How does a person with bipolar act
What are the signs and symptoms of bipolar disorder?
What is the treatment for mania, hypomania and depression?
You can check what treatment and care is recommended for bipolar disorders on the National Institute for Health and Care Excellence (NICE) website.
NICE produce guidelines for how health professionals should treat certain conditions. You can download these from their website at:
www.nice.org.uk.
The NHS doesn’t have to follow these recommendations. But they should have a good reason for not following them.
What medications are recommended?
Mood stabilisers are usually used to manage mania, hypomania and depressive symptoms.
The mood stabilisers we talk about in this factsheet are:
- Lithium
- Certain antipsychotic medication
- Certain anticonvulsive medication
- Certain benzodiazepine medication
Mania and hypomania
You should be offered a mood stabiliser to help manage your mania or hypomania. Your doctor may refer to your medication as ‘antimanic’ medication.
If you are taking antidepressants your doctor may advise you to withdraw from taking them.
You will usually be offered an antipsychotic first. The common antipsychotics used for the treatment of bipolar disorder are:
- Haloperidol
- Olanzapine
- Quetiapine
- Risperidone
If the first antipsychotic you are given doesn’t work, then you should be offered a different antipsychotic medication from the list above.
If a different antipsychotic doesn’t work, then you may be offered lithium to take alongside it. If the lithium doesn’t work you may be offered sodium valproate to take with an antipsychotic. Sodium valproate is an anticonvulsive medication.
Sodium Valproate shouldn’t be given to girls or young women who might want to get pregnant.
Your doctor should think about giving you benzodiazepine medication short term.
Your doctor will suggest different dosages and combinations to you depending on what works best for you.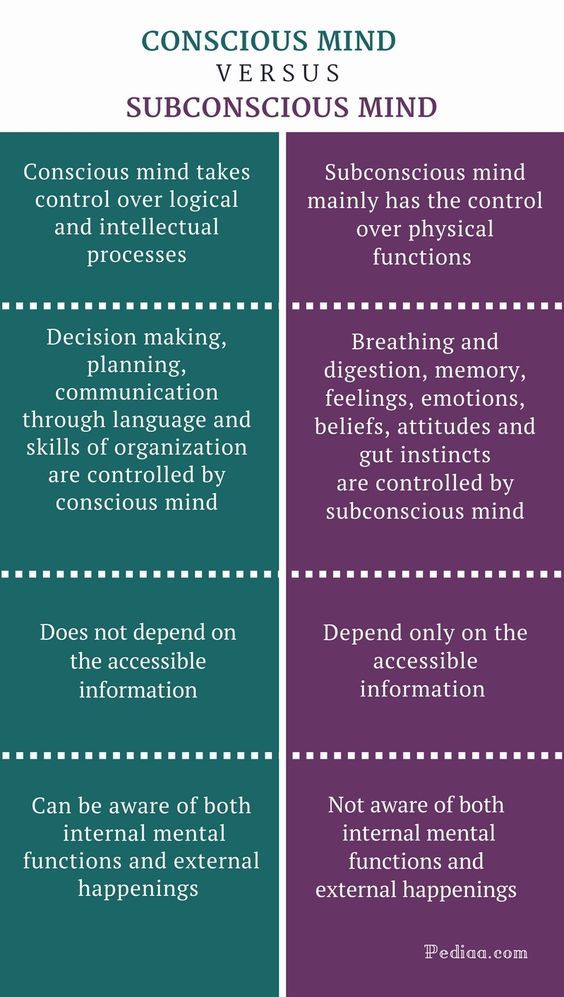 Your personal preferences should be listened to.
Your personal preferences should be listened to.
Depression
Your doctor should offer you medication to treat depressive symptoms. You may be offered the following medication:
- Fluoxetine with Olanzapine
- Quetiapine
- Olanzapine or
- Lamotrigine
Fluoxetine is an antidepressant. Lamotrigine is an anticonvulsant medication.
Your doctor can prescribe the above medication alongside:
- Lithium, and
- Sodium valproate.
If you would like to take medication, doctors will use different dosages and combinations depending on what works best for you. Your personal preferences should be listened to.
You can find more information about:
- Mood stabilisers by clicking here.
- Antipsychotics by clicking here.
- Antidepressants by clicking here.
- Benzodiazepines by clicking here.
- Medication – choice and managing problems by clicking here.
What psychological treatments are recommended?
If you have an episode of depression you should be offered medication and a high intensity talking therapy, such as:
- cognitive behavioural therapy (CBT), or
- interpersonal therapy.
What is cognitive behavioural therapy (CBT)?
CBT is a talking therapy that can help you manage your problems by changing the way you think and behave.
What is interpersonal therapy?
Interpersonal therapy is a talking therapy that focuses on you and your relationships with other people.
You can find more information about ‘Talking therapies’ by clicking here.
What are the long-term treatments for bipolar disorder?
Bipolar disorder is a life-long and often recurring illness. You may need long term support to help manage your condition.
What medication options are there?
Your doctor will look at what medication worked for you during episodes of mania or depression. They should ask you whether you want to continue this treatment or if you want to change to lithium.
Lithium usually works better than other types of medication for long-term treatment. Your doctor should give you information about how to take lithium safely. If lithium doesn't work well enough or causes you problems, you may be offered:
If lithium doesn't work well enough or causes you problems, you may be offered:
- Valproate,
- Olanzapine, or
- Quetiapine.
Your doctor should monitor your health. Physical health checks should be done at least once a year. These checks will include:
- measuring your weight,
- blood and urine tests,
- checking your liver and heart, and
- checking your pulse and blood pressure.
What psychological treatments are recommended?
You should be offered a psychological therapy that is specially designed for bipolar disorder. You could have individual or group therapy.
The aim of your therapy is to stop you from becoming unwell again. This is known as ‘relapse.’ Your therapy should help you to:
- understand your condition,
- think about the effect that your thoughts and behaviour have on your mood,
- monitor your mood, thoughts and behaviour,
- think about risk and distress,
- make plans to stay well,
- make plans to follow if you start to become unwell,
- be aware of how you communicate, and
- manage difficulties you may have in day to day life.
If you live with your family or are in close contact with them, you should also be offered ‘family intervention.’
Family intervention is where you and your family work with mental health professionals to help to manage relationships. This should be offered to people who you live with or who you are in close contact with.
The support that you and your family are given will depend on what problems there are and what preferences you all have. This could be group family sessions or individual sessions. Your family should get support for 3 months to 1 year and should have at least 10 planned sessions.
Is there any other support?
Your mental health team should give you advice about exercise and healthy eating.
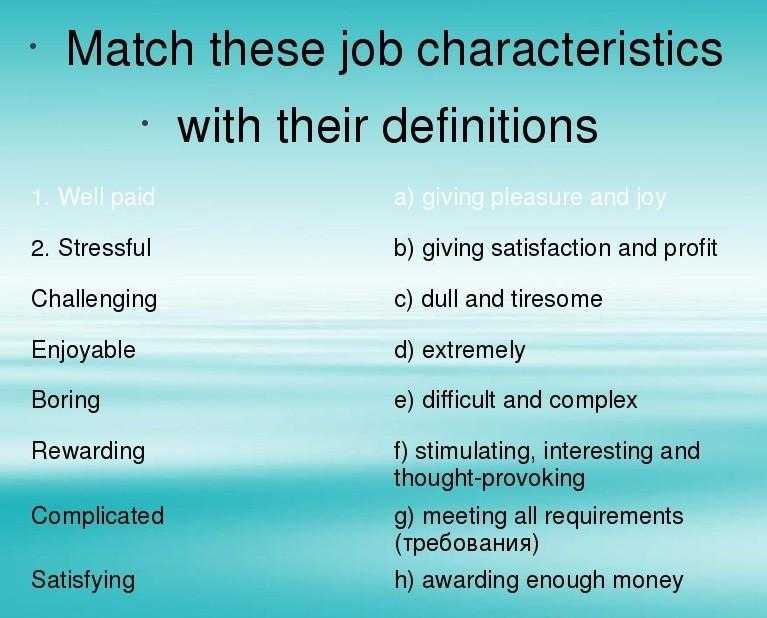
If you want to return to work, you should be offered support with that including training. You should get this support if your care is managed by your GP or by your community mental health team.
