Someone with schizophrenia
Schizophrenia - Symptoms and causes
Overview
Schizophrenia is a serious mental disorder in which people interpret reality abnormally. Schizophrenia may result in some combination of hallucinations, delusions, and extremely disordered thinking and behavior that impairs daily functioning, and can be disabling.
People with schizophrenia require lifelong treatment. Early treatment may help get symptoms under control before serious complications develop and may help improve the long-term outlook.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
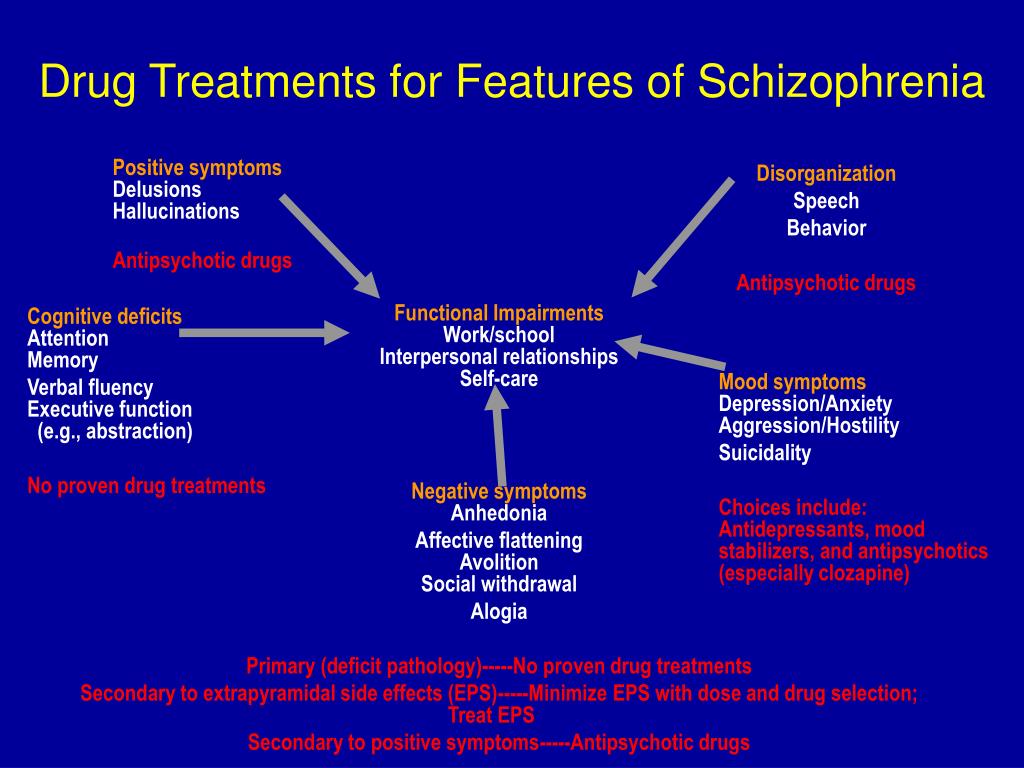
Schizophrenia involves a range of problems with thinking (cognition), behavior and emotions. Signs and symptoms may vary, but usually involve delusions, hallucinations or disorganized speech, and reflect an impaired ability to function. Symptoms may include:
- Delusions. These are false beliefs that are not based in reality.
For example, you think that you're being harmed or harassed; certain gestures or comments are directed at you; you have exceptional ability or fame; another person is in love with you; or a major catastrophe is about to occur. Delusions occur in most people with schizophrenia.
- Hallucinations. These usually involve seeing or hearing things that don't exist. Yet for the person with schizophrenia, they have the full force and impact of a normal experience. Hallucinations can be in any of the senses, but hearing voices is the most common hallucination.
- Disorganized thinking (speech). Disorganized thinking is inferred from disorganized speech. Effective communication can be impaired, and answers to questions may be partially or completely unrelated. Rarely, speech may include putting together meaningless words that can't be understood, sometimes known as word salad.
- Extremely disorganized or abnormal motor behavior.
 This may show in a number of ways, from childlike silliness to unpredictable agitation. Behavior isn't focused on a goal, so it's hard to do tasks. Behavior can include resistance to instructions, inappropriate or bizarre posture, a complete lack of response, or useless and excessive movement.
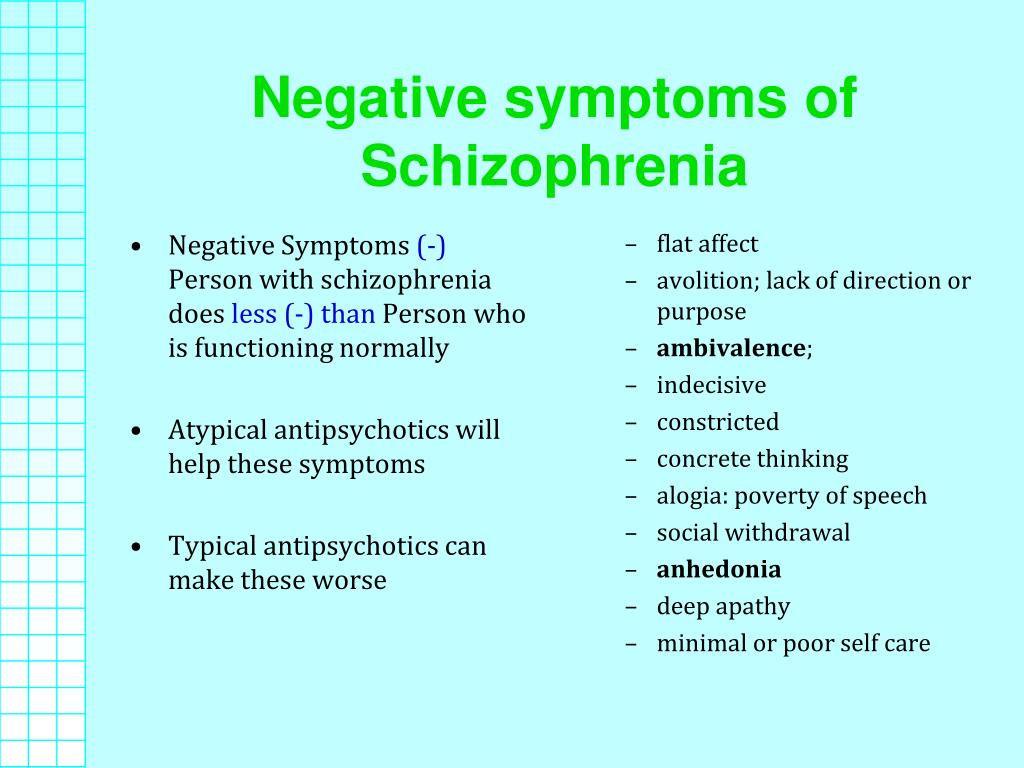
This may show in a number of ways, from childlike silliness to unpredictable agitation. Behavior isn't focused on a goal, so it's hard to do tasks. Behavior can include resistance to instructions, inappropriate or bizarre posture, a complete lack of response, or useless and excessive movement. - Negative symptoms. This refers to reduced or lack of ability to function normally. For example, the person may neglect personal hygiene or appear to lack emotion (doesn't make eye contact, doesn't change facial expressions or speaks in a monotone). Also, the person may lose interest in everyday activities, socially withdraw or lack the ability to experience pleasure.
Symptoms can vary in type and severity over time, with periods of worsening and remission of symptoms. Some symptoms may always be present.
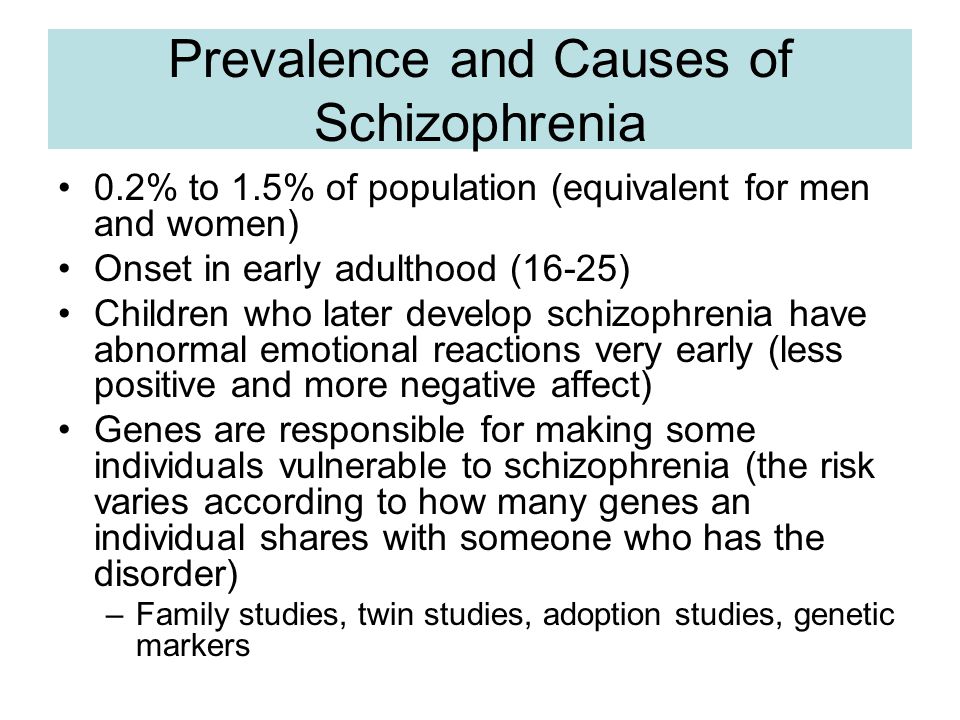
In men, schizophrenia symptoms typically start in the early to mid-20s. In women, symptoms typically begin in the late 20s. It's uncommon for children to be diagnosed with schizophrenia and rare for those older than age 45.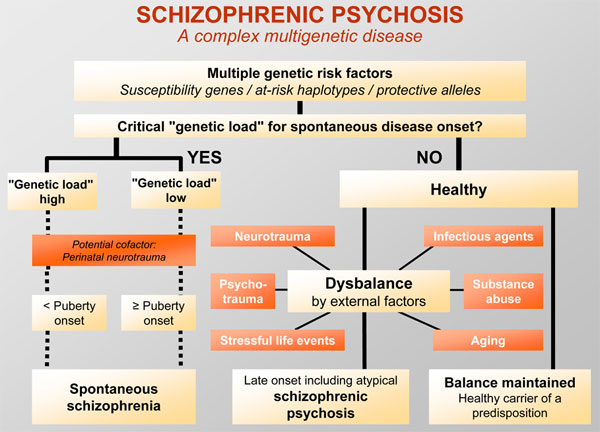
Symptoms in teenagers
Schizophrenia symptoms in teenagers are similar to those in adults, but the condition may be more difficult to recognize. This may be in part because some of the early symptoms of schizophrenia in teenagers are common for typical development during teen years, such as:
- Withdrawal from friends and family
- A drop in performance at school
- Trouble sleeping
- Irritability or depressed mood
- Lack of motivation
Also, recreational substance use, such as marijuana, methamphetamines or LSD, can sometimes cause similar signs and symptoms.
