Source of gaba
Physiology, GABA - StatPearls - NCBI Bookshelf
Benjamin E. Jewett; Sandeep Sharma.
Author Information and Affiliations
Last Update: July 25, 2022.
Introduction
Gamma-aminobutyric acid (GABA) is an amino acid that serves as the primary inhibitory neurotransmitter in the brain and a major inhibitory neurotransmitter in the spinal cord. It exerts its primary function in the synapse between neurons by binding to post-synaptic GABA receptors which modulate ion channels, hyperpolarizing the cell and inhibiting the transmission of an action potential. The clinical significance of GABA cannot be underestimated. Disorder in GABA signaling is implicated in a multitude of neurologic and psychiatric conditions. Modulation of GABA signaling is the basis of many pharmacologic treatments in neurology, psychiatry, and anesthesia.[1][2][3]
Cellular Level
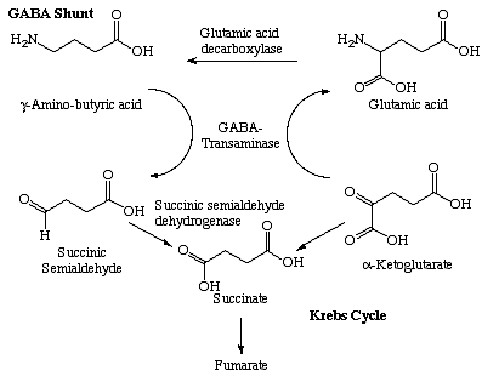
GABA is synthesized in the cytoplasm of the presynaptic neuron from the precursor glutamate by the enzyme glutamate decarboxylase, an enzyme which uses vitamin B6 (pyridoxine) as a cofactor. After synthesis, it is loaded into synaptic vesicles by the vesicular inhibitory amino acid transporter. SNARE complexes help dock the vesicles into the plasma membrane of the cell. When an action potential reaches the presynaptic cell, voltage-gated calcium channels open and calcium binds to synaptobrevin, which results in the fusion of the vesicle with the plasma membrane and releases GABA into the synaptic cleft where it can bind with GABA receptors. GABA can then be degraded extracellularly or taken back up into glia or the presynaptic cell. It is degraded by GABA-transaminase into succinate semialdehyde which then enters the citric acid cycle.
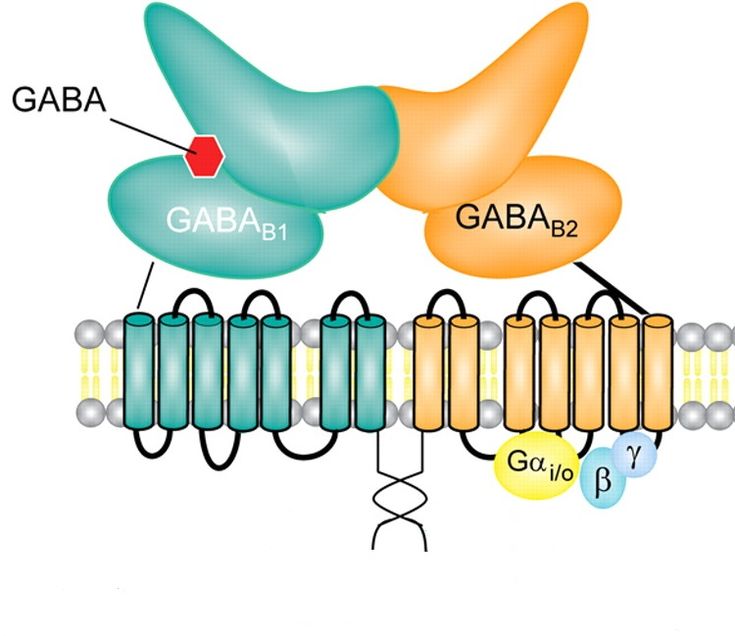
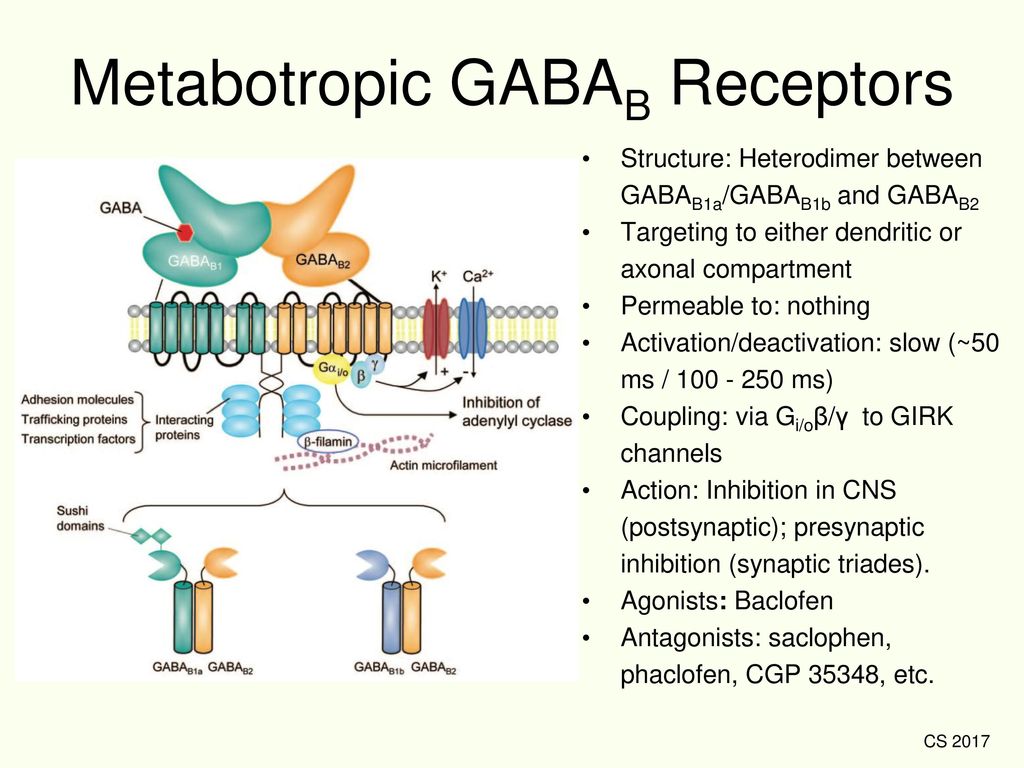
GABA binds to two major post-synaptic receptors, the GABA-A and GABA-B receptors. The GABA-A receptor is an ionotropic receptor that increases chloride ion conductance into the cell in the presence of GABA. The extracellular concentration of chloride is normally much higher than the intracellular concentration. Consequently, the influx of negatively charged chloride ions hyperpolarizes the cell, inhibiting the creation of an action potential. The GABA-B receptor functions via a metabotropic G-protein coupled receptor which increases postsynaptic potassium conductance and decreases presynaptic calcium conductance, which consequently hyperpolarizes the postsynaptic cell and prevents the conduction of an action potential in the presynaptic cell. Consequently, regardless of binding to GABA-A or GABA-B receptors, GABA serves an inhibitory function.[4][5][6]
The GABA-B receptor functions via a metabotropic G-protein coupled receptor which increases postsynaptic potassium conductance and decreases presynaptic calcium conductance, which consequently hyperpolarizes the postsynaptic cell and prevents the conduction of an action potential in the presynaptic cell. Consequently, regardless of binding to GABA-A or GABA-B receptors, GABA serves an inhibitory function.[4][5][6]
Development
Due to extracellular concentrations of chloride being lower than intracellular levels in the developing brain, GABA has an excitatory role in the fetal and neonatal brain. When GABA-A receptors open chloride channels in the developing brain, the cell becomes hypopolarized and thus more likely to fire an action potential. Consequently, drugs that increase GABA signaling have been reported to be of limited efficacy in the treatment of seizures in preterm neonates.
Organ Systems Involved
GABA is found throughout the human body, though the role that it plays in many regions remains an area of active research. GABA is the primary inhibitory neurotransmitter in the brain, and it is a major inhibitory neurotransmitter in the spinal cord. The insulin-producing beta-cells of the pancreas produce GABA. It functions to inhibit pancreatic alpha cells, stimulate beta-cell growth, and convert alpha-cells to beta cells. GABA also has been found in varying low concentrations within other organ systems, though the significance and function of this are unclear.[7]
GABA is the primary inhibitory neurotransmitter in the brain, and it is a major inhibitory neurotransmitter in the spinal cord. The insulin-producing beta-cells of the pancreas produce GABA. It functions to inhibit pancreatic alpha cells, stimulate beta-cell growth, and convert alpha-cells to beta cells. GABA also has been found in varying low concentrations within other organ systems, though the significance and function of this are unclear.[7]
Function
Because GABA is the fundamental neurotransmitter for inhibiting neuronal firing, its function is determined by the neural circuit that it is inhibiting. It is involved in complex circuits throughout the central nervous system. For example, GABA is released by striatal neurons in both the direct and indirect pathways projecting to the globus pallidus, which in turn extends GABA neurons to other brain areas, inhibiting unwanted motor signals. Another example is that GABA signaling in the medulla is involved in the maintenance of respiratory rate. Increased GABA signaling reduces the respiratory rate. A third example is found in the spinal cord, where GABA serves in the inhibitory interneurons. These neurons help to integrate excitatory proprioceptive signals, allowing for the spinal cord to integrate sensory information and create smooth movements.[8][9][10]
Increased GABA signaling reduces the respiratory rate. A third example is found in the spinal cord, where GABA serves in the inhibitory interneurons. These neurons help to integrate excitatory proprioceptive signals, allowing for the spinal cord to integrate sensory information and create smooth movements.[8][9][10]
Pathophysiology
GABA is involved in several disease states:
Pyridoxine deficiency is a rare disease in which the vitamin is not available for the synthesis of GABA. It usually presents as frequent seizures during infancy that are resistant to treatment with anticonvulsants but responds very well to vitamin supplementation.
The clinical features of hepatic encephalopathy are thought to be due to elevated ammonia levels binding to the GABA-A/GABA complex and increasing chloride ion permeability.
The symptoms of Huntington disease are partially caused by a lack of GABA in the striatal projections to the globus pallidus.
Dystonia and spasticity are believed to be related to a deficiency in GABA signaling.[11][12][13]
Clinical Significance
GABA is of great clinical significance. Medications that act on the GABA receptor are commonly used as therapeutic medications and substances of abuse, and it is unlikely that any physician, regardless of specialty, will not encounter clinical situations that involve GABA.
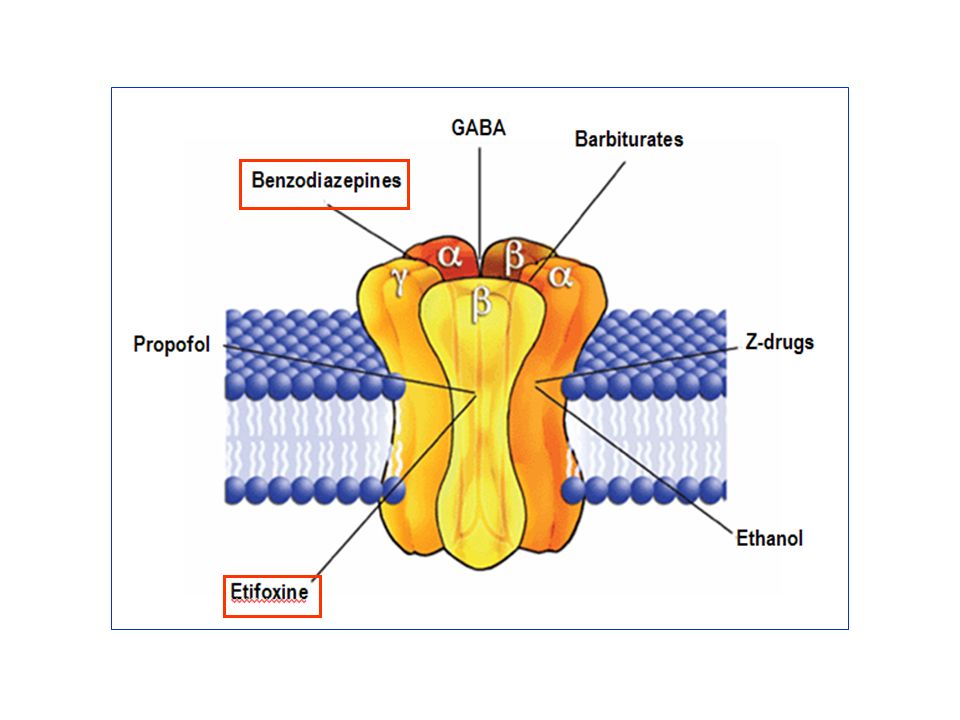
There are numerous uses for drugs that modulate GABA signaling. Benzodiazepines are a drug class that exerts its effects by binding to the GABA-A receptor, resulting in increased chloride ion permeability by changing the frequency with which the chloride channels open. They are used in surgical anesthesia, the treatment of epilepsy, REM-sleep disorders, alcohol withdrawal, essential tremor, and muscle spasticity. They are also common drugs of abuse. Ethanol, one of the oldest and most widely-used psychoactive substances, also exerts effects on the GABA-A receptor. Alcohol withdrawal is treated with GABA modulating drugs, such as benzodiazepines. Furthermore, ethanol and benzodiazepines exhibit cross-tolerance with one another due to their similar mechanism of action. Overdosing or taking multiple GABA modulating drugs can result in respiratory depression due to increased GABA signaling in the medulla of the brain stem.
