Withdrawing from effexor xr
Effexor Withdrawal: Symptoms & Timeline
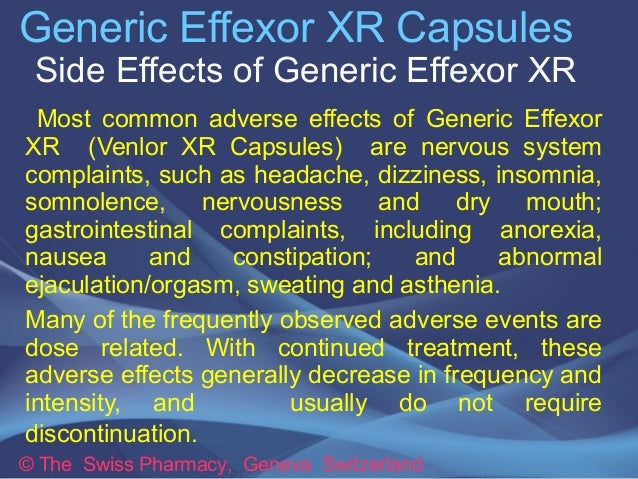
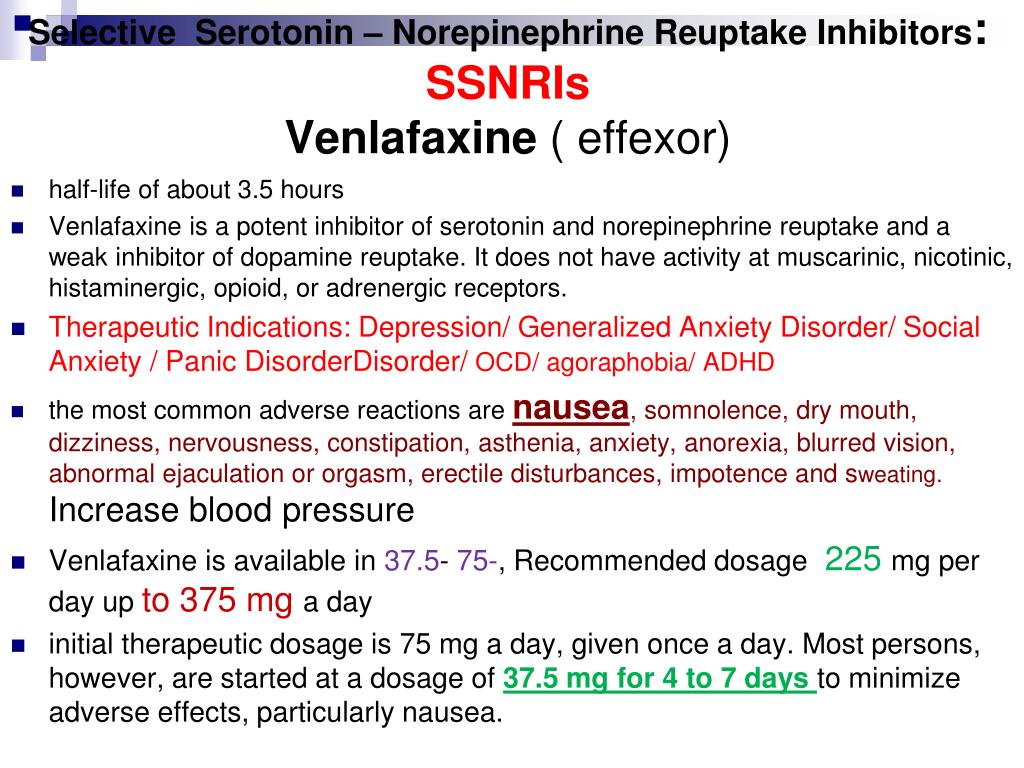
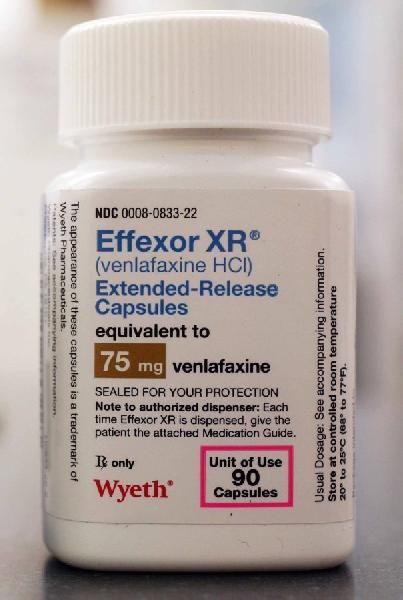
Effexor (venlafaxine) is notorious for causing uncomfortable withdrawal symptoms, known as “antidepressant discontinuation syndrome.” Effexor is generally prescribed starting at 75 mg per day, but the max dose can range from 225 mg daily to 375 mg daily, depending on the dosage form of the drug. Skipping doses of Effexor or quitting the drug cold turkey, especially at higher doses, can lead to unpleasant withdrawal symptoms. For this reason, it’s important to take Effexor exactly as your doctor prescribes.
Effexor Withdrawal
When your body becomes used to a substance, suddenly stopping it can cause withdrawal symptoms. Someone who abruptly stops taking Effexor may start to experience withdrawal symptoms 8–12 hours after the last dose. Effexor withdrawal symptoms usually resolve within two weeks.
The most reliable way to prevent or minimize withdrawal symptoms is to gradually taper the Effexor dose over a minimum of two weeks, although a longer taper may be needed. No matter what, it is important to taper Effexor under a doctor’s supervision, especially if you are taking Effexor for a mental health condition like depression. Suddenly stopping Effexor while leaving your mental health untreated may be dangerous.