Compared with schizophrenia symptoms in adults, teens may be:
- Less likely to have delusions
- More likely to have visual hallucinations
When to see a doctor
People with schizophrenia often lack awareness that their difficulties stem from a mental disorder that requires medical attention. So it often falls to family or friends to get them help.
Helping someone who may have schizophrenia
If you think someone you know may have symptoms of schizophrenia, talk to him or her about your concerns. Although you can't force someone to seek professional help, you can offer encouragement and support and help your loved one find a qualified doctor or mental health professional.
If your loved one poses a danger to self or others or can't provide his or her own food, clothing, or shelter, you may need to call 911 or other emergency responders for help so that your loved one can be evaluated by a mental health professional.
In some cases, emergency hospitalization may be needed. Laws on involuntary commitment for mental health treatment vary by state. You can contact community mental health agencies or police departments in your area for details.
Suicidal thoughts and behavior
Suicidal thoughts and behavior are common among people with schizophrenia. If you have a loved one who is in danger of attempting suicide or has made a suicide attempt, make sure someone stays with that person.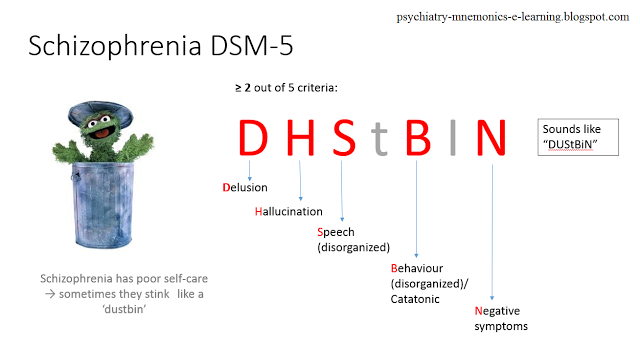 Call 911 or your local emergency number immediately. Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
Call 911 or your local emergency number immediately. Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
Request an appointment
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health. Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Causes
It's not known what causes schizophrenia, but researchers believe that a combination of genetics, brain chemistry and environment contributes to development of the disorder.
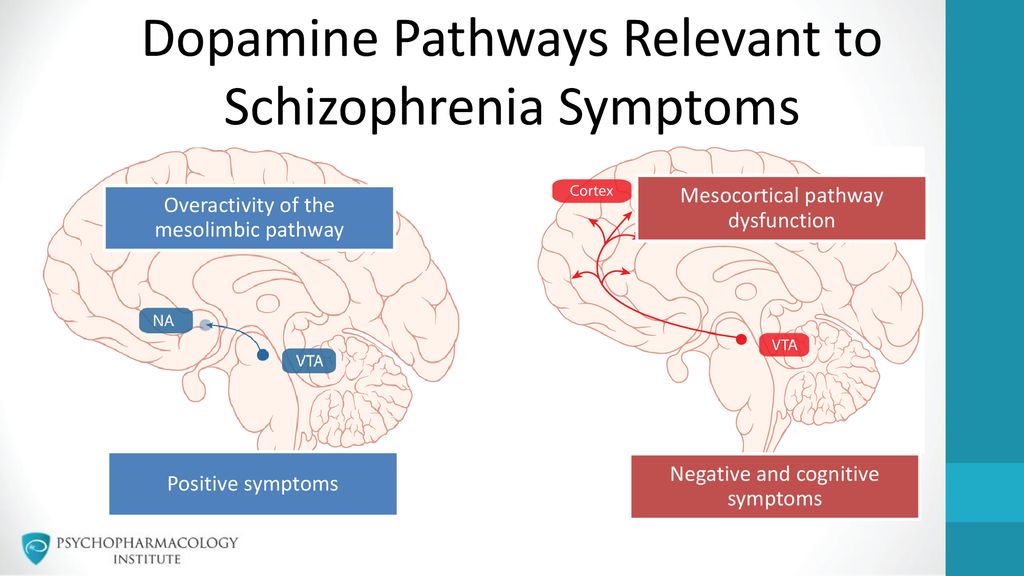
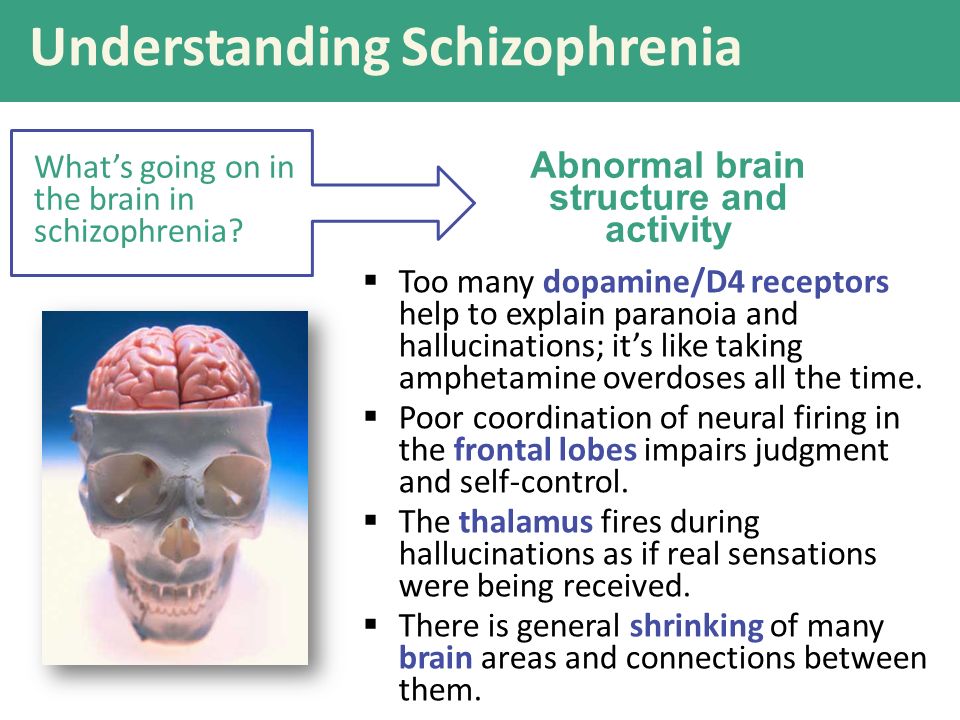
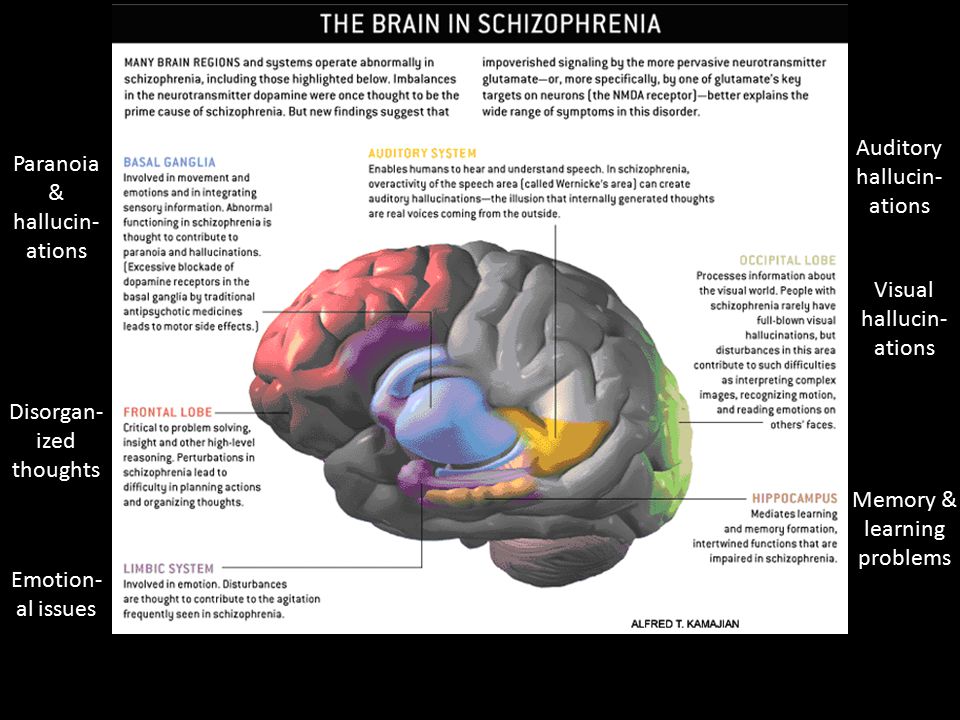
Problems with certain naturally occurring brain chemicals, including neurotransmitters called dopamine and glutamate, may contribute to schizophrenia. Neuroimaging studies show differences in the brain structure and central nervous system of people with schizophrenia. While researchers aren't certain about the significance of these changes, they indicate that schizophrenia is a brain disease.