You might not be able to work or to find any.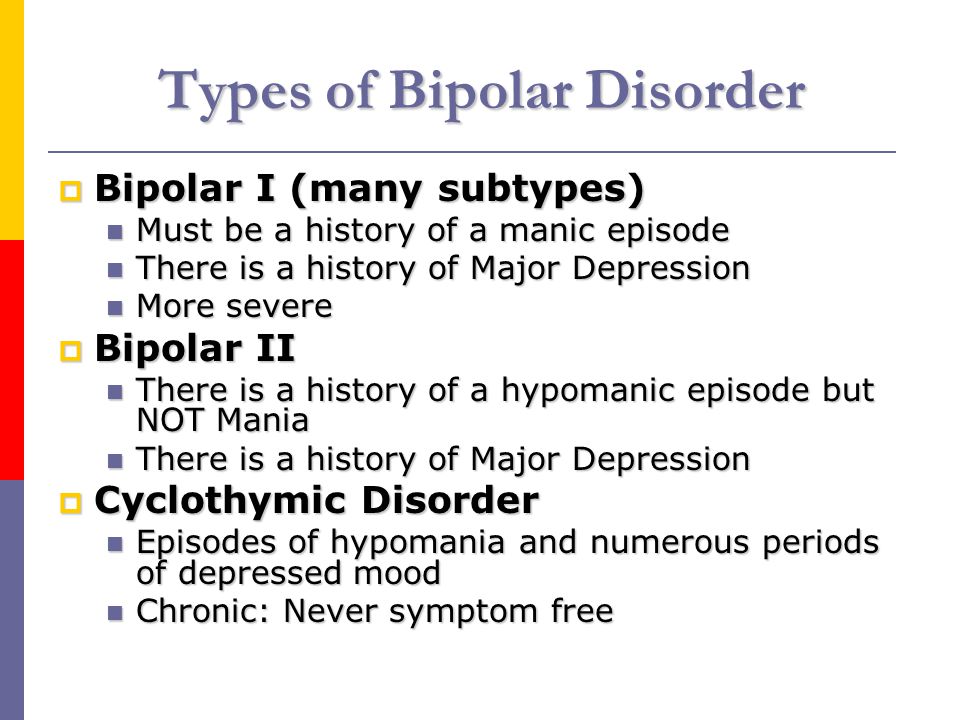 Your healthcare professionals should think about other activities that could help you back to employment in the future.
Your healthcare professionals should think about other activities that could help you back to employment in the future.
Your healthcare team should help you to make a recovery plan. The plan should help you to identify early warning signs and triggers that may make you unwell again and ways of coping. Your plan should also have people to call if you become very distressed.
You should be encouraged to make an ‘advance statement.’ This is an instruction to health professionals about what you would like to happen with your care if you ever lack mental capacity to make your own decisions.
What is the Care Programme Approach?
You may be assessed under the Care Programme Approach (CPA) if you have complex needs or you are vulnerable.
CPA is a package of care that is used by secondary mental health services. You will have a care plan and someone to coordinate your care. All care plans should include a crisis plan.
CPA aims to support your mental health recovery by helping you to understand your:
- strengths,
- goals,
- support needs, and
- difficulties.

CPA should be available if you have a wide range of needs from different services or you are thought to be a high risk. Both you and your GP should be given a copy of your care plan.
Your carers can be involved in your care plan and given a copy if you give your consent for this to happen.
You can find more information about:
- Care Programme Approach by clicking here.
- Planning your care. Advance statements and advance decisions by clicking here.
- Mood stabilisers by clicking here.
- Antipsychotics by clicking here.
- Antidepressants by clicking here.
- Medication. Choice and managing problems by clicking here.
- Talking therapies by clicking here.
What if I’m not happy with my treatment?
If you aren’t happy with your treatment you can:
- talk to your doctor about your treatment options,
- ask for a second opinion,
- get an advocate to help you speak to your doctor,
- contact Patient Advice and Liaison Service (PALS), or
- make a complaint.

There is more information about these options below.
How can I speak to my doctor about my treatment options?
You can speak to your doctor about your treatment. Explain why you aren’t happy with it. You could ask what other treatments you could try.
Tell your doctor if there is a type of treatment that you would like to try. Doctors should listen to your preference. If you aren’t given this treatment, ask your doctor to explain why it isn’t suitable for you.
What’s a second opinion?
A second opinion means that you would like a different doctor to give their opinion about what treatment you should have. You can also ask for a second opinion if you disagree with your diagnosis.
You don’t have a right to a second opinion. But your doctor should listen to your reason for wanting a second opinion.
What is advocacy?
An advocate is independent from the mental health service. They are free to use. They can be useful if you find it difficult to get your views heard.
There are different types of advocates available. Community advocates can support you to get a health professional to listen to your concerns. And help you to get the treatment that you would like. NHS complaints advocates can help you if you want to complain about the NHS.
You can search online to search for a local advocacy service.
What is the Patient Advice and Liaison Service (PALS)?
PALS is part of the NHS. They give information and support to patients and a good place to start if you’re not happy with any aspect of the NHS.
You can find your local PALS’ details through this website link:
www.nhs.uk/Service-Search/Patient-advice-and-liaison-services-(PALS)/LocationSearch/363.
How can I complain?
You can complain about your treatment or any other aspect of the NHS verbally or in writing. See our information on ‘Complaining about the NHS or social services’ for more information.
You can find out more about:
- Medication.
 Choice and managing problems by clicking here.
Choice and managing problems by clicking here. - Second opinions by clicking here.
- Advocacy by clicking here.
- Complaining about the NHS or social services by clicking here.
What can I do to manage my symptoms?
You can learn to manage your symptoms by looking after yourself. Selfcare is how you take care of your diet, sleep, exercise, daily routine, relationships and how you are feeling.
What lifestyle changes can I make?
Making small lifestyle changes can improve your wellbeing and can help your recovery.
Routine helps many people with their mental wellbeing. It will help to give a structure to your day and may give you a sense of purpose. This could be a simple routine such as eating at the same time each day, going to bed at the same time each day and buying food once per week.
Your healthcare professionals should offer you a combined healthy eating, exercise and sleep programme.
You can find more information about wellbeing any physical health at:
www. rethink.org/advice-and-information/living-with-mental-illness/wellbeing-physical-health/.
rethink.org/advice-and-information/living-with-mental-illness/wellbeing-physical-health/.
What are support groups?
You could join a support group. A support group is where people come together to share information, experiences and give each other support.
You might be able to find a local group by searching online. The charity Bipolar UK have an online support group. They also have face to face support groups in some areas of the country. Their contact details are in the Useful contacts at the bottom of this page.
Rethink Mental Illness have support groups in some areas. You can find out what is available in your area if you follow this link: www.rethink.org/about-us/our-support-groups. Or you can contact our General Enquiries team on 0121 522 7007 or [email protected] for more information.
What are recovery colleges?
Recovery colleges are part of the NHS. They offer free courses about mental health to help you manage your symptoms. They can help you to take control of your life and become an expert in your own wellbeing and recovery. You can usually self-refer to a recovery college. But the college may inform your care team.
You can usually self-refer to a recovery college. But the college may inform your care team.
Unfortunately, recovery colleges aren’t available in all areas. To see if there is a recovery college in your area you can use a search engine such as Google.
What is a Wellness Recovery Action Plan (WRAP)?
Learning to spot early signs of mania or depression is important in self-management. The idea of the WRAP is to help you stay well and achieve what you would like to. The WRAP looks at areas like how you are affected by your illness and what you could do to manage them.