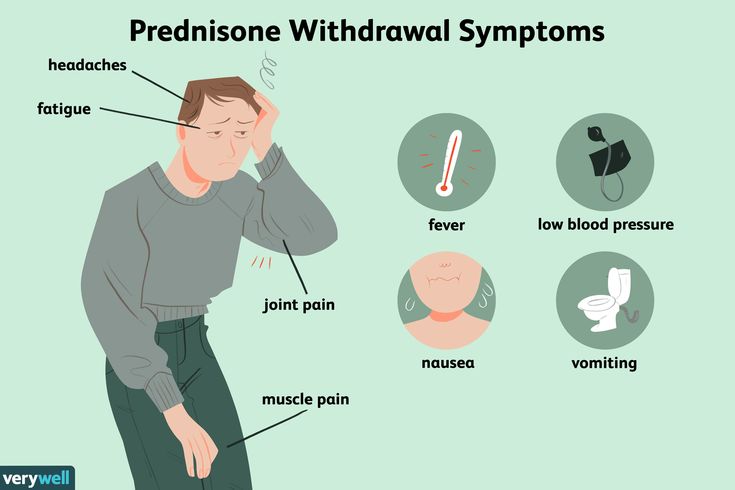
Effexor Withdrawal Symptoms
Among antidepressants, Effexor is one of the most difficult to quit. Antidepressant discontinuation syndrome (ADS) is characterized by a variety of withdrawal symptoms that occur because of physical dependence. Dependence develops with the regular use of antidepressants. Though it usually develops in six weeks or more, it can develop within just three weeks in some cases.
The presence and severity of Effexor withdrawal symptoms do not seem to be correlated with dose. Currently, it is impossible to reliably predict who will experience symptoms of ADS.
Effexor Brain Zaps
Venlafaxine has one of the highest rates of “brain zap” frequency associated with antidepressant discontinuation. Brain zaps are an electric shock sensation that may also include visual disturbances. Doctors are not sure why this phenomenon occurs. Although this symptom resolves quickly in most people, others experience brain zaps for months or years.
Brain zaps are an electric shock sensation that may also include visual disturbances. Doctors are not sure why this phenomenon occurs. Although this symptom resolves quickly in most people, others experience brain zaps for months or years.
Other Effexor Withdrawal Symptoms
Other common Effexor withdrawal symptoms can be uncomfortable or even debilitating, including:
- Vertigo
- Electric shock sensations in hands or feet
- Nausea
- Lethargy
- Flu-like symptoms
- Loss of coordination
- Anxiety
- Irritability
- Vivid dreams
- Insomnia
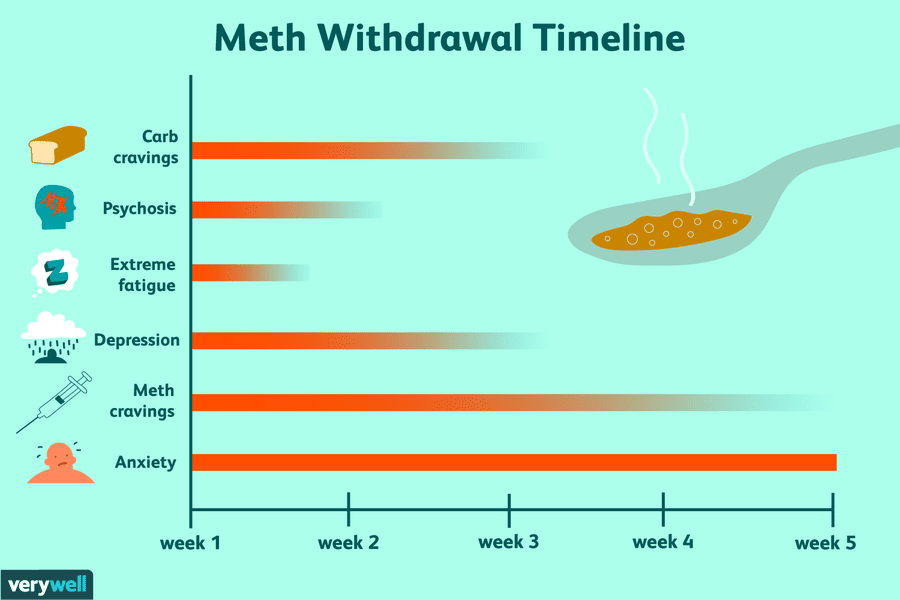
Effexor Withdrawal Timeline
The Effexor withdrawal timeline can vary. Symptoms typically begin as early as 12 hours after the last dose and generally resolve within one to two weeks. Because Effexor has a half-life of four hours, it is completely out of the system within a day. Antidepressants with longer half-lives stay in the body for longer amounts of time and may limit the onset and severity of ADS.
Factors Affecting Effexor Withdrawal
ADS typically affects about 20% of people who abruptly stop antidepressant use. However, Effexor may have a somewhat higher rate of ADS frequency — possibly up to 34%. There is currently no reliable way to predict the occurrence of ADS or its severity. Studies have even shown that higher Effexor doses are not predictive of ADS development.
A number of studies have shown that people who taper off of Effexor are significantly less likely to experience ADS, and their symptoms are milder and resolve more quickly compared to people who abruptly stop taking Effexor.
Effexor Withdrawal Treatment
The most reliable way to prevent Effexor withdrawal is to work with your doctor to develop a tapering regime. If you abruptly stop taking Effexor and are experiencing withdrawal symptoms, the only proven way to relieve them is to resume taking Effexor and gradually taper the dose with your doctor. Some studies have shown that cognitive behavioral therapy or mindfulness-based therapies can help people better manage their symptoms.
Medical Detox
Medical detox is not required for Effexor withdrawal, but people with ADS could find success in a rehab center that can help them taper off Effexor safely while providing behavioral therapy and other treatment.
People who take Effexor along with other substances may benefit from a medical detox to avoid withdrawal complications. This is especially true if you take Effexor for a mental health condition, which can worsen withdrawal symptoms.
How to Taper Off Effexor
Anyone who is considering quitting Effexor or other antidepressants should consult with a medical professional. Several studies have shown that the best way to prevent ADS and withdrawal symptoms is to gradually discontinue use.
An Effexor taper schedule may vary from person to person, but a general guideline is to reduce the Effexor dose by 10 mg every two weeks, for a minimum of four weeks. Your doctor can work with you to develop an appropriate tapering schedule that is most effective for your unique situation.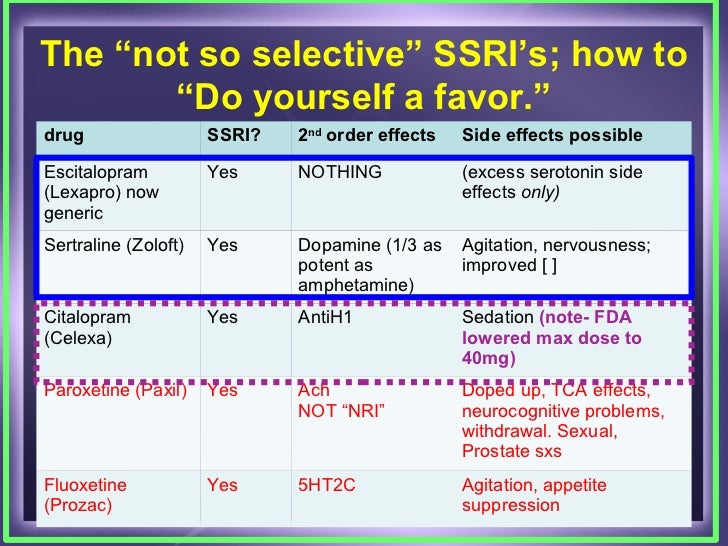
Effexor Withdrawal Remedies
There are no verified remedies for Effexor withdrawal. If you stop Effexor and start to notice withdrawal symptoms, talk to your prescriber immediately. They may be able to restart you on Effexor or another antidepressant, which can resolve your withdrawal.