Risk factors
Although the precise cause of schizophrenia isn't known, certain factors seem to increase the risk of developing or triggering schizophrenia, including:
- Having a family history of schizophrenia
- Some pregnancy and birth complications, such as malnutrition or exposure to toxins or viruses that may impact brain development
- Taking mind-altering (psychoactive or psychotropic) drugs during teen years and young adulthood
Complications
Left untreated, schizophrenia can result in severe problems that affect every area of life. Complications that schizophrenia may cause or be associated with include:
Complications that schizophrenia may cause or be associated with include:
- Suicide, suicide attempts and thoughts of suicide
- Anxiety disorders and obsessive-compulsive disorder (OCD)
- Depression
- Abuse of alcohol or other drugs, including nicotine
- Inability to work or attend school
- Financial problems and homelessness
- Social isolation
- Health and medical problems
- Being victimized
- Aggressive behavior, although it's uncommon
Prevention
There's no sure way to prevent schizophrenia, but sticking with the treatment plan can help prevent relapses or worsening of symptoms. In addition, researchers hope that learning more about risk factors for schizophrenia may lead to earlier diagnosis and treatment.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Helping Someone with Schizophrenia - HelpGuide.
 org
orgWhen a loved one has schizophrenia
The love and support of family and friends plays an important role in schizophrenia treatment and recovery. If you have a loved one with schizophrenia, you may be struggling with any number of difficult emotions, including fear, guilt, anger, and frustration. You may feel helpless in the face of your loved one’s symptoms, worried about the stigma of schizophrenia, or confused and embarrassed by their strange behaviors. You may even be tempted to hide your loved one’s illness from others.
But it’s important to remember that a diagnosis of schizophrenia is not a life-sentence. Recovery is possible, especially with your love and support. To help someone with schizophrenia, it’s crucial you:
- Accept the illness and its difficulties.
- Not buy into the myth that someone with schizophrenia can't get better or live a full and meaningful life.
- Do your best to help your loved one feel better and enjoy life.
- Pay attention to your own needs.
- Maintain your sense of humor and remain hopeful.
While dealing with a loved one’s schizophrenia can be challenging, the following strategies can help you guide your loved one on the road to recovery without losing sight of your own hopes and dreams.
Tips for helping a loved one with schizophrenia
Educate yourself. Learning about schizophrenia and its treatment will allow you to make informed decisions about how best to cope with symptoms, encourage your loved one to pursue self-help strategies, handle setbacks, and work towards recovery.
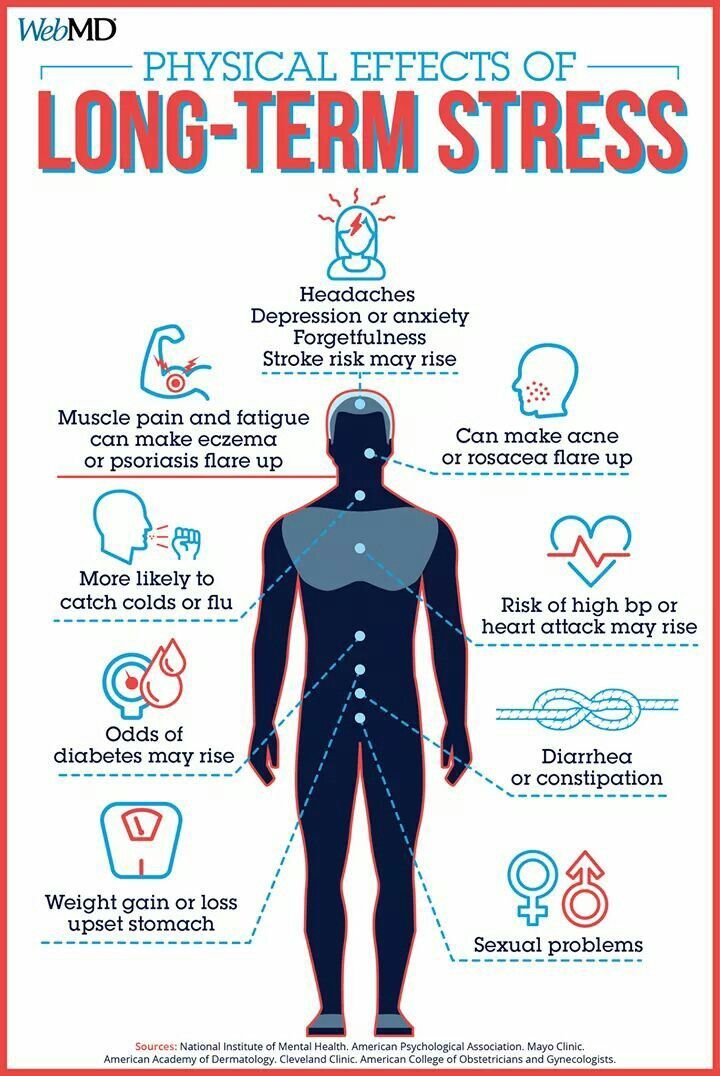
Reduce stress. Stress can cause schizophrenia symptoms to flare up, so it's important to create a structured and supportive environment for your loved one.
Set realistic expectations. It's important to be realistic about the challenges of schizophrenia. Help your loved one set and achieve manageable goals, and be patient with the pace of recovery.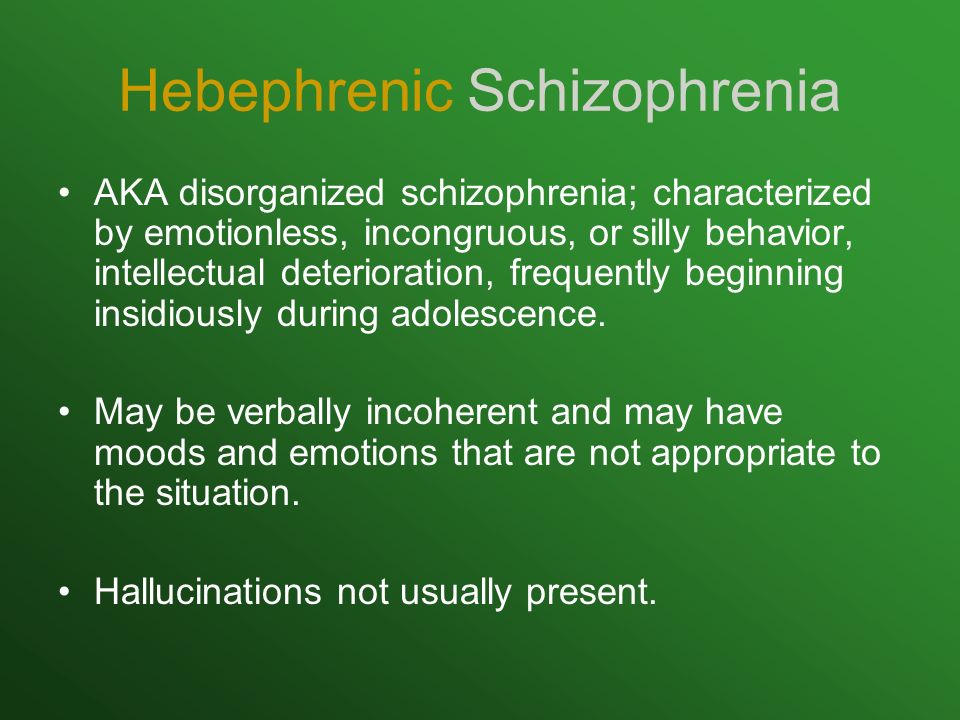
Empower your loved one. Be careful that you're not taking over and doing things for your loved one that they are capable of doing. Support your loved one while still encouraging as much independence and self-help as possible.
Helping someone with schizophrenia tip 1: Encourage treatment and self-help
Encouraging treatment and self-help is a cornerstone of helping a loved one with schizophrenia. While medication is an important element of schizophrenia treatment, your loved one's recovery depends on other factors as well. Self-help strategies such as changing to a healthy diet, managing stress, exercising, and seeking social support can have a profound effect on your loved one's symptoms, feelings, and self-esteem. And the more someone does for themselves, the less hopeless and helpless they'll feel, and the more likely their doctor will be able to reduce their medication. Your encouragement and support can be crucial to your loved one starting and continuing a program of self-help.
[Read: How to Help Someone with Mental Illness Accept Treatment]
Starting treatment
Often, the first challenge of treatment is convincing the person with schizophrenia to see a doctor. To people experiencing delusions, hallucinations, and paranoia, there is no need for medical intervention because the voices and conspiracy theories are real.
If a loved one with schizophrenia is reluctant to see a doctor, try to:
Provide options. Your loved one may be more willing to see a doctor if he or she has some control over the situation. If your relative appears suspicious of you, suggest that another person accompany them to the appointment. You can also give your loved one a choice of doctors.
