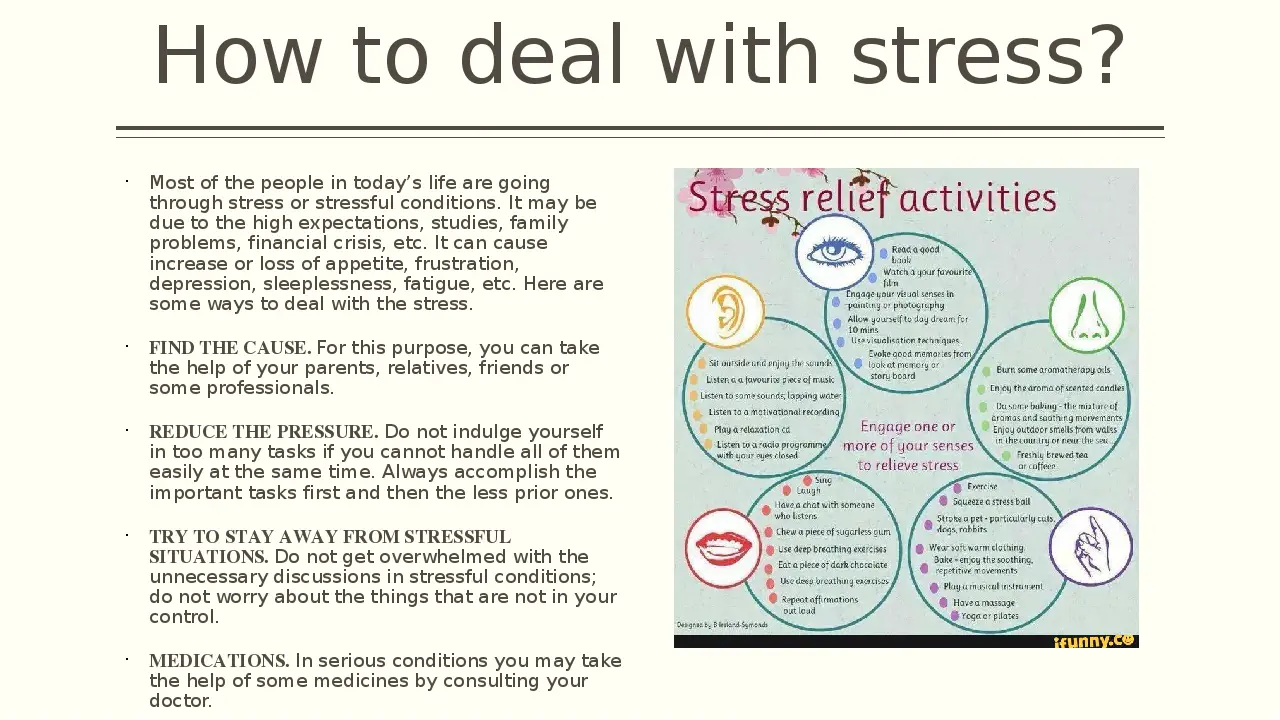
Treatment options for major depressive disorder include medication, psychological, interventional, and lifestyle changes. Medications and/or psychotherapy are used initially to treat MDD.
Combination treatment, including both drugs and psychotherapy, has been shown to be more effective than either treatment alone. Electroconvulsive therapy has been shown to be more effective than any other treatment for severe major depression.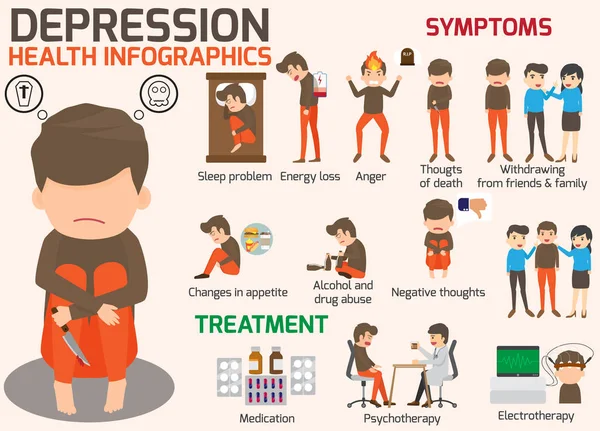
Patient psychotherapy:
Depression education and treatment can be provided to all patients. When appropriate, education may be provided to eligible family members.