In addition, it is important to focus on your health, as this may ease withdrawal symptoms. Some tips include:
- Eat a nutritious diet
- Stay well-hydrated
- Consider regular, light exercise, like yoga
- Consider therapy or counseling, especially if you were taking Effexor for a mental health condition
Alternative Treatments for Effexor Withdrawal
Cross-tapering may be an effective method to prevent or minimize Effexor ADS symptoms. Cross-tapering involves transitioning from high doses of Effexor to another antidepressant, often duloxetine, that has a similar makeup. However, there is a risk of serotonin syndrome if cross-tapering is done incorrectly. A “wash-out” period of approximately five half-lives — about 20 hours for Effexor — must be done before starting another medication that inhibits serotonin reuptake.
A “wash-out” period of approximately five half-lives — about 20 hours for Effexor — must be done before starting another medication that inhibits serotonin reuptake.
Outpatient Treatment for Effexor Withdrawal
Outpatient rehab programs that offer cognitive behavioral therapies and other forms of psychotherapy may help people experiencing Effexor withdrawal symptoms. Behavioral therapies are also likely to be incredibly beneficial for people who are concerned about experiencing a recurrence of depression or anxiety.
Detoxing From Effexor at Home
Many people who stop using Effexor, either abruptly or with a taper, do so at home. Since quitting abruptly can increase the risk of ADS, it’s essential to follow your doctor’s advice when it comes to quitting Effexor and home and managing side effects. This includes having a friend or loved one available for support, or to help identify mood changes that can come from stopping an antidepressant.
If you have severe mood swings after stopping Effexor or start thinking about harming yourself or others, seek medical attention right away. Call 911 or the National Suicide Prevention Lifeline at 1-800-273-8225. If you don’t have access to a phone, you can chat online with the hotline.
Call 911 or the National Suicide Prevention Lifeline at 1-800-273-8225. If you don’t have access to a phone, you can chat online with the hotline.
Finding a Detox Center
If you are concerned about Effexor ADS, it is advised to follow a tapering regimen under the care of medical professionals. Look for a rehab facility that has experience with tapering clients off of antidepressants and provides cognitive behavioral therapy.
If you are experiencing antidepressant withdrawal syndrome, The Recovery Village Columbus can help. Our experts will work with you to develop a tapering plan and provide cognitive behavioral therapy to help you overcome withdrawal symptoms and prevent the return of depression. Contact us today to learn about treatment programs that can work well for you.
Editor – Erica Weiman
Erica Weiman graduated from Pace University in 2014 with a master's in Publishing and has been writing and editing ever since. Read more
Medically Reviewed By – Dr. Jessica Pyhtila, PharmD
Jessica Pyhtila, PharmD
Dr. Jessica Pyhtila is a Clinical Pharmacy Specialist based in Baltimore, Maryland with practice sites in inpatient palliative care and outpatient primary care at the Department of Veteran Affairs. Read more
Drugs.com. “Venlafaxine.” October 1, 2021. Accessed March 7, 2022.
Drugs.com. “Venlafaxine ER.” September 1, 2021. Accessed March 7, 2022.
Campagne, DM. “Venlafaxine and Serious Withdrawal Sympt[…]: Warning to Drivers.” Medscape General Medicine, July 6, 2005. Accessed March 7, 2022.
Warner, CH; Bobo, W; et al. “Antidepressant Discontinuation Syndrome.” American Family Physician, August 2006. Accessed March 7, 2022.
Papp, A; Onton, JA. “Brain Zaps: An Underappreciated Symptom […]sant Discontinuation.” The Primary Care Companion for CNS Disorders, 2018. Accessed March 7, 2022.
Maund, E; Stuart, B; et al. “Managing Antidepressant Discontinuation: A Systematic Review.” Annals of Family Medicine, February 2019. Accessed March 7, 2022.
Keks, N; Hope, J; et al. “Switching and stopping antidepressants.” Australian Prescriber, June 2016. Accessed March 7, 2022.
Outhoff, K. “Switching antidepressants.” South African Family Practice, 2015. Accessed March 7, 2022.
Medical Disclaimer
The Recovery Village aims to improve the quality of life for people struggling with a substance use or mental health disorder with fact-based content about the nature of behavioral health conditions, treatment options and their related outcomes. We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare provider.
Effexor Withdrawal: Symptoms and What You Need To Know
Withdrawal doesn’t only happen if you quit smoking, give up alcohol or recreational drugs.
Some prescription medications, including the antidepressant medication Effexor, can cause a number of withdrawal symptoms if you miss a dose or abruptly stop taking it.
This isn’t a reason to avoid Effexor (the brand name of the medication venlafaxine).
However, if you use the antidepressant, follow your doctor’s instructions for taking it and, if you wish to change your dose or discontinue the medication, talk to your healthcare provider about how best to do so.
In this article, we’ll discuss what Effexor is and how it works.
Then we’ll dive into the symptoms of withdrawal and the timeline for those effects.
Lastly, we’ll share tips for coping with Effexor withdrawal.
Feeling Down?
Take our free assessment and learn about your options.
Get Started
What Is Effexor?