Focus on a particular symptom. Someone with schizophrenia may resist seeing a doctor out of fear of being judged or labeled “crazy.” You can make the doctor less threatening by suggesting a visit in order to deal with a specific symptom such as insomnia or lack of energy.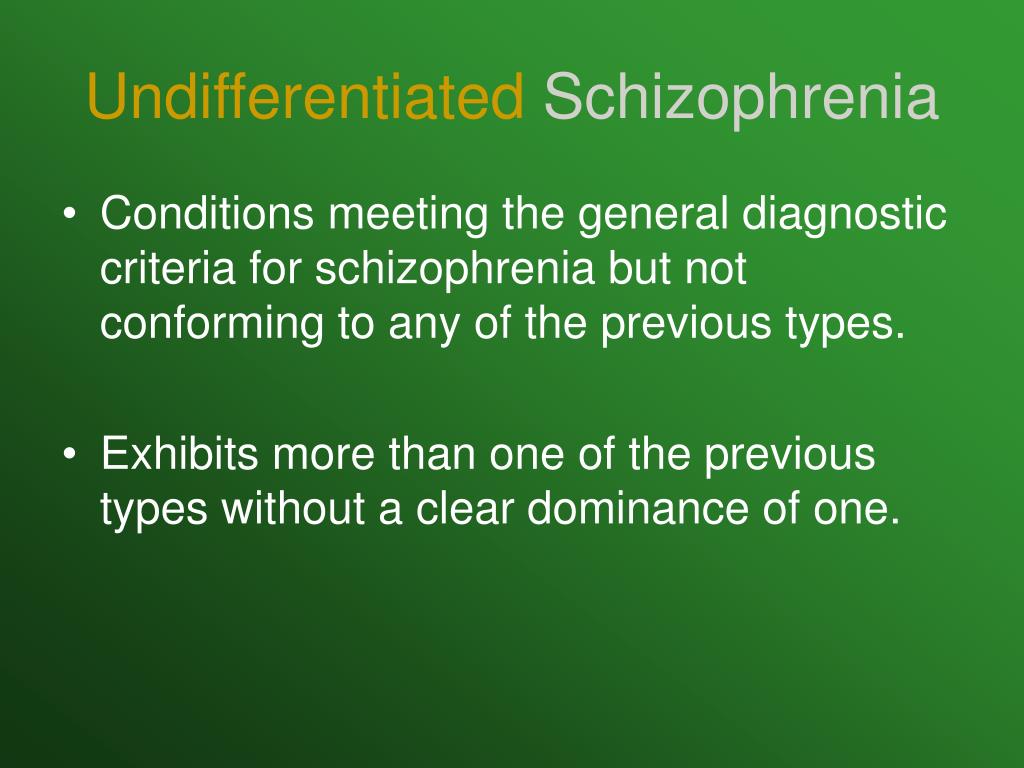
Tips for supporting a loved one's schizophrenia treatment
Seek help right away. Early intervention makes a difference in the course of schizophrenia, so help your loved one find a good doctor and start treatment.
Be collaborative. When your loved one has a voice in their own treatment, they will be more motivated to work towards recovery.
Encourage self-help. Since schizophrenia is often episodic, periods of remission from the severest symptoms can provide an opportunity for your loved one to employ self-help strategies that may limit the length and frequency of future episodes.
Tip 2: Build your support network
To better support and care for someone with schizophrenia, you need to find help, encouragement, and understanding from others. The more support you have, the better it will be for both you and your loved one.
Recognize your own limits. Be realistic about the level of support and care you can provide. You can't do it all, and you won't be much help to a loved one if you're exhausted, so seek help where you can.
You can't do it all, and you won't be much help to a loved one if you're exhausted, so seek help where you can.
Join a support group. Meeting others who know first-hand what you're going through can help reduce feelings of isolation and fear. Support groups provide an invaluable venue for the relatives of people with schizophrenia to share experiences, advice, and information.
Turn to trusted friends and family members. Ask loved ones if you can call on them for support. Most people will be flattered by your request.
Seek out new friends. If you don't feel that you have anyone to turn to, it's never too late to build new friendships and improve your support network.
Take advantage of support services. Ask your loved one's doctor or therapist about respite services and other support available in your area, or contact local hospitals and mental health clinics.
Speak to a Licensed Therapist
The world's largest therapy service. 100% online. Get matched with a professional, licensed, and vetted therapist in less than 48 hours.
100% online. Get matched with a professional, licensed, and vetted therapist in less than 48 hours.
Get 20% off
Professional online therapy and tools based on proven CBT strategies. Get instant help, along with your own personalized therapy toolbox.
Get 20% off
Affiliate Disclosure
Tip 3: Monitor medication
Once in treatment, careful monitoring can ensure that your loved one stays on track and gets the most out of medication.
Take side effects seriously. Many people with schizophrenia stop taking their medication because of side effects. Bring any distressing side effects to the attention of the doctor, who may be able to reduce the dose, switch to another antipsychotic, or add medication to counter the side effect.
Encourage your loved one to take medication regularly. Even with side effects under control, some people with schizophrenia refuse medication or have trouble remembering their daily dose.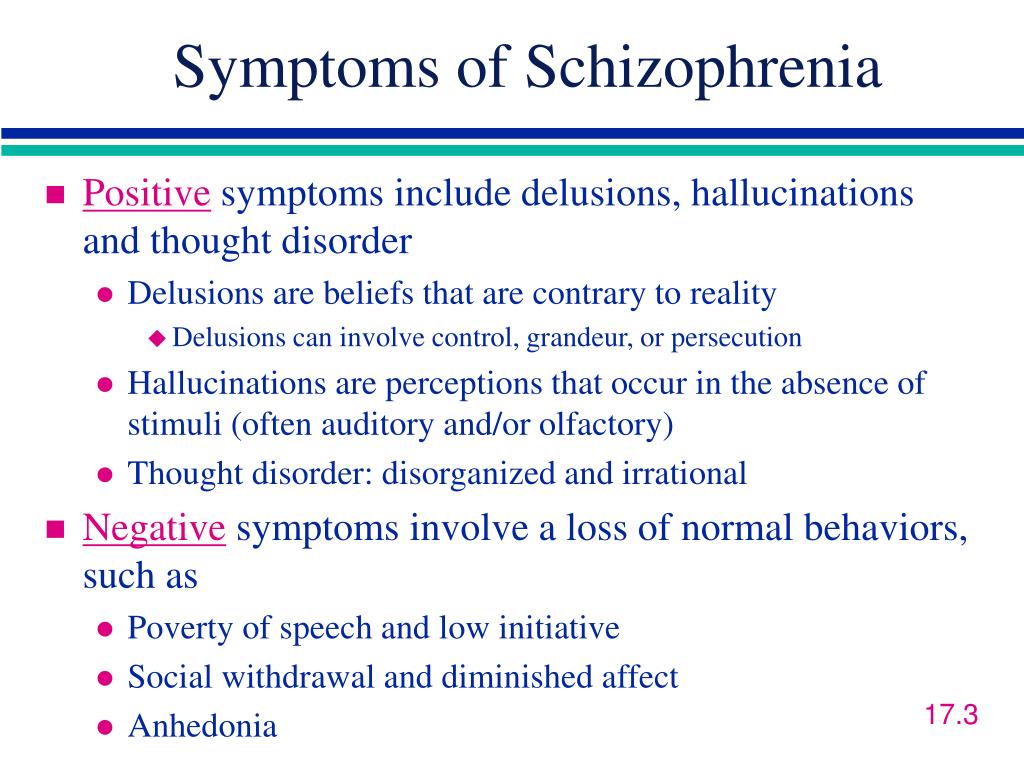 Medication reminder apps, weekly pillboxes, and calendars can help. Some medications are available as long-lasting weekly or monthly injections instead of daily pills.
Medication reminder apps, weekly pillboxes, and calendars can help. Some medications are available as long-lasting weekly or monthly injections instead of daily pills.
Be careful to avoid drug interactions. Help your loved one avoid any dangerous drug interactions by giving the doctor a complete list of the drugs and supplements they're taking. Mixing alcohol or illegal drugs with schizophrenia medication is harmful, so talk to the doctor if your relative has a substance abuse problem.
Track your family member's progress. A mood-tracking app, journal, or diary is a good way to track changes in your family member's behavior, outlook, and other symptoms in response to medication.
Tip 4: Watch for signs of relapse
Stopping medication is the most frequent cause of relapse in schizophrenia, so it's extremely important that your family member continues to take all medication as directed. While relapse can occur even if a person is taking medication as prescribed, you may be able to prevent a full-blown crisis by recognizing the warning signs and taking immediate steps.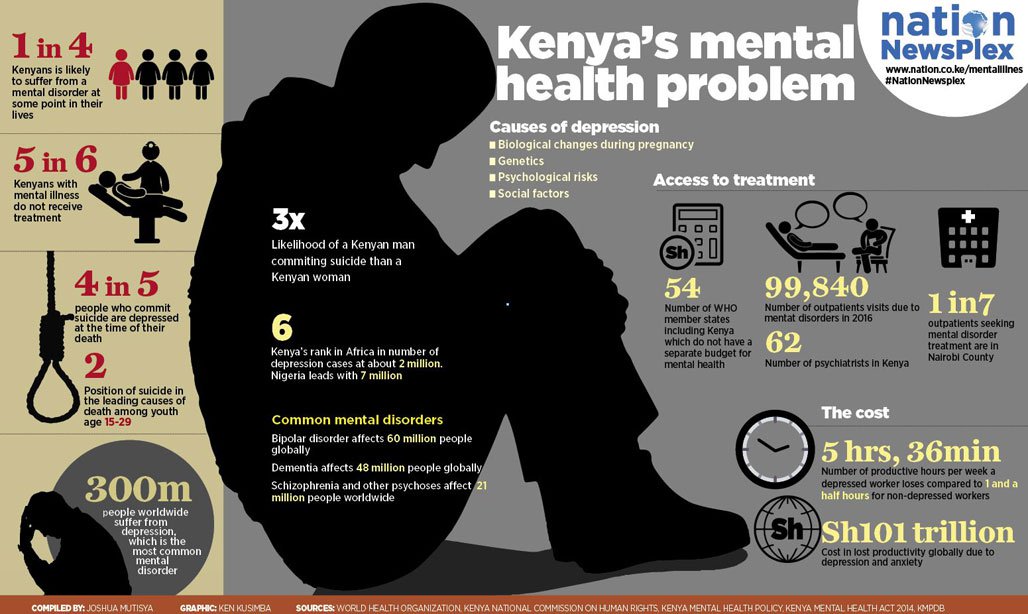
Common warning signs of schizophrenia relapse
- Insomnia
- Social withdrawal
- Deterioration of personal hygiene
- Increasing paranoia
- Hostility
- Confusing or nonsensical speech
- Strange disappearances
- Hallucinations
Tip 5: Prepare for crisis situations
Despite your best efforts to prevent relapse, there may be times when your loved one's condition deteriorates rapidly and hospitalization is required to keep them safe. Having an emergency plan ready for an acute psychotic episode will help you handle the crisis safely and quickly. A good emergency plan for someone with schizophrenia includes:
- Emergency contact information for your loved one's doctor and therapists.