Information about available treatment options will help patients make informed decisions, anticipate side effects, and follow prescribed treatment. Another important aspect of education was informing patients and concerned family members about the delayed duration of antidepressant onset of action.
Pharmacotherapy and acute treatment:
Antidepressants may be used as the primary treatment for patients with moderate or severe depression.
Clinical features that may indicate that the drug is a preferred therapeutic agent include a history of previous positive response to antidepressants, severity of symptoms, significant sleep disturbance and appetite disturbance.
Patients with severe depression with psychotic features will require antidepressant and antipsychotic and/or electroconvulsive therapy (ECT).
All antidepressants are effective, although their side effects vary. The following drugs have been approved by the FDA for the treatment of MDD:
- Fluoxetine, sertraline, citalopram, escitalopram, paroxetine, and fluvoxamine are examples of selective serotonin reuptake inhibitors (SSRIs). They are commonly used as first line therapy and are the most commonly prescribed antidepressants.
- Venlafaxine, duloxetine, desvenlafaxine, levomilnacipran and milnacipran are examples of serotonin and norepinephrine reuptake inhibitors (SNRIs). They are often used to treat depressed people who also have pain problems.
- Trazodone, vilazodone and vortioxetine are serotonin modulators.
- Bupropion and mirtazapine are examples of atypical antidepressants. When patients experience sexual side effects from SSRIs or SNRIs, they are often recommended as monotherapy or as adjunctive drugs.
- Amitriptyline, imipramine, clomipramine, doxepin, nortriptyline and desipramine are tricyclic antidepressants (TCAs).
- Tranylcypromine, phenelzine, selegiline, and isocarboxazid are examples of monoamine oxidase inhibitors (MAOIs). Due to the high prevalence of side effects and death in overdose, MAOIs and TCAs are not commonly used.
- Other drugs that can be used to improve the effectiveness of antidepressants include mood stabilizers and antipsychotics.
The role of yoga and meditation in managing depression:
Originating in ancient India, yoga is recognized as a form of alternative medicine using mind-body practice. Yoga philosophy is based on 8 elements that are best described as the ethical principles of a meaningful and purposeful life. Yoga can help with depression through the following mechanisms:
- Muscle relaxation resulting in less pain
- Creating Balanced Energy
- Decreased breathing and heart rate
- Lowering blood pressure and cortisol levels
- Increase blood flow
- Reducing stress and anxiety through tranquility
- Improve pre-existing ailments such as arthritis, cancer, mental illness and more.
Treatment of major depressive disorder (MDD) in children and adolescents
Psychotherapy is important for both patients and their families, so everyone knows about the plan and goals of treatment. When the patient receives information, the severity of symptoms decreases. Mental education may include knowledge about the signs and symptoms of depression, the clinical course of the illness, the risk of exacerbation, treatment options, and parental advice on how to interact with depressed young people.
According to research by Sandra Mullen, psychotherapy, along with medication, is often recommended for the treatment of major depressive disorder (MDD) in children and adolescents diagnosed with depression, suicidal ideation, and transient hypomania/mania.
Treatment of bipolar depression
Bipolar depression remains a clinical problem. Treatment options are limited, especially in the treatment of the acute phase of bipolar depression. There are currently only three approved drugs: OFC, quetiapine (immediate or extended release) and lurasidone (lithium monotherapy or adjuvant therapy or valproate). All three agents have similar efficacy profiles. They differ in duration.
There are currently only three approved drugs: OFC, quetiapine (immediate or extended release) and lurasidone (lithium monotherapy or adjuvant therapy or valproate). All three agents have similar efficacy profiles. They differ in duration.
