Social anxiety disorder psychotherapy
Social anxiety disorder (social phobia) - Diagnosis and treatment
Diagnosis
Your health care provider will want to determine whether other conditions may be causing your anxiety or if you have social anxiety disorder along with another physical or mental health disorder.
Your health care provider may determine a diagnosis based on:
- Physical exam to help assess whether any medical condition or medication may trigger symptoms of anxiety
- Discussion of your symptoms, how often they occur and in what situations
- Review of a list of situations to see if they make you anxious
- Self-report questionnaires about symptoms of social anxiety
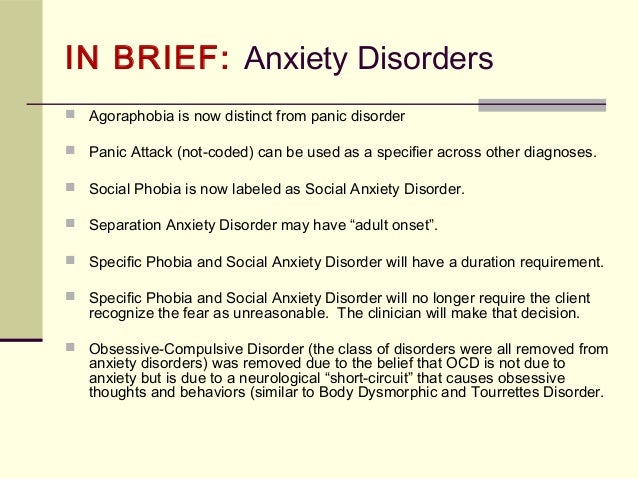
- Criteria listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association
DSM-5 criteria for social anxiety disorder include:
- Persistent, intense fear or anxiety about specific social situations because you believe you may be judged negatively, embarrassed or humiliated
- Avoidance of anxiety-producing social situations or enduring them with intense fear or anxiety
- Excessive anxiety that's out of proportion to the situation
- Anxiety or distress that interferes with your daily living
- Fear or anxiety that is not better explained by a medical condition, medication or substance abuse
Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your social anxiety disorder (social phobia)-related health concerns Start Here
Treatment
Treatment depends on how much social anxiety disorder affects your ability to function in daily life. The most common treatment for social anxiety disorder includes psychotherapy (also called psychological counseling or talk therapy) or medications or both.
Psychotherapy
Psychotherapy improves symptoms in most people with social anxiety disorder. In therapy, you learn how to recognize and change negative thoughts about yourself and develop skills to help you gain confidence in social situations.
Cognitive behavioral therapy (CBT) is the most effective type of psychotherapy for anxiety, and it can be equally effective when conducted individually or in groups.
In exposure-based CBT, you gradually work up to facing the situations you fear most. This can improve your coping skills and help you develop the confidence to deal with anxiety-inducing situations. You may also participate in skills training or role-playing to practice your social skills and gain comfort and confidence relating to others. Practicing exposures to social situations is particularly helpful to challenge your worries.
First choices in medications
Though several types of medications are available, selective serotonin reuptake inhibitors (SSRIs) are often the first type of drug tried for persistent symptoms of social anxiety. Your health care provider may prescribe paroxetine (Paxil) or sertraline (Zoloft).
The serotonin and norepinephrine reuptake inhibitor (SNRI) venlafaxine (Effexor XR) also may be an option for social anxiety disorder.
To reduce the risk of side effects, your health care provider may start you at a low dose of medication and gradually increase your prescription to a full dose. It may take several weeks to several months of treatment for your symptoms to noticeably improve.
Other medications
Your health care provider may also prescribe other medications for symptoms of social anxiety, such as:
- Other antidepressants. You may have to try several different antidepressants to find the one that's most effective for you with the fewest side effects.

- Anti-anxiety medications. Benzodiazepines (ben-zoe-die-AZ-uh-peens) may reduce your level of anxiety. Although they often work quickly, they can be habit-forming and sedating, so they're typically prescribed for only short-term use.
- Beta blockers. These medications work by blocking the stimulating effect of epinephrine (adrenaline). They may reduce heart rate, blood pressure, pounding of the heart, and shaking voice and limbs. Because of that, they may work best when used infrequently to control symptoms for a particular situation, such as giving a speech. They're not recommended for general treatment of social anxiety disorder.
Stick with it
Don't give up if treatment doesn't work quickly. You can continue to make strides in psychotherapy over several weeks or months. Learning new skills to help manage your anxiety takes time. And finding the right medication for your situation can take some trial and error.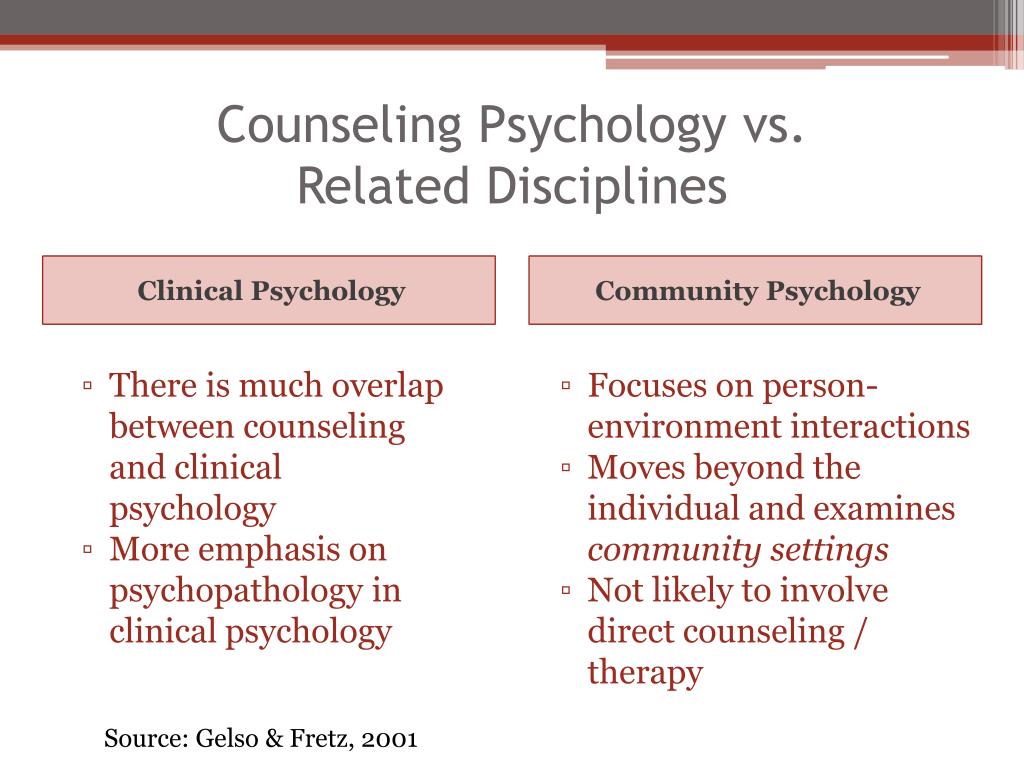
For some people, the symptoms of social anxiety disorder may fade over time, and medication can be discontinued. Others may need to take medication for years to prevent a relapse.