- The address and phone number of the hospital you will go to for psychiatric admission.
- Friends or relatives who will take care of other children or dependents while you deal with the crisis.
It's also wise to go over the emergency plan with your family member. The crisis situation may be less frightening to your loved one if they know what to expect during an emergency.
10 tips for handling a schizophrenia crisis
- Remember that you cannot reason with acute psychosis.
- The person may be terrified by their own feelings of loss of control.
- Don't express irritation or anger.
- Speak quietly and calmly, do not shout or threaten the person.
- Don't use sarcasm as a weapon.
- Decrease distractions by turning off the TV, computer, any fluorescent lights that hum, etc.
- Ask any casual visitors to leave—the fewer people the better.
- Avoid direct, continuous eye contact.
- Avoid touching the person.
- Sit down and ask the person to sit down as well.
Tip 6: Explore housing options
Someone with schizophrenia needs a stable, supportive place to live, but finding the right living situation can be challenging.
- Can your loved one care for themselves?
- How much support do they need with daily activities?
- Does your loved one have a drug or alcohol problem?
- How much treatment supervision does your loved one require?
Living with family
Living with family can be a good option for someone with schizophrenia if their family members understand the illness well, have a strong support system of their own, and are able to provide whatever assistance is needed.
At-home arrangements are less likely to be successful if the person with schizophrenia uses drugs or alcohol, resists taking medication, or is aggressive or uncooperative.
| Choosing the Right Housing Option for Someone with Schizophrenia |
| Living with family works best if: |
|
| Living with family is not advised if: |
|
Try not to feel guilty if you are unequipped to house someone with schizophrenia. If you can't look after your own needs or those of other family members while caring for your loved one, they will be better off elsewhere.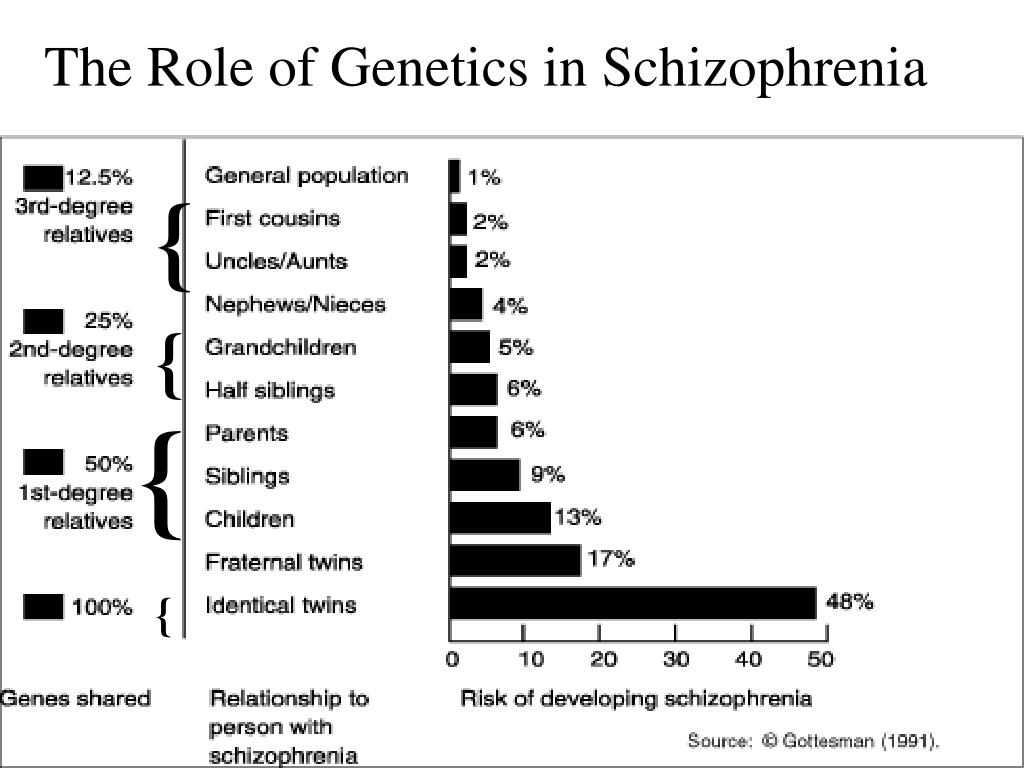
Residential options outside the family home
If an at-home living arrangement isn't the right fit, explore the residential facilities in your community.
Options in your area may include:
Residential treatment facilities or 24-hour care homes. A more structured living environment for those requiring greater assistance or suffering an acute psychotic episode.
Transitional group home. An intensive program that helps individuals transition back into society and avoid relapse after a crisis or hospitalization.
Foster or boarding homes. A group living situation offering a degree of independence, while providing meals and other basic necessities.
Supervised apartments. Residents live alone or share an apartment, with staff members available on-site to provide assistance and support.
Tip 7: Take care of yourself
Taking care of yourself isn't selfish. In fact, it's just as important for your loved one with schizophrenia that you look after your own health needs.
In fact, it's just as important for your loved one with schizophrenia that you look after your own health needs.
Schizophrenia can place an incredible amount of stress on the family. It can take over your life and burn you out. And if you're stressed, you'll make the person with schizophrenia stressed and trigger or exacerbate their symptoms.
Since adopting healthy lifestyle habits is also important for your loved one in managing schizophrenia symptoms, by taking care of your own health you can act as a role model. You may even be able to pursue some of these steps together, helping to motivate and encourage each other.
Connect with others. Social interaction with someone who cares about you is the most effective way to relieve stress. It's important for both you and the person with schizophrenia to have other people you can connect with face-to-face—someone you can talk to for an uninterrupted period of time, someone who will listen without judging or continually becoming distracted.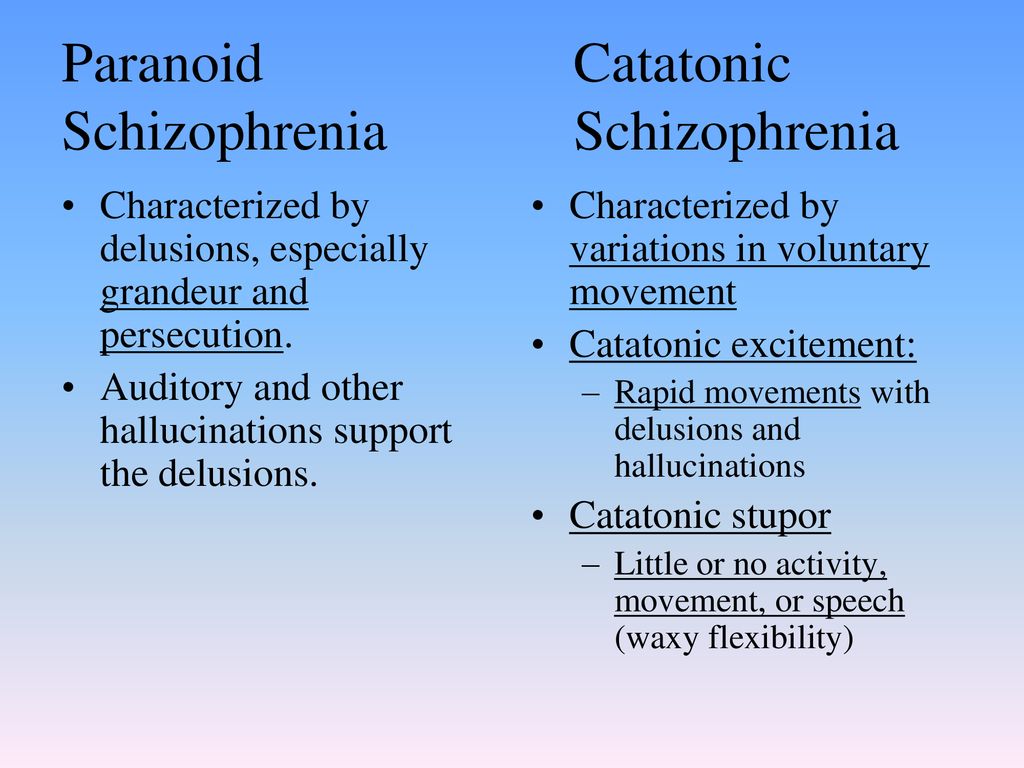 That person may be a friend, family member, clergy member, or professional therapist.
That person may be a friend, family member, clergy member, or professional therapist.
Get regular exercise. Physical activity reduces stress and releases endorphins, powerful chemicals in your brain that energize your spirits and make you feel good. Whether you exercise alone, with a friend, or with your loved one with schizophrenia, aim for 30 minutes of activity on most days, or if it's easier, three 10-minute sessions.
Eat a healthy diet. What you eat has a direct impact on the way you feel. Minimize sugar and refined carbs, foods that quickly lead to a crash in mood and energy. Boost your intake of Omega-3 fatty acids from fatty fish, fish oil, walnuts, and flaxseeds to help improve your focus, energy, and outlook. The same diet tips can help manage your loved one's symptoms, too.