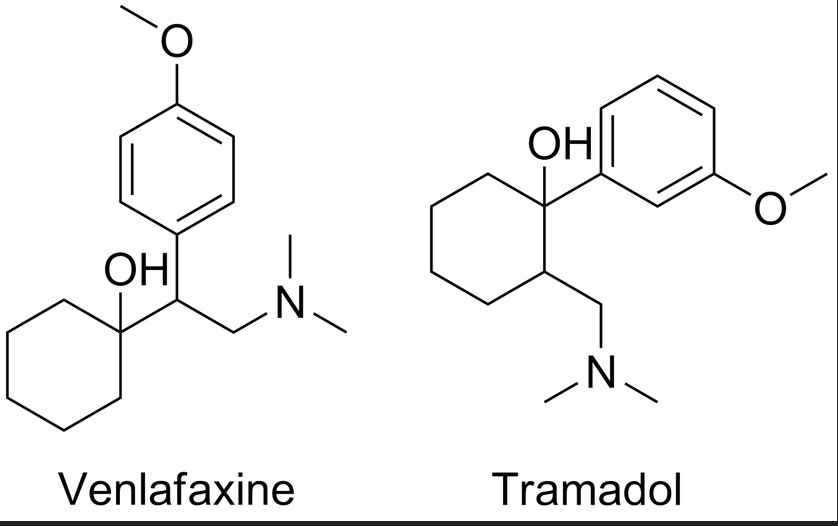
Effexor is the brand name of the antidepressant venlafaxine.
It belongs to a class of prescription drugs called serotonin-norepinephrine reuptake inhibitors (SNRIs).
Effexor is available as an immediate-release tablet or as an extended-release tablet called Effexor XR.
Effexor uses
Effexor has FDA (Food and Drug Administration) approval for the treatment of major depressive disorder (MDD), generalized anxiety disorder (GAD), panic disorder, and social anxiety disorder (sometimes called social phobia).
When appropriate, a healthcare provider may prescribe Effexor off-label to treat:
- Attention deficit disorder
- Obsessive-compulsive disorder (OCD)
- Premenstrual dysphoric disorder (PMDD)
- Post-traumatic stress disorder (PTSD
- Fibromyalgia
- Diabetic neuropathy
- Complex pain syndromes
- Hot flashes
- Migraine
How Effexor works
Although researchers are still working to understand the roots of depression and anxiety, many believe that the medical conditions are connected to the bioavailability of neurotransmitters like serotonin, dopamine, and norepinephrine.
In addition to emotional well-being, these brain chemicals affect memory, sleep function, appetite, metabolism, and other functions.
Effexor blocks how quickly your body reabsorbs serotonin, dopamine, and norepinephrine, leading to higher levels in the brain and improving mood, energy, and sleep.
Symptoms of Effexor Withdrawal
When you take any antidepressant medication, after time, your body becomes used to the resulting increased level of neurotransmitters in the brain.
So if you stop taking Effexor or any other antidepressant too quickly, it can cause a cluster of symptoms called antidepressant discontinuation syndrome.
Generally speaking, antidepressant discontinuation syndrome causes uncomfortable but not serious side effects.
Effexor withdrawal symptoms are similar to those of selective serotonin reuptake inhibitors (SSRIs) but can be notably more intense.
Symptoms include:
- Irritability
- Restlessness
- Nausea or vomiting
- Dizziness
- Nightmares
- Headache
- Confusion
- Brain zaps (a feeling of electric shocks in the brain)
- Prickly skin sensations
- Flu-like symptoms
- Sweating
- Difficulty concentrating
- Worsening anxiety or symptoms of depression
- Fatigue
Discontinuation symptoms can develop quickly.
If you forget an Effexor dose and begin to experience adverse effects, take your medicine as soon as possible (unless it’s close to the time or your next dose) or seek medical advice.
Do not drive or operate heavy machinery while you feel disoriented or have other severe symptoms.
Timeline for Effexor Withdrawal
Every person is different.
Some experience Effexor discontinuation syndrome more quickly than others: A portion of people report experiencing withdrawal symptoms in as little as 8-12 hours after their last dose.
Physical symptoms can last 3-5 days, and emotional symptoms may continue for up to 1-2 weeks.
Tips for Coping With Effexor Withdrawal
If you wish to reduce your Effexor dose or discontinue the medication entirely, talk to your doctor or medical professional.
If they give their approval, you can take action to reduce the chances of experiencing adverse effects.
Closely follow the taper dosage
Your healthcare can help you manage your withdrawal period by tapering your prescription to gently yet quickly decrease your dependence on the drug.
Follow their instructions carefully. Failure to do so can lead to uncomfortable symptoms.
Try psychotherapy
Studies show that cognitive-behavioral therapy (CBT) or mindfulness-based cognitive therapy (MBCT) may help patients quit antidepressants without increasing the risk of a relapse or new episode of depression.
Your healthcare provider may be able to refer you to therapists who are experienced in helping patients wean off of antidepressants.
Lifestyle changes
Implementing healthy lifestyle changes by getting regular physical activity, eating a healthy diet, sleeping well, and reducing stress may help you manage your mood and reduce your risk of developing symptoms of Effexor withdrawal.
Over-the-counter medications
A few OTC medications may help remedy some symptoms of antidepressant discontinuation syndrome:
- Pain relievers such as ibuprofen (Advil) and acetaminophen (Tylenol) can help manage body aches.
- Anti-nausea medication may help reduce GI discomfort.
- Sleep aids may help promote quality rest.
Keep in communication with your healthcare provider
Work with your doctor to create a discontinuation plan.
Then when you begin tapering your medication, contact them at any time if you experience withdrawal symptoms or need health advice or support.
Feeling Down?
Take our free assessment and learn about your options.
Get Started
When to See a Doctor
If you are interested in discontinuing Effexor, talk to your healthcare provider.
They can work with you to ease you off of Effexor and reduce your chances of uncomfortable side effects.
If you take Effexor and experience any unexpected symptoms—including high fever, seizure, heart palpitations, or loss of consciousness—you may have serotonin syndrome.
Call your doctor or go to the nearest hospital for medical treatment.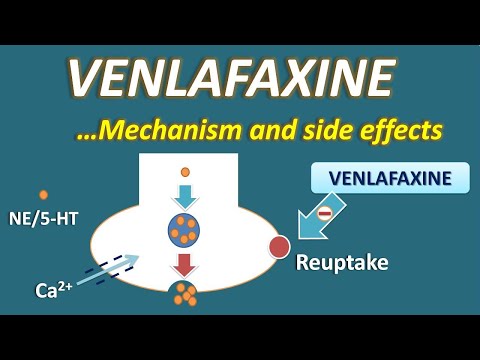
Very rarely, patients develop an allergic reaction to Effexor.