To make the most of treatment, keep your medical or therapy appointments, challenge yourself by setting goals to approach social situations that cause you anxiety, take medications as directed, and talk to your health care provider about any changes in your condition.
Alternative medicine
Several herbal remedies have been studied as treatments for anxiety, but results are mixed. Before taking any herbal remedies or supplements, talk with your health care team to make sure they're safe and won't interact with any medications you take.
More Information
- Social anxiety disorder (social phobia) care at Mayo Clinic
- Cognitive behavioral therapy
- Psychotherapy
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.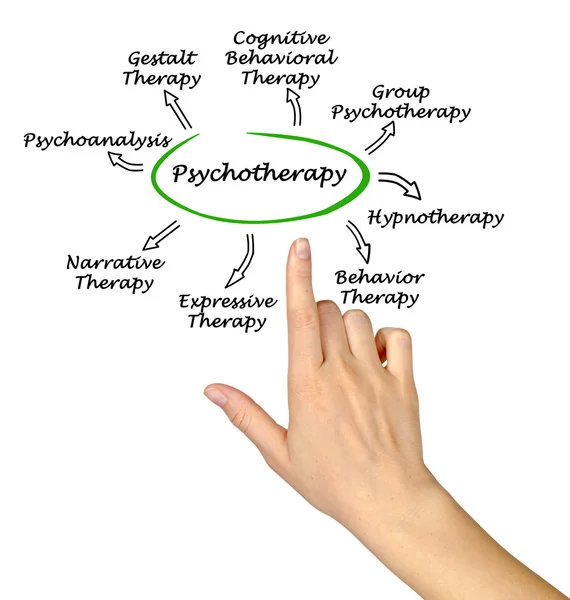
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Lifestyle and home remedies
Although social anxiety disorder generally requires help from a medical expert or qualified psychotherapist, you can try some of these techniques to handle situations that are likely to trigger symptoms:
- Learn stress-reduction skills.
- Get physical exercise or be physically active on a regular basis.
- Get enough sleep.
- Eat a healthy, well-balanced diet.
- Avoid alcohol.
- Limit or avoid caffeine.
- Participate in social situations by reaching out to people with whom you feel comfortable.
Practice in small steps
First, consider your fears to identify what situations cause the most anxiety. Then gradually practice these activities until they cause you less anxiety. Begin with small steps by setting daily or weekly goals in situations that aren't overwhelming. The more you practice, the less anxious you'll feel.
Consider practicing these situations:
- Eat with a close relative, friend or acquaintance in a public setting.
- Purposefully make eye contact and return greetings from others, or be the first to say hello.
- Give someone a compliment.
- Ask a retail clerk to help you find an item.

- Get directions from a stranger.
- Show an interest in others — ask about their homes, children, grandchildren, hobbies or travels, for instance.
- Call a friend to make plans.
Prepare for social situations
At first, being social when you're feeling anxious is challenging. As difficult or painful as it may seem initially, don't avoid situations that trigger your symptoms. By regularly facing these kinds of situations, you'll continue to build and reinforce your coping skills.
These strategies can help you begin to face situations that make you nervous:
- Prepare for conversation, for example, by reading about current events to identify interesting stories you can talk about.
- Focus on personal qualities you like about yourself.
- Practice relaxation exercises.
- Learn stress management techniques.
- Set realistic social goals.
- Pay attention to how often the embarrassing situations you're afraid of actually take place.
 You may notice that the scenarios you fear usually don't come to pass.
You may notice that the scenarios you fear usually don't come to pass. - When embarrassing situations do happen, remind yourself that your feelings will pass and you can handle them until they do. Most people around you either don't notice or don't care as much as you think, or they're more forgiving than you assume.
Avoid using alcohol to calm your nerves. It may seem like it helps temporarily, but in the long term it can make you feel even more anxious.
Coping and support
These coping methods may help ease your anxiety:
- Routinely reach out to friends and family members.
- Join a local or reputable internet-based support group.
- Join a group that offers opportunities to improve communication and public speaking skills, such as Toastmasters International.
- Do pleasurable or relaxing activities, such as hobbies, when you feel anxious.
Over time, these coping methods can help control your symptoms and prevent a relapse.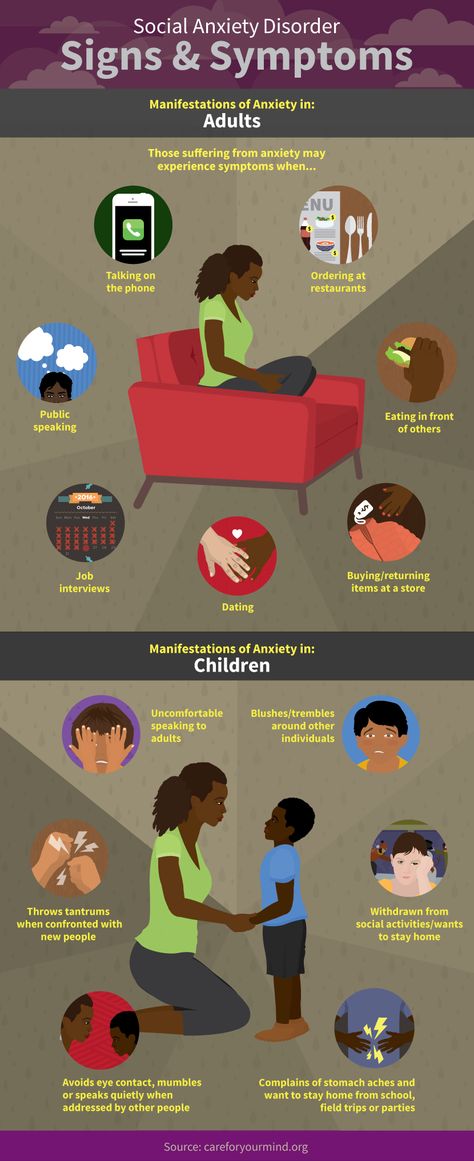 Remind yourself that you can get through anxious moments, that your anxiety is short-lived and that the negative consequences you worry about so much rarely come to pass.
Remind yourself that you can get through anxious moments, that your anxiety is short-lived and that the negative consequences you worry about so much rarely come to pass.
Preparing for your appointment
You may see your primary care provider, or your provider may refer you to a mental health professional. Here's some information to help you get ready for your appointment.
What you can do
Before your appointment, make a list of:
- Situations you've been avoiding, especially those that are important to your functioning
- Any symptoms you've been experiencing, and for how long, including any symptoms that may seem unrelated to the reason for your appointment
- Key personal information, especially any significant events or changes in your life shortly before your symptoms appeared
- Medical information, including other physical or mental health conditions with which you've been diagnosed
- Any medications, vitamins, herbs or other supplements you're taking, including dosages
- Questions to ask your health care provider or a mental health professional
You may want to ask a trusted family member or friend to go with you to your appointment, if possible, to help you remember key information.
Some questions to ask your health care provider may include:
- What do you believe is causing my symptoms?
- Are there any other possible causes?
- How will you determine my diagnosis?
- Should I see a mental health specialist?
- Is my condition likely temporary or chronic?
- Are effective treatments available for this condition?
- With treatment, could I eventually be comfortable in the situations that make me so anxious now?