Practice acceptance. Instead of dwelling on the unfairness of your loved one's diagnosis, accept your feelings, even the negative ones.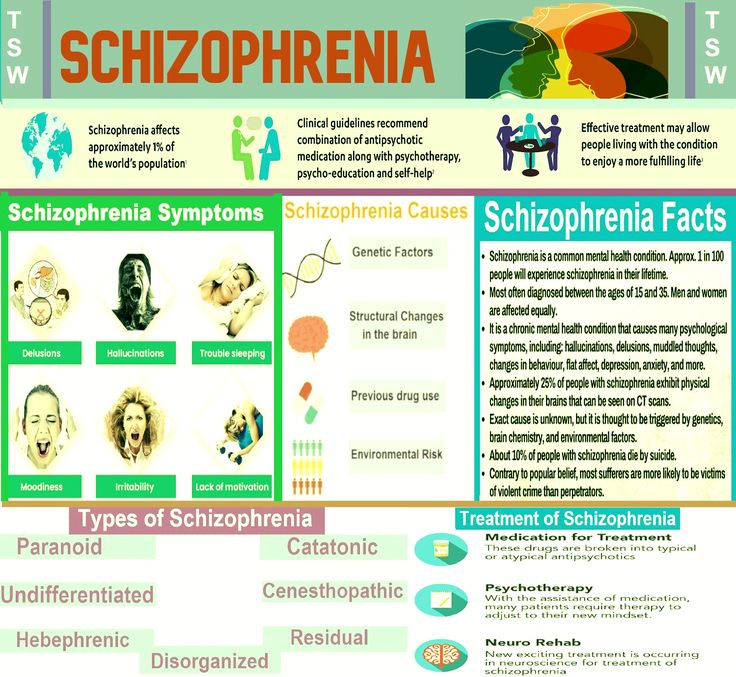 It can make a huge difference in your ability to manage stress and balance your moods. See HelpGuide's Emotional Intelligence Toolkit for more.
It can make a huge difference in your ability to manage stress and balance your moods. See HelpGuide's Emotional Intelligence Toolkit for more.
Seek out joy. Making time for fun isn't indulgent—it's necessary. Schedule time into your day for things you enjoy, whether it's spending time in nature, visiting friends, or reading a good book. Encourage your loved one with schizophrenia to do the same.
Look after your health. Neglecting your health will only add to the stress in your life. Get enough sleep and stay on top of any medical conditions.
Use relaxation techniques. Techniques such as meditation, deep breathing, yoga, or progressive muscle relaxation can put the brakes on stress and bring your mind and body back into balance.
Helplines and support
- In the U.S.
Call 1-800-950-6264 or visit NAMI.
 org
org - UK
Call 0300 5000 927 or visit Rethink: Schizophrenia
- Australia
Call 1800 18 7263 or visit Sane Australia
- Canada
Visit Canadian Mental Health Association for links to helplines and services
- India
Call the Vandrevala Foundation Helpline at 1860 2662 345 or 1800 2333 330
Last updated or reviewed on February 24, 2023
Schizophrenia
Schizophrenia- Healthcare issues »
- A
- B
- B
- G
- D
- E
- and
- 9000 About
- P
- P
- With
- T
- U
- F
- x
- S
- B
- E
- S
- I
005
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find country »
- A
- B
- C
- g
- D
- E
- and
- th
- K
- L
- 9000 N
- 9000
- in
- f
- x
- C
- hours
- Sh
- Sh.
- 9000 WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Events
- Photo reports
- case studies
- Questions and answers
- Speeches
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/
- Schizophrenia
Key Facts
- Schizophrenia is a severe mental disorder that affects approximately 24 million people, or 1 in 300 people worldwide.
- Schizophrenia causes psychosis, is associated with severe disability, and can negatively affect all areas of life, including personal, family, social, academic and work life.
- People with schizophrenia are often subject to stigma, discrimination and human rights violations.
- Worldwide, more than two thirds of people with psychosis do not receive specialized mental health care.
- There are a number of effective options for helping patients with schizophrenia, which can lead to a complete recovery of at least one in three patients.
Symptoms
Schizophrenia is characterized by significant disturbances in the perception of reality and behavioral changes, such as:
People with schizophrenia often also experience persistent cognitive or thinking problems that affect memory, attention, or problem-solving skills.
At least one third of patients with schizophrenia experience complete remission of symptoms (1). In some, periods of remission and exacerbation of symptoms follow each other throughout life, in others there is a gradual increase in symptoms.
Scope and impact
Schizophrenia affects approximately 24 million people, or 1 in 300 people (0.32%) worldwide. Among adults, the rate is 1 in 222 (0.45%) (2). Schizophrenia is less common than many other mental disorders. Onset is most common in late adolescence and between the ages of 20 and 30; while women tend to have a later onset of the disease.
Schizophrenia is often accompanied by significant stress and difficulties in personal relationships, family life, social contacts, studies, work or other important areas of life.
People with schizophrenia are 2-3 times more likely to die early than the population average (2).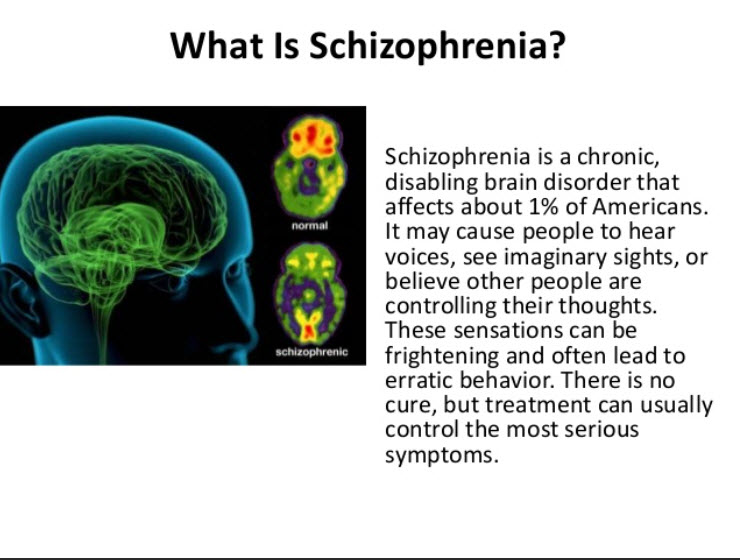 It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
Patients with schizophrenia often become the object of human rights violations both within the walls of psychiatric institutions and in everyday life. Significant stigmatization of people with this disease is a widespread phenomenon that leads to their social isolation and has a negative impact on their relationships with others, including family and friends. This creates grounds for discrimination, which in turn limits access to health services in general, education, housing and employment.
Humanitarian emergencies and health crises can cause intense stress and fear, disrupt social support mechanisms, lead to isolation and disruption of health services and supply of medicines. All these shocks can have a negative impact on the lives of people with schizophrenia, in particular by exacerbating existing symptoms of the disease. People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion.
Causes of schizophrenia
Science has not established any single cause of the disease. It is believed that schizophrenia may be the result of the interaction of a number of genetic and environmental factors. Psychosocial factors may also influence the onset and course of schizophrenia. In particular, heavy marijuana abuse is associated with an increased risk of this mental disorder.
Assistance services
At present, the vast majority of people with schizophrenia do not receive mental health care worldwide. Approximately 50% of patients in psychiatric hospitals are diagnosed with schizophrenia (4). Only 31.3% of people with psychosis get specialized mental health care (5). Much of the resources allocated to mental health services are inefficiently spent on the care of patients admitted to psychiatric hospitals.
Available scientific evidence clearly indicates that hospitalization in psychiatric hospitals is not an effective way of providing care for mental disorders and is regularly associated with the violation of the fundamental rights of patients with schizophrenia. Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is important the patient with schizophrenia, his family members and members of local communities.
Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is important the patient with schizophrenia, his family members and members of local communities.
Schizophrenia management and care
There are a number of effective approaches to treating people with schizophrenia, including medication, psychoeducation, family therapy, cognitive behavioral therapy, and psychosocial rehabilitation (eg, life skills education).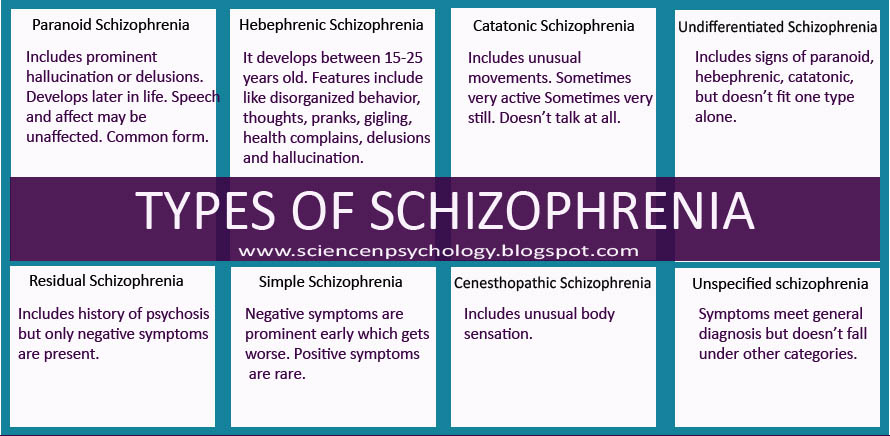 The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
WHO action
steps are in place to ensure that appropriate services are provided to people with mental disorders, including schizophrenia. One of the key recommendations The action plan is to transfer the function of providing assistance from institutions to local communities. WHO Special Mental Health Initiative aims to further progress towards the goals of the Comprehensive Plan mental health action 2013–2030 by ensuring that 100 million more people have access to quality and affordable mental health care.
The WHO Mental Health Gap Action Program (mhGAP) is working to develop evidence-based technical guidelines, tools and training packages to scale up services in countries, especially in low-resource settings. The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The WHO QualityRights project aims to improve the quality of care and better protect human rights in mental health and social care settings and to expand opportunities of various organizations and associations to defend the rights of persons with mental disorders and psychosocial disabilities.