There are guides that can help with this. You can ask your healthcare professional to make one with you or ask them for a template of one. There is more information about the WRAP in the further reading section at the bottom of this page.
Rethink Mental Illness has created a guide called ‘Staying well with bipolar’. This is a guide based on information from people who have or support someone with bipolar disorder. You can download it here:
You can download it here:
www.rethink.org/living-with-mental-illness/staying-well-with-bipolar.
You can find more information about ‘Recovery’ by clicking here.
Bipolar disorder - Symptoms and causes
Overview
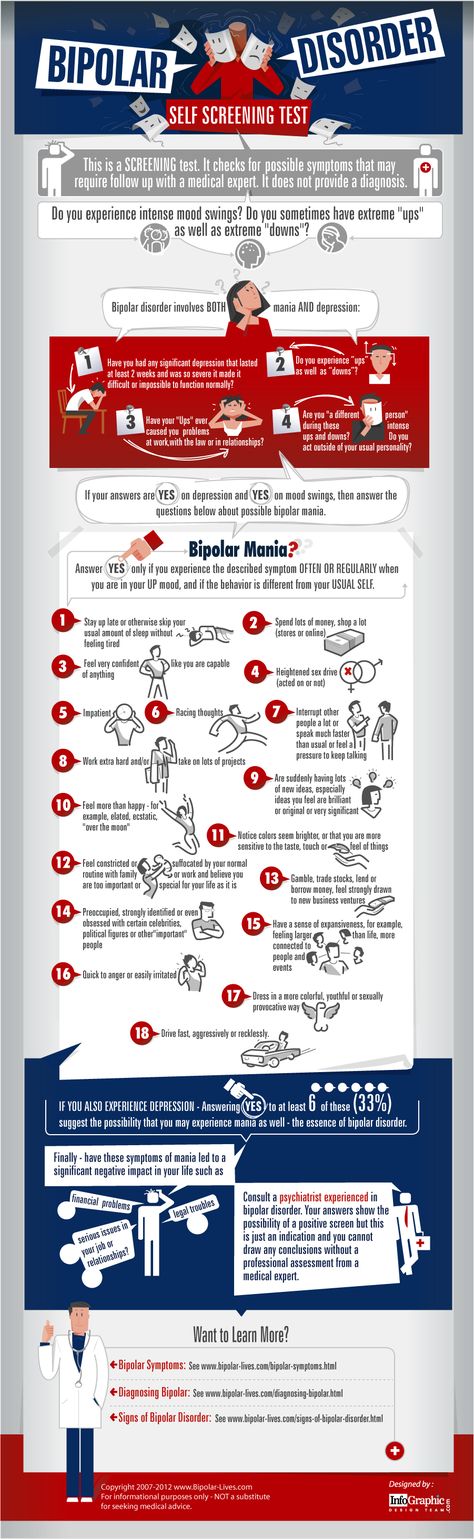
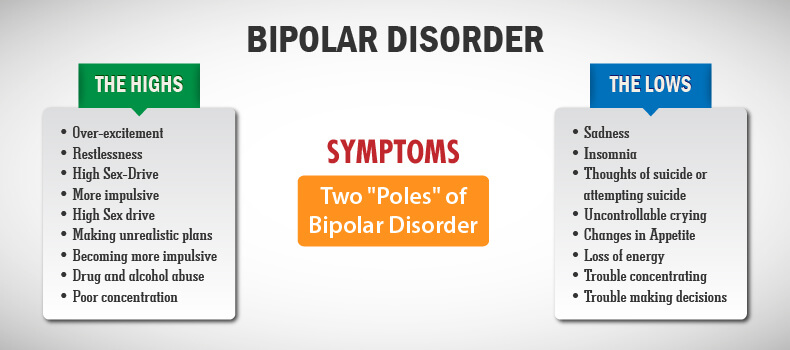
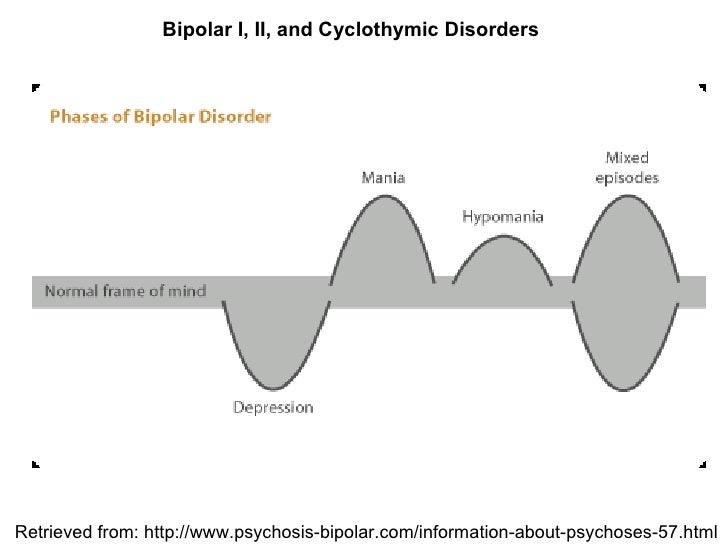
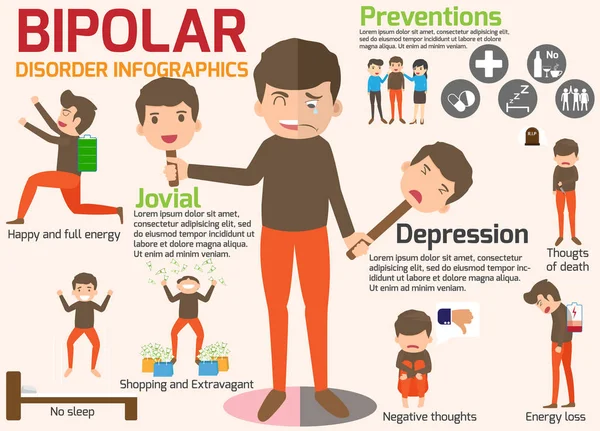
Bipolar disorder, formerly called manic depression, is a mental health condition that causes extreme mood swings that include emotional highs (mania or hypomania) and lows (depression).
When you become depressed, you may feel sad or hopeless and lose interest or pleasure in most activities. When your mood shifts to mania or hypomania (less extreme than mania), you may feel euphoric, full of energy or unusually irritable. These mood swings can affect sleep, energy, activity, judgment, behavior and the ability to think clearly.
Episodes of mood swings may occur rarely or multiple times a year. While most people will experience some emotional symptoms between episodes, some may not experience any.
Although bipolar disorder is a lifelong condition, you can manage your mood swings and other symptoms by following a treatment plan. In most cases, bipolar disorder is treated with medications and psychological counseling (psychotherapy).
In most cases, bipolar disorder is treated with medications and psychological counseling (psychotherapy).
Bipolar disorder care at Mayo Clinic
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
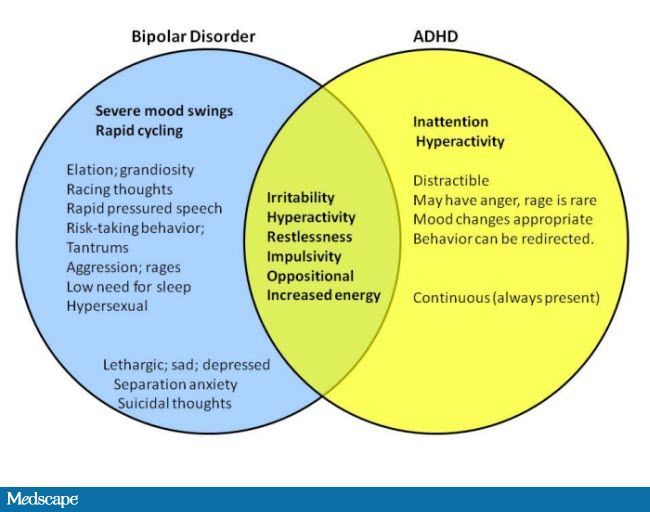
There are several types of bipolar and related disorders. They may include mania or hypomania and depression. Symptoms can cause unpredictable changes in mood and behavior, resulting in significant distress and difficulty in life.