If you experience rash, tingling skin, difficulty breathing or speaking, or swelling in your face, lips, tongue, or throat, you may have a life-threatening condition called anaphylaxis.
Call 911 or go to your nearest emergency room.
How K Health Can Help
Think you might need a prescription for Effexor (Venlafaxine)?
K Health has clinicians standing by 24/7 to evaluate your symptoms and determine if Effexor is right for you.
Get started with our free assessment, which will tell you in minutes if treatment could be a good fit. If yes, we’ll connect you right to a clinician who can prescribe medication and have it shipped right to your door.
Frequently Asked Questions
How long do withdrawals last from Effexor?
While everyone is different, most people with discontinuation symptoms experience discomfort for 1–2 weeks before their symptoms fade away.
Why is Effexor withdrawal so bad?
Effexor affects brain chemistry: It increases the levels of neurotransmitters, which leads to changes in mood, appetite, and sleep. When you stop taking Effexor, your brain chemistry has to adjust. This can cause uncomfortable physical and emotional side effects.
How long does withdrawal from venlafaxine take?
Some patients report feeling the effects of withdrawal from venlafaxine (Effexor) within 8-12 hours after their last dose. Usually those symptoms last a few weeks before tapering off completely.
How do you survive Effexor withdrawal?
Effexor withdrawal is uncomfortable but not medically dangerous. If you are discontinuing your medication and feel ill, talk to your doctor. In addition to tapering your prescription slowly, they can recommend over-the-counter treatment options and lifestyle changes that can help remedy any adverse side effects of withdrawal.
If you are discontinuing your medication and feel ill, talk to your doctor. In addition to tapering your prescription slowly, they can recommend over-the-counter treatment options and lifestyle changes that can help remedy any adverse side effects of withdrawal.
K Health articles are all written and reviewed by MDs, PhDs, NPs, or PharmDs and are for informational purposes only. This information does not constitute and should not be relied on for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment.
K Health has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references.
-
Brain 5-HT Deficiency Increases Stress Vulnerability and Impairs Antidepressant Responses Following Psychosocial Stress.
 (2015).
(2015).
https://www.pnas.org/content/112/8/2557 -
The Neurobiology of Depression—Revisiting the Serotonin Hypothesis. I. Cellular and Molecular Mechanisms. (2012).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3405681/ -
Relationship of Neurotransmitters to the Symptoms of Major Depressive Disorder.
 (2008)
(2008)
https://pubmed.ncbi.nlm.nih.gov/18494537/ -
Venlafaxine. (2021).
https://www.ncbi.nlm.nih.gov/books/NBK535363/ -
Venlafaxine (Effexor).
 (2020).
(2020).
https://www.nami.org/About-Mental-Illness/Treatments/Mental-Health-Medications/Types-of-Medication/Venlafaxine-(Effexor) -
Venlafaxine and Serious Withdrawal Symptoms: Warning to Drivers. (2005).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1681629/ -
Venlafaxine Withdrawal Syndrome.
 (2011).
(2011).
https://pubmed.ncbi.nlm.nih.gov/21448114/ -
Venlafaxine XR Therapy for Major Depression and Anxiety Disorders. The Clinical Implications That Its Advantages Pose. (1999).
https://pubmed.ncbi.nlm.nih.gov/19667502/
Venlafaxine: Pediatric Medication | Memorial Sloan Kettering Cancer Center
Pediatric Medicine
Share Provided by Lexicomp ® , this document contains all the information you need to know about this medicine, including indications, directions for use, side effects, and when your healthcare provider should be contacted.
Trade names: USA
Effexor XR
Brand names: Canada
ACT Venlafaxine XR; APO-Venlafaxine XR; Auro-Venlafaxine XR; Effexor XR; M-Venlafaxine XR; PMS-Venlafaxine XR; PMSC-Venlafaxine XR; RIVA-Venlafaxine XR [DSC]; SANDOZ Venlafaxine XR; TARO-Venlafaxine XR; TEVA-Venlafaxine XR; Venlafaxine XR
Warning
- Drugs like this have increased the likelihood of suicidal thoughts or actions in children and young people. This risk may be higher in people who have tried or had suicidal thoughts in the past. All people taking this drug must be closely monitored. If you develop or worsen disorders such as depression, nervousness, anxiety, grouchiness, panic attacks, and changes in mood or behavior, contact your doctor immediately. Contact your doctor immediately if you have suicidal thoughts or suicide attempts.
- This drug is not approved for use in children. Consult your doctor.
What is this drug used for?
- Used to treat depression.
- Used to treat anxiety.
- Used to treat panic attacks.
- This drug can be given to children for other indications. Consult your doctor.
What do I need to tell the doctor BEFORE my child takes this drug?
- If your child has an allergy to this drug, any of its ingredients, other drugs, foods, or substances. Tell the doctor about the allergy and how it manifested itself in the child.
- If your child has high blood pressure.
- If your child has angle-closure glaucoma.
- If your child is taking weight loss medications.
- If your child has taken medications for depression or certain other illnesses in the last 14 days. These include isocarboxazid, phenelzine, and tranylcypromine. An episode of very high blood pressure may occur.
- If the child is receiving any of the following drugs: linezolid or methylene blue.
This list of drugs and conditions that may interact with this drug is not exhaustive.
Talk to your doctor or pharmacist about all medicines your child is taking (prescription and over-the-counter, natural, and vitamins) and any health problems. You need to make sure that this drug is safe to use for your child's illnesses and in combination with other drugs he or she is already taking. Do not start, stop taking, or change the dosage of any drug your child is taking without the doctor's approval.
What do I need to know or do while my child is taking this drug?
All forms:
- Tell all health care providers who care for your child that your child is taking this drug. These are your child's doctors, nurses, pharmacists and dentists.
- Check with your child's doctor before using marijuana, other forms of cannabis, or prescription or over-the-counter drugs that may slow your child's progress.
- Have your child avoid tasks or activities that require attention until you see how this drug works for your child. This includes cycling, playing sports, or using items such as scissors, lawn mowers, electric scooters, toy cars, or motorized vehicles.

- Treatment of a child with this drug should not be abruptly stopped without the consent of the doctor. This can increase your child's risk of side effects. Sometimes they can be severe and last for a long time. If needed, this drug should be stopped gradually for your child as directed by the doctor. Tell the doctor if your child develops new symptoms or if existing ones get worse.