The WHO guidelines on community mental health services and human rights-based approaches provide information for all stakeholders who intend to develop or transform mental health systems and services. health in accordance with international human rights standards, including the UN Convention on the Rights of Persons with Disabilities.
Bibliography
(1) Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J.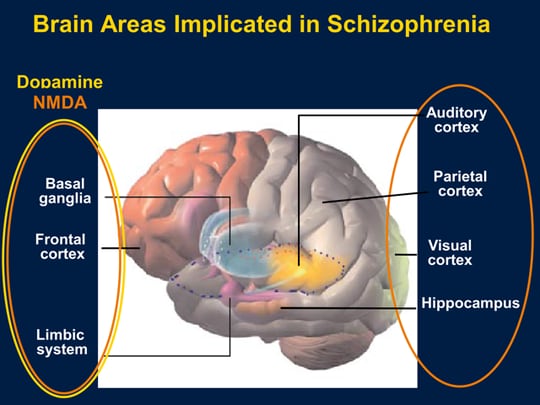 Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
(2) Institute of Health Metrics and Evaluation (IHME). Global Health Data Exchange (GHDx). http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/27a7644e8ad28e739382d31e77589dd7 (accessed 25 September 2021)
(3) LaursenTM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annual Review of Clinical Psychology , 2014;10, 425-438.
(4) WHO. Mental health systems in selected low- and middle-income countries: a WHO-AIMS cross-national analysis. WHO: Geneva, 2009
(5) Jaeschke K et al. Global estimates of service coverage for severe mental disorders: findings from the WHO Mental Health Atlas 2017 Glob Ment Health 2021;8:e27.
"I saw creatures from a parallel reality" How people with schizophrenia live: Lenta.ru
Schizophrenia is a severe mental disorder that affects more than 20 million people worldwide. Often people with this disease hallucinate, hear voices, see things that are not really there, and are prone to delusional ideas. Lenta.ru, with the support of the pharmaceutical company Gedeon Richter, talked to people diagnosed with schizophrenia and learned how to identify a mental disorder and what to do about it.
Often people with this disease hallucinate, hear voices, see things that are not really there, and are prone to delusional ideas. Lenta.ru, with the support of the pharmaceutical company Gedeon Richter, talked to people diagnosed with schizophrenia and learned how to identify a mental disorder and what to do about it.
Sarah, age 28: “It all started innocently: I felt like I could hear people's thoughts”
I was diagnosed with paranoid schizophrenia while in a psychiatric hospital. The diagnosis was made almost immediately, after the first consultation of specialists.
Every person with schizophrenia experiences a different course of the disease. Anything can serve as a trigger for its development - any severe stress, childbirth, death of a loved one or drug use.
The first symptoms of the disease appeared a year and a half ago, I was 27. Then I was a master student, a trainee teacher in one of the leading universities in the country. It all started quite innocently: I seemed to hear people's thoughts. To some extent, it was interesting - it seemed to me that my superpowers had awakened. I could ride in a trolleybus and hear the buzz of other people's thoughts: “I need to pick up the child from the garden”, “I'm sad”, “I want to buy a TV”. And this at a time when I have no children, and I do not need a TV. Fortunately, this did not affect the quality of life and work, I could control it.
To some extent, it was interesting - it seemed to me that my superpowers had awakened. I could ride in a trolleybus and hear the buzz of other people's thoughts: “I need to pick up the child from the garden”, “I'm sad”, “I want to buy a TV”. And this at a time when I have no children, and I do not need a TV. Fortunately, this did not affect the quality of life and work, I could control it.
After some time, the colors began to thicken - this coincided with the increased level of responsibility at work and the approaching deadline for defending a master's thesis. I could no longer move away from other people's thoughts, they literally settled in my head, there was no more room left for me. When I was in any society, I heard non-verbal threats from others. I was scared to ride the subway because I was convinced that anyone could read my mind.
Image: Sveta Kobrakova
Philosophy examination was the culmination. Then I was convinced that someone took the brain out of my head, so I don’t remember anything. It became clear to me that something was wrong with me.
It became clear to me that something was wrong with me.
The disease worsened my condition, it became more and more difficult to live in a world that seemed to take up arms against me. But in reality, my own brain turned against me, which seems even more terrifying.
I told my parents everything, they took me to my native provincial town and sent me to the center of border conditions. There I was prescribed antipsychotic drugs.
Surely everyone has heard the expression "suffering from schizophrenia" - and this perfectly describes the disease. The disease torments, exhausts, makes existence unbearable. The most terrible thing is, let's say, the seal of fate imposed by her. Chronic... incurable... progressive... All these words lie like tombstones on us, people with a diagnosis.
Isolation from the world, the impossibility of realization, invalidization, stigmatization - this is the round dance that we face. We will never be able to communicate with this world, to speak out into it.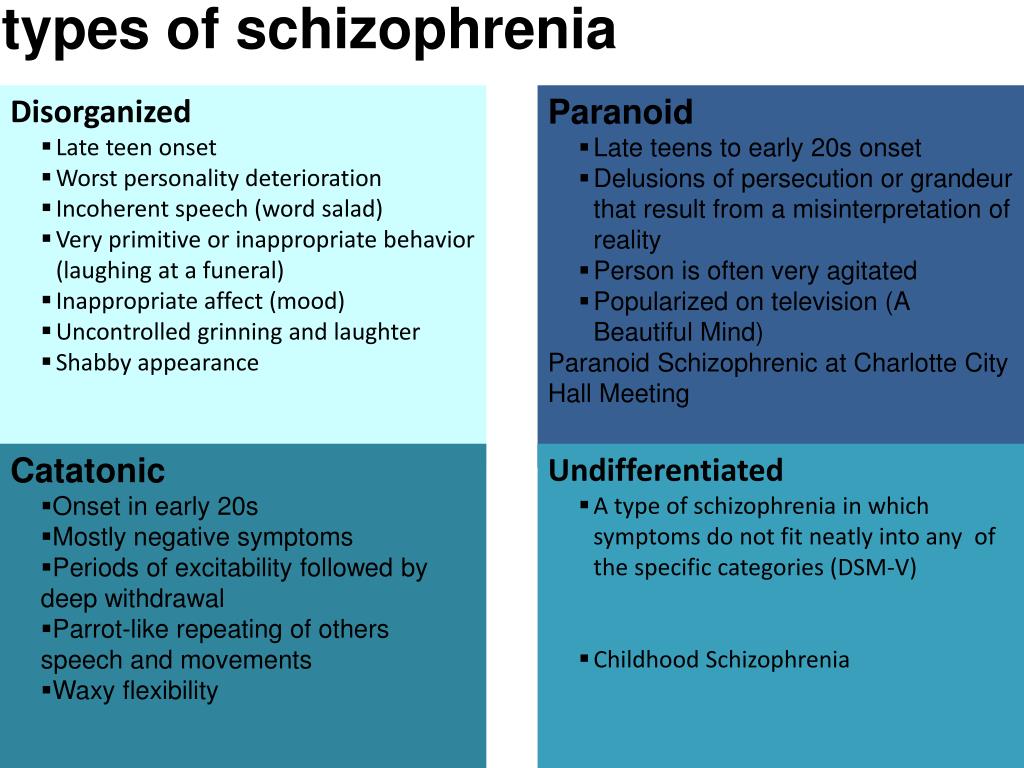 We will never be understood, because it cannot be explained in the way that love, earache or despair, which all people have experienced in one way or another, can be explained.
We will never be understood, because it cannot be explained in the way that love, earache or despair, which all people have experienced in one way or another, can be explained.
Image: Sveta Kobrakova
There are people with schizophrenia who, under the supervision of a specialist, as a result of many years of trying different drugs, were able to find the optimal treatment regimen. A good example is Elin Sachs, an American professor, Ph.D. Her book "The center cannot hold" at some point lit up my life with hope and showed that it's too early to give up - everything can be changed. Yes, you have to constantly fight, become a real warrior, but it's worth it.
Schizophrenia is a reason for getting a disability, but not in all cases. Although I am registered with the PND, I managed to avoid disability. And yet, I have some limitations in life in general and in work in particular. I can't teach anymore, I can't drive. I think that the work does not shine for me in responsible leadership positions.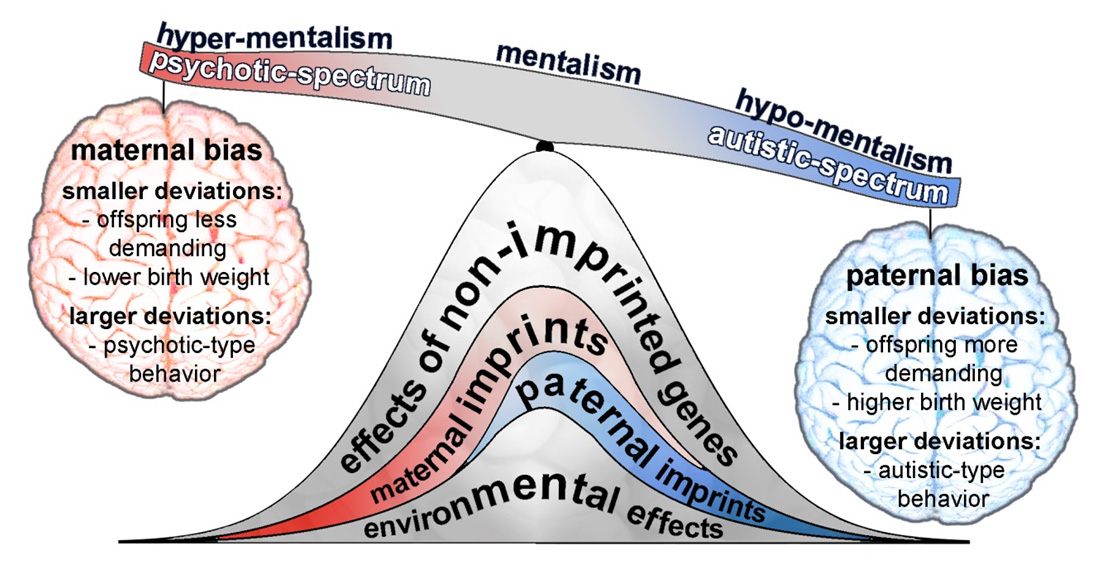
It is impossible to completely recover from schizophrenia, but it is possible to achieve stable remission and complete social and labor rehabilitation.