Alcohol withdrawal is treated with GABA modulating drugs, such as benzodiazepines. Furthermore, ethanol and benzodiazepines exhibit cross-tolerance with one another due to their similar mechanism of action. Overdosing or taking multiple GABA modulating drugs can result in respiratory depression due to increased GABA signaling in the medulla of the brain stem.
Many other drugs modulate GABA signaling, including the following:
Barbiturates, sedative drugs which increase the duration at which the chloride channel is open when GABA binds the GABA-A receptor
Vigabatrin, an antiepileptic inhibitor of GABA transaminase
Propofol, a sedative commonly used in general anesthesia and allosteric modulator and agonist of the GABA-A receptor
Flumazenil, a benzodiazepine antagonist which binds to the GABA-A receptor and can reverse benzodiazepine intoxication and improve mental status in hepatic encephalopathy
Baclofen, a muscle relaxant and GABA-B agonist
Valproic acid, a mood stabilizer and anti-epileptic that is hypothesized to have an inhibitory effect on GABA uptake
Zolpidem, a sedative-hypnotic, exerts its effects on the GABA-A receptor
Gabapentin, commonly prescribed to treat neuropathic pain, partially exerts its effects by increasing GABA synthesis via modulation of glutamate dehydrogenase[14][15][16][17]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Pedrón VT, Varani AP, Bettler B, Balerio GN. GABAB receptors modulate morphine antinociception: Pharmacological and genetic approaches. Pharmacol Biochem Behav. 2019 May;180:11-21. [PubMed: 30851293]
- 2.
Kondziella D. The Top 5 Neurotransmitters from a Clinical Neurologist's Perspective. Neurochem Res. 2017 Jun;42(6):1767-1771. [PubMed: 27822666]
- 3.
Olsen RW. GABAA receptor: Positive and negative allosteric modulators. Neuropharmacology. 2018 Jul 01;136(Pt A):10-22. [PMC free article: PMC6027637] [PubMed: 29407219]
- 4.
Südhof TC. Neurotransmitter release: the last millisecond in the life of a synaptic vesicle. Neuron. 2013 Oct 30;80(3):675-90. [PMC free article: PMC3866025] [PubMed: 24183019]
- 5.
Leinekugel X, Khalilov I, McLean H, Caillard O, Gaiarsa JL, Ben-Ari Y, Khazipov R. GABA is the principal fast-acting excitatory transmitter in the neonatal brain.
 Adv Neurol. 1999;79:189-201. [PubMed: 10514814]
Adv Neurol. 1999;79:189-201. [PubMed: 10514814]- 6.
Allen MJ, Sabir S, Sharma S. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Feb 17, 2022. GABA Receptor. [PubMed: 30252380]
- 7.
Khanna A, Walcott BP, Kahle KT. Limitations of Current GABA Agonists in Neonatal Seizures: Toward GABA Modulation Via the Targeting of Neuronal Cl(-) Transport. Front Neurol. 2013;4:78. [PMC free article: PMC3691543] [PubMed: 23805124]
- 8.
Wang Q, Ren L, Wan Y, Prud'homme GJ. GABAergic regulation of pancreatic islet cells: Physiology and antidiabetic effects. J Cell Physiol. 2019 Sep;234(9):14432-14444. [PubMed: 30693506]
- 9.
Tong Y. Seizures caused by pyridoxine (vitamin B6) deficiency in adults: A case report and literature review. Intractable Rare Dis Res. 2014 May;3(2):52-6. [PMC free article: PMC4204538] [PubMed: 25343127]
- 10.
Raymond LA. Striatal synaptic dysfunction and altered calcium regulation in Huntington disease.
 Biochem Biophys Res Commun. 2017 Feb 19;483(4):1051-1062. [PubMed: 27423394]
Biochem Biophys Res Commun. 2017 Feb 19;483(4):1051-1062. [PubMed: 27423394]- 11.
Hammond JB, Ahmad F. Hepatic encephalopathy and role of antibenzodiazepines. Am J Ther. 1998 Jan;5(1):33-6. [PubMed: 10099035]
- 12.
Termsarasab P, Thammongkolchai T, Frucht SJ. Medical treatment of dystonia. J Clin Mov Disord. 2016;3:19. [PMC free article: PMC5168853] [PubMed: 28031858]
- 13.
Yamada KA, Norman WP, Hamosh P, Gillis RA. Medullary ventral surface GABA receptors affect respiratory and cardiovascular function. Brain Res. 1982 Sep 23;248(1):71-8. [PubMed: 6289995]
- 14.
Ahnert-Hilger G, Kutay U, Chahoud I, Rapoport T, Wiedenmann B. Synaptobrevin is essential for secretion but not for the development of synaptic processes. Eur J Cell Biol. 1996 May;70(1):1-11. [PubMed: 8738414]
- 15.
Wan Y, Wang Q, Prud'homme GJ. GABAergic system in the endocrine pancreas: a new target for diabetes treatment.
 Diabetes Metab Syndr Obes. 2015;8:79-87. [PMC free article: PMC4322886] [PubMed: 25678807]
Diabetes Metab Syndr Obes. 2015;8:79-87. [PMC free article: PMC4322886] [PubMed: 25678807]- 16.
Korpi ER, Sinkkonen ST. GABA(A) receptor subtypes as targets for neuropsychiatric drug development. Pharmacol Ther. 2006 Jan;109(1-2):12-32. [PubMed: 15996746]
- 17.
Jembrek MJ, Vlainic J. GABA Receptors: Pharmacological Potential and Pitfalls. Curr Pharm Des. 2015;21(34):4943-59. [PubMed: 26365137]
Dietary Neurotransmitters: A Narrative Review on Current Knowledge
1. Millstine D., Chen C., Bauer B. Complementary and integrative medicine in the management of headache. BMJ. 2017;357:j1805. doi: 10.1136/bmj.j1805. [PubMed] [CrossRef] [Google Scholar]
2. Pasca L., De Giorgis V., Macasaet J.A., Trentani C., Tagliabue A., Veggiotti P. The changing face of dietary therapy for epilepsy. Eur. J. Pediatr. 2016;175:1267–1276. doi: 10.1007/s00431-016-2765-z. [PubMed] [CrossRef] [Google Scholar]
3. Wang L., Xiong N., Huang J. , Guo S., Liu L., Han C., Zhang G., Jiang H., Ma K., Xia Y., et al. Protein-restricted diets for ameliorating motor fluctuations in Parkinson’s disease. Front. Aging Neurosci. 2017;9:206. doi: 10.3389/fnagi.2017.00206. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
, Guo S., Liu L., Han C., Zhang G., Jiang H., Ma K., Xia Y., et al. Protein-restricted diets for ameliorating motor fluctuations in Parkinson’s disease. Front. Aging Neurosci. 2017;9:206. doi: 10.3389/fnagi.2017.00206. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
4. Briguglio M., Dell’Osso B., Galentino R., Zanaboni Dina C., Banfi G., Porta M. Tics and obsessive-compulsive disorder in relation to diet: Two case reports. L'Encephale. 2017 doi: 10.1016/j.encep.2017.06.004. [PubMed] [CrossRef] [Google Scholar]
5. Guallar E., Stranges S., Mulrow C., Appel L.J., Miller E.R., 3rd. Enough is enough: Stop wasting money on vitamin and mineral supplements. Ann. Intern. Med. 2013;159:850–851. doi: 10.7326/0003-4819-159-12-201312170-00011. [PubMed] [CrossRef] [Google Scholar]
6. Choi S., DiSilvio B., Fernstrom M.H., Fernstrom J.D. Effect of chronic protein ingestion on tyrosine and tryptophan levels and catecholamine and serotonin synthesis in rat brain. Nutr. Neurosci.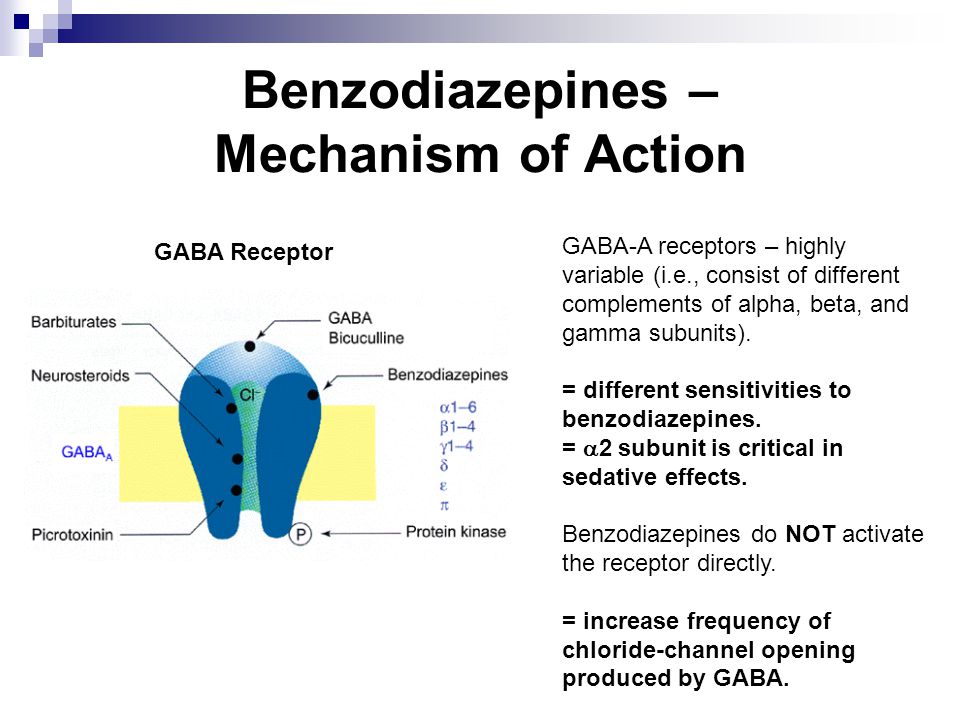 2011;14:260–267. doi: 10.1179/1476830511Y.0000000019. [PubMed] [CrossRef] [Google Scholar]
2011;14:260–267. doi: 10.1179/1476830511Y.0000000019. [PubMed] [CrossRef] [Google Scholar]
7. Fallon S., Shearman E., Sershen H., Lajtha A. Food reward-induced neurotransmitter changes in cognitive brain regions. Neurochem. Res. 2007;32:1772–1782. doi: 10.1007/s11064-007-9343-8. [PubMed] [CrossRef] [Google Scholar]
8. Bender A., Hagan K.E., Kingston N. The association of folate and depression: A meta-analysis. J. Psychiatr. Res. 2017;95:9–18. doi: 10.1016/j.jpsychires.2017.07.019. [PubMed] [CrossRef] [Google Scholar]
9. Roshchina V. Neurotransmitters in Plant Life. Science Publishers; Dubai, UAE: 2001. [Google Scholar]
10. Naila A., Flint S., Fletcher G., Bremer P., Meerdink G. Control of biogenic amines in food—Existing and emerging approaches. J. Food Sci. 2010;75:R139–R150. doi: 10.1111/j.1750-3841.2010.01774.x. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
11. Odjakova M., Hadjiivanova C. Animal neurotransmitter substances in plants. Bulg. J. Plant Physiol. 1997;23:94–102. [Google Scholar]
Plant Physiol. 1997;23:94–102. [Google Scholar]
12. Hartmann E., Kilbinger H. Occurrence of light-dependent acetylcholine concentrations in higher plants. Experientia. 1974;30:1397–1398. doi: 10.1007/BF01919649. [PubMed] [CrossRef] [Google Scholar]
13. Fluck R.A., Jaffe M.J. The acetylcholine system in plants. In: Smith H., editor. Commentaries in Plant Science. Pergamon Press; Oxford, UK: 1976. pp. 119–136. [Google Scholar]