- Bipolar I disorder. You've had at least one manic episode that may be preceded or followed by hypomanic or major depressive episodes. In some cases, mania may trigger a break from reality (psychosis).
- Bipolar II disorder. You've had at least one major depressive episode and at least one hypomanic episode, but you've never had a manic episode.
- Cyclothymic disorder.
 You've had at least two years — or one year in children and teenagers — of many periods of hypomania symptoms and periods of depressive symptoms (though less severe than major depression).
You've had at least two years — or one year in children and teenagers — of many periods of hypomania symptoms and periods of depressive symptoms (though less severe than major depression). - Other types. These include, for example, bipolar and related disorders induced by certain drugs or alcohol or due to a medical condition, such as Cushing's disease, multiple sclerosis or stroke.
Bipolar II disorder is not a milder form of bipolar I disorder, but a separate diagnosis. While the manic episodes of bipolar I disorder can be severe and dangerous, individuals with bipolar II disorder can be depressed for longer periods, which can cause significant impairment.
Although bipolar disorder can occur at any age, typically it's diagnosed in the teenage years or early 20s. Symptoms can vary from person to person, and symptoms may vary over time.
Mania and hypomania
Mania and hypomania are two distinct types of episodes, but they have the same symptoms.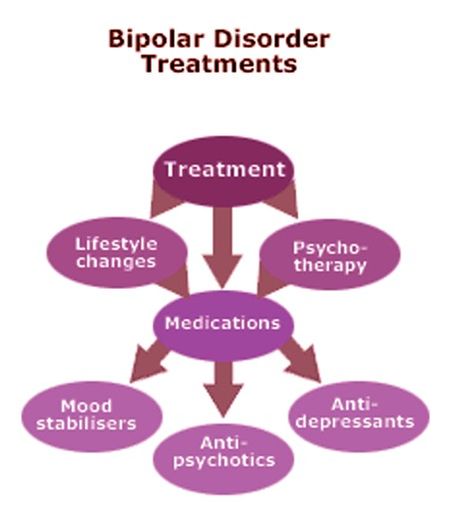 Mania is more severe than hypomania and causes more noticeable problems at work, school and social activities, as well as relationship difficulties. Mania may also trigger a break from reality (psychosis) and require hospitalization.
Mania is more severe than hypomania and causes more noticeable problems at work, school and social activities, as well as relationship difficulties. Mania may also trigger a break from reality (psychosis) and require hospitalization.
Both a manic and a hypomanic episode include three or more of these symptoms:
- Abnormally upbeat, jumpy or wired
- Increased activity, energy or agitation
- Exaggerated sense of well-being and self-confidence (euphoria)
- Decreased need for sleep
- Unusual talkativeness
- Racing thoughts
- Distractibility
- Poor decision-making — for example, going on buying sprees, taking sexual risks or making foolish investments
Major depressive episode
A major depressive episode includes symptoms that are severe enough to cause noticeable difficulty in day-to-day activities, such as work, school, social activities or relationships. An episode includes five or more of these symptoms:
- Depressed mood, such as feeling sad, empty, hopeless or tearful (in children and teens, depressed mood can appear as irritability)
- Marked loss of interest or feeling no pleasure in all — or almost all — activities
- Significant weight loss when not dieting, weight gain, or decrease or increase in appetite (in children, failure to gain weight as expected can be a sign of depression)
- Either insomnia or sleeping too much
- Either restlessness or slowed behavior
- Fatigue or loss of energy
- Feelings of worthlessness or excessive or inappropriate guilt
- Decreased ability to think or concentrate, or indecisiveness
- Thinking about, planning or attempting suicide
Other features of bipolar disorder
Signs and symptoms of bipolar I and bipolar II disorders may include other features, such as anxious distress, melancholy, psychosis or others.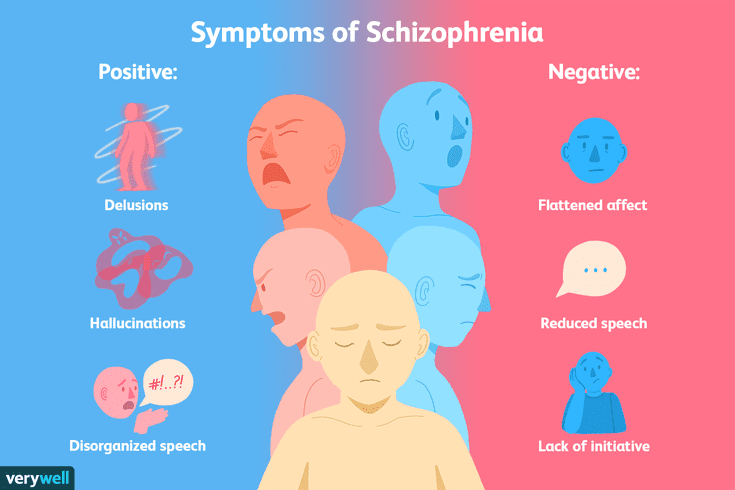 The timing of symptoms may include diagnostic labels such as mixed or rapid cycling. In addition, bipolar symptoms may occur during pregnancy or change with the seasons.
The timing of symptoms may include diagnostic labels such as mixed or rapid cycling. In addition, bipolar symptoms may occur during pregnancy or change with the seasons.
Symptoms in children and teens
Symptoms of bipolar disorder can be difficult to identify in children and teens. It's often hard to tell whether these are normal ups and downs, the results of stress or trauma, or signs of a mental health problem other than bipolar disorder.
Children and teens may have distinct major depressive or manic or hypomanic episodes, but the pattern can vary from that of adults with bipolar disorder. And moods can rapidly shift during episodes. Some children may have periods without mood symptoms between episodes.
The most prominent signs of bipolar disorder in children and teenagers may include severe mood swings that are different from their usual mood swings.
When to see a doctor
Despite the mood extremes, people with bipolar disorder often don't recognize how much their emotional instability disrupts their lives and the lives of their loved ones and don't get the treatment they need.
And if you're like some people with bipolar disorder, you may enjoy the feelings of euphoria and cycles of being more productive. However, this euphoria is always followed by an emotional crash that can leave you depressed, worn out — and perhaps in financial, legal or relationship trouble.
If you have any symptoms of depression or mania, see your doctor or mental health professional. Bipolar disorder doesn't get better on its own. Getting treatment from a mental health professional with experience in bipolar disorder can help you get your symptoms under control.
When to get emergency help
Suicidal thoughts and behavior are common among people with bipolar disorder. If you have thoughts of hurting yourself, call 911 or your local emergency number immediately, go to an emergency room, or confide in a trusted relative or friend. Or contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline, available 24 hours a day, seven days a week. Or use the Lifeline Chat. Services are free and confidential.
Or use the Lifeline Chat. Services are free and confidential.