- Am I at increased risk of other mental health problems?
- Are there any brochures or other printed material that I can have? What websites do you recommend?
Don't hesitate to ask other questions during your appointment.
What to expect from your health care provider
Your health care provider or a mental health professional will likely ask you a number of questions. Be ready to answer them to reserve time to go over any points you want to focus on.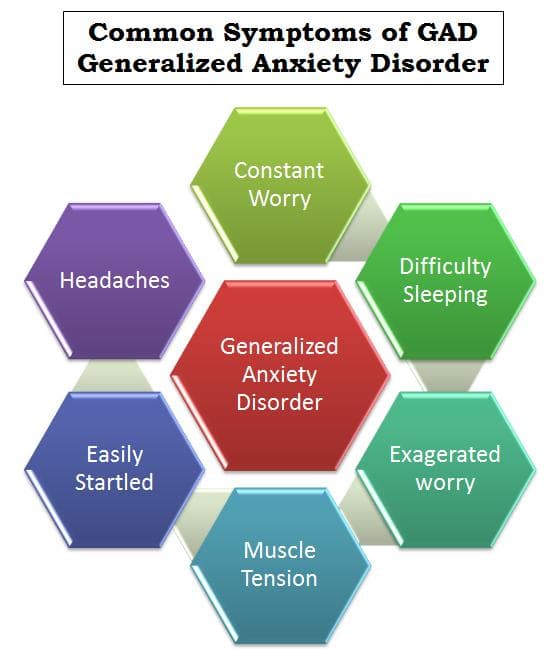 Your health care provider may ask:
Your health care provider may ask:
- Does fear of embarrassment cause you to avoid doing certain activities or speaking to people?
- Do you avoid activities in which you're the center of attention?
- Would you say that being embarrassed or looking stupid is among your worst fears?
- When did you first notice these symptoms?
- When are your symptoms most likely to occur?
- Does anything seem to make your symptoms better or worse?
- How are your symptoms affecting your life, including work and personal relationships?
- Do you ever have symptoms when you're not being observed by others?
- Have any of your close relatives had similar symptoms?
- Have you been diagnosed with any medical conditions?
- Have you been treated for mental health symptoms or mental illness in the past? If yes, what type of therapy was most beneficial?
- Have you ever thought about harming yourself or others?
- Do you drink alcohol or use recreational drugs? If so, how often?
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Social anxiety disorder (social phobia) - Symptoms and causes
Overview
It's normal to feel nervous in some social situations.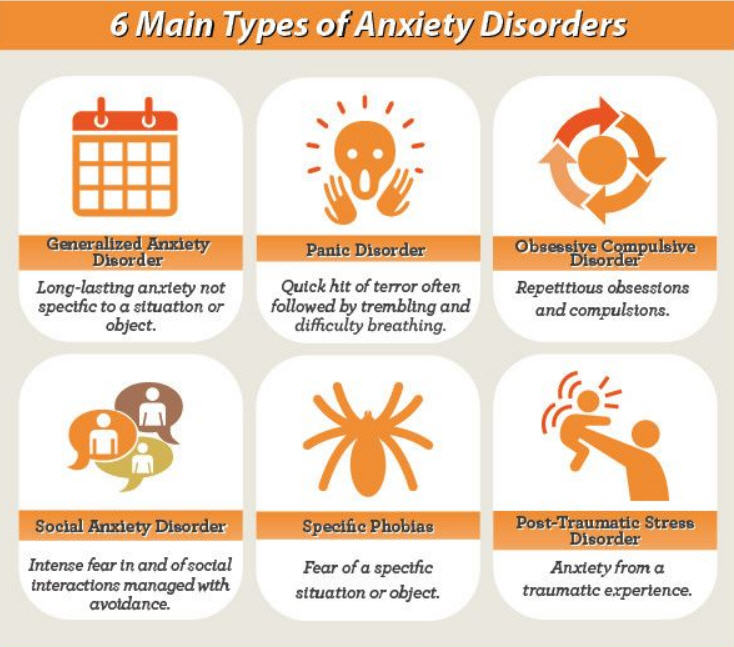 For example, going on a date or giving a presentation may cause that feeling of butterflies in your stomach. But in social anxiety disorder, also called social phobia, everyday interactions cause significant anxiety, self-consciousness and embarrassment because you fear being scrutinized or judged negatively by others.
For example, going on a date or giving a presentation may cause that feeling of butterflies in your stomach. But in social anxiety disorder, also called social phobia, everyday interactions cause significant anxiety, self-consciousness and embarrassment because you fear being scrutinized or judged negatively by others.
In social anxiety disorder, fear and anxiety lead to avoidance that can disrupt your life. Severe stress can affect your relationships, daily routines, work, school or other activities.
Social anxiety disorder can be a chronic mental health condition, but learning coping skills in psychotherapy and taking medications can help you gain confidence and improve your ability to interact with others.
Social anxiety disorder care at Mayo Clinic
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
Feelings of shyness or discomfort in certain situations aren't necessarily signs of social anxiety disorder, particularly in children.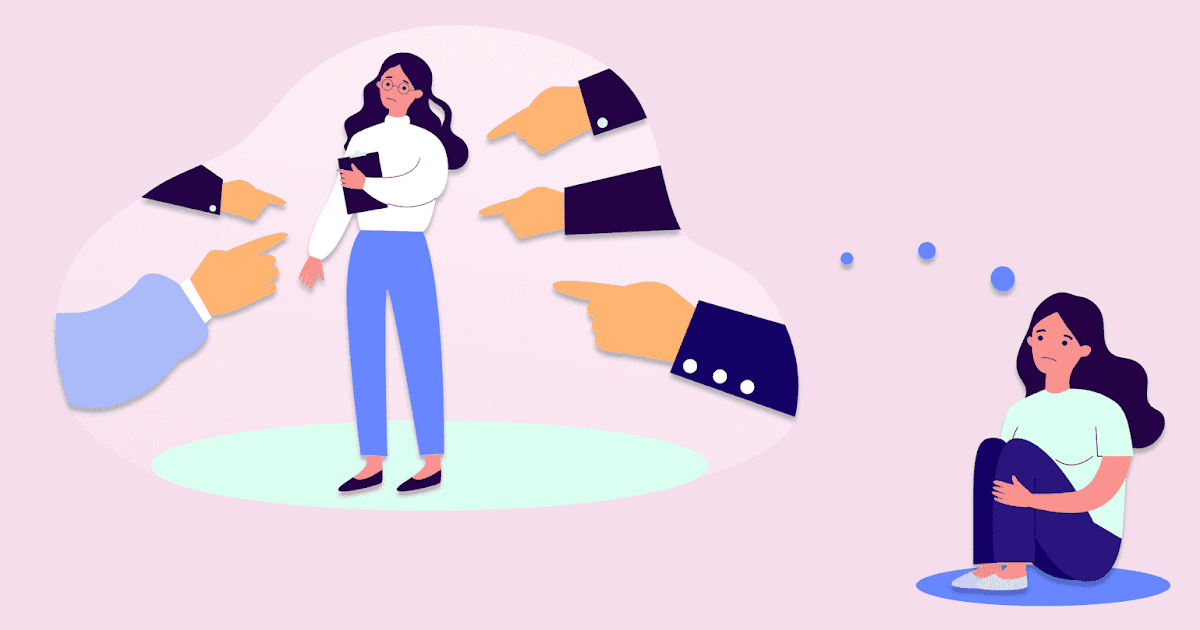 Comfort levels in social situations vary, depending on personality traits and life experiences. Some people are naturally reserved and others are more outgoing.