14. Fryer A., Christopoulos A., Nathanson N. Muscarinic Receptors. 1st ed. Springer; Berlin, Germany: 2012. [Google Scholar]
15. Wessler I., Kilbinger H., Bittinger F., Kirkpatrick C.J. The biological role of non-neuronal acetylcholine in plants and humans. Jpn. J. Pharmacol. 2001;85:2–10. doi: 10.1254/jjp.85.2. [PubMed] [CrossRef] [Google Scholar]
16. Wessler I., Kirkpatrick C.J., Racke K. Non-neuronal acetylcholine, a locally acting molecule, widely distributed in biological systems: Expression and function in humans. Pharmacol. Ther. 1998;77:59–79. doi: 10.1016/S0163-7258(97)00085-5. [PubMed] [CrossRef] [Google Scholar]
1998;77:59–79. doi: 10.1016/S0163-7258(97)00085-5. [PubMed] [CrossRef] [Google Scholar]
17. Barnes J., Anderson L., Phillipson D. Herbal Medicines. 3rd ed. Pharmaceutical Press; London, UK: 2007. 440p [Google Scholar]
18. European Pharmacopoeia Commission . European Pharmacopoeia: Published under the Direction of the Council of Europe (Partial Agreement) in Accordance with the Convention on the Elaboration of a European Pharmacopoeia. 2nd ed. Maisonneuve; Sainte Ruffine, France: 1981. [Google Scholar]
19. Rangan C., Barceloux D.G. Food additives and sensitivities. Dis. Mon. 2009;55:292–311. doi: 10.1016/j.disamonth.2009.01.004. [PubMed] [CrossRef] [Google Scholar]
20. Jinap S., Hajeb P. Glutamate. Its applications in food and contribution to health. Appetite. 2010;55:1–10. doi: 10.1016/j.appet.2010.05.002. [PubMed] [CrossRef] [Google Scholar]
21. Zhang Y., Venkitasamy C., Pan Z., Liu W., Zhao L. Novel umami ingredients: Umami peptides and their taste. J. Food Sci. 2017;82:16–23. doi: 10.1111/1750-3841.13576. [PubMed] [CrossRef] [Google Scholar]
Food Sci. 2017;82:16–23. doi: 10.1111/1750-3841.13576. [PubMed] [CrossRef] [Google Scholar]
22. Skypala I.J., Williams M., Reeves L., Meyer R., Venter C. Sensitivity to food additives, vaso-active amines and salicylates: A review of the evidence. Clin. Transl. Allergy. 2015;5:34. doi: 10.1186/s13601-015-0078-3. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
23. Gan R., Lui W., Wu K., Chan C., Dai S., Sui Z., Corke H. Bioactive compounds and bioactivities of germinated edible seeds and sprouts: An updated review. Trends Food Sci. Technol. 2017;59:1–14. doi: 10.1016/j.tifs.2016.11.010. [CrossRef] [Google Scholar]
24. Martinez-Villaluenga C., Kuo Y.-H., Lambein F., Frias J., Vidal-Valverde C. Kinetics of free protein amino acids, free non-protein amino acids and trigonelline in soybean (Glycine max L.) and lupin (Lupinus angustifolius L.) sprouts. Eur. Food Res. Technol. 2006;224:177–186. doi: 10.1007/s00217-006-0300-6. [CrossRef] [Google Scholar]
25. Li L., Liu B., Zheng X. Bioactive ingredients in adzuki bean sprouts. J. Med. Plants Res. 2011;5:5894–5898. [Google Scholar]
Li L., Liu B., Zheng X. Bioactive ingredients in adzuki bean sprouts. J. Med. Plants Res. 2011;5:5894–5898. [Google Scholar]
26. Xu J., Hu Q. Changes in γ-aminobutyric acid content and related enzyme activities in Jindou 25 soybean (Glycine max L.) seeds during germination. LWT Food Sci. Technol. 2014;55:341–346. doi: 10.1016/j.lwt.2013.08.008. [CrossRef] [Google Scholar]
27. Kuo Y., Rozan P., Lambein F., Frias J., Vidal-Valverde C. Effects of different germination conditions on the contents of free protein and non-protein amino acids of commercial legumes. Food Chem. 2004;86:537–545. doi: 10.1016/j.foodchem.2003.09.042. [CrossRef] [Google Scholar]
28. Xu J.G., Hu Q.P., Duan J.L., Tian C.R. Dynamic changes in gamma-aminobutyric acid and glutamate decarboxylase activity in oats (Avena nuda L.) during steeping and germination. J. Agric. Food Chem. 2010;58:9759–9763. doi: 10.1021/jf101268a. [PubMed] [CrossRef] [Google Scholar]
29. Van Hung P., Maeda T. , Morita N. Improvement of nutritional composition and antioxidant capacity of high-amylose wheat during germination. J. Food Sci. Technol. 2015;52:6756–6762. doi: 10.1007/s13197-015-1730-6. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
, Morita N. Improvement of nutritional composition and antioxidant capacity of high-amylose wheat during germination. J. Food Sci. Technol. 2015;52:6756–6762. doi: 10.1007/s13197-015-1730-6. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
30. Oh S., Moon Y., Oh C. γ-Aminobutyric Acid (GABA) Content of Selected Uncooked Foods. Prev. Nutr. Food Sci. 2003;8:75–78. doi: 10.3746/jfn.2003.8.1.075. [CrossRef] [Google Scholar]
31. Lin L.Y., Peng C.C., Yang Y.L., Peng R.Y. Optimization of bioactive compounds in buckwheat sprouts and their effect on blood cholesterol in hamsters. J. Agric. Food Chem. 2008;56:1216–1223. doi: 10.1021/jf072886x. [PubMed] [CrossRef] [Google Scholar]
32. Akihiro T., Koike S., Tani R., Tominaga T., Watanabe S., Iijima Y., Aoki K., Shibata D., Ashihara H., Matsukura C., et al. Biochemical mechanism on GABA accumulation during fruit development in tomato. Plant Cell Physiol. 2008;49:1378–1389. doi: 10.1093/pcp/pcn113. [PubMed] [CrossRef] [Google Scholar]
33. Park K.B., Oh S.H. Production of yogurt with enhanced levels of gamma-aminobutyric acid and valuable nutrients using lactic acid bacteria and germinated soybean extract. Bioresour. Technol. 2007;98:1675–1679. doi: 10.1016/j.biortech.2006.06.006. [PubMed] [CrossRef] [Google Scholar]
Park K.B., Oh S.H. Production of yogurt with enhanced levels of gamma-aminobutyric acid and valuable nutrients using lactic acid bacteria and germinated soybean extract. Bioresour. Technol. 2007;98:1675–1679. doi: 10.1016/j.biortech.2006.06.006. [PubMed] [CrossRef] [Google Scholar]
34. Kim J.Y., Lee M.Y., Ji G.E., Lee Y.S., Hwang K.T. Production of gamma-aminobutyric acid in black raspberry juice during fermentation by Lactobacillus brevis GABA100. Int. J. Food Microbiol. 2009;130:12–16. doi: 10.1016/j.ijfoodmicro.2008.12.028. [PubMed] [CrossRef] [Google Scholar]
35. Steenbergen L., Sellaro R., Stock A.K., Beste C., Colzato L.S. gamma-Aminobutyric acid (GABA) administration improves action selection processes: A randomised controlled trial. Sci. Rep. 2015;5:12770. doi: 10.1038/srep12770. [PMC free article] [PubMed] [CrossRef] [Google Scholar]Retracted
36. Zhao M., Ma Y., Wei Z.Z., Yuan W.X., Li Y.L., Zhang C.H., Xue X.T., Zhou H.J. Determination and comparison of gamma-aminobutyric acid (GABA) content in pu-erh and other types of Chinese tea. J. Agric. Food Chem. 2011;59:3641–3648. doi: 10.1021/jf104601v. [PubMed] [CrossRef] [Google Scholar]
J. Agric. Food Chem. 2011;59:3641–3648. doi: 10.1021/jf104601v. [PubMed] [CrossRef] [Google Scholar]
37. Funayama S., Hikino H. Hypotensive principles of Phytolacca roots. J. Nat. Prod. 1979;42:672–674. doi: 10.1021/np50006a015. [PubMed] [CrossRef] [Google Scholar]
38. Carratu B., Boniglia C., Giammarioli S., Mosca M., Sanzini E. Free amino acids in botanicals and botanical preparations. J. Food Sci. 2008;73:C323–C328. doi: 10.1111/j.1750-3841.2008.00767.x. [PubMed] [CrossRef] [Google Scholar]
39. Feldman J.M., Lee E.M., Castleberry C.A. Catecholamine and serotonin content of foods: Effect on urinary excretion of homovanillic and 5-hydroxyindoleacetic acid. J. Am. Diet Assoc. 1987;87:1031–1035. [PubMed] [Google Scholar]
40. Kanazawa K., Sakakibara H. High content of dopamine, a strong antioxidant, in Cavendish banana. J. Agric. Food Chem. 2000;48:844–848. doi: 10.1021/jf9909860. [PubMed] [CrossRef] [Google Scholar]
41. Udenfriend S., Lovenberg W., Sjoerdsma A. Physiologically active amines in common fruits and vegetables. Arch. Biochem. Biophys. 1959;85:487–490. doi: 10.1016/0003-9861(59)90516-8. [PubMed] [CrossRef] [Google Scholar]
Physiologically active amines in common fruits and vegetables. Arch. Biochem. Biophys. 1959;85:487–490. doi: 10.1016/0003-9861(59)90516-8. [PubMed] [CrossRef] [Google Scholar]