If you have a loved one who is in danger of suicide or has made a suicide attempt, make sure someone stays with that person. Call 911 or your local emergency number immediately. Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
Request an appointment
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health. Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information.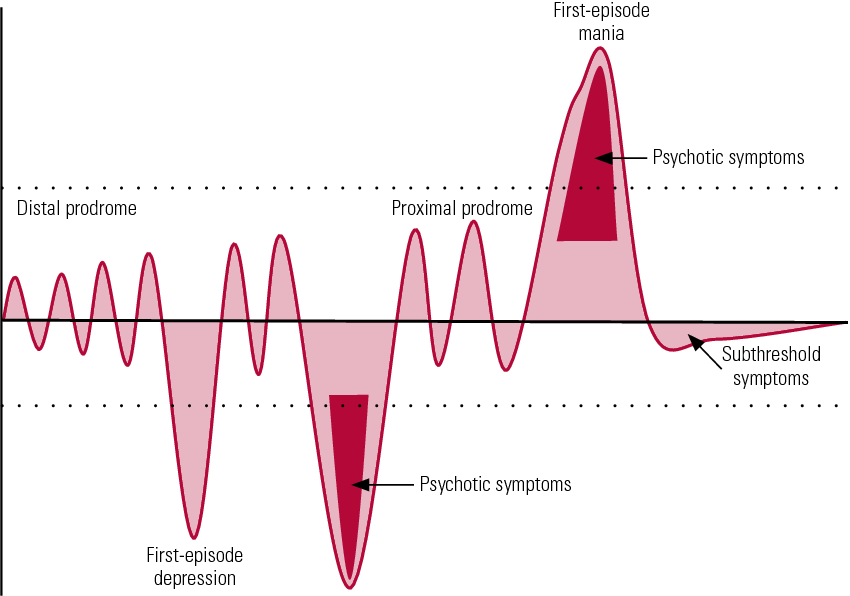 If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Causes
The exact cause of bipolar disorder is unknown, but several factors may be involved, such as:
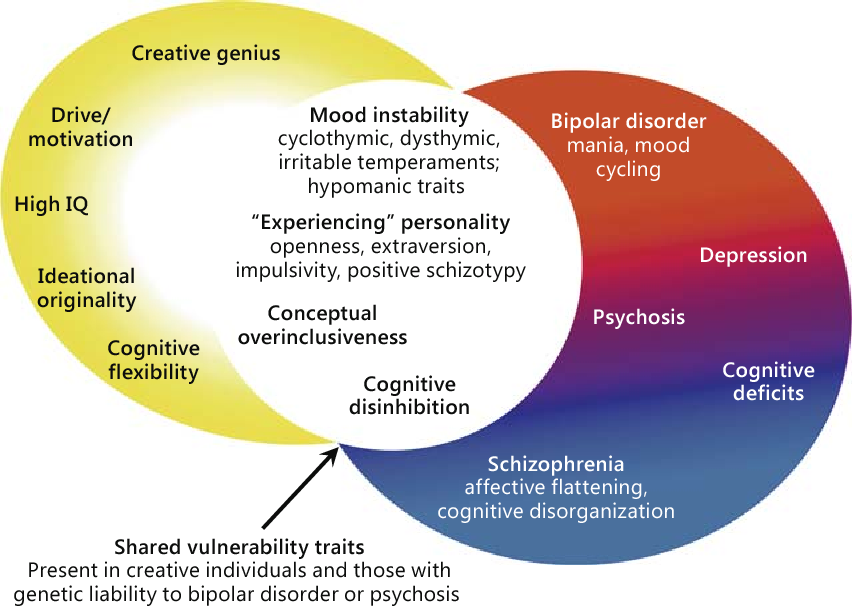
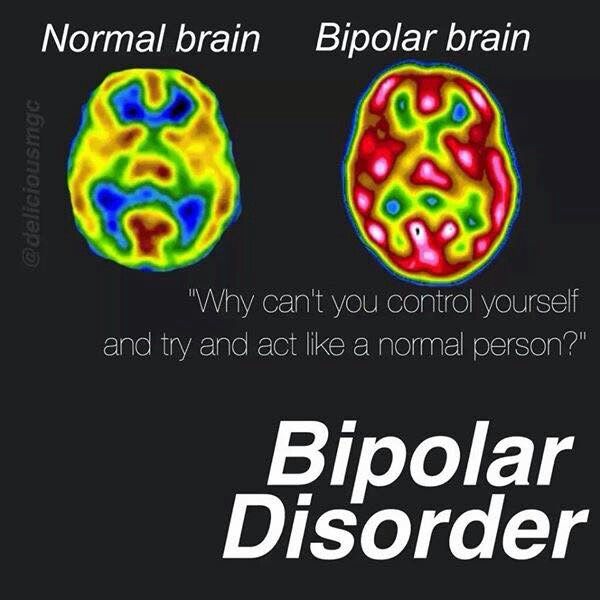
- Biological differences. People with bipolar disorder appear to have physical changes in their brains. The significance of these changes is still uncertain but may eventually help pinpoint causes.
- Genetics. Bipolar disorder is more common in people who have a first-degree relative, such as a sibling or parent, with the condition. Researchers are trying to find genes that may be involved in causing bipolar disorder.
Risk factors
Factors that may increase the risk of developing bipolar disorder or act as a trigger for the first episode include:
- Having a first-degree relative, such as a parent or sibling, with bipolar disorder
- Periods of high stress, such as the death of a loved one or other traumatic event
- Drug or alcohol abuse
Complications
Left untreated, bipolar disorder can result in serious problems that affect every area of your life, such as:
- Problems related to drug and alcohol use
- Suicide or suicide attempts
- Legal or financial problems
- Damaged relationships
- Poor work or school performance
Co-occurring conditions
If you have bipolar disorder, you may also have another health condition that needs to be treated along with bipolar disorder. Some conditions can worsen bipolar disorder symptoms or make treatment less successful. Examples include:
- Anxiety disorders
- Eating disorders
- Attention-deficit/hyperactivity disorder (ADHD)
- Alcohol or drug problems
- Physical health problems, such as heart disease, thyroid problems, headaches or obesity
More Information
- Bipolar disorder care at Mayo Clinic
- Bipolar disorder and alcoholism: Are they related?
Prevention
There's no sure way to prevent bipolar disorder. However, getting treatment at the earliest sign of a mental health disorder can help prevent bipolar disorder or other mental health conditions from worsening.
However, getting treatment at the earliest sign of a mental health disorder can help prevent bipolar disorder or other mental health conditions from worsening.
If you've been diagnosed with bipolar disorder, some strategies can help prevent minor symptoms from becoming full-blown episodes of mania or depression:
- Pay attention to warning signs. Addressing symptoms early on can prevent episodes from getting worse. You may have identified a pattern to your bipolar episodes and what triggers them. Call your doctor if you feel you're falling into an episode of depression or mania. Involve family members or friends in watching for warning signs.
- Avoid drugs and alcohol. Using alcohol or recreational drugs can worsen your symptoms and make them more likely to come back.
- Take your medications exactly as directed. You may be tempted to stop treatment — but don't. Stopping your medication or reducing your dose on your own may cause withdrawal effects or your symptoms may worsen or return.
By Mayo Clinic Staff
Related
Associated Procedures
News from Mayo Clinic
Products & Services
Bipolar affective disorder (BAD), its signs, types and methods of treatment
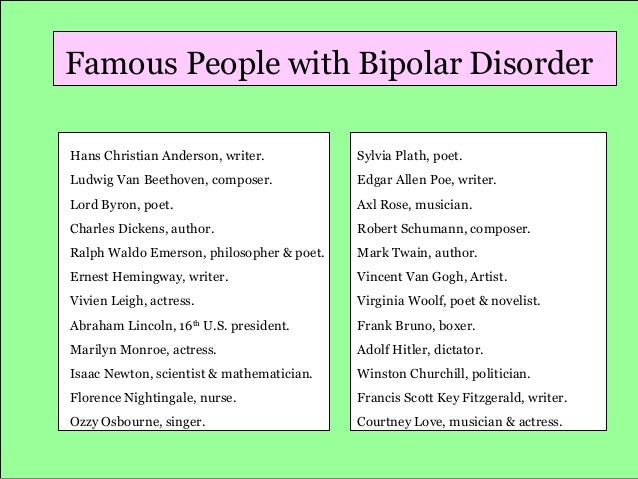
Manifestations of various emotions, a change in a person's mood, manifestations of both sadness and joy are normal and depend on many factors - from temperament and character to ongoing events that influence from the outside. However, when these changes are excessive, often unexpected and for no apparent reason, emotions get out of control, or a person remains in a radically positive or negative mood for a long time, it is very likely that bipolar disorder can be diagnosed. This disease was first described at the end of 19century, the famous German psychiatrist Emil Kripelin, calling it manic-depressive psychosis. Many world famous personalities such as Vincent van Gogh, Isaac Newton, Ludwig van Beethoven, Abraham Lincoln suffered from this disease.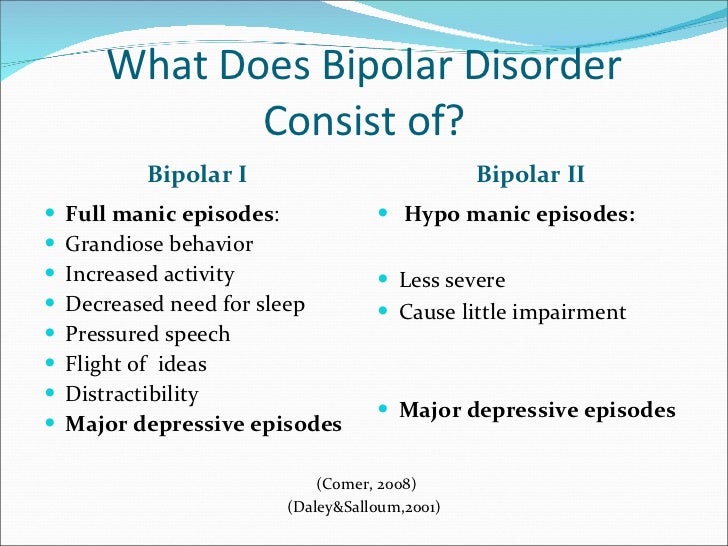 The pronounced form of this disease, which in the international classification of diseases is called bipolar affective disorder (BAD), is detected in 3% of the world's population.