Comfort levels in social situations vary, depending on personality traits and life experiences. Some people are naturally reserved and others are more outgoing.
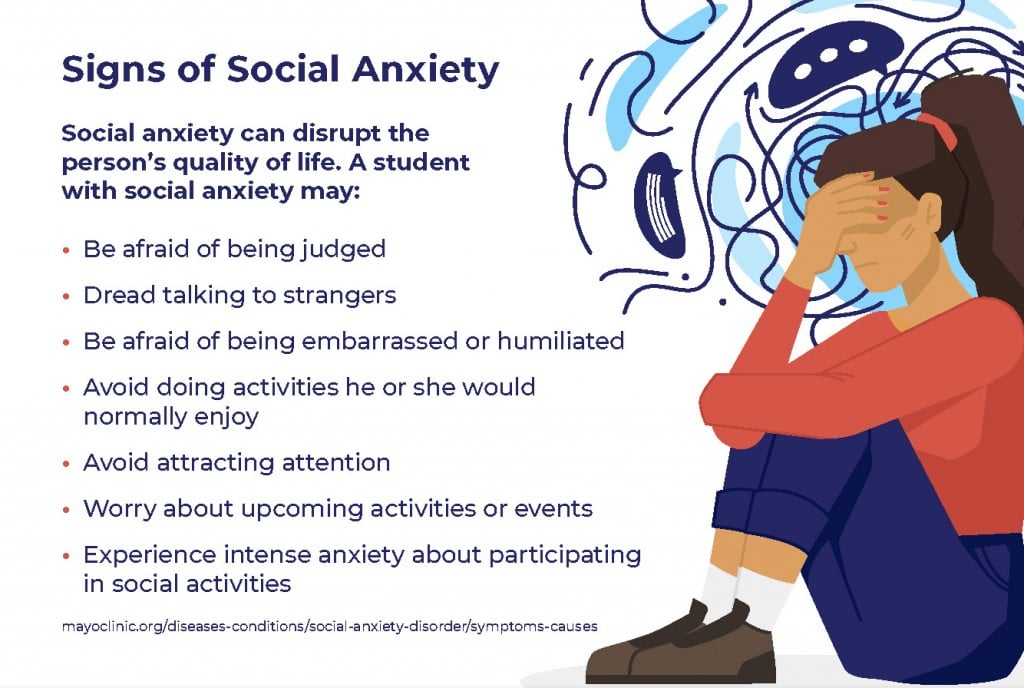
In contrast to everyday nervousness, social anxiety disorder includes fear, anxiety and avoidance that interfere with relationships, daily routines, work, school or other activities. Social anxiety disorder typically begins in the early to mid-teens, though it can sometimes start in younger children or in adults.
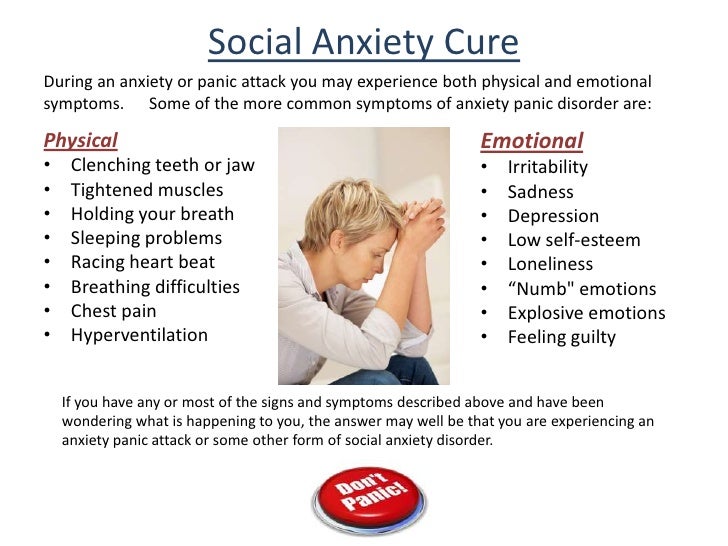
Emotional and behavioral symptoms
Signs and symptoms of social anxiety disorder can include constant:
- Fear of situations in which you may be judged negatively
- Worry about embarrassing or humiliating yourself
- Intense fear of interacting or talking with strangers
- Fear that others will notice that you look anxious
- Fear of physical symptoms that may cause you embarrassment, such as blushing, sweating, trembling or having a shaky voice
- Avoidance of doing things or speaking to people out of fear of embarrassment
- Avoidance of situations where you might be the center of attention
- Anxiety in anticipation of a feared activity or event
- Intense fear or anxiety during social situations
- Analysis of your performance and identification of flaws in your interactions after a social situation
- Expectation of the worst possible consequences from a negative experience during a social situation
For children, anxiety about interacting with adults or peers may be shown by crying, having temper tantrums, clinging to parents or refusing to speak in social situations.
Performance type of social anxiety disorder is when you experience intense fear and anxiety during speaking or performing in public but not in other types of more general social situations.
Physical symptoms
Physical signs and symptoms can sometimes accompany social anxiety disorder and may include:
- Blushing
- Fast heartbeat
- Trembling
- Sweating
- Upset stomach or nausea
- Trouble catching your breath
- Dizziness or lightheadedness
- Feeling that your mind has gone blank
- Muscle tension
Avoiding common social situations
Common, everyday experiences may be hard to endure when you have social anxiety disorder, including:
- Interacting with unfamiliar people or strangers
- Attending parties or social gatherings
- Going to work or school
- Starting conversations
- Making eye contact
- Dating
- Entering a room in which people are already seated
- Returning items to a store
- Eating in front of others
- Using a public restroom
Social anxiety disorder symptoms can change over time. They may flare up if you're facing a lot of changes, stress or demands in your life. Although avoiding situations that produce anxiety may make you feel better in the short term, your anxiety is likely to continue over the long term if you don't get treatment.