42. Wichers H., Visser J., Huizing H., Pras N. Occurrence of L-DOPA and dopamine in plants and cell cultures of Mucuna pruriens and effects of 2,4-D and NaCl on these compounds. Plant Cell Tissue Organ Cult. 1993;33:259–264. doi: 10.1007/BF02319010. [CrossRef] [Google Scholar]
43. Cassani E., Cilia R., Laguna J., Barichella M., Contin M., Cereda E., Isaias I.U., Sparvoli F., Akpalu A., Budu K.O., et al. Mucuna pruriens for Parkinson’s disease: Low-cost preparation method, laboratory measures and pharmacokinetics profile. J. Neurol. Sci. 2016;365:175–180. doi: 10.1016/j.jns.2016.04.001. [PubMed] [CrossRef] [Google Scholar]
44. Gerrard J.W., Richardson J.S., Donat J. Neuropharmacological evaluation of movement disorders that are adverse reactions to specific foods. Int. J. Neurosci. 1994;76:61–69.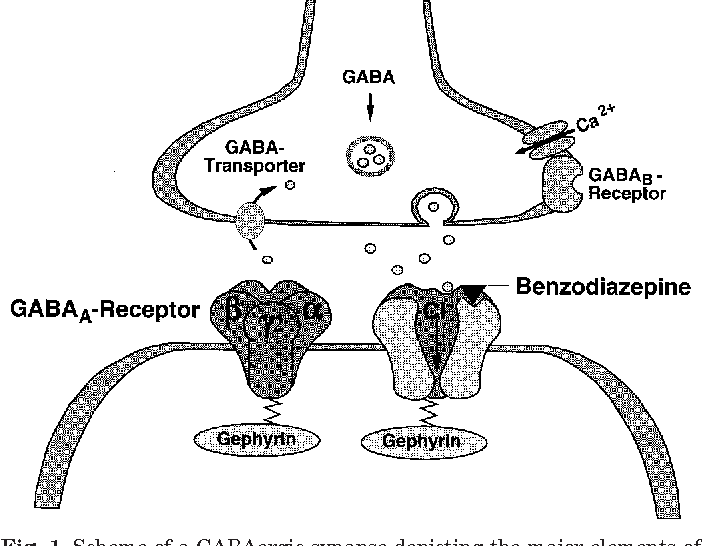 doi: 10.3109/00207459408985992. [PubMed] [CrossRef] [Google Scholar]
doi: 10.3109/00207459408985992. [PubMed] [CrossRef] [Google Scholar]
45. Huang X., Mazza G. Application of LC and LC-MS to the analysis of melatonin and serotonin in edible plants. Crit. Rev. Food Sci. Nutr. 2011;51:269–284. doi: 10.1080/10408398.2010.529193. [PubMed] [CrossRef] [Google Scholar]
46. Adão R.C., Glória M.B.A. Bioactive amines and carbohydrate changes during ripening of ‘Prata’ banana (Musa acuminata × M. balbisiana) Food Chem. 2005;90:705–711. doi: 10.1016/j.foodchem.2004.05.020. [CrossRef] [Google Scholar]
47. Kang S., Back K. Enriched production of N-hydroxycinnamic acid amides and biogenic amines in pepper (Capsicum annuum) flowers. Sci. Hortic. 2006;108:337–341. doi: 10.1016/j.scienta.2006.01.037. [CrossRef] [Google Scholar]
48. Ly D., Kang K., Choi J.Y., Ishihara A., Back K., Lee S.G. HPLC analysis of serotonin, tryptamine, tyramine, and the hydroxycinnamic acid amides of serotonin and tyramine in food vegetables. J. Med. Food. 2008;11:385–389. doi: 10.1089/jmf.2007.514. [PubMed] [CrossRef] [Google Scholar]
Med. Food. 2008;11:385–389. doi: 10.1089/jmf.2007.514. [PubMed] [CrossRef] [Google Scholar]
49. Lavizzari T., Teresa Veciana-Nogues M., Bover-Cid S., Marine-Font A., Carmen Vidal-Carou M. Improved method for the determination of biogenic amines and polyamines in vegetable products by ion-pair high-performance liquid chromatography. J. Chromatogr. A. 2006;1129:67–72. doi: 10.1016/j.chroma.2006.06.090. [PubMed] [CrossRef] [Google Scholar]
50. Foy J.M., Parratt J.R. 5-Hydroxytryptamine in pineapples. J. Pharm. Pharmacol. 1961;13:382–383. doi: 10.1111/j.2042-7158.1961.tb11840.x. [PubMed] [CrossRef] [Google Scholar]
51. Council N.R. Toxicants Occurring Naturally in Foods. National Academy of Sciences; Washington, DC, USA: 1973. [Google Scholar]
52. Feldman J.M., Lee E.M. Serotonin content of foods: Effect on urinary excretion of 5-hydroxyindoleacetic acid. Am. J. Clin. Nutr. 1985;42:639–643. doi: 10.1093/ajcn/42.4.639. [PubMed] [CrossRef] [Google Scholar]
53. Bowden K., Brown B.G., Batty J.E. 5-Hydroxytryptamine: Its occurrence in cowhage. Nature. 1954;174:925–926. doi: 10.1038/174925a0. [PubMed] [CrossRef] [Google Scholar]
Bowden K., Brown B.G., Batty J.E. 5-Hydroxytryptamine: Its occurrence in cowhage. Nature. 1954;174:925–926. doi: 10.1038/174925a0. [PubMed] [CrossRef] [Google Scholar]
54. Engstrom K., Lundgren L., Samuelsson G. Bioassay-guided isolation of serotonin from fruits of Solanum tuberosum L. Acta Pharm. Nord. 1992;4:91–92. [PubMed] [Google Scholar]
55. Kang S., Kang K., Lee K., Back K. Characterization of tryptamine 5-hydroxylase and serotonin synthesis in rice plants. Plant Cell Rep. 2007;26:2009–2015. doi: 10.1007/s00299-007-0405-9. [PubMed] [CrossRef] [Google Scholar]
56. Ramakrishna A., Giridhar P., Sankar K.U., Ravishankar G.A. Melatonin and serotonin profiles in beans of Coffea species. J. Pineal Res. 2012;52:470–476. doi: 10.1111/j.1600-079X.2011.00964.x. [PubMed] [CrossRef] [Google Scholar]
57. Badria F. Melatonin, serotonin, and tryptamine in some egyptian food and medicinal plants. J. Med. Food. 2002;5:153–157. doi: 10.1089/10966200260398189. [PubMed] [CrossRef] [Google Scholar]
58. Collier H.O., Chesher G.B. Identification of 5-hydroxytryptamine in the sting of the nettle (urtica dioica) Br. J. Pharmacol. Chemother. 1956;11:186–189. doi: 10.1111/j.1476-5381.1956.tb01051.x. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Collier H.O., Chesher G.B. Identification of 5-hydroxytryptamine in the sting of the nettle (urtica dioica) Br. J. Pharmacol. Chemother. 1956;11:186–189. doi: 10.1111/j.1476-5381.1956.tb01051.x. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
59. Carnevale G., Di Viesti V., Zavatti M., Zanoli P. Anxiolytic-like effect of Griffonia simplicifolia Baill. seed extract in rats. Phytomedicine. 2011;18:848–851. doi: 10.1016/j.phymed.2011.01.016. [PubMed] [CrossRef] [Google Scholar]
60. Ferreira I.M., Pinho O. Biogenic amines in Portuguese traditional foods and wines. J. Food Prot. 2006;69:2293–2303. doi: 10.4315/0362-028X-69.9.2293. [PubMed] [CrossRef] [Google Scholar]
61. Shalaby A. Significance of biogenic amines to food safety and human health. Food Res. Int. 1996;29:675–690. doi: 10.1016/S0963-9969(96)00066-X. [CrossRef] [Google Scholar]
62. Emmelin N., Feldberg W. Pharmacologically active substances in the fluid of nettle hairs (Urtica urens) J. Physiol. 1947;106:14. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
63. Ough C.S. Measurement of histamine in California wines. J. Agric. Food Chem. 1971;19:241–244. doi: 10.1021/jf60174a038. [PubMed] [CrossRef] [Google Scholar]
64. Bodmer S., Imark C., Kneubuhl M. Biogenic amines in foods: Histamine and food processing. Inflamm. Res. 1999;48:296–300. doi: 10.1007/s000110050463. [PubMed] [CrossRef] [Google Scholar]
65. Latorre-Moratalla M.L., Bover-Cid S., Veciana-Nogues M.T., Vidal-Carou M.C. Control of biogenic amines in fermented sausages: Role of starter cultures. Front. Microbiol. 2012;3:169. doi: 10.3389/fmicb.2012.00169. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
66. Kalac P., Svecova S., Pelikanova T. Levels of biogenic amines in typical vegetable products. Food Chem. 2002;77:349–351. doi: 10.1016/S0308-8146(01)00360-0. [CrossRef] [Google Scholar]
67. Shukla S., Kim J., Kim M. Occurrence of Biogenic Amines in Soybean Food Products. In: El-Shemy H., editor. Soybean and Health.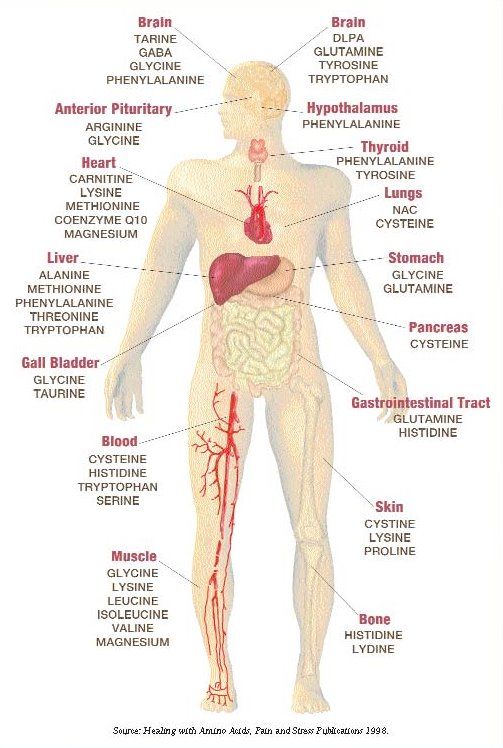 InTech; Shanghai, China: 2011. pp. 189–190. [Google Scholar]
InTech; Shanghai, China: 2011. pp. 189–190. [Google Scholar]
68. Roshchina V.V. The Fluorescence Methods to Study Neurotransmitters (Biomediators) in Plant Cells. J. Fluoresc. 2016;26:1029–1043. doi: 10.1007/s10895-016-1791-6. [PubMed] [CrossRef] [Google Scholar]
69. Stickel F., Droz S., Patsenker E., Bogli-Stuber K., Aebi B., Leib S.L. Severe hepatotoxicity following ingestion of herbalife nutritional supplements contaminated with Bacillus subtilis. J. Hepatol. 2009;50:111–117. doi: 10.1016/j.jhep.2008.08.017. [PubMed] [CrossRef] [Google Scholar]
70. Lyte M. Probiotics function mechanistically as delivery vehicles for neuroactive compounds: Microbial endocrinology in the design and use of probiotics. Bioessays. 2011;33:574–581. doi: 10.1002/bies.201100024. [PubMed] [CrossRef] [Google Scholar]
71. Barrett E., Ross R.P., O’Toole P.W., Fitzgerald G.F., Stanton C. gamma-Aminobutyric acid production by culturable bacteria from the human intestine. J. Appl. Microbiol. 2012;113:411–417. doi: 10.1111/j.1365-2672.2012.05344.x. [PubMed] [CrossRef] [Google Scholar]
2012;113:411–417. doi: 10.1111/j.1365-2672.2012.05344.x. [PubMed] [CrossRef] [Google Scholar]
72. Xu N., Wei L., Liu J. Biotechnological advances and perspectives of gamma-aminobutyric acid production. World J. Microbiol. Biotechnol. 2017;33:64. doi: 10.1007/s11274-017-2234-5. [PubMed] [CrossRef] [Google Scholar]
73. Siragusa S., De Angelis M., Di Cagno R., Rizzello C.G., Coda R., Gobbetti M. Synthesis of gamma-aminobutyric acid by lactic acid bacteria isolated from a variety of Italian cheeses. Appl. Environ. Microbiol. 2007;73:7283–7290. doi: 10.1128/AEM.01064-07. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