- High blood pressure has happened with this drug. Monitor your child's blood pressure as directed by your doctor.
- Alcohol can interact with this drug. Make sure your child does not drink alcohol.
- This drug may increase the risk of bleeding. Sometimes bleeding can be life-threatening. Consult your doctor.
- If your child has bipolar disorder, manic episodes may occur while taking this drug. Call your doctor if your child has signs of a manic episode.
- Some patients may be at increased risk of eye problems when using this drug. Your child's doctor may order an eye examination to see if your child is at increased risk for these eye problems.
 Call the doctor right away if your child has eye pain, vision changes, swelling, or redness around the eye.
Call the doctor right away if your child has eye pain, vision changes, swelling, or redness around the eye. - This drug may cause low sodium levels in the blood. In very severe cases, it can be deadly. Consult your doctor.
- The use of this drug was accompanied by an increase in cholesterol levels. If you have any questions, please consult your doctor.
- This drug may affect the results of some lab tests. Tell all health care workers and laboratory workers who provide your child's health care that your child is taking this drug.
- In some cases, the drug may affect the growth rate in children and adolescents. They may need regular growth rate checks. Consult your doctor.
If your daughter is pregnant or breastfeeding:
- Consult physician if your daughter is pregnant, pregnant, or breastfeeding. The benefits and risks for your daughter and her baby will need to be discussed.
- Taking this drug in the middle or late pregnancy may cause some health problems for the mother or the newborn.
 Consult your doctor.
Consult your doctor.
Sustained release capsules:
- You may see particles of this drug in your child's stool. This is normal and does not cause concern.
Extended release tablets:
- The shell of the tablet can sometimes be seen in the baby's stool. This is normal and does not cause concern.
What side effects should I report to my child's doctor right away?
WARNING/CAUTION: Although rare, some people may have very serious and sometimes deadly side effects of this drug. Call your child's doctor right away or get medical help if your child has any of the following signs or symptoms that could be associated with a very bad side effect:
- Signs of an allergic reaction, such as rash, hives, itching, red and swollen skin with blisters or peeling, possibly accompanied by fever, wheezing or wheezing, tightness in the chest or throat, difficulty breathing, swallowing or speaking, unusual hoarseness, swelling in the mouth, face, lips, tongue or throat.

- Signs of low sodium levels such as headache, trouble concentrating, memory impairment, confused thinking, weakness, seizures, problems with balance.
- signs of bleeding, such as vomiting or coughing up blood; vomiting of the type of coffee grounds; blood in the urine; black, red, or tarry stools; bleeding from the gums; non-cyclic vaginal bleeding; bruises that appear or increase for no reason; bleeding that you cannot stop.
- Signs of high blood pressure, such as a very severe headache, or dizziness, or loss of consciousness, or blurred vision.
- Pain or pressure in the chest.
- Seizures.
- Dyspnea.
- Cough.
- Bone pain.
- A severe and sometimes deadly complication called serotonin syndrome can occur. This risk may be increased if the child is also taking certain other drugs. Call your child's healthcare provider right away if your child has agitation, balance problems, confusion, hallucinations, high fever, tachycardia or abnormal heart rhythm, flushing, muscle twitching or stiffness, seizures, tremors or tremors, excessive sweating, severe diarrhea, nausea or vomiting, a very severe headache.

If your child is or may be sexually active:
- Against the background of taking such drugs, violations of sexual function were noted. These included decreased interest in sex, problems achieving orgasm, problems ejaculating, or problems getting or maintaining an erection. Talk to your doctor if your child has problems with sexual function or has questions.
What are some other side effects of this drug?
Any drug can have side effects. However, for many people, side effects are either minor or non-existent. Contact your child's doctor or seek medical attention if any of these or other side effects bother your child or if they persist:
- Anxiety.
- Weight loss.
- Feeling dizzy, drowsy, tired or weak.
- Shiver.
- Headache.
- Nervous tension and agitation.
- Constipation, diarrhea, nausea, vomiting, or decreased appetite.
- Dry mouth.
- Gas formation.
- Sleep disorders.
- Excessive sweating.
- Strange or unusual dreams.
- Yawn.
This list of possible side effects is not exhaustive. If you have any questions about side effects, ask your child's doctor. Talk to your child's doctor about side effects.
You can report side effects to the National Health Board.
What is the best way to give this drug?
Give this drug to your child as directed by your doctor. Read all the information provided to you. Strictly follow all instructions.
All forms:
- Give this drug with food.
- Give this drug at the same time of day.
- Keep giving this drug as directed by your child's doctor or other health care provider, even if your child is feeling well.
Sustained release capsules:
- The child should swallow the drug whole. Do not let your child crush, chew, or dissolve the capsules or their contents.

- You can sprinkle the contents of the capsules into applesauce. Do not let your child chew the drug. Have your child swallow the medication immediately and drink it with cool water.
Extended release tablets:
- Ask your child to swallow whole. Ask your child not to chew, break, or crush the tablet.
- Give this drug with a full glass of water.
What if my child misses a dose of medication?
- Give the missed dose as soon as possible.
- If it is time for your child to take the next dose, do not take the missed dose and then go back to your child's normal schedule.
- Do not give a double dose at the same time or additional doses.
How do I store and/or discard this drug?
- Store at room temperature in a dry place. Do not store in the bathroom.
- Keep all medicines in a safe place. Keep all medicines out of the reach of children and pets.
- Dispose of unused or expired drugs.
 Do not empty into a toilet or sewer unless instructed to do so. If you have any questions about disposing of medicines, ask your pharmacist. Drug disposal programs may be in place in your area.
Do not empty into a toilet or sewer unless instructed to do so. If you have any questions about disposing of medicines, ask your pharmacist. Drug disposal programs may be in place in your area.
General information about medicines
- If your child's symptoms or health problems do not improve, or worsen, contact your child's doctor.
- Do not share your child's medicine with others and do not give anyone else's medicine to your child.
- Some medicines may come with other patient information leaflets. If you have questions about this drug, talk with your child's doctor, nurse, pharmacist, or other health care professional.
- If you think you have overdosed, call a poison control center or get medical help right away. Be prepared to tell or show what drug you took, how much, and when it happened.
