Pandas syndrome rage
PANDAS Symptoms Checklist - PANDAS Network
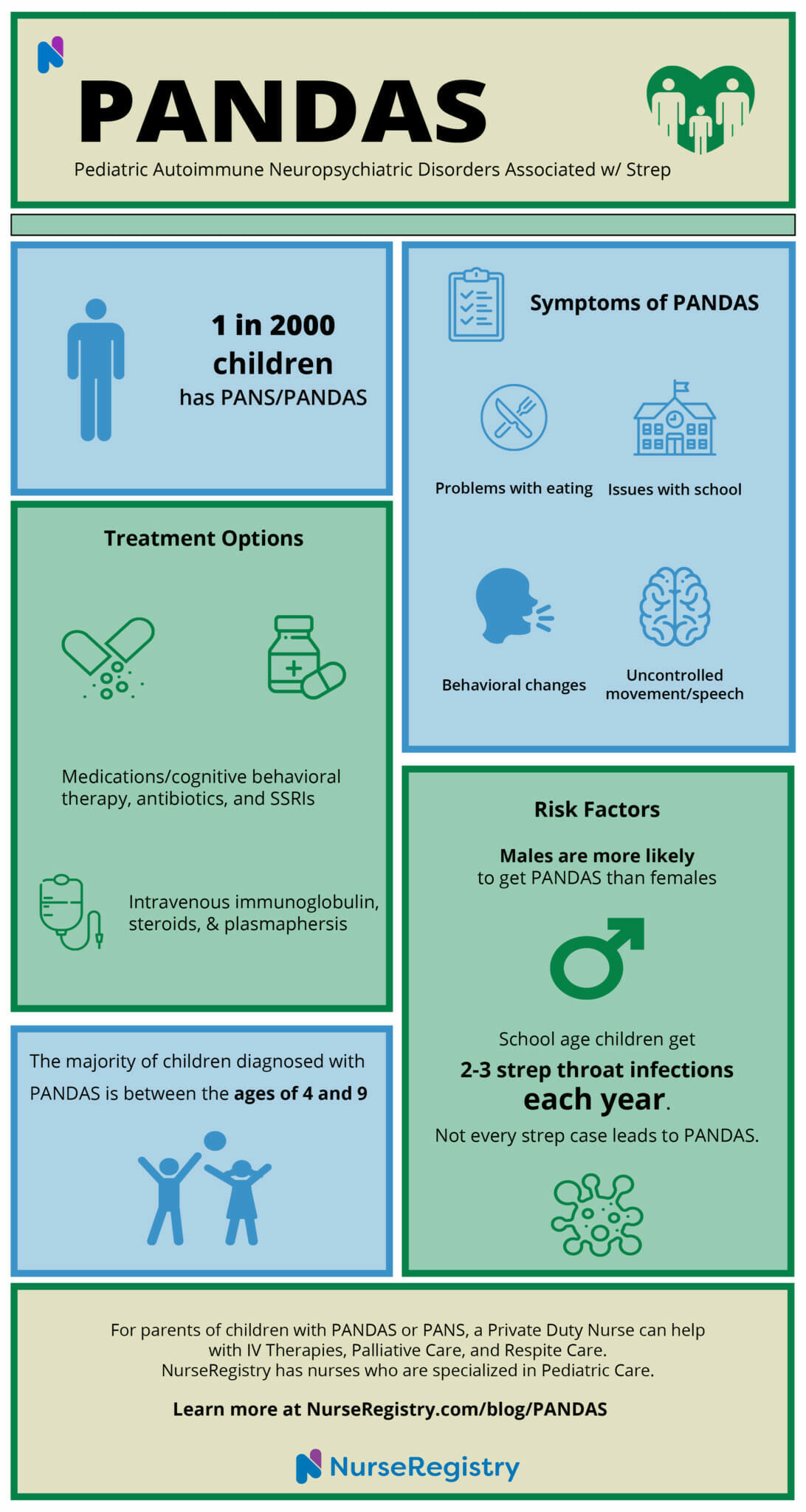
Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS) present as neurological, mental and physical disturbances following infection with streptococcal-A, commonly known as strep throat. It is believed that PANDAS is an autoimmune disorder, and the strep bacteria causes the immune system to attack healthy cells in the brain. A PANDAS diagnosis is based on the collection of symptoms, test results (such as a throat culture or blood test) and your child’s medical history. There is currently no definitive test for PANDAS, but identifying PANDAS symptoms and signs can help confirm a diagnosis.
PANDAS Symptoms ChecklistPANDAS causes a sudden onset of behavioral and neurological problems after a strep infection. Your child may exhibit other symptoms in addition to these, but the following are the most common among children with confirmed diagnoses:
- Sudden onset of OCD-like symptoms.
- Irritability or aggression.
- Depression or extreme moodiness.
- Poor motor coordination.
- Tics or unusual movements.
- Sensitivity to light, sound or touch.
- Visual hallucinations.
- Sleep disturbances or fatigue.
Clinical diagnostic criteria for PANDAS/PANS are specific and consist of the following:
- The sudden, dramatic onset of obsessive-compulsive disorder or extremely restricted food intake.
- The simultaneous appearance of additional neuropsychiatric symptoms with acute, severe onset from at least two of the following seven categories:
- Aggression, irritability or oppositional behaviors.
- Anxiety.
- A decline in school performance.
- Motor or sensory abnormalities.
- Emotional lability or depression.
- Behavioral (developmental) regression.
- Somatic symptoms, such as enuresis, sleep disturbances or increased urinary frequency.

- These symptoms are not better explained by another known medical condition or neurological disorder, such as Tourette disorder, Sydenham’s chorea or systemic lupus erythematosus.