The pronounced form of this disease, which in the international classification of diseases is called bipolar affective disorder (BAD), is detected in 3% of the world's population.
CONTENT OF THE ARTICLE
- 1. Bipolar Personality Disorder - Overview
- 2. Symptoms and signs
- 3. Types of Bipolar Disorder
- 4. Phases of Bipolar Disorder
- 5. Bipolar disorder in women
- 6. Treatment of Bipolar Personality Disorder
It is not uncommon for women to be treated with a combination of drug therapy and cognitive behavioral or interpersonal therapy with a psychotherapist.
Bipolar personality disorder - general information
According to statistics, bipolar disorder affects people from 14 to 44 years old. Unlike adults, children and adolescents experience more frequent mood swings from mania to depression, sometimes several times a day. 90% of young people make their debut precisely from the phase of depression or melancholy. Another feature of bipolar disorder is that, due to the low level of diagnosis, the patient can live with this disease for 5-10 years without knowing the cause of the painful symptoms.
Another feature of bipolar disorder is that, due to the low level of diagnosis, the patient can live with this disease for 5-10 years without knowing the cause of the painful symptoms.
Most often, bipolar disorder is diagnosed in people whose immediate family members have had a similar problem. The causes of this disease are unknown, but stress, overstrain, and various diseases can provoke the manifestation of its symptoms. However, having fenced off a person from the influence of these factors, it is impossible to get rid of the problem, you need to seek help from a psychotherapist.
Bipolar disorder is a disease that cannot be completely cured. But with properly selected medication and psychotherapy, the quality of life is significantly improved and the periods between phases are lengthened. The person remains socialized and able to work.
Symptoms and signs
From the name it is clear that we are talking about two different poles of affective manifestations, that is, mood manifestations. One of these conditions is depression. Depression in bipolar disorder is pronounced, with vivid symptoms. It can last up to a year and is manifested not only by low mood, lack of ability to enjoy and interest in ongoing events, but also by psychosis, when ideas of self-accusation arise, the patient feels inferior, unnecessary, poisoning the life of others. There are also nihilistic thoughts about suffering from some kind of severe illness, despite medical evidence to the contrary. There may be delusional thoughts, as well as suicidal thoughts and even attempts.
One of these conditions is depression. Depression in bipolar disorder is pronounced, with vivid symptoms. It can last up to a year and is manifested not only by low mood, lack of ability to enjoy and interest in ongoing events, but also by psychosis, when ideas of self-accusation arise, the patient feels inferior, unnecessary, poisoning the life of others. There are also nihilistic thoughts about suffering from some kind of severe illness, despite medical evidence to the contrary. There may be delusional thoughts, as well as suicidal thoughts and even attempts.
The other pole of bipolar disorder is a hypomanic state or hypomania, the characteristic features of which are an increased euphoric emotional background, the patient is constantly on the move, hyperactive, and is distinguished by very fast, associative speech. The patient is constantly cheerful, often hypersexual, almost always awake or sleeping 2-3 hours a day.
Hypomania is often followed by a manic bipolar state with psychotic manifestations. The patient develops convictions in his own greatness, he believes that he is capable of anything, feels that he has a special calling in this world or that he is a descendant of great people. In extended manic episodes of mania with psychotic manifestations, anger, irritability, and direct aggression often occur. This condition leads the patient into extremely unpleasant and sometimes dangerous situations.
The patient develops convictions in his own greatness, he believes that he is capable of anything, feels that he has a special calling in this world or that he is a descendant of great people. In extended manic episodes of mania with psychotic manifestations, anger, irritability, and direct aggression often occur. This condition leads the patient into extremely unpleasant and sometimes dangerous situations.
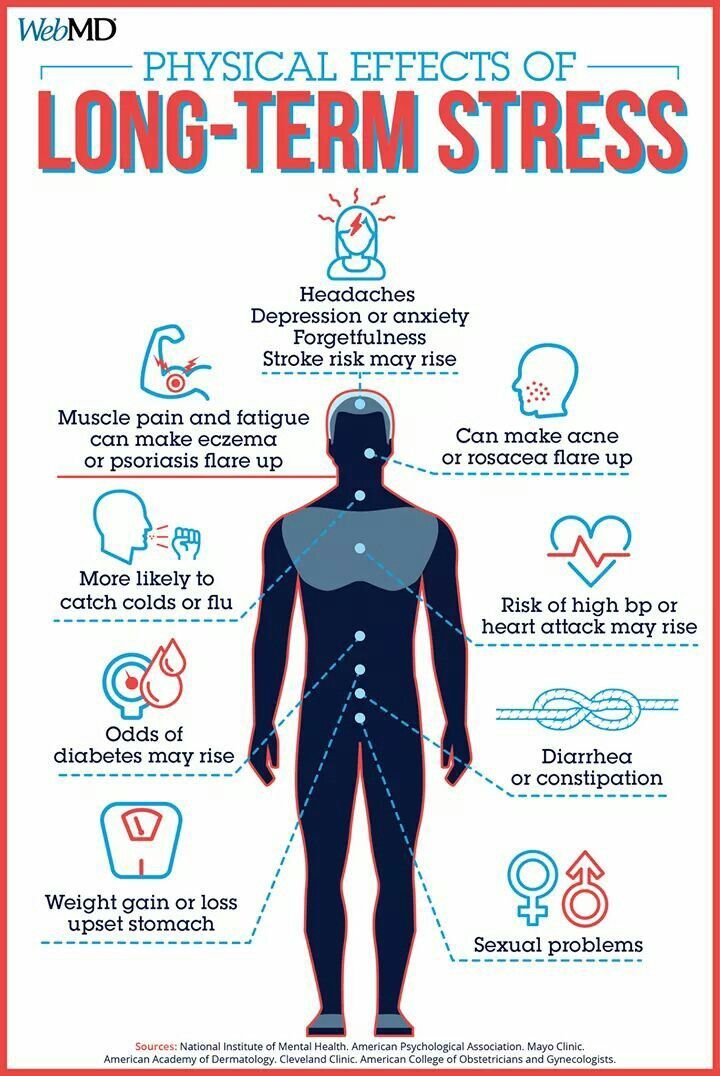
In addition to the typical symptoms of the disease, there are a large number of comorbid mental disorders. Comorbid mental disorders are those that accompany the underlying disease. The most common disorder of this kind is anxiety, which is manifested, among other things, by nonspecific autonomic symptoms, including sweating, palpitations, tremors of the limbs, various disorders of the gastrointestinal tract, dizziness, headaches, suffocation, and many others. In the case when these symptoms occur suddenly, mainly in public places, they are called panic attacks.