Consumer Use of Information and Limitation of Liability
This summary information includes a summary of the diagnosis, treatment, and/or drug product. It is not intended to be a comprehensive source of data and should be used as a tool to help the user understand and/or evaluate potential diagnostic and treatment options. It does NOT include all information about conditions, treatments, medications, side effects, or risks that may apply to a particular patient. It should not be considered medical advice or a substitute for medical advice, diagnosis or treatment provided by a physician based on a medical examination and assessment of the patient's specific and unique circumstances. Patients should consult with their physician for full information about their health, medical issues, and treatment options, including any risks or benefits regarding the use of medications. This information is not a guarantee that a treatment or drug is safe, effective, or approved for a particular patient. UpToDate, Inc. and its subsidiaries disclaim any warranties or liabilities related to this information or its use. The use of this information is subject to the Terms of Use found at https://www.
It is not intended to be a comprehensive source of data and should be used as a tool to help the user understand and/or evaluate potential diagnostic and treatment options. It does NOT include all information about conditions, treatments, medications, side effects, or risks that may apply to a particular patient. It should not be considered medical advice or a substitute for medical advice, diagnosis or treatment provided by a physician based on a medical examination and assessment of the patient's specific and unique circumstances. Patients should consult with their physician for full information about their health, medical issues, and treatment options, including any risks or benefits regarding the use of medications. This information is not a guarantee that a treatment or drug is safe, effective, or approved for a particular patient. UpToDate, Inc. and its subsidiaries disclaim any warranties or liabilities related to this information or its use. The use of this information is subject to the Terms of Use found at https://www.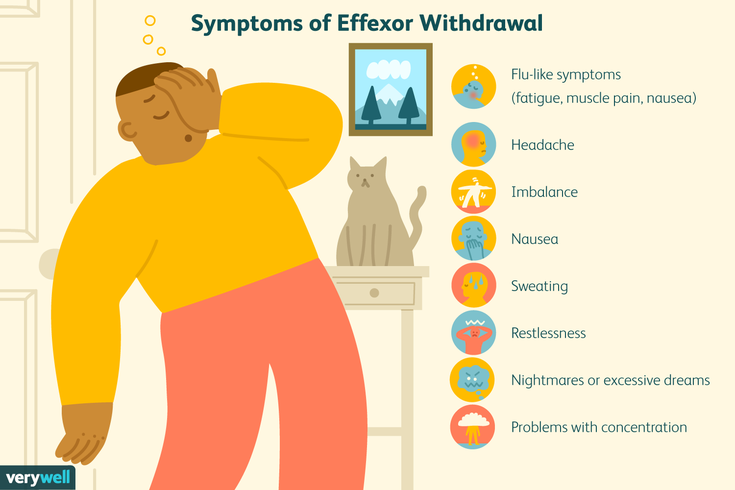 wolterskluwer.com/en/know/clinical-effectiveness-terms.
wolterskluwer.com/en/know/clinical-effectiveness-terms.
Last revision date
2022-09-01
Copyright
© UpToDate, Inc. and its affiliates and/or licensors, 2023. All rights reserved.
Date last updated
Monday, December 12, 2022
Memorial Sloan Kettering Cancer Center
Adult Medication
ShareThis document provided by Lexicomp ® , contains all the information you need about the drug, including indications, directions for use, side effects, and when you should contact your healthcare provider.
Trade names: USA
Effexor XR
Brand names: Canada
ACT Venlafaxine XR; APO-Venlafaxine XR; Auro-Venlafaxine XR; Effexor XR; M-Venlafaxine XR; PMS-Venlafaxine XR; PMSC-Venlafaxine XR; RIVA-Venlafaxine XR [DSC]; SANDOZ Venlafaxine XR; TARO-Venlafaxine XR; TEVA-Venlafaxine XR; Venlafaxine XR
Warning
- Drugs like this have increased the likelihood of suicidal thoughts or actions in children and young people.
 This risk may be higher in people who have tried or had suicidal thoughts in the past. All people taking this drug must be closely monitored. If you develop or worsen disorders such as depression, nervousness, anxiety, grouchiness, panic attacks, and changes in mood or behavior, contact your doctor immediately. Contact your doctor immediately if you have suicidal thoughts or suicide attempts.
This risk may be higher in people who have tried or had suicidal thoughts in the past. All people taking this drug must be closely monitored. If you develop or worsen disorders such as depression, nervousness, anxiety, grouchiness, panic attacks, and changes in mood or behavior, contact your doctor immediately. Contact your doctor immediately if you have suicidal thoughts or suicide attempts. - This drug is not approved for use in children. Consult your doctor.
What is this drug used for?
- Used to treat depression.
- Used to treat anxiety.
- Used to treat panic attacks.
- This drug may also be used for other indications. Consult your doctor.
What should I tell my doctor BEFORE taking this drug?
- If you have an allergy to this drug, any of its ingredients, other drugs, foods or substances. Tell your doctor about your allergies and how they have manifested.
- If you have high blood pressure.
- For narrow angle glaucoma.
- If you are taking weight loss medications.
- If you are taking any of the following drugs: linezolid or methylene blue.
- If you have taken medications for depression or Parkinson's disease in the past 14 days. These include isocarboxazid, phenelzine, tranylcypromine, selegiline, or rasagiline. An episode of very high blood pressure may occur.
This list of drugs and conditions that may interact with this drug is not exhaustive.
Tell your doctor and pharmacist about all medicines you take (prescription and over-the-counter, natural products and vitamins) and any health problems you have. You need to make sure that this drug is safe for your conditions and in combination with other drugs you are already taking. Do not start or stop taking any drug or change the dosage without your doctor's advice.
What do I need to know or do while taking this drug?
All forms:
- Tell all your health care workers that you are taking this drug.
 These are doctors, nurses, pharmacists and dentists.
These are doctors, nurses, pharmacists and dentists. - Avoid driving and other activities that require increased attention until you see how this drug affects you.
- Treatment with this drug should not be abruptly stopped without the consent of the doctor. This can increase the risk of side effects. Sometimes they can be severe and last for a long time. If necessary, this drug should be stopped gradually, as instructed by your doctor. Tell your doctor if you develop new symptoms or if existing ones worsen.
- High blood pressure has happened with this drug. Monitor your blood pressure as directed by your doctor.
- Avoid drinking alcohol while taking this drug.
- Check with your doctor before using marijuana, other forms of cannabis, or prescription or over-the-counter drugs that can slow you down.
- This drug may increase the risk of bleeding. Sometimes bleeding can be life-threatening. Consult your doctor.
- If you have bipolar disorder, manic episodes may occur while taking this drug.