Non-approved agents and treatments
Non-pharmacological drugs such as lamotrigine, antidepressants, modafinil, pramipexole, ketamine, and electroconvulsive therapy (ECT) are often prescribed for the treatment of acute bipolar depression.
Treatment of recurrent depression:
Some patients may experience recurrent episodes of depression throughout their lives unless supportive care is used to prevent relapse. Treatment should include psychotherapy and pharmacotherapy, and the dose should generally not be reduced after remission has been achieved.
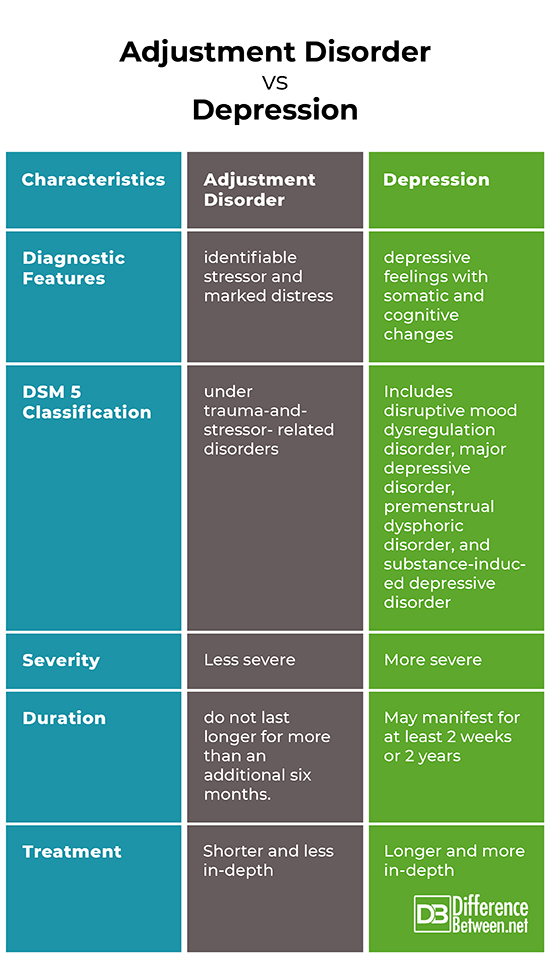
Differential
Critical to rule out depressive disorder due to another medical condition, depressive disorder due to psychoactive substances/drugs, dysthymia, cyclothymia, bereavement, adjustment disorder with depressed mood, bipolar disorder, schizoaffective disorder, schizophrenia, anxiety disorders and eating disorders when assessed for DMD. Depressive symptoms can develop as a result of the following factors:
Depressive symptoms can develop as a result of the following factors:
- Neurological causes such as cerebrovascular accident, multiple sclerosis, epilepsy, Parkinson's disease and Alzheimer's disease.
- Endocrine diseases such as diabetes, thyroid disease and adrenal disease.
- Metabolic disorders such as hypercalcemia, hyponatremia
- Drugs/substances causing dependence: steroids, antihypertensives, anticonvulsants, antibiotics, sedatives, sleeping pills, alcohol, stimulant withdrawal.
- Nutrient deficiencies such as vitamin D, B12, B6, iron or folate deficiency
- Infectious diseases such as HIV and syphilis
- Malignant neoplasms
Prognosis
Episodes of depression in untreated major depressive disorder can last 6 to 12 months. Approximately two-thirds of people with MDD think about suicide, and 10 to 15% commit suicide. MDD is a chronic relapsing disease; the recurrence rate after the first episode is about 50%, 70% after the second episode and 90% after the third episode. Approximately 5-10% of people with MDD develop bipolar disorder.
Approximately 5-10% of people with MDD develop bipolar disorder.
Patients with mild episodes, no psychotic symptoms, improved adherence, a reliable support system, and adequate premorbid functioning have a positive prognosis for MDD. In the presence of a concomitant mental disorder, personality disorder, multiple hospitalizations and advanced age, the prognosis is poor.
Complications
MDD is one of the leading causes of disability in the world. This not only causes severe functional impairment, but also negatively affects interpersonal relationships, reducing the quality of life. Individuals with MDD are at significant risk of developing comorbid anxiety and drug use disorders, which increase the risk of suicide.