Types of bipolar disorder
Bipolar disorder can be of Ι and ΙΙ types.
Bipolar I disorder is a condition in which the patient has persistent manias, i.e. overexcitation, enthusiastic inappropriate behavior, manic psychosis, as well as severe depressions. Symptoms of this type are more severe, so hospitalization is indicated in most cases.
Bipolar I disorder is characterized by short periods of hypomania followed by periods of deep depression. Hypomania is a pre-manic state with less active manifestations. Hypomania lasts a very short period of time - from several days to several hours, so sometimes patients do not even notice them and do not inform the doctor about it. Only careful, painstaking work with the patient makes it possible to identify hypomania, make the correct diagnosis and prescribe treatment.
Phases of bipolar disorder
There are several phases of bipolar personality disorder:
- Depressive (unipolar depression). People experience a depressed mood, despair and despondency, complain of a lack of energy and mental concentration, they can either eat too much or too little and sleep.
At the peak of bipolar depressive disorder, depersonalization and derealization may occur. The boundaries of their own "I" and the world around them become blurred, patients experience difficulties in perceiving what is happening. Familiar places seem new, the colors of the surrounding world change, the patient constantly experiences a feeling of "déjà vu". Sounds become muffled, even if someone is talking very close, it seems to the patient that the voice is coming from afar.
- Manic (hypomanic). In this state, patients are full of energy, overly happy or optimistic, euphoric, and have extremely high self-esteem. At first glance, these are positive signs, but when a person experiences large-scale manic episodes, these symptoms and such an emotional state can reach dangerous extremes. A patient in this phase may indiscriminately spend huge amounts of money or behave carelessly, not realizing the full danger. In conversation, people may choke on words, speak at a high speed, or jump from one thought to another.
 These episodes may also be accompanied by delusions of grandeur or the adoption of serious decisions without thinking about the further consequences.
These episodes may also be accompanied by delusions of grandeur or the adoption of serious decisions without thinking about the further consequences.
In the development of the manic phase, the following stages of development can be distinguished:
- Hypomania - increased excitement, emotional upsurge.
- Mania - all signs are more pronounced, aggression, irritability, irascibility and rage are possible.
- Phase peak. The patient constantly experiences nervous excitement, he cannot relax. All his emotions are "heated" to the limit, coordination of movements is disturbed, thoughts are illogical and abrupt, in speech he constantly jumps from one sentence to another.
- Relief of symptoms. The patient gradually calms down. Movement disorders are on the decline. The speed of thinking and increased emotional mood remain unchanged.
- Return to normal.
- Mixed. Sometimes people have complaints that are characteristic of both depression and mania at the same time.
 They may also experience frequent phasing—4 or more episodes in one year.
They may also experience frequent phasing—4 or more episodes in one year.
In the intervals between depressive and manic phases in bipolar disorder, there is a light period during which the general background of mood becomes relatively stable, the person continues to adequately respond to certain events, the emotional sphere is under his control. This is the main criterion for remission of bipolar disease.
Bipolar disorder in women
Statistically, type Ι bipolar disorder occurs with the same frequency in men and women, and type ΙΙ disease is more often diagnosed in women. It is also known that the female course of the disease is characterized by rapid cycles and mixed episodes. Comorbidities often include eating disorders, borderline personality disorder, alcohol or drug addiction, and psychotropic drug abuse. Women are more susceptible to such somatic diseases as migraine (intense headaches), thyroid pathologies, diabetes, and obesity.
For women, a special technique is being developed to alleviate this disorder, since from adolescence to menopause there are specific changes in hormonal levels that must be taken into account. In addition, psychotropic substances, which are supposed to stabilize the condition, can adversely affect the intrauterine development of the fetus if the woman is in position. It is noted that in the first trimester of pregnancy this disorder is milder, but after childbirth they often have to deal with postpartum depression. Thus, at each stage of the development of the female body, a competent doctor must review and adjust the treatment regimen. Often in the treatment of women, a complex method is used that combines drug therapy and cognitive-behavioral or interpersonal therapy with a psychotherapist. This approach gives the fastest results.
In addition, psychotropic substances, which are supposed to stabilize the condition, can adversely affect the intrauterine development of the fetus if the woman is in position. It is noted that in the first trimester of pregnancy this disorder is milder, but after childbirth they often have to deal with postpartum depression. Thus, at each stage of the development of the female body, a competent doctor must review and adjust the treatment regimen. Often in the treatment of women, a complex method is used that combines drug therapy and cognitive-behavioral or interpersonal therapy with a psychotherapist. This approach gives the fastest results.
Treatment for bipolar disorder
Attempts to get rid of bipolar disorder on your own do not bring the desired result and, ultimately, lead to an aggravation of the situation, including the development of drug or alcohol addiction. In the diagnosis of the disease, keeping a mood diary can help, where the patient records all his thoughts, emotions, feelings, changes in mood.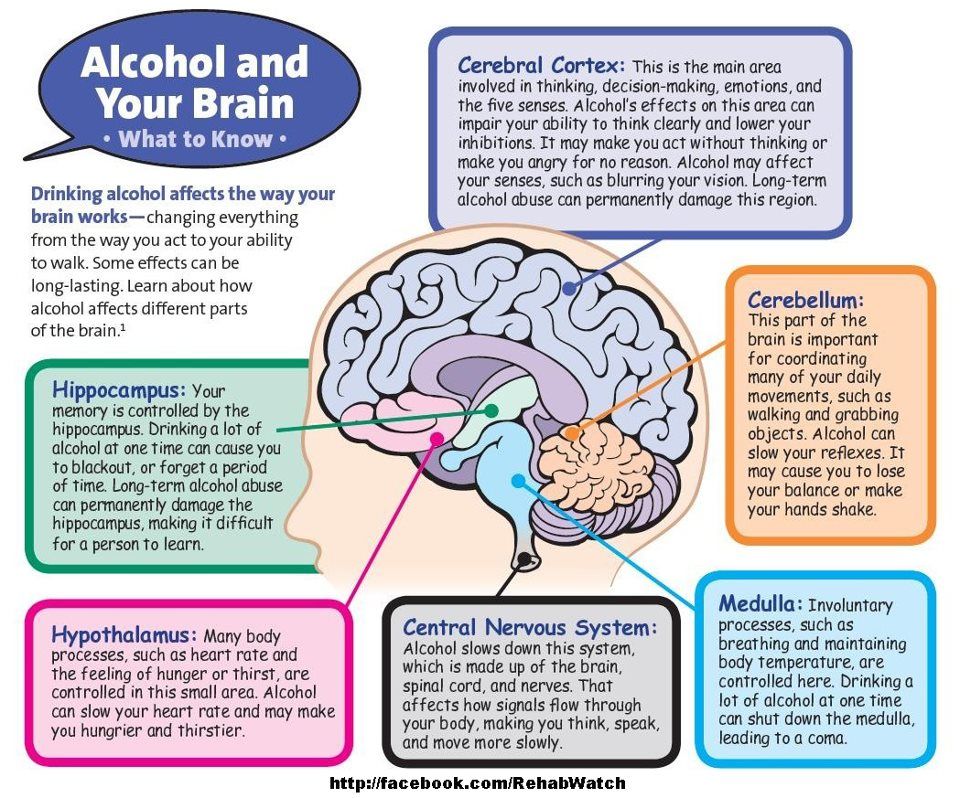 Such records will help the doctor to assess the mental state in detail and make the correct diagnosis. If you suspect bipolar disorder, you should consult a doctor, and the sooner a person realizes that he has a disease and comes to the clinic for help, the sooner professional help will be provided to him and painful symptoms will be replaced by a stable condition. It is impossible to get rid of the disease on your own, since a person cannot fully adequately assess not only his actions, but also the alternation of the phases of the disease.