If these symptoms sound familiar, and your child has had strep throat or recurring strep infections, it’s imperative to discuss this with your doctor. Left untreated, PANDAS symptoms often become more severe over time. There are several scales that are used to identify symptom severity for PANS and PANDAS. These include scales for neuropsychiatric symptoms, ratings for the severity of OCD symptoms and tics and a scale to evaluate caregiver burden (how much assistance your child needs to function). In addition to this checklist, these scales can help you present your child’s symptoms to their healthcare provider. You can find them here.
What Are Common Symptoms of PANDAS/PANS?Signs of PANDAS are unique to each person, but the defining feature of PANDAS is the acute onset of disabling anxiety and mood lability with tics or obsessive-compulsive-like behavior. In PANDAS, symptoms come on abruptly (flare) and remit. This may come in cycles and include mental health disturbances, physical symptoms and behavioral issues. Keep in mind that while these symptoms generally appear right after a strep infection, some children experience symptoms four to six months later if their antibiotic treatment did not fully destroy the bacteria.
In PANDAS, symptoms come on abruptly (flare) and remit. This may come in cycles and include mental health disturbances, physical symptoms and behavioral issues. Keep in mind that while these symptoms generally appear right after a strep infection, some children experience symptoms four to six months later if their antibiotic treatment did not fully destroy the bacteria.
The symptoms for PANS (pediatric acute-onset neuropsychiatric syndrome) are extremely similar to PANDAS, but PANS is associated with other infections, such as Lyme disease, influenza or the common cold, while PANDAS is only associated with strep. Criteria for diagnosing PANDAS is similar to PANS and include the abrupt, pre-pubertal onset of obsessions, compulsions or tics. But for PANDAS, these must be associated with streptococcal infection and other neuropsychiatric symptoms. Some common symptoms include:
Behavioral problemsMost children with PANDAS will exhibit sudden anger, irritability, episodes of extreme rage, screaming or violent behavior.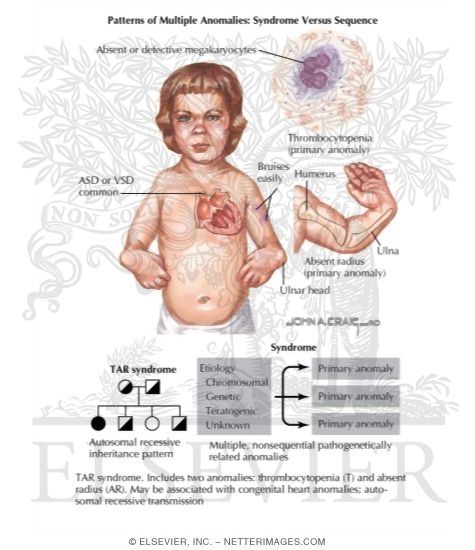 These episodes can be severe and last up to an hour in some cases.
These episodes can be severe and last up to an hour in some cases.
Obsessive-compulsive symptoms are different for everyone. Some common ones include:
- Contamination. Your child may fear germs or repeatedly wash their hands.
- Worry for self or others. They may worry that something they do will harm others or that someone or something is going to hurt them or their family.
- Doubting. A need for constant reassurance, or an inability to make decisions.
- Hoarding. Inability to get rid of objects that have no use.
- Number and color obsessions. Fixation on a certain number or color.
- Morality. They experience guilt and worry about being “bad.”
- Symmetry urges. The need to put items in order by color or number.
Motor tics are repetitive sounds and movements that are hard to control. They can appear as a series—performed in order—and provide relief for anxiety or discomfort. Your child may also grunt, cough, hum or repeat words. Additionally, they may experience facial grimacing, jerk their head, twitch their nose or repeatedly blink their eyes.
They can appear as a series—performed in order—and provide relief for anxiety or discomfort. Your child may also grunt, cough, hum or repeat words. Additionally, they may experience facial grimacing, jerk their head, twitch their nose or repeatedly blink their eyes.
These can come in waves and cause intense emotional instability.
Academic skill regressionYour child may have symptoms similar to ADHD that impact their academic performance, such as hyperactivity, inability to sustain attention and poor impulse control. PANDAS can also cause brain fog, a decline in math skills and changes in handwriting.
Extreme rage or emotional labilityEmotional lability is a neurological symptom that reduces an individual’s ability to control their emotional responses. Emotional lability can lead to uncontrollable laughing or crying. Extreme rage is another symptom that leads to violent behavior, uncontrollable screaming, throwing items and breaking objects.
Your child may experience sensory sensitivity, hallucinations or react negatively to loud noises and light.
Sleep issuesPANDAS can cause difficulty sleeping, oversleeping and excessive fatigue. Your child may also develop a problem with bedwetting or night terrors.
Restrictive eatingThis symptom can present as either refusing food or selective eating. Restrictive eating can be due to sensory sensitivities, fear of vomiting, fear of contamination or difficulty swallowing. Restrictive eating can lead to malnutrition. Contact your doctor immediately if your child experiences significant weight loss.
Poor coordinationYour child may lose balance, have an unusual gait or have difficulty walking.
PANDAS is evaluated on a case-by-case basis and can be mild, moderate or severe. Your provider can help assess your child’s case by determining how much the symptoms interfere with daily life and inhibit your child from engaging in regular activities.
Parents often want to know if their child can outgrow PANDAS. Researchers are currently studying this, as PANDAS is a relatively new disease, and it can be difficult even to diagnose the illness. Currently, we do not have long-term data on this newly identified illness, but there is some evidence that points to puberty helping reduce symptoms of PANDAS—though it is not proven at this time. That’s why it is absolutely critical that parents of children with PANDAS or PANS remain vigilant in protecting their children from contracting strep, as the best cure is prevention in the case of this disease. Additionally, PANDAS/PANS parents need to seek prompt treatment if their child does contract strep to minimize the likelihood of developing PANDAS/PANS or worsening existing symptoms.