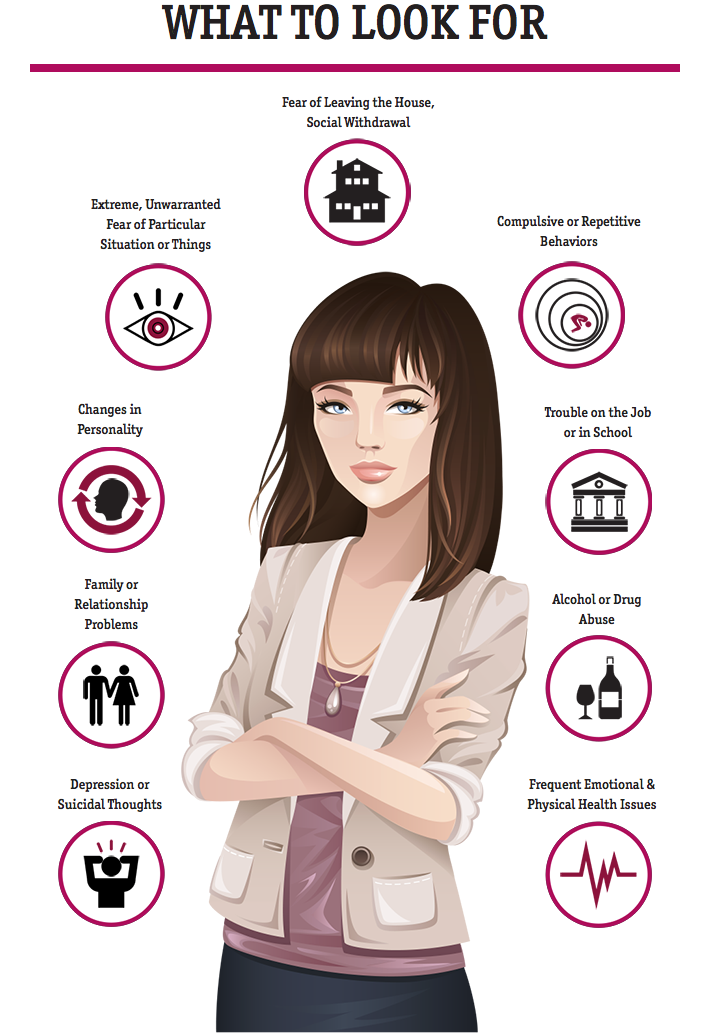
When to see a doctor
See your doctor or a mental health professional if you fear and avoid normal social situations because they cause embarrassment, worry or panic.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you.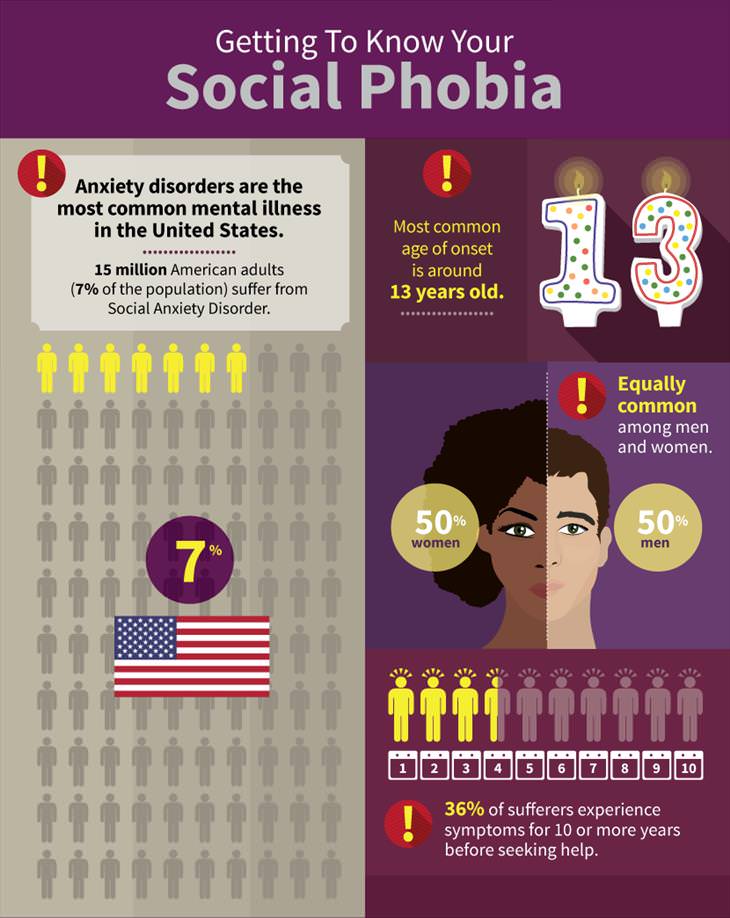 If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
Like many other mental health conditions, social anxiety disorder likely arises from a complex interaction of biological and environmental factors. Possible causes include:
- Inherited traits. Anxiety disorders tend to run in families. However, it isn't entirely clear how much of this may be due to genetics and how much is due to learned behavior.

- Brain structure. A structure in the brain called the amygdala (uh-MIG-duh-luh) may play a role in controlling the fear response. People who have an overactive amygdala may have a heightened fear response, causing increased anxiety in social situations.
- Environment. Social anxiety disorder may be a learned behavior — some people may develop significant anxiety after an unpleasant or embarrassing social situation. Also, there may be an association between social anxiety disorder and parents who either model anxious behavior in social situations or are more controlling or overprotective of their children.
Risk factors
Several factors can increase the risk of developing social anxiety disorder, including:
- Family history. You're more likely to develop social anxiety disorder if your biological parents or siblings have the condition.
- Negative experiences. Children who experience teasing, bullying, rejection, ridicule or humiliation may be more prone to social anxiety disorder.
 In addition, other negative events in life, such as family conflict, trauma or abuse, may be associated with this disorder.
In addition, other negative events in life, such as family conflict, trauma or abuse, may be associated with this disorder. - Temperament. Children who are shy, timid, withdrawn or restrained when facing new situations or people may be at greater risk.
- New social or work demands. Social anxiety disorder symptoms typically start in the teenage years, but meeting new people, giving a speech in public or making an important work presentation may trigger symptoms for the first time.
- Having an appearance or condition that draws attention. For example, facial disfigurement, stuttering or tremors due to Parkinson's disease can increase feelings of self-consciousness and may trigger social anxiety disorder in some people.
Complications
Left untreated, social anxiety disorder can control your life. Anxieties can interfere with work, school, relationships or enjoyment of life. This disorder can cause:
- Low self-esteem
- Trouble being assertive
- Negative self-talk
- Hypersensitivity to criticism
- Poor social skills
- Isolation and difficult social relationships
- Low academic and employment achievement
- Substance abuse, such as drinking too much alcohol
- Suicide or suicide attempts
Other anxiety disorders and certain other mental health disorders, particularly major depressive disorder and substance abuse problems, often occur with social anxiety disorder.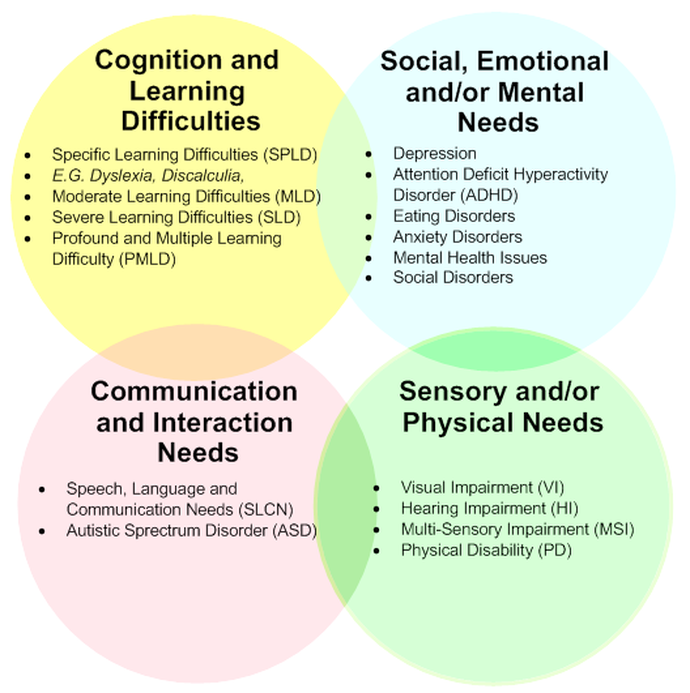
Prevention
There's no way to predict what will cause someone to develop an anxiety disorder, but you can take steps to reduce the impact of symptoms if you're anxious:
- Get help early. Anxiety, like many other mental health conditions, can be harder to treat if you wait.