74. Moo-Chang K., Seok-Cheol C. Production of GABA (gamma amino butyric acid) by lactic acid bacteria. Korean J. Food Sci. Anim. Resour. 2013;33:377–389. [Google Scholar]
75. Kadir S.A., Wan-Mohtar W., Mohammad R., Lim S., Mohammed A., Saari N. Evaluation of commercial soy sauce koji strains of Aspergillus oryzae for gamma-aminobutyric acid (GABA) production.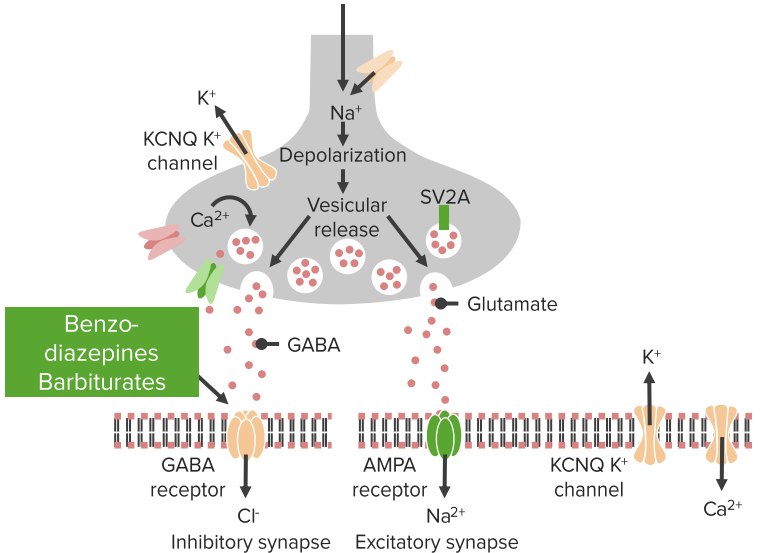 J. Ind. Microbiol. Biotechnol. 2016;43:1387–1395. doi: 10.1007/s10295-016-1828-5. [PubMed] [CrossRef] [Google Scholar]
J. Ind. Microbiol. Biotechnol. 2016;43:1387–1395. doi: 10.1007/s10295-016-1828-5. [PubMed] [CrossRef] [Google Scholar]
76. Nikmaram N., Dar B.N., Roohinejad S., Koubaa M., Barba F.J., Greiner R., Johnson S.K. Recent advances in gamma-aminobutyric acid (GABA) properties in pulses: An overview. J. Sci. Food Agric. 2017;97:2681–2689. doi: 10.1002/jsfa.8283. [PubMed] [CrossRef] [Google Scholar]
77. Asano Y., Hiramoto T., Nishino R., Aiba Y., Kimura T., Yoshihara K., Koga Y., Sudo N. Critical role of gut microbiota in the production of biologically active, free catecholamines in the gut lumen of mice. Am. J. Physiol. Gastrointest. Liver Physiol. 2012;303:G1288–G1295. doi: 10.1152/ajpgi.00341.2012. [PubMed] [CrossRef] [Google Scholar]
78. O’Mahony S.M., Clarke G., Borre Y.E., Dinan T.G., Cryan J.F. Serotonin, tryptophan metabolism and the brain-gut-microbiome axis. Behav. Brain Res. 2015;277:32–48. doi: 10.1016/j.bbr.2014.07.027. [PubMed] [CrossRef] [Google Scholar]
79. Cryan J.F., Dinan T.G. Mind-altering microorganisms: The impact of the gut microbiota on brain and behaviour. Nat. Rev. Neurosci. 2012;13:701–712. doi: 10.1038/nrn3346. [PubMed] [CrossRef] [Google Scholar]
Cryan J.F., Dinan T.G. Mind-altering microorganisms: The impact of the gut microbiota on brain and behaviour. Nat. Rev. Neurosci. 2012;13:701–712. doi: 10.1038/nrn3346. [PubMed] [CrossRef] [Google Scholar]
80. Thomas C.M., Hong T., van Pijkeren J.P., Hemarajata P., Trinh D.V., Hu W., Britton R.A., Kalkum M., Versalovic J. Histamine derived from probiotic Lactobacillus reuteri suppresses TNF via modulation of PKA and ERK signaling. PLoS ONE. 2012;7:e31951. doi: 10.1371/journal.pone.0031951. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
81. Iyer L.M., Aravind L., Coon S.L., Klein D.C., Koonin E.V. Evolution of cell-cell signaling in animals: Did late horizontal gene transfer from bacteria have a role? Trends Genet. 2004;20:292–299. doi: 10.1016/j.tig.2004.05.007. [PubMed] [CrossRef] [Google Scholar]
82. Yunes R.A., Poluektova E.U., Dyachkova M.S., Klimina K.M., Kovtun A.S., Averina O.V., Orlova V.S., Danilenko V.N. GABA production and structure of gadB/gadC genes in Lactobacillus and Bifidobacterium strains from human microbiota.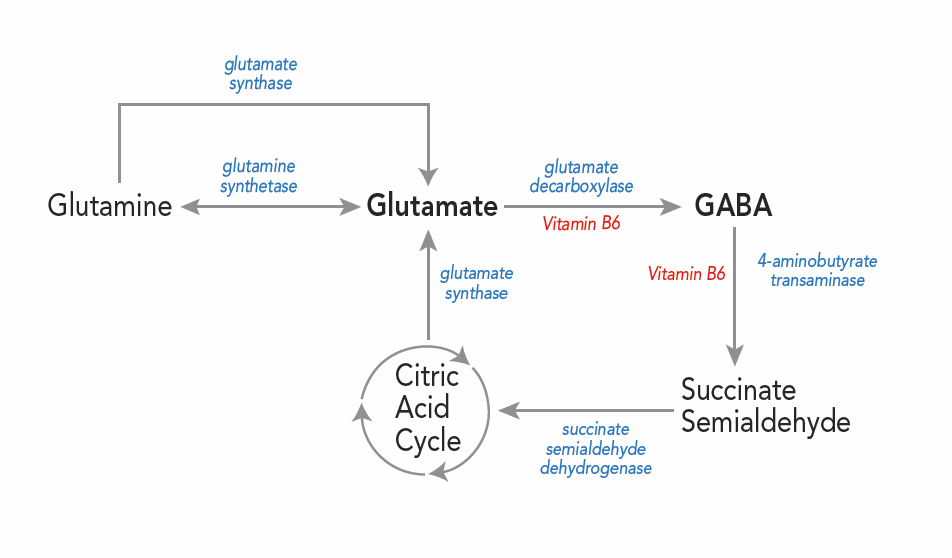 Anaerobe. 2016;42:197–204. doi: 10.1016/j.anaerobe.2016.10.011. [PubMed] [CrossRef] [Google Scholar]
Anaerobe. 2016;42:197–204. doi: 10.1016/j.anaerobe.2016.10.011. [PubMed] [CrossRef] [Google Scholar]
83. Tetel M.J., de Vries G.J., Melcangi R.C., Panzica G., O’Mahony S.M. Steroids, stress and the gut microbiome-brain axis. J. Neuroendocrinol. 2018;30 doi: 10.1111/jne.12548. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
84. Javurek A.B., Spollen W.G., Johnson S.A., Bivens N.J., Bromert K.H., Givan S.A., Rosenfeld C.S. Effects of exposure to bisphenol A and ethinyl estradiol on the gut microbiota of parents and their offspring in a rodent model. Gut Microbes. 2016;7:471–485. doi: 10.1080/19490976.2016.1234657. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
85. Eisenhofer G., Aneman A., Friberg P., Hooper D., Fandriks L., Lonroth H., Hunyady B., Mezey E. Substantial production of dopamine in the human gastrointestinal tract. J. Clin. Endocrinol. Metab. 1997;82:3864–3871. doi: 10.1210/jcem.82.11.4339. [PubMed] [CrossRef] [Google Scholar]
86. Smith T.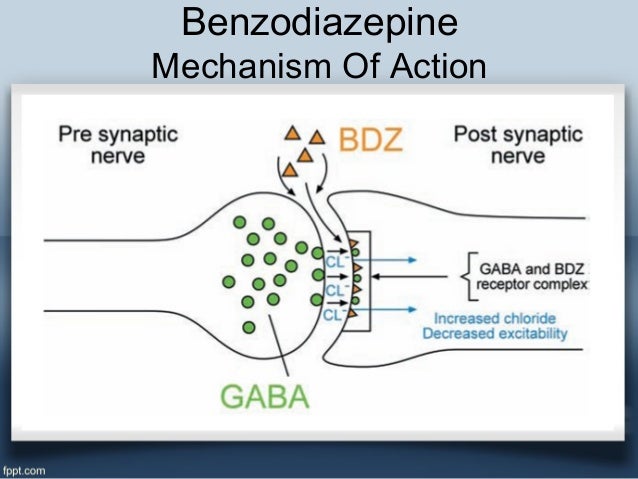 K., Park K.J., Hennig G.W. Colonic migrating motor complexes, high amplitude propagating contractions, neural reflexes and the importance of neuronal and mucosal serotonin. J. Neurogastroenterol. Motil. 2014;20:423–446. doi: 10.5056/jnm14092. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
K., Park K.J., Hennig G.W. Colonic migrating motor complexes, high amplitude propagating contractions, neural reflexes and the importance of neuronal and mucosal serotonin. J. Neurogastroenterol. Motil. 2014;20:423–446. doi: 10.5056/jnm14092. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
87. Abbott N. Inflammatory mediators and modulation of blood-brain barrier permeability. Cell Mol. Neurobiol. 2000;20:131–147. doi: 10.1023/A:1007074420772. [PubMed] [CrossRef] [Google Scholar]
88. Nakatani Y., Sato-Suzuki I., Tsujino N., Nakasato A., Seki Y., Fumoto M., Arita H. Augmented brain 5-HT crosses the blood-brain barrier through the 5-HT transporter in rat. Eur. J. Neurosci. 2008;27:2466–2472. doi: 10.1111/j.1460-9568.2008.06201.x. [PubMed] [CrossRef] [Google Scholar]
89. Young L.W., Darios E.S., Watts S.W. An immunohistochemical analysis of SERT in the blood-brain barrier of the male rat brain. Histochem. Cell Biol. 2015;144:321–329. doi: 10.1007/s00418-015-1343-1.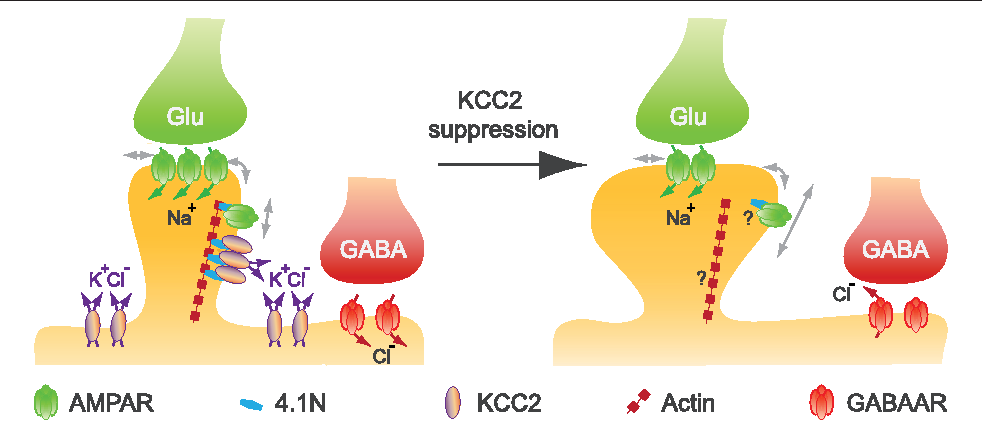 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
[PMC free article] [PubMed] [CrossRef] [Google Scholar]
90. Benarroch E.E. Circumventricular organs: Receptive and homeostatic functions and clinical implications. Neurology. 2011;77:1198–1204. doi: 10.1212/WNL.0b013e31822f04a0. [PubMed] [CrossRef] [Google Scholar]
91. Alstadhaug K. Histamine in migraine and brain. Headache. 2014;54:246–259. doi: 10.1111/head.12293. [PubMed] [CrossRef] [Google Scholar]
92. Konig J., Wells J., Cani P.D., Garcia-Rodenas C.L., MacDonald T., Mercenier A., Whyte J., Troost F., Brummer R.-J. Human Intestinal Barrier Function in Health and Disease. Clin. Transl. Gastroenterol. 2016;7:e196. doi: 10.1038/ctg.2016.54. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
93. Kwok R.H. Chinese-restaurant syndrome. N. Engl. J. Med. 1968;278:796. [PubMed] [Google Scholar]
94. Leussink V.I., Hartung H.P., Stuve O., Kieseier B.C. Vestibular hypofunction after monosodium glutamate ingestion: Broadening the spectrum of ‘Chinese restaurant syndrome’ J.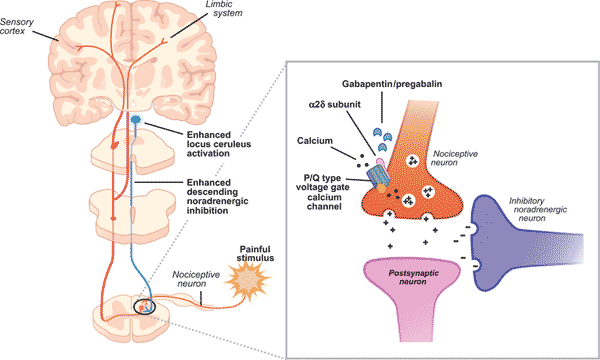 Neurol. 2016;263:1027–1028. doi: 10.1007/s00415-016-8110-7. [PubMed] [CrossRef] [Google Scholar]
Neurol. 2016;263:1027–1028. doi: 10.1007/s00415-016-8110-7. [PubMed] [CrossRef] [Google Scholar]
95. Obayashi Y., Nagamura Y. Does monosodium glutamate really cause headache? A systematic review of human studies. J. Headache Pain. 2016;17:54. doi: 10.1186/s10194-016-0639-4. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
96. Yang W.H., Drouin M.A., Herbert M., Mao Y., Karsh J. The monosodium glutamate symptom complex: Assessment in a double-blind, placebo-controlled, randomized study. (6 Pt 1)J. Allergy Clin. Immunol. 1997;99:757–762. doi: 10.1016/S0091-6749(97)80008-5. [PubMed] [CrossRef] [Google Scholar]
97. Quines C.B., Rosa S.G., Da Rocha J.T., Gai B.M., Bortolatto C.F., Duarte M.M., Nogueira C.W. Monosodium glutamate, a food additive, induces depressive-like and anxiogenic-like behaviors in young rats. Life Sci. 2014;107:27–31. doi: 10.1016/j.lfs.2014.04.032. [PubMed] [CrossRef] [Google Scholar]
98. Hawkins R.A., O’Kane R.L., Simpson I.A., Vina J.R.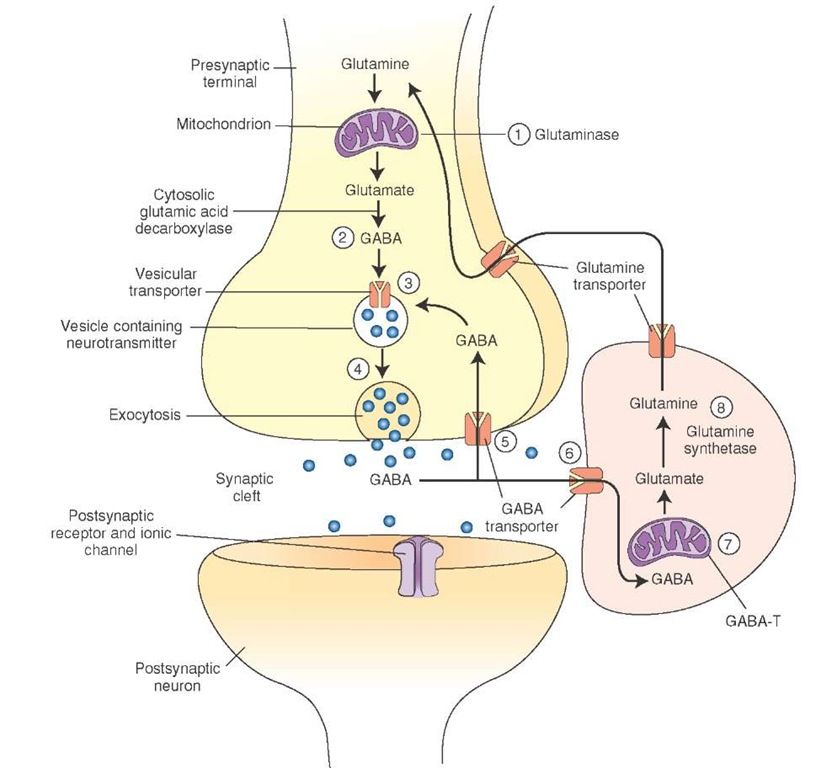 Structure of the blood-brain barrier and its role in the transport of amino acids. J. Nutr. 2006;136(Suppl. S1):218S–226S. doi: 10.1093/jn/136.1.218S. [PubMed] [CrossRef] [Google Scholar]
Structure of the blood-brain barrier and its role in the transport of amino acids. J. Nutr. 2006;136(Suppl. S1):218S–226S. doi: 10.1093/jn/136.1.218S. [PubMed] [CrossRef] [Google Scholar]