Are There PANDAS Symptoms in Adults?While it may be possible for an adult to develop PANDAS, there hasn’t been much research done in this area.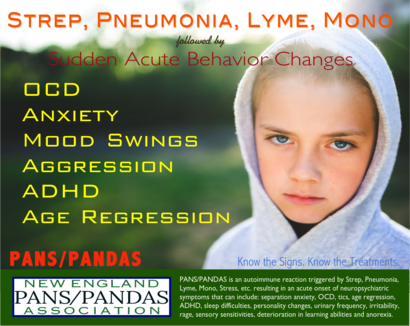 Currently, it is understood that PANDAS is a pediatric disease and symptoms seem to disappear in adulthood. It is not believed that a person would present with PANDAS symptoms later in life. As we continue to do more research on PANS and PANDAS, we will find out more about how it affects different age groups.
Currently, it is understood that PANDAS is a pediatric disease and symptoms seem to disappear in adulthood. It is not believed that a person would present with PANDAS symptoms later in life. As we continue to do more research on PANS and PANDAS, we will find out more about how it affects different age groups.
If you’re looking for additional resources and community support, join the PANDAS Network support group as a family or treating professional member.
Complete Guide to PANS and PANDAS
PANS and PANDAS are severe forms of obsessive-compulsive disorder (OCD) that appear suddenly (acute onset) in young children, accompanied by other confusing and distressing symptoms. This guide explains how to recognize PANS and PANDAS, how they’re diagnosed, and what the recommended treatments are.
What Is Acute Onset OCD?
For most children with OCD, symptoms come on gradually. At first a child is often able to hide both his fears and the rituals he develops to calm them. Eventually the fears become too overwhelming, and the rituals too time consuming, to conceal from parents.
Eventually the fears become too overwhelming, and the rituals too time consuming, to conceal from parents.
But there is another kind of OCD in which full-blown symptoms come on virtually overnight. This happens to some young children after they’ve had an infection, usually strep. It’s thought to be the result of the child’s immune system erroneously attacking brain cells. It may be accompanied by other symptoms, including restricted eating, anger, and depression.
“Parents, with great reluctance, talk about their child being possessed, either by a demon or by aliens,” says Dr. Susan Swedo, a pediatrician who has been studying the syndrome for decades.
What Are PANS and PANDAS?
PANS and PANDAS are conditions that a child can develop following an infection, usually strep. They are diagnosed if a child has sudden, severe OCD and other disturbing symptoms.
PANS (pediatric acute-onset neuropsychiatric syndrome) is a more general term that does not specify the type of infection thought to trigger the symptoms. It’s called “acute onset” because the behavior changes come on suddenly, reaching full-scale intensity within 24 to 48 hours. It’s a syndrome because there are quite a few other symptoms that appear alongside the intense anxiety.
It’s called “acute onset” because the behavior changes come on suddenly, reaching full-scale intensity within 24 to 48 hours. It’s a syndrome because there are quite a few other symptoms that appear alongside the intense anxiety.
PANDAS (pediatric autoimmune neuropsychiatric disorder associated with streptococcal infections) is a more specific term used when the triggering infection is strep. PANDAS is a subgroup of PANS. Some 86 percent of acute onset OCD cases are linked to strep.
Children especially at risk are those who have what doctors call “occult” or hidden strep infections — that is, children who can be “carriers” of the infection but don’t get symptoms themselves, and hence don’t get treatment.
PANS cases have also been linked to other infections, including Lyme disease, mononucleosis, mycoplasma (walking pneumonia) and the flu (such as h2N1).
PANS and PANDAS are episodic disorders. Symptoms may disappear for extended periods then reappear, stimulated by a later exposure to strep of some other bacteria or virus.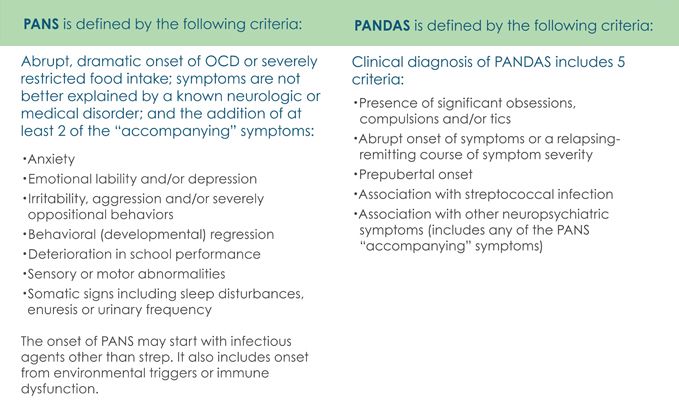 Symptoms may get increasingly severe with multiple recurrences.
Symptoms may get increasingly severe with multiple recurrences.
Symptoms of PANS and PANDAS include:
- Acute-onset OCD
- Severe separation anxiety
- Handwriting suddenly becomes unrecognizable
- Drawings look like scribbles
- Has trouble eating
- Starts wetting the bed
- Can’t manage the math or reading he could do effortlessly the previous week
- Irritable
- Emotionally erratic
- Panic attacks
- Suicidal thoughts
Controversy Over Causes
While this syndrome has been recognized for decades, the link between the symptoms and an infection has been the subject of intense controversy, with some researchers and clinicians claiming insufficient evidence, and denying children treatment to fight the sometimes elusive infection.
But the medical community has coalesced around a clearer description of the symptoms, their causes, and how they should be treated. This should make it easier for parents to get care for severely affected children.
This should make it easier for parents to get care for severely affected children.