- Keep a journal. Keeping track of your personal life can help you and your mental health professional identify what's causing you stress and what seems to help you feel better.
- Set priorities in your life. You can reduce anxiety by carefully managing your time and energy. Make sure that you spend time doing things you enjoy.
- Avoid unhealthy substance use. Alcohol and drug use and even caffeine or nicotine use can cause or worsen anxiety. If you're addicted to any of these substances, quitting can make you anxious. If you can't quit on your own, see your health care provider or find a treatment program or support group to help you.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Treatment of social anxiety disorder - PsyAndNeuro.ru
Social anxiety disorder (SAD) is one of the most common anxiety disorders (8-12% of the global population). It is more common in women than in men; more often in developed countries than in developing ones. STR begins at a young age (average age 12) and continues as a chronic disease. In epidemiological studies, the following factors that increase the risk of SAD have been noted: low educational level, low socioeconomic status, celibacy, and comorbid depression.
Up to 72% of patients with SAD suffer from another psychiatric disorder. The most common are depression and other anxiety disorders. Also diagnosed with SAD are anxiety disorder, body dysmorphic disorder, substance abuse, ADHD, and schizophrenia.
Here is an overview translation of the clinical guidelines for the treatment of social anxiety disorder, compiled by the experts of the Canadian Association of Anxiety Disorders. The translation was prepared jointly by the scientific Internet portal "Psychiatry & Neuroscience" and the Clinic of Psychiatry "Doctor SAN" (St. Petersburg). You can download the whole recommendation file from the link.
The translation was prepared jointly by the scientific Internet portal "Psychiatry & Neuroscience" and the Clinic of Psychiatry "Doctor SAN" (St. Petersburg). You can download the whole recommendation file from the link.
Diagnosis
SAD is characterized by a constant fear that in a social situation a person will say or do something that will cause a negative evaluation from other people. Social situations are avoided or experienced in a state of distress, while the person understands that his fear is excessive and irrational. Avoidance behavior and anxiety lead to significant functional impairment.
The DSM-IV-TR did not mention fear and avoidance associated with medical problems, but the DSM-V indicates that SAD may be secondary to physical illness. Some patients experience social anxiety due to symptoms of their illnesses (e.g. stuttering, shaking from Parkinson's disease, obesity, burn or injury marks).
DSM-5 criteria for diagnosis of pages (sociophobia)
1- Fear and anxiety about social situations in which other people can be evaluated by
2- Fear that anxiety symptoms will be negatively assessed by other people
3 - Social situation:
- Almost always provokes fear or anxiety
- Avoided or experienced with fear or anxiety
4 - Fear, anxiety or avoidance:
- Not commensurate with the actual danger of a particular social situation
- Lasts for a long time, usually more than 6 months and functional impairment
5 – If any medical condition (e.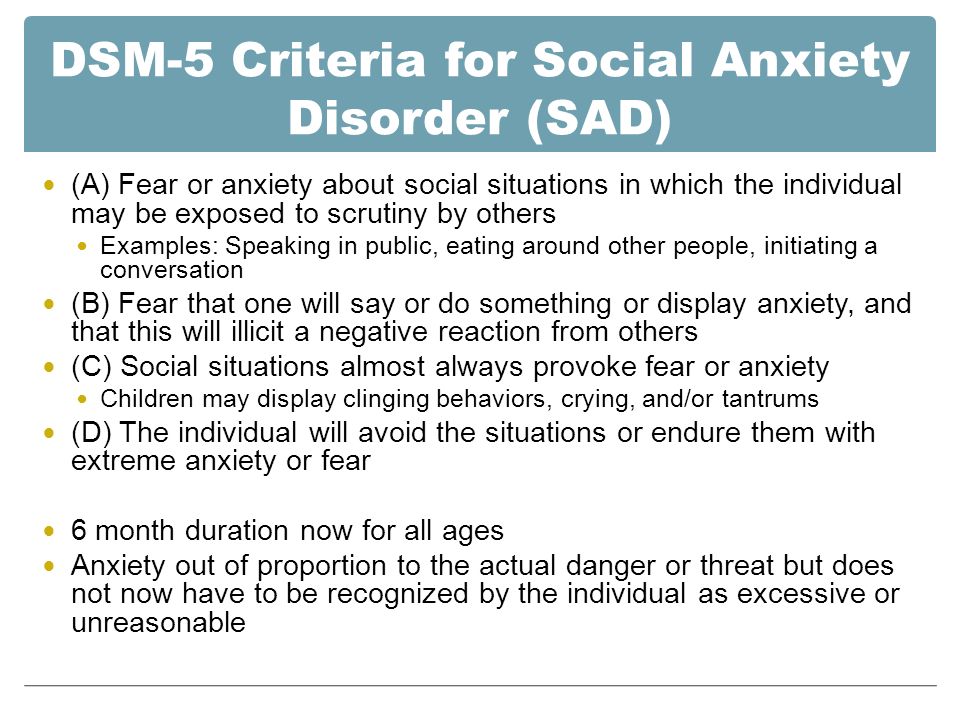 g. stuttering, obesity) is present, anxiety is not adequate to its severity
g. stuttering, obesity) is present, anxiety is not adequate to its severity
A specific type of SAD - fear associated exclusively with public speaking
Psychological support The cognitive techniques of CBT target maladaptive thoughts and attitudes, the behavioral component is usually reduced to exposure therapy. The effectiveness of CBT has been proven by many RCTs and meta-analyses. There are studies showing similar efficacy of CBT and pharmacotherapy in the treatment of acute SAD. It is reported that after completion of treatment, the improvement achieved with CBT lasts longer, compared with the results of pharmacotherapy. CBT for STR can be done individually or in a group. Although several studies favor individual psychotherapy, meta-analyses have not found a significant difference in effectiveness.
The effectiveness of CBT components has also been studied. Exposure therapy has been proven to work without the addition of other components of CBT.
CBT with an emphasis on interpersonal relationships produces the same results as standard CBT, but it also increases relationship satisfaction. The effectiveness of interpersonal psychotherapy in CBT does not have a sufficient evidence base, there are studies that say that it is ineffective. It appears to be less effective than traditional CBT.
Mindfulness-based cognitive therapy is also less effective than CBT, but still able to improve the condition in SAD.