Such records will help the doctor to assess the mental state in detail and make the correct diagnosis. If you suspect bipolar disorder, you should consult a doctor, and the sooner a person realizes that he has a disease and comes to the clinic for help, the sooner professional help will be provided to him and painful symptoms will be replaced by a stable condition. It is impossible to get rid of the disease on your own, since a person cannot fully adequately assess not only his actions, but also the alternation of the phases of the disease.
Bipolar disorder is one of the few mental disorders in which medication is indicated in 100% of cases, and psychotherapy is an auxiliary tool. This disease is incurable, but its diagnosis and treatment is extremely important. Treatment can reduce the number of episodes, their severity and intensity, as well as prevent negative life events, help prevent relationship breakups, job loss, and even suicidal attempts. Thus, the quality of life of a patient with bipolar disorder who is undergoing treatment will be several times higher than that of a person who neglects treatment. If the patient loses touch with reality and harms himself and others, he is subject to hospitalization, outpatient treatment in this case is not permissible.
If the patient loses touch with reality and harms himself and others, he is subject to hospitalization, outpatient treatment in this case is not permissible.
If you have a disease, it is recommended to exclude coffee, strong tea, alcoholic and energy drinks from your diet in order not to provoke an overexcited state. If possible, you should stop smoking and in no case should you take even soft drugs. It is also very important to establish a sleep pattern, sleep at least 8 hours a day and try to go to bed at about the same time. You should learn to recognize mood swings and notice the early manifestations of new episodes.
If you suspect that you have bipolar personality disorder, there is no need to panic, only a doctor can diagnose the disease, so you need to make an appointment with a psychotherapist with extensive experience in managing such patients at our MedAstrum clinic. If the diagnosis is confirmed, the doctor will make the necessary medication, if necessary, prescribe psychotherapeutic sessions and give recommendations for further lifestyle adjustments.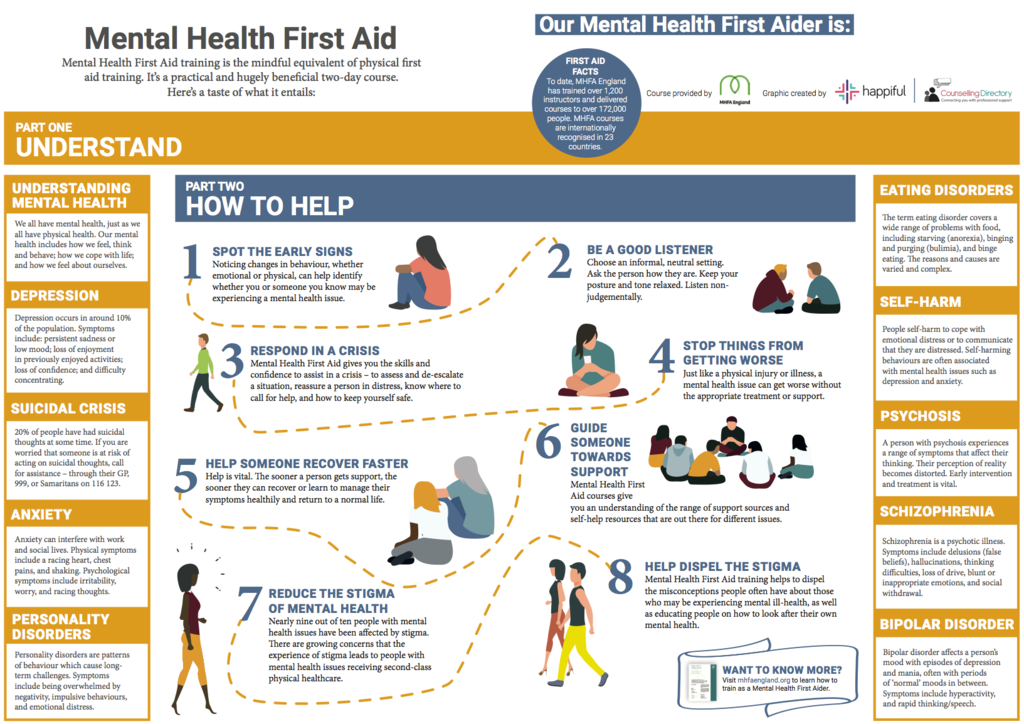 You can make an appointment yourself on the website or by contacting our administrators.
You can make an appointment yourself on the website or by contacting our administrators.
Bipolar disorder | Symptoms, complications, diagnosis and treatment
Bipolar disorder, formerly called manic depression, is a mental health condition that causes extreme mood swings that include emotional highs (mania or hypomania) and lows (depression). Episodes of mood swings may occur infrequently or several times a year.
When you become depressed, you may feel sad or hopeless and lose interest or pleasure in most activities. When the mood shifts to mania or hypomania (less extreme than mania), you may feel euphoric, full of energy or unusually irritable. These mood swings can affect sleep, energy, alertness, judgment, behavior, and the ability to think clearly.
Although bipolar disorder is a lifelong condition, you can manage your mood swings and other symptoms by following a treatment plan. In most cases, bipolar disorder is treated with medication and psychological counseling (psychotherapy).
Symptoms
There are several types of bipolar and related disorders. They may include mania, hypomania, and depression. The symptoms can lead to unpredictable changes in mood and behavior, leading to significant stress and difficulty in life.
- Bipolar I. You have had at least one manic episode, which may be preceded or accompanied by hypomanic or major depressive episodes. In some cases, mania can cause a break with reality (psychosis).
- Bipolar disorder II. You have had at least one major depressive episode and at least one hypomanic episode, but never had a manic episode.
- Cyclothymic disorder. You have had at least two years - or one year in children and adolescents - many periods of hypomanic symptoms and periods of depressive symptoms (though less severe than major depression).
- Other types. These include, for example, bipolar and related disorders caused by certain drugs or alcohol or due to health conditions such as Cushing's disease, multiple sclerosis, or stroke.
Bipolar II is not a milder form of Bipolar I but is a separate diagnosis. Although bipolar I manic episodes can be severe and dangerous, people with bipolar II can be depressed for longer periods of time, which can cause significant impairment.
Although bipolar disorder can occur at any age, it is usually diagnosed in adolescence or early twenties. Symptoms can vary from person to person, and symptoms can change over time.
Mania and hypomania
Mania and hypomania are two different types of episodes, but they share the same symptoms. Mania is more pronounced than hypomania and causes more noticeable problems at work, school, and social activities, as well as relationship difficulties. Mania can also cause a break with reality (psychosis) and require hospitalization.
Both a manic episode and a hypomanic episode include three or more of these symptoms:
- Abnormally optimistic or nervous
- Increased activity, energy or excitement
- Exaggerated sense of well-being and self-confidence (euphoria)
- Reduced need for sleep
- Unusual talkativeness
- Distractibility
- Poor decision-making - for example, in speculation, in sexual encounters or in irrational investments
Major depressive episode
Major depressive episode includes symptoms that are severe enough to cause noticeable difficulty in daily activities such as work, school, social activities, or relationships. Episode includes five or more of these symptoms:
Episode includes five or more of these symptoms:
- Depressed mood, such as feeling sad, empty, hopeless, or tearful (in children and adolescents, depressed mood may manifest as irritability)
- Marked loss of interest or feeling of displeasure in all (or nearly all) activities
- Significant weight loss with no diet, weight gain, or decreased or increased appetite (in children, failure to gain weight as expected may be a sign of depression)
- Either insomnia or sleeping too much
- Either restlessness or slow behavior
- Fatigue or loss of energy
- Feelings of worthlessness or excessive or inappropriate guilt
- Decreased ability to think or concentrate, or indecisiveness
- Thinking, planning or attempting suicide
Other features of bipolar disorder
Signs and symptoms of bipolar I and bipolar II disorder may include other signs such as anxiety disorder, melancholia, psychosis, or others.