Dr. Swedo, who headed the pediatrics and developmental neuroscience branch of the National Institutes of Mental Health until she retired in 2019, first identified PANDAS in 1998, and has been in the vanguard of research and advocacy ever since. The larger category, PANS, was added in 2010 to account for cases that could not be linked definitively to strep infections.
There is now broad acceptance that PANDAS is, like rheumatic fever, a misdirected immune response to the strep bacteria, which mimics human heart or brain tissue. The immune system attacks the heart (in the case of rheumatic faver) or brain (in the case of PANDAS), causing this array of mental health symptoms.
What Does PANS Look Like in Children?
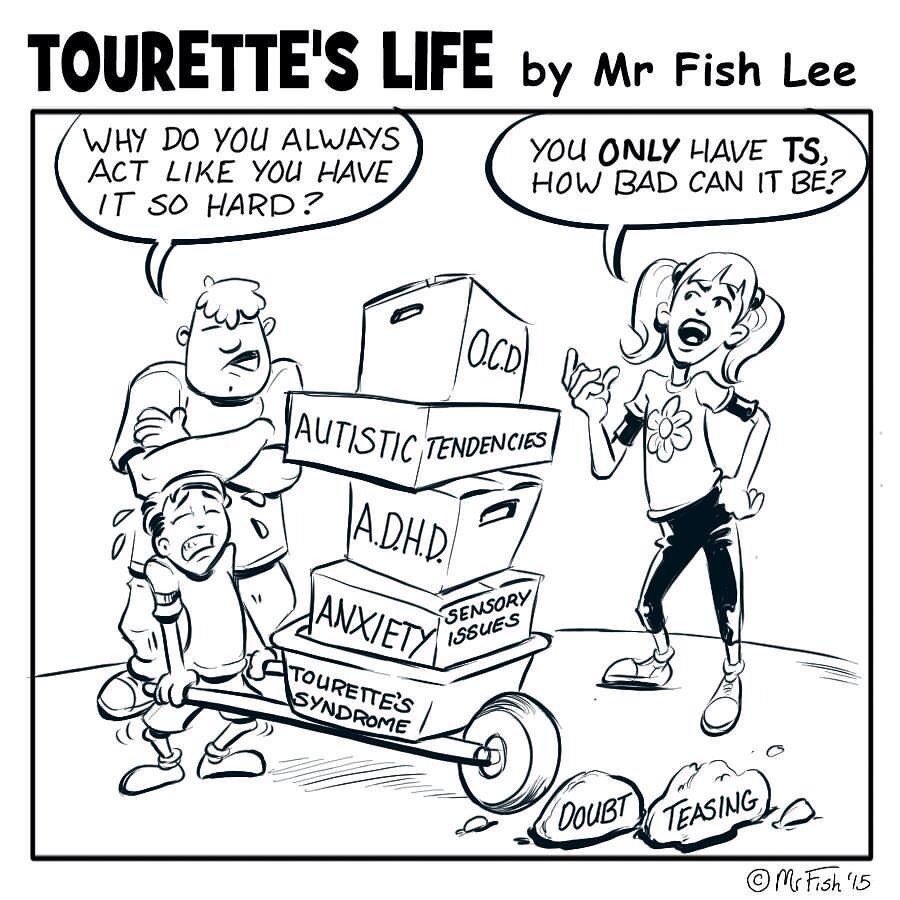
“What this is not is garden variety OCD, Tourette’s, ADHD, conduct disorder — anything else,” explains Dr. Swedo. “We’re talking about a six-year-old, seven-year-old, maybe as young as three or four, who undergoes an acute behavioral change, a very, very dramatic onset. ”
”
Acute onset OCD might take the form of a child suddenly asking for constant reassurance, or engaging in endless handwashing. Many children with PANS become obsessive about food, severely restricting what they will eat because of acute fears of contamination, choking or vomiting. This can develop into anorexia, and can result in extreme weight loss, necessitating hospitalization and the use of a feeding tube.
Separation anxiety can also appear suddenly, sometimes so overwhelming that a 10-year-old, or even a 14-year-old suddenly has to start sleeping with their mother. And panic attacks are common. “In those first few days, the child is in state of near-constant panic,” Dr. Swedo adds. “These changes are not subtle.”
Criteria for a PANS Diagnosis
All children with the disorder have acute onset of OCD symptoms or eating restrictions. But they also have a debilitating and baffling set of other neurological symptoms with similarly sudden onset.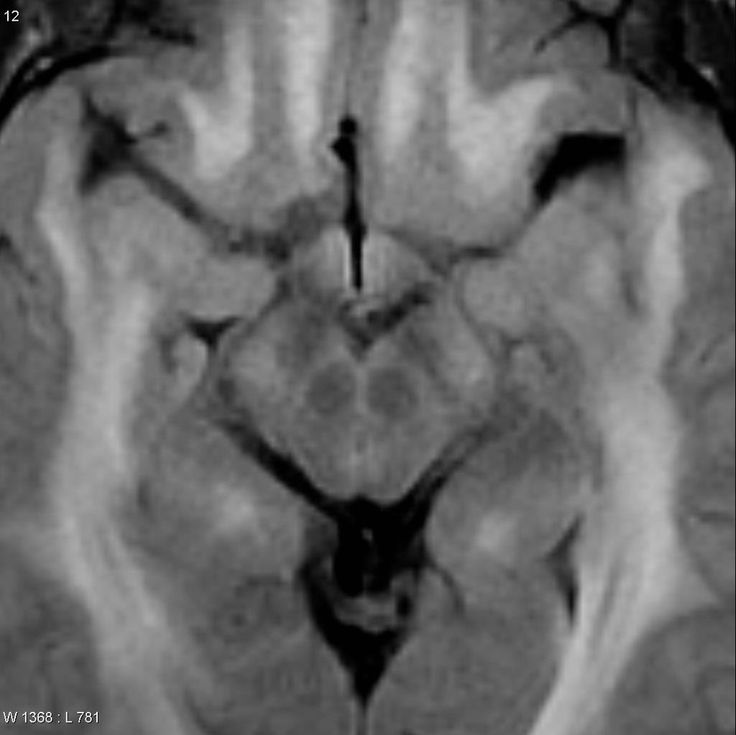 To be diagnosed with PANS they must have two of the following seven criteria:
To be diagnosed with PANS they must have two of the following seven criteria:
- Separation anxiety, panic, other forms of anxiety
- Behavioral regression: Kids suddenly acting much younger than they should for their age, such as reverting to baby talk.