Diabetes, hypertension, chronic obstructive pulmonary disease and coronary heart disease may be aggravated by depression. People who are depressed are more likely to engage in self-destructive behavior as a coping method. Left untreated, MDD can be quite debilitating.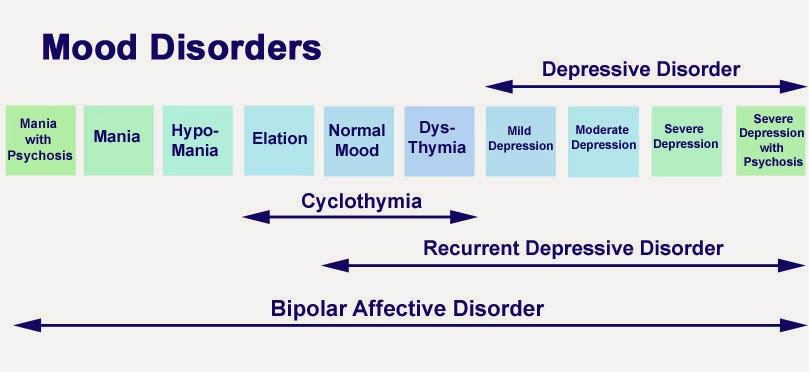
Findings
In 2008, WHO classified major depressive disorder (MDD) as the third leading cause of disease burden worldwide and is expected to be number one by 2030.
Diagnosis is made when a person has a persistently low or depressed mood, anhedonia (loss of interest in pleasure), feelings of guilt or worthlessness, lack of energy, poor concentration, changes in appetite, psychomotor retardation or agitation, trouble sleeping, or suicidal thoughts.
Effective and successful treatment of MDD requires a multidisciplinary approach. These collaborative services include primary care physicians and psychiatrists, as well as nurses, therapists, social workers and caregivers. Screening for depression in primary care settings is critical.
Kübler-Ross Model Grief counseling Emotion Divorce, others, text, logo png
Kübler-Ross model Grief counseling Emotion Divorce, others, text, logo pngtags
- text,
- others,
- anger,
- divorce,
- psychotherapist,
- grief,
- wines,
- grief Counseling,
- paper,
- line,
- emotion,
- diagram,
- death,
- severe bereavement,
- complex grief disorder,
- gap,
- brand,
- region,
- trauma center,
- png,
- transparent png,
- no background,
- free download
 99KB )
99KB ) - Image size
- 609x500px
- File size
- 103.99KB
- MIME type
- Image/png
resize PNG
width(px)
height(px)
Non-Commercial Use, DMCA Contact Us
- Black ribbon Awareness ribbon Mourning Red ribbon, ribbon, ribbon, logo png 768x768px 20.74KB
- Emoticon Computer Icons Emoji Symbol Anger, Emoji, angle, text png 768x768px 36.96KB
- Psychology Psychologist Psychotherapist, postman, text, hand png 500x500px 38.08KB
- Computer Icons Psychology Mental disorder Mind, mind, miscellaneous, text png 1749x1946px 66.29KB
- Psychologist Bottenago Polpenazze del Garda Dott.ssa Elisa Boggeri Psicologa Psicoterapeuta Sessuologa Clinica Psychology, psychology symbol, heart, head png 512x512px 33.51KB
- Psychotherapist Family therapy Relationship counseling Health Care, health, text, logo png 963x874px 24.73KB
- Emotion Feeling Graphic design Anger, true color words, emotion, feeling png 640x532px 298.1KB
- Breakup songs, Love Broken heart Breakup emotion, Breakup, miscellaneous, text png 1000x500px 156.54KB
- Clinical psychology Psychologist Counseling Psychiatrist, Counseling, miscellaneous, angle png 1200x1200px 35.62KB
- Conversations That Matter: Tools for Conversations When the Stakes Are High Conflict Resolution Author Difficult Conversations Book, book, text, author png 500x500px 213.82KB
- Light Film Yagami Near Death, others, television, angle png 1600x533px 86.45KB
- Severe anxiety Depression Hypnotherapy Fears, phobias, and rituals, Horton, love, text png 1200x1200px 118.19KB
- Syntax and semantics of Python Programming language Syntax and semantics of Python Source code, coding, blue, text png 584x436px 37.