ICBT (Internet-assisted CBT) is a new type of psychotherapy that makes CBT more accessible to patients with anxiety and mood disorders. Studies have compared ICBT and CBT (individual and group). ICBT has been shown to be effective in the treatment of STR. Most ICBT programs involve minimal contact with a psychotherapist via email or telephone. Many programs include participants communicating on Internet forums. It remains unclear whether the participation of a psychotherapist is a prerequisite for ICBT. Studies comparing psychotherapist-led ICBT and non-psychotherapist-guided ICBT provide conflicting results. All RCTs assumed that before starting ICBT, the patient had previously communicated with a psychotherapist in person or by phone and contacted him after the end of the course. Little is known about the effectiveness of self-treatment (ICBT or self-help books) that is given without prior conversation and follow-up contact with a psychotherapist.
Studies comparing psychotherapist-led ICBT and non-psychotherapist-guided ICBT provide conflicting results. All RCTs assumed that before starting ICBT, the patient had previously communicated with a psychotherapist in person or by phone and contacted him after the end of the course. Little is known about the effectiveness of self-treatment (ICBT or self-help books) that is given without prior conversation and follow-up contact with a psychotherapist.
Combination of psychotherapy and pharmacological treatment
Pharmacotherapy does not enhance the effects of CBT, although one study found that the combination of phenelzine with CBT worked better than phenelzine and CBT alone. D-cycloserine taken during exposure enhances their therapeutic effect. There is also a study proving that the combination of psychodynamic group therapy with clonazepam works better than clonazepam without psychotherapy.
Duration of effect of psychotherapy
The results achieved with CBT are noted during visits to the doctor for 6-12 months. Sustained improvement has been reported for five years after treatment. Improvement after ICBT is noted at follow-up visits one to five years after the end of treatment. The long-term effect of psychotherapy is longer than the effect of pharmacotherapy remaining after stopping treatment.
Sustained improvement has been reported for five years after treatment. Improvement after ICBT is noted at follow-up visits one to five years after the end of treatment. The long-term effect of psychotherapy is longer than the effect of pharmacotherapy remaining after stopping treatment.
Pharmacological treatment
Providence levels
1-at least 2 RCTs with a placebo control
2-at least 1 RCT with a placebo control or active control of
9000 3 3,000 3 3,000 3 – Study without control group, with at least 10 participants4 – Case reports or expert opinion
Evidence levels do not tell the nature of the result (positive, negative, questionable), they tell the quality of the analysis performed.
Recommended treatment
The first line - Processing levels 1 or 2, as well as clinically proven efficiency and safety
, second line - the level of evidence 3, as well as the clinically proven efficiency and safety
Third line - Evidence level 4 and clinically proven efficacy and safety
Not recommended - No effect with evidence level 1 or 2
First line
SSRIs, SNRIs, anticonvulsants, and benzodiazepines have been shown to be effective in treating STR.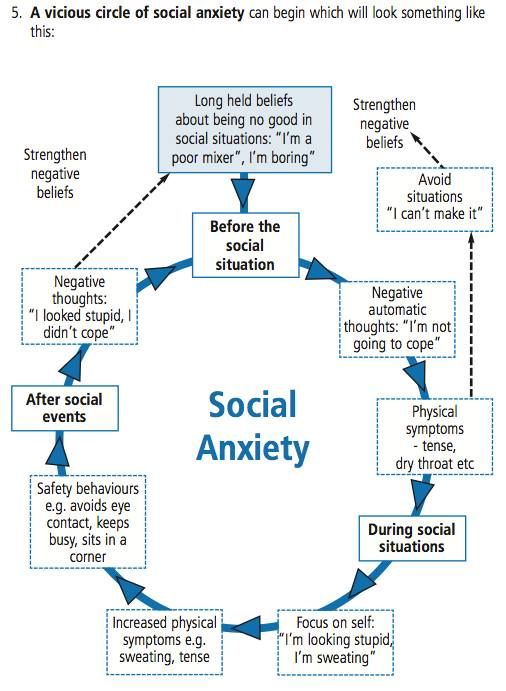 Evidence for the effectiveness of citalopram in SR is low, but it is probably as effective as other SSRIs, in contrast to fluoxetine, which has been shown to be ineffective in SR in studies and therefore can be considered the least effective SSRI.
Evidence for the effectiveness of citalopram in SR is low, but it is probably as effective as other SSRIs, in contrast to fluoxetine, which has been shown to be ineffective in SR in studies and therefore can be considered the least effective SSRI.
Pregabalin: Pregabalin is effective in the treatment of SAD at high doses (600 mg/day) but not at low doses (150-300 mg/day). Although the effectiveness of pregabalin is level 1 evidence, it is not clear how effective it is compared to that of SSRIs. In addition, the effectiveness of SSRIs has a wider spectrum in relation to typical comorbid conditions.
Second line
Benzodiazepines: Meta-analysis showed that benzodiazepines are as effective as SSRIs, but because they have little effect on typical addiction conditions and may form comorbid conditions in individuals substance abusers, benzodiazepines are recommended as second-line treatment.
Antidepressants: RCTs have shown citalopram to be as effective as moclobemide. Phenelzine has been shown to be effective, but due to dietary restrictions, drug interactions, and the risk of hypertensive crisis, it is recommended as a second-line agent. Anticonvulsants: There is (second level) evidence that gabapentin is as effective as tiagabine.
Phenelzine has been shown to be effective, but due to dietary restrictions, drug interactions, and the risk of hypertensive crisis, it is recommended as a second-line agent. Anticonvulsants: There is (second level) evidence that gabapentin is as effective as tiagabine.
Third line
Antidepressants: Fluoxetine efficacy studies are inconsistent. A large RCT showed a positive effect as strong as CBT. But two other, smaller RCTs showed no effect. Therefore, it can be assumed that fluoxetine is less effective than other SSRIs.
Same situation with moclobemide. Several RCTs showed a positive effect, a few did not. Moclobemide is more effective than CBT at the beginning of psychotherapy, but after 6 months CBT shows a stronger effect than moclobemide. Two small RCTs of mirtazapine produced conflicting results, one was effective, the other was not. Comparison of the efficacy of 60 mg/day duloxetine with 120 mg/day duloxetine showed no benefit from the higher dose.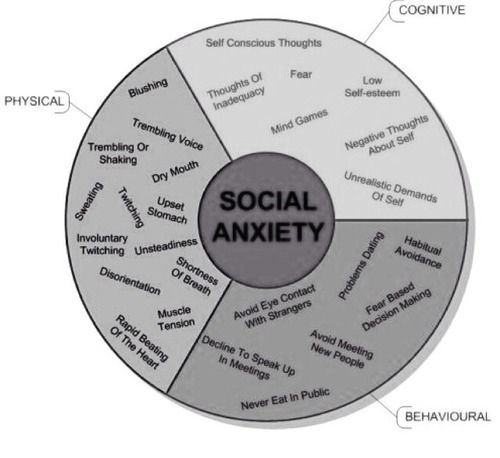
All of these drugs, as well as anticonvulsants, olanzapine, selegelin, atomoxetine, can be recommended as third-line agents for patients who have not responded to first-line and second-line drugs as monotherapy and in combination with additional drugs.
Additive drugs
The strategy of using additional drugs has been studied in patients who have not responded adequately to antidepressant treatment and can be used in cases of resistant SAD.