- Emotional lability: These children can be severely depressed, even suicidal
- Irritability, aggression and /or severely oppositional behaviors
- Deterioration in school performance: Sudden decline in math and reading competence, memory and concentration; increase in hyperactivity
- Motor or sensory abnormalities: Their handwriting and drawing deteriorates dramatically (also linked to regression), and they may be distressed by noise or light
- Somatic symptoms: These include sleep disturbances, betwetting and other changes in urinary frequency or intensity
If You Think Your Child Might Have PANS
Parents’ first stop when they experience such a dramatic behavior change is usually the pediatrician, or in extreme cases, the emergency room, Dr. Swedo notes. She recommends that you refrain from insisting to the doctor that your child has PANS, and bringing along articles on the disorder as backup, since medical professionals tend to be skeptical of a parental rush to diagnosis.
Swedo notes. She recommends that you refrain from insisting to the doctor that your child has PANS, and bringing along articles on the disorder as backup, since medical professionals tend to be skeptical of a parental rush to diagnosis.
The best way to present this, she says, is: “I’m really worried about my child’s brain. There’s been an abrupt change in his behavior. This is what I’ve seen at home. It’s completely out of character.” The goal, as she puts it, is to partner with the doctor in terms of let’s figure it out together. PANS is one possible explanation for the sudden changes in behavior, but your physician will want to consider others as well.
In the past, pediatricians and other doctors have often dismissed families describing acute-onset OCD, Dr. Swedo said, assuming that parents must have missed earlier, less severe symptoms. But PANS and PANDAS should now be much more widely recognized.
It’s also good to check with your child’s teacher or school to see if strep has been going around. A child doesn’t have to have symptoms of strep to have an infection—some kids never get symptomatic.
A child doesn’t have to have symptoms of strep to have an infection—some kids never get symptomatic.
What Should You Expect Your Doctor to Do?
If a child has urinary symptoms, Dr. Swedo recommends urinalysis and urine culture. She recommends a throat culture to look for strep, and an exam to see if an occult, or hidden, strep infection is observable.
If the rapid strep test is positive, she recommends a three-week course of antibiotics, to aggressively treat a possible sinus infection. Sinusitis is the trigger of symptoms for many kids, she says.
And Dr. Swedo also recommends that the pediatrician schedule a follow-up visit for three days later, to check in with the family. “The family stress is through the roof with this syndrome — by some measures higher than kids who’ve been diagnosed with leukemia,” she notes. “So a physician treating the medical causes should also make a referral, immediately, to a psychologist or psychiatrist—whatever is available in your area.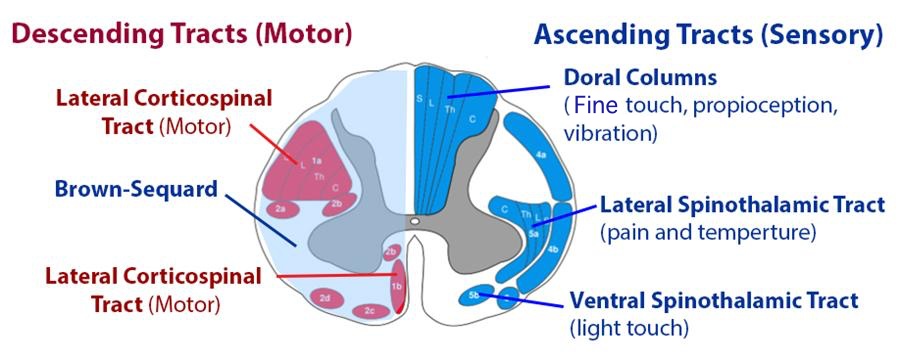 ”
”
Many children respond within the first week of the antibiotic treatment. The longer the symptoms have been active before the child starts treatment, the longer the response may take. If the symptoms disappear, you finish the course of antibiotics and then practice what Dr. Swedo calls “watchful waiting.” Some kids, however, don’t respond to the antibiotic treatment alone. And many will have later episodes when symptoms recur, triggered by another infection.
Treatment for Subsequent Episodes
Treatment for recurrences of PANDAS involves targeting what Dr. Swedo calls the three S’s: “the symptoms, the source, and the system.”
- The treatment for the symptoms — OCD and other forms of severe anxiety — is cognitive behavioral therapy (specifically, exposure and response prevention) and anti-depressant (also called anti-obsessional) medication, a selective serotonin reuptake inhibitor or SSRI. These treatments have been shown to be effective in reducing the symptoms, but they do not target the source of the problem.
- The treatment for the source — the infection — is another course of antibiotics.
- The system refers to the immune system, which is attacking the brain and generating these neuropsychiatric symptoms. The first-line treatment for the misfiring immune system is with IVIG, or intravenous immunoglobulin. IVIG is made from healthy blood plasma and is thought to balance the immune system. IVIG is recommended only for severe cases in which repeated courses of antibiotics combined with CBT and SSRIs were not successful in stopping the flare-up of symptoms.