 01KB
01KB - Anger Computer Icons, angry emoji, miscellaneous, text png 1067x1067px 30.57KB
- Frames Line art, text frame, miscellaneous, angle png 2232x2232px 96.36KB
- Paper Printing File Document Folders, stack, angle, text png 600x494px 82.79KB
- Career Portable Web Graphics Guide services Job, career, text, logo png 671x498px 57.07KB
- Medicine Health Care Physician General medical examination, health, blue, text png 2133x2129px 103.91KB
- National Day of Mourning Death Condolence Black ribbon, others, miscellaneous, ribbon png 3900x3000px 545.
 13KB
13KB - Computer Icons Drawing, contact, miscellaneous, angle png 600x564px 21.98KB
- Counseling psychology Personality psychology, others, text, logo png 512x512px 15.74KB
- Master of Social Work Group psychotherapy, Pride Community Center, text, hand png 960x701px 144.42KB
- Deezer Logo Spotify Music, spotify logo, text, rectangle png 1068x601px 73.21KB
- Fear Anxiety Phobia Panic Anxiety, others, love, miscellaneous png 640x640px 93.19KB
- Kiss of Death Animation Studio Anime Trigger, Anime, television, blue png 1920x1080px 158.
 54KB
54KB - Pakistan Institute of Management Consulting Psychology Student Career Counseling Psychotherapist, student, blue, text png 580x435px 144.23KB
- Sadness Depression Feeling Love, Depression, love, miscellaneous png 1200x1200px 28.69KB
- checklist illustration, Computer Icons Checklist Iconfinder, Check, Checklist, Document, Form, List, Report, Test Icon | Icon, miscellaneous, angle png 512x512px 27.82KB
- Enneagram Enneagram of personality Personality type Psychology Psyche, ali logo, angle, text png 1585x1568px 234.89KB
- Biological life cycle Birth Death, Human Life, text, public Relations png 600x572px 176.
 99KB
99KB - Malang State University Yogyakarta State University graphs State university, Monash University logo, cdr, text png 798x398px 69.34KB
- Broken heart Love Romance Drawing, heart, love, angle png 980x852px 76.64KB
- multicolored texts, Infographic Organizational chart, Business information exploded chart, business Woman, text png 1524x1680px 186.91KB
- Counseling psychology Individual anger management Relationship counseling Grief, depression, miscellaneous, text png 1200x1200px 28.88KB
- Cognitive psychology Computer Icons Psychotherapist Personality, psychology, miscellaneous, blue png 1600x1600px 22.
 24KB
24KB - Treatment-resistant depression Major depressive disorder Sadness Mixed anxiety-depressive disorder, hay, text, logo png 858x647px 570.68KB
- Centers for Disease Control and Prevention Logo Brand CDC Font, FAMILY LOGO, blue, angle png 600x500px 218.46KB
- zumba text, Zumba Dance Fitness Center, losing, miscellaneous, purple png 600x600px 51.59KB
- English 英会話 Counseling Logo, Counseling, blue, text png 507x507px 55.08KB
- Genetics Genetic carrier Genetic disorder X-linked recessive inheritance, Heartbeat, text, logo png 752x1098px 33.
 8KB
8KB - Harry Potter and the Deathly Hallows Hermione Granger Symbol Decal, Harry Potter, angle, text png 600x501px 54.36KB
- Parental Advisory Parental Music Resource Center Poster, products album cover, miscellaneous, text png 800x800px 9.95KB
- Mountain logo, Foothills Bowling Center The mountains are calling and I must go. mountains, angle, text png 749x535px 36.52KB
- Quotation Text Font, quotation, love, angle png 800x340px 46.65KB
- Paper Learning Documentation Book Manuscript, stack of papers, angle, text png 640x490px 191.