Preparation | Level of evidence |
| SSRI | 1 |
| Escitalopram | 1 |
| Fluvoxamine | 1 |
| Paroxetine | 1 |
| Sertraline | 1 |
| Fluoxetine | 1 (inconsistent data) |
| Citalopram | 2 |
| Paroxetine as adjunct | 3 |
| SNRI | |
| Venlafaxine | 1 |
| Duloxetine | 2 |
| TCA | |
| Clomipramine | 3 |
| Imipramine | 3 (negative) |
| IMAO and OIMAO | |
| Phenelzine | 1 |
| Moclobemide | 1 (inconsistent data) |
| Other antidepressants | |
| Mirtazapine | 1 (inconsistent data) |
| Bupropion | 3 |
| Benzodiazepines | |
| Clonazepam | 1 |
| Alprazolam | 2 |
| Bromazepam | 2 |
| Clonazepam as add-on | 2 (negative) |
| Anticonvulsants | |
| Pregabalin | 1 |
| Gabapentin | 2 |
| Levetiracetam | 2 (negative) |
| Divalproex | 3 |
| Tiagabin | 3 |
| Topiramate | 3 |
| Other drugs | |
| Atenolol | 1 (negative result) |
| Buspirone | 1 (negative result) |
| Atomoxetine | 1 (inconsistent data) |
| Propranolol | 2 (negative result) |
| Selegiline | 3 |
| Pergolide | 3 (negative) |
| Buspirone as add-on | 3 |
| Pindolol as adjuvant | 2 (negative) |
| Atypical antipsychotics | |
| Olanzapine | 2 |
| Quetiapine | 2 (negative result) |
| Aripiprazole as add-on | 3 |
| Risperidone as add-on | 3 |
| First line: Escitalopram, fluvoxamine, paroxetine, pregabalin, sertraline, venlafaxine Second line: Alprazolam, bromazepam, citalopram, clonazepam, gabapentin, phenelzine Third line: Atomoxetine, bupropion, clomipramine, divalproex, duloxetine, fluoxetine, mirtazapine, moclobemide, olanzapine, selegiline, tiagabine, topiramate Complementary drugs (third line): Aripiprazole, buspirone, paroxetine, risperidone Not recommended as adjuncts: Clonazepam, pindolol Not recommended: Atenolol*, Buspirone, Imipramine, Levetiracetam, Propranolol*, Quetiapine *Beta-blockers have been successfully used during public speaking. |
Maintenance pharmacological therapy
Meta-analysis showed that long-term use of SSRIs (3-6 months) effectively prevented relapse (relative risk = 0.39). Pregabalin has also been shown to be effective in preventing relapse. There are studies showing the effectiveness of long-term use of moclobemide in preventing relapse.
Biological and alternative therapies
Biological therapy: Neuro-Psychophysical Optimization Radioelectric Asymmetric Brain Stimulation (NPPO-REAC) protocol has been shown to be as effective as sertraline.
Alternative therapy: St. John's wort is not effective in the treatment of CRT and is not recommended for use (Evidence level 2).
Translated by: Filippov D.S.
Source: Katzman et al.: Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessivecompulsive disorders.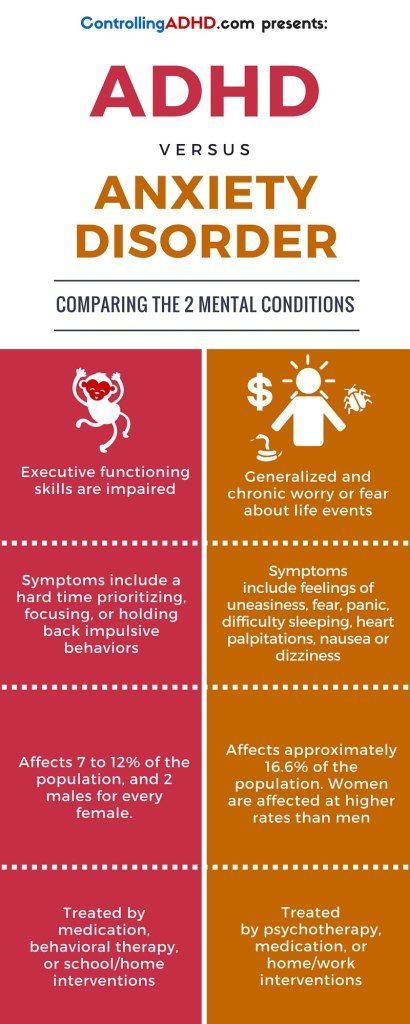 BMC Psychiatry 2014 14
BMC Psychiatry 2014 14
what is it? Types and symptoms of social anxiety disorder
Doctors Reviews
Social anxiety disorder (social phobia) is a pathological condition characterized by extreme fear arising from the condition or threat of involvement in social situations. The need to participate in such situations causes significant stress, which greatly complicates everyday life. Fear arises from apparent or actual scrutiny from others.
In a significant number of cases, social phobia begins in childhood or adolescence.
Factors that increase the likelihood of developing social anxiety disorder:
- new social environment or professional responsibilities: the need to meet new people, public speaking, etc.;
- negative life experience: if a person had experience of failure (unsuccessful performance, communication ending in conflict, public refusal or humiliation, etc.), then he may form negative expectations from any communications;
- family inheritance;
- temperament: a shy and reserved person, when faced with a new situation or with new people, may be at greater risk of developing social phobia;
- physiological deficiencies (stuttering, birthmarks, etc.
 ) - a person may be embarrassed by his appearance or think that he is not able to meet the expectations of others.
) - a person may be embarrassed by his appearance or think that he is not able to meet the expectations of others.
Social anxiety disorder is divided into two main varieties:
- Social anxiety disorder associated with situations of public activity. The difficulty is caused by the need to speak to the public (to give a speech, speak at sporting events, etc.).
- Social Anxiety Disorder Associated with Social Interactions: Anxiety triggered by situations such as talking to strangers, needing help, sitting next to strangers (e.g. at the same table in a cafe), going to public toilets, etc.
Read more
Leave a request for a consultation
and our specialist will contact you at any time convenient for you
Our doctors
Abdulova Laysan Rustamovna
Psychiatrist
Specialist experience over
2 years
Arbuzov Igor Evgenievich
Psychiatrist
Specialist experience over
8 years
Bazanova Irina Sergeevna
Psychiatrist
Specialist experience over
2 years
Zuikova Nadezhda Leonidovna
Psychotherapist
Specialist experience over
34 years
Kakadzhikova Jamal Guychgeldiyevna
Psychiatrist
Komova Alexandra Vladimirovna
Psychiatrist
Professional experience over
1 year
Korobkova Irina Grigorievna
Psychiatrist
Specialist experience over
9 years
Korobushkina Natalya Valerievna
Psychiatrist
Specialist experience over
3 years
Mikhailova Zoya Igorevna
Psychiatrist
Specialist experience over
5 years
Parshakova Ekaterina Sergeevna
Psychiatrist
Sarycheva Anna Alexandrovna
Psychiatrist
Tsyganova Anna Sergeevna
Psychiatrist
Comprehensive diagnostics
in 3 days
Diagnostic and treatment programs for anxiety, depression
and sleep disorders in our hospital
Read more>>>
Reviews
Read all reviews
Nadezhda Leonidovna thank you for being you! thanks to you, life is changing for the better, I admire in.