- If IVIG, in turn, is not successful, children are treated with plasmapheresis (the removal, filtering and return of blood plasma). A review of 40 patients treated with plasmapheresis, published last year, showed an average improvement of 65% at 6 months following treatment, and 78% at longer-term follow-up.
Dr. Swedo notes that these three targets for treatment — symptoms, source, and system — are exactly the same if you were treating a child with asthmatic childhood pneumonia. “You treat the source — this is the pneumonia part — with antibiotics. You treat the symptoms with cough syrup – you don’t ask the child to cough for the next month, until the pneumonia resolves. And you treat the immune system with the inhaled steroid, the Singulair, and all the rest.”
“You treat the source — this is the pneumonia part — with antibiotics. You treat the symptoms with cough syrup – you don’t ask the child to cough for the next month, until the pneumonia resolves. And you treat the immune system with the inhaled steroid, the Singulair, and all the rest.”
Long-term Antibiotics for PANDAS
Children who’s had a recurrence of PANDAS are often given antibiotics for an extended period as a form of prevention, or prophylaxis, for recurring strep infections. Strep is so common in the school population that it is now recommended that prophylaxis continue until patients are about 21, Dr Swedo says. “You want to get them through college, boot camp — places where they’re going to have high exposure to things like mono and strep.” Research shows that antibiotic prophylaxis can reduce significantly the number of episodes of PANDAS symptoms a child experiences.
Unfortunately, even the strep prophylaxis won’t prevent all later episodes of PANDAS symptoms because the immune system, once primed, continues to react dangerously to other kinds of infections as well, misidentifying the brain as foreign, and generating symptoms.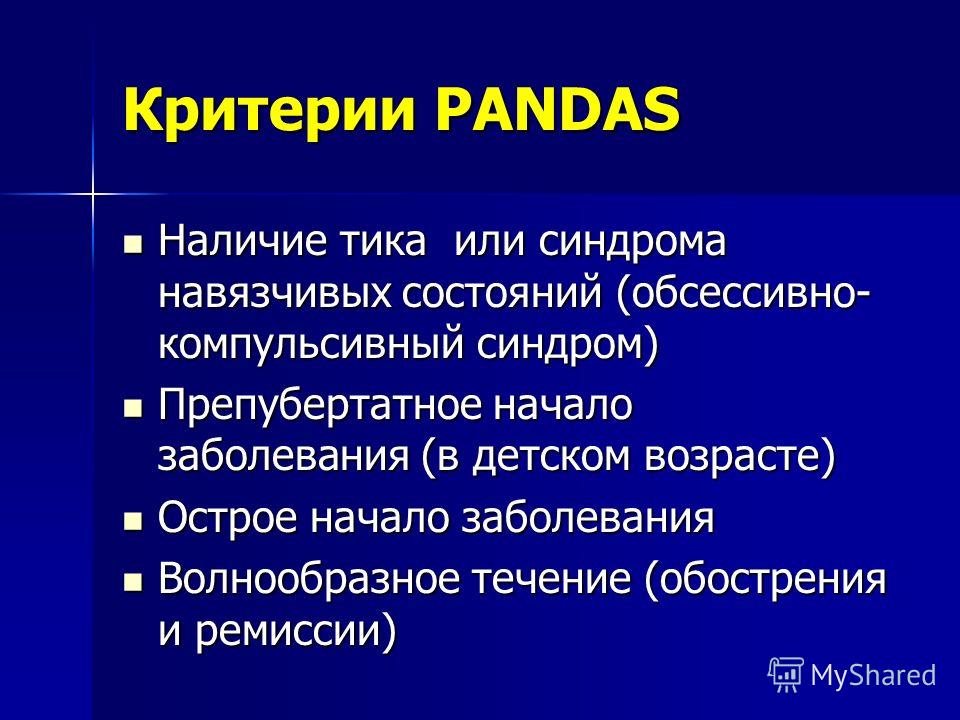
“But by preventing the strep,” Dr. Swedo notes, “you prevent over three quarters of those episodes, and you get them down to the point where then symptoms can be controlled with traditional anti-depressant medications and CBT.”
Other Resources
For more information on PANS and PANDAS, we recommend these resources:
PANDAS Physicians Network
This resource for physicians and medical professionals publishes consensus treatment protocols and guidelines for PANDAS. These guidelines were developed by the Diagnostic and Therapeutics subcommittee composed of PANDAS/PANS clinicians and researchers from medical institutions including Harvard, Yale, Stanford, Columbia, Georgetown and the National Institute of Mental Health. PPN also offers an archive of published studies on PANDAS/PANS.
National Institute of Mental Health
The NIMH offers an extensive information sheet about PANDAS/PANS, including history, diagnostic criteria, treatment options, and a list of research papers.
The International OCD Foundation
The IOCDF offers detailed information about PANDAS/PANS from diagnosis to treatment.
PANDAS Network
This non-profit organization founded by parents offers information and advocacy to improve the lives of children with PANDAS/PANS.
PANDAS syndrome. What is PANDAS Syndrome?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
PANDAS syndrome is an autoimmune neuropsychiatric pathology that develops in children due to streptococcal infection. The symptom complex of the disease is extremely diverse - from sudden anxiety and neurosis-like obsessive states to hyperkinesis and involuntary shouting out of words. The diagnosis is made on the basis of a psychiatric examination and laboratory confirmation of the presence of a streptococcal infection. Treatment includes antibiotics, intravenous immunoglobulin, psychotropic drugs. Sometimes the symptoms completely regress without therapy.
Treatment includes antibiotics, intravenous immunoglobulin, psychotropic drugs. Sometimes the symptoms completely regress without therapy.
ICD-10
F06.8 Other specified mental disorders due to damage and dysfunction of the brain or physical disease
- Causes
- Pathogenesis
- Symptoms
- Complications
- Diagnostics
- Treatment of PANDAS syndrome
- Prognosis and prevention
- Prices for treatment
General
PANDAS is an English abbreviation in which P stands for childhood, A for autoimmune, N for neuropsychiatric, D for disorder, A for associated, S for streptococcal infection. The term was first used in 1998 by the American pediatrician S. Shwedo and his colleagues. According to some sources, the disease occurs in one child out of 200. The true prevalence of the condition is unknown. Prepubertal children (7 to 12 years of age) usually suffer. Boys are more often ill, the ratio with girls is 2.6-4.7:1.
Boys are more often ill, the ratio with girls is 2.6-4.7:1.
PANDAS syndrome
Causes
It is believed that the occurrence of pathology is associated with a past infection caused by group A beta-hemolytic streptococcus (GABHS), for example, acute tonsillitis, scarlet fever, or chronic tonsillitis. Due to the peculiarities of the structure of the cell wall, the bacterium is able to trigger autoimmune reactions, namely, the production of autoantibodies that attack its own cells and body tissues, including brain cells.
In itself, the presence of streptococcal bacteria in the human body does not ensure the development of the disease, much depends on the immunogenetic predisposition. The syndrome occurs only in individuals whose blood contains specific alloantigens D8 / 17 on B-lymphocytes. The same marker is found in patients with another autoimmune pathology associated with GABHS, acute rheumatic fever.
Pathogenesis
The pathological reactions of the PANDAS syndrome are based on immune autoaggression. Along with other pathogenic properties (virulence, production of toxins), GABHS has the phenomenon of molecular mimicry. The structure of the bacterial wall of streptococcus is very similar to the structure of the membranes of some cells of the central nervous system.
Antibodies developed against GABHS, in addition to the pathogenic pathogen, attack the cells of the basal ganglia located in the caudate nucleus, globus pallidus, striatum, etc. These subcortical structures of the brain regulate motor (coordination of movements, skeletal muscle tone) and autonomic (control over respiratory rate and heartbeat, activity of the gastrointestinal tract) functions.
The basal ganglia are directly involved in the processes of higher nervous activity - memory, emotional reactions, speed of information processing. The defeat of these parts of the nervous system determines the main clinical picture of the PANDAS syndrome. According to most experts, the penetration of autoantibodies into the brain tissue is associated with a high permeability of the blood-brain barrier in children.
The defeat of these parts of the nervous system determines the main clinical picture of the PANDAS syndrome. According to most experts, the penetration of autoantibodies into the brain tissue is associated with a high permeability of the blood-brain barrier in children.
Symptoms
The disease occurs and proceeds acutely, which distinguishes it from most childhood neuropsychiatric disorders of other etiologies. The clinical picture varies considerably. The child becomes restless, irritable, emotionally unstable, his mood changes dramatically and often, concentration of attention is lost, memorization of new information and the ability to learn worsen.
The most typical obsessive-compulsive states are: repetitive actions (blinking, tilting the head to the side, shrugging), the desire to perform motor rituals (raising the leg high when descending stairs, repeatedly tying and untying shoelaces). Sleep is disturbed.
Characterized by unreasonable anxiety or fear. Often there is spontaneous uncontrolled shouting of words or repeated clattering, smacking, involuntary muscle twitches, tics, sweeping irregular movements of the limbs or head (hyperkinesis). Perhaps paroxysmal frequent sneezing, hiccups, sniffing for several hours.
Often there is spontaneous uncontrolled shouting of words or repeated clattering, smacking, involuntary muscle twitches, tics, sweeping irregular movements of the limbs or head (hyperkinesis). Perhaps paroxysmal frequent sneezing, hiccups, sniffing for several hours.
A distinctive feature of PANDAS syndrome is the spontaneous disappearance of symptoms during sleep. The average duration of an attack is 10-12 weeks, after which recovery occurs. Sometimes there is a tendency to an undulating course, especially often this is observed in chronic tonsillitis, the exacerbation of which leads to a relapse of neuropsychic manifestations.
Complications
Specific complications that pose a threat to the patient's life are extremely rare in PANDAS syndrome. Clinical symptoms of the disease significantly impair the quality of life of the child. Due to the backlog in school, children are sometimes left for the second year or temporarily transferred to home schooling. The disease has a particularly strong effect on socialization in society.
The disease has a particularly strong effect on socialization in society.
Some disorders (severe anxiety, compulsions) can become the basis for the development of neurotic or mental disorders. Involuntary movements or increased motor activity in some cases lead to injuries. Suicidal tendencies or excessively aggressive behavior are possible, in which the patient becomes dangerous to himself and to others, which requires isolation of the patient and constant monitoring.
Diagnostics
Children with PANDAS syndrome are supervised by pediatricians, child psychiatrists and neurologists. Diagnosis is difficult due to the diversity of the clinical picture. Take into account age (7-12 years), the presence of signs of streptococcal infection (hyperemia of the pharynx, raids on the tonsils, enlargement and soreness of the cervical lymph nodes) or an indication of a sore throat. To clarify the diagnosis, an additional examination is prescribed, including:
- Laboratory blood tests.
 In the general analysis, there may be signs of inflammation - leukocytosis, an increase in ESR. Biochemical analysis reveals serological markers of streptococcal infection - elevated titers of antistreptolysin-O (ASLO), anti-DNase B and rheumatoid factor (RF).
In the general analysis, there may be signs of inflammation - leukocytosis, an increase in ESR. Biochemical analysis reveals serological markers of streptococcal infection - elevated titers of antistreptolysin-O (ASLO), anti-DNase B and rheumatoid factor (RF). - Immunological and bacteriological studies. To confirm the presence of GABHS in the body, immunochromatographic express diagnostics (streptatest) and bacterial culture of a swab from the pharynx and tonsils are used.