99. Okita Y., Nakamura H., Kouda K., Takahashi I., Takaoka T., Kimura M., Sugiura T. Effects of vegetable containing gamma-aminobutyric acid on the cardiac autonomic nervous system in healthy young people. J. Physiol. Anthropol. 2009;28:101–107. doi: 10.2114/jpa2.28.101. [PubMed] [CrossRef] [Google Scholar]
100. Takanaga H., Ohtsuki S., Hosoya K., Terasaki T. GAT2/BGT-1 as a system responsible for the transport of gamma-aminobutyric acid at the mouse blood-brain barrier. J. Cereb. Blood Flow Metab. 2001;21:1232–1239. doi: 10.1097/00004647-200110000-00012. [PubMed] [CrossRef] [Google Scholar]
101. Maintz L., Novak N. Histamine and histamine intolerance. Am. J. Clin. Nutr. 2007;85:1185–1196. doi: 10.1093/ajcn/85.5.1185. [PubMed] [CrossRef] [Google Scholar]
102. Sharma S., Zhuang Y.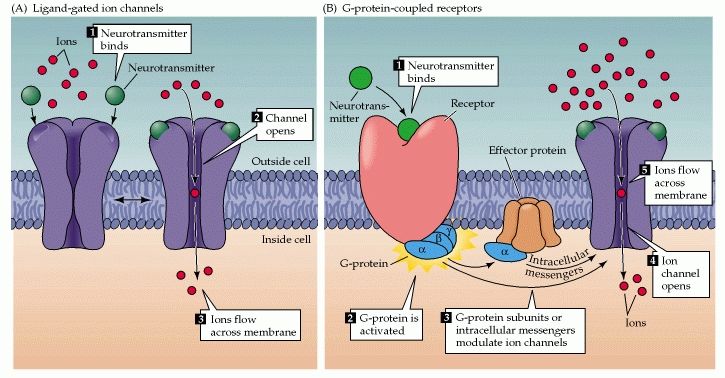 , Gomez-Pinilla F. High-fat diet transition reduces brain DHA levels associated with altered brain plasticity and behaviour. Sci. Rep. 2012;2:431. doi: 10.1038/srep00431. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
, Gomez-Pinilla F. High-fat diet transition reduces brain DHA levels associated with altered brain plasticity and behaviour. Sci. Rep. 2012;2:431. doi: 10.1038/srep00431. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
103. Peters S.L., Biesiekierski J.R., Yelland G.W., Muir J.G., Gibson P.R. Randomised clinical trial: Gluten may cause depression in subjects with non-coeliac gluten sensitivity—An exploratory clinical study. Aliment. Pharmacol. Ther. 2014;39:1104–1112. doi: 10.1111/apt.12730. [PubMed] [CrossRef] [Google Scholar]
104. Garcia-Lopez R., Perea-Milla E., Garcia C.R., Rivas-Ruiz F., Romero-Gonzalez J., Moreno J.L., Faus V., del Castillo Aguas G., Ramos Diaz J.C. New therapeutic approach to Tourette Syndrome in children based on a randomized placebo-controlled double-blind phase IV study of the effectiveness and safety of magnesium and vitamin B6. Trials. 2009;10:16. doi: 10.1186/1745-6215-10-16. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
105. Belzeaux R., Annweiler C., Bertrand J.A., Beauchet O., Pichet S., Jollant F., Turecki G., Richard-Devantoy S. Association between hypovitaminosis D and cognitive inhibition impairment during major depression episode. J. Affect. Disord. 2017;225:302–305. doi: 10.1016/j.jad.2017.08.047. [PubMed] [CrossRef] [Google Scholar]
Belzeaux R., Annweiler C., Bertrand J.A., Beauchet O., Pichet S., Jollant F., Turecki G., Richard-Devantoy S. Association between hypovitaminosis D and cognitive inhibition impairment during major depression episode. J. Affect. Disord. 2017;225:302–305. doi: 10.1016/j.jad.2017.08.047. [PubMed] [CrossRef] [Google Scholar]
106. Pardridge W.M. Blood-brain barrier biology and methodology. J. Neurovirol. 1999;5:556–569. doi: 10.3109/13550289909021285. [PubMed] [CrossRef] [Google Scholar]
107. Logan A.C., Jacka F.N. Nutritional psychiatry research: An emerging discipline and its intersection with global urbanization, environmental challenges and the evolutionary mismatch. J. Physiol. Anthropol. 2014;33:22. doi: 10.1186/1880-6805-33-22. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
108. Institute of Food Technologists Foundation (IFT) Making Decisions about the Risks of Chemicals in Foods with Limited Scientific Information. Institute of Food Technologists Foundation; Chicago, IL, USA: 2009. [Google Scholar]
[Google Scholar]
109. Roshchina V.V., Bezuglov V.V., Markova L.N., Sakharova N.Y., Buznikov G.A., Karnaukhov V.N., Chailakhyan L.M. Interaction of living cells with fluorescent derivatives of biogenic amines. Dokl. Biochem. Biophys. 2003;393:346–349. doi: 10.1023/B:DOBI.0000010300.50906.68. [PubMed] [CrossRef] [Google Scholar]
110. Briguglio M., Dina C.Z., Servello D., Porta M. Tourette Syndrome and Nutritional Implications; Proceedings of the Annual Meeting of the European Society for the Study of Tourette Syndrome—9th European Conference on Tourette Syndrome and Tic Disorders; Warsaw, Poland. 9–10 June 2016. [Google Scholar]
GABA (GABA) what it is, how it works and what are the benefits
Contents:
➦ What is gamma-aminobutyric acid (GABA)
➦ How does GABA work?
➦ What are the benefits of GABA?
➦ GABA for athletes
➦ Gamma aminobutyric acid deficiency symptoms
➦ How to increase the level of Gamma?
➦ What is gamma-aminobutyric acid?
➦ The most popular GABA supplements in Phytomarket
➦ GABA in food products
➦ Gaba tea as a source of acid
➦ How to take a GABA supplement
➦ Side effects of GABA
➦ Frequently asked questions answered
Gamma-aminobutyric acid preparations are becoming increasingly popular among natural remedies with anti-stress properties.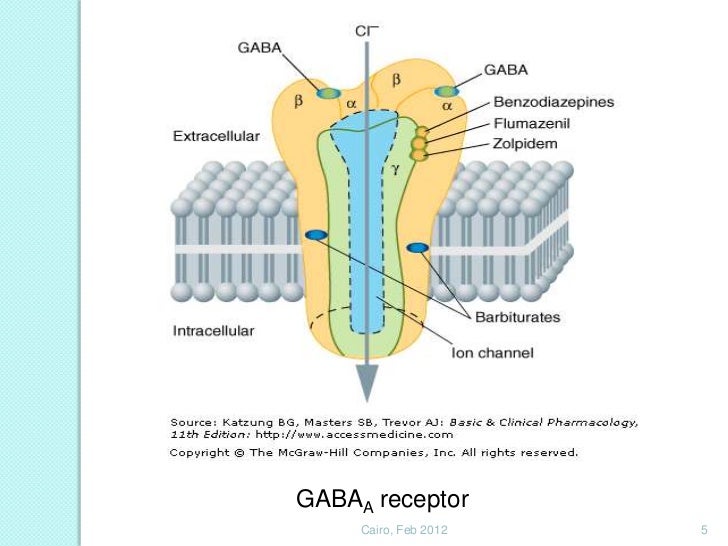 They are able to eliminate anxiety and improve sleep, they are also in demand in sports practice to enhance the growth of muscle mass. Learn about the benefits of this substance for the body and how it can be used in everyday life.
They are able to eliminate anxiety and improve sleep, they are also in demand in sports practice to enhance the growth of muscle mass. Learn about the benefits of this substance for the body and how it can be used in everyday life.
What is gamma-aminobutyric acid (GABA)
Gamma-aminobutyric acid (chemical formula C4H9NO2) or GABA is an organic substance that is synthesized by the body and is present in all areas of the brain. It is the main inhibitory neurotransmitter in the central nervous system, that is, it slows down the transmission of nerve impulses, and competes with glutamate, the main excitatory neurotransmitter, affecting approximately 30-40% of synaptic connections. In nature, this substance is present in some plants, such as valerian or green tea.
Neurotransmitters influence our thoughts, feelings, sensations. An imbalance between the main neurotransmitters (serotonin, dopamine, GABA and acetylcholine) can manifest itself in various psychological disorders.
The main task of GABA is to block unnecessary information flows to create parity between the processes of excitation and inhibition in our brain, providing functions such as attention, motor and emotional control.
Gamma-aminobutyric acid receptors are found in high concentration in the cerebellum, thalamus and spinal cord. Moreover, recent studies have shown that GABA molecules are also present in the walls of the uterus, spermatozoa, retina, lungs and respiratory tract, as well as in the insulin-producing beta cells of the pancreas.
A bit of history
The presence of GABA in the brain became known in 1950, when the American scientist Eugene Roberts, while studying free amino acids, came across a compound whose migration on paper chromatograms did not correspond to any compound containing known amino acids. He drew attention to the presence of this substance in various tissues of the central nervous system: the brain, cerebellum and spinal cord of vertebrates and suggested a direct or indirect connection with the conduction of nerve signals. 7 years later, researchers in Canada reported that the unknown compound with neuronal inhibitory activity was GABA. A number of subsequent discoveries have determined its role in our brain.
7 years later, researchers in Canada reported that the unknown compound with neuronal inhibitory activity was GABA. A number of subsequent discoveries have determined its role in our brain.
How does GABA work?
GABA is an amino acid that occurs as a result of processes occurring in different cells and, above all, in nerve cells. The "chemistry" of the brain is such that the main brake for the mediator - gamma-aminobutyric acid is a product of the main excitatory neurotransmitter - glutamate, which produces it under the action of the enzyme glutamate decarboxylase (GAD), and vitamin B6 acts as a cofactor. It all happens in a part of the brain called the hippocampus. Maintaining a balance between these two neurotransmitters is a key condition for physical and mental health, as well as good mood. A low level of GABA leads to the development of anxiety, depression, impairs concentration, attention, and some cognitive functions.