 Call your doctor if you have signs of a manic episode.
Call your doctor if you have signs of a manic episode. - Some patients may be at increased risk of eye problems when using this drug. Your doctor may order an eye examination to see if you are at increased risk for these eye problems. Call your doctor right away if you have eye pain, vision changes, swelling or redness around the eye.
- This drug may cause low sodium levels in the blood. In very severe cases, it can be deadly. Consult your doctor.
- The use of this drug was accompanied by an increase in cholesterol levels. If you have any questions, please consult your doctor.
- This drug may affect the results of some lab tests. Tell all your health care workers and laboratory staff that you are taking this drug.
- If you are 65 years of age or older, use this drug with caution. You may experience more side effects.
- In some cases, the drug may affect the growth rate in children and adolescents. They may need regular growth rate checks.
 Consult your doctor.
Consult your doctor. - Tell your doctor if you are pregnant, planning to become pregnant, or breastfeeding. The benefits and risks for you and your child will need to be discussed.
- Taking this drug in the middle or late pregnancy may cause some health problems for the mother or the newborn. Consult your doctor.
Sustained release capsules:
- Particles of this drug can be observed in the feces. This is normal and does not cause concern.
Extended release tablets:
- The shell of the tablet can sometimes be seen in the stool. This is normal and does not cause concern.
What side effects should I report to my doctor immediately?
WARNING. In rare cases, this drug can cause serious and sometimes deadly side effects in some patients. Contact your doctor or seek medical attention right away if you have any of the following signs or symptoms that may be associated with serious side effects:
- Signs of an allergic reaction, such as rash, hives, itching, red and swollen skin with blisters or peeling, possibly accompanied by fever, wheezing or wheezing, tightness in the chest or throat, difficulty breathing, swallowing or speaking, unusual hoarseness, swelling in the mouth, face, lips, tongue or throat.
- Signs of low sodium levels such as headache, trouble concentrating, memory impairment, confused thinking, weakness, seizures, problems with balance.
- signs of bleeding, such as vomiting or coughing up blood; vomiting of the type of coffee grounds; blood in the urine; black, red, or tarry stools; bleeding from the gums; non-cyclic vaginal bleeding; bruises that appear or increase for no reason; bleeding that you cannot stop.
- Signs of high blood pressure, such as a very severe headache, or dizziness, or loss of consciousness, or blurred vision.
- Seizures.
- Pain or pressure in the chest.
- Dyspnea.
- Cough.
- Bone pain.
- Against the background of taking such drugs, violations of sexual function were noted. These included decreased interest in sex, problems achieving orgasm, problems ejaculating, or problems getting or maintaining an erection. If you have problems with sexual function or have questions, consult your doctor.

- A severe and sometimes deadly complication called serotonin syndrome can occur. This risk may be increased if certain other drugs are taken at the same time. Call your doctor right away if you experience agitation, balance problems, confusion, hallucinations, high fever, tachycardia or abnormal heart rhythms, flushing, muscle twitching or stiffness, seizures, tremors or tremors, excessive sweating, severe diarrhea, nausea or vomiting , a very severe headache.
What are some other side effects of this drug?
Any medicine can have side effects. However, for many people, side effects are either minor or non-existent. Contact your doctor or seek medical attention if these or any other side effects bother you or do not go away:
- Sleep disorders.
- Nervous tension and agitation.
- Anxiety.
- Weight loss.
- Feeling dizzy, drowsy, tired or weak.
- Shiver.
- Headache.
- Excessive sweating.
- Constipation, diarrhea, abdominal pain, nausea, vomiting, or decreased appetite.
- Gas formation.
- Dry mouth.
- Strange or unusual dreams.
- Yawn.
This list of possible side effects is not exhaustive. If you have any questions about side effects, please contact your doctor. Talk to your doctor about side effects.
You can report side effects to the National Health Board.
You can report side effects to the FDA at 1-800-332-1088. You can also report side effects at https://www.fda.gov/medwatch.
What is the best way to take this drug?
Use this drug as directed by your doctor. Read all the information provided to you. Strictly follow all instructions.
All editions:
- Take this drug with food.
- Take this drug at about the same time of day.
- Keep taking this drug as instructed by your doctor or other health care professional, even if you feel well.
Sustained release capsules:
- Swallow whole. Do not crush, chew, or dissolve the capsules or their contents.
- You can sprinkle the contents of the capsule into applesauce. Do not chew. Swallow immediately and drink cool water.
Extended release tablets:
- Swallow whole. Do not chew, break or crush.
- Take this drug with a full glass of water.
What if I miss a dose of a drug?
- Take the missed dose as soon as you can.
- If it's time for your next dose, don't take the missed dose and then go back to your regular dosing schedule.
- Do not take 2 doses or an additional dose at the same time.
How do I store and/or discard this drug?
- Store at room temperature in a dry place. Do not store in the bathroom.
- Keep all medicines in a safe place. Keep all medicines out of the reach of children and pets.
- Dispose of unused or expired drugs.
Do not empty into a toilet or sewer unless instructed to do so. If you have any questions about disposing of medicines, ask your pharmacist. Drug disposal programs may be in place in your area.
General information about medicines
- If your health does not improve or even worsens, see your doctor.
- Do not give your medicine to anyone and do not take other people's medicines.
- Some medicines may come with other patient information leaflets. If you have questions about this drug, talk with your doctor, nurse, pharmacist, or other health care professional.
- A separate instruction for patients is attached to the drug. Please read this information carefully. Reread it each time you refill your supply. If you have any questions about this drug, ask your doctor, pharmacist, or other health care professional.
- If you think you have overdosed, call a poison control center or get medical help right away. Be prepared to tell or show what drug you took, how much, and when it happened.
Consumer Use of Information and Limitation of Liability
This summary information includes a summary of the diagnosis, treatment, and/or drug product. It is not intended to be a comprehensive source of data and should be used as a tool to help the user understand and/or evaluate potential diagnostic and treatment options. It does NOT include all information about conditions, treatments, medications, side effects, or risks that may apply to a particular patient. It should not be considered medical advice or a substitute for medical advice, diagnosis or treatment provided by a physician based on a medical examination and assessment of the patient's specific and unique circumstances. Patients should consult with their physician for full information about their health, medical issues, and treatment options, including any risks or benefits regarding the use of medications. This information is not a guarantee that a treatment or drug is safe, effective, or approved for a particular patient.