People with a disease need support, so the relatives of the "ill" person need to be ready to fight. The most qualified specialists are also needed. But in no case should you turn to psychics, shamans and magicians who exorcise demons. So you can lose very valuable time, money and also aggravate the disease.
Image: Sveta Kobrakova
If you notice that there is a big difference between reality and what is happening in your head, you should go to a specialist. You should always be very critical of yourself and include rational thinking. That is, for example, what is the probability that you are the earthly incarnation of some god?
I would like to appeal to everyone who has encountered schizophrenia: be strong, do not give up, do not spare money for specialists and drugs - all this will pay off with your condition.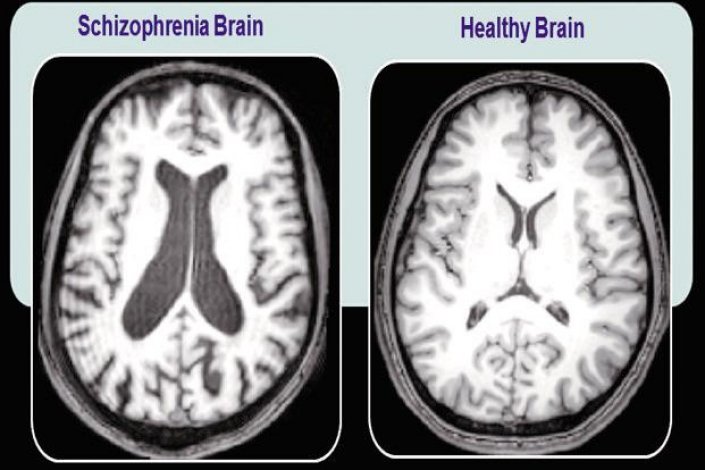 The path will be long and difficult, but worth it. Find those who understand you, do not stigmatize the disease, get treated - and you will achieve remission. Well, get as creative as possible.
The path will be long and difficult, but worth it. Find those who understand you, do not stigmatize the disease, get treated - and you will achieve remission. Well, get as creative as possible.
In 2019, Gedeon Richter launched a new drug on the Russian market that can alleviate the positive and negative symptoms of the disease
Ekaterina, 37: “I started seeing creatures from a parallel reality”
Schizophrenia usually seems to be something irreparable. Immediately, pictures are drawn about the absence of a future, about life in a mental hospital. But today it is not so! Many people diagnosed with schizophrenia are quite successful, both professionally and personally.
Yes, the diagnosis is really difficult to accept. I sobbed when the specialist suggested that I had schizophrenia - it's like finding out that you are mortally ill, only not in body, but in soul and mind.
There is a problem that a person with such a diagnosis, without explaining anything, is prescribed a bunch of rather heavy drugs with a huge number of side effects. And people do not even understand why all this is necessary and whether it is necessary at all. People do not know that drugs can be changed, the dose adjusted. This often leads to an unauthorized refusal of drug treatment, which, with the right selection of drugs, makes it possible to be conscious. Some 50 years ago, patients did not have such an opportunity!
And people do not even understand why all this is necessary and whether it is necessary at all. People do not know that drugs can be changed, the dose adjusted. This often leads to an unauthorized refusal of drug treatment, which, with the right selection of drugs, makes it possible to be conscious. Some 50 years ago, patients did not have such an opportunity!
When the first signs of the disease appeared, I didn't even understand that it was a disease - that's its cunning. At some point, I began to live in two realities, as it were. And every day these realities became more. It's like living in different dimensions, in which it is not space that differs, but your life, experience, destiny.
It is very difficult to describe... Imagine that there is you, and there is another you, only he is in another dimension. Perhaps in another time. There are many of you, and they are all connected. Their own future, the future of their loved ones and all the events around depend on the actions of each of these personalities. Then the ball grows to such a size that it is impossible to unravel it. And despair sets in. Like an abyss into which you are rapidly drawn in, from which you cannot get out.
Then the ball grows to such a size that it is impossible to unravel it. And despair sets in. Like an abyss into which you are rapidly drawn in, from which you cannot get out.
At some point, I began to see different creatures, as if from a parallel reality. Some were aggressive and attacked me, others defended. But I understood that only I see it, and I did not tell anyone about it.
Image: Sveta Kobrakova
Well, then the moment came when some symptoms came to the surface. Relatives realized that it was bad, and called an ambulance. I was not dangerous either for myself or for others, so at first the doctors did not want to take me away - there was no reason for this. But then they saw my old, many years old, scars from self-harm, and it was these scars that became the reason for admission to the hospital.
I would not wish anyone, not a single person in the world, to get this disease. It is difficult to convey the full range of feelings that one has to experience in a state of psychosis (I have had three of these over the past year and a half). You find yourself in circumstances that you cannot influence in any way, and together with you, through your fault, people dear to you are here. What can a person experience who, for example, is sure that he is locked forever in his apartment with his children, and at that time a night has come that will never end? It is fear and utter despair.
You find yourself in circumstances that you cannot influence in any way, and together with you, through your fault, people dear to you are here. What can a person experience who, for example, is sure that he is locked forever in his apartment with his children, and at that time a night has come that will never end? It is fear and utter despair.
When you come out of psychosis, the recovery period begins. This is also very difficult. It can be very difficult to do at least something - even get out of bed. It happens that there is a complete emptiness inside, and you do not feel anything, nothing at all - neither joy, nor sadness, nor love, nor pain, or any other experiences. And here again there is a feeling of guilt, because you cannot even carry out everyday activities.
Once I almost went out the window of the sixth floor, and my children were nearby. It didn't happen because I wanted to take my own life. It was just that at that moment in my reality, I believed that my physical body was invulnerable. But I was lucky, I was stopped. The mother-in-law, seeing me standing at the window, said in a calm voice: “Close it, please.” And I closed.
But I was lucky, I was stopped. The mother-in-law, seeing me standing at the window, said in a calm voice: “Close it, please.” And I closed.
Image: Sveta Kobrakova
At one moment I realized that I need relatives, children, and this is more important for me than "superpowers". And I have to do everything to live in the real world. When I realized this, my healing became conscious. I began to cooperate more actively with specialists, listen to their recommendations, search for information, read literature related to psychiatry. It was a lot of work, but it was important for me to return - for the sake of those who need me. The key, in my opinion, is just this: find the strength in yourself to admit that you are sick and begin to be treated.
If you are a relative of a person who has experienced schizophrenia, you need to understand that schizophrenia is not a whim, not fooling around, not laziness, not mental retardation. This is a disease that needs to be treated, and the sooner you start, the better. It is desirable that the treatment consists not only in observation by a specialist, but also in work with a psychotherapist, a social worker, and participation in self-help groups.
It is desirable that the treatment consists not only in observation by a specialist, but also in work with a psychotherapist, a social worker, and participation in self-help groups.
If one person in the family is ill, then everyone needs support and help. The problem is not only with the patient. One way or another, this situation affects the whole family. For children, this is generally a serious trauma, so you can’t taboo this topic, somehow hush it up. Children of people with mental illness need support in this matter.
I want to draw attention to the word "support". Not guardianship. In no case should you do everything for the patient, it only hurts. And there is no need to load him with some kind of excessive activity, especially if this activity is not in the sphere of his interests. It is necessary to support and encourage him in all endeavors, talents, abilities. I know from experience that often the phrase “Cheer up, we will overcome this” is sometimes more important than long motivating conversations.
I have three children. The eldest was seven years old when I first went to the hospital. The fact that I was sick, we did not talk to him right away. The topic was almost taboo in our family, and even then I did not recognize the disease in myself. But it was clear that the older child was going through. Everything changed after the third episode - then we talked. I said that in all the variety of different diseases, there are also mental ones. My son has changed right before my eyes, now he asks various questions about the disease, goes to events with me and is quite well versed in the topic of mental health. Children are able to understand, you just need to call a spade a spade, although it is scary to admit a lot to yourself.
I took medication for about three years. Today I manage to do without them. I take them occasionally when I feel some of the familiar signals of an oncoming psychosis. But this happens extremely rarely - against the background, for example, of a strong stressful situation. Of course, I am satisfied that I live in our time, and I have a chance to help myself with medicines. They don’t torture me with a lobotomy, they don’t put a wet rag on me, they don’t hang me from the ceiling. Once upon a time, these methods were considered quite adequate, however, as we know now, all this did not work or only made things worse.
Of course, I am satisfied that I live in our time, and I have a chance to help myself with medicines. They don’t torture me with a lobotomy, they don’t put a wet rag on me, they don’t hang me from the ceiling. Once upon a time, these methods were considered quite adequate, however, as we know now, all this did not work or only made things worse.
Image: Sveta Kobrakova
I like the comparison of schizophrenia with influenza, although it is not correct enough. Is it possible to get rid of the flu forever? No. For some period of time you feel bad, you need to take antipyretic and drink a lot, observe bed rest. And then everything went away, and you don’t need to do anything special to feel good. But the symptoms can return, and you need to be prepared for this.
Treatment allows you to live a full life. But you need to understand that drugs alone are not enough. Medicines only provide an opportunity to return to reality in order to fully work on the deeper causes of the disease.