To understand the role of GABA, it is important to know how it interacts with its receptor. When GABA binds to the GABA receptor, the latter changes shape slightly, allowing ions to pass through its central channel. This leads to a decrease in the excitability of the neuron, which is why GABA is called an inhibitory neurotransmitter.
When GABA binds to the GABA receptor, the latter changes shape slightly, allowing ions to pass through its central channel. This leads to a decrease in the excitability of the neuron, which is why GABA is called an inhibitory neurotransmitter.
Getting into the brain from food, supplements or drugs, GABA becomes not just an additional inhibitory neurotransmitter, but also food for neurons, as it is captured by mitochondria. In neurons, it performs two tasks: about 1% of the substance works as a neurotransmitter, and 99% provides energy exchange in mitochondria during ATP synthesis and glucose breakdown. This substance stimulates metabolism, saturates the brain with oxygen and improves blood circulation throughout the body.
What are the benefits of GABA?
The main function of gamma-aminobutyric acid is to reduce the neural activity of the neurons to which it attaches. It prevents long-term activation of neurons and also plays a neurotrophic role by promoting the growth of certain neurons.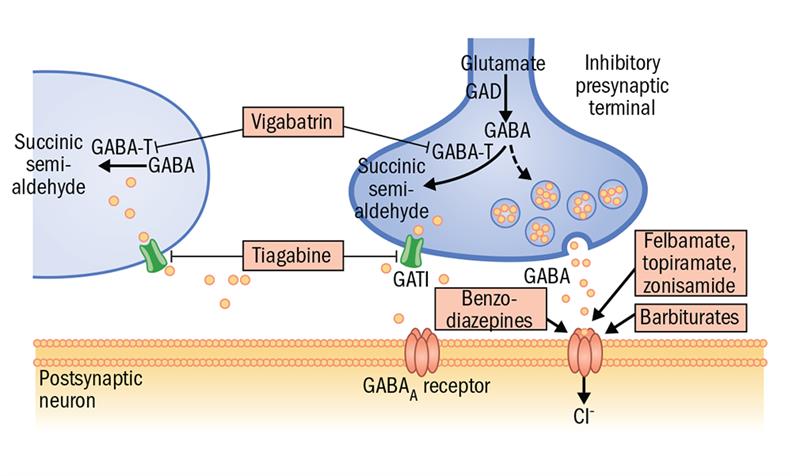
The main functions of the GABA:
- Regulation by motor activity
- Providing memory and thinking processes
- Anti -icing effect
- Activation of energy processes
- Acceleration exchange.
The inhibitory effects of GABA serve to counteract the excitatory (activator) effects of glutamate. Indeed, when the brain is overexcited, it can contribute to feelings of restlessness, irritability, and even insomnia. Taking GABA helps to correct the imbalance associated with anxiety, has a relaxing and sedative effect. It is also associated with better sleep quality, allowing you to switch off, helping you fall asleep faster.
GABA plays a stabilizing role on a mental and physical level, helping to restore balance and maintain normal mood. This substance is involved in certain stages of memory and can be used to relax, control fear or anxiety, which manifests itself in overexcitation.
GABA has been scientifically proven to significantly stimulate growth hormone (HGH = Human Growth Hormone) secretion during the early stages of deep sleep.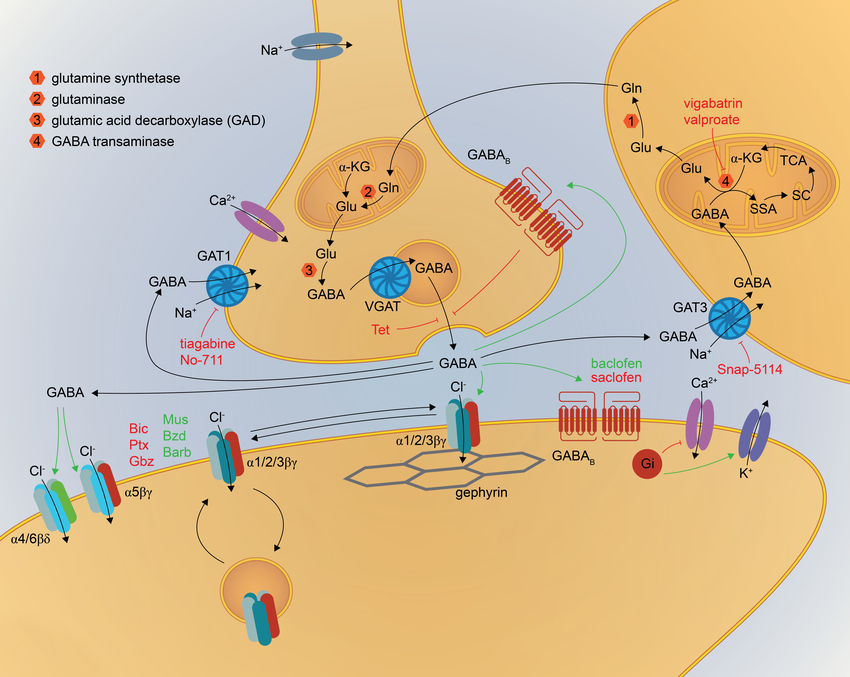 Growth hormone is one of the muscle growth hormones in the human body. It helps to reduce body fat and stimulates muscle growth. GABA acts on certain chains of neurons that stimulate the hypothalamus so that more growth hormones are released. This ability is highly valued by athletes.
Growth hormone is one of the muscle growth hormones in the human body. It helps to reduce body fat and stimulates muscle growth. GABA acts on certain chains of neurons that stimulate the hypothalamus so that more growth hormones are released. This ability is highly valued by athletes.
Based on GABA, nootropics are produced - drugs that improve the higher functions of the human brain. They are widely used in the treatment of strokes, brain injuries, age-related changes, when the performance of the brain is significantly reduced. The advantages of nootropics over other drugs that affect synaptic activity are that they do not cause addiction and dependence, unlike psychomotor stimulants and antipsychotics. And because GABA is an inhibitory neurotransmitter, it is widely used in the treatment of epilepsy.
Thus, tableted gamma-aminobutyric acid contributes to the overall strengthening of the nervous system, in particular, such brain functions as thinking, perception and attention.
GABA receptors are located, among other things, in the hypothalamus, which controls circadian rhythms and is directly related to sleep. Many insomnia medications, as well as their herbal counterparts, raise GABA levels, thereby improving the quality of sleep.
What are the benefits of GABA?
Thanks to numerous studies, today GABA is officially recognized as an effective cytoprotective antihypoxant and antioxidant for various organs and systems. She is credited with antitumor and anti-inflammatory properties, as well as the ability to positively influence the functioning of the immune system.
The effect of GABA on sleep is especially noticeable. Under its influence, mental excitation decreases, the energy processes of the brain are activated, the respiratory activity of tissues and glucose utilization improve, which leads to high-quality deep sleep.
GABA action on the body:
- Promises to calm and relax
- controls “panic” conditions associated with anxiety
- reduces muscle tone
- reduces cramps
- , reduces muscle ceremonials
- normalizes blood pressure
- helps control anxiety
- promotes quality sleep
- reduces blood sugar levels
- improves overall immunity
- accelerates the recovery process after injuries
- improves sexual activity
GABA preparations are used to treat mental retardation, cerebral palsy, post-stroke conditions, and also restore brain function after injuries. Taking GABA supplements is appropriate for high mental, physical and psychological stress. They help to normalize the work of the brain, cope with stress.
Taking GABA supplements is appropriate for high mental, physical and psychological stress. They help to normalize the work of the brain, cope with stress.
GABA for athletes
Many professional athletes today recognize the benefits of GABA for athletic performance. The advantage of sports nutrition based on it is high efficiency in the absence of a hormonal component. Acting on the anterior pituitary gland of the brain, GABA stimulates the production of growth hormone, which increases the growth of muscle tissue and reduces the percentage of body fat. This is especially important for bodybuilders and athletes.
The advantages of a margin for athletes:
➦ Raises the content of growth hormone by 4-6 times, being a safe alternative to steroids
➦ stimulates the production of somatotropin even after training
➦ participates in the process of fat-burning, contributing to a faster
➦ helps to quickly achieve a beautiful relief body
➦ normalizes the functioning of the nervous system
➦ eliminates insomnia, improves sleep
➦ accelerates recovery after injuries: dislocations and sprains.
GABA supplements are consistently in high demand among professional athletes and amateurs, which is the best confirmation of their high effectiveness. Single negative reviews are associated with the incorrect use of drugs with GAB or a violation of the training process.
It is important to remember that all dietary and sports supplements are taken in a certain dosage, courses, after consultation with a doctor.
Gamma aminobutyric acid (GABA) deficiency symptoms
GABA is synthesized naturally by the body. When its level in the body is sufficient, we experience peace and well-being. With a deficiency of GABA, there is an imbalance between the processes of excitation and inhibition, which leads to disturbances in the functioning of the nervous system: from increased anxiety and irritability to insomnia. Low levels of this neurotransmitter cause difficulty falling asleep despite being tired, as well as restlessness, recurring muscle or neuropathic pain, and a tendency to be irritable. In children, this manifests itself in the form of hyperactivity, attention deficit disorder, problems with perseverance and attention.
In children, this manifests itself in the form of hyperactivity, attention deficit disorder, problems with perseverance and attention.
Here are some of the symptoms indicating a marriage deficiency:
✔ Nervousness and inability to concentrate
✔ periodically occurring Tremor
✔ Frequent breathing difficulties
✔ Strong sweating
,✔ Fatigue even after a good night sleep
✔ mood swings
✔ mental confusion
The most severe case, which is associated with a lack of γ-aminobutyric acid, is epilepsy. This neurological disease is caused by the fact that as a result of malformations or brain tumors, a huge wave of excitation periodically occurs in some of its areas (most often in the local area), which leads to an epileptic seizure. Using preparations containing GABA, it is possible to enhance the work of the GABA system by suppressing the activity of the excitatory neurotransmitter.
Deficiency cases for which GABA is recommended:
✔ Trouble falling asleep due to nervousness and anxiety
✔ Inability to relax
✔ Constant feeling of physical tension
✔ Mood and behavior disorder
How to increase the level of Gamk?
In a healthy body with a balanced diet and a proper lifestyle, the production of gamma-aminobutyric acid is regulated independently, but bad habits, stress and certain diseases can provoke its deficiency. GABA is naturally present in plants, but it is primarily synthesized endogenously by our bodies from glutamic acid.
GABA is naturally present in plants, but it is primarily synthesized endogenously by our bodies from glutamic acid.
Restore the GABA balance in the body will help the consumption of food or special supplements containing gamma-aminobutyric acid, as well as glutamine, since GABA is its derivative. This substance is found in animal proteins: eggs, white meat, legumes such as lentils or chickpeas, leafy vegetables such as spinach and parsley. And to turn it into GABA, it is important to take supplements with vitamin B6 and magnesium.
Some plant extracts may also interfere with GABA production. For example, lemon balm is a transaminase inhibitor, and consuming it increases GABA levels in the brain, as it will be less degraded. GABA stimulants include: inositol, glutamic acid, melatonin (at night), thiamine (vitamin B1), niacinamide (vitamin B3), pyridoxine, valerian, passionflower 200–1000 mg.
| Connection name | What does it contain |
| Inositol, a sugar normally synthesized by the body | fruits, vegetables, legumes, seeds, oilseeds |
| Branched-chain amino acids (leucine) | turkey meat, spirulina, beans, pistachios, whey |
| Isoleucine | nuts of all kinds, seeds, lentils, rye, eggs, chicken |
| Valine | peanuts, mushrooms, soybeans, lupins, parmesan, all kinds of seeds |
| Arginine | pumpkin seeds and peanuts |
| Coenzyme Q10 | spinach, broccoli and cauliflower |
| Ribose | mushrooms |
| vitamin C | Brussels sprouts, bell peppers and citrus fruits |
| All B vitamins, including B6. | nuts (especially walnuts), tomatoes, potatoes, cabbage, cereals, citrus fruits, berries |
The following measures will help to stimulate the production of GABA:
+ good rest
+ breathing techniques to reduce stress
+ meditation practices
+ physical activity
What is GABA?
GABA is found naturally in foods such as chestnuts, potatoes, rice, astragalus, fresh leaves of selected teas from which natural GABA extracts are obtained.
It is also found in medications and supplements for anxiety, anxiety, blood pressure and sleep, and sports nutrition for athletes and bodybuilders.