- EEG. When conducting a 12-hour video-EEG monitoring, an electroencephalogram revealed increased convulsive activity, spike waves during a night's sleep.
Determination of specific antibodies to the basal ganglia in the blood significantly increases the reliability of the diagnosis, but this analysis is practically not used in clinical practice. Differential diagnosis is carried out with Sydenham's chorea, Tourette's syndrome, temporal epilepsy, etc. The following criteria for PANDAS syndrome are taken into account:
- presence of obsessive-compulsive disorders, tics;
- onset in prepubertal age;
- acute onset and paroxysmal course;
- association with GABHS infection;
- other neurological disorders.
Treatment of PANDAS syndrome
Depending on the severity of symptoms and mental status, patients may be treated as outpatients or inpatients. With severe behavioral disorders, round-the-clock monitoring is necessary. Some children experience spontaneous regression of disorders. Particular attention is paid to psychotherapy: individual conversations, training in special techniques for controlling tics and obsessive movements.
Sleep disturbances are corrected by non-drug methods - a strict regime of awakening and going to bed, the complete exclusion of the use of caffeine and caffeinated drinks (cola, "energy"), the distribution of activity during the day with the inclusion of physical exercises. The following drugs are used:
- Etiotropic therapy. Since the main cause of PANDAS syndrome is GABHS infection, for its eradication, all patients are prescribed antibacterial agents - phenoxymethylpenicillin, amoxicillin.
- Pathogenetic therapy. In order to suppress autoimmune damage to the basal ganglia, immunomodulatory drugs are used. In mild cases, NSAIDs are sufficient. With disadaptation, glucocorticosteroids or immunoglobulin are used. In extremely severe mental disorders, plasmapheresis or strong immunosuppressants (mycophenolate) are indicated.
- Symptomatic therapy. Antidepressants, SSRI inhibitors, are effective in relieving the symptoms of OCD. For increased anxiety, benzodiazepines or atypical antipsychotics are recommended.
Prognosis and prevention
PANDAS syndrome has a favorable prognosis. The life expectancy of patients does not differ from that in the general population. Lethal outcomes are casuistry. All clinical signs in the vast majority of cases respond well to treatment, in some children spontaneous recovery is possible without therapy.
To prevent exacerbation of chronic tonsillitis and subsequent neuropsychic attacks, antibiotic prophylaxis and courses of manual or hardware washing of tonsil lacunae are carried out. If, despite these measures, relapses continue, it is recommended to surgically remove the focus of persistent infection (palatine tonsils) - tonsillectomy.
If, despite these measures, relapses continue, it is recommended to surgically remove the focus of persistent infection (palatine tonsils) - tonsillectomy.
You can share your medical history, what helped you in the treatment of PANDAS-syndrome.
Sources
- PANDAS syndrome in cardiorheumatology / Evtushenko S.K., Perepechaenko Yu.M., Evtushenko L.F., Morozova T.M.// Bulletin of physiotherapy and balneology - 2005 - No. 4.
- PANDAS-syndrome/ Swedo S. E., Klesling L.// J. Reumatologi - 1994 - No. 3.
- Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS): an evolving concept/ Macerollo A., Martino D.// Tremor Other Hyperkinet Mov (NY) - 2013.
- Revised Treatment Guidelines Released for Pediatric Acute Onset Neuropsychiatric Syndrome (PANS/PANDAS) – 2017.
- can not be used for self-diagnosis and self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests.
 For diagnosis and proper treatment, you should contact your doctor.
For diagnosis and proper treatment, you should contact your doctor. How to detect PANDAS syndrome | Directory of medical laboratory Optimum (Sochi, Adler)
Get test results
- Home
- How to recognize the disease
- Childhood diseases
- PANDAS syndrome
More about the doctor
PANDAS syndrome is a neuropsychic autoimmune pathology that develops in a child who has had a streptococcal infection - most often its causative agent is group A beta-hemolytic streptococcus.
Diagnosis of PANDAS syndrome
- Collecting an anamnesis to clarify past infectious diseases and listen to the patient's complaints.
- Physical examination - to detect redness of the throat, swollen cervical lymph nodes, plaque on the tonsils.

- Hemograms - to detect inflammatory markers (increased erythrocyte sedimentation rate and leukocyte count).
- Biochemical blood test - to measure the level of ASLO (antistreptolysin-O), rheumatoid factor, C-reactive protein, anti-deoxyribonuclease.
- Bacteriological culture of scrapings from the pharynx - to identify and identify the causative agent of infection.
- Serological screening - to detect specific antibodies to gangliosides and double-stranded DNA.
- Universal rapid test - for the rapid detection of the presence of group A beta-hemolytic streptococcus.
Causes of development
The occurrence of PANDAS-syndrome is associated with scarlet fever, acute tonsillitis or chronic tonsillitis. A feature of the structure of the cell walls of their pathogen is the ability to "start" the production of autoimmune antibodies, which attack the cells of their own body. Predisposing factors - immunogenetic predisposition and the presence of other autoimmune pathologies.
Pathogenesis
Pathological reactions develop due to immune aggression - specific antibodies produced against beta-hemolytic streptococcus A act against cells of a large structure surrounding the limbic system of the brain and regulating movement coordination, skeletal muscle tone, respiratory rate and heart rate muscles, activity of the digestive tract, processes of higher nervous activity.
Symptoms and first signs
PANDAS-syndrome is characterized by an acute course – a sick child has:
- restlessness;
- emotional instability;
- irritability;
- impaired concentration;
- loss of learning ability;
- frequent blinking, sneezing, shrugging, smacking, head tilting to one side;
- sleep disorder;
- unreasonable fear;
- hyperkinesis.
A distinctive feature of the pathology is the spontaneous disappearance of clinical manifestations during sleep.