Studies have shown that with long-term use of products and preparations with gamma-aminobutyric acid, it is possible to raise its level in the body to the optimum.
The most popular GABA supplements in Phytomarket
More items in Vitamins for the nervous system!
GABA in food
Foods rich in gamma-aminobutyric acid include:
| Food | Quantitative content of GABA per 100 g |
| Gaba tea | 150-400 mg |
| Tomatoes (depending on variety), sauerkraut, fermented soybeans | to 63 mg |
| Germinated rice, especially anoxic fermented in nitrogen | 25. |
| Eggplant | 20 mg |
| Potato | 16 to 35 mg |
| Grapefruits | 23 mg |
| Peaches | 13 mg |
| Kiwi | 11 mg |
| Oranges | 11.5 mg |
| Carrot | 10 mg |
| Shiitake mushrooms | 8 mg |
| Green soybeans | 6 mg |
| Beets | 4 to 8 mg |
Based on this table, we can conclude that the most complete natural source of GABA is Gaba tea.
Gaba tea as a source of acid
Gaba Tea is a unique product produced in the north of Taiwan. Now he is at the peak of popularity. Due to its richness in GABA molecules, it has a large list of benefits for human health. Among them: support for memory, relaxation, fighting stress and depression, building muscle mass and delaying aging. Studies have shown that regular consumption of Gaba tea helps reduce blood pressure, boost immunity, and improve sexual function.
Gaba is not a type of tea, but a special oxygen-free fermentation technology that releases gamma-aminobutyric acid. The origins of this unusual drink are the Japanese. In the late 1980s, a team at the National Tea Experiment Station, led by Dr. Tsushima Tojiro, experimentally determined that fresh tea leaves release large amounts of GABA during fermentation in the absence of oxygen.
It is believed that unlike synthetic GABA, which hardly crosses the protective blood-brain barrier to access the brain, the gamma-aminobutyric acid contained in the natural tea leaf is absorbed much better.
Today, Taiwan is the world's largest producer and supplier of Gaba tea. The delicious taste, as well as the extraordinary health benefits, have earned Taiwanese Gaba tea a prominent place in catalogs of exceptional teas.
How much Gamma in tea?
The largest plant source of GABA is the Taiwanese version of Oolong tea. 100 g of the product contains 150-400 mg of gamma-aminobutyric acid.
How is Gaba tea made?
High quality fresh leaves are used in the production, which are placed under vacuum in sealed bags and kept at a temperature of at least 40 ˚C for about 8 hours. Then they are taken out into the air and shaken thoroughly for several minutes. This cycle is repeated 5 times with slight variations in air exposure time between vacuum steps. This anaerobic reaction develops the natural potential of gamma-aminobutyric acid in the leaves, and also provides a rich fruity taste of tea: baked apple with hints of cinnamon and nutmeg.
How to brew Gaba tea?
To make Gaba tea not only healthy, but also tasty, you need to brew it properly.
Proceed as follows :
- Boil water
- Preheat the kettle with hot water
- Put 7 grams of tea (approximately 1.5-2 tablespoons), fill with hot water and immediately drain (rinsing tea) 906 6 again and wait about 10 seconds
- Repeat the previous step several times, increasing the steeping time by 10-20 seconds.
How to take for sleep?
As a remedy for insomnia, Gaba tea is best consumed at least 2-3 hours before bedtime.
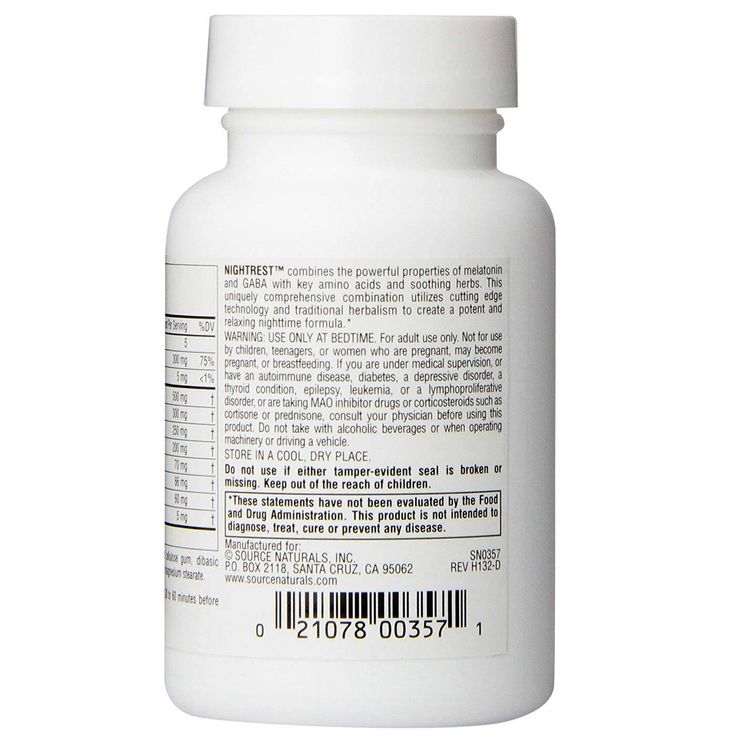
How to take GABA supplement
The positive effect of GABA intake is observed when taking at least 2g / day after about a week. It is recommended to start with 0.5 g - 1 g per day, gradually increasing the dose to 4 g. Small doses of the supplement do not work, since only a small part of the substance penetrates the brain.
It is best to take a GABA supplement before bed or after a workout on an empty stomach with water or juice, but not in the morning, as this may affect performance. The course is at least 1 month. A break while taking GABA is not regulated.
It is desirable to combine the use of GABA with the intake of vitamin B6. In case of its shortage, sleep disturbance, nervousness and other unpleasant symptoms may occur. In addition to B6, GABA can be taken along with 5-HTP, as well as magnesium and zinc, which are responsible for activating GABA receptors.
Side effects of GABA
GABA has very few side effects. In very rare cases, tingling on the skin may be felt, even less often: nausea, vomiting, insomnia, fluctuations in blood pressure (during the first days of treatment), dyspepsia, hyperthermia, a feeling of heat. Such side effects may be associated with individual intolerance.
On the other hand, the simultaneous use of GABA and anxiolytics may be associated with an increased risk of sedation, so it is important to consult a doctor in advance.
Overdose of drugs that inhibit GABA reuptake can cause an excess of GABA, which is manifested by neurological and psychiatric symptoms: memory loss, convulsions, hallucinations and cognitive impairment.
Contraindications to the use of GABA drugs are hypersensitivity, children under 1 year of age, acute renal failure, pregnancy and lactation.
Answers to popular questions:
When is the best time to drink GABA?
Best GABA supplement to take before bed or after workout
How much GABA to take?
It is recommended to start with 0.5 g - 1 g per day, gradually increasing the dose to 4 g. For a noticeable effect, take the supplement for at least 1 month. Break while taking GABA is not regulated
Where are GABA receptors located?
Neurons carrying receptors for GABA molecules can be found in almost any area of the brain.
How long will it take to see a noticeable result?
Noticeable improvement can be seen as early as a week after taking a GABA supplement.
Brewer's yeast: real benefit or harm? Isotonic for athletes and not only. Everything you need to know about drink
features and characteristics! Overview Foods-Body.ua
Topics of articles
- Amino acids
- Antioxidants
- Dietary supplements (biological supplements)
- vitamins
- For weight loss
- For joints and ligaments
- Meal Replacements
- Creatine
- Massagers
- Nutrition and training
- Pre-workouts
- Medications that increase testosterone
- natural extracts
- Fish oil and omega
- Special preparations
- simulators
- About manufacturers
Foods-body
Gamma-aminobutyric acid or simply GABA is a chemical compound from the group of amino acids that does not have proteins in its structure.
This is a natural substance synthesized in the human body from the amino acid glutamine. The first studies, during which aminobutyric acid was identified, were carried out as early as 1954-1956. Then it was only possible to determine its presence in the human central nervous system. It was possible to complete the synthesis of the substance in question only in 1963 year.
The main task of this compound is that it inhibits the transmission of certain impulses and relaxes the nervous system. It helps a person return to a calm, stable state and quickly get out of depression or stress.
In a normal state, the production of a substance is independently regulated in the human body, but bad habits or any shocks can provoke a failure. That is why it is important to maintain the level of gaba in the body through proper nutrition or by taking special nutritional supplements based on this component.
Benefits of gamma-aminobutyric acid (GABA)
GABA is one of the most important inhibitory neurotransmitters in the nervous system. It is widely used in medical practice, as it is an effective assistant in the treatment of mental disorders, and also has a relaxing and sedative effect. The substance activates metabolic processes, saturates the brain with oxygen and improves blood circulation throughout the body.
Constant stress and anxiety are known to weaken the immune system, they are also often accompanied by sleep disturbance, which in turn also negatively affects the functioning of the immune system. GABA helps reduce stress and promote a healthy immune response to stressors.
The compound plays an important role in ensuring a good night's rest, it improves the quality of sleep, and its lack is one of the main causes of insomnia.
In addition, it regulates motor activity, improves memory and thinking processes, and also has an anticonvulsant effect. Being one of the most important components of the blood and the brain, gamma-aminobutyric acid is able to improve the blood supply to the brain, activate energy processes and increase the respiratory activity of tissues. In addition, it accelerates the utilization of glucose and helps to remove toxic metabolic products.
Speaking of other equally important effects that the product in question has on the body, we can highlight the following:
• helps in the fight against vascular pathologies;
• normalizes blood pressure;
• improves liver function;
• relieves nervous tension;
• relieves negative symptoms of stress;
• has a positive effect on the state of the nervous system as a whole;
• has a relaxing effect;
• speeds up the process of falling asleep;
• increases the body's resistance to stressful situations;
• normalizes the functioning of the cardiovascular system;
• increases the ability to concentrate;
• Supports optimal brain function in old age.
Who needs additional intake of GABA
Most often, gamma-aminobutyric acid is used as an additional agent in the treatment of diseases such as epilepsy, arterial hypertension, endogenous depression, atherosclerosis.
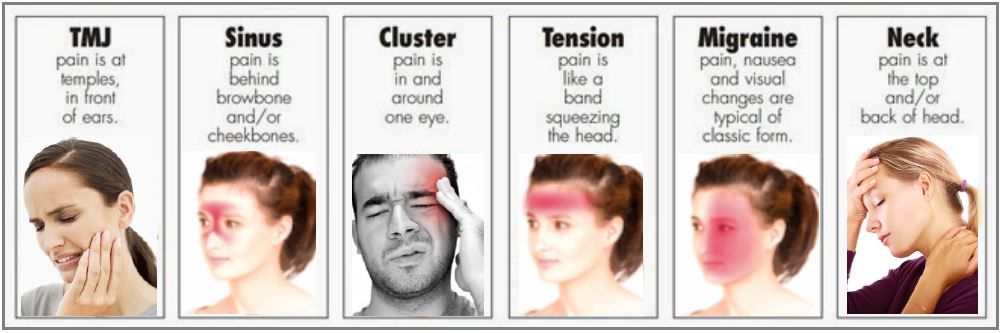
It can also bring undeniable benefits to patients recovering from traumatic brain injury. In addition, GABA can help people who experience problems with sexual function and those who often suffer from headaches and dizziness.
It is recommended to use the product additionally for babies who are lagging behind in development and for those who have disorders in the functioning of the speech apparatus.
What role does GABA play in the lives of athletes
For bodybuilders and people involved in various sports, this product is of particular interest. This is due to the fact that it helps to increase somatotropin or growth hormone, which in turn has an anabolic and fat-burning effect. Due to the increased level of somatotropin, muscle mass gain is accelerated, strength indicators increase, and the process of burning subcutaneous fat is activated.
A very important benefit of supplements based on this component for athletes is that they help to fall asleep faster and deepen sleep.
Thus, the restoration of muscle fibers damaged during physical exertion is much faster and more efficient. Among other things, the substance in question is able to prevent muscle cramps and reduce the level of cortisol or the stress hormone, which enhances catabolic processes in the muscles.
The main symptoms of GABA deficiency
People who have a lack of this compound cannot work productively during the daytime, and they also have problems with sleep, a feeling of anxiety and unreasonable aggression.
Other signs of deficiency include:
• panic attacks;
• trouble concentrating;
• persistent headaches;
• poor resistance to stress;
• inability to calm down;
• increased night sweats;
• constant fatigue;
• visual impairment.
Deficiencies in this compound can be replenished either through regular dietary intake or by supplementing with GABA in tablet, capsule